
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 12 September 2023
Sec. Neuropsychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1243655
This article is part of the Research TopicCurrent Trends on Emotional Processing: Contributions of Acquired Brain Injury, Neurodegenerative Diseases, and AgeingView all 5 articles
 Vasudeva Murthy Challakere Ramaswamy1
Vasudeva Murthy Challakere Ramaswamy1 Tony Butler2
Tony Butler2 Bianca Ton2
Bianca Ton2 Kay Wilhelm2
Kay Wilhelm2 Philip B. Mitchell2
Philip B. Mitchell2 Lee Knight2
Lee Knight2 David Greenberg2,3
David Greenberg2,3 Andrew Ellis2,3
Andrew Ellis2,3 Stephen Allnutt2
Stephen Allnutt2 Jocelyn Jones4
Jocelyn Jones4 Val Gebski5
Val Gebski5 Vaughan Carr2,6
Vaughan Carr2,6 Rodney J. Scott1
Rodney J. Scott1 Peter William Schofield1,7*
Peter William Schofield1,7*Background: Traumatic brain injury (TBI) is a major public health problem that may be associated with numerous behavioral problems, including impulsivity, aggression and violence. Rates of self-reported TBI are high within offender populations, but the extent to which TBI is causally implicated in causing illegal behavior is unclear. This study examined the psychological and functional correlates of histories of traumatic brain injury in a sample of impulsive violent offenders.
Methods: Study participants, all men, had been recruited to participate in a randomized controlled trial of sertraline to reduce recidivism. Study entry criteria were an age of at least 18 years, a documented history of two or more violent offenses and a score of 70 or above on the Barratt Impulsiveness Scale. An extensive list of standardized questionnaires was administered to obtain information on previous TBI and other neuropsychiatric conditions or symptoms.
Results: In the sample of 693 men, 66% were aged between 18 and 35 years old, and 55% gave a history of TBI (“TBI+”). Overall, 55% of study participants reported at least one TBI. High levels of neuropsychiatric symptomatology were reported. In 75% of TBI+ individuals, their most severe TBI (by self-report) was associated with loss of consciousness (LOC) < 30 min. Compared to TBI- (those without history of TBI) participants, TBI+ individuals were more impulsive (Eysenck Impulsivity), irritable, angry, and reported higher levels of assaultive behavior, depressive symptomology, alcohol use disorder, suicidal ideation, suicide attempts, and lower quality of life. Potential “dose effects” of TBI severity and frequency in terms of neuropsychiatric symptomatology were identified.
Conclusion: Like other studies of offender populations, single and multiple TBIs were very common. The associations of TBI, TBI severity, and TBI frequency (i.e., TBI “burden”) with adverse neuropsychiatric phenomena suggest TBI contributes importantly to offender morbidity but the select nature of the sample and cross-sectional study design constrain the interpretation of these findings.
Violence, defined as “the intentional, threatened or actual, use of physical force or power, against oneself, another person, or a group or community, that either results in, or has a high probability of resulting in, injury, death, psychological harm, maldevelopment or deprivation” accounts for many millions of deaths world-wide annually, and is a major public health problem (Krug et al., 2002; Abubakar et al., 2015).
A history of TBI has been identified as one of many risk factors for violence and, conversely, TBI might arise as a consequence of violent behavior (Morrell et al., 1998; Slaughter et al., 2003; Schofield et al., 2006a). TBI is common in offender populations and, among individuals who have committed violent crimes (Fazel et al., 2011), and significantly exceeds rates in the general, non-offender population (Schofield et al., 2014).
The extent to which TBI might operate as a risk factor for violence or criminality remains unclear. Longitudinal and linkage studies, where the temporality of TBI can be established (i.e., that it precedes offending) have suggested an up to a two-fold increase in the risk of offending outcomes, but such studies generally lack any proxy measure for pre TBI behavioral characteristics that might represent a confound (Shiroma et al., 2010; Elbogen et al., 2015; Schofield et al., 2015; Ray and Richardson, 2017).
Specifically, the trait of impulsivity or poor self-control, is typically established early in life, and might explain an apparent association of TBI with offending, given that this trait increases the risk of both outcomes (Romer, 2010; Kocka and Gagnon, 2014). Lack of high quality, or indeed any, index of TBI severity often represents a limitation in studies of TBI in offender populations. What data are available are generally based on self-report, in large non-selected samples of offenders the report of TBI impact is mild, findings that might serve to cast doubt, in those instances (i.e., of mild TBI), on a likely causal association of TBI with subsequent offending.
In the present study, we had the opportunity to examine self-reported data on past TBI, neuropsychiatric symptoms and conditions and indices of impulsivity in a sample of impulsive individuals who had previously been found guilty of violent offenses. These data comprise baseline information from a larger randomized controlled trial of sertraline designed to determine whether that medication might reduce repeat offending (Butler et al., 2021). We used these data to examine associations between the presence and severity of TBI and various neuropsychiatric characteristics, seeking to determine the extent to which, in this sample of violent offenders, those with past TBI differed from those without such a history and whether “dose effects” related to frequency or severity of TBI related to subjective neuropsychiatric phenomena.
Study participants were all men who met the criteria for randomization in the ReINVEST study (Butler et al., 2021). That study enrolled men who were at least 18 years old and had a prior conviction or were charged (with or without imprisonment) for 2 or more violent offenses (e.g., manslaughter, robbery, assault) and scored 70 or higher on the Barratt Impulsiveness Scale (Barratt et al., 1995) Other requirements were that participants were able to communicate in English, were medically fit and could give informed consent (Butler et al., 2021). Participants with active major mental illness (major depression or psychosis/schizophrenia) were deemed ineligible for participation.
Participants were asked to complete the medical history questionnaire which included the following questions about past episodes of TBI; “Have you ever had a head injury where you passed out or had a ‘blackout’?” and “How often have you experienced a head injury?” Up to five separate episodes of traumatic brain injury were recorded and participants were asked to report the TBI in order of severity. The first reported TBI was the most severe. The traumatic brain injury questionnaire included the following questions: How long were you unconscious (blackout)? When did this happen? Additional information included whether they suffered a skull fracture or bleeding on the head or surgical procedure on the head?
If the participant suffered multiple TBIs, they were instructed to provide information related to their most severe form of TBI under the first episode of TBI, followed by other episodes of TBIs. The burden of TBI was determined in this study based on LOC, the number of TBIs and duration since the severe TBI.
Demographic data was collected relating to age, gender, ethnicity, marital status, children, education, employment, and accommodation.
Baseline assessments included administration of the Barratt Impulsiveness Scale (BIS-11) and the Eysenck Impulsivity Questionnaire (EIQ) providing information on state and trait indices of aspects of impulsive behavior. The Anger Irritability and Aggression Questionnaire (AIAQ) was used to measure the subjective level of anger and aggression in recent weeks and the State Trait Anger Expression Inventory (STAXI-2) was used to measure the subjective level of anger in different situations. The Beck Depression Inventory-II (BDI-II) examined symptoms in the past week potentially indicative of a mood disorder. The Alcohol Use Disorders Identification Test (AUDIT) measured alcohol consumption in the 12 months prior to incarceration. AUDIT identified safe, harmful and hazardous levels of alcohol consumption. The Kessler Psychological Distress Scale (K-10) is a 10-item questionnaire that provides a global measure of distress based on questions about anxiety and depressive symptoms in the past 4 weeks. The International Personality Disorder Examination (IPDE) was used to categorize participants as having Impulsive Personality Disorder, Dissocial Personality Disorder and Borderline Personality Disorder. As a measure of reading ability, Wechsler Individual Achievement Test Score was collected. In addition, details of substance use and abuse were collected and psychiatric assessment recorded information on suicide attempts, self-harm and sexual abuse as part of the routine reception interview.
The Duke Social Support Scale provided information on social interaction and the Quality-of-Life Short Form Questionnaire (SF-12) assessed health-related quality of life.
Descriptive statistics were used to describe the sample characteristics, presence of TBI, self-reported duration of any LOC, time of occurrence, the severity of the head injury, symptoms following head injury, and overall response distribution of the psychological and functional measures. Hosmer-Lemeshow goodness of fit test based on chi-square formulation was used to investigate the association of the presence of TBI with sample characteristics, personality disorder, psychiatric assessment, and substance abuse. This procedure was repeated on different study outcomes including duration of LOC, time of occurrence, and duration of LOC among participants who reported only one episode of TBI. Fisher’s exact test was used when the expected count assumption of the chi-square test was not achieved. Meanwhile, One-way ANOVA (equal variance not assumed) was performed to investigate the study outcome with continuous numerical covariates including demographic characteristics, and psychological and functional measures. Pairwise comparison test using the Bonferroni method was applied where one-way ANOVA is significant in more than 2 groups. All statistical procedures were two-sided and computed on R4.3.3. All results are interpreted at the 5% significance level.
Data cleaning procedure was employed prior to data analysis. Out of 935 participants, 244 participants with incomplete data were removed. The 244 participants were missing mostly TBI history, AUDIT, AIAQ, STAXI-2, substance abuse, SF-12, Duke and demographic data. A total of 693 individuals with complete data were used for the analyses. Table 1 shows the socio-demographic characteristics of the sample of impulsive violent offenders. About 66% of the study participants were between 18 and 35 years old. The majority of them were of non-Aboriginal descent (85%), and 86% lived with their parents, partners or relatives at the time of recruitment. Half of them had never married and 41% had been unemployed for at least 6 months. On average, the number of different schools before dropping out was 4.42 (SD = 3.46). One third had left school without completing a high school qualification. Three quarters (75%) had been suspended from school and 40% had been expelled.
As indicated in Table 2, 55% of study participants reported at least one TBI. Table 2 shows that the majority of episodes of LOC after traumatic brain injury lasted only a brief moment (63%) and this trend was also seen in participants with single episode of TBI (TBI 1) (62%), two episodes of TBI (TBI 2) (65%) and three episodes of TBI (TBI 3) (74%). In 75% of all TBI+ individuals, the most severe TBI was associated with LOC < 30 min, consistent with mild TBI, about half of the TBIs occurred more than 10 years ago and 11% of them were associated with skull fractures. One fifth (20%) of participants reported “weakness” in some part of their body after TBI.
Univariate analysis showed significant associations between any TBI with LOC and employment, accommodation, and suspension from school. The number of TBI cases was significantly higher among those who had been unemployed in the last 6 months (45%, p = 0.027) and who lived with their partner (32%, p = 0.006) or with relatives (31%, p = 0.006) and they had had higher school suspensions (79%, p = 0.02) than those without TBI.
Table 3 shows the psychological and functional factors in relation to the presence or absence of any reported past history of TBI. Univariate analyses revealed that TBI was significantly associated with higher scores for impulsivity, irritability, anger lability, direct assault, depression score, anger expression-out, anger expression-in, alcohol use disorder, suicidal ideation, and suicidal attempt. TBI was also significantly associated with lower quality of life score in terms of physical health and mental health according to the SF-12. Overall substance abuse (former and current) was not significant but when all the individual drugs were analyzed, former Methyl enedioxy methamphetamine (MDMA) substance abuse was significantly higher in those with TBI (p = 0.037).
In Table 4, we compared groups defined by the reported severity (duration of LOC) among those who reported only a single TBI. The only significant differences were that those with LOC >30 min (mean = 50.76) scored lower on the quality-of-life physical health score and on the Duke Social support scale than those with LOC <30 min (Table 4).
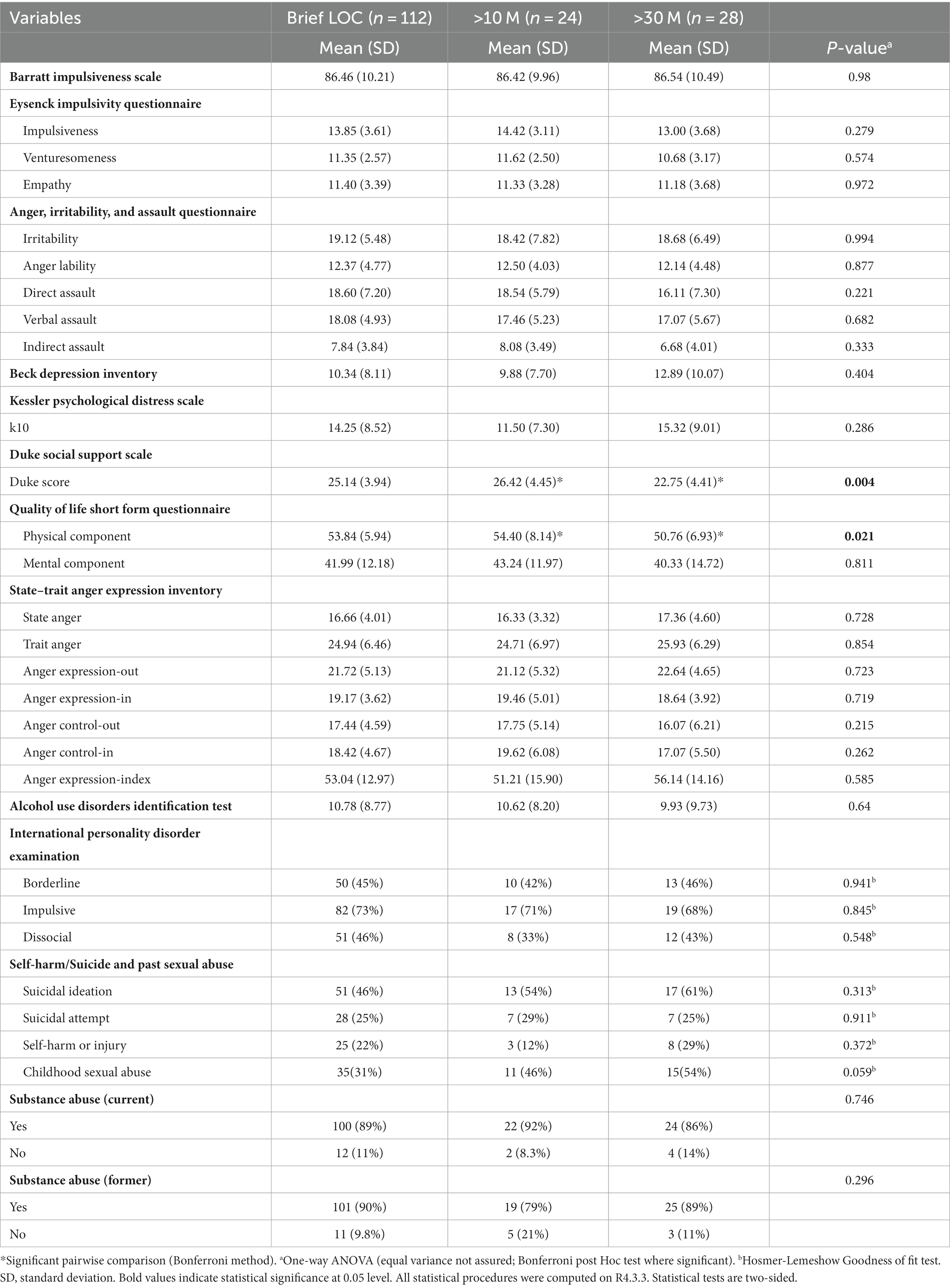
Table 4. Participant psychological and functional measures by severity of brain injury based on people LOC (minutes) and people who had only one episode of TBI.
We then sought further evidence for possible “dose effects” of TBI by comparing groups defined by reported numbers of TBIs (1, 2, >2) (Table 5). Here, there were more differences. For the most part, the characteristics of those who reported only one TBI were similar to those reporting 2 TBIs, while those reporting >2 TBIs differed with respect to the less frequent categories in more ways. Thus, the number of TBIs was significantly, positively associated with impulsiveness (Barratt), level of depression, psychological distress, alcohol use disorder (AUDIT), dissocial personality, suicidal ideation and suicidal attempt, and inversely with social support and quality of life. Substance abuse overall (former and current) was not significant, but when analyzing all individual drugs, current cannabis abuse was significantly higher among those >2TBI (50%, p = 0.026).
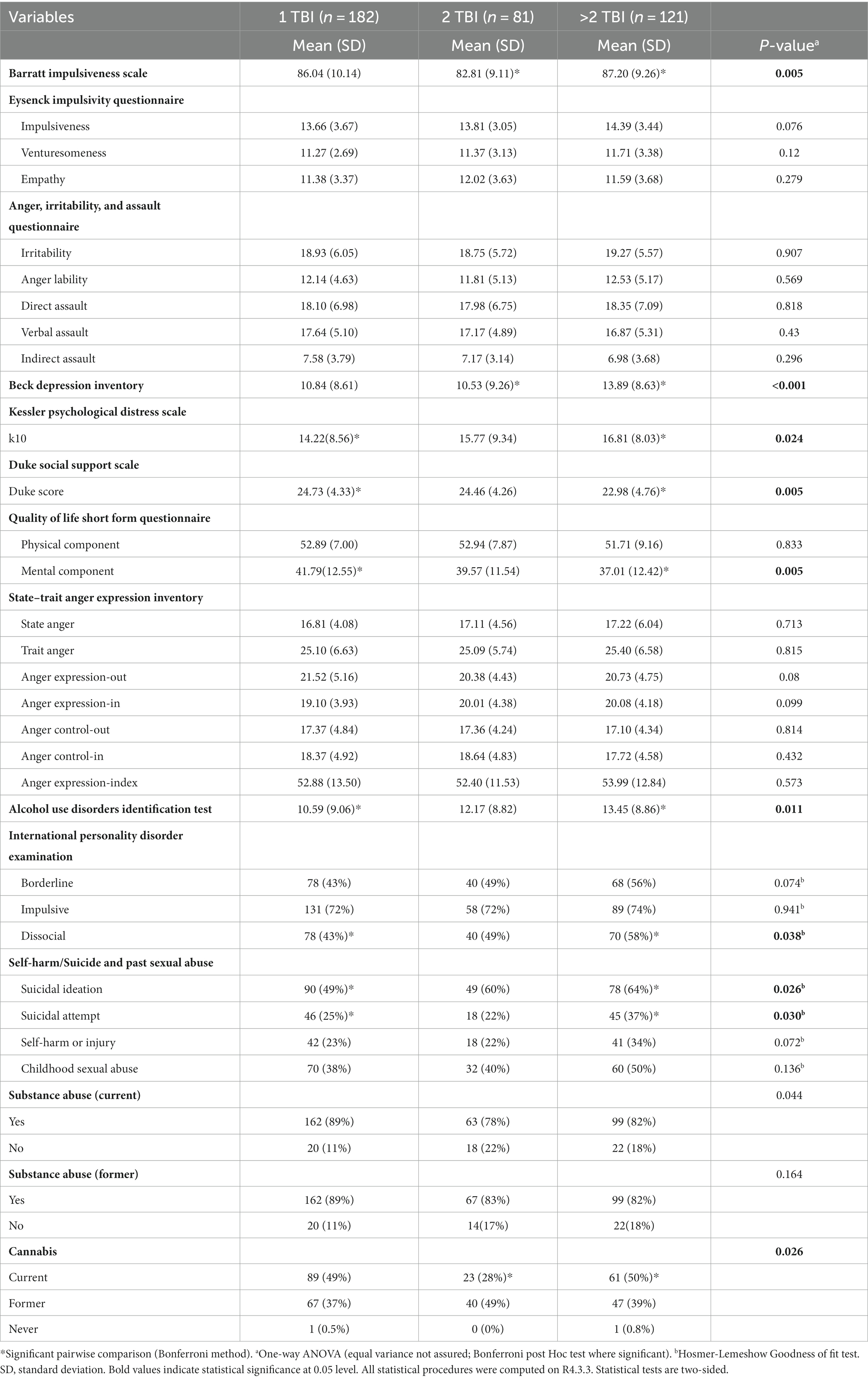
Table 5. Participant psychological and functional measures by severity of head injury based on Number of TBI.
We then compared TBI- participants with TBI+ participants who reported a history of a single mild TBI. In univariate analyses (Table 6), those with mild TBI had significantly higher scores than those with no TBI on scales of direct assault (mean = 18.60, p = 0.006), verbal assault (mean = 18.08, p = 0.008), indirect assault (mean = 7.84, p = 0.009), anger expression-out (mean = 21.72, p < 0.001), and anger expression-index (mean = 53.04, p = 0.043). Furthermore, relative to TBI-, those with a single mild TBI included a significantly higher proportion of current (89%, p = 0.022) and former (90%, p = 0.024) substance abusers.
In this sample of highly selected, impulsive and violent men, 55% reported a history of at least one TBI associated with some alteration of consciousness, a prevalence consistent with rates found in prisoner populations in the literature (Farrer and Hedges, 2011; Shiroma et al., 2012; Durand et al., 2017). Although the majority of TBIs in our sample were, on the basis of duration of self-reported LOC, mild, a considerable number were potentially associated with complications (skull fracture and “body weakness,” albeit transient). Further, in terms of the “dose” of TBI within this sample, 47% of those with any TBI reported only one, 21% reported two TBIs and the remaining 31% reported three or more TBIs. Again, this aligns with the results of other previous studies in prison/offender populations which indicate that a history of multiple TBIs is far from uncommon (Barnfield and Leathem, 1998; Slaughter et al., 2003; Schofield et al., 2006a,b).
TBI aside, neuropsychiatric conditions are highly prevalent in offender populations, and the current sample is no exception. Based upon the International Personality Disorder Examination, impulsive personality disorder was present in over 70% of the sample, likely a reflection of their offending history and the recruitment criteria requiring a threshold (high) score on the Barratt Impulsiveness Scale for inclusion. Borderline (47%) and dissocial (46%) personality disorders were also extremely common. Reflective of early life disadvantage, a history of sexual abuse was highly prevalent as were high rates of past suicidal ideation, self-harm or suicidal attempts. Such findings are particularly notable in light of the exclusionary criteria such that individuals with active major mental illness were not recruited into the ReINVEST study (Butler et al., 2021). High levels of anger and distress, and current and past substance abuse were other notable findings.
There is a growing literature relating to TBI within offender populations and the possible etiological/causal role of TBI for offending and the special needs/challenges that prisoners with a history of TBI might present. This is important as some of their behaviors (including impulsivity), may reflect neuropsychiatric sequelae of TBI. Cross sectional studies are inherently limited with respect to establishing causal relationships, but they may nevertheless yield interesting results of relevance to this issue. In a previous study by our group, we collected “control” data by telephone interview to supplement previously-collected data from recent prison entrants (Schofield et al., 2006b; Perkes et al., 2011). Past TBI history and some simple behavioral data, including questionnaire-derived estimates of impulsivity, were obtained from both samples. The control group (non-offending men) was purposefully recruited from the same regions of residence as the pre-incarceration residences of the offenders (also all male). Surprisingly, 82% of prisoners and 71.5% of community participants reported at least one past TBI of any severity (prevalence not significantly different) while levels of impulsivity were profoundly lower (p < 0.001) in the community non-offending sample (Perkes et al., 2011). When the history of any TBI with LOC was compared (64.5% of prisoners and 32.2%) the difference was significant but still far less so than the difference in impulsivity scores, which were comparably high among prisoners with and without past TBI history. Such findings speak to the complexity of the TBI-offending association (including the importance of severity of TBI when exploring its potential role in offending), the potential high relevance of impulsivity for offending and the relevance of socioeconomic status for TBI prevalence (i.e., given the very high rates in the control sample).
The present study shares certain features with our earlier (Perkes et al., 2011) study described above, but there are also important differences. The present offending sample was highly select (previously violent and impulsive) and, also by contrast with the earlier study, we did not recruit a separate control sample. Thus, for the present study, we were interested in the “burden” of neuropsychiatric morbidity and the association of these with self-reported TBIs in our sample who were at high risk of reoffending due to their impulsivity and past history of violent offending. While the present analyses do not directly contribute to the literature that seeks to clarify the extent to which TBI plays a role in the offending cycle, they do set the scene for reflections on the current status of that issue, in light of recent data from other studies, discussed below.
On the question of causation, the relevant studies that are most methodologically sound are longitudinal, often linkage, studies in which the temporal sequence of TBI exposure and the offending outcome can be more or less assured (Timonen et al., 2002; Fazel et al., 2011; Schofield et al., 2015). Typically, however, such studies lack data on TBI severity or any proxy for pre-injury behavioral characteristics. Both of these issues are of some relevance to the plausibility of TBI playing a causal role in the commission of an offense. Several large record linkage studies have adduced evidence suggesting that TBI constitutes a risk factor for offending, and a longitudinal birth cohort study in which adjustment was made for preinjury early behavior problems obtained similar findings (Timonen et al., 2002; Fazel et al., 2011; McKinlay et al., 2014; Schofield et al., 2015). However, studies in which a control cohort comprised individuals who sustained non-TBI injuries found no heightened risk for offending among those with TBI, relative to that control group (Kennedy et al., 2017; Bonow et al., 2019). That provocative finding raised the possibility that (preinjury) impulsivity or risk-taking behavior (such as might increase risk for any injury) might represent a confound. Seen in this light, the occurrence of a mild TBI might constitute a proxy for risk taking or impulsivity that represents the actual underlying risk factor for offending behavior. The plausibility of the hypothesis that mild TBI may be causally implicated in offending depends on the nature of the neuropsychiatric consequences of TBI that might be anticipated, either following a single event or when multiple instances occur.
It has been long recognized that multiple TBIs, even when classified as mild TBI, can have cumulative deleterious effects (Gronwall and Wrightson, 1975; Carlsson et al., 1987). There is increasing concern about repetitive TBI in contact sports athletes (Mayer et al., 2017) being associated with symptoms of depression, anxiety and cognitive impairment (Bailes et al., 2014) or, more controversially, chronic traumatic encephalopathy (Geddes et al., 1999; Omalu et al., 2005; McKee et al., 2009; Gavett et al., 2011; Russo et al., 2023), associated with symptoms of depression, impulsivity, aggression and increased suicidality (McKee et al., 2009, 2013). TBI sequelae such as post-traumatic stress disorder (PTSD), depression and generalized anxiety disorder are associated with overactivity of the underlying neural circuits and increased risk of impulsive aggression (Mattson, 2003). PTSD is a debilitating condition characterized by symptoms such as avoidance behavior, hyperarousal and intrusive memories but may also be associated with antisocial behaviors such as aggression, anger, impulsivity and suicidal tendencies (Dileo et al., 2008).
In our study, there were significant differences between groups defined by the number of reported TBIs (1, 2, >2), consistent with possible “dose effects” with respect to Beck Depression Inventory, psychological distress, quality of life, suicide ideation and suicidal attempts. The >2 TBIs category also had lower social supports, and were most impulsive of the three categories of TBI frequency without an obvious gradient of effect. That the >2 TBIs group reported greater substance abuse, including alcohol, may perhaps reflect consequences rather than causes of those exposures, recognizing that all of the above is necessarily speculative.
It has become increasingly apparent that a single mild TBI may be complicated by long-term physical, cognitive, and emotional consequences which may include an increase in aggression and impulsivity. When considering the effects of a single mild TBI, it is important to note that the definition encompasses a considerable spectrum of severity, e.g., from transient alterations in awareness to LOC lasting up to 30 min on one clinical measure (McKinlay et al., 2016; McInnes et al., 2017; Mosti and Coccaro, 2018).
Results from recent large cohort studies with pre-injury assessments have substantially contributed to our knowledge of complications by reporting actual change scores associated with the TBI, meaning that post TBI symptoms cannot be solely attributable to pre-injury characteristics. The Project on Human Development in Chicago Neighborhoods study involved a longitudinal assessment of 1,827 adolescents with serial assessments (Connolly and McCormick, 2019). Multivariate analyses were conducted to investigate the relationship between mild TBI and a range of important symptoms and, importantly, investigators were able to measure changes in key indices of neuropsychiatric functioning associated with a new mild TBI while adjusting for preexisting, previously measured, characteristics. Their data compellingly demonstrated increases in aggressive behavior, anxiety and depression and delinquency among those with a mild TBI (Connolly and McCormick, 2019). Studies of veterans exposed to mild TBI caused by blast injuries are also instructive and relevant. The context and unpredictable nature of blast injury in theaters of war is such that it is relatively implausible to invoke the victims’ own behavior as a risk for its occurrence. The frequency of the event, availability of relevant preinjury behavioral/psychometric data and availability of appropriate control data from uninjured victims has yielded abundant data, albeit recognizing that blast mild TBI may have its own unique characteristics and thus not constitute the perfect model for non-blast sustained mild TBI. In one recent study, indices of disinhibition were significantly elevated in veterans with blast induced mild TBI relative to their preinjury scores and to non-injured controls (Schindler et al., 2017).
In relation to the possible dose effects of a single TBI, we established categories of severity based upon the duration of LOC (Table 4) for those individuals in our study who reported one past TBI only. Here, significant differences, with the most severe group being associated with the most adverse circumstances, were reported with respect to the physical quality of life and social support only. When we compared individuals who had sustained a single mild TBI with the remaining sample of TBI- individuals (Table 6), there were significant differences with respect to levels of anger and substance use (in both instances more in the mild TBI group). The significance of those latter group associations is especially unclear as bidirectional causation is plausible (that is, anger and substance abuse might both lead to, or be consequences of, TBI).
It is well established that socio-demographic variables such as age, poverty and unemployment are influential in terms of an individual’s criminal risk (Krug et al., 2002 Mundia et al., 2016; Siever, 2018). In this study, 66% of the participants were between 18 and 35 years old. Age appears to be one of the critical variables as criminal behavior peaks in late adolescence and early adulthood (Shulman et al., 2013), and TBI is also very common in children, adolescents, and young adults (McCormick et al., 2021). Although mild TBI does not result in long-lasting cognitive, physical, or neurological symptoms in most cases (Mosti and Coccaro, 2018), the effects of such injury may be different in the immature compared to the adult brain (Kirkwood et al., 2006). Several other studies of adolescents have shown that head injury is associated with an increase in aggressive behavior (Jones et al., 2018) and other externalizing problems (Anderson et al., 2009; Keightley et al., 2014; Connolly and McCormick, 2019; McCormick et al., 2021).
We found a significant association between TBI and employment, accommodation, and suspension from school (Table 1). Several factors such as emotional support, mental health and participation in work are associated with better quality of life (Steadman-Pare et al., 2001). On the contrary, social isolation and restricted lifestyle coupled with impulsivity may make individuals prone to suicidal behavior and alcohol abuse (Ponsford et al., 2007; Larney et al., 2012). In the tests measuring alcohol use (AUDIT) and suicidal behavior (ideation and attempt), scores were significantly higher in participants with TBI and increased with the frequency of TBIs. Violence related to alcohol abuse has been widely reported, and several factors have been associated with chronic alcohol use and violence, including psychiatric comorbidities such as personality disorders and mood disorders (Siever, 2018; Sontate et al., 2021). Long-term alcohol abuse can also lead to morphological changes in brain areas involved in self-control, decision-making, and emotional processing (Sontate et al., 2021). The correlation found between TBI and suicidal ideation in the offender population is consistent with the literature (Larney et al., 2012).
The association between TBI and criminality is very complex. Study participants who are, perhaps developmentally, impulsive and violent are inherently more risk-taking and less harm avoidant. Thus, pre-existing factors may predispose individuals to TBI and conversely, TBI may contribute to an exacerbation of impulsive behavior and poorer social skills (Williams et al., 2018). The disruption of communication and social learning leads to problematic interpersonal relationships and severe self-identification problems associated with complex trauma (Hart et al., 2012; Williams et al., 2018). Especially in the brains of young people, the neural systems responsible for important socialization skills are still immature and can be more easily disrupted by TBI (Williams et al., 2018). Injury at this stage of life can increase impulsivity, and impair social judgment (Max et al., 2001) and these behavioral changes are likely to increase the risk of offending.
Developing services to reduce the disability associated with TBI and the re-offending risk is a very complex task. We have been impressed by the literature suggesting the high importance of impulsivity and poor self-control as risk factors for offending. Indeed, these considerations, together with the evidence to suggest that SSRIs may reduce impulsivity and aggression prompted us to undertake the ReINVEST study from which the current sample of participants were drawn (Butler et al., 2021). More generally, we hypothesize that targeting adverse neuropsychiatric conditions or syndromes, associated or comorbid with TBI, for which there is an evidence-base supporting efficacy, might yield significant benefits—not only in the quality of life for the patient but in terms of reduced recidivism. Suitable screening for such conditions should be undertaken, allowing for diversion when appropriate. Evidence already exists to support the benefit of antipsychotics for individuals with psychosis and is suggestive of the benefit of stimulants for people with attention deficit hyperactivity disorder (Lichtenstein et al., 2012; Fazel et al., 2014). Both psychosis and ADHD are over-represented in offender populations (Butler et al., 2006; Young et al., 2015). We will soon be reporting our findings from the results of the ReINVEST trial (Butler et al., 2021), examining the possible benefits of SSRIs for impulsive violent individuals who contributed to the present study.
We acknowledge important limitations, several alluded to already. By virtue of the parent study from which these data were drawn, all study participants were violent offenders and all had threshold levels of impulsivity. This selective nature of the sample leads to at least the potential for correlations between some variables to be spurious (Elwert and Winship, 2014). Furthermore, most of the data presented here was based on self-report, with limited available information on the validity and accuracy of individuals’ recall. A previous study (Schofield et al., 2011) suggested that prisoner self-report of TBI is generally accurate when compared with evidence documented in hospital medical records. Subjective reports of a history of TBI may be subject to error and/or recall biases, as can reports on the duration of reported LOC as an index of severity of TBI. There were no control data (i.e., on non-impulsive non-offenders) to use for comparison. Despite these limitations, we considered that, given the unique nature of the sample, the relative richness of the data relating to participant characteristics, including neuropsychiatric phenomena and information on multiple instances of TBI, the narrowly targeted analyses seeking associations between neuropsychiatric phenomena and TBI history could be justified.
In conclusion, the impulsive individuals with histories of violence who participated in this study reported high levels of anger, distress, substance abuse and early life trauma as well as high rates of past TBI and, frequently, multiple TBI with a hard-to-quantify contribution toward their current levels of criminal justice engagement and neuropsychiatric morbidity. Increased public health efforts, targeting social disadvantage and early childhood adversity, are fundamental to minimizing the prevalence of such conditions that present expensive and complex challenges for the criminal justice system, public health and forensic clinicians. Nevertheless, defining the treatable (in adulthood), and treating appropriately, should continue to be rewarding challenges.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The study was approved by these independent ethics committees: the University of New South Wales Human Research Ethics Committee (HREC) (HC11390, HC17771), Aboriginal Health and Medical Research Council HREC (822/11) and Corrective Services NSW HREC (09/26576). Approval from the NSW Justice Health and Forensic Mental Health Network HREC (G8/14) will allow participants to continue the study while in detention. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
VCR and PS defined the objectives for the study. VCR managed the data and analyzed and interpreted the results, and wrote the first draft of the manuscript. PS and TB critically reviewed and edited the final version. BT, LK, RS, PM, JJ, DG, SA, VC, AE, VG, and KW revised the manuscript. All authors read and approved the final manuscript.
The ReINVEST trial was initially funded by the National Health and Medical Research Council (GNT0533559) and subsequently by the NSW Department of Communities and Justice. The funding agencies had no role in study design, data collection, data analysis, data interpretation, or report writing.
The authors would like to thank the National Health and Medical Research Council, members of the ReINVEST clinical team and all participants in the study.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
AIAQ, Anger Irritability and Aggression Questionnaire; AUDIT, The Alcohol Use Disorders Identification Test; BDI-II, The Beck Depression Inventory – II; BIS, Barratt Impulsiveness Scale; EIQ, Eysenck Impulsivity Questionnaire; IPDE, The International Personality Disorder Examination; K-10, The Kessler Psychological Distress Scale; LOC, Loss of Consciousness; NSW, New South Wales; OFC, Orbitofrontal cortex; PTSD, Post-traumatic stress disorder; TBI, Traumatic brain injury; SF-12, Short Form-12; STAXI-2, The State Trait Anger Expression Inventory.
Abubakar, I. I., Tillmann, T., and Banerjee, A. (2015). Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990-2013: a systematic analysis for the global burden of disease study 2013. Lancet 385, 117–171. doi: 10.1016/S0140-6736(14)61682-2
Anderson, V., Spencer-Smith, M., Leventer, R., Coleman, L., Anderson, P., Williams, J., et al. (2009). Childhood brain insult: can age at insult help us predict outcome? Brain 132, 45–56. doi: 10.1093/brain/awn293
Bailes, J. E., Dashnaw, M. L., Petraglia, A. L., and Turner, R. C. (2014). Cumulative effects of repetitive mild traumatic brain injury. Prog. Neurol. Surg. 28: 50–62. doi: 10.1159/000358765
Barnfield, T. V., and Leathem, J. M. (1998). Incidence and outcomes of traumatic brain injury and substance abuse in a New Zealand prison population. Brain Inj. 12, 455–466. doi: 10.1080/026990598122421
Barratt, E., Stanford, M. S., and Costello, C. G. (1995). Barratt impulsiveness scale, version 11 (BIS-11), in impulsiveness in personality characteristics of the personality disordered client. Wiley: New York, NY.
Bonow, R. H., Wang, J., Zatzick, D. F., Rivara, F. P., and Rowhani-Rahbar, A. (2019). Traumatic brain injury and the risk for subsequent crime perpetration. J. Head Trauma Rehabil. 34, E61–E69. doi: 10.1097/HTR.0000000000000413
Butler, T., Andrews, G., Allnutt, S., Smith, N., Sakashita, C., and Basson, J. (2006). Mental disorders in Australian prisoners: a comparison with a community sample. Aust. N. Z. J. Psychiatr. 40, 272–276. doi: 10.1080/j.1440-1614.2006.01785.x
Butler, T., Schofield, P. W., Knight, L., Ton, B., Greenberg, D., Scott, R. J., et al. (2021). Sertraline hydrochloride for reducing impulsive behavior in male, repeat-violent offenders (ReINVEST): protocol for a phase IV, double-blind, placebo-controlled, randomised clinical trial. BMJ Open 11:e044656. doi: 10.1136/bmjopen-2020-044656
Carlsson, G. S., Svärdsudd, K., and Welin, L. (1987). Long-term effects of head injuries sustained during life in three male populations. J. Neurosurg. 67, 197–205. doi: 10.3171/jns.1987.67.2.0197
Connolly, E. J., and McCormick, B. F. (2019). Mild traumatic brain injury and psychopathology in adolescence: evidence from the project on human development in Chicago neighborhoods. J. Adolesc. Health 65, 79–85. doi: 10.1016/j.jadohealth.2018.12.023
Dileo, J. F., Brewer, W. J., Hopwood, M., Anderson, V., and Creamer, M. (2008). Olfactory identification dysfunction, aggression and impulsivity in war veterans with post-traumatic stress disorder. Psychol. Med. 38, 523–531. doi: 10.1017/S0033291707001456
Durand, E., Chevignard, M., Ruet, A., Dereix, A., Jourdan, C., and Pradat-Diehl, P. (2017). History of traumatic brain injury in prison populations: a systematic review. Ann. Phys. Rehabil. Med. 60, 95–101. doi: 10.1016/j.rehab.2017.02.003
Elbogen, E. B., Wolfe, J. R., Cueva, M., Sullivan, C., and Johnson, J. (2015). Longitudinal predictors of criminal arrest after traumatic brain injury: results from the traumatic brain injury model system national database. J. Head Trauma Rehabil. 30, E3–E13. doi: 10.1097/HTR.0000000000000083
Elwert, F., and Winship, C. (2014). Endogenous selection Bias: the problem of conditioning on a collider variable. Annu. Rev. Sociol. 40, 31–53. doi: 10.1146/annurev-soc-071913-043455
Farrer, T. J., and Hedges, D. W. (2011). Prevalence of traumatic brain injury in incarcerated groups compared to the general population: a meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 35, 390–394. doi: 10.1016/j.pnpbp.2011.01.007
Fazel, S., Lichtenstein, P., Grann, M., and Långström, N. (2011). Risk of violent crime in individuals with epilepsy and traumatic brain injury: a 35-year Swedish population study. PLoS Med. 8:e1001150. doi: 10.1371/journal.pmed.1001150
Fazel, S., Zetterqvist, J., Larsson, H., Långström, N., and Lichtenstein, P. (2014). Antipsychotics, mood stabilisers, and risk of violent crime. Lancet 384, 1206–1214. doi: 10.1016/S0140-6736(14)60379-2
Gavett, B. E., Stern, R. A., and McKee, A. C. (2011). Chronic traumatic encephalopathy: a potential late effect of sport-related concussive and subconcussive head trauma. Clin. Sports Med. 30, 179–188. doi: 10.1016/j.csm.2010.09.007
Geddes, J. F., Vowles, G. H., Nicoll, J. A. R., and Révész, T. (1999). Neuronal cytoskeletal changes are an early consequence of repetitive head injury. Acta Neuropathol. 98, 171–178. doi: 10.1007/s004010051066
Gronwall, D., and Wrightson, P. (1975). Cumulative effect of concussion. Lancet 306, 995–997. doi: 10.1016/S0140-6736(75)90288
Hart, T., Vaccaro, M. J., Hays, C., and Maiuro, R. D. (2012). Anger self-management training for people with traumatic brain injury: a preliminary investigation. J. Head Trauma Rehabil. 27, 113–122. doi: 10.1097/HTR.0b013e31820e686c
Jones, K. M., Barker-Collo, S., Parmar, P., Starkey, N., Theadom, A., Ameratunga, S., et al. (2018). Trajectories in health recovery in the 12 months following a mild traumatic brain injury in children: findings from the BIONIC study. J. Prim. Health Care 10, 81–89. doi: 10.1071/HC17038
Keightley, M. L., Côté, P., Rumney, P., Hung, R., Carroll, L. J., Cancelliere, C., et al. (2014). Psychosocial consequences of mild traumatic brain injury in children: results of a systematic review by the international collaboration on mild traumatic brain injury prognosis. Arch. Phys. Med. Rehabil. 95, S192–S200. doi: 10.1016/j.apmr.2013.12.018
Kennedy, E., Heron, J., and Munafò, M. (2017). Substance use, criminal behavior and psychiatric symptoms following childhood traumatic brain injury: findings from the ALSPAC cohort. Eur. Child Adolesc. Psychiatry 26, 1197–1206. doi: 10.1007/s00787-017-0975-1
Kirkwood, M. W., Yeates, K. O., and Wilson, P. E. (2006). Pediatric sport-related concussion: a review of the clinical Management of an oft-Neglected Population. Pediatrics 117, 1359–1371. doi: 10.1542/peds.2005-0994
Kocka, A., and Gagnon, J. (2014). Definition of impulsivity and related terms following traumatic brain injury: a review of the different concepts and measures used to assess impulsivity, disinhibition and other related concepts. Behav. Sci. 4, 352–370. doi: 10.3390/bs4040352
Krug, E. G., Mercy, J. A., Dahlberg, L. L., and Zwi, A. B. (2002). The world report on violence and health. Lancet 360, 1083–1088. doi: 10.1016/S0140-6736(02)11133-0
Larney, S., Topp, L., Indig, D., O’driscoll, C., and Greenberg, D. (2012). A cross-sectional survey of prevalence and correlates of suicidal ideation and suicide attempts among prisoners in New South Wales, Australia. BMC Public Health. 12, 1–7. doi: 10.1186/1471-2458-12-14
Lichtenstein, P., Halldner, L., Zetterqvist, J., Sjölander, A., Serlachius, E., Fazel, S., et al. (2012). Medication for attention defcit–hyperactivity disorder and criminality. N. Engl. J. Med. 367, 2006–2014. doi: 10.1056/NEJMoa1203241
Mattson, M. P. (2003). Neurobiology of aggression: understanding and preventing violence. Totowa, New Jersey: Humana Press Inc, Springer Science & Business Media.
Max, J. E., Robertson, B. A. M., and Lansing, A. E. (2001). The phenomenology of personality change due to traumatic brain injury in children and adolescents. J. Neuropsychiatry Clin. Neurosci. 13, 161–170. doi: 10.1176/jnp.13.2.161
Mayer, A. R., Quinn, D. K., and Master, C. L. (2017). The spectrum of mild traumatic brain injury: a review. Neurology 89, 623–632. doi: 10.1212/WNL.0000000000004214
McCormick, B. F., Connolly, E. J., and Nelson, D. V. (2021). Mild traumatic brain injury as a predictor of classes of youth internalizing and externalizing psychopathology. Child Psychiatry Hum. Dev. 52, 166–178. doi: 10.1007/s10578-020-00992-9
McInnes, K., Friesen, C. L., MacKenzie, D. E., Westwood, D. A., and Boe, S. G. (2017). Mild traumatic brain injury (mTBI) and chronic cognitive impairment: a scoping review. PLoS One 12:e0174847. doi: 10.1371/journal.pone.0174847
McKee, A. C., Cantu, R. C., Nowinski, C. J., Hedley-Whyte, E. T., Gavett, B. E., Budson, A. E., et al. (2009). Chronic traumatic encephalopathy in athletes: progressive tauopathy after repetitive head injury. J. Neuropathol. Exp. Neurol. 68, 709–735. doi: 10.1097/NEN.0b013e3181a9d503
McKee, A. C., Stein, T. D., Nowinski, C. J., Stern, R. A., Daneshvar, D. H., Alvarez, V. E., et al. (2013). The spectrum of disease in chronic traumatic encephalopathy. Brain 136, 43–64. doi: 10.1093/brain/aws307
McKinlay, A., Corrigan, J., Horwood, L. J., and Fergusson, D. M. (2014). Substance abuse and criminal activities following traumatic brain injury in childhood, adolescence, and early adulthood. J. Head Trauma Rehabil. 29, 498–506. doi: 10.1097/HTR.0000000000000001
McKinlay, A., Horwood, L. J., and Fergusson, D. M. (2016). Accuracy of self-report as a method of screening for lifetime occurrence of traumatic brain injury events that resulted in hospitalization. J. Int. Neuropsychol. Soc. 22, 717–723. doi: 10.1017/S1355617716000497
Morrell, R. F., Merbitz, C. T., Jain, S., and Jain, S. (1998). Traumatic brain injury in prisoners. J. Offender Rehabil. 27, 1–8. doi: 10.1300/J076v27n03_01
Mosti, C., and Coccaro, E. F. (2018). Mild traumatic brain injury and aggression, impulsivity, and history of other- and self-directed aggression. J. Neuropsychiatry Clin. Neurosci. 30, 220–227. doi: 10.1176/appi.neuropsych.17070141
Mundia, L., Matzin, R., Mahalle, S., Hamid, M. H., and Osman, R. S. (2016). Contributions of sociodemographic factors to criminal behavior. Psychol. Res. Behav. Manag. 9, 147–156. doi: 10.2147/PRBM.S95270
Omalu, B. I., DeKosky, S. T., Minster, R. L., Kamboh, M. I., Hamilton, R. L., and Wecht, C. H. (2005). Chronic traumatic encephalopathy in a National Football League Player. Neurosurgery 57, 128–134. doi: 10.1227/01.NEU.0000163407.92769.ED
Perkes, I., Schofield, P. W., Butler, T. G., and Hollis, S. (2011). Traumatic brain injury rates and sequelae: a comparison of prisoners with a matched community sample in Australia. Brain Inj. 25, 131–141. doi: 10.3109/02699052.2010.536193
Ponsford, J., Whelan-Goodinson, R., and Bahar-Fuchs, A. (2007). (2007). Alcohol and drug use following traumatic brain injury: a prospective study. Brain Inj. 21, 1385–1392. doi: 10.1080/02699050701796960
Ray, B., and Richardson, N. J. (2017). Traumatic brain injury and recidivism among returning inmates. Crim. Justice Behav. 44, 472–486. doi: 10.1177/0093854816686631
Romer, D. (2010). Adolescent risk taking, impulsivity, and brain development: implications for prevention. Dev. Psychobiol. 52, 263–276. doi: 10.1002/dev.20442
Russo, M. J., Salvat, F., Kanevsky, A., Allegri, R. F., and Sevlever, G. (2023). Acute and subacute clinical markers after sport-related concussion in rugby union players. J. Sci. Med. Sport 26, 345–350. doi: 10.1016/j.jsams.2023.05.007
Schindler, A. G., Meabon, J. S., Pagulayan, K. F., Hendrickson, R. C., Meeker, K. D., Cline, M., et al. (2017). Blast-related disinhibition and risk seeking in mice and combat veterans: potential role for dysfunctional phasic dopamine release. Neurobiol. Dis. 106, 23–34. doi: 10.1016/j.nbd.2017.06.004
Schofield, P. W., Butler, T., Hollis, S., and D’Este, C. (2011). Are prisoners reliable survey respondents? A validation of self-reported traumatic brain injury (TBI) against hospital medical records. Brain Inj. 25, 74–82. doi: 10.3109/02699052.2010.531690
Schofield, P. W., Butler, T. G., Hollis, S. J., Smith, N. E., Lee, S. J., and Kelso, W. M. (2006a). Traumatic brain injury among Australian prisoners: rates, recurrence and sequelae. Brain Inj. 20, 499–506. doi: 10.1080/02699050600664749
Schofield, P. W., Butler, T. G., Hollis, S. J., Smith, N. E., Lee, S. J., and Kelso, W. M. (2006b). Neuropsychiatric correlates of traumatic brain injury (TBI) among Australian prison entrants. Brain Inj. 20, 1409–1418. doi: 10.1080/02699050601130443
Schofield, P. W., Malacova, E., Preen, D. B., D’Este, C., Tate, R., Reekie, J., et al. (2015). Does traumatic brain injury lead to criminality? A whole-population retrospective cohort study using linked data. PLoS One 10:e0132558. doi: 10.1371/journal.pone.0132558
Schofield, P. W., Moore, T. M., and Gardner, A. (2014). Traumatic brain injury and olfaction: a systematic review. Front. Neurol. 5:5. doi: 10.3389/fneur.2014.00005
Shiroma, E. J., Ferguson, P. L., and Pickelsimer, E. E. (2012). Prevalence of traumatic brain injury in an offender population: a meta-analysis. J. Head Trauma Rehabil. 27, E1–E10. doi: 10.1097/HTR.0b013e3182571c14
Shiroma, E. J., Pickelsimer, E. E., Ferguson, P. L., Gebregziabher, M., Lattimore, P. K., Nicholas, J. S., et al. (2010). Association of medically attended traumatic brain injury and in-prison behavioral infractions: a statewide longitudinal study. J. Correct. Health Care 16, 273–286. doi: 10.1177/1078345810378253
Shulman, E. P., Steinberg, L. D., and Piquero, A. R. (2013). The age–crime curve in adolescence and early adulthood is not due to age differences in economic status. J. Youth Adolesc. 42, 848–860. doi: 10.1007/s10964-013-9950-4
Siever, L. J. (2018). Neurobiology of aggression and violence. Am. J. Psychiatr. 165, 429–442. doi: 10.1176/appi.ajp.2008.07111774
Slaughter, B., Fann, J. R., and Ehde, D. (2003). Traumatic brain injury in a county jail population: prevalence, neuropsychological functioning and psychiatric disorders. Brain Inj. 17, 731–741. doi: 10.1080/0269905031000088649
Sontate, K. V., Rahim Kamaluddin, M., Naina Mohamed, I., Mohamed, R. M. P., Shaikh, M. F., Kamal, H., et al. (2021). Alcohol, aggression, and violence: from public health to neuroscience. Front. Psychol. 12:699726. doi: 10.3389/fpsyg.2021.699726
Steadman-Pare, D., Colantonio, A., Ratcliff, G., Chase, S., and Vernich, L. (2001). Factors associated with perceived quality of life many years after traumatic brain injury. J Head Trauma Rehabil 16, 330–342. doi: 10.1097/00001199-200108000-00004
Timonen, M., Miettunen, J., Hakko, H., Zitting, P., Veijola, J., von Wendt, L., et al. (2002). The association of preceding traumatic brain injury with mental disorders, alcoholism and criminality: the Northern Finland 1966 Birth Cohort Study. Psychiatry Res. 113, 217–26. doi: 10.1016/s0165-1781(02)00269-x
Williams, W. H., Chitsabesan, P., Fazel, S., McMillan, T., Hughes, N., Parsonage, M., et al. (2018). Traumatic brain injury: a potential cause of violent crime? Lancet Psychiatry 5, 836–844. doi: 10.1016/S2215-0366(18)30062-2
Keywords: traumatic brain injury, offending potential, impulsivity, orbitofrontal cortex (OFC), violent behavior
Citation: Challakere Ramaswamy VM, Butler T, Ton B, Wilhelm K, Mitchell PB, Knight L, Greenberg D, Ellis A, Allnutt S, Jones J, Gebski V, Carr V, Scott RJ and Schofield PW (2023) Self-reported traumatic brain injury in a sample of impulsive violent offenders: neuropsychiatric correlates and possible “dose effects”. Front. Psychol. 14:1243655. doi: 10.3389/fpsyg.2023.1243655
Received: 21 June 2023; Accepted: 28 August 2023;
Published: 12 September 2023.
Edited by:
Fabrizio Stasolla, Giustino Fortunato University, ItalyReviewed by:
Kriti Mishra, Lincoln County Hospital, United KingdomCopyright © 2023 Challakere Ramaswamy, Butler, Ton, Wilhelm, Mitchell, Knight, Greenberg, Ellis, Allnutt, Jones, Gebski, Carr, Scott and Schofield. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Peter William Schofield, cGV0ZXIuc2Nob2ZpZWxkQGhlYWx0aC5uc3cuZ292LmF1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.