- Department of Psychology, Sapienza University, Via dei Marsi, Rome, Italy
Background: During pregnancy, body size rapidly modifies over a relatively short period. Literature emphasizes the need to identify the factors that influence body image during peripartum as the extent of women’s adaptation to these changes has significant repercussions on both mother’s and newborn’s health. Emotion regulation strategies (i.e., expressive suppression and cognitive reappraisal) were linked to body image in the general and clinical population, but no studies were conducted in the peripartum. The present study aims to investigate the longitudinal impact of prepartum body image disturbances on postpartum body image disturbances and to evaluate the mediational role of emotional regulation strategies.
Methods: A total of 133 pregnant women completed a three-phase longitudinal study. Women answered online questionnaires during the second (T1) and the third (T2) trimesters of pregnancy, and at about 6 months postpartum (T3).
Results: Findings indicated that body image disturbances at T1 were a significant predictor of body image disturbances in the postpartum (1 year after the first assessment). Moreover, cognitive reappraisal measured at T2 partially mediated this relationship: body image disturbances in the second trimester of pregnancy were linked to less use of cognitive reappraisal in the third trimester of pregnancy, and this, in turn, was associated with worse body image disturbances at 6 months after birth.
Conclusion: Findings of this longitudinal study highlight the importance of assessing body image disturbances during pregnancy to early identify women at risk, and suggest cognitive reappraisal as a possible target intervention.
1. Introduction
Body image disturbance (or “negative body image”) is a multidimensional construct, that refers to negative perceptions, feelings, behaviors, beliefs, and attitudes toward aspects of one’s body (Cash et al., 2004). While body dissatisfaction mainly concerns negative feelings about one’s body, body image disturbance is defined by a negative evaluation of one’s appearance not only on emotional terms but also on perceptual, cognitive, and behavioral ones. A negative body image includes preoccupation and worries related to weight or body aspects including the resulting interference with daily life or functioning (Phillips, 2005).
During pregnancy, body size and weight rapidly change over a relatively short period, leading the woman to move away from the socio-culturally prescribed “thin ideal” and triggering additional body image concerns (Skouteris et al., 2005; Duncombe et al., 2008; Watson et al., 2015). Although the normal societal pressure to conform to body shape ideals may be reduced during pregnancy (Duncombe et al., 2008), several studies reported an increase in body dissatisfaction during the peripartum period (Fuller-Tyszkiewicz et al., 2013), with further intensifications in the postpartum (Hodgkinson et al., 2014; Tavakoli et al., 2021). Indeed, during the postpartum period, most women report more concerns about their inability to return to their pre-pregnancy body weight, resulting in higher body dissatisfaction (Lovering et al., 2018; Nagl et al., 2021).
The extent of pregnant women’s adaptation to their changing bodies has significant implications. Body image disturbances during pregnancy significantly increase the risk of developing perinatal depression (Silveira et al., 2015; Riquin et al., 2019), with subsequent negative implications on mother–child interactions and caretaking activities (Slomian et al., 2019). Negative body image is associated with problematic parent–child feeding interactions (Bergmeier et al., 2020), with lower breastfeeding intentions (Barnes et al., 1997), and poorer mother-fetal and mother-newborn attachment quality (Huang et al., 2004; Williams, 2019). Furthermore, during the peripartum, dissatisfaction with one’s body is associated with higher rates of unhealthy behaviors, like skipping meals, self-induced vomiting, and laxative use as extreme weight control conducts (Clark and Ogden, 1999; Neiterman and Fox, 2017). Besides being detrimental to the women, these unhealthy dieting and dysfunctional conducts are also harmful to the fetus and the baby’s development (Chan et al., 2020).
Not all women report an increase in worries and concerns about their bodies during pregnancy, and psychosocial characteristics may mediate this relationship. Indeed, studies highlighted that some pregnant women are even more satisfied with their bodies than non-pregnant women (Richardson, 1990; Loth et al., 2012). For this reason, the literature emphasizes the need to identify the factors that differently contribute to negative body image (Sweeney and Fingerhut, 2013; Watson et al., 2015).
In the non-pregnant population, researchers studied the role of emotion regulation strategies, evidencing positive associations between emotional regulation difficulties and body image (i.e., Hayaki et al., 2002; Sim and Zeman, 2006; Hughes and Gullone, 2011). Two of the most explored emotional regulation strategies are cognitive reappraisal and expressive suppression. Cognitive reappraisal is an antecedent-focused strategy that consists of the cognitive change of the emotional impact of a situation; it is considered a positive strategy consisting in the reinterpretation of a stressor with an effective alteration of its emotional trajectory, which predicts lower negative affect (Gross and John, 2003; Aldao et al., 2010). In contrast, expressive suppression is the inhibition of the already-formed emotional response (Gross and John, 2003; Gross and Thompson, 2007; Gross, 2015). As a response-focused strategy that comes late in the emotion-generative process, suppression of emotions is considered an inefficient strategy, creating a discrepancy between the inner experience and the outer expression of emotion (Gross and John, 2003). It is associated with more negative feelings, lower levels of self-esteem, and worst relationships with others (Gross, 1998; McLean et al., 2007; Berking and Wupperman, 2012; Kraiss et al., 2020).
Studies on body image highlighted that subjects with greater use of expressive suppression report higher levels of negative body image than those who use cognitive reappraisal as a usual strategy (Geller et al., 2000; Hughes and Gullone, 2011; Kiriukhina and Polskaya, 2021). Conversely, cognitive reappraisal strategies are associated with higher body image satisfaction, less shape, and eating concerns, with greater acceptance of physical appearance changes, and with more frequent adoption of healthy behaviors (Siân et al., 2010; Prefit et al., 2020). Literature has also evidenced that a negative body image is related to increased cognitive arousal, higher distress, more negative thoughts, and reduced use of adaptive emotion regulation strategies (Cash et al., 2005; Sim and Zeman, 2005; Ferreira and Trindade, 2015). Moreover, in the non-pregnant population, it is well documented that a reduced ability to properly regulate one’s feeling through adaptive emotional regulation strategies may lead to different expressions of psychopathology (Lappanen et al., 2022; Miu et al., 2022; Stellern et al., 2023). However, as recently pointed out by Penner and Rutherford (2022), there is limited research evaluating the role of emotion regulation on women’s mental health throughout the perinatal period (Penner and Rutherford, 2022). This is surprising, considering that pregnancy is a period full of physiological and emotional changes, in which emotion regulation strategies may play a crucial role in reducing or exacerbating the distress or the risk of psychopathology (Rutherford et al., 2015; Coo et al., 2020; McDonald et al., 2021; Taubman-Ben-Ari et al., 2021). Considering body image, to the best of our knowledge, no studies evaluated the relationship of emotional regulation with body image disturbances during the peripartum period.
Based on the above considerations, we hypothesize that women reporting more body image disturbances during pregnancy will be at greater risk of postpartum body image disturbances. Moreover, we aim to examine the mediating role of emotional regulation strategies in this relationship. In particular, we assume that prepartum body image disturbances will be negatively associated with the use of cognitive reappraisal and that this in turn will negatively predict body image disturbances in the postpartum. Conversely, we expect that negative body image in the second trimester of pregnancy will be positively associated with the use of expressive suppression in the third trimester of pregnancy, which, in turn, will positively predict body image disturbances at 6 months after birth.
2. Materials and methods
2.1. Participants and procedures
Two hundred and thirty healthy pregnant women accepted to participate in a three-phase longitudinal study. Women were directly and opportunistically recruited through private maternity centers, schools, family associations, and diagnostic clinics in Italy between February 2018 and October 2020. Inclusion was limited to women in the second trimester of pregnancy (the fourth, fifth, or sixth month) and who were fluent in Italian. We choose not to include women in the first trimester as body changes are not so evident in this period. All participants took part on a voluntary basis and were not remunerated. After explaining the procedure of the study and signing the informed consent form, women in the second semester of pregnancy were asked to complete an online questionnaire (T1). Participants were required to provide an email address and a phone number for further contact. During the third trimester and after the baby was 6 months old, participants were contacted again by email or phone message and asked to complete a second (T2) and a third (T3) online questionnaire. To guarantee participants’ anonymity, a personal alphanumeric code was assigned to each participant and used to access the online questionnaires and implemented through the survey editor SurveyMonkey. Out of the 230 pregnant women who completed valid baseline measurements, participants included in the final analyses were the 133 women with complete data for all variables at baseline and follow-ups, including covariates. All participants gave fully informed written consent to participate in the study, and ethical approval was obtained by the Institutional Review Board of the Psychology Department, Sapienza University of Rome (Prot. n. 0000102 of 24/01/2018).
2.2. Measures
2.2.1. Body image disturbance
The Body Image Disturbance Questionnaire (BIDQ) was used to assess body image disturbance or “negative body image” (Cash et al., 2004; Cash and Grasso, 2005) at T1, T2, and T3. Permission to use the questionnaire was obtained by the authors. The seven items of the scale explored concerns, preoccupations, distress, and impairment in social or occupational functioning related to participants’ body appearance (Cash, 2002; Cash and Grasso, 2005). An example item is: “Are you concerned about the appearance of some part(s) of your body which you consider especially unattractive?” Responses to each statement are scored on a five-point Likert scale ranging from 1 to 5. The total score is taken as the mean of the seven items, with a higher score indicating higher levels of body image disturbance (Cash et al., 2004). The scale showed excellent internal consistency and test–retest reliability (Cash and Grasso, 2005; Hrabosky et al., 2009) and was used in previous studies on pregnant women (Shloim et al., 2019). The BIDQ was translated into Italian. A factor analysis using Principal Axis Factoring method was applied to the T1 BIDQ responses to verify the one-factor structure of the questionnaire The values of the Kaiser–Meyer–Olkin (KMO) of 0.822 and the result of Bartlett’s test [χ2(21) = 388.23, p < 0.001] indicated the suitability of the data for factor analysis (Hutcheson and Sofroniou, 1999). The Italian version of BIDQ proved to be one-dimensional, as indicated by the total variance explained by this factor (50.01%) and the fact that all the seven items of the BIDQ loaded onto this factor and had good to excellent factor loadings (range: 0.55–0.81) (Tabachnick and Fidell, 2013). In the current sample, Cronbach’s alphas were α = 0.82 (T1), α = 0.87 (T2), and α = 0.89 (T3) and McDonald’s omega were ω = 0.81 (T1), ω = 0.86 (T2), and ω = 0.88 (T3). To further explore the change over time of the variable, we calculate a change score (i.e., subtraction of T1 Body Image Disturbance from T3 Body Image Disturbance). Positive scores indicated an increase in body image disturbance over time.
2.2.2. Emotion regulation
Emotion regulation was evaluated at T2 using the Italian version of the Emotion Regulation Questionnaire (ERQ; Gross and John, 2003; Balzarotti et al., 2010). The 10-item scale measures participants’ typical use of cognitive reappraisal and expressive suppression as strategies to regulate emotional responses (Gross and John, 2003; Gross, 2015). Each item is scored on a seven-point Likert scale ranging from 1 (strongly disagree) to 7 (strongly agree). The questionnaire provides two mean scores related to the six-item cognitive reappraisal subscale (ERQ-R) and the four-item expressive suppression subscale (ERQ-S). Two examples of items are “I control my emotions by changing the way I think about the situation I’m in” for the Cognitive Reappraisal subscale, and “I control my emotions by not expressing them” for the Expressive Suppression Subscale. Greater scores at each subscale indicate greater emotion regulation strategy use. The scale showed good factorial validity and internal consistency reliability (Balzarotti et al., 2010; Preece et al., 2020, 2021) and was used in recent peripartum research (Zemestani and Fazeli Nikoo, 2020; Taubman-Ben-Ari et al., 2021). Cronbach’s alpha for the ERQ-R and ERQ-S subscales at T2 was α = 0.89 and α = 0.75, respectively. McDonald’s omega for the ERQ-R and ERQ-S subscales at T2 were 0.90 and 0.76, respectively.
2.2.3. Covariates
Participants’ age, educational levels, and parity were recorded by the T1 self-report questionnaire. The delivery method was recorded at postpartum assessment. Height was measured at T1, and weight was measured at each phase of the study (i.e., T1, T2, and T3). BMI was calculated using the standard formula (kg/m2). To explore the change over time of BMI, we also calculate two change scores (i.e., subtraction of T1 BMI from T3 BMI and subtraction of T1 BMI from T2 BMI). Positive scores indicated an increase in BMI. Depressive symptoms at T1 were assessed using the Italian version of the Edinburgh Postnatal Depression Scale (EDPS; Cox et al., 1987; Benvenuti et al., 1999). This instrument evaluates depressive symptoms in the previous week using a four-point Likert scale. Total scores ranged from 0 to 30, with higher scores indicating a greater frequency of depressive symptoms. The EPDS has been shown to be a reliable instrument for screening depressive symptoms in the peripartum period (Bergink et al., 2011; Levis et al., 2020) with a clinical cut-off of 12 in the Italian population (Benvenuti et al., 1999). In the current study, Cronbach’s alpha was α = 0.79 and McDonald’s omega was 0.80.
2.3. Statistical analyses
Data analyses were conducted using IBM SPSS Statistic version 28 (SPSS Inc.). Sensitivity analyses were carried out to check for significant differences in the characteristics of participants between those who only completed the first assessment (T1) and those with full data. Using independent t and χ2 tests, women were compared on age, education, parity, BMI, prepartum depressive symptoms, and prepartum body image disturbance. Descriptive statistics were calculated for each variable of the study. Means (M), standard deviations (SD), and min/max range were presented for all continuous variables. Data on categorical variables were presented as the number of participants (N) and percentages. Paired t-test was used to explore the change in body image disturbance from the prepartum to the postpartum period. Pearson’s product–moment correlation coefficients (r) were calculated to explore the relations among covariates, T1 depressive symptoms, T1 body image disturbances, T2 cognitive reappraisal, T2 expressive suppression, T3 body image disturbances, change scores in BMI from T1 to T3, and change scores in BIDQ from T1 to T3. The effect size of absolute value of r was considered small (0.10), medium (0.30), or large (0.50; Cohen, 1988). To examine whether emotion regulation would mediate the relationship between prepartum and postpartum body image disturbance, bootstrap mediation analysis for simple mediation through model 4 of SPSS PROCESS macro 4.0 was applied (Preacher and Hayes, 2008; Hayes, 2017). The method included 5,000 bootstrap samples for coefficient and indirect estimation and 95% bias-corrected confidence intervals (CI) for the indirect effect.
To minimize the potential bias of the simultaneous measurement of two variables, we considered each variable of the mediation model at a different time point.
Change scores in BMI (T3-T1) was entered as covariate. We reported the unstandardized effect size (b) and the 95% bias-corrected CI for the indirect effect model. If the 95% CI does not include zero, the mediation effect is significant.
3. Results
The participation rate in the entire study is 57.8%. Compared to the women who completed all the phases of the study (N = 133), those who did not complete the second and third assessments (N = 97) were more likely to have high levels of depressive symptoms at T1 [t(228) = 2.452; p = 0.015]. There were no other significance differences: age [t(228) = 0.678; p = 0.499], education [χ2(5) = 9.293, p = 0.098], BMI [t(228) = 0.307; p = 0.759], and body image disturbance at T1 [t(228) = −0.711; p = 0.478].
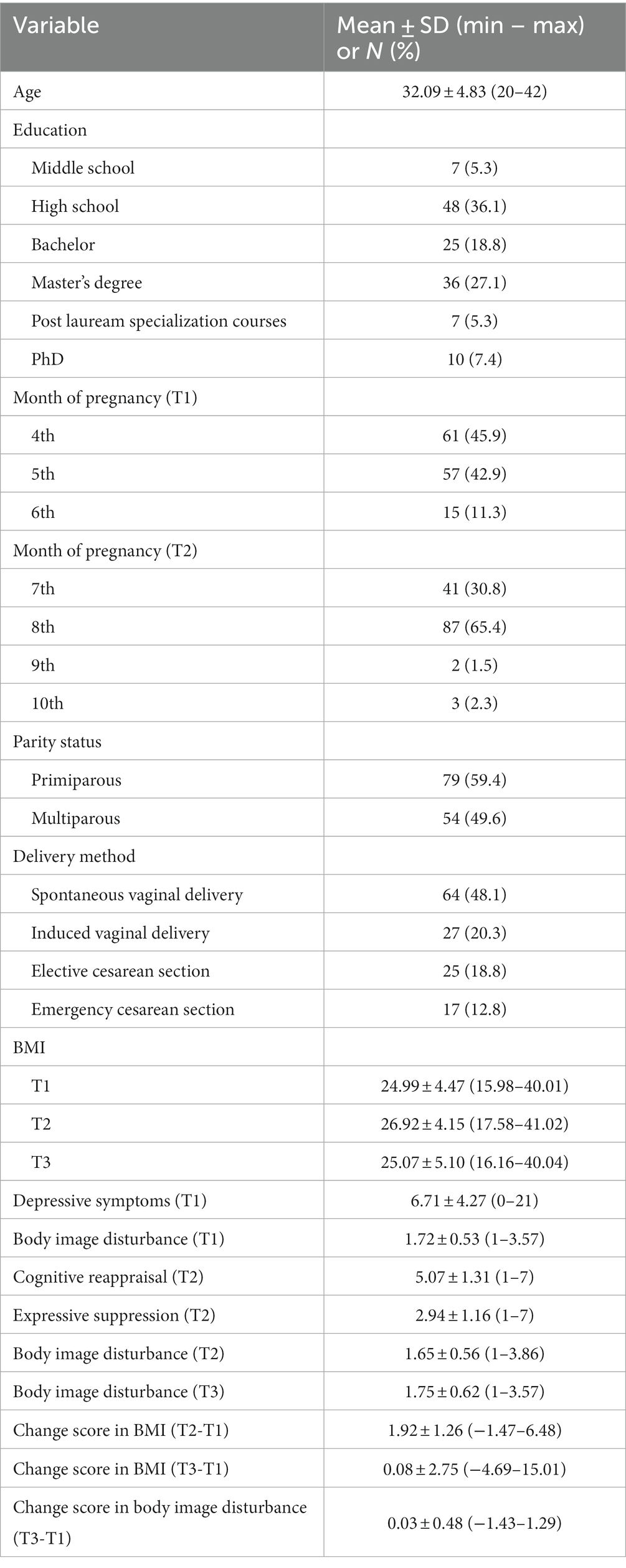
Table 1 shows the demographic characteristics of the sample. The average age of the sample was 32.09 (SD = 4.83) years, with an age range between 20 and 42. More than half of the participants had at least a university education (58.6%), were primiparous (59.4%), and had a vaginal delivery (68.4%).
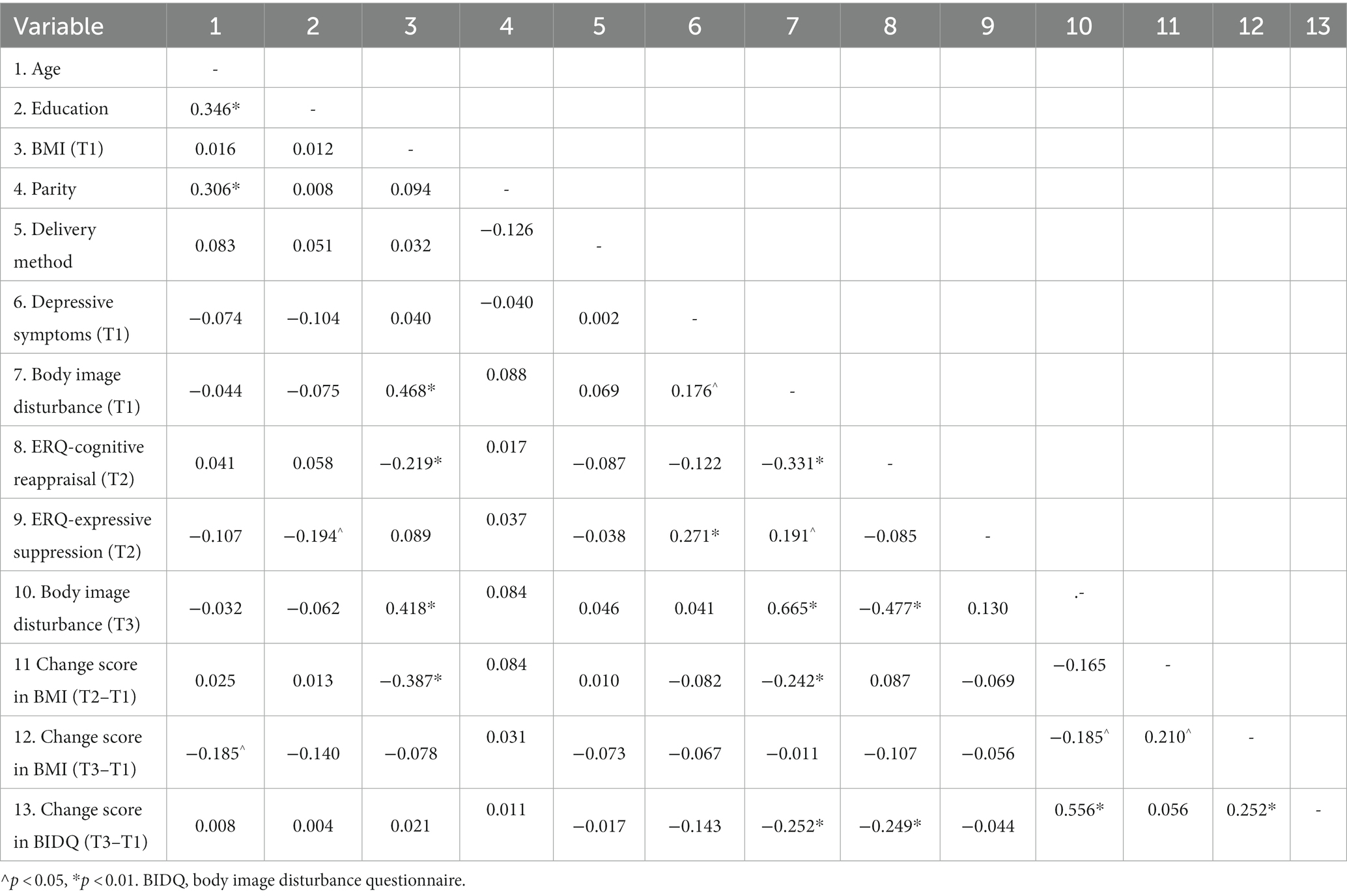
Body image disturbance did not change significantly over the peripartum period [t(132) = −0.804, p = 0.422]. Depression scores ranged from 0 to 21, with 21.1% of women above the cut-off score of 12 in the prepartum period (T1). Correlations among the variables of interest considered are reported in Table 2. Depressive symptoms at the initial phase of pregnancy were weakly correlated with body image disturbance at the same time (r = 0.176, p = 0.042) and with the expressive suppression subscale at T2 (r = 0.271, p = 0.002). Moreover, greater levels of body image disturbance at T1 were weakly correlated with higher levels of expressive suppression at T2 (r = 0.191, p = 0.028), and moderately associated with levels of cognitive reappraisal at T2 (r = −0.331, p < 0.001) and strongly associated higher levels of body image disturbance at postpartum (r = 0.665, p < 0.001). Greater usage of cognitive reappraisal strategy was moderately correlated with lower levels of body image disturbance at T3 (r = −0.477, p < 0.001). Moreover, a greater increase in the BMI change from T1 to T3 was correlated with a higher increase in the BDI scores from T1 to T3 (r = 0.252, p = 0.003).
Given the correlation results, we examined the indirect effect of prepartum body image disturbances on postpartum body image disturbances through cognitive reappraisal levels. Change score in BMI (T3-T1) was considered as the only covariate of the path analysis, since other potential covariates were not significantly related the mediator or the outcome variable (Frigon and Laurencelle, 1993). Preacher and Hayes (2008) bootstrapping estimates of indirect effects were employed. The overall model was significant, F(3, 129) = 50.909, p < 0.001, adj. R2 = 0.542. Figure 1 displays the unstandardized regression coefficients among the model variables. Higher prepartum body image disturbances were associated with lower levels of cognitive reappraisal (b = −0.727, 95% CI [−1.083, −0.370]). Moreover, the relationship between cognitive reappraisal and postpartum body image disturbances was significant (b = −0.142, 95% CI [−0.209, −0.076]). The total effect of prepartum body image disturbances on postpartum body image disturbances was significant (b = 0.776, 95% CI [0.630, 0.922]), as well as the direct effect of body image disturbances during pregnancy on body image after childbirth, when the cognitive reappraisal was included in the model (b = 0.673, 95% CI [0.527, 0.818]). The indirect effect of cognitive reappraisal at T2 in the model was significant (b = 0.103, SE = 0.036, 95% CI [0.043, 0.184]), indicating that higher cognitive reappraisal levels at T2 significantly and partially mediated the relationship between prepartum and postpartum body image disturbances scores.
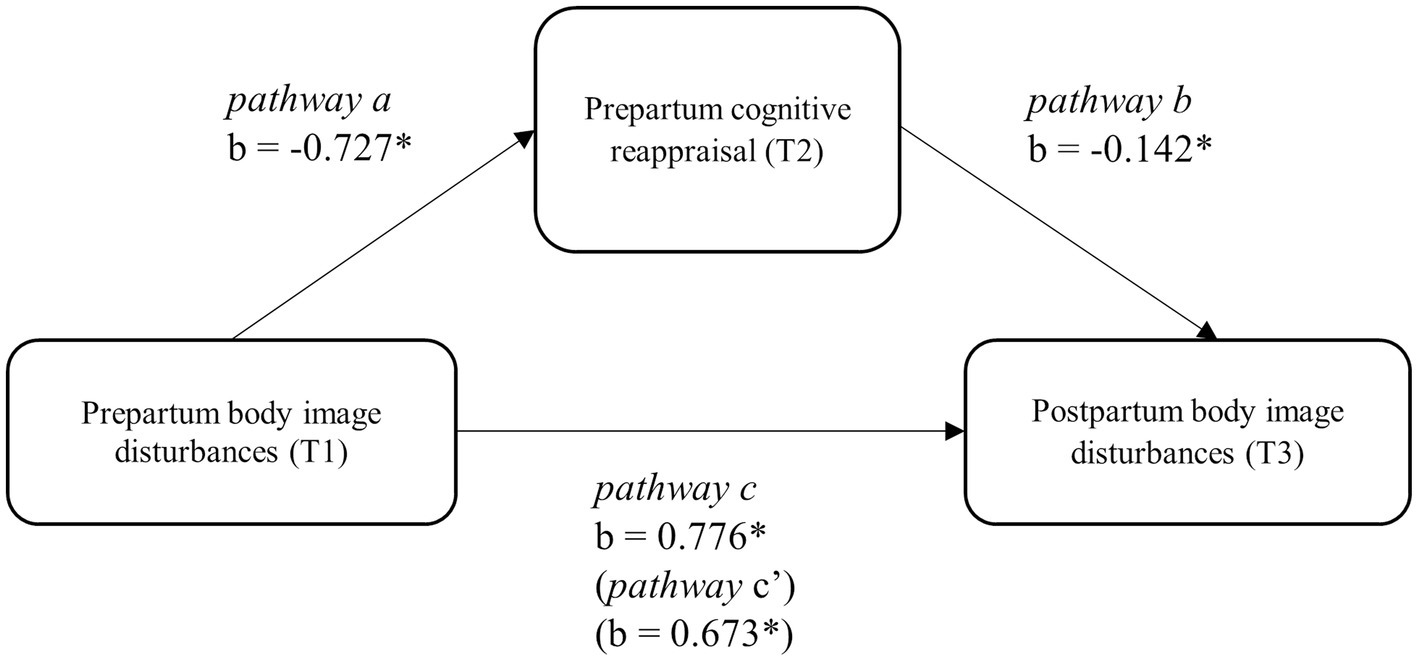
Figure 1. Mediation model of prepartum body image disturbance and postpartum body image disturbance through prepartum cognitive reappraisal. *p < 0.05.
4. Discussion
The present study aimed to assess body image disturbances in the peripartum period and their relationship with emotional regulation strategies. First, we hypothesized that a negative body image in the second trimester of pregnancy would affect body image disturbances evaluated 6 months after childbirth. Second, we hypothesized that emotional regulation strategies evaluated in the third trimester of pregnancy would play a mediating role in this relationship. Extending the scarce literature on the role of emotion regulation on women’s mental health throughout the perinatal period (Penner and Rutherford, 2022), the findings of the present study confirmed that prepartum body image disturbances predicted postpartum body image disturbances and proved that cognitive reappraisal partially mediated this relationship.
In the present study, pregnancy levels of body image disturbances were predictive of body image disturbances 6 months after birth. This is in line with previous longitudinal studies (Skouteris et al., 2005; Shloim et al., 2019) and is relevant as a negative body image experienced during the peripartum period may lead to negative consequences for the mother and the child (Fuller-Tyszkiewicz et al., 2013; Silveira et al., 2015; Bergmeier et al., 2022).
Regarding the main aim of the study, i.e., the mediational role of emotional regulation strategies, findings indicated that cognitive reappraisal partially mediated the relationship between body image disturbances during pregnancy and body image disturbances in the postpartum period.
Considering the pathway that links body image disturbances to cognitive reappraisal in pregnancy, our findings suggested that higher levels of body image disturbances in the second trimester of pregnancy might have influenced the use of cognitive reappraisal as an emotional regulation strategy in late pregnancy. Although our study is the first, to our knowledge, which has highlighted the association between negative body image and cognitive reappraisal in pregnant women, these findings are in line with previous studies on the non-pregnant population, in which the link between body image and emotion dysregulation was already established. Indeed, studies on the non-pregnant population showed that unsatisfaction with physical changes could affect emotional distress altering one’s body-related feelings and perceptions, resulting in more negative views and attitudes toward life (Duggan et al., 2013) and emotional regulation difficulties (Haynos and Fruzzetti, 2011; Cheng and Wei, 2022). People who experience higher discontent related to their appearance are more likely to develop emotional distress due to an inability to achieve their ideal and may use ineffective emotional regulation strategies to manage this discomfort (Sim and Zeman, 2005; Hughes and Gullone, 2011; Wilson et al., 2014). Indeed, to face these negative emotions, individuals with body image disturbance may exhibit an alteration in the representation of their bodies, may report negative thoughts about their image, exaggerated attention to their physical changes and experience different body-checking behaviors (Cash, 2002; Carey and Preston, 2019). These attitudes about one’s body can prevent individuals from focusing on internal states, leading to less awareness and acceptance of one’s emotions and to a consequent lack of access to adaptive emotion regulation strategies (Sim and Zeman, 2005; Lavender et al., 2015; Fernandes et al., 2017). A negative body image may also influence individuals’ ability to shift attention and to positively reevaluate the circumstances (Jones and Rogers, 2003; Siân et al., 2010). Previous studies in non-pregnant populations investigated the relationship between body image and other dysfunctional emotional regulation strategies, like avoidance, body-related co-rumination, and reduced levels of positive rational acceptance, and evidenced that a negative body image was significantly associated with emotion regulation difficulties (Cash et al., 2005; Ferreira and Trindade, 2015; Kiriukhina and Polskaya, 2021). Our study extends these results being the first that longitudinally evaluate the negative association of body disturbances with cognitive reappraisal in peripartum women. Different processes may explain this relationship including impaired interoceptive awareness (Füstös et al., 2013). Future studies are needed to further investigate possible mediational pathways.
Cognitive reappraisal in pregnancy was negatively associated with body image disturbances at 6 months postpartum. In previous research on the non-pregnant population, this adaptive strategy was related to a lower risk of body dissatisfaction (Siân et al., 2010; Prefit et al., 2020). Moreover, this finding is consistent with earlier research showing the importance of cognitive reappraisal in regulating stressful emotions in expecting mothers (Taubman-Ben-Ari et al., 2021). Former studies also showed that lowering thin ideals and expectations or accepting transformations in one’s body may lead to lower levels of negative body image and eating concerns (Webster and Tiggemann, 2003; Ferreira and Trindade, 2015). In this view, the process of reevaluating pregnant body shapes related to the specific moment of new motherhood may be a way to modify and adjust one’s perception, preventing the dysfunctional pressure to reach a strict pre-pregnancy thin ideal (Richardson, 1990). Although cognitive reappraisal training was effective in reducing body dissatisfaction in the general population (Fitzpatrick et al., 2019; Prefit et al., 2020), more studies are needed to evaluate whether this training may be useful also for pregnant women, especially for those who are more at risk for body image disturbances.
Finally, unlike expected, no relationship was found between expression suppression in pregnancy and body image disturbances in postpartum. In the non-pregnant population, expressive suppression is widely recognized as one of the main maladaptive emotional regulation strategies, predicting several repercussions on physical and mental health (Gross and John, 2003; Aldao et al., 2010). Moreover, previous studies reported a positive association between greater use of expressive suppression and higher levels of body dissatisfaction, evidencing that the inhibition of emotional expression is significantly correlated to negative feelings and thoughts about the body (Geller et al., 2000; Hayaki et al., 2002; Naumann et al., 2016; Kiriukhina and Polskaya, 2021). In our hypotheses, expressive suppression would have exacerbated body image disturbances in pregnancy and further maintained them in the postpartum; however, in our data, expressive suppression was only positively correlated with body image disturbances in the prepartum but not in the postpartum. It is possible that emotional suppression may be less relevant in the peripartum compared to pregnant women or women in the general population. This may be due to the fact that in the peripartum, women may experience more intense emotions compared to the general population (Pearson et al., 2009; Newham and Martin, 2013). Expression of these emotions during pregnancy is socially accepted and this may lead women to use fewer suppression strategies. Consistently, the means of expressive suppression in our sample were quite low. Future studies may confirm whether the role of expressive suppression is less relevant in the peripartum compared to other life periods.
4.1. Limitations
The findings of this study need to be seen in the light of some limitations. The first consideration is that all the variables were evaluated through self-report questionnaires not specifically developed to be used in pregnant women. However, all the used measures were widely used in the general, clinical, and pregnant populations. Secondly, we have to highlight the lack of a back-translation for the BIDQ, even if the translated version demonstrated adequate psychometric properties. Another limitation is the fact that we did not record the number of women who initially declined to take part in the research who may had different characteristics compared to those who consented. It must be noted, that among those who participated, women who withdrew from the study were more depressed than those who answered all the phases of the survey. Although there were no differences in body image disturbances between the women who did not participate in all the research phases and those who did, it is possible that depressed women who withdraw from the study would have had more probability of developing body image disturbances over time or that suppression would have differently affected this relationship. It has also to be noted that the levels of body image disturbances in our sample were very low, both during pregnancy and at 6 months postpartum. Moreover, in this study, we focused on negative body image. Future studies should evaluate positive aspects of body image also considering that pregnancy may be a time of relief from thinness ideals. Furthermore, we did not have a measure of cognitive reappraisal at T1. Therefore, it was not possible to control for the baseline level of cognitive reappraisal and it was not possible to measure cognitive reappraisal changes as a result of the level of body image disturbance. Similarly, we did not evaluate how emotional regulation strategies changed from pre-pregnancy to the peripartum period over time. Finally, since body image disturbances are related to depressive symptoms, future studies may need to consider the effects of the examined relationship also on postpartum depression.
5. Implications for practice and/or policy
Acknowledging the limitations above, we believe that the implications of our study are numerous. First, it highlights the importance of assessing women at risk for body image disturbances in the early stages of pregnancy. Second, since the positive re-evaluation of one’s pregnancy-related body changes can protect from developing body image disturbances in the postpartum, cognitive reappraisal as a key intervention target may be appropriate, especially for those women who are more at risk. Future studies with clinical trials are needed to evaluate whether implementing interventions based on adaptive emotional regulation strategies may be effective in protecting from body image disturbances in the postpartum period.
6. Conclusion
In conclusion, our findings suggested that prepartum body image disturbances predicted postpartum body image disturbances and proved that cognitive reappraisal partially mediated this relationship. The present study has several strengths. While most of the research on body image in pregnancy used cross-sectional designs, the longitudinal design of the present study allowed us to evidence the significant association between negative body image during pregnancy and body image disturbances in the postpartum. Moreover, the mediational model highlighted the importance of considering cognitive reappraisal as an adaptive emotion regulation strategy implicated in the relationship between prenatal and postpartum body image disturbances. As body image also had a role in influencing cognitive reappraisal strategies, more studies on this link are foreseen.
Data availability statement
The datasets presented in this article are not readily available because the raw data supporting the conclusions of this article will not be made available by the authors. Requests to access the datasets should be directed to Q2F0ZXJpbmEuZ3Jhbm9AdW5pcm9tYTEuaXQ=.
Ethics statement
The studies involving humans were approved by Institutional Review Board of the Psychology Department, Sapienza University of Rome (Prot. n. 0000102 of 24/01/2018). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
CG conceived the study and revised the manuscript. CS and CG analyzed data. MS wrote a first draft. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by PRIN grant (Progetti di Ricerca di Rilevante Interesse Nazionale, Edit. 2017, Prot. n. 2017BC4MST) to CG.
Acknowledgments
The authors thank all the participants who took part in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Aldao, A., Nolen-Hoeksema, S., and Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 30, 217–237. doi: 10.1016/j.cpr.2009.11.004
Balzarotti, S., John, O. P., and Gross, J. J. (2010). An Italian adaptation of the emotion regulation questionnaire. Eur. J. Psychol. Assess. 26, 61–67. doi: 10.1027/1015-5759/a000009
Barnes, J., Stein, A., Smith, T., and Pollock, J. I. (1997). Extreme attitudes to body shape, social and psychological factors and a reluctance to breast feed. ALSPAC study team. Avon longitudinal study of pregnancy and childhood. J. R. Soc. Med. 90, 551–559. doi: 10.1177/014107689709001007
Benvenuti, P., Ferrara, M., Niccolai, C., Valoriani, V., and Cox, J. L. (1999). The Edinburgh postnatal depression scale: validation for an Italian sample. J. Affect. Disord. 53, 137–141. doi: 10.1016/S0165-0327(98)00102-5
Bergink, V., Kooistra, L., Lambregtse-van den Berg, M. P., Wijnen, H., Bunevicius, R., van Baar, A., et al. (2011). Validation of the Edinburgh depression scale during pregnancy. J. Psychosom. Res. 70, 385–389. doi: 10.1016/j.jpsychores.2010.07.008
Bergmeier, H., Hill, B., Haycraft, E., Blewitt, C., Lim, S., Meyer, C., et al. (2022). Maternal body dissatisfaction in pregnancy, postpartum and early parenting: an overlooked factor implicated in maternal and childhood obesity risk. Appetite 147:104525. doi: 10.1016/j.appet.2019.104525
Bergmeier, H., Paxton, S. J., Milgrom, J., Anderson, S. E., Baur, L., Hill, B., et al. (2020). Early mother-child dyadic pathways to childhood obesity risk: a conceptual model. Appetite 144:104459. doi: 10.1016/j.appet.2019.104459
Berking, M., and Wupperman, P. (2012). Emotion regulation and mental health recent finding, current challenges, and future directions. Curr. Opin. Psychiatry 25, 128–134. doi: 10.1097/YCO.0b013e3283503669
Carey, M., and Preston, C. (2019). Investigating the components of body image disturbances within eating disorders. Front. Psychol. 10:635. doi: 10.3389/fpsyt.2019.00635
Cash, T. F. (2002). A “Negative Body Image”: Evaluating Epidemiological Evidence. Body Image: A Handbook of Theory, Research and Clinical Practice. New York: The Guildford Press
Cash, T. F., and Grasso, K. (2005). The norms and stability of new measures of the multidimensional body image construct. Body Image 2, 199–203. doi: 10.1016/j.bodyim.2005.03.007
Cash, T. F., Phillips, K. A., Santos, M. T., and Hrabosky, J. I. (2004). Measuring “negative body image”: validation of the body image disturbance questionnaire in a nonclinical population. Body Image 1, 363–372. doi: 10.1016/j.bodyim.2004.10.001
Cash, T. F., Santos, M. T., and Williams, E. F. (2005). Coping with body-image threats and challenges: validation of the body image coping strategies inventory. J. Psychosom. Res. 58, 190–199. doi: 10.1016/j.jpsychores.2004.07.008
Chan, Y. C., Lee, A. M., Koh, Y. W., Lam, K. S., Lee, C. P., Leung, K. Y., et al. (2020). Associations of body dissatisfaction with anxiety and depression in the pregnancy and postpartum periods: a longitudinal study. J. Affect. Disord. 263, 582–592. doi: 10.1016/j.jad.2019.11.032
Cheng, D., and Wei, M. (2022). Modified dual pathway model for binge eating: the role of emotion dysregulation. Couns. Psychol. 50, 536–560. doi: 10.1177/00110000221077936
Clark, M., and Ogden, J. (1999). The impact of pregnancy on eating behaviour and aspects of weight concern. Int. J. Obes. Relat. Metab. Disord. J. Int. Assoc. Stud. Obes. 23, 18–24. doi: 10.1038/sj.ijo.0800747
Cohen, J. (1988). Statistical Power Analysis for the Behavioral Sciences, Hillsdale, New Jersey: Erlbaum.
Coo, S., García, M. I., Prieto, F., and Medina, F. (2020). The role of interpersonal emotional regulation on maternal mental health. J. Reprod. Infant Psychol. 40, 3–21. doi: 10.1080/02646838.2020.1825657
Cox, J. L., Holden, J. M., and Sagovsky, R. (1987). Detection of postnatal depression: development of the 10-item Edinburgh postnatal depression scale. Br. J. Psychiatry 150, 782–786. doi: 10.1192/bjp.150.6.782
Duggan, J. M., Toste, J. R., and Heath, N. L. (2013). An examination of the relationship between body image factors and non-suicidal self-injury in young adults: the mediating influence of emotion dysregulation. Psychiatr. Res. 206, 256–264. doi: 10.1016/j.psychres.2012.11.016
Duncombe, D., Wertheim, E. H., Skouteris, H., Paxton, S. J., and Kelly, L. (2008). How well do women adapt to changes in their body size and shape across the course of pregnancy? J. Health Psychol. 13, 503–515. doi: 10.1177/1359105308088521
Fernandes, J., Ferreira-Santos, F., Miller, K., and Torres, S. (2017). Emotional processing in obesity: a systematic review and exploratory meta-analysis. Obes. Rev. 19, 111–120. doi: 10.1111/obr.12607
Ferreira, C., and Trindade, I. A. (2015). Body image-related cognitive fusion as a main mediational process between body-related experiences and women’s quality of life. Eat. Weight Disord. Stud. Anorex. Bulimia Obes. 20, 91–97. doi: 10.1007/s40519-014-0155-y
Fitzpatrick, S., Macdonald, D. E., Mcfarlane, T., and Trottier, K. (2019). An experimental comparison of emotion regulation strategies for reducing acute distress in individuals with eating disorders. Can. J. Behav. Sci. 51, 90–99. doi: 10.1037/cbs0000119
Frigon, J.-Y., and Laurencelle, L. (1993). Analysis of covariance: A proposed algorithm. Educational and Psychological Measurement, 53, 1–18. doi: 10.1177/0013164493053001001
Fuller-Tyszkiewicz, M., Skouteris, H., Watson, B. E., and Hill, B. (2013). Body dissatisfaction during pregnancy: a systematic review of cross-sectional and prospective correlates. J. Health Psychol. 18, 1411–1421. doi: 10.1177/1359105312462437
Füstös, J., Gramann, K., Herbert, B. M., and Pollatos, O. (2013). On the embodiment of emotion regulation: interoceptive awareness facilitates reappraisal. Soc. Cogn. Affect. Neurosci. 8, 911–917. doi: 10.1093/scan/nss089
Geller, J., and Cockell, S. J. And Goldner, E. M. (2000). Inhibited expression of negative emotions and interpersonal orientation in anorexia nervosa. Int. J. Eat. Disord. 28: 8–19. doi: 10.1002/1098-108x(200007)28:1<8::aid-eat2>3.0.co;2-u
Gross, J. J. (1998). Antecedent-and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J. Pers. Soc. Psychol. 74, 224–237. doi: 10.1037//0022-3514.74.1.224
Gross, J. J. (2015). Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26. doi: 10.1080/1047840X.2014.940781
Gross, J. J., and John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85, 348–362. doi: 10.1037/0022-3514.85.2.348
Gross, J. J., and Thompson, R. A. (2007). “Emotion regulation: conceptual foundations” in Handbook of Emotion Regulation. ed. J. J. Gross (New York, NY: Guilford Press), 3–26.
Hayaki, J., Friedman, M., and Brownell, K. D. (2002). Emotional expression and body dissatisfaction. Int. J. Eat. Disord. 31, 57–62. doi: 10.1002/eat.1111
Hayes, A. F. (2017). Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. 2nd Edn. New York: The Guilford Press.
Haynos, A. F., and Fruzzetti, A. E. (2011). Anorexia nervosa as a disorder of emotion dysregulation: evidence and treatment implications. Clin. Psychol. Sci. Pract. 18, 183–202. doi: 10.1111/j.1468-2850.2011.01250.x
Hodgkinson, E. L., Smith, D. M., and Wittkowski, A. (2014). Women’s experiences of their pregnancy and postpartum body image: a systematic review and meta-syntehsis. BMC Pregnancy Childbirth 14, 1–11. doi: 10.1186/1471-2393-14-330
Hrabosky, J. I., Cash, T. F., Veale, D., Neziroglu, F., Soll, E. A., Garner, D. M., et al. (2009). Multidimensional body image comparisons among patients with eating disorders, body dysmorphic disorder, and clinical controls: a multisite study. Body Image 6, 155–163. doi: 10.1016/j.bodyim.2009.03.001
Huang, H. C., Wang, S. Y., and Chen, C. H. (2004). Body image, maternal-fetal attachment, and choice of infant feeding method: a study in Taiwan. Birth 31, 183–188. doi: 10.1111/j.0730-7659.2004.00303.x
Hughes, E. K., and Gullone, E. (2011). Emotion regulation moderates relationships between body image concerns and psychological symptomatology. Body Image 8, 224–231. doi: 10.1016/j.bodyim.2011.04.001
Hutcheson, G., and Sofroniou, N. (1999) The Multivariate Social Scientist: Introductory Statistics Using Generalized Linear Models. Thousand Oaks, CA: Sage Publication
Jones, N., and Rogers, P. J. (2003). Preoccupation, food, and failure: an investigation of cognitive performance deficits in dieters. Int. J. Eat. Disord. 33, 185–192. doi: 10.1002/eat.10124
Kiriukhina, N. A., and Polskaya, N. A. (2021). Emotion dysregulation and body dissatisfaction in female population. Clin. Psychol. Spec. Educ. 10, 126–147. doi: 10.17759/cpse.2021100308
Kraiss, J. T., Klooster, P. M., Moskowitz, J. T., and Bohlmeijer, E. T. (2020). The relationship between emotion regulation and well-being in patients with mental disorders: a meta-analysis. Compr. Psychiatry 102:152189. doi: 10.1016/j.comppsych.2020.152189
Lappanen, J., Brown, D., Mclinden, H., Williams, S., and Tchanturia, K. (2022). The role of emotion regulation in eating disorders: a netword meta-analysis approach. Front. Psychol. 13:793094. doi: 10.3389/fpsyt.2022.793094
Lavender, J. M., Wonderlich, S. A., Engel, S. G., Gordon, K. H., Kaye, W. H., and Mitchell, J. E. (2015). Dimensions of emotion dysregulation in anorexia nervosa and bulimia nervosa: a conceptual review of the empirical literature. Clin. Psychol. Rev. 40, 111–122. doi: 10.1016/j.cpr.2015.05.010
Levis, B., Negeri, Z., Sun, Y., Benedetti, A., and Thombs, B. D. (2020). Accuracy of the Edinburgh postnatal depression scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ 371, 1–11. doi: 10.1136/bmj.m4022
Loth, K. A., Bauer, K. W., Wall, M., Berge, J., and Neumark-Szteiner, D. (2012). Body satisfaction during pregnancy. Body Image 8, 297–300. doi: 10.1016/j.bodyim.2011.03.002
Lovering, M. E., Rodgers, R. F., George, J. E., and Franko, D. L. (2018). Exploring the tripartite influence model of body dissatisfaction in postpartum women. Body Image 24, 44–54. doi: 10.1016/j.bodyim.2017.12.001
Mcdonald, H. M., Sherman, K. A., and Kasparian, N. A. (2021). A mediated model of mindful awareness, emotion regulation, and maternal mental health during pregnancy and postpartum. Aust. J. Psychol. 73, 368–380. doi: 10.1080/00049530.2021.1908846
Mclean, C. P., Miller, N. A., and Hope, D. A. (2007). Mediating social anxiety and disordered eating: the role of expressive suppression. Eat. Disord. 15, 41–54. doi: 10.1080/10640260601044485
Miu, A. C., Szentágotai-Tătar, A., Balázsi, R., Nechita, D., Bunea, I., and Pollak, S. D. (2022). Emotion regulation as a mediatore between childhood adversity and psychopathology: a meta analysis. Clin. Psychol. Rev. 93, 1–11. doi: 10.1016/j.cpr.2022.102141
Nagl, M., Jepsen, L., Linde, K., and Kersting, A. (2021). Social media use and postpartum body image dissatisfaction: the role of appearance-related social comparisons and thin-ideal internalisation. Midwifery 100:103038. doi: 10.1016/j.midw.2021.103038
Naumann, E., Tuschen-Caffier, B., Voderholzer, U., Schäfer, J., and Svaldi, J. (2016). Effects of emotional acceptance and rumination on media-induced body dissatisfaction in anorexia and bulimia nervosa. J. Psychiatr. Res. 82, 119–125. doi: 10.1016/j.jpsychires
Neiterman, E., and Fox, B. (2017). Controlling the unruly maternal body: losing and gaining control over the body during pregnancy and the postpartum period. Soc. Sci. Med. 174, 142–148. doi: 10.1016/j.socscimed.2016.12.029
Newham, J. J., and Martin, C. R. (2013). Measuring fluctuations in maternal well-being across pregnancy. J. Reprod. Infant Psychol. 31, 531–540. doi: 10.1080/02646838.2013.834040
Pearson, R. M., Evans, S. L., and Evans, J. (2009). Emotional sensitivity for motherhood: late pregnancy is associated with enhanced accuracy to encode emotional faces. Horm. Behav. 56, 557–563. doi: 10.1016/j.yhbeh.2009.09.013
Penner, F., and Rutherford, H. K. (2022). Emotion regulation during pregnancy: a call for action for increased research, screening and intervention. Archiv. Women Mental Health 25, 527–531. doi: 10.1007/s00737-022-01204-0
Phillips, K. A. (2005). The Broken Mirror: Understanding and Treating Body Dysmorphic Disorder. USA: Oxford University Press
Preacher, K. J., and Hayes, A. F. (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behav. Res. Methods 40, 879–891. doi: 10.3758/BRM.40.3.879
Preece, D. A., Becerra, R., Hasking, P., Mcevoy, P. M., Boyes, M., Sauer-Zavala, S., et al. (2021). The emotion regulation questionnaire: psychometric properties and relations with affective symptoms in a United States general community sample. J. Affect. Disord. 284, 27–30. doi: 10.1016/j.jad.2021.01.071
Preece, D. A., Becerra, R., Robinson, K., and Gross, J. J. (2020). The emotion regulation questionnaire: psychometric properties in general community samples. J. Pers. Assess. 102, 348–356. doi: 10.1080/00223891.2018.1564319
Prefit, A. B., Cândea, D. M., and Szentagotai-Tātar, A. (2020). Effects of acceptance and reappraisal on body dissatisfaction: an experimental comparison of two adaptive emotion regulation strategies. Eat. Weight Disord. Stud. Anorex. Bulimia Obes. 25, 803–809. doi: 10.1007/s40519-019-00691-y
Richardson, P. (1990). Women’s experiences of body change during normal pregnancy. Matern. Child Nurs. J. 19, 93–111.
Riquin, E., Lamas, C., Nicolas, I., Dugre Lebigre, C., Curt, F., Cohen, H., et al. (2019). A key for perinatal depression early diagnosis: the body dissatisfaction. J. Affect. Disord. 245, 340–347. doi: 10.1016/j.jad.2018.11.032
Rutherford, H. J. V., Wallace, N. S., Laurent, H. K., and Mayes, L. C. (2015). Emotion regulation in parenthood. Dev. Rev. 36, 1–14. doi: 10.1016/j.dr.2014.12.008
Shloim, N., Rudolf, M. C. J., Feltbower, R. G., Blundell-Birtill, P., and Hetherington, M. M. (2019). Israeli and British women’s wellbeing and eating behaviours in pregnancy and postpartum. J. Reprod. Infant Psychol. 37, 123–138. doi: 10.1080/02646838.2018.1529408
Siân, A., Mclean, B. S., Paxton, S. J., and Wertheim, E. H. (2010). Factors associated with body dissatisfaction and disordered eating in women in midlife. Int. J. Eat. Disord. 43, 527–536. doi: 10.1002/eat.20737
Silveira, M. L., Ertel, K. A., Dole, N., and Chasan-Taber, L. (2015). The role of body image in prenatal and postpartum depression: a critical review of the literature. Arch. Womens Ment. Health 18, 409–421. doi: 10.1007/s00737-015-0525-0
Sim, L., and Zeman, J. (2005). Emotion regulation factors as mediators between body dissatisfaction and bulimic symptoms in early adolescent girls. J. Early Adolesc. 25, 478–496. doi: 10.1177/0272431605279838
Sim, L., and Zeman, J. (2006). The contribution of emotion regulation to body dissatisfaction and disordered eating in early adolescent girls. J. Youth Adolesc. 35, 207–216. doi: 10.1007/s10964-005-9003-8
Skouteris, H., Carr, R., Wertheim, E. H., Paxton, S. J., and Duncombe, D. (2005). A prospective study of factors that lead to body dissatisfaction during pregnancy. Body Image 2, 347–361. doi: 10.1016/j.bodyim.2005.09.002
Slomian, J., Honvo, G., Emonts, P., Reginster, J. Y., and Bruyère, O. (2019). Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Women Health 15:174550651984404. doi: 10.1177/1745506519844044
Stellern, J., Xiao, K. B., Grennell, E., Sanches, M., Gowin, J. L., and Sloan, M. (2023). Emotion regulation in substance use disorders: a systematic review and meta-analysis. Addiction 118, 30–47. doi: 10.1111/add.16001
Sweeney, A. C., and Fingerhut, R. (2013). Examining relationships between body dissatisfaction, maladaptive perfectionism, and postpartum depression symptoms. J. Obstet. Gynecol. Neonatal. Nurs. 42, 551–561. doi: 10.1111/1552-6909.12236
Tabachnick, B. G., and Fidell, L. S. (2013). Using Multivariate Statistics (6th ed.). Boston, MA: Pearson
Taubman-Ben-Ari, O., Chasson, M., Horowitz, E., Azuri, J., and Davidi, O. (2021). Personal growth in early pregnancy: the role of perceived stress and emotion regulation. J. Reprod. Infant Psychol. 40, 550–562. doi: 10.1080/02646838.2021.1925096
Tavakoli, M., Hasanpoor-Azghady, S. B., and Farahani, L. A. (2021). Predictors of mother’s postpartum body dissatisfaction based on demographic and fertility factors. BMC Pregnancy Childbirth 21:8. doi: 10.1186/s12884-020-03501-x
Watson, B., Fuller-Tyszkiewicz, M., Broadbent, J., and Skouteris, H. (2015). The meaning of body image experiences during the perinatal period: a systematic review of the qualitative literature. Body Image 14, 102–113. doi: 10.1016/j.bodyim.2015.04.005
Webster, J., and Tiggemann, M. (2003). The relationship between Women’s body satisfaction and self-image across the life span: the role of cognitive control. J. Genet. Psychol. Res. Theory Hum. Dev. 164, 241–252. doi: 10.1080/00221320309597980
Williams, K. (2019). The relationship between body image and mother to infant attachment in the postpartum period Doctoral dissertation, University of Leeds.
Wilson, A. C., Wilhelm, S., and Hartmann, A. S. (2014). Experiential avoidance in body dismorphic disorder. Body Image 11, 380–383. doi: 10.1016/j.bodyim.2014.06.006
Keywords: pregnancy, emotion regulation strategies, body image disturbances, cognitive reappraisal, postpartum body image
Citation: Spinoni M, Singh Solorzano C and Grano C (2023) A prospective study on body image disturbances during pregnancy and postpartum: the role of cognitive reappraisal. Front. Psychol. 14:1200819. doi: 10.3389/fpsyg.2023.1200819
Edited by:
Erika Comasco, Uppsala University, SwedenReviewed by:
Ingela Lundin Kvalem, University of Oslo, NorwayGiulia Casu, University of Bologna, Italy
Copyright © 2023 Spinoni, Singh Solorzano and Grano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Caterina Grano, Y2F0ZXJpbmEuZ3Jhbm9AdW5pcm9tYTEuaXQ=
 Marta Spinoni
Marta Spinoni Claudio Singh Solorzano
Claudio Singh Solorzano Caterina Grano
Caterina Grano