
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychol. , 29 June 2023
Sec. Psychology for Clinical Settings
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1193608
Objective: This study aimed to explore the effectiveness and applicability of a psychological intervention using virtual reality (VR) to reduce preoperative anxiety in patients undergoing carotid artery stenting (CAS).
Methods: A total of 114 patients aged 18–86 years who were scheduled to undergo CAS were randomized to the VR and control groups. Patients in the VR group used a VR headset to view a 16-min psychological intervention video, while those in the control group used a tablet for viewing. The primary assessment instrument was the State Anxiety Inventory (S-AI), which was given 20 min before and after the intervention and 24 h after surgery. Secondary assessment tools were the Self-efficacy for Managing Chronic Disease (SEMCD-6) scale, which was completed before the intervention and 24 h after the operation, a smart bracelet to assess sleep quality, monitored in the evening before the operation, and the VR Suitability and Satisfaction Questionnaire, completed 24 h after the operation.
Results: The two groups were similar in terms of demographic information, preintervention STAI scores and preintervention SEMCD-6 scores (p > 0.05). S-AI scores were lower in both groups after the intervention and surgery, and the scores of the VR group were lower than those of the control group (p = 0.036, p = 0.014). SEMCD-6 scores post-surgery had improved in both groups, but the VR group had significantly higher scores than the control group (p = 0.005). Smart bracelet measurements showed no significant differences in postintervention sleep quality between the two groups (p = 0.540). For satisfaction, the VR group scored higher in all aspects except scheduling. A total of 47 (85.45%) patients reported having a comfortable experience, and only 5 (9.09%) experienced mild adverse effects.
Conclusion: The use of a virtual reality psychological intervention was beneficial to reduce the anxiety of patients before CAS and improved their self-efficacy. As virtual reality devices evolve and demonstrate better comfort and safety, more comprehensive and in-depth research of the use of VR to reduce patient anxiety should be performed in the future.
Clinical trial registration:https://www.chictr.org.cn/showproj.aspx?proj=186412, identifier ChiCTR2200066219.
According to data from a global disease burden study, stroke is the second leading cause of death around the world and the leading cause of death and disability among adults in China (GBD 2019 Stroke Collaborators, 2021). The prevention and timely treatment of stroke is of paramount importance. After continuous development, carotid artery stenting (CAS), as a minimally invasive intervention, has become an important means to prevent and treat ischemic stroke and is a positive complement to classic carotid endarterectomy (Gaba et al., 2018; AbuRahma et al., 2022). Preoperative anxiety is associated with postoperative acute and chronic pain, nausea, and cognitive dysfunction and may even increase postoperative morbidity and mortality (Williams et al., 2013; Suffeda et al., 2016). A meta-analysis indicated that the preoperative anxiety of patients undergoing elective surgery has always been an urgent problem, and social support plays an important role (Friedrich et al., 2022; Kok et al., 2022). Although anti-anxiety drugs are usually used before an operation to improve patients’ comfort, randomized controlled trials have shown that they may cause adverse reactions such as dyspnea, drowsiness, anesthetic interference, and prolonged recovery time (Kain et al., 2000; Maurice-Szamburski et al., 2015). Studies have suggested that patients with preoperative anxiety disorders may also benefit from a variety of nonpharmacological approaches, such as cognitive behavioral therapy, music therapy, and relaxation therapy (Wang et al., 2022).
New techniques have been implemented in the health care industry; for instance, artificial intelligence has been implemented in image identification and disease diagnosis (Lee and Yoon, 2021). Computer technology is the core of virtual reality (VR) technology, and special input/output equipment creates an interactive simulation system between people and the virtual environment. Through visual, auditory and tactile feedback, users can feel a sense of immersion (Slater, 2018; Riva et al., 2019; Ugras et al., 2022). Of all VR devices, the most realistic is the 720 viewing angle immersive virtual experience offered by head-mounted displays (HMDs) (Cipresso et al., 2018). As an emerging technology, VR has gradually been applied to clinical patient research in addition to its wide application in medical education, such as anatomy education and operation training for surgeons and nurses (Mahmood et al., 2018; Sun et al., 2022). Interventions for negative patient emotions, including anxiety and stress, have become an important area for VR applications. First, VR could provide immersive meditation relaxation as a distraction to alleviate pain, anxiety and depression (Darnall et al., 2020; Ong et al., 2020; Bosso et al., 2022). Second, it can ease fear and anxiety during surgery or treatment by making patients more aware and familiar with medical procedures through virtual reality exposure (Ekelis et al., 2017; Kapikiran et al., 2022; Ugras et al., 2022). The unique, imaginary and interactive characteristics of VR intervene to promote better immersion, interest and compliance to obtain a better intervention effect (Chen et al., 2021; Xuefang et al., 2021; Zhang et al., 2021). In some medical centers, VR has been used for the health education and psychological care of surgical patients to help them face the disease and surgery in a positive way (Collins et al., 2018; Balsam et al., 2019; Noben et al., 2019; Chan et al., 2020; Hendricks et al., 2020; Turan et al., 2021; Hermans et al., 2023).
However, most previous studies have failed to compare the effects of VR and regular screen interventions or combine virtual exposure and distraction interventions. At the same time, we did not retrieve any research on VR anxiety interventions for CAS patients. Therefore, we used the latest HMD device to verify whether the preoperative anxiety of CAS patients can be reduced with a comprehensive VR psychological intervention.
This study was designed following the CONSORT reporting guidelines and was a single-blind, single-center clinical trial conducted from November 2022 to February 2023 at a tertiary public hospital in Chengdu, China. Patients undergoing CAS treatment for the first time were randomized into the control group or VR group for the preoperative psychological intervention (Figure 1). The trial protocol was approved by the Medical Ethics Committee of West China Hospital, Sichuan University (No: 2022/1427), and the participants provided written consent. The study has been registered as a clinical trial (No: ChiCTR2200066219).
This study included 128 patients from the Department of Neurology, West China Hospital, Sichuan University. The inclusion criteria were as follows: inpatients aged 18–90 years who met the surgical and anesthetic guidelines and were scheduled to undergo CAS. The exclusion criteria included (1) a communication or cognitive impairment to understanding and cooperating in the trial; (2) symptoms such as dizziness, headache, or vomiting that were inappropriate for the use of VR equipment; (3) an audio-visual impairment to wearing and viewing VR videos (e.g., eye disease); (4) a previous history of CAS; and (5) a history of epilepsy or psychosis. The risks and benefits of this study were explained to all patients who met the inclusion criteria, and the participants signed informed consent forms for the trial 1 day before the procedure. Ultimately, 114 individuals were included for randomization grouping. Demographic information included in the assessment included age, sex, residence, education level, income, comorbidities, the duration of illness, sleep quality and the number of stents. No remuneration was provided to the patients in this study.
Patients were randomly assigned at a ratio of 1:1 to the control or VR intervention group by the computerized random number generator WRandom1.0 (Lezhizhe Co., Ltd., Shengzhen, China). Random numbers were confidentially assigned to patients by a separate nurse using an envelope who was not involved in any subsequent interventions and outcome assessments. All patients were operated on by the same group of physicians on Mondays, Wednesdays, and Fridays, and outcomes were evaluated by another investigator without knowledge of the subgroups and interventions. Due to differences in intervention equipment, the patients and their families were not blinded.
The whole intervention video lasted for 18 min and consisted of three parts: Part 1: Introduction to the surgery (4 min). This part included an introduction to the operating room and CAS simulation animation, which was produced by Feiteng Culture Communication (Hefei, China) with the participation of clinical nurses, surgeons, and anesthesiologists from the neurology department. Part 2: Patient interview (8 min). This part included an interview with 5 postoperative patients and their families, focusing on feelings about the surgery, coping with anxiety and blessings. The interviews were filmed in the neurology ward using a professional Insta360 VR camera (Insta Corp, Shenzhen China) and edited and produced by professionals. Part 3: Scenic tour (5 min). The scenes were selected from the most frequently used scenes in previous studies, such as beaches, waterfalls, and forests, and the copyrights were purchased from online platforms (The interview outline and intervention video are in Annexes 1, respectively).
For the intervention group, the YVR2 device was used (Yuweia Technology Corp, Shanghai, China). It is an advanced HMD with Pancake’s ultra-short-focus optical technology (Yuweia Technology Co., Ltd., 2023). The pancake optical technology makes VR devices at least 40% less thick and is supposed to effectively address blurring and distortion at the edges of the field of view to reduce dizziness and improve user comfort and immersion (Cakmakci et al., 2021). For the control group, we used an iPad Air (Apple Inc., California, USA) as the video intervention tool.
Psychological care was provided for patients by a uniformly trained clinical nurse on the ward the afternoon before surgery. The routine consisted of the clinical nurse introducing herself to the patient, gaining trust to assess their anxiety, and then providing comfort and support as needed. In addition, patients were invited to watch a video of the intervention on an iPad Air. Of course, this is a flat version of the video, and patients can only see a frontal view. The aim was to enable patients to fully understand the procedure, receive support from other patients and mentally relax.
Clinical nurses conducted routine psychological care with patients the afternoon before surgery. Then, the patient was asked to watch the intervention video with the VR equipment, and the video content was the same as that of the control group. The device could track head movements, and patients could enjoy various images in the panorama video from any angle (Figure 2). The device was disinfected with alcohol wipes before use and equipped with disposable eye protection shields to prevent cross-contamination.
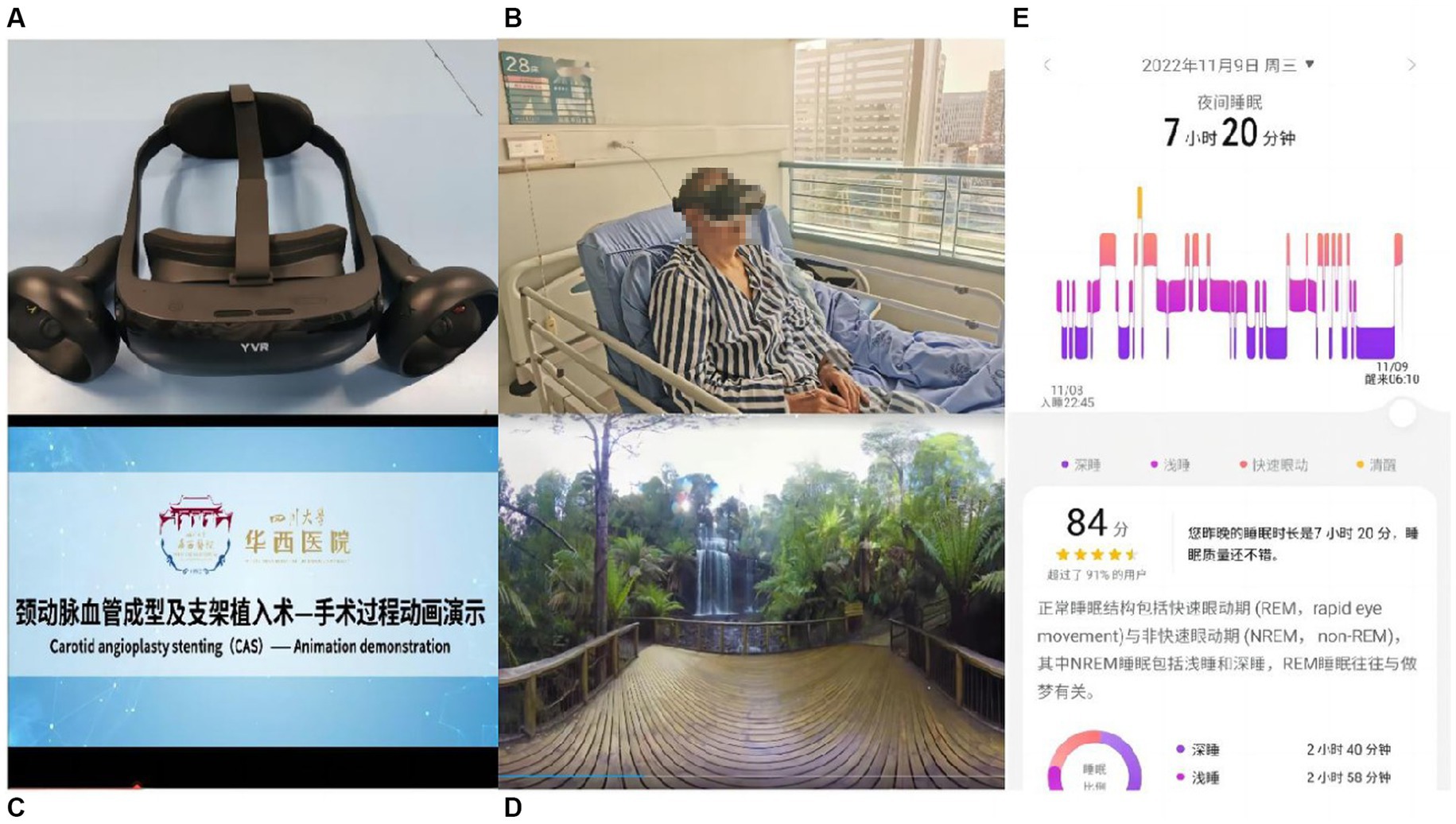
Figure 2. Overview of virtual reality (VR) hardware and intervention. (A) Superior view of the virtual reality (VR) headmet. (B) VR device on the patient. (C) Animation video screenshot of the operation. (D) Screenshot of natural scenery sightseeing video. (E) Screenshot of sleep monitoring application.
The state–trait anxiety inventory (STAI) is a valuable tool for presurgical anxiety assessment and is widely used in anxiety-related scientific research. It was developed by Charles D. Spielberg et al. and includes 2 subscales: the State Anxiety Inventory (S-AI) and the Trait Anxiety Inventory (T-AI). The S-AI describes an unpleasant emotional experience that is generally transient. The T-AI, on the other hand, is used to describe a relatively stable anxiety tendency that is a personality trait with individual differences. The two subscales consist of 20 questions each and are scored on a 4-point Likert scale, with a total score of 20–80, with higher scores representing higher levels of anxiety (Spielberger, 1983). In this study, the S-AI was selected as the main outcome, and Cronbach’s α coefficient was 0.923.
Baseline sleep quality was assessed using the Pittsburgh Sleep Quality Index (PSQI) before the intervention (the Chinese version of the PSQI’s Cronbach’s α coefficient is 0.832). The postintervention evaluation of sleep quality was based on the Huawei Smart Bracelet 7 (HUAWEI Corp, China). The bracelet connects to a mobile app via Bluetooth and generates a sleep report that covers sleep duration, deep sleep, light sleep, REM sleep ratio, the number of awakenings, and the sleep quality score. Since the procedure was scheduled 1 day in advance, sleep monitoring was only performed on the night before surgery.
The scale was designed by Lorig et al. at Stanford University to reflect the self-efficacy of patients with chronic diseases regarding symptom management, role functioning, emotional control, and communication with physicians. The SEMCD-6 scale includes 2 dimensions of disease symptom management (Items 1–4) and disease co-occurrence management (Items 5–6), with 6 items in total. Each item is scored from “not confident at all” to “absolutely confident” on a scale of l to 10, and the total self-efficacy score is the mean score of each item. The higher the patient’s score is, the higher their level of self-efficacy. When the self-efficacy score is >7, the likelihood of completing a task or behavior increases (Lorig et al., 2001). Cronbach’s α coefficient of the SEMCD-6 scale is 0.90.
This is a self-developed questionnaire, including 5 aspects: form of intervention, content design, schedule, manners, and communication. This questionnaire is scored using a 5-point Likert scale, with 1 = particularly dissatisfied, 2 = unsatisfied, 3 = acceptable, 4 = satisfied, and 5 = very satisfied. The maximum total score is 25, and this score indicates the level of patient satisfaction. Cronbach’s α coefficient of the PISQ is 0.82.
This is a self-developed questionnaire that includes 4 aspects: comfort of use, fatigue, reuse intention, and discomfort symptoms. This questionnaire was only completed by the patients in the VR intervention group to investigate their feelings of use and safety. The assessment time was 20 min after the intervention.
As mentioned earlier, our psychological intervention was provided the afternoon before the operation. Before the intervention, we extracted patient demographic data from the medical record system, and we asked the patient for information that was not included in the system. Then, the patients were evaluated with the PQSI, STAI, and SECD-6 scales. At 20 min after the intervention, anxiety was assessed with the S-AI, and a Huawei Smart Bracelet 7 was worn to monitor sleep quality. Finally, 24 h after the operation, we evaluated the patients for the last time with the S-AI, SECD-6 scale, Psychological Care Satisfaction Questionnaire and Patient VR Adaptation Questionnaire.
The main outcome indicator of this study was the S-AI score, and concerning the experimental results, the standard deviation of the difference between the S-AI scores of the two groups was σ = 3.1 points and the tolerance error was δ = 3.4 points According to the formula n1 = n2 = 51. In addition, a 20% data incompleteness rate was expected, and a total of 124 patients was required for the sample.
In this study, all data are presented as the mean (SD), median (IQR), or number (%). SPSS 24.0 for Windows (IBM, Corp) was used for all statistical analyses. T tests or Mann–Whitney U tests were used to analyze continuous variables (age, anxiety scores, satisfaction scores, self-efficacy scores) and ordered categorical variables (education level, income, duration of illness, alcohol consumption, smoking). The χ2 test was used for categorical variables (sex, residence, comorbidity history, type of anesthesia, etc.). Repeated measure ANOVA was used for the analysis of multiple continuous variables (S-AI scores). If Mauchly’s test of sphericity was satisfied (p ≥ 0.05), the within-subjects effect test was used, and when it was not satisfied (P<0.05), using Greenhouse–Geisser correction. When the interaction effects showed significant differences, further simple effects analysis was used. A p value less than 0.05 was considered statistically significant.
As shown in Figure 1, a total of 128 patients were initially planned to be included in the study, while 114 patients were randomized into the two groups, with 52 completing the final intervention in the control group (age 64.8 ± 11.3 years) and 55 completing the final intervention in the VR group (age 65.2 ± 10.0 years). Baseline data for all general information were comparable in both groups (Table 1). There was a male predominance (control group 84.6% vs. VR group 78.2%), which was in line with the epidemiological characteristics of stroke. In terms of regional factors, patients from rural areas accounted for more than half of the sample (control group 51.9% vs. VR group 54.5%), and most of the patients had a junior/vocational school education or less (control group 90.4% vs. VR group 79.2%), which may lead to a low level of awareness of the disease and a high level of anxiety. The difference in the PSQI (Pittsburgh Sleep Quality Index) scores between the two groups was not statistically significant (control group 9.19 ± 3.59 vs. VR group 9.25 ± 3.26, p = 0.931), indicating that their mean sleep quality in the last month was similar. STAI scores (Split into the S-AI and T-AI scores) were at comparable levels in both groups before the intervention (p = 0.993, p = 0.915). In addition, most patients had other serious comorbidities (control group 76.9% vs. VR group 76.4%), and most procedures were performed with a single stent placed under local anesthesia.
S-AI scores were analyzed using a two-way repeated measures ANOVA. Since the data did not meet the Mauchly’s spherical hypothesis test (p = 0.000), Greenhouse–Geisser correction was used. The test showed a statistically significant group*time interaction, F (Interaction) = 3.355, p = 0.048.
Before the intervention, the difference between the control group (48.94 ± 9.48) and the VR group (48.93 ± 10.47) was not statistically significant (p = 0.994 > 0.05); after the intervention, the difference between the control group (43.46 ± 8.53) and the VR group (40.11 ± 7.77) was statistically significant (p < 0.001); at the time of the operation, the difference between the control group (38.27 ± 6.83) and the VR group (35.02 ± 6.59) was statistically significant (p < 0.001) (Tables 1, 2).
Using simple effects analysis, statistically significant differences (p < 0.001) were found between pre-intervention (48.94 ± 9.48) and post-intervention (43.46 ± 8.53) and between pre-intervention (48.94 ± 9.48) and pre-operation (38.27 ± 6.83) in the control group; the differences between post-intervention (43.46 ± 8.53) and pre-operation (38.27 ± 6.83) were statistically significant (p < 0.001). In the VR group, the differences between pre-intervention (48.93 ± 10.47) and post-intervention (40.11 ± 7.77) and between pre-intervention (48.93 ± 10.47) and pre-operation (35.02 ± 6.59) were statistically significant (p < 0.001); the differences between post-intervention (40.11 ± 7.77) and pre-operation (35.02 ± 6.59) was statistically significant (p < 0.001) (Table 3).
Overall, the S-AI scores were at the same level in both groups before the intervention, and both showed a decreasing trend with time progression after the intervention, but the scores in the VR group were significantly lower than those in the control group both after and before the intervention (p < 0.01) (Figure 3).
The results of sleep quality monitored by the smart bracelet showed no substantial differences in any evaluation aspects, especially in sleep quality scores (control group 72.25 ± 8.69 vs. VR 76.27 ± 8.52, p = 0.540) (Table 2). In terms of SEMCD-6 scores, there was no significant difference between the two groups before the intervention (control group 6.33 ± 1.22 vs. VR group 6.27 ± 1.13, p = 0.772) (Table 2). The post operation SEMCD-6 score was higher in the VR group than in the control group, and the difference was statistically significant (control group 7.25 ± 0.95 vs. VR group 7.82 ± 1.08, p = 0.005). Referring to satisfaction ratings, all sections and total scores were significantly higher in the VR group than in the control group, except for the “Schedule” section, where the difference between the two groups was not considerable (control group 4.0 [4.0, 5.0] vs. VR group 5.0 [5.0, 5.0], p = 0.079) (Table 2).
Regarding the applicability of the VR intervention, 47 (85.45%) patients reported that they felt relatively or extremely comfortable and would like to use it again, and 48 (87.27%) patients reported almost or no fatigue while using the device (Table 4). Regarding discomfort symptoms, 5 (9.09%) patients eventually complained of mild adverse effects, including dizziness, nausea, and palpitations, which were resolved with short breaks.
This study combined a previous VR exposure stimulation intervention and distraction intervention, making patients familiar with the operation process by using peer support and animation demonstration and alleviating their nervousness by using a virtual sightseeing experience. The results indicated that an improved psychological care effect was achieved.
After decades of development, CAS has become an important measure for stroke prevention and treatment (Gaba et al., 2018; AbuRahma et al., 2022), and perioperative physiological indicators, particularly blood pressure stability, are essential for the safety and prognosis of CAS surgery (AbuRahma et al., 2022). Preoperative anxiety in patients undergoing cerebrovascular surgery is common and may trigger a stress reaction in the body, causing sympathetic nerve excitement and hormone disorders (Sun et al., 2021; Liu et al., 2023). It also leads to abnormal changes in physiological indicators such as blood pressure, heart rate, and blood glucose and affects the prognosis of surgery (Cusack and Buggy, 2020). The preoperative anxiety of the patients in our study was high, which is also consistent with the findings of a large sample study reporting that more than 40% of adult patients undergoing elective surgery were in a high state of anxiety preoperatively (Aust et al., 2018). Studies have demonstrated that preoperative psychological care is an important way of reducing patients’ negative emotions and enhancing their self-efficacy, and many innovative approaches can be effective in enhancing the effects of psychological care (Hanalis-Miller et al., 2022).
Our study showed that compared with baseline, after the psychological intervention, the state anxiety of the CAS patients was reduced, and that in the VR group was more obviously relieved. Namely, nursing care through immersion virtual reality has a deeper influence on patients, which is consistent with the effectiveness of VR interventions in reducing preoperative anxiety reported in previous studies (Niki et al., 2020; Turrado et al., 2021). Multiple studies have noted that preoperative anxiety in children undergoing elective surgery and general anesthesia is significantly reduced by preoperative virtual experiences or distraction therapy in the operating room (Park et al., 2019; Chen et al., 2022). Our findings may further support this opinion in adult interventional procedures. First, the main reason may be that patients’ fear of the unknown can be effectively reduced when they obtain correct medical information comprehensively and as much as possible before the operation (Ayyadhah Alanazi, 2014; Tulloch and Rubin, 2019). Second, VR videos enable patients to focus on the intervention and avoid distractions due to the surrounding environment, which can further improve the effectiveness of patient care (Bosso et al., 2022). In addition, studies have suggested that VR video relaxation meditation can improve patients’ sleep quality before surgery, thereby supporting its effectiveness in reducing anxiety in patients, but no positive result was obtained in this study (Goldenhersch et al., 2022). In summary, VR psychological interventions have unique advantages in improving patients’ cognition of the operation and dispersing stress emotions, which is more conducive to reducing preoperative anxiety.
The sleep quality score is an important indicator for evaluating the degree of anxiety, which can cause decreased sleep quality and insomnia. Unfortunately, in our study, there was no significant difference in preoperative sleep quality monitored by the HUAWEI smart bracelet 7 between the two groups, which might be because the duration or frequency of the intervention was not sufficient to cause observable differences. The change in self-efficacy for managing chronic disease (SEMCD-6) is a secondary evaluation standard, which involves a patient’s confidence and beliefs in adhering to the long-term treatment of their disease. Higher self-efficacy was associated with better health, aggressive treatment behaviors, and mental health (Levett and Grimmett, 2019; Incirkuş and Özkan Nahcivan, 2020). Previous studies have shown that self-efficacy has a significant negative correlation with emotional disorders such as anxiety and depression, and self-efficacy improvement plays an important role in reducing anxiety in patients (Lorig et al., 2001; Tsay and Chao, 2002). The patients in the VR group, who had higher SEMCD-6 scores, had greater confidence and initiative regarding the treatment after receiving psychological care. This also proves the conclusion that VR interventions could reduce preoperative anxiety more effectively, which was similar to the research of Chang et al. (2021) on cardiovascular intervention surgery. In terms of patient satisfaction, the VR group had a significantly higher score than the control group, and there was no significant difference except for “Schedule.” The patients expressed high levels of interest and support for the VR intervention method. Surgical demonstration and patient-supported content enabled patients to increase positive cognition and have good expectations for the surgery, and the natural and scenic immersion experience enabled patients to be well adjusted during the closed-loop management of the ward due to COVID-19. Therefore, the results of this study also suggested the potential application value of VR devices for psychological interventions in closed-loop management and unaccompanied medical units in the future.
The VR suitability survey for the VR group showed that the vast majority (92.45%) of patients indicated that the VR device was comfortable during use and that they would like to experience it again. Very few patients (9.09%) reported slight discomfort during use, but all patients completed the intervention, and their vertigo and fatigue were relieved after rest without serious adverse reactions. In general, VR devices have good applicability for patients undergoing cerebrovascular stenting.
This study has the following limitations. First, the trial was a single-center study at a national critical care center in Chengdu, China. The cognitive level determined by demographic factors such as the educational level and economic condition may only represent a local level in the southwest region of China, which may limit the generalizability of our study results. Second, the intervention was mainly evaluated using scales, and patient satisfaction and anxiety levels may need more physiological indicators for further verification. Third, this study cannot point out the specific mechanism why VR is better than tablet in relieving anxiety. Because we have applied the comprehensive intervention of virtual exposure and distraction, it is impossible to distinguish which of the two methods is more effective. Finally, some stroke patients with poor consciousness and those who were unable to cooperate were excluded, which makes the application effect of VR equipment in more critical patients unclear and may bias the research results. In the future, more studies with scientific research designs should be conducted.
The VR-based psychological intervention was beneficial to reduce patients’ anxiety before CAS and improve their self-efficacy. With the development and update of technology, VR has already shown better comfort and safety. In future research, more objective evaluation criteria should be explored to evaluate the VR intervention effect more accurately. At the same time, we need to further optimize the intervention content to improve the effect of clinical application.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
The studies involving human participants were reviewed and approved by the Medical Ethics Committee of West China Hospital, Sichuan University. The patients/participants provided their written informed consent to participate in this study.
YL and RW: concept and design, and drafting of the manuscript. YL, RW, and YZ: acquisition, analysis, or interpretation of data. LF and WH: critical revision of the manuscript for important intellectual content and obtained funding and supervision. YL: statistical analysis. WH: administrative, technical, or material support. All authors contributed to the article and approved the submitted version.
This study was supported by the National Key Clinical Specialties Construction Project and West China Nursing Discipline Development Special Fund Project, Sichuan University, No: HXHL21004/HXHL20021.
Sincere thanks to the physicians and nurses from Department of Neurology, Intervention Surgery Center, and psychologists from the Mental Health Center, West China hospitals. Thanks for their guidance for our research and assistance in video capture and data collection. The authors would also like to thank the patients who participated in the video capture and for sharing their surgical feelings.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1193608/full#supplementary-material
AbuRahma, A. F., Avgerinos, E. D., Chang, R. W., Darling, R. C., Duncan, A. A., Forbes, T. L., et al. (2022). The Society for Vascular Surgery implementation document for management of extracranial cerebrovascular disease. J. Vasc. Surg. 75, 26S–98S. doi: 10.1016/j.jvs.2021.04.074
Aust, H., Eberhart, L., Sturm, T., Schuster, M., Nestoriuc, Y., Brehm, F., et al. (2018). A cross-sectional study on preoperative anxiety in adults. J. Psychosom. Res. 111, 133–139. doi: 10.1016/j.jpsychores.2018.05.012
Ayyadhah Alanazi, A. (2014). Reducing anxiety in preoperative patients: a systematic review. Br. J. Nurs. 23, 387–393. doi: 10.12968/bjon.2014.23.7.387
Balsam, P., Borodzicz, S., Malesa, K., Puchta, D., Tymińska, A., Ozierański, K., et al. (2019). Oculus study: virtual reality-based education in daily clinical practice. Cardiol. J. 26, 260–264. doi: 10.5603/CJ.a2017.0154
Bosso, L., Espejo, T., Taffé, P., Caillet-Bois, D., Christen, T., Berna, C., et al. (2022). Analgesic and anxiolytic effects of virtual reality during Minor procedures in an emergency department: a randomized controlled study. Ann. Emerg. Med. 81, 84–94. doi: 10.1016/j.annemergmed.2022.04.015
Cakmakci, O., Qin, Y., Bosel, P., and Wetzstein, G. (2021). Holographic pancake optics for thin and lightweight optical see-through augmented reality. Opt. Express 29, 35206–35215. doi: 10.1364/OE.439585
Chan, J. J. I., Yeam, C. T., Kee, H. M., Tan, C. W., Sultana, R., Sia, A. T. H., et al. (2020). The use of pre-operative virtual reality to reduce anxiety in women undergoing gynecological surgeries: a prospective cohort study. BMC Anesthesiol. 20:261. doi: 10.1186/s12871-020-01177-6
Chang, S.-L., Kuo, M.-J., Lin, Y.-J., Chen, S.-A., Chen, C.-T., Yang, Y.-Y., et al. (2021). Virtual reality-based preprocedural education increases preparedness and satisfaction of patients about the catheter ablation of atrial fibrillation. J. Chin. Med. Assoc. 84, 690–697. doi: 10.1097/JCMA.0000000000000555
Chen, Y.-J., Wang, C.-J., and Chen, C.-W. (2022). Effects of virtual reality on preoperative anxiety in children: a systematic review and meta-analysis of randomised controlled trials. J. Clin. Nurs. 32, 2494–2504. doi: 10.1111/jocn.16394
Chen, G., Zhao, Y., Xie, F., Shi, W., Yang, Y., Yang, A., et al. (2021). Educating outpatients for bowel preparation before colonoscopy using conventional methods vs virtual reality videos plus conventional methods: a randomized clinical trial. JAMA Netw. Open 4:e2135576. doi: 10.1001/jamanetworkopen.2021.35576
Cipresso, P., Giglioli, I. A. C., Raya, M. A., and Riva, G. (2018). The past, present, and future of virtual and augmented reality research: a network and cluster analysis of the literature. Front. Psychol. 9:2086. doi: 10.3389/fpsyg.2018.02086
Collins, M. K., Ding, V. Y., Ball, R. L., Dolce, D. L., Henderson, J. M., and Halpern, C. H. (2018). Novel application of virtual reality in patient engagement for deep brain stimulation: a pilot study. Brain Stimul. 11, 935–937. doi: 10.1016/j.brs.2018.03.012
Cusack, B., and Buggy, D. J. (2020). Anaesthesia, analgesia, and the surgical stress response. BJA Educ. 20, 321–328. doi: 10.1016/j.bjae.2020.04.006
Darnall, B. D., Krishnamurthy, P., Tsuei, J., and Minor, J. D. (2020). Self-administered skills-based virtual reality intervention for chronic pain: randomized controlled pilot study. JMIR Form. Res. 4:e17293. doi: 10.2196/17293
Ekelis, K., Calnan, D., Simmons, N., MacKenzie, T. A., and Kakoulides, G. (2017). Effect of an immersive preoperative virtual reality experience on patient reported outcomes: a randomized controlled trial. Ann. Surg. 265, 1068–1073. doi: 10.1097/SLA.0000000000002094
Friedrich, S., Reis, S., Meybohm, P., and Kranke, P. (2022). Preoperative anxiety. Curr. Opin. Anaesthesiol. 35, 674–678. doi: 10.1097/ACO.0000000000001186
Gaba, K., Ringleb, P. A., and Halliday, A. (2018). Asymptomatic carotid stenosis: intervention or best medical therapy? Curr. Neurol. Neurosci. Rep. 18:80. doi: 10.1007/s11910-018-0888-5
GBD 2019 Stroke Collaborators (2021). Global, regional, and national burden of stroke and its risk factors, 1990–2019: a systematic analysis for the global burden of disease study 2019. Lancet. Neurol. 20, 795–820. doi: 10.1016/S1474-4422(21)00252-0
Goldenhersch, E., Engelen, M., Urlings, J., Aardoom, J. J., Hilt, A. D., Woudenberg, T., et al. (2022). A preoperative virtual reality app for patients scheduled for cardiac catheterization: pre–post questionnaire study examining feasibility, usability, and acceptability. JMIR Cardio 6:29473. doi: 10.2196/29473
Hanalis-Miller, T., Nudelman, G., Ben-Eliyahu, S., and Jacoby, R. (2022). The effect of pre-operative psychological interventions on psychological, physiological, and immunological indices in oncology patients: a scoping review. Front. Psychol. 13:839065. doi: 10.3389/fpsyg.2022.839065
Hendricks, T. M., Gutierrez, C. N., Stulak, J. M., Dearani, J. A., and Miller, J. D. (2020). The use of virtual reality to reduce preoperative anxiety in first-time sternotomy patients: a randomized controlled pilot trial. Mayo Clin. Proc. 95, 1148–1157. doi: 10.1016/j.mayocp.2020.02.032
Hermans, A. N. L., Betz, K., Verhaert, D. V. M., den Uijl, D. W., Clerx, K., Debie, L., et al. (2023). 360° virtual reality to improve patient education and reduce anxiety towards atrial fibrillation ablation. Europace. 25, 855–862. doi: 10.1093/europace/euac246
Incirkuş, K., and Özkan Nahcivan, N. (2020). Validity and reliability study of the Turkish version of the self-efficacy for managing chronic disease 6-item scale. Turk. J. Med. Sci. 50, 1254–1261. doi: 10.3906/sag-1910-13
Kain, Z. N., Sevarino, F., Pincus, S., Alexander, G. M., Wang, S. M., Ayoub, C., et al. (2000). Attenuation of the preoperative stress response with midazolam: effects on postoperative outcomes. Anesthesiology 93, 141–147. doi: 10.1097/00000542-200007000-00024
Kapikiran, G., Bulbuloglu, S., and Saritas, S. (2022). The effect of video training before organ transplant surgery on patient satisfaction and anxiety: head mounted display effect. Clin. Simul. Nurs. 62, 99–106. doi: 10.1016/j.ecns.2021.09.001
Kok, X. L. F., Newton, J. T., Jones, E. M., and Cunningham, S. J. (2022). Social support and pre-operative anxiety in patients undergoing elective surgical procedures: a systematic review and meta-analysis. J. Health Psychol. 28, 309–327. doi: 10.1177/13591053221116969
Lee, D., and Yoon, S. N. (2021). Application of artificial intelligence-based technologies in the healthcare industry: opportunities and challenges. Int. J. Environ. Res. Public Health 18:271. doi: 10.3390/ijerph18010271
Levett, D. Z. H., and Grimmett, C. (2019). Psychological factors, prehabilitation and surgical outcomes: evidence and future directions. Anaesthesia 74, 36–42. doi: 10.1111/anae.14507
Liu, N.-Z., Xie, W.-J., Kang, Z.-M., Lin, G.-J., Chen, S.-D., and Zhang, J.-Y. (2023). Influence of psychological intervention on patients undergoing spinal anesthesia: a randomized trial. Eur. Rev. Med. Pharmacol. Sci. 27, 122–129. doi: 10.26355/eurrev_202301_30862
Lorig, K. R., Sobel, D. S., Ritter, P. L., Laurent, D., and Hobbs, M. (2001). Effect of a self-management program on patients with chronic disease. Eff. Clin. Pract. 4, 256–262.
Mahmood, T., Scaffidi, M. A., Khan, R., and Grover, S. C. (2018). Virtual reality simulation in endoscopy training: current evidence and future directions. World J. Gastroenterol. 24, 5439–5445. doi: 10.3748/wjg.v24.i48.5439
Maurice-Szamburski, A., Auquier, P., Viarre-Oreal, V., Cuvillon, P., Carles, M., Ripart, J., et al. (2015). Effect of sedative premedication on patient experience after general anesthesia: a randomized clinical trial. JAMA 313, 916–925. doi: 10.1001/jama.2015.1108
Niki, K., Yahara, M., Inagaki, M., Takahashi, N., Watanabe, A., Okuda, T., et al. (2020). Immersive virtual reality reminiscence reduces anxiety in the oldest-old without causing serious side effects: a single-center, pilot, and randomized crossover study. Front. Hum. Neurosci. 14:598161. doi: 10.3389/fnhum.2020.598161
Noben, L., Goossens, S. M. T. A., Truijens, S. E. M., van Berckel, M. M. G., Perquin, C. W., Slooter, G. D., et al. (2019). A virtual reality video to improve information provision and reduce anxiety before cesarean delivery: randomized controlled trial. JMIR Mental Health 6:e15872. doi: 10.2196/15872
Ong, T. L., Ruppert, M. M., Akbar, M., Rashidi, P., Ozrazgat-Baslanti, T., Bihorac, A., et al. (2020). Improving the intensive care patient experience with virtual reality-a feasibility study. Crit. Care Explor. 2:e0122. doi: 10.1097/CCE.0000000000000122
Park, J.-W., Nahm, F. S., Kim, J.-H., Jeon, Y.-T., Ryu, J.-H., and Han, S.-H. (2019). The effect of mirroring display of virtual reality tour of the operating theatre on preoperative anxiety: a randomized controlled trial. IEEE J. Biomed. Health Inform. 23, 2655–2660. doi: 10.1109/JBHI.2019.2892485
Riva, G., Wiederhold, B. K., and Mantovani, F. (2019). Neuroscience of virtual reality: from virtual exposure to embodied medicine. Cyberpsychol. Behav. Soc. Netw. 22, 82–96. doi: 10.1089/cyber.2017.29099.gri
Slater, M. (2018). Immersion and the illusion of presence in virtual reality. Br. J. Psychol. 109, 431–433. doi: 10.1111/bjop.12305
Spielberger, C. D. (1983). Manual for the state: (self evaluation questionnaire). Washington: Consulting Psychologists Press.
Suffeda, A., Meissner, W., Rosendahl, J., and Guntinas-Lichius, O. (2016). Influence of depression, catastrophizing, anxiety, and resilience on postoperative pain at the first day after otolaryngological surgery: a prospective single center cohort observational study. Medicine 95:e4256. doi: 10.1097/MD.0000000000004256
Sun, P., Zhao, Y., Men, J., Ma, Z.-R., Jiang, H.-Z., Liu, C.-Y., et al. (2022). Application of virtual and augmented reality technology in hip surgery: systematic review. J. Med. Internet Res. 25:e37599. doi: 10.2196/37599
Sun, X., Zhong, W., Lu, J., and Zhuang, W. (2021). Influence of psychological nursing intervention on psychological state, treatment compliance, and immune function of postoperative patients with rectal Cancer. J. Oncol. 2021, 1071490–1071496. doi: 10.1155/2021/1071490
Tsay, S.-L., and Chao, Y.-F. C. (2002). Effects of perceived self-efficacy and functional status on depression in patients with chronic heart failure. J. Nurs. Res. 10, 271–278. doi: 10.1097/01.jnr.0000347608.76047.7a
Tulloch, I., and Rubin, J. S. (2019). Assessment and management of preoperative anxiety. J. Voice 33, 691–696. doi: 10.1016/j.jvoice.2018.02.008
Turan, A. Z., Yilmaz, M., and Saracoglu, T. (2021). The effect of virtual reality glasses on anxiety during surgery under spinal anesthesia: a randomized controlled study. Anaesth. Pain Intensive Care 25:1469. doi: 10.35975/apic.v25i2.1469
Turrado, V., Guzmán, Y., Jiménez-Lillo, J., Villegas, E., Lacy, F.B.de, Blanch, J., et al., (2021). Exposure to virtual reality as a tool to reduce peri-operative anxiety in patients undergoing colorectal cancer surgery: a single-center prospective randomized clinical trial. Surg. Endosc., 35, 4042–4047. doi: 10.1007/s00464-021-08407-z
Ugras, G. A., Kanat, C., Yaman, Z., Yilmaz, M., and Turkmenoglu, M. O. (2022). The effects of virtual reality on preoperative anxiety in patients undergoing colorectal and abdominal wall surgery: a randomized controlled trial. J. Perianesth. Nurs. 38, 277–283. doi: 10.1016/j.jopan.2022.07.005
Wang, R., Huang, X., Wang, Y., and Akbari, M. (2022). Non-pharmacologic approaches in preoperative anxiety, a comprehensive review. Front. Public Health 10:854673. doi: 10.3389/fpubh.2022.854673
Williams, J. B., Alexander, K. P., Morin, J.-F., Langlois, Y., Noiseux, N., Perrault, L. P., et al. (2013). Preoperative anxiety as a predictor of mortality and major morbidity in patients aged 70 years undergoing cardiac surgery. Am. J. Cardiol. 111, 137–142. doi: 10.1016/j.amjcard.2012.08.060
Xuefang, L., Guihua, W., and Fengru, M. (2021). The effect of early cognitive training and rehabilitation for patients with cognitive dysfunction in stroke. Int. J. Methods Psychiatr. Res. 30:e1882. doi: 10.1002/mpr.1882
Yuweia Technology Co., Ltd.. (2023). YVR2, the unchallenged choice for pros. Available at: www.yvr.cn/new
Keywords: stroke, carotid artery stenting, preoperative anxiety, virtual reality, psychosocial, intervention
Citation: Liu Y, Wang R, Zhang Y, Feng L and Huang W (2023) Virtual reality psychological intervention helps reduce preoperative anxiety in patients undergoing carotid artery stenting: a single-blind randomized controlled trial. Front. Psychol. 14:1193608. doi: 10.3389/fpsyg.2023.1193608
Received: 31 March 2023; Accepted: 14 June 2023;
Published: 29 June 2023.
Edited by:
Valeria Donisi, University of Verona, ItalyReviewed by:
Elisabetta Patron, University of Padua, ItalyCopyright © 2023 Liu, Wang, Zhang, Feng and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Feng, ZmVuZ2xpbmcyMTZAMTYzLmNvbQ==; Wenxia Huang, SHVhbmd3ZW54aWEzMzFAc2N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.