
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 03 July 2023
Sec. Psychology for Clinical Settings
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1178560
 Chad E. Cook1,2,3
Chad E. Cook1,2,3 Antoine Bailliard1,4
Antoine Bailliard1,4 Jennifer A. Bent5*
Jennifer A. Bent5* Joel E. Bialosky6,7
Joel E. Bialosky6,7 Elisa Carlino8
Elisa Carlino8 Luana Colloca9
Luana Colloca9 Jorge E. Esteves10,11
Jorge E. Esteves10,11 Dave Newell12
Dave Newell12 Alvisa Palese13
Alvisa Palese13 William R. Reed14
William R. Reed14 Jennifer Plumb Vilardaga15
Jennifer Plumb Vilardaga15 Giacomo Rossettini16
Giacomo Rossettini16Objective: Emerging literature suggests contextual factors are important components of therapeutic encounters and may substantially influence clinical outcomes of a treatment intervention. At present, a single consensus definition of contextual factors, which is universal across all health-related conditions is lacking. The objective of this study was to create a consensus definition of contextual factors to better refine this concept for clinicians and researchers.
Design: The study used a multi-stage virtual Nominal Group Technique (vNGT) to create and rank contextual factor definitions. Nominal group techniques are a form of consensus-based research, and are beneficial for identifying problems, exploring solutions and establishing priorities.
Setting: International.
Main outcome measures: The initial stages of the vNGT resulted in the creation of 14 independent contextual factor definitions. After a prolonged discussion period, the initial definitions were heavily modified, and 12 final definitions were rank ordered by the vNGT participants from first to last.
Participants: The 10 international vNGT participants had a variety of clinical backgrounds and research specializations and were all specialists in contextual factors research.
Results: A sixth round was used to identify a final consensus, which reflected the complexity of contextual factors and included three primary domains: (1) an overall definition; (2) qualifiers that serve as examples of the key areas of the definition; and (3) how contextual factors may influence clinical outcomes.
Conclusion: Our consensus definition of contextual factors seeks to improve the understanding and communication between clinicians and researchers. These are especially important in recognizing their potential role in moderating and/or mediating clinical outcomes.
Tools such as patient reported outcome measures (PROMs), physical performance measures, and patient experience measures, are used to measure a patient’s health outcomes (Herbert et al., 2005), and are influenced by a number of internal (within the person) and external (outside the person) factors. These factors may include comorbidities (Tousignant-Laflamme et al., 2017), cognition and mood (Tousignant-Laflamme et al., 2017), socioeconomic and social status (Rethorn et al., 2022; Sharpe et al., 2023), and care timing and provider specialization (Ojha et al., 2016; Hudon et al., 2019; Lentz et al., 2020). Targeted treatment/interventions may also influence outcomes but are commonly moderated and/or mediated by factors such as expectations (Bishop et al., 2013; Eklund et al., 2019), aspects of the patient-clinician relationship (Kelley et al., 2014), legal status (Rodeghero et al., 2015), workers compensation (Rodeghero et al., 2015), social risk variables (Rethorn et al., 2022; Sharpe et al., 2023), common factors such as engagement and/or interaction skills (Miciak et al., 2012), and natural history (Centers of Disease Control and Prevention, 2012). These factors influence disparate individuals differently; consequently, understanding the role that interventions contribute toward patient outcomes becomes challenging.
The ecological landscape in which the clinical encounter occurs, which is sometimes referred to as therapeutic context, consists of a range of factors increasingly referred to as contextual factors (McLaren and Hawe, 2005). Although increasingly well studied, contextual factors/effects are defined differently across a majority of studies (Kaplan et al., 2010; Kelley et al., 2014; Testa and Rossettini, 2016; Nielsen et al., 2019, 2021; Rollet et al., 2021; Sevilla Guerra et al., 2022; Sherriff et al., 2022). Definitions have included sociodemographic variables (Nielsen et al., 2019), person-related factors (race, age, patient beliefs and characteristics) (Nielsen et al., 2019), and physical and social environments (Sevilla Guerra et al., 2022). At a micro-level, contextual factors have been defined by seemingly disparate terms such as therapeutic alliance (Kelley et al., 2014), one’s role in the environment (Kaplan et al., 2010), treatment characteristics (Sherriff et al., 2022), healthcare processes (Rollet et al., 2021), placebo or nocebo effects (Testa and Rossettini, 2016), government agencies (Kaplan et al., 2010), and cultural beliefs. Occasionally, at a macro-level, they are described as confounders or effect modifiers that are not an outcome of the study, but need to be recognized (and measured) (Nielsen et al., 2021; Sevilla Guerra et al., 2022).
Recently, through a multi-step process (semi-structured interviews and a Delphi method), the Outcome Measures in Rheumatology (OMERACT) initiative created a consensus definition for contextual factors (Nielsen et al., 2021). The principal goal of OMERACT was to identify contextual factors that were relevant for clinical trials. Initially, OMERACT defined a contextual factor as a “variable that is not an outcome of the study, but needs to be recognized (and measured) to understand the study results. This includes potential confounders and effect modifiers” (Boers et al., 2014). Through semi-structured interviews and Delphi research, the OMERACT group further qualified contextual factor types (relevant for clinical trials) as: (1) effect modifying (those that modify the treatment effect); (2) outcome influencing (those that predict the prognosis and may confound results); and (3) measurement affecting (those that influence measurement properties such as reliability and validity).
The OMERACT’s broad definition is useful for understanding results in a clinical trial, in that it exists within a more historic paradigm that seeks to remove effects rather than enhance them. In this role it fails to resolve some of the confusion associated with the multitudes of ways contextual factors are presently defined (specifically, whether internal and external domains are potentially contextual factors). For example, it does not include qualifiers to improve one’s understanding, and provides no guidance as to how clinicians may identify contextual factors within clinical encounters in order to enhance positive and minimize negative effects. Subsequently, the objective of this study was to create a consensus definition of contextual factors to better encapsulate this concept to both guide clinicians in clinical scenarios as well as broaden definitions for researchers.
This study used a virtual nominal group technique (vNGT) (Potter et al., 2004), and included researchers and research clinicians from multiple professions who specialized in the study of contextual effects research. We elected to use a vNGT versus a Delphi method because the vNGT allows real time connections between participants (Potter et al., 2004), immediate feedback and flexibility when sharing ideas (Potter et al., 2004; Gattrell et al., 2022), greater discussion in the later stages of consensus development-thus improving refinement of ideas (Cantrill et al., 2011), all in a shorter time span (Potter et al., 2004). An vNGT has been shown to be viable and potentially advantageous to use online (Mason et al., 2021). It has been used previously to identify key implementation factors for COVID-19 vaccination (Michel et al., 2021), establish the core components of home-based rehabilitation for survivors of stroke with severe disability (Fisher et al., 2021), and selecting intervention content to target barriers and enablers of recognition and response to deteriorating patients (Smith et al., 2022). Similar to the OMERACT group, we endeavored to identify a consensus definition that reflects the complexity of contextual factors and describe how contextual factors may influence clinical outcomes, but were also interested in a more detailed set of qualifiers that serve as examples of the key areas of the definition.
The mixed methods study used a vNGT (Potter et al., 2004). The vNGT was performed in October of 2022. Nominal group techniques are beneficial for identifying problems, exploring solutions and establishing priorities, and encourages contributions from all participants and treats each person equally (Potter et al., 2004). The Institutional Review Board of Duke University, Durham, North Carolina, USA, approved the study (ro00111522-INIT-1.0).
Optimal NGT participants are stated to include five to nine individuals (Potter et al., 2004), but values may vary. The first and senior author were responsible for recruitment and reflected the ACCORD guidelines for consensus development (van Zuuren et al., 2022). Three drivers primarily drove recruitment: (1) the expertise of the researchers in contextual factors research (determined by publication and/or presentations); (2) the clinical background (when appropriate); and (3) by specialization (e.g., neuroscience, community engagement). The first and senior author also endeavored to balance participants by sex and years of experience. After assembling a short-list of potential participants, the first and senior author invited participation through an email. All potential vNGT members agreed to participate.
Participants were provided with pre-work prior to the vNGT. Each individual was provided with an article (Potter et al., 2004) that outlined the vNGT processes and were asked to consider early development of their own versions of a definition for contextual factors.
During the virtual session, a five-stage vNGT process following the protocol by Potter et al. (2004) was used (Figure 1). The virtual session was conducted using Microsoft Zoom (Microsoft Corp, Redmond, WA) and the moderator for the session was a mixed-methods researcher with a contextual factors background and prior experience with vNGT research and moderation.
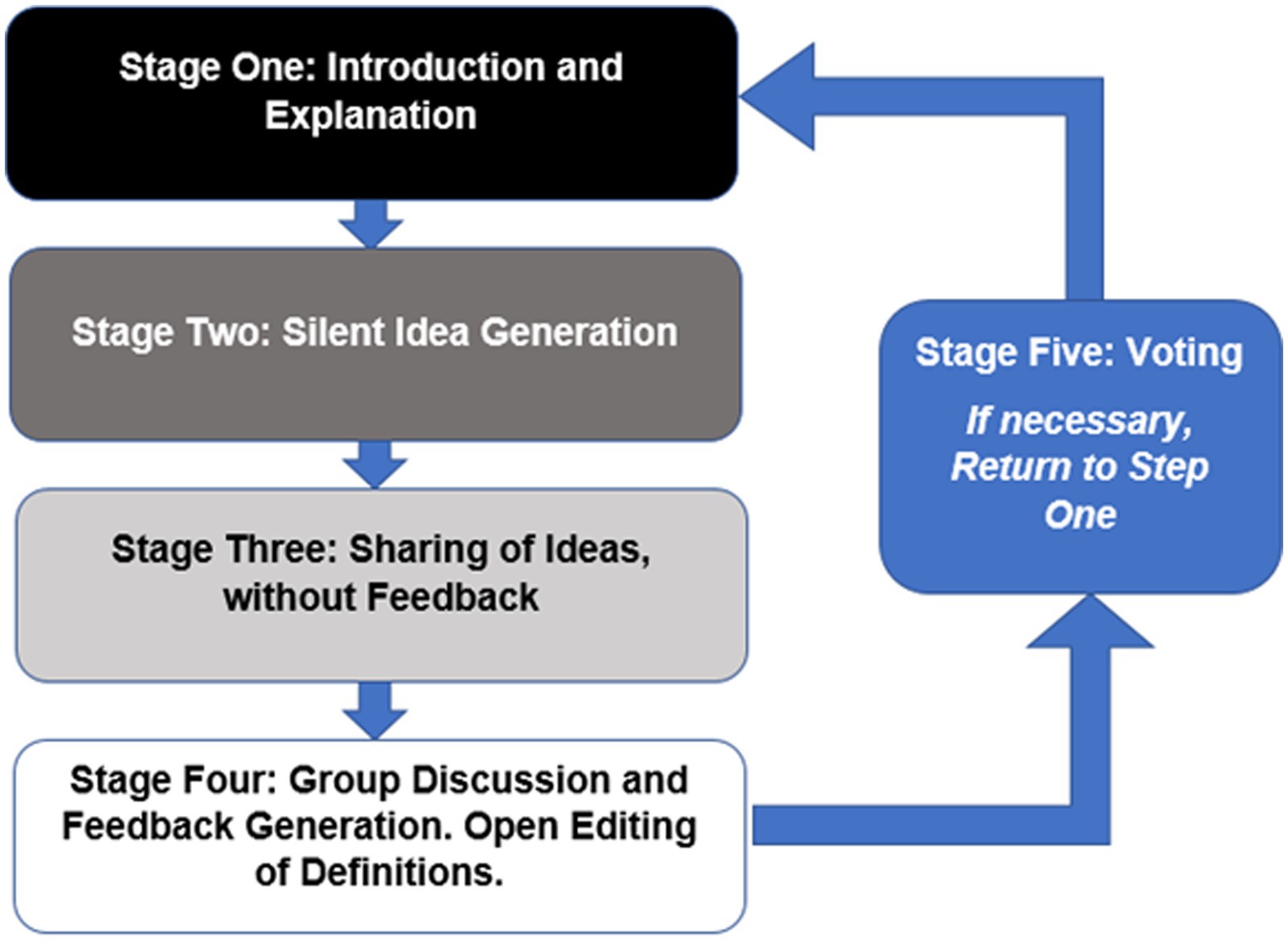
Figure 1. The Five Stage Process of a Virtual Nominal Group Technique according to Potter et al. (2004).
Stage one (Introduction and Explanation): An introduction and welcome to all participants with an explanation of the purpose and procedure of the workshop.
Stage two (Silent Idea Generation): The question was introduced to the participants: “What is a working definition of contextual factors”? All participants were asked to create a list of ideas that come to mind when considering the question and to place these ideas on a shared Google document. During this stage, all participants were asked not to consult or discuss ideas with each other. A total of 10 min was provided for each participant to create his or her selected definitions.
Stage three (Sharing Ideas): During Stage three, each participant introduced their definitions that were recorded on the google documents. This document was shared on the screen so that all participants can see the list in real time. This stage continued in a round robin format until all ideas had been presented. No debate or discussion occurred at this stage.
Stage four (Group Discussion): Participants were invited to seek verbal explanation or further details about any ideas that were produced during stage three. The moderator ensured that each person was able to contribute and that all ideas were discussed without spending too long on a single idea. At this stage, participants were able to suggest new items for discussion or combining of items to modify the current list. Each participant “owned” each definition and edited the definition only if they agreed on the change requested.
Unique to this vNGT, participants had up to 1 week to modify or delete their own contributions or request edits to another definition that they did not generate. We elected to provide additional time to edit each person’s definition, since the concept is complex and since there were a variety of definitions presented in Stage two and three, which were further discussed and modified in Stage four.
Stage five (Voting): During stage five, and after the week of modifying or deleting their own contributions, vNGT participants were allowed to “rank order” the definitions generated during stage four. Rank ordering was performed using a Qualtrics survey and a “ranking” function. In this survey, each NGT participant ranked all 12 definitions from 1 (top choice) to 12 (lowest choice).
Modifications of a five round NGT are not uncommon and may be warranted when working with complex populations or topics that require maturation before final evaluation (McMillan et al., 2016). If consensus voting does not identify a clear ranked winner, a sixth round, which includes re-voting on the top ranked choices, can be implemented to assure a true consensus choice (Potter et al., 2004; McMillan et al., 2016). Our vNGT used a sixth round of voting to identify a clear consensus definition.
The vNGT included 10 individuals with clinical/research backgrounds in rehabilitation (chiropractic, osteopathy, physical therapy, or occupational therapy), clinical psychology, medicine, and nursing. Advanced research training included community engagement, molecular biology, nursing science, neurobiology, neuroscience, placebo/nocebo, rehabilitation medicine, and social determinants of health (Table 1). The vNGT participants averaged 19 publications on contextual factors, and represented 4 countries across two continents.
Stage two generated 14 definitions of contextual factors (Table 2). Seven vNGT participants submitted one definition, whereas two participants submitted two definitions and one submitted three. Consistent domains included internal and external factors, which influenced outcomes associated with any of the treatments provided. Stage four refined the definitions through audience (clinicians and researchers) discussion and the need for a single consensus definition including qualifiers that help define the definition and how contextual factors may influence outcomes.
At the end of Stage four (consolidation of ideas), there were 12 definitions that were rank ordered (Table 3). Three definitions were clearly ranked higher than (Table 4) the remaining nine with the majority (80%) of the vNGT selecting these choices as one of the top three selections. These three were similar in content and scope and finished with mean “ranked” scores of 3.0, 3.7 and 3.8, respectively. Following a further poll of the group it was felt that it was necessary to vote again (Round six), but to only include the three aforementioned definitions. Upon re-vote, one clear winner was identified.
Contextual factors (CFs) are components of all therapeutic encounters and may constitute the entirety of the perceived effects of the intervention itself or be additive to effects of interventions such as pharmacological and nonpharmacological treatments. CFs are perceived cues that affect both the patient and practitioner and can arise from previous experiences and immediate dynamics within the encounter, or a combination of both. CFs fall into broad categories that can include patient characteristics, practitioner characteristics, treatment characteristics, characteristics of the dynamic between the patient and practitioner and characteristics of the setting within which the encounter is being delivered. CFs can be complexly interwoven in the patients and practitioners experience so as to influence what patients and practitioners expect the outcome of the encounter to be. Through such conscious and unconscious expectations, involving a range of specific neurological pathways, CFs can directly influence (both positively and negatively) symptoms and characteristics associated with the presenting condition. The proportion of clinical effects observed associated with CFs can vary from large to small depending on the characteristics of the patient, practitioner, condition and intervention.
The goal of the study was to develop a consensus-derived definition of contextual factors. The study methodology used an vNGT, which is beneficial for identifying problems (Young et al., 2021), exploring solutions and establishing priorities, and providing a meaningful and economical method of soliciting contributions from all participants (Potter et al., 2004). Our final consensus selection reflects the complexity of a definition of contextual factors and includes: (1) an overall definition, (2) qualifiers that serve as examples of the key areas of the definition and (3) how contextual factors may influence clinical outcomes. We feel this harmonized definition will improve the understanding of contextual factors and will help clinicians recognize their potential role in moderating and/or mediating these factors to positively impact clinical outcomes. Further, we feel the findings may also improve interpretation of research and deserve additional discussion.
The vNGT participants identified the influence of contextual factors as mediators, moderators, or confounding variables and felt that contextual factors included both internal and external factors. These fell into broad categories that included patient characteristics, practitioner characteristics, treatment characteristics, characteristics of the dynamic between the patient and practitioner and characteristics of the setting within which the encounter is being delivered. This suggests that who is enrolled in a study, who provides care in a study, and where that study is performed may influence clinical outcomes. The OMERACT group (Nielsen et al., 2021) defined contextual factors as personal factors, disease-related factors, and environmental factors, each with a possibility of being effect modifying, outcome influencing, and measurement affecting (Nielsen et al., 2021). Similarities between the two definitions include the multidimensional aspect of the definitions and the role of contextual factors in influencing clinical outcomes. Differences include the more granular aspects of the vNGT definition, less explicitness in its effect-modifying role [which is well detailed in the OMERACT example (Nielsen et al., 2021)] and the omission of disease-related factors in the vNGT definition.
Our initial set of 14 definitions identified a number of common elements associated with contextual factors. The biggest differences across initial definitions included whether contextual factors were considered as placebo/nocebo effects, whether the factors were actively or passively perceived (or both), and whether contextual factors were considered moderators of treatment (e.g., age, sex, socioeconomic status), mediators of treatment (e.g., self-efficacy, fear, psychological mood) or both. Discussion during stage three highlighted the inconsistent domains involved in the role of cultural versus political versus power imbalances, whether contextual factors were a measurable mechanism, whether placebo/nocebo effects were a necessity within the definition, if a contextual factor was a “nonspecific” finding, and its role as a prognostic mediator/moderator. Thus, the emerging findings mirror the heterogeneity of conceptual definition and the variability of dimensions associated with contextual factors reported in the literature (McLaren and Hawe, 2005; Kaplan et al., 2010; Testa and Rossettini, 2016; Nielsen et al., 2019, 2021; Rollet et al., 2021; Sevilla Guerra et al., 2022; Sherriff et al., 2022). Our work acknowledged and established an initial synthesis of these complex and important domains, which may in turn be fruitful to consider in future work.
Despite a wide range of clinical backgrounds and research training expertise, we were pleased with the collaborative nature of our vNGT. With appropriate pre-work and judicious use of time (Potter et al., 2004), we were able to consolidate many disparate initial thoughts to common themes within the two-hour timeframe. When properly employed, consensus agreement methods create structured environments for which experts are prompted to give the best available information, allowing solutions to problems that may remain otherwise unsolved (Fink et al., 1984). This requires the process to be deliberately inclusive, participatory, collaborative, and cooperative, with an ultimate goal of a final consensus agreement (Black et al., 1999). A fundamental element of this methodology is that it does not require all participants to agree on all topics (it implies only general agreement) nor does it assure unanimity.
At the end of stage four, vNGT participants were allocated 1 week to modify their own definitions of contextual factors and then were given a 48-h window to rank order the final definitions. Eventually, a sixth round was deemed necessary to further separate three competing definitions. During stage four, notable harmonizing occurred across each of the definitions, especially our first goal of obtaining an overall definition. A majority also agreed that contextual factors moderated or mediated clinical outcomes and compared to the initial set of definitions, most included qualifying statements with the definitions as well. The qualifying statements, such as patient and provider personal, historical, cultural, environmental, physical, and rhetorical dimensions around the therapeutic encounter and the patient-clinician interaction, are what separates our definition from that of the OMERACT group (Nielsen et al., 2021).
Although this study provided new insights into contextual factors’ definition, some limitations are worth mentioning. Firstly, although we exceeded the recommended panel size of an NGT, we involved a small sample of participants from a restricted number of healthcare fields, possibly leaving others unrepresented (e.g., midwifery, speech therapy, and optometry). Regardless, we ensured adequate representativeness of contextual factors experts in our vNGT by balancing the number of males and females (M: F = 6:4) and including clinicians and clinical researchers from more than one country (Manera et al., 2019). Secondly, compared to conducting an in-person NGT, using a virtual Zoom platform could have produced a limited interaction between participants with potentially diverging opinions, thus introducing bias. Nevertheless, the limited time and resource requirements of the vNGT, together with the presence of an experienced moderator, guaranteed a satisfactory quality of the participatory process, considering all participants’ views equally and minimizing any dominant effects (Manera et al., 2019). Thirdly, our vNGT participants had a predominant musculoskeletal background. Lastly, we should have compared the definition of contextual factors obtained with our vNGT with other methods (e.g., Delphi, brainstorming) to evaluate their similarities and differences. However, we deliberately used the vNGT because it represents a suitable consensus method to reach an agreement on a single and complex topic among the participants (Manera et al., 2019).
Our study, involving a panel of international experts with a majority musculoskeletal background, offered the opportunity to identify a definition of contextual factors, find their qualifiers and understand their impact on the therapeutic outcome. This initial definition may help clinicians and researchers embrace the complexity that underlies the construct of contextual factors. We acknowledge different opinions can coexist; we present our definition as a starting point for future studies on the topic. A Delphi method may be a useful approach to determine consensus across a broader background of individuals and is a recommended follow-up step to this research.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by The Institutional Review Board of Duke University, Durham, North Carolina, USA, approved the study (ro00111522-INIT-1.0). The patients/participants provided their written informed consent to participate in this study.
CC and GR contributed to the conception and design of the study and wrote the first draft of the manuscript. AB, JAB, JEB, EC, LC, JE, DN, AP, WR, and JV wrote sections of the manuscript. All authors contributed to manuscript revision, read and approved the submitted version.
This was a NIH U24 supported research study [1U24AT011969-01, Force-Based Manipulation network (ForceNet)]; Administering institutes or centers National Center for Complementary and Integrative Health, https://reporter.nih.gov/search/Hq4YC-ZDk0yDq2PgxIHgVA/project-details/10450926. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
GR leads education programmes on placebo, nocebo effects and contextual factors in healthcare to under- and post-graduate students along with private CPD courses. CC receives honoraria from book sales and continuing education courses, and is a consultant for Revenite and the Hawkins Foundation. None of the honoraria or consulting work has a competing interest with the work provided in this paper.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Bishop, M. D., Mintken, P. E., Bialosky, J. E., and Cleland, J. A. (2013). Patient expectations of benefit from interventions for neck pain and resulting influence on outcomes. J. Orthop. Sports Phys. Ther. 43, 457–465. doi: 10.2519/jospt.2013.4492
Black, N., Murphy, A., Lamping, D., McKee, M., Sanderson, C., Askham, J., et al. (1999). Consensus development methods: a review of best practice in creating clinical guidelines. J. Health Serv. Res. Policy 4, 236–248. doi: 10.1177/135581969900400410
Boers, M., Kirwan, J. R., Wells, G., Beaton, D., Gossec, L., d’Agostino, M. A., et al. (2014). Developing core outcome measurement sets for clinical trials: OMERACT filter 2.0. J. Clin. Epidemiol. 67, 745–753. doi: 10.1016/j.jclinepi.2013.11.013
Cantrill, J. A., Sibbald, B., and Buetow, S. (2011). The Delphi and nominal group techniques in health services research. Int. J. Pharm. Pract. 4, 67–74. doi: 10.1111/j.2042-7174.1996.tb00844.x
Centers of Disease Control and Prevention. (2012) Principles of Epidemiology, Lesson 1, Section 9. Natural history and Spectrum of disease. Available at: https://www.cdc.gov/csels/dsepd/ss1978/lesson1/section9.html (Accessed December 2022).
Eklund, A., De Carvalho, D., Pagé, I., Wong, A., Johansson, M. S., Pohlman, K. A., et al. (2019). Expectations influence treatment outcomes in patients with low back pain. A secondary analysis of data from a randomized clinical trial. Eur. J. Pain 23, 1378–1389. doi: 10.1002/ejp.1407
Fink, A., Kosecoff, J., Chassin, M., and Brook, R. H. (1984). Consensus methods: characteristics and guidelines for use. Am. J. Public Health 74, 979–983. doi: 10.2105/AJPH.74.9.979
Fisher, R. J., Riley-Bennett, F., Russell, L., Lee, C., Sturt, R., Walker, M., et al. (2021). Nominal group technique to establish the core components of home-based rehabilitation for survivors of stroke with severe disability. BMJ Open 11:e052593. doi: 10.1136/bmjopen-2021-052593
Gattrell, W. T., Hungin, A. P., Price, A., Winchester, C. C., Tovey, D., Hughes, E. L., et al. (2022). ACCORD guideline for reporting consensus-based methods in biomedical research and clinical practice: a study protocol. Res. Integr. Peer Rev. 7:3. doi: 10.1186/s41073-022-00122-0
Herbert, R., Jamtvedt, G., Mead, J., and Hagen, K. B. (2005). Outcome measures measure outcomes, not effects of intervention. Aust. J. Physiother. 51, 3–4. doi: 10.1016/S0004-9514(05)70047-7
Hudon, A., Lippel, K., and MacEachen, E. (2019). Mapping first-line health care providers’ roles, practices, and impacts on care for workers with compensable musculoskeletal disorders in four jurisdictions: a critical interpretive synthesis. Am. J. Ind. Med. 62, 545–558. doi: 10.1002/ajim.22972
Kaplan, H. C., Brady, P. W., Dritz, M. C., Hooper, D. K., Linam, W. M., Froehle, C. M., et al. (2010). The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 88, 500–559. doi: 10.1111/j.1468-0009.2010.00611.x
Kelley, J. M., Kraft-Todd, G., Schapira, L., Kossowsky, J., and Riess, H. (2014). The influence of the patient-clinician relationship on healthcare outcomes: a systematic review and meta-analysis of randomized controlled trials. PLoS One 9:e94207. doi: 10.1371/journal.pone.0094207
Lentz, T. A., Goode, A. P., Thigpen, C. A., and George, S. Z. (2020). Value-based care for musculoskeletal pain: are physical therapists ready to deliver? Phys. Ther. 100, 621–632. doi: 10.1093/ptj/pzz171
Manera, K., Hanson, C. S., Gutman, T., and Tong, A. (2019). “Consensus methods: nominal group technique” in Handbook of research methods in health social sciences. ed. P. Liamputtong (Singapore: Springer)
Mason, S., Ling, J., Mosoiu, D., Arantzamendi, M., Tserkezoglou, A. J., Predoiu, O., et al. (2021). Undertaking research using online nominal group technique: lessons from an international study (RESPACC). J. Palliat. Med. 24, 1867–1871. doi: 10.1089/jpm.2021.0216
McLaren, L., and Hawe, P. (2005). Ecological perspectives in health research. J. Epidemiol. Community Health 59, 6–14. doi: 10.1136/jech.2003.018044
McMillan, S. S., King, M., and Tully, M. P. (2016). How to use the nominal group and Delphi techniques. Int. J. Clin. Pharm. 38, 655–662. doi: 10.1007/s11096-016-0257-x
Michel, D. E., Iqbal, A., Faehrmann, L., Tadić, I., Paulino, E., Chen, T. F., et al. (2021). Using an online nominal group technique to determine key implementation factors for COVID-19 vaccination programmes in community pharmacies. Int. J. Clin. Pharm. 43, 1705–1717. doi: 10.1007/s11096-021-01335-x
Miciak, M., Gross, D. P., and Joyce, A. (2012). A review of the psychotherapeutic ‘common factors’ model and its application in physical therapy: the need to consider general effects in physical therapy practice. Scand. J. Caring Sci. 26, 394–403. doi: 10.1111/j.1471-6712.2011.00923.x
Nielsen, S. M., Boers, M., de Wit, M., Shea, B., van der Windt, D. A., Reeves, B. C., et al. (2021). OMERACT consensus-based operational definition of contextual factors in rheumatology clinical trials: a mixed methods study. Semin. Arthritis Rheum. 51, 601–606. doi: 10.1016/j.semarthrit.2021.03.013
Nielsen, S. M., Tugwell, P., de Wit, M. P. T., Boers, M., Beaton, D. E., Woodworth, T. G., et al. (2019). Contextual factors working group. Identifying provisional generic contextual factor domains for clinical trials in rheumatology: results from an OMERACT initiative. J. Rheumatol. 46, 1159–1163. doi: 10.3899/jrheum.181081
Ojha, H. A., Wyrsta, N. J., Davenport, T. E., Egan, W. E., and Gellhorn, A. C. (2016). Timing of physical therapy initiation for nonsurgical management of musculoskeletal disorders and effects on patient outcomes: a systematic review. J. Orthop. Sports Phys. Ther. 46, 56–70. doi: 10.2519/jospt.2016.6138
Potter, M., Gordon, S., and Hamer, P. (2004). The nominal group technique: a useful consensus methodology in physiotherapy research. N. Z. J. Physiother. 32, 126–130.
Rethorn, Z. D., Cook, C. E., Park, C., Somers, T., Mummaneni, P. V., Chan, A. K., et al. (2022). Social risk factors predicting outcomes of cervical myelopathy surgery. J. Neurosurg. Spine, 37, 41–8. doi: 10.3171/2021.12.SPINE21874
Rodeghero, J. R., Cook, C. E., Cleland, J. A., and Mintken, P. E. (2015). Risk stratification of patients with low back pain seen in physical therapy practice. Man. Ther. 20, 855–860. doi: 10.1016/j.math.2015.04.007
Rollet, Q., Tron, L., De Mil, R., Launoy, G., and Guillaume, É. (2021). Contextual factors associated with cancer screening uptake: a systematic review of observational studies. Prev. Med. 150:106692. doi: 10.1016/j.ypmed.2021.106692
Sevilla Guerra, S., Jean, E., Kilpatrick, K., Zabalegui, A., and Martínez Gaitero, C. (2022). Contextual factors of advanced practice nursing development: a network analysis. Int. J. Nurs. Pract. :e13114. doi: 10.1111/ijn.13114
Sharpe, J. A., Miller, R., Cook, C. E., et al. (2023). Social risk factors are associated with disability prevalence – results from 17 states in the 2017 behavioral risk factor surveillance system. Am. J. Health Promot. 37, 453–463. doi: 10.1177/08901171221132390
Sherriff, B., Clark, C., Killingback, C., and Newell, D. (2022). Impact of contextual factors on patient outcomes following conservative low back pain treatment: systematic review. Chiropr. Man. Therap. 30:20. doi: 10.1186/s12998-022-00430-8
Smith, D., Cartwright, M., Dyson, J., Hartin, J., and Aitken, L. M. (2022). Selecting intervention content to target barriers and enablers of recognition and response to deteriorating patients: an online nominal group study. BMC Health Serv. Res. 22:766. doi: 10.1186/s12913-022-08128-6
Testa, M., and Rossettini, G. (2016). Enhance placebo, avoid nocebo: how contextual factors affect physiotherapy outcomes. Man. Ther. 24, 65–74. doi: 10.1016/j.math.2016.04.006
Tousignant-Laflamme, Y., Martel, M. O., Joshi, A. B., and Cook, C. E. (2017). Rehabilitation management of low back pain – it’s time to pull it all together! J. Pain Res. 10, 2373–2385. doi: 10.2147/JPR.S146485
van Zuuren, E. J., Logullo, P., Price, A., Fedorowicz, Z., Hughes, E. L., and Gattrell, W. T. (2022). Existing guidance on reporting of consensus methodology: a systematic review to inform ACCORD guideline development. BMJ Open 12:e065154. doi: 10.1136/bmjopen-2022-065154
Keywords: placebo, contextual factors, clinical outcomes, nominal group technique, consensus research
Citation: Cook CE, Bailliard A, Bent JA, Bialosky JE, Carlino E, Colloca L, Esteves JE, Newell D, Palese A, Reed WR, Vilardaga JP and Rossettini G (2023) An international consensus definition for contextual factors: findings from a nominal group technique. Front. Psychol. 14:1178560. doi: 10.3389/fpsyg.2023.1178560
Received: 06 March 2023; Accepted: 07 June 2023;
Published: 03 July 2023.
Edited by:
Michael Swain, Macquarie University, AustraliaReviewed by:
Carlo Ammendolia, University of Toronto, CanadaCopyright © 2023 Cook, Bailliard, Bent, Bialosky, Carlino, Colloca, Esteves, Newell, Palese, Reed, Vilardaga and Rossettini. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jennifer A. Bent, SmVubmlmZXIuYmVudEBkdWtlLmVkdQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.