
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 01 February 2023
Sec. Environmental Psychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1131076
 Rui Zhang
Rui Zhang Chengli Wang*
Chengli Wang*Objective: Medical isolation is one of the most effective measures to slow the spread of the virus when dealing with a pandemic. Millions of people in China have undergone centralized medical isolation (CMI) during the COVID-19 pandemic. This study aims to assess the centralized medical isolation group’s COVID-19 risk perception and to explore the influencing factors.
Methods: A total of 400 participants (200 who had experienced CMI and 200 who had not experienced) completed a questionnaire related to COVID-19 risk perceptions. The questionnaire was designed with the Cognitive-Experiential Self-Theory (CEST) and the Common Sense Model of Risk Perception (CSM). It adopted nine questions to measure risk perception in terms of Emotional feelings, Cognitive judgment, and Mental representation of unusual severity. Descriptive statistical analysis, correlation analysis, and multiple linear regression analysis were conducted with SPSS 26.0 software.
Results: The mean risk perception score for the CMI group was 30.75, with a standard deviation of 7.503, which was significantly higher than that in the non-centralized medical isolation (NCMI) group (risk perception score was 28.2, and the standard deviation was 7.129). The results show that risk perceptions were higher for older age, risk perceptions were higher for higher education, risk perceptions were higher for those who had received the COVID-19 vaccination, and risk perceptions were higher for those who lived in a family with children.
Conclusion: Risk perception is significantly higher in CMI groups than in NCMI groups. The government should draw more care to the risk perception and psychological wellbeing of the CMI group and provide extra support and assistance to the elderly and those raising younger children. In dealing with future pandemics like the COVID-19 outbreak, the government should actively guide the public to properly isolate at home and cautiously implement a CMI policy.
Since the end of 2019, the COVID-19 outbreak has become a severe global pandemic affecting people’s daily lives and economic activities. The COVID-19 pandemic is still not effectively controlled in some countries. However, an increasing number of countries are reducing their precautionary measures and seeking to enter a phase of normalization where they can coexist with COVID-19. China is gradually relaxing its control of COVID-19, mainly by releasing restrictions on the movement of people across regions, replacing the mandatory centralized medical isolation (CMI) of confirmed cases with voluntary centralized medical or home isolation, and abolishing the checking of negative nucleic acid certificates from the public in the vast majority of premises.
Medical isolation is a measure of isolation for people who are carriers of a specific virus or have developed a specific disease (Jiang et al., 2022). During the COVID-19 pandemic, many countries worldwide implemented medical isolation policies. Most countries had required people who tested positive for nucleic acid for COVID-19 to be quarantined at home for 5–10 days, which could end on its own when the nucleic acid test turned negative. According to an Agence France-Presse (AFP) report on 29 March 2020, more than 3.38 billion people worldwide were required to comply with medical isolation measures to fight COVID-19. This figure represents about 43% of the global population1. China has adopted more stringent medical isolation measures than most countries. China has CMI for confirmed cases, suspected cases, close contacts of asymptomatic infected people, and people entering the country, requiring them to undergo daily morning and evening temperature and health status monitoring and regular nucleic acid collection. There are two types of CMI in China, one for hotel isolation (mainly for entry personnel and close contacts of COVID-19 confirmed cases) and one for square-cabin hospital isolation (mainly for COVID-19 lightly infected patients, asymptomatic infected patients, and a few close contacts). According to official data released by China, 189,669 people were still under medical isolation and observation related to COVID-19 in China as of 19 November 20222.
Although the risk posed by COVID-19 to public health is decreasing, there are still many people whose risk perceptions have been or are being affected. Risk perceptions are people’s beliefs, attitudes, judgments and emotions about risks (Slovic, 1987; Zhang Y. B. et al., 2020). In response to a pandemic like the COVID-19 outbreak, the public’s willingness and behavior to maintain social distance, voluntarily vaccinate, observe travel restrictions, and comply with quarantine measures can slow the spread of the pandemic and accelerate the recovery of the public health system (Brewer et al., 2007; Ferrer and Klein, 2015; Wise et al., 2020; Zhang et al., 2023). When the public’s risk perception is high, they will adopt stricter preventive behaviors and are more inclined to comply with government pandemic prevention measures. When the public’s risk perception is low, they will adopt lower levels of preventive behavior and may even fight against some of the prevention measures (Weinstein and Nicolich, 1993; Taghrir et al., 2020). Multiple factors can influence the public’s perception of risk. Luo et al. (2021) conducted a literature review based on international databases and showed that isolation, mental disorders, and restricted social activities due to blockades increased the fear of COVID-19. The mean fear of COVID-19 was higher in women than in men (20.67 vs. 18.21). Females in Asia (18.36) and Australia (17.43) had the highest mean and lowest mean fear of COVID-19, and females in hospital staff (19.51) and university students (17.95) had the lowest mean fear. Several studies have been conducted to demonstrate the impact of home isolation and social distance on public perceptions of risk during the COVID-19 outbreak. The study conducted by Parisi et al. (2021) showed that women in Italy tended to go out less and take personal protective measures during the COVID-19 pandemic. The resulting physical distance and housing isolation exacerbated family conflicts and affected community neighborhoods. Zhang M. M. et al. (2020) found that home isolation caused many negative emotional reactions in nurses and that the nurses’ positive emotions gradually increased as the isolation period ended. Abu Jamileh et al. (2021) conducted a cross-sectional study in Saudi Arabia with parents of children aged 6–14 years, and found that children experienced mild-to-severe psychological impact on behaviors and feelings during home isolation during COVID-19 pandemic. Denerel et al. (2022) found that home isolation affected the mental health of athletes, although this effect was weaker compared to non-athletes. Slone et al. (2022) found that home isolation caused psychological distress in the public and that the severity of this psychological distress was inversely related to the public’s ability to exercise Self-Mastery (Self-Mastery refers to a sense of having control over life events and is reflected in a self-perception of strength and the capacity to cope with and overcome obstacles by relying on personal efforts). Shechory and Laufer surveyed Israelis living in conflict zones. They found that respondents feared COVID-19 more than terrorism during Israel’s enforced blockade. These respondents living in conflict areas did not show higher levels of resilience when faced with new threats during the COVID-19 pandemic. However, they may have been more adept at dealing with long-standing threats, such as terrorism (Shechory, and Laufer, 2021). The results of a study conducted by Rania and Coppola in Italy, which lasted 14 days, showed that fear of COVID-19 was an emotional state experienced by the population as a whole and that there was a positive correlation between COVID-19-related fear, feelings of isolation, mental health and a positive sense of social distance. Younger people were likelier to be lonely and less likely to accept the imposed social distance than older people (Rania and Coppola, 2022). Ju et al. (2021) assessed the psychological state of the COVID-19 patients and found that the form and duration of isolation significantly affected levels of depression and anxiety, with home isolated patients experiencing significantly less depression and anxiety, compared to centrally isolated patients who did not. Although some scholars have focused on the home isolation group, few have studied the risk perception of the CMI group.
Medical isolation effectively slowed the spread of the virus in the early stages of countries’ response to COVID-19, and it is still likely to be seen as one of the core measures to deal with future pandemics. Therefore, it is essential to assess and analyze the risk perceptions of CMI groups in order for governments to optimize medical isolation policies and better respond to public health emergencies. This study will assess the COVID-19 risk perceptions of CMI groups and analyze the factors influencing them based on research data. On this basis, we will compare the risk perceptions of CMI groups with those of non-centralized medical isolation (NCMI) groups to analyze better and demonstrate the impact of centralized isolation measures on public risk perception. This study will contribute to the development of risk perception research and provide a reference for the government to optimize its policy on CMI.
Participants included 200 respondents undergoing CMI and 200 who had not experienced CMI. The study was conducted only for the public over 18, and the questionnaires completed by the participants were anonymous. The study was approved by the Ethics Committee of the School of Public Policy and Management of the China University of Mining and Technology (approved 6-2022). This survey was conducted by the researchers from China University of Mining and Technology. All respondents completed the questionnaire voluntarily. The respondents had freedom not to do so and could withdraw their consent during the research.
Centralized medical isolation groups (CMI groups): The researchers randomly selected five CMI sites in Jiangsu Province, China. After consultation and communication with the staff in charge of the isolation sites, the researchers pushed an electronic version of the questionnaire to the isolated people and collected the data. The researchers set up the questionnaire to be filled in only once by the same account to prevent duplication.
Non-centralized medical isolation groups (NCMI groups): The research site was a city in Jiangsu Province. The researchers used a multi-stage stratified random sampling method. The questionnaires were distributed and collected face-to-face. The researchers verbally asked the respondents if they had experienced CMI before distributing the questionnaire, and if they had, they would not be selected as respondents.
The COVID-19 pandemic has the characteristics of a massive stressor (intimidating, prolonged, unpredictable, and severe consequences). These characteristics of COVID-19 inevitably affect the risk perception for individuals and the general public. Existing risk perception measurement studies may provide a framework for insight into the assessment of risk perception of the COVID-19 pandemic in this study. Slovic (1987) proposed a psychometric model to assess risk perception characteristics, mainly regarding risk familiarity and controllability dimensions. Shi et al. (2003) used the model proposed by Slovic to assess the public’s risk perception of severe acute respiratory syndrome coronavirus (SARS) information, and some valuable evidence was obtained. However, this assessment is ex post-oriented, with minimal applicability during the outbreak. Xie et al. (2005) developed a three-dimensional, 11-item SARS risk perception assessment tool based on Slovic’s model, including apprehensiveness, controllability, and likelihood of infection. This tool has the advantage of assessing the risk perception of the outbreak/virus from three dimensions but still has the disadvantage of simplifying the risk perception.
This study referred to the above studies and designed a questionnaire based on the Cognitive-Experiential Self-Theory (CEST) and the Common Sense Model of Risk Perception (CSM). The basic assumption of CEST is that humans respond through both empirical and rational systems (Pacini et al., 1998). The empirical system is primarily non-verbal and imaginative and learns automatically from experience; the rational system is the human-specific verbal reasoning system. The failure of one of these two systems can lead to adaptation problems for the individual. For example, there is a discrepancy between knowledge and action: the risk of not wearing a mask despite knowing the risk of infection is not based on a genuine fear of the new coronavirus. Another example is the lack of scientific knowledge about the NIV when one is so afraid that one cannot leave the house even when the pandemic has improved. When both failures occur, individuals exhibit more severe maladjustment, which may explain the wide range of reactions and behaviors during a pandemic. The CEST illustrates the need to balance perceptions and feelings in measuring public perceptions of risk in significant public health emergencies.
The CSM is a model of health threat self-regulation developed by Leventhal et al. (1998) The model suggests that health threat information activates and develops a risk representation of the disease, which includes identification, etiology, timeline, consequences, and cure. Individuals, groups, and societies use risk representations to move toward selecting and using health threat control procedures. Specifically, risk representations include two intertwined components that are difficult to separate: the representation of the disease/threat/risk and the emotional response. Emotions are infused into cognitive processes, influencing cognitive reasoning and distillation. The final response of the individual as a problem solver does not depend solely on the cognitive representation or the emotional response but rather on the final risk management decision as a result of the integration of the two.
In addition, we referenced the Perceived Risk of HIV Scale (PRHS) developed by Lucy et al. (2012) to provide a more operational sample reference for item writing for this study. Ultimately, we measured respondents’ COVID-19 risk perceptions in the questionnaire with three variables. These variables include the individual’s emotional feelings about their infection with COVID-19, their cognitive judgment of the vulnerability to infection, and the mental representation of unusual severity. Specifically, emotional feelings about one’s infection reflected a range of emotions, such as worry, fear, and even dread (Cui et al., 2021). The judgment of vulnerability refers to the respondent’s perception of how likely they are to be infected with COVID-19 (Capone et al., 2021). The mental representation of unusual severity reflects the level of alertness to the risk of COVID-19 and is a mixture of perceptions and feelings (Xi et al., 2020). The specific items set in the questionnaire are shown in Table 1.
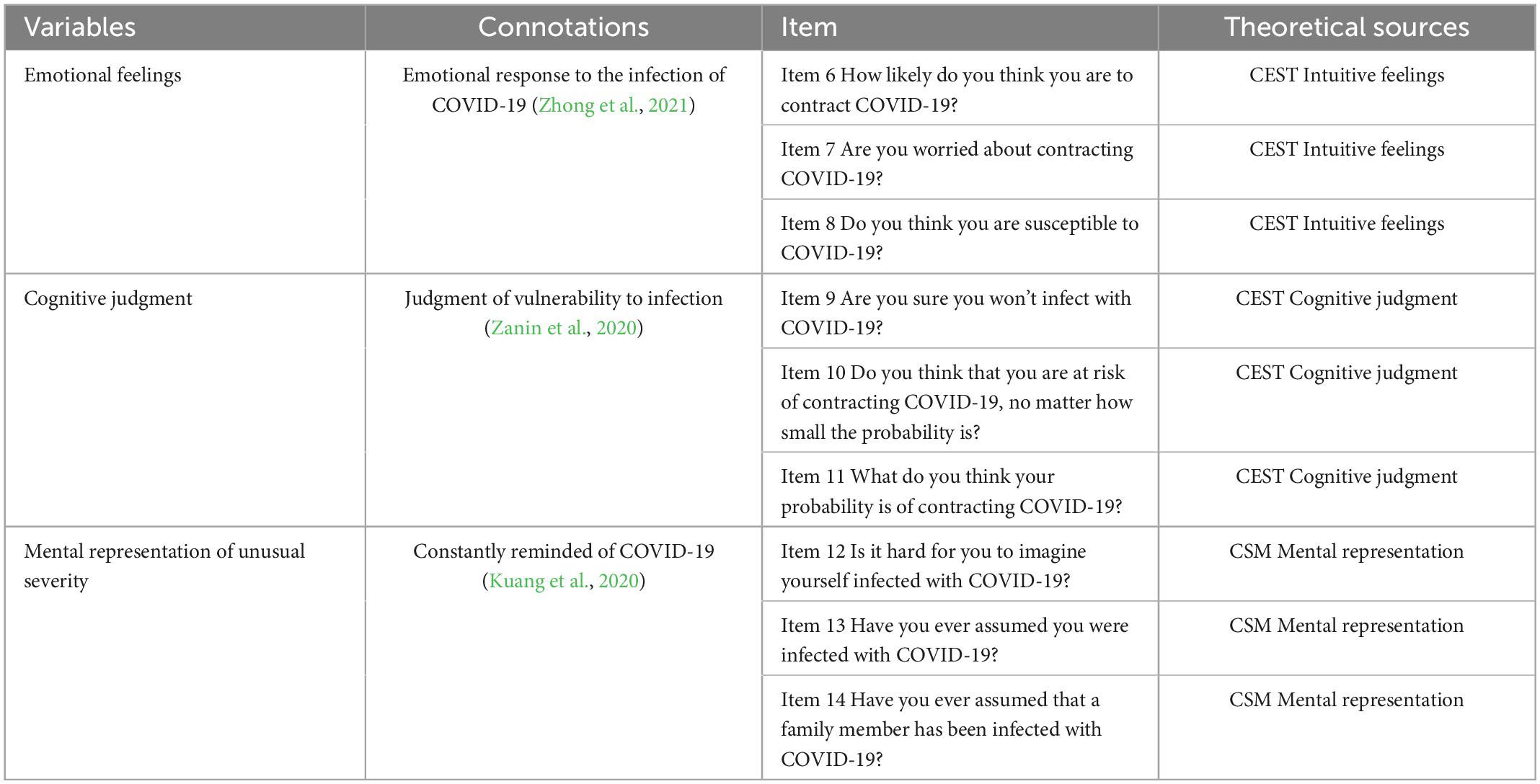
Table 1. Questionnaire items designed based on Cognitive-Experiential Self-Theory (CEST) and Common Sense Model of Risk Perception (CSM).
After validating the questionnaire with the Delphi method, a questionnaire containing four sections was designed for this study. The first part was respondent characteristics, including gender, age, whether or not they had received the COVID-19 vaccination, whether or not they live in a family with children, and education. The second part is about emotional feelings. The third part is about cognitive judgments. The fourth part is about the mental representation of unusual severity. Parts 2, 3, and 4 are scored on a five-point scale, totaling 45 points for the nine questions. Higher scores represent a higher risk perception among the respondents.
This study adopted SPSS 26.0 for statistical analysis. Descriptive statistical analysis, reliability analysis, validity analysis, correlation analysis, and multiple linear regression analysis were conducted for this study. Frequency and composition ratios were used to describe the general information. Means and standard deviations were used to describe the scores, and the questionnaire scores were tested for normality. One-way ANOVA was used to compare the differences in the COVID-19 risk perceptions among people with different characteristics. Multiple linear regression analysis was applied to explore the factors influencing the COVID-19 risk perceptions.
In this study, 400 questionnaires were distributed and returned, of which 380 were valid, and the effective response rate of the questionnaires was 95%. The Effect Size for the data in this study was taken as the Pearson linear correlation coefficient between the variables (x1-x2, x1-x3,., x8-x9 with 9 questions as variables), with a significance level of 0.01, Power is taken as 0.9, and a two-tailed test is performed. The required sample size calculated from the t-test in Python is at least 210. Therefore, a sample size of 380 to meet the needs of this study. The Kaiser-Meyer-Olkin (KMO) test for the data was 0.923, which was greater than 0.9. The Bartlett test was 0, which was less than 0.05. The Cronbach Alpha result was 0.81, which was greater than 0.7. The above tests proved that the data had high reliability and validity and were suitable for analysis. Of the 380 valid questionnaires, 193 were from the CMI group, and 187 were from the NCMI group. The basic information of the respondents is shown in Table 2.
The mean risk perception score for the CMI group was 30.75, with a standard deviation of 7.503. Regarding the emotional feelings, 15.5% of the CMI group felt they were very likely to contract COVID-19, 14% were always worried about contracting COVID-19, and 12.4% felt they were highly vulnerable to contracting COVID-19. Regarding the cognitive judgment, only 4.7% of the CMI group were confident that they would not contract COVID-19, 20.2% strongly believed they were at risk of contracting COVID-19 regardless of the odds, and 16.6% believed that they would inevitably contract COVID-19. Regarding the mental representation of unusual severity, only 6.2% of the CMI group felt they could not imagine themselves with a COVID-19 infection, 18.7% always assumed that they had been infected with COVID-19, and 21.2% always assumed that a family member had been infected with COVID-19. The full results for the centrally isolated group are shown in Appendix A.
Pearson, Kendall, and Spearman correlations were performed to test different characteristics of the CMI group with risk perception scores, and all showed that COVID-19 vaccination, age, whether living in a family with children, education and risk perception scores were significantly correlated, while gender and risk perception scores were not significantly correlated (The correlation analysis results are available in Table 3).
We conducted a multiple linear regression analysis to analyze further the relationship between different characteristics of the CMI group and risk perceptions. We set gender, COVID-19 vaccination, age, whether living in a family with children and education as independent variables and risk perception scores as dependent variables. The F-value was 56.344, and the p-value was less than 0.01, indicating that the regression model was statistically significant (ANOVA test results are available in Table 4).
Then, we conducted a multiple linear regression analysis (The results are available in Table 5). All five independent variables had a p-value of less than 0.05 in the regression model, indicating that they all had a regression effect on the dependent variable. The gender variable was not correlated with the risk perception score, but a regression effect relationship existed. According to the usual standard and existing research practices, we believe that the gender variable was not correlated with risk perception scores (Li and Chen, 2010; Sheng et al., 2022; Xiong et al., 2022). Therefore, we can get the following results in the CMI group: risk perceptions were higher for older age (p < 0.01); risk perceptions were higher for higher education (p < 0.01); risk perceptions were higher for those who had received the COVID-19 vaccination (p < 0.05); and risk perceptions were higher for those who lived in a family with children (p < 0.01).
The average risk perception score for the non-centralized medical isolation (UCMI) group was 28.2 with a standard deviation of 7.129, significantly lower than that of the CMI group (average risk perception score of 30.75 with a standard deviation of 7.503). As shown in Figure 1, we calculated mean scores for each of the nine items measuring risk perception. We found that all scores for the risk perception component of the NCMI group were lower than those of the CMI group. This comparison strongly suggests that experiencing CMI increases the public’s perception of risk.
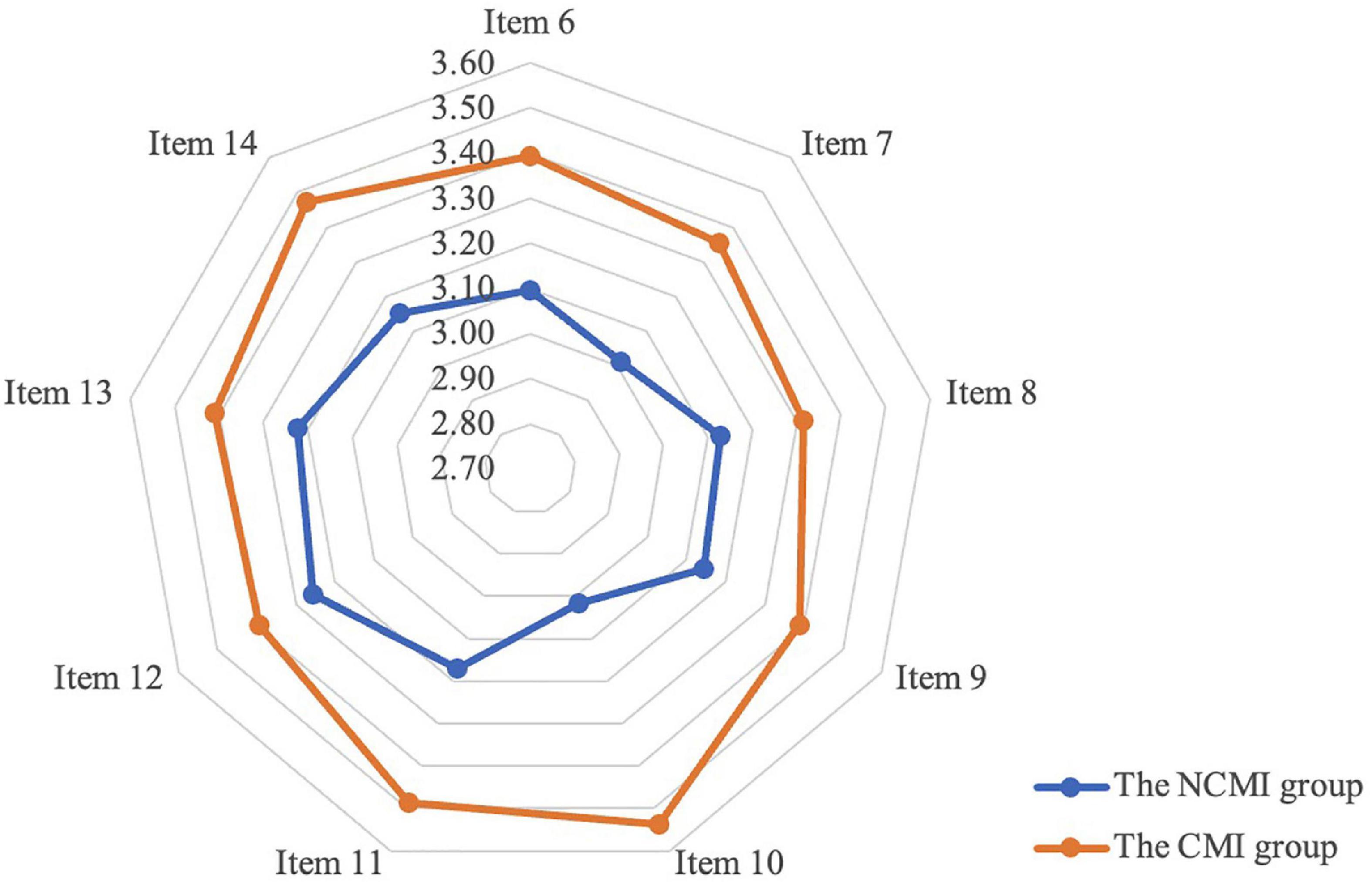
Figure 1. Comparison of risk perception scores between the centralized medical isolation (CMI) group and the non-centralized medical isolation (NCMI) group.
In order to compare the differences in the influencing factors between the CMI group and the NCMI group, correlation and regression analyses were conducted on the risk perception data from the NCMI group (the analysis results are available in Table 6). The results show that gender, COVID-19 vaccination and education did not have a statistically significant regression effect relationship on risk perception scores. Meanwhile, risk perceptions were higher for older age (p < 0.01) and higher for those living in a family with children (p < 0.01). Compared to the CMI group, there was no significant effect of COVID-19 vaccination and education on the risk perceptions of the NCMI group. Such results also suggest that age and living in a family with children significantly affected the public’s perception of risk, regardless of whether they had experienced CMI or not.
The mean risk perception score for the CMI group was 30.75 (out of a total of 45), with a standard deviation of 7.503, placing the risk perception at a high level. After correlation analysis, multiple regression analysis, and comparative analysis, we found that four factors influenced the risk perception of the CMI group.
Firstly, risk perceptions were higher for older age (p < 0.01). The average age of cases of death due to COVID-19 (direct effect or complication) reported from various countries is above 70 years. Public data from the centers for disease control and prevention (CDC) in the USA also show a higher risk of hospitalization and mortality in the older age group following the COVID-19 infection3. Thus, the older age group’s COVID-19 risk perceptions are higher than that of the younger age group (Batsis et al., 2021).
Secondly, risk perceptions were higher for those who had received the COVID-19 vaccination (p < 0.05). Protective behaviors of the public were strongly related to risk perception. When the public have a higher perception of risk, they will have the tendency to adopt protective behaviors to protect themselves (Abdelrahman, 2020; de Bruin and Bennett, 2020). Therefore, groups who had received the COVID-19 vaccination tended to have higher risk perceptions.
Thirdly, risk perceptions were higher for higher education (p < 0.01). More educated people generally had a higher willingness and ability to obtain information, and receiving more information increased their risk perception (Yu et al., 2020). The more educated group typically had relatively lower perceived severity and higher levels of COVID-19 apprehension compared to the less educated group (Rattay et al., 2021).
Fourth, the risk perception of living in a family with children was higher (p < 0.01). Although children are less likely than adults to develop critical illness from COVID-19, COVID-19 is a significant threat to children with underlying medical conditions (Dong et al., 2020). Infection with COVID-19 has an incalculable psychological impact on children and a potential risk of sequelae (Spinelli et al., 2020). People living in families with children are concerned about their children becoming infected with COVID-19, and they must put the extra effort into protecting their children from COVID-19. Furthermore, CMI is a totally closed process during which no relatives are allowed to visit. Groups with children in CMI may be concerned that their children are not better cared for at home, which is one of the key factors contributing to their perception of higher risk. Therefore, the risk perception of COVID-19 is higher among those living in families with children.
The level of COVID-19 risk perceptions was higher in the CMI group compared to the NCMI group. Age and living in a family with children had a significant effect on the COVID-19 risk perceptions in both the CMI groups and the NCMI groups. The COVID-19 vaccination and education did not have a significant effect on the COVID-19 risk perceptions in NCMI groups compared to CMI groups. These results suggest that the public is more concerned about the impact of COVID-19 on the elderly and children, regardless of whether they are in CMI. The CMI groups are people who test positive for nucleic acid for COVID-19 or are close contacts of confirmed cases and they have a greater probability to be detected as infected with COVID-19 (Ju et al., 2021). In addition, the CMI groups are subject to strict epidemiological standards during isolation and are restricted in their freedom for short periods (about 7 days). These measures further increase the psychological stress of the CMI groups and significantly increase their perception of risk.
Among the studies conducted, the study by Alessia et al. (2021) and He et al. (2021) showed an effect of age on the COVID-19 risk perception, with the older the group, the higher the perceived severity of COVID-19. The study results of Ding et al. (2020) and Ning et al. (2020) showed higher risk perception in the highly educated group. The study by He et al. (2021), Yan et al. (2021), and Cao et al. (2022) demonstrated higher risk perception in groups living in a family with children. Our results are consistent with the above studies. In contrast to these studies, we set the question “Have you ever received the COVID-19 vaccination.” Most of the studies that have been done on “risk perception” and “vaccination” have discussed what factors influence people’s perception of the risk of vaccines. However, few studies have captured the perceived risk status of vaccinated and unvaccinated groups. This study compares this and demonstrates that risk perceptions are higher among vaccinated groups, which is essential to studies on risk perceptions of COVID-19 and public self-protection behaviors. The conclusions drawn from this comparative analysis are more objective and scientific than those from studies of a single group.
In the COVID-19 pandemic, CMI policies were implemented mainly in mainland China. For countries that have implemented or are likely to implement CMI policies in similar pandemics in the future, it is crucial to focus on the CMI groups.
Firstly, governments should be cautious in their choice of CMI policies. This study has demonstrated a higher level of risk perception among the CMI groups compared to the NCMI groups. Considering that medical isolation will remain one of the essential measures in dealing with similar pandemics in the future, governments should adopt a more humane approach to medical isolation policies (Zhang, 2020). For example, governments should take the initiative to guide the public toward proper home isolation, and provide CMI and the necessary support for those who do not have access to home isolation.
Secondly, in practice, the government should pay more attention to the CMI groups. Considering the negative psychological impact of CMI, the government should give the CMI groups more care and attention to their psychological health during the isolation period (Wang et al., 2021). The government may consider online interventions for the public during their intensive medical isolation to prevent psychological discomfort and mental depression. At the end of the isolation period, the government should provide free psychological health services to those who need them (Li et al., 2021). For older people and groups raising younger children, the government should provide them with additional help and support.
Finally, this study took the CMI groups as the study object. It demonstrated that the CMI groups had a higher perception of risk than the NCMI groups. Our results have allowed scholars to focus more on the risk perceptions and psychological health issues of the CMI groups and have provided a basis for further research. The comparative analysis of the CMI and NCMI groups in this study also provides a perspective for further research.
This study focuses on the CMI groups in the COVID-19 pandemic, which is one of the strengths. Government and scholars have ignored the COVID-19 risk perceptions in the CMI population. There are no government policies in place to address the psychological and mental health recovery of CMI groups, and few scholars have conducted research on the risk perceptions of CMI groups. However, at least millions of people in China have experienced CMI, and these people’s risk perceptions and psychological health status deserve attention and study. Moreover, medical isolation is an effective means of slowing down the spread of the virus. Therefore, this study’s analysis of risk perceptions of the CMI groups can provide a reference for the government when developing isolation policies in response to similar pandemics in the future. Another strength of this study is that it is a comparative study, which makes the findings more convincing. This study examined both the CMI and NCMI groups. This allowed for an analysis of the risk perceptions of the CMI groups and the factors influencing them, as well as a comparison of their risk perceptions with those of the NCMI groups.
There are some limitations in this study. Ideally, collecting as much basic information about the respondents as possible would have enabled a more accurate analysis of the factors influencing risk perception. However, due to concerns about influencing respondents’ willingness to answer questions, some specific basic information was not collected in this study (presence of accident and commercial insurance in the family, personal income, and presence of chronic diseases). In addition, the length of CMI has a potential impact on the public’s perception of risk, but we did not consider this in the questionnaire, which is a limitation of this study and one of the directions for further research.
This study showed that the COVID-19 risk perceptions was higher in the CMI groups compared to the NCMI groups. Age, COVID-19 vaccination, living in a family with children, and education significantly influenced risk perception in the CMI groups. In the future, scholars can further explore the relationship between income, insurance, chronic illness, and COVID-19 risk perception, particularly the impact of the length of CMI on public risk perception. Countries worldwide may adopt various isolation policies in respond to future pandemics like the COVID-19 outbreak, including CMI. Therefore, governments should pay more attention to the CMI groups to protect their physical health, and ensure their psychological and mental wellbeing. The public is more hopeful that the government has absorbed all the policy lessons learned and that future public health emergencies will not disrupt lives, livelihoods, and wellbeing on the same scale at which COVID-19 did.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was approved by the Ethics Committee of the School of Public Policy and Management of the China University of Mining and Technology (approved 6-2022). This study does not involve human or animal experiments.
RZ: conceptualization, methodology, formal analysis, and writing—original draft. RZ and CW: investigation and writing—review and editing. Both authors read and agreed to the published version of the manuscript.
This research was supported by the Postgraduate Research & Practice Innovation Program of Jiangsu Province (Grant KYCX21_2109).
We thank the questionnaire respondents for their time. We also thank the peer reviewers for their helpful comments and patience. We would especially like to thank Dr. Juchao Li for the assistance with data processing.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abdelrahman, M. (2020). Personality traits, risk perception, and protective behaviors of Arab residents of Qatar during the COVID-19 pandemic. Int. J. Mental Health Addict. 1, 237–248. doi: 10.1007/s11469-020-00352-7
Abu Jamileh, K., Al Hariri, I., Ali, M. R., Saiyed, N. S., Farouk, I. M., Makki, K. H., et al. (2021). Psychological impact of home isolation on children aged 6-14 years during the COVID-19 pandemic in Tabuk, Saudi Arabia 2020. Saudi Med. J. 10, 1098–1102. doi: 10.15537/smj.2021.42.10.20210091
Alessia, R., Floris, T. V., Serena, L., Irene, C., Martine, V., Filippo, R., et al. (2021). Risk perception in a real-world situation (COVID-19): How it changes from 18 to 87 years old. Front. Psychol. 12:646558. doi: 10.3389/fpsyg.2021.646558
Batsis, J. A., Daniel, K., Eckstrom, E., Goldlist, K., Kusz, H., Lane, D., et al. (2021). Promoting healthy aging during COVID-19. J. Am. Geriatr. Soc. 3, 572–580. doi: 10.1111/jgs.17035
Brewer, N. T., Chapman, G. B., Gibbons, F. X., Gerrard, M., McCaul, K. D., and Weinstein, N. D. (2007). Meta-analysis of the relationship between risk perception and health behavior: The example of vaccination. Health Psychol. 2, 136–145. doi: 10.1037/0278-6133.26.2.136
Cao, Y., Chai, J. X., Guo, M. J., Yu, T., Qian, Y. L., and Liu, X. R. (2022). Levels of perceived risk of novel coronavirus pneumonia among parents of children in Beijing under regular prevention and control in 2021. J. Prevent. Med. Inform. Available online at: http://kns.cnki.net/kcms/detail/51.1276.R.20221027.1134.001.html
Capone, V., Donizzetti, A. R., and Park, M. S. A. (2021). Validation and psychometric evaluation of the COVID-19 risk perception scale (CoRP): a new brief scale to measure individuals’ risk perception. Int. J. Mental Health Addict. [Epub ahead of print] doi: 10.1007/s11469-021-00660-6
Cui, X. Q., Hao, Y. H., Tang, S. Y., Fan, S. K., Tang, Y. R., Ning, N., et al. (2021). Reliability testing and application of the COVID-19 pandemic risk perception scale - an empirical study based on a large data sample. Chin. J. Public Health 7, 1086–1089. doi: 10.11847/zgggws1133952
de Bruin, W. B., and Bennett, D. (2020). Relationships between initial COVID-19 risk perceptions and protective health behaviors: a national survey. Am. J. Prevent. Med. 2, 157–167. doi: 10.1016/j.amepre.2020.05.001
Denerel, N., Senisik, S., Koyagasioglu, O., Cigdem, S., and Tunc, S. (2022). Effects of long-duration home isolation linked to the COVID-19 pandemic on mental health of adolescent athletes. Pediatr. Exerc. Sci. 4, 170–176. doi: 10.1123/pes.2020-0164
Ding, Y. N., Du, X. Y., Li, Q. M., Zhang, M., Zhang, Q. J., Tan, X. D., et al. (2020). Risk perception of coronavirus disease 2019 (COVID-19) and its related factors among college students in China during quarantine. PLoS One 8:e0237626. doi: 10.1371/journal.pone.0237626
Dong, Y. Y., Mo, X., Hu, Y. B., Qi, X., Jiang, F., Jiang, Z. Y., et al. (2020). Epidemiology of COVID-19 among children in China. Pediatrics 6, doi: 10.1542/peds.2020-0702
Ferrer, R., and Klein, W. M. (2015). Risk perceptions and health behavior. Curr. Opin. Psychol. 5, 85–89. doi: 10.1016/j.copsyc.2015.03.012
He, S., Kong, L. N., and Liu, W. W. (2021). Analysis of risk perceptions and related factors concerning COVID-19 epidemic in Chongqing China. J. Commun. Health 46, 278–285. doi: 10.1007/s10900-020-00870-4
Jiang, L. F., Luo, X. L., Zheng, Y. T., Ye, C. M., and Sun, X. Y. (2022). A study of the psychological situation of inmates in isolation at the Centralized Isolation Medical Observation Site. Modern Prevent. Med. 21, 4003–4008. doi: 10.20043/j.cnki.MPM.202202329
Ju, Y. M., Chen, W. T., Liu, J., Yang, A. P., Shu, K. L., Zhou, Y., et al. (2021). Effects of centralized isolation vs. home isolation on psychological distress in patients with COVID-19. J. Psychosom. Res. 143:110365. doi: 10.1016/j.jpsychores.2021.110365
Kuang, J. Y., Ashraf, S., Das, U., and Bicchieri, C. (2020). Awareness, risk perception, and stress during the COVID-19 pandemic in communities of Tamil Nadu, India. Int. J. Environ. Res. Public Health 19:7177. doi: 10.3390/ijerph17197177
Leventhal, H., Leventhal, E. A., and Contrada, R. J. (1998). Self-regulation, health, and behavior: A perceival-cognitive approach. Psychol. Health 4, 717–733. doi: 10.1080/08870449808407425
Li, B., Fan, B. F., Xie, B., Chen, Y., and He, Q. (2021). Construction of a model for the management of psychological services in centralized isolation medical observation sites. Chin. J. Public Health 7, 1082–1085. doi: 10.11847/zgggws1132472
Li, X. S., and Chen, Z. Z. (2010). How to properly apply SPSS software to do principal component analysis. Stat. Res. 8, 105–108. doi: 10.19343/j.cnki.11-1302/c.2010.08.016
Lucy, E. N., Dennis, G. F., and Grace, L. R. (2012). Development of the perceived risk of HIV scale. AIDS Behav. 16, 1075–1083.
Luo, F. X., Gheshlagh, R. G., Dalvand, S., Saedmoucheshi, S., and Li, Q. Y. (2021). Systematic review and meta-analysis of fear of COVID-19. Front. Psychol. 12:661078. doi: 10.3389/fpsyg.2021.661078
Ning, L. W., Niu, J. Y., Bi, X. J., Yang, C., Liu, Z., Wu, Q. H., et al. (2020). The impacts of knowledge, risk perception, emotion and information on citizens’ protective behaviors during the outbreak of COVID-19: a cross-sectional study in China. BMC Public Health 1:1751. doi: 10.1186/s12889-020-09892-y
Pacini, R., Muir, F., and Epstein, S. (1998). Depressive realism from the perspective of cognitive-experiential self-theory. J. Pers. Soc. Psychol. 4, 1056–1068. doi: 10.1037/0022-3514.74.4.1056
Parisi, R., Lagomarsino, F., Rania, N., and Coppola, I. (2021). Women face to fear and safety devices during the COVID-19 pandemic in Italy: Impact of physical distancing on individual responsibility, intimate, and social Relationship. Front. Public Health 9:622155. doi: 10.3389/fpubh.2021.622155
Rania, N., and Coppola, I. (2022). The fear of contagion and the attitude toward the restrictive measures imposed to face COVID-19 in Italy: The psychological consequences caused by the pandemic one year after it began. Front. Psychol. 13:805706. doi: 10.3389/fpsyg.2022.805706
Rattay, P., Michalski, N., Domanska, O. M., Kaltwasser, A., De Bock, F., Wieler, L. H., et al. (2021). Differences in risk perception, knowledge and protective behavior regarding COVID-19 by education level among women and men in Germany. Results from the COVID-19 Snapshot Monitoring (COSMO) study. PLoS One 5:e0251694. doi: 10.1371/journal.pone.0251694
Shechory, B. M., and Laufer, A. (2021). Fear of the unknown: Does fear of terrorism differ from fear of contracting COVID-19? Front. Psychol. 12:660777. doi: 10.3389/fpsyg.2021.660777
Sheng, J. L., Li, J. C., and Yang, J. (2022). Tail dependency and risk spillover between oil market and Chinese sectoral stock markets-An assessment of the 2013 refined oil pricing reform. Energies 16:6070. doi: 10.3390/en15166070
Shi, K., Lu, J. F., Fan, H. X., Jia, J. M., Song, Z. L., Li, W. D., et al. (2003). A model for predicting the rational characteristics and psychological behaviour of the population in 17 cities during the SARS crisis. Chin. Sci. Bull. 13, 1378–1383.
Slone, M., Pe’er, A., and Mor, F. (2022). Previous trauma exposure and self-mastery as moderators of psychiatric effects of home isolation during the Covid-19 pandemic: a field study. BMC Psychiatry 22:450. doi: 10.1186/s12888-022-04087-8
Spinelli, M., Lionetti, F., Pastore, M., and Fasolo, M. (2020). Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Front. Psychol. 11:1713. doi: 10.3389/fpsyg.2020.01713
Taghrir, M. H., Borazjani, R., and Shiraly, R. (2020). COVID-19 and Iranian medical students; A survey on their related-knowledge, Preventive behaviors and risk perception. Arch. Iran. Med. 4, 249–254. doi: 10.34172/aim.2020.06
Wang, W., Huang, C., Pang, X. H., Wang, Y., and Sun, X. G. (2021). Investigation of a centralized isolation medical observation site for COVID-19 in Beijing. Chin. J. Public Health 7, 1077–1081. doi: 10.11847/zgggws1134202
Weinstein, N. D., and Nicolich, M. (1993). Correct and incorrect interpretations of correlations between risk perceptions and risk behaviors. Health Psychol. 3, 235–245. doi: 10.1037/0278-6133.12.3.235
Wise, T., Zbozinek, T. D., Michelini, G., Hagan, C. C., and Mobbs, D. (2020). Changes in risk perception and self-reported protective behavior during the first week of the COVID-19 pandemic in the United States. R. Soc. Open Sci. 9:200742. doi: 10.1098/rsos.200742
Xi, J. Z., She, Z., Ju, K., Zhao, J. J., Hou, X. L., Peng, Y. N., et al. (2020). Development and validation of the COVID-19 outbreak risk perception scale. J. Capital Norm. Univ. 4, 131–141.
Xie, X. F., Zheng, R., Xie, D. M., and Wang, H. (2005). Analysis of the phenomenon of psychological panic in SARS. Acta Sci. Nat. Univ. Pekinen. 4, 628–639. doi: 10.13209/j.0479-8023.2005.082
Xiong, Y. C., Zhang, C. L., Qi, H., Zhang, R., and Zhang, Y. B. (2022). How to measure the safety cognition capability of urban residents? an assessment framework based on cognitive progression theory. Front. Psychol. 13:707172. doi: 10.3389/fpsyg.2022.707172
Yan, J. Q., Kim, S., Zhang, S. X., Foo, M. D., Alvarez-Risco, A., Del-Aguila-Arcentales, S., et al. (2021). Hospitality workers’ COVID-19 risk perception and depression: A contingent model based on transactional theory of stress model. 95:102935. doi: 10.1016/j.ijhm.2021.102935
Yu, T. K., Lavallee, J. P., Di, G. B., Chang, I. C., and Yu, T. Y. (2020). Risk perception and response toward climate change for higher education students in Taiwan. Environ. Sci. Pollut. Res. 20, 24749–24759. doi: 10.1007/s11356-019-07450-7
Zanin, G. M., Gentile, E., Parisi, A., and Spasiano, D. (2020). A preliminary evaluation of the public risk perception related to the COVID-19 health emergency in Italy. Int. J. Environ. Res. Public Health 9:3024. doi: 10.3390/ijerph17093024
Zhang, M. M., Niu, N., Zhi, X. X., Zhu, P., Wu, B., Wu, B. N., et al. (2020). Nurses’ psychological changes and coping strategies during home isolation for the 2019 novel coronavirus in China: A qualitative study. J. Adv. Nurs. 1, 308–317. doi: 10.1111/jan.14572
Zhang, R., Wang, C. L., Li, C. G., and Xiong, Y. C. (2023). Policy implementation challenges and the ritualization of public health emergency plans: An investigation of urban communities in Jiangsu Province, China. Front. Public Health 10:1047142. doi: 10.3389/fpubh.2022.1047142
Zhang, X. Y. (2020). The improvement of the administrative isolation system of epidemic prevention from the perspective of the rule of law - A study on the example of administrative isolation of human epidemic prevention. Admin. Reform. 8, 27–33. doi: 10.14150/j.cnki.1674-7453.2020.08.004
Zhang, Y. B., Huang, Y. S., Wang, Y. B., and Casey, T. W. (2020). Who uses a mobile phone while driving for food delivery? The role of personality, risk perception, and driving self-efficacy. J. Safety Res. 73, 69–80. doi: 10.1016/j.jsr.2020.02.014
Zhong, Y. P., Liu, W. H., Lee, T. Y., and Zhao, H. (2021). Risk perception, knowledge, information sources and emotional states among COVID-19 patients in China. Nurs. Outl. 1, 13–21. doi: 10.1016/j.outlook.2020.08.005
Keywords: COVID-19, risk perception, centralized medical isolation, psychological health, cognitive-experiential self-theory (CEST), common sense model of risk perception (CSM)
Citation: Zhang R and Wang C (2023) Risk perception of COVID-19 and its related factors among centralized medical isolation groups in China. Front. Psychol. 14:1131076. doi: 10.3389/fpsyg.2023.1131076
Received: 24 December 2022; Accepted: 13 January 2023;
Published: 01 February 2023.
Edited by:
Hui Qi, North China Institute of Science and Technology, ChinaReviewed by:
Zenan Sun, Jiangsu University, ChinaCopyright © 2023 Zhang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chengli Wang,  Y3VtdHNzY2ljb21lQDE2My5jb20=
Y3VtdHNzY2ljb21lQDE2My5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.