
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
HYPOTHESIS AND THEORY article
Front. Psychol. , 22 June 2023
Sec. Health Psychology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1121986
This article is part of the Research Topic Coping with Life Stress, volume II View all 15 articles
Background: Maintaining good mental health is important during a crisis. However, little attention has been given to how people achieve this, or how they evaluate emotions associated with stressors, such as the COVID-19 pandemic. This study aims to (1) investigate whether emotion regulation, in particular cognitive reappraisal and suppression, moderates the relationship between COVID-19 stress and general mental distress and (2) examine gender differences in the interrelations between COVID-19 stress, emotion regulation, and mental distress.
Methods: Data from a population in Norway (n = 1.225) were collected using a cross-sectional survey during the early months of the COVID-19 pandemic. Emotion regulation was measured using the Emotion Regulation Questionnaire Scale (ERQ), COVID-19 stress with the COVID-19 Stress Scale, and mental distress with the Patient Health Questionnaire 4 (PHQ-4). Moderation analyses were conducted using the PROCESS macro for SPSS.
Results: There was a strong association between COVID-19 stress and general mental distress (r = 0.61). The moderation analyses showed substantial moderation effects of cognitive reappraisal and suppression on the relationship between COVID-19 stress and mental distress. Cognitive reappraisal served as a buffer (p = 0.001) and suppression (p = 0.002) exacerbated the relation between COVID-19 stress and mental distress. Men had higher scores of suppression (p < 0.001), and women had higher scores of cognitive reappraisal (p = 0.025). The buffering effect of cognitive reappraisal presented itself only in women (p < 0.001), while the exacerbation effect of suppression appeared only in men (p < 0.001).
Conclusion: The current study suggests that COVID-19 pandemic-related stress is easier to deal with for those who have the tendency to cognitively reappraise. In contrast, suppression is associated with symptoms of depression and anxiety. The prevention of mental distress can be supported by guiding people about the importance of using healthy emotion regulation strategies, as well as helping them to become more aware of the way they interpret and regulate their emotions. Gender differences in emotion regulation suggest gender awareness, e.g., tailored programs for men and women.
In early 2020, SARS-CoV-2 infected millions of people and the death toll associated with COVID-19 increased rapidly worldwide (WHO, 2020; Schöley et al., 2022). To limit and delay the COVID-19 outbreak, societies went into lockdown, and both the pandemic and its aftermath changed the daily life of most people globally (OECD, 2021; WHO, 2022b). During the first year of the pandemic the global prevalence of anxiety and depression increased by 25% (WHO, 2022a). This increase in mental distress is documented in numerous systematic reviews and meta-analyses reporting that the COVID-19 pandemic has generated major psychological health problems worldwide (e.g., Cénat et al., 2021; Wu et al., 2021; Robinson et al., 2022). Today, research shows that many people have rebounded from the mental distress caused by the pandemic, mostly returning to previous health. However, a small but significant number of individuals are still suffering from mental health problems (Lopez-Leon et al., 2021; Saunders et al., 2021; Robinson et al., 2022). Moreover, mental health problems are associated with long COVID, a chronic condition with high incidence rates (Lopez-Leon et al., 2021; Sachs et al., 2022).
According to the Lancet COVID-19 commission, governments around the world were too slow to acknowledge the seriousness of the pandemic and act with urgency in response (Sachs et al., 2022). Norway with a population of 5.3 million people was probably among the first countries to implement a nationwide lockdown on March 12, 2020 (Ursin et al., 2020; Andreas, 2021). The lockdown in Norway included school closures, working from home and limitations on nonessential services (sports, non-essential business etc.). Overall, only grocery stores, pharmacies, and gas stations remained open. The authorities also implemented forced self-isolation for those at risk of infection and those who were infected. In addition, they implemented several quarantine restrictions, travel restrictions, prohibition from staying overnight in holiday cabins across municipal borders, as well as spatial distancing and the compulsory wearing of face masks in public places (Ursin et al., 2020; Andreas, 2021; Blix et al., 2021). Experiencing the outbreak of a novel and life-threatening virus disease, together with the restrictions on individuals’ autonomy and freedom, seems to have prompted an increase in mental distress in many people in Norway, particularly during the first months of the COVID-19 outbreak (Hoffart et al., 2020; Blix et al., 2021; Ebrahimi et al., 2021; Ernstsen and Havnen, 2021; Lassen et al., 2022). Even though Norway’s mortality and infection rate from Sars-CoV-2 were low compared to many other countries (Hvide and Johnsen, 2022), loneliness and fear were reported as substantial factors associated with mental distress during the outbreak (Hoffart et al., 2020; Bemanian et al., 2021; Blix et al., 2021; Ebrahimi et al., 2021).
Although individuals may face the same stressful event (for example COVID-19) there are individual differences in how associated negative emotions are experienced or regulated (Gross and John, 2003; Too and Butterworth, 2018; Raymond et al., 2019). Recent studies found that during the COVID-19 pandemic, several resources and resilience factors played moderating and/or mediating roles in the associations between stressful experiences and mental health, e.g., individuals’ sense of meaning of life (Schnell and Krampe, 2020), locus of control (Krampe et al., 2021), psychological flexibility (Smith et al., 2020), personality traits (Bacon and Corr, 2020; Smith et al., 2020; Liu et al., 2021; Abdelrahman, 2022; Lassen et al., 2022), as well as emotion regulation abilities (Xu et al., 2020; Liang et al., 2021; Ye et al., 2021; Gullo et al., 2022; Vertsberger et al., 2022). These findings imply that the way individuals deal with negative emotions in their daily lives, as well as under long term crises (e.g., pandemic), can either be a motivation for coping or it can have a negative impact on mental health and well-being (Garland et al., 2011; Conway et al., 2013; Xu et al., 2020).
Gross (1998b) differentiates between two emotion regulation strategies in his process model of emotion regulation: cognitive reappraisal and suppression. Both cognitive reappraisal and suppression behaviour operate along a continuum from conscious, effortful controlled regulation of emotions to unconscious, effortless, and automatic regulation (Gross and Thompson, 2006; Bargh and Williams, 2007). Emotion regulation is an important protective factor, and it concerns individuals’ attempts to control (modify) their emotions to respond in a flexible and adaptive way to the environment (Gross, 1998a; Boyes et al., 2016). Cognitive reappraisal involves a reinterpretation of a situation into a more positive light (Ford et al., 2017), changing its potential meaning. Notably, it is not the situation itself that is changed, it is the individual’s evaluation of the situation (Gross and Barrett, 2011; Raymond et al., 2019). Cognitive reappraisal can be employed prior to experiencing an emotion (Gross, 1998a), and it is therefore an effective strategy to reduce negative emotions through reframing emotion-eliciting experiences or stimuli (Gross and John, 2003). The second major emotion regulation strategy is suppression, involving the conscious inhibition of one’s emotion expressive behaviors, whether they are covert, overt or both (Lazarus and Alfert, 1964; Gross, 1998a). Suppression is a response-focused strategy that intervenes once an emotion is “under way,” or after the emotional response has been triggered (Gross, 1998a). For example, an individual may not be able to express their anxiety or fear about COVID-19, and may thus suppress their outer expression of negative emotion by putting on a façade of control, mutual agreement, or by becoming “paralyzed” by overwhelming negative emotions and therefore being unable to move forward. An individual inner emotion would thus remain unchanged, meaning that the expression of negative emotions is suppressed.
Cognitive reappraisal and suppression differ in their adaptiveness in regard to promoting or undermining psychological health (for review, see Aldao and Nolen-Hoeksema, 2010). Extensive research shows that cognitive reappraisal is beneficial for psychological health (for review, see Webb et al., 2012; Hu et al., 2014), and that it is linked to resilience, positive affect, mental well-being, increased life satisfaction, better job performance, as well as favorable cognitive and social outcomes (Gross and John, 2003; John and Gross, 2004; Kashdan et al., 2006; Kraiss et al., 2020). In contrast, suppression is considered a maladaptive strategy, associated with worse psychological health outcomes (Aldao et al., 2010; Hu et al., 2014; Chervonsky and Hunt, 2017; Cameron and Overall, 2018). The tendency to withhold the expression of emotions is linked to, for example, impaired interpersonal relationships, greater anxiety and depression, poorer life satisfaction, lack of authenticity, lower self-esteem and increased negative emotions (Gross and John, 2003; Kashdan et al., 2006; English and John, 2013). The differential effects of cognitive reappraisal and suppression have also been confirmed in several correlational studies during the pandemic (Cardi et al., 2021; Liang et al., 2021; Low et al., 2021; Santi et al., 2021; Ye et al., 2021; Gullo et al., 2022).
Moreover, previous research found that emotion regulation is a significant moderator of the association between stress and symptoms of anxiety and depression. While cognitive reappraisal seems to buffer the relationship between stress and symptoms of anxiety and depression (Troy et al., 2010; Vanderhasselt et al., 2014; Johnson et al., 2016), suppression seems to exacerbate the relationship between stress and anxiety/depression (Boyes et al., 2016; Hosogoshi et al., 2020). Recent COVID-19 studies also investigated the moderating role of emotion regulation in diverse populations. The majority of the investigations found that cognitive reappraisal buffered the positive relationships between diverse types of perceived stress and subjective health (Prikhidko et al., 2020; Xu et al., 2020; Yang et al., 2020; Gröndal et al., 2021; Kuhlman et al., 2021; Raio et al., 2021; Ye et al., 2021; Chen et al., 2022; Vertsberger et al., 2022), while suppression exacerbated these relationships (Wu et al., 2021; Ye et al., 2021; Chen et al., 2022). However, some investigations did not find the buffering effect of cognitive reappraisal (Zhang et al., 2021) or the exacerbating effect of suppression (Yang et al., 2020; Gröndal et al., 2021; Raio et al., 2021).
Various studies indicate gender differences in emotion regulation (Tamres et al., 2002; Nolen-Hoeksema, 2012; Rogier et al., 2019). Women generally seem to use more emotion regulation strategies than men, including cognitive reappraisal, but not expressive suppression (Tamres et al., 2002; Goubet and Chrysikou, 2019). Importantly, data suggest that women apply emotion regulation strategies in more flexible ways (Goubet and Chrysikou, 2019). Concerning gender differences in the use of the specific strategies of cognitive reappraisal and suppression, the evidence is inconsistent. Several researchers showed that women have a stronger tendency to use cognitive reappraisal (Tamres et al., 2002; Nolen-Hoeksema and Aldao, 2011; Megıas-Robles et al., 2019; Rogier et al., 2019), while men seem to tend toward expressive suppression (Flynn et al., 2010; Megıas-Robles et al., 2019; Rogier et al., 2019; Santi et al., 2021). However, some studies did not find these differences for either cognitive reappraisal (Santi et al., 2021) or suppression (Tamres et al., 2002; Nolen-Hoeksema and Aldao, 2011). The evidence is also inconclusive regarding the interplay of emotion regulation, stress and mental distress. On the one hand, convincing data suggest that the interrelations of emotion regulation and forms of stress and mental distress are rather similar in women and men (Aldao and Nolen-Hoeksema, 2012; Lutz et al., 2022). On the other hand, a variety of gender differences have been reported. For example, in several studies, gender moderated the associations of reappraisal and suppression with diverse mental health outcomes, with significant effects sometimes only in men (Flynn et al., 2010; Rogier et al., 2019; Jiang et al., 2022), sometimes only in women (Nolen-Hoeksema, 2012; Rogier et al., 2019), and sometimes in different ways in men and women (Flynn et al., 2010; Megıas-Robles et al., 2019; Zhang et al., 2020; Jiang et al., 2022). Gender analyses of emotion regulation are sparse in psychosocial COVID-19 research. While Li et al. (2022) found higher reappraisal scores in women and higher suppression scores in men, Canlı and Karaşar (2020) and Santi et al. (2021) reported higher suppression scores in men, but no gender differences for reappraisal. Rodas et al. (2022) stated some moderation effects of gender but they did not describe these. Muñoz-Navarro et al. (2021) found that emotion regulation strategies mediated the associations between COVID-19 worries and anxiety differently in women and men. Finally, Panno et al. (2022) showed that cognitive reappraisal was negatively associated with COVID-19 stress and general mental distress in women but not in men, while there were no gender effects for the association of suppression with COVID-19 stress and mental distress. To our knowledge, until now, gender comparisons have not been published for the buffering and exacerbating effects of reappraisal and suppression, respectively.
The aims of this study were to (1) investigate whether emotion regulation moderated the relationship between COVID-19 stress and general mental distress during the first months of the pandemic in a community sample from Norway (Figure 1), and (2) examine in an exploratory way to what extent there were gender differences in the interrelations between COVID-19 stress, emotion regulation, and mental distress. After descriptive analyses, we performed moderation analyses for the complete sample. In the next step, we compared men and women regarding the study variables and repeated moderation analysis separately for women and men. We argue that high cognitive reappraisal will buffer the relationship between COVID-19 stress and general mental distress, and suppression will strengthen the relationship between COVID 19 stress and general mental distress. Previous research, using the same dataset, showed that COVID-19 stress was positively related to general mental distress in a population in Norway during the early months of the COVID-19 pandemic (Krampe et al., 2021). Consequently, COVID-19 stress and general mental distress are key research variables in this study. Age was included as a covariate, given that research shows emotion regulation behaviour is linked to lifespan (Carstensen et al., 2011). Regarding gender differences, we expected women to show higher scores of cognitive reappraisal and men to show higher scores of expressive suppression. Given the conflicting evidence on gender effects within the relations of stress, emotion regulation and mental health, the separate moderation analyses for women and men were performed in an explorative way.
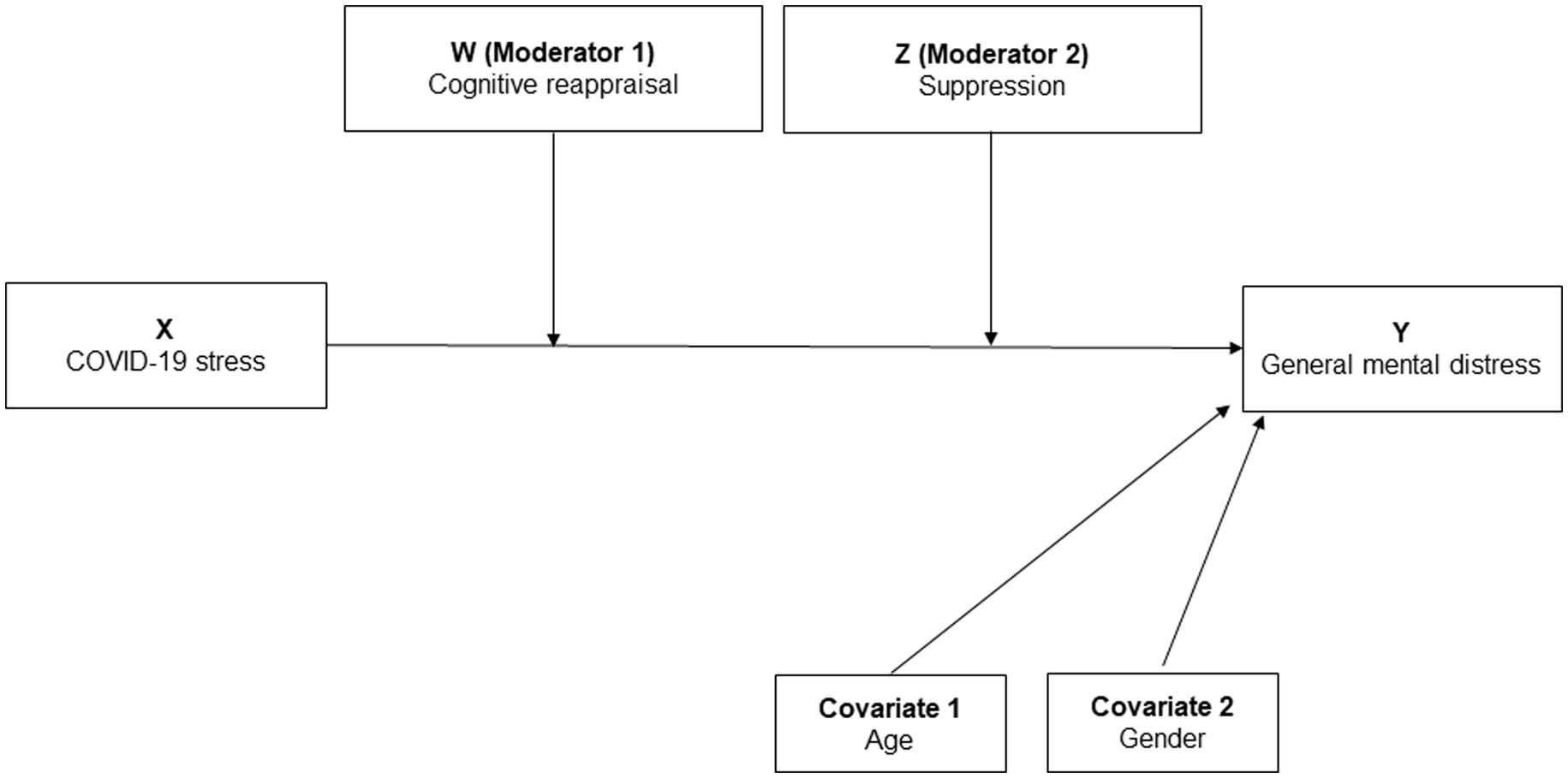
Figure 1. Conceptual model of how cognitive reappraisal (ERQ-CR) and suppression (ERQ-S) moderate the relationship between COVID-19 stress and general mental distress (PHQ 4) (double moderator, PROCESS model 2, n = 1,207).
This cross-sectional study was conducted in Norway (n = 1,225) from the period May 26th to June 4th 2020. During this time the Norwegian Government’s COVID-19 regulations were gradually eased (Hansen et al., 2021). The study was distributed on several web pages of the collaborating institutions (e.g., Innlandet Hospital Trust, MF Specialized University, University of Stavanger) as well as forwarded by social media (e.g., Facebook). All participants expressed their informed consent by explicitly agreeing to continue with the questionnaire after being informed about the study’s aims, employed data protection, participants’ rights, and contact points for questions or concerns. Participation was voluntary and with no compensation. Ethical approval was obtained by Personvernombudet Innlandet Hospital Trust, Norway, No. 20/02104–1.
The COVID-19 Stress Scale comprises seven items and involves a broad range of affective stress reactions to the pandemic situation (e.g., feelings of intolerability, boredom, anger and being left alone) as well as fears and pessimism about personal resources and the future (Schnell and Krampe, 2020). Sample items include “I am irritated” and “I am afraid of the pandemic and what will happen to us.” The response scale ranged from 0 (strongly disagree) to 5 (strongly agree). Cronbach’s alpha in this study was α = 0.73. Confirmatory factor analyses were conducted showing a one-dimensional model of COVID-19 stress (Krampe et al., 2021). The scale has proven valid in several studies (Schnell and Krampe, 2020, 2022a,b; Dyrendal and Hestad, 2021; Krampe et al., 2021; Schnell et al., 2021).
General mental distress was measured with the Patient Health Questionnaire 4, PHQ-4 (4 items) (Kroenke et al., 2009, 2010). The PHQ-4 has demonstrated good reliability and validity in both clinical and population samples in Norway (Andreassen et al., 2019; Solem et al., 2021) and measures core symptoms of current depression and anxiety. Participants were asked to respond to the items in regard to the past two weeks (“Over the last 2 weeks, how often have you been bothered by the following problems?”). Sample items included “Little interest or pleasure in doing things” (depression) and “Feeling nervous, anxious or on edge” (anxiety). The response scale ranged from 0 = not at all to 3 = nearly every day. The sum score ranges from 0 to12, and cut-off points > 2, >3, and > 5 indicate mild, moderate, and severe mental distress, respectively (Kroenke et al., 2009; Kerper et al., 2014). Cronbach’s alpha in this study was α = 0.82.
Emotion regulation was measured using the 10-item Emotion Regulation Questionnaire (ERQ: Gross and John, 2003). This is one of the most widely used instruments to measure emotion regulation and has shown good psychometric properties in both clinical and population samples (Gómez-Ortiz et al., 2016; Sætren et al., 2019; Preece et al., 2020). Instructions were adjusted to how participants generally regulated their emotions when encountering stressful situations during COVID-19 restrictions. Participants were asked to rate the degree to which they regulated their emotions via cognitive reappraisal (6 items, sample item, e.g., “When I want to experience more positive emotions, I change my way of thinking”) – or via suppression (4 items, sample item, e.g., “I control my feelings by not expressing them”). The response scale ranged from 1 (strongly disagree) to 7 (strongly agree). The measures were translated from English into Norwegian and then professionally and independently back-translated to ensure language equivalence. After some adjustment, the back-translation was approved by the original developer James Gross (personal communication). In this study, Cronbach’s alphas of the two subscales were α = 0.88 for cognitive reappraisal and α = 0.81 for suppression.
For all statistical tests, a two tailed value of p < 0.05 was considered statistically significant. Due to their small number, data from participants identifying as gender diverse were excluded from analyses that contained gender as a variable (n = 2). To test whether cognitive reappraisal and suppression moderate the relationship between COVID-19 stress and general mental distress (HQ1) a double moderation analysis was conducted using PROCESS 4.1 macro for SPSS (version 27), model 2 (Hayes and Andrew, 2013; Figure 1). PROCESS is a widely used regression-based path analytic approach to modeling mediation and moderation relationships, and therefore appropriate for testing our first hypothesis (Hayes et al., 2017). The moderation analyses employed bootstrapping with 5,000 samples. Independent t-test and a gender specific moderation analysis were applied to evaluate any gender differences in emotion regulation.
Means, standard deviations and inter-correlations among the study variables are reported in Table 1. While COVID-19 stress and general mental distress showed a large positive correlation, all other correlations were of moderate to small size. Both COVID-19 stress and general mental distress correlated negatively with cognitive reappraisal and positively with suppression. Younger age was related to higher values in COVID-19 stress, general mental distress, and suppression. Gender was only marginally related to COVID-19 stress, general mental distress, cognitive reappraisal and age, but markedly associated with suppression (Table 2).
Cognitive reappraisal and suppression moderated the relationship between COVID-19 stress and general mental distress (Table 3). As expected, the positive relationship between COVID-19 stress and general mental distress was moderated negatively by cognitive reappraisal (B = −0.17, SE = 0.05, p ≤ 0.001) and positively by suppression (B = 0.15, SE = 0.05, p = 0.002) (Table 3). Both cognitive reappraisal and suppression acted as independent moderators (Figure 2). When COVID-19 stress was low, general mental distress was also low, regardless of the extent of emotion regulation through cognitive reappraisal or suppression. However, with increasing COVID-19 stress, general mental distress levels were significantly higher for those who suppressed their emotions and for those who used less cognitive reappraisal. The model was significant at F(7, 1,199) =125.22, p < 0.001. COVID-19 stress, cognitive reappraisal, suppression, age and gender explained 42% of the variance in general mental distress.
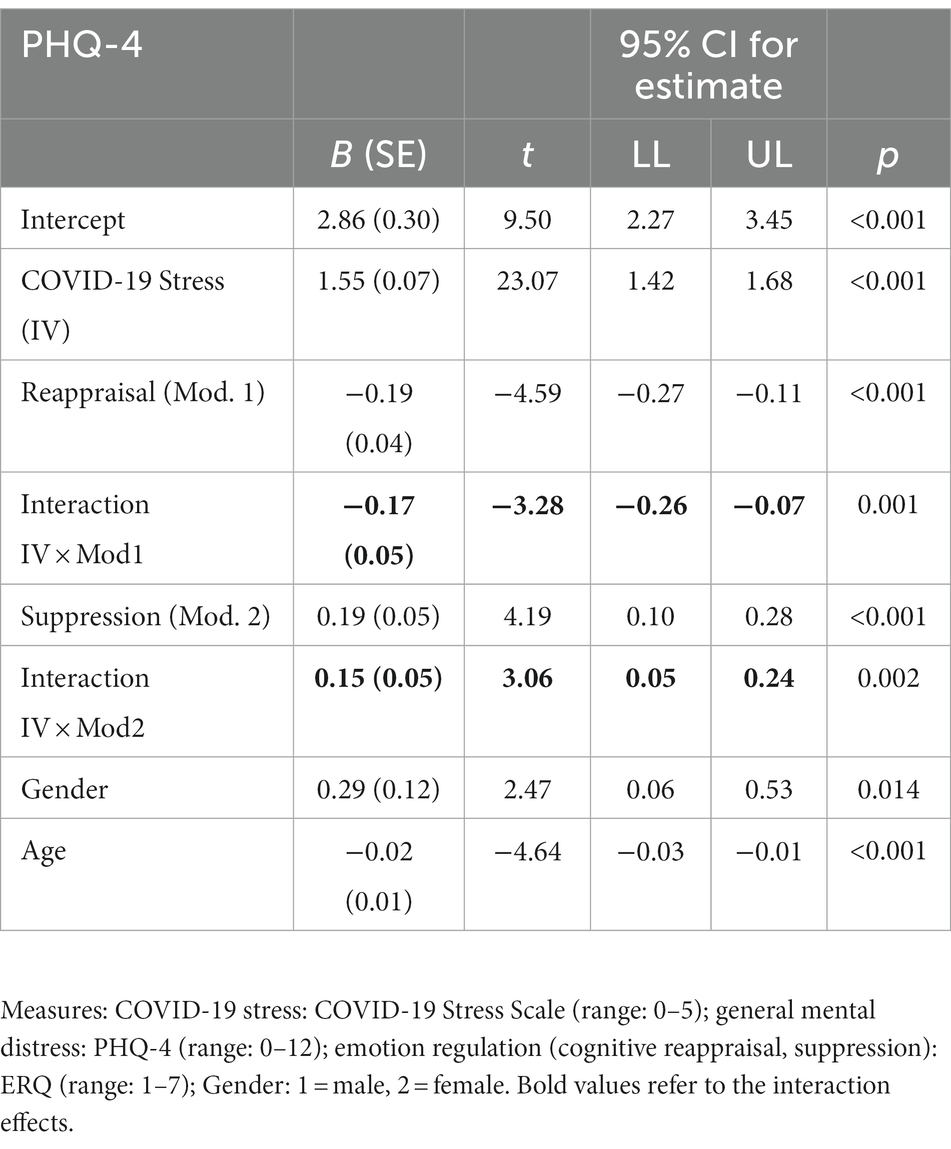
Table 3. Cognitive reappraisal and suppression as moderators of the relationship between COVID-19 stress and general mental distress; n = 1,207.
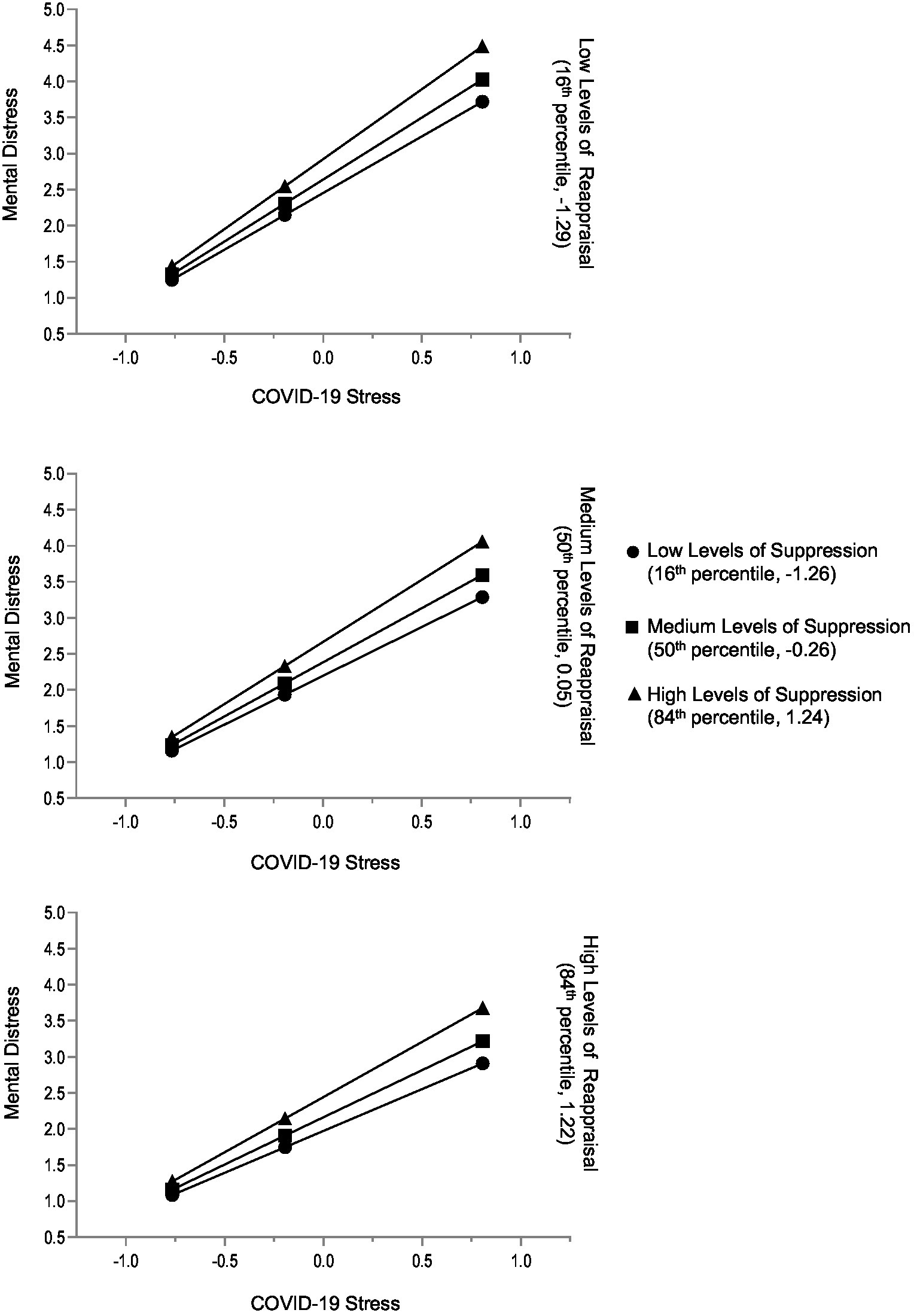
Figure 2. Total sample: conditional effects of COVID-19 stress on general mental distress for low, medium, and high levels of reappraisal and low, medium, and high levels of suppression. The variables ERQ Suppression, ERQ Reappraisal, and COVID-19 Stress Scale were mean centered prior to analysis (n = 1,207).
There were no statistically significant differences between women and men concerning mean scores of COVID-19 stress, general mental distress, or age (Table 4). Moreover, women and men did not differ significantly regarding rates of general mental distress for the cut-offs >5 (w: 9.3%, m: 8.3%, p = 0.600), >3 (w: 30.4%, m: 24.8%, p = 0.057), and >2 (46.6%, m, 40.5% p = 0.058). Consistent with our hypotheses, men reported using suppression to a higher degree than women, with a small to medium observed effect (Hedges’ g = 0.4). Women, on the other hand, used significantly more reappraisal than men, with a rather small observed effect (Hedges’ g = −0.15).
Separate moderation analyses were performed for women and men. Both regression models were significant: For women at F(6, 877) = 106.82, p < 0.001, and 42% of the variance explanation in general mental distress; for men at F(6, 316) = 142.54, p < 0.001, and 45% of the variance explanation in general mental distress. The models revealed significant gender differences. In women, the directions of regression coefficients remained equal to the ones of the regression model for the total sample. However, the effect sizes were higher for reappraisal and its interaction with COVID-19 stress and slightly lower for suppression. Importantly, the interaction of suppression and COVID-19 stress was not significant (Table 4). Independent of each other, COVID-19 stress and suppression were associated with higher, and reappraisal with lower mental distress. With increasing COVID-19 stress, mental distress levels were not significantly different for women who used more suppression. However, they were significantly higher for those who used less cognitive reappraisal (Table 5 and Figure 3).

Table 5. Differential moderation effects of emotion regulation in women and men: cognitive reappraisal and suppression as moderators of the relationship between COVID-19 stress and general mental distress.
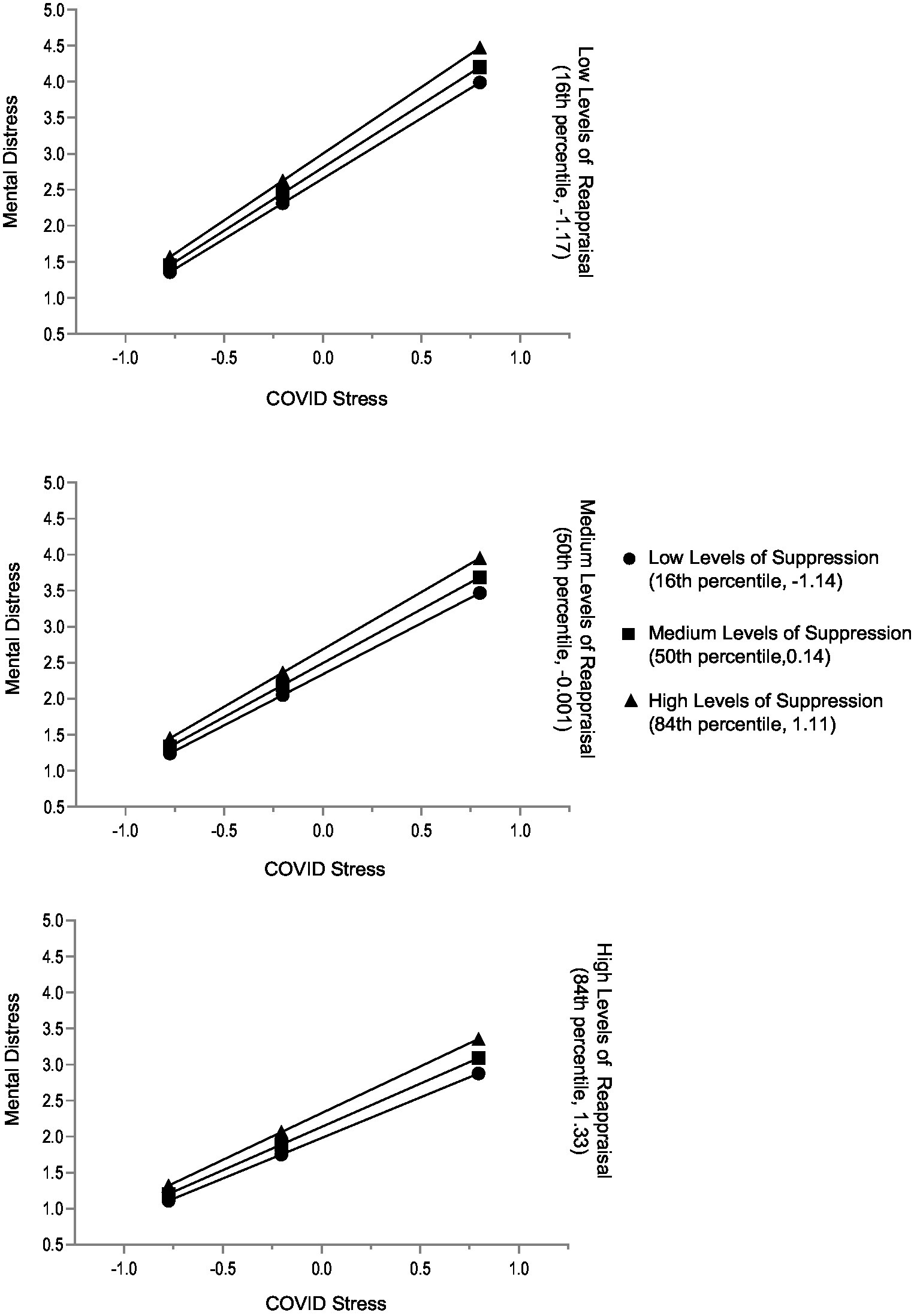
Figure 3. Women: conditional effects of COVID-19 stress on general mental distress for low, medium, and high levels of reappraisal and low, medium, and high levels of suppression. The variables ERQ Suppression, ERQ Reappraisal, and COVID-19 Stress Scale were mean centered prior to analysis (n = 884).
In men, both the main regression effects of reappraisal and its interaction effect with COVID-19 stress were not significant. Compared with the model of the total sample, the main effect of suppression and its interaction effect with COVID-19 stress were larger (Table 5). Independent of each other, COVID-19 stress and suppression were associated with higher mental distress. With increasing COVID-19 stress, mental distress levels were significantly higher for men who used more suppression (Table 5 and Figure 4). The results of the gender-specific moderation analyses are also supported by the zero-order correlational patterns of the subsamples of women and men (Supplementary Table S1).
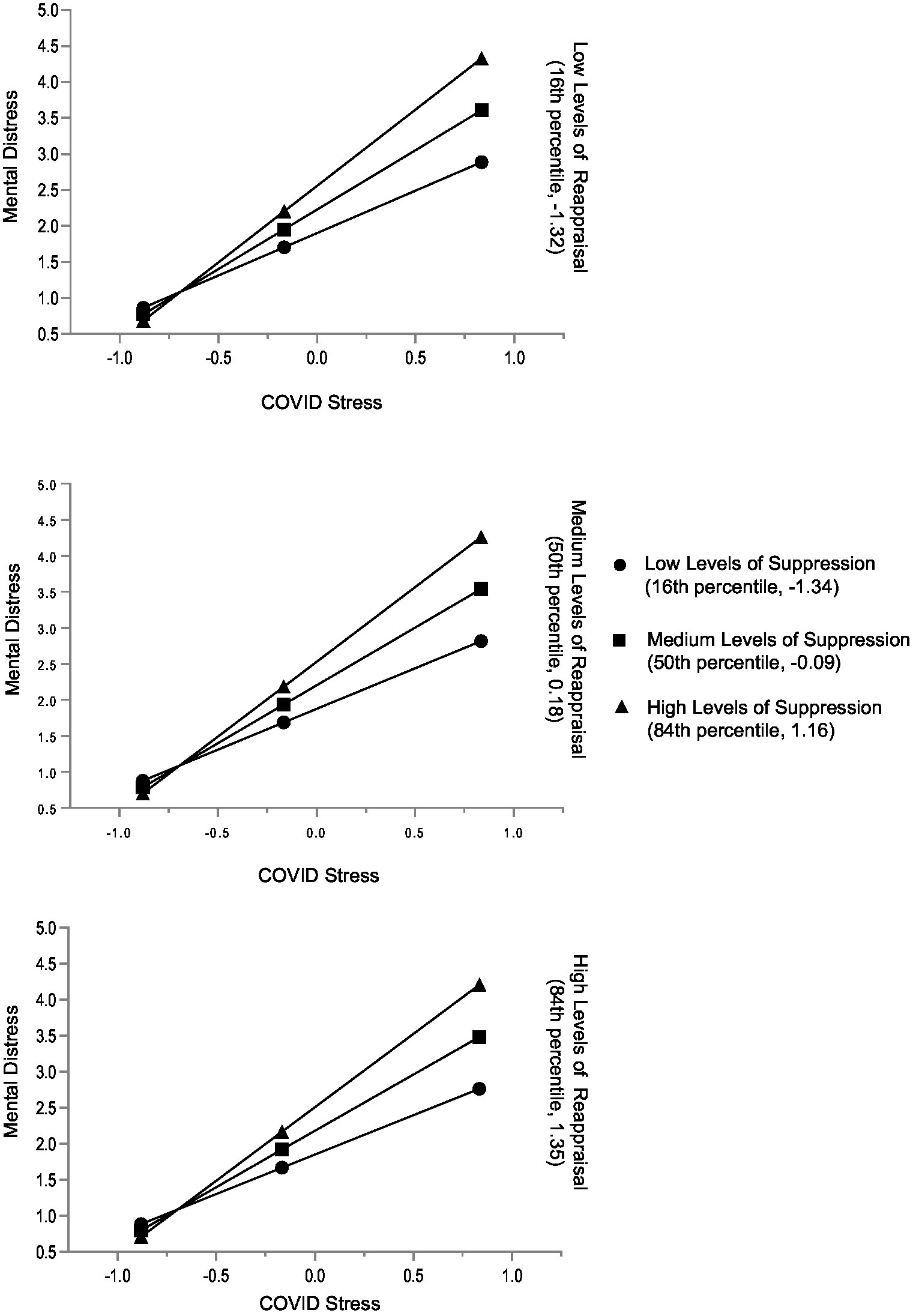
Figure 4. Men: conditional effects of COVID-19 stress on general mental distress for low, medium, and high levels of reappraisal and low, medium, and high levels of suppression. The variables ERQ Suppression, ERQ Reappraisal, and COVID-19 Stress Scale were mean centered prior to analysis (n = 323).
This study investigated whether cognitive reappraisal and expressive suppression moderated the relationship between COVID-19 stress and general mental distress during the early months of the COVID-19 pandemic in Norway. We found that cognitive reappraisal and suppression were differently related to COVID-19 stress and had opposite associations with general distress. Moreover, both variables served as moderators of the relationship between COVID-19 stress and general mental distress. While suppression worsened the relationship between COVID-19 stress and general mental distress, cognitive reappraisal buffered the relationship. When COVID-19 stress was low, this was also the case for general mental distress, and the mode of emotion regulation did not matter. This changed with increasing severity of COVID-19 stress. Here, lower cognitive reappraisal and higher emotion suppression were associated with elevated levels of general mental distress. Our findings revealed two significant gender differences. (1) Men had higher scores of expressive suppression, and women had higher scores of cognitive reappraisal. (2) Gender-specific moderation analyses suggest differential ways of emotion regulation. In women, cognitive reappraisal showed a significant negative relation to mental distress, and a substantial buffering effect of the relation between COVID-19 stress and mental distress. While suppression was positively related to higher distress, it did not buffer the relation between COVID-19 stress and mental distress. In men, cognitive reappraisal was not significantly related to mental distress, and it did not show a buffering effect. However, suppression was significantly associated with higher mental distress, and as a moderator, it substantially exacerbated the association of COVID-19 stress and mental distress. All in all, our data suggest that constructive emotion regulation became particularly relevant in situations of high COVID-19 stress.
Overall, our results are consistent with pre-pandemic research on emotion regulation showing that reappraisal buffered and suppression exacerbated associations between stress and symptoms of mental distress like anxiety and depression (e.g., Troy et al., 2010; Vanderhasselt et al., 2014; Boyes et al., 2016). The findings of the study at hand are also in line with recent COVID-19 studies that replicated the stress-distress buffering effect of cognitive reappraisal and the exacerbating effect of expressive suppression (Prikhidko et al., 2020; Xu et al., 2020; Yang et al., 2020; Gröndal et al., 2021; Kuhlman et al., 2021; Raio et al., 2021; Ye et al., 2021; Zhang et al., 2021; Chen et al., 2022; Vertsberger et al., 2022).
Our results concerning gender-specific differentiations confirm extensive previous research that suggested gender differences in emotion regulation (Tamres et al., 2002; Nolen-Hoeksema, 2012; Goubet and Chrysikou, 2019; Rogier et al., 2019). The higher use of reappraisal by women and of suppression by men is in accordance with several previous studies before and during the COVID-19 pandemic (Tamres et al., 2002; Flynn et al., 2010; Nolen-Hoeksema and Aldao, 2011; Megıas-Robles et al., 2019; Rogier et al., 2019; Canlı and Karaşar, 2020; Santi et al., 2021; Li et al., 2022).
We are unaware of previous investigations comparing women and men regarding stress-distress buffering and exacerbating moderator effects of cognitive reappraisal and expressive suppression, respectively. However, our data fit into the puzzle of different gender-specific results of moderation analyses of emotion regulation before the COVID-19 pandemic (Flynn et al., 2010; Nolen-Hoeksema, 2012; Megıas-Robles et al., 2019; Rogier et al., 2019; Zhang et al., 2020; Jiang et al., 2022; Lutz et al., 2022), and also during the pandemic (Muñoz-Navarro et al., 2021; Santi et al., 2021; Panno et al., 2022; Rodas et al., 2022). At this point, we suggest that further studies are necessary with the aim of exploring potential superordinate factors and processes to explain common patterns and pathways underlying the diverse findings on specific moderation effects.
As previously stated, people’s emotion regulation abilities seem to be influenced by contextual factors (Troy et al., 2010; Gross, 2015; Tamir, 2016; Troy et al., 2017). Research shows that in contexts of uncontrollable stressors, cognitive reappraisal becomes particularly beneficial for people’s mental health. However, contextual factors are defined as all intervening factors that affect a complex phenomenon (c.f. Ploeg et al., 2019) (e.g., transactions between individuals and the environment) (Nolen-Hoeksema, 2012). Examples of (external) contextual factors in this study are the culture, welfare, state of health, living conditions, severity of the COVID-19 restrictions, COVID-19 mortality rates, leadership (authorities) and political trust. The Norwegian lockdown was relatively short in duration (From March 11th 2020, with a gradual relaxation in April 2020). At the time of performing this study, the authorities in Norway were gradually dispensing with some of COVID-19 restrictions (Ursin et al., 2020), although social distancing, social isolation, working from home and travel restrictions were still applicable (Knudsen et al., 2021). Health and welfare are contextual factors that may have influenced our findings (Sachs et al., 2022). Norway is ranked among the top 10 countries of the world in GNP per capita, with a high level of welfare and strong and resilient national health systems, including public health (OECD, 2020; Britannica, 2022), (e.g., Sachs et al., 2022). The COVID-19 mortality rate in Norway was low (0.45%) compared to its neighboring countries (1.6–2%) and further afield, such as Italy and Spain (7–10%) (Sciencenorway, 2022). Another contextual factor that may have influenced our findings was that the public had a high level of trust in the Norwegian authorities and viewed them as being transparent and honest (Offerdal et al., 2021; Ihlen et al., 2022).Moreover, lifespan (individual factors) also appears to influence people’s emotion regulation behaviour (Carstensen et al., 2011; Kunzmann and Wrosch, 2018). Lifespan changes are associated with improved emotional stability (e.g., using more adaptive emotion regulation strategies) and well-being (Martins et al., 2016; Livingstone and Isaacowitz, 2018). A comparative study of COVID-19 stress and general mental distress between Norway and Germany/Austria (Krampe et al., 2021) (same data set) shows that Norwegian citizens had better mental health, indicated by less COVID-19 stress and general mental distress. Other studies comparing mental health/well-being before and during the onset of the pandemic in Norway found only a slight increase in mental health issues, particularly in vulnerable groups (Hoffart et al., 2020; Ebrahimi et al., 2021). However, constructive use of cognitive reappraisal is not always easy (Troy et al., 2018) and requires sufficient mental resources, such as vitality and mental well-being (Troy et al., 2018; Haver et al., 2021; Wu et al., 2021). Since cognitive reappraisal is closely linked to lifespan (average age: 52 years) and mental health/well-being, we believe that contextual and individual factors may have influenced our findings.
In terms of suppression, numerous COVID-19 studies indicate that lack of social support, loss of community and friendship worsened psychological distress (e.g., Banerjee and Rai, 2020; Jain et al., 2020; Smith et al., 2020; Philpot et al., 2021; von Mohr et al., 2021). It is well-researched that social connectedness e.g., social networking, community, engagement and friendly touch, acts as a buffer against various forms of distress (for review, see Gariépy et al., 2016). Having positive relationships is associated with mental health, particularly in times of crisis and involves the opportunity to express both negative and positive emotions through verbal and non-verbal communication (Phutela, 2015). It may thus be argued that worries, together with social distancing and social isolation (e.g., felt left to themselves), may have diminished the likelihood of using cognitive reappraisal or other adaptive emotion regulation strategies. Suppressors often experience lack of communication skills and poor relationships and they do not normally share their emotional experiences with others (Gross, 2015). In the long term this may lead to rumination thinking or at worst catastrophic thinking (Aldao and Nolen-Hoeksema, 2010), undermining psychological health (Aldao et al., 2010). That said, we do not yet know whether suppression was frequently or chronically used by the study subjects before the pandemic. Thus, this interpretation has to be handled with caution. Finally, we found a small to medium negative association between age and suppression, showing that younger people are more prone to using suppression. Most research shows that older adults are more consistent in their emotion regulation pattern across situations and are more likely to regulate their emotions by engaging in cognitive reappraisal (John and Gross, 2004; Webb et al., 2012; Sims et al., 2015). These differences in emotion regulation may be linked to the fact that older adults have longer life experience: they are less physiologically reactive, they experience higher well-being and they have learned which strategies are most effective to achieve their personal goals (Carstensen et al., 2011; Eldesouky and English, 2018).
Previous research shows gender differences in emotion regulation, particularly in terms of a flexible use of emotion regulation (Nolen-Hoeksema and Aldao, 2011; Goubet and Chrysikou, 2019). Flexible use of emotion regulation (e.g., contextual emotion regulation) refers to matching emotion regulation strategies to environmental circumstances (Aldao et al., 2015; Ullah et al., 2018). Our findings revealed that cognitive reappraisal was negatively related to general mental distress in women but not in men. The moderating role of cognitive reappraisal was significant for women but not for men. This may be linked to previous research arguing that women are more interpersonally oriented – they are more likely than men to seek social support in stressful times and are more prone to experiencing and expressing emotions. Women also have a larger repertoire of different emotion regulation strategies and are more skilled in the emotional domain than men (Brackett et al., 2006; Nolen-Hoeksema, 2012; Chaplin and Aldao, 2013). Several investigations have revealed that women are better at cognitive reappraisal (Tamres et al., 2002; Nolen-Hoeksema and Aldao, 2011; Megıas-Robles et al., 2019; Rogier et al., 2019; Li et al., 2022). These studies, along with our data, may indicate that men engage less in cognitive reappraisal but it is also possible that men use cognitive reappraisal unconsciously and thus do not report it (Nolen-Hoeksema, 2012).
In terms of suppression, our findings revealed that suppression was positively related to general mental distress in both women and men. When examining the moderation role, suppression was significant for men but not for women. These gender differences can be linked to the flexible use of emotion regulation, which involves a sensitivity to the situational demands (context), ability to use different emotion regulation strategies (large repertoire) and the ability to switch emotion regulation strategy if needed (Aldao et al., 2015; Eldesouky and English, 2018; Goubet and Chrysikou, 2019). Notably, flexible use of emotion regulation is found to be adaptive when it results in an enhanced likelihood of achieving personal and meaningful goals (Aldao et al., 2015; Rogier et al., 2019). For example, by engaging in risk-reducing behaviour or responding to environmental demands (e.g., following the government restrictions) the women in this study may have used suppression as a problem-focused strategy, enabling the threat to be endured and/or minimized. Thus, they were able to replace an uncomfortable emotion (anger, fear) with a more acceptable one or protect their relatives from discomfort or pain (e.g., alleviate their relatives’ fear). Suppression may therefore have had a functional and adaptive role during the pandemic, serving to mobilize energy for these women and help them pursue their goals (Tamir, 2016; Rogier et al., 2019). This use of suppression may have enabled women to adapt to the pandemic more effectively (e.g., Troy et al., 2013). Concerning men and their use of suppression, our findings are in line with previous meta-analyses, reviews and recent studies showing that men are more likely to engage in suppressing than women (Aldao et al., 2010; Flynn et al., 2010; Webb et al., 2012; Megıas-Robles et al., 2019; Rogier et al., 2019). These findings were also confirmed during the pandemic (e.g., Italy, Turkey; China) (Canlı and Karaşar, 2020; Santi et al., 2021; Li et al., 2022). A potential explanation is complex but may be linked to women reporting more symptoms of anxiety and depression, for example, through emotional expression, venting of emotions and social support, which in turn decreases suppression. Men on the other hand are more likely to hide, remove, reduce or deflect their emotions and depression symptoms. Men also have a greater tendency to use alcohol to cope (Nolen-Hoeksema, 2012; Cavanagh et al., 2016). However, our findings must be interpreted with caution since gender differences in emotion regulation are relatively complex. The gender difference in emotion regulation can be linked to several factors, such as social cultural norms (e.g., masculinity, femininity), values, personality, stereotypes, emotion regulation abilities (flexibility), and biological and psychological explanations (Matsumoto et al., 2008; Chaplin and Aldao, 2013; Lopez-Zafra and Gartzia, 2014; Costa et al., 2017; Rogier et al., 2019).
There are several limitations to the present study. Firstly, the study was conducted in Norway with a relatively high level of health and subjective well-being. Surveys conducted to measure life satisfaction in terms of ‘the happiest country’ have ranked Norway in the top 10 since 2012 (OECD, 2020). Cultural beliefs (e.g., collectivistic vs. individual cultures) and cultural differences, such as norms, values, stereotypes, are all important moderators and mediators in the relationship between emotion regulation and psychological health (Hu et al., 2014; Troy et al., 2018). Moreover, contextual factors, such as welfare, trust in government, infection rates and morality rates during the outbreak of the pandemic are also important aspects in any choice of emotion regulation. Investigating emotion regulation in different countries and contexts is thus required. Secondly, although the study covered a wide age range, the sample was not representative of the general population. Gender differences, as well as education level and life span may have influenced choice of emotion regulation. The sample may thus have been biased, with an overrepresentation of women, relatively high average age and highly educated individuals. Thirdly, this study has surveyed cognitive reappraisal and suppression, two of many identified strategies that individuals use to regulate their emotions (Parkinson and Totterdell, 1999). In order to further increase our understanding of which emotion regulation strategies constitute effective emotion regulation during crisis, a wider range of strategies should be included (e.g., maladaptive emotion regulation: rumination, catastrophizing). Fourthly, to strengthen the validity and to extend our knowledge during (global) crisis, longitudinal studies are required to see how individuals’ emotion regulation strategies fluctuate over time and the extent of their impact on psychological health, including short-and long-time effects of emotion regulation. Finally, to expand our conceptual understanding of emotion regulation during crises and to generate relevant hypotheses future research should include more qualitative studies. Despite these limitations, the convenience sampling of this material is coherent and consistent. The present study is well suited as a study aiming to explore new knowledge about COVID-19 stress, emotion regulation and general mental distress during a global health crisis.
This study examines emotion regulation in times of crises. The study also provides a more nuanced understanding of the role of cognitive reappraisal and suppression in a Scandinavian context. Even though COVID-19 now appears to be under control in most countries, it is important to note that new variants of the virus and new pandemics, alongside energy crises, economic crises and natural disasters may arise in the future. Given that cognitive reappraisal and suppression have different influences on the relationships between COVID-19 stress and general mental distress, health authorities should implement emotion regulation programs to promote a healthy and flexible use of emotion regulation. In practical terms, our findings suggest preventive measure responses through health promoting programs for developing/building psychological resilience in adolescents throughout their lives. Vulnerable groups, such as the youngest, would particularly benefit from emotion regulation training in times of crisis (e.g., web-based mindfulness programs). Health authorities should therefore be encouraged to develop health promoting programs (e.g., online self-guided), followed by preventive measures and interventions in school. Moreover, the findings in this study emphasize the importance of considering gender differences in future emotion regulation research. Consequently, it is vital to acknowledge that differences may exist between genders in terms of emotion regulation. This requires gender awareness, e.g., tailored programs for men and women.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by Personvernombudet Innlandet Hospital Trust, Norway, No 20/02104–1. All participants expressed their informed consent by explicitly agreeing to continue with the questionnaire after being informed about the study’s aims, employed data protection, participants’ rights, and contact points for questions or concerns. All methods were carried out in accordance with relevant guidelines and regulations. Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
AH wrote the first draft of the manuscript and, together with HK, TS, and LD performed the statistical analyses. LD and GS conceptualized, developed, and concluded the survey. AH contributed to the conceptualization and development of the survey. LD, TS, and HK performed data curation and project administration of the data set. AH, HK, and TS finalized the manuscript. All authors discussed the results, commented on the manuscript, contributed to critical revision of the manuscript, and read and approved the final manuscript.
This study was funded by Innlandet Hospital Trust. Research number/Grant: 677300.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1121986/full#supplementary-material
Abdelrahman, M. (2022). Personality traits, risk perception, and protective behaviors of Arab residents of Qatar during the COVID-19 pandemic. Int. J. Mental Health Addict. 20, 237–248. doi: 10.1007/s11469-020-00352-7
Aldao, A., and Nolen-Hoeksema, S. (2010). Specificity of cognitive emotion regulation strategies: a transdiagnostic examination. Behav. Res. Ther. 48, 974–983. doi: 10.1016/j.brat.2010.06.002
Aldao, A., and Nolen-Hoeksema, S. (2012). The influence of context on the implementation of adaptive emotion regulation strategies. Behav. Res. Ther. 50, 493–501. doi: 10.1016/j.brat.2012.04.004
Aldao, A., Nolen-Hoeksema, S., and Schweizer, S. (2010). Emotion-regulation strategies across psychopathology: a meta-analytic review. Clin. Psychol. Rev. 30, 217–237. doi: 10.1016/j.cpr.2009.11.004
Aldao, A., Sheppes, G., and Gross, J. J. (2015). Emotion regulation flexibility. Cognit. Ther. Res. 39, 263–278. doi: 10.1007/s10608-014-9662-4
Andreas, B., and Brunborg, G. S. (2021). Self-reported mental and physical health among Norwegian adolescents before and during the COVID-19 pandemic. JAMA Netw. Open 4:e2121934. doi: 10.1001/jamanetworkopen.2021.21934
Andreassen, T., Hansen, B. T., Engesæter, B., Hashim, D., Støer, N. C., Tropé, A., et al. (2019). Psychological effect of cervical cancer screening when changing primary screening method from cytology to high-risk human papilloma virus testing. Int. J. Cancer 145, 29–39. doi: 10.1002/ijc.32067
Bacon, A. M., and Corr, P. J. (2020). Coronavirus (COVID-19) in the United Kingdom: a personality-based perspective on concerns and intention to self-isolate. Br. J. Health Psychol. 25, 839–848. doi: 10.1111/bjhp.12423
Banerjee, D., and Rai, M. (2020). Social isolation in COVID-19: the impact of loneliness. Int. J. Social Psychiatry 66, 525–527. doi: 10.1177/0020764020922269
Bargh, J. A., and Williams, L. E. (2007). “The nonconscious regulation of emotion” in Handbook of emotion regulation. ed. J. J. Gross (New York, NY: The Guildford Press), 429–445.
Bemanian, M., Mæland, S., Blomhoff, R., Rabben, Å. K., Arnesen, E. K., Skogen, J. C., et al. (2021). Emotional eating in relation to worries and psychological distress amid the COVID-19 pandemic: a population-based survey on adults in Norway. Int. J. Environ. Res. Public Health 18:130. doi: 10.3390/ijerph18010130
Blix, I., Birkeland, M. S., and Thoresen, S. (2021). Worry and mental health in the COVID-19 pandemic: vulnerability factors in the general Norwegian population. BMC Public Health 21:928. doi: 10.1186/s12889-021-10927-1
Boyes, M. E., Hasking, P. A., and Martin, G. (2016). Adverse life experience and psychological distress in adolescence: moderating and mediating effects of emotion regulation and rumination. Stress. Health 32, 402–410. doi: 10.1002/smi.2635
Brackett, M. A., Rivers, S. E., Shiffman, S., Lerner, N., and Salovey, P. (2006). Relating emotional abilities to social functioning: a comparison of self-report and performance measures of emotional intelligence. J. Pers. Soc. Psychol. 91, 780–795. doi: 10.1037/0022-3514.91.4.780
Britannica . (2022). Government and society_Health and welfare. https://www.britannica.com/place/Norway/Health-and-welfare (Accessed August 5, 2022)
Cameron, L. D., and Overall, N. C., (2018) Suppression and expression as distinct emotion-regulation processes in daily interactions: Longitudinal and meta-analyses. Emotion 18: 465–480. doi: 10.1037/emo0000334
Canlı, D., and Karaşar, B. (2020). Health anxiety and emotion regulation during the period of COVID-19 outbreak in Turkey. Psychiatr. Danub. 32, 513–520. doi: 10.24869/psyd.2020.513
Cardi, V., Albano, G., Gentili, C., and Sudulich, L. (2021). The impact of emotion regulation and mental health difficulties on health behaviours during COVID19. J. Psychiat. Res. 143, 409–415. doi: 10.1016/j.jpsychires.2021.10.001
Carstensen, L. L., Scheibe, S., Ersner-Hershfield, H., Brooks, K. P., Turan, B., Ram, N., et al. (2011). Emotional experience improves with age: evidence based on over 10 years of experience sampling. Psychol. Aging 26, 21–33. doi: 10.1037/a0021285
Cavanagh, A., Caputi, P., Wilson, C. J., and Kavanagh, D. (2016). Gender differences in self-reported depression and co-occurring anxiety and stress in a vulnerable community population. Austral. Psychol. 51, 411–421. doi: 10.1111/ap.12184
Cénat, J. M., Blais-Rochette, C., Kokou-Kpolou, C. K., Noorishad, P.-G., Mukunzi, J. N., McIntee, S.-E., et al. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295:113599. doi: 10.1016/j.psychres.2020.113599
Chaplin, T. M., and Aldao, A. (2013). Gender differences in emotion expression in children: a meta-analytic review. Psychol. Bull. 139, 735–765. doi: 10.1037/a0030737
Chen, S., Zhou, W., Luo, T., and Huang, L. (2022). Relationships between mental health, emotion regulation, and meaning in life of frontline nurses during the COVID-19 outbreak. Front. Psych. 13:798406. doi: 10.3389/fpsyt.2022.798406
Chervonsky, E., and Hunt, C. (2017). Suppression and expression of emotion in social and interpersonal outcomes: a meta-analysis. Emotion 17, 669–683. doi: 10.1037/emo0000270
Conway, A. M., Tugade, M. M., Catalino, L. I., and Fredrickson, B. L. (2013). “The broaden-and build theory of positive emotions: form, function, and mechanisms” in The Oxford handbook of happiness. eds. S. A. David, I. Boniwell, and A. C. Ayers (Oxford: Oxford University Press), 17–34.
Costa, C., Bakas, F. E., Breda, Z., and Durão, M. (2017). Emotional female managers: how gendered roles influence tourism management discourse. J. Hospital. Tourism Manage. 33, 149–156. doi: 10.1016/j.jhtm.2017.09.011
Dyrendal, A., and Hestad, K. (2021). Trust in crisis: conspiracy mentality, lack of trust and religiosity predicted conspiracy beliefs about COVID-19 in a Norwegian sample. Approaching Religion 11, 98–114. doi: 10.30664/ar.107485
Ebrahimi, O. V., Hoffart, A., and Johnson, S. U. (2021). Physical distancing and mental health during the COVID-19 pandemic: factors associated with psychological symptoms and adherence to pandemic mitigation strategies. Clin. Psychol. Sci. 9, 489–506. doi: 10.1177/2167702621994545
Eldesouky, L., and English, T. (2018). Another year older, another year wiser? Emotion regulation strategy selection and flexibility across adulthood. Psychol. Aging 33, 572–585. doi: 10.1037/pag0000251
English, T., and John, O. P. (2013). Understanding the social effects of emotion regulation: the mediating role of authenticity for individual differences in suppression. Emotion 13, 314–329. doi: 10.1037/a0029847
Ernstsen, L., and Havnen, A. (2021). Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. 77, 309–312. doi: 10.1016/j.sleep.2020.08.030
Flynn, J. J., Hollenstein, T., and Mackey, A. (2010). The effect of suppressing and not accepting emotions on depressive symptoms: is suppression different for men and women? Personal. Individ. Differ. 49, 582–586. doi: 10.1016/j.paid.2010.05.022
Ford, B. Q., Karnilowicz, H. R., and Mauss, I. B. (2017). Understanding reappraisal as a multicomponent process: the psychological health benefits of attempting to use reappraisal depend on reappraisal success. Emotion 17, 905–911. doi: 10.1037/emo0000310
Gariépy, G., Honkaniemi, H., and Quesnel-Vallée, A. (2016). Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry 209, 284–293. doi: 10.1192/bjp.bp.115.169094
Garland, E. L., Gaylord, S. A., and Fredrickson, B. L. (2011). Positive reappraisal mediates the stress-reductive effects of mindfulness: an upward spiral process. Mindfulness 2, 59–67. doi: 10.1007/s12671-011-0043-8
Gómez-Ortiz, O., Romera, E. M., Ortega-Ruiz, R., Cabello, R., and Fernández-Berrocal, P. (2016). Analysis of emotion regulation in Spanish adolescents: validation of the emotion regulation questionnaire. Front. Psychol. 6:1959. doi: 10.3389/fpsyg.2015.01959
Goubet, K. E., and Chrysikou, E. G. (2019). Emotion regulation flexibility: gender differences in context sensitivity and repertoire. Front. Psychol. 10:935. doi: 10.3389/fpsyg.2019.00935
Gröndal, M., Ask, K., Luke, T. J., and Winblad, S. (2021). Self-reported impact of the COVID-19 pandemic, affective responding, and subjective well-being: a Swedish survey. PLoS One 16:e0258778. doi: 10.1371/journal.pone.0258778
Gross, J. J. (1998a). Antecedent – and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J. Pers. Soc. Psychol. 74, 224–237. doi: 10.1037/0022-3514.74.1.224
Gross, J. J. (1998b). The emerging field of emotion regulation: an integrative review. Rev. General Psychol. 2, 271–299. doi: 10.1037/1089-2680.2.3.271
Gross, J. J. (2015). Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26. doi: 10.1080/1047840X.2014.940781
Gross, J. J., and Barrett, L. F. (2011). Emotion generation and emotion regulation: one or two depends on your point of view. Emot. Rev. 3, 8–16. doi: 10.1177/1754073910380974
Gross, J. J., and John, O. P. (2003). Individual differences in two emotion regulation processes: implications for affect, relationships, and well-being. J. Pers. Soc. Psychol. 85, 348–362. doi: 10.1037/0022-3514.85.2.348
Gross, J. J., and Thompson, R. A. (2006). “Emotion regulation: conceptual foundations” in Handbook of emotion regulation. ed. J. J. Gross (New York, NY: The Guildford Press), 3–26.
Gullo, S., Omar Carlo, G., Gelo, G. B., Coco, G. L., Lagetto, G., Esposito, G., et al. (2022). The role of emotion regulation and intolerance to uncertainty on the relationship between fear of COVID-19 and distress. Curr. Psychol. 25, 1–12. doi: 10.1007/s12144-022-03071-5
Hansen, T., Nilsen, T. S., Baeksan, Y., Knapstad, M., Skogen, J. C., Vedaa, Ø., et al. (2021). Locked and lonely? A longitudinal assessment of loneliness before and during the COVID-19 pandemic in Norway. Scand. J. Public Health 49, 766–773. doi: 10.1177/1403494821993711
Haver, A., Akerjordet, K., Robinson, L., and Caputi, P. (2021). Investigating emotion regulation strategies to facilitate the well-being of managers. Scand. J. Work Organ. Psychol. 6:10. doi: 10.16993/sjwop.147
Hayes,, and Andrew, F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Methodology in the social sciences. 1 New York, NY: The Guilford Press.
Hayes, A. F., Montoya, A. K., and Rockwood, N. J. (2017). The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Austral. Market. J. 25, 76–81. doi: 10.1016/j.ausmj.2017.02.001
Hoffart, A., Johnson, S. U., and Ebrahimi, O. V. (2020). Loneliness and social distancing during the COVID-19 pandemic: risk factors and associations with psychopathology. Front. Psych. 11:589127. doi: 10.3389/fpsyt.2020.589127
Hosogoshi, H., Takebayashi, Y., Ito, M., Fujisato, H., Kato, N., Nakajima, S., et al. (2020). Expressive suppression of emotion is a moderator of anxiety in a unified protocol for transdiagnostic treatment of anxiety and depressive disorders: a secondary analysis. J. Affect. Disord. 277, 1–4. doi: 10.1016/j.jad.2020.07.132
Hu, T., Zhang, D., Wang, J., Mistry, R., Ran, G., and Wang, X. (2014). Relation between emotion regulation and mental health: a meta-analysis review. Psychol. Rep. 114, 341–362. doi: 10.2466/03.20.PR0.114k22w4
Hvide, H. K., and Johnsen, J. (2022). COVID-19 and mental health: a longitudinal population study from Norway. Eur. J. Epidemiol. 37, 167–172. doi: 10.1007/s10654-021-00836-3
Ihlen, Ø., Just, S. N., Kjeldsen, J. E., Mølster, R., Offerdal, T. S., Rasmussen, J., et al. (2022). Transparency beyond information disclosure: strategies of the Scandinavian public health authorities during the COVID-19 pandemic. J. Risk Res 25, 1176–1189. doi: 10.1080/13669877.2022.2077416
Jain, A., Bodicherla, K. P., Raza, Q., and Sahu, K. K. (2020). Impact on mental health by "living in isolation and quarantine" during COVID-19 pandemic. J. Family Med. Prim. Care 9, 5415–5418. doi: 10.4103/jfmpc.jfmpc_1572_20
Jiang, X., Moreno, J., and Ng, Z. (2022). Examining the interplay of emotion regulation strategies, social stress, and gender in predicting life satisfaction of emerging adults. Pers. Individ. Differ. 185:111255. doi: 10.1016/j.paid.2021.111255
John, O. P., and Gross, J. J. (2004). Healthy and unhealthy emotion regulation: personality processes, individual differences, and life span development. J. Pers. 72, 1301–1334. doi: 10.1111/j.1467-6494.2004.00298.x
Johnson, J., O'Connor, D. B., Jones, C., Jackson, C., Hughes, G. J., and Ferguson, E. (2016). Reappraisal buffers the association between stress and negative mood measured over 14 days: implications for understanding psychological resilience. Eur. J. Personal. 30, 608–617. doi: 10.1002/per.2080
Kashdan, T. B., Barrios, V., Forsyth, J. P., and Steger, M. F. (2006). Experiential avoidance as a generalized psychological vulnerability: comparisons with coping and emotion regulation strategies. Behav. Res. Ther. 44, 1301–1320. doi: 10.1016/j.brat.2005.10.003
Kerper, L. F., Claudia, D., Tillinger, J., Wegscheider, K., Salz, A.-L., Weiss-Gerlach, E., et al. (2014). Screening for depression, anxiety, and general psychological distress in pre-operative surgical patients: a psychometric analysis of the patient health questionnaire 4 (PHQ-4). Clin. Health Promot. 4, 5–14. doi: 10.29102/clinhp.14002
Knudsen, A. K., Skrindo, K. S.-L., Gustavson, K., Hotopf, M., Kessler, R. C., Krokstad, S., et al. (2021). Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: a population-based repeated cross-sectional analysis. Lancet Regional Health Europe 4:100071. doi: 10.1016/j.lanepe.2021.100071
Kraiss, J. T., ten Klooster, P. M., Moskowitz, J. T., and Bohlmeijer, E. T. (2020). The relationship between emotion regulation and well-being in patients with mental disorders: a meta-analysis. Compr. Psychiatry 102:152189. doi: 10.1016/j.comppsych.2020.152189
Krampe, H., Danbolt, L. J., Haver, A., Stålsett, G., and Schnell, T. (2021). COVID-19 stress and general mental distress: results of a Norwegian and a German-speaking cross-sectional survey. BMC Psychiatry 21:437. doi: 10.1186/s12888-021-03418-5
Kroenke, K., Spitzer, R. L., Williams, J. B. W., and Löwe, B. (2009). An ultra-brief screening scale for anxiety and depression: the PHQ–4. Psychosomatics 50, 613–621. doi: 10.1176/appi.psy.50.6.613
Kroenke, K., Spitzer, R. L., Williams, J. B. W., and Löwe, B. (2010). The patient health questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry 32, 345–359. doi: 10.1016/j.genhosppsych.2010.03.006
Kuhlman, K. R., Straka, K., Mousavi, Z., Tran, M.-L., and Rodgers, E. (2021). Predictors of adolescent resilience during the COVID-19 pandemic: cognitive reappraisal and humor. J. of Adolesc. Health 69, 729–736. doi: 10.1016/j.jadohealth.2021.07.006
Kunzmann, U., and Wrosch, C. (2018). Comment: the emotion–health link: perspectives from a lifespan theory of discrete emotions. Emot. Rev. 10, 59–61. doi: 10.1177/1754073917719332
Lassen, E. R., Hagen, K., Kvale, G., Eid, J., Le Hellard, S., and Solem, S. (2022). Personality traits and hardiness as risk- and protective factors for mental distress during the COVID-19 pandemic: a Norwegian two-wave study. BMC Psychiatry 22:610. doi: 10.1186/s12888-022-04237-y
Lazarus, R. S., and Alfert, E. (1964). Short-circuiting of threat by experimentally altering cognitive appraisal. J. Abnormal Soc. Psychol. 69, 195–205. doi: 10.1037/h0044635
Li, N., Fan, L., Wang, Y., Wang, J., and Huang, Y. (2022). Risk factors of psychological distress during the COVID-19 pandemic: the roles of coping style and emotional regulation. J. Affect. Disord. 299, 326–334. doi: 10.1016/j.jad.2021.12.026
Liang, Z., Mazzeschi, C., and Delvecchio, E. (2021). The impact of parental stress on Italian adolescents’ internalizing symptoms during the COVID-19 pandemic: a longitudinal study. Int. J. Environ. Res. Public Health 18:8074. doi: 10.3390/ijerph18158074
Liu, S., Lithopoulos, A., Zhang, C.-Q., Garcia-Barrera, M. A., and Rhodes, R. E. (2021). Personality and perceived stress during COVID-19 pandemic: testing the mediating role of perceived threat and efficacy. Pers. Individ. Differ. 168:110351. doi: 10.1016/j.paid.2020.110351
Livingstone, K. M., and Isaacowitz, D. M. (2018). The roles of age and attention in general emotion regulation, reappraisal, and expressive suppression. Psychol. Aging 33, 373–383. doi: 10.1037/pag0000240
Lopez-Leon, S., Wegman-Ostrosky, T., Perelman, C., Sepulveda, R., Rebolledo, P. A., Cuapio, A., et al. (2021). More than 50 long-term effects of COVID-19: a systematic review and meta-analysis. Sci. Rep. 11:16144. doi: 10.1038/s41598-021-95565-8.
Lopez-Zafra, E., and Gartzia, L. (2014). Perceptions of gender differences in self-report measures of emotional intelligence. Sex Roles 70, 479–495. doi: 10.1007/s11199-014-0368-6
Low, R. S. T., Overall, N. C., Chang, V. T., Henderson, A. M. E., and Sibley, C. G. (2021). Emotion regulation and psychological and physical health during a nationwide COVID-19 lockdown. Emotion 21, 1671–1690. doi: 10.1037/emo0001046
Lutz, N. M., Neufeld, S. A. S., Hook, R. W., Jones, P. B., Bullmore, E. T., Goodyer, I. M., et al. (2022). Why is non-suicidal self-injury more common in women? Mediation and moderation analyses of psychological distress, emotion dysregulation, and impulsivity. Archives Suicide Res 13, 1–17. doi: 10.1080/13811118.2022.2084004
Martins, B., Sheppes, G., Gross, J. J., and Mather, M. (2016). Age differences in emotion regulation choice: older adults use distraction less than younger adults in high-intensity positive contexts. J. Gerontol. Series B 73:gbw028. doi: 10.1093/geronb/gbw028
Matsumoto, D., Yoo, S. H., and Nakagawa, S. (2008). Culture, emotion regulation, and adjustment. J. Pers. Soc. Psychol. 94, 925–937. doi: 10.1037/0022-3514.94.6.925
Megıas-Robles, A., Gutierrez-Cobo, M. J., Gomez-Leal, R., Cabello, R., Gross, J. J., and Fernandez-Berrocal, P. (2019). Emotionally intelligent people reappraise rather than suppress their emotions. PLoS One 14:e0220688. doi: 10.1371/journal.pone.0220688
Muñoz-Navarro, R., Malonda, E., Llorca-Mestre, A., Cano-Vindel, A., and Fernández-Berrocal, P. (2021). Worry about COVID-19 contagion and general anxiety: moderation and mediation effects of cognitive emotion regulation. J. Psychiatr. Res. 137, 311–318. doi: 10.1016/j.jpsychires.2021.03.004
Nolen-Hoeksema, S. (2012). Emotion regulation and psychopathology: the role of gender. Ann. Rev. Clin. Psychol. 8, 161–187. doi: 10.1146/annurev-clinpsy-032511-143109
Nolen-Hoeksema, S., and Aldao, A. (2011). Gender and age differences in emotion regulation strategies and their relationship to depressive symptoms. Personal. Individ. Differ. 51, 704–708. doi: 10.1016/j.paid.2011.06.012
OECD , (2020). OECD economic surveys norway . Better Life Index. Available at: https://www.oecdbetterlifeindex.org/countries/norway/ (Accessed October 20, 2022)
OECD (2021). Tackling the mental health impact of the COVID-19 crisis: an integrated, whole-of-society response. Available at: https://www.oecd.org/coronavirus/policy-responses/tackling-the-mental-health-impact-of-the-covid-19-crisis-an-integrated-whole-of-society-response-0ccafa0b/ (Accessed July 5, 2022)
Offerdal, T. S., Just, S. N., and Ihlen, O. (2021). Public ethos in the pandemic rhetorical situation: strategies for building trust in authorities’ risk communication. J. Int. Crisis Risk Commun. Res. 4, 247–270. doi: 10.30658/jicrcr.4.2.3
Panno, A., Theodorou, A., Massullo, C., Bratman, G. N., Imperatori, C., Carbone, G. A., et al. (2022). The psychological impact of the COVID-19 lockdown in Italy: the moderating role of gender and emotion regulation. Health Care Women Inter. 28, 1–18. doi: 10.1080/07399332.2022.2083622
Parkinson, Brian, and Totterdell, Peter. (1999). Classifying affect regulation strategies. Cognit. Emot. 13, 277–303. doi: 10.1080/026999399379285
Philpot, L. M., Ramar, P., Roellinger, D. L., Barry, B. A., Sharma, P., and Ebbert, J. O. (2021). Changes in social relationships during an initial “stay-at-home” phase of the COVID-19 pandemic: a longitudinal survey study in the U.S. Soc. Sci. Med. 274:113779. doi: 10.1016/j.socscimed.2021.113779
Ploeg, J., Wong, S. T., Hassani, K., Yous, M.-L., Fortin, M., Kendall, C., et al. (2019). Contextual factors influencing the implementation of innovations in community-based primary health care: the experience of 12 Canadian research teams. Prim. Health Care Res. Dev. 20:e107. doi: 10.1017/S1463423619000483
Preece, D. A., Becerra, R., Robinson, K., and Gross, J. J. (2020). The emotion regulation questionnaire: psychometric properties in general community samples. J. Pers. Assess. 102, 348–356. doi: 10.1080/00223891.2018.1564319
Prikhidko, A., Long, H., and Wheaton, M. G. (2020). The effect of concerns about COVID-19 on anxiety, stress, parental burnout, and emotion regulation: the role of susceptibility to digital emotion contagion. Front. Public Health 8:567250. doi: 10.3389/fpubh.2020.567250
Raio, C. M., Harp, N. R., Brown, C. C., and Neta, M. (2021). Reappraisal—but not suppression—tendencies determine negativity bias after laboratory and real-world stress exposure. Affect. Sci. 2, 455–467. doi: 10.1007/s42761-021-00059-5
Raymond, C., Marin, M.-F., Juster, R.-P., and Lupien, S. J. (2019). Should we suppress or reappraise our stress?: the moderating role of reappraisal on cortisol reactivity and recovery in healthy adults. Anxiety Stress Coping 32, 286–297. doi: 10.1080/10615806.2019.1596676
Robinson, E., Sutin, A. R., Daly, M., and Jones, A. (2022). A systematic review and meta-analysis of longitudinal cohort studies comparing mental health before versus during the COVID-19 pandemic in 2020. J. Affect. Disord. 296:567. doi: 10.1016/j.jad.2021.09.098
Rodas, J. A., Jara-Rizzo, M. F., Greene, C. M., Moreta-Herrera, R., and Oleas, D. (2022). Cognitive emotion regulation strategies and psychological distress during lockdown due to COVID-19. Int. J. Psychol. 57, 315–324. doi: 10.1002/ijop.12818
Rogier, G., Garofalo, C., and Velotti, P. (2019). Is emotional suppression always bad? A matter of flexibility and gender differences. Curr. Psychol. 38, 411–420. doi: 10.1007/s12144-017-9623-7
Sachs, J. D., Abdool, S. S., Karim, L. A., Allen, J., Brosbøl, K., Colombo, F., et al. (2022). The lancet commission on lessons for the future from the COVID-19 pandemic. Lancet 400, 1224–1280. doi: 10.1016/S0140-6736(22)01585-9
Sætren, S. S., Sütterlin, S., Lugo, R. G., Prince-Embury, S., and Makransky, G. (2019). A multilevel investigation of resiliency scales for children and adolescents: the relationships between self-perceived emotion regulation, vagally mediated heart rate variability, and personal factors associated with resilience. Front. Psychol. 10:438. doi: 10.3389/fpsyg.2019.00438
Santi, G., Quartiroli, A., Costa, S., di Fronso, S., Montesano, C., Di Gruttola, F., et al. (2021). The impact of the COVID-19 lockdown on coaches’ perception of stress and emotion regulation strategies. Front. Psychol. 11:601743. doi: 10.3389/fpsyg.2020.601743
Saunders, R., Buckman, J. E. J., Fonagy, P., and Fancourt, D. (2021). Understanding different trajectories of mental health across the general population during the COVID-19 pandemic. Psychol. Med. 52, 4049–4057. doi: 10.1017/S0033291721000957
Schnell, T., and Krampe, H. (2020). Meaning in life and self-control buffer stress in times of COVID-19: moderating and mediating effects with regard to mental distress. Front. Psych. 11. doi: 10.3389/fpsyt.2020.582352
Schnell, T., and Krampe, H. (2022a). Meaningfulness buffers and crisis of meaning mediates the longitudinal effect of COVID-19 stress on general mental distress. BMC Psychiatry [Preprint]. doi: 10.21203/rs.3.rs-1135588/v1
Schnell, T., and Krampe, H. (2022b). Meaningfulness protects from and crisis of meaning exacerbates general mental distress longitudinally. BMC Psychiatry 22:285. doi: 10.1186/s12888-022-03921-3
Schnell, T., Spitzenstätter, D., and Krampe, H. (2021). Compliance with COVID-19 public health guidelines: an attitude-behaviour gap bridged by personal concern and distance to conspiracy ideation. Psychol. Health 37, 1680–1701. doi: 10.1080/08870446.2021.1974861
Schöley, J., Aburto, J. M., Kashnitsky, I., Kniffka, M. S., Zhang, L., Jaadla, H., et al. (2022). Life expectancy changes since COVID-19. Nat. Hum. Behav. 6, 1649–1659. doi: 10.1038/s41562-022-01450-3
Sciencenorway . (2022). Very low mortality rate from coronavirus in Norway compared to other countries. Available at: https://sciencenorway.no/covid19-crisis-epidemic/very-low-mortality-rate-from-coronavirus-in-norway-compared-to-other-countries/1661751 (Accessed July 5, 2022)
Sims, T., Hogan, C. L., and Carstensen, L. L. (2015). Selectivity as an emotion regulation strategy: lessons from older adults. Curr. Opin. Psychol. 3, 80–84. doi: 10.1016/j.copsyc.2015.02.012
Smith, B. M., Twohy, A. J., and Smith, G. S. (2020). Psychological inflexibility and intolerance of uncertainty moderate the relationship between social isolation and mental health outcomes during COVID-19. J. Context. Behav. Sci. 18, 162–174. doi: 10.1016/j.jcbs.2020.09.005
Solem, S., Pedersen, H., Nesse, F., Janssen, A. G., Kennair, L. E. O., Hagen, R., et al. (2021). Validity of a Norwegian version of the desire thinking questionnaire (DTQ): associations with problem drinking, nicotine dependence and problematic social media use. Clin. Psychol. Psychother. 28, 615–622. doi: 10.1002/cpp.2524
Tamir, M. (2016). Why do people regulate their emotions? A taxonomy of motives in emotion regulation. Personal. Soc. Psychol. Rev. 20, 199–222. doi: 10.1177/1088868315586325
Tamres, L. K., Janicki, D., and Helgeson, V. S. (2002). Sex differences in coping behavior: a meta-analytic review and an examination of relative coping. Personal. Soc. Psychol. Rev. 6, 2–30. doi: 10.1207/S15327957PSPR0601_1
Too, L. S., and Butterworth, P. (2018). Psychosocial job stressors and mental health: the potential moderating role of emotion regulation. J. Occup. Environ. Med. 60, e518–e524. doi: 10.1097/JOM.0000000000001416
Troy, A. S., Ford, B. Q., McRae, K., Zarolia, P., and Mauss, I. B. (2017). Change the things you can: emotion regulation is more beneficial for people from lower than from higher socioeconomic status. Emotion 17, 141–154. doi: 10.1037/emo0000210./
Troy, A. S., Shallcross, A. J., Brunner, A., Friedman, R., and Jones, M. C. (2018). Cognitive reappraisal and acceptance: effects on emotion, physiology, and perceived cognitive costs. Emotion 18, 58–74. doi: 10.1037/emo0000371
Troy, A. S., Shallcross, A. J., and Mauss, I. B. (2013). A person-by-situation approach to emotion regulation:cognitive reappraisal can either help or hurt, depending on the context. Psychol Sci. 24, 2505–2514. doi: 10.1177/0956797613496434
Troy, A. S., Wilhelm, F. H., Shallcross, A. J., and Mauss, I. B. (2010). Seeing the silver lining: cognitive reappraisal ability moderates the relationship between stress and depressive symptoms. Emotion 10, 783–795. doi: 10.1037/a0020262
Ullah, N., Treur, J., and Koole, S. L. (2018). A computational model for flexibility in emotion regulation. Procedia Comput. Sci. 145, 572–580. doi: 10.1016/j.procs.2018.11.100
Ursin, G., Skjesol, I., and Tritter, J. (2020). The COVID-19 pandemic in Norway: the dominance of social implications in framing the policy response. Health Policy Technol. 9, 663–672. doi: 10.1016/j.hlpt.2020.08.004
Vanderhasselt, M.-A., Koster, E. H. W., Onraedt, T., Bruyneel, L., Goubert, L., and De Raedt, R. (2014). Adaptive cognitive emotion regulation moderates the relationship between dysfunctional attitudes and depressive symptoms during a stressful life period: a prospective study. J. Behav. Ther. Experiment. Psychiatry 45, 291–296. doi: 10.1016/j.jbtep.2014.01.003
Vertsberger, D., Roskam, I., Talmon, A., van Bakel, H., Hall, R., Mikolajczak, M., et al. (2022). Emotion regulation during the COVID-19 pandemic: risk and resilience factors for parental burnout (IIPB). Cognit. Emot. 36, 100–105. doi: 10.1080/02699931.2021.2005544
von Mohr, M., Kirsch, L. P., and Fotopoulou, A. (2021). Social touch deprivation during COVID-19: effects on psychological wellbeing and craving interpersonal touch. R. Soc. Open Sci. 8:210287. doi: 10.1098/rsos.210287
Webb, T. L., Miles, E., and Sheeran, P. (2012). Dealing with feeling: a meta-analysis of the effectiveness of strategies derived from the process model of emotion regulation. Psychol. Bull. 138, 775–808. doi: 10.1037/a0027600
WHO . (2020). WHO director-General's opening remarks at the media briefing on COVID-19. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (Accessed August 20, 2022)
WHO (2022a). COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide. Available at: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (Accessed March 2, 2022)
WHO (2022b). Mental Health and COVID-19: Early evidence of the pandemic’s impact. Available at: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (Accessed August 16, 2022)
Wu, S., Zhang, K., Parks-Stamm, E. J., Zhonghui, H., Ji, Y., and Cui, X. (2021). Increases in anxiety and depression during COVID-19: a large longitudinal study from China. Front. Psychol. 12:706601. doi: 10.3389/fpsyg.2021.706601
Xu, C., Yanjun, X., Song, X., Zhang, Q., Liu, X., Shao, Y., et al. (2020). Cognitive reappraisal and the association between perceived stress and anxiety symptoms in COVID-19 isolated people. Front. Psych. 11:858. doi: 10.3389/fpsyt.2020.00858
Yang, Y., Liu, K., Li, S., and Shu, M. (2020). Social media activities, emotion regulation strategies, and their interactions on people’s mental health in COVID-19 pandemic. Int. J. Environ. Res. Public Health 17:8931. doi: 10.3390/ijerph17238931
Ye, B., Dehua, W., Wang, P., Im, H., Liu, M., Wang, X., et al. (2021). COVID-19 stressors and poor sleep quality: the mediating role of rumination and the moderating role of emotion regulation strategies. Int. J. Behav. Med. 29, 416–425. doi: 10.1007/s12529-021-10026-w
Zhang, L., Jiamei, L., Li, B., Wang, X., and Shangguan, C. (2020). Gender differences in the mediating effects of emotion-regulation strategies: forgiveness and depression among adolescents. Pers. Individ. Differ. 163:110094. doi: 10.1016/j.paid.2020.110094
Zhang, Y.-t., Li, R.-t., Sun, X.-j., Peng, M., and Li, X. (2021). Social media exposure, psychological distress, emotion regulation, and depression during the COVID-19 outbreak in community samples in China. Front. Psych. 12:644899. doi: 10.3389/fpsyt.2021.644899
Keywords: COVID-19, anxiety, depression, emotion regulation, moderator analysis, public mental health, reappraisal, suppression
Citation: Haver A, Krampe H, Danbolt LJ, Stålsett G and Schnell T (2023) Emotion regulation moderates the association between COVID-19 stress and mental distress: findings on buffering, exacerbation, and gender differences in a cross-sectional study from Norway. Front. Psychol. 14:1121986. doi: 10.3389/fpsyg.2023.1121986
Received: 12 December 2022; Accepted: 15 May 2023;
Published: 22 June 2023.
Edited by:
Changiz Mohiyeddini, Oakland University William Beaumont School of Medicine, United StatesReviewed by:
Xihui Chen, Zhejiang University of Technology, ChinaCopyright © 2023 Haver, Krampe, Danbolt, Stålsett and Schnell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Annie Haver, YW5uaWUuaGF2ZXJAdWlzLm5v
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.