
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 17 April 2023
Sec. Psycho-Oncology
Volume 14 - 2023 | https://doi.org/10.3389/fpsyg.2023.1092060
 Malihe Shams1†
Malihe Shams1† Susanna Pardini2*†
Susanna Pardini2*† Paola Del Bianco1
Paola Del Bianco1 Caterina Calabrese1
Caterina Calabrese1 Gian Luca De Salvo1
Gian Luca De Salvo1 Caterina Novara2
Caterina Novara2Background: Breast cancer diagnosis and treatment compromise well-being in a pervasive way, and negative consequences may remain after recovery. The psychological side of breast cancer has been extensively investigated; however, the role of intrusive thoughts and intolerance of uncertainty have been studied less systematically.
Objectives: The present study aimed to prospectively evaluate worry content, depression, anxiety, and post-traumatic stress symptoms and to define the role of the trait of worry and intolerance of uncertainty (IU) related to breast cancer.
Methods: Patients with their first breast cancer diagnosis were enrolled in a single-center, prospective observational trial. The trait of worry and IU were assessed using the Penn State Worry Questionnaire (PSWQ) and the Intolerance of Uncertainty Scale-Revised (IUS-R). The psychological aspects were evaluated using the Worry Domains Questionnaire (WDQ), the Beck Anxiety (BAI), Beck Depression Inventory-II (BDI-II), and the Impact of Event Scale-Revised (IES-R). Questionnaires were administered in a randomized sequence at diagnosis (T0), 3 months post-diagnosis (T1), and 12 months post-diagnosis (T2).
Results: One hundred and fifty eligible patients were enrolled in the study and provided the T0 assessment. Further compliance rates were 57% at T1 and 64% at T2. All patients showed a significant and continuous increase in the IES-R scale (p < 0.0001) from diagnosis to the end of the study, while no significant changes were observed for the WDQ, BAI, and BDI-II scales. The clinical PSWQ levels and/or high levels of the IUS-R score were the only variables that aided the distinction between patients who maintain high levels of depression, anxiety, and post-traumatic disorders and those who did not.
Conclusion: An early assessment of the components of the trait of worry and intolerance of uncertainty could be critical in identifying patients with a higher psychopathological risk. Furthermore, if future studies confirm the present findings, support and monitoring throughout the prognosis may present crucial benefits, and possibly affect the course of treatment.
Breast cancer is a pathology that can affect women at any age after puberty with an increased rate in later life. It is considered the most prevalent cancer globally, with 2.3 million women diagnosed in 2020 (WHO, 2021).
Breast cancer diagnosis presents challenges to the patient’s physical and psychological well-being (Dooley et al., 2017). Frequently, treatments deployed in order to manage the disease (e.g., radiotherapy, chemotherapy, hormonal, or antibody therapy) can negatively impact the quality of life even after recovery (Fong et al., 2012; Moo et al., 2018). Therefore, the end of treatment should be considered a critical moment in which the patient’s worries related to the actual or perceived loss of support from healthcare centers, and apprehension associated with the possibility of relapse are considered (Cappiello et al., 2007; Costanzo et al., 2007).
The psychological side of breast cancer has been extensively investigated, showing that anxiety, distress and depression are some of the more common psychological disorders experienced during the entire disease trajectory (e.g., Mertz et al., 2012; Lo-Fo-Wong et al., 2016; Ng et al., 2017; Gieseler et al., 2018; Guimond et al., 2019; Dinapoli et al., 2021).
The perceived sudden and catastrophic nature of a cancer diagnosis may promote the onset of Post-Traumatic Stress Disorder (PTSD) (Wu et al., 2016; Van Oers, 2019). Among women with breast cancer, PTSD prevalence varies considerably, up to 32.3% of the population. Heterogeneity could be related to the age at the moment of diagnosis, educational level, socioeconomic status, and the stage of diagnosis (Naidich and Motta, 2000; Wu et al., 2016; Brown et al., 2020). Moreover, there was no agreement between studies investigating the evolution of symptomatology over time. In this regard, to address the issue a literature review has highlighted four heterogeneous developmental trajectories of PTSD symptomatology (Van Oers, 2019): (1) a symptom reduction after diagnosis and during the treatment phase (Mehnert and Koch, 2007; Vin-Raviv et al., 2013; Bulotiene and Matuiziene, 2014; Voigt, 2016; Chan et al., 2018); (2) an increase of symptoms as a function of time (Cordova et al., 2017); (3) a symptom fluctuation during the first years after diagnosis (ibidem); (4) a presence of symptoms at a subclinical level that could be followed by a PTSD diagnosis (Utzon-Frank et al., 2014). Contrarily, research by Voigt (2016) showed that PTSD symptomatology has already been present at the diagnosis phase and that adjuvant and surgical therapies (such as mastectomy) did not promote symptomatology deterioration.
Recent literature has displayed that particular psychological trait constructs, such as Intolerance of Uncertainty (IU), can contribute to the presence of common psychological disorders (e.g., anxiety, depression, and post-traumatic disorders), both in people with and without a cancer diagnosis (e.g., Lerman et al., 1995; Mathews and MacLeod, 2002; Costa-Requena et al., 2011; Oglesby et al., 2016; Tan et al., 2016; Hill and Hamm, 2019; Romeo et al., 2022). Indeed, IU can be defined as a predictor and a maintenance factor of anxiety components already studied independently on cancer (Freeston et al., 1994; Dugas et al., 1997). It could be defined as a dispositional psychological construct characterized by a pervasive difficulty in tolerating aversive reactions to situations perceived as unclear or poorly controlled and negative beliefs on uncertainty (Buhr and Dugas, 2009; Bottesi et al., 2019).
More recent studies have shown a trans-diagnostic role of IU as a common factor in other psychopathologies besides anxiety disorders, such as depression and post-traumatic stress disorder (Einstein, 2014; Carleton, 2016a,b; Bottesi et al., 2019). The malleability of IU in various pathologies highlights the importance of its treatment by deploying a protocol compared to the mere focus on specific disorder features (McEvoy and Erceg-Hurn, 2016; Norton and Paulus, 2016).
Another important related trait construct to IU is Worry, defined as an excessive and uncontrollable concern about what could happen in the future that impacts different aspects of daily life (e.g., finances, relations, work). This construct is characterized by cognitive and emotional processes centered around the perception of uncontrollable fear and is focused on adverse outcomes involving a high level of selective attention on what is perceived as dangerous, usually connected to biased information processing aimed at managing the situation (Borkovec, 1994; Roemer et al., 1997; Craske and Tsao, 1999; Barlow, 2002; Borkovec et al., 2002). One crucial aspect of worry as a trait is its role in affecting distress in uncertainty by increasing a distorted perception of control over future situations (Greco and Roger, 2003). Like IU, the trait of worry has a pervasive impact characterizing anxiety and depressive disorders (Barlow, 1988; Molina and Borkovec, 1994; Dugas et al., 1998). In general, people that display high IU and worry features could experience a greater fear of cancer recurrence, and have distress, anxiety, post-traumatic and depressive symptoms when they are obliged to cope with uncertain situations such as waiting for medical results or the oncological disease prognosis (e.g., Shaha et al., 2008; Eisenberg et al., 2015; Cessna Palas et al., 2021). Demographic features could have a role in moderating the relationship between mental health and intolerance of uncertainty (e.g., Hill and Hamm, 2019).
Not many studies in the literature investigated the longitudinal course of psychological symptoms following a breast cancer diagnosis. A recent longitudinal study put in light how essential is investigate psychological symptomatology during the different phases of cancer from diagnosis to the follow-up after treatment, since it permits to understand the presence of risk and protective factors able in influencing the patients’ well-being (Romeo et al., 2020). This research investigated the relationship between depressive symptomatology, assessed at the time of diagnosis and 2 years later, and the Posttraumatic Growth, showing how positive psychological changes experienced after the struggle with cancer where higher in the group of patients that were no longer depressed rather than individuals that continued in experiencing depressive symptoms (Romeo et al., 2020).
To the best of our knowledge, the impact of IU and worry as a trait and predictive constructs on other common psychological problems have not been deeply longitudinally studied during different salient phases in a sample composed of individuals with breast cancer (Hill and Hamm, 2019). This type of analysis could be valuable to the identification and implementation of specific psychological rehabilitation protocols for breast cancer patients promoting overall well-being (Ramírez-Vélez et al., 2021).
The primary aim of this study was to prospectively evaluate worry content, depression, anxiety, and post-traumatic stress symptoms and to define whether the trait of worry and IU related to breast cancer were associated with high levels of psychopathological symptoms from diagnosis through treatment and follow-up. A secondary aim was to assess whether socio-demographics, clinical, and treatment variables influenced baseline trait components.
It has been expected that participants characterized by higher levels of worry, and IU present more anxiety, depression, and traumatic events than the others, independently from the assessment phase.
The study was designed as a single-center, prospective, observational cohort investigation. Patients were eligible and included in the study if they had histologically proven diagnosis of primary breast carcinoma, were aged between 18 and 75, and were able to understand the investigational nature of the study. Patients were excluded if they: (1) could not adequately understand the Italian language, (2) had a psychological or psychopharmacological treatment in progress, (3) had a head injury, degenerative or cardiological disease, (4) previously received a cancer diagnosis other than breast carcinoma and have already undergone treatment. All eligible patients signed an Independent Ethics Committee/Institutional Review Board-approved written informed consent form before the baseline assessment. The current study was conducted following the Declaration of Helsinki and the protocol n. 642 identified by “IOV-BC-1-2015 IT&W” was approved by the IOV Ethical Committee on 12 December 2015.
Female patients who underwent primary surgery at the Veneto Institute of Oncology (Italy) were asked to complete a randomized sequence of questionnaires at diagnosis (T0), during treatment at 3 months post-diagnosis (T1), and during the follow-up at 12 months after diagnosis (T2). Each patient self-reported socio-demographic information about age, marital status, cohabitation, level of education, and current employment. Clinical data were also collected and included the type of surgery, stage of disease, and type of treatment planned.
Between November 2015 and March 2017, 150 eligible patients were enrolled in the study. All patients provided a baseline assessment at diagnosis, and further compliance rates over the study period were 57% (85 patients) at T1, and 64% (96 patients) at T2. Of 150 eligible patients at baseline, 55 completed the questionnaires at all 3-time points, and 24 completed only the baseline assessment. The main reason for missing questionnaires was the difficulty in intercepting and engaging the patients during treatment and follow-up visits.
The IU was measured using the Intolerance of Uncertainty Scale-Revised (IUS-R; Freeston et al., 1994; Bottesi et al., 2015), a 12-items short form of the original version (Bottesi et al., 2019) that measures reactions to uncertainty, ambiguous situations, and the future (e.g., Uncertain events upset me greatly). This shorter version was used for the current study because the 27-item version has several items that appear to pertain specifically to GAD and might better account for symptoms of worry as a trait than those of other anxiety disorders (Carleton et al., 2010; Gentes and Ruscio, 2011). Participants rate each item on the IUS-R from 1 (Not at all characteristics of me) to 5 (Entirely characteristic of me), with total scores ranging from 12 to 60, and higher scores indicating greater IU. The measure consists of a total score and two subscales representing approach and avoidance responses to uncertainty, respectively (Birrell et al., 2011). The “Prospective IU” subscale measures the desire for predictability, preferences for knowing what the future holds, anxiety about future uncertain events, and active engagement in seeking information to increase certainty. The “Inhibitory IU” measures avoidance and paralysis in the face of uncertainty. The IUS-R total and subscale scores have good psychometric properties in both clinical and non-clinical samples (Carleton et al., 2007, 2012; Khawaja and Yu, 2010; McEvoy and Mahoney, 2011; Helsen et al., 2013; Jacoby et al., 2013) and internal consistency has also been confirmed for the current sample (0.82 < Cronbach’s α < 0.90; 0.66 < McDonald’s ωh < 0.72; 0.87 < McDonald’s ωt < 0.92) (Flora, 2020). For this study, we used the IUS-R total score. Considering the average and standard deviation obtained by a sample of the general Italian population (M = 26.73; SD = 8.20), patients were split into high and low IUS groups based on the current sample median of 27.
The Penn State Worry Questionnaire (PSWQ; Meyer et al., 1990; Morani et al., 1999) was used to assess the WCP; it has 16 items on a Likert scale from 1 to 5. Scores range from 16 to 80, with higher scores indicative of higher levels of trait worry. Eleven items are worded in the direction of pathological worry, with higher numbers indicating more worry (e.g., Once I start worrying, I cannot stop). In comparison, the remaining five items are worded to indicate that worry is not a problem, with higher numbers indicating less worry (e.g., I never worry about anything). The total score was split into high and low PSWQ groups based on the recommended cut-off score of 41. The higher PSWQ scores reflect greater levels of pathological worry. Its internal consistency was good (original version: Cronbach’s α = 0.93; Italian version α = 0.85). The current study highlighted excellent internal consistency (Cronbach’s α = 0.90; McDonald’s ωh = 0.78; McDonald’s ωt = 0.93) (Flora, 2020).
The Worry Domains Questionnaire (WDQ; Tallis et al., 1994; Morani et al., 1999) is a self-report questionnaire based on 25 items investigating worry content. The scoring is based on a Likert scale from 0 to 4. Higher scores indicate higher worry experienced about specific domains. The WDQ yields a total score, which is the sum of scores on five subscales titled (1) Relationships, (2) Lack of Confidence, (3) Aimless Future, (4) Work, and (5) Financial. Good internal consistency has been evidenced for the current sample (0.74 < Cronbach’s α < 0.93; 0.58 < McDonald’s ωh < 0.79; 0.78 < McDonald’s ωt < 0.94) (Flora, 2020).
The Beck Anxiety Inventory (BAI; Beck et al., 1988; Sica et al., 2009) is a 21-question multiple-choice self-report inventory used for measuring the severity of anxiety. The questions ask about common symptoms of anxiety that the subject has had during the past week. Each item of the BAI is scored on a scale of 0 (not at all) to 3 (severely), with higher scores indicative of higher anxiety severity. The original and the Italian versions showed good internal consistency (Cronbach’s α = 0.92 and 0.89, respectively) and adequate test–retest reliability. The current study showed good internal consistency (Cronbach’s α = 0.91; McDonald’s ωh = 0.59; McDonald’s ωt = 0.93; Flora, 2020).
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996; Ghisi et al., 2006) is a 21-items self-report questionnaire, rated on a four-point Likert scale ranging from 0 to 3, used to assess the severity of depressive symptoms. Higher scores indicate higher depressive symptoms severity. The original and the Italian versions showed excellent internal consistency (Cronbach’s α = 0.93 and 0.87, respectively) and test–retest reliability (r = 0.93 and 0.76, respectively). In the current study, the questionnaire proved good internal consistency (Cronbach’s α = 0.88; McDonald’s ωh = 0.57; McDonald’s ωt = 0.90; Flora, 2020).
The Impact of Event Scale-Revised (IES-R; Weiss and Marmar, 1997; Pietrantonio et al., 2003) is a 22-item self-report measure that assesses subjective distress caused by traumatic events. Respondents are asked to identify a specific stressful life event and then indicate how distressed or bothered they were during the past 7 days by each “difficulty” listed. Items are rated on a 5-point scale ranging from 0 (“not at all”) to 4 (“extremely”). The IES-R yields a total score (ranging from 0 to 88), and subscale scores can also be calculated for the Intrusion, Avoidance, and Hyperarousal subscales. A score above 50 indicates a probable case of PTSD. Internal consistency in the current study was from 0.82 to 0.90, for Cronbach’s α; from 0.65 to 0.82 for McDonald’s ωh; from 0.88 to 0.95 for McDonald’s ωt (Flora, 2020).
Statistical analyzes were performed using the SAS statistical package (SAS Institute Inc., 2013), RStudio (RStudio Team, 2020), and R software (R Core Team, 2020). Clinical and demographic variables are described using the median and interquartile ranges for quantitative data, frequencies, and percentages for categorical data. The PSWQ and IUS-R scales were analyzed as continuous and dichotomous variables to assess their distribution within socio-demographics, clinical, and treatment variables and to define patient groups to be compared in terms of worry content, anxiety, depression, and distress caused by traumatic events, respectively.
Linear regression models were used to evaluate the impact of clinical characteristics on trait variables at diagnosis. Mixed-effects linear models were fitted for each measure to examine the change within and between groups of interest. A mixed-effects logistic model analyzed the presence of specific stressful life events reported over time and between patients’ characteristics. The mixed models included the time of questionnaire assessment, the group, and their interaction, as fixed effects, and an unstructured covariance structure for the random effects.
All statistical tests used a two-sided 1% significance level (2-sided) to reduce the possibility of false-positive statistical testing.
The entire sample is composed of 150 patients. No statistically significant differences between patients who returned the questionnaires and those who did not regarding sociodemographic and clinical variables were observed (Supplementary Table S1). The baseline characteristics of patients are summarized in Table 1. Most of them had stage I-II invasive breast carcinoma (81.7%), and out of 120 patients with available data for surgery, 41 (34.2%) had a mastectomy.
The Worry and IU trait constructs, measured by the PSWQ and the IUS-R scales, remained stable over time, and the baseline assessment did not differ among patients’ characteristics (Supplementary Tables S2, S3).
The WDQ total and subscales scores remained unchanged across the study period, except for the subscale “Lack of confidence” which increased during treatment for patients who have higher baseline IUS-R levels (at diagnosis: 4.6 points, 95% CI: 3.8 to 5.4; 3 months post-diagnosis: 5.5 points, 95% CI: 4.4 to 6.5), and decreased at follow-up (12 months post-diagnosis: 4.0 points, 95% CI: 3.0 to 5.0; p = 0.0017) and for patients reporting both a higher baseline IUS-R and PSWQ levels (at diagnosis: 5.1 points, 95% CI: 4.2 to 5.9; 3 months post-diagnosis: 6.1 points, 95% CI: 4.9 to 7.2; 12 months post-diagnosis: 4.5 points, 95% CI: 3.4 to 5.6; p = 0.0023; Figure 1A; Table 2; Supplementary Table S4).
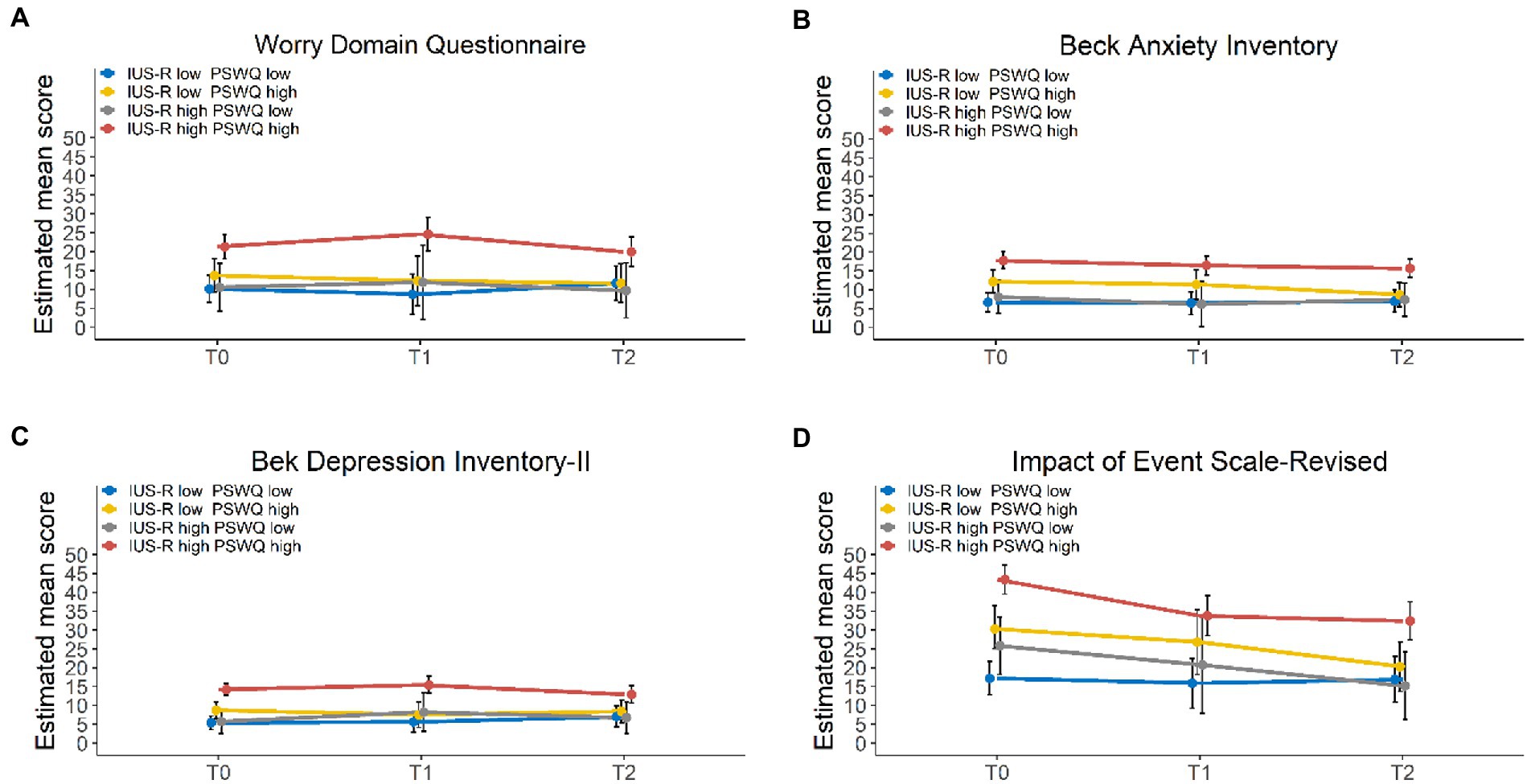
Figure 1. Trends over time of the WDQ (A), BAI (B), BDI-II (C), and IES-R (D) scores of 4 groups divided based on the PSWQ and the IUS-R clinical cut-off (T0: N = 150; T1: N = 85; T2: N = 96). PSWQ = Penn State Worry Questionnaire; IUS-R = Intolerance of Uncertainty-Revised. T0: at diagnosis, T1: 3 months post-diagnosis, T2: 12 months post-diagnosis.
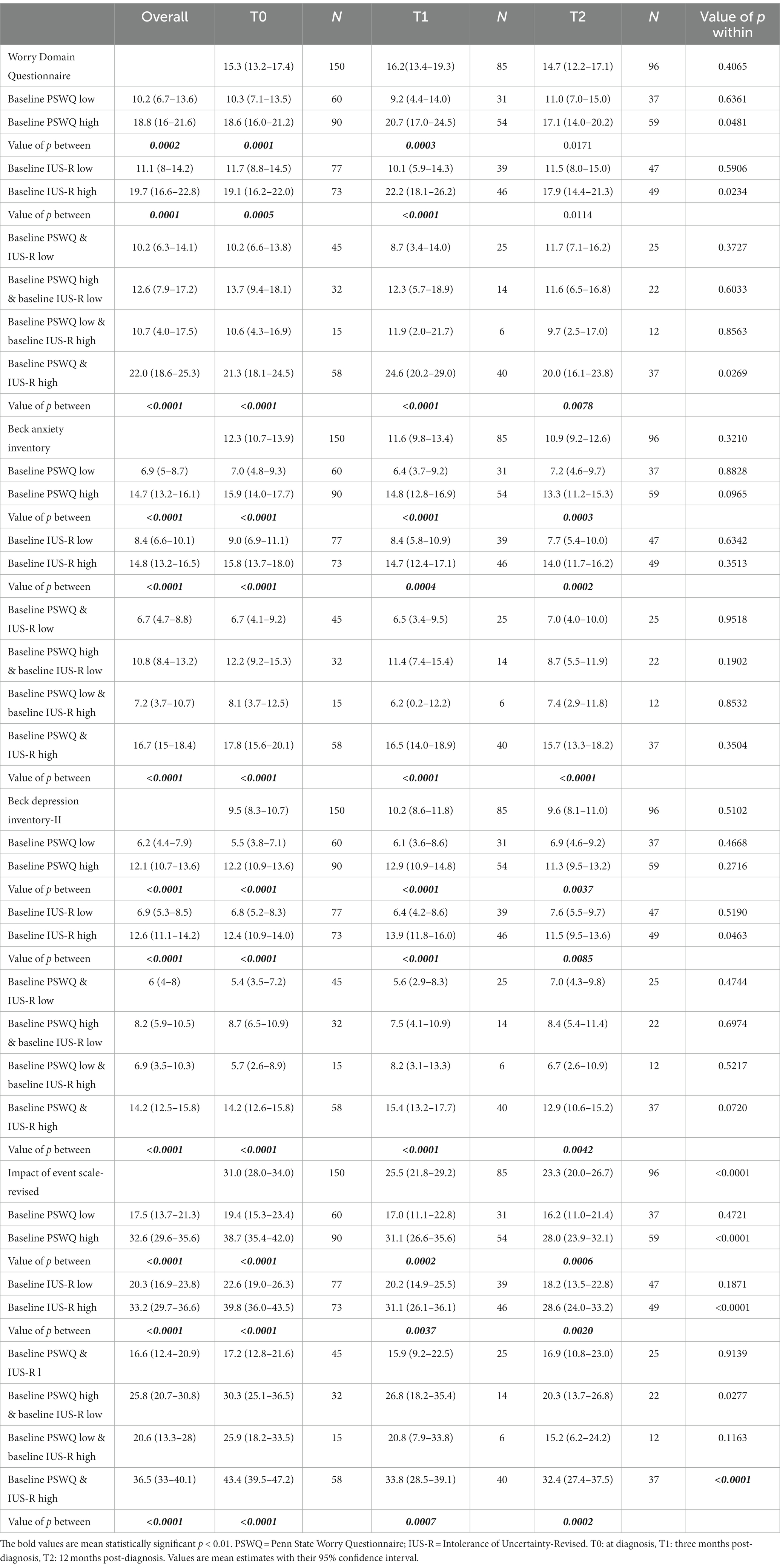
Table 2. Mean changes over time and across clinical characteristics of the worry content, anxiety, depression, and post-traumatic stress symptom scales (T0: N = 150; T1: N = 85; T2: N = 96).
Overall, patients reporting elevated baseline PSWQ or/and IUS-R levels had a statistically significantly worse WDQ score at T0 that remained impaired throughout the study (Table 2). Similar patterns were observed for WDQ “Lack of confidence,” “Aimless future,” and “Work” subscales. This impairment was observed for the WDQ “Financial” subscale only for patients with pathological PSWQ (Supplementary Table S4).
The BAI and the BDI-II scores (Figures 1B,C; Table 2) did not significantly change over time. Similarly to what was observed for the WDQ scale, high PSWQ and/or IUS-R scores were significantly associated with a detrimental impact on anxiety and depressive symptoms.
The IES-R scale and all subscales displayed a statistically significant reduction across the study period. This improvement was observed in particular for patients reporting high PSWQ and/or IUS-R scores at diagnosis (Figure 1D; Table 2; Supplementary Table S5). Moreover, high PSWQ and/or IUS-R levels significantly worsened distress caused by traumatic events (Table 2).
Considering the specific stressful life events identified in the IES–R, disease was reported at diagnosis by 36.7% of patients. This percentage decreased to 20% 12 months post-diagnosis, although not statistically significant (Table 3).
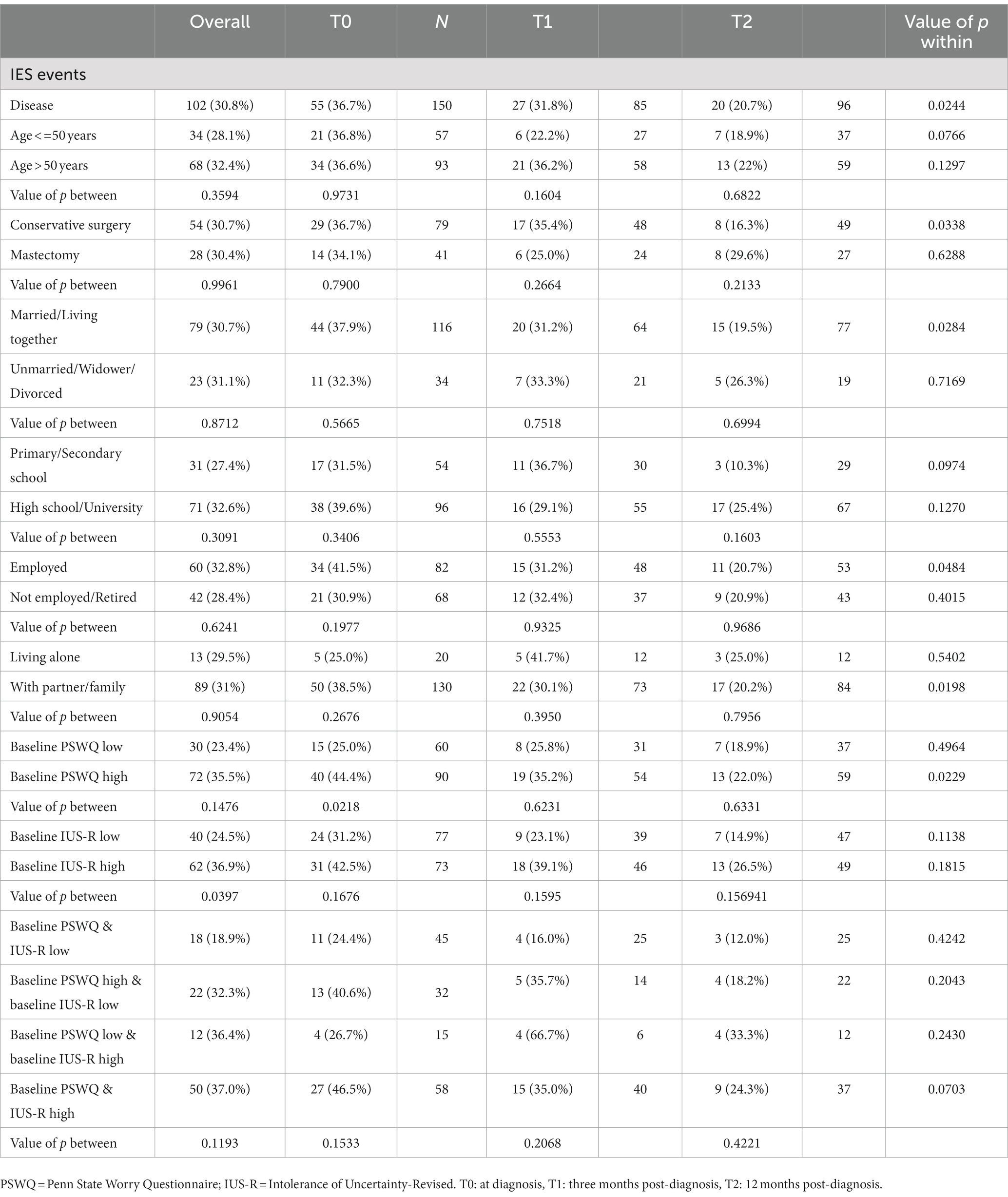
Table 3. Frequency of events reported over time: overall and according to patient characteristics (T0: N = 150; T1: N = 85; T2: N = 96).
The current study investigated the trait of worry, intolerance of uncertainty, depression, anxiety, and post-traumatic symptoms related to breast cancer and how they change from diagnosis through treatment and follow-up. Considering that worry and IU are dispositional traits, we also aimed to understand whether breast cancer patients with a difficulty in managing uncertainty and worry traits showed high levels of worry content, depression, anxiety, and post-traumatic stress symptoms over time.
First, we demonstrated a longitudinal stability of the trait constructs measured by the PSWQ and the IUS-R scales, in line with studies that showed how IU and trait of worry seems to be stable over time and across situation (e.g., Dugas et al., 2004; Mahoney and McEvoy, 2012; Brintzinger et al., 2021; Lauriola et al., 2023). Coherently with literature (e.g., Carleton et al., 2012), we evidenced that the trait of worry and intolerance of uncertainty were related to high levels of worry contents, anxiety, and depressive symptoms, underlying the connection between IU and trait of worry with other psychopathological symptoms. Therefore, IU and the trait of worry should be considered two relevant aspects that could help to discriminate between patients who maintain high depression, anxiety, and post-traumatic disorders scores. These data align with the description of the IU and trait of worry as trans-diagnostic constructs identified as factors that play a central role in developing and maintaining different psychopathology (such as obsessive–compulsive disorder, generalized anxiety disorder, and depression), in line with other studies that focused their investigation on sample with and without the presence of a cancer diagnosis (e.g., Eisenberg et al., 2015; Carleton, 2016a,b; Cessna Palas et al., 2021). If our outcomes are confirmed, screening and intervention in preventing dysfunctional responses to stressors, as are the diagnostic and treatment processes related to breast cancer, could be considered valid procedures that improve the patients’ quality of life.
Our results are in line with what emerged in the literature related to the communication of the cancer phase (e.g., Gieseler et al., 2018), also highlighting how this moment is a crucial, sensitive, and challenging situation for people, independently of the socio-demographic variables. Indeed, cancer events described as traumatic experiences are particularly salient during the period close to the communication of the diagnosis than during the treatment period. The diagnosis communication could be perceived as a discrepancy between what is happening and the ability to cope with the event (Gieseler et al., 2018). The fact that the cancer event is less referred to as a traumatic episode in the subsequent assessment phases could be interpreted as a physiological process of habituation and elaboration, concurrently with the planning of treatment. Although with a different method and timing, a similar trend has been observed by Chan and colleagues Chan et al. (2018), who have analyzed PTSD features over 4 years, showing a general decrease in symptomatology. These data confirm the need to consider cancer as a traumatic event and to evaluate, in a systematic way, PTSD symptoms following a cancer diagnosis. Also, some socio-demographic features must be considered as protective factors of psychopathological manifestation related to cancer; in line with what has been highlighted by two studies (Cordova et al., 2017; Van Oers, 2019), social support, living together, and socio-economic status could play a role as predisposition factors in the development of PTSD. Although it is important to consider that no differences between groups have been shown for these variables, socio-demographic features, including a support network related to the person, have been considered influential elements of the quality of life, the general well-being, and the ability to manage cancer. Future studies could also considering to investigate the coping strategies and Posttraumatic Growth as possible risk and protective factors related to psychological symptoms. Moreover, it seems that intolerance of uncertainty and worry as a trait influenced patients’ mental health condition all the time, independently of the assessment phase and other features. For this reason, our outcome focus on the importance to consider IU and trait of worry as a potential therapeutic target (e.g., Brown et al., 2017), as well as the prominence in assessing and managing IU and trait of worry since the diagnosis phase to promote a better mental health condition of patients with a breast cancer diagnosis.
A limitation of this study is the presence of questionnaires that need to be included. As in other studies with a longitudinal design, missing data increased over time. However, since 84% of patients completed the questionnaires at least in two assessment phases, the potential biasing effect of missing data may have been less strongly affected by the results of the comparisons over time and the overall mean between groups.
The presence of clinically significant worry as a trait and IU features at the beginning of the breast cancer diagnostic procedure should be carefully considered in the intervention planning by the clinician. The systematic assessment of worry and IU could be helpful in managing the psychological problems that during treatment and follow-up stages tend to remain high and seem precisely influenced by traits such as intolerance for uncertainty and the trait of worry.
Globally, our results indicate that processing traits variables, such as worry and intolerance of uncertainty, can have a significant impact on the global psychological condition of patients. An early assessment of the components of worry as a trait and intolerance of uncertainty could be important in identifying those people with a higher psychopathological risk (e.g., Brown et al., 2017). In addition, monitoring and support throughout the disease would be desirable if further studies confirmed these data. Overall, outcomes show the importance of promoting specific psychological rehabilitation protocols for breast cancer patients’ global well-being (Ramírez-Vélez et al., 2021).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The current study was conducted following the Declaration of Helsinki and the protocol n. 642 identified by IOV-BC-1-2015 IT&W and approved by the IOV Ethical Committee on 12/15/2015. The patients/participants provided their written informed consent to participate in this study.
SP, CN, and MS: conceptualization of the protocol. MS, SP, and CN: methodology. CC and SP: investigation. PDB and GLDS: curation and formal analysis. SP and CC: writing and original draft preparation. CN, PDB, and MS: supervised. All authors contributed to the manuscript editing and revision, and they have read and agreed to the published version of the manuscript.
This research was funded by Italian Ministry of Health Ricerca Corrente.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1092060/full#supplementary-material
Barlow, D. H.. (1988). Anxiety and its Disorders: The Nature and Treatment of Anxiety and Panic. New York: Guilford Press.
Barlow, D. H.. (2002). Anxiety and its Disorders: The Nature and Treatment of Anxiety and Panic. 2nd. New York: The Guilford Press.
Beck, A. T., Epstein, N., Brown, G., and Steer, R. A. (1988). An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 56, 893–897. doi: 10.1037/0022-006X.56.6.893
Beck, A. T., Steer, R. A., and Brown, G. K. (1996). Beck Depression Inventory (BDI-II). London, England: Pearson.
Birrell, J., Meares, K., Wilkinson, A., and Freeston, M. (2011). Toward a definition of intolerance of uncertainty: a review of factor analytical studies of the intolerance of uncertainty scale. Clin. Psychol. Rev. 31, 1198–1208. doi: 10.1016/j.cpr.2011.07.009
Borkovec, T. D. (1994). “The nature, functions, and origins of worry” in Worrying: Perspectives on Theory, Assessment and Treatment. eds. G. Davey and F. Tallis (Chichester: John Wiley & Sons), 5–33.
Borkovec, T. D., Newman, M. G., Pincus, A. L., and Lytle, R. (2002). A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. J. Consult. Clin. Psychol. 70, 288–298. doi: 10.1037/0022-006X.70.2.288
Bottesi, G., Ghisi, M., Altoè, G., Conforti, E., Melli, G., and Sica, C. (2015). The Italian version of the depression anxiety stress Scales-21: factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 60, 170–181. doi: 10.1016/j.comppsych.2015.04.005
Bottesi, G., Noventa, S., Freeston, M. H., and Ghisi, M. (2019). Seeking certainty about intolerance of uncertainty: addressing old and new issues through the intolerance of uncertainty scale-revised. PLoS One 14:e0211929. doi: 10.1371/journal.pone.0211929
Brintzinger, M., Tschacher, W., Endtner, K., Bachmann, K., Reicherts, M., Znoj, H., et al. (2021). Patients’ style of emotional processing moderates the impact of common factors in psychotherapy. Psychotherapy 58, 472–484. doi: 10.1037/pst0000370
Brown, L. C., Murphy, A. R., Lalonde, C. S., Subhedar, P. D., Miller, A. H., and Stevens, J. S. (2020). Posttraumatic stress disorder and breast cancer: risk factors and the role of inflammation and endocrine function. Cancer 126, 3181–3191. doi: 10.1002/cncr.32934
Brown, M., Robinson, L., Campione, G. C., Wuensch, K., Hildebrandt, T., and Micali, N. (2017). Intolerance of uncertainty in eating disorders: a systematic review and meta-analysis. Eur. Eat. Disord. Rev. 25, 329–343. doi: 10.1002/erv.2523
Buhr, K., and Dugas, M. J. (2009). The role of fear of anxiety and intolerance of uncertainty in worry: an experimental manipulation. Behav. Res. Ther. 47, 215–223. doi: 10.1016/j.brat.2008.12.004
Bulotiene, G., and Matuiziene, M. (2014). Posttraumatic stress in breast cancer patients. Acta Med. Litu. 21, 43–50. doi: 10.6001/actamedica.v21i2.2940
Cappiello, M., Cunningham, R. S., Tish Knobf, M., and Erdos, D. (2007). Breast cancer survivors: information and support after treatment. Clin. Nurs. Res. 16, 278–293. doi: 10.1177/1054773807306553
Carleton, R. N. (2016a). Fear of the unknown: one fear to rule them all? J. Anxiety Disord. 41, 5–21. doi: 10.1016/j.janxdis.2016.03.011
Carleton, R. N. (2016b). Into the unknown: a review and synthesis of contemporary models involving uncertainty. J. Anxiety Disord. 39, 30–43. doi: 10.1016/j.janxdis.2016.02.007
Carleton, R. N., Gosselin, P., and Asmundson, G. J. (2010). The intolerance of uncertainty index: replication and extension with an English sample. Psychol. Assess. 22, 396–406. doi: 10.1037/a0019230
Carleton, R. N., Mulvogue, M. K., Thibodeau, M. A., McCabe, R. E., Antony, M. M., and Asmundson, G. J. (2012). Increasingly certain about uncertainty: intolerance of uncertainty across anxiety and depression. J. Anxiety Disord. 26, 468–479. doi: 10.1016/j.janxdis.2012.01.011
Carleton, R. N., Norton, M. P. J., and Asmundson, G. J. (2007). Fearing the unknown: a short version of the intolerance of uncertainty scale. J. Anxiety Disord. 21, 105–117. doi: 10.1016/j.janxdis.2006.03.014
Cessna Palas, J. M. C., Hyland, K. A., Nelson, A. M., Small, B. J., Jim, H. S., and Jacobsen, P. B. (2021). An examination of the relationship of patient modifiable and non-modifiable characteristics with fear of cancer recurrence among colorectal cancer survivors. Support. Care Cancer 29, 869–876. doi: 10.1007/s00520-020-05552-4
Chan, C. M. H., Ng, C. G., Taib, N. A., Wee, L. H., Krupat, E., and Meyer, F. (2018). Course and predictors of post-traumatic stress disorder in a cohort of psychologically distressed patients with cancer: a 4-year follow-up study. Cancer 124, 406–416. doi: 10.1002/cncr.30980
Cordova, M. J., Riba, M. B., and Spiegel, D. (2017). Post-traumatic stress disorder and cancer. Lancet Psychiatry 4, 330–338. doi: 10.1016/S2215-0366(17)30014-7
Costanzo, E. S., Lutgendorf, S. K., Mattes, M. L., Trehan, S., Robinson, C. B., Tewfik, F., et al. (2007). Adjusting to life after treatment: distress and quality of life following treatment for breast cancer. Br. J. Cancer 97, 1625–1631. doi: 10.1038/sj.bjc.6604091
Costa-Requena, G., Rodríguez, A., Fernández, R., Palomera, E., and Gil, F. L. (2011). Cognitive processing variables in breast cancer: worry and distress at the end of treatment. J. Cancer Educ. 26, 375–379. doi: 10.1007/s13187-010-0140-8
Craske, M. G., and Tsao, J. C. (1999). Self-monitoring with panic and anxiety disorders. Psychol. Assess. 11, 466–479. doi: 10.1037/1040-3590.11.4.466
Dinapoli, L., Colloca, G., Di Capua, B., and Valentini, V. (2021). Psychological aspect to consider in breast cancer diagnosis and treatment. Curr. Oncol. Rep. 23:38. doi: 10.1007/s11912-021-01049-3
Dooley, L. N., Slavich, G. M., Moreno, P. I., and Bower, J. E. (2017). Strength through adversity: moderate lifetime stress exposure is associated with psychological resilience in breast cancer survivors. Stress. Health 33, 549–557. doi: 10.1002/smi.2739. Epub 2017 Jan 4
Dugas, M. J., Buhr, K., and Ladouceur, R.. (2004). The Role of Intolerance of Uncertainty in Etiology and Maintenance. New York: Guilford Press.
Dugas, M. J., Freeston, M. H., and Ladouceur, R. (1997). Intolerance of uncertainty and problem orientation in worry. Cogn. Ther. Res. 21, 593–606. doi: 10.1023/A:1021890322153
Dugas, M. J., Gagnon, F., Ladouceur, R., and Freeston, M. H. (1998). Generalized anxiety disorder: a preliminary test of a conceptual model. Behav. Res. Ther. 36, 215–226. doi: 10.1016/s0005-7967(97)00070-3
Einstein, D. A. (2014). Extension of the transdiagnostic model to focus on intolerance of uncertainty: a review of the literature and implications for treatment. Clin. Psychol. 21, 280–300. doi: 10.1111/cpsp.12077
Eisenberg, S. A., Kurita, K., Taylor-Ford, M., Agus, D. B., Gross, M. E., and Meyerowitz, B. E. (2015). Intolerance of uncertainty, cognitive complaints, and cancer-related distress in prostate cancer survivors. Psychooncology 24, 228–235. doi: 10.1002/pon.3590
Flora, D. B. (2020). Your coefficient alpha is probably wrong, but which coefficient omega is right? A tutorial on using R to obtain better reliability estimates. Adv. Methods Pract. Psychol. Sci. 3, 484–501. doi: 10.1177/2515245920951747
Fong, D. Y., Ho, J. W., Hui, B. P., Lee, A. M., Macfarlane, D. J., Leung, S. S., et al. (2012). Physical activity for cancer survivors: meta-analysis of randomised controlled trials. BMJ 344:e70. doi: 10.1136/bmj.e70
Freeston, M. H., Rhéaume, J., Letarte, H., Dugas, M. J., and Ladouceur, R. (1994). Why do people worry? Personal. Individ. Differ. 17, 791–802. doi: 10.1016/0191-8869(94)90048-5
Gentes, E. L., and Ruscio, A. M. (2011). A meta-analysis of the relation of intolerance of uncertainty to symptoms of generalized anxiety disorder, major depressive disorder, and obsessive–compulsive disorder. Clin. Psychol. Rev. 31, 923–933. doi: 10.1016/j.cpr.2011.05.001
Ghisi, M., Flebus, G. B., Montano, A., Sanavio, E., and Sica, C.. (2006). Beck Depression Inventory-II. Manuale Italiano. Firenze: Organizzazioni Speciali.
Gieseler, F., Gaertner, L., Thaden, E., and Theobald, W. (2018). Cancer diagnosis: a trauma for patients and doctors alike. Oncologist 23, 752–754. doi: 10.1634/theoncologist.2017-0478
Greco, V., and Roger, D. (2003). Uncertainty, stress, and health. Pers. Individ. Differ. 34, 1057–1068. doi: 10.1016/S0191-8869(02)00091-0
Guimond, A. J., Ivers, H., and Savard, J. (2019). Clusters of psychological symptoms in breast cancer: is there a common psychological mechanism? Cancer Nurs. 43, 343–353. doi: 10.1097/NCC.0000000000000705
Helsen, K., Van den Bussche, E., Vlaeyen, J. W., and Goubert, L. (2013). Confirmatory factor analysis of the Dutch intolerance of uncertainty scale: comparison of the full and short version. J. Behav. Ther. Exp. Psychiatry 44, 21–29. doi: 10.1016/j.jbtep.2012.07.004
Hill, E. M., and Hamm, A. (2019). Intolerance of uncertainty, social support, and loneliness in relation to anxiety and depressive symptoms among women diagnosed with ovarian cancer. Psychooncology 28, 553–560. doi: 10.1002/pon.4975
Jacoby, R. J., Fabricant, L. E., Leonard, R. C., Riemann, B. C., and Abramowitz, J. S. (2013). Just to be certain: confirming the factor structure of the intolerance of uncertainty scale in patients with obsessive-compulsive disorder. J. Anxiety Disord. 27, 535–542. doi: 10.1016/j.janxdis.2013.07.008
Khawaja, N. G., and Yu, L. N. H. (2010). A comparison of the 27-item and 12-item intolerance of uncertainty scales. Clin. Psychol. 14, 97–106. doi: 10.1080/13284207.2010.502542
Lauriola, M., Iannattone, S., and Bottesi, G. (2023). Intolerance of uncertainty and emotional processing in adolescence: separating between-person stability and within-person change. Res. Child Adolesc. Psychopathol. 27, 1–14. doi: 10.1007/s10802-022-01020-1
Lerman, C., Lustbader, E., Rimer, B., Daly, M., Miller, S., Sands, C., et al. (1995). Effects of individualized breast cancer risk counseling: a randomized trial. J. Natl. Cancer Inst. 87, 286–292. doi: 10.1093/jnci/87.4.286
Lo-Fo-Wong, D. N., de Haes, H. C., Aaronson, N. K., van Abbema, D. L., den Boer, M. D., van Hezewijk, M., et al. (2016). Predictors of enduring clinical distress in women with breast cancer. Breast Cancer Res. Treat. 158, 563–572. doi: 10.1007/s10549-016-3896-7
Mahoney, A. E. J., and McEvoy, P. M. (2012). Trait versus situation-specific intolerance of uncertainty in a clinical sample with anxiety and depressive disorders. Cogn. Behav. Ther. 41, 26–39. doi: 10.1080/16506073.2011.622131
Mathews, A., and MacLeod, C. (2002). Induced processing biases have causal effects on anxiety. Cogn. Emot. 16, 331–354. doi: 10.1080/02699930143000518
McEvoy, P. M., and Erceg-Hurn, D. M. (2016). The search for universal transdiagnostic and trans-therapy change processes: evidence for intolerance of uncertainty. J. Anxiety Disord. 41, 96–107. doi: 10.1016/j.janxdis.2016.02.002
McEvoy, P. M., and Mahoney, A. E. (2011). Achieving certainty about the structure of intolerance of uncertainty in a treatment-seeking sample with anxiety and depression. J. Anxiety Disord. 25, 112–122. doi: 10.1016/j.janxdis.2010.08.010
Mehnert, A., and Koch, U. (2007). Prevalence of acute and post-traumatic stress disorder and comorbid mental disorders in breast cancer patients during primary cancer care: a prospective study. Psychooncology 16, 181–188. doi: 10.1002/pon.1057
Mertz, B. G., Bistrup, P. E., Johansen, C., Dalton, S. O., Deltour, I., Kehlet, H., et al. (2012). Psychological distress among women with newly diagnosed breast cancer. Eur. J. Oncol. Nurs. 16, 439–443. doi: 10.1016/j.ejon.2011.10.001
Meyer, T. J., Miller, M. L., Metzger, R. L., and Borkovec, T. D. (1990). Development and validation of the penn state worry questionnaire. Behav. Res. Ther. 28, 487–495. doi: 10.1016/0005-7967(90)90135-6
Molina, S., and Borkovec, T. D. (1994). “The Penn State worry questionnaire: Pyschometric properties and associated characteristics” in Worrying: Perspectives on Theory, Assessment and Treatment. eds. G. C. L. Davey and F. Tallis (West Sussex: John Wiley & Sons Ltd)
Moo, T. A., Sanford, R., Dang, C., and Morrow, M. (2018). Overview of breast cancer therapy. PET Clin. 13, 339–354. doi: 10.1016/j.cpet.2018.02.006
Morani, S., Pricci, D., and Sanavio, E. (1999). Penn state worry questionnaire e worry domains questionnaire. Presentazione delle versioni italiane ed analisi della fedeltà. Psicoterapia Cogn. Comport. 5, 13–34.
Naidich, J. B., and Motta, R. W. (2000). PTSD-related symptoms in women with breast cancer. J. Psychother. Independent Pract. 1, 35–54. doi: 10.1300/J288v01n01_04
Ng, C. G., Mohamed, S., Kaur, K., Sulaiman, A. H., Zainal, N. Z., Taib, N. A., et al. (2017). Perceived distress and its association with depression and anxiety in breast cancer patients. PLoS One 12:e0172975. doi: 10.1371/journal.pone.0172975
Norton, P. J., and Paulus, D. J. (2016). Toward a unified treatment for emotional disorders: update on the science and practice. Behav. Ther. 47, 854–868. doi: 10.1016/j.beth.2015.07.002
Oglesby, M. E., Boffa, J. W., Short, N. A., Raines, A. M., and Schmidt, N. B. (2016). Intolerance of uncertainty as a predictor of post-traumatic stress symptoms following a traumatic event. J. Anxiety Disord. 41, 82–87. doi: 10.1016/j.janxdis.2016.01.005
Pietrantonio, F., De Gennaro, L., Di Paolo, M. C., and Solano, L. (2003). The impact of event scale: validation of an Italian version. J. Psychosom. Res. 55, 389–393. doi: 10.1016/s0022-3999(02)00638-4
R Core Team. (2020). R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing. Available at: https://www.R-project.org/.
Ramírez-Vélez, R., Zambom-Ferraresi, F., García-Hermoso, A., Kievisiene, J., Rauckiene-Michealsson, A., and Agostinis-Sobrinho, C. (2021). Evidence-based exercise recommendations to improve mental wellbeing in women with breast cancer during active treatment: a systematic review and meta-analysis. Cancers (Basel) 13:264. doi: 10.3390/cancers13020264
Roemer, L., Molina, S., and Borkovec, T. D. (1997). An investigation of worry content among generally anxious individuals. J. Nerv. Ment. Dis. 185, 314–319. doi: 10.1097/00005053-199705000-00005
Romeo, A., Di Tella, M., Ghiggia, A., Tesio, V., Torta, R., and Castelli, L. (2020). Posttraumatic growth in breast cancer survivors: are depressive symptoms really negative predictors? Psychol. Trauma 12, 244–250. doi: 10.1037/tra0000508
Romeo, A., Novello, F., and Castelli, L. (2022). Intolerance to uncertainty and adult separation anxiety in relatives of COVID-19 inpatients. Minerva Psychiatry 63, 311–313. doi: 10.23736/S2724-6612.22.02364-8
RStudio Team. (2020). RStudio: Integrated Development for R. Boston, MA: RStudio, PBC. Available at: http://www.rstudio.com/.
Shaha, M., Cox, C. L., Talman, K., and Kelly, D. (2008). Uncertainty in breast, prostate, and colorectalcancer: implications for supportive care. J. Nurs. Scholarsh. 40, 60–67. doi: 10.1111/j.1547-5069.2007.00207.x
Sica, C., Ghisi, M., Altoè, G., Chiri, L. R., Franceschini, S., Coradeschi, D., et al. (2009). The Italian version of the obsessive compulsive inventory: its psychometric properties on community and clinical samples. J. Anxiety Disord. 23, 204–211. doi: 10.1016/j.janxdis.2008.07.001
Tallis, F., Davey, G. C. L., and Bond, A. (1994). “The worry domains questionnaire” in Worrying: Perspectives on Theory, Assessment and Treatment. eds. G. C. L. Davey and F. Tallis (New York: John Wiley & Sons), 285–297.
Tan, H. J., Marks, L. S., Hoyt, M. A., Kwan, L., Filson, C. P., Macairan, M., et al. (2016). The relationship between intolerance of uncertainty and anxiety in men on active surveillance for prostate cancer. J. Urol. 195, 1724–1730. doi: 10.1016/j.juro.2016.01.108
Utzon-Frank, N., Breinegaard, N., Bertelsen, M., Borritz, M., Eller, N. H., Nordentott, M., et al. (2014). Occurrence of delayed-onset post-traumatic stress disorder: a systematic review and meta-analysis of prospective studies. Scand. J. Work Environ. Health 40, 215–229. doi: 10.5271/sjweh.3420
Van Oers, H. (2019). Aspects of post-traumatic stress disorder symptomatology in patients with breast cancer: a review of prevalence, risk and mediating factors. World Sci. News 120, 266–274.
Vin-Raviv, N., Hillyer, G. C., Hershman, D. L., Galea, S., Leoce, N., Bovbjerg, D. H., et al. (2013). Racial disparities in post-traumatic stress after diagnosis of localized breast cancer: the BQUAL study. J. Natl. Cancer Inst. 105, 563–572. doi: 10.1093/jnci/djt024
Voigt, V.. (2016). Cognitive Impairment and Posttraumatic Stress in Breast Cancer Patients during the First Year after Diagnosis. PhD Thesis. Munich: Ludwig-Maximilian University.
Weiss, D. S., and Marmar, C. R. (1997). “The impact of event scale–revised” in Assessing Psychological Trauma and PTSD. eds. J. P. Wilson and T. M. Keane (New York: Guilford Press), 399–411.
WHO. (2021). [Homepage on the Internet]. Breast Cancer. Available at: https://www.who.int/news-room/fact-sheets/detail/breast-cancer. (Accessed March 26, 2021).
Keywords: breast cancer, intolerance of uncertainty, worry, longitudinal study, psychological assessment
Citation: Shams M, Pardini S, Del Bianco P, Calabrese C, De Salvo GL and Novara C (2023) The predictive role of intolerance of uncertainty and trait of worry in breast cancer patients: A prospective, observational, single-center clinical study. Front. Psychol. 14:1092060. doi: 10.3389/fpsyg.2023.1092060
Received: 07 November 2022; Accepted: 30 March 2023;
Published: 17 April 2023.
Edited by:
Andreas Dinkel, Technical University of Munich, GermanyReviewed by:
Jan Christopher Cwik, University of Cologne, GermanyCopyright © 2023 Shams, Pardini, Del Bianco, Calabrese, De Salvo and Novara. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Susanna Pardini, c3VzYW5uYS5wYXJkaW5pQHBoZC51bmlwZC5pdA==
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.