- 1Department of Social and Behavioural Sciences, City University of Hong Kong, Kowloon, Hong Kong SAR, China
- 2The Jockey Club School of Public Health and Primary Care, The Chinese University of Hong Kong, Shatin, Hong Kong SAR, China
- 3School of Health and Wellbeing, University of Bolton, Bolton, United Kingdom
- 4Centre for Mental Health and Society, Bangor University, Bangor, United Kingdom
- 5Felizberta Lo Padilla Tong School of Social Sciences, Caritas Institute of Higher Education, Tseung Kwan O, New Territories, Hong Kong SAR, China
- 6Caritas Institute of Higher Education, Tseung Kwan O, New Territories, Hong Kong SAR, China
Introduction: Existing caregiver assessment tools were long criticized for focusing on the needs and burden while neglecting the importance of the resources. The current study aimed to develop a multidimensional and time-effective assessment tool that measures both needs and resources of non-paid family caregivers of older adults for screening and service-matching purposes.
Methods: Items of the Caregiver Needs and Resources Assessment (CNRA) were developed from extensive literature reviews and focus group interviews of family caregivers and social workers in the field. In addition, we collected 317 valid responses from family caregivers of older adults from local non-government organizations in examining the psychometric properties of the CNRA.
Results: The results revealed a 12-factor structure that fitted nicely into the conceptual frame of needs and resources domains. Need factors were positively associated with mental health symptoms, while resource factors were positively associated with peace in mind, meaning-making, and personal gain measures. The 36-item CNRA revealed good internal reliability and convergent validity.
Discussion: The CNRA has the potential to be used as a compact yet balanced assessment tool for understanding both the needs and resources of caregivers for human service professionals.
Introduction
The declining global fertility rate and extended longevity have significant implications for the healthcare systems and the support of family caregivers. In the year 2019’s global forecast, the number of people aged 65 years or over would be doubled from 703 billion in 2019 to 1.5 billion in 2050, and the proportion of older people would be up from one in 11 in 2019 to one in six people by 2050 (United Nations, Department of Economic and Social Affairs, and Population Division, 2020). Global aging goes with the increase in healthcare needs and costs of society, and a substantial growth conjecture is expected in the spending on long-term services and supports (Anastos-Wallen et al., 2020). Although caregiving by professionals is increasing in proportion to advancements in social and health services, a considerable amount of caregiving is still delivered by family members in high-, middle-, and low-income countries (Pandian et al., 2016; Hinton et al., 2019). Caregiving at home was deemed preferable by older adults for staying in their familiar living environment (Chui, 2008) and possibly reducing the probability of nursing home entry (Charles and Sevak, 2005). Family caregivers play the central position in the long-term care, and medical decision-making of their beloved family members with functional limitations in the self-care (Feinberg and Houser, 2012; Abreu et al., 2020), yet the demands for family caregivers of older family members are heavier than ever. Not only because the capacity to care for the older family members declines with the decreased household sizes and the increase in women’s employment rate, but our health system also relies more on family caregivers to provide care to older adults during crises such as the 2019 Coronavirus Disease (COVID-19) pandemic (Au Yeung et al., 2020; Kent et al., 2020). There is restricted access or curtailment in health and community services under the social distancing measures, which substantially disrupt the daily caregiving routine of the family caregivers (Lum et al., 2020; Chan et al., 2021), bring frustration to help-seeking (Kent et al., 2020), and impede access to medication (Wong and Cheung, 2020). Handling the household chores also brings fear of infection to the caregivers and the possible transmission to the care recipients (Kent et al., 2020; Lightfoot et al., 2021). Informal help availability and social support are reduced, making the family caregivers solely responsible for the caregiving tasks (Lightfoot et al., 2021; Savla et al., 2021). The increased use of online communication and activities may require family members’ assistance for older adults with low digital literacy (Kent et al., 2020). In the face of the growth of the aging population worldwide and the surge in caregiving demands amid the pandemic, we need a simple yet embracive triage tool in profiling the needs and resources of the caregivers to facilitate timely allocation of hit-the-spot support and interventions to the family caregivers in healthcare and community settings. Therefore, the aim of the project was to develop the Caregiver Needs and Resources Assessment (CNRA), a quick profiling tool that can help human service professionals, including social workers, medical and paramedical professionals, to understand caregivers’ situations and discuss the possible resources that can remediate their disrupted routines in the triage stage.
In the initial stage of case management, it is vital to distinguish between individuals who cannot cope with their current situation and thus assistance is urgently needed, and those who can overcome the caregiving burden on their own for more effective and efficient resource allocation (Jones and Griffiths, 2007). Being simple and easy are important attributes of an effective assessment tool for better acceptance and dissemination in self-administration and community setting (e.g., Chung et al., 2015). The development of CNRA was intended to be multi-faceted that enable the caregivers and human service professionals to get a quick initial idea about the unmet needs and resources possessed by the caregivers for further evaluation and referral of services. The human service professionals can, therefore, discuss with the caregivers for the services that best suit the caregivers’ situation among the available service options (Feinberg and Ellano, 2000; Kelly et al., 2013).
In the migration from a problem-solving and disease-based approach to strengths-based social work practice, the emphasis changes from remediating the immediate instrumental problems of the individuals to discovering and realizing the resources of the individuals from their environment as a resilient strategy during adversity (Guo and Tsui, 2010). An accurate understanding of the caregivers’ needs and resources is essential for a tailored intervention plan that can maximize their resources to reduce their burden, facilitate sustainable care for frail older adults, build their care capacity, and improve their quality of life.
One commonly used assessment tool among the non-government organizations (NGOs) that provide caregiver supporting services is the Zarit Burden Interview (ZBI; Zarit et al., 1980). This inventory has been adopted as an outcome measure in intervention studies (Tremont et al., 2013; e.g. Hashimoto et al., 2017) or in surveys (e.g., Cheng et al., 2013; Kwok et al., 2013) to evaluate the level of burden among caregivers. However, ZBI received critiques, including its “strain” focus and neglecting the positive impacts of caregiving (Chou et al., 2003) and the unstable and unreplicable factor structure in different caregiver samples (3-factor structure in Knight et al., 2000 and Springate and Tremont, 2014; 4-factor structure in Cheng et al., 2014; 5-factor structure in Lu et al., 2009). Other available assessment tools, for example, the Caregiver Self-Assessment Questionnaire (Epstein-Lubow et al., 2010), Behavioral and Instrumental Stressors in Dementia (Keady and Nolan, 1996), Comprehensive Needs Assessment Tool for Cancer Caregivers (Shin et al., 2011), the Caregiver Need Assessment (Moroni et al., 2008), and the Multidimensional Caregiver Burden Inventory (Novak and Guest, 1989) have been developed in the sake of measuring the needs of family caregivers in general or with care recipients of specific types of illness or limitations. Still, these tools fall short in capturing the resources possessed by the caregivers. This “pathological” view in assessing caregiver needs obscures the possibility of seeing how accepting the responsibility as the caregiver can facilitate the establishment of purpose, stimulation of personal growth, and cultivation of wisdom (Roth et al., 2015; Borson, 2021).
To capture the modifiable social contingencies potentially possessed by the caregivers that can shield the adversities in caregiving, the development of the CNRA was grounded on two dominant theoretical frameworks in the caregiving literature, namely, the Stress Process Model (SPM; Pearlin et al., 1990) and the Dual Process Model (DPM; Stroebe and Schut, 1999, 2001). SPM views caregiving stress as the product of the caregiving contexts, primary stressors (i.e., direct hardships anchored in caregiving), and secondary stressors (i.e., strains indirectly related to caregiving) that one is exposed to. Coping and resources, such as psychosocial maturity, social support, and better self-esteem (e.g., Benson, 2014), are mediators that can intervene in multiple points of the stress process, and the impact on caregivers vary as the mix of the stressors and resources vary considerably among caregivers. Under the tenet of SPM, caregiving stressors can be categorized into primary stressors stemming directly from the conditions and behaviors of the care recipients and secondary stressors generated by these conditions and behaviors. Two categories of secondary stressors are described: role strains (family conflict, job-caregiving conflict, economic problems, and construction of social life) and intrapsychic strains (self-esteem, mastery, loss of self, role captivity, competence, and gain). The SPM provides a valuable framework in identifying modifiable social factors in stressful encounters (Turner, 2009).
DPM describes bereavement as a dynamic process in the bereaved individual alternating between loss-orientation (dealing with the loss experience) and restoration-orientation (dealing with the arrangements for reorganizing one’s life without the deceased person). It suggests that a unique combination of stressors and resources, either contextual, social, or personal, would contribute to the varying appraisal of the stressful life event and its mental and physical health consequences. Although DPM pertains to the bereavement process, it echoes with SPM, emphasizing the interplay between stressors and resources in stressful life events under the stress and coping paradigm (Boerner et al., 2004).
Inspired by these models and given the inadequacy of the assessment tool in practice, we aimed to develop the Caregiver Needs and Resources Assessment (CNRA) which will facilitate social workers and healthcare professionals in the case management of caregivers such as triage, screening and service matching. In assessing its construct validity, we examined its relationship with common mental health and general well-being indicators, including caregiver quality of life, life satisfaction, and psychological distress.
Methodology
Item development and pilot test
In the initial phase of scale items development, we administered a semi-structured interview to four family caregivers and eight social workers from the four collaborating NGOs. The family caregivers interviewed were taking care of their frail older family members and were service users of the four collaborating NGOs. We asked questions tapped on their daily caregiving routines, major events of taking care of frail older adults, and their needs, resources, and coping strategies in caregiving in the semi-structured interview. Domains of needs and resources included psychological, physiological, social, environmental and others, and we openly asked about the sub-domains and other major domains that were relevant and important. We also consulted the social workers on the current practice of needs assessment in the interview. All interviews were audio-recorded with the participants’ consent.
Several themes emerged from the qualitative data and echoed with the literature regarding the needs and resources in caregiving. Interviewees brought up their psychological burden, including the sense of loss of self (Skaff and Pearlin, 1992; Noonan and Tennstedt, 1997), tiredness (Aarsland et al., 1999), the emergence of anxiety and depression symptoms (Pagel et al., 1985; Denno et al., 2013), and helplessness (Pagel et al., 1985). Various physiological symptoms were reported, including sleep problems, loss of appetite, and other health problems (van Wijngaarden et al., 2004; McCurry et al., 2007). Role conflicts with their family members, colleagues, and care recipients (Kramer and Kipnis, 1995; Stephens et al., 2001), and loss of social life (Skaff and Pearlin, 1992; Galvin et al., 2010), were common complaints among caregivers. Themes related to resources pertained spiritual and religious belief, coping strategies, meaning-making (Noonan and Tennstedt, 1997), resilience, moral commitment (Chang et al., 1998; Stuckey, 2001), the role recognition as a caregiver (Noonan and Tennstedt, 1997), support from professionals such as social workers, therapists (Reinhard, 1994; Sabella and Suchan, 2019) and community resources, support and recognition from other family members (Lidell, 2002), the closeness with the care recipient (Fauth et al., 2012; Rattinger et al., 2016), and healthy lifestyle (Mochari-Greenberger and Mosca, 2012).
Alongside these themes extracted in the qualitative analyses, we also extensively reviewed measurement tools in the field pertaining to the resources and needs of the caregivers, including the Multidimensional Caregiver Burden Inventory (Novak and Guest, 1989), Modified Caregiver Strain Index (Thornton and Travis, 2003), Work–Family Conflict Scale (Haslam et al., 2015), WHOQOL Spirituality, Religiousness and Personal Beliefs (SRPB) Field-Test Instrument (WHO, 2002), Perceived Social Support for Caregivers and Social Conflict scales (Goodman, 1991), and the measures assessing caregiving stress used in the study of Pearlin et al. (1990). We compiled an exhaustive list of caregiver needs and resources items. The research team has generated 133 questions based on the resources and needs dimensions. We presented the preliminary items to 14 family care and gerontology experts, including 10 social workers involved in caregiving support services and 4 researchers. They then commented on the provisional list of items regarding their relevance to the dimensions, uniqueness, and comprehensibility of the wordings. After the consultation, the provisional CNRA evolved into a 42-item version. We used a 5-point Likert scale (1 = never, 2 = occasional, 3 = neutral, 4 = often, 5 = most of the time) for the caregivers in evaluating their situation referring to the past month. We administered the 42-item version of CNRA to a group of 10 adult caregivers to collect their feedback regarding the potential problems in the administration, including the comprehensibility and phrasing of the items and the sequence of the items. We polished the items and kept the 42 items for the subsequent field test following the pilot test.
Field testing
Ethical approval for human research was obtained from the Human Subject Ethics Sub-Committee of the City University of Hong Kong (Reference Number: 3-7-201905-01). Caregivers of frail older adults were recruited from four government-funded local community centers for older adults between August and December 2019. The four local community centers for older adults were located in the three main regions of Hong Kong (namely the Hong Kong Island, Kowloon, and the New Territories) and served needed caregivers of different socioeconomic statuses. Nonpaid caregivers who were taking care of a frail older adult (with at least one ADL or IADL difficulty) in their families and were aged 18 or above were eligible to participate. Paid formal caregivers were excluded from the study. Written consent was obtained from each participant at the beginning of the study, and the purpose and procedure of the study were explained. They were then asked to complete the survey. We interviewed illiterate participants with trained interviewers to complete the survey. The trained social workers interviewed the illiterate participants using the translated script provided by the research team to ensure that translated verbal Chinese in the script carried the equivalent semantic meaning as written Chinese on the questionnaire. Participation in this study was entirely voluntary, and a small financial compensation of HKD100 was provided to each participant after they had completed the questionnaire for their time and effort in participation. Service users of the participating NGOs were invited to join the study. We determined the target sample size based on the subject-to-variable ratios of 5:1 (Hatcher, 1994) to 10:1 (Nunnally, 1978), which required a sample size between 210 to 420 for our 42-item CNRA.
Procedures and measures
Considering the coverage of needs and resources of caregiving in the CNRA items, participants completed measures of caregiving burden, positive aspects of caregiving, general health status, personal gain, and peace of mind to test the construct validity of the scale. Considering our inclusion of both needs and resources related items in the pool, we expected the items to cluster into need-and resource-related factors. In examining the convergent validity of the CNRA, we used the extensively adopted caregiving burden scales, ZBI and MCBI, to verify the needs factors and the measurement of perceived resources for verifying the resource factors. We expected the need-related factors to be associated with general health and mental health measures in terms of predictive validity. In contrast, resource-related factors would be related to meaning-making and positive aspects of caregiving. Differences in the needs and resources factors were examined across demographic groups, including sex, age, relationship with the care recipients, and job status.
Caregiving burden
The perceived caregiving burden was assessed by the 12-item Chinese version of Zarit Burden Interview (ZBI; Tang et al., 2016) and the Multidimensional Caregiver Burden Inventory (MCBI; Novak and Guest, 1989). For ZBI, participants were asked to rate their agreement with each statement on a five-point Likert scale (1 = never, 5 = always). Sample items include “Do you feel that because of the time you spend with your relative that you do not have enough time for yourself?” and “Do you feel stressed between caring for your relative and trying to meet other responsibilities for your family or work?” A higher score indicates a higher perceived burden. The Cronbach’s alpha (α) of ZBI in our sample was 0.858.
The MCBI comprises 24 items covering five dimensions of burden, including time-dependence, developmental, physical, social, and emotional burdens. The perceived burden items were measured using a five-point Likert scale (1 = never; 5 = always). Sample items include “My care receiver needs my help to perform many daily tasks” and “I’m physically tired.” A higher score indicates a higher perceived burden. The Cronbach’s α of MCBI in our sample was 0.927.
Psychological distress
The caregivers’ psychological distress was assessed using the 12-item General Health Questionnaire (GHQ-12, Goldberg et al., 1997). Sample items of GHQ-12 include “Been losing confidence in self” and “Able to concentrate.” The participants rated the statement on a 5-point Likert scale ranging from 1 to 5 (instead of a 4-point Likert scale ranging from 0 to 3 as in the original GHQ-12 to maintain the consistency of scale point used in the survey). Higher GHQ-12 scores indicate more psychological distress. It had good reliability in our current sample (Cronbach’s α = 0.867).
General health status
The health status of the caregiver was evaluated by the Chinese version of the five-item of EuroQol-five dimensions (EQ-5D-5L; Cheung et al., 2016), covering five dimensions, namely, mobility, self-care, usual activities, pain and discomfort, and anxiety and depression. The participants were asked to rate their agreement with each statement using a five-point Likert scale (1 = no problem; 5 = severe problem) for all five items. To compute a single score in indicating the general health status of the caregivers, we adopted the method suggested by Devlin and Krabbe (2013) and Oppe et al. (2014), with scores of 1 and 0 indicating full health and death, respectively, and negative scores represent health status that is worse than death. We used the Hong Kong value set in computing the score (Wong et al., 2018), with the possible value ranging from 1 (for the health state 11,111) and-0.8637 (for the health state 55,555). The Cronbach’s α of ΕQ-5D-5L was 0.700.
Positive aspects of caregiving
The perceived positive aspects of caregiving were assessed by the Chinese version of the 11-item Positive Aspects of Caregiving Scale (PACS; Boerner et al., 2004; Lou et al., 2015). PACS (α = 0.924) comprises two factors, namely, enriching life (PACS_E; α = 0.894) and affirming self (PACS_A; α = 0.884). The participants were asked to rate their agreement on each statement on a five-point Likert scale (1 = strongly disagree; 5 = strongly agree). Samples items include “Feel strong and confident” and “Enable me to learn new skills.” A higher score of PACS indicates higher perceived benefits of engaging in caregiving.
Personal gain
The four-item Personal Gain Scale (PGS; Pearlin et al., 1990; Skaff and Pearlin, 1992) was employed to assess the caregiver’s personal growth and awareness of their inner strengths from the caregiving experience. The participants were asked to rate their agreement with each statement on a five-point Likert scale (1 = very much; 5 = not at all, instead of a four-point Likert scale in the original measure to keep the rating scale consistency in the survey) about inner strengths, self-confidence, growth, and new learning. Sample items include “Become more self-confident” and “Learned to do thing you did not do before.” A higher score represents more personal gain as a result of caregiving. The Cronbach’s α of PGS was 0.893.
Personal resources
We modified the 35-item Retirement Resources Inventory (RRI, Leung and Earl, 2012) to measure the perceived resources of caregivers. Participants rated the extent of each type of resource they had for assisting their caregiving tasks on a 5-point Likert scale from 1 to 5. Sample items of RRI included “I possess income to support my/my family living expenses” and “I would consider interactions with friends (in general) to be supportive.” A higher score represents higher perceived resources in the caregiver. The RRI revealed good reliability in our sample, with Cronbach’s α at 0.834.
Peace of mind
The perceived peace of mind of the caregiver was evaluated by the 7-item Peace of Mind scale (PoM; Lee et al., 2013; Yu et al., 2020). Participants were asked to rate their agreement with each statement on a 5-point Likert scale (1 = not at all; 5 = all the time). Sample items include “I feel content and comfortable with myself in daily life” and “My lifestyle gives me feelings of peace and stability.” The Cronbach’s α of PoM was 0.865.
Statistical analyses
A factor analysis was conducted using the principal axis factoring with oblimin rotation (as we expected that resulting factors would be correlated). A parallel analysis (Horn, 1965) was conducted on the 42 initial items by comparing the obtained eigenvalues from the factor analysis with the eigenvalues of a randomly generated dataset to determine the number of factors to be retained. Scree plot, Kaiser criterion (with an eigenvalue larger than 1.0), and the factor solution’s interpretability were also used as the aids of our judgment. The cutoff of the primary factor loading was set at 0.30 or above (Costello and Osborne, 2005), while the cutoff of the cross-loading was set at 0.30 or lower (Howard, 2016).
Results
Participants
We recruited 365 family caregivers of older adults. After discarding cases with incomplete responses of the CNRA, 317 participants were retained, with their mean age at 65.81 years (SD = 12.79, range = 27–95), and 79.18% being female. On average, they have been taking care of an older family member for 8.52 years (SD = 9.87, range = 0–65). Most of them were either spouse (45.89%) or child (46.52%) of the care recipients. Half of them (55.21%) have completed secondary or above education. There were 16.83% of the participants reported having a full-time job. Demographic information of the caregivers and care recipients are shown in Supplementary Tables 1, 2, respectively.
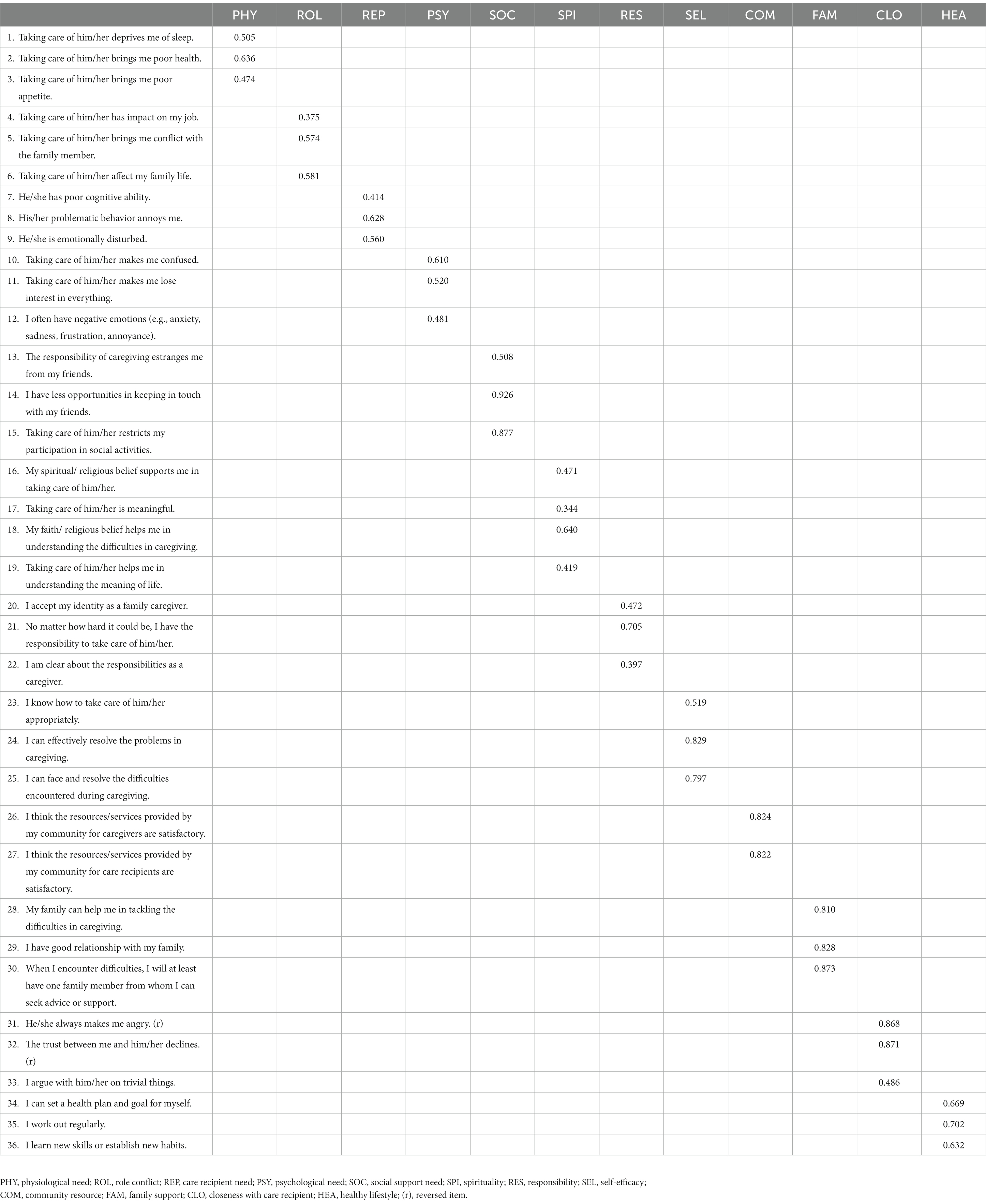
Factor structure
The results of the parallel analysis suggested a factor solution of 12 factors, which explained 59.84% of the total variance (by calculating the mean of communalities). We dropped six items for their weak primary factor loading (less than 0.30) or strong cross-loading (greater than 0.30). The second round of parallel analysis and principal axis factoring was conducted on the remaining 36 items. Parallel analysis again suggested a 12-factor solution. The factor structure fit our data well (CFI = 0.912, AGFI = 0.945, RMSEA = 0.054, SRMR = 0.058). The factor loadings of the 36 items of CNRA are presented in Table 1. The 12 factors can be semantically divided into two dimensions, namely, needs and resources. The needs dimension included physiological needs (3 items), role conflict (3 items), care recipient’s needs (3 items), psychological needs (3 items), and social support needs (3 items). The resources dimension consisted of seven factors, labeled as spirituality (4 items), self-efficacy (3 items), responsibility and commitment as a caregiver (3 items), community resources (2 items), family support (3 items), healthy lifestyle (3 items), and closeness with care recipient (3 items). Table 2 presents the descriptive statistics and the correlations of the 12 factors of the CNRA. The CNRA subscales exhibited reliabilities, with Cronbach’s alpha ranging from 0.705 to 0.888.
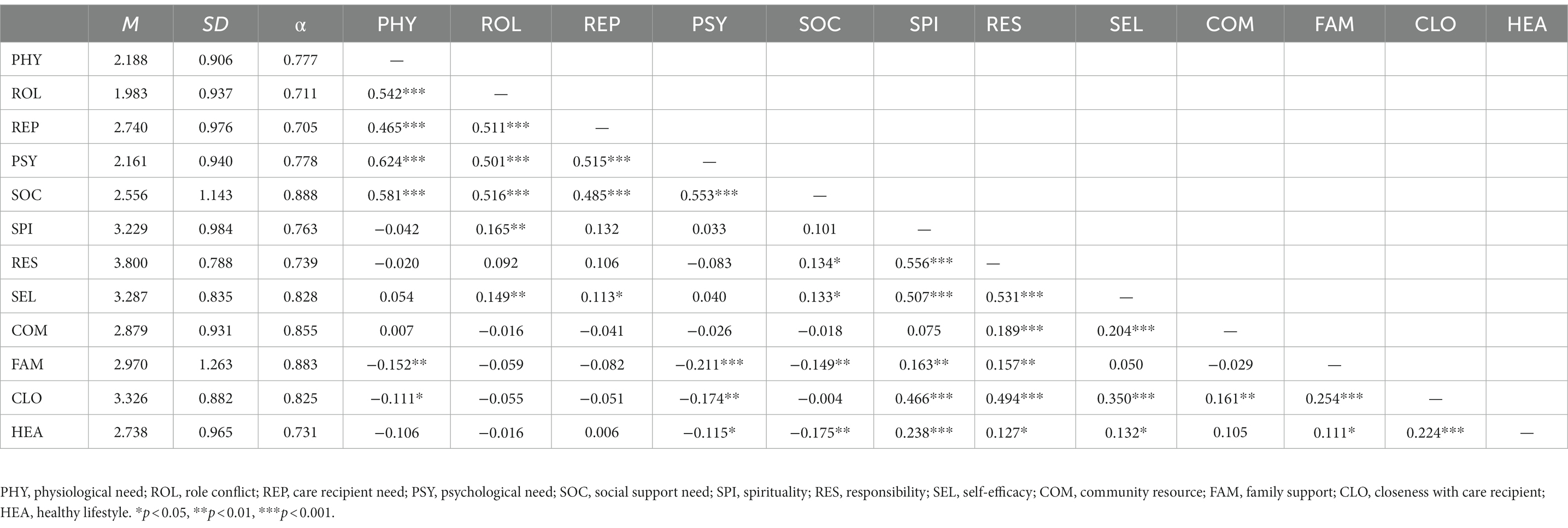
Table 2. Descriptive statistics of the 12 factors of the caregiver needs and resources assessment (N = 317).
Convergent and predictive validity
The correlations between the CNRA factors and validation measures were shown in Table 3. The needs factors (i.e., physiological needs, role conflict, care recipient needs, psychological needs, and social needs) were positively correlated with caregiving burden (measured by ZBI, rs = 0.591–0.704, ps < 0.001; measured by MCBI, rs = 0.559–0.729, ps < 0.001), psychological distress (measured by GHQ, rs = 0.356–0.686, ps < 0.001), and negatively with general health status (measured by EQ5D, rs = −0.218 – -0.388, ps < 0.01). On the other hand, resources factors, including spirituality, self-efficacy, responsibility, community resources, family support, and healthy lifestyle, closeness with care recipients were found associating with peace of mind (rs = 0.185–0.381, ps < 0.001), affirming self (measured by PACS_A, rs = 0.122–0.372, ps < 0.05), enriching life (measured by PACS_E, rs = 0.155–0.536, ps < 0.01), positive gain (measured by PGS, rs = 0.146–0.498, ps < 0.01), and perceived resources (measured by RRI, rs = 0.117–0.416, ps < 0.05).
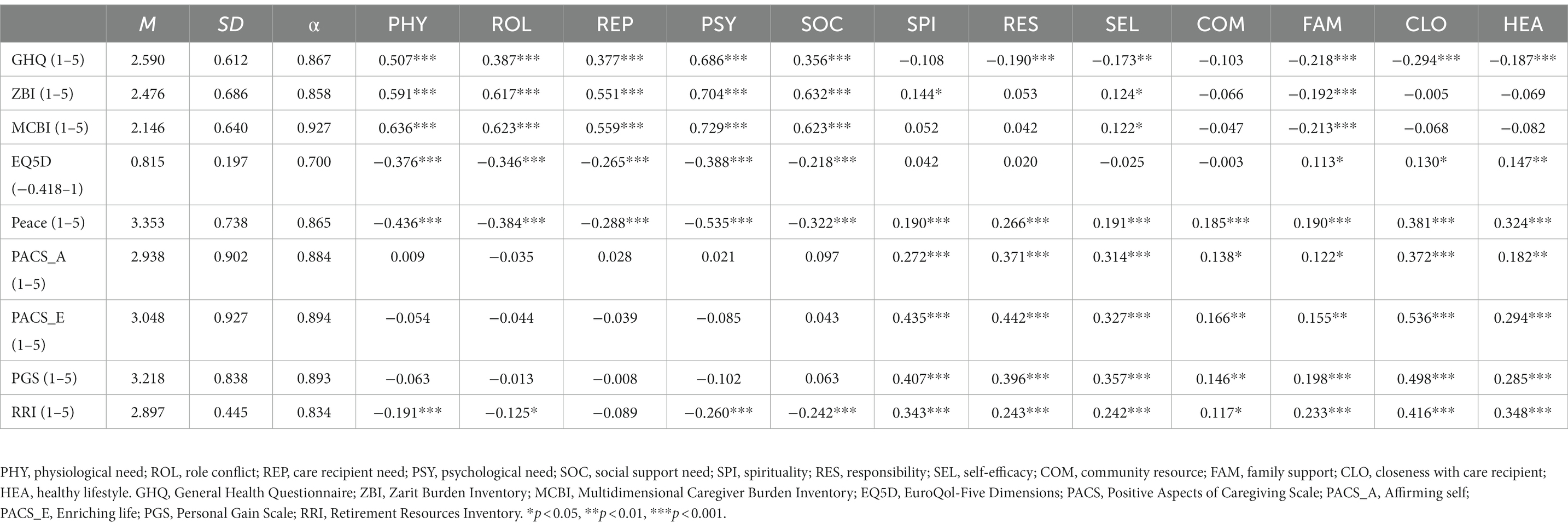
Table 3. Correlations between Caregiver Need Assessment constructs, burden and well-being measures (N = 317).
Demographic differences in caregiver’s needs and resources
There were demographic differences in caregivers’ needs and resources measured by the CNRA (Table 4). Gender differences were revealed in all of the need measures, and female caregivers reported higher needs in all domains than male caregivers. Caregivers of age 65 or above reported less role conflict, spiritual resources, and family support, but more community resources and a healthy lifestyle. Similarly, spouse caregivers reported less role conflict, spiritual resources, and family support, but higher physiological and psychological needs and more community resources. Caregivers who had full-time jobs reported less social support and a less healthy lifestyle.
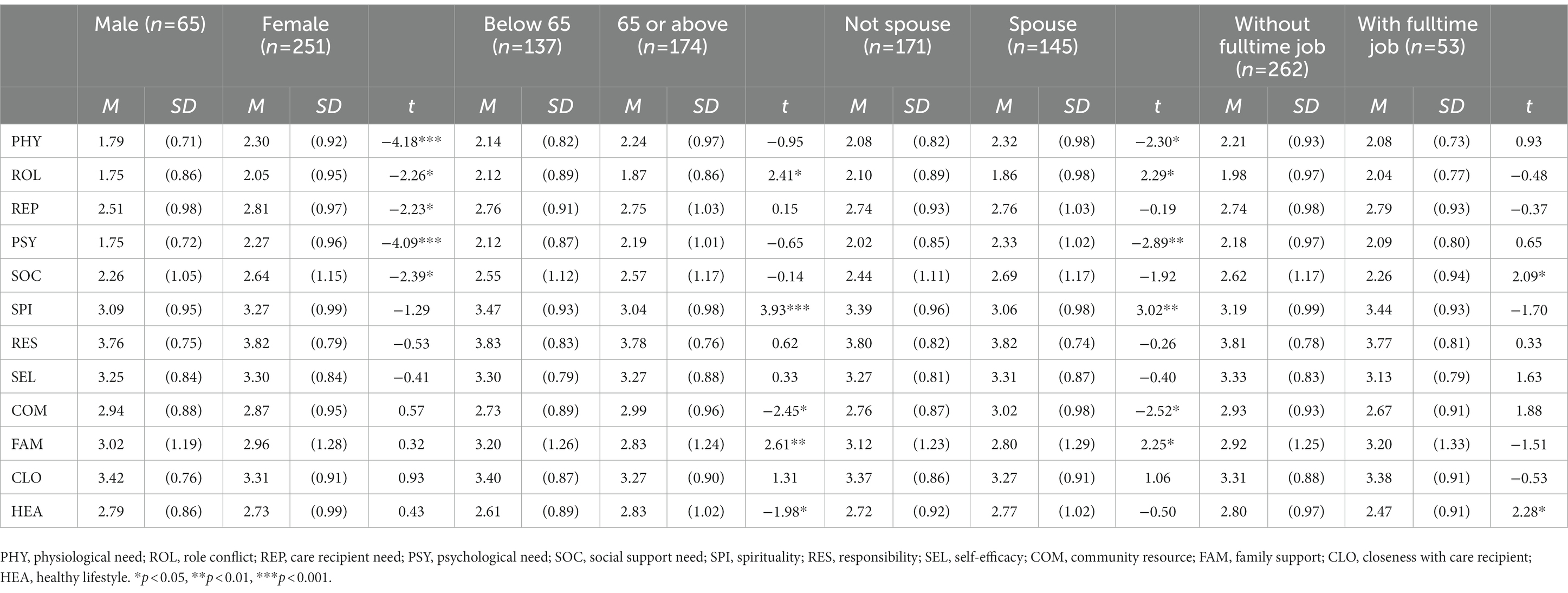
Table 4. Mean differences in the caregivers’ needs and resources across demographic groups (N = 317).
Discussion
The current study developed and examined the psychometric properties of a caregiver needs and resources assessment, an indigenously developed screening tool tapping the needs and resources of caregivers who provide support and care to their older adult family members. In our field testing, the exploratory factor analysis revealed a 12-factor model for the 36 items retained in the CNRA. The 12 factors can be semantically categorized into needs factors and resources factors. In examining the convergent validity, all needs factors positively correlated with more pathological or negative constructs, including mental health symptoms and caregiving burden, and negatively correlated with general health. All resources factors are positively associated with positive constructs, including meaning-making, peace of mind, and perceived resources.
The five needs factors tapped into the stressors or burden in different domains, including the burden on the caregivers’ health (physiological needs; e.g., Vitaliano et al., 2003), deprivation of social life (social needs; e.g., Palamaro Munsell et al., 2012), psychological burden (psychological needs; e.g., Baillie et al., 1988; González-Salvador et al., 1999), conflicts between different roles (role conflict; e.g., Kramer and Kipnis, 1995; Gordon et al., 2012), and the functional deterioration of the care recipients (Ornstein and Gaugler, 2012; care recipient needs; e.g., Lin, 2020). These factors reflect the stressors of the caregivers on different facets that compose the needs to be fulfilled or addressed, which is often the main focus of the caregiver assessment tools in the field (e.g., ZBI and MCBI). The association between caregiving burden and mental and physical health was well discussed in the literature (e.g., Chang et al., 2010; de Oliveira et al., 2015; Del-Pino-Casado et al., 2019), especially when the care recipients are in poor functional capacity (e.g., Morimoto, 2003). Our five factors on the needs dimension have revealed good convergent validity for their positive associations with ZBI and MCBI. These need factors also revealed good predictive validity for positive associations with mental health symptoms and negative associations with general health status.
As advocated in SPM and DPM, integrated consideration of both the needs or burden experienced and the resources possessed by the caregivers are needed to understand the caregivers’ appraisal of their stressful events (Pearlin et al., 1990; Stroebe and Schut, 1999). More studies stress the importance of considering the positive aspects and resources in the caregiving (Kramer and Kipnis, 1995; Boerner et al., 2004; Yu et al., 2018). Preserving and enhancing the positive aspects and resources of the caregivers can serve to provide protective factors to the caregivers in the face of stress (Yu et al., 2018). It is also suggested that the positive aspects and resources during the caregiving process could enhance the adaptation after the loss of care recipients (Boerner et al., 2004).
In our CNRA, we have seven factors related to the resources domain, including the spirituality and religious belief that provide meaning and substance in life and the way to handle loss and suffering (spirituality; e.g., Chang et al., 1998; Puchalski and Sandoval, 2003; Puchalski, 2012), self-efficacy or perceived capacity in carrying out caregiving tasks (self-efficacy; e.g., Merluzzi et al., 2011; Cheng et al., 2014; Durmaz and Okanlı, 2014; Yildiz et al., 2017), the commitment and perceived responsibility in taking care of the their frail family members (responsibility; e.g., Häggström et al., 2010; Qiu et al., 2018), community services and resources (community resources; e.g., Yamashita and Amagai, 2008; Weber et al., 2011), the instrumental and emotional support from other family members (family support; e.g., Lidell, 2002; Fauth et al., 2012; Feng and Magen, 2016), the awareness in maintaining good health and wellness (healthy lifestyle; e.g., Beesley et al., 2011), as well as the emotional closeness with the care recipients (closeness with care recipients; e.g., Lyonette and Yardley, 2003). The resources factors revealed good convergent validity in their positive associations with RRI and PACS. They also showed good predictive validity in positively associating with peace in mind and perceived gain.
The demographic analyses revealed important caregivers’ needs and resources between demographic groups. Specifically, male caregivers reported fewer needs than female caregivers. This evidence again supported the notion of the gendered nature of caregiving (Xiong et al., 2020). For example, in comparison with female caregivers, male caregivers are less likely to consider it a family or filial obligation to take care of their frail family members As such, they are more willing to seek help, share the caregiving burden with others, and engage in activities that provide respite from the caregiving burden (Brown and Chen, 2008; Xiong et al., 2020). Interestingly, younger and non-spouse (who were usually the child) caregivers reported more role conflicts, more spiritual resources, more family support but fewer community resources. In terms of resources, younger caregivers are higher in digital literacy and more accessible to online resources. This is particularly important during the COVID-19 pandemic to look for spiritual resources and connect with the family members online. In Hong Kong, since resources for caregivers are offered mainly through the services of older people in social services organizations, the services available may not fit the needs of younger and working caregivers or be able to reach them. Caregivers with full-time jobs reported less social support needs and a less healthy lifestyle. A full-time job could provide social support from the colleagues and supervisors (Boumans and Dorant, 2021). Yet, dual responsibilities dealing with the job and caregiving tasks may bring a less healthy lifestyle (Bainbridge et al., 2021).
To our best knowledge, CNRA is the first assessment tool that provides a one-stop solution in assessing and differentiating caregiver needs and resources with good psychometric properties. We believe the development of the CNRA would have several important practical implications. First, the extensive coverage of caregiving needs and resources would be useful in a case management setting as a quick triage tool to overview the profile of needs and resources of a particular caregiver. It could serve as a reminder for both the case managers and the clients not to overlook a balanced view of both needs and resources that the clients carry. Second, the CNRA can facilitate the prioritization and tailor-making of the services and intervention plans that best suit the situation of a particular caregiver. With the easily interpretable scores of CNRA on hand, the case managers can discuss with clients their needs and resources in working on the preferred case management plans and objectives. Third, this scale can be applied in the social work training module for caregiver needs and resources assessment, as there is no standardized assessment tool in the field. Using the CRNA makes it possible to unify the assessment quality for novice and experienced social workers. CNRA also offers an embracive profile of caregiving needs and resources that takes around an hour or less for the initial triage interview. Timely and accurate assessment of the needs and resources of caregivers can make quick allocation of services and development of intervention plans possible and, in turn, lower their caregiving burden as quickly as possible. Theoretically, CNRA could serve as a handy measurement tool in verifying the relationship between caregivers’ needs and resources in future studies.
We admitted there were several limitations in the current findings. First, because the sample was recruited from the caregivers who were using services in the collaborating NGOs in Hong Kong, further studies would be needed in other samples of caregivers who are not using NGOs services, as well as samples from different cultures, to examine the stability of the factor structure revealed in the current study, Second, the validation of the CNRA relied on self-report measures. The use of more objective outcome measures can better verify the scale’s construct validity. Third, the cross-sectional design did not enable us to draw a strong conclusion about the predictive validity of the factors. The use of longitudinal design would be helpful to see if the needs and resources factors can predict mental health symptoms and meaning-making in the caregiving process at a later time in future studies. Despite the limitations, we believe the CNRA would be a helpful tool for the case management of caregivers in different service settings.
The development of the CNRA serves to respond to the paradigm shift from a disease-based and problem-solving approach to a strength-and resilience-based approach to managing caregiving stress. The CNRA, as a triage tool, provides a balanced and embracive view of both needs and resources in handling caregiving stress, which would benefit both the clients and workers in liaising the development of a tailored-made intervention plan.
Author’s note
The Chinese version of CNRA was validated in this study. The English version presented in the article was for demonstration only. The Chinese items and the scoring system are presented in Supplementary Table 3. This scale can be used for non-commercial research and educational purposes without seeking written permission.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by Human Subject Ethics Sub-Committee of City University of Hong Kong (Reference Number: 3-7-201905-01). The patients/participants provided their written informed consent to participate in this study.
Author contributions
K-KL, DY, MC, and AC conceptualized the study, developed the methodology, and obtained funding support. BL managed data collection. K-KL, CL, EC, and BL analyzed and interpreted the data. TWL supervised the execution of the project. CL wrote the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Simon K.Y. Lee Foundation.
Acknowledgments
The authors would like to thank all participants in this study. The authors would also like to express the greatest appreciation to Simon K.Y. Lee Foundation, Lui Shu Ho Jeffrey, and Chan Hau Lung for their support in the operation of the project and the four local NGOs (Hong Kong Christian Service, S. K. H. Wong Tai Sin District Elderly Community Centre, Methodist Centre, and Baptist Oi Kwan Social Service) for their support in the recruitment of participants.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2023.1063440/full#supplementary-material
References
Aarsland, D., Larsen, J. P., Karlsen, K., Lim, N. G., and Tandberg, E. (1999). Mental symptoms in Parkinson’s disease are important contributors to caregiver distress. Int. J. Geriatr. Psychiatry 14, 866–874. doi: 10.1002/(SICI)1099-1166(199910)14:10<866::AID-GPS38>3.0.CO;2-Z
Abreu, W., Tolson, D., Jackson, G. A., and Costa, N. (2020). A cross-sectional study of family caregiver burden and psychological distress linked to frailty and functional dependency of a relative with advanced dementia. Dementia 19, 301–318. doi: 10.1177/1471301218773842
Anastos-Wallen, R., Werner, R. M., and Chatterjee, P. (2020). Prevalence of informal caregiving in states participating in the US patient protection and affordable care act balancing incentive program, 2011-2018. JAMA Netw. Open 3:e2025833. doi: 10.1001/jamanetworkopen.2020.25833
Au Yeung, T., Chan, F. H., Chan, T., Kng, C. P., Lee, J. S., Luk, J. K., et al. (2020). COVID-19 and older adults: experience in Hong Kong. Asian J. Gerontol. Geriatr. 15, 54–59. doi: 10.12809/ajgg-2020-424-oa
Baillie, V., Norbeck, J. S., and Barnes, A. (1988). Stress, social support, and psychological distress of family caregivers of the elderly. Nurs. Res. 37, 217–222. doi: 10.1097/00006199-198807000-00009
Bainbridge, H. T. J., Palm, E., and Fong, M. M. (2021). Unpaid family caregiving responsibilities, employee job tasks and work-family conflict: a cross-cultural study. Hum. Resour. Manag. J. 31, 658–674. doi: 10.1111/1748-8583.12333
Beesley, V. L., Price, M. A., and Webb, P. M., Australian Ovarian Cancer Study Group, and Australian Ovarian Cancer Study—Quality of Life Study Investigators (2011). Loss of lifestyle: health behaviour and weight changes after becoming a caregiver of a family member diagnosed with ovarian cancer. Support. Care Cancer 19, 1949–1956. doi: 10.1007/s00520-010-1035-2
Benson, J. E. (2014). Reevaluating the “subjective weathering” hypothesis: subjective aging, coping resources, and the stress process. J. Health Soc. Behav. 55, 73–90. doi: 10.1177/0022146514521214
Boerner, K., Schulz, R., and Horowitz, A. (2004). Positive aspects of caregiving and adaptation to bereavement. Psychol. Aging 19, 668–675. doi: 10.1037/0882-7974.19.4.668
Borson, S. (2021). Assessing caregiver needs. Int. Psychogeriatr. 33, 331–334. doi: 10.1017/S1041610220003877
Boumans, N. P. G., and Dorant, E. (2021). The relationships of job and family demands and job and family resources with family caregivers’ strain. Scand. J. Caring Sci. 35, 567–576. doi: 10.1111/scs.12873
Brown, J., and Chen, S.-L. (2008). Help-seeking patterns of older spousal caregivers of older adults with dementia. Issues Ment. Health Nurs. 29, 839–852. doi: 10.1080/01612840802182854
Chan, C. K., Tang, M. Y., and Lee, M. L. (2021). Delivering social services during the COVID-19 pandemic: the case of older people centers in Hong Kong. J. Soc. Serv. Res. 48, 1–11. doi: 10.1080/01488376.2021.1956670
Chang, H.-Y., Chiou, C.-J., and Chen, N.-S. (2010). Impact of mental health and caregiver burden on family caregivers’ physical health. Arch. Gerontol. Geriatr. 50, 267–271. doi: 10.1016/j.archger.2009.04.006
Chang, B.-H., Noonan, A. E., and Tennstedt, S. L. (1998). The role of religion/spirituality in coping with caregiving for disabled elders. Gerontologist 38, 463–470. doi: 10.1093/geront/38.4.463
Charles, K. K., and Sevak, P. (2005). Can family caregiving substitute for nursing home care? J. Health Econ. 24, 1174–1190. doi: 10.1016/j.jhealeco.2005.05.001
Cheng, S.-T., Kwok, T., and Lam, L. C. W. (2014). Dimensionality of burden in Alzheimer caregivers: confirmatory factor analysis and correlates of the Zarit burden interview. Int. Psychogeriatr. 26, 1455–1463. doi: 10.1017/S104161021400101X
Cheng, S.-T., Lam, L. C. W., and Kwok, T. (2013). Neuropsychiatric symptom clusters of Alzheimer disease in Hong Kong Chinese: correlates with caregiver burden and depression. Am. J. Geriatr. Psychiatry 21, 1029–1037. doi: 10.1016/j.jagp.2013.01.041
Cheung, P. W. H., Wong, C. K. H., Samartzis, D., Luk, K. D. K., Lam, C. L. K., Cheung, K. M. C., et al. (2016). Psychometric validation of the EuroQoL 5-dimension 5-level (EQ-5D-5L) in Chinese patients with adolescent idiopathic scoliosis. Scoliosis Spinal Disord. 11:19. doi: 10.1186/s13013-016-0083-x
Chou, K.-R., Chu, H., Tseng, C.-L., and Lu, R.-B. (2003). The measurement of caregiver burden. J. Med. Sci. Taiwan 23, 73–82.
Chui, E. (2008). Ageing in place in Hong Kong—challenges and opportunities in a capitalist Chinese City. Ageing Int. 32, 167–182. doi: 10.1007/s12126-008-9015-2
Chung, M.-H., Chen, L.-K., Peng, L.-N., and Chi, M.-J. (2015). Development and validation of the health literacy assessment tool for older people in Taiwan: potential impacts of cultural differences. Arch. Gerontol. Geriatr. 61, 289–295. doi: 10.1016/j.archger.2015.06.015
Costello, A. B., and Osborne, J. (2005). Best practices in exploratory factor analysis: four recommendations for getting the most from your analysis. Pract. Assess. Res. Eval. 10, 1–9. doi: 10.7275/JYJ1-4868
de Oliveira, G. R., Neto, J. F., de Camargo, S. M., Lucchetti, A. L. G., Espinha, D. C. M., and Lucchetti, G. (2015). Caregiving across the lifespan: comparing caregiver burden, mental health, and quality of life: caregiving across the lifespan. Psychogeriatrics 15, 123–132. doi: 10.1111/psyg.12087
Del-Pino-Casado, R., Rodríguez Cardosa, M., López-Martínez, C., and Orgeta, V. (2019). The association between subjective caregiver burden and depressive symptoms in carers of older relatives: a systematic review and meta-analysis. PLoS One 14:e0217648. doi: 10.1371/journal.pone.0217648
Denno, M. S., Gillard, P. J., Graham, G. D., DiBonaventura, M. D., Goren, A., Varon, S. F., et al. (2013). Anxiety and depression associated with caregiver burden in caregivers of stroke survivors with spasticity. Arch. Phys. Med. Rehabil. 94, 1731–1736. doi: 10.1016/j.apmr.2013.03.014
Devlin, N. J., and Krabbe, P. F. M. (2013). The development of new research methods for the valuation of EQ-5D-5L. Eur. J. Health Econ. 14, 1–3. doi: 10.1007/s10198-013-0502-3
Durmaz, H., and Okanlı, A. (2014). Investigation of the effect of self-efficacy levels of caregiver family members of the individuals with schizophrenia on burden of care. Arch. Psychiatr. Nurs. 28, 290–294. doi: 10.1016/j.apnu.2014.04.004
Epstein-Lubow, G., Gaudiano, B. A., Hinckley, M., Salloway, S., and Miller, I. W. (2010). Evidence for the validity of the American Medical Association’s caregiver self-assessment questionnaire as a screening measure for depression. J. Am. Geriatr. Soc. 58, 387–388. doi: 10.1111/j.1532-5415.2009.02701.x
Fauth, E., Hess, K., Piercy, K., Norton, M., Corcoran, C., Rabins, P., et al. (2012). Caregivers’ relationship closeness with the person with dementia predicts both positive and negative outcomes for caregivers’ physical health and psychological well-being. Aging Ment. Health 16, 699–711. doi: 10.1080/13607863.2012.678482
Feinberg, L., and Ellano, C. (2000). Promoting consumer direction for family caregiver support: an agency-driven model. Generations 24, 47–53.
Feinberg, L., and Houser, A. N. (2012). Assessing family caregiver needs: Policy and practice considerations. AARP Public Policy Institute. Available at: https://www.caregiving.org/wp-content/uploads/2010/11/AARP-caregiver-fact-sheet.pdf
Feng, B., and Magen, E. (2016). Relationship closeness predicts unsolicited advice giving in supportive interactions. J. Soc. Pers. Relatsh. 33, 751–767. doi: 10.1177/0265407515592262
Galvin, J. E., Duda, J. E., Kaufer, D. I., Lippa, C. F., Taylor, A., and Zarit, S. H. (2010). Lewy Body Dementia: Caregiver Burden and Unmet Needs. Alzheimer Dis. Assoc. Disord. 24, 177–181. doi: 10.1097/WAD.0b013e3181c72b5d
Goldberg, D. P., Gater, R., Sartorius, N., Ustun, T. B., Piccinelli, M., Gureje, O., et al. (1997). The validity of two versions of the GHQ in the WHO study of mental illness in general health care. Psychol. Med. 27, 191–197. doi: 10.1017/S0033291796004242
González-Salvador, M. T., Arango, C., Lyketsos, C. G., and Barba, A. C. (1999). The stress and psychological morbidity of the Alzheimer patient caregiver. Int. J. Geriatr. Psychiatry 14, 701–710. doi: 10.1002/(sici)1099-1166(199909)14:9<701::aid-gps5>3.0.co;2-#
Goodman, C. C. (1991). Perceived social support for caregiving: measuring the benefit of self-help/support group participation. J. Gerontol. Soc. Work 16, 163–175. doi: 10.1300/J083v16n03_13
Gordon, J. R., Pruchno, R. A., Wilson-Genderson, M., Murphy, W. M., and Rose, M. (2012). Balancing caregiving and work: role conflict and role strain dynamics. J. Fam. Iss. 33, 662–689. doi: 10.1177/0192513X11425322
Guo, W., and Tsui, M. (2010). From resilience to resistance: a reconstruction of the strengths perspective in social work practice. Int. Soc. Work. 53, 233–245. doi: 10.1177/0020872809355391
Häggström, E., Mamhidir, A.-G., and Kihlgren, A. (2010). Caregivers’ strong commitment to their relationship with older people. Int. J. Nurs. Pract. 16, 99–105. doi: 10.1111/j.1440-172X.2010.01818.x
Hashimoto, M., Kato, S., Tanabe, Y., Katakura, M., Mamun, A. A., Ohno, M., et al. (2017). Beneficial effects of dietary docosahexaenoic acid intervention on cognitive function and mental health of the oldest elderly in Japanese care facilities and nursing homes. Geriatr. Gerontol. Int. 17, 330–337. doi: 10.1111/ggi.12691
Haslam, D., Filus, A., Morawska, A., Sanders, M. R., and Fletcher, R. (2015). The work–family conflict scale (WAFCS): development and initial validation of a self-report measure of work–family conflict for use with parents. Child Psychiatry Hum. Dev. 46, 346–357. doi: 10.1007/s10578-014-0476-0
Hatcher, L. (1994). A step-by-step approach to using the SAS system for factor analysis and structural equation modeling. Cary, North Carolina: SAS Institute.
Hinton, L., Tran, D., Nguyen, T.-N., Ho, J., and Gitlin, L. (2019). Interventions to support family caregivers of people living with dementia in high, middle and low-income countries in Asia: a scoping review. BMJ Glob. Health 4:e001830. doi: 10.1136/bmjgh-2019-001830
Horn, J. L. (1965). A rationale and test for the number of factors in factor analysis. Psychometrika 30, 179–185. doi: 10.1007/BF02289447
Howard, M. C. (2016). A review of exploratory factor analysis decisions and overview of current practices: what we are doing and how can we improve? Int. J. Hum.-Comput. Interact. 32, 51–62. doi: 10.1080/10447318.2015.1087664
Jones, C., and Griffiths, R. D. (2007). Patient and caregiver counselling after the intensive care unit: what are the needs and how should they be met? Curr. Opin. Crit. Care 13, 503–507. doi: 10.1097/MCC.0b013e3282efb83e
Keady, J., and Nolan, M. (1996). Behavioural and instrumental stressors in dementia (BISID): refocussing the assessment of caregiver need in dementia. J. Psychiatr. Ment. Health Nurs. 3, 163–172. doi: 10.1111/j.1365-2850.1996.tb00083.x
Kelly, K., Wolfe, N., Gibson, M. J., and Feinberg, L. (2013). Listening to family caregivers: The need to include family caregiver assessment in Medicaid home-and community-based service waiver programs. AARP Public Policy Institute. Available at: https://www.aarp.org/content/dam/aarp/research/public_policy_institute/ltc/2013/the-need-to-include-family-caregiver-assessment-medicaid-hcbs-waiver-programs-report-AARP-ppi-ltc.pdf
Kent, E. E., Ornstein, K. A., and Dionne-Odom, J. N. (2020). The family caregiving crisis meets an actual pandemic. J. Pain Symptom Manage. 60, e66–e69. doi: 10.1016/j.jpainsymman.2020.04.006
Knight, B. G., Fox, L. S., and Chou, C.-P. (2000). Factor structure of the burden interview. J. Clin. Geropsychol. 6, 249–258. doi: 10.1023/A:1009530711710
Kramer, B. J., and Kipnis, S. (1995). Eldercare and work-role conflict: toward an understanding of gender differences in caregiver Burden1. Gerontologist 35, 340–348. doi: 10.1093/geront/35.3.340
Kwok, T., Wong, B., Ip, I., Chui, K., Young, D., and Ho, F. (2013). Telephone-delivered psychoeducational intervention for Hong Kong Chinese dementia caregivers: a single-blinded randomized controlled trial. Clin. Interv. Aging 8, 1191–1197. doi: 10.2147/CIA.S48264
Lee, Y.-C., Lin, Y.-C., Huang, C.-L., and Fredrickson, B. (2013). The construct and measurement of peace of mind. J. Happiness Stud. 14, 571–590. doi: 10.1007/s10902-012-9343-5
Leung, C. S. Y., and Earl, J. K. (2012). Retirement resources inventory: construction, factor structure and psychometric properties. J. Vocat. Behav. 81, 171–182. doi: 10.1016/j.jvb.2012.06.005
Lidell, E. (2002). Family support—a burden to patient and caregiver. Eur. J. Cardiovasc. Nurs. 1, 149–152. doi: 10.1016/S1474-51510200004-X
Lightfoot, E., Yun, H., Moone, R., Otis, J., Suleiman, K., Turck, K., et al. (2021). Changes to family caregiving of older adults and adults with disabilities during COVID-19. Gerontol. Geriatr. Med. 7:233372142110024. doi: 10.1177/23337214211002404
Lin, M.-C. (2020). Communication neglect, caregiver anger and hostility, and perceptions of older care receivers’ cognitive status and problem behaviors in explaining elder abuse. J. Elder Abuse Negl. 32, 235–258. doi: 10.1080/08946566.2020.1741054
Lou, V. W. Q., Lau, B. H.-P., and Cheung, K. S.-L. (2015). Positive aspects of caregiving (PAC): scale validation among Chinese dementia caregivers (CG). Arch. Gerontol. Geriatr. 60, 299–306. doi: 10.1016/j.archger.2014.10.019
Lu, L., Wang, L., Yang, X., and Feng, Q. (2009). Zarit caregiver burden interview: development, reliability and validity of the Chinese version. Psychiatry Clin. Neurosci. 63, 730–734. doi: 10.1111/j.1440-1819.2009.02019.x
Lum, T., Shi, C., Wong, G., and Wong, K. (2020). COVID-19 and long-term care policy for older people in Hong Kong. J. Aging Soc. Policy 32, 373–379. doi: 10.1080/08959420.2020.1773192
Lyonette, C., and Yardley, L. (2003). The influence on carer wellbeing of motivations to care for older people and the relationship with the care recipient. Ageing Soc. 23, 487–506. doi: 10.1017/S0144686X03001284
McCurry, S. M., Logsdon, R. G., Teri, L., and Vitiello, M. V. (2007). Sleep disturbances in caregivers of persons with dementia: contributing factors and treatment implications. Sleep Med. Rev. 11, 143–153. doi: 10.1016/j.smrv.2006.09.002
Merluzzi, T. V., Philip, E. J., Vachon, D. O., and Heitzmann, C. A. (2011). Assessment of self-efficacy for caregiving: the critical role of self-care in caregiver stress and burden. Palliat. Support. Care 9, 15–24. doi: 10.1017/S1478951510000507
Mochari-Greenberger, H., and Mosca, L. (2012). Caregiver burden and nonachievement of healthy lifestyle behaviors among family caregivers of cardiovascular disease patients. Am. J. Health Promot. 27, 84–89. doi: 10.4278/ajhp.110606-QUAN-241
Morimoto, T. (2003). Caregiver burden and health-related quality of life among Japanese stroke caregivers. Age Ageing 32, 218–223. doi: 10.1093/ageing/32.2.218
Moroni, L., Sguazzin, C., Filipponi, L., Bruletti, G., Callegari, S., Galante, E., et al. (2008). Caregiver need assessment: a questionnaire for caregiver demand. G. Ital. Med. Lav. Ergon. 30, B84–B90.
Noonan, A. E., and Tennstedt, S. L. (1997). Meaning in caregiving and its contribution to caregiver well-Being1. Gerontologist 37, 785–794. doi: 10.1093/geront/37.6.785
Novak, M., and Guest, C. (1989). Application of a multidimensional caregiver burden inventory. Gerontologist 29, 798–803. doi: 10.1093/geront/29.6.798
Oppe, M., Devlin, N. J., van Hout, B., Krabbe, P. F. M., and de Charro, F. (2014). A program of methodological research to arrive at the new international EQ-5D-5L valuation protocol. Value Health 17, 445–453. doi: 10.1016/j.jval.2014.04.002
Ornstein, K., and Gaugler, J. E. (2012). The problem with “problem behaviors”: a systematic review of the association between individual patient behavioral and psychological symptoms and caregiver depression and burden within the dementia patient–caregiver dyad. Int. Psychogeriatr. 24, 1536–1552. doi: 10.1017/S1041610212000737
Pagel, M. D., Becker, J., and Coppel, D. B. (1985). Loss of control, self-blame, and depression: an investigation of spouse caregivers of Alzheimer’s disease patients. J. Abnorm. Psychol. 94, 169–182. doi: 10.1037//0021-843x.94.2.169
Palamaro Munsell, E., Kilmer, R. P., Cook, J. R., and Reeve, C. L. (2012). The effects of caregiver social connections on caregiver, child, and family well-being. Am. J. Orthopsychiatry 82, 137–145. doi: 10.1111/j.1939-0025.2011.01129.x
Pandian, J. D., Gandhi, D. B. C., Lindley, R. I., and Bettger, J. P. (2016). Informal caregiving: a growing need for inclusion in stroke rehabilitation. Stroke 47, 3057–3062. doi: 10.1161/STROKEAHA.116.013701
Pearlin, L. I., Mullan, J. T., Semple, S. J., and Skaff, M. M. (1990). Caregiving and the stress process: an overview of concepts and their measures. Gerontologist 30, 583–594. doi: 10.1093/geront/30.5.583
Puchalski, C. M. (2012). Spirituality in the cancer trajectory. Ann. Oncol. 23, iii49–iii55. doi: 10.1093/annonc/mds088
Puchalski, C., and Sandoval, C. (2003). “Spiritual care” in A clinical guide to supportive & palliative care for HIV/AIDS. eds. J. F. O’Neill, P. A. Selwyn, and H. Schietinger (U.S.: U.S. Department of Health and Human Services, Health Resources and Services Administration, HIV/AIDS Bureau), 289–299.
Qiu, X., Sit, J. W. H., and Koo, F. K. (2018). The influence of Chinese culture on family caregivers of stroke survivors: a qualitative study. J. Clin. Nurs. 27, e309–e319. doi: 10.1111/jocn.13947
Rattinger, G. B., Fauth, E. B., Behrens, S., Sanders, C., Schwartz, S., Norton, M. C., et al. (2016). Closer caregiver and care-recipient relationships predict lower informal costs of dementia care: the Cache County dementia progression study. Alzheimers Dement. 12, 917–924. doi: 10.1016/j.jalz.2016.03.008
Reinhard, S. C. (1994). Living with mental illness: effects of professional support and personal control on caregiver burden. Res. Nurs. Health 17, 79–88. doi: 10.1002/nur.4770170203
Roth, D. L., Fredman, L., and Haley, W. E. (2015). Informal caregiving and its impact on health: a reappraisal from population-based studies. Gerontologist 55, 309–319. doi: 10.1093/geront/gnu177
Sabella, S. A., and Suchan, C. S. (2019). The contribution of social support, professional support, and financial hardship to family caregiver life satisfaction after traumatic brain injury. J. Head Trauma Rehabil. 34, 233–240. doi: 10.1097/HTR.0000000000000471
Savla, J., Roberto, K. A., Blieszner, R., McCann, B. R., Hoyt, E., and Knight, A. L. (2021). Dementia caregiving during the “stay-at-home” phase of COVID-19 pandemic. J. Gerontol. Ser. B 76, e241–e245. doi: 10.1093/geronb/gbaa129
Shin, D. W., Park, J.-H., Shim, E.-J., Park, J.-H., Choi, J.-Y., Kim, S. G., et al. (2011). The development of a comprehensive needs assessment tool for cancer-caregivers in patient–caregiver dyads. Psychooncology 20, 1342–1352. doi: 10.1002/pon.1857
Skaff, M. M., and Pearlin, L. I. (1992). Caregiving: role engulfment and the loss of self 1. Gerontologist 32, 656–664. doi: 10.1093/geront/32.5.656
Springate, B. A., and Tremont, G. (2014). Dimensions of caregiver burden in dementia: impact of demographic, mood, and care recipient variables. Am. J. Geriatr. Psychiatry 22, 294–300. doi: 10.1016/j.jagp.2012.09.006
Stephens, M. A. P., Townsend, A. L., Martire, L. M., and Druley, J. A. (2001). Balancing parent care with other roles: Interrole conflict of adult daughter caregivers. J. Gerontol. Ser. B 56, P24–P34. doi: 10.1093/geronb/56.1.P24
Stroebe, M., and Schut, H. (1999). The dual process model of coping with bereavement: rationale and description. Death Stud. 23, 197–224. doi: 10.1080/074811899201046
Stroebe, M., and Schut, H. (2001). “Meaning making in the dual process model of coping with bereavement” in Meaning reconstruction & the experience of loss. ed. R. Neimeyer (Washington: American Psychological Association), 55–73.
Stuckey, J. C. (2001). Blessed assurance: the role of religion and spirituality in Alzheimer’s disease caregiving and other significant life events. J. Aging Stud. 15, 69–84. doi: 10.1016/S0890-4065(00)00017-7
Tang, J. Y., Ho, A. H., Luo, H., Wong, G. H., Lau, B. H., Lum, T. Y., et al. (2016). Validating a Cantonese short version of the Zarit burden interview (CZBI-short) for dementia caregivers. Aging Ment. Health 20, 996–1001. doi: 10.1080/13607863.2015.1047323
Thornton, M., and Travis, S. S. (2003). Analysis of the reliability of the modified caregiver strain index. J. Gerontol. B Psychol. Sci. Soc. Sci. 58, S127–S132. doi: 10.1093/geronb/58.2.S127
Tremont, G., Davis, J., Papandonatos, G. D., Grover, C., Ott, B. R., Fortinsky, R. H., et al. (2013). A telephone intervention for dementia caregivers: background, design, and baseline characteristics. Contemp. Clin. Trials 36, 338–347. doi: 10.1016/j.cct.2013.07.011
Turner, R. J. (2009). “Understanding health disparities: the promise of the stress process model” in Advances in the conceptualization of the stress process. eds. W. R. Avison, C. S. Aneshensel, S. Schieman, and B. Wheaton (New York, NY: Springer New York), 3–21.
United Nations, Department of Economic and Social Affairs, and Population Division. (2020). World population ageing, 2019 highlights. United Nations: Department of Economic and Social Affairs, and Population Division.
van Wijngaarden, B., Schene, A. H., and Koeter, M. W. J. (2004). Family caregiving in depression: impact on caregivers’ daily life, distress, and help seeking. J. Affect. Disord. 81, 211–222. doi: 10.1016/S0165-0327(03)00168-X
Vitaliano, P. P., Zhang, J., and Scanlan, J. M. (2003). Is caregiving hazardous to one’s physical health? A meta-analysis. Psychol. Bull. 129, 946–972. doi: 10.1037/0033-2909.129.6.946
Weber, S. R., Pirraglia, P. A., and Kunik, M. E. (2011). Use of services by community-dwelling patients with dementia: a systematic review. Am. J. Alzheimers Dis. Dementiasr 26, 195–204. doi: 10.1177/1533317510392564
WHO (2002). WHOQOL-SRPB field-test instrument. Available at: https://apps.who.int/iris/bitstream/handle/10665/77777/WHO_MSD_MER_Rev?sequence=1.
Wong, J. S. H., and Cheung, K. M. C. (2020). Impact of COVID-19 on Orthopaedic and trauma service: an epidemiological study. J. Bone Jt. Surg. 102:e80. doi: 10.2106/JBJS.20.00775
Wong, E. L. Y., Ramos-Goñi, J. M., Cheung, A. W. L., Wong, A. Y. K., and Rivero-Arias, O. (2018). Assessing the use of a feedback module to model EQ-5D-5L health states values in Hong Kong. Patient-Patient-Centered Outcomes Res. 11, 235–247. doi: 10.1007/s40271-017-0278-0
Xiong, C., Biscardi, M., Astell, A., Nalder, E., Cameron, J. I., Mihailidis, A., et al. (2020). Sex and gender differences in caregiving burden experienced by family caregivers of persons with dementia: a systematic review. PLoS One 15:e0231848. doi: 10.1371/journal.pone.0231848
Yamashita, M., and Amagai, M. (2008). Family caregiving in dementia in Japan. Appl. Nurs. Res. 21, 227–231. doi: 10.1016/j.apnr.2007.01.009
Yildiz, E., Karakaş, S. A., Güngörmüş, Z., and Cengiz, M. (2017). Levels of care burden and self-efficacy for informal caregiver of patients with cancer. Holist. Nurs. Pract. 31, 7–15. doi: 10.1097/HNP.0000000000000185
Yu, D. S. F., Cheng, S.-T., and Wang, J. (2018). Unravelling positive aspects of caregiving in dementia: an integrative review of research literature. Int. J. Nurs. Stud. 79, 1–26. doi: 10.1016/j.ijnurstu.2017.10.008
Yu, S., Zhang, F., Nunes, L. D., Deng, Y., and Levesque-Bristol, C. (2020). Basic psychological needs as a predictor of positive affects: a look at peace of mind and vitality in Chinese and American college students. J. Posit. Psychol. 15, 488–499. doi: 10.1080/17439760.2019.1627398
Keywords: caregivers, Hong Kong, assessment, scale development, caregivers’ needs, caregivers’ resources
Citation: Li K-K, Leung CLK, Yeung D, Chiu MYL, Chong AML, Lam BCY, Chung EKH and Lo TW (2023) Development and validation of the caregiver needs and resources assessment. Front. Psychol. 14:1063440. doi: 10.3389/fpsyg.2023.1063440
Edited by:
Jianfei Xie, Third Xiangya Hospital, Central South University, ChinaReviewed by:
Cosmos Yarfi, University of Health and Allied Sciences, GhanaHany Ibrahim, Ain Shams University, Egypt
Copyright © 2023 Li, Leung, Yeung, Chiu, Chong, Lam, Chung and Lo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Kin-Kit Li, YmVuLmxpQGNpdHl1LmVkdS5oaw==; Cyrus L. K. Leung, Y3lydXNsZXVuZ0BjdWhrLmVkdS5oaw==
 Kin-Kit Li
Kin-Kit Li Cyrus L. K. Leung
Cyrus L. K. Leung Dannii Yeung
Dannii Yeung Marcus Y. L. Chiu3,4
Marcus Y. L. Chiu3,4 Beck C. Y. Lam
Beck C. Y. Lam Edwin K. H. Chung
Edwin K. H. Chung T. Wing Lo
T. Wing Lo