
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 07 December 2022
Sec. Positive Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.991239
This article is part of the Research Topic Positive Psychology in Health Management View all 18 articles
Introduction: Anxiety often precedes depression, and the pathway from anxiety to depression may be affected by multiple exposures. Our research aims to explore the mediating effect of the social support availability (SSA) between anxiety and depression and how it is moderated by psychological capital.
Methods: A cross-sectional study was conducted among Chinese emergency physicians at the top-level general hospitals in eastern China. Data were collected via the questionnaire including anxiety and depression subscales of Symptom Checklist-90, Psychological Capital Questionnaire as well as Social Support Rating Scale. The PROCESS v3.4 macro was employed to assess the mediating role of SSA and a moderating role of psychological capital.
Results: A total of 536 valid samples were filtered. Anxiety, depression, SSA, and psychological capital were significant correlated. Anxiety was positively associated with depression (β = 0.82, p < 0.001), and the SSA mediated the relationship between anxiety and depression (indirect effect = 0.013, 95%BootCI [0.005, 0.023]). Psychological capital (specifically, self-efficacy, hope and resilience) further played a moderating role in the relationship between SSA and depression (β = 0.06, p < 0.01).
Conclusion: The mental health of emergency physicians should be concerned. In order to decrease anxiety and depression, SSA and psychological capital should be increased as the interventions for emergency physicians.
Depression is common in medical practitioners across all stages of their careers (Center et al., 2003; Bailey et al., 2018), even occurs much more frequently than in the general population (Eckleberry-Hunt and Lick, 2015). Medical staffs always have poorer mental health than the general population (Rajasekar and Krishnan, 2021). The morbidity of depression among medical staff was estimated between 12.3 and 45.5% (Paiva et al., 2018; de Wit, 2020; Elhadi et al., 2020). In addition, anxiety is also the common mental health problem for medical staff (Medisauskaite and Kamau, 2019). A Brazilian survey showed that the positive rate of anxiety was 56.6% among 1,419 doctors (de Mélo Silva Júnior et al., 2022). Because of the special nature of the work, emergency physicians (EPs) need to be ready to provide medical services for emergency cases and suffer from huge occupational stress (Basu et al., 2020; Janicki et al., 2020; Pujo et al., 2021). A longitudinal study found the anxiety level of medical residents among EPs were higher than other department doctors (González-Cabrera et al., 2018), and a study at east Africa’s largest public hospital displayed that 40.6% of EPs had the moderate to severe range of depression disorders (Iheanacho et al., 2022). There are lots of factors that affect the mental health of EPs and work environment is one of the factors (Rasmussen et al., 2014). In China, large population leads to a crowded and noisy emergency environment, which is not only bad for the work of EPs, but also reduces patients’ satisfaction (Lin et al., 2013). The recent research discovered that a total of 35.6% of EPs suffered from depression among 15,243 Chinese samples (Chen et al., 2022).
Anxiety disorders refer to a group of mental disorders in which patients experience excessive worry and constant fear, and depression is a common psychiatric disorder characterized by sadness, loss of interest or pleasure, feelings of tiredness and poor concentration (World Health Organization, 2017). Because of similarity in symptoms, anxiety and depression often go together (Groen et al., 2020) as the most common comorbidity in psychiatry, while the mechanism of the comorbidity is still unclear (Ter Meulen et al., 2021). Previous study discovered that the overlapping symptoms act as a bridge linking the anxiety and depression (Groen et al., 2020). Nevertheless, either anxiety or depression has a respective component to differentiate both, for anxiety is characterized by psychological hyperarousal and depression is characterized by anhedonia (Joiner, 1993), and anxiety precedes depression in the temporal order of onset of most cases (Moscati et al., 2016; Demyttenaere and Heirman, 2020). Starr et al. (2014) found that anxiety may develop into depression if limiting interpersonal interaction, because the decrease or loss of social relationships is harmful to mental health (Chu, 2017). In conclusion, anxiety and depression are highly correlated and anxiety may be a precursor to depression. Thus, we proposed the hypothesis.
Hypothesis 1: anxiety is highly related to depression among EPs in China.
Social support, as a crucial social factor beneficial to human health, has long been recognized and well-documented for several decades (Cobb, 1976; Ditzen and Heinrichs, 2014), but the concrete definition of social support is not uniform (Cohen, 1988). In general, social support is defined as the material, information and emotional support that an individual receives in a network of social relationships (Cohen and Wills, 1985; Cohen, 1988; Ditzen and Heinrichs, 2014). That means, the individual’s social support concerns two parties: actual received social support and subjective perceived social support. The social support availability (SSA) is defined as the extent to which individuals utilize the social support that available to them, which belongs to subjective perceived social support (Xiao, 1994). Compared with actual received social support, the SSA should be most effective in altering subjective cognitive appraisals if the counter the specific needs elicited by the stressful event (Cohen and McKay, 2020). In term of the relationship between stress or negative emotions and perceived social support, Barrera proposed the social support deterioration model that stress or negative emotions can deteriorate the perceived availability or effectiveness of social support (Barrera, 1986). Hindmarch (1998) found that anxious individuals will have cognitive biases and cannot perceive things correctly, which verified the deterioration model. Existing empirical research found that perceived social support can mediate the relationship between anxiety and life satisfaction (Yu et al., 2020), quality of life (Kugbey et al., 2020; Yang and Lu, 2022), and depression (Dour et al., 2014). However, less research has been done on the relationship between SSA (as a component of social support) and anxiety or depression. A study found that anxiety was negatively associated with perceived availability of social support (Den Oudsten et al., 2010). And a recent survey found social support including the dimension of SSA mediated the relationship between the psychological capital and depression among EPs in China (Xu et al., 2022a). Furthermore, low levels of perceived social support may lead to hopelessness and helplessness, which in turn can trigger depression (Johnson et al., 2001). Nonetheless, the role of SSA in the relationship between anxiety and depression was still unclear. Thus, based on the deterioration model, we proposed this hypothesis.
Hypothesis 2: SSA paly a mediating role in the relationship between anxiety and depression among EPs in China.
Psychological capital (PsyCap), as an emerging positive psychological resource, is defined as ‘a positive state of mind exhibited during the growth and development of an individual,’ comprising four core components: self-efficacy, optimism, hope, resilience (Luthans et al., 2007b). PsyCap has been proven to be effective in improving individual performance and relieving negative emotions. Empirical research showed that PsyCap was negatively associated with psychological symptoms, such as anxiety (Minglu et al., 2020) and depression (Shen et al., 2014), and could improve nurses’ care competencies (Guo et al., 2021) and quality of life of cancer patients (Guo et al., 2022). And PsyCap also played a mediating role in the relationship between anxiety or depression and other related variables (Rahimnia et al., 2013; Jiang, 2021; Zhao et al., 2021). What’s more, PsyCap could moderate the relationship between perceived stress and negative emotions (Wang et al., 2021b) or anxiety (Yang and Yang, 2022). The study of Xu et al. (2022b) found that college freshmen with high level of PsyCap reduced the more effect of interpersonal sensitivity on depression than that with low PsyCap. However, there was little exploration about the moderating effect of PsyCap in the relationship between anxiety, SSA and depression. Hence, we proposed the following hypothesis.
Hypothesis 3: PsyCap has the moderating effect on one or more paths of the mediating model.
In summary, based on the appraisal perspective of buffering effect of social support and the dynamic effect model of PsyCap, the present study constructed the moderated mediation model (Figure 1). The aim of our study was to explore the mediating (SSA) and moderating (PsyCap) mechanisms in the relationship between anxiety and depression among EPs in China.
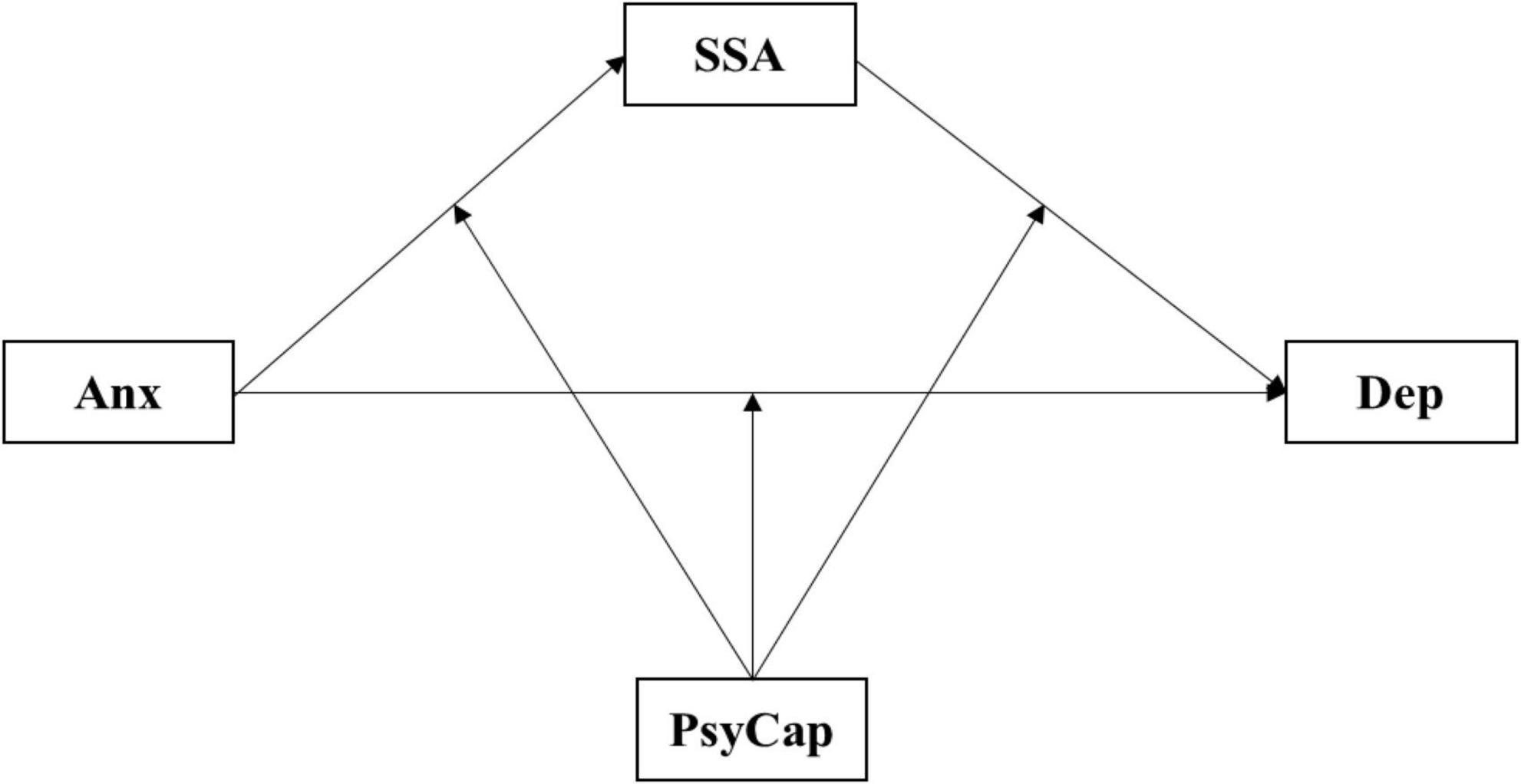
Figure 1. The hypothetical moderated mediation model. Dep, depression; Anx, anxiety; SSA, social support availability; PsyCap, psychological capital.
This study was performed from July to August 2017 by a cross-sectional survey in Jiangsu Province in eastern China. The dataset was constructed from 33 tertiary grade-A (top-level) general hospitals in 13 prefecture-level cities of the province. Before the formal investigation, researchers first contacted the relevant staffs of hospitals to introduce the purpose and details in order to achieve approval. The researchers recruited college students to train as investigators. After completing the training, the investigators went to the target hospitals that achieved approval with the paper questionnaire to collect data. With the cooperation of the emergency department director, the EPs were called together for on-site questionnaire distribution, filling and retrieval. Before filling out, the investigator told the purpose and guidance of the study. EPs who filled out and submitted questionnaire were considered as contenting to participate in this study.
The inclusion criteria for respondents included: (1) those who volunteered to participate in our survey and followed the principle of informed consent, and (2) who understood the interview questions. The exclusion criteria were: (1) those who refused to sign the informed consent, and (2) the uncompleted answers.
An anonymous self-reported questionnaire in Chinese was distributed to all the selected EPs. The questionnaire contained two parts: the first part had the social demographic and other relevant features of the EPs that act as control variables in the model, including gender, age, working-years, education background and professional post; in the second part, we used the following maturity scales as the measuring tool: anxiety and depression subscales of Symptom Checklist 90 (SCL-90), Psychological Capital Questionnaire 24 (PCQ-24), and Social Support Rating Scale (SSRS). All scales that in Chinese, were standardized and suited to the Chinese population (see below for details).
The Symptom Checklist-90-Revised (SCL-90-R) is a 90-item self-report symptom inventory developed by Derogatis et al. (1976) in the mid-1970s and widely exploited to measure psychological status or screen for mental disorders. The SCL-90 consists of nine subscales with a total of 90 items: somatization, obsessive-compulsive, interpersonal sensitivity, hostility, phobic anxiety, paranoid ideation, psychoticism, anxiety, and depression. Each item is scored by Likert 5-point scale ranging from 1 (no symptoms), 2 (mild), 3 (moderate), 4 (serious), to 5 (severe), with a higher score representing a more evident degree of psychological distress symptoms. The SCL-90 has been proved to have acceptable psychometric properties for the screening of anxiety and depression among Chinese doctors (Dai et al., 2015). In addition, the standard (the mean of the sample plus a standard deviation) recommended by Dang et al. (2020) was acted as the positive threshold of anxiety and depression. In our study, the Cronbach’s α for depression and anxiety subscale was 0.89 and 0.88, respectively.
PsyCap was measured via the Psychological Capital Questionnaire (PCQ-24), which was developed by Luthans et al. (2007a) and the Chinese version has shown good reliability among Chinese physicians (Tian et al., 2020). The PCQ-24 consists of four dimensions (i.e., self-efficacy, hope, optimism, and resilience), with each dimension including six items. Each of the items is scored on a Likert 6-point scale, with 1 indicating potent disagreement and 6 indicating strong agreement. A higher score generally indicates a higher level of PsyCap and better mental health. In our study, the Cronbach’s α was 0.93 for the total scale, with 0.74, 0.88, 0.88, and 0.83 for the subscales of self-efficacy, hope, resilience, and optimism, respectively.
Social support rate scale (SSRS), compiled by Xiao, was adopted to measure individuals’ social support, including three dimensions: objective social support, subjective social support, and the availability of social support (Xiao, 1994). The SSA subscale contained three items, such as “How often you participate in activities organized by groups (party member organizations, trade unions, student unions, etc.).” Each item scoring 1–4 points, with a higher score representing better SSA. It has been demonstrated to be a reliable and valid measure for assessing SSA among Chinese physicians (Song et al., 2021). In our study, the Cronbach’s α was 0.64 for the subscale of SSA.
The study was reviewed and approved by the ethics committee at Xuzhou Medical University. All research methods were performed in accordance with relevant guidelines of Declaration of Helsinki. Completion of the surveys was deemed as an indication of participant consent.
Descriptive analysis was used to describe and compare the socio-demographic data (e.g., gender, age, and working-years). For continuous variables, mean and standard deviation (SD) were used; and for discrete variables, rate (or proportion) was used. Pearson’s correlation analyses of the four variables (PsyCap, SSA, anxiety and depressive symptoms) were performed using SPSS version 21.0. AMOS 24.0 was employed to test the validity of scales. G*power 3.1.9.2 was used to calculate the sample size. To test the significance of the moderated mediation model in this study, we adopted model 4 and 59 of PROCESS v3.4 macro for SPSS provided by Hayes and Rockwood (2019). This approach is based on ordinary least-squares regression and the bootstrap method. A simple slope test was used to initially probe the moderating effect. The bootstrapped conditional effect was used to show the interactions and the Johnson–Neyman (J–N) technique was applied for probing interactions more specifically (Hayes, 2018). The J–N technique can identify regions in the range of the moderator variable where the effect of the antecedent variable on the outcome variable is statistically significant or not significant. The number of bootstrap confidence intervals was 5,000.
We adopted the G*power 3.1.9.2 to calculate the sample size. A total of 536 of 593 EPs submitted valid questionnaires, with the response rate of 90.4%. Post hoc analysis in G*power was employed to compute the achieved power (1-β) of the simple size of our study. Because the process macro was based on the multiple regression model, fixed model of linear multiple regression was set as the statistical test. The calculated parameters were as follows: effect size f2 was inputted as 0.15, α was 0.05, the total sample was 536, and the number of final predictors was 10. The result showed that a statistical power of 100% was achieved in the regression model, indicated that 536 EPs reached the necessary sample size.
Harman’s single-factor test was used to probe common method bias. The result found that nine factors had eigenvalues greater than 1, and the first factor of the amount of variation explained was 29.38%, less than 40% of the critical criterion. Therefore, the common method bias in our study was not strong.
To test the construct validity, we assessed for discriminant validity and convergent validity. The discriminant validity was measured by comparing the AVE square root of the scales with the correlation coefficient between the scale variable and other variables. If the AVE square root > the absolute value of correlation coefficient, it showed that the constructs had adequate discriminant validity (Fornell and Larcker, 1981). As shown in Table 1, the AVE square root of four scales were between 0.63 and 0.79, which higher than the absolute value of correlation coefficient except for the coefficient between anxiety and depression. Previous researches had demonstrated that anxiety and depression subscales of SCL-90 have greatly discriminant validity (Morgan et al., 1998; Bech et al., 2014). In general, the constructs had adequate discriminant validity in our study.
The convergent validity was evaluated the magnitude of the standardized factor loadings (SFL) and composite reliability (CR). The SFL values of the measurement model of scales were between 0.572 and 0.913 except for only three items (0.446, 0.464, and 0.467), which were above the threshold of 0.5 in general (Hair et al., 2010). Furthermore, the CR values of four constructs ranged from 0.65 to 0.89, which all exceeded the convergent validity threshold of 0.6 (Hair et al., 2010). Hence, the convergent validity of scales was appropriate.
For reliability, we additionally reported the CR values besides the Cronbach’s α coefficient. The CR values for the scales ranged from 0.65 to 0.89, which agreed with Fornell–Larcker criteria of 0.6 (Fornell and Larcker, 1981). Therefore, the scales used in our study had acceptable reliability.
A total of 593 emergency physicians were recruited in this study, and 536 valid data were screened out according to the exclusion criteria (the effective response rate = 90.4%), including 330 (61.6%) males and 206 (38.4%) females. 54.9% of emergency physicians were between the ages of 26 and 35. 67.4% of samples have been working for less than 10 years. See Table 2 for more details.
According to the standard recommended by Dang, we used 2.1 (1.52/1.56 + 0.54) as the positive threshold for anxiety and depression subscales in the present study. We found that 16.6% (89/536) of EPs had reach the threshold of anxiety, and 16% (86/536) of EPs could been considered had depression. In addition, the proportion of the comorbidity of anxiety and depression among EPs is 12.13% (65/536) in the present study.
Pearson’s correlation analysis revealed that significant correlations existed between these variables. Specifically, depression was negatively related to SSA and PsyCap (r = –0.22 and –0.43, p < 0.001, respectively). Anxiety was also negatively associated with SSA and PsyCap (r = –0.17 and –0.39, p < 0.001, respectively). In addition, a positive correlation between PsyCap and SSA was identified (r = 0.20, p < 0.001). Moreover, the four components of PsyCap are all negatively related to anxiety and depression (Table 1).
As shown in Table 3, anxiety had a negative impact on SSA (β = –0.17, p < 0.001). With the statistically significant effect of SSA on depression (β = –0.08, p < 0.001), it appears that anxiety had a positive direct effect (β = 0.86, p < 0.001), and further had an indirect effect on depression via the partially mediating role of SSA (indirect effect = 0.013, BootSE = 0.005, 95%BootCI [0.005, 0.023]) (Table 4). Hence, hypothesis 1 and 2 was supported.
In the moderation analysis, the interaction of PsyCap and anxiety was insignificant (β = –0.01, p = –0.115), which displayed that PsyCap had no moderating effect in the relationship between anxiety and depression. Meanwhile, the interact term of anxiety and SSA was also insignificant (β = –0.02, p = 0.569), whereas the interaction of SSA and PsyCap was statistically significant (β = 0.06, p = 0.004) (Table 3). This indicated that PsyCap played a moderating role in the link between SSA and depression.
In term of probing the moderation, when PsyCap was divided into high and low groups by M ± 1 SD, the simple slope test indicated that compared with EPs in high groups, the effect of SSA on depression was more pronounced among the low group (Figure 2). The analysis of conditional indirect effect also confirmed that the indirect effect was not significant when PsyCap was in the high group (Table 5). Furthermore, the J–N technique indicated that the standardized score of 0.386 on the PsyCap can be regarded as a point of transition between the statistically significant effect and the non-significant effect of SSA on depression (Figure 3). In addition, we also explored the moderating role of four components of PsyCap in the model. Results showed that self-efficacy (β = 0.07, p = 0.004), hope (β = 0.06, p = 0.010), and resiliency (β = 0.05, p = 0.015) had significant moderating effect in the link from SSA to depression except for optimism (β = 0.03, p = 0.143, Table 6). In all, hypothesis 3 was partially supported.
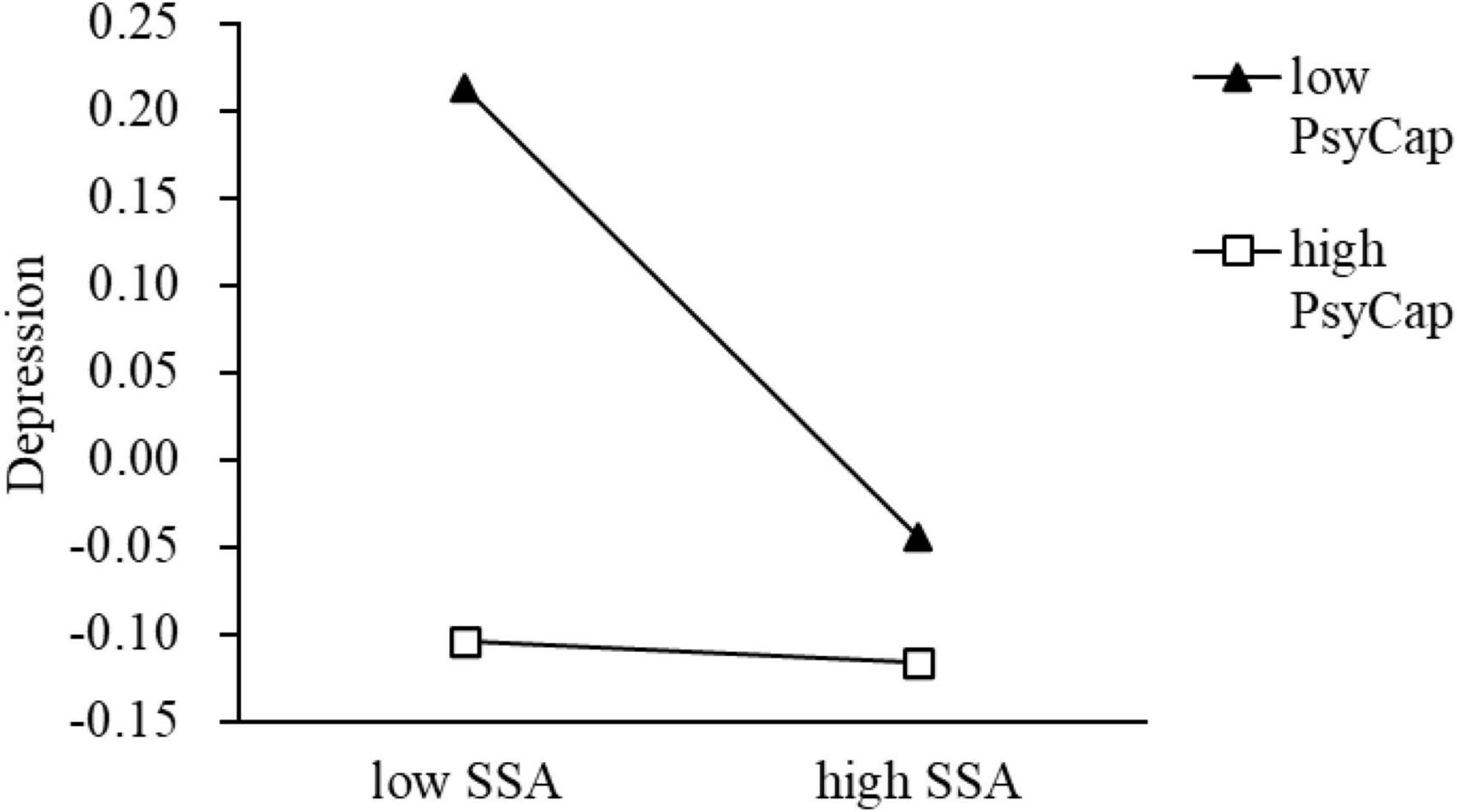
Figure 2. The simple slope test of the moderating effect of PsyCap on the relationship between SSA and depression. SSA, social support availability; PsyCap, psychological capital.
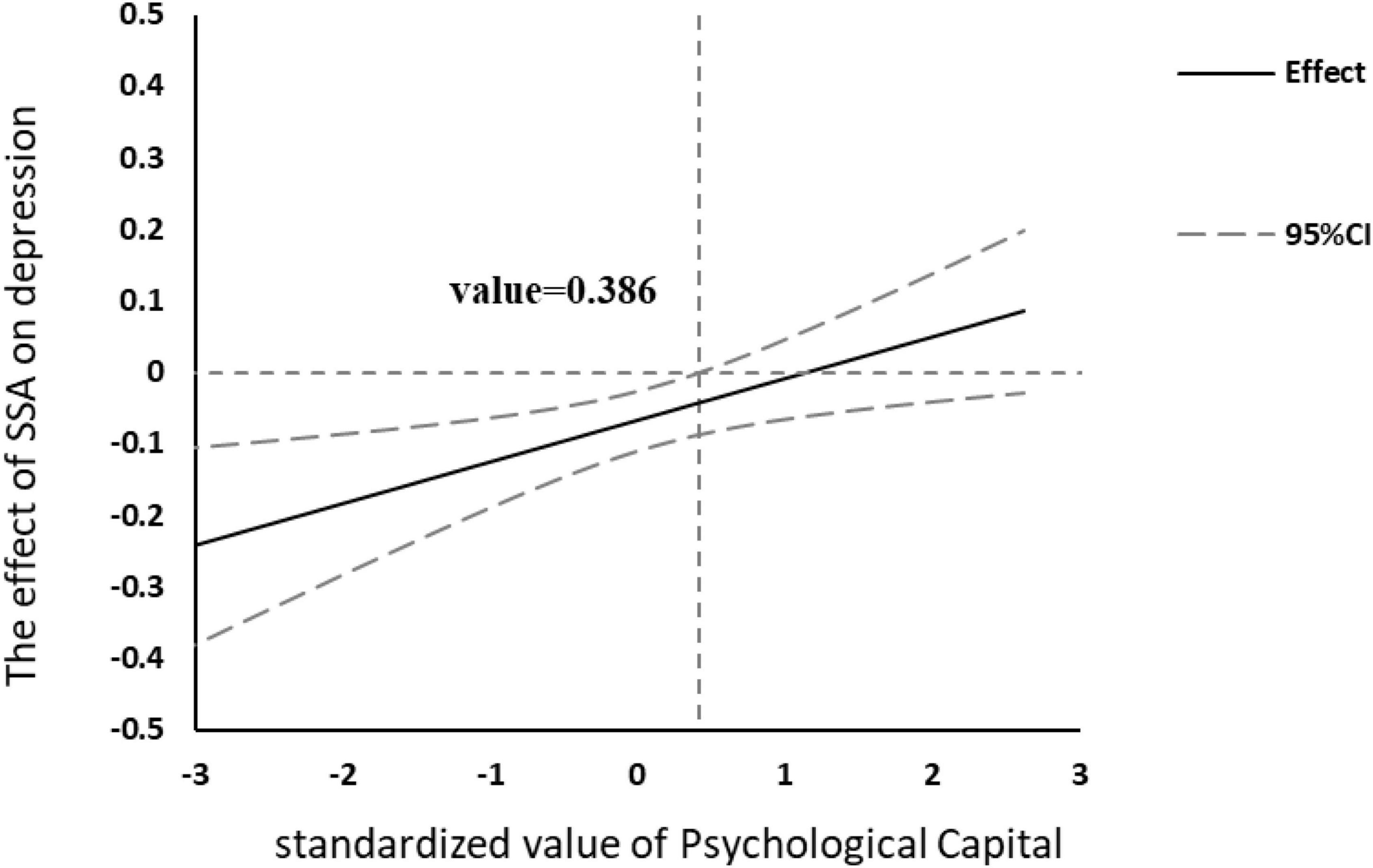
Figure 3. Effect of social support availability (SSA) on depression at different levels of psychological capital (PsyCap). The moderating effect of PsyCap was existed when the value of PsyCap ≤ 0.386.
This cross-sectional survey was conducted to find the psychological symptoms (anxiety and depressive symptoms), SSA and PsyCap level of EPs in China. And to date, this investigation was the first study to explore the moderation mediation mechanism of SSA and PsyCap in the link from anxiety to depression (SSA as the mediating variable and PsyCap as the moderating variable). Interestingly, in our study the positive rates for anxiety and depression were almost the same (16%) and the proportion that met the positive criteria for both symptoms was 12.13%. The regression model also showed anxiety had a strong positive association with depression. This result reaffirmed the high comorbidity of anxiety and depression at the cross-sectional level, which was consent with the conclusion of large cohort study (Lamers et al., 2011).
Central to our research findings is the examination in which SSA and PsyCap are postulated as intervening variables in the relationship between anxiety and depression in a model. Our findings demonstrated that the mediation effect of SSA in the pathway from anxiety to depression and the moderating role of PsyCap in the link between SSA and depression were both significant. The findings also provided new insights into the detail of how PsyCap can play a significant moderating role. Specifically, it was found that the moderating effect PsyCap on the link between SSA and depression was significant only when PsyCap was at the low level.
In our study, SSA played a mediating role in the link from anxiety to depression, which verified the subjective cognitive appraisal of social support (Cohen and McKay, 2020). When an individual’s evaluation of an event tends to be negative, the negative belief about self will occur, which is central to the development of depression (Otani et al., 2018). High level of SSA can make individuals have less negative appraisal of stressful events (Lakey and Cohen, 2000). The specificity of the occupation requests the EPs to be fully prepared for unpredictable emergency incidents, which brings them frequently negative emotions or behaviors by the patients from different types of families, especially those who are drunk, irritable, aggressive or even violent (Liu et al., 2015). These factors have been proven to be risk factors for depression among EPs in China (Chen et al., 2022). When EPs are confronted with these stressful anxiety events, the appraisal system is activated. If they are proactive and have resources available for support that are sufficient to deal with these things, that is, high levels of SSA, then the level of depression will be reduced and. Relatively, if EPs don’t seek support from friends and family in a timely and active manner, that is, the level of SSA is low, they wrongly believe subjectively that no one helps them, amplifying the negative appraisals of stressful events and deteriorating the anxiety symptoms into depression (Hart and Hittner, 1991; Starr et al., 2014).
Through the moderation analysis, we found that the significant dynamic effect of PsyCap in the relationship between SSA and depression. Compared to EPs with high PsyCap, the alleviating effect of SSA on depression was more significant. Specifically, when the amount of PsyCap was below a certain value (varied according to the sample specific value), the effect of SSA on alleviating depression became more pronounced with the adding PsyCap score. But when the PsyCap score reached a critical value, the moderating effect was non-significant. The possible interpretation for this may be twofold. First, people with low level of PsyCap are not very good at perceiving and utilizing social support. They cannot make good use of the resources of social support around when suffering from stress. Second, high PsyCap is associated with low depression (Bakker et al., 2017), and the promoting interaction between PsyCap and social support (Liu et al., 2013) makes individuals with high psychological capital have no great improvement in the utilization of social support. Therefore, for EPs with high PsyCap, if depression symptoms occur, they need to find other psychological resources for relief.
Based on the moderation analysis of overall PsyCap, we further conducted the same model to explore the moderating effect of four components of PsyCap. The results indicated that self-efficacy, hope and resiliency exerted the identical dynamic effect as PsyCap, that was these traits could enhance SSA in alleviating depressive symptoms. This corroborated previous research and further explored the interaction between SSA and these psychological traits. Holahan and Holahan (1987) found self-efficacy could function indirectly through its effect on social support in preventing depression by a longitudinal study. A recent study also showed that self-efficacy and social support could alleviate depression and improve psychological well-being among Chinese nurses (Xie et al., 2020). The growth of low level of self-efficacy can make individuals better use of the social support around them and believe in their ability to regard demands as challenges rather than treats (Weber et al., 2013). Similarly, a study (Tao et al., 2022) found that hope protected individuals from depression by enhancing social support (including the SSA dimension). Another study (Zhao et al., 2018) showed that resiliency moderated the relationship between social support and depressive symptoms. These traits can help EPs discover the positive connotation behind stressful events and fully tap their supports to cope with these difficulties (Feng and Yin, 2021). Unexpectedly, optimism did not have the moderating effect in our study. We inferred that this may be due to the cultural differences in optimism. The effect of optimism on individuals’ behavior differed by nationality and culture (Wang et al., 2021a). In general, due to the influence of Confucian culture, Chinese had lower level of optimism than western group (Moyer et al., 2009). Coupled with overwhelming workload, optimism may have little effect on SSA of EPs.
Our study is not free from limitations. First, due to the cross-sectional observational nature of our study, the time causality between these factors cannot be robustly determined and established. We can only try to explore the underlying mechanisms. Second, we did not examine the precedence of anxiety and depression and the bidirectional causal relationship between anxiety and depression may be more complicated. Confounding factors are not the only ones included in our study, such as genetic, socio-environmental stressors, etc. Third, the subscale that was used to assess SSA was not custom-designed. It is necessary to develop a specialized measurement scale in the further researches. Fourth, our sample only focus on the EPs of the top-level hospital in Jiangsu province. There is a need for further studies to authenticate whether our conclusion can be generalized to other medical practitioners in other grade hospitals or other Chinese provinces with different profiles.
The value of the present study was to verify the subjective cognitive appraisal theory of SSA and the dynamic effect of PsyCap in relieving symptoms of anxiety and depression among EPs in China. First, our study demonstrated the high co-existence of anxiety and depression at the data level. In clinical diagnosis, the two are generally not diagnosed separately (Ter Meulen et al., 2021). Therefore, mental health needs close attention among EPs, especially for anxiety and depressive symptoms. Second, the present study found that SSA mediated the conduction pathway from anxiety to depression, which verified the appraisal mechanism of social support for individual mental health protection. Specifically, SSA could reduce the effect of anxiety in depression among EPs. This reminds EPs that when they experience psychological symptoms, such as anxiety, they need to actively seek support around them in time and improve SSA to buffer the negative impact of psychological stress. Third, our study displayed that PsyCap played a moderating role in the link between SSA and depression. More importantly, we found that the moderating effect of PsyCap only works in the low level. Therefore, psychological capital intervention can be applied to enhance SSA to further alleviate anxiety and depressive symptoms. Hospitals should organize activities to improve PsyCap of EPs with low PsyCap, which focus on self-efficacy, hope and resiliency. EPs with high PsyCap need to keep the status quo, make their anxiety and depression at a low level, and ensure their mental health. According to the ‘Healthy China 2030’ program, EPs should be more likely to have priority over others to be screened for depression to prevent mental health problems. With their mental health improved, they can provide better medical care services.
Our study explored the mediating role of SSA and the moderation effect of PsyCap in the relationship between anxiety and depression. The results found that anxiety had a strong association with depression and SSA mediated the pathway between the two. Furthermore, PsyCap moderated the second half of the mediated pathway (the link from SSA to depression). More specifically, the alleviating effect of PsyCap was more pronounced at low level of PsyCap.
The original contributions presented in this study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
XL and HX developed the rationale for the study. HX and LP analyzed and interpreted data as well as wrote up the initial draft of the manuscript. HX and ZW revised subsequent manuscripts. All authors read and approved the final manuscript.
This work was supported by the Social Science Foundation of Jiangsu project (project number: 18GLD010), the College Philosophy and Social Science Foundation of Jiangsu project (project number: 2018SJA0956), and Xuzhou Science and Technology Project under Grant (KC21306). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
The authors appreciate all the volunteers participating in the study as investigators, who rendered assistance in obtaining written informed consent for the survey and in distributing questionnaires to the subjects. The authors also appreciate all the respondents from the general hospitals and all the participants who made this study possible.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Bailey, E., Robinson, J., and Mcgorry, P. (2018). Depression and suicide among medical practitioners in Australia. Intern. Med. J. 48, 254–258. doi: 10.1111/imj.13717
Bakker, D. J., Lyons, S. T., and Conlon, P. D. (2017). An exploration of the relationship between psychological capital and depression among first-year doctor of veterinary medicine students. J. Vet. Med. Educ. 44, 50–62. doi: 10.3138/jvme.0116-006R
Barrera, M. (1986). Distinctions between social support concepts, measures, and models. Am. J. Community Psychol. 14, 413–445. doi: 10.1007/BF00922627
Basu, S., Harris, A., Mason, S., and Norman, J. (2020). A longitudinal assessment of occupational stress in emergency department nursing staff. J. Nurs. Manag. 28, 167–174. doi: 10.1111/jonm.129
Bech, P., Bille, J., Moller, S. B., Hellstrom, L. C., and Ostergaard, S. D. (2014). Psychometric validation of the hopkins symptom checklist (SCL-90) subscales for depression, anxiety, and interpersonal sensitivity. J. Affect. Disord. 160, 98–103. doi: 10.1016/j.jad.2013.12.005
Center, C., Davis, M., Detre, T., Ford, D. E., Hansbrough, W., Hendin, H., et al. (2003). Confronting depression and suicide in physicians: A consensus statement. JAMA 289, 3161–3166. doi: 10.1001/jama.289.23.3161
Chen, Y., Shen, X., Feng, J., Lei, Z., Zhang, W., Song, X., et al. (2022). Prevalence and predictors of depression among emergency physicians: A national cross-sectional study. BMC Psychiatry 22:69. doi: 10.1186/s12888-022-03687-8
Chu, L. C. (2017). Impact of providing compassion on job performance and mental health: The moderating effect of interpersonal relationship quality. J. Nurs. Scholarsh. 49, 456–465. doi: 10.1111/jnu.12307
Cobb, S. (1976). Presidential address-1976. Social support as a moderator of life stress. Psychosom. Med. 38, 300–314. doi: 10.1097/00006842-197609000-00003
Cohen, S. (1988). Psychosocial models of the role of social support in the etiology of physical disease. Health Psychol. 7, 269–297. doi: 10.1037//0278-6133.7.3.269
Cohen, S., and McKay, G. (2020). “Social support, stress and the buffering hypothesis: A theoretical analysis,” in Handbook of psychology and health, Vol. IV. Abingdon: Taylor & Francis Press.
Cohen, S., and Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychol. Bull. 98, 310–357. doi: 10.1037/0033-2909.98.2.310
Dai, Y., Zhang, B., Sun, H., Li, Z., Shen, L., and Liu, Y. (2015). Prevalence and correlates of psychological symptoms in Chinese doctors as measured with the SCL-90-R: A meta-analysis. Res. Nurs. Health 38, 369–383. doi: 10.1002/nur.21673
Dang, W., Xu, Y., Ji, J., Wang, K., Zhao, S., Yu, B., et al. (2020). Study of the SCL-90 scale and changes in the Chinese norms. Front. Psychiatry 11:524395. doi: 10.3389/fpsyt.2020.524395
de Mélo Silva Júnior, M. L., ValençA, M. M., and Rocha-Filho, P. A. S. (2022). Individual and residency program factors related to depression, anxiety and burnout in physician residents - a Brazilian survey. BMC Psychiatry 22:272. doi: 10.1186/s12888-022-03916-0
de Wit, K. (2020). Burnout and depression among Canadian emergency physicians. CJEM 22, 559–560. doi: 10.1017/cem.2020.475
Demyttenaere, K., and Heirman, E. (2020). The blurred line between anxiety and depression: Hesitations on comorbidity, thresholds and hierarchy. Int. Rev. Psychiatry 32, 455–465. doi: 10.1080/09540261.2020.1764509
Den Oudsten, B. L., Van Heck, G. L., Van Der Steeg, A. F., Roukema, J. A., and De Vries, J. (2010). Personality predicts perceived availability of social support and satisfaction with social support in women with early stage breast cancer. Support Care Cancer 18, 499–508. doi: 10.1007/s00520-009-0714-3
Derogatis, L. R., Rickels, K., and Rock, A. F. (1976). The SCL-90 and the MMPI: A step in the validation of a new self-report scale. Br. J. Psychiatry 128, 280–289. doi: 10.1192/bjp.128.3.280
Ditzen, B., and Heinrichs, M. (2014). Psychobiology of social support: The social dimension of stress buffering. Restor. Neurol. Neurosci. 32, 149–162. doi: 10.3233/RNN-139008
Dour, H. J., Wiley, J. F., Roy-Byrne, P., Stein, M. B., Sullivan, G., Sherbourne, C. D., et al. (2014). Perceived social support mediates anxiety and depressive symptom changes following primary care intervention. Depress. Anxiety 31, 436–442. doi: 10.1002/da.22216
Eckleberry-Hunt, J., and Lick, D. (2015). Physician depression and suicide: A shared responsibility. Teach. Learn. Med. 27, 341–345. doi: 10.1080/10401334.2015.1044751
Elhadi, M., Khaled, A., Malek, A. B., El-Azhari, A. E., Gwea, A. Z., Zaid, A., et al. (2020). Prevalence of anxiety and depressive symptoms among emergency physicians in Libya after civil war: A cross-sectional study. BMJ Open 10:e039382. doi: 10.1136/bmjopen-2020-039382
Feng, L., and Yin, R. (2021). Social support and hope mediate the relationship between gratitude and depression among front-line medical staff during the pandemic of COVID-19. Front. Psychol. 12:623873. doi: 10.3389/fpsyg.2021.623873
Fornell, C., and Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 18, 39–50. doi: 10.1177/002224378101800104
González-Cabrera, J., Fernández-Prada, M., Iribar, C., Molina-Ruano, R., Salinero-Bachiller, M., and Peinado, J. (2018). Acute stress and anxiety in medical residents on the emergency department duty. Int. J. Environ. Res. Public Health 15:506. doi: 10.3390/ijerph15030506
Groen, R. N., Ryan, O., Wigman, J. T. W., Riese, H., Penninx, B., Giltay, E. J., et al. (2020). Comorbidity between depression and anxiety: Assessing the role of bridge mental states in dynamic psychological networks. BMC Med. 18:308. doi: 10.1186/s12916-020-01738-z
Guo, Y. F., Cross, W. M., Lam, L., Plummer, V., Wang, X. X., and Wang, S. S. (2021). Association between psychological capital and spiritual care competencies of clinical nurses: A multicentre cross-sectional study. J. Nurs. Manage. 29, 1713–1722. doi: 10.1111/jonm.13303
Guo, Y. F., Wang, K. F., Cross, W., Lam, L., Plummer, V., and Li, J. (2022). Quality of life in cancer patients with different preferences for nurse spiritual therapeutics: The role of psychological capital. J. Adv. Nurs. 78, 991–1000. doi: 10.1111/jan.15023
Hair, J. F. Jr., Black, W. C., Babin, B. J., and Anderson, R. E. (2010). Multivariate data analysis: A global perspective, 7th Edn. Upper Saddle River, NJ: Pearson Education.
Hart, K. E., and Hittner, J. B. (1991). Irrational beliefs, perceived availability of social support, and anxiety. J. Clin. Psychol. 47, 582–587. doi: 10.1002/1097-4679(199107)47:4<582::aid-jclp2270470418<3.0.co;2-z
Hayes, A. F. (2018). An Introduction to mediation, moderation, and conditional process analysis: A regression-baesd approach. New York, NY: Guilford Press.
Hayes, A. F., and Rockwood, N. J. (2019). Conditional process analysis: Concepts, computation, and advances in the modeling of the contingencies of mechanisms. Am. Behav. Sci. 64, 19–54. doi: 10.1177/0002764219859633
Hindmarch, I. (1998). Cognition and anxiety: The cognitive effects of anti-anxiety medication. Acta Psychiatr. Scand. Suppl. 393, 89–94. doi: 10.1111/j.1600-0447.1998.tb05972.x
Holahan, C. K., and Holahan, C. J. (1987). Self-efficacy, social support, and depression in aging: A longitudinal analysis. J. Gerontol. 42, 65–68. doi: 10.1093/geronj/42.1.65
Iheanacho, T., Maciejewski, K. R., Ogudebe, F., Chumo, F., Slade, T., Leff, R., et al. (2022). Prevalence and correlates of depression and substance use disorders in emergency department populations: A cross-sectional study at East Africa’s largest public hospital. Afr. J. Emerg. Med. 12, 307–314. doi: 10.1016/j.afjem.2022.06.008
Janicki, A. J., Frisch, S. O., Patterson, P. D., Brown, A., and Frisch, A. (2020). Emergency medicine residents experience acute stress while working in the emergency department. West. J. Emerg. Med. 22, 94–100. doi: 10.5811/westjem.2020.10.47641
Jiang, Y. (2021). Problematic social media usage and anxiety among university students during the COVID-19 pandemic: The mediating role of psychological capital and the moderating role of academic burnout. Front. Psychol. 12:612007. doi: 10.3389/fpsyg.2021.612007
Johnson, J. G., Alloy, L. B., Panzarella, C., Metalsky, G. I., Rabkin, J. G., Williams, J. B., et al. (2001). Hopelessness as a mediator of the association between social support and depressive symptoms: Findings of a study of men with HIV. J. Consult. Clin. Psychol. 69, 1056–1060. doi: 10.1037//0022-006x.69.6.1056
Joiner, T. E. (1993). Discrimination between anxiety and depression. J. Nerv. Ment. Dis. 181, 708–709. doi: 10.1097/00005053-199311000-00014
Kugbey, N., Oppong Asante, K., and Meyer-Weitz, A. (2020). Depression, anxiety and quality of life among women living with breast cancer in Ghana: Mediating roles of social support and religiosity. Support Care Cancer 28, 2581–2588. doi: 10.1007/s00520-019-05027-1
Lakey, B., and Cohen, S. (2000). “Social support theory and measurement,” in Social support measurement and intervention: A guide for health and social scientists, eds S. Cohen, L. G. Underwood, and B. H. Gottlieb (Oxford: Oxford University Press), 29–52. doi: 10.1093/med:psych/9780195126709.003.0002
Lamers, F., Van Oppen, P., Comijs, H. C., Smit, J. H., Spinhoven, P., Van Balkom, A. J., et al. (2011). Comorbidity patterns of anxiety and depressive disorders in a large cohort study: The Netherlands study of depression and anxiety (NESDA). J. Clin. Psychiatry 72, 341–348. doi: 10.4088/JCP.10m06176blu
Lin, Y. K., Lee, W. C., Kuo, L. C., Cheng, Y. C., Lin, C. J., Lin, H. L., et al. (2013). Building an ethical environment improves patient privacy and satisfaction in the crowded emergency de partment: A quasi-experimental study. BMC Med. Ethics 14:8. doi: 10.1186/1472-6939-14-8
Liu, H., Zhao, S., Jiao, M., Wang, J., Peters, D. H., Qiao, H., et al. (2015). Extent, nature, and risk factors of workplace violence in public tertiary hospitals in China: A cross-sectional survey. Int. J. Environ. Res. Public Health 12, 6801–6817. doi: 10.3390/ijerph120606801
Liu, L., Pang, R., Sun, W., Wu, M., Qu, P., Lu, C., et al. (2013). Functional social support, psychological capital, and depressive and anxiety symptoms among people living with HIV/AIDS employed full-time. BMC Psychiatry 13:324. doi: 10.1186/1471-244X-13-324
Luthans, F., Youssef, C., and Avolio, B. (2007b). Psychological capital. New York: Oxford University Press.
Luthans, F., Avolio, B. J., Avey, J. B., and Norman, S. M. (2007a). Positive psychological capital :Measurement and relationship with performance and satisfaction. Pers. Psychol. 60, 541–572. doi: 10.1111/j.1744-6570.2007.00083.x
Medisauskaite, A., and Kamau, C. (2019). Reducing burnout and anxiety among doctors: Randomized controlled trial. Psychiatry Res. 274, 383–390. doi: 10.1016/j.psychres.2019.02.075
Minglu, L., Fang, F., Guanxi, L., Yuxiang, Z., Chaoqiong, D., and Xueqin, Z. (2020). Influencing factors and correlation of anxiety, psychological stress sources, and psychological capital among women pregnant with a second child in Guangdong and Shandong province. J. Affect. Disord. 264, 115–122. doi: 10.1016/j.jad.2019.11.148
Morgan, C. D., Wiederman, M. W., and Magnus, R. D. (1998). Discriminant validity of the Scl-90 dimensions of anxiety and depression. Assessment 5, 197–201. doi: 10.1177/107319119800500210
Moscati, A., Flint, J., and Kendler, K. S. (2016). Classification of anxiety disorders comorbid with major depression: Common or distinct influences on risk? Depress. Anxiety 33, 120–127. doi: 10.1002/da.22432
Moyer, C. A., Yang, H., Kwawukume, Y., Gupta, A., Zhu, Y., Koranteng, I., et al. (2009). Optimism/pessimism and health-related quality of life during pregnancy across three continents: A matched cohort study in China, Ghana, and the United States. BMC Pregnancy Childbirth 9:39. doi: 10.1186/1471-2393-9-39
Otani, K., Suzuki, A., Matsumoto, Y., and Shirata, T. (2018). Close relation of interpersonal sensitivity with negative core beliefs about the self, the central construct of cognitive vulnerability to depression. Psychiatry Res. 263, 162–165. doi: 10.1016/j.psychres.2018.03.015
Paiva, C. E., Martins, B. P., and Paiva, B. S. R. (2018). Doctor, are you healthy? A cross-sectional investigation of oncologist burnout, depression, and anxiety and an investigation of their associated factors. BMC Cancer 18:1044. doi: 10.1186/s12885-018-4964-7
Pujo, J. M., Kraiem, H., Daniel, P., Omri, M., Fremery, A., Rémi, M., et al. (2021). Work-related stress assessment in an emergency department in French Guiana. Br. J. Nurs. 30, 540–546. doi: 10.12968/bjon.2021.30.9.540
Rahimnia, F., Mazidi, A., and Mohammadzadeh, Z. (2013). Emotional mediators of psychological capital on well-being: The role of stress, anxiety, and depression. Manag. Sci. Lett. 3, 913–926. doi: 10.1111/ecc.13346
Rajasekar, G., and Krishnan, R. (2021). Mental health of medical practitioner. Indian J. Psychol. Med. 43, 279–285. doi: 10.1177/02537176211006874
Rasmussen, K., Pedersen, A. H., Pape, L., Mikkelsen, K. L., Madsen, M. D., and Nielsen, K. J. (2014). Work environment influences adverse events in an emergency department. Dan. Med. J. 61:A4812.
Shen, X., Yang, Y. L., Wang, Y., Liu, L., Wang, S., and Wang, L. (2014). The association between occupational stress and depressive symptoms and the mediating role of psychological capital among Chinese university teachers: A cross-sectional study. BMC Psychiatry 14:329. doi: 10.1186/s12888-014-0329-1
Song, X., Li, H., Jiang, N., Song, W., Ding, N., and Wen, D. (2021). The mediating role of social support in the relationship between physician burnout and professionalism behaviors. Patient Educ. Couns. 104, 3059–3065. doi: 10.1016/j.pec.2021.04.025
Starr, L. R., Hammen, C., Connolly, N. P., and Brennan, P. A. (2014). Does relational dysfunction mediate the association between anxiety disorders and later depression? Testing an interpersonal model of comorbidity. Depress. Anxiety 31, 77–86. doi: 10.1002/da.22172
Tao, Y., Yu, H., Liu, S., Wang, C., Yan, M., Sun, L., et al. (2022). Hope and depression: The mediating role of social support and spiritual coping in advanced cancer patients. BMC Psychiatry 22:345. doi: 10.1186/s12888-022-03985-1
Ter Meulen, W. G., Draisma, S., Van Hemert, A. M., Schoevers, R. A., Kupka, R. W., Beekman, A. T. F., et al. (2021). Depressive and anxiety disorders in concert-A synthesis of findings on comorbidity in the NESDA study. J. Affect. Disord. 284, 85–97. doi: 10.1016/j.jad.2021.02.004
Tian, F., Shu, Q., Cui, Q., Wang, L., Liu, C., and Wu, H. (2020). The mediating role of psychological capital in the relationship between occupational stress and fatigue: A cross-sectional study among 1,104 Chinese physicians. Front. Public Health 8:12. doi: 10.3389/fpubh.2020.00012
Wang, W., Mehmood, A., Li, P., Yang, Z., Niu, J., Chu, H., et al. (2021b). Perceived stress and smartphone addiction in medical college students: The mediating role of negative emotions and the moderating role of psychological capital. Front. Psychol. 12:660234. doi: 10.3389/fpsyg.2021.660234
Wang, J., Cui, R., Stolarz-Fantino, S., Fantino, E., and Liu, X. (2021a). Differences in mood, optimism, and risk-taking behavior between American and Chinese college students. Front. Psychol. 12:781609. doi: 10.3389/fpsyg.2021.781609
Weber, M., Ruch, W., Littman-Ovadia, H., Lavy, S., and Gai, O. (2013). Relationships among higher-order strengths factors, subjective well-being, and general self-efficacy–The case of Israeli adolescents. Pers. Individ. Differ. 55, 322–327. doi: 10.1016/j.paid.2013.03.006
Xiao, S. Y. (1994). Theoretical foundation and research application about the social support rating scale. J. Clin. Psychiatry 4, 98–100.
Xie, J., Liu, M., Zhong, Z., Zhang, Q., Zhou, J., Wang, L., et al. (2020). Relationships among character strengths, self-efficacy, social support, depression, and psychological well-being of hospital nurses. Asian Nurs. Res. 14, 150–157. doi: 10.1016/j.anr.2020.06.002
Xu, H., Liu, X., and Zeng, P. (2022a). The mediating role of social support in the relationship between psychological capital and depression among Chinese emergency physicians. Psychol. Res. Behav. Manag. 15, 977–990. doi: 10.2147/PRBM.S360611
Xu, H., Peng, L., Wang, Z., Zeng, P., and Liu, X. (2022b). Interpersonal sensitivity on college freshmen’s depression: A moderated moderation model of psychological capital and family support. Front. Psychiatry 13:921045. doi: 10.3389/fpsyt.2022.921045
Yang, Y., and Lu, X. (2022). Social anxiety and subjective quality of life among Chinese left-behind children: The mediating role of social support. Front. Psychol. 13:836461. doi: 10.3389/fpsyg.2022.836461
Yang, Y., and Yang, P. (2022). Effect of college students’ academic stress on anxiety under the background of the normalization of COVID-19 pandemic: The mediating and moderating effects of psychological capital. Fron. Psychol. 13:880179. doi: 10.3389/fpsyg.2022.880179
Yu, M., Qiu, T., Liu, C., Cui, Q., and Wu, H. (2020). The mediating role of perceived social support between anxiety symptoms and life satisfaction in pregnant women: A cross-sectional study. Health Qual. Life Outcomes 18:223. doi: 10.1186/s12955-020-01479-w
Zhao, X., Zhang, D., Wu, M., Yang, Y., Xie, H., Li, Y., et al. (2018). Loneliness and depression symptoms among the elderly in nursing homes: A moderated mediation model of resilience and social support. Psychiatry Res. 268, 143–151. doi: 10.1016/j.psychres.2018.07.011
Keywords: depression, anxiety, psychological capital, social support availability, emergency physician, moderated mediation model
Citation: Xu H, Peng L, Wang Z and Liu X (2022) Effects of psychological capital and social support availability on anxiety and depression among Chinese emergency physicians: Testing moderated mediation model. Front. Psychol. 13:991239. doi: 10.3389/fpsyg.2022.991239
Received: 11 July 2022; Accepted: 22 November 2022;
Published: 07 December 2022.
Edited by:
Yufang Guo, Shandong University, ChinaCopyright © 2022 Xu, Peng, Wang and Liu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xin Liu, bHhAeHpobXUuZWR1LmNu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.