- 1Department of Neurology, Xiangya Hospital, Central South University, Changsha, Hunan, China
- 2Department of Neurology, Hainan General Hospital, Haikou, Hainan, China
- 3National Clinical Research Center for Geriatric Disorders, Central South University, Changsha, China
- 4Engineering Research Center of Hunan Province in Cognitive Impairment Disorders, Central South University, Changsha, China
- 5Hunan International Scientific and Technological Cooperation Base of Neurodegenerative and Neurogenetic Diseases, Changsha, China
- 6Key Laboratory of Hunan Province in Neurodegenerative Disorders, Central South University, Changsha, China
- 7Department of Geriatrics, Xiangya Hospital, Central South University, Changsha, Hunan, China
- 8Key Laboratory of Organ Injury, Aging and Regenerative Medicine of Hunan Province, Changsha, China
Background: The Chinese version of the Mini-Mental State Examination (MMSE-C) and the Beijing version of the Montreal Cognitive Assessment (MoCA-BJ) are the most commonly used scales to screen for Alzheimer’s disease (AD) among Chinese patients; however, their consistency varies according to populations and languages. Equivalent conversion of MMSE-C and MoCA-BJ scores is important for meta-analysis.
Materials and methods: MMSE-C and MoCA-BJ scoring were performed on the enrolled patients with AD (n = 332). Consistency analysis of MMSE-C and MoCA-BJ scores of patients in the conversion groups was performed. The circle-arc method was used to convert the MMSE-C scores of the conversion groups into MoCA-BJ scores, and the conversion formula was generated. The MMSE-C data of the verification group was converted to MoCA-BJ according to the formula, and the consistency analysis of the original MoCA-BJ of the verification group and the converted MoCA-BJ was performed to verify the conversion model.
Results: The results of the consistency analysis of MMSE-C and MoCA-BJ in group A showed that the correlation coefficients of the total group, high education years subgroup, medium education years subgroup, and low education years subgroup were 0.905 (P < 0.001), 0.874 (P < 0.001), 0.949 (P < 0.001), and 0.874 (P < 0.001), respectively, with high consistency and statistical significance. After applying the circle-arc method for equivalent conversion, the consistency analysis results of the original and the converted MoCA-BJ of the patients in group B of the total group, high education years subgroup, medium education years subgroup, and low education years subgroup were 0.891 (P < 0.001), 0.894 (P < 0.001), 0.781 (P < 0.001), 0.909 (P < 0.001), respectively, with high consistency and statistical significance.
Conclusion: We established and validated a model of MMSE-C and MoCA-BJ score conversion for Chinese patients with AD using the circle-arc method. This model could be useful for multi-centers clinical trials and meta-analysis.
Introduction
Alzheimer’s disease (AD) is a neurodegenerative disease characterized by progressive cognitive dysfunction and abnormal mental behavior (Sperling et al., 2011). Its two diagnostic neuropathological hallmarks are numerous extracellular deposits of amyloid-β (Aβ) plaques and neurofibrillary tangles (Braak and Braak, 1996). Neuropsychological assessment is used to assist in the diagnosis of AD and evaluate the efficacy of the treatment (Ashford et al., 2006). Currently, there are various neurological assessment scales in clinical practice (Tsoi et al., 2015); the Mini-Mental State Examination (MMSE) (Folstein et al., 1975) and the Montreal Cognitive Assessment (MoCA) (Nasreddine et al., 2005) are the two most common ones.
The MMSE scale covers six aspects, including orientation (time and place), registration, attention and calculation, recall, language (naming, retelling, listening and understanding, reading, and writing), and visual construction, with a total score of 30 (Folstein et al., 1975). The MMSE score abnormal interpretation criteria varies according to the educational levels of the subjects (Tombaugh and McIntyre, 1992).
The MoCA scale involves eight cognitive domains, including attention and concentration, executive function, memory, language, visuospatial skills, abstract thinking, computation, and orientation, with a total score of 30 (Nasreddine et al., 2005). The boundary value of the MoCA scale is 26 points for normal and cognitive impairment. If the duration of education of the subject is not more than 12°years, one point is added to the original score (Lee et al., 2008; Siciliano et al., 2019).
The MMSE is greatly affected by age, socioeconomic status, and education level (Crum et al., 1993), for example, it is not sensitive enough for elderly subjects (> 75–80°years), patients with mild cognitive impairment, and subjects with a high education level (Nys et al., 2005). Meanwhile, MoCA showed a higher detection rate for mild cognitive impairment (MCI) than MMSE and a lower detection rate for moderate and severe dementia than MMSE (Roalf et al., 2012; Huang et al., 2018). MoCA includes more heavily weighted visuospatial and executive function measurements, which may reduce the impact of the ceiling and learning effects (Kasten et al., 2010) but increase the likelihood of the floor effect (Federico et al., 2018). MoCA also has limitations, its data should stratified by age, education, ethnically diverse, and population (Dong et al., 2013). MoCA is less widely used as MMSE (Dong et al., 2013).
Mini-mental state examination (MMSE) and MoCA can be affected by differences in culture and language (Larner, 2012; Verghese et al., 2012). The MMSE and MoCA have been translated into local Chinese language. In China, the Chinese version of the MMSE (MMSE-C) (Zhang, 2003) and the Beijing version of the Montreal Cognitive Assessment (MoCA-BJ) (Yu et al., 2012) are the two most widely used.
Given that both scales are widely used in clinical screening, as well as in clinical trials and cohort studies, a rule to facilitate conversions and comparison of data from different centers and clinical trials would be essential (Wong et al., 2013; Helmi et al., 2016). Therefore, the establishment of validity consistency conversion of MMSE-C and MoCA-BJ is not only conducive to the continuity of cognitive tracking in clinical settings but also to the comparison and integration of cognitive data from heterogeneous longitudinal studies.
Therefore, this study had the following aims: (1) to estimate the level of agreement between MMSE-C and MoCA-BJ within the total and different educational levels Chinese AD patients, (2) to derive a conversion model for the two scales using the circle-arc method, and (3) to validate the conversion model in a small sample of patients with AD.
Materials and methods
Participants
We enrolled 322 patients who met the diagnostic criteria of “clinically possible and probable AD” in the 2011 NIA-AA diagnostic guidelines, from January 1, 2016, to April 1, 2019, at Xiangya Hospital of Central South University. Patients with structural brain lesions (tumor or stroke), and patients with a previous diagnosis of schizophrenia or bipolar disorder with psychotic features were excluded. We included patients who undertook both the MMSE-C and MoCA-BJ in the same session. The study was approved by the Ethics Committee of Xiangya Hospital of Central South University, and the subjects provided informed consent.
Procedures
Patients with AD (n = 322) were randomly divided into the conversion group A (n = 161) and the validation group B (n = 161) and stratified according to their length of education. The consistency of MMSE-C and MoCA-BJ was analyzed for group A data, and the conversion formula was generated using the Circular-arc method to obtain the MoCA-BJ score from 0 to 30 MMSE-C points. According to the conversion table obtained above, the converted MoCA-BJ was obtained for group B, and the consistency of the formula was verified by comparing the converted MoCA-BJ with the original MoCA-BJ in group B.
Equivalent conversion method
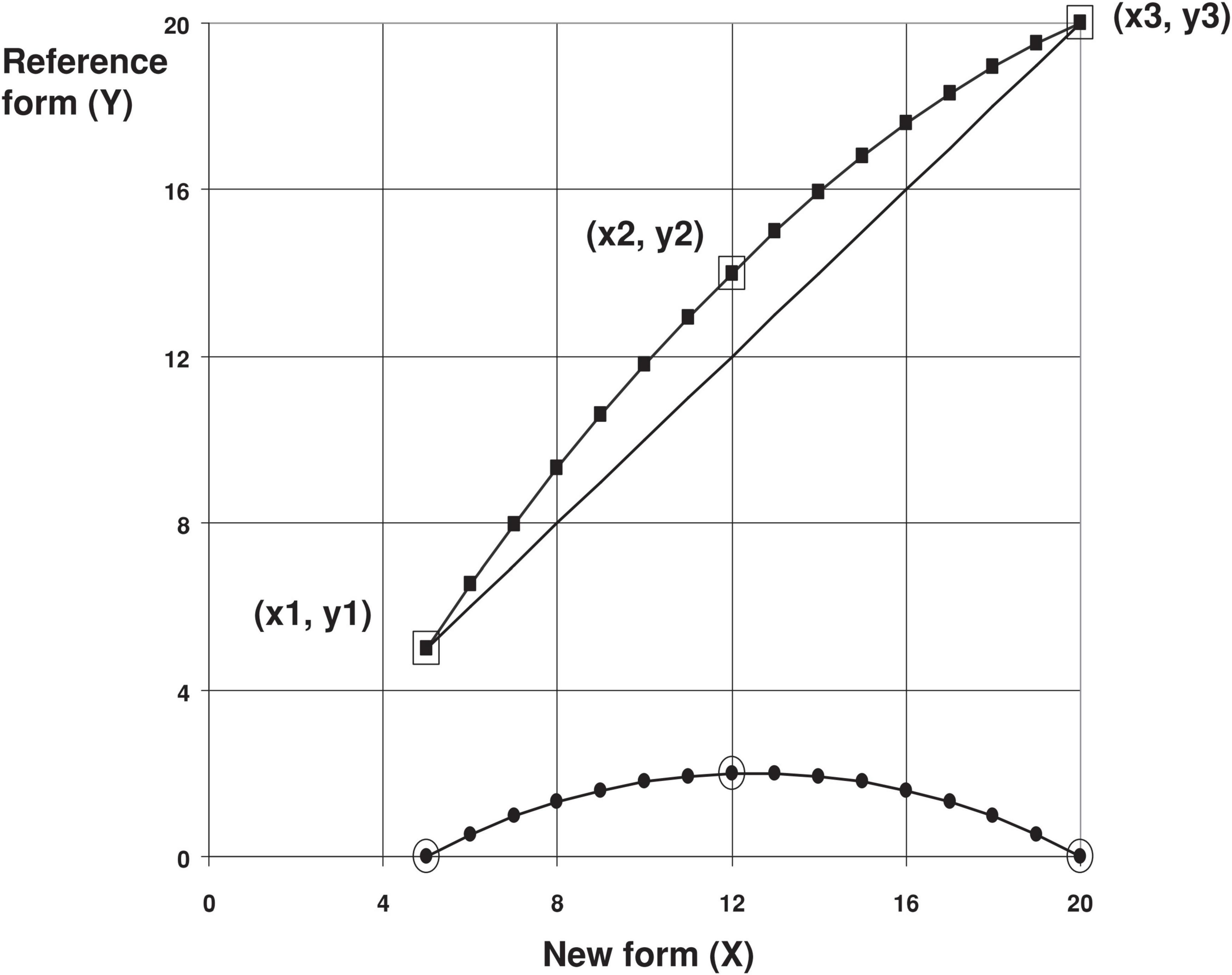
The circle-arc method (Livingston and Kim, 2009) is an equivalent conversion method for grades and rating scales, and the MoCA-BJ conversion of MMSE-C is more consistent than the linear method. Therefore, this study applies this method to the MoCA-BJ conversion of MMSE-C. According to the nadir (x1, y1), zenith (x3, y3), and midpoint (x2, y2) (Figure 1) of a set of data, the method applies the following formula for calculation and conversion to obtain the converted data.
(This formula is used when Y* is positive)
(This formula is used when Y* is negative)
Statistical analysis
SPSS 19.0 software was used for data analysis. Categorical variables are expressed in quantity (percentage) and analyzed using the chi-square test. Continuous variables are expressed as mean ± standard deviation or median (interquartile interval, IQR), according to the situation, and analyzed by a t-test or Mann–Whitney U test. Pearson or Spearman correlation analysis was used to test the consistency, and statistical significance was set at P < 0.05.
Results
Patients’ characteristics
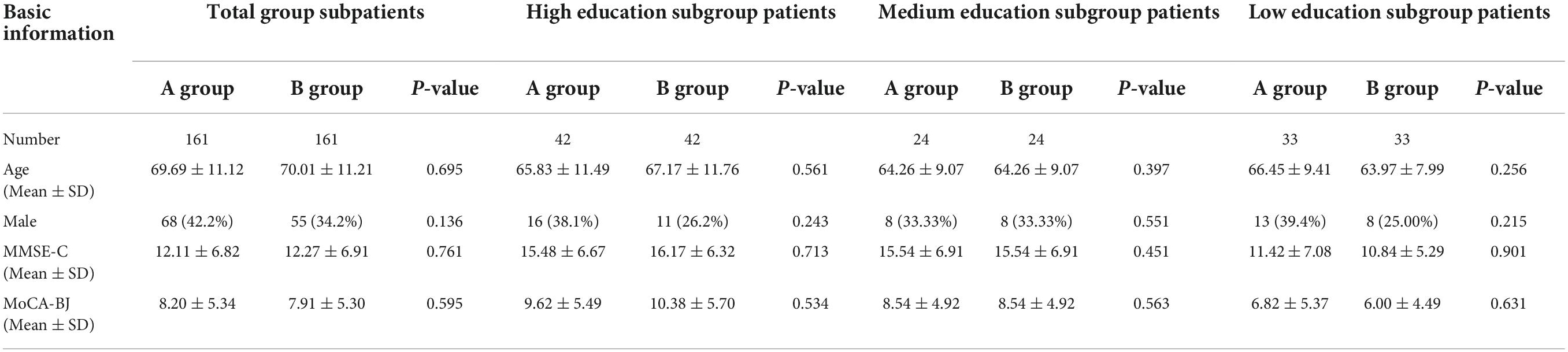
A total of 322 patients with AD were included in this study. Group A of the total group included 161 patients, their mean age was 69.69 ± 11.12°years, and 68 (42.2%) of them were men. The mean MMSE-C and MoCA-BJ scores were 12.11 ± 6.82 (range, 2–28) and 8.2 ± 5.34 (range, 0–25), respectively. Group B of the total group included 161 patients; the mean age was 70.01 ± 11.21°years and 55 (34.2%) of them were men. The mean MMSE-C and MoCA-BJ scores were 12.27 ± 6.91 (range, 1–27) and 7.91 ± 5.30 (range, 0–22), respectively. Depending on the level of education, the participants were classified into three subgroups: low education years subgroup (6 or fewer years of education, n = 66, group A = 33, group B = 33), medium education years subgroup (7–9°years of education, n = 48, group A = 24, group B = 24), and high education years subgroup (10 or more years of education, n = 84, group A = 42, group B = 42). The demographic and scale data according to the four groups are presented in Table 1. There were no statistically significant differences in age, sex, MMSE-C, or MoCA-BJ between groups A and B.
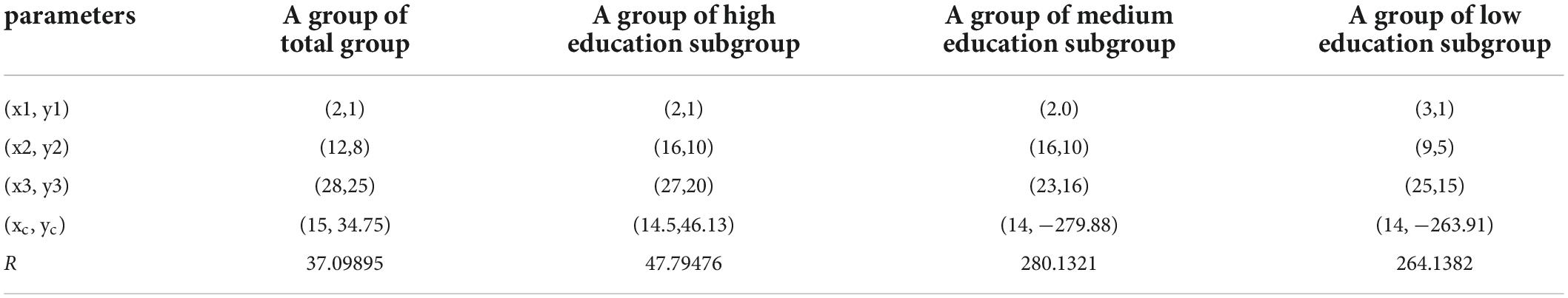
Applying the circle-arc method for equivalent conversion
Based on the data nadir (x1, y1), zenith (x3, y3), and midpoint (x2, y2) of group A of every subgroup (Table 2), we used the circle-arc formula to calculate the relevant parameters such as xc, yc, and r. The MMSE-C scale in group B was then substituted into the formula to get converted MoCA-BJ of group B. The same flow passes were applied in each subgroup, and the MMSE-C scale and converted MoCA-BJ of group B were shown in Table 3.
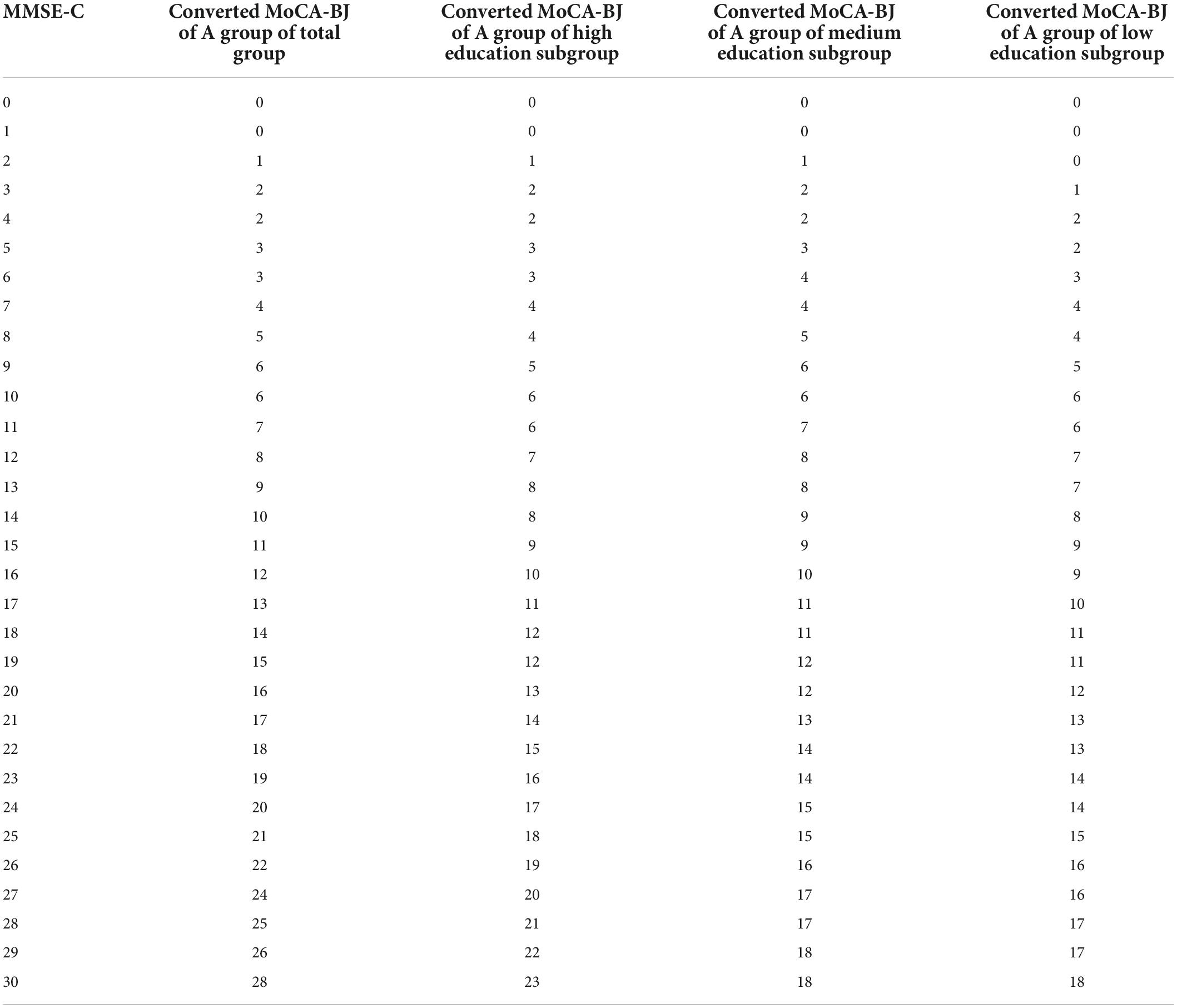
Table 3. Mini-mental state examination (MMSE-C) and converted montreal cognitive assessment (MoCA-BJ) of group.
The distribution of mini-mental state examination and original montreal cognitive assessment of group A, converted and original montreal cognitive assessment of group B, and converted montreal cognitive assessment and original mini-mental state examination of group B
The original MoCA-BJ and MMSE-C of group A of the total group were approximately linearly distributed, indicating good consistency (Figure 2A). The converted and the original MoCA-BJ in group B of the total group were approximately linear (Figure 2B). The distribution of the converted MoCA-BJ and MMSE-C scores in group B of the total group were also approximately linear (Figure 2C). The original MoCA-BJ and MMSE-C in group A of each subgroup were approximately linearly distributed, indicating good consistency (Figures 2D,G,J). The converted and original MoCA-BJ in group B of each subgroup were approximately linear (Figures 2E,H,K, respectively). The converted MoCA-BJ and MMSE-C in group B of each subgroup were approximately linear (Figures 2F,I,L, respectively).
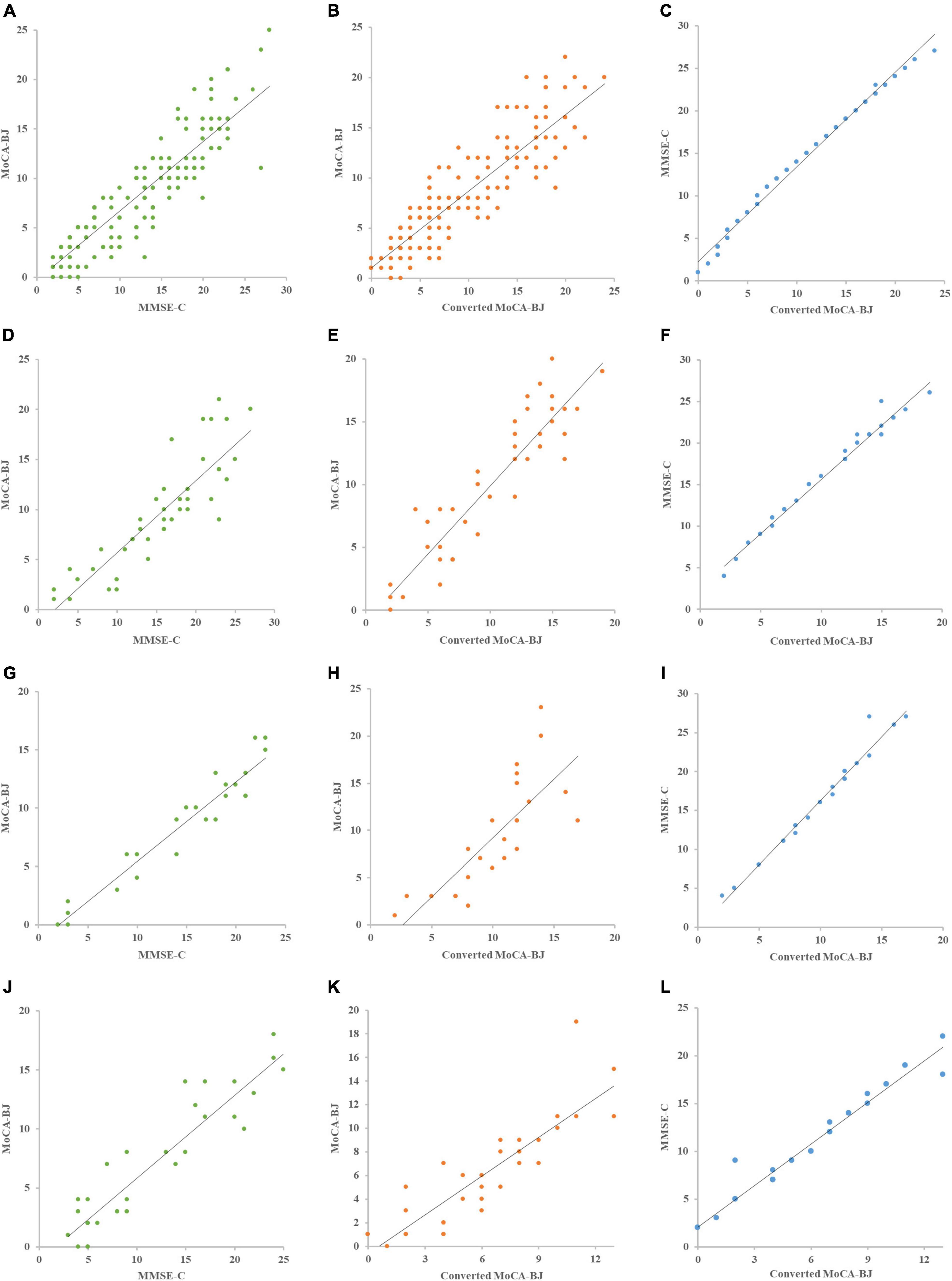
Figure 2. Mini-mental state examination, montreal cognitive assessment, converted MoCA-BJ distribution scatter plot of groups. (A–C) The MMSE-C, MoCA-BJ, and converted MoCA-BJ distribution scatter plot of tatol group, (D–F) the MMSE-C, MoCA-BJ, and converted MoCA-BJ distribution scatter plot of high education subgroup, (G-I) the MMSE-C, MoCA-BJ, and converted MoCA-BJ distribution scatter plot of medium education subgroup, (J-L) the MMSE-C, MoCA-BJ, and converted MoCA-BJ distribution scatter plot of low education subgroup.
Consistency statistical analysis of mini-mental state examination and montreal cognitive assessment of group A and converted montreal cognitive assessment and original montreal cognitive assessment of group B
Consistency analysis of MMSE-C and MoCA-BJ in group A of the total group showed that the correlation coefficient was 0.905 (P < 0.001) (Table 4). After equivalent conversion by the circle-arc method, the consistency analysis of the original and the converted MoCA-BJ in group B of the total group showed that the correlation coefficient was 0.891 (P < 0.001) (Table 4). The consistency analysis of MMSE-C and MoCA-BJ in group A of each subgroups were 0.874 (P < 0.001), 0.949 (P < 0.001), and 0.874 (P < 0.001) (Table 4), respectively. After equivalent conversion by the circle-arc method, consistency analysis of the original and the converted MoCA-BJ in group B of each subgroups showed that the correlation coefficients were 0.894 (P < 0.001), 0.781 (P < 0.001), and 0.909 (P < 0.001) (Table 4), respectively.
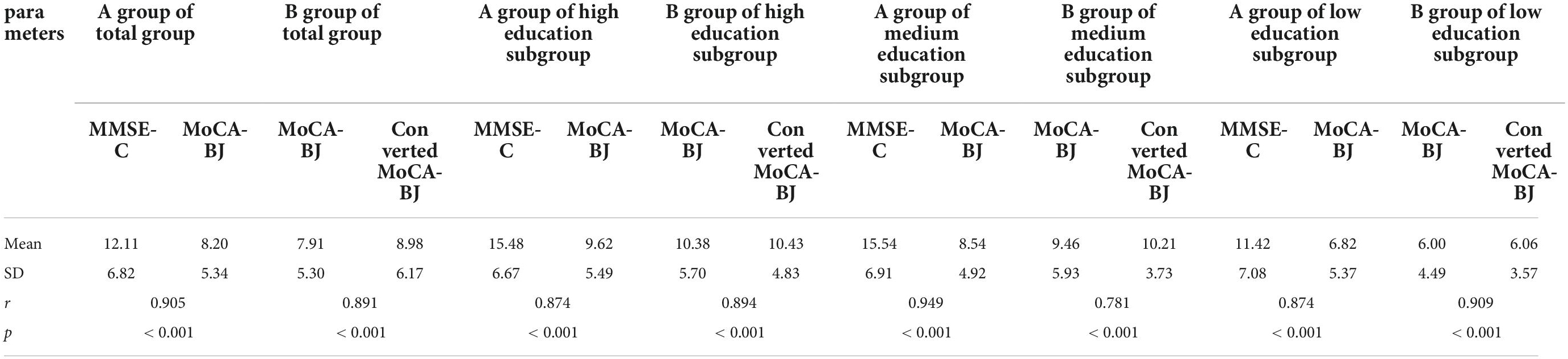
Table 4. Consistency analysis of montreal cognitive assessment (MoCA-BJ) with mini-mental state examination (MMSE-C) or converted montreal cognitive assessment (MoCA-BJ).
Discussion
In this study, Chinese patients with AD were selected for consistency analysis of MMSE-C and MoCA-BJ scores, and the correlation coefficient was 0.905 (P < 0.001), which was consistent with previous findings (Cao et al., 2012; Lam et al., 2013; Chen et al., 2016). In the subgroup stratified by education background, the consistency analysis of the two scales was also statistically significant. This result suggests that the two Chinese versions of the scales are highly correlated and could undergo equivalent conversion.
In this study, MoCA-BJ and MMSE-C were transformed by the circle-arc method and a transformation model was verified. Most previous studies have used the equal percentile equivalence method or the linear equivalence method to convert the MMSE-C and MoCA-BJ scores. For example, the equivalent percentile equivalency method was used in patients with AD (Roalf et al., 2017), all-cause dementia (Bergeron et al., 2017), and Parkinson’s disease (Van Steenoven et al., 2014) to explore the consistency of MoCA-BJ conversion into MMSE-C, and the conclusions were inconsistent. Therefore, later studies have used the equal percentile equivalency method plus linear smoothing to convert MMSE and MoCA in PD and the control group (Lawton et al., 2016), and the results show that the original and the converted MMSE have good consistency, but that makes the calculations harder. The circle-arc method uses the two endpoints and one middle point of the data to obtain the conversion of two kinds of data based on not establishing the computational linear model. The method can be used in small samples (Livingston and Kim, 2009) and can be requires simple calculations. The equivalent design of the arc method can be applied to cases where the available sample of the tester is not enough for equivalent conversion by the traditional method (Sooyeon and Livingston, 2009). The main advantage of the equivalent percentile equivalency method is its accuracy in the upper and lower tail of the score distribution (Sooyeon and Livingston, 2009), which helps avoid the difficulty in equivalent conversion caused by the estimated score probability in the innumerable data area of the scoring scale. In the process of equivalent conversion, the circle-arc method is simple: it involves adding the smoothing model to the equivalent percentile equivalency method.
In this study, a small sample was used to verify the MMSE-C and MoCA-BJ transformation models established by the arc method above. In B group of the total group, the converted MoCA-BJ had a high consistency with the original MoCA-BJ. In addition, subgroup analysis was conducted based on the years of education. No matter if one was in the high years of education, medium years of education, or low years of education subgroups, the converted MoCA-BJ had a high consistency with the original MoCA-BJ in group B, which was consistent with the relevant research results (Van Steenoven et al., 2014; Chen et al., 2016; Helmi et al., 2016; Lawton et al., 2016).
This study had some limitations. First, it was a single-center study and has not been validated in other centers. Second, the conversion of MMSE-C to MOCA-BJ was only performed in patients with AD, and further validation in other patients is required. Although there was stratification according to educational background, the study did not test whether there were differences in conversion between different educational backgrounds. Therefore, the next step is to expand the sample size to verify this transformation.
Conclusion
This study found that the MMSE-C and MoCA-BJ have higher consistency in Chinese patients with AD. We established and validated a model of MMSE-C and MoCA-BJ score conversion for Chinese patients with AD using the circle-arc method. The transformation model can allow multiple centers and clinical trials to apply the equivalent conversion of MMSE-C scores to MoCA-BJ scores and further apply it to meta-analysis.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
LW was the guarantor and contributed to the conception of the study. LZ and ZL participated in the analysis and interpretation of the data and drafted the initial manuscript. HL participated in the cognitive assessment. BJ, XL, YZ, and LS revised the article critically for important intellectual content. All authors read and approved the final manuscript.
Funding
This study supported by the National Key R&D Program of China (Nos. 2020YFC2008500, 2017YFC0840100, 2017YFC0840104, 2018YFC1312003, and 2016YFC1306000), the National Natural Science Foundation of China (Nos. 81671075, 81971029, 82071216, and 81901171), Hunan Innovative Province Construction Project (No. 2019SK2335), the Youth Science Foundation of Xiangya Hospital (No. 2018Q020), and the Hainan Province Clinical Medical Center.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ashford, J. W., Borson, S., O’Hara, R., Dash, P., Frank, L., Robert, P., et al. (2006). Should older adults be screened for dementia? Alzheimers Dement 2, 76–85. doi: 10.1016/j.jalz.2006.02.005
Bergeron, D., Flynn, K., Verret, L., Poulin, S., Bouchard, R. W., Bocti, C., et al. (2017). Multicenter Validation of an MMSE-MoCA Conversion Table. J. Am. Geriatr. Soc. 65, 1067–1072. doi: 10.1111/jgs.14779
Braak, H., and Braak, E. (1996). Evolution of the neuropathology of Alzheimer’s disease. Acta Neurol. Scand. Suppl. 165, 3–12. doi: 10.1111/j.1600-0404.1996.tb05866.x
Cao, L., Hai, S., Lin, X., Shu, D., Wang, S., Yue, J., et al. (2012). Comparison of the saint louis university mental status examination, the mini-mental state examination, and the montreal cognitive assessment in detection of cognitive impairment in chinese elderly from the geriatric department. J. Am. Med. Dir. Assoc. 13, 626–629. doi: 10.1016/j.jamda.2012.05.003
Chen, K. L., Xu, Y., Chu, A. Q., Ding, D., Liang, X. N., Nasreddine, Z. S., et al. (2016). Validation of the chinese version of montreal cognitive assessment basic for screening mild cognitive impairment. J. Am. Geriatr. Soc. 64, e285–e290. doi: 10.1111/jgs.14530
Crum, R. M., Anthony, J. C., Bassett, S. S., and Folstein, M. F. (1993). Population-based norms for the Mini-Mental State Examination by age and educational level. JAMA 269, 2386–2391.
Dong, Y., Yean Lee, W., Hilal, S., Saini, M., Wong, T. Y., Chen, C. L., et al. (2013). Comparison of the Montreal Cognitive Assessment and the Mini-Mental State Examination in detecting multi-domain mild cognitive impairment in a Chinese sub-sample drawn from a population-based study. Int. Psychogeriatr. 25, 1831–1838. doi: 10.1017/S1041610213001129
Federico, A., Tinazzi, M., and Tamburin, S. (2018). MoCA for cognitive screening in Parkinson’s disease: Beware of floor effect. Mov. Disord. 33:499. doi: 10.1002/mds.27329
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). “Mini-mental state”, A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res 123, 189–198. doi: 10.1016/0022-3956(75)90026-6
Helmi, L., Meagher, D., O’Mahony, E., O’Neill, D., Mulligan, O., Murthy, S., et al. (2016). Agreement and conversion formula between mini-mental state examination and montreal cognitive assessment in an outpatient sample. World J. Psychiatry 6, 358–364. doi: 10.5498/wjp.v6.i3.358
Huang, L., Chen, K. L., Lin, B. Y., Tang, L., Zhao, Q. H., Lv, Y. R., et al. (2018). Chinese version of Montreal Cognitive Assessment Basic for discrimination among different severities of Alzheimer’s disease. Neuropsychiatr. Dis. Treat 14, 2133–2140. doi: 10.2147/NDT.S174293
Kasten, M., Bruggemann, N., Schmidt, A., and Klein, C. (2010). Validity of the MoCA and MMSE in the detection of MCI and dementia in Parkinson disease. Neurology 73, 1738–1745. doi: 10.1212/WNL.0b013e3181e7948a
Lam, B., Middleton, L. E., Masellis, M., Stuss, D. T., Harry, R. D., Kiss, A., et al. (2013). Criterion and convergent validity of the Montreal cognitive assessment with screening and standardized neuropsychological testing. J. Am. Geriatr. Soc. 61, 2181–2185. doi: 10.1111/jgs.12541
Lawton, M., Kasten, M., May, M. T., Mollenhauer, B., Schaumburg, M., and Liepelt-Scarfone, I. (2016). Validation of conversion between mini-mental state examination and montreal cognitive assessment. Mov. Disord. 31, 593–596. doi: 10.1002/mds.26498
Lee, J. Y., Cho, S. J., Na, D. L., Kim, S. K., Youn, J. H., Kwon, M., et al. (2008). Brief screening for mild cognitive impairment in elderly outpatient clinic: validation of the Korean version of the Montreal Cognitive Assessment. J. Geriatr. Psychiatry Neurol. 21, 104–110. doi: 10.1177/0891988708316855
Livingston, S. A., and Kim, S. (2009). The Circle-Arc Method for Equating in Small Samples. J. Educ. Meas. 46, 330–343. doi: 10.1177/0013164419878483
Nasreddine, Z. S., Phillips, N. A., Bédirian, V., Charbonneau, S., Whitehead, V., Collin, I., et al. (2005). The Montreal Cognitive Assessment, MoCA: a brief screening tool for mild cognitive impairment. J. Am. Geriatr. Soc. 534, 695–699. doi: 10.1111/j.1532-5415.2005.53221.x
Nys, G. M., van Zandvoort, M. J., de Kort, P. L., Jansen, B. P., Kappelle, L. J., and de Haan, E. H. (2005). Restrictions of the Mini-Mental State Examination in acute stroke. Arch. Clin. Neuropsychol. 205, 623–629. doi: 10.1016/j.acn.2005.04.001
Roalf, D. R., Moberg, P. J., Xie, S. X., Wolk, D. A., Moelter, S. T., and Arnold, S. E. (2012). Comparative accuracies of two common screening instruments for classification of Alzheimer’s disease, mild cognitive impairment, and healthy aging. Alzheimers Dement 9, 529–537. doi: 10.1016/j.jalz.2012.10.001
Roalf, D. R., Moore, T. M., Mechanic-Hamilton, D., Wolk, D. A., Arnold, S. E., Weintraub, D. A., et al. (2017). Bridging cognitive screening tests in neurologic disorders: A crosswalk between the short Montreal Cognitive Assessment and Mini-Mental State Examination. Alzheimers Dement 13, 947–952. doi: 10.1016/j.jalz.2017.01.015
Siciliano, M., Chiorri, C., Passaniti, C., Sant’Elia, V., Trojano, L., and Santangelo, G. (2019). Comparison of alternate and original forms of the Montreal Cognitive Assessment (MoCA): an Italian normative study. Neurol. Sci. 40, 691–702. doi: 10.1007/s10072-019-3700-7
Sooyeon, K., and Livingston, S. A. (2009). Methods of linking with small samples in a common-Item design: An Empirical Comparison. Educ. Test. Serv. 2009, i1–i4.
Sperling, R. A., Aisen, P. S., Beckett, L. A., Bennett, D. A., Craft, S., Fagan, A. M., et al. (2011). Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement 73, 280–292. doi: 10.1016/j.jalz.2011.03.003
Tombaugh, T. N., and McIntyre, N. J. (1992). The mini-mental state examination: a comprehensive review. J. Am. Geriatr. Soc. 409, 922–935. doi: 10.1111/j.1532-5415.1992.tb01992.x
Tsoi, K. K., Chan, J. Y., Hirai, H. W., Wong, S. Y., and Kwok, T. C. (2015). Cognitive tests to detect dementia: A systematic review and meta-analysis. JAMA. Intern. Med. 1759, 1450–1458.
Van Steenoven, I., Aarsland, D., Hurtig, H., Chen-Plotkin, A., Duda, J. E., Rick, J., et al. (2014). Conversion between mini-mental state examination, montreal cognitive assessment, and dementia rating scale-2 scores in Parkinson’s disease. Mov. Disord. 29, 1809–1815. doi: 10.1002/mds.26062
Verghese, J., Noone, M. L., Johnson, B., Ambrose, A. F., Wang, C., Buschke, H., et al. (2012). Picture-based memory impairment screen for dementia. J. Am. Geriatr. Soc. 60, 2116–2120. doi: 10.1111/j.1532-5415.2012.04191.x
Wong, G. K., Lam, S. W., Wong, A., Ngai, K., Poon, W. S., and Mok, V. (2013). Comparison of montreal cognitive assessment and mini-mental state examination in evaluating cognitive domain deficit following aneurysmal subarachnoid haemorrhage. PLoS One 8:e59946. doi: 10.1371/journal.pone.0059946
Yu, J., Li, J., and Huang, X. (2012). The Beijing version of the Montreal Cognitive Assessment as a brief screening tool for mild cognitive impairment: a community-based study. BMC. Psychiatry. 12:156. doi: 10.1186/1471-244X-12-156
Keywords: MMSE-C, MoCA-BJ, AD, circle-arc method, consistency analysis, conversion model
Citation: Zhou L, Lin Z, Jiao B, Liao X, Zhou Y, Li H, Shen L and Weng L (2022) Consistency analysis and conversion model establishment of mini-mental state examination and montreal cognitive assessment in Chinese patients with Alzheimer’s disease. Front. Psychol. 13:990666. doi: 10.3389/fpsyg.2022.990666
Received: 10 July 2022; Accepted: 30 August 2022;
Published: 23 September 2022.
Edited by:
Emilia Salvadori, University of Florence, ItalyReviewed by:
Edoardo Nicolò Aiello, University of Milano-Bicocca, ItalyAndrea Bosco, University of Bari Aldo Moro, Italy
Copyright © 2022 Zhou, Lin, Jiao, Liao, Zhou, Li, Shen and Weng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ling Weng, bGluZ3dlbmdAY3N1LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Lu Zhou
Lu Zhou Zhichuan Lin2†
Zhichuan Lin2† Bin Jiao
Bin Jiao Yafang Zhou
Yafang Zhou Lu Shen
Lu Shen Ling Weng
Ling Weng