
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 19 October 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.968902
This article is part of the Research TopicCOVID-19: Vaccine and Vaccination CommunicationView all 28 articles
 Hai The Hoang1
Hai The Hoang1 Xuan Thanh Kieu Nguyen2
Xuan Thanh Kieu Nguyen2 Son Van Huynh3
Son Van Huynh3 Thuy Doan Hua3
Thuy Doan Hua3 Hien Thi Thuy Tran3
Hien Thi Thuy Tran3 Vinh-Long Tran-Chi3*
Vinh-Long Tran-Chi3*The Coronavirus disease pandemic of 2019 is a vast worldwide public health hazard, impacting people of all ages and socioeconomic statuses. Vaccination is one of the most effective methods of controlling a pandemic like COVID-19. This study aims to investigate the relationship between the number of vaccination injections and fear of COVID-19 and test whether beliefs benefit from vaccination COVID-19 mediate the effect of fear of COVID-19 on the number of vaccination injections. A total of 649 Vietnamese adults were enrolled online to finish answering, including scales The Health Belief Model (HBM) and The Fear of COVID-19 (FCV-19S), consisting of 340 (52.4%) males and 309 (47.6%) females. The data were analyzed using variance, regression, and a simple mediation model. The total score of COVID-19 fear was M = 22.26, SD = 5.49. Vietnamese fear of COVID-19 was at a medium level. Our results suggest that 18- to 20-year-olds are more fearful of COVID-19 than others. People who received the first dosage exhibited a greater fear of COVID-19 than those who received the second dose and were not inoculated. Additionally, the beliefs benefit of vaccination COVID-19 has a role in the relationship between the number of vaccination injections and fear of COVID-19. During the pandemic, adults in Vietnam are more afraid of COVID-19 than during prior outbreaks. Besides, the Vietnamese populace demonstrated a considerable demand for and high acceptability of the COVID-19 vaccine. The current study indicates that psychological counselors and therapists should counsel clients on the value of vaccination and address the fear of COVID-19 as public understanding of the benefits of vaccines increases. To further clarify the effect of this issue on the correlation between fear of COVID-19 and the number of vaccinations, the results of this study indicate that the existing vaccine communication factor for COVID-19 vaccination should be modified to increase confidence in the benefits of immunization.
In December 2019, an outbreak of disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was discovered in Wuhan, China (Lu et al., 2020). On 11 March 2020, the World Health Organization (WHO) declared COVID-19 a global pandemic (McKay et al., 2020). Because of its great transmission capacity, the virus spread quickly worldwide, infecting nearly all countries in a short period (Rothe et al., 2020). Internationally, about 278 million COVID-19 infections and 5.4 million fatalities were documented as of 26 December 2021 (World Health Organization, 2021a). During the epidemic, novel COVID-19 variants known as Delta (B.1.617.2) and Omicron (B.1.1.529) were more aggressive and transmissible than previously circulating strains (Shiehzadegan et al., 2021; Ferré et al., 2022). The number of cases in this spread of the new type has been fast-growing, impacting countries all over the world (Johnson, 2022).
Vietnam has experienced four epidemic waves, with cases increasing in later waves (Hoang et al., 2022). Prior to April 2021, Vietnam was one of the few countries in the world that had avoided the COVID-19 pandemic (Quach and Hoang, 2020). As a result of proactive disease preventive measures, the number of confirmed cases was low, with the majority of them were in people entering the country (Dao and Nguyen, 2020). However, more than a year after the first case was reported, Vietnam entered the fourth pandemic wave on 27 April 2021 (Hoang et al., 2022). During the ongoing wave, 1,728,405 confirmed cases and 39,133 deaths were recorded on 31 December 2021 (Ministry of Health, 2021b). The country accounts for 99.6% and 99.9% of total cases and deaths, respectively (Hoang et al., 2022). This epidemic is regarded as the most severe and has resulted in the greatest number of deaths (Le et al., 2021).
Faced with this dire situation, the Vietnamese government implemented emergency rules across the nation, imposing further limitations such as school closures, staying at home, and only venturing outside for food purchases or emergencies (Minister, 2020). These measures, however, have had a negative psychological (Brooks et al., 2020), social (Chen et al., 2020), and economic impacts (Nicola et al., 2020).
The coronavirus disease 2019 (COVID-19) pandemic has imposed a significant illness burden worldwide, and there are no antiviral therapies for COVID-19 (Huang et al., 2020). Vaccination is one of the most efficient and cost-effective strategies for public health, contributing to the decreased incidence of many infectious illnesses (Rémy et al., 2015). Similarly, vaccines against COVID-19 are critical for preventing and controlling COVID-19 (Lurie et al., 2020). Because immunization is the most effective health intervention for preventing and controlling COVID-19, experts from all over the globe fought to create a safe and effective vaccine at record speed (Weintraub et al., 2021). As of 31 December 2021, a total of 9.14 billion vaccine doses have been administered (World Health Organization, 2021b), and the most widely used are mRNA vaccines, including the BNT162b2 (Pfizer-BioNTech, New York, NY, USA—Mainz, Germany) and mRNA-1273 (Moderna, Cambridge, MA, USA) vaccines, and viral vector vaccines, such as Ad26.CoV2.S (Johnson & Johnson, New Brunswick, NJ, USA), ChAdOx (AstraZeneca, Cambridge, UK), Sputnik V (Gamaleya Research Institute of Epidemiology and Microbiology, Moscow, Russia), and the inactivated virus alum-adjuvanted candidate vaccine CoronaVac (Sinovac, Beijing, China) (Kyriakidis et al., 2021; World Health Organization, 2021b).
In Vietnam, to date, vaccines in Emergency Use Authorization by NRA consist of AstraZeneca, Pfizer, Moderna, Johnson & Johnson (Janssen), Sinopharm BIBP, Sputnik V, Hayat-Vax COVID-19 (Sinopharm manufacturing site), and Abdala, and recently Covaxin (produced by Bharat Biotech International Limited, India) (Nguyen et al., 2021b). COVID-19 immunization began in Vietnam on 8 March 2021, with frontline healthcare personnel, followed by essential service providers, teachers, persons with chronic conditions, and those living in epidemic regions (Nguyen et al., 2021b). Subsequently, Vietnam's largest-ever COVID-19 vaccination campaign started in July 2021 (Ministry of Health, 2021a). As of 26 December, a total of 146,335,052 doses had been administered: 77,138,616 individuals aged 12 years and older had finished the first dosage (78.5% of the total population) and 66,402,056 people aged 12 years and older had completed the second dose (67.6% of the total population) (Ministry of Health, 2021b). Despite this, insufficient evidence on new vaccinations' effectiveness and long-term negative effects generate apprehension among the general public when determining whether to receive the COVID-19 vaccine (Jain et al., 2021). As of January 2022, only 61% of the world's population had gotten at least one dosage of COVID-19 (Opel et al., 2020). Although significant progress has been achieved, there are still significant hurdles ahead in future COVID-19 immunization, one of which is the public acceptability of the COVID-19 vaccine (Rosen et al., 2021). However, for the vaccine to be successful, it is expected that at least 70–80% of the population would need to get at least one dose before becoming resistant to the COVID-19 virus (Bartsch et al., 2020).
It has been shown that the success of any vaccination program is based on how well the public accepts vaccines, which is influenced by various concerns of the public (Dror et al., 2020; Pogue et al., 2020). In Vietnam, a study of 425 individuals with chronic diseases showed that while they had good beliefs about the vaccination, they were concerned about its adverse effects, need, and cost (Huynh et al., 2021). Despite their strong belief in the necessity of vaccination, a poll of 398 students discovered that 17% were vaccine-hesitant or refused to be vaccinated (Khuc et al., 2021). Besides that, their risk-benefit assessment influenced their intention to get a COVID-19 vaccine (Duong et al., 2022). Therefore, research on public belief in COVID-19 immunization is necessary to inform policymakers as they create a campaign to raise vaccination rates.
According to previous studies and theories of health behavior, many factors influenced the acceptance or uptake of the COVID-19 vaccine, such as the health belief model or protection motivation theory (Glanz et al., 2008; Cheney and John, 2013). The HBM constructs have been employed in numerous earlier research as an important predictor of influenza vaccination uptake (Tsutsui et al., 2012). These factors include disease risk perception, vaccine safety, efficacy perception, general vaccination attitude, past vaccination history, doctor recommendations, price (Wang et al., 2018), vaccination convenience, and sociodemographic characteristics (Bish et al., 2011). Specifically, in the context of COVID-19, studies have found an association between vaccination intention and conspiracy theories (Earnshaw et al., 2020), belief in the government and those who developed the vaccine (Freeman et al., 2022), low economic status, limited education (Bertoncello et al., 2020), vaccine effectiveness, side effects of the vaccine (Pogue et al., 2020), benefits on vaccination intention (Wong et al., 2020), and how long it has been tested (Wang et al., 2020).
Belief in the safety and efficiency of vaccines, in immunization providers, and in the health system, all impact vaccination decisions (Larson et al., 2014; Paterson et al., 2016; Thomson et al., 2016). It is vital, given the expanding number of recommended or obligatory immunizations and complicated data on vaccine safety and efficacy. The public depends on medical experts' skill, judgment, and ability to interpret data appropriately (Serpell and Green, 2006; Jackson et al., 2008; Vaughan and Tinker, 2009; Brown et al., 2010; Larson et al., 2015; Schmid et al., 2017). People will trust immunization to lower illness risk and severity (Champion and Skinner, 2008). COVID-19 immunization is vital to prevent and control the virus as it spreads globally (Lurie et al., 2020). Since immunization is the best approach to prevent and control COVID-19, specialists raced to discover a safe and effective vaccine (Weintraub et al., 2021).
Subjective levels of anxiety, fear, and individual risk appear to be major predictors of vaccination acceptance (Bendau et al., 2021). Fear of COVID-19 as a direct result of the pandemic was measured using the FCoV-19S, a reliable and valid instrument for measuring COVID-19 fear in the general population (Ahorsu et al., 2020). Hence, Barua et al. (2020) established a severity scale based on the percentiles of the FCV-19S score along these lines: FCV-19S was classified as low (score ≤17), moderate (score 18-23), and high (score ≥24).
According to Pelegrín-Borondo et al. (2021), fear of COVID-19 correlates with a greater chance of immunization. Fear of COVID-19 also influences acceptance of vaccines and fear of vaccines (e.g., Cordoba-Sanchez et al., 2019; Kyaw et al., 2019; Maltezou et al., 2019; Abebe et al., 2019; Anraad et al., 2020; Nguyen et al., 2020; Otieno et al., 2020). In a similar context, the research by Pelegrín-Borondo et al. (2021) found that Oxford-AstraZeneca is pleased with the effect of cognitive vaccination effectiveness on verified COVID-19 vaccine uptake. This result is consistent with previous studies on vaccine acceptance, in which high perceived vaccine efficacy was identified as one of the primary drivers of vaccine acceptance (Alkuwari et al., 2011; Oldin et al., 2019; Teo et al., 2019; Nguyen et al., 2020). Given its significance in assessing the safety and efficiency of the vaccine, the outcomes of this phase will serve as the foundation for establishing the vaccine's perceived effectiveness among the public. Positive findings will make it simpler to persuade people of the proposed vaccine's efficacy, hence increasing its acceptability (Esen and Derya, 2010).
In Vietnam, from April to June 2020, Vietnamese youth's fear of COVID-19 is moderate before the first vaccination (Pham et al., 2021). Medical staff is also at the average level as of October 2021 (Doan et al., 2021), outpatients are also at the average level from 7 April to 31 May 2020 (Nguyen et al., 2021a), and April 2020 medical students at the low end (Nguyen et al., 2020). Thus, most are at an average of 19.2–21/35 for young people, medical staff, outpatients from 4/2020 to 10/2021 (Doan et al., 2021; Nguyen et al., 2021a; Pham et al., 2021), and only births medical staff is on the low end of 16.7/35 (Nguyen et al., 2020). Besides that, those with higher risk perception and more anxiety exhibited significantly higher vaccine acceptance in Turkey, the United Kingdom (Salali and Uysal, 2020), and France (Detoc et al., 2020).
Concerning COVID-19 vaccination, one study found that perceptions of the benefits of COVID-19 vaccination have the greatest influence on the development of a firm intention to be vaccinated (Wong et al., 2020). In contrast, another found that perceptions of susceptibility and seriousness of COVID-19 strongly influence a desire to be vaccinated against it (Graffigna et al., 2020). According to Kowk et al., who conducted a cross-sectional study among nurses, individuals with higher vaccine confidence were more able to accept a COVID-19 vaccine (Kwok et al., 2021). Another study discovered that trust and faith in vaccinations resulted in a higher probability of vaccination intention (Leng et al., 2021). In comparison, vaccination hesitancy is connected with a drop in intention to receive vaccine COVID-19 shots (Gagneux-Brunon et al., 2021).
In a recent study, Reuken et al. (2020) found that people who are more fearful of COVID-19 use personal protective equipment, wash their hands, and prefer to get medical help online. The people who do these things would be more likely to get vaccinated if they were afraid. Head et al. (2020) found that people who were afraid of COVID-19 were more likely to get vaccinated with COVID-19 vaccines and that fear of COVID-19 was positively related to the intention to get vaccinated.
According to Scrima et al. (2022), fear of COVID-19 was associated with an increased likelihood of getting the vaccine. These findings may be explained by the dual process of defense (Pyszczynski et al., 1999) that is incorporated into the Terror Management Health Model (Courtney et al., 2020). According to Sekizawa et al. (2022), waves one and three showed that participants with mild and severe fear of COVID-19 were less likely to be undecided regarding vaccination than those without fear of COVID-19. Concerning COVID-19 fear, various research has examined the link between fear of dogs and vaccination reluctance (Killgore et al., 2021; Okubo et al., 2021; Willis et al., 2021; Hwang et al., 2022). Except for Kasrine Al Halabi et al. (2021), fear of COVID-19 was related to the desire to get vaccinated. People afraid of getting sick seem to be more eager to vaccinate (Bhanu et al., 2021). Recent model research on the COVID-19 vaccine revealed that fear of the COVID-19 vaccine had a minimal influence on the desire to get immunization (Pelegrín-Borondo et al., 2021). These behaviors indicate that fearful people are more likely to receive vaccinations.
The COVID-19 pandemic has had a negative impact on Vietnamese people's mental health in general. COVID-19 cases and deaths are routinely recorded. Furthermore, the COVID-19 pandemic has harmed public perception of the virus by increasing the dread of the virus. This has an impact on the rate of immunization among the general population. Moreover, it is possible that people will not get vaccines because they do not comprehend the benefits of vaccination. However, to the best of the research team's knowledge, there has been very little research on COVID-19 fears and beliefs about the benefits of vaccination, particularly in Vietnam. In this study, we examine the mediating relationship between the number of COVID-19 vaccination injections and fear of COVID-19 and test whether beliefs about the benefits of vaccination mediate the effect of fear of COVID-19 on the number of vaccinations. Thus, the following null hypotheses were included in this study:
Ho1: There is no significant difference between the ages when considering the Fear of COVID-19 scale and beliefs benefit from vaccination COVID-19 subscale.
Ho2: There is no significant interaction between ages and the number of vaccination injections when considered jointly on the variables Fear of COVID-19 and beliefs benefit of vaccination COVID-19.
Ho3: Benefits of the COVID-19 vaccination perspective do not mediate the relationship between fear of COVID-19 and the number of COVID-19 vaccination injections.
For this research, respondents (over 18 years of age) lived in Vietnam. There were 649 participants accepted in this sample, and respondents were 52.4% male (N = 340) and 47.6% female (N = 309). Most participants were under 39 years of age (79.8%), 16.9% were between 49 and 49 years, and only 3.2% were over 50 years. Furthermore, amount of people not vaccinated yet was n = 6 (0.9%), Administered dose 1 was n = 118 (18.2%), and Administered dose 2 was n = 525 (80.9%). A detailed description of the participants is presented in Table 1.
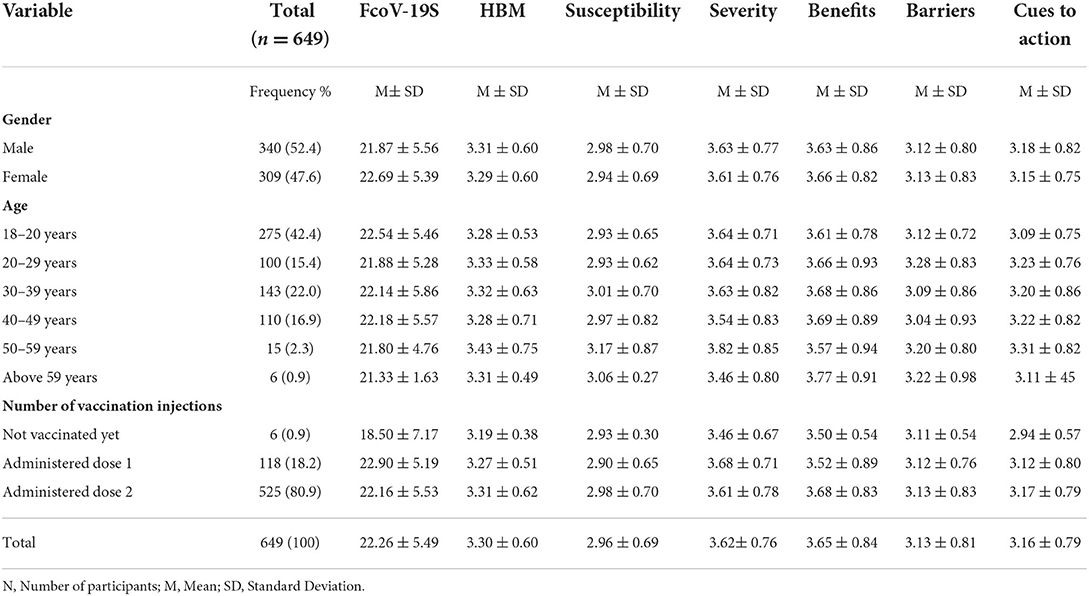
Table 1. Participants' characteristics and scores on the fear of COVID-19 scale (FCoV-19S), and Health Belief Model scale (HBM).
The Health Belief Model (HBM) in the context of the COVID-19 pandemic was developed by (Stefanut et al., 2021) based on The Health Belief Model (HBM) by Rosenstock (1974) to investigate predictors of vaccination intent. The original HBM in the context of the COVID-19 pandemic consisted of 19 items, measuring five factors: (I) perceived susceptibility (this refers to the probability that the person will contract the disease); (II) perceived severity (this takes into account the seriousness of the consequences of becoming ill); (III) perceived benefits (the positive consequences of adopting preventive behaviors); (IV) perceived barriers (obstacles that could prevent the person adopting the intended behavior); and (V) cues to action (stimuli that contribute to the decision to adopt the intended behavior).
Each item was responded to on a 5-point Likert scale ranging from one to five (1 = “strongly disagree,” 2 = “disagree,” 3 = “neutral,” 4 = “agree,” 5 = “strongly agree”). Stefanut et al. (2021) reported Cronbach's α as follows: for susceptibility 0.70; for severity 0.75; for benefits 0.88; for barriers 0.89; and for cues to action 0.77.
Cronbach's α for the total scale was 0.91 in this study. Subscales of scale HBM are as follows: Susceptibility 0.78; severity 0.85; benefits 0.85; barriers 0.84; and cues to action 0.65. In the present study, the CFA showed that the measurement was an adequate fit, CMIN/df = 4.216 (p < 0.001); GFI = 0.907; CFI = 0.933; TLI = 0.911; RMSEA = 0.070; and 90% CI (0.06, 0.061).
The fear of the COVID-19 scale was designed to measure individuals' fear of COVID-19 fast and is valid in assessing COVID-19 fear among the general population (Ahorsu et al., 2020). The questionnaire comprised seven items. Participants express their level of agreement using a 5-point Likert scale ranging from one to five (1 = “strongly disagree,” 2 = “disagree,” 3= “neutral,” 4 = “agree,” 5 = “strongly agree”). Total scores vary from 7 to 35, and the total scores show the level of their fear of COVID-19. There is no severity category for the FCV-19S to conduct inferential studies (Ahorsu et al., 2020). As a result, Barua et al. (2020) established a severity scale based on the percentiles of the FCV-19S score along these lines: FCV-19S was classified as low (score ≤17), moderate (score 18–23), and high (score ≥24). Ahorsu et al. (2020) reported that the dependability of the FCV-19S is satisfactory, particularly in terms of test-retest (intraclass correlation coefficient = 0.72) and internal consistency (Cronbach's alpha = 0.82).
This study used the Vietnamese version of the Likert-type FCV19S with seven items (Nguyen et al., 2020). For the sample used in the investigation, the instrument demonstrated good reliability (α = 0.87). The CFA indicated that the measurement was a good fit, CMIN/df = 5.910 (p < 0.001); GFI = 0.984; CFI = 0.987; TLI = 0.955; RMSEA = 0.087; and 90% CI (0.061, 0.116).
Our study collected data using an online survey using Google Forms. Invitations to participate in the study were distributed to the respondents via email and social media such as Twitter and Facebook. Data collection took place between 18 November and 30 December 2021. A total of 670 questionnaires were distributed, of which 649 were valid. Participants (over 18 years of age) who lived in Vietnam volunteered to participate in this study; 649 surveys of eligible respondents were returned (96.7% response rate), which is higher than the 30% response rate required by most researchers for the study (Dillman, 2011).
Before taking the survey, participants were given informed consent, and the conditions of anonymity and confidentiality were discussed. Participants were informed of the study's goals and requested to submit sociodemographic information such as gender, age, and the number of vaccination injections. Participants were fully volunteered, without remuneration, and free to leave at any moment. The survey took about 10 to 15 min to complete. Participants were asked to contact the research team through email or phone if they required clarification during the survey. The study was conducted according to Vietnam and international ethics and privacy laws. Approval for the study was obtained from the Ethics Committee of the Department of Science and Technology—the Ho Chi Minh City University of Education (under the Vietnamese MoET) (NV2021.19.02.DH), which complies with the International Guideline for Human Research protection as required by the Declaration of Helsinki on human participants.
Items of two scales in this study include The Health Belief Model (HBM) (Rosenstock, 1974; Stefanut et al., 2021) and The Fear of the COVID-19 (FCV-19S) (Ahorsu et al., 2020), and measures were forward and back-translated in this study. The English version was first translated into Vietnamese by a native Vietnamese speaker fluent in English. Then, the Vietnamese version was forwarded to a professional translator for re-translation into English (native speaker of English and fluent in Vietnamese). Finally, the research team compared the two versions (the English-translated version and the Vietnamese back-translated version) to the original version for content accuracy and discrepancies.
The Social Sciences Statistics Program (SPSS) version 22.0 was utilized for data processing. Descriptive statistics were employed to characterize the characteristics of the individuals. The analysis of variance (ANOVA) was conducted to test whether there were any statistically significant variations between ages, fear of COVID-19, and the number of vaccination injections. Linear regression analysis examined the relationship between the predictor variables (fear of COVID-19 and health belief) and the dependent variable (number of vaccination injections). PLS-SEM was the favored and superior method for estimating models of the mediation analysis (Sarstedt et al., 2020). PROCESS is a macro available in SPSS that simplifies the estimate of mediation process models. Instead of manually coding a single model using syntax language, researchers utilizing PROCESS can choose from various models described by Hayes et al. (2017). Therefore, we utilized the bootstrapping method in conjunction with the PROCESS macro in SPSS to test the mediation hypothesis. We employed a bootstrap approach (Shrout and Bolger, 2002) in this investigation to test the statistical significance of the expected indirect impact. We used 5,000 bootstrap samples and bias-corrected 95% confidence intervals for the bootstrap technique.
The COVID-19 fear score of seven items ranged from 18.14 (SD = 7.10) to 25.50 (SD = 7.14). The total score of COVID-19 fear was M = 22.26, SD = 5.49. Vietnamese fear of COVID-19 was at a medium level (Table 1).
Most of the participants had positive beliefs in relation to the COVID-19 vaccination (3.30 ± 0.60), with a high mean score for the benefits of vaccination (M = 3.65, SD = 0.84) and perceived severity (M = 3.62, SD = 0.76) but a slightly lower score (M = 3.16, SD = 0.79) for cues to action. The low mean score for the perceived susceptibility was M = 2.96, SD = 0.69. However, the items of barriers to vaccination also reported a high score (M = 3.13, SD = 0.81).
A multivariate analysis of variance (MANOVA) was performed with age. The number of vaccination injections is the independent variable, and the FCV-19S and beliefs benefit of vaccination COVID-19 scale are the dependent variables. The null hypotheses were tested with a one-way MANOVA procedure performed by SPSS. To run MANOVA, we conducted a preliminary assumption check for normality and homogeneity of variance-covariance matrices. Suppose the sizes of groups are approximately equal or the size of the largest group is less than about 1.5 times the size of the smallest group, then MANOVA is robust to violations of the homogeneity of variance/covariance matrices (Leech et al., 2013). The largest group in this research (n = 549) was about 87.5 times larger than the smallest group (n = 6), and the multivariate homogeneity of variance-covariance matrices tested with Box's M-test revealed that the M-value of 57.411 was significant (p = 0.002). Therefore, the assumption of homogeneity of covariance matrices was not satisfied. For this reason, a more robust statistic, Pillai's Trace value, was used for reporting the result.
Based on the significant effects found from the MANOVA, a separate two-way analysis of variance (ANOVA) for each dependent variable was conducted without undue inflation of the experiment's Type I error (Grimm and Yarnold, 1995). Levene's Test of Equality of Error Variances tests the assumption of MANOVA and ANOVA that the variances of each variable are equal across the groups. If Levene's test is significant, the assumption has not been satisfied. In this study, the value of Levene's test was significant for the FCOV-19S scale [F(11,636) = 1.739, p = 0.061], while it came out to be non-significant for beliefs benefit of vaccination COVID-19 subscale [F(11,636) = 2.314, p < 0.05]. So, for the FCV-19S scale, the assumption that the variances of each variable are equal across the groups was met. When the follow-up ANOVAs were conducted, the Perceived Benefits subscale results were interpreted cautiously (Table 2). There was a non-significant difference in age when they were considered on the FCV-19S scale and beliefs benefit of vaccination COVID-19 subscale, Pillai's Trace value =0.021; F(10,1272) = 1.364, p = 0.192, partial η2 = 0.011. Therefore, the results suggested that the first hypothesis (Ho1) was not rejected.
The results revealed that there was a significant multivariate effect for interaction between ages and the number of vaccination injections when considered jointly on the variables Fear of COVID-19; beliefs benefit of vaccination COVID-19, Pillai's Trace value = 0.032; [F(4,1272) = 5.164, p ≤ 0.001, partial η2= 0.016]. Accordingly, the results suggested that the second hypothesis (Ho2) was rejected. A separate ANOVA was conducted for each dependent variable, with each ANOVA evaluated at an alpha level of 0.025 (i.e., 0.05/2). There was a significant difference between the number of vaccination injections when considering the variables jointly with Fear of COVID-19 [F(2,636) = 4.105, p < 0.05, partial η2 = 0.021]. Follow-up univariate analysis revealed that individuals who had received one dose of vaccine (M = 3.27; SD= 0.74) reported more fear than those who had received two doses of vaccine (M = 3.16; SD = 0.79) or had not been vaccinated (M = 2.64; SD = 1.02). Additionally, teenagers aged 18 to 20 years (M = 3.22; SD = 0.78), 20 to 29 years (M = 3.12; SD = 0.75), 30 to 39 years (M = 3.16; SD = 0.83), 40 to 49 years (M = 3.16; SD = 0.79), and 18 to 20 years (M = 3.22; SD = 0.78) had the highest degree of fear of COVID-19. Finally, those aged 50 to 59 years (M = 3.11; SD = 0.68) and those aged above 59 years (M = 3.04; SD = 0.23) reported less fear of COVID-19.
There was a significant difference between the number of vaccination injections when considering the variables Beliefs benefit of vaccination COVID-19 jointly, [F(2,636) = 6.653, p < 0.05, partial η2 = 0.020]. Follow-up univariate analysis revealed that individuals who had received two doses of vaccine (M = 3.68; SD = 0.83) reported more benefits from vaccination than those who had received one dose of vaccine (M = 3.52; SD = 0.89) or had not been vaccinated (M = 3.50; SD = 54). Additionally, those aged above 59 years (M = 3.77; SD = 0.91) had the highest degree of Perceived benefits from vaccination. Those aged 50 to 59 years (M = 3.57; SD = 0.94), 18 to 20 years (M = 3.61; SD = 0.78), 20 to 29 years (M = 3.66; SD = 0.93; 30 to 39 years (M = 3.68; SD = 0.86), and 40 to 49 years (M = 3.69; SD = 6.89) reported less benefits of vaccination.
We used a simple mediation model to examine the indirect effect of fear of COVID-19 on the number of vaccination injections through benefits as presented in Figure 1. If the 95% CI for these estimates does not include zero, the indirect effect is statistically significant (Shrout and Bolger, 2002).
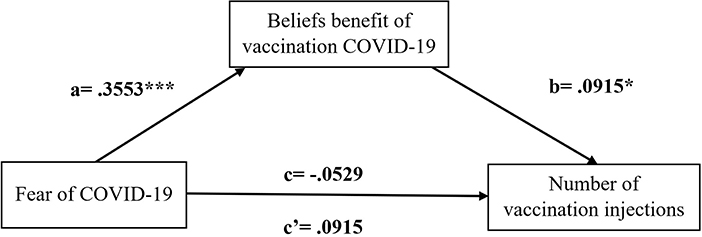
Figure 1. Simple mediation model with unstandardized coefficients. a = total effect of fear of COVID-19 on beliefs benefits of vaccination COVID-19. b= effect of benefit on Number of COVID-19 vaccination injections. c = total effect of fear of COVID-19 on the Number of COVID-19 vaccination injections without accounting for the mediators. c' = direct effect of fear of COVID-19 on the Number of COVID-19 vaccination injections once mediators have been included in the model. *p < 0.05, ***p < 0.001.
In the first (simple) regression, fear of COVID-19 is a significant (positive) predictor of beliefs benefit of vaccination COVID-19 vaccination (b = 0.0547, S.E = 0.0057, p < 0.001). This coefficient reflects the direct effect of fear of COVID-19 on the belief benefit of vaccination of COVID-19 within the path model. Besides that, the standardized path coefficient is also provided, which is 0.3553.
In the second regression, fear of COVID-19 (b = −0.0041, S.E = 0.0032, p > 0.005) is not a significant predictor of the number of vaccination injections. However, the perceived belief benefit of vaccination COVID-19 is a significant predictor of the number of vaccination injections (b = 0.0458, S.E = 0.0210, p ≤ 0.005). These coefficients reflect the direct effects of perceived beliefs benefit of vaccination COVID-19 on the number of vaccination injections within the path model. The standardized path coefficients for this portion of the model are −0.0259 and 0.0915 for Fear of COVID-19 and perceived beliefs benefit of vaccination COVID-19, respectively.
Table 3 shows the total effect (c) of fear of COVID-19 on number of vaccination injections was not significant, b = −0.011, SE = 0.021, 95% CI [−0.052 to 0.030]. The direct effect (c') of fear of COVID-19 on number of vaccination injections was not significant, b = −0.028, SE = 0.022, 95% CI [−0.072 to 0.015]. The indirect effect was statistically significant, b = 0.017, SE =0.008, 95% CI [0.002 to 0.033]. The results suggested that fear of COVID-19 on the number of vaccination injections through beliefs benefit of vaccination COVID-19. Therefore, the third hypothesis should be rejected.
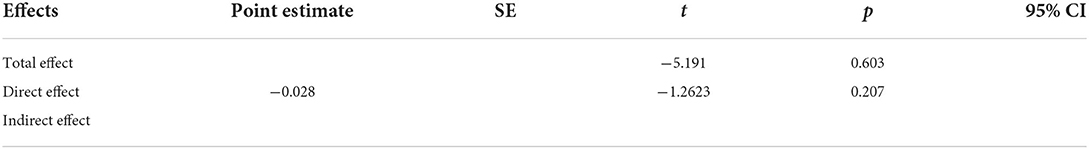
Table 3. Total direct and indirect effects of fear of COVID-19 on the number of vaccination injections attitudes through beliefs benefits of vaccination COVID-19.
The main purposes of the present research were (i) to investigate the relationship between the fear of COVID-19 and the beliefs benefit of vaccination COVID-19 and the number of vaccination injections and (ii) to test whether the beliefs benefit of vaccination COVID-19 mediate the effect of the fear of COVID-19 on the number of vaccination injections.
Our research yielded a few crucial results. First, people have a moderate fear of COVID-19 (M = 22.26 ± 5.49). Second, 18- to 20-year-olds are more fearful of COVID-19 than other age groups. Third, people who got the first dose had a higher fear of COVID-19 than those who got the second dose and were not immunized. Fourth, the belief benefit of vaccination COVID-19 would predict the number of vaccination injections. Fifth, the belief benefit of vaccination COVID-19 would operate as a mediator between fear of COVID-19 and the number of vaccination injections.
The overall mean fear of COVID-19 score was 22.62 ± 5.49 in the present sample. Other Vietnamese studies have used the same tool to assess levels of fear about COVID-19. A mean score of 19.6 ± 5.2 was reported for a survey conducted from 1 October 2021 to 20 October 2021, in a sample of 208 hospital healthcare workers (Doan et al., 2021). Another study comprising 4,348 outpatients was conducted from 7 April to 31 May 2020; a mean score of 20.6 ± 5.4 for COVID-19 fear (Nguyen et al., 2021a). A cross-sectional study was conducted from 7 to 29 April 2020 on 5,423 students at universities across Vietnam; a mean score of 16.7 ± 5.3 (Nguyen et al., 2020). Thus, the present sample showed higher fear of COVID-19 scores, albeit comparisons were limited due to study implementation time and sample representativeness among Vietnamese studies. There are several possible explanations for this finding. First, this investigation was undertaken 6 months after the fourth COVID-19 outbreak in Vietnam began. During the fourth outbreak, from 27 April 2021 to 31 December 2021, 1,728,405 cases and 32,133 deaths were registered (Ministry of Health, 2021b). The outbreak has the most severe impact. The number of infected people and deaths increases every day. From 18 November to 30 December 2021, Vietnam recorded 649,273 infections. Second, during the fourth wave of the epidemic, the Vietnamese government implemented social distancing policies for a long time to limit infection (Ministry of Health, 2021b). Above all, surrounding deaths are among the strongest reasons for people's fear (Rodríguez-Hidalgo et al., 2020). In Vietnam, 32,133 people have died from COVID-19 fourth outbreak, accounting for 1.9% percent of the total number of illnesses (Ministry of Health, 2021b).
This research shows there is a difference between age and fear of COVID-19. This finding supports our hypothesis that adolescents are more likely to fear COVID-19 than other age groups. This finding is consistent with the study of Kim et al. (2020), and adolescents are among the most mentally impacted populations due to pandemics (Kim et al., 2020). Furthermore, the fear of COVID-19 was significantly related to the year in which the students were enrolled. First-year students were more fearful than those in the following years of study (2nd, 3rd, and 4th). Thus, fear appears to be age-related, with younger students being more fearful of the disease (Martínez-Lorca et al., 2020). This conclusion might be explained why older people are not always more concerned about mortality (Neimeyer, 1985). Haktanir et al. (2020) found similar results in the Turkish population (Haktanir et al., 2020). This result might be explained why older people were not necessarily more concerned about dying (Neimeyer, 1985). However, in a study conducted on the Italian population (Soraci et al., 2020), there was no difference in fear of COVID-19 scores based on age. On the other hand, research in other nations indicates that the elderly are more fearful of contracting COVID-19 infection than younger persons (De Leo and Trabucchi, 2020; Meng et al., 2020).
Furthermore, the study discovered that persons who got influenza vaccination in the first dosage feared COVID-19 more than those who received the second dose and were not immunized. People afraid of COVID-19 were more likely to get vaccinated with COVID-19 vaccines, and that fear of COVID-19 was positively related to the intention to get vaccinated (Scrima et al., 2022). As the number of individuals who receive vaccinations grows (Mathieu et al., 2021), it has been demonstrated that vaccination is useful in lowering mortality and hospitalizations (Abu-Raddad et al., 2021; Pilishvili et al., 2021). Comparing persons who got only one dosage of the vaccination to those who received two doses of the vaccine, those who received two doses had higher and better immunity (Mahase, 2020; Chung et al., 2021).
Our research has revealed an important connection between the Health Belief Model (HBM) instrument and the COVID-19 pandemic in Vietnam. Consistent with previous research on this topic, the acceptance of vaccine use has been explained by various health behavior models; the Health Belief Model (HBM) has been used to predict preventive health behaviors (Janz and Becker, 1984). Numerous studies have investigated the HBM constructs influencing COVID-19 vaccination, which are essential for targeted interventions to increase vaccine acceptance, particularly among Vietnamese individuals (Coe et al., 2012; Kayoll et al., 2019; Wong et al., 2020; Li et al., 2021). More specifically, concerning COVID-19 vaccination, our study found that perceptions of the beliefs benefit of COVID-19 vaccination have the greatest influence on developing a firm intention to be vaccinated. Another study found that perceptions of the benefits of COVID-19 vaccination have the greatest influence on the development of a firm intention to be vaccinated (Wong et al., 2020). In contrast, another found that perceptions of susceptibility and seriousness of COVID-19 strongly influence a desire to be vaccinated against it (Graffigna et al., 2020). According to Kowk et al., who conducted a cross-sectional study among nurses, individuals with higher vaccine confidence were more able to accept a COVID-19 vaccine (Kwok et al., 2021). Another study discovered that trust and faith in vaccinations resulted in a higher probability of vaccination intention (Leng et al., 2021). The concept of vaccination communication encompasses numerous interventions with diverse goals, such as informing or educating, reminding, or recalling, increasing community ownership, teaching skills, providing support, facilitating decision-making, and facilitating communication (Kaufman et al., 2017). In our study, informing individuals of the benefits of vaccination about their fear of COVID-19 and the number of vaccinations they will receive will facilitate their immunization decisions.
This study demonstrates that the number of COVID-19 vaccination injections correlate positively with the belief that vaccination is beneficial. This finding reflects that individuals with a high belief level benefit from vaccination COVID-19 report a greater vaccine readiness rate. This is an unexpected discovery. Another study discovered a significant correlation between benefits and the COVID-19 vaccine acceptance rate. As the COVID-19 risk perception and the vaccine's perceived benefits increased, the reported COVID-19 vaccine acceptance rate also increased (Al-Mistarehi et al., 2021). Past interventions incorporating components targeting similar beliefs successfully boosted knowledge, attitudes/beliefs, and uptake of other vaccines (McRee et al., 2018; Reiter et al., 2018). Thus, our findings add empirical evidence to the literature on the number of vaccination injections by demonstrating that the belief benefits of vaccination COVID-19 mediate fear of COVID-19. A Polish study by Szmyd et al. (2021) showed that a willingness to Vaccination is significantly supported by the growing fear of COVID-19. Furthermore, unvaccinated individuals tend to be more fearful of COVID than latent individuals (Štěpánek et al., 2021). Previous models did not address the function of beliefs benefit of vaccination COVID-19 as a mediator in the association between fear of COVID-19 and the number of vaccination injections. This insight will aid in developing more focused therapies. The COVID-19 vaccine revealed that fear of the COVID-19 vaccine had little effect on the desire to receive an immunization (Pelegrín-Borondo et al., 2021). These behaviors indicate that fearful individuals are more likely to receive vaccinations against COVID-19. This study's findings will provide clinical psychologists with a stronger scientific foundation for providing psychological advice to individuals regarding the booster dose of the COVID-19 vaccine after the third and fourth doses.
The research has some limitations. First, we recruit subjects by convenience sampling, limiting the study's generalizability to a sample of the Vietnamese population. The majority of participants in this study are urban residents who have received two vaccine doses. Consequently, the findings of the study are limited to this group. Considering this limitation, more studies with a large and diverse sample size might be conducted (e.g., children, adolescents, university students). Second, due to the cross-sectional design of our study, causal inferences cannot be made. As a result, the mediation effects can only be investigated within the expected paradigm, and future research should employ a longitudinal design to demonstrate the causal relationships between fear of COVID-19, the Beliefs benefit of vaccination COVID-19, and the number of vaccination injections.
There is evidence that the COVID-19 pandemic has increased fear levels in the general population. Exploring the causes of elevated COVID-19 dread is critical so that counselors and doctors can provide prompt psychological therapies. According to the current study, information on beliefs about the benefits of vaccination acts as a mediator between fear of COVID-19 and the number of shots, implying that those who are afraid of COVID-19 have a greater degree of influenza vaccination. The availability of information about the benefits of vaccinations has grown, leading to higher flu vaccination rates. When the COVID-19 outbreak strikes, young individuals are more fearful than older folks, according to research. People who got the first vaccination dosage are more afraid of COVID-19 than those who received the second dose and did not get the vaccine. This is the first study to demonstrate a link between vaccination benefits, number of shots, and fear of COVID-19, and the findings will help guide future research.
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Participants gave their explicit written consent to participate in this study.
HH and SH contributed to the conception and design of the study. HH, XN, TH, and HT organized the database. XN, TH, and V-LT-C performed the statistical analysis. V-LT-C, XN, TH, and HT wrote the first draft of the manuscript. All authors contributed to manuscript revision, read, and approved the submitted version.
The authors would like to express their gratitude to the participants for their assistance with data collecting.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.968902/full#supplementary-material
Abebe, A. M., Mengistu, T., and Mekuria, A. D. (2019). Measles case, immunization coverage and its determinant factors among 12–23 month children, in Bassona Worena Woreda, Amhara Region, Ethiopia, 2018. BMC Res. Notes 12, 1–6. doi: 10.1186/s13104-019-4104-8
Abu-Raddad, L. J., Chemaitelly, H., and Butt, A. A. (2021). Effectiveness of the BNT162b2 Covid-19 Vaccine against the B. 1.1. 7 and B. 1.351 Variants. N. Engl. J. Med. 385, 187–189. doi: 10.1056/NEJMc2104974
Ahorsu, D. K., Lin, C.-Y., Imani, V., Saffari, M., Griffiths, M. D., and Pakpour, A. H. (2020). The fear of COVID-19 scale: development and initial validation. Int. J. Ment. Health Addict. 20, 1537–1545. doi: 10.1007/s11469-020-00270-8
Alkuwari, M.G., Aziz, N.A., Nazzal, Z.A.S., and Al-Nuaimi, S.A. (2011). Pandemic influenza A/H1N1 vaccination uptake among health care workers in Qatar: motivators and barriers. Vaccine 29, 2206–2211. doi: 10.1016/j.vaccine.2010.08.093
Al-Mistarehi, A.-H., Kheirallah, K. A., Yassin, A., Alomari, S., Aledrisi, M. K., Ata, E. M. B., et al. (2021). Determinants of the willingness of the general population to get vaccinated against COVID-19 in a developing country. Clin. Exp. Vaccine Res. 10, 171–182. doi: 10.7774/cevr.2021.10.2.171
Anraad, C., Lehmann, B. A., Visser, O., van Empelen, P., Paulussen, T. G., Ruiter, R. A., et al. (2020). Social-psychological determinants of maternal pertussis vaccination acceptance during pregnancy among women in the Netherlands. Vaccine 38, 6254–6266. doi: 10.1016/j.vaccine.2020.07.047
Bartsch, S. M., O'Shea, K. J., Ferguson, M. C., Bottazzi, M. E., Wedlock, P. T., Strych, U., et al. (2020). Vaccine efficacy needed for a COVID-19 coronavirus vaccine to prevent or stop an epidemic as the sole intervention. Am. J. Prev. Med. 59, 493–503. doi: 10.1016/j.amepre.2020.06.011
Barua, L., Zaman, M. S., Omi, F. R., and Faruque, M. (2020). Psychological burden of the COVID-19 pandemic and its associated factors among frontline doctors of Bangladesh: a cross-sectional study. F1000Research 9, 1304. doi: 10.12688/f1000research.27189.1
Bendau, A., Plag, J., Petzold, M. B., and Ströhle, A. (2021). COVID-19 vaccine hesitancy and related fears and anxiety. Int. Immunopharmacol. 97, 107724. doi: 10.1016/j.intimp.2021.107724
Bertoncello, C., Ferro, A., Fonzo, M., Zanovello, S., Napoletano, G., Russo, F., et al. (2020). Socioeconomic determinants in vaccine hesitancy and vaccine refusal in Italy. Vaccines 8, 276. doi: 10.3390/vaccines8020276
Bhanu, C., Gopal, D. P., Walters, K., and Chaudhry, U. A. (2021). Vaccination uptake amongst older adults from minority ethnic backgrounds: a systematic review. PLoS Med. 18, e1003826. doi: 10.1371/journal.pmed.1003826
Bish, A., Yardley, L., Nicoll, A., and Michie, S. (2011). Factors associated with uptake of vaccination against pandemic influenza: a systematic review. Vaccine 29, 6472–6484. doi: 10.1016/j.vaccine.2011.06.107
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Brown, K. F., Kroll, J. S., Hudson, M. J., Ramsay, M., Green, J., Long, S. J., et al. (2010). Factors underlying parental decisions about combination childhood vaccinations including MMR: a systematic review. Vaccine 28, 4235–4248. doi: 10.1016/j.vaccine.2010.04.052
Champion, V. L., and Skinner, C. S. (2008). “The health belief model” in Health Behavior and Health Education: Theory, Research, and Practice, eds K. Glanz, B. K. Rimer, and K. Viswanath (San Francisco, CA: Jossey-Bass), 45–65.
Chen, I.-H., Chen, C.-Y., Pakpour, A. H., Griffiths, M. D., and Lin, C.-Y. (2020). Internet-related behaviors and psychological distress among schoolchildren during COVID-19 school suspension. J. Am. Acad. Child Adolesc. Psychiatry 59, 1099. doi: 10.1016/j.jaac.2020.06.007
Cheney, M. K., and John, R. (2013). Underutilization of influenza vaccine: a test of the health belief model. Sage Open 3, 2158244013484732. doi: 10.1177/2158244013484732
Chung, H., He, S., Nasreen, S., Sundaram, M. E., Buchan, S. A., Wilson, S. E., et al. (2021). Effectiveness of BNT162b2 and mRNA-1273 covid-19 vaccines against symptomatic SARS-CoV-2 infection and severe covid-19 outcomes in Ontario, Canada: test negative design study. BMJ 374, 1943. doi: 10.1136/bmj.n1943
Coe, A. B., Gatewood, S. B. S., Moczygemba, L. R., Goode, J. V., and Beckner, J. O. (2012). The use of the health belief model to assess predictors of intent to receive the novel H1N1 influenza vaccine. Inov. Pharm. 3, 1–11. doi: 10.24926/iip.v3i2.257
Cordoba-Sanchez, V., Tovar-Aguirre, O. L., Franco, S., Ortiz, N. E. A., Louie, K., Sanchez, G. I., et al. (2019). Perception about barriers and facilitators of the school-based HPV vaccine program of Manizales, Colombia: a qualitative study in school-enrolled girls and their parents. Prevent. Med. Rep. 16, 100977. doi: 10.1016/j.pmedr.2019.100977
Courtney, E. P., Goldenberg, J. L., and Boyd, P. (2020). The contagion of mortality: a terror management health model for pandemics. Br. J. Soc. Psychol. 59, 607–617. doi: 10.1111/bjso.12392
Dao, T. L., and Nguyen, T. D. (2020). Controlling the COVID-19 pandemic: Useful lessons from Vietnam. Travel Med. Infect. Dis. 37, 101822. doi: 10.1016/j.tmaid.2020.101822
De Leo, D., and Trabucchi, M. (2020). COVID-19 and the fears of Italian senior citizens. Int. J. Environ. Res. Public Health 17, 3572. doi: 10.3390/ijerph17103572
Detoc, M., Bruel, S., Frappe, P., Tardy, B., Botelho-Nevers, E., and Gagneux-Brunon, A. (2020). Intention to participate in a COVID-19 vaccine clinical trial and to get vaccinated against COVID-19 in France during the pandemic. Vaccine 38, 7002–7006. doi: 10.1016/j.vaccine.2020.09.041
Dillman, D. A. (2011). Mail and Internet Surveys: The Tailored Design Method: 2007 Update With New Internet, Visual, and Mixed-Mode Guide. Hoboken, NJ: John Wiley and Sons.
Doan, Q.-H., Tran, N.-N., Than, M.-H., Nguyen, H.-T., Bui, V.-S., Nguyen, D.-H., et al. (2021). Associated Factors with Perceived Fear of COVID-19 among Vietnamese Hospital Healthcare Workers during Fourth Wave of the COVID-19 Pandemic: Policy Implications for Interconnected and Social-and Personal-Based Health Support. Healthcare 9, 1713. doi: 10.3390/healthcare9121713
Dror, A. A., Eisenbach, N., Taiber, S., Morozov, N. G., Mizrachi, M., Zigron, A., et al. (2020). Vaccine hesitancy: the next challenge in the fight against COVID-19. Eur. J. Epidemiol. 35, 775–779. doi: 10.1007/s10654-020-00671-y
Duong, M. C., Nguyen, H. T., and Duong, M. (2022). Evaluating COVID-19 vaccine hesitancy: a qualitative study from Vietnam. Diabetes Metab. Syndrome 16, 102363. doi: 10.1016/j.dsx.2021.102363
Earnshaw, V. A., Eaton, L. A., Kalichman, S. C., Brousseau, N. M., Hill, E. C., and Fox, A. B. (2020). COVID-19 conspiracy beliefs, health behaviors, and policy support. Transl. Behav. Med. 10, 850–856. doi: 10.1093/tbm/ibaa090
Esen, S., and Derya, T. (2010). Knowledge, attitudes and anxiety towards influenza A/H1N1 vaccination of healthcare workers in Turkey. BMC Infect. Dis. 10, 1–6. doi: 10.1186/1471-2334-10-281
Ferré, V. M., Peiffer-Smadja, N., Visseaux, B., Descamps, D., Ghosn, J., and Charpentier, C. (2022). Omicron SARS-CoV-2 variant: What we know and what we don't. Anaesthesia Critical Care Pain Med. 41, 100998. doi: 10.1016/j.accpm.2021.100998
Freeman, D., Waite, F., Rosebrock, L., Petit, A., Causier, C., East, A., et al. (2022). Coronavirus conspiracy beliefs, mistrust, and compliance with government guidelines in England. Psychol. Med. 52, 251–263. doi: 10.1017/S0033291720001890
Gagneux-Brunon, A., Detoc, M., Bruel, S., Tardy, B., Rozaire, O., Frappe, P., et al. (2021). Intention to get vaccinations against COVID-19 in French healthcare workers during the first pandemic wave: a cross-sectional survey. J. Hosp. Infection 108, 168–173. doi: 10.1016/j.jhin.2020.11.020
Glanz, K., Rimer, B. K., and Viswanath, K. (2008). Health Behavior and Health Education: Theory, Research, and Practice. San Francisco, CA: John Wiley and Sons.
Graffigna, G., Palamenghi, L., Boccia, S., and Barello, S. (2020). Relationship between citizens' health engagement and intention to take the COVID-19 vaccine in Italy: a mediation analysis. Vaccines 8, 576. doi: 10.3390/vaccines8040576
Grimm, L. G., and Yarnold, P. R. (1995). Reading and understanding multivariate statistics. Washington, DC: American Psychological Association.
Haktanir, A., Seki, T., and Dilma,ç, B. (2020). Adaptation and evaluation of Turkish version of the fear of COVID-19 scale. Death Stud. 461–9. doi: 10.1080/07481187.2020.1773026
Hayes, A. F., Montoya, A. K., and Rockwood, N. J. (2017). The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Aust. Mark. J. 25, 76–81. doi: 10.1016/j.ausmj.2017.02.001
Head, K. J., Kasting, M. L., Sturm, L. A., Hartsock, J. A., and Zimet, G. D. (2020). A national survey assessing SARS-CoV-2 vaccination intentions: implications for future public health communication efforts. Sci. Commun. 42, 698–723. doi: 10.1177/1075547020960463
Hoang, V. T., Pham, T. D., Nguyen, Q. T., Nguyen, D. C., Nguyen, D. T., Nguyen, T. B., et al. (2022). Seroprevalence of SARS-CoV-2 among high-density communities and hyper-endemicity of COVID-19 in Vietnam. Trop. Med. Int. Health 27, 515–521. doi: 10.1111/tmi.13744
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. doi: 10.1016/S0140-6736(20)30183-5
Huynh, G., Van Nguyen, T., Nguyen, D. D., Lam, Q. M., Pham, T. N., and Nguyen, H. T. N. (2021). Knowledge about COVID-19, beliefs and vaccination acceptance against COVID-19 among high-risk people in Ho Chi Minh City, Vietnam. Infect. Drug Resist. 14, 1773–1780. doi: 10.2147/IDR.S308446
Hwang, S. E., Kim, W.-H., and Heo, J. (2022). Sociodemographic, psychological, and experiential predictors of COVID-19 vaccine hesitancy in South Korea, October-December 2020. Hum. Vac. Immunother. 18, 1–8. doi: 10.1080/21645515.2021.1983389
Jackson, C., Cheater, F. M., and Reid, I. (2008). A systematic review of decision support needs of parents making child health decisions. Health Expect. 11, 232–251. doi: 10.1111/j.1369-7625.2008.00496.x
Jain, J., Saurabh, S., Kumar, P., Verma, M. K., Goel, A. D., Gupta, M. K., et al. (2021). COVID-19 vaccine hesitancy among medical students in India. Epidemiol. Infect. 149, E132. doi: 10.1017/S0950268821001205
Janz, N. K., and Becker, M. H. (1984). The Health Belief Model: a decade later. Health Educ. Behav. 11, 1–47. doi: 10.1177/109019818401100101
Johnson, A. G. (2022). COVID-19 incidence and death rates among unvaccinated and fully vaccinated adults with and without booster doses during periods of Delta and Omicron variant emergence −25 US Jurisdictions, April 4–December 25, 2021. Morbid. Mortal. Wkly. Rep. 71, 132–138. doi: 10.15585/mmwr.mm7104e2
Kasrine Al Halabi, C., Obeid, S., Sacre, H., Akel, M., Hallit, R., Salameh, P., et al. (2021). Attitudes of Lebanese adults regarding COVID-19 vaccination. BMC Public Health 21, 1–7. doi: 10.1186/s12889-021-10902-w
Kaufman, J., Ryan, R., Glenton, C., Lewin, S., Bosch-Capblanch, X., Cartier, Y., et al. (2017). Childhood vaccination communication outcomes unpacked and organized in a taxonomy to facilitate core outcome establishment. J. Clin. Epidemiol. 84, 173–184. doi: 10.1016/j.jclinepi.2017.02.007
Kayoll, V. G., Julia, L., Coretta, M. J., Palmer, M. H., Moore, A. D., and Hamilton, J. B. (2019). African-American Parents' and Daughters' Beliefs about HPV Infection and the HPV Vaccine. Public Health Nurs. 36, 134–143.
Khuc, Q. V., Nguyen, T., Nguyen, T., Pham, L., Le, D.-T., Ho, H.-H., et al. (2021). Young adults' intentions and rationales for COVID-19 vaccination participation: evidence from a student survey in Ho Chi Minh City, Vietnam. Vaccines 9, 794. doi: 10.3390/vaccines9070794
Killgore, W. D., Cloonan, S. A., Taylor, E. C., and Dailey, N. S. (2021). The COVID-19 vaccine is here—now who is willing to get it? Vaccines 9, 339. doi: 10.3390/vaccines9040339
Kim, U., Bhullar, N., and Debra, J. (2020). Life in the pandemic: Social isolation and mental health. J. Clin. Nurs. 29, 2756–2757. doi: 10.1111/jocn.15290
Kwok, K. O., Li, K.-K., Wei, W. I., Tang, A., Wong, S. Y. S., and Lee, S. S. (2021). Influenza vaccine uptake, COVID-19 vaccination intention and vaccine hesitancy among nurses: a survey. Int. J. Nurs. Stud. 114, 103854. doi: 10.1016/j.ijnurstu.2020.103854
Kyaw, W. M., Chow, A., Hein, A. A., Lee, L. T., Leo, Y. S., and Ho, H. J. (2019). Factors influencing seasonal influenza vaccination uptake among health care workers in an adult tertiary care hospital in Singapore: A cross-sectional survey. Am. J. Infect. Control 47, 133–138. doi: 10.1016/j.ajic.2018.08.011
Kyriakidis, N. C., López-Cortés, A., González, E. V., Grimaldos, A. B., and Prado, E. O. (2021). SARS-CoV-2 vaccines strategies: a comprehensive review of phase 3 candidates. NPJ Vaccines 6, 1–17. doi: 10.1038/s41541-021-00292-w
Larson, H. J., Jarrett, C., Eckersberger, E., Smith, D. M., and Paterson, P. (2014). Understanding vaccine hesitancy around vaccines and vaccination from a global perspective: a systematic review of published literature, 2007–2012. Vaccine 32, 2150–2159. doi: 10.1016/j.vaccine.2014.01.081
Larson, H. J., Schulz, W. S., Tucker, J. D., and Smith, D. M. (2015). Measuring vaccine confidence: introducing a global vaccine confidence index. PLoS Curr. 7, 1–29. doi: 10.1371/currents.outbreaks.ce0f6177bc97332602a8e3fe7d7f7cc4
Le, H. N. M., Nguyen, K. Q., Tran, N. L., and Phan, N. Q. K., and Nguyen, T. H. (2021). COVID-19 timeline of vietnam: important milestones through four waves of the pandemic and lesson learned. Front. Public Health 9, 709067. doi: 10.3389/fpubh.2021.709067
Leech, N., Barrett, K., and Morgan, G. A. (2013). SPSS for Intermediate Statistics: Use and Interpretation. New York, NY: Routledge.
Leng, A., Maitland, E., Wang, S., Nicholas, S., Liu, R., and Wang, J. (2021). Individual preferences for COVID-19 vaccination in China. Vaccine 39, 247–254. doi: 10.1016/j.vaccine.2020.12.009
Li, P. W., Haridah, A., and Pooi, F. W. (2021). Will they, or Won't they? Examining patients' vaccine intention for flu and COVID-19 using the Health Belief Model. Res. Soc. Administ. Pharm. 17, 1596–1605. doi: 10.1016/j.sapharm.2020.12.012
Lu, H., Stratton, C. W., and Tang, Y. W. (2020). Outbreak of pneumonia of unknown etiology in Wuhan, China: The mystery and the miracle. J. Med. Virol. 92, 401–402. doi: 10.1002/jmv.25678
Lurie, N., Saville, M., Hatchett, R., and Halton, J. (2020). Developing Covid-19 vaccines at pandemic speed. N. Engl. J. Med. 382, 1969–1973. doi: 10.1056/NEJMp2005630
Mahase, E. (2020). Covid-19: Pfizer vaccine efficacy was 52% after first dose and 95% after second dose, paper shows. BMJ 371, m4826 doi: 10.1136/bmj.m4826
Maltezou, H. C., Pelopidas Koutroumanis, P., Kritikopoulou, C., Theodoridou, K., Katerelos, P., and Tsiaousi, I. (2019). Knowledge about influenza and adherence to the recommendations for influenza vaccination of pregnant women after an educational intervention in Greece. Human Vac. Immunother. 15, 1070–1074. doi: 10.1080/21645515.2019.1568158
Martínez-Lorca, M., Martínez-Lorca, A., Criado-Álvarez, J. J., Armesilla, M. D. C., and Latorre, J. M. (2020). The fear of COVID-19 scale: Validation in spanish university students. Psychiatry Res. 293, 113350. doi: 10.1016/j.psychres.2020.113350
Mathieu, E., Ritchie, H., Ortiz-Ospina, E., Roser, M., Hasell, J., Appel, C., et al. (2021). A global database of COVID-19 vaccinations. Nat. Hum. Behav. 5, 947–953. doi: 10.1038/s41562-021-01122-8
McKay, B., Calfas, J., and Ansari, T. (2020). Coronavirus Declared Pandemic by World Health Organization. The Wall Street Journal. Available onlin at: https://www.wsj.com/articles/u-s-coronavirus-cases-top-1-000-11583917794.
McRee, A.-L., Shoben, A., Bauermeister, J. A., Katz, M. L., Paskett, E. D., and Reiter, P. L. (2018). Outsmart HPV: acceptability and short-term effects of a web-based HPV vaccination intervention for young adult gay and bisexual men. Vaccine 36, 8158–8164. doi: 10.1016/j.vaccine.2018.01.009
Meng, H., Xu, Y., Dai, J., Zhang, Y., Liu, B., and Yang, H. (2020). Analyze the psychological impact of COVID-19 among the elderly population in China and make corresponding suggestions. Psychiatry Res. 289, 112983. doi: 10.1016/j.psychres.2020.112983
Minister, P. (2020). Chi thị sô 16/CT-TTg ngày 31/3/2020, vê thụ'c hiên các biên pháp câp bách phòng, chông dịch COVID-19 [Directive No. 16/CT-TTg dated 31/3/2020, On the implementation of urgent measures to prevent and control COVID-19]. Available online at: https://tulieuvankien.dangcongsan.vn/Uploads/2020/3/7/31/Chi-thi-16.1.jpg.
Ministry of Health (2021a). Expanding Priority Groups in the Largest-Ever COVID-19 Vaccination Campaign [in Vietnamese]. Available online at: https://ncov.moh.gov.vn/en/-/6847912-298
Ministry of Health (2021b). Information About Coronavirus Diease Outbreak COVID-19 [in Vietnamese]. Available online at: https://ncov.moh.gov.vn/
Neimeyer, R. A. (1985). Actualization, integration, and fear of death: A test of the additive model. Death Stud. 9, 235–244. doi: 10.1080/07481188508252520
Nguyen, H. T., Do, B. N., Pham, K. M., Kim, G. B., Dam, H. T., Nguyen, T. T., et al. (2020). Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17, 4164. doi: 10.3390/ijerph17114164
Nguyen, M. H., Pham, T., Nguyen, K. T., Nguyen, Y. H., Tran, T. V., Do, B. N., et al. (2021a). Negative impact of fear of COVID-19 on health-related quality of life was modified by health literacy, eHealth literacy, and digital healthy diet literacy: a multi-hospital survey. Int. J. Environ. Res. Public Health 18, 4929. doi: 10.3390/ijerph18094929
Nguyen, T. V., Dai Tran, Q., Phan, L. T., Vu, L. N., Truong, D. T. T., Truong, H. C., et al. (2021b). In the interest of public safety: rapid response to the COVID-19 epidemic in Vietnam. BMJ Global Health 6, e004100. doi: 10.1136/bmjgh-2020-004100
Nicola, M., Alsafi, Z., Sohrabi, C., Kerwan, A., Al-Jabir, A., Iosifidis, C., et al. (2020). The socio-economic implications of the coronavirus pandemic (COVID-19): a review. Int. J. Surgery 78, 185–193. doi: 10.1016/j.ijsu.2020.04.018
Okubo, R., Yoshioka, T., Ohfuji, S., Matsuo, T., and Tabuchi, T. (2021). COVID-19 vaccine hesitancy and its associated factors in Japan. Vaccines 9, 662. doi: 10.3390/vaccines9060662
Oldin, C., Golsäter, M., Schollin Ask, L., Fredriksson, S., and Stenmarker, M. (2019). Introduction of rotavirus vaccination in a Swedish region: Assessing parental decision-making, obtained vaccination coverage and resulting hospital admissions. Acta Paediatr. Int. J. Paediatr. 108, 1329–1337. doi: 10.1111/apa.14674
Opel, D. J., Salmon, D. A., and Marcuse, E. K. (2020). Building trust to achieve confidence in COVID-19 vaccines. JAMA Network Open 3, e2025672–e2025672. doi: 10.1001/jamanetworkopen.2020.25672
Otieno, N. A., Otiato, F., Nyawanda, B., Adero, M., Wairimu, W. N., and Ouma, D. (2020). Drivers and barriers of vaccine acceptance among pregnant women in Kenya. Human Vac. Immunother. 16, 2029–2037. doi: 10.1080/21645515.2020.1723364
Paterson, P., Meurice, F., Stanberry, L. R., Glismann, S., Rosenthal, S. L., and Larson, H. J. (2016). Vaccine hesitancy and healthcare providers. Vaccine 34, 6700–6706. doi: 10.1016/j.vaccine.2016.10.042
Pelegrín-Borondo, J., Arias-Oliva, M., Almahameed, A. A., and Román, M. P. (2021). Covid-19 vaccines: a model of acceptance behavior in the healthcare sector. Eur. Res. Manag. Bus. Econ. 27, 100171. doi: 10.1016/j.iedeen.2021.100171
Pham, V. T., Huynh, V. S., Dang-Thi, N. T., and Tran-Chi, V. L. (2021). Fear of COVID-19 among Vietnamese Undergraduates and Predictors of their Fear. J. Biochem. Technol. 12, 27–32. doi: 10.51847/iSWa5cqOkF
Pilishvili, T., Fleming-Dutra, K. E., Farrar, J. L., Gierke, R., Mohr, N. M., Talan, D. A., et al. (2021). Interim estimates of vaccine effectiveness of Pfizer-BioNTech and Moderna COVID-19 vaccines among health care personnel-−33 US sites, January–March 2021. Morbid. Mortal. Wkly. Rep. 70, 753–758. doi: 10.15585/mmwr.mm7020e2
Pogue, K., Jensen, J. L., Stancil, C. K., Ferguson, D. G., Hughes, S. J., Mello, E. J., et al. (2020). Influences on attitudes regarding potential COVID-19 vaccination in the United States. Vaccines 8, 582. doi: 10.3390/vaccines8040582
Pyszczynski, T., Greenberg, J., and Solomon, S. (1999). A dual-process model of defense against conscious and unconscious death-related thoughts: an extension of terror management theory. Psychol. Rev. 106, 835–845. doi: 10.1037/0033-295X.106.4.835
Quach, H.-L., and Hoang, N.-A. (2020). COVID-19 in Vietnam: a lesson of pre-preparation. J. Clin. Virol. 127, 104379. doi: 10.1016/j.jcv.2020.104379
Reiter, P. L., Katz, M. L., Bauermeister, J. A., Shoben, A. B., Paskett, E. D., and McRee, A.-L. (2018). Increasing human papillomavirus vaccination among young gay and bisexual men: a randomized pilot trial of the outsmart HPV intervention. LGBT Health 5, 325–329. doi: 10.1089/lgbt.2018.0059
Rémy, V., Zöllner, Y., and Heckmann, U. (2015). Vaccination: the cornerstone of an efficient healthcare system. J. Market Access Health Policy 3, 27041. doi: 10.3402/jmahp.v3.27041
Reuken, P. A., Rauchfuss, F., Albers, S., Settmacher, U., Trautwein, C., Bruns, T., et al. (2020). Between fear and courage: Attitudes, beliefs, and behavior of liver transplantation recipients and waiting list candidates during the COVID-19 pandemic. Am. J. Transplant. 20, 3042–3050. doi: 10.1111/ajt.16118
Rodríguez-Hidalgo, A. J., Pantaleón, Y., Dios, I., and Falla, D. (2020). Fear of COVID-19, stress, and anxiety in university undergraduate students: a predictive model for depression. Front. Psychol. 11, 591797. doi: 10.3389/fpsyg.2020.591797
Rosen, B., Waitzberg, R., Israeli, A., Hartal, M., and Davidovitch, N. (2021). Addressing vaccine hesitancy and access barriers to achieve persistent progress in Israel's COVID-19 vaccination program. Isr. J. Health Policy Res. 10, 1–20. doi: 10.1186/s13584-021-00481-x
Rosenstock, I. M. (1974). Historical origins of the health belief model. Health Educ. Monogr. 2, 328–335. doi: 10.1177/109019817400200403
Rothe, C., Schunk, M., Sothmann, P., Bretzel, G., Froeschl, G., Wallrauch, C., et al. (2020). Transmission of 2019-nCoV infection from an asymptomatic contact in Germany. N. Engl. J. Med. 382, 970–971. doi: 10.1056/NEJMc2001468
Salali, G. D., and Uysal, M. S. (2020). COVID-19 vaccine hesitancy is associated with beliefs on the origin of the novel coronavirus in the UK and Turkey. Psychol. Med. 19, 1–3. doi: 10.1017/S0033291720004067
Sarstedt, M., Hair Jr, J. F., Nitzl, C., Ringle, C. M., and Howard, M. C. (2020). Beyond a tandem analysis of SEM and PROCESS: use of PLS-SEM for mediation analyses!. Int. J. Market Res. 62, 288–299. doi: 10.1177/1470785320915686
Schmid, P., Rauber, D., Betsch, C., Lidolt, G., and Denker, M.-L. (2017). Barriers of influenza vaccination intention and behavior–a systematic review of influenza vaccine hesitancy, 2005–2016. PLoS ONE 12, e0170550. doi: 10.1371/journal.pone.0170550
Scrima, F., Miceli, S., Caci, B., and Cardaci, M. (2022). The relationship between fear of COVID-19 and intention to get vaccinated. The serial mediation roles of existential anxiety and conspiracy beliefs. Pers. Individual Diff. 184, 111188. doi: 10.1016/j.paid.2021.111188
Sekizawa, Y., Hashimoto, S., Denda, K., Ochi, S., and So, M. (2022). Association between COVID-19 vaccine hesitancy and generalized trust, depression, generalized anxiety, and fear of COVID-19. BMC Public Health 22, 1–17. doi: 10.1186/s12889-021-12479-w
Serpell, L., and Green, J. (2006). Parental decision-making in childhood vaccination. Vaccine 24, 4041–4046. doi: 10.1016/j.vaccine.2006.02.037
Shiehzadegan, S., Alaghemand, N., Fox, M., and Venketaraman, V. (2021). Analysis of the delta variant B. 1.617. 2 COVID-19. Clinics Pract. 11, 778–784. doi: 10.3390/clinpract11040093
Shrout, P. E., and Bolger, N. (2002). Mediation in experimental and nonexperimental studies: new procedures and recommendations. Psychol. Methods 7, 422. doi: 10.1037/1082-989X.7.4.422
Soraci, P., Ferrari, A., Abbiati, F. A., Del Fante, E., De Pace, R., and Urso, A. (2020). Validation and psychometric evaluation of the Italian Version of the Fear of COVID-19 Scale. Int. J. Ment. Health Addict. 20, 1913–1922. doi: 10.1007/s11469-020-00277-1
Stefanut, A. M., Vintil,ă, M., Tomi,tă, M., Treglia, E., Lungu, M. A., and Tomassoni, R. (2021). The influence of health beliefs, of resources, of vaccination history, and of health anxiety on intention to accept COVID-19 vaccination. Front. Psychol. 12. 729803. doi: 10.3389/fpsyg.2021.729803
Štěpánek, L., Janošíkov,á, M., Nakládalová, M., Štěpánek, L., Boriková, A., and Vildová, H. (2021). Motivation to COVID-19 vaccination and reasons for hesitancy in employees of a Czech tertiary care hospital: a cross-sectional survey. Vaccines 9, 863. doi: 10.3390/vaccines9080863
Szmyd, B., Karuga, F. F., Bartoszek, A., Staniecka, K., Siwecka, N., Bartoszek, A., et al. (2021). Attitude and behaviors towards SARS-CoV-2 vaccination among healthcare workers: a cross-sectional study from Poland. Vaccines 9, 218. doi: 10.3390/vaccines9030218
Teo, L. M., Smith, H. E., Lwin, M.O., and Tang, W. E. (2019). Attitudes and perception of influenza vaccines among older people in Singapore: a qualitative study. Vaccine 37, 6665–6672. doi: 10.1016/j.vaccine.2019.09.037
Thomson, A., Robinson, K., and Vallée-Tourangeau, G. (2016). The 5As: a practical taxonomy for the determinants of vaccine uptake. Vaccine 34, 1018–1024. doi: 10.1016/j.vaccine.2015.11.065
Tsutsui, Y., Benzion, U., and Shahrabani, S. (2012). Economic and behavioral factors in an individual's decision to take the influenza vaccination in Japan. J. Socio Econ. 41, 594–602. doi: 10.1016/j.socec.2012.05.001
Vaughan, E., and Tinker, T. (2009). Effective health risk communication about pandemic influenza for vulnerable populations. Am. J. Public Health 99, S324–S332. doi: 10.2105/AJPH.2009.162537
Wang, J., Jing, R., Lai, X., Zhang, H., Lyu, Y., Knoll, M. D., et al. (2020). Acceptance of COVID-19 Vaccination during the COVID-19 Pandemic in China. Vaccines 8, 482. doi: 10.3390/vaccines8030482
Wang, Q., Yue, N., Zheng, M., Wang, D., Duan, C., Yu, X., et al. (2018). Influenza vaccination coverage of population and the factors influencing influenza vaccination in mainland China: a meta-analysis. Vaccine 36, 7262–7269. doi: 10.1016/j.vaccine.2018.10.045
Weintraub, R. L., Subramanian, L., Karlage, A., Ahmad, I., and Rosenberg, J. (2021). COVID-19 Vaccine To Vaccination: Why Leaders Must Invest In Delivery Strategies Now: Analysis describe lessons learned from past pandemics and vaccine campaigns about the path to successful vaccine delivery for COVID-19. Health Aff. 40, 33–41. doi: 10.1377/hlthaff.2020.01523
Willis, D. E., Andersen, J. A., Bryant-Moore, K., Selig, J. P., Long, C. R., Felix, H. C., et al. (2021). COVID-19 vaccine hesitancy: Race/ethnicity, trust, and fear. Clin. Transl. Sci. 14, 2200–2207. doi: 10.1111/cts.13077
Wong, L. P., Alias, H., Wong, P.-F., Lee, H. Y., and AbuBakar, S. (2020). The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Human Vaccines Immunother. 16, 2204–2214. doi: 10.1080/21645515.2020.1790279
World Health Organization (2021a). WHO Coronavirus (COVID-19) Dashboard. Available online at: https://covid19.who.int/
World Health Organization (2021b). COVID-19 news_3 November 2021. Available online at: https://covid19.who.int/
Keywords: beliefs, benefits of vaccination, fear of COVID-19, vaccination injections, health belief model
Citation: Hoang HT, Nguyen XTK, Huynh SV, Hua TD, Tran HTT and Tran-Chi V-L (2022) The effect of vaccination beliefs regarding vaccination benefits and COVID-19 fear on the number of vaccination injections. Front. Psychol. 13:968902. doi: 10.3389/fpsyg.2022.968902
Received: 14 June 2022; Accepted: 21 September 2022;
Published: 19 October 2022.
Edited by:
Victoria Team, Monash University, AustraliaReviewed by:
Assis Kamu, Universiti Malaysia Sabah, MalaysiaCopyright © 2022 Hoang, Nguyen, Huynh, Hua, Tran and Tran-Chi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Vinh-Long Tran-Chi, bG9uZ3RjdkBoY211ZS5lZHUudm4=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.