
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 08 July 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.933207
This article is part of the Research TopicPsychological Impact of COVID-19 on individuals: Through Active Choices and Passive AdaptionView all 17 articles
 Qiaoyan Jin1,2†
Qiaoyan Jin1,2† Wenxian Ma2†
Wenxian Ma2† Yang Zhang1,2†
Yang Zhang1,2† Huiyuan Wang1
Huiyuan Wang1 Juanjuan Hao1
Juanjuan Hao1 Yan Geng1
Yan Geng1 Bo Zhong1
Bo Zhong1 Jing Li1
Jing Li1 Wei Hou1*
Wei Hou1* Shemin Lu2*
Shemin Lu2*Purpose: A large body of evidence has revealed that the sudden outbreak of public health emergencies induces dramatic effects on the mental health of the general public. We aimed to investigate the level of anxiety sensitivity and its risk factors in children and adolescents from northwest China during the COVID-19 pandemic lockdown in early 2020.
Methods: A cross-sectional survey was conducted through the Wenjuanxing platform using a convenience sampling method between 18 and 26 February 2020. The self-designed questionnaire contained sociodemographic characteristics, factors associated with the COVID-19 pandemic, and the Childhood Anxiety Sensitivity Index (CASI) scale. The data from 1,091 valid questionnaires from students aged 9–17 years were analyzed using ANOVA, multiple linear regression, and binary logistic regression.
Results: The average CASI scores were 11.47 ± 6.631, and 642 students (58.9%) had prominent anxiety sensitivity. Gender, education level, family members participating in anti-COVID-19 work, getting ill and needing medical help during the lockdown, feeling afraid or having heart palpitations on hearing things associated with COVID-19, believing that COVID-19 would have adverse impacts on themselves or their family in the future, and fear of infection were identified as significant factors for elevated levels of anxiety sensitivity (p < 0.05). We established a multiple linear regression model for the anxiety sensitivity score. Risk factors found for anxiety sensitivity in children and adolescents during the COVID-19 lockdown included studying in secondary or high school, becoming ill during the pandemic, feeling afraid or experiencing rapid heartbeat or palpitations on hearing about the COVID-19 pandemic, thinking that COVID-19 would have an adverse impact on themselves or their family in the future, and fear of infection.
Conclusions: During the COVID-19 pandemic and home quarantine, scores measuring the prevalence of anxiety sensitivity in children and adolescents from northwest China were elevated. We should develop measures that especially target possible risk factors to intervene against and prevent anxiety sensitivity in children and adolescents in both the current and future pandemics.
Coronavirus disease 2019 (COVID-19) is an emerging infectious disease caused by severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) (Commission, 2020) that has resulted in a global pandemic with an enormous impact on the health and routine activities of people worldwide (Fang et al., 2021a; Who, 2022). Sufficient data from previous studies on epidemics have revealed that public health emergencies arouse a series of mental health problems besides physical disease. In an investigation of a severe Legionnaires' Disease outbreak in Japan, 13.7% of the survivors demonstrated that they suffered from depressive symptoms (Tsuruta et al., 2005). In a survey on the 2005 SARS pandemic in China, Wu et al. reported that nearly 18% of respondents reported symptoms related to post-traumatic stress disorder (PTSD), anxiety, and depression (Wu et al., 2005). A more recent study reported that 83.1% of respondents had some anxiety about the swine flu outbreak in 2011 (Kanadiya and Sallar, 2011).
COVID-19, without exception, has been found to be a tremendous stressor affecting people's psychological wellbeing. For instance, Tian et al. (2020) found that COVID-19 had significant adverse sociopsychological effects on the Chinese public. Li et al. (2020) found that negative emotions (e.g., anxiety, depression, and indignation) and sensitivity to social risks increased, while scores of positive emotions (e.g., measured by the Oxford Happiness Questionnaire) and life satisfaction decreased 1 week after the declaration of the COVID-19 lockdown. Kim et al. (2021) found a high prevalence of depression and anxiety in society during the COVID-19 pandemic in Korea. Moreover, many Americans have increasingly used prescription drugs to deal with stress and anxiety related to the pandemic (Digon, 2020). These studies consistently showed that people's psychological wellbeing has been negatively influenced by the COVID-19 pandemic and its related control measures. These abnormal conditions of physiology drive behaviors that can include evacuation panic, resistance to public health measures, overburdening of hospitals and clinicians, blaming the government, and abandoning responsibilities to families and jobs. This cascade of effects has caused more severe and disabling ramifications from the COVID-19 pandemic than the disease itself.
Many studies of the impact of the pandemic on psychological conditions have focused on such changes in different populations, such as health care workers (Hao et al., 2021), medical students (ElHawary et al., 2021; Halperin et al., 2021), university students (Jiang, 2020; Mao et al., 2021), confirmed patients (Klaser et al., 2021; Shah et al., 2021), and sick persons with different illnesses (Colombo et al., 2020; Kotecha, 2020; Di Riso et al., 2021). Children and adolescents are a worthwhile study segment, as their comprehension of pandemic-related knowledge is limited, they have insufficient self-protective skills, and they heavily depend on adults for emotional support and physical care (Mollborn and Lawrence, 2018; Leach et al., 2021; Qiu et al., 2021). Therefore, they have been identified as a vulnerable segment of the population in psychosocial characteristics (Perrin et al., 2009; Stevenson et al., 2009) and are prone to suffering mental health problems when coping with disasters (Furr et al., 2010; Pfefferbaum et al., 2015).
Before the COVID-19 pandemic, however, few data existed on the effects of public health emergencies on the mental health of children and adolescents. Many researchers, realizing this lack, made calls for policymakers and clinicians to take the mental health needs of children and adolescents into account when making decisions during the influenza pandemic of 2009 (Perrin et al., 2009; Stevenson et al., 2009). During the COVID-19 pandemic, the psychological conditions of children and adolescents have attracted the attention of researchers. Studies revealed that this demographic suffers from a range of psychological disorders (Wang et al., 2020; Zhou et al., 2020a; McArthur et al., 2021; Ravens-Sieberer et al., 2021), such as depression, anxiety, insomnia, and stress. It is worth noting that, because of varying sociocultural and economic contexts (Dowd et al., 2011; Burgard et al., 2013; Fang et al., 2021b; Wu et al., 2022a), the mental health status of children and adolescents varies by region (Compton et al., 2006; Chen et al., 2020). Studies in China during the COVID-19 pandemic, however, have been conducted on a population mainly from the provinces in southeast and central China, including Henan (Xu et al., 2021), Hubei (Xie et al., 2020), Guangdong (Qin et al., 2021), Guangxi (Chi et al., 2021), Shanghai (Tang et al., 2021), Beijing, and Zhejiang (Chen et al., 2020). Few studies involved children and adolescents from northwest China, where population density is low, the economic situation is poor, and ethnic minorities are concentrated. Therefore, assessing the mental health condition of these children and adolescents was an unmet need.
Anxiety sensitivity refers to the belief that anxiety-related sensory arousal will have negative consequences for the individual, such as death, mental disorders, and social rejection; this belief, in turn, generates fear in the form of primary sensory arousal (Reiss et al., 1986; Taylor et al., 2007). In this way, anxiety sensitivity is a relatively stable indicator that reflects the degree of fear in individuals (Taylor et al., 2007). In addition to being a risk factor for anxiety disorders, anxiety sensitivity can predict anxiety, and non-anxiety disorders (Olatunji and Wolitzky-Taylor, 2009), such as depression, substance abuse, and suicide (Naragon-Gainey, 2010; Oglesby et al., 2015). Therefore, anxiety sensitivity can be used to screen high-risk populations with mental disorders (Schmidt et al., 2010; Noël and Francis, 2011). Indeed, research from the COVID-19 pandemic shows that anxiety sensitivity is increased in adults and is positively associated with suicidal ideation (Allan et al., 2021), depression, and anxiety (Avidor et al., 2021). Taken together, these studies demonstrate that anxiety sensitivity could be a significant predictor of COVID-19-related fear and consequent safety behaviors (Mayorga et al., 2022). Thus, the primary aim of the present study was to assess the anxiety sensitivity of children and adolescents in northwest China early in the pandemic. The purpose was to learn how to take measures to prevent and reduce adverse mental health outcomes and maladaptive behavioral responses resulting from current and future pandemics.
Since the outbreak of COVID-19, many efforts have been made to explore factors influencing psychological abnormalities in children and adolescents (Zhou et al., 2020b; Qin et al., 2021; Ravens-Sieberer et al., 2021; Tang et al., 2021). These researchers have confirmed that risk factors include mainly disturbance of routine life, lack of face-to-face contact with peers, fears of infection, and poor efficiency of online learning. However, the influence of physical conditions on mental health in this period has not been investigated, while evidence has shown that physical disease is a significant influencing factor (Ohrnberger et al., 2017; Felix et al., 2020). To fill these gaps, we explored risk factors associated with anxiety sensitivity in children and adolescents from northwest China during the COVID-19 pandemic. Our purpose was to provide a scientific basis for formulating precise psychological preventions and interventions.
It is well-known that cross-sectional questionnaire surveys are generally quick, easy, convenient, and cost-effective to perform. They are particularly suitable for estimating the prevalence of disease in a population and exploring or screening for possible risk factors (Sedgwick, 2014). Thus, we employed a cross-sectional questionnaire in our study. Because of home quarantine during the pandemic, face-to-face interviews could not be conducted. Therefore, the study questionnaire was distributed and retrieved online using the program “Questionnaire Star” (https://www.wjx.cn/), which is widely used and well-recognized as a professional online survey tool (Qin et al., 2021; Tang et al., 2021).
Children and adolescents aged 9–17 years were recruited using a convenience sampling method from 18 to 26 February 2020, following a month of the COVID-19 outbreak and subsequent lockdown in China, i.e., the peak of the pandemic. The subjects were mainly from Gansu, Shaanxi, and Xinjiang provinces, all located in northwest China. Teachers sent the link address of the questionnaire to a WeChat group that included teachers, participants, and parents. Then, participants were directed to the Questionnaire Star program by the link address and completed the questionnaire if they were interested. Before filling out the questionnaire, participants provided informed consent. Meanwhile, the teachers were responsible for explaining the manual procedures for the survey in detail. A phone number and WeChat ID for a pediatrician were also included in the questionnaire so that participants could consult and interact with the pediatrician at any time. The entire survey was carried out using voluntary, anonymous, and confidential principles.
In the preface, the purpose and organization of the survey were described. According to the wishes of the students and their guardians, every student filled out the questionnaire voluntarily. All participants could submit, terminate, and repost the questionnaire directly, even though they had started to fill it out with prior consent. The study was approved by the ethics committee of the Second Affiliated Hospital of Xi'an Jiaotong University and carried out following American Association for Public Opinion Research (AAPOR) reporting guidelines.
The survey questionnaire was self-designed and consisted of three sections. Its rationality and functionality were assessed by a pilot study that preceded the study.
Sociodemographic characteristics were chosen by the authors. They included a set of questions regarding sex, age, ethnicity, place of residence, education level, and the number of people residing in the same home during the lockdown.
Using factors that may affect anxiety sensitivity in the context of a pandemic, as reported in previous literature, the research team selected factors associated with the COVID-19 pandemic. All the factors were probed as close-ended questions. The response options allowed various levels of choice. Generally, factors were divided into three categories.
The first category asked about the condition of the respondent's physical health. Participants were asked to indicate the following: (1) whether you have suffered from chronic disease in the 6 months prior to the pandemic (i.e., up to now, illness that has lasted for at least 6 months); (2) whether you have gone to see a doctor due to illness in the 3 months prior to the pandemic; and (3) whether you have gone to see a doctor due to illness during the period of the pandemic.
The second category dealt with the knowledge of COVID-19. Participants were asked the following: (1) Whether your family often talks about the COVID-19 pandemic. Answer options were: never, sometimes, or often. (2) How well do you understand the novel coronavirus and its outbreak (assessed by knowledge of its cause, transmission route, and preventive measures for COVID-19)? Answer options were: nothing, a little, or familiar. (3) What is your attitude toward taking self-protective measures (e.g., wearing a mask, hand washing)? Answer options were: actively, passively, or not taking any protective measures. (4) Whether you feel afraid or your heart beats fast when you hear things associated with COVID-19. Answer options were: never, sometimes, often, or always. (5) Whether family members have been involved in anti-COVID-19 efforts. Answer options were: yes or no. (6) Whether you perceive that the pandemic will have adverse impacts on yourself or your family in the future. Answer options were: yes or no. (7) Whether you think you might have COVID-19 at this time. Answer options were: yes or no. (8) Whether you have close contacts diagnosed with COVID-19. Answer options were: yes or no.
The last third and final category were about the routines of the participants. Participants were asked: (1) How much time do you spend on entertainment (e.g., playing games, listening to music, browsing the web, watching TV, etc.) per day? Answer options were <1, 1–2, or >2 h/day. (2) How much time do you spend on physical activity per day. Answer options were: <0.5, 0.5–1, or >1 h/day. (3) How much time do you spend studying per day? Answer options were: <1, 1–2, or >2 h/day.
The Childhood Anxiety Sensitivity Index (CASI) is an 18-item self-reported Likert scale that can be used to assess anxiety sensitivity. It was developed by Silverman et al. (1999) on the basis of the Anxiety Sensitivity Index. The scale is rated on a 3-point scale ranging from 1 to 3 (“none” to “a lot”), and total scores range from 0 to 36, with higher scores indicating a higher level of anxiety sensitivity. Ren Fang (2008) demonstrated that the Chinese version of CASI has good reliability, validity, and strong internal consistency. The internal consistency for the present sample is 0.896, and the cutoff values are 9 for boys and 11 for girls, indicating anxiety sensitivity, respectively (Ren Fang, 2012). Although several hierarchical models have been proposed for the factor structure of CASI, in this study, a 3-factor model was administered because of its stability and consistency (Francis et al., 2019).
Categorical variables were presented as numbers and percentages, and continuous variables were presented as the mean ± SD. A two-sample independent t-test was used for comparisons between the two groups. One-way ANOVA was used for multigroup comparisons, and the least significant difference (LSD) method was used for pair comparisons. Multiple linear regression analysis was used to analyze factors influencing the CASI score. Binary logistic regression was used to analyze risk factors associated with high anxiety sensitivity. p < 0.05 was considered significant. All statistical tests were undertaken using SPSS Statistics software version 16.0 (IBM, Armonk, NY, USA).
A total of 1,141 questionnaires were retrieved in this study. Questionnaires with incomplete information and time spent of <90 s were deleted to ensure the reliability of data. In the final analysis, 1,091 (95.62%) questionnaires were included.
The general demographic data are shown in Table 1. Study participants comprised 593 females (54.4%) and 498 males (45.6%) with an average age of 13.27 ± 2.443 years. Among participants, 808 (74.1%) were of Han nationality, and 283 (25.9%) were others. In terms of education level, 524 (48.0%) respondents were enrolled in primary school, 296 (27.1%) were in secondary school, and 271 (24.8%) were in high school. Participants were from urban (19.6%), suburban (19.2%), and rural (61.1%) areas. Among respondents, 156 (14.3%) stated that their family members participated in anti-COVID-19 work. The average number of people living in the same home during the lockdown was 4.58 ± 1.258; among them, 948 (86.9%) were living with their parents, 398 (36.5%) were living with their grandparents, 726 (66.5%) were living with their siblings, and 48 (4.4%) were living with other people. Other respondent demographics and characteristics associated with the COVID-19 pandemic are presented in Table 1.
The total CASI scores in this study ranged from 0 to 36, with an average score of 11.47 ± 6.631. Overall, 642 (58.8%) respondents reported anxiety sensitivity. Owing to sex differences in the threshold for anxiety sensitivity, the prevalence rates of anxiety sensitivity in female and male participants were 56.8 and 61.2%, respectively (Table 5). Additionally, as Table 2 shows, an in-depth analysis of three dimensions of anxiety sensitivity found that the levels of physical concerns, mental concerns, and social concerns differed significantly between respondents with or without anxiety sensitivity.
One-way ANOVA and the t-test were used to analyze factors influencing CASI scores. The results are shown in Table 3. Several factors were significantly related to CASI scores: gender, ethnicity, educational level, physical condition during the lockdown, discussion about COVID-19 within the family, knowledge about COVID-19, attitude toward taking protective measures, feeling afraid or experiencing rapid heartbeat or palpitations on hearing about COVID-19, perceiving that COVID-19 had adverse impacts on self or family, family members being involved in anti-epidemic work, and fear of infection. Further analysis by the LSD method found that the scores of high school students were significantly higher than those of secondary school students (p = 0.045), and those of secondary school students were significantly higher than those of primary school students (p = 0.002). The scores of those whose family members discussed the pandemic of COVID-19 sometimes (p = 0.001) or often (p < 0.001) were significantly higher than those whose family members did not. The scores of those who thought they were familiar with (p = 0.002) or knew a little (p < 0.001) about COVID-19 were significantly higher than those who did not (p < 0.001); the scores of those who took protective measures actively (p = 0.015) or passively (p = 0.016) were significantly higher than those who did not. Lastly, the scores of those who felt afraid and alarmed to the point of experiencing rapid heartbeats or palpitations when hearing things related to the epidemic were significantly higher than those who did not have these responses (p < 0.001).
In addition, we conducted multiple linear regression analysis by a variable with the aforementioned significant factors, age, and number of people in the same home during the lockdown in order to identify the significant factors correlated with the level of anxiety sensitivity. Finally, we constructed a multiple linear regression model of anxiety sensitivity scores from the factors obtained (Table 4), including gender, school grade level, seeking medical help because of illness during the lockdown, feeling afraid, or experiencing rapid heartbeat on hearing things related to COVID-19, family members participating in anti-COVID-19 work, perceiving that COVID-19 would have an adverse impact on self or family, and fear of infection.
We performed a binary logistic regression analysis to identify risk factors for anxiety sensitivity in children and adolescents from northwest China. As Table 5 shows, there were several risk factors for anxiety sensitivity in children and adolescents during lockdown: learning stage in secondary school (OR, 1.743; 95% CI [1.274–2.384]) or high school (OR, 2.151; 95% CI [1.544–2.997]); becoming ill and needing to go to hospital during the lockdown (OR, 1.462; 95% CI [1.038–2.059]); being afraid of hearing things related to COVID-19 either sometimes (OR, 2.900; 95% CI [2.187–3.846]), often (OR, 2.522; 95% CI [1.595–3.988]), or always (OR, 4.061; 95% CI [1.945–8.480]); believing that COVID-19 would have an adverse impact on self or family (OR, 1.513; 95% CI [1.135–2.017]); and fear of infection (OR, 1.703; 95% CI [1.187–2.444]).
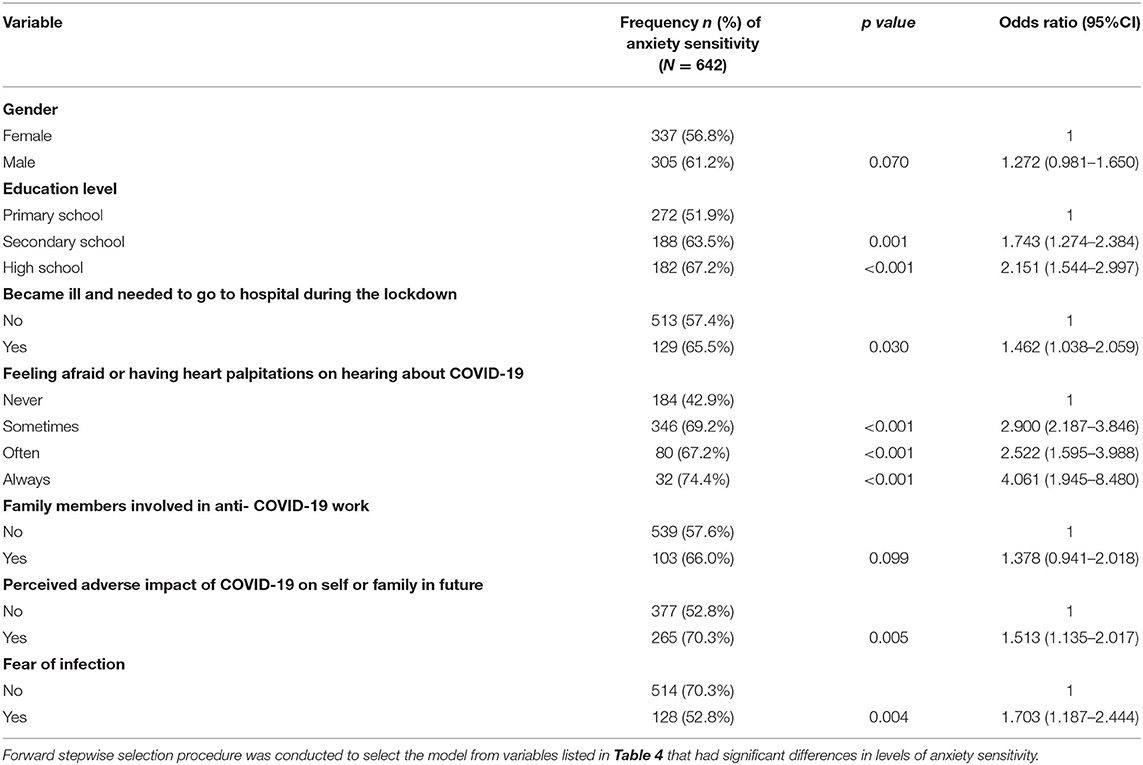
Table 5. Factors related to anxiety sensitivity in children and adolescents during the COVID-19 lockdown.
This is one of few studies, to our knowledge, that describes the psychological condition of children and adolescents from the northwest China during the pandemic. We found that the level of anxiety sensitivity became dramatically elevated during the pandemic. We also revealed several possible risk factors associated with high anxiety sensitivity: studying in secondary or high school, becoming ill, feeling afraid or having heart palpitations on hearing about the COVID-19 pandemic, thinking that COVID-19 would have an adverse impact on self or family in the future, and fear of infection. Together, these results will help us to better understand the mental health conditions of children and adolescents when faced with current or future emerging infectious disease outbreaks and epidemics. Thus, we will be able to provide scientific guidance to formulate targeted policies to prevent such mental illness and intervene when it occurs.
Initially, our results showed that the level of anxiety sensitivity in children and adolescents from northwest China during the pandemic increased significantly, exceeding that of children and adolescents assessed prior to the outbreak of COVID-19 (Ren Fang, 2012). Due to the lack of data on the anxiety sensitivity of children and adolescents in other parts of China during the pandemic, it is not possible to compare the levels of anxiety sensitivity of children and adolescents in northwest China with those from other parts of China. In our sample, 58.8% of participants met the screening criteria for anxiety sensitivity. In related research, Tang et al. (2021) reported on the prevalence of depressive symptoms (19.7%) and anxiety symptoms (24.9%) in children and adolescents from Shanghai during the pandemic, and Xie et al. (2020) reported on the prevalence of depressive symptoms (26.5%) and anxiety symptoms (19.6%) in children and adolescents in Wuhan. Although the rate of abnormal psychological status among children and adolescents varied in the different studies, these findings consistently suggest that the COVID-19 pandemic has had an adverse impact on the psychological status of children and adolescents.
As is well-known, the physical disease can influence psychological conditions. However, the most interesting and concerning findings of the present study are that becoming ill and needing medical treatment during the lockdown was a risk factor for anxiety sensitivity, whereas having the chronic disease in the preceding 6 months or experiencing illness and seeking medical advice in the past 3 months was not a risk factor. This difference might be due to the variety of clinical symptoms of COVID-19 (Huang et al., 2020). Also, it is difficult for children and adolescents to distinguish the symptoms of the general disease from those of COVID-19, and they may have guessed that they were infected with COVID-19, thus elevating their levels of anxiety sensitivity. Those with chronic diseases or experience seeking medical advice previously, by contrast, knew their health conditions well and were less likely to make false assumptions and guesses.
Similar to the findings of Zhou et al. (2020b), our study revealed that the higher the school grade level, the higher the CASI score. This correlation may be due to the fact that middle school students attach more importance to their academic achievements and interpersonal communication (Wang et al., 2007). Moreover, as school age increases, students' academic stress significantly increases, and interpersonal relationships become more complicated. After the outbreak of COVID-19, lockdown measures and postponement of the spring semester disturbed learning schedules and daily life (Fang et al., 2019, 2021c; Wu et al., 2022b). Although students could study and communicate online, poor learning efficiency and restrictions on communication with peers may have increased their anxiety sensitivity.
The COVID-19 pandemic is the most serious public health event these children and adolescents have experienced. In this survey, 62.4% of the respondents felt afraid and experienced a rapid heartbeat when they heard information about COVID-19. Further analysis found that concerns about the adverse impacts of COVID-19 on themselves and their families in the future, fears of being infected with COVID-19, and fears upon hearing information about the pandemic were all risk factors for anxiety sensitivity. On the one hand, this might be related to their young age and lack of mental resilience in response to adversity (Liu Wen and Lin, 2019). On the other hand, a virus that is highly contagious has a high rate of mortality, has no specific treatment, and has increasing numbers of confirmed cases and deaths might have aggravated their fears and anxiety sensitivity. Meanwhile, in order to control the spread of disease, governments implementing strict lockdowns might also have disturbed parents' careers and family economics (Chen et al., 2022; Fang et al., 2022), while postponement of school re-openings might have interfered with children's schoolwork, resulting in enhanced anxiety sensitivity among children and adolescents.
Because the pandemic was ongoing during the investigation period, the study had to take a convenience sampling approach and be conducted online; thus, the sample size is relatively small, which limits the applicability and generalizability of the results. Also, because of the nature of a cross-sectional study, the ability to establish causal relationships between risk factors and anxiety sensitivity was limited. Therefore, longitudinal follow-up studies should be conducted that expand sample sources and investigate the respondents face to face. This will improve the study design and increase the applicability and generalizability of the results.
During the COVID-19 pandemic and home quarantine, children and adolescents from northwest China experienced elevated levels of anxiety sensitivity. Therefore, the whole society should be aware of the negative impact of the pandemic on the mental health of children and adolescents and develop timely and effective interventions to prevent and intervene during pandemics so as to avoid more severe and disabling consequences. Specifically, parents should pay more attention to the physical health of their children during lockdowns and help them to seek medical help as soon as symptoms appear. Doctors should give them professional advice and allay their doubts and concerns about COVID-19, thereby reducing their anxiety sensitivity. The media should report information related to the pandemic accurately to avoid excessive exaggeration of its seriousness. At the same time, because the pandemic is dangerous, it is imperative to take strict control measures that interfere with people's daily routines. Schools and parents should encourage students to view the pandemic from a long-term perspective with a positive, optimistic aspect. In this way, they will help children to accept and adapt to lockdown measures with heartfelt understanding so as to relieve their anxiety.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Second Affiliated Hospital of Xi'an Jiaotong University. Written informed consent from the participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
QJ, WM, and YZ designed the questionnaire, organized the survey, and carried out the literature searches and manuscript preparation. HW, YG, and JH assisted with data acquisition and analyses. BZ and JL carried out manuscript editing. WH and SL undertook a manuscript review. All authors approved the final version of the manuscript.
This work was supported by the Foundation of the Second Affiliated Hospital of Xi'an Jiaotong University [Grant No. YJ (QN)201808] and the Project of Shaanxi Province to Improve Public Science Quality (Grant No. 2021PSL93).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would express our gratitude to the participants for completing the survey questionnaire. We especially appreciate the teachers who were responsible for assigning the online questionnaire to students. We further thank the guardians of children and adolescents for their assistance in filling out the questionnaires.
Allan, N. P., Volarov, M., Koscinski, B., Pizzonia, K. L., Potter, K., Accorso, C., et al. (2021). Lonely, anxious, and uncertain: critical risk factors for suicidal desire during the COVID-19 pandemic. Psychiatry Res. 304, 114144. doi: 10.1016/j.psychres.2021.114144
Avidor, S., Abu Hamam, A., and Lahav, Y. (2021). The toll of feeling older: subjective age moderates the associations between anxiety sensitivity and symptoms of anxiety and depression during COVID-19 pandemic. J. Gerontol. B Psychol. Sci. Soc. Sci. 77, e5–e10. doi: 10.1093/geronb/gbab082
Burgard, S. A., Elliott, M. R., Zivin, K., and House, J. S. (2013). Working conditions and depressive symptoms: a prospective study of US adults. J. Occup. Environ. Med. 55, 1007–1014. doi: 10.1097/JOM.0b013e3182a299af
Chen, G., Fang, J., Gozgor, G., and Pekel, S. (2022). Measuring uncertainty in export destinations and its impact on economic growth: evidence from Turkey. Emerg. Mark. Finance Trade. 1–16. doi: 10.1080/1540496X.2022.2068412
Chen, S., Cheng, Z., and Wu, J. (2020). Risk factors for adolescents' mental health in wuhan a comparison between Wuhan and other urban area ofchina. Global Health 16, 96. doi: 10.1186/s12992-020-00627-7
Chi, X., Liang, K., Chen, S. T., Huang, Q., Huang, L., Yu, Q., et al. (2021). Mental health problems among Chinese adolescents: the importance of nutrition and physical activity. Int. J. Clin. Health Psychol. 21, 100218. doi: 10.1016/j.ijchp.2020.100218
Colombo, C., Burgel, P. R., Gartner, S., Van Koningsbruggen-Rietschel, S., Naehrlich, L., Sermet-Gaudelus, I., et al. (2020). Impact of COVID-19 on people with cystic fibrosis. Lancet Respir. Med. 8, E35–E36. doi: 10.1016/S2213-2600(20)30177-6
Commission, China National Health. (2020). Update on the Novel Coronavirus Pneumonia Outbreak. Beijing: China National Health Commission. Available online at: http://www.nhc.gov.cn/yzygj/s7653p/202001/4294563ed35b43209b31739bd0785e67.shtml (accessed April 2, 2020).
Compton, W. M., Conway, K. P., Stinson, F. S., and Grant, B. F. (2006). Changes in the prevalence of major depression and comorbid substance use disorders in the United States between 1991-1992 and 2001-2002. Am. J. Psychiatry 163, 2141–2147. doi: 10.1176/ajp.2006.163.12.2141
Di Riso, D., Spaggiari, S., Cambrisi, E., Ferraro, V., Carraro, S., and Zanconato, S. (2021). Psychosocial impact of COVID-19 outbreak on Italian asthmatic children and their mothers in a post lockdown scenario. Sci. Rep. 11, 9152. doi: 10.1038/s41598-021-88152-4
Digon, S. (2020). Anti-Anxiety Prescription Meds Increase amid COVID-19 Pandemic, Report Says International Business Times. Available online at: https://www.webmd.com/lung/news/20200417/anxiety-depression-prescriptions-spiked-in-march
Dowd, J. B., Albright, J., Raghunathan, T. E., Schoeni, R. F., Leclere, F., and Kaplan, G. A. (2011). Deeper and wider: income and mortality in the USA over three decades. Int. J. Epidemiol. 40, 183–188. doi: 10.1093/ije/dyq189
ElHawary, H., Salimi, A., Barone, N., Alam, P., and Thibaudeau, S. (2021). The effect of COVID-19 on medical students' education and wellbeing: a cross-sectional survey. Can. Med. Educ. J. 12, 92–99. doi: 10.36834/cmej.71261
Fang, J., Gozgor, G., Lau, C. K. M., and Seetaram, N. (2022). Does policy uncertainty affect economic globalization? An empirical investigation. Appl. Econ. 54, 2510–2528. doi: 10.1080/00036846.2021.1998324
Fang, J., Gozgor, G., and Nolt, J. H. (2021a). Globalisation, economic uncertainty and labour market regulations: implications for the COVID-19 crisis. World Econ. 1–23. doi: 10.1111/twec.13230
Fang, J., Gozgor, G., and Yan, C. (2021b). Does globalisation alleviate polarisation? World Econ. 44, 1031–1052. doi: 10.1111/twec.13048
Fang, J., Wu, W., Lu, Z., and Cho, E. (2019). Using Baidu Index to nowcast mobile phone sales in China. Singapore Econ. Rev. 64, 83–96. doi: 10.1142/S021759081743007X
Fang, J., Zhang, X., Tong, Y., Xia, Y., Liu, H., and Wu, K. (2021c). Baidu Index and COVID-19 epidemic forecast: evidence from China. Front. Public Health 9, 685141. doi: 10.3389/fpubh.2021.685141
Felix, E., Rubens, S., and Hambrick, E. (2020). The relationship between physical and mental health outcomes in children exposed to disasters. Curr. Psychiatry Rep. 22, 33. doi: 10.1007/s11920-020-01157-0
Francis, S. E., Noël, V. A., and Ryan, S. L. (2019). A systematic review of the factor structure of anxiety sensitivity among children: current status and recommendations for future directions. Child Youth Care Forum 48, 603–632. doi: 10.1007/s10566-019-09502-y
Furr, J. M., Corner, J. S., Edmunds, J. M., and Kendall, P. C. (2010). Disasters and youth: a meta-analytic examination of posttraumatic stress. J. Consult. Clin. Psychol. 78, 765–780. doi: 10.1037/a0021482
Halperin, S. J., Henderson, M. N., Prenner, S., and Grauer, J. N. (2021). Prevalence of anxiety and depression among medical students during the COVID-19 pandemic: a cross-sectional study. J. Med. Educ. Curric. Dev. 8, 2382120521991150. doi: 10.1177/2382120521991150
Hao, Q., Wang, D., Xie, M., Tang, Y., Dou, Y., Zhu, L., et al. (2021). Prevalence and risk factors of mental health problems among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Front. Psychiatry 12, 567381. doi: 10.3389/fpsyt.2021.567381
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395, 497–506. doi: 10.1016/S0140-6736(20)30183-5
Jiang, R. (2020). Knowledge, attitudes and mental health of university students during the COVID-19 pandemic in China. Child. Youth Serv. Rev. 119, 105494. doi: 10.1016/j.childyouth.2020.105494
Kanadiya, M. K., and Sallar, A. M. (2011). Preventive behaviors, beliefs, and anxieties in relation to the swine flu outbreak among college students aged 18-24 years. Z. Gesundh. Wiss. 19, 139–145. doi: 10.1007/s10389-010-0373-3
Kim, D. M., Bang, Y. R., Kim, J. H., and Park, J. H. (2021). The prevalence of depression, anxiety and associated factors among the general public during COVID-19 pandemic: a cross-sectional study in Korea. J. Korean Med. Sci. 36, e214. doi: 10.3346/jkms.2021.36.e214
Klaser, K., Thompson, E. J., Nguyen, L. H., Sudre, C. H., Antonelli, M., Murray, B., et al. (2021). Anxiety and depression symptoms after COVID-19 infection: results from the COVID Symptom Study app. J. Neurol. Neurosurg. Psychiatry 92, 1254–1258. doi: 10.1136/jnnp-2021-327565
Kotecha, R. S. (2020). Challenges posed by COVID-19 to children with cancer. Lancet Oncol. 21, 235–235. doi: 10.1016/S1470-2045(20)30205-9
Leach, L. S., Dinh, H., Cooklin, A., Nicholson, J. M., and Strazdins, L. (2021). Australian parents' work-family conflict: accumulated effects on children's family environment and mental health. Soc. Psychiatry Psychiatr. Epidemiol. 56, 571–581. doi: 10.1007/s00127-020-01944-3
Li, S., Wang, Y., Xue, J., Zhao, N., and Zhu, T. (2020). The impact of COVID-19 epidemic declaration on psychological consequences: a study on active Weibo users. Int. J. Environ. Res. Public Health 17, 2032. doi: 10.3390/ijerph17062032
Liu Wen, Y. Z., and Lin, D. (2019). A meta-analysis of the relationship between resilience and mental health in children and adolescents. Stud. Psychol. Behav. 17, 31–37. Available online at: https://psybeh.tjnu.edu.cn/CN/Y2019/V17/I1/31
Mao, J., Gao, X., Yan, P., Ren, X., Guan, Y., and Yan, Y. (2021). Impact of the COVID-19 pandemic on the mental health and learning of college and university students: a protocol of systematic review and meta-analysis. BMJ Open 11, e046428. doi: 10.1136/bmjopen-2020-046428
Mayorga, N. A., Garey, L., Viana, A., Cardoso, J. B., Schmidt, N. B., and Zvolensky, M. J. (2022). Psychological distress and physical health symptoms in the Latinx population during the COVID-19 pandemic: exploring the role of anxiety sensitivity. Cognit. Ther. Res. 46, 20–30. doi: 10.1007/s10608-021-10243-3
McArthur, B. A., Racine, N., McDonald, S., Tough, S., and Madigan, S. (2021). Child and family factors associated with child mental health and well-being during COVID-19. Eur. Child Adolesc. Psychiatry. 24, 1–11. doi: 10.1007/s00787-021-01849-9
Mollborn, S., and Lawrence, E. (2018). Family, peer, and school influences on children's developing health lifestyles. J. Health Soc. Behav. 59, 133–150. doi: 10.1177/0022146517750637
Naragon-Gainey, K. (2010). Meta-analysis of the relations of anxiety sensitivity to the depressive and anxiety disorders. Psychol. Bull. 136, 128–150. doi: 10.1037/a0018055
Noël, V. A., and Francis, S. E. (2011). A meta-analytic review of the role of child anxiety sensitivity in child anxiety. J. Abnorm. Child Psychol. 39, 721–733. doi: 10.1007/s10802-011-9489-3
Oglesby, M. E., Capron, D. W., Raines, A. M., and Schmidt, N. B. (2015). Anxiety sensitivity cognitive concerns predict suicide risk. Psychiatry Res. 226, 252–256. doi: 10.1016/j.psychres.2014.12.057
Ohrnberger, J., Fichera, E., and Sutton, M. (2017). The relationship between physical and mental health: a mediation analysis. Soc. Sci. Med. 195, 42–49. doi: 10.1016/j.socscimed.2017.11.008
Olatunji, B. O., and Wolitzky-Taylor, K. B. (2009). Anxiety sensitivity and the anxiety disorders: a meta-analytic review and synthesis. Psychol. Bull. 135, 974–999. doi: 10.1037/a0017428
Perrin, P. C., McCabe, O. L., Everly, G. S. Jr., and Links, J. M. (2009). Preparing for an influenza pandemic: mental health considerations. Prehosp. Disaster Med. 24, 223–230. doi: 10.1017/S1049023X00006853
Pfefferbaum, B., Jacobs, A. K., Griffin, N., and Houston, J. B. (2015). Children's disaster reactions: the influence of exposure and personal characteristics. Curr. Psychiatry Rep. 17, 56. doi: 10.1007/s11920-015-0598-5
Qin, Z., Shi, L., Xue, Y., Lin, H., Zhang, J., Liang, P., et al. (2021). Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw. Open 4, e2035487. doi: 10.1001/jamanetworkopen.2020.35487
Qiu, Y., Xu, L., Pan, Y., He, C., Huang, Y., Xu, H., et al. (2021). Family resilience, parenting styles and psychosocial adjustment of children with chronic illness: a cross-sectional study. Front. Psychiatry 12, 646421. doi: 10.3389/fpsyt.2021.646421
Ravens-Sieberer, U., Kaman, A., Erhart, M., Devine, J., Schlack, R., and Otto, C. (2021). Impact of the COVID-19 pandemic on quality of life and mental health in children and adolescents in Germany. Eur. Child Adolesc. Psychiatry. 31, 1–14. doi: 10.1007/s00787-021-01889-1
Reiss, S., Peterson, R. A., Gursky, D. M., and Mcnally, R. J. (1986). Anxiety sensitivity, anxiety frequency and the prediction of fearfulness. Behav. Res. Ther. 24, 1–8. doi: 10.1016/0005-7967(86)90143-9
Ren Fang, W. X. Z. J. (2008). Application of childhood anxiety sensitivity index scale. Chin. J. Child Health Care 16, 518–520.
Ren Fang, Z. S. (2012). Application of childhood anxiety sensitivity index. Chin. J. Child Health Care 20, 330–332.
Schmidt, N. B., Keough, M. E., Mitchell, M. A., Reynolds, E. K., Macpherson, L., Zvolensky, M. J., et al. (2010). Anxiety sensitivity: prospective prediction of anxiety among early adolescents. J. Anxiety Disord. 24, 503–508. doi: 10.1016/j.janxdis.2010.03.007
Sedgwick, P. (2014). Cross-sectional studies: advantages and disadvantages. Br. Med. J. 348, g2276. doi: 10.1136/bmj.g2276
Shah, R., Ali, F. M., Nixon, S. J., Ingram, J. R., Salek, S. M., and Finlay, A. Y. (2021). Measuring the impact of COVID-19 on the quality of life of the survivors, partners and family members: a cross-sectional international online survey. BMJ Open 11, e047680. doi: 10.1136/bmjopen-2020-047680
Silverman, W. K., Ginsburg, G. S., and Goedhart, A. W. (1999). Factor structure of the childhood anxiety sensitivity index. Behav. Res. Ther. 37, 903–917. doi: 10.1016/S0005-7967(98)00189-2
Stevenson, E., Barrios, L., Cordell, R., Delozier, D., Gorman, S., Koenig, L. J., et al. (2009). Pandemic influenza planning: Addressing the needs of children. Am. J. Public. Health. 99, S255–S260. doi: 10.2105/AJPH.2009.159970
Tang, S., Xiang, M., Cheung, T., and Xiang, Y. T. (2021). Mental health and its correlates among children and adolescents during COVID-19 school closure: the importance of parent-child discussion. J. Affect. Disord. 279, 353–360. doi: 10.1016/j.jad.2020.10.016
Taylor, S., Zvolensky, M. J., Cox, B. J., Deacon, B., Heimberg, R. G., Ledley, D. R., et al. (2007). Robust dimensions of anxiety sensitivity: development and initial validation of the Anxiety Sensitivity Index-3. Psychol. Assess. 19, 176–188. doi: 10.1037/1040-3590.19.2.176
Tian, F., Li, H., Tian, S., Yang, J., Shao, J., and Tian, C. (2020). Psychological symptoms of ordinary Chinese citizens based on SCL-90 during the level I emergency response to COVID-19. Psychiatry Res. 288, 112992. doi: 10.1016/j.psychres.2020.112992
Tsuruta, K., Fujii, Y., Maeda, H., Murakata, T., and Kato, T. (2005). Mental health status and effects on daily life of patients of a large outbreak of Legionnaires Disease. Nihon Koshu Eisei Zasshi 52, 308–318. doi: 10.11236/jph.52.4-308
Wang, G., Zhang, Y., Zhao, J., Zhang, J., and Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395, 945–947. doi: 10.1016/S0140-6736(20)30547-X
Wang, H., Fan Fang, S. L., and Tong, N. (2007). Relationship between the anxiety transformation of children around adolescence and their self-concept. Chin. J. Pract. Pediatr. 22, 530–532.
Who (2022). Who Coronavirus (COVID-19) Dashboard 2021. Available online at: https://covid19.who.int/ (accessed April 3, 2022).
Wu, K. K., Chan, S. K., and Ma, T. M. (2005). Posttraumatic stress, anxiety, and depression in survivors of severe acute respiratory syndrome (SARS). J. Trauma. Stress 18, 39–42. doi: 10.1002/jts.20004
Wu, W., Wang, L., Erzurumlu, Y. O., Gozgor, G., and Yang, G. (2022a). Effects of country and geopolitical risks on income inequality: evidence from emerging economies. Emerg. Mark. Finance Trade. 1–13. doi: 10.1080/1540496X.2022.2070002
Wu, W., Zhang, H., Huang, L., and Wang, L. (2022b). Measuring the market power of China's medical product exports. Front. Public Health 10, 875104. doi: 10.3389/fpubh.2022.875104
Xie, X., Xue, Q., Zhou, Y., Zhu, K., Liu, Q., Zhang, J., et al. (2020). Mental health status among children in home confinement during the coronavirus disease 2019 outbreak in Hubei Province, China. JAMA Pediatr. 174, 898–900. doi: 10.1001/jamapediatrics.2020.1619
Xu, Q., Mao, Z., Wei, D., Liu, P., Fan, K., Wang, J., et al. (2021). Prevalence and risk factors for anxiety symptoms during the outbreak of COVID-19: a large survey among 373216 junior and senior high school students in China. J. Affect. Disord. 288, 17–22. doi: 10.1016/j.jad.2021.03.080
Zhou, S. J., Wang, L. L., Yang, R., Yang, X. J., Zhang, L. G., Guo, Z. C., et al. (2020a). Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med. 74, 39–47. doi: 10.1016/j.sleep.2020.06.001
Zhou, S. J., Zhang, L. G., Wang, L. L., Guo, Z. C., Wang, J. Q., Chen, J. C., et al. (2020b). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adolesc. Psychiatry 29, 749–758. doi: 10.1007/s00787-020-01541-4
Keywords: anxiety sensitivity, children and adolescents, child psychology, COVID-19 pandemic, lockdowns, quarantine, risk factors
Citation: Jin Q, Ma W, Zhang Y, Wang H, Hao J, Geng Y, Zhong B, Li J, Hou W and Lu S (2022) Risk Factors Associated With Increased Anxiety Sensitivity in Children and Adolescents in Northwest China During COVID-19 Pandemic Lockdown. Front. Psychol. 13:933207. doi: 10.3389/fpsyg.2022.933207
Received: 30 April 2022; Accepted: 10 June 2022;
Published: 08 July 2022.
Edited by:
Jianchun Fang, Zhejiang University, ChinaReviewed by:
Changshan Liu, Second Hospital of Tianjin Medical University, ChinaCopyright © 2022 Jin, Ma, Zhang, Wang, Hao, Geng, Zhong, Li, Hou and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei Hou, aG91d2VpMTAxMEB4anR1LmVkdS5jbg==; Shemin Lu, bHVzaGVtaW5AbWFpbC54anR1LmVkdS5jbg==
†These authors have contributed equally to this work
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.