- 1Graduate School, Hebei Medical University, Shijiazhuang, China
- 2Editorial Department of Nursing Practice and Research, Children’s Hospital of Hebei Province, Shijiazhuang, China
- 3Department of Scientific Research, Children’s Hospital of Hebei Province, Shijiazhuang, China
- 4Party and Government Integrated Office, Children’s Hospital of Hebei Province, Shijiazhuang, China
Background: The mental health of medical students is an issue worthy of attention, especially during COVID-19. Many studies have shown that depression and anxiety are the main problems faced by medical students. To assess the pooled prevalence of depression and anxiety among medical students worldwide, we conducted this meta-analysis.
Methods: According to PRISMA, we used a computerized strategy to search studies in EMBASE, PubMed, PsycArticles, Web of Science, and China Biology Medicine disc. The pooled prevalence of depression and anxiety was calculated by a random-effects model. Heterogeneity was explored by subgroup analysis. Sensitivity analysis and publication bias were also carried out in this meta-analysis.
Results: Of 1316 studies, 41 studies were selected based on 36608 medical students. The pooled depression prevalence was 37.9% (95% CI: 30.7–45.4%), and pooled anxiety prevalence was 33.7% (95% CI: 26.8–41.1%). The prevalence of depression and anxiety among medical students varied by gender, country, and continent.
Conclusion: The data reported that the prevalence of depression and anxiety among medical students during COVID-19 was relatively higher than those of the general population and the healthcare workers. The impact of COVID-19 on medical students and how to protect the mental health of medical students are needed to determine through further research.
Systematic Review Registration: [https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42021274015], identifier [CRD42021274015].
Introduction
College students were considered to be a sensitive and special group, and their mental health seemed to be more troubled, as their vulnerability is exacerbated by their inability to adapt to the new environment of universities, higher education plans, and the insufficient identification and utilization of social resources (Acharya et al., 2018). Many studies had investigated the mental health problems of college students and explored the related influencing factors. They suggested that college students’ mental health was affected by academic education, psychological elasticity, stress level, and other factors (Torres et al., 2017; Acharya et al., 2018; Alqudah et al., 2021; Alyoubi et al., 2021).
In December 2019, unexplained pneumonia suddenly broke out, which had swept the globe in a short time (Galea et al., 2020). With numerous infected people appearing every day, the government took lockdown measures to control and prevent the serious epidemic (Pierce et al., 2020; Tran et al., 2020; Basheti et al., 2021; Fancourt et al., 2021). Some studies had reported that mental health was related to COVID-19. A cross-sectional study conducted in China shows that Chinese people’s anxiety, depression, and drinking levels are more significant than before, and their mental health status decreases during the outbreak of COVID-19 (Ahmed et al., 2020). Some studies have shown that anxiety and depression are common mental health problems faced by college students during COVID-19, and they are at a high risk level (Naser et al., 2020); similarly, research results show that college students are vulnerable to psychological problems during the pandemic of COVID-19 and isolation and distance learning has a significant impact on students’ anxiety levels (Alqudah et al., 2021); In addition to COVID-19 patients and medical staff, college students are another group of people who are particularly prone to mental health disorders during the pandemic. Even if not during the outbreak of COVID-19, college students are experiencing considerable anxiety and depression due to academic pressure (Deng et al., 2021). Some related meta-analyses also confirmed this, the prevalence of depression and anxiety among college students increased during the COVID-19 (Deng et al., 2021; Guo et al., 2021).
Compared with other higher education, medical education was regarded as one of the training programs with the highest academic and emotional requirements out of any profession (Azad et al., 2017; Quek et al., 2019; Zeng et al., 2019). This demand and pressure caused a negative impact on the medical students’ mental health (Basudan et al., 2017; Shao et al., 2020). School closures, online teaching, and the inability to complete hospital internships had changed the inherent training model of medical students (Abbasi et al., 2020; Byrnes et al., 2020; Farooq et al., 2020; Soled et al., 2020; Bilgi et al., 2021). The study of medical students of bezmialem vakif University shows that many students are deeply affected by the epidemic process, no matter how long they have studied in medical school, one of the main reasons is the interruption of educational activities (Bilgi et al., 2021). The challenges of COVID-19 to global medical students’ mental health were unknown, especially the pooled prevalence of depression and anxiety, although some researchers were concerned about medical students’ mental health during this special period (Liu et al., 2020; Nakhostin-Ansari et al., 2020; Gupta et al., 2021). However, available studies had varied widely in terms of countries, assessments, and sample sizes, and in addition, there had been considerable variations in the reported prevalence of depression and anxiety. Therefore, for future researchers to quickly grasp the depression and anxiety of medical students during the epidemic, to facilitate their further research, this meta-analysis was conducted.
Methods
Data Sources and Search Strategy
This systematic review and meta-analysis had already been registered on PROSPERO before review initiation (CRD42021274015). We searched five databases (EMBASE, PubMed, PsycArticles, Web of Science, and China Biology Medicine disc) to identify the studies, and the final retrieval time of the literature was August 18, 2021. A search strategy consisting of three separate parts was applied to each database (“anxiety” OR “depression”) AND (“medical student*” OR “students, medical*”) AND (“COVID-19” OR “pneumonia” OR “Coronavirus” OR “SARS-COV-2”), and the publication time was limited to 2019-2021. The reference lists of relevant articles were searched for additional eligible papers (Supplementary Material 1).
Selection Criteria
Literature inclusion criteria: (1) The sample population consisting of students from medical colleges or medical-related majors; (2) Validated instrument was used to screen depression or anxiety and explicit cutoff value was given in the article; (3) Research conducted during COVID-19; (4) Published articles in English. Exclusion criteria were: (1) Qualitative studies, oral presentations, letter or non-original research; (2) Medical students with mental illness were not excluded; (3) Lack of useful information or the data needed.
Study Selection
After duplicate publications were excluded, irrelevant literature was further excluded through titles and abstracts. Then appraised the remaining articles according to inclusion and exclusion criteria of literature formulated in advance by reading the full texts. Reference lists of the selected articles were checked to identify further articles. The whole process was completed by two researchers independently, and disagreements were resolved through discussion, or a third arbitrator, if necessary.
Data Collection
Two researchers independently reviewed the full text of eligible studies and extracted the following data by using the predefined standardized form: The first author, year of publication, country, study period, study design, sample size, female ratio, assessment tools, and the event of depression or anxiety. For longitudinal studies, data collected during COVID-19 were included. Disagreements were resolved by consensus.
Quality Assessment
AHRQ (Agency for Healthcare Research and Quality criteria) was used to evaluate the methodological quality of the literature included in our meta-analysis, which is suitable for cross-sectional studies (Zhang et al., 2021b). There are 11 questions in total, those who meet the requirements will get 1 point. After scoring each item, according to the total score, each study quality was assessed as follows: low-quality = 0–3; moderate-quality = 4–7; high-quality = 8–11.
Analysis
We utilized software R (“meta” package) to perform meta-analytic calculations. To ensure that the prevalence proportions conform to the normal distribution, we converted the data through PRAW (untransformed), PLN (log transformation), PLOGIT (logit transformation), PAS (arcsine transformation), and PFT (Freeman–Tukey double arcsine transformation) (Barendregt et al., 2013; Luo et al., 2021). Based on the high expected heterogeneity between studies, the random-effects model was used in our meta-analyses. We calculated the pooled prevalence of depression and anxiety, and its corresponding 95% confidence interval (CI). According to the recommendations of the Cochrane Handbook, heterogeneity was estimated by Cochran’s Q test (p < 0.10) and the I2 statistic: the cutoff value of 75% indicates high heterogeneity. The source of heterogeneity was explored through subgroup analysis, we conducted additional subgroup analysis by countries, assessment tools, gender, and continents. The stability and reliability of pooled prevalence were evaluated by sensitivity analysis (Liu et al., 2021). Egger test of bias was used to assess the publication bias (Egger et al., 1997).
Results
Literature Screening
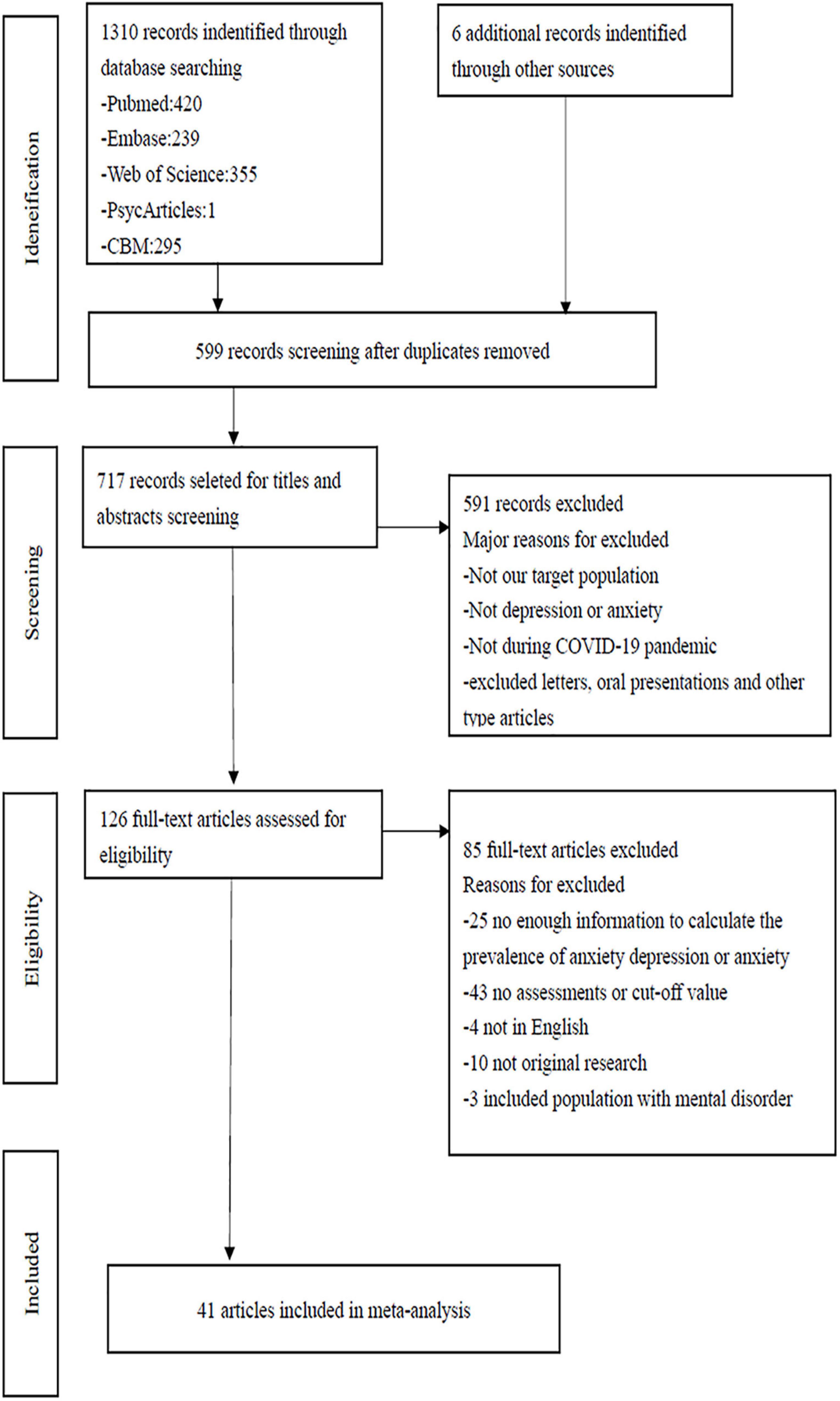
A total of 1310 articles were identified from the electronic database; 6 additional papers were found through a references list check. First, 465 duplicate literatures were excluded, two researchers independently evaluated the remaining 717 articles through title and abstract, irrelevant literature was further excluded. And then appraised the remaining articles according to inclusion and exclusion criteria of literature formulated in advance, 591 articles that did not meet the inclusion criteria were further excluded. The remaining 126 articles were evaluated through reading the full text to determine whether they were included in the meta-analysis. Reference lists of the selected articles were checked to identify further articles. The whole process was completed by two researchers independently, and disagreements were resolved through discussion, or a third arbitrator, if necessary. Ultimately, 41 studies were included in meta-analysis (Figure 1).
Study Characteristics
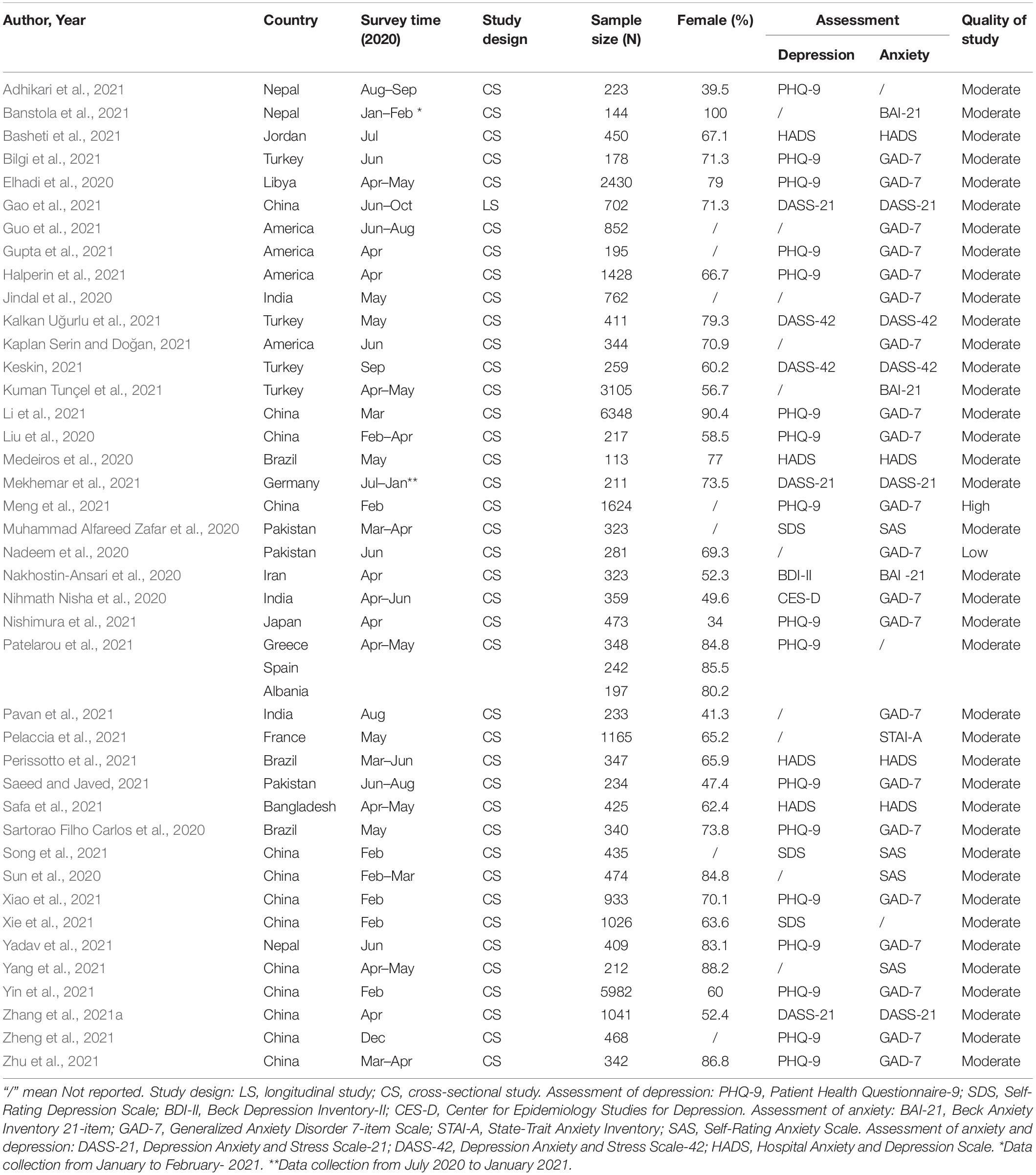
Table 1 shows the overall characteristics of the 41 included studies (Elhadi et al., 2020; Jindal et al., 2020; Liu et al., 2020; Medeiros et al., 2020; Muhammad Alfareed Zafar et al., 2020; Nadeem et al., 2020; Nakhostin-Ansari et al., 2020; Nihmath Nisha et al., 2020; Sartorao Filho Carlos et al., 2020; Sun et al., 2020; Adhikari et al., 2021; Banstola et al., 2021; Basheti et al., 2021; Bilgi et al., 2021; Gao et al., 2021; Guo et al., 2021; Gupta et al., 2021; Halperin et al., 2021; Kalkan Uğurlu et al., 2021; Kaplan Serin and Doğan, 2021; Keskin, 2021; Kuman Tunçel et al., 2021; Li et al., 2021; Mekhemar et al., 2021; Meng et al., 2021; Nishimura et al., 2021; Patelarou et al., 2021; Pavan et al., 2021; Pelaccia et al., 2021; Perissotto et al., 2021; Saeed and Javed, 2021; Safa et al., 2021; Song et al., 2021; Xiao et al., 2021; Xie et al., 2021; Yadav et al., 2021; Yang et al., 2021; Yin et al., 2021; Zhang et al., 2021a; Zheng et al., 2021; Zhu et al., 2021). On the whole, 40 cross-sectional studies and 1 longitudinal study were included in our study. We included the two surveys of the longitudinal study, as they were conducted during the pandemic (Gao et al., 2021). Included studies came from 15 countries, including China, Turkey, the United States, Nepal, Brazil, India, and other countries. The included studies were conducted from January 2020 to February 2021. The minimum sample size of the included study is more than 100 and the maximum sample size is 6348. One of the studies was a transnational study, and the sample population came from Albania (n = 197), Greece (n = 348), and Spain (n = 242) (Patelarou et al., 2021). Of the 41 included studies, 38 studies reported anxiety prevalence and 31 studies reported depression prevalence. In total, 36608 participants were included. One study included 195 participants, 6 of whom only participated in the depression survey and did not complete the anxiety-related survey (Gupta et al., 2021).
Quality of Study
According to the methodological quality evaluation of the literature by two researchers, forty studies were of moderate quality, one of high quality (Meng et al., 2021), and one of low quality (Nadeem et al., 2020). Our meta-analysis will not include low quality studies (Supplementary Material 2).
Prevalence of Depression and Anxiety
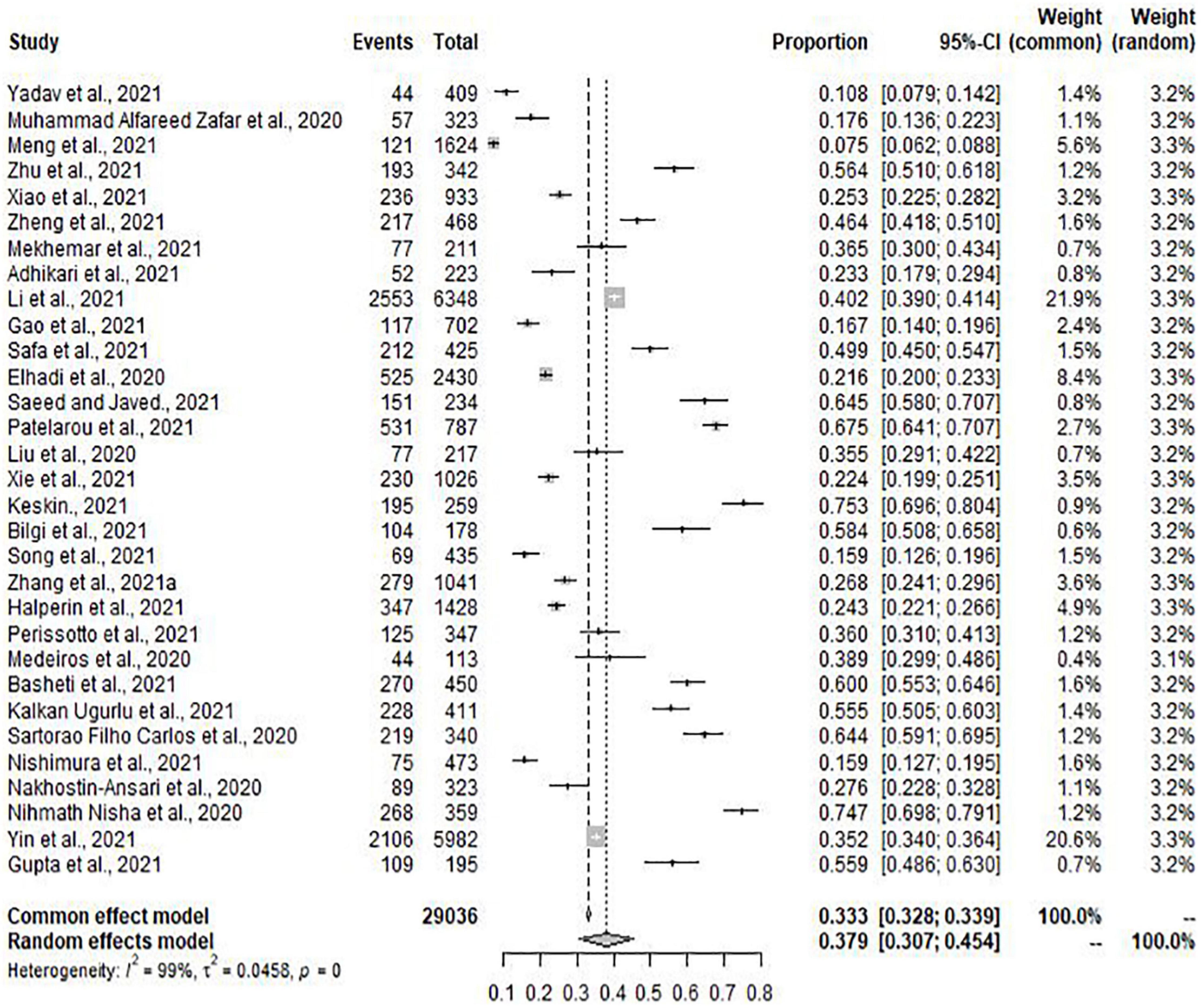
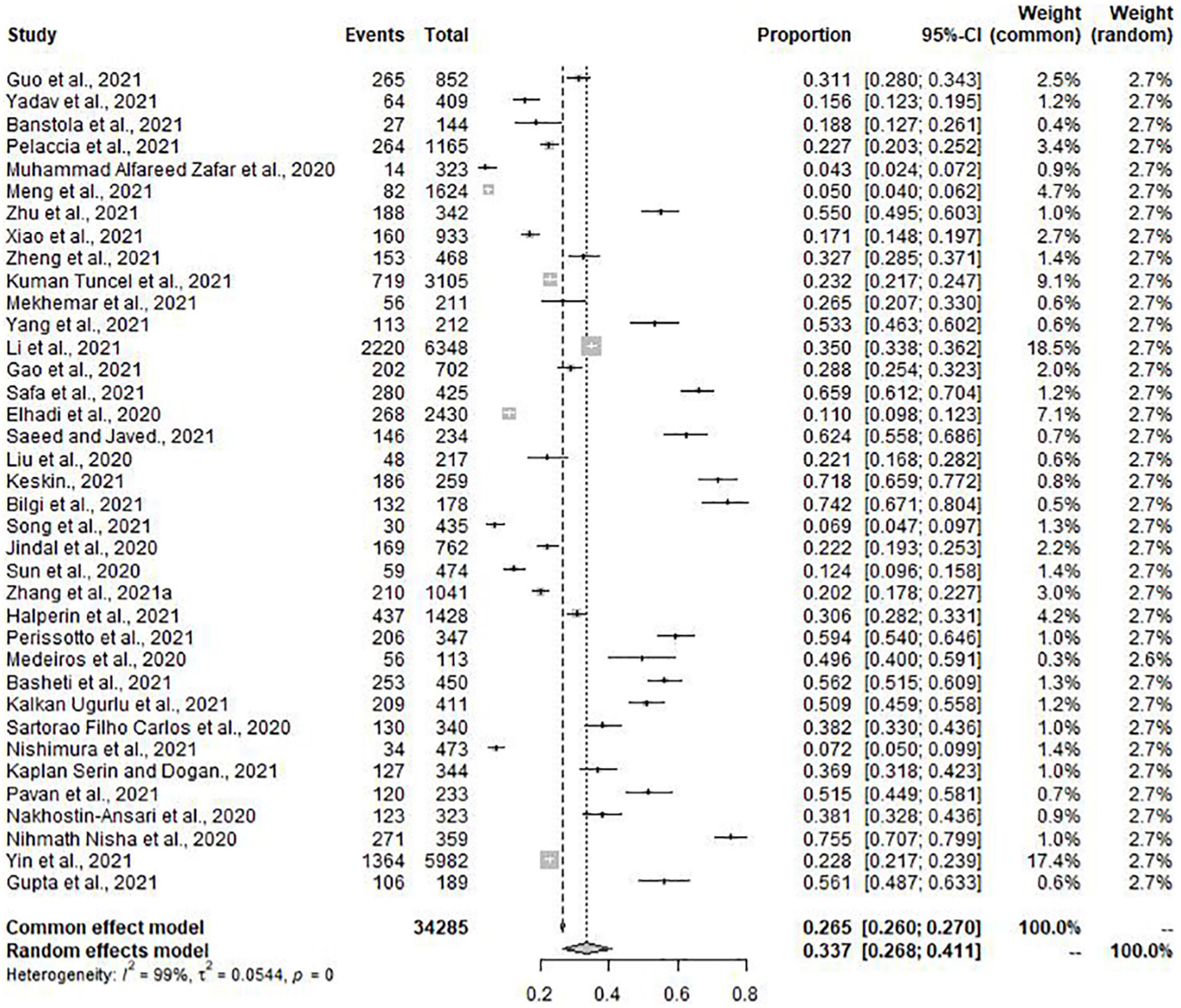
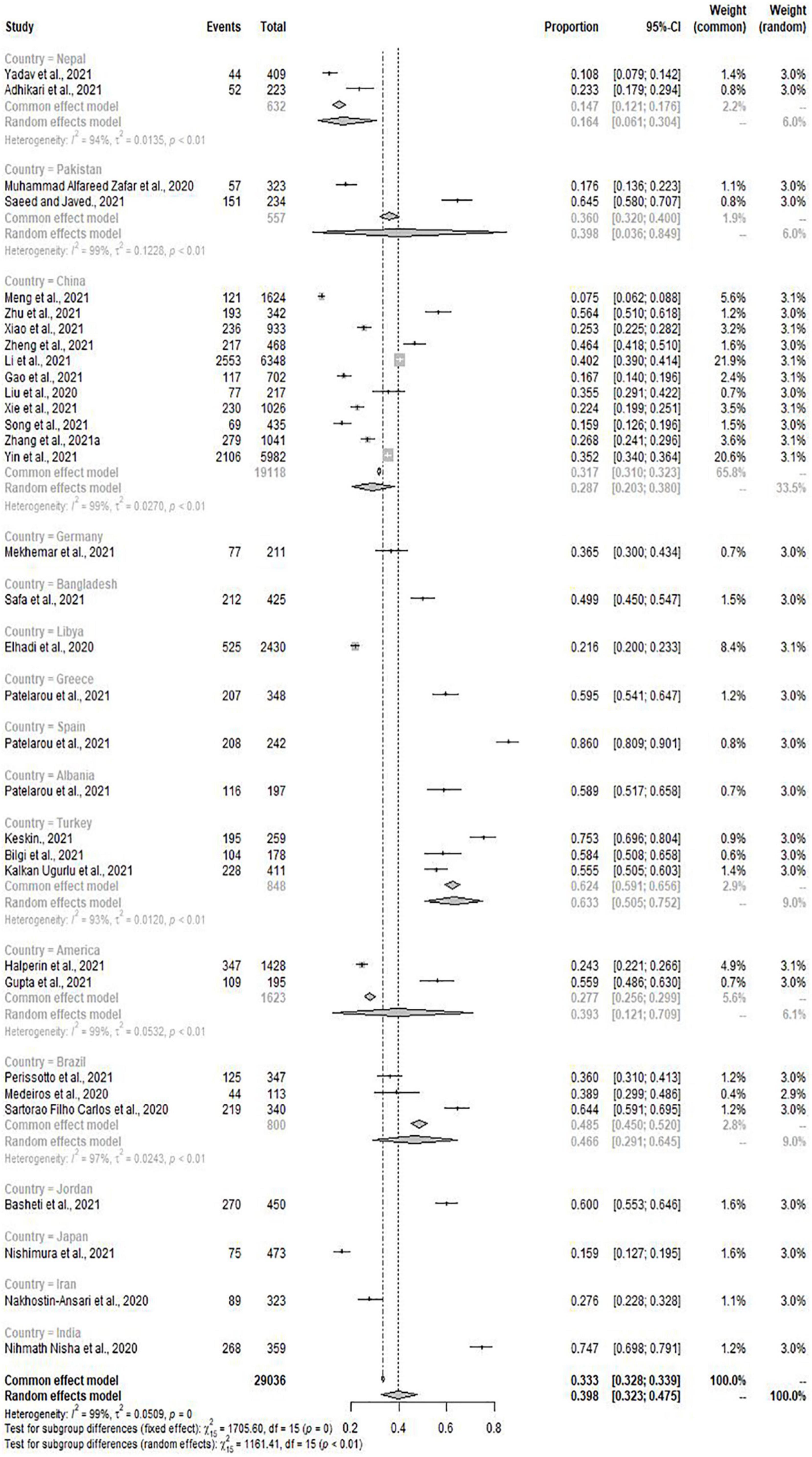
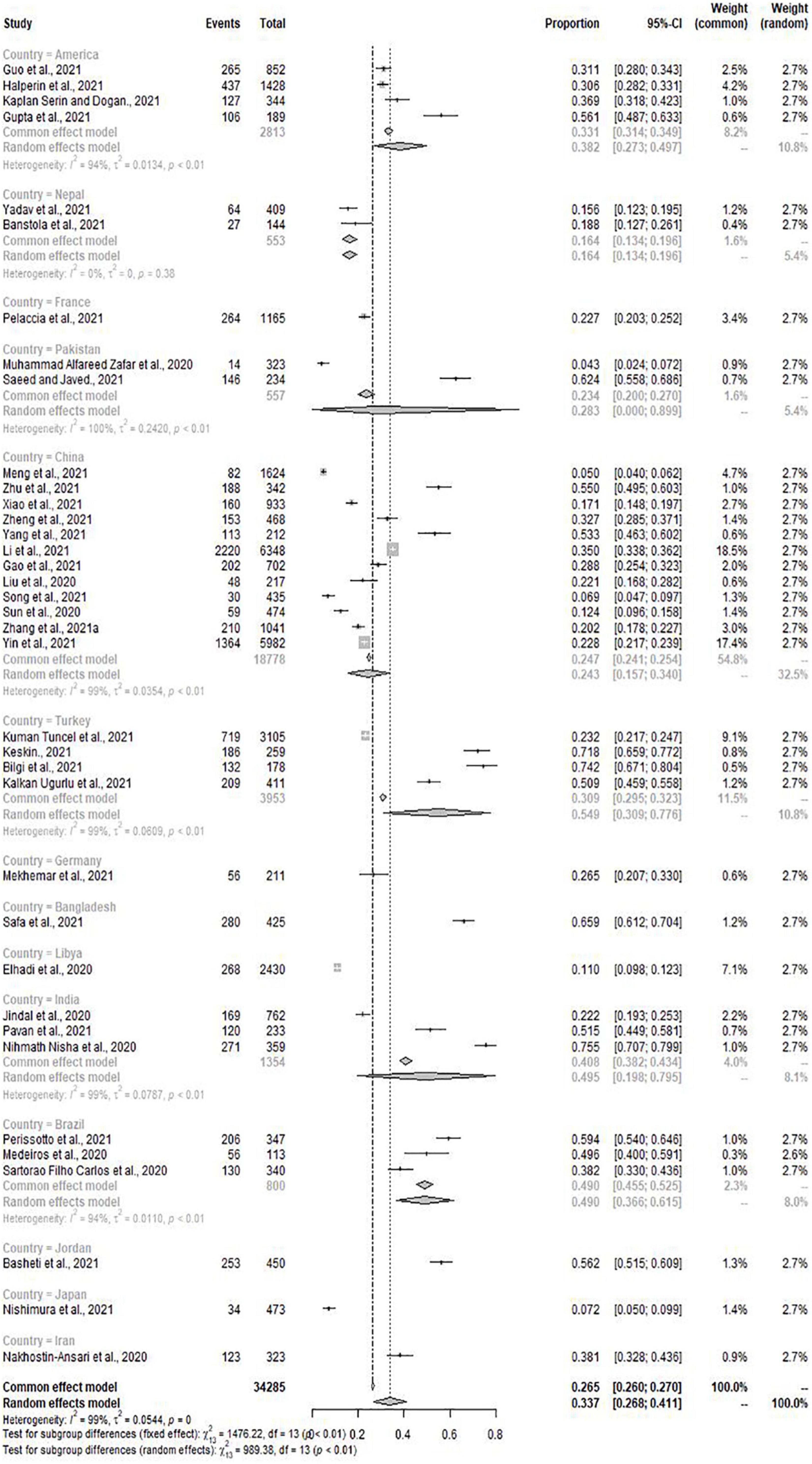
Meta-analysis included 31 of the total studies with depression (n = 29036), the pooled prevalence of depression was 37.9% (95% CI: 30.7–45.4%) with high heterogeneity (I2 = 99%, p = 0.00) (Figure 2). Of the 41 studies, 37 studies (n = 34285) with the condition of anxiety were conducted to meta-analysis. The pooled prevalence of anxiety was 33.7% (95% CI: 26.8–41.1%) with high heterogeneity (I2 = 99%, p = 0.00) (Figure 3).
Subgroup Analysis
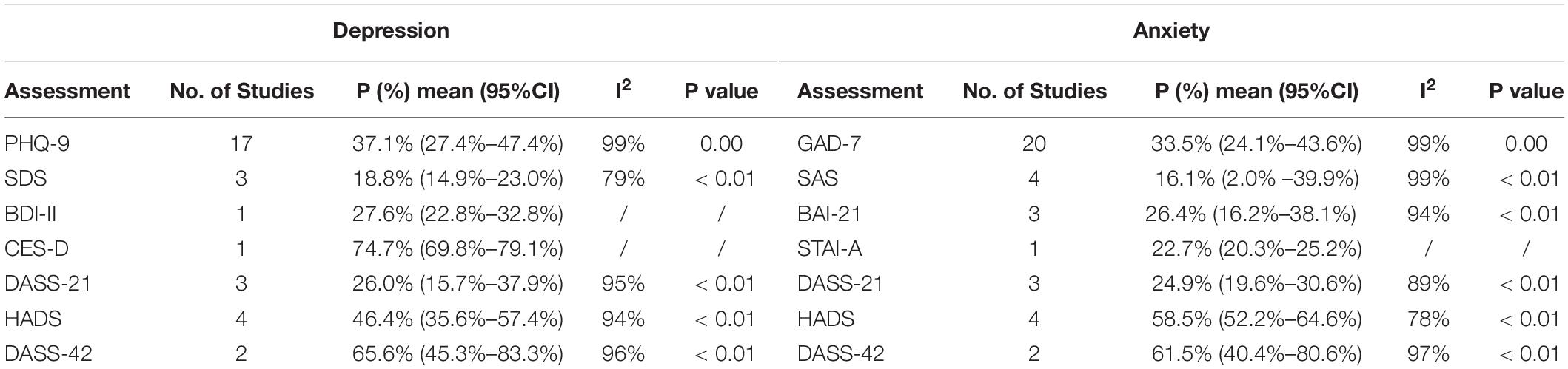
According to subgroup analysis of assessment instruments, the lowest pooled prevalence of anxiety was 16.1% (95% CI: 2.0–39.9%) used SAS with high heterogeneity (I2 = 99%, p < 0.01). The pooled prevalence of depression used SDS was 18.8% (95% CI: 14.9–23.0%) with high heterogeneity (I2 = 79%, p < 0.01) (Table 2).
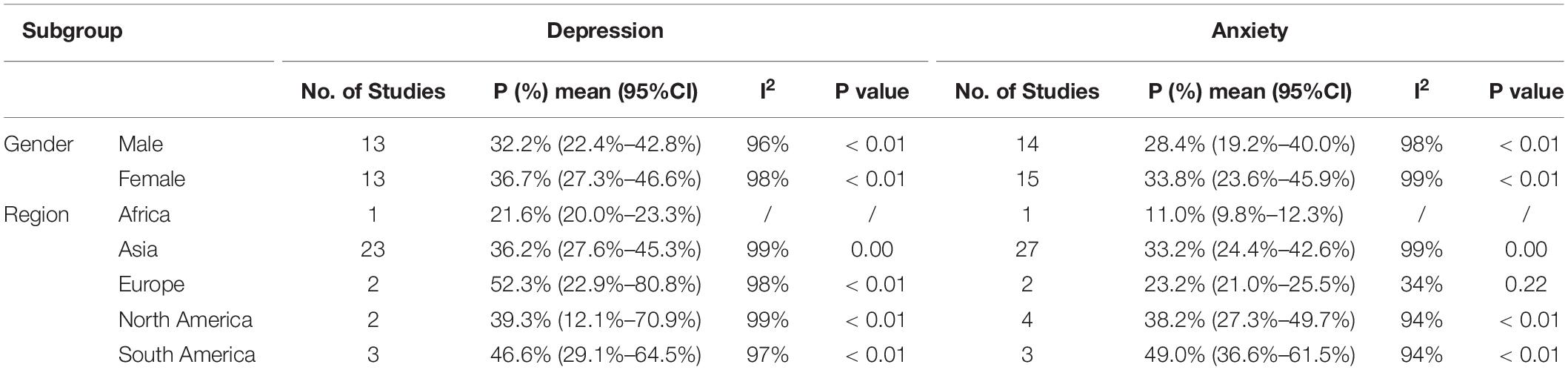
When classified according to countries, the prevalence of depression and anxiety in Japan was significantly lower than in other countries (15.9%, 95% CI: 12.7–19.5%; 7.2%, 95% CI: 5.0–9.9%). Interestingly, the prevalence of depression in Spanish medical students was the highest (86.0%, 95% CI: 80.9–90.1%), and Bangladesh had the highest prevalence of anxiety among many countries (65.9%, 95% CI: 61.2–70.4%) (Figures 4, 5). Then, we conducted subgroup analysis according to the geographical location of the countries, and found that the prevalence of depression was the highest (52.3%, 95% CI: 22.9–80.8%) but the prevalence of anxiety was relatively low (23.2%, 95% CI: 21.0–25.5%) in Europe. At the same time, we found that the pooled prevalence of anxiety in female was higher than that in male (33.8%, 95% CI: 23.6–45.9%; 28.4%, 95% CI:19.2–40.0%), the pooled prevalence of depression also showed this characteristic (36.7%, 95% CI: 27.3–46.6%; 32.2%, 95% CI:22.4–42.8%) (Table 3).
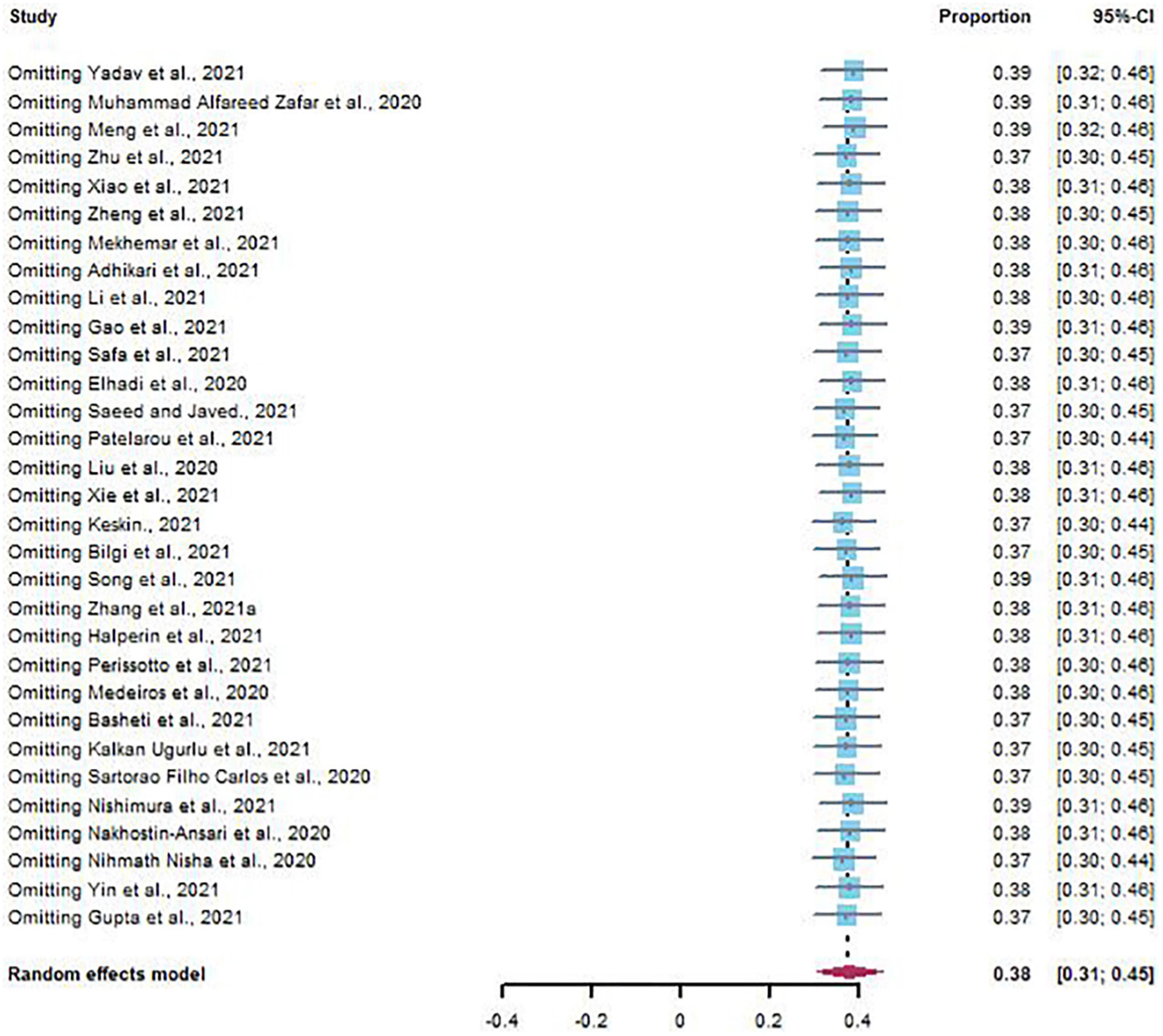
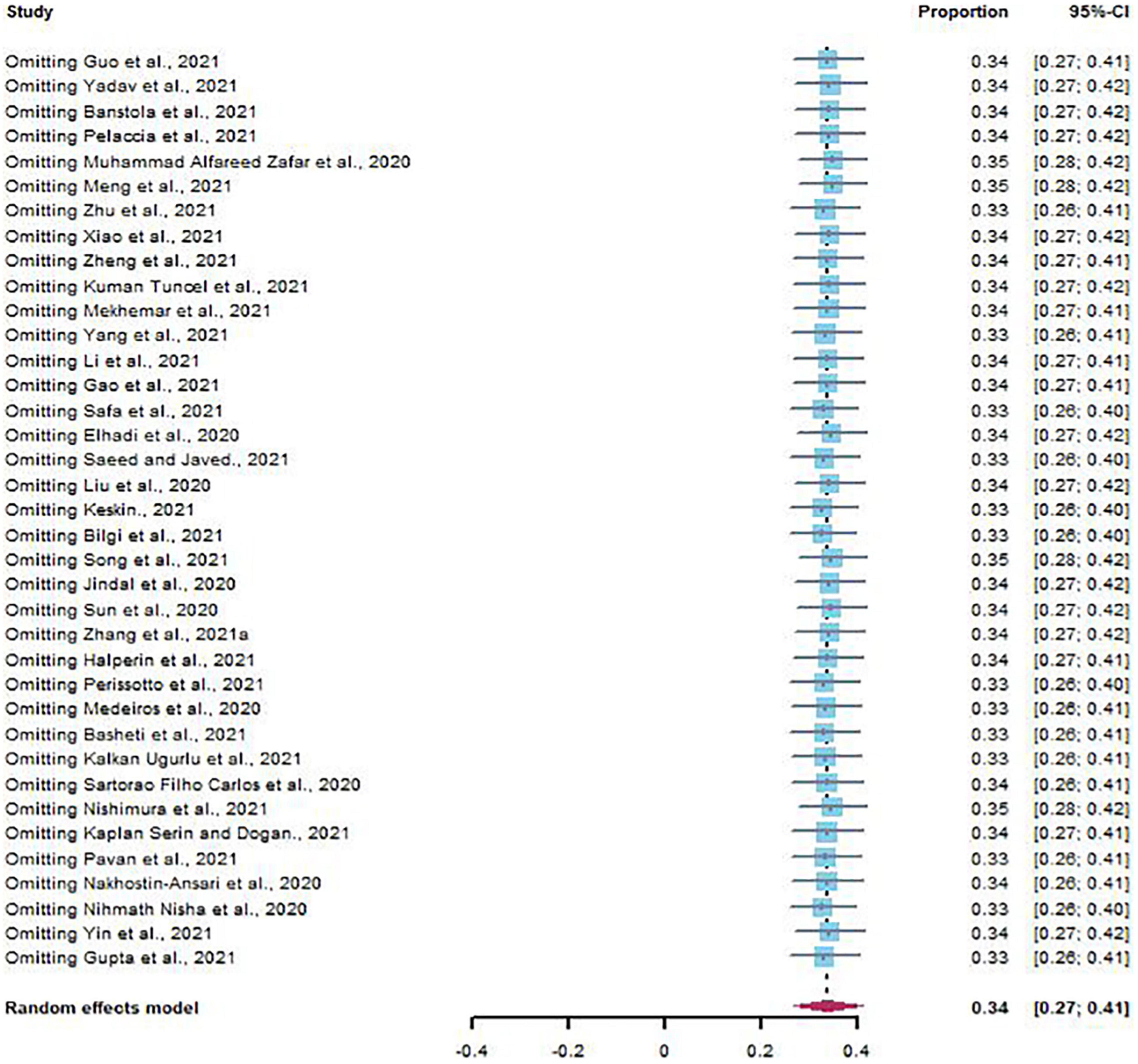
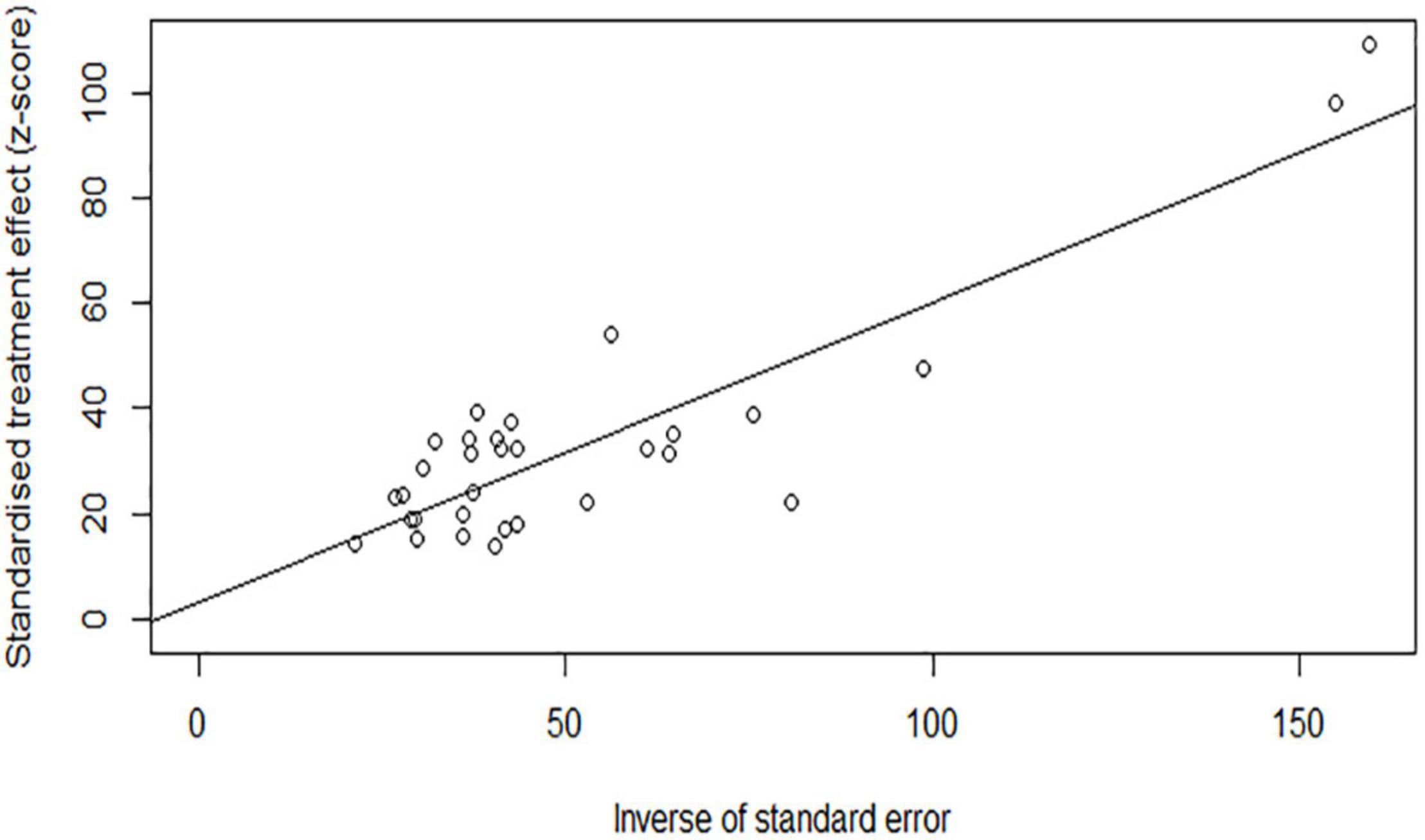
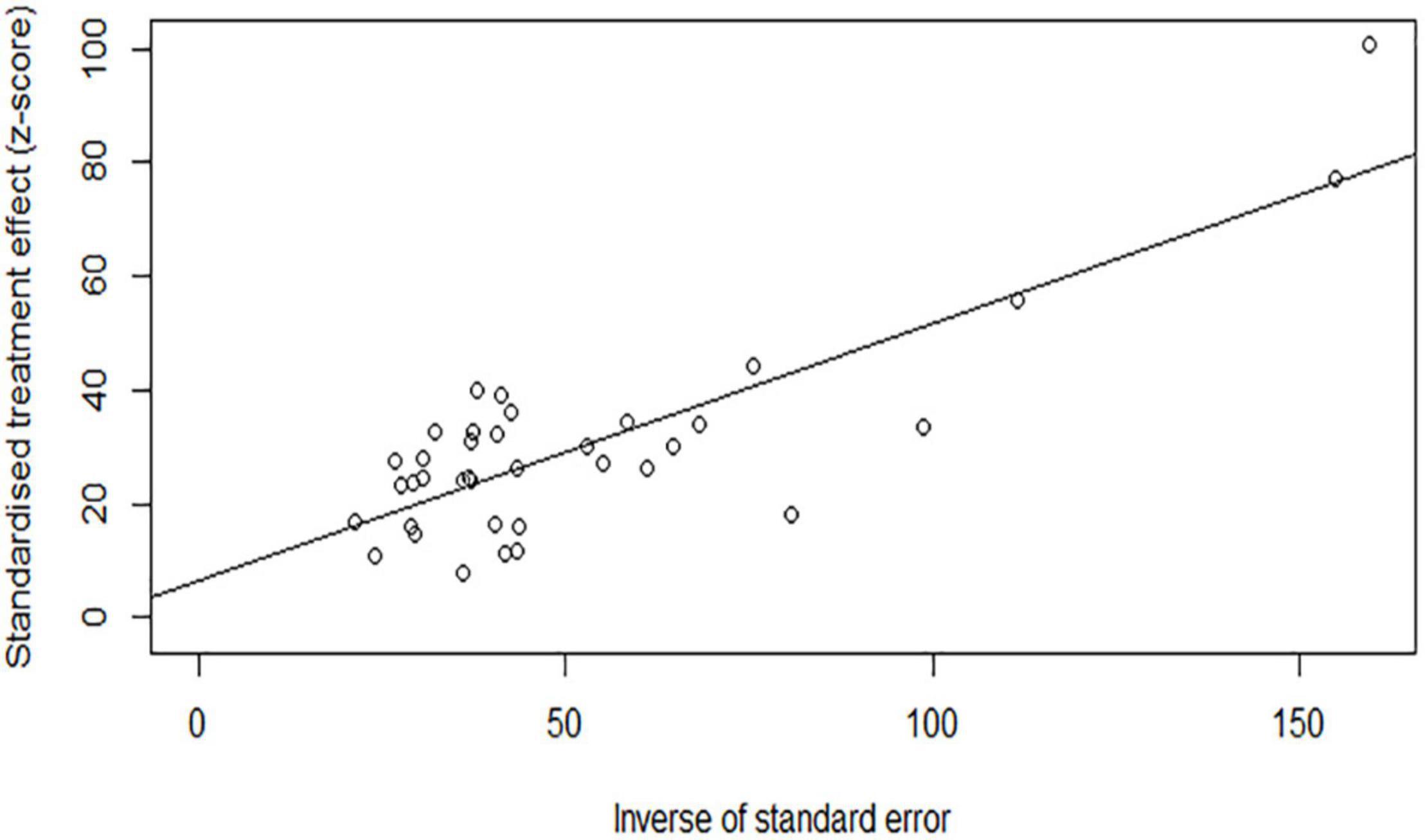
Sensitivity Analysis and Publication Bias
The results of sensitivity analysis showed that there was no significant change in the prevalence of depression and anxiety (Figures 6, 7). Similarly, Egger’s regression test showed that there was no publication bias on depression and anxiety (p = 0.3742, p = 0.0528) (Figures 8, 9).
Discussion
We conducted this systematic review and meta-analysis to determine the prevalence of depression and anxiety in medical students over the world during the COVID-19 pandemic. In our study, we find that the pooled prevalence of depression and anxiety among medical students was 37.9%, 95% CI: 30.7–45.4%; 33.7%, 95% CI: 26.8–41.1%, more prominent relative to the general population and healthcare workers (Pappa et al., 2020; Castaldelli-Maia et al., 2021; Cénat et al., 2021; Raoofi et al., 2021; Sahebi et al., 2021; Santabárbara et al., 2021). This seemed to be consistent with the prevalence of anxiety reported by Quek et al. (2019) (33.8%, 95% CI: 29.2–38.7%). However, we found that the research they included had a heavy period, from 1998 to 2019, while the research we included was more concentrated. We inferred that an excessive period might have an impact on the pooled prevalence of anxiety. Another study reported that the prevalence of anxiety among medical students during the epidemic was 28%, which was lower than our conclusion (Lasheras et al., 2020). We found that their latest literature search time was August 26, 2020, although the epidemic situation had been partially controlled at that time, its influence still existed. Even in China, medical students deferred enrollment until October 1, 2020. Repeated signs of the epidemic situation and the fear of returning to school, the impact of these factors on the mental health among medical students needed to be considered. In addition, we also found that the prevalence of depression among medical students was relatively high during the COVID-19 compared with before (Puthran et al., 2016; Rotenstein et al., 2016).
Interestingly, when we performed a subgroup analysis based on the sample source countries, we found that the pooled prevalence of depression and anxiety among Chinese medical students was not prominent (28.7%, 95% CI: 20.3–38.0%; 24.3%, 95% CI: 15.7–34.0%). We further divided countries according to continents and conducted subgroup analysis. It was noted that the prevalence of depression was the highest in Europe (52.3%, 95% CI: 22.9–80.8%) and relatively low in Asia (36.2%, 95% CI: 27.6–45.3%). In terms of anxiety prevalence, Europe is at a low level (23.2%, 95% CI: 21.0–25.5%), and South America has the highest anxiety prevalence (49.0%, 95% CI: 36.6–61.5%). Research showed that rumors about the epidemic affected the mental health of citizens (Ahmed et al., 2020; Xiong et al., 2020), and the mental health of the population was also related to the nationwide epidemic control (Jiang, 2020). Limited outdoor activities, increased new cases and fear of the possibility to be infected were identified to impact mental health (Jiang, 2020; Wang et al., 2020c; Kaplan Serin and Doğan, 2021). In particular, the closure of schools and online teaching had brought unprecedented challenges to the education of medical students (Bilgi et al., 2021), and the effects of social distance and self-isolation might make students feel more vulnerable and lonelier, increasing depression and anxiety symptoms (Huang et al., 2020). Similarly, in some countries, medical students were limited to a clinical internship during the epidemic. Sudden changes impacted the traditional training mode of medical students (Abbasi et al., 2020; Keskin and Özkan, 2021). The impact of COVID-19 on psychological and mental health can be reduced by timely updating the relevant accurate information such as the number of new epidemic cases and the route of transmission (Wang et al., 2020a). Benefit from the rapid and effective measures taken by the Chinese government, the epidemic was quickly and effectively controlled and the public panic was reduced (Lau et al., 2020; Pan et al., 2020; Li et al., 2021).
Finally, we found that the prevalence of depression and anxiety in female medical students was higher than that in males, and some previous studies have reported a similar situation (Puthran et al., 2016; Quek et al., 2019; Alyoubi et al., 2021; Luo et al., 2021). Females seemed to be more vulnerable to mental health problems than males (Baxter et al., 2013; Qiu et al., 2020; Xiong et al., 2020; Kalkan Uğurlu et al., 2021), we speculated that it was related to females unique physiological and psychological factors: females are more likely to articulate their worries and emotions (Basudan et al., 2017; Lin et al., 2021). When we performed subgroup analysis according to the assessment tools, we found that different depression and anxiety assessment tools also brought different prevalence rates of depression and anxiety. Due to the diversity of sample sources and the high heterogeneity of subgroup analysis, we could not infer the impact of different assessment tools on the prevalence of depression and anxiety among medical students.
COVID-19 has a huge impact on mental health. An American study showed that the prevalence of depressive symptoms was more than 3 times higher during COVID-19 compared with before (Ettman et al., 2020). Economic turmoil, home quarantine and the uncertainty of COVID-19 cases had brought great stress to the people, accompanied by an increase in the level of anxiety and depression during the COVID-19 pandemic (Shehata et al., 2021). Studies have shown that strict government policies slow down the spread of COVID-19, but such interventions disrupt daily life and lead to adverse mental health outcomes, especially strict blockade measures and home confinement with unknown duration. Epidemiological monitoring and targeted intervention should be implemented in time to prevent further mental health problems (Rossi et al., 2020; Wang et al., 2020b; Ding et al., 2021). Personal exposure to COVID-19 is an important risk factor for increased anxiety and depressive symptoms during pandemic (Ding et al., 2021). The prevalence of anxiety was more significant in people who had infected with COVID-19 or knew someone who had experienced illness (Shabahang et al., 2021). In addition, less exercise and lack of social support can also lead to more anxiety and depression symptoms (Kong et al., 2020; Shah et al., 2021).
Although study had shown that the harm caused by COVID-19 pandemic to the overall mental health of the population will improve over time (Gallagher et al., 2021), epidemics and other health emergencies may lead to harmful and long-term psychosocial consequences, which cannot be ignored (Dong and Bouey, 2020). Even if the epidemic ends, its negative socio-economic consequences, such as work difficulties, may also have an adverse impact on the mental health of the population (Rossi et al., 2020). Without intervention and appropriate health and social policies, mental health problems will have serious adverse consequences. The government plays an important role in reducing the prevalence of anxiety and depression during COVID-19. The government’s decisive and rapid epidemic prevention measures can help to reduce the further spread of the COVID-19 and protect the mental health of the public (Wang et al., 2020b; Zhang et al., 2021c). In addition, family companionship can reduce anxiety and depression levels (Shah et al., 2021).
Conclusion
In conclusion, this systematic review and meta-analysis reported a relatively high prevalence of depression and anxiety. The prevalence of depression and anxiety was 37.9%, 33.7%, higher than that of the general population and healthcare workers. The prevalence varied in different countries. Researchers can further explore the differences and influencing factors of mental health among medical students with different cultural backgrounds.
Limitations and Strengths
In conclusion, this systematic review and meta-analysis reported a relatively high prevalence of depression and anxiety. For its high heterogeneity, we tried to use extensive subgroup analysis to reveal the source of heterogeneity. According to the results of subgroup analysis, we found that the combined prevalence was not reversed, indicating that our results remained relatively stable. Secondly, only studies published in English were eligible to be included in the meta-analysis, which limits the estimation of prevalence to a certain extent. In addition, most studies were descriptive, the association between COVID-19 and medical students’ depression and anxiety may not imply a causal relation. Moreover, the prevalence of the included studies was estimated by self-report, and the differences in individual emotional expressions are also factors that need further consideration. Then, due to the small number of studies in some countries, although we combine countries into continents for subgroup analysis, the number of studies in Africa is still small, and future researchers should pay attention to this problem. However, we have to say that our meta-analysis includes a sizeable sample size (n = 36608). Despite some limitations, the findings still have some key significance. Importantly, they support other researchers to grasp the prevalence of depression and anxiety in medical students during COVID-19, to make corresponding psychological intervention measures.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author Contributions
QJ conducted the data analyses and wrote the manuscript. HH and HY conducted the literature search. YQ and HS conducted the study quality assessment. DY conducted the supervision, review, and editing. All authors approved the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.846789/full#supplementary-material
References
Abbasi, M. S., Ahmed, N., Sajjad, B., Alshahrani, A., Saeed, S., Sarfaraz, S., et al. (2020). E-Learning perception and satisfaction among health sciences students amid the COVID-19 pandemic. Work 67, 549–556. doi: 10.3233/wor-203308
Acharya, L., Jin, L., and Collins, W. (2018). College life is stressful today - emerging stressors and depressive symptoms in college students. J. Am. Coll. Health 66, 655–664. doi: 10.1080/07448481.2018.1451869
Adhikari, A., Sujakhu, E., G, C. S., and Zoowa, S. (2021). Depression among medical students of a medical college in Nepal during COVID-19 Pandemic: a descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 59, 645–648. doi: 10.31729/jnma.5441
Ahmed, M. Z., Ahmed, O., Aibao, Z., Hanbin, S., Siyu, L., and Ahmad, A. (2020). Epidemic of COVID-19 in China and associated psychological problems. Asian J. Psychiatr. 51:102092. doi: 10.1016/j.ajp.2020.102092
Alqudah, A., Al-Smadi, A., Oqal, M., Qnais, E. Y., Wedyan, M., Abu Gneam, M., et al. (2021). About anxiety levels and anti-anxiety drugs among quarantined undergraduate Jordanian students during COVID-19 pandemic. Int. J. Clin. Pract. 75:e14249. doi: 10.1111/ijcp.14249
Alyoubi, A., Halstead, E. J., Zambelli, Z., and Dimitriou, D. (2021). The impact of the COVID-19 Pandemic on students’ mental health and sleep in Saudi Arabia. Int. J. Environ. Res. Public Health 18:9344. doi: 10.3390/ijerph18179344
Azad, N., Shahid, A., Abbas, N., Shaheen, A., and Munir, N. (2017). Anxiety And depression in medical students of a private medical college. J. Ayub. Med. Coll. Abbottabad 29, 123–127.
Banstola, B., Shakya, N., and Sharma, P. (2021). Anxiety among nursing students towards clinical placement during covid-19 in a tertiary hospital of nepal: a descriptive cross-sectional study. JNMA J. Nepal Med. Assoc. 59, 542–546. doi: 10.31729/jnma.6132
Barendregt, J. J., Doi, S. A., Lee, Y. Y., Norman, R. E., and Vos, T. (2013). Meta-analysis of prevalence. J. Epidemiol. Community Health 67, 974–978. doi: 10.1136/jech-2013-203104
Basheti, I. A., Mhaidat, Q. N., and Mhaidat, H. N. (2021). Prevalence of anxiety and depression during COVID-19 pandemic among healthcare students in Jordan and its effect on their learning process: a national survey. PLoS One 16:e0249716. doi: 10.1371/journal.pone.0249716
Basudan, S., Binanzan, N., and Alhassan, A. (2017). Depression, anxiety and stress in dental students. Int. J. Med. Educ. 8, 179–186. doi: 10.5116/ijme.5910.b961
Baxter, A. J., Scott, K. M., Vos, T., and Whiteford, H. A. (2013). Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol. Med. 43, 897–910. doi: 10.1017/s003329171200147x
Bilgi, K., Aytas, G., Karatoprak, U., Kazancioglu, R., and Ozcelik, S. (2021). The effects of coronavirus disease 2019 outbreak on medical students. Front. Psychiatry 12:637946. doi: 10.3389/fpsyt.2021.637946
Byrnes, Y. M., Civantos, A. M., Go, B. C., McWilliams, T. L., and Rajasekaran, K. (2020). Effect of the COVID-19 pandemic on medical student career perceptions: a national survey study. Med. Educ. Online 25:1798088. doi: 10.1080/10872981.2020.1798088
Castaldelli-Maia, J. M., Marziali, M. E., Lu, Z., and Martins, S. S. (2021). Investigating the effect of national government physical distancing measures on depression and anxiety during the COVID-19 pandemic through meta-analysis and meta-regression. Psychol. Med. 51, 881–893. doi: 10.1017/S0033291721000933
Cénat, J. M., Blais-Rochette, C., Kokou-Kpolou, C. K., Noorishad, P.-G., Mukunzi, J. N., McIntee, S.-E., et al. (2021). Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 295:113599. doi: 10.1016/j.psychres.2020.113599
Deng, J., Zhou, F., Hou, W., Silver, Z., Wong, C. Y., Chang, O., et al. (2021). The prevalence of depressive symptoms, anxiety symptoms and sleep disturbance in higher education students during the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res. 301:113863. doi: 10.1016/j.psychres.2021.113863
Ding, K. L., Yang, J. Z., Chin, M. K., Sullivan, L., Demirhan, G., Violant-Holz, V., et al. (2021). Mental health among adults during the COVID-19 pandemic lockdown: a cross-sectional multi-country comparison. Int. J. Environ. Res. Public Health 18:2686. doi: 10.3390/ijerph18052686
Dong, L., and Bouey, J. (2020). Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 26, 1616–1618. doi: 10.3201/eid2607.200407
Egger, M., Davey Smith, G., Schneider, M., and Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. Bmj 315, 629–634. doi: 10.1136/bmj.315.7109.629
Elhadi, M., Buzreg, A., Bouhuwaish, A., Khaled, A., Alhadi, A., Msherghi, A., et al. (2020). Psychological impact of the civil war and COVID-19 on Libyan medical students: a cross-sectional study. Front. Psychol. 11:570435. doi: 10.3389/fpsyg.2020.570435
Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., and Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Netw. Open 3:e2019686. doi: 10.1001/jamanetworkopen.2020.19686
Fancourt, D., Steptoe, A., and Bu, F. (2021). Trajectories of anxiety and depressive symptoms during enforced isolation due to COVID-19 in England: a longitudinal observational study. Lancet Psychiatry 8, 141–149. doi: 10.1016/s2215-0366(20)30482-x
Farooq, F., Rathore, F. A., and Mansoor, S. N. (2020). Challenges of online medical education in Pakistan during COVID-19 Pandemic. J. Coll. Physicians Surg. Pak. 30, 67–69. doi: 10.29271/jcpsp.2020.Supp1.S67
Galea, S., Merchant, R. M., and Lurie, N. (2020). The mental health consequences of COVID-19 and physical distancing: the need for prevention and early intervention. JAMA Intern. Med. 180, 817–818. doi: 10.1001/jamainternmed.2020.1562
Gallagher, M. W., Smith, L. J., Richardson, A. L., and Long, L. J. (2021). Six month trajectories of COVID-19 experiences and associated stress, anxiety, depression, and impairment in American adults. Cognit. Ther. Res. 1–13. doi: 10.1007/s10608-021-10277-7 [Epub ahead of print].
Gao, F., Jiao, S. X., Bi, Y. Q., Huang, Z. Y., Wang, P., Zhang, B. Y., et al. (2021). The Impact of the SARS-COV-2 pandemic on the mental health and employment decisions of medical students in North China. Front. Psychiatry 12:641138. doi: 10.3389/fpsyt.2021.641138
Guo, A. A., Crum, M. A., and Fowler, L. A. (2021). Assessing the psychological impacts of COVID-19 in undergraduate medical students. Int. J. Environ. Res. Public Health 18:2952. doi: 10.3390/ijerph18062952
Gupta, P., Anupama, B. K., and Ramakrishna, K. (2021). Prevalence of depression and anxiety among medical students and house staff during the COVID-19 health-care crisis. Acad. Psychiatry 45, 575–580. doi: 10.1007/s40596-021-01454-7
Halperin, S. J., Henderson, M. N., Prenner, S., and Grauer, J. N. (2021). Prevalence of anxiety and depression among medical students during the Covid-19 Pandemic: a cross-sectional study. J. Med. Educ. Curric. Dev. 8:2382120521991150. doi: 10.1177/2382120521991150
Huang, C., Wang, Y., Li, X., Ren, L., Zhao, J., Hu, Y., et al. (2020). Clinical features of patients infected with 2019 novel coronavirus in Wuhan. China Lancet 395, 497–506. doi: 10.1016/S0140-6736(20)30183-5
Jiang, R. (2020). Knowledge, attitudes and mental health of university students during the COVID-19 pandemic in China. Child Youth Serv. Rev. 119:105494. doi: 10.1016/j.childyouth.2020.105494
Jindal, V., Mittal, S., Kaur, T., Bansal, A. S., Kaur, P., Kaur, G., et al. (2020). Knowledge, anxiety and the use of hydroxychloroquine prophylaxis among health care students and professionals regarding COVID-19 pandemic. Adv. Respir. Med. 88, 520–530. doi: 10.5603/ARM.a2020.0163
Kalkan Uğurlu, Y., Mataracı Değirmenci, D., Durgun, H., and Gök Uğur, H. (2021). The examination of the relationship between nursing students’ depression, anxiety and stress levels and restrictive, emotional, and external eating behaviors in COVID-19 social isolation process. Perspect. Psychiatr. Care 57, 507–516. doi: 10.1111/ppc.12703
Kaplan Serin, E., and Doğan, R. (2021). The relationship between anxiety and hopelessness levels among nursing students during the COVID-19 pandemic and related factors. Omega. doi: 10.1177/00302228211029144 [Epub ahead of print].
Keskin, G. (2021). Self-report measurement of depression, anxiety, and stress caused by covid-19 pandemic in senior undergraduate dental students. Pesqui. Bras. Odontopediatria Clin. Integr. 21:e0243. doi: 10.1590/PBOCI.2021.102
Keskin, S.Özkan, B. (2021). Mental statuses of nursing students in the covid-19 pandemic period: a systematic review. Ann. Clin. Anal. Med. 12, 245–249. doi: 10.4328/ACAM.20654
Kong, X. Y., Kong, F. Y., Zheng, K. L., Tang, M., Chen, Y., Zhou, J. H., et al. (2020). Effect of psychological-behavioral intervention on the depression and anxiety of COVID-19 patients. Front. Psychiatry 11:586355. doi: 10.3389/fpsyt.2020.586355
Kuman Tunçel, Ö, Taşbakan, S. E., Gökengin, D., Erdem, H. A., Yamazhan, T., Sipahi, O. R., et al. (2021). The deep impact of the COVID-19 pandemic on medical students: an online cross-sectional study evaluating Turkish students’ anxiety. Int. J. Clin. Pract. 75:e14139. doi: 10.1111/ijcp.14139
Lasheras, I., Gracia-García, P., Lipnicki, D. M., Bueno-Notivol, J., López-Antón, R., de la Cámara, C., et al. (2020). Prevalence of anxiety in medical students during the covid-19 pandemic: a rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 17, 1–12. doi: 10.3390/ijerph17186603
Lau, H., Khosrawipour, V., Kocbach, P., Mikolajczyk, A., Schubert, J., Bania, J., et al. (2020). The positive impact of lockdown in Wuhan on containing the COVID-19 outbreak in China. J. Travel Med. 27:taaa037. doi: 10.1093/jtm/taaa037
Li, D., Zou, L., Zhang, Z., Zhang, P., Zhang, J., Fu, W., et al. (2021). The psychological effect of COVID-19 on home-quarantined nursing students in China. Front. Psychiatry 12:652296. doi: 10.3389/fpsyt.2021.652296
Lin, T., Stone, S. J., Heckman, T. G., and Anderson, T. (2021). Zoom-in to zone-out: therapists report less therapeutic skill in telepsychology versus face-to-face therapy during the COVID-19 pandemic. Psychotherapy 58, 449–459. doi: 10.1037/pst0000398
Liu, J., Zhu, Q., Fan, W., Makamure, J., Zheng, C., and Wang, J. (2020). Online mental health survey in a medical college in China during the COVID-19 outbreak. Front. Psychiatry 11:459. doi: 10.3389/fpsyt.2020.00459
Liu, Z. H., Jin, Y., Rao, W. W., Zhang, Q., Zhang, J., Jackson, T., et al. (2021). The prevalence of painful physical symptoms in major depressive disorder: a systematic review and meta-analysis of observational studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 111:110372. doi: 10.1016/j.pnpbp.2021.110372
Luo, W., Zhong, B. L., and Chiu, H. F. (2021). Prevalence of depressive symptoms among Chinese university students amid the COVID-19 pandemic: a systematic review and meta-analysis. Epidemiol. Psychiatr. Sci. 30:e31. doi: 10.1017/s2045796021000202
Medeiros, R. A., Vieira, D. L., Freitas da Silva, E. V., de Lucas Rezende, L. V. M., dos Santos, R. W., et al. (2020). Prevalence of symptoms of temporomandibular disorders, oral behaviors, anxiety, and depression in dentistry students during the period of social isolation due to COVID-19. J. Appl. Oral Sci. 28:e20200445. doi: 10.1590/1678-7757-2020-0445
Mekhemar, M., Attia, S., Doerfer, C., and Conrad, J. (2021). Dental students in Germany throughout the COVID-19 pandemic: a psychological assessment and cross-sectional survey. Biology 10:611. doi: 10.3390/biology10070611
Meng, N., Liu, Z., Wang, Y., Feng, Y., Liu, Q., Huang, J., et al. (2021). Beyond sociodemographic and COVID-19-related factors: the association between the need for psychological and information support from school and anxiety and depression. Med. Sci. Monit. 27:e929280. doi: 10.12659/MSM.929280
Muhammad Alfareed Zafar, S., Junaid Tahir, M., Malik, M., Irfan Malik, M., Kamal Akhtar, F., and Ghazala, R. (2020). Awareness, anxiety, and depression in healthcare professionals, medical students, and general population of Pakistan during COVID-19 Pandemic: a cross sectional online survey. Med. J. Islamic Repub. Iran 34:131. doi: 10.34171/mjiri.34.131
Nadeem, N., Baig, I., Ilyas, J., Azam, F., Rashid, H., Aftab, R. K., et al. (2020). Anxiety levels due to COVID-19:comparison between medical and non-medical students. Pakistan Postgrad. Med. J. 31:02.
Nakhostin-Ansari, A., Sherafati, A., Aghajani, F., Khonji, M. S., Aghajani, R., and Shahmansouri, N. (2020). Depression and anxiety among Iranian medical students during COVID-19 pandemic. Iran J. Psychiatry 15, 228–235. doi: 10.18502/ijps.v15i3.3815
Naser, A. Y., Dahmash, E. Z., Al-Rousan, R., Alwafi, H., Alrawashdeh, H. M., Ghoul, I., et al. (2020). Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10:e01730. doi: 10.1002/brb3.1730
Nihmath Nisha, S., Francis, Y. M., Balaji, K., Raghunath, G., and Kumaresan, M. (2020). A survey on anxiety and depression level among South Indian medical students during the COVID 19 pandemic. Int. J. Res. Pharm. Sci. 11, 779–786. doi: 10.26452/ijrps.v11iSPL1.3082
Nishimura, Y., Ochi, K., Tokumasu, K., Obika, M., Hagiya, H., Kataoka, H., et al. (2021). Impact of the COVID-19 pandemic on the psychological distress of medical students in Japan: cross-sectional survey study. J. Med. Internet Res. 23:e25232. doi: 10.2196/25232
Pan, S. L., Cui, M., and Qian, J. (2020). Information resource orchestration during the COVID-19 pandemic: a study of community lockdowns in China. Int. J. Inf. Manag. 54:102143. doi: 10.1016/j.ijinfomgt.2020.102143
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: a systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907. doi: 10.1016/j.bbi.2020.05.026
Patelarou, A., Mechili, E. A., Galanis, P., Zografakis-Sfakianakis, M., Konstantinidis, T., Saliaj, A., et al. (2021). Nursing students, mental health status during COVID-19 quarantine: evidence from three European countries. J. Ment Health 30, 164–169. doi: 10.1080/09638237.2021.1875420
Pavan, G., Choudhary, K., Ponnala, V. R., Veeri, R. B., Kumar, R., Chattu, V. K., et al. (2021). Covid-19 impact on the mental health of indian pharmacy students: an online survey. Int. J. Pharm. Res. 13, 3022–3027. doi: 10.31838/ijpr/2021.13.02.396
Pelaccia, T., Sibilia, J., Fels, E., Gauer, L., Musanda, A., Severac, F., et al. (2021). And if we had to do it all over again, would we send medical students to the emergency departments during a pandemic? lessons learned from the COVID-19 outbreak. Intern. Emerg. Med. 16, 1967–1974. doi: 10.1007/s11739-020-02629-0
Perissotto, T., Rodrigues Pereira da Silva, T. C., Choueiri Miskulin, F. P., Pereira, M. B., Neves, B. A., Almeida, B. C., et al. (2021). Mental health in medical students during COVID-19 quarantine: a comprehensive analysis across year-classes. Clinics 76:e3007. doi: 10.6061/clinics/2021/e3007
Pierce, M., Hope, H., Ford, T., Hatch, S., Hotopf, M., John, A., et al. (2020). Mental health before and during the COVID-19 pandemic: a longitudinal probability sample survey of the UK population. Lancet Psychiatry 7, 883–892. doi: 10.1016/s2215-0366(20)30308-4
Puthran, R., Zhang, M. W. B., Tam, W. W., and Ho, R. C. (2016). Prevalence of depression amongst medical students: a meta-analysis. Med. Educ. 50, 456–468. doi: 10.1111/medu.12962
Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., and Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 33:e100213. doi: 10.1136/gpsych-2020-100213
Quek, T. T., Tam, W. W., Tran, B. X., Zhang, M., Zhang, Z., Ho, C. S., et al. (2019). The global prevalence of anxiety among medical students: a meta-analysis. Int. J. Environ. Res. Public Health 16:2735. doi: 10.3390/ijerph16152735
Raoofi, S., Pashazadeh Kan, F., Rafiei, S., Khani, S., Hosseinifard, H., Tajik, F., et al. (2021). Anxiety during the COVID-19 pandemic in hospital staff: systematic review plus meta-analysis. BMJ Support. Palliat. Care. doi: 10.1136/bmjspcare-2021-003125 [Epub ahead of print].
Rossi, R., Socci, V., Talevi, D., Mensi, S., Niolu, C., Pacitti, F., et al. (2020). COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front. Psychiatry 11:790. doi: 10.3389/fpsyt.2020.00790
Rotenstein, L. S., Ramos, M. A., Torre, M., Segal, J. B., Peluso, M. J., Guille, C., et al. (2016). Prevalence of depression, depressive symptoms, and suicidal ideation among medical students a systematic review and meta-analysis. JAMA Am. Med. Assoc. 316, 2214–2236. doi: 10.1001/jama.2016.17324
Saeed, N., and Javed, N. (2021). Lessons from the COVID-19 pandemic: perspectives of medical students. Pakistan J. Med. Sci. 37, 1402–1407. doi: 10.12669/pjms.37.5.4177
Safa, F., Anjum, A., Hossain, S., Trisa, T. I., Alam, S. F., Abdur Rafi, M., et al. (2021). Immediate psychological responses during the initial period of the COVID-19 pandemic among Bangladeshi medical students. Child. Youth Serv. Rev. 122:105912. doi: 10.1016/j.childyouth.2020.105912
Sahebi, A., Nejati-Zarnaqi, B., Moayedi, S., Yousefi, K., Torres, M., and Golitaleb, M. (2021). The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog. Neuropsychopharmacol. Biol. Psychiatry 107:110247. doi: 10.1016/j.pnpbp.2021.110247
Santabárbara, J., Lasheras, I., Lipnicki, D. M., Bueno-Notivol, J., Pérez-Moreno, M., López-Antón, R., et al. (2021). Prevalence of anxiety in the COVID-19 pandemic: an updated meta-analysis of community-based studies. Prog. Neuropsychopharmacol. Biol. Psychiatry 109:110207. doi: 10.1016/j.pnpbp.2020.110207
Sartorao Filho Carlos, I., Rodrigues Wilson Conti De, L., Beauchamp De Castro, R., Marcal Arlete, A., Pavelqueires, S., et al. (2020). Impact of COVID-19 pandemic on mental health of medical students:a cross-sectional study using GAD-7 and PHQ-9 questionnaires. medRxiv % [Preprint] w20200335258.
Shabahang, R., Aruguete, M. S., Rezaei, S., and McCutcheon, L. E. (2021). Psychological determinants and consequences of COVID-19 anxiety: a web-based study in Iran. Health psychol. Res. 9:24841. doi: 10.52965/001c.24841
Shah, S. M. A., Mohammad, D., Qureshi, M. F. H., Abbas, M. Z., and Aleem, S. (2021). Prevalence, psychological responses and associated correlates of depression, anxiety and stress in a global population, during the coronavirus disease (COVID-19) pandemic. Community Ment. Health J. 57, 101–110. doi: 10.1007/s10597-020-00728-y
Shao, R., He, P., Ling, B., Tan, L., Xu, L., Hou, Y., et al. (2020). Prevalence of depression and anxiety and correlations between depression, anxiety, family functioning, social support and coping styles among Chinese medical students. BMC Psychol. 8:38. doi: 10.1186/s40359-020-00402-8
Shehata, G. A., Gabra, R., Eltellawy, S., Elsayed, M., Gaber, D. E., and Elshabrawy, H. A. (2021). Assessment of anxiety, depression, attitude, and coping strategies of the Egyptian population during the COVID-19 pandemic. J. Clin. Med. 10:3989. doi: 10.3390/jcm10173989
Soled, D., Goel, S., Barry, D., Erfani, P., Joseph, N., Kochis, M., et al. (2020). Medical student mobilization during a crisis: lessons from a COVID-19 medical student response team. Acad. Med. 95, 1384–1387. doi: 10.1097/acm.0000000000003401
Song, H. T., Ge, C. H., Chang, L. X., Zhao, T. T., Wu, W., Ge, D. X., et al. (2021). Investigation on the psychological status of college students during the coronavirus disease-2019 epidemic. J. Gen. Psychol. 1–12. doi: 10.1080/00221309.2021.1893637 [Epub ahead of print].
Sun, Y., Wang, D., Han, Z., Gao, J., Zhu, S., and Zhang, H. (2020). Disease prevention knowledge, anxiety, and professional identity during COVID-19 pandemic in nursing students in Zhengzhou, China. J. Korean Acad. Nurs. 50, 533–540. doi: 10.4040/jkan.20125
Torres, C., Otero, P., Bustamante, B., Blanco, V., Díaz, O., and Vázquez, F. L. (2017). Mental health problems and related factors in Ecuadorian college students. Int. J. Environ. Res. Public Health 14:530. doi: 10.3390/ijerph14050530
Tran, B. X., Nguyen, H. T., Le, H. T., Latkin, C. A., Pham, H. Q., Vu, L. G., et al. (2020). Impact of COVID-19 on economic well-being and quality of life of the Vietnamese during the national social distancing. Front. Psychol. 11:565153. doi: 10.3389/fpsyg.2020.565153
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020a). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17:1729. doi: 10.3390/ijerph17051729
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020b). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 87, 40–48. doi: 10.1016/j.bbi.2020.04.028
Wang, Z. H., Yang, H. L., Yang, Y. Q., Liu, D., Li, Z. H., Zhang, X. R., et al. (2020c). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 275, 188–193. doi: 10.1016/j.jad.2020.06.034
Xiao, H., Shu, W., Li, M., Li, Z., Tao, F., Wu, X., et al. (2021). Social distancing among medical students during the 2019 coronavirus disease pandemic in China: disease awareness, anxiety disorder, depression, and behavioral activities. Int. J. Environ. Res. Public Health 17:5047. doi: 10.3390/ijerph18010148
Xie, J., Li, X., Luo, H., He, L., Bai, Y., Zheng, F., et al. (2021). Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front. Public Health 8:588578. doi: 10.3389/fpubh.2020.588578
Xiong, J., Lipsitz, O., Nasri, F., Lui, L. M. W., Gill, H., Phan, L., et al. (2020). Impact of COVID-19 pandemic on mental health in the general population: a systematic review. J. Affect. Disord. 277, 55–64. doi: 10.1016/j.jad.2020.08.001
Yadav, R. K., Baral, S., Khatri, E., Pandey, S., Pandeya, P., Neupane, R., et al. (2021). Anxiety and depression among health sciences students in home quarantine during the COVID-19 pandemic in selected provinces of nepal. Front. Public Health 9:580561. doi: 10.3389/fpubh.2021.580561
Yang, K. H., Wang, L., Liu, H., Li, L. X., and Jiang, X. L. (2021). Impact of coronavirus disease 2019 on the mental health of university students in Sichuan Province, China: an online cross-sectional study. Int. J. Ment. Health Nurs. 30, 875–884. doi: 10.1111/inm.12828
Yin, Y., Yang, X., Gao, L., Zhang, S., Qi, M., Zhang, L., et al. (2021). The association between social support, COVID-19 exposure, and medical students’. Ment. Health Front. Psychiatry 12:555893. doi: 10.3389/fpsyt.2021.555893
Zeng, W., Chen, R., Wang, X., Zhang, Q., and Deng, W. (2019). Prevalence of mental health problems among medical students in China: a meta-analysis. Medicine 98:e15337. doi: 10.1097/md.0000000000015337
Zhang, K., Peng, Y., Zhang, X., and Li, L. (2021a). Psychological burden and experiences following exposure to COVID-19: a qualitative and quantitative study of Chinese medical student volunteers. Int. J. Environ. Res. Public Health 18:4089. doi: 10.3390/ijerph18084089
Zhang, Y., Bao, X., Yan, J., Miao, H., and Guo, C. (2021b). Anxiety and depression in Chinese students during the COVID-19 pandemic: a meta-analysis. Front. Public Health 9:697642. doi: 10.3389/fpubh.2021.697642
Zhang, Y. Y., Bao, X. Q., Yan, J. X., Miao, H. L., and Guo, C. (2021c). Anxiety and depression in Chinese students during the COVID-19 pandemic: a meta-analysis. Front. Public Health 9:697642.
Zheng, X., Guo, Y., Yang, H., Luo, L., Ya, B., Xu, H., et al. (2021). A cross-sectional study on mental health problems of medical and nonmedical students in Shandong during the COVID-19 epidemic recovery period. Front. Psychiatry 12:680202. doi: 10.3389/fpsyt.2021.680202
Keywords: COVID-19, medical students, depression, anxiety, meta-analysis
Citation: Jia Q, Qu Y, Sun H, Huo H, Yin H and You D (2022) Mental Health Among Medical Students During COVID-19: A Systematic Review and Meta-Analysis. Front. Psychol. 13:846789. doi: 10.3389/fpsyg.2022.846789
Received: 31 December 2021; Accepted: 04 April 2022;
Published: 10 May 2022.
Edited by:
María Cristina Richaud, Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), ArgentinaReviewed by:
Quan Zhuang, Central South University, ChinaJosué Quinde, Adventist University of Plata, Argentina
Copyright © 2022 Jia, Qu, Sun, Huo, Yin and You. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dianping You, aGJ5b3VkaWFucGluZ0AxNjMuY29t
 Qingwen Jia1
Qingwen Jia1 Dianping You
Dianping You