
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 02 September 2022
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.834957
 Thao Thi Phuong Nguyen1,2*
Thao Thi Phuong Nguyen1,2* Tham Thi Nguyen1,2
Tham Thi Nguyen1,2 Vu Trong Anh Dam1,2
Vu Trong Anh Dam1,2 Thuc Thi Minh Vu3
Thuc Thi Minh Vu3 Hoa Thi Do3
Hoa Thi Do3 Giang Thu Vu4
Giang Thu Vu4 Anh Quynh Tran5
Anh Quynh Tran5 Carl A. Latkin6
Carl A. Latkin6 Brian J. Hall7,8
Brian J. Hall7,8 Roger C. M. Ho8,9
Roger C. M. Ho8,9 Cyrus S. H. Ho9
Cyrus S. H. Ho9Introduction: This study aimed to explore the mental wellbeing profiles and their related factors among urban young adults in Vietnam.
Methods: A cross-sectional study was conducted in Hanoi, which is the capital of Vietnam. There were 356 Vietnamese who completed the Mental Health Inventory-5 (MHI-5) questionnaire. The Latent Profile Analysis (LPA) was used to identify the subgroups of mental wellbeing through five items of the MHI-5 scale as the continuous variable. Multinomial logistic regression was used to determine factors related to subgroups.
Results: Three classes represented three levels of MHI-5 score, which included “Poor mental health,” “Fair mental health,” and “Good mental health,” were, respectively, 14.3, 46.6, and 39.0%. Compared to a low household economy, participants with an average household economy had 2.11 and 4.79 times higher odds of being in a good mental health class relative to fair and poor mental health classes. Respondents with more than two acute symptoms had 3.85 times higher odds of being in a good mental health class relative to a poor mental health class, as compared to those without acute symptoms. Regarding the measurement of the Perceived Social Support Scale (MSPSS), people having support from their family had 1.80 and 2.23 times higher odds of being in classes of fair and good mental health relative to the poor mental health class; and participants having friend support also had 1.87 times higher odds of being in a good mental health class compared with the fair mental health class, as the MSPSS score increased by 1 unit. People with Rosenberg’s self-esteem scale increased by 1 score, those who had 1.17, 1.26, and 1.47 times higher odds of being in a good compared to fair mental health class, fair compared to poor mental health class, and good compared to poor mental health class, respectively.
Conclusion: Our findings were given to promote a new classification method for mental health screening among the general population. The current findings could be used as evidence to develop policies and plans that focus on encouraging early screening for mental health problems among the general young population in the future.
The World Health Organization (WHO) defines mental health as “a state of wellbeing in which the individual realizes his or her own abilities, can cope with the normal stresses of life, can work productively, and is able to make a contribution to his or her community” (World Health Organization, 2010). Mental health issues affect not only a small segment of the population but also society as a whole. Therefore, ensuring the mental health of all residents is a major challenge for global development and health care systems across nations (World Health Organization, 2003). In Northern Vietnam, a longitudinal study from 2006 to 2013 indicated a depressive trajectory among adolescents and young adults (Bui et al., 2018). Furthermore, the prevalence of suicidal thoughts and having suicide plans were, respectively, 14.1 and 5.7%, which was quite high in this vulnerable population (Le et al., 2016). According to a review by UNICEF, the prevalence of mental health issues among young Vietnamese people ranged from 8 to 29% (UNICEF, 2018). Numerous national surveys among Vietnamese youth were conducted in nearly all regions between 2003 and 2010 (Niemi et al., 2010; Weiss et al., 2012; Thai et al., 2020). However, most of the mentioned studies just described the prevalence of mental health problems among young people without any information on the general population’s classification or screening of mental health issues. Moreover, these studies have not yet provided in-depth analytical methods to identify the related factors affecting the mental health of young Vietnamese people.
Nowadays, various screening tools have been developed to assist in detecting psychological and psychiatric problems. These tools were mainly based on the principles of symptom scoring and had good sensitivity to detect signs of poor mental health. Some of these could be completed in only a few minutes with 20 to 30 items, even shorter instruments, but showed good performance to detect mental health problems (Berwick et al., 1991; Whooley et al., 1997; Rumpf et al., 2001). The Mental Health Inventory-5 (MHI-5) as a five-item questionnaire is used to assess general community mental health (Berwick et al., 1991). This short instrument was developed from both versions of the Medical Outcome Study (MOS) questionnaires: MOS Short Form 20 (Stewart et al., 1988) and MOS Short Form 36 (Ware and Sherbourne, 1992). In a prior study, MHI-5 had been demonstrated to be as good as the more comprehensive and commonly used general health questionnaire (GHQ) (Goldberg and Blackwell, 1970). The performance of MHI-5 was assessed as similar to GHQ-12 in a previous study by McCabe et al. (1996). However, they did not find which might be used as the gold standard for psychiatric screening (Goldberg, 1988). The MHI-5 scale has been developed and validated in the Vietnamese version through an SF-36 survey of 1610 Vietnamese aged over 15 years (Watkins et al., 2000). Furthermore, this research just focuses on testing the psychometric properties of a culturally relevant translation of the medical outcomes. Similarly, this scale has also been used for screening mental health problems among women (Collier et al., 2020), the elderly (Nguyen and Kruse, 2012), or cardiovascular patients (Van Nguyen et al., 2020) in Vietnam.
In a large cohort of the surveyed population, it was likely that different profiles of mental levels existed, which means individuals were classified into the same mental health classes. A previous study regarding mental screening among American adolescents showed three latent classes included flourishing mentally healthy, moderately mentally status, and languishing status (Keyes, 2006). Those who were flourishing mentally group had the greatest psychosocial functions, whereas those who were languishing had the most depressive symptoms and behavioral issues (Keyes, 2006). The majority of mental health screening studies use MHI-5 based on cut-off points (Berwick et al., 1991; Rumpf et al., 2001; Cuijpers et al., 2009) or exploratory factor analysis (EFA) (Rivera-Riquelme et al., 2019) to test the mental health factor structures of participants. However, these studies had not indicated latent profiles of mental levels which might exist. Latent Profile Analysis (LPA) has the potential for latent variable modeling as well as creating and expanding theoretical thinking on the existence of various profiles in variables (Hirschi and Valero, 2015; Gillet et al., 2018). To the best of our knowledge, there are very few studies that specifically target LPA on the MHI-5 scale. After reviewing the literature, we found two studies relative to this topic, which included a longitudinal study of 9,683 women in 2015 (Leigh et al., 2016) and a cross-sectional study of 409 young Finnish men in 2022 (Appelqvist-Schmidlechner et al., 2022). Therefore, this study aimed to explore the mental wellbeing profiles and their related factors among urban young adults in Vietnam.
The study was designed as a cross-sectional investigation of the young Vietnamese population from May 2020 to September 2020. A research facility was established at the Institute for Preventive Medicine and Public Health, Hanoi Medical University, which was implemented to collect voluntary participants.
Participants were recruited following the inclusion criteria: (1) aged 18 to 25; (2) currently living in Hanoi, Vietnam; and (3) willing to sign informed consent and engage in the research. Exclusion criteria included: (1) participants who got serious illnesses; and (2) could not answer questions. The study used both methods of random and convenience sampling, with a completion rate of approximately 100%. During the data collection period, once participants agreed to participate in this study by signing informed consent, a face-to-face interview was conducted for 20–25 min by investigators who were well-trained to use questionnaires. Additionally, the interview took place in a closed room, to ensure privacy and limit outside influences.
We used the registrar’s database of all currently enrolled students at Hanoi Medical University in 2020, with approximately 6,000 students and 1,000 graduate or professional students. A preliminary list was established based on the simple random sample selection, with 10% of students and 20% of graduate/professional students aged 18 to 25 living in Hanoi, Vietnam. Therefore, 600 students and 200 graduate or professional students were collected for the preliminary list. There were 80% of students and 90% of graduate/professional students who had phone numbers. A phone message about the study and a participating invitation would be randomly sent to people on the preliminary list. Approximately 20.8% of students and 55.5% of graduate/professional students responded that they could participate in our study. Those were invited to the research facility and conducted a face-to-face interview. Before starting the interview, participants would be given a written consent form to sign if they decided to participate. There were three research assistants who conducted the direct interviews. As a consequence, the study sample size was collected from a preliminary list of 200 participants, including 100 undergraduates and 100 graduate/professional students. To expand and diversify the study sample, after finishing the interview, we requested participants invite others, such as friends or relatives, to participate in the survey. As a result, the present study recruited a further 156 people from the initial group. A total of 356 participants were recruited for our study.
To collect data, a semi-structured questionnaire consisting of seven main components was developed, including (1) socio-demographic characteristics; (2) alcohol consumption; (3) health conditions; (4) General Self-efficacy scale; (5) Multidimensional Scale of Perceived Social Support scale; (6) Rosenberg Self-Esteem scale; and (7) Mental Health Inventory scale. Before collecting data, this questionnaire was piloted on 10 people of different genders, ages, and occupations to secure the text and logical issue of each question and modify the question with unclear meaning.
Respondents answered questions including gender (male/female), age (unit; year), education level that participants completed (high school or lower/tertiary and upper), marital status (single/married), job (students/others), and household economy (low/average/high).
We used the Alcohol Use Disorders Identification Test-Consumption (AUDIT-C) scale to evaluate the alcohol consumption of participants. The AUDIT-C scale has been used in many studies in Vietnam. Moreover, the Vietnamese version of this tool was also validated elsewhere (Giang et al., 2005, 2008; Tran et al., 2013, 2014). This tool includes three questions with an overall score of 12 points. People are considered Hazardous drinking when the total score of questions 1 and 2 accounts for four points (male) or three points (female). The indicator of Binge drinking is determined when respondents answer the frequency of consuming six or more drinks at one time (Bush et al., 1998). The Cronbach’s alpha of the AUDIT-C scale was 0.71 in the current study.
To explore information about acute symptoms and chronic diseases that participants experienced, two questions were developed, including (1) “Have you ever been experienced any acute symptoms during the last 4 weeks?” (Yes/No), and (2) “Have you ever been diagnosed with any chronic diseases during the last three months?” (Yes/No). If participants indicated “yes” to the above question, they were then asked to self-report their symptoms or conditions. These acute symptoms could include headaches, backaches, allergies, constipation, coughs/sore throats, sneezes/runny noses, fever, helminth infections, diarrhea, gynecologic diseases, skin diseases, eye diseases, etc., that they experienced in the last 4 weeks and chronic diseases they experienced in the last 3 months. The chronic diseases consist of hypertension, cardiovascular disease, diabetes, cancer, asthma, epilepsy/psychiatry, stomach/digestive, chronic obstructive pulmonary disease, etc.
A 10 items of the GSE are created to assess a general sense of perceived self-efficacy with the aim in mind to predict coping with daily hassles as well as adaptation after experiencing all kinds of stressful life events. For each item, a four-point Likert scale is used, ranging from 1 (not at all true) to 4 (exactly true). The total score of GES is calculated by summing all items. After calculating, the score ranged from 10 to 40, with a higher score indicating more self-efficacy (Schwarzer and Jerusalem, 1995). Furthermore, the internal reliability of GSE was reported to be between 0.76 and 0.90. The GSE has been used and validated as a unidimensional construct in some countries. This tool was considered an easy-to-manage and comprehensive evaluation measurement of self-esteem among young adults (Luszczynska et al., 2005; Leung and Leung, 2011; Teo and Kam, 2014). In Vietnam, this tool had also been utilized in previous studies (Goto et al., 2010). In this study, the Cronbach’s alpha for this scale was good at 0.84.
It is a self-reported measure of subjectively assessed social support. The MSPSS consists of 12 items that are divided into three subdomains [including friends (4 items), family (4 items), and significant other (4 items)]. Each item is measured by 7 Likert points from 1 (very strongly disagree) to 7 (very strongly agree) (Zimet et al., 1990). The total score of each domain is summed and then divided by 4 (Zimet, 2016). The higher score of each domain indicates the higher perceived social support. To date, MSPSS has been widely used and validated in some countries, including Vietnam (Wongpakaran et al., 2011; Guan et al., 2014; Lam et al., 2021; Cartwright et al., 2022; Nguyen et al., 2022). In this study, the Cronbach’s alpha for this scale was good at 0.91.
A 10-item scale that measures global self-worth by measuring both positive and negative feelings about oneself. Items 2, 5, 6, 8, and 9 are used to measure negative feelings, while other items are utilized to assess positive feelings about A 10-item scale that measures global self-worth by measuring both positive and negative feelings about oneself. For negative items, a four-point Likert scale is used, including 1-strongly agree, 2-agree, 3-disagree, and 4-strongly disagree. Meanwhile, the options for positive items are reversed, ranging from 1-Strongly Disagree, 2-disagree, 3-agree, and 4-strongly agree. Finally, the total score of all items is calculated, with a higher score indicating higher self-esteem (Kielkiewicz et al., 2020). The Rosenberg self-esteem scale has been validated in some countries, including Vietnam (Martín-Albo et al., 2007; Wongpakaran and Wongpakaran, 2012; Mullen et al., 2013; Kourakou et al., 2021). This tool has also been widely applied in some studies (Nguyen et al., 2010; Nguyen D. T. et al., 2019). In this study, the Cronbach’s alpha for this scale was 0.70.
MHI-5 is considered a simple and valid instrument to detect depressive symptoms among the general population (Yamazaki et al., 2005; Kelly et al., 2008; Cuijpers et al., 2009). This scale consists of 5 dimensions, which is known as a subscale of the Short-Form Health Survey Questionnaire (SF-36) (Ware and Sherbourne, 1992; Stoll et al., 2001). In particular, the MHI-5 investigates the mental health status during the last month since the interview, with items including (1) feeling nervous; (2) loss of pleasure; (3) feeling calm and peaceful; (4) feeling downhearted and blue; and (5) feeling happy. For each item, a 6-point Likert scale is used, including 1 “all of the time,” 2 “most of the time,” 3 “a good bit of the time,” 4 “some of the time,” 5 “a litter of the time,” and 6 “none of the time” (Berwick et al., 1991). However, the scores of items (3) and (5) talking about positive feelings are reversed, with a range of scores from 1 “none of the time” to 6 “all of the time.” In studies with the Vietnamese population, the MHI-5 scale was also applied in some studies to assess mental health problems (Daly et al., 2019). In this study, the Cronbach’s alpha of MHI-5 was good at 0.84.
Latent Profile Analysis is a type of categorical latent variable modeling that focuses on identifying latent subpopulations within a population based on a collection of factors (Collins and Lanza, 2009; Wang and Hanges, 2011; Howard and Hoffman, 2018). LPA has the potential to answer specific research issues as well as to create and expand theoretical thinking on the existence of various profiles in variables (Hirschi and Valero, 2015; Gillet et al., 2018). In particular, LPA assumes that each person may be classified into subpopulations with varying degrees of probability based on the information collected from participants. By using LPA, categorical latent variables are identified, so investigators can get a parsimonious representation of structures in the form of groups (Woo et al., 2018). The MHI-5 scale is a comprehensive assessment instrument for screening the mental wellbeing in the community (Daly et al., 2019), but there is a lack of investigations that could distinguish subgroups on this measurement. Therefore, in this study, LPA was applied to determine group of people (categorical latent variables) who had similar responses to five items of the MHI-5 scale.
Latent Profile Analysis was used to identify the subgroups of mental wellbeing status, with MPLUS version 8.5 (Asparouhov and Muthén, 2021). Five items of the MHI-5 scale as a continuous variable were selected to perform LPA (Rhemtulla et al., 2012). A model containing one to six profiles was used to determine the number of suitable classes. To determine the number of latent profiles with the best accurate classification and goodness of fit, each model was assessed by the following several indices: the lower Akaike Information Criterion (AIC) (Akaike, 1987), the lower Bayesian Information Criterion (BIC) (Schwarz, 1978), the lower sample-size adjusted Bayesian information criterion (aBIC) (Sclove, 1987), the higher entropy value (Celeux and Soromenho, 1996), the significant bootstrapped likelihood ratio test (BLRT) (Nylund et al., 2007), the significant Lo– Mendell–Rubin adjusted likelihood ratio test (LMR-LRT), the significant Adjusted Lo-Mendell-and Rubin likelihood ratio test (LMRa-LRT) (Lo et al., 2001). These tests were calculated for model fit decision purposes by comparing models where a significant p-value (p < 0.05) showed that a k-class model fitted better than the (k-1) – class model (Toker, 2016).
Both descriptive and analytical statistics were used to address the main aims of the study by STATA version 16. Continuous variables were presented as mean and standard deviation (SD), while categorical variables were presented as frequency with percentage. Descriptive, analytical statistics and multinomial logistic regression between all variables were calculated using STATA version 16 (StataCorp LP, College Station, TX, United States). We used Kruskal-Wallis tests for continuous variables and χ2 tests for categorical variables to compare the differences between three classes of mental wellbeing and some characteristics. Multinomial logistic regression models were utilized to determine factors related to the level of mental wellbeing among participants. The social-demographic characteristics, health status, alcohol consumption, General Self-efficacy cale, Multidimensional Scale of Perceived Social Support, and Rosenberg self-esteem scale were all potential covariates for the full model. A p value (p) < 0.05 was considered statistically significant.
This study was ethically approved by the Institutional Ethical Review Board at Hanoi Medical University on March 13, 2020. Informed consent would be supplied to participants before starting the study. People would sign the written consent if they decided to participate. Participation was completely voluntary; they could feel free to decline to join for any reason. Even after signing the consent form, they could also stop participating in this project at any time or refuse to answer any individual questions. Collected data was saved in a secured system and served for study purposes only.
A study sample consisting of 356 participants with a mean age of 22.03 (SD = ± 3.21) was assessed for mental health status by using the MHI-5.
Table 1 describes the percentage of responses and the average score of each question according to the 6 answer options of the MHI-5 scale. In terms of questions 1, 2, and 4, the majority of participants answer with the levels of “some of the time” and “a little of the time.” By contrast with questions 3 and 5, most respondents reported “most of the time” and “a good bit of time.” On the MHI-5 scale, the mean score for each item ranged from 3.98 to 4.75 points.
Table 2 demonstrated a latent profile class with the largest model of four classes of the MHI-5 scale. Several models were selected according to the suitable indicators (AIC, BIC, and aBIC) and test values (LMR-LPT, LMRa-LRT, and BLRT). A model with three classes was the most suitable based on the values of fit indexes and tests. In particular, the indicators of AIC, BIC, and aBIC reduced significantly when more classes were added to the model. Therefore, the model with two and three classes was preferred. Although the four class-models showed the favored values of AIC, BIC, aBIC, examining three tests (LMR-LPT, LMRa-LRT, and BLRT) determined three class-models with p < 0.05, which was the most appropriate model.
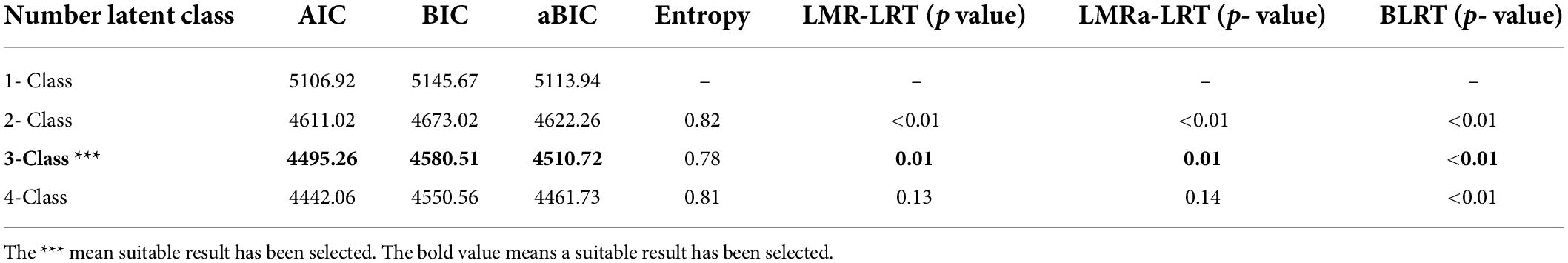
Table 2. Comparison of LPA models with different latent classes based on model selection statistics and the most suitable model.
In Figure 1, the total mean score MHI-5 from five questions was divided into three classes, which included “poor mental health,” “fair mental health,” and “good mental health.” The respective mean scores of the three classes were 14.33% (poor mental health), 46.63% (fair mental health), and 39.04% (good mental health). In terms of poor mental health class, the mean score of items 1, 2, 3, 4, and 5 was reported at 2.86 ± 0.69, 3.61 ± 0.85, 2.68 ± 0.73, 3.37 ± 0.66, and 2.61 ± 0.80, respectively. Regarding the fair mental health class, the mean score of item 1 was 4.10 ± 0.73, item 2 was 4.51 ± 0.68, item 3 was 3.74 ± 0.85, item 4 was 4.55 ± 0.66, and item 5 was 3.92 ± 0.75. Compared to other groups, each item of MHI-5 scale in the good mental health class had the higher score, with 5.24 ± 0.65 (item 1), 5.47 ± 0.65 (item 2), 4.73 ± 0.79 (item 3), 5.40 ± 0.55 (item 4), and 4.91 ± 0.73 (item 5).
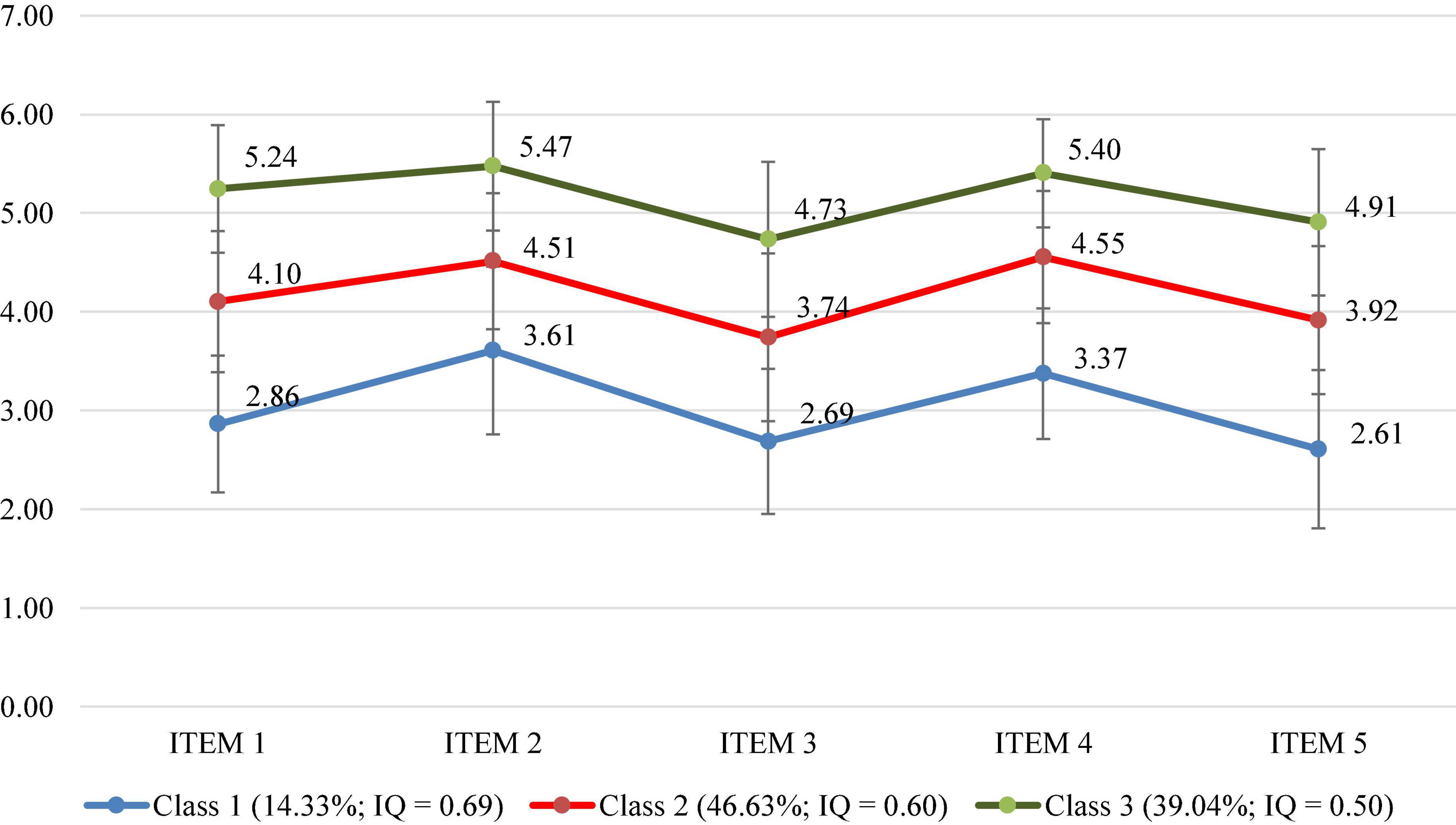
Figure 1. LPA on the three classes of the MHI-5. Class 1, Poor mental health; Class 2, Fair mental health; Class 3, Good mental health; IQ, Inter-quartile range; ITEM 1, Feeling nervous; ITEM 2, Loss of pleasure; ITEM 3, Feeling calm and peaceful; ITEM 4, Feeling downhearted and blue; and ITEM 5, Feeling happy.
Table 3 describes some characteristics among 356 participants regarding the MHI-5 scale. The majority of respondents were female (72.08%), students (89.61%), and educated at the level of high school or lower (83.15%). The majority of participants with more than two acute symptoms occupied 60.11%. Regarding the AUDIT-C scale, Hazardous and Binger drinking indicators were found to be 77.12 and 84.27%, respectively. In terms of the MSPSS scale, participants who belong to the good mental health class have higher mean points (of all three domains, including family, friends, and significant others) than the two remaining classes, with mean values of 5.65, 5.47, and 5.30. The differences between groups are statistically significant with a p < 0.05. Similarly, the mean score of the General Self-efficacy Scale and the Rosenberg Self-esteem Scale also show a higher value in the good mental health class than in the two remaining classes. These differences were also statistically significant (p < 0.05).
In Table 4 compared to participants with a low household economy, those with an average household economy had 2.11 and 4.79 times higher odds of being in a good mental health class relative to those with a fair mental health class (OR = 2.11; 95%CI: 1.07; 4.14; p < 0.05) and a poor mental health class (OR = 4.79; 95%CI: 1.51; 15.20; p < 0.001).
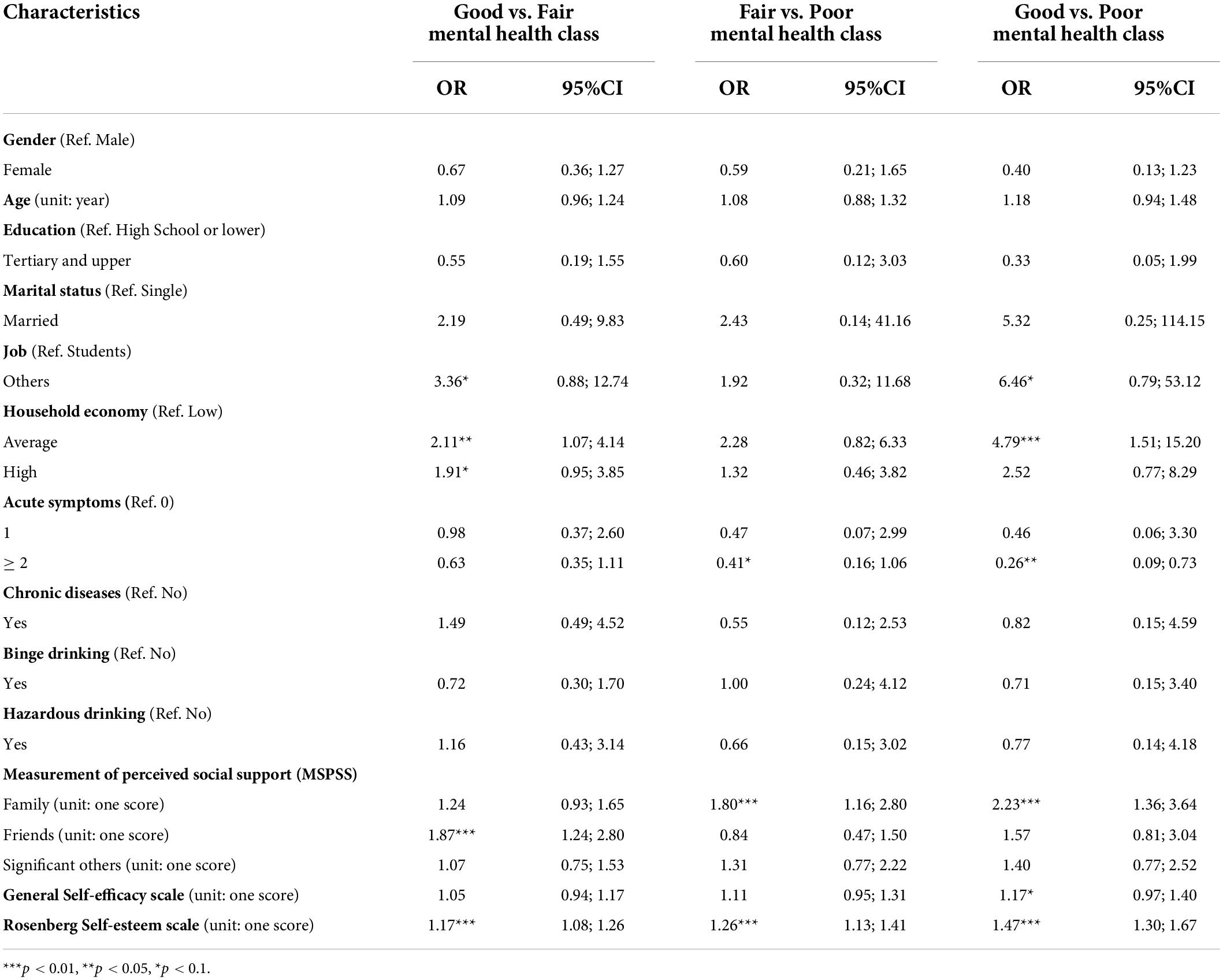
Table 4. Selected results of multinomial logistic regression: Prediction of the patterns of the MHI-5.
Furthermore, the odds ratio for participants with more than two acute symptoms was 0.26 (OR = 0.26, 95%CI: 0.09; 0.73), indicating that those had 3.85 times higher odds of being in a good mental health class relative to a poor mental health class, as compared to those without acute symptoms.
Regarding the measurement of the perceived social support scale, people who received higher support from their family had a higher odds ratio of being in fair and good mental health classes about 1.80 times (OR = 1.80; 95%CI = 1.16; 2.80) and 2.23 times (OR = 2.23; 95%CI = 1.36; 3.64) than in poor mental health class.
Similarly, participants who received the highest support from their friends were more likely in the good mental health class compared to the fair mental health class by 1.87 times (OR = 1.87; 95%CI = 1.24; 2.80).
Related to Rosenberg’s self-esteem scale, participants have 1.17, 1.26, and 1.47 times higher odds of being in a good compared to fair mental health class (OR = 1.17, 95%CI: 1.08; 1.26), fair compared to poor mental health class (OR = 1.26, 95%CI: 1.13; 1.41), and good compared to poor mental health class (OR = 1.47, 95%CI: 1.30; 1.67), as Rosenberg’s self-esteem score increased by 1 unit.
The current study was considered the first work in Vietnam using the LPA approach to explore unobserved subgroups of the mental health status of the young population. Our findings determined three latent subgroups based on the MHI-5 score from the study samples. The majority of respondents were classified as having fair mental health (46.63%), while those who were assessed as having poor mental health accounted for the smallest proportion (14,33%). Notably, receiving family and friend support (according to the MSPSS scale) was significantly related to having better mental health than the other groups. Moreover, it was the same case with the high individual’s self-esteem score as well as the household income aspect, which was at an average level compared to other groups. People with more than two acute symptoms, on the other hand, saw their mental health get worse in a big way.
In detecting mental health issues, the MHI-5 was proved to be the comprehensive and commonly used General Health Questionnaire (Goldberg and Blackwell, 1970; Berwick et al., 1991). This measurement has good performance characteristics in screening for mental health issues in the general population (Rumpf et al., 2001). Moreover, the MHI-5 was widely utilized as a mental component of the SF-36 scale in previous studies in Vietnam (Watkins et al., 2000). Therefore, we decided to use the MHI-5 as a screening tool to classify people through LPA analysis. The percentage of mental health symptoms in the present study was consistent with the UNICEF report in 2015, with the prevalence of general mental health problems in Vietnam ranging from 8 to 29% (Unicef Viet Nam, 2020). In 2019, similar data was also identified with 14.4% of common mental disorders through a population-based cross-sectional survey (Nguyen T. et al., 2019). According to the Vietnam National Mental Hospital, the prevalence of 10 common disorders occupied 14.2% in 2014 (World Health Organization, 2021). Compared to a latent profile study using the MHI-5 scale for screening mental health status (with three latent profiles from poor to good mental health) among Australian women (2015), that identified people who were still alive between 1996 and 2008 had poor mental health were 28 and 17.4%, respectively (Leigh et al., 2016). Furthermore, our respondents were classified into fair and good mental health, those who perceived social support at high levels from family and friends, compared to participants identified with poor mental health status. Indeed, community support was of the highest importance when an individual suffered health issues. This point was demonstrated in the previous research (Bloor et al., 2004; Reblin and Uchino, 2008; Uchino et al., 2012). In addition, many scholars showed evidence that social supports such as family and significant others have effects on health issues, for example, the neuroendocrine, immune functions (Uchino, 2006), and cardiovascular responses (Uno et al., 2002). They also argued that the effectiveness of social support brought a buffering effect on depression and stressful life events (Komatsu et al., 2010), leading to a positive effect on mental health (Veselska et al., 2010). Our results emphasized that family and significant others seemed to make the greatest contribution to good mental health status and chronic disease (Vassilev et al., 2013).
Likewise, people with higher Rosenberg self-esteem scores are more likely to be in the better mental health groups, according to the current findings. In 2001, Richard et al. indicated regulation of emotional states was affected mainly by self-esteem (Robins et al., 2001). People with high self-esteem could regulate their emotional states by reducing negative thoughts and concerns about potential threats (Brown and Marshall, 2001). According to Watson et al. (1988), low self-esteem individuals tend to have a negative self view, whereas high termed positive self-esteem individuals tend to be secure and satisfied with themselves (Watson et al., 1988). Various researchers also found a correlation between low mental health and general self-esteem (Henriksen et al., 2017; Nguyen D. T. et al., 2019). Many studies had declared that a good mood reduces self-control because a happy (vs. unhappy) status tended to prolong the time for positive mood & less mental illness symptoms (Isen and Simmonds, 1978; Wegener and Petty, 1994). Moreover, participants with an average income compared to those with a low-income were more likely to be in better mental health groups. This result was completely consistent with a population-based cross-sectional survey in Vietnam’s southern provinces, which showed participants who had mid-level or advantaged economic status were less likely to have family members with any psychotic symptoms (Nguyen T. et al., 2019). At the individual level, psychotic symptoms may onset coinciding with adverse events which are influenced by factors at the household level such as financial constraints or lack of social support (Dutta et al., 2019). Negative effects of economic shocks such as financial crises, getting fired, or income loss according to the household aspect of mental health status, which was demonstrated by previous studies (Baird et al., 2013; Marcus, 2013; Adhvaryu et al., 2019).
One of the notable results was that participants who experienced more than two acute symptoms had a significant association with deteriorating mental health. Previous studies indicated the inverse association between acute diseases and mental illnesses such as stress, anxiety, depression, etc. These issues often occur when people are hospitalized with severe illnesses. The health status of those with more mental illness tended to deteriorate during and after hospitalization (Covinsky et al., 1997). The systematic review research result was implemented among survivors of cancer in 134 publications and indicated similarity in the above-discussed point with the effects of acute symptoms of cancer diseases and mental health status on survivorship (Van Leeuwen et al., 2018). Furthermore, in Switzerland, a retrospective study identified that a quarter of patients who frequently used the emergency department suffered from mental disorders, and those were more likely to be in personality disorders (Slankamenac et al., 2020). Recently, numerous epidemic outbreaks led to mental health changes followed by an increase in confirmed cases, such as the COVID-19 pandemic, Middle East Respiratory Syndrome, etc., (Jeong et al., 2016; Shi et al., 2020). These contexts could lead to depressive symptoms, anxiety, insomnia, acute stress, and latent risks among the general population.
Our findings demonstrated several implications that could be helpful to improve mental health status based on the discussed evidence. First and foremost, our results reflected the MHI-5 score, which corresponded to the middle and poor mental health classes among the study population. Thus, raising optimal mental health as well as health-related quality of life was presented with the warning need to further study and expand mental healthcare aspects. Second, the risk factors lead to mental illness prevention needed to address (1) general community education related to mental problems and prevention; (2) improved approaches and care for the high-risk groups; and (3) emphasis on limiting access to high-risk factors causing mental illness from the analyzed study, such as acute diseases, economic problems, and lack of social support. Third, we further posited that approaching mental problems based on the LPA analysis would explore the following implications: (1) social-supports played an important role (particularly with family & significant others) in mental health, thus, it was necessary to increase an intimate connection between individuals, families, and communities; (2) people with higher Rosenberg self-esteem scores were found to have better mental health status, so future intervention strategies may refer to our findings for comprehensive effectiveness; and (3) policies development to promote and improve the mental health in the general community and strengthen the health care system.
This study provided a valuable picture of the mental health of the general population and specifically young people in Vietnam. However, the findings of our study also entailed several limitations and sources of bias. First, no causal conclusions could be drawn because our research used a cross-sectional study. Second, a lack of participation on the part of those respondents who were identified as having mental problems was probably caused by selection bias. This would be challenging to prevent because participants attended voluntarily and there was no effort to access the mental patients. Third, the majority of participants were female (72.1%) and students (89.6%), so the study sample was non-representative of urban young adults in Vietnam. Moreover, we were not able to get a larger and more complete sample due to participants recruited during the outbreak of COVID-19. Hence, future research needs to extend the sample collection and ensure the representation of the study population. Hence, future research is needed to extend the sample collection. For future research, it would be helpful to consider the social-ecological effects of using the MHI-5 scale to evaluate the general Vietnamese population, especially the loneliness scores, which could be used to help formulate policies to improve mental health in the community.
We found substantial evidence that the variables including self-esteem, perceived social support, and household economy on average are associated with higher profiles of mental health status. The impacts of acute symptoms on mental health outcomes were still insufficient, but our findings showed evidence that greater acute symptoms are related to more mental problems. For this study, evidence was given to raise awareness of mental health in the community and develop policies to promote social support and strengthen the general health care system.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Institutional Ethical Review Board in Hanoi Medical University, Vietnam. The patients/participants provided their written informed consent to participate in this study.
TTPN, TV, HD, GV, CL, BH, RH, and CH: conceptualization. TTPN, TTN, VD, and AT: data curation. TTPN, TTN, and VD: formal analysis. TTPN, TV, HD, CL, BH, RH, and CH: methodology. TTPN, TV, HD, GV, and AT: supervision. TTN and VD: investigation. TTPN, TTN, VD, and GV: writing – original draft. TTPN, TTN, VD, TV, HD, GV, AT, CL, BH, RH, and CH: writing – review and editing. All authors contributed to the article and approved the submitted version.
This study received funding from Gia Lam Urban Development And Investment Company Limited, Vingroup, and was supported by the Vingroup Innovation Foundation (VINIF) (Grant No. VINIF.2019.DA14). The funder was not involved in the study design, collection, analysis, interpretation of data, the writing of this article, or the decision to submit it for publication. The Publication fee for the manuscript was funded by the NUS Department of Psychological Medicine (R-177-000-100-001/R-177-000-003-001) and NUS iHeathtech Other Operating Expenses (R-722-000-004-731).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Adhvaryu, A., Fenske, J., and Nyshadham, A. (2019). Early life circumstance and adult mental health. J. Polit. Econ. 127, 1516–1549. doi: 10.1086/701606
Akaike, H. (1987). Factor analysis and AIC. Selected papers of hirotugu akaike. Berlin: Springer, 371–386. doi: 10.1007/978-1-4612-1694-0_29
Appelqvist-Schmidlechner, K., Raitanen, J., Vasankari, T., Kyröläinen, H., Häkkinen, A., Honkanen, T., et al. (2022). Relationship between accelerometer-based physical activity, sedentary behavior, and mental health in young finnish men. Front. Public Health 10:820852. doi: 10.3389/fpubh.2022.820852
Asparouhov, T., and Muthén, B. (2021). Expanding the Bayesian structural equation, multilevel and mixture models to logit, negative-binomial, and nominal variables. Struct. Equ. Model. 28, 1–16. doi: 10.1080/10705511.2020.1764360
Baird, S., De Hoop, J., and Özler, B. (2013). Income shocks and adolescent mental health. J. Hum. Resour. 48, 370–403. doi: 10.1353/jhr.2013.0014
Berwick, D. M., Murphy, J. M., Goldman, P. A., Ware, J. E. Jr., Barsky, A. J., and Weinstein, M. C. (1991). Performance of a five-item mental health screening test. Med. care 29, 169–176. doi: 10.1097/00005650-199102000-00008
Bloor, L. E., Uchino, B. N., Hicks, A., and Smith, T. W. (2004). Social relationships and physiological function: The effects of recalling social relationships on cardiovascular reactivity. Ann. Behav. Med. 28, 29–38. doi: 10.1207/s15324796abm2801_5
Brown, J. D., and Marshall, M. A. (2001). Self-esteem and emotion: Some thoughts about feelings. Pers. Soc. Psychol. Bull. 27, 575–584. doi: 10.1177/0146167201275006
Bui, Q. T., Vu, L. T., and Tran, D. M. (2018). Trajectories of depression in adolescents and young adults in vietnam during rapid urbanisation: Evidence from a longitudinal study. J. Child Adolesc. Ment. Health 30, 51–59. doi: 10.2989/17280583.2018.1478299
Bush, K., Kivlahan, D. R., McDonell, M. B., Fihn, S. D., and Bradley, K. A. (1998). The AUDIT alcohol consumption questions (AUDIT-C): An effective brief screening test for problem drinking. Ambulatory Care quality improvement project (ACQUIP). Alcohol use disorders identification test. Arch. Intern. Med. 158, 1789–1795. doi: 10.1001/archinte.158.16.1789
Cartwright, A. V., Pione, R. D., Stoner, C. R., and Spector, A. (2022). Validation of the multidimensional scale of perceived social support (MSPSS) for family caregivers of people with dementia. Aging Ment. Health 26, 286–293. doi: 10.1080/13607863.2020.1857699
Celeux, G., and Soromenho, G. (1996). An entropy criterion for assessing the number of clusters in a mixture model. J. Classif. 13, 195–212. doi: 10.1007/BF01246098
Collier, K. M., Weiss, B., Pollack, A., and Lam, T. (2020). Explanatory variables for women’s increased risk for mental health problems in vietnam. Soc. Psychiatry Psychiatr. Epidemiol. 55, 359–369. doi: 10.1007/s00127-019-01761-3
Collins, L. M., and Lanza, S. T. (2009). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. New York, NY: John Wiley & Sons. doi: 10.1002/9780470567333
Covinsky, K. E., Fortinsky, R. H., Palmer, R. M., Kresevic, D. M., and Landefeld, C. S. (1997). Relation between symptoms of depression and health status outcomes in acutely ill hospitalized older persons. Ann. Intern. Med. 126, 417–425. doi: 10.7326/0003-4819-126-6-199703150-00001
Cuijpers, P., Smits, N., Donker, T., Ten Have, M., and de Graaf, R. (2009). Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item mental health inventory. Psychiatry Res. 168, 250–255. doi: 10.1016/j.psychres.2008.05.012
Daly, A., Carey, R. N., Darcey, E., Chih, H., LaMontagne, A. D., Milner, A., et al. (2019). Using three cross-sectional surveys to compare workplace psychosocial stressors and associated mental health status in six migrant groups working in Australia compared with Australian-born workers. Int. J. Environ. Res. Public Health 16:735. doi: 10.3390/ijerph16050735
Dutta, M., Spoorthy, M. S., Patel, S., and Agarwala, N. (2019). Factors responsible for delay in treatment seeking in patients with psychosis: A qualitative study. Indian J. Psychiatry 61:53.
Giang, K. B., Allebeck, P., Spak, F., Van Minh, H., and Dzung, T. V. (2008). Alcohol use and alcohol consumption–related problems in rural vietnam: An epidemiological survey using AUDIT. Subst. Use Misuse 43, 481–495. doi: 10.1080/10826080701208111
Giang, K. B., Spak, F., Dzung, T. V., and Allebeck, P. (2005). The use of audit to assess level of alcohol problems in rural vietnam. Alcoh. Alcohol. 40, 578–583. doi: 10.1093/alcalc/agh198
Gillet, N., Morin, A. J., Sandrin, E., and Houle, S. A. (2018). Investigating the combined effects of workaholism and work engagement: A substantive-methodological synergy of variable-centered and person-centered methodologies. J. Vocat. Behav. 109, 54–77. doi: 10.1016/j.jvb.2018.09.006
Goldberg, D. P., and Blackwell, B. (1970). Psychiatric illness in general practice: A detailed study using a new method of case identification. Br med J 2, 439–443. doi: 10.1136/bmj.2.5707.439
Goto, A., Nguyen, Q. V., Nguyen, T. T. V., Pham, N. M., Chung, T. M. T., Trinh, H. P., et al. (2010). Associations of psychosocial factors with maternal confidence among Japanese and vietnamese mothers. J. Child Fam. Stud. 19, 118–127. doi: 10.1007/s10826-009-9291-9
Guan, N. C., Sulaiman, A. R., Seng, L. H., Ann, A. Y. H., Wahab, S., and Pillai, S. K. (2014). Factorial validity and reliability of the Tamil version of multidimensional scale of perceived social support among a group of participants in university malaya medical centre, malaysia. Indian J. Psychol. Med. 35, 385–388. doi: 10.4103/0253-7176.122234
Henriksen, I. O., Ranøyen, I., Indredavik, M. S., and Stenseng, F. (2017). The role of self-esteem in the development of psychiatric problems: A three-year prospective study in a clinical sample of adolescents. Child Adolesc. Psychiatry Ment. Health 11, 1–9. doi: 10.1186/s13034-017-0207-y
Hirschi, A., and Valero, D. (2015). Career adaptability profiles and their relationship to adaptivity and adapting. J. Vocat. Behav. 88, 220–229. doi: 10.1016/j.jvb.2015.03.010
Howard, M. C., and Hoffman, M. E. (2018). Variable-centered, person-centered, and person-specific approaches: Where theory meets the method. Organization. Res. Methods 21, 846–876. doi: 10.1177/1094428117744021
Isen, A. M., and Simmonds, S. F. (1978). The effect of feeling good on a helping task that is incompatible with good mood. Soc. Psychol. 41, 346–349. doi: 10.2307/3033588
Jeong, H., Yim, H. W., Song, Y.-J., Ki, M., Min, J.-A., Cho, J., et al. (2016). Mental health status of people isolated due to middle east respiratory syndrome. Epidemiol. Health 38:e2016048. doi: 10.4178/epih.e2016048
Kelly, M. J., Dunstan, F. D., Lloyd, K., and Fone, D. L. (2008). Evaluating cutpoints for the MHI-5 and MCS using the GHQ-12: A comparison of five different methods. BMC Psychiatry 8:10. doi: 10.1186/1471-244X-8-10
Keyes, C. L. (2006). Mental health in adolescence: Is America’s youth flourishing? Am. J. Orthopsychiatry 76, 395–402. doi: 10.1037/0002-9432.76.3.395
Kielkiewicz, K., Mathúna, C. Ó, and McLaughlin, C. (2020). Construct validity and dimensionality of the rosenberg self-esteem scale and its association with spiritual values within irish population. J. Relig. Health 59, 381–398. doi: 10.1007/s10943-019-00821-x
Komatsu, Y., Kai, Y., Nagamatsu, T., Shiwa, T., Suyama, Y., and Sugimoto, M. (2010). Buffering effect of social support in the workplace on job strain and depressive symptoms. Sangyo Eiseigaku Zasshi 52, 140–148. doi: 10.1539/sangyoeisei.B9012
Kourakou, A., Tigani, X., Bacopoulou, F., Vlachakis, D., Papakonstantinou, E., Simidala, S., et al. (2021). The rosenberg self-esteem scale: Translation and validation in the Greek Language in adolescents. Adv. Exp. Med. Biol. 1339, 97–103. doi: 10.1007/978-3-030-78787-5_13
Lam, T. Q., Linh, T. T., and Thuy, L. B. (2021). The impact of social support on infertility-related stress: A study in the vietnamese context. Open J. Social. Sci. 9, 259–273. doi: 10.4236/jss.2021.912017
Le, M. T., Holton, S., Nguyen, H. T., Wolfe, R., and Fisher, J. (2016). Poly-victimisation and health risk behaviours, symptoms of mental health problems and suicidal thoughts and plans among adolescents in Vietnam. Int. J. Ment. Health Syst. 10, 1–12. doi: 10.1186/s13033-016-0099-x
Leigh, L., Byles, J. E., Chojenta, C., and Pachana, N. A. (2016). Late life changes in mental health: A longitudinal study of 9683 women. Aging Ment. Health 20, 1044–1054. doi: 10.1080/13607863.2015.1060943
Leung, D. Y., and Leung, A. Y. (2011). Factor structure and gender invariance of the Chinese general self-efficacy scale among soon-to-be-aged adults. J. Adv. Nurs. 67, 1383–1392. doi: 10.1111/j.1365-2648.2010.05529.x
Lo, Y., Mendell, N. R., and Rubin, D. B. (2001). Testing the number of components in a normal mixture. Biometrika 88, 767–778. doi: 10.1093/biomet/88.3.767
Luszczynska, A., Scholz, U., and Schwarzer, R. (2005). The general self-efficacy scale: Multicultural validation studies. J. Psychol. 139, 439–457. doi: 10.3200/JRLP.139.5.439-457
Marcus, J. (2013). The effect of unemployment on the mental health of spouses–Evidence from plant closures in Germany. J. Health Econ. 32, 546–558. doi: 10.1016/j.jhealeco.2013.02.004
Martín-Albo, J., Núñez, J. L., Navarro, J. G., and Grijalvo, F. (2007). The Rosenberg Self-Esteem Scale: Translation and validation in university students. .Spanish J. Psychol. 10, 458–467. doi: 10.1017/S1138741600006727
McCabe, C. J., Thomas, K. J., Brazier, J. E., and Coleman, P. (1996). Measuring the mental health status of a population: A comparison of the GHQ-12 and the SF-36 (MHI-5). Cambridge: Cambridge University Press.
Mullen, S. P., Gothe, N. P., and McAuley, E. (2013). Evaluation of the factor structure of the rosenberg self-esteem scale in older adults. Pers. Individ. Dif. 54, 153–157. doi: 10.1016/j.paid.2012.08.009
Nguyen, D. T., Wright, E. P., Dedding, C., Pham, T. T., and Bunders, J. (2019). Low self-esteem and its association with anxiety, depression, and suicidal ideation in vietnamese secondary school students: A cross-sectional study. Front. Psychiatry 10:698. doi: 10.3389/fpsyt.2019.00698
Nguyen, T., Tran, T., Tran, H., Tran, T., and Fisher, J. (2019). The burden of clinically significant symptoms of common and severe mental disorders among adults in vietnam: A population-based cross-sectional survey. BMC Public Health 19:1173. doi: 10.1186/s12889-019-7513-7
Nguyen, H. T., Dunne, M. P., and Le, A. V. (2010). Multiple types of child maltreatment and adolescent mental health in viet nam. Bull. World Health Organ. 88, 22–30. doi: 10.2471/BLT.08.060061
Nguyen, M. H., and Kruse, A. (2012). The effects of Tai Chi training on physical fitness, perceived health, and blood pressure in elderly vietnamese. Open Access J. Sports Med. 3:7. doi: 10.2147/OAJSM.S27329
Nguyen, T. T. P., Nguyen, T. T., Do, H. N., Vu, T. B. T., Vu, K. L., Do, H. M., et al. (2022). Parent-child relationship quality and internet use in a developing country: Adolescents’ perspectives. Front. Psycho.l 13:847278. doi: 10.3389/fpsyg.2022.847278
Niemi, M., Thanh, H. T., Tuan, T., and Falkenberg, T. (2010). Mental health priorities in vietnam: A mixed-methods analysis. BMC Health Serv. Res. 10:257. doi: 10.1186/1472-6963-10-257
Nylund, K. L., Asparouhov, T., and Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: A monte carlo simulation study. Struct. Equ. Model. 14, 535–569. doi: 10.1080/10705510701575396
Reblin, M., and Uchino, B. N. (2008). Social and emotional support and its implication for health. Curr. Opin. Psychiatry 21:201. doi: 10.1097/YCO.0b013e3282f3ad89
Rhemtulla, M., Brosseau-Liard, P. É, and Savalei, V. (2012). When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychol. Methods 17:354. doi: 10.1037/a0029315
Rivera-Riquelme, M., Piqueras, J. A., and Cuijpers, P. (2019). The revised mental health inventory-5 (MHI-5) as an ultra-brief screening measure of bidimensional mental health in children and adolescents. Psychiatry Res. 274, 247–253. doi: 10.1016/j.psychres.2019.02.045
Robins, R. W., Tracy, J. L., Trzesniewski, K., Potter, J., and Gosling, S. D. (2001). Personality correlates of self-esteem. J. Res. Pers. 35, 463–482. doi: 10.1006/jrpe.2001.2324
Rumpf, H.-J., Meyer, C., Hapke, U., and John, U. (2001). Screening for mental health: Validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res. 105, 243–253. doi: 10.1016/S0165-1781(01)00329-8
Schwarz, G. (1978). Estimating the dimension of a model. Ann. Stat. 6, 461–464. doi: 10.1214/aos/1176344136
Schwarzer, R., and Jerusalem, M. (1995). “Generalized self-efficacy scale,” in Measures in health psychology: A user’s portfolio Causal and control beliefs, eds J. Weinman, S. Wright, and M. Johnston (Windsor, UK: NFER-NELSON), 35–37. doi: 10.1037/t00393-000
Sclove, S. L. (1987). Application of model-selection criteria to some problems in multivariate analysis. Psychometrika 52, 333–343. doi: 10.1007/BF02294360
Shi, L., Lu, Z.-A., Que, J.-Y., Huang, X.-L., Liu, L., Ran, M.-S., et al. (2020). Prevalence of and risk factors associated with mental health symptoms among the general population in China during the coronavirus disease 2019 pandemic. JAMA Netw. Open 3, e2014053–e. doi: 10.1001/jamanetworkopen.2020.14053
Slankamenac, K., Heidelberger, R., and Keller, D. I. (2020). Prediction of recurrent emergency department visits in patients with mental disorders. Front. Psychiatry 11:48. doi: 10.3389/fpsyt.2020.00048
Stewart, A. L., Hays, R. D., and Ware, J. E. Jr. (1988). The MOS short-form general health survey: Reliability and validity in a patient population. Medical Care 26, 724–735. doi: 10.1097/00005650-198807000-00007
Stoll, T., Kauer, Y., Büchi, S., Klaghofer, R., Sensky, T., and Villiger, P. (2001). Prediction of depression in systemic lupus erythematosus patients using SF-36 mental health scores. Rheumatology 40, 695–698. doi: 10.1093/rheumatology/40.6.695
Teo, T., and Kam, C. (2014). A measurement invariance analysis of the general self-efficacy scale on two different cultures. J. Psychoeduc. Assess. 32, 762–767. doi: 10.1177/0734282914531707
Thai, T. T., Vu, N. L. L. T., and Bui, H. H. T. (2020). Mental health literacy and help-seeking preferences in high school students in ho Chi Minh City, Vietnam. Sch. Ment. Health 12, 378–387. doi: 10.1007/s12310-019-09358-6
Toker, T. (ed.) (2016). A comparison of latent class analysis and the mixture Rasch model: A cross-cultural comparison of 8th grade mathematics achievement in the fourth International Mathematics and Science Study (TIMSS-2011). Denver, CO: University of Denver.
Tran, B. X., Nguyen, L. T., Do, C. D., Nguyen, Q. L., and Maher, R. M. (2014). Associations between alcohol use disorders and adherence to antiretroviral treatment and quality of life amongst people living with HIV/AIDS. BMC Public Health 14:27. doi: 10.1186/1471-2458-14-27
Tran, B. X., Nguyen, N., Ohinmaa, A., Duong, A. T., Nguyen, L. T., Van Hoang, M., et al. (2013). Prevalence and correlates of alcohol use disorders during antiretroviral treatment in injection-driven HIV epidemics in vietnam. Drug Alcoh. Depend. 127, 39–44. doi: 10.1016/j.drugalcdep.2012.06.009
Uchino, B. N. (2006). Social support and health: A review of physiological processes potentially underlying links to disease outcomes. Journal of behavioral medicine 29, 377–387. doi: 10.1007/s10865-006-9056-5
Uchino, B. N., Bowen, K., Carlisle, M., and Birmingham, W. (2012). Psychological pathways linking social support to health outcomes: A visit with the “ghosts” of research past, present, and future. Soc. Sci. Med. 74, 949–957. doi: 10.1016/j.socscimed.2011.11.023
Unicef Viet Nam (2020). Mental health and psychosocial wellbeing among children and young people in selected provinces and cities in Viet Nam. Hanoi: UNICEF Viet Nam.
UNICEF (2018). Mental health and psychosocial wellbeing among children and young people in selected provinces and cities in Viet Nam. Hanoi: UNICEF.
Uno, D., Uchino, B. N., and Smith, T. W. (2002). Relationship quality moderates the effect of social support given by close friends on cardiovascular reactivity in women. Int. J. Behav. Med. 9, 243–262. doi: 10.1207/S15327558IJBM0903_06
Van Leeuwen, M., Husson, O., Alberti, P., Arraras, J. I., Chinot, O. L., Costantini, A., et al. (2018). Understanding the quality of life (QOL) issues in survivors of cancer: Towards the development of an EORTC QOL cancer survivorship questionnaire. Health Qual. Life Outcomes 16, 1–15. doi: 10.1186/s12955-018-0920-0
Van Nguyen, H., Khuong, L. Q., Nguyen, A. T., Nguyen, A. L. T., Nguyen, C. T., Nguyen, H. T. T., et al. (2020). Changes in, and predictors of, quality of life among patients with unstable angina after percutaneous coronary intervention. J. Eval. Clin. Pract. doi: 10.1111/jep.13416
Vassilev, I., Rogers, A., Blickem, C., Brooks, H., Kapadia, D., Kennedy, A., et al. (2013). Social networks, the ‘work’and work force of chronic illness self-management: A survey analysis of personal communities. PLoS One 8:e59723. doi: 10.1371/journal.pone.0059723
Veselska, Z., Madarasova Geckova, A., Gajdosova, B., Orosova, O., van Dijk, J. P., and Reijneveld, S. A. (2010). Socio-economic differences in self-esteem of adolescents influenced by personality, mental health and social support. Eur. J. Public Health 20, 647–652. doi: 10.1093/eurpub/ckp210
Wang, M., and Hanges, P. J. (2011). Latent class procedures: Applications to organizational research. Organ. Res. Methods 14, 24–31. doi: 10.1177/1094428110383988
Ware, J. E. Jr., and Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36): I. Conceptual framework and item selection. Med Care 30, 473–483. doi: 10.1097/00005650-199206000-00002
Watkins, R., Plant, A., Sang, D., O’Rourke, T., and Gushulak, B. (2000). Development of a vietnamese version of the short form-36 health survey. Asia Pac. J. Public Health 12, 118–123. doi: 10.1177/101053950001200211
Watson, D., Clark, L. A., and Carey, G. (1988). Positive and negative affectivity and their relation to anxiety and depressive disorders. J. Abnorm. Psychol. 97:346. doi: 10.1037/0021-843X.97.3.346
Wegener, D. T., and Petty, R. E. (1994). Mood management across affective states: The hedonic contingency hypothesis. J. Pers. Soc. Psychol. 66:1034. doi: 10.1037/0022-3514.66.6.1034
Weiss, B., Ngo, V. K., Dang, H.-M., Pollack, A., Trung, L. T., Tran, C. V., et al. (2012). A model for sustainable development of child mental health infrastructure in the lmic world: Vietnam as a case example. Int. Perspect. Psychol. 1:63. doi: 10.1037/a0027316
Whooley, M. A., Avins, A. L., Miranda, J., and Browner, W. S. (1997). Case-finding instruments for depression: Two questions are as good as many. J. Gen. Intern. Med. 12, 439–445. doi: 10.1046/j.1525-1497.1997.00076.x
Wongpakaran, T., and Wongpakaran, N. (2012). A comparison of reliability and construct validity between the original and revised versions of the Rosenberg Self-Esteem Scale. Psychiatry Investig. 9, 54–58. doi: 10.4306/pi.2012.9.1.54
Wongpakaran, T., Wongpakaran, N., and Ruktrakul, R. (2011). Reliability and validity of the multidimensional scale of perceived social support (MSPSS): Thai version. Clin. Pract. Epidemiol. Ment. Health 7:161. doi: 10.2174/1745017901107010161
Woo, S. E., Jebb, A. T., Tay, L., and Parrigon, S. (2018). Putting the “person” in the center: Review and synthesis of person-centered approaches and methods in organizational science. Organizational Research Methods 21, 814–845. doi: 10.1177/1094428117752467
World Health Organization (2010). Mental health: Strengthening our response. Geneva: World Health Organization.
Yamazaki, S., Fukuhara, S., and Green, J. (2005). Usefulness of five-item and three-item Mental Health Inventories to screen for depressive symptoms in the general population of Japan. Health Qual. Life Outcomes 3, 1–7. doi: 10.1186/1477-7525-3-48
Zimet, G. (2016). Multidimensional scale of perceived social support (MSPSS) scale items and scoring information. Available online at: https://www.researchgate.net/publication/311534896 (accessed November 8, 2022).
Keywords: mental health, urban population, adults, Latent Profile Analysis, Vietnam
Citation: Nguyen TTP, Nguyen TT, Dam VTA, Vu TTM, Do HT, Vu GT, Tran AQ, Latkin CA, Hall BJ, Ho RCM and Ho CSH (2022) Mental wellbeing among urban young adults in a developing country: A Latent Profile Analysis. Front. Psychol. 13:834957. doi: 10.3389/fpsyg.2022.834957
Received: 14 December 2021; Accepted: 04 August 2022;
Published: 02 September 2022.
Edited by:
Eleni Petkari, Universidad Internacional de La Rioja, SpainReviewed by:
Weili Lu, Rutgers, The State University of New Jersey, United StatesCopyright © 2022 Nguyen, Nguyen, Dam, Vu, Do, Vu, Tran, Latkin, Hall, Ho and Ho. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Thao Thi Phuong Nguyen, bmd1eWVudHBodW9uZ3RoYW83M0BkdXl0YW4uZWR1LnZu
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.