
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 22 February 2022
Sec. Developmental Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.788290
This article is part of the Research Topic Innovations in the Mental Health Applications of interRAI Assessments View all 22 articles
Background: The interRAI 0–3 Early Years was recently developed to support intervention efforts based on the needs of young children and their families. One aspect of child development assessed by the Early Years instrument are motor skills, which are integral for the maturity of cognition, language, social-emotional and other developmental outcomes. Gross motor development, however, is negatively impacted by pre-term birth and low birth weight. For the purpose of known-groups validation, an at-risk sample of preterm children using the interRAI 0–3 Early Years was included to examine correlates of preterm risk and the degree of gross motor delay.
Methods: Participant data included children and families (n = 591) from 17 health agencies in Ontario, Canada. Data were collected as part of a pilot study using the full interRAI 0–3 Early Years assessment. Correlational analyses were used to determine relationships between prenatal risk and preterm birth and bivariate analyses examined successful and failed performance of at-risk children on gross motor items. A Kruskal-Wallis test was used to determine the mean difference in gross motor scores for children born at various weeks gestation.
Results: Correlational analysis indicated that prenatal and perinatal factors such as maternal nicotine use during pregnancy did not have significant influence over gross motor achievement for the full sample, however, gross motor scores were lower for children born pre-term or low birth weight based on bivariate analysis. Gross motor scores decreased from 40 weeks’ gestation (mean rank = 310.77), to moderate to late preterm (mean rank = 258.96), and to very preterm (mean rank = 234.54), however extremely preterm (mean rank = 236.28) performed comparably to very preterm.
Interpretation: The interRAI 0–3 was evaluated to determine its efficacy and report findings which confirm the literature regarding delay in gross motor performance for preterm children. Findings confirm that pre-term and low birth weight children are at greater risk for motor delay via the interRAI 0–3 Early Years gross motor domain.
Children who are born preterm (PT), or low birth weight (LBW) face additional barriers as compared to normal birth weight and full-term children, including risk of chronic developmental (i.e., motor, cognitive, communicative), behavioral, socio-emotional, and psychological difficulties. These children are also more likely to have a diagnosed neurodevelopmental or learning disability as compared to full-term children (Cheadle and Goosby, 2010; Shah et al., 2013; Månsson and Stjernqvist, 2014; Gladstone et al., 2015; Fevang et al., 2016; Johnson et al., 2016). When born LBW or PT, the neonate can be impacted by immediate medical complications such as respiratory distress or intraventricular hemorrhage, and future conditions of diabetes, heart disease and other health conditions (OECD, 2013). In concert, families undergo significant stress due to the additional challenges in financially, physically, and emotionally supporting their child (Cheadle and Goosby, 2010; Hodek et al., 2011; Gerstein and Poehlmann-Tynan, 2015). Preterm birth and low birthweight also impact the longitudinal health and well-being of children and their families, making this an expansive population serviced by hospitals and other treatment facilities in Canada (Lim et al., 2009; Treyvaud et al., 2014).
Children born prior to 37 weeks’ gestation are considered PT, and infants with a birthweight of under 5.5 pounds are identified as LBW regardless of gestational age (World Health Organization et al., 2012; OECD, 2013). Although infant mortality has decreased in many developed countries, the incidence of children born with low birth weight is increasing, with estimates in Canada at 6.3 percent, and late preterm births rising 20% from 1990 to 2006 in the United States (National Center for Health Statistics, 2009; OECD, 2013). Increasingly, more attention has been given to children born late preterm, between the gestational age of 34–36 weeks of pregnancy, due to recently observed disparities in health and developmental outcomes (Raju, 2006; National Center for Health Statistics, 2009; Woythaler et al., 2011; Johnson et al., 2015), however, extremely low birthweight (ELBW, < 1,000 g) or very preterm (VPT, 28–32 weeks) children are still at greatest risk (Mikkola et al., 2005; Cheadle and Goosby, 2010; Gladstone et al., 2015; Fevang et al., 2016). Internationally, the prevalence of preterm births falls around 10–11 percent, with LBW and PT more common in developing countries (Beck et al., 2010; Blencowe et al., 2012).
Preventable conditions such as poor maternal mental and physical health, maternal smoking or use of toxic substances, mothers’ age at birth, and inadequate prenatal care provide some explanation for the cause of this condition (Bandstra et al., 2010; World Health Organization et al., 2012; Finnegan, 2013; Bouras et al., 2015). A common maternal health complication is gestational diabetes during pregnancy. Type 2 diabetes as diagnosed at or before 26 weeks’ gestation was found to be a leading risk for the later diagnosis of Autism Spectrum Disorder (ASD), while controlling for several other common predictors such as maternal smoking, body mass index and socio-economic status (Xiang et al., 2015). Maternal age during pregnancy has also been found to predict low birth weight and preterm birth, in addition to elective caesarian surgery, and post-health outcomes for the mother (Oakley et al., 2016). Prenatal exposure to substances such as illicit drugs and alcohol, are responsible for health and developmental problems in childhood and adolescence and can lead to increased likelihood of preterm birth (Bandstra et al., 2010; Finnegan, 2013; O’Keeffe et al., 2014). Finally, maternal stress in utero is linked to low birth weight or preterm birth, however this evidence has not been conclusive when examining stress hormones (Nkansah-Amankra et al., 2010; Kramer et al., 2013; Romero-Gonzalez et al., 2018).
Non-maternal characteristics of preterm birth include being a product of multiple birth, and time spent in a neonatal intensive care unit (NICU). Many preterm or low birth weight children are likely to have spent time in a NICU, impacting the development of sensory systems and ultimately affecting later outcomes in language, cognition and motor areas (Subedi et al., 2017; Vandormael et al., 2019). In one study, preterm children were assessed at multiple time points from 9 months of age into kindergarten, and authors found that the extent of preterm birth as measured by gestational age no longer predicted child outcomes, but rather, the increased length of stay in NICU predicted milestone achievement more substantially (Subedi et al., 2017). Due to any number of maternal and non-maternal issues, children born preterm or low birth weight have broad deficits impacting their development.
Researchers have been examining the continued effects of PT and LBW, including a number of health and developmental issues that are present prior to and beyond kindergarten. Major areas of research revolve around the social competence and behavioral presentation of children born PT or LBW, as well as their cognitive development and academic performance in later life.
Children born PT and LBW display greater dysfunctional behavior, reduced social competence, and a wide range of psychosocial concerns as compared to their full term and normal-birth-weight peers (Jones et al., 2013; Fevang et al., 2016). In a meta-analysis of recent literature, authors found that young children born with severe levels of PT or LBW struggled with poor emotional regulation, social skills, and had more attentional problems as compared to full term children, which predicted future dysfunctional behavior into school age, regardless of cognitive performance (Arpi and Ferrari, 2013). LBW and preterm birth also lead to high levels of maternal stress and burdens in child-parent interactions, potentially impacting the behavioral outcomes of these children (Yates et al., 2010; Woythaler et al., 2011; Poulsen et al., 2013; Ritter et al., 2013; Gerstein and Poehlmann-Tynan, 2015; Fevang et al., 2016; Gerstein et al., 2017). Executive functioning is significantly correlated with childhood social competence, with impairments in executive function prevalent amongst PT and LBW children, particularly childhood inhibitory control (Jones et al., 2013; Ritter et al., 2013; Alduncin et al., 2014).
Children with severe low birth weight and very preterm birth who demonstrate an early delay in executive functioning, may also display cognitive impairment beyond adolescence and into adulthood (Ritter et al., 2013; Eryigit Madzwamuse et al., 2015). It has also been observed that late and moderately preterm children demonstrate significant delays in cognitive function as well (Johnson et al., 2015). In the early years, low birth weight and preterm children demonstrate significantly lower motor, communication and cognitive skills as compared to full-term children (Månsson and Stjernqvist, 2014; Peyton et al., 2018). Even the early abilities of infants to use gestures and other forms of receptive language is affected by these vulnerabilities, which tends to create conditions for future identification of learning disabilities in the school setting (Barre et al., 2011; Johnson et al., 2016; Stolt et al., 2016). Likewise, childhood motor development, often seen as partly responsible for early cognitive function, is negatively impacted by pre-term birth or low birth weight, regardless of diagnosis of physical disability (Van Hus et al., 2013; Sansavini et al., 2014). It is this coordinated process of tuning the gross and fine motor systems that prepares children for more complex tasks in later childhood. Motor skills are crucial in determining independence of children on such tasks as dressing, feeding, hygiene-related activities, as well as on oral and written academic tasks in school settings (Houwen et al., 2016; MacDonald et al., 2016). Children across all levels of severity are at risk for achieving lower IQ scores, more likely to receive placement in special education, as well as decreased academic scores across reading, writing and mathematics as compared to normal-birthweight children (Poulsen et al., 2013; Basten et al., 2015). Even while controlling for the effects of family socio-economic status, for instance, the poor educational performance of preterm children can lead to future decreases in educational attainment later in life, and similarly, less well-paying positions of employment (Basten et al., 2015).
The early intervention literature pertaining to preterm and low birth weight children is scarce and often immaterial (see Johnson (2009), Evans et al. (2017)), however, the early effects of LBW and PT birth on infant and toddler development should be explored in order to enhance early intervention efforts.
With early intervention, it is also crucial to use strong measures of infant and toddler development that pertain to the unique needs of low birthweight and preterm children across specific developmental domains. Few recent studies have evaluated currently used infant and toddler assessments of developmental milestones (see Greene et al. (2012), Sansavini et al. (2014), Lefebvre et al. (2016), Agarwal et al. (2017)). Commonly administered instruments have also been criticized for inaccurate cut offs amongst very preterm or low birth weight children (such as by overestimating motor impairment), as well as unexplained variance in predicting future motor function and classification instability over time (see Luttikhuizen dos Santos et al. (2013), Lobo et al. (2014), Duncan et al. (2015)). In a recent meta-analysis investigating the predictive capacity of future cognitive outcomes for preterm and low birth weight children, common early childhood assessments such as the Bayley Scales of Infant Development, had greater specificity overall, but sensitivity was typically lower when examining future outcomes (Wong et al., 2016). Wong et al. (2016) recommended that test developers examine more closely the predictive accuracy of their screens, and link to consistent follow up assessment in order to increase the odds of detecting later delay. However, others have discovered findings that are strongly predictive of determining developmental delay amongst preterm and low birth weight infants (Agarwal et al., 2017). The accuracy of tests is also important to help determine resource allocation. The resources needed to service this population in Canada ranges based on birthweight and preterm birth, with the cost growing substantially higher than for children born full term and normal birthweight (Lim et al., 2009). For instance, those who are born in the range of 1,000–1,499 grams, cost an average of $50,000 as newborns, and for those born preterm at any gestational age, costing $9,233 and up to $84,235 when extremely preterm (Lim et al., 2009). Thus, for the purposes of early intervention, it is crucial to determine the immediate consequences of preterm and low birth weight newborns by evaluating commonly administered screening and assessment tools for this population.
interRAI is a non-profit conglomerate of researchers from around the world, who develop assessment systems to target the needs of individuals across the lifespan. The child and youth suite of assessments includes the interRAI 0–3 Early Years (Stewart et al., 2017), which has been developed to identify the overall developmental needs of young children between 0 and 47 months of age, as well as their family. The interRAI 0–3 captures more than 650 items that seek insight on ecological risk factors, family dynamics, medical and mental health information, as well as all areas of early development. It provides information specific to early identification and intervention (e.g., preterm birth, low birthweight, caregiver distress, emotion dysregulation). Items include multilevel assessment of frequency and intensity (e.g., Present recently but not exhibited in last 3 nights/days), performance and capacity of tasks (e.g., Extensive assistance- help throughout task, but performs 50% or more of task on own), and age-related items indicating presence or non-presence of developmental achievement (e.g., Grasping- picks up tiny objects with fingertips (e.g., food crumbs, peas)). Items are carried forward from the child and youth suite of instruments as applicable, and new items undergo a rigorous approval process by an Instrument and Systems Development (ISD) committee before pilot and publication. The interRAI 0–3 Early Years is currently in pilot testing, evaluating the efficacy of its items and scales before final approval for submission to publication can be given.
This newly established instrument, however, has yet to explore the development of preterm children under the age of four in the motor domain. In the present study, data from the interRAI 0–3 Early Years was used to explore the motor findings of children at risk due to issues such as preterm birth, or low birthweight, seeking to understand how children between 6 and 47 months perform on gross motor outcomes based on extent of prematurity and other risk factors.
Participants completed the interRAI 0–3 Early Years as a part of a pilot study across 17 sites which provide developmental or mental health services in Ontario, Canada. This convenience sample included 591 children between the ages of 6–47 months of age (M = 31.6, SD = 12.71), with a majority of male participants (62.4%; see Table 1). As many as 20.3% (n = 120) identified as preterm (< 37 weeks) by the assessor during intake. This item utilized a binary response item to record for preterm birth based on caregiver response or an examination of medical documentation. More children were identified as preterm based on a separate item on the 0–3 Early Years, indicated by the number of weeks premature. This item indicated that 24.3% of children had a gestational age under 39 weeks. The majority were considered moderate to late preterm (16.4%), and only 11.2% of the sample was considered low birthweight. Much of the sample had been placed in some level of neonatal care after birth (43.1%), and 28.3% of mothers had health complications during the pregnancy or delivery. The most common health complications included gestational diabetes, hypertensive disorders, and fetal distress.
The interRAI 0–3 Early Years is a needs-based integrated assessment-to-intervention system that amalgamates social, psychiatric, medical, functional, psychological, and environmental constructs to evaluate and intervene based on the needs of young children and their families. Upon intake within child and family agencies across Ontario, assessors who received training on the interRAI 0–3 began to collect data with the child and family using the above measures. The interRAI 0–3 training included an overview of the form, manual, coding procedures, and practice using case studies. Pediatricians, psychiatrists, psychologists, infant therapists, early childhood educators, child and youth workers, child life specialists, and early intervention teams administered the interRAI 0–3. Assessors were required to have a diploma or degree in early child development, at least 2 years of work experience with young children, and have received the comprehensive interRAI 0–3 2-day assessor training program. The interRAI 0–3 uses a clinician-rated semi-structured interview format and requires approximately 45–90 min to complete depending on case complexity, age of the child and assessor experience. Initial assessments may require additional time due to the novelty of the case. Clinicians were given explicit instruction to use information from multiple sources such as medical documentation where approved, as well as information from the caregivers, extended family, childcare providers or other individuals relevant to the context of the family. If clinicians felt that there was incongruent information based on the report from multiple sources, clinicians were asked to make observational judgments to validate their decisions where possible. The focus of the interRAI 0–3 Early Years measure was the Gross Motor domain, which is a multi-item scale that assesses the developmental milestones achieved in multiple age intervals including early mobility in infancy and the progression of climbing and running as the child matures in age. The presence of these milestones is determined using a 2-point coding structure (0 = No to 1 = Yes), which is summed to provide a composite score based on the age range completed.
To test for gross motor performance, corrected age was used for children above 24 months by subtracting weeks premature by chronological age, indicating the child’s corrected age at assessment. For children under 24 months, gross motor outcomes were not adjusted based on corrected age.
The current study initially sought to examine the correlations between risk items (i.e., premature birth, low birthweight, neonatal intensive care, maternal nicotine and alcohol use, and maternal health problems) and performance on gross motor milestones as a means to discover convergence between risk items and associations with gross motor performance. Next, bivariate associations were used to discover the successful and failed performance of at risk and no risk children on the interRAI 0–3 gross motor domain. Initially, contingency tables and chi square were calculated for predictors of developmental outcomes for premature children based on the literature. Proposed variables that contribute to poor developmental outcomes included maternal age, premature birth, birthweight, maternal health problems, stay in NICU, as well as maternal nicotine and alcohol use. Though important to this research, variables not included in the analysis were assistive reproductive technology used to achieve pregnancy, and child is a product of multiple birth, as this subsample of participants was not substantive. This dataset includes some missing data, which was unreported or not inputted into beta software by assessors.
Finally, an independent-samples Kruskal-Wallis test was conducted to examine the gross motor outcomes of children born extremely preterm (at or below 28 weeks’ gestation), very preterm (at or below 32 weeks’ gestation), moderate to late preterm (33–39 weeks’ gestation) and at 40 weeks’ gestation or having no reported preterm birth. A non-parametric test was chosen as a test of normality revealed that homogeneity of variances could not be assumed. Box-plots were used to determine differences in scores across levels of prematurity, a means test was carried out and post hoc tests were used to determine levels of significance among gross motor scores between categories.
Initially, Pearson-product moment correlations were run to seek evidence between performance on gross motor items and variables that place children at risk of poor performance (see Table 2). Items from the interRAI 0–3 that were used included preterm birth and low birthweight, stay in a NICU, maternal health problems during pregnancy and maternal nicotine use during pregnancy. Interestingly, the findings showed significant negative correlations between performance on gross motor and all risk-oriented items except for nicotine use during pregnancy, however, the strength of relationship between other items was weak. While the direction of the relationship is not clear, either an improvement in performance on gross motor leads to decreased risk, or an increase in risk leads to poor performance on gross motor items. Correlations between risk-items were also sought, indicating convergence between constructs that are commonly known to load together. Children with any known risk, such as preterm birth, was found to relate to other risk factors such as receipt of neonatal intensive care.
Using items from the interRAI 0–3, common predictive risk factors were chosen to explore associations with developmental outcomes on the gross motor domain as a stronger measure of relationships between variables (see Table 3). The findings suggest that children with no identified risks were more likely to achieve gross motor milestones at a higher rate than those with identified risk factors. The gross motor findings indicated that within the at-risk group, most children identified as being preterm, low birthweight or having other risks for developmental delay were found to succeed or fail milestones nearly equally. The risk estimates for each variable, however, show that passing as compared to failing gross motor milestones for preterm birth, low birthweight, maternal health issues during pregnancy, or being in neonatal intensive care does not increase the risk estimate to above 1. Conversely, maternal nicotine use (1.27), and alcohol use during pregnancy (5.51) did lead to an increased risk estimate, with the group that failed gross motor milestones (1.16; 3.62), respectively, showing a risk estimate above 1.
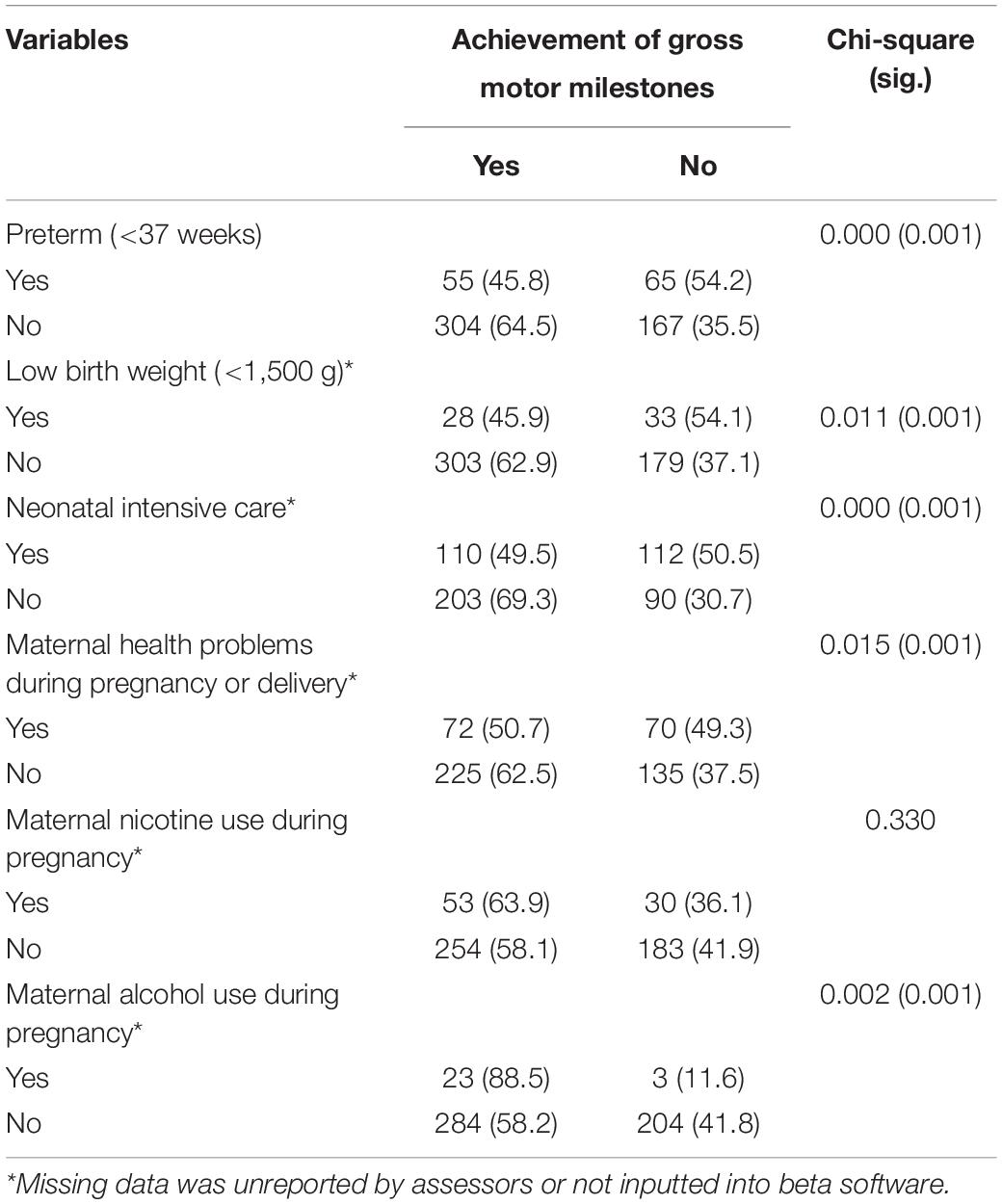
Table 3. Bivariate association between achievement of gross motor milestones and predictors for children 6–47 months (n = 591).
Initially, the number of weeks a child was born prematurely was converted into categories of extremely premature, very premature, moderate to late premature and 40 weeks’ gestation. Children who were at least 2 years of age and were born prematurely, would be asked to perform a set of items within their corrected age range. For children under 24 months, gross motor items were not adjusted based on corrected age. These variables were then examined for normal distribution according to the Shapiro-Wilk’s test of normality. The results indicate that although the very preterm category was considered normally distributed, all other levels of prematurity did not meet the normality assumption.
Given the low and unequal sample sizes within each category, a non-parametric test was selected in order to reduce type I error (Kruskal and Wallis, 1952). An independent-samples Kuskal-Wallis Test was used, and initial examination of the boxplot indicated that distributions of gross motor scores were different for each level of premature birth. The distributions of gross motor scores were significantly different across categories of prematurity [H(3) = 15.520, p = 0.001], thus the null hypothesis was rejected. Gross motor scores decreased from 40 weeks’ gestation (mean rank = 310.77), to moderate to late preterm (mean rank = 258.96), and to very preterm (mean rank = 234.54), however extremely preterm (mean rank = 236.28) performed comparably to very preterm.
Given the level of significance, pairwise comparisons using Bonferroni correction were executed. Accepting statistical significance based on adjusted p-values at the p < 0.05 level revealed differences between gross motor scores for two categories. Post hoc analysis showed statistical significance between gross motor scores for very preterm birth and 40 weeks’ gestation (p = 0.04), and between moderate to late preterm and 40 weeks’ gestation (p = 0.04), but not between other groups.
The present study examined relationships between perinatal and prenatal risk for gross motor delay, including preterm birth and low birthweight, stay in NICU, maternal health problems as well as nicotine and alcohol use during pregnancy. Next, the mean gross motor scores of children were compared based on levels of preterm birth.
Initially, a correlation matrix was generated to examine the relationship between risk-items on the interRAI 0–3 and their association with pass/fail performance of gross motor milestones. The results indicated that items such as preterm birth and low birthweight, time in a NICU, and maternal health problems during pregnancy or delivery are all positively and significantly correlated with one another, however, maternal nicotine and alcohol use were not correlated with these other risk factors, rather correlated with one another. An increase in any one of the correlated risk factors indicate that the others will also linearly increase. This is an important finding, as it shows that multiple interRAI 0–3 items that link to preterm birth show convergence, however, this also increases the likelihood of multicollinearity in any logistic model. Additionally, these items all show a negative relationship with pass/fail outcomes from the gross motor domain, which is a common finding in the literature for preterm children. Conversely, alcohol use during pregnancy showed a positive statistically significant relationship, which is likely due to limited sample size (n = 26). Moreover, nicotine use was also scarcely reported amongst maternal participants (n = 83), finding no association to PT, or LBW. Additionally, the relationship between poor performance on gross motor outcomes was expected to be stronger for the at-risk population given the literature which shows that prenatal and perinatal factors have significant influence over gross motor achievement (Ghassabian et al., 2016a,b; Yaari et al., 2018). The present study found that the strength of correlations with gross motor outcomes ranged between –0.108 for maternal health problems during pregnancy and –0.200 for stay in a NICU. Finally, the risk estimate seemed to be highest for variables pertaining to alcohol and nicotine use, more than other perinatal and prenatal factors.
Of the risk factors discussed in this study, of particular interest was the necessity of neonatal intensive care. Much of the current literature shows that children born preterm require care by specialists in a NICU, and that a longer period of time spent in this type of care forecasts poorer developmental outcomes (Subedi et al., 2017). Staying in a NICU is also hypothesized to impact the infant beyond the effects of their prematurity or low birthweight by having increased medical interventions and reducing holding behavior (Pineda et al., 2018). An increase in holding the child leads to stronger tuning of the reflexes based on parent interventions (Pineda et al., 2018). There is evidence to suggest that neuromuscular development can be delayed due to length of stay in a NICU (Zuccarini et al., 2016), thus future research should further investigate this relationship using data from the interRAI 0–3 Early Years instrument.
The interRAI 0–3 adjusts for prematurity within all developmental domains for children under 24 months, which also may be responsible for the weak correlation with gross motor performance. Several assessments that measure child development correct for age by subtracting the number of weeks premature, by the child’s chronological age (see Bayley (2006), Bricker and Squires (2009)). We employed the same process to ensure that we capture accurately, the gross motor development of preterm children, as they are still biologically maturing. However, this has been criticized for underserving populations of children still considered at-risk for delay, noting that intervention services may be offered to less children who could still benefit from access (Yaari et al., 2018). Thus, it has been recommended that chronological and corrected age be considered for intervention purposes (Yaari et al., 2018). Future research using the interRAI 0–3 should examine participants scores within their age range without correcting for prematurity to find any measurable differences.
Bivariate associations with risk factors including preterm birth, low birthweight, time spent in a NICU and maternal health problems during pregnancy. These risk factors were found to be associated with higher risk of failure on gross motor domain items from the interRAI 0–3 by comparing at-risk children to the rest of the study population. For instance, 45.8% of children born preterm (< 37 weeks’ gestation), achieved motor outcomes as compared to 64.5% of children who were not born preterm. Similarly, children born with low birthweight achieved gross motor outcomes 45.9% of the time, with 62.9% of full-term children achieving milestones for their corrected age. This further reflects findings in the literature that suggest children who are considered preterm or low birthweight function below full term peers on motor outcomes (Sansavini et al., 2014; Lean et al., 2018; Yaari et al., 2018).
Within the group of preterm children in this study, more participants were likely to fail motor milestones. Specifically, of the children born preterm, 45.8% were able to achieve gross motor milestones, and 54.2% did not, and nearly identical findings for were discovered for the passing (45.9%) and failing (54.1%) low birthweight group. Yet, amongst the full-term cohort 64.5% of children achieved gross motor milestones for their age, and only 35.5% failed such milestones. Studies have found poorer results in very preterm and low birthweight children across all developmental domains (Lean et al., 2018; Yaari et al., 2018), thus future research should investigate associations between prenatal and perinatal risk factors using the extent of preterm birth. It may be that for children born pre-term, more immediate intervention services were given, leading to an indiscriminate difference between the participants who achieved or did not achieve particular milestones. Another important consideration pertains to the male predominance in this study (62.4%). Some authors suggest that evaluation of motor outcomes should include age and sex-specific assessment of motor skills during the early years given differences in fundamental motor skills (Kokštejn et al., 2017).
Lastly, the Kruskal-Wallis test was used to determine the mean difference in gross motor scores for children considered 40 weeks’ gestation, moderate to late preterm, very preterm and extremely preterm. Distributions amongst the groups varied at a statistically significant level, [H(3) = 15.520, p = 0.001], indicating that level of preterm birth effects the gross motor abilities of children, based on corrected age. The mean rank of 40 weeks’ gestation was highest, then moderate to late preterm, and very preterm, however, extremely preterm children performed slightly better, but not statistically superior to the very preterm category. Research suggests that the most at-risk groups (i.e., very preterm) tend to do most poorly on functional assessments, finding a reduced effect with children who are less severe (Schonhaut et al., 2013). It is posited that the small number of participants in the extremely preterm group (n = 16) were not sufficient to capture changes in the distribution. The only groups that were statistically significantly different in their achievement of gross motor milestones were the moderate to late preterm and the very preterm groups as compared to children considered 40 week’s gestation.
It must also be considered a limitation that the moderate to late preterm week’s gestation included cases of children between 33 and 39 weeks as opposed to 32–37 weeks in order to reduce case overlap and capture all children born before 40 weeks. In future, the moderate to late preterm group could be parsed out into early term and late preterm as sample size increases. The sample size of each group should be considered a limitation to interpretation of these findings. With an increased sample size, it would be interesting to examine preterm gross motor scores in infants as compared to older children in our sample, as there are early neuromuscular differences which lead to poor object manipulation at 6 months, and later motor difficulties in children at the age of 2 years (Zuccarini et al., 2016; Allotey et al., 2018).
The present study findings confirm that very preterm children perform poorly on gross motor outcomes as compared to full-term children, however, that late and moderate preterm birth are still suggestive of concern. Recent studies have been done to explore late preterm children, noticing significant differences in achievement across a broad range of milestones both early in childhood and later into school-age (Raju, 2006; National Center for Health Statistics, 2009; Woythaler et al., 2011; Johnson et al., 2015). The findings from this study reflect much of what is found in the literature and confirm the presence of concern for this population using data collected from interRAI 0–3. This helps to substantiate the use of the interRAI 0–3 as an instrument that accounts for levels of prematurity and prenatal and perinatal risk. Further research should explore predictive models based on maternal and post-term risk in order to replicate past studies and confirm the use of the interRAI 0–3 as predicting poorer developmental outcomes for this population. Future work should also consist of measuring the impact of preterm birth on different age cohorts in order to explore the longitudinal effects on gross motor development. Preterm birth and skill development in domains such as language, executive function and social-emotional areas should also be explored in order to replicate findings on preterm performance.
Following this, it would be interesting to explore different age groupings to see what is predictive for individual age ranges. This has been done in other research to counter the issue of developmental change, and more closely examine psychometric properties that appear to improve with the age at assessment (Schonhaut et al., 2013). The study population used for analysis also amalgamated new intake cases and those that may have been in a clinical program receiving early intervention. These cases could not be separated because this pilot study was the first of its kind to evaluate the interRAI 0–3, thus all cases in the database were considered an initial assessment. Future work will have the capability to separate first assessment from routine or discharge assessments. Finally, children who were considered preterm or low birthweight may have experienced other medical comorbidities or multiple diagnoses that impacted the association with these items. With increased data collection efforts, supplementary research into the role that comorbid diagnoses have on the preterm or low birthweight population could expand the impact of the interRAI 0–3.
Children who are preterm and low birthweight have been found to exhibit more delayed developmental trajectories than child who are born full-term and normal birthweight. With the incidence of low birth weight and late preterm birth rising, increased emphasis should be placed on investigating this vulnerable population. The interRAI 0–3 was examined for associations between risk factors for delay and levels of preterm birth on gross motor outcomes, which was an integral part of test development efforts.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study involved human participants and was approved by the University of Western Ontario Research Ethics Board (REB # 108024). The patients/participants provided their written informed consent to participate in this study.
JI composed the literature review, developed the analytical strategy, and performed the statistical analysis. SS provided intellectual direction, provided critical feedback to the manuscript, and was involved in the writing and reviewing of the final manuscript. Both authors contributed to the article and approved the submitted version.
This study was supported by a contribution from the London Community Foundation Community Vitality Grant.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to sincerely thank the children, youth, and their families, along with the service providers within the agencies for their participation in the research.
Agarwal, P. K., Shi, L., Daniel, L. M., Yang, P. H., Khoo, P. C., Quek, B. H., et al. (2017). Prospective evaluation of the ages and stages questionnaire 3rd edition in very-low-birthweight infants. Dev. Med. Child Neurol. 59, 484–489. doi: 10.1111/dmcn.13307
Alduncin, N., Huffman, L. C., Feldman, H. M., and Loe, I. M. (2014). Executive function is associated with social competence in preschool-aged children born preterm or full term. Early Hum. Dev. 90:299. doi: 10.1016/j.earlhumdev.2014.02.011
Allotey, J., Zamora, J., Cheong-See, F., Kalidindi, M., Arroyo-Manzano, D., Asztalos, E., et al. (2018). Cognitive, motor, behavioural and academic performances of children born preterm: a meta-analysis and systematic review involving 64 061 children. BJOG 125, 16–25. doi: 10.1111/1471-0528.14832
Arpi, E., and Ferrari, F. (2013). Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev. Med. Child Neurol. 55, 788–796. doi: 10.1111/dmcn.12142
Bandstra, E. S., Morrow, C. E., Mansoor, E., and Accornero, V. H. (2010). Prenatal drug exposure: infant and toddler outcomes. J. Addict. Dis. 29, 245–258. doi: 10.1080/10550881003684871
Barre, N., Morgan, A., Doyle, L. W., and Anderson, P. J. (2011). Language abilities in children who were very preterm and/or very low birth weight: a meta-analysis. J. Pediatr. 158, 766–774.
Basten, M., Jaekel, J., Johnson, S., Gilmore, C., and Wolke, D. (2015). Preterm birth and adult wealth: mathematics skills count. Psychol. Sci. 26, 1608–1619. doi: 10.1177/0956797615596230
Bayley, N. (2006). Bayley Scales of Infant and Toddler Development-Third Edition. San Antonio: Harcourt Assessments, Inc.
Beck, S., Wojdyla, D., Say, L., Betran, A. P., Merialdi, M., Requejo, J. H., et al. (2010). The worldwide incidence of pre-term birth: a systematic review of maternal mortality and morbidity. Bull. WHO 88, 31–38. doi: 10.2471/BLT.08.062554
Blencowe, H., Cousens, S., Oestergaard, M. Z., Chou, D., Moller, A. B., Narwal, R., et al. (2012). National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet 379, 2162–2172.
Bouras, G., Theofanopoulou, N., Mexi-Bourna, P., Poulios, A., Michopoulos, I., Tassiopoulou, I., et al. (2015). Preterm birth and maternal psychological health. J. Health Psychol. 20, 1388–1396. doi: 10.1177/1359105313512353
Bricker, D., and Squires, J. (2009). Ages & Stages Questionnaires, Third Edition (ASQ-3): Technical Report. Baltimore: Brookes Publishing Company.
Cheadle, J. E., and Goosby, B. J. (2010). Birth weight, cognitive development, and life chances: a comparison of siblings from childhood into early adulthood. Soc. Sci. Res. 39, 570–584. doi: 10.1016/j.ssresearch.2010.03.003
Duncan, A. F., Bann, C., Boatman, C., Hintz, S. R., Vaucher, Y. E., Vohr, B. R., et al. (2015). Do currently recommended bayley-III cutoffs overestimate motor impairment in infants born <27 weeks gestation? J. Perinatol. 35:516. doi: 10.1038/jp.2014.243
Eryigit Madzwamuse, S., Baumann, N., Jaekel, J., Bartmann, P., and Wolke, D. (2015). Neuro-cognitive performance of very preterm or very low birth weight adults at 26 years. J. Child Psychol. Psychiatry 56, 857–864. doi: 10.1111/jcpp.12358
Evans, T., Boyd, R. N., Colditz, P., Sanders, M., and Whittingham, K. (2017). Mother-very preterm infant relationship quality: RCT of baby triple P. J. Child Fam. Stud. 26, 284–295. doi: 10.1007/s10826-016-0555-x
Fevang, S. K. E., Hysing, M., Markestad, T., and Sommerfelt, K. (2016). Mental health in children born extremely preterm without severe neurodevelopmental disabilities. Pediatrics 137:e20153002–e20153002. doi: 10.1542/peds.2015-3002
Finnegan, L. (2013). Substance Abuse in Canada: Licit and Illicit Drug Use During Pregnancy: Maternal, Neonatal and Early Childhood Consequences. Ottawa: Canadian Centre on Substance Abuse.
Gerstein, E. D., and Poehlmann-Tynan, J. (2015). Transactional Processes in Children born Preterm: influences of Mother-Child Interactions and Parenting Stress. J. Fam. Psychol. 29, 777–787. doi: 10.1037/fam0000119
Gerstein, E. D., Woodman, A. C., Burnson, C., Cheng, E. R., and Poehlmann-Tynan, J. (2017). Trajectories of externalizing and internalizing behaviors in preterm children admitted to a neonatal intensive care unit. J. Pediatr. 187, 111–118. doi: 10.1016/j.jpeds.2017.04.047
Ghassabian, A., Sundaram, R., Bell, E., Bello, S. C., Kus, C., and Yeung, E. (2016a). Gross motor milestones and subsequent development. Pediatrics 138:e20154372. doi: 10.1542/peds.2015-4372
Ghassabian, A., Sundaram, R., Wylie, A., Bell, E., Bello, S. C., and Yeung, E. (2016b). Maternal medical conditions during pregnancy and gross motor development up to age 24 months in the upstate KIDS study. Dev. Med. Child Neurol. 58, 728–734. doi: 10.1111/dmcn.12947
Gladstone, M., Oliver, C., and Van den Broek, N. (2015). Survival, Morbidity, Growth and Developmental Delay for Babies Born Preterm in Low and Middle Income Countries – A Systematic Review of Outcomes Measured. PLoS One 10:e0120566. doi: 10.1371/journal.pone.0120566
Greene, M. M., Patra, K., Nelson, M. N., and Silvestri, J. M. (2012). Evaluating preterm infants with the bayley-III: patterns and correlates of development. Res. Dev. Disabil. 33, 1948–1956. doi: 10.1016/j.ridd.2012.05.024
Hodek, J., von der Schulenburg, J., and Mittendorf, T. (2011). Measuring economic consequences of preterm birth - methodological recommendations for the evaluation of personal burden on children and their caregivers. Health Econ. Rev. 1:6. doi: 10.1186/2191-1991-1-6
Houwen, S., Visser, L., van der Putten, A., and Vlaskamp, C. (2016). The interrelationships between motor, cognitive, and language development in children with and without intellectual and developmental disabilities. Res. Dev. Disabil. 53, 19–31. doi: 10.1016/j.ridd.2016.01.012
Johnson, S. (2009). Randomized trial of a parenting intervention for very preterm infants: outcome at 2 years. J. Pediatr. 155, 488.e–494.e. doi: 10.1016/j.jpeds.2009.04.013
Johnson, S., Evans, T. A., Draper, E. S., Field, D. J., Manktelow, B. N., Marlow, N., et al. (2015). Neurodevelopmental outcomes following late and moderate prematurity: a population-based cohort study. Arch. Dis. Child. 100, F301–F308. doi: 10.1136/archdischild-2014-307684
Johnson, S., Strauss, V., Gilmore, C., Jaekel, J., Marlow, N., and Wolke, D. (2016). Learning disabilities among extremely preterm children without neurosensory impairment: comorbidity, neuropsychological profiles and scholastic outcomes. Early Hum. Dev. 103, 69–75. doi: 10.1016/j.earlhumdev.2016.07.009
Jones, K. M., Champion, P. R., and Woodward, L. J. (2013). Social competence of preschool children born very preterm. Early Hum. Dev. 89, 795–802. doi: 10.1016/j.earlhumdev.2013.06.008
Kokštejn, J., Musálek, M., and Tufano, J. J. (2017). Are sex differences in fundamental motor skills uniform throughout the entire preschool period? PLoS One 12:e0176556. doi: 10.1371/journal.pone.0176556
Kramer, M. S., Lydon, J., Goulet, L., Kahn, S., Dahhou, M., Platt, R. W., et al. (2013). Maternal Stress/Distress, hormonal pathways and spontaneous preterm birth. Paediatr. Perinat. Epidemiol. 27, 237–246. doi: 10.1111/ppe.12042
Kruskal, W. H., and Wallis, W. A. (1952). Use of ranks in one-criterion variance analysis. J. Am. Stat. Assoc. 47, 583–621.
Lean, R. E., Paul, R. A., Smyser, C. D., Smyser, T. A., and Rogers, C. E. (2018). Social adversity and cognitive, language, and motor development of very preterm children from 2 to 5 years of age. J. Pediatr. 203, 177–184. doi: 10.1016/j.jpeds.2018.07.110
Lefebvre, F., Gagnon, M., Luu, T. M., Lupien, G., and Dorval, V. (2016). In extremely preterm infants, do the movement assessment of infants and the alberta infant motor scale predict 18-month outcomes using the bayley-III? Early Hum. Dev. 94, 13–17. doi: 10.1016/j.earlhumdev.2016.01.012
Lim, G., Tracey, J., Boom, N., Karmakar, S., Wang, J., Berthelot, J., et al. (2009). CIHI survey: hospital costs for preterm and small-for-gestational age babies in Canada. Healthc. Q. 12, 20–24. doi: 10.12927/hcq.2013.21121
Lobo, M. A., Paul, D. A., Mackley, A., Maher, J., and Galloway, J. C. (2014). Instability of delay classification and determination of early intervention eligibility in the first two years of life. Res. Dev. Disabil. 35, 117–126. doi: 10.1016/j.ridd.2013.10.017
Luttikhuizen dos Santos, E. S., de Kieviet, J. F., Königs, M., van Elburg, R. M., and Oosterlaan, J. (2013). Predictive value of the bayley scales of infant development on development of very preterm/very low birth weight children: a meta-analysis. Early Hum. Dev. 89, 487–496. doi: 10.1016/j.earlhumdev.2013.03.008
Månsson, J., and Stjernqvist, K. (2014). Children born extremely preterm show significant lower cognitive, language and motor function levels compared with children born at term, as measured by the Bayley-III at 2.5 years. Acta Paediatr. 103, 504–511. doi: 10.1111/apa.12585
MacDonald, M., Lipscomb, S., McClelland, M. M., Duncan, R., Becker, D., Anderson, K., et al. (2016). Relations of preschoolers’ visual-motor and object manipulation skills with executive function and social behavior. Res. Q. Exerc. Sport 87, 396–407.
Mikkola, K., Ritari, N., Tommiska, V., Salokorpi, T., Lehtonen, L., Tammela, O., et al. (2005). Neurodevelopmental outcome at 5 years of age of a national cohort of extremely low birth weight infants who were born in 1996-1997. Pediatrics 116, 1391–1400. doi: 10.1542/peds.2005-0171
National Center for Health Statistics (2009). Born a Bit Too Early: Recent Trends in Late Preterm Births. Centers for Disease Control and Prevention. Available online at: https://www-cdc-gov.proxy1.lib.uwo.ca/nchs/products/databriefs/db24.htm (accessed May 19, 2020).
Nkansah-Amankra, S., Luchok, K. J., Hussey, J. R., Watkins, K., and Liu, X. (2010). Effects of maternal stress on low birth weight and preterm birth outcomes across neighborhoods of south carolina, 2000–2003. Matern. Child Health J. 14, 215–226. doi: 10.1007/s10995-009-0447-4
Oakley, L., Penn, N., Pipi, M., Oteng-Ntim, E., and Doyle, P. (2016). Risk of adverse obstetric and neonatal outcomes by maternal age: quantifying individual and population level risk using routine UK maternity data. PloS One 11:e0164462. doi: 10.1371/journal.pone.0164462
O’Keeffe, L. M., Greene, R. A., and Kearney, P. M. (2014). The effect of moderate gestational alcohol consumption during pregnancy on speech and language outcomes in children: a systematic review. Syst. Rev. 3:1. doi: 10.1186/2046-4053-3-1
Peyton, C., Schreiber, M. D., and Msall, M. E. (2018). The test of infant motor performance at 3 months predicts language, cognitive, and motor outcomes in infants born preterm at 2 years of age. Dev. Med. Child Neurol. 60, 1239–1243. doi: 10.1111/dmcn.13736
Pineda, R., Bender, J., Hall, B., Shabosky, L., Annecca, A., and Smith, J. (2018). Parent participation in the neonatal intensive care unit: predictors and relationships to neurobehavior and developmental outcomes. Early Hum. Dev. 117, 32–38. doi: 10.1016/j.earlhumdev.2017.12.008
Poulsen, G., Wolke, D., Kurinczuk, J. J., Boyle, E. M., Field, D., Alfirevic, Z., et al. (2013). Gestational age and cognitive ability in early childhood: a Population-based cohort study. Paediatr. Perinat. Epidemiol. 27, 371–379. doi: 10.1111/ppe.12058
Raju, T. N. (2006). The problem of late-preterm (near-term) births: a workshop summary. Pediatr. Res. 60, 775–776. doi: 10.1203/01.pdr.0000246074.73342.1e
Ritter, B. C., Nelle, M., Perrig, W., Steinlin, M., and Everts, R. (2013). Executive functions of children born very preterm—deficit or delay? Eur. J. Pediatr. 172, 473–483. doi: 10.1007/s00431-012-1906-2
Romero-Gonzalez, B., Caparros-Gonzalez, R. A., Gonzalez-Perez, R., Delgado-Puertas, P., and Peralta-Ramirez, M. I. (2018). Newborn infants’ hair cortisol levels reflect chronic maternal stress during pregnancy. PloS One 13:e0200279. doi: 10.1371/journal.pone.0200279
Sansavini, A., Pentimonti, J., Justice, L., Guarini, A., Savini, S., Alessandroni, R., et al. (2014). Language, motor and cognitive development of extremely preterm children: modeling individual growth trajectories over the first three years of life. J Commun. Disord. 49:55. doi: 10.1016/j.jcomdis.2014.02.005
Schonhaut, L., Armijo, I., Schönstedt, M., Alvarez, J., and Cordero, M. (2013). Validity of the ages and stages questionnaires in term and preterm infants. Pediatrics 131, e1468–e1474. doi: 10.1542/peds.2012-3313
Shah, P. E., Robbins, N., Coelho, R. B., and Poehlmann, J. (2013). The paradox of prematurity: the behavioral vulnerability of late preterm infants and the cognitive susceptibility of very preterm infants at 36 months post-term. Infant Behav. Dev. 36, 50–62. doi: 10.1016/j.infbeh.2012.11.003
Stewart, S. L., Iantosca, J. M., Klassen, J. A., Cloutier, S. E., Tucker, M., Fisman, S., et al. (2017). interRAI 0-3 Assessment Form and User’s Manual. Version 1. Washington, DC: interRAI.
Stolt, S., Lind, A., Matomäki, J., Haataja, L., Lapinleimu, H., and Lehtonen, L. (2016). Do the early development of gestures and receptive and expressive language predict language skills at 5 in prematurely born very-low-birth-weight children? J. Commun. Disord. 61, 16–28. doi: 10.1016/j.jcomdis.2016.03.002
Subedi, D., DeBoer, M. D., and Scharf, R. J. (2017). Developmental trajectories in children with prolonged NICU stays. Arch. Dis. Child. 102, 29–34. doi: 10.1136/archdischild-2016-310777
Treyvaud, K., Lee, K. J., Doyle, L. W., and Anderson, P. J. (2014). Very preterm birth influences parental mental health and family outcomes seven years after birth. J. Pediatr. 164, 515–521. doi: 10.1016/j.jpeds.2013.11.001
Van Hus, J. W., Jeukens-Visser, M., Koldewijn, K., Geldof, C. J., Kok, J. H., Nollet, F., et al. (2013). Sustained developmental effects of the infant behavioral assessment and intervention program in very low birth weight infants at 5.5 years corrected age. J. Pediatr. 162, 1112–1119. doi: 10.1016/j.jpeds.2012.11.078
Vandormael, C., Schoenhals, L., Hüppi, P. S., Filippa, M., and Borradori Tolsa, C. (2019). Language in preterm born children: atypical development and effects of early interventions on neuroplasticity. Neural Plast. 2019, 6873210–6873270. doi: 10.1155/2019/6873270
Wong, H. S., Santhakumaran, S., Cowan, F. M., Modi, N., and Medicines for Neonates Investigator Group. (2016). Developmental assessments in preterm children: a meta-analysis. Pediatrics 138:e20160251. doi: 10.1542/peds.2016-0251
World Health Organization, March of Dimes, The Partnership for Maternal, Newborn & Child Health, and Save the Children (2012). Born Too Soon: The Global Action Report on Preterm Birth. Geneva: World health organization.
Woythaler, M. A., McCormick, M. C., and Smith, V. C. (2011). Late preterm infants have worse 24-month neurodevelopmental outcomes than term infants. Pediatrics 127, e622–e629. doi: 10.1542/peds.2009-3598
Xiang, A. H., Wang, X., Martinez, M. P., Walthall, J. C., Curry, E. S., Page, K., et al. (2015). Association of maternal diabetes with autism in offspring. JAMA 313, 1425–1434. doi: 10.1001/jama.2015.2707
Yaari, M., Mankuta, D., Harel- Gadassi, A., Friedlander, E., Bar-Oz, B., Eventov-Friedman, S., et al. (2018). Early developmental trajectories of preterm infants. Res. Dev. Disabil. 81, 12–23. doi: 10.1016/j.ridd.2017.10.018
Yates, T. M., Obradoviæ, J., and Egeland, B. (2010). Transactional relations across contextual strain, parenting quality, and early childhood regulation and adaptation in a high-risk sample. Dev. Psychopathol. 22, 539–555. doi: 10.1017/S095457941000026X
Keywords: preterm, low birth weight, interRAI, early years, validation
Citation: Iantosca JAM and Stewart SL (2022) Evaluation of the InterRAI Early Years for Degree of Preterm Birth and Gross Motor Delay. Front. Psychol. 13:788290. doi: 10.3389/fpsyg.2022.788290
Received: 04 October 2021; Accepted: 27 January 2022;
Published: 22 February 2022.
Edited by:
Natacha Akshoomoff, University of California, San Diego, United StatesReviewed by:
Jessie Maxwell, University of New Mexico, United StatesCopyright © 2022 Iantosca and Stewart. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jo Ann M. Iantosca, am8tYW5uLmlhbnRvc2NhQHNlbmVjYWNvbGxlZ2UuY2E=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.