
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 22 April 2022
Sec. Quantitative Psychology and Measurement
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.773447
This article is part of the Research Topic Measurement in Health Psychology View all 24 articles
Social support by healthcare providers has been increasingly investigated during the past decade, but studies have made different choices concerning its measurement. To evaluate how social support from a healthcare provider impacts the perceived quality of care and patient outcomes, reliable and valid instruments capable of measuring specific aspects of the construct are needed. In study 1, we tested the factor structure and the psychometric properties of a new Healthcare Provider Social Support measure (HPSS) for oncology settings. One-hundred-sixty-two patients (89 females; M age = 58.97, SD age = 13.28) from religious and government-operated hospitals completed the HPSS during day treatment. We modeled the HPSS factor structure to represent four related aspects: Emotional, Informational, Appraisal, and Instrumental social support. Study 2 preliminarily assessed the concurrent validity of the HPSS with patient perceptions of the patient-doctor relationship. Sixty-nine patients (40 females; M age = 53.67, SD age = 13.74) completed the HPPS with scales assessing perceived doctor-patient communication and patient trust in the healthcare provider. Study 1, using Exploratory Structural Equation Modeling, showed that a bifactor model had an excellent fit. The analysis supported the use of subscale scores, which were more tenable than a single total score in terms of bifactor model indices. This conclusion was also supported by greater scalability of the subscales in a Mokken Scale Analysis. Oncology patients treated in the religious hospital perceived greater Emotional, Informational, and Instrumental social support from their healthcare provider than those treated in government-operated. Study 2 showed that patient ratings of healthcare provider social support, except Instrumental, were positively correlated with better doctor communication skills and greater trust in the physician. Multiple regression analyses showed that Informational and Emotional support provided a unique contribution to building trust in the physician, controlling for the doctor’s communication skills. The study results showed that the four social support ratings were reliable and valid, sharpening the distinction between functional components in the formal healthcare system.
The quality of close relationships and the sense of social connectedness are reliable predictors of health and longevity (Holt-Lunstad et al., 2017; Schetter, 2017). Not surprisingly, the WHO enlisted social support networks among the most critical determinants of health (Commission on Social Determinants of Health, 2008). Social support networks perform four main functions: Emotional, Informational, Appraisal, and Instrumental. Briefly, Emotional support (also called affective or attachment) refers to demonstrations of love and caring, encouragement, and empathy from which one derives a sense of security (Thoits, 2011). Informational support is defined as providing facts or advice that may help a person solve problems (Wang et al., 2014). Instrumental support is intended as a form of practical, tangible help, provided through material assistance or practical tasks (Langford et al., 1997; Wang et al., 2014). Last, Appraisal support consists of expressions that affirm the appropriateness of acts or statements made by another (Langford et al., 1997).
Both informal and formal networks can support people affected by chronic diseases. Thus, this article refers to social support activated or required to cope with adverse life events and chronic health problems, defined as problem-oriented social support (e.g., Suurmeijer et al., 1995). Research has consistently demonstrated several benefits that medical patients receive from their informal networks (e.g., family, friends, and relatives). In conditions like diabetes, these benefits include improving emotion regulation, coping, glycemic control, and quality of life (Van Dam et al., 2005; Strom and Egede, 2012; Hill-Briggs et al., 2021). Social support also enhanced functional status and quality of life in people with heart failure, influencing treatment and health management behaviors (Graven and Grant, 2013, 2014; Bucholz et al., 2014).
In oncology patients, social support was found to address psychological problems resulting from a poor adjustment to cancer and its treatment (Rizalar et al., 2014). For example, by fostering acceptance, positive reframing of the situation, and maintaining the patient’s sense of humor, social support networks help patients be more determined in their fight against the disease and counteract helplessness-hopelessness and anxious preoccupations (Kawa, 2017; Lauriola and Tomai, 2019; Tomai et al., 2019). Moreover, several authors (Pinquart and Duberstein, 2010; Ikeda et al., 2013; Yağmur and Duman, 2016) reported significant correlations of social support with “hard” health outcomes, such as tumor initiation, cell proliferation, and life extension.
It is worth noting that social support may unintentionally hurt the patient’s wellbeing. Previous research has indicated that, contrary to caregivers’ intentions, patients who report unmet needs may perceive some forms of support as ineffective or troublesome (Breuer et al., 2017; Sebri et al., 2021). In particular, social support turns out unsupportive when the helper does not understand or effectively correspond to the recipient’s desires (Nouman and Zanbar, 2020). For example, this can happen within close relationships, when help is not sought or when support becomes controlling, oppressive, or, conversely, too superficial and neglecting the consequences of illness (Mazzoni and Cicognani, 2016; Mazzoni et al., 2017). Therefore, paying attention to the type of support a patient needs and how that support is provided will be the best way to address patients’ specific needs.
In addition to family and friends, healthcare professionals (e.g., doctors and nurses) can provide social support to patients suffering from chronic diseases, thus becoming a formal social support network. For instance, a supportive healthcare provider helped diabetic patients to defuse health distress and improve glycemia (Venkatesh and Weatherspoon, 2013; Wardian and Sun, 2014). Similarly, according to a recent study (Ban et al., 2021), the medical staff reduced cancer patients’ fear of illness progression by providing social support. Indeed, identifying patients at risk for psychosocial vulnerability due to low healthcare support appears to be a relevant health outcome (Usta, 2012).
How do formal social support networks work in oncology units? Are there similar functions that informal and formal networks perform for cancer patients? Healthcare social support functions have been less extensively studied than informal network ones. Nevertheless, given the increasing interest in improving healthcare quality and patient experience, constructs similar to social support functions have been used in medical settings (e.g., Donabedian, 2005; Beattie et al., 2015; Hancock et al., 2020). For instance, healthcare quality indicators include ratings of physicians’ interpersonal skills and information provision (Brédart et al., 2005a,b). Trust in oncologists reflects the patients’ beliefs about the healthcare provider’s ability to provide appropriate, reliable, and hopefully successful treatment (Müller et al., 2014). Communication is also considered a core clinical skill for establishing an excellent patient–doctor relationship (Malley and Fernández, 2010). When clinicians are better communicators, they can effectively convey information to patients, encouragement, and tangible support (Street et al., 2009). In sum, a health professional’s interpersonal competence and patient trust in the healthcare provider might be associated with one’s perception of social support. Still, they are not part of the construct as defined in psychosocial research (Barrera and Ainlay, 1983).
Where scholars have explicitly addressed healthcare social support, methodological approaches to obtaining reliable and valid measures have been varied and scattered. Previous research lacked a clear connection with the fourfold structure of the construct. For instance, some studies assessed multiple aspects of social support but used a single global score (Katz et al., 2003; Reynolds and Perrin, 2004). This choice, however, does not make fine-grained distinctions between how the healthcare provider can support the patient and improve the therapeutic relationship. Other studies focused either on emotional support (Kuuppelomäki, 2003; Wenrich et al., 2003; Ansmann et al., 2012) or informational support (Rutten et al., 2005). Underlying this approach, emotional and informational supports are viewed as functionally independent and not interchangeable. Another original approach combined two questions for each type of social support function into a single dichotomous indicator (Arora and Gustafson, 2009), assuming that healthcare provider social support could be a categorical variable. Unclear boundaries exist between informal networks’ social support functions and other proxy constructs used in medical research (e.g., communication skills).
Healthcare social support depends not only on individual actors (e.g., doctors or nurses) but also on the hospital’s mission and organizational culture. Ansmann et al. (2014), for example, emphasized the importance of hospital characteristics in fostering a better patient-doctor relationship. Hospitals in which the local culture emphasized cost control typically reported greater dissatisfaction with physicians’ interpersonal skills and information provision (Zhou et al., 2011). By contrast, non-profit hospitals imbibed in a religious culture promote a more inclusive and respectful atmosphere (Whitley, 2012). Religious hospitals have traditionally been reputed to provide a higher quality of care than government-operated hospitals (Fleming, 1981). Indeed, the organization’s charitable mission to serve and care for the person, along with a religious institutional identity, promotes the humanization of health care (e.g., Reinikka and Svensson, 2010; Calegari et al., 2015). Thus, religious hospitals can offer close and sensitive listening to the patient’s narratives and more compassionate care services, including care for the poor and vulnerable (White and Begun, 1998; White et al., 2010). Users themselves describe religious hospitals as more reliable and attractive than government-operated ones (Seemann et al., 2015). Considering this literature, a healthcare provider social support measure could also be a valuable tool to compare hospitals, outpatient clinics, particular services, or departments.
The role of social support from healthcare providers is a challenging and understudied area of research. There is a need to understand how and when the support provided by health professionals may influence the quality of care and which social support function has the most significant impact on the quality-of-care cancer patients receive in oncology centers. The present study sought to develop a Healthcare Provider Social Support scale (HPSS), sharpening the distinction between Emotional, Informational, Instrumental, and Appraisal functions in the formal oncology care system. These domains were inspired by Cutrona and Russell (1987). However, we did not develop items related to “Opportunity for Nurturance” (i.e., the sense of being needed by others for their wellbeing) and “Social Integration” (i.e., the importance of belonging to a group that shares similar interests). These forms of social support primarily belong to informal networks (Cutrona and Russell, 1987).
To the best of our knowledge, no previous study has developed a psychometric tool that reflects the construct’s fourfold model, which proved to be valid for assessing patients’ social support from their informal network. Study 1 was designed to preliminary assess the HPSS dimensionality and reliability in a sample of patients recruited from 2 day-treatment oncology units. According to the multidimensionality of the construct, we hypothesized that at least four factors are identified in the factor analysis of a reliable item set. These factors should correspond to perceived Emotional, Informational, Instrumental, and Appraisal support. A subsequent study used an independent patient sample to assess the relationships between HPSS ratings and other related constructs in the nomological network, such as doctor communication skills and the patient’s trust in the physician. We hypothesized that greater healthcare provider support perceptions are associated with patient-centered communication and greater trust in the physician.
Investigating the factor structure of a new scale is vital to establishing its psychometric properties. Confirmatory Factor Analysis (CFA) is commonly used for this purpose. Nevertheless, CFA has recently complained about failing to account for the imperfect nature of items, as evidenced by significant item correlations with non-target constructs or cross-loadings on more than a factor (Marsh et al., 2014; Morin et al., 2016). As a result, CFA may produce inaccurate estimates of factor correlations, necessitating general or method factors to achieve an acceptable fit (Morin et al., 2016; Joshanloo et al., 2017). In the present study, we used Exploratory Structural Equation Modeling (ESEM), a new approach that overcomes the limitations of CFA (Asparouhov and Muthén, 2009). In ESEM, cross-loadings on non-target factors are allowed in addition to primary loadings on target factors. Thus, ESEM is more efficient than CFA in the estimation of complex models because it provides more accurate estimates of factor loadings and correlations, preventing artificial inflation of factor loadings on the general factor (Marsh et al., 2014; Morin et al., 2016). We further examined the HPSS dimensionality and reliability using Mokken Scaling Analysis (MSA) to provide a sensitivity analysis for ESEM results. As shown in Figure 1, we tested the following factor models, each based on different theoretical assumptions. Like previous studies (Katz et al., 2003; Reynolds and Perrin, 2004), the unifactorial model assumes that all HPSS items measure the generalized patient’s perception of the healthcare provider’s support (Figure 1A). The four-factor model is consistent with the view that patients could discriminate between ways a doctor had supported them (Figure 1B). Assuming correlated factors would imply that the four social support functions were somewhat interrelated. Small factor correlations would show that different types of support are distinct but related aspects. Moderate factor correlations would indicate substantial overlap, suggesting a hierarchical arrangement of factors. In a bifactor model, every item is targeted to load primarily on general and specific factors (Figure 1C). For example, an item describing an emotionally supportive act is hypothesized to load on a generalized support perception factor and a specific emotional support one.
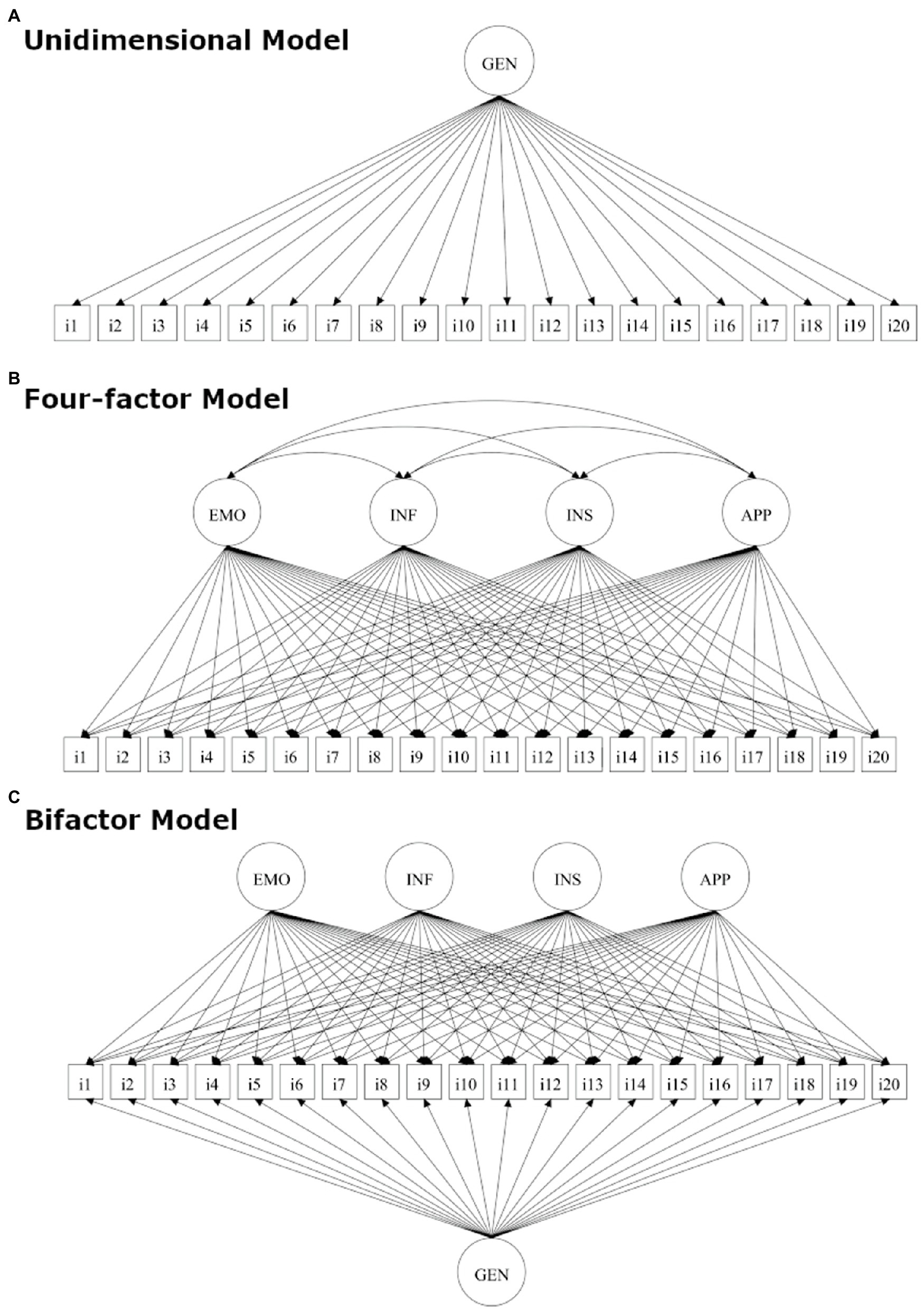
Figure 1. Schematic representations of the models tested in the present study: (A) unidimensional model; (B) four-factor model; and (C) bifactor model. EMO, emotional support; INF, informational support; INS, instrumental support; APP, appraisal support; and GEN, general support.
As a by-product of the study, we explored whether the HPSS ratings could detect differences between two healthcare providers. In keeping with the literature (Zhou et al., 2011; Whitley, 2012; Ansmann et al., 2014), we expected that patient ratings of perceived social support on the HPSS would differ between two oncology centers reputed for religious and government-operated organizational culture, respectively. Last, we explored whether the HPSS was sensitive to how patients at different stages of disease perceived their healthcare provider as providing support for all types or just for specific kinds. This hypothesis was motivated by studies showing that a patient’s need for support from a healthcare provider may change during the cancer experience. For instance, late in the course of cancer, especially when patients perceive a poorer prognosis, there is a greater need for emotional and instrumental support from health professionals (e.g., Arora and Gustafson, 2009).
One-hundred-sixty-two consecutive patients were recruited from two oncology centers in Rome, Italy, hereafter referred to as hospitals R and G, and surveyed for this study. R was a reputed religious hospital receiving public funding; G was a government-operated hospital. All participants were patients with a confirmed cancer diagnosis receiving chemotherapy in day-treatment units. Inclusion criteria for the study were: a performance status (ECOG) of 0 or 1, age over 18 years old, written comprehension of the Italian language, and ability to fill in a paper and pencil questionnaire. Exclusion criteria were a refusal to cooperate and mental disorders due to medical conditions. The refusal rate was around 5% in both hospitals. No cases were excluded for secondary mental disorders. The ethical review board of Hospital R approved all aspects of this study. Participation was voluntary, and patients had the right to withdraw from the study. Consent was obtained before data collection. Patient characteristics are shown in Table 1.
The HPSS administered in the present study consisted of 20 items arranged in four domains selected according to how social support functions have been operationally defined in existing scales used for informal social networks (e.g., Cutrona and Russell, 1987). The item format included the main statement (e.g., “the doctor was listening to you when you talked about your feelings”), followed by one or more illustrative examples (e.g., “pausing to talk to you or beyond the time strictly necessary to carry out his work; or leaving you time to talk to him about your fears”). The authors of this article developed the descriptive statements, which were reviewed with a medical oncologist in one of the two hospitals mentioned above. Thus, domain selection and statement generation followed what Magasi et al. (2012) considered an “etic” approach to content validity, i.e., how clinicians, researchers, or subject matter experts view the concepts to be measured. The illustrative examples were obtained from qualitative interviews with patients conducted by a hospital psychologist. Accordingly, these examples reflected an “emic” approach, i.e., they capitalized on insiders’ first-hand experience of the concept being measured (Magasi et al., 2012). The English translation of the HPSS, scoring instructions, and preliminary reference data are reported in Supplementary Materials. Patients were asked to rate their doctors’ social support behaviors during the visits or when they stay in the hospital using a five-point frequency scale (1 = Never; 2 = Rarely; 3 = Sometimes; 4 = Often; 5 = Always). Patients were instructed to resort to the examples if the main statement was unclear. Before the study, the HPSS was piloted with a small sample of patients to ensure the understandability of item content, examples, response format, and instructions. No particular problems were encountered in the pilot study.
Before ESEM, we assessed item descriptive statistics and item-rest correlations (IRC). In classical test theory, IRC is an index of item discrimination, indicating the extent to which an item separates individuals with high and low scores on the total scale scores. IRCs >0.50, 0.30, and 0.10 are considered strong, moderate, and weak discrimination, respectively (Bechger et al., 2003). Distributional assumptions were checked using the MVN package for R (Korkmaz et al., 2019). Because Shapiro–Wilk’s test is sensitive to small departures from univariate normality, it was used in conjunction with an established rule of thumb. Accordingly, we interpreted univariate skewness and kurtosis following Kline (2015), with critical values set at 3 and 10, respectively.
One-hundred-fifty-eight patients (98%) were complete cases. Sporadic missing data were observed. The missing data pattern did not reveal configurations that would indicate missingness not at random (Little’s MCAR test = 59.41, df = 61, p = 0.534). Therefore, we imputed missing data based on the SPSS Expectation–Maximization procedure. There were no discernible differences between complete-case and imputed data set analyses that would invalidate the study’s conclusions. However, in ESEM analysis, we used the imputed dataset to maximize the sample size.
ESEM analyses were conducted using Mplus (Version 8.4). We compared a bifactor model with the one-factor and four-factor models (Figure 1). A bifactor model is a latent structure in which each item loads on a general factor common to all items and a group factor common to some items. The general factor represents the target domain that one is most interested in (e.g., social support by a healthcare provider). The group factors represent narrow factors that explain item responses not accounted for by the general factor (e.g., information provision). According to Marsh et al. (2014), we used a Target Rotation because it provides a robust a priori model, allows more control over the model’s specification, and makes it easier to interpret the results. Because the HPSS uses Likert-type items, we carried out the analysis using robust least squares estimators (DWLS). This method is recommended to handle ordinal categorical data and has no distributional assumptions (Rhemtulla et al., 2012).
The model’s fit was assessed using the DWLSχ2 and other descriptive indices (Kline, 2015). CFI and TLI are incremental indices that compare the fit of the factor model to that of a null model, in which all items are assumed to be uncorrelated. CFI and TLI values >0.90 indicate acceptable fit, while values >0.95 indicate a good fit. The RMSEA measures the difference between the reproduced correlation matrix and the population correlation matrix, controlling sampling variability. An RMSEA of 0.05 or less indicates a close fit, and values up to 0.08 represent a reasonable approximation error. The 90% CI point estimate is also commonly reported to indicate the possibility of a close or exact fit.
The standardized factor loading matrix was analyzed using Dueber (2021) bifactor indices calculator package for R. It provides valuable factor and item statistics for addressing scale dimensionality and evaluating the appropriateness of the bifactor model solution. The ECV assesses the proportion of shared variance explained by each factor in the model, either general or group factors. For the general factor, ECVG supports unidimensionality when values greater than 0.70 are obtained. ECVS reflects the proportion of shared variance in subscale items explained by each specific factor. At the item level, IECV assesses how variance in each item can be attributed to the related variation in the general factor alone. Item unidimensionality is supported when values greater than 0.80 are obtained (Rodriguez et al., 2016). The Average Relative Parameter Bias (ARPB) cumulatively assesses the difference between an item’s loading on the general factor in the bifactor model and the corresponding loading in the unidimensional model. According to Rodriguez et al. (2016), ARPB values less than 0.15 support unidimensionality. RPB can be used to detect items for which substantial multidimensionality exists at the item level.
Using the Mokken package for R (van der Ark, 2007), we carried out the Mokken Scale Analysis (MSA). It is a nonparametric analog of Rasch analysis but has fewer assumptions about the shape of item characteristic curves (ICC). However, MSA assumes local independence, namely that participants’ responses to one item are independent of responses to other scale items if the underlying latent construct has been partialled out. This assumption was tested using W1 and W3 indices (Straat et al., 2016), which flag positive and negative locally dependent item pairs, respectively. Another assumption is monotonicity, namely that the probability of endorsing a specific item response category is a monotonically increasing function of the latent trait. This assumption, and the related non-intersection of item response curves, was tested through visual inspection of the ICC. After verifying these assumptions, we examined the Scalability of the HPSS total score and subscales scores. Scalability is the extent to which individual items in a scale measure the latent characteristic being measured. In MSA, Loevinger’s coefficient H test the level of Scalability for each item (Hi) and the entire set of items that form a scale or a subscale (Hj). A scale based on items with high Hi is highly scalable and likely to be unidimensional. Hj values greater than 0.30 are considered acceptable. According to Sijtsma and Molenaar (2002), Hj values in the range between 1.00 and 0.50 indicate strong Scalability and unidimensionality. Moderate and weak scalability ranges are between 0.49 and 0.40 and between 0.39 and 0.30, respectively.
As one can see from Table 2, means and SDs were comparable across items within each social support domain, showing item homogeneity. Even though the Shapiro–Wilks test was significant (all p-s < 0.01), the univariate skewness and kurtosis were within the acceptable limits of 3 and 10, respectively. The IRC was above the strong discrimination level for all Emotional, Informational, and Instrumental items, while it was close for Appraisal support items (Table 2). Overall, the item set proved adequate to be submitted to factor analysis.
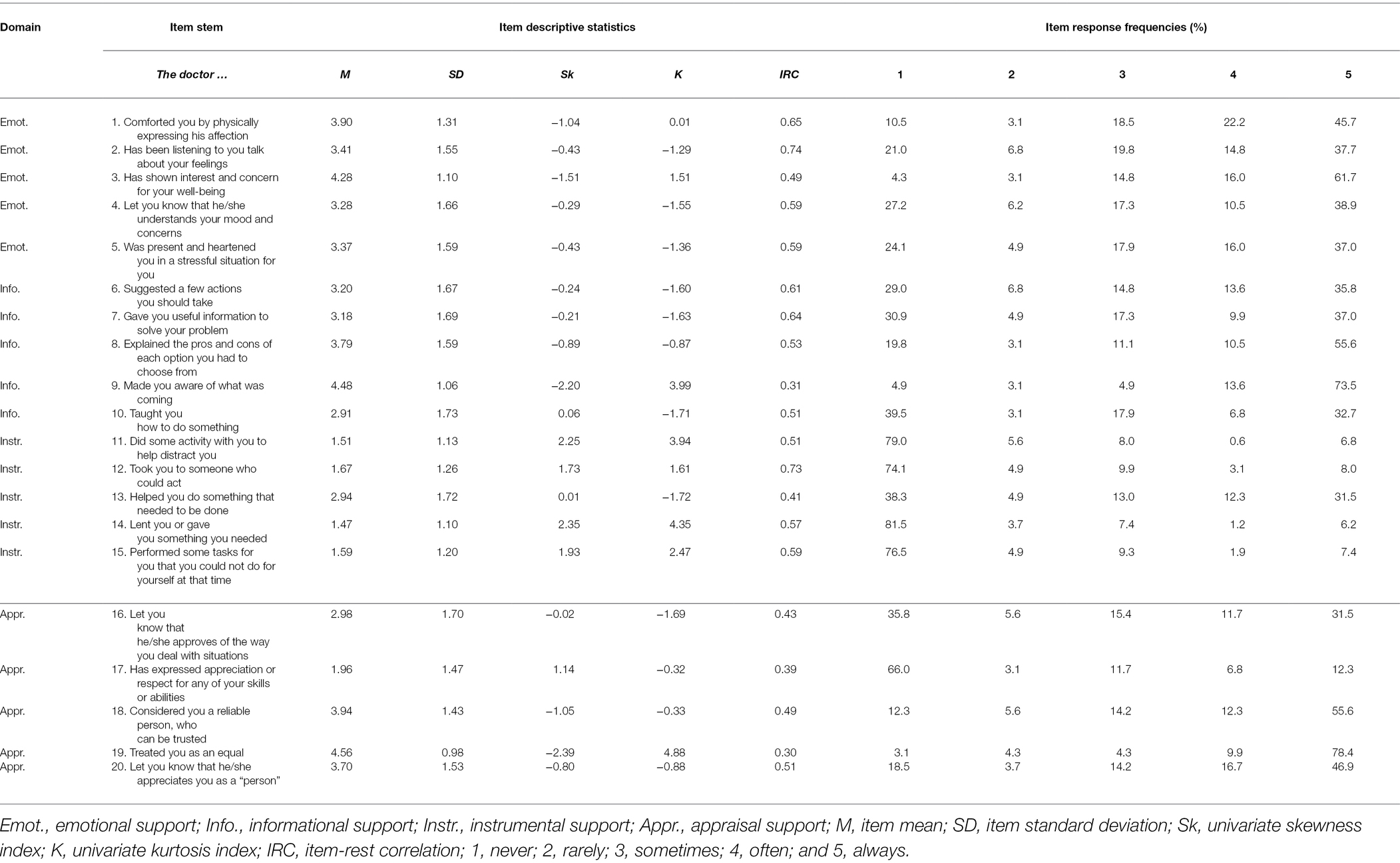
Table 2. Descriptive statistics and response frequencies for the Healthcare Perceived Social Support items.
First, we tested the unifactor model, which assumed that all items would measure only a general perception that healthcare was supportive. This hypothesis was rejected (χ2 = 554.22; df = 170; p < 0.001; TLI = 0.816; CFI = 0.835; RMSEA = 0.118; SRMR = 0.127). Next, we tested the four-factor model with correlated factors, which approached the good fit for most indices (χ2 = 148.51; df = 116; p < 0.023; TLI = 0.977; CFI = 0.986; RMSEA = 0.042; SRMR = 0.043). The target loadings were all statistically significant for this model (all p-s < 0.005) and were all greater than 0.40 for Emotional (λrange = 0.62–0.85), Informational (λrange = 0.43–0.75) and Instrumental support (λrange = 0.47–0.83; Table 3, Panel a). Except for item #16 (λ = 0.30), the Appraisal factor also loaded on items greater than 0.40. The factor loadings for appraisal support were also more heterogeneous than for Emotional, Informational, and Instrumental support (λrange = 0.30–0.81). Although there were many significant non-target cross-loadings (i.e., 22 out of 60), these were greater than the target loading only for item #16 (Table 4, Panel a). Item simplicity (i.e., IFS > 0.70) was supported for most HPSS items. As one can see from Table 4 (Panel b), the factor correlations were significant, with a moderate effect size. The four-factor model with correlated factors expands on the one-factor model, showing that the perceived healthcare support could be broken down into separate but still related functional components. Moderate factor correlations can be explained by a general domain factor, suggesting a bifactor model approach to represent the structure of the HPSS.
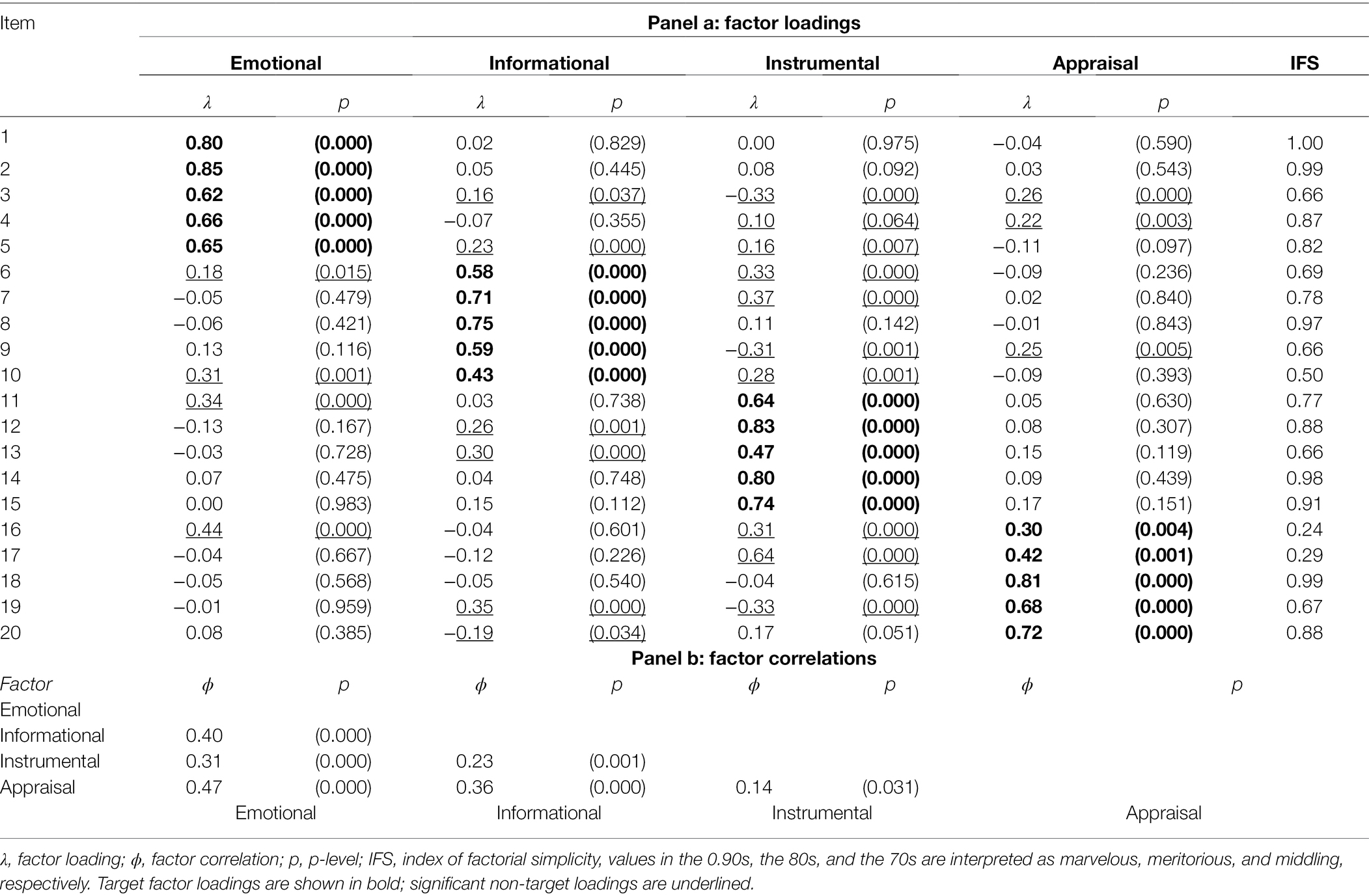
Table 3. Standardized factor loadings and factor intercorrelations from the exploratory structural equation modeling four-factor solution of the HPSS.
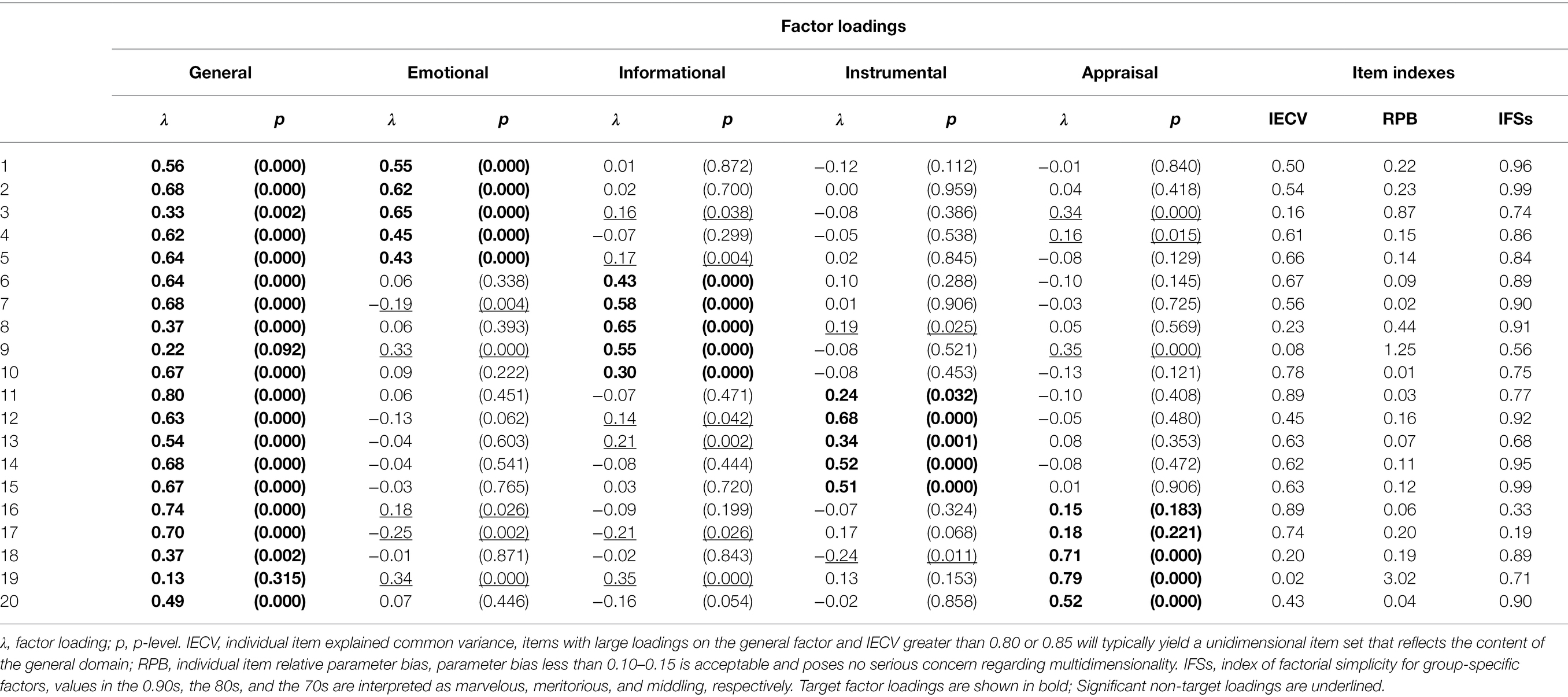
Table 4. Standardized factor loadings and factor intercorrelations from the exploratory structural equation modeling bifactor solution of the HPSS.
The bifactor model provided a nearly perfect fit (χ2 = 121.71; df = 100; p = 0.069; TLI = 0.982; CFI = 0.991; RMSEA = 0.037; SRMR = 0.039) and was significantly better than the four-factor model (Δχ2 = 28.43; df = 16; p < 0.05). As seen in Table 5, all items (except #9 and #19) significantly loaded on the general factor, and the coefficients were generally moderate to large (λrange = 0.37–0.80). Except for Appraisal Support, for which only three target loadings out of five were statistically significant (λrange = 0.52–0.79), all target loadings identified Emotional (λrange = 0.43–0.65), Informational (λrange = 0.30–0.65) and Instrumental support (λrange = 0.24–0.62) factors (Table 5). As in the previous analysis, the significant cross-loadings did not threaten the simplicity of the factor solution. The index of simplicity calculated for the four group factors showed that the items maintained good purity as indicators of Emotional, Informational, Instrumental, and Appraisal support (Table 4).
Given that HPSS items entangled general and specific sources of variance, the following analyses were performed to determine whether total or subscale scores are supported. The general factor explained about half of the common variance in perceived social support (ECVG = 51%) the remaining common variance was explained almost equally by Affective (ECVS = 14%), Informational (ECVS = 12%), Instrumental (ECVS = 10%), and Appraisal (ECVS = 13%) factors. The model ARPB was equal to 37%. Given ECVG < 70% and ARPB >15%, we can conclude that multidimensionality cannot be neglected in modeling the health provider social support construct using the HPSS scale. At the item level, only four items (#10, #11, #16, and #17) with IECV >0.80 varied between participants because of variation in the general factor only. The remaining items entangled to varying degrees a portion of variance related to the general factor and a portion related to the group factor (IECVrange = 0.02–0.67).
Following Rodriguez et al. (2016), we compared the reliability ω coefficients separately assessed for each subscale to the corresponding hierarchical ones (ωsh) in which the general factor variance was partialled out. This comparison is to assess the unique information provided by each of the subscale scores relative to the total reliable variance in each subscale. The resulting ω coefficients were high: 0.92, 0.90, 0.89, and 0.92 for Emotional, Informational, Appraisal, and Instrumental subscales, respectively. The ωsh dropped to 0.41, 0.39, 0.59, and 0.29, respectively. For the total score, instead, the proportion of reliable variance was ω = 0.95, with 81% of the variance depending on the general domain factor (i.e., ωh = 0.81). So, using the total score would dilute too much the variance of the specific factors present in the subscales.
First, we evaluated the local independence assumption. For the total score (20 items), we found only one flagged item pair (i.e., #2 with #3) to be positively locally dependent; no negative local dependence was found. For the Affective and Instrumental subscales (with five items each), we found one flagged item pair to be positively locally dependent (i.e., #2 with #3 and #12 with #13, respectively). No violations were detected for the Informational and Appraisal subscales. Therefore, the local independence assumption was only sporadically violated. Second, we inspected the item characteristic curves reported in Supplementary Materials. All items comprising the total score had monotonically non-decreasing patterns, and no significant violations were detected (Supplementary Figure S1; Supplementary Table S1). The analysis of subscales revealed some violations of the monotonicity assumptions (Supplementary Figure S2); however, only three items (#2, #8, and #18 belonging to Emotional, Information, and Appraisal scores, respectively) yielded statistically significant violations (Supplementary Table S2). Taken together, the assumptions for testing item scalability are overall tenable, with a few exceptions.
Table 5 shows the scalability coefficients Hi for specific items under total and subscale scoring approaches. The global Hj for the total scale and separate subscales were also reported. Using the total score approach, five items out of 20 were poorly scalable, and the resulting scale was weakly scalable. Conversely, scoring the HPSS according to a subscale approach made most items moderately to highly scalable. The Emotional and Instrumental HPSS subscales were strong, while the Informational and Appraisal ones were moderate. The Mokken reliability coefficients were 0.88 for the total score and 0.83, 0.77, 0.83, and 0.69 for the Emotional, Informational, Instrumental, and Appraisal subscales.
One of the intended applications of the HPSS could be assessing the perceived level of social support provided by healthcare providers in different hospitals, outpatient clinics, services, or departments in studies of healthcare quality. We piloted this approach, involving hospitals R and G in the HPSS preliminary validation study. Patients were also stratified by disease stage (i.e., stages I–III vs. stage IV) in data analysis because the patient’s need for support from a healthcare provider may change during the cancer experience. The analysis of Emotional, Informational, Instrumental, Appraisal support by hospital and disease stage revealed statistically significant multivariate main effects for the hospital (F = 20.83; df = 4,157; p < 0.001) and hospital × support function interaction (F = 6.39; df = 3,155; p < 0.001) accounting for 12 and 11% of the variance in the combined dependent variables, respectively. Follow-up univariate analyses were examined to determine which functional components of social support accounted for the multivariate effect. Significance was determined at p < 0.0125 (i.e., α = 0.05/4) to control for familywise type 1 error. Group means are shown in Figure 2. Patients receiving treatment in the religious hospital felt more supported than those treated in the public hospital from an emotional, informative, and practical point of view. There was no difference in esteem support. Using the HPSS total score as the dependent variable, we found that patients at hospital R perceived their healthcare provider to be overall more supportive.
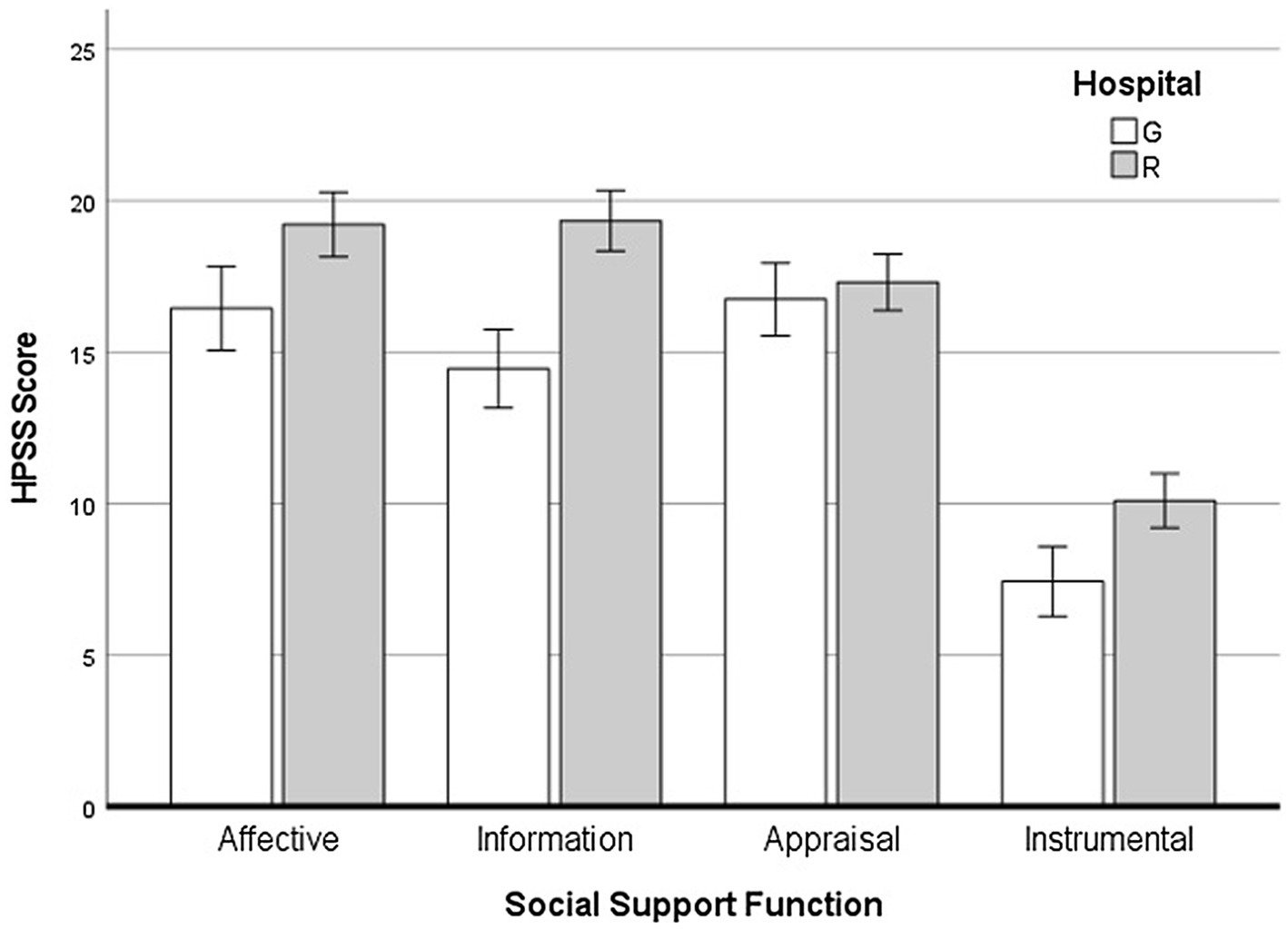
Figure 2. Differences between government-operated (G) and religious (R) hospitals across different social support functions.
The previous study showed that the HPSS scale has a solid factorial structure and that the four social support functions can be reliably measured. However, examining only the factorial structure of the scale is not sufficient to demonstrate the validity of HPSS scores. Given that validation of a new measure is a laborious process that requires a range of empirical evidence, in this study, we surveyed an independent sample of oncology patients to take the first step in this direction. As part of criterion-related validity assessment, we aimed to establish the correlations between HPSS scores and two critical variables in the physician-patient relationship. These were the physician’s communication skills and the patient’s trust toward the healthcare provider. Recent studies have reinforced the view that patients of health professionals with better communication skills develop trusting relationships with their doctors (Chandra et al., 2018) and have better health outcomes (Howick et al., 2018; Noble, 2020). Accordingly, we expected the HPSS scores to positively correlate with the doctor’s communication skills and the patient’s trust toward the health care provider.
Sixty-nine non-consecutive patients were recruited from one oncology center in Naples, Italy. As in Study 1, all participants had a confirmed cancer diagnosis and received chemotherapy in a day-treatment unit. Inclusion and exclusion criteria were the same as in Study 1. The refusal rate was around 10%, and no cases were excluded because of secondary mental disorders. The ethical review board at Sapienza University in Rome approved the study. As a condition of participation, all patients provided their informed consent. Characteristics of patients can be found in Table 1.
Same as in Study 1.
This 11-item scale (TPS; Anderson and Dedrick, 1990) is one of the most widely used tools to assess patients’ trust in their physician (Müller et al., 2014). In the absence of a formal validation study for this scale in Italian, the second author of this paper translated items and instructions for use in the present study, receiving back-translation feedback from an expert bilingual professional translator. The TPS uses a five-point response scale (1 = Strongly Disagree to 5 = Strongly Agree) and yields a total score reflecting greater trust.
This scale consists of 15 items designed to assess patient perceptions of physician interpersonal and communication skills (CAT; Makoul et al., 2007). The Italian translation of the CAT has been recently tested in an outpatient surgical clinic (Scala et al., 2016). Patients are asked to answer each item based on a single, recent physician interaction. The CAT yields a summary score reflecting the patient’s overall satisfaction.
Pearson’s r was used to assess the correlations among variables. Nonlinear correlations were explored using the nlcor R package (Ranjan and Najari, 2022). The unique contribution of social support and communication scores in predicting trust was explored using linear regression analyses. The sequence of analyses and the choice of independent and dependent variables was guided by emerging findings in the correlation analyses and the reviewed literature. As in Study 1, sporadic missing data were observed (59 patients, 86%, were complete cases), and the missing data pattern was completely random (Little’s MCAR test = 472.14, df = 471, p = 0.477). Due to the relatively small sample size, missing data were imputed, as in Study 1.
Table 6 reports descriptive statistics, reliability coefficients, and correlations among HPSS scores, Trust in Physician, and Physician’s Communication Skills. Nonlinear correlations were virtually identical to Pearson correlations, supporting the linearity and monotonicity of all relationships. All the coefficients were positive and statistically significant. The correlations among HPSS scores were very high, reflecting a substantial proportion of shared common variance. Emotional and Informational support functions were more strongly associated with Physician’s Communication Skills than Instrumental and Appraisal ones. The total HPSS score was also strongly associated with the communication score. This result showed that physicians with better communication skills were more effective in providing social support to their patients, making them feel secure (i.e., Emotional support) and informed about their treatment and medical status (i.e., Informational support).
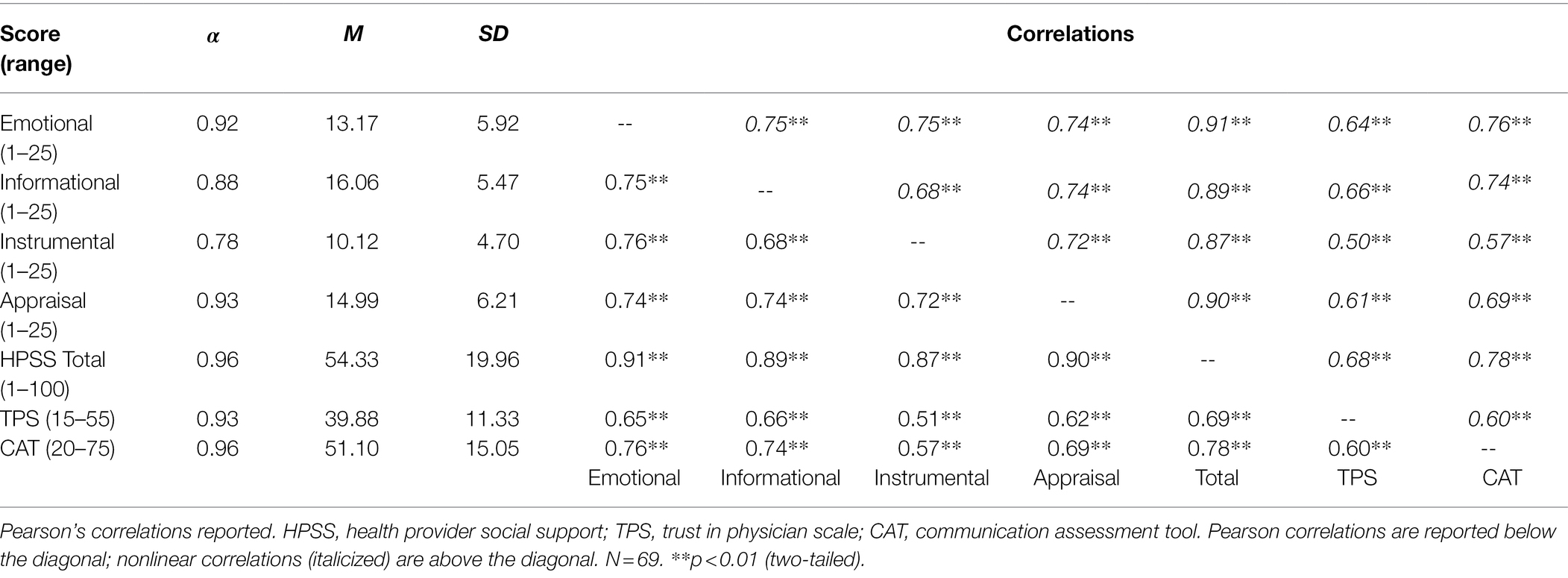
Table 6. Descriptive statistics and intercorrelations among HPSS scores, trust in physician, and physician’s communication skills.
Similarly, Emotional, Informational, and Appraisal support functions and the HPSS total score were more strongly associated with Trust in Physician than Instrumental support. Physician’s Communication Skills were also associated with the perceived trust, but the correlation was slightly lower than those assessed between trust and social support functions. These findings suggested that healthcare provider social support and doctor-patient communication are fundamental to developing a trusting relationship and therapeutic alliance with their doctors.
Although correlations in a cross-sectional study cannot prove causal relationships, the data collected are consistent with the view that Affective, Informational, Instrumental social support, and Physician’s Communication Skills could predict Trust to a different extent and better than instrumental support. We performed linear regression analyses to explore this possibility and disentangle unique social support and communication contributions. We used the HPSS scores as predictors of trust, controlling for Physician’s Communication Skills. These analyses showed that Emotional (Beta = 0.46; t-value = 3.02; p = 0.004), Informational (Beta = 0.50; t-value = 3.33; p = 0.001), and the HPSS total score (Beta = 0.59; t-value = 3.79; p < 0.001) remained statistically associated with Trust, making Physician’s Communication skills no longer significant. Both Appraisal support (Beta = 0.39; t-value = 2.89; p = 0.005) and Physician’s Communication skills (Beta = 0.32; t-value = 2.38; p = 0.021) uniquely predicted Trust scores. Confirming the correlations reported In Table 6, Instrumental support did not predict Trust score, and Physician’s Communication was the only significant predictor (Beta = 0.46; t-value = 3.80; p < 0.001). Overall, these analyses showed that Emotional and Informational healthcare supports were essential to building trusting relationships above and beyond Physician’s Communication skills.
In the present study, we proposed a new scale, the HPSS, to assess healthcare social support in oncology settings. The scale was designed according to a multidimensional approach, as established in psychosocial research where social networks perform Emotional, Informational, Appraisal, and Instrumental functions (Cutrona and Russell, 1987; Langford et al., 1997; Thoits, 2011; Wang et al., 2014).
Although still preliminary, the results obtained from two studies of patients recruited from different oncology day-treatment units are promising and can be summarized as follows. First, the HPSS had a multidimensional structure. Second, the HPSS subscales proved reliable and preserved a good degree of specific information. Third, we detected differences in perceived social support between patients admitted to religious and government-operated hospitals. Fourth, the Affective, Informational, and Appraisal functions were positively correlated with doctor communication skills and patient’s trust in the physician.
Regarding the factor structure, our study showed that the four-factor model had a good fit to the data, outperforming the unifactorial model. Other studies measured healthcare provider social support either as Emotional or as Informational, implicitly assuming that these functions were enough to cover the content domain and precluding comprehensive tests of construct dimensionality (Kuuppelomäki, 2003; Wenrich et al., 2003; Rutten et al., 2005; Ansmann et al., 2012). Our findings indicated that oncology patients could discriminate how a healthcare provider could support them beyond merely demonstrating love and caring, encouragement, and empathy (Thoits, 2011) or providing facts or advice (Wang et al., 2014). Instrumental and Appraisal emerged as distinct social support factors. In a doctor-patient relationship, it could be argued that providing practical, tangible help to patients (Langford et al., 1997; Wang et al., 2014) or endorsing the appropriateness of acts or statements made by patients (Langford et al., 1997) is not required. Nevertheless, even assuming this is true for all medical specialties, it is still possible that other health professionals (e.g., nurses or physical therapists) might contribute to enhancing the perceived quality of care by providing complementary functions of social support. Foreshadowing future research, one could investigate whether Instrumental and Appraisal items apply equally well to physicians and other members of a multidisciplinary oncology care team.
Our study also revealed that a general factor coexisted with the abovementioned factors. CFA has recently complained about necessitating insubstantial or inflated general factors to achieve an acceptable fit (Morin et al., 2016; Joshanloo et al., 2017). Because we used an ESEM approach, which does not produce such statistical artifacts, we are reasonably confident that the general factor represented an additional source of reliable variance. However, the general factor could be challenging to explain. Alternative interpretations are possible. On the one hand, the general factor might reflect a “true” perception that accounts for patients’ overall feelings of being supported by healthcare professionals. This interpretation is consistent with previous research considering healthcare social support as a single evaluative dimension, disregarding fine-grained distinctions between specific functions (Katz et al., 2003; Reynolds and Perrin, 2004). On the other hand, the general factor could reflect acquiescence, social desirability, or other response sets. We believe that the first interpretation is the most likely. However, we cannot rule out the second interpretation based on the present study. Thus, future research should validate the general factor against independent response-bias measures.
Although our study supported the construct validity of the HPSS, a few items showed low loadings on the target factors or lacked factorial simplicity in ESEM analysis; a few others were shown to violate Mokken scaling assumptions. As noted elsewhere (e.g., Morin et al., 2015), the inherent difficulty in producing items that perfectly reflect the constructs intended to measure could explain these defects. However, we cannot exclude other possibilities. For example, in developing the HPSS, we adopted a mostly etic approach to content validity and item generation. However, the items also reflected an emic view of patients in the illustrative examples provided below each item (see Supplementary Materials). While combining etic/emic approaches is desirable to widen the content coverage (Magasi et al., 2012), the specific item format (i.e., general statement + illustrative examples) might have increased the item complexity. Of course, defective items might be dropped out from a revision of the HPSS; however, we did not find severely biased or insubstantial items in the present study. So, we think modifying items could be more appropriate than a deletion. Notably, notwithstanding imperfections, the subscale scores preserved a non-negligible amount of reliable information and were reasonably scalable. Therefore, we recommend using subscales in clinical assessment and research applications.
The present study also made some steps toward a more robust assessment of criterion-related and concurrent validity of the HPSS scores. In keeping with previous research (White and Begun, 1998; Reinikka and Svensson, 2010; White et al., 2010; Zhou et al., 2011; Whitley, 2012; Calegari et al., 2015; Seemann et al., 2015), we expected the HPSS to be sensitive to differences in perceived support provided to patients admitted to religious or government-operated hospitals. This hypothesis was supported for Emotional, Informational, and Instrumental support, perceived higher by patients in the religious hospital. This finding implies that the HPSS could be used in quality of care research to assess and compare hospitals, outpatient clinics, particular services, or departments. As part of criterion-related validity, we also expected stage-related differences in perceived social support as suggested by previous research (Arora and Gustafson, 2009). This hypothesis was not confirmed, however. Either the patients have not changed their demands on the doctors, or the doctors may not have adapted to the patient’s changing needs. A longitudinal study would be needed to address this issue.
Construct validation is a long-term endeavor, requiring multiple studies and accumulating evidence for the instrument’s validity. Our study aimed to establish the correlations between HPSS scores and two critical variables in the physician-patient relationship as part of this process. Constructs similar to social support functions have been used in medical research (Donabedian, 2005; Brédart et al., 2005a,b; Malley and Fernández, 2010; Müller et al., 2014). From our perspective, a physician’s communication skills and trustworthiness are not social support variables; nevertheless, we expected to see positive correlations between HPSS scores and these variables. Overall, our hypotheses about the relationships of HPSS ratings with similar constructs in the nomological network were confirmed.
Beyond merely providing initial evidence of HPSS concurrent validity, the correlation pattern reported in the present study was compatible with the view that healthcare provider social support was needed to develop a trusting doctor-patient relationship, above and beyond the physician’s excellent communication abilities. Indeed, Affective and Informational scores remained statistically associated with patients’ trust in their physician, controlling for the physician’s communication skills. Not only were the patients of doctors with excellent communication skills more likely to develop trustworthy relationships (Chandra et al., 2018), but specific healthcare support functions can also have a unique role in increasing patients’ trust.
The present study is not exempt from limitations. First, the sample used was non-probabilistic and relatively small for structural equation modeling. Nevertheless, we surveyed consecutive clinical patients from different oncology units with a high response rate. So, our sample reflects the typical user of these health services. At the same time, the result of our study might not apply to other clinical populations suffering from different diseases or psychological disorders. Although no golden rule exists for establishing the minimum sample size for structural equation modeling (Kline, 2015), analyses carried out on small samples may fail to converge or provide an improper solution. In our study, we did not encounter any of these problems; therefore, we believe the sample size was sufficient, at least from a computational point of view. Of course, future studies should consider cross-validation of the factor structure on a larger sample. Second, the factors emerging from structural equation modeling need further validation. In particular, the “true” nature of the general factor needs to be clarified. To this purpose, a new data collection must include external measures of social desirability and acquiescence to rule out the possibility that the general factor captured primarily response set variance. Third, the sample size of Study 2 was somewhat limited, and the research design was cross-sectional. Therefore, caution must be exercised to avoid overgeneralizing the results and speculating on possible causal relationships between the variables involved. More research is needed with larger samples and longitudinal designs to rule out alternative interpretations of correlational evidence. Last, all variables in the study are self-reported. This characteristic of our research might have inflated the observed correlations between HPSS scores and the criteria used in the second study. Future validation studies of healthcare social support functions are needed and should compare self-reported data to data extracted from medical records or clinical test results.
Our study showed that patients can discriminate well between different ways healthcare providers can support them, and the scale proposed here can measure healthcare support as a multidimensional construct. Because healthcare provider social support can soothe psychological distress resulting from a poor adjustment to chronic conditions, a multidimensional scale might help to profile which type of social support is more salient in particular healthcare services, and which is lacking. Further longitudinal studies are needed to clarify the reciprocal relationships between social support, physician–patient communication, trust, quality of care, and health outcomes.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Studies involving human participants were reviewed and approved by the Hospital R Ethics Committee (Study 1) and the Ethics Review Committee for Psychological Research, Department of Social and Developmental Psychology, Sapienza University of Rome (Study 2). The Hospital R ethics committee waived the requirement for written informed consent for participation in Study 1. We obtained written informed consent from all patients participating in Study 2 as per the Ethics Review Committee for Psychological Research recommendations.
MT and ML contributed equally to the theoretical and empirical aspects of the study. All authors contributed to the article and approved the submitted version.
This work was supported by the Sapienza Institutional Research grants (RP1181642870C00B, RM11916B7E07E816).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
The authors wish to thank Valentina Romeo and Cristina Soldati (Study 1), Ludovica Maria Ercolessi and Romeo Miraglia (Study 2) for help in data collection, and all medical professionals, nurses, and healthcare teams involved in the study. The authors also express sincere gratitude to all patients and their caregivers for participating in this study.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.773447/full#supplementary-material
Anderson, L. A., and Dedrick, R. F. (1990). Development of the trust in physician scale: a measure to assess interpersonal trust in patient-physician relationships. Psychol. Rep. 67, 1091–1100. doi: 10.2466/pr0.1990.67.3f.1091
Ansmann, L., Kowalski, C., Ernstmann, N., Ommen, O., and Pfaff, H. (2012). Patients’ perceived support from physicians and the role of hospital characteristics. Int. J. Qual. Health Care 24, 501–508. doi: 10.1093/intqhc/mzs048
Ansmann, L., Wirtz, M., Kowalski, C., Pfaff, H., Visser, A., and Ernstmann, N. (2014). The impact of the hospital work environment on social support from physicians in breast cancer care. Patient Educ. Couns. 96, 352–360. doi: 10.1016/j.pec.2014.07.016
Arora, N. K., and Gustafson, D. H. (2009). Perceived helpfulness of physicians’ communication behavior and breast cancer patients’ level of trust over time. J. Gen. Intern. Med. 24, 252–255. doi: 10.1007/s11606-008-0880-x
Asparouhov, T., and Muthén, B. (2009). Exploratory structural equation modeling. Struct. Equ. Model. 16, 397–438. doi: 10.1080/10705510903008204
Ban, Y., Li, M., Yu, M., and Wu, H. (2021). The effect of fear of progression on quality of life among breast cancer patients: the mediating role of social support. Health Qual. Life Outcomes 19:178. doi: 10.1186/s12955-021-01816-7
Barrera, M., and Ainlay, S. L. (1983). The structure of social support: a conceptual and empirical analysis. J. Community Psychol. 11, 133–143. doi: 10.1002/1520-6629(198304)11:2<133::AID-JCOP2290110207>3.0.CO;2-L
Beattie, M., Murphy, D. J., Atherton, I., and Lauder, W. (2015). Instruments to measure patient experience of healthcare quality in hospitals: a systematic review. Syst. Rev. 4:97. doi: 10.1186/s13643-015-0089-0
Bechger, T. M., Maris, G., Verstralen, H. H. F. M., and Béguin, A. A. (2003). Using classical test theory in combination with item response theory. Appl. Psychol. Meas. 27, 319–334. doi: 10.1177/0146621603257518
Brédart, A., Bottomley, A., Blazeby, J. M., Conroy, T., Coens, C., D’Haese, S., et al. (2005a). An international prospective study of the EORTC cancer in-patient satisfaction with care measure (EORTC IN-PATSAT32). Eur. J. Cancer 41, 2120–2131. doi: 10.1016/j.ejca.2005.04.041
Brédart, A., Bouleuc, C., and Dolbeault, S. (2005b). Doctor-patient communication and satisfaction with care in oncology. In Current Opinion in Oncology 17, 351–354).
Breuer, N., Sender, A., Daneck, L., Mentschke, L., Leuteritz, K., Friedrich, M., et al. (2017). How do young adults with cancer perceive social support? A qualitative study. J. Psychosoc. Oncol. 35, 292–308. doi: 10.1080/07347332.2017.1289290
Bucholz, E. M., Strait, K. M., Dreyer, R. P., Geda, M., Spatz, E. S., Bueno, H., et al. (2014). Effect of low perceived social support on health outcomes in young patients with acute myocardial infarction: results from the VIRGO (variation in recovery: role of gender on outcomes of young AMI patients) study. J. Am. Heart Assoc. 3:e001252. doi: 10.1161/JAHA.114.001252
Calegari, R. C., Massarollo, M. C., and Santos, M. J. (2015). Humanização da assistência à saúde na percepção de enfermeiros e médicos de um hospital privado. Rev. Esc. Enferm. USP 49, 42–47. doi: 10.1590/S0080-623420150000800006
Chandra, S., Mohammadnezhad, M., and Ward, P. (2018). Trust and communication in a doctor-patient relationship: a literature review. J. Health Commun. 3:36. doi: 10.4172/2472-1654.100146
Commission on Social Determinants of Health (2008). Closing the gap in a generation: health equity through action on the socialdeterminants of health. World Health Organ. 6, 102–105. doi: 10.1080/17441692.2010.514617
Cutrona, C. E., and Russell, D. W. (1987). “The provisions of social relationships and adaptation to stress” in Advanced Personal Relationships (Issue October). eds. D. Perlman and W. Jones (Greenwich, CT: JAI Press)
Donabedian, A. (2005). Evaluating the quality of medical care. Milbank Q. 83, 691–729. doi: 10.1111/j.1468-0009.2005.00397.x
Dueber, D. (2021). BifactorIndicesCalculator: Bifactor Indices Calculator. R package version 0.2.2. Retrieved from https://CRAN.R-project.org/package=BifactorIndicesCalculator
Graven, L. J., and Grant, J. (2013). The impact of social support on depressive symptoms in individuals with heart failure: update and review. J. Cardiovasc. Nurs. 28, 429–443. doi: 10.1097/JCN.0b013e3182578b9d
Graven, L. J., and Grant, J. S. (2014). Social support and self-care behaviors in individuals with heart failure: an integrative review. Int. J. Nurs. Stud. 51, 320–333. doi: 10.1016/j.ijnurstu.2013.06.013
Hancock, S. L., Ryan, O. F., Marion, V., Kramer, S., Kelly, P., Breen, S., et al. (2020). Feedback of patient-reported outcomes to healthcare professionals for comparing health service performance: a scoping review. BMJ Open 10:e038190. doi: 10.1136/bmjopen-2020-038190
Hill-Briggs, F., Adler, N. E., Berkowitz, S. A., Chin, M. H., Gary-Webb, T. L., Navas-Acien, A., et al. (2021). Social determinants of health and diabetes: a scientific review. Diabetes Care 44, 258–279. doi: 10.2337/dci20-0053
Holt-Lunstad, J., Robles, T. F., and Sbarra, D. A. (2017). Advancing social connection as a public health priority in the United States. Am. Psychol. 72, 517–530. doi: 10.1037/amp0000103
Howick, J., Moscrop, A., Mebius, A., Fanshawe, T. R., Lewith, G., Bishop, F. L., et al. (2018). Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis. J. R. Soc. Med. 111, 240–252. doi: 10.1177/0141076818769477
Ikeda, A., Kawachi, I., Iso, H., Iwasaki, M., Inoue, M., and Tsugane, S. (2013). Social support and cancer incidence and mortality: the JPHC study cohort II. Cancer Causes Control 24, 847–860. doi: 10.1007/s10552-013-0147-7
Joshanloo, M., Jose, P. E., and Kielpikowski, M. (2017). The value of exploratory structural equation modeling in identifying factor overlap in the mental health continuum-short form (MHC-SF): a study with a New Zealand sample. J. Happiness Stud. 18, 1061–1074. doi: 10.1007/s10902-016-9767-4
Katz, M. R., Irish, J. C., Devins, G. M., Rodin, G. M., and Gullane, P. J. (2003). Psychosocial adjustment in head and neck cancer: the impact of disfigurement, gender and social support. Head Neck 25, 103–112. doi: 10.1002/hed.10174
Kawa, M. H. (2017). Influence of perceived social support and meaning in life on fighting spirit: a study of cancer patients. Int. J. Adv. Educ. Res. 2, 86–93.
Korkmaz, S., Goksuluk, D., and Zararsiz, G. (2019). MVN: an R package for assessing multivariate normality. R J. 6:151. doi: 10.32614/rj-2014-031
Kuuppelomäki, M. (2003). Emotional support for dying patients: the nurses’ perspective. Eur. J. Oncol. Nurs. 7, 120–129. doi: 10.1016/S1462-3889(03)00002-4
Langford, C. P. H., Bowsher, J., Maloney, J. P., and Lillis, P. P. (1997). Social support: a conceptual analysis. J. Adv. Nurs. 25, 95–100. doi: 10.1046/j.1365-2648.1997.1997025095.x
Lauriola, M., and Tomai, M. (2019). Biopsychosocial correlates of adjustment to cancer during chemotherapy: the key role of health-related quality of life. Sci. World J. 2019:9750940. doi: 10.1155/2019/9750940
Magasi, S., Ryan, G., Revicki, D., Lenderking, W., Hays, R. D., Brod, M., et al. (2012). Content validity of patient-reported outcome measures: perspectives from a PROMIS meeting. Qual. Life Res. 21, 739–746. doi: 10.1007/s11136-011-9990-8
Makoul, G., Krupat, E., and Chang, C. H. (2007). Measuring patient views of physician communication skills: development and testing of the communication assessment tool. Patient Educ. Couns. 67, 333–342. doi: 10.1016/j.pec.2007.05.005
Malley, J., and Fernández, J.-L. (2010). Measuring quality in social care services: theory and practice. Ann. Public Coop. Econ. 81, 559–582. doi: 10.1111/j.1467-8292.2010.00422.x
Marsh, H. W., Morin, A. J. S., Parker, P. D., and Kaur, G. (2014). Exploratory structural equation modeling: an integration of the best features of exploratory and confirmatory factor analysis. Annu. Rev. Clin. Psychol. 10, 85–110. doi: 10.1146/annurev-clinpsy-032813-153700
Mazzoni, D., and Cicognani, E. (2016). Positive and problematic support, stress and quality of life in patients with systemic lupus erythematosus. Anxiety Stress Coping 29, 542–551. doi: 10.1080/10615806.2015.1134785
Mazzoni, D., Cicognani, E., and Prati, G. (2017). Health-related quality of life in systemic lupus erythematosus: a longitudinal study on the impact of problematic support and self-efficacy. Lupus 26, 125–131. doi: 10.1177/0961203316646459
Morin, A. J. S., Arens, A. K., and Marsh, H. W. (2016). A Bifactor exploratory structural equation modeling framework for the identification of distinct sources of construct-relevant psychometric multidimensionality. Struct. Equ. Model. Multidiscip. J. 23, 116–139. doi: 10.1080/10705511.2014.961800
Morin, A. J. S., Katrin Arens, A., and Marsh, H. W. (2015). A bifactor exploratory structural equation modeling framework for the identification of distinct sources of construct-relevant psychometric multidimensionality. Struct. Equ. Model. 23, 116–139. doi: 10.1080/10705511.2014.961800
Müller, E., Zill, J. M., Dirmaier, J., Härter, M., and Scholl, I. (2014). Assessment of trust in physician: a systematic review of measures. PLoS One 9:e106844. doi: 10.1371/journal.pone.0106844
Noble, L. M. (2020). “Doctor-patient communication and adherence to treatment,” in Adherence to Treatment in Medical Conditions, CRC Press. 51–82. doi: 10.1201/9781003072348
Nouman, H., and Zanbar, L. (2020). Support or stressor? The community as a predictor of perceptions of infertility. Soc. Work Health Care 59, 650–667. doi: 10.1080/00981389.2020.1852360
Pinquart, M., and Duberstein, P. (2010). Associations of social networks with cancer mortality: a meta- analysis. Crit. Rev. Oncol. Hematol. 75, 122–137. doi: 10.1016/j.critrevonc.2009.06.003
Ranjan, C., and Najari, V. (2022). nlcor: Compute Nonlinear Correlations. R package version 2.3. [Source code] Retrieved from https://rdrr.io/github/ProcessMiner/nlcor/src/R/correlations.R
Reinikka, R., and Svensson, J. (2010). Working for god? Evidence from a change in financing of nonprofit health care providers in Uganda. J. Eur. Econ. Assoc. 8, 1159–1178. doi: 10.1111/j.1542-4774.2010.tb00551.x
Reynolds, J. S., and Perrin, N. A. (2004). Mismatches in social support and psychology adjustment to breast cancer. Health Psychol. 23, 425–430. doi: 10.1037/0278-6133.23.4.425
Rhemtulla, M., Brosseau-Liard, P. É., and Savalei, V. (2012). When can categorical variables be treated as continuous? A comparison of robust continuous and categorical SEM estimation methods under suboptimal conditions. Psychol. Methods 17, 354–373. doi: 10.1037/a0029315
Rizalar, S., Ozbas, A., Akyolcu, N., and Gungor, B. (2014). Effect of perceived social support on psychosocial adjustment of Turkish patients with breast cancer. Asian Pac. J. Cancer Prev. 15, 3429–3434. doi: 10.7314/APJCP.2014.15.8.3429
Rodriguez, A., Reise, S. P., and Haviland, M. G. (2016). Applying bifactor statistical indices in the evaluation of psychological measures. J. Pers. Assess. 98, 223–237. doi: 10.1080/00223891.2015.1089249
Rutten, L. J. F., Arora, N. K., Bakos, A. D., Aziz, N., and Rowland, J. (2005). Information needs and sources of information among cancer patients: a systematic review of research (1980–2003). Patient Educ. Couns. 57, 250–261. doi: 10.1016/j.pec.2004.06.006
Scala, D., Menditto, E., Armellino, M. F., Manguso, F., Monetti, V. M., Orlando, V., et al. (2016). Italian translation and cultural adaptation of the communication assessment tool in an outpatient surgical clinic. BMC Health Serv. Res. 16:163. doi: 10.1186/s12913-016-1411-9
Schetter, C. D. (2017). Moving research on health and close relationships forward-a challenge and an obligation: introduction to the special issue. Am. Psychol. 72, 511–516. doi: 10.1037/amp0000158
Sebri, V., Mazzoni, D., Triberti, S., and Pravettoni, G. (2021). The impact of unsupportive social support on the injured self in breast cancer patients. Front. Psychol. 12:722211. doi: 10.3389/fpsyg.2021.722211
Seemann, A.-K., Drevs, F., Gebele, C., and Tscheulin, D. K. (2015). Are religiously affiliated hospitals more than just nonprofits? A study on stereotypical patient perceptions and preferences. J. Relig. Health 54, 1027–1039. doi: 10.1007/s10943-014-9880-9
Sijtsma, K., and Molenaar, I. (2002). Introduction to Nonparametric Item Response Theory. Thousand Oaks: Sage Publications.
Straat, J. H., van der Ark, L. A., and Sijtsma, K. (2016). Using conditional association to identify locally independent item sets. Methodology 12, 117–123. doi: 10.1027/1614-2241/a000115
Street, R. L., Makoul, G., Arora, N. K., and Epstein, R. M. (2009). How does communication heal? Pathways linking clinician-patient communication to health outcomes. Patient Educ. Couns. 74, 295–301. doi: 10.1016/j.pec.2008.11.015
Strom, J. L., and Egede, L. E. (2012). The impact of social support on outcomes in adult patients with type 2 diabetes: a systematic review. Curr. Diab. Rep. 12, 769–781. doi: 10.1007/s11892-012-0317-0
Suurmeijer, T. P. B. M., Doeglas, D. M., Briançon, S., Krijnen, W. P., Krol, B., Sanderman, R., et al. (1995). The measurement of social support in the ‘European research on incapacitating diseases and social support’: the development of the social support questionnaire for transactions (SSQT). Soc. Sci. Med. 40, 1221–1229. doi: 10.1016/0277-9536(94)00253-P
Thoits, P. A. (2011). Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 52, 145–161. doi: 10.1177/0022146510395592
Tomai, M., Lauriola, M., and Caputo, A. (2019). Are social support and coping styles differently associated with adjustment to cancer in early and advanced stages? Mediterr. J. Clin. Psychol. 7, 71–24. doi: 10.6092/2282-1619/2019.7.1983
Usta, Y. Y. (2012). Importance of social support in cancer patients. Asian Pac. J. Cancer Prev. 13, 3569–3572. doi: 10.7314/APJCP.2012.13.8.3569
Van Dam, H. A., Van Der Horst, F. G., Knoops, L., Ryckman, R. M., Crebolder, H. F. J. M., and Van Den Borne, B. H. W. (2005). Social support in diabetes: a systematic review of controlled intervention studies. Patient Educ. Couns. 59, 1–12. doi: 10.1016/j.pec.2004.11.001
van der Ark, L. A. (2007). Mokken scale analysis in R. J. Stat. Softw. 20, 1–19. doi: 10.18637/jss.v020.i11
Venkatesh, S., and Weatherspoon, L. (2013). Social and health care provider support in diabetes self-management. Am. J. Health Behav. 37, 112–121. doi: 10.5993/AJHB.37.1.13
Wang, X., Cai, L., Qian, J., and Peng, J. (2014). Social support moderates stress effects on depression. Int. J. Ment. Heal. Syst. 8:41. doi: 10.1186/1752-4458-8-41
Wardian, J., and Sun, F. (2014). Factors associated with diabetes-related distress: implications for diabetes self-management. Soc. Work Health Care 53, 364–381. doi: 10.1080/00981389.2014.884038
Wenrich, M. D., Curtis, J. R., Ambrozy, D. A., Carline, J. D., Shannon, S. E., and Ramsey, P. G. (2003). Dying patients’ need for emotional support and personalized care from physicians: perspectives of patients with terminal illness, families, and health care providers. J. Pain Symptom Manag. 25, 236–246. doi: 10.1016/S0885-3924(02)00694-2
White, K. R., and Begun, J. W. (1998). How does catholic hospital sponsorship affect services provided? Inquiry 35, 398–407.
White, K. R., Chou, T. H., and Dandi, R. (2010). Catholic hospital services for vulnerable populations: are system values sufficient determinants? Health Care Manag. Rev. 35, 175–186. doi: 10.1097/HMR.0b013e3181cafa20
Whitley, R. (2012). Religious competence as cultural competence. Transcult. Psychiatry 49, 245–260. doi: 10.1177/1363461512439088
Yağmur, Y., and Duman, M. (2016). The relationship between the social support level perceived by patients with gynecologic cancer and mental adjustment to cancer. Int. J. Gynecol. Obstet. 134, 208–211. doi: 10.1016/j.ijgo.2015.12.010
Keywords: social support, healthcare, day treatment, cancer patients, scale construction and validation
Citation: Tomai M and Lauriola M (2022) Separate but Related: Dimensions of Healthcare Provider Social Support in Day-Treatment Oncology Units. Front. Psychol. 13:773447. doi: 10.3389/fpsyg.2022.773447
Received: 09 September 2021; Accepted: 08 March 2022;
Published: 22 April 2022.
Edited by:
Paola Gremigni, University of Bologna, ItalyReviewed by:
Ilaria Setti, University of Pavia, ItalyCopyright © 2022 Tomai and Lauriola. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Manuela Tomai, bWFudWVsYS50b21haUB1bmlyb21hMS5pdA==; Marco Lauriola, bWFyY28ubGF1cmlvbGFAdW5pcm9tYTEuaXQ=
†These authors have contributed equally to this work and share first authorship
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.