
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 03 March 2022
Sec. Psychopathology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.737513
 Sherryl H. Goodman1
Sherryl H. Goodman1 Maria Muzik2,3
Maria Muzik2,3 Diana I. Simeonova1
Diana I. Simeonova1 Sharon A. Kidd4
Sharon A. Kidd4 Margaret Tresch Owen5
Margaret Tresch Owen5 Bruce Cooper4
Bruce Cooper4 Christine Y. Kim1,6
Christine Y. Kim1,6 Katherine L. Rosenblum2,3
Katherine L. Rosenblum2,3 Sandra J. Weiss4*
Sandra J. Weiss4*Ample research links mothers’ postpartum depression (PPD) to adverse interactions with their infants. However, most studies relied on general population samples, whereas a substantial number of women are at elevated depression risk. The purpose of this study was to describe mothers’ interactions with their 6- and 12-month-old infants among women at elevated risk, although with a range of symptom severity. We also identified higher-order factors that best characterized the interactions and tested longitudinal consistency of these factors from 6 to 12 months of infant age. We leveraged data from eight projects across the United States (n = 647), using standardized depression measures and an adaptation of the NICHD Mother-Infant Interaction Scales. Overall, these depression-vulnerable mothers showed high levels of sensitivity and positive regard and low levels of intrusiveness, detachment, and negative regard with their infants. Factor analyses of maternal behaviors identified two overarching factors—“positive engagement” and “negative intrusiveness” that were comparable at 6 and 12 months of infant age. Mothers’ ability to regulate depressed mood was a key behavior that defined “positive engagement” in factor loadings. An exceptionally strong loading of intrusiveness on the second factor suggested its central importance for women at elevated depression risk. Mothers with severe depressive symptoms had significantly more “negative intrusiveness” and less “positive engagement” with their 6-month-old infants than women with moderate or fewer depressive symptoms, suggesting a potential tipping point at which symptoms may interfere with the quality of care. Results provide the foundation for further research into predictors and moderators of women’s interactions with their infant among women at elevated risk for PPD. They also indicate a need for evidence-based interventions that can support more severely depressed women in providing optimal care.
Postpartum depression (PPD) occurs in approximately 13% of women (Bauman et al., 2020) and is associated (concurrently and prospectively) with adverse psychological and developmental functioning in children (Stein et al., 2014; Weiss and Leung, 2021). Efforts to understand why or how PPD is linked to offspring functioning suggest the salience of interactions between mothers and their infants in mediating outcomes (Murray et al., 2015; Jones et al., 2019; Goodman et al., 2020; Pelham et al., 2021). The qualities of mothers’ interactions with their infants can be reliably and validly measured with observational coding or rating (Tryphonopoulos et al., 2016; Bornstein et al., 2020). Elevated depressive symptom levels have been associated with maternal interactions that are more negative or coercive, less positive, and more disengaged (Lovejoy et al., 2000; Hakanen et al., 2019), albeit not all mothers with elevated depression exhibit such behaviors (Goodman et al., 2017; Weiss and Leung, 2021). Yet, it is unclear whether these qualities of parenting generalize to mothers who are at elevated risk for PPD but do not necessarily have PPD or experience high symptom levels. Better understanding the nature of maternal interactions among these women can enhance our ability to target our interventions more effectively and prevent potentially adverse outcomes for children. Thus, we aimed to identify higher-order factors that best characterize maternal behaviors of women at risk for PPD when interacting with their 6-month-old infants and to test the longitudinal consistency of these factors from 6 to 12 months of infant age.
Population-based research shows that, among women in general, risk factors for PPD are highly prevalent, and their presence may be more the norm than the exception (Norhayati et al., 2015; Zhao and Zhang, 2020; Ahmad et al., 2021; Liu et al., 2021). Recent reviews of research to date have identified primary risks for PPD. These include the following: a previous history of depression and anxiety (including depression during pregnancy), negative attitudes toward the pregnancy, premenstrual syndrome, stressful life events (including parenting stress), a history of abuse, current domestic violence, perinatal complications, and a high-risk pregnancy, having a low birth weight or prematurely born infant, hormonal dysregulation, young age, socioeconomic disadvantage, sleep dysfunction, nutritional deficiencies, lack of exercise, lack of social support, acculturation, and marital or partner dissatisfaction (Ghaedrahmati et al., 2017; Chen et al., 2019; Hutchens and Kearney, 2020). From among these many factors, we focus on three in this study: (1) history of depression, including bipolar depression (Bukh et al., 2016; Mandelli et al., 2016; Silverman et al., 2017; Buckman et al., 2018), (2) having a medically high-risk pregnancy or a preterm, low birth weight infant (Carson et al., 2015; Hawes et al., 2016; Shlomi Polachek et al., 2016; de Paula Eduardo et al., 2019), and (3) a history of childhood maltreatment (Hutchens et al., 2017; Humphreys et al., 2020; Perry et al., 2020; Weiss et al., 2021). We were able to leverage data from women representing these important risk populations from previously funded studies of our research group. Availability of these data presented an important opportunity to expand knowledge about these risks. Sampling such populations, relative to general population samples, may yield a more ecologically valid representation of populations experiencing PPD.
A focus on women at elevated risk for PPD is important for three reasons. First are the high rates of occurrence in the population for these particular risk groups. Among US women, approximately 22% experience depression in contrast to 15% of men (Centers for Disease Control and Prevention (CDC), 2020). The lifetime prevalence of delivering a preterm, low birth weight infant is on average 12%, but with substantially higher percentages among women of specific racial/ethnic groups (Schaaf et al., 2013; Frey and Klebanoff, 2016; Keiser et al., 2019). The prevalence of various types of childhood maltreatment is also substantial, including 20% for sexual abuse, 22% for physical abuse, and 28.4% for emotional abuse among women in North America (Stoltenborgh et al., 2015; Moody et al., 2018).
Second, each of these elevated risks for PPD pose risks for adverse outcomes for the offspring. Depression in women during the perinatal period is reliably associated with elevated risk for the development of a broad range of adverse outcomes in offspring, beginning during infancy (Goodman and Lusby, 2014) and throughout development (Stein et al., 2014). Research indicates that children of mothers with bipolar depression are at particular risk of psychopathology and varied developmental problems (Lau et al., 2018), including mood and sleeping disorders (Sandstrom et al., 2019; Wescott et al., 2019). Among women with a preterm, low birth weight infant, PPD has also been linked to the child’s emotional and behavioral problems (Gueron-Sela et al., 2015; Kleine et al., 2021), including depressive and anxiety disorders (Weiss and Leung, 2021). Similarly, PPD among women who experience trauma has been associated with their child’s increased risk of emotional and behavioral problems (Choi et al., 2017). Plant et al. (2017) found that the effects of PPD in traumatized women carried forward into early adolescence of the offspring, with maladaptive parenting playing a mediating role.
A third reason to focus on women at elevated risk for depression stems from previous studies of interactions with their infants. Women’s history of depression is associated with their providing less optimal qualities of interaction with their young children, even when symptom-free (Kluczniok et al., 2016) while mothers’ bipolar depression is associated with less attunement and less dyadic coordination (Anke et al., 2019). A history of child maltreatment is linked to less sensitivity toward infants by mothers (Fuchs et al., 2017), and having a medically fragile infant (such as those born prematurely) is related to more intrusive behavior as well as greater remoteness and negative affect when mothers are depressed (Neri et al., 2015). Findings from these studies raise concern about maternal interactions among these groups of women who are at elevated risk for PPD. However, many of the previous studies are of small samples and examine each risk factor in isolation, despite knowledge that risk factors co-occur (Goodman and Tully, 2009). There is a lack of knowledge about maternal behavior that may cross-over risk factors and be more generally representative of women at elevated risk. Moreover, researchers often rely on idiosyncratic approaches to measuring mothers’ qualities of interacting with their infant, giving less attention to higher-order constructs that may characterize interactions with the infant across high-risk populations.
In the study described here, we address these shortcomings by examining mothers’ interactions with infants among a relatively large sample that includes women with a range of symptom severity and across a spectrum of these risks for PPD. In addition, we extend studies of individual parenting characteristics that have used a well-established measure of mother–infant interaction by identifying overarching constructs from interaction qualities in the measure that are salient for mothers at elevated depression risk. Our specific aims were as follows: (1) to describe mothers’ interaction with their infants among a group of women at elevated risk for PPD, including qualities of interaction particularly salient to depression; (2) to identify higher-order factors that best characterize maternal behaviors of women at risk for PPD when interacting with their 6-month-old infants, (3) and to test the longitudinal consistency of these factors from 6 to 12 months of infant age. Although our primary focus was to identify overarching constructs that reflect maternal interactions in high-risk groups regardless of symptom severity, we also examined differences in these interactions based on level of depression severity.
To address our aims, we leveraged and merged data from eight samples of women at diverse risk for PPD. These samples were derived from a network of researchers affiliated with the National Network of Depression Centers, each of whom had obtained video-recorded observations of mother–infant interaction as part of previously funded research with women at heightened risk for PPD. The eight samples were from three universities in different geographic regions of the United States (California, Georgia, Michigan). Three of the projects were conducted at X University, three at University of XX, and two at University of XXX. All women in these projects ranged from 18 to 45 years of age. X University: In two projects, women were recruited during pregnancy from hospital and community clinics and had a history of a primary diagnosis of Major Depressive Disorder. In the 3rd project, women were recruited through a Women’s Health Program in the Department of Psychiatry and Behavioral Sciences and had a history of Bipolar I or Bipolar II Disorder. All women and their infants were followed from pregnancy to 12 months postnatal, collecting data at various time points. University of XX: All women from projects at XX had either delivered a preterm infant or were at risk of preterm delivery when enrolled in the study. Women in two XX projects were recruited from neonatal intensive care units in three major teaching hospitals while women in the 3rd project were recruited from obstetric clinics affiliated with XX, the Public Health Department or the city’s General Hospital. One study followed women and their infants from recruitment during the 1st week of life through 6 months postnatal. In a second study, they were followed from birth to 2 years of age, and in the last study, women were followed from the 3rd trimester of pregnancy to 12 months postnatal. Data were collected at various time points throughout the projects. University of XXX: In one study, women were recruited either during pregnancy or within the first 4 months postpartum and had a history of childhood maltreatment (sexual, physical, and emotional abuse or neglect). In the second project, they were enrolled in the first 12 weeks of pregnancy and had a history of Major Depressive Disorder. Women were recruited either from three prenatal care clinics or through community advertisement. Women and their infants were followed from enrollment to 14 or 18 months postpartum (depending on the project), collecting data at various time points.
Although the eight research projects recruited women at different time points to address the specific goals of their original funding, all had data on women’s depression and interactions with their infants at 6 months postpartum. Each project used (a) questionnaires and interviews to measure sample characteristics and depression, and (b) video records to capture mothers’ interactions (n = 647 at infant age 6 months; n = 346 at 12 months). Six out of the eight projects collected data at 12 months of infant age, allowing for a test of consistency (internal validity) of the parenting constructs that would be derived from the 6 months data. Institutional Review Boards at the three universities approved the research projects.
All projects had similar recruitment approaches, with participants being recruited either during pregnancy or in the early postpartum at obstetric and/or neonatal units or through advertisements. Further, all participants were at elevated risk of depression, with risk defined as women with either: (a) a history of major depressive disorder or bipolar disorder; (b) a history of childhood maltreatment; or (c) delivery of a preterm or low birth weight infant.
Each project measured mothers’ depression symptom severity at infants’ ages 6 and 12 months with either: the Beck Depression Inventory (Beck et al., 1988, 1997), the Postpartum Depression Screening Scale (Beck and Gable, 2000), or the Patient Health Questionnaire-9 (Kroenke et al., 2001). Each of these measures has established validity and reliability, including for perinatal populations. We harmonized depression data by using validated cut-points for each measure that have been determined previously by researchers who developed the measures (Beck et al., 1997; Beck and Gable, 2001; Kroenke et al., 2001). Based on these cut-points, we combined women across projects into comparable depression severity groups (i.e., none or minimal, mild, moderate, and severe) at each of the two infant ages. An ordinal variable was created for each cut-point (e.g., 1 = none or minimal depression and 2 = mild depression) that allowed us to group women across projects who met criteria for each category when performing our analyses.
In all of our study projects, mothers’ interaction was observed during an unstructured free-play procedure, with the same basic instructions to mothers to “please play with your baby in a way that is typical for you.” These similarities reduced the likelihood of confounding effects from different interactional scenarios. In order to standardize timing of the ratings, we followed a practice, common in the field, of rating the first 5 minutes of directed play interaction for all videos, regardless of duration (e.g., Hirsh-Pasek et al., 2015). In their meta-analytic review of mothers’ depression in relation to parent–child interaction qualities, Lovejoy et al. (2000) found weak and inconsistent evidence that interaction duration was a moderator. Further supporting the use of 5-min observational samples, a large longitudinal study reported evidence for construct validity of a latent parenting construct derived from observational ratings of a 5-min teaching task (Nordahl et al., 2020).
Although the context for assessment of mother interaction had many similarities across the studies, protocols of the different projects varied in whether observations occurred at home or in a lab. However, we examined the effects of the setting in which observations were recorded as well as the effect of project site and found that they did not influence mothers’ interaction. In tests of between-subjects effects using a general linear model, partial eta squared tests for effect size of project site (a, b, c) ranged from 0.000 to 0.004 (at p = 0.34 or greater); for effect size of setting (lab versus home) ranged from 0.002 to 0.003, at p = 0.19 or greater.
We used a well-regarded rating system from the NICHD Study of Early Child Care and Youth Development (SECCYD) to analyze qualities of mothers’ interaction from video records (see NICHD Early Child Care Research Network, 1999). Although the original NICHD SECCYD mother–infant interaction rating system also included infant rating items and one dyadic item, we used only the parent items in the study reported here. In addition, we added two items from the Parent-Child Early Relational Assessment (Clark, 1985) to enhance salience of the rating system for comorbid mood problems common in interactions of women at risk of depression. These items included mothers’ Depressed/Withdrawn/Apathetic Mood and Anxious Mood. Our final measure consisted of nine items: Sensitivity/Responsiveness to Distress, Sensitivity/Responsiveness to Nondistress, Intrusiveness, Detachment/Disengagement, Stimulation of Development, Positive Regard for the Child, Negative Regard for the Child, Depressed/Withdrawn/Apathetic Mood, and Anxious Mood.
We used 5-point versions of the rating scales, from 1 (not at all characteristic) to 5 (highly characteristic), which were expansions of the original 4-item version (Owen, 2006). Several large-scale longitudinal studies have used the 5-point and/or a 7-point version (Mills-Koonce et al., 2007; Nordahl et al., 2020). This rating system yields strong evidence for reliability and validity, including inter-rater reliability estimates (Fuligni and Brooks-Gunn, 2013). Predictive validity includes support from the NICHD SECCYD and other work (e.g., Campbell et al., 2004; Booth-LaForce and Oxford, 2008; Norcross et al., 2017). Overall, the rating system has shown a high level of validity as a measure of mother–infant relationship quality.
The two items included from the Parent-Child Early Relational Assessment are also rated on a 5-point Likert-type scale (PCERA; Clark, 1999). The PCERA has good discriminant validity, distinguishing between parents based on various definitions of high risk (e.g., psychiatric diagnoses), and is sensitive to therapeutic intervention change (Clark, 1999; Clark et al., 2008; Unternaehrer et al., 2019). In factor analytic work, depressed/withdrawn/apathetic mood (reverse scored) loaded on a factor of Parental Positive Affective Involvement and Verbalization; anxious mood loaded on a factor of Parental Intrusiveness, Insensitivity, and Inconsistency (Clark, 1999).
At each site, at least two research assistants completed the ratings. We followed recommended procedures in training observers to obtain and maintain reliability (Bakeman and Goodman, 2019). We took several steps to achieve the criterion we set for reliability: observers differing by no more than 1 point on no more than 4 items for ratings of 4 consecutive videos relative to “master ratings” of an expert who had been responsible for the centralized coding of parent–child interactions in the NICHD SECCYD. Once observers met this criterion, they independently rated all the videos with 6-month-olds. Prior to rating the videos with 12-month-olds, observers participated in a brief training on developmental norms for this age and discussed how observations might differ for various items from mothers’ interactions with 6-month-old infants. We required observers to meet the criterion for reliability for coding videos of 12-month-old infants, based on our expert’s “master ratings” of 12-month-olds.
We determined inter-observer reliability by having at least 20% of randomly selected video segments at each infant age rated by a second trained observer. Across sites, observers had adequate agreement as determined by being within 1 point on each rating scale, that is, greater than 0.80 on all items. They had agreement between 0.90 and 1.00 on most items. All sites used one REDCap database to enter ratings as well as information on the context within which the interaction occurred and the video quality. Using a double data entry system for accuracy, there were errors of less than 1% across sites.
To examine Aim 1, we used descriptive statistics to compute sample means for the rating items at each age. For Aim 2, we used two methods to identify factors that might reflect underlying constructs that could characterize maternal interaction behavior. First, we estimated exploratory factor analyses (EFA) to determine how specific rating items might group together to form latent variables. We computed the EFA with the item scores from mothers’ interactions with their 6-month-old infants. Then, we performed a confirmatory factor analysis (CFA) to determine how well the factor structure identified at 6 months fit the items rated when infants were 12 months old. This latter measurement model addressed our aim of testing the longitudinal consistency of these factors from 6 to 12 months of infant age (Aim 3).
Because the rating scales were short Likert-type scales and many of their distributions were skewed, they did not meet the necessary assumptions for ordinary least squares analyses using product–moment correlations. Thus, we used an EFA using robust maximum likelihood (MLR) with a probit link for both 6- and 12-month items, treating indicators as ordinal. We carried out the EFAs for both ages using GEOMIN oblique rotation to assist in achieving a solution with simple structure, while still allowing factors to be correlated. In this approach, we expected each factor to have item loadings of 0.40 or larger and expected items to load strongly on a single factor. Given the number of items, we examined from one- to three-factor solutions only. In addition to evaluating the pattern matrices estimated with the oblique rotation, we examined the scree plot of eigenvalues. We computed the CFA at 12 months to establish that the factors at 12 months had support for metric invariance when compared with those from the 6-month solution. Further, we examined the 6- and 12-month factor structures in the same model, with MLR and a probit link, using numerical integration with Monte Carlo estimation. This analysis employed full information maximum likelihood (FIML) with the expectation–maximization algorithm to accommodate missing data at 12 months.
Lastly, we employed general linear models to examine differences in mean scores on the factors we identified across women who had varying levels of depression severity at each infant age. We carried out statistical analyses with Stata 15 and Mplus. We evaluated all tests of significance with a two-sided alpha of 0.05.
Women were, on average, 31.3 years old (±5.9). 87.5% were married or lived with a partner. Most women had a bachelor’s degree or some graduate education (63%). 66% reported their racial and ethnic heritage as White/European American, 15% were Black/African American, 10% were Hispanic American/Latina, 6% were Asian American, and 3% reported other or mixed race/ethnicity. 17% received government assistance and were below the poverty level. A third of the women reported minimal satisfaction with the support they were receiving. In addition, 21% met the threshold for clinical anxiety and 33% reported a history of physical or sexual abuse. Infants’ average gestational age at birth was 36.7 weeks (±4.1); 30% were born preterm. Male to female split among infants was 50:50. Further details can be found in Table 1.
At 6 months postpartum, 7.7% (n = 50) of the women reported severe depressive symptoms, 14.7% (n = 95) reported moderate symptoms, 19.2% (n = 124) reported mild depression, and 58% (n = 378) had minimal or no depressive symptoms. At 12 months postpartum, 5.8% (n = 20) of the women met criteria for severe depression. 7.8% (n = 27) of the women reported moderate symptoms, 15% (n = 52) reported mild depression, and 71.4% (n = 247) endorsed minimal or no depressive symptoms.
Table 2 presents the rating scale item means and standard deviations at each age. Given few instances of infant distress, we eliminated consideration of the item Sensitivity to Distress. Item means indicate that observers rated mothers in our sample as being on the higher end for sensitivity and positive regard, in the moderate range of cognitive stimulation, and low on intrusiveness, detachment, and negative regard. Table 3 shows bivariate correlations among items. Overall, items had significant relationships with one another. An exception is the item anxious mood, which had low correlations with other items at 6 months and non-significant relationships with all but one item (negative regard) at 12 months.
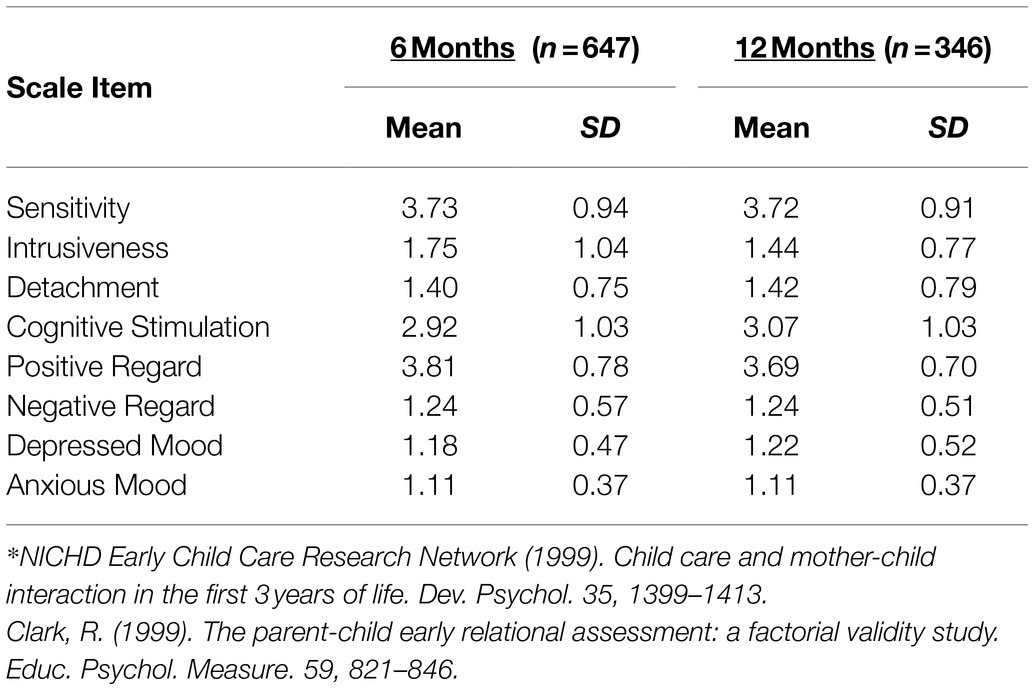
Table 2. Means and standard deviations (SD) for interaction rating scale* item scores at infant ages 6 and 12 months.
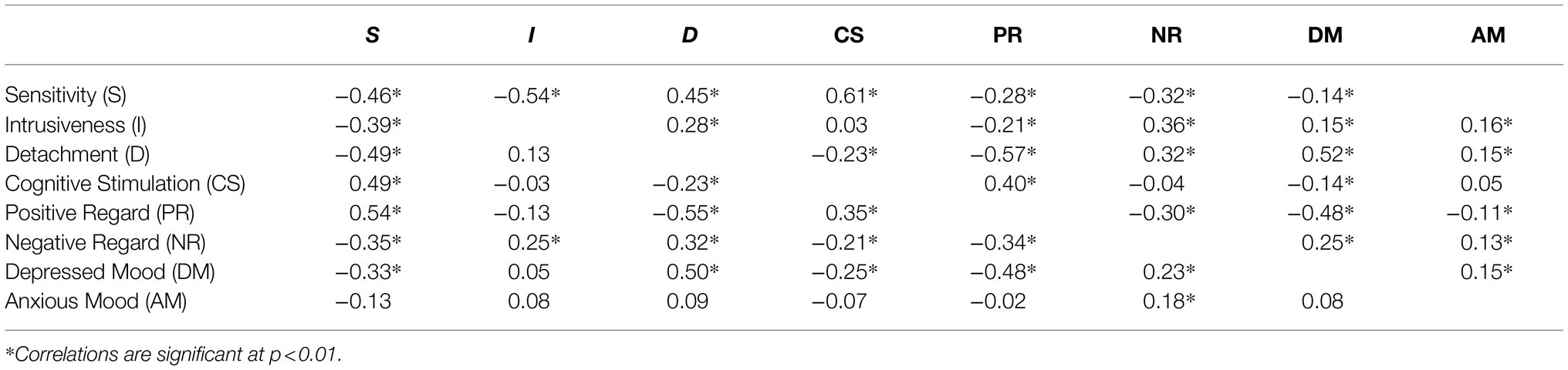
Table 3. Bivariate spearman correlations for mothers’ interaction items at 6 months (upper triangle) and 12 months (lower triangle) postpartum.
A scree plot for initial EFA on items rating mothers’ interaction with their 6-month-olds (see Figure 1) indicates that the eigenvalue for one of the factors was quite strong (λ = 4.10), explaining much of the variance in the rating items. However, a second factor also exceeded an eigenvalue of 1 (λ = 1.25), with one being the accepted minimal criterion for a factor to be useful in explaining the variance contributed to a construct by at least two items in the measure. Based on these findings, we examined both a one- and two-factor solution in our EFA.
In the EFA for the one-factor solution, anxious mood did not meet the criterion of 0.40 to be retained in a well-defined factor. The Bayesian Information Criterion (BIC) was 9241.22. A two-factor solution using geomin oblique rotation improved the BIC to 9082.23. In addition, a chi-square difference of 320.50 (df = 7, p = 0.000) between models indicated that the 2-factor solution significantly improved the fit. The item anxious mood again did not load on either factor (loadings were −0.23 and 0.24, respectively). In light of this finding, we computed the final EFA for the 6-month ratings of maternal behavior without anxious mood. Loadings for the final two-factor solution are shown in Table 4.
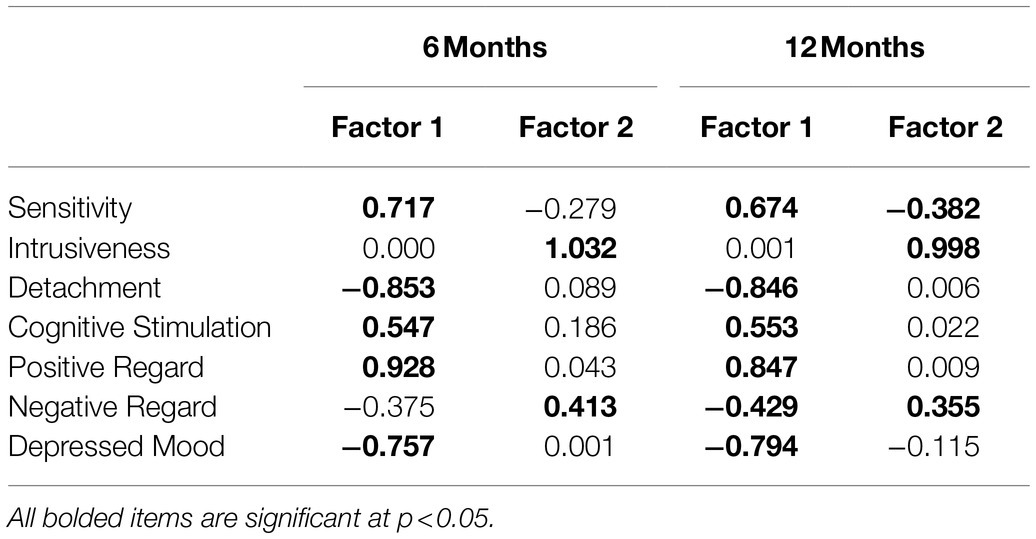
Table 4. Final factor loadings for two-factor solution of scale items reflecting maternal behaviors at 6 and 12 months postpartum.
Using the established criterion of 0.40 as a desired loading for a well-defined factor, Factor 1 consisted of five items: positive regard, sensitivity, cognitive stimulation, detachment (negatively loaded), and depressed/withdrawn/apathetic mood (negatively loaded). We defined this factor as Positive Engagement. Factor 2 consisted of two items: intrusiveness and negative regard, which we labeled Negative Intrusiveness. The two factors were moderately intercorrelated, r = −0.39, p = 0.0000.
Factor loadings for a 2-factor structure of mothers’ interactions with their 12-month-old infants are shown in Table 4, again using goemin oblique rotation. Items loaded in a similar pattern to that found for the 6-month data, with sensitivity, detachment, cognitive stimulation, positive regard, and depressed mood all clearly loading on one factor while intrusiveness loaded on another. The only difference between the 6- and 12-month loadings was for negative regard. As with the 6-month data, it cross-loaded on both factors. However, the strength of its loading was slightly stronger on Factor 1 than on Factor 2 at 12 months. When we estimated factor structure for both 6- and 12-month data in the same model (using FIML with the probit link and an EMA algorithm), the pattern of coefficients was consistent with our prior analyses, supporting a cross-loading of negative regard on both factors and its slightly stronger loading on Factor 1 than Factor 2 at 12 months. Finally, we estimated an additional model in which the factor loadings were constrained to be the same for each item. For example, the factor loading for the item positive regard was constrained to be equal on the first factor for the 6-month data and the 12-month data. In comparing the BIC of the constrained model (12949.62) to that of the unconstrained model (12991.72), the constrained model showed a significant improvement in fit by 50 points. This provides evidence that the constrained model fits the data better than a model with factor loadings free to vary, supporting metric invariance of the 6- and 12-month factor solutions.
Table 5 shows data on differences for factor scores of women who had varied degrees of symptom severity at both infant ages. With 6-month-old infants, women with severe depressive symptoms differed significantly on both factor scores from women in all other symptom groups. Women classified as having severe depressive symptoms were significantly lower on Factor 1, F = 4.04 (df = 3), p = 0.007, and significantly higher on Factor 2, F = 7.48 (df = 3), p = 0.000. With their 12-month-old infants, maternal symptom severity was not associated with scores on either factor. Analyses of variance yielded F = 0.92 (df = 3), p = 0.43 for Factor 1 and F = 1.98 (df = 3), p = 0.12 for Factor 2.
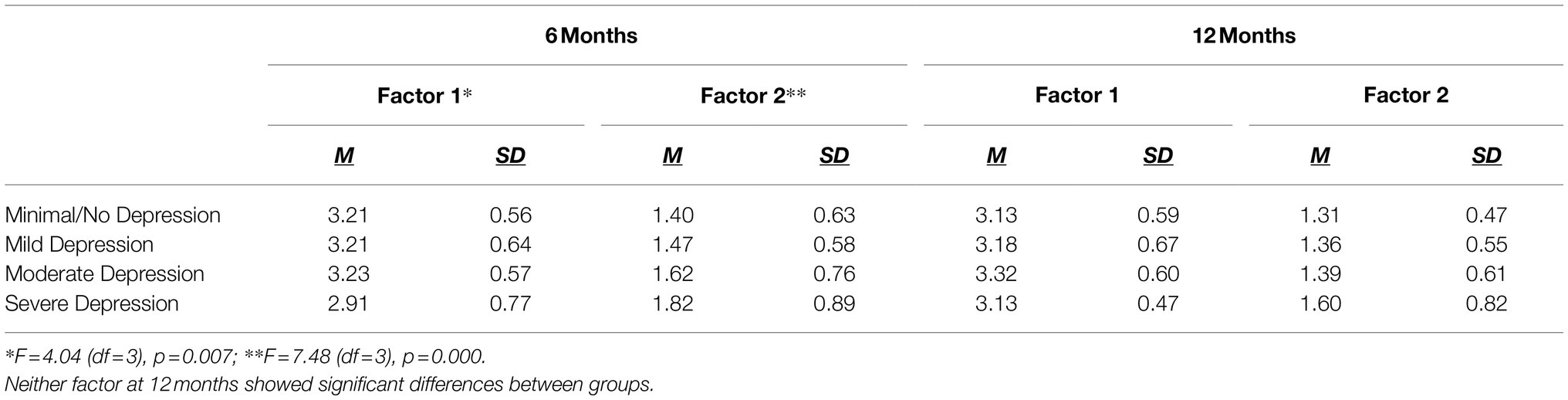
Table 5. Factor scores for women with different degrees of depression severity at 6 and 12 months postpartum.
Understanding interaction with infants among women with PPD is important given evidence that qualities of interaction may mediate associations between PPD and offspring’s development of psychopathology (Goodman et al., 2020). However, research efforts to understand mother–infant interaction in women with PPD may be misinformed if they do not study women at elevated risk for PPD who have a range of symptoms, including women who present with minimal or no symptoms in spite of elevated risk. To address this important gap in knowledge, we took advantage of a consortium of researchers affiliated with the National Network of Depression Centers, harmonizing data from eight projects that had enrolled women at elevated risk for PPD and had video records of mother–infant interactions.
As a result of their elevated risk, the prevalence and severity of mothers’ depression in our sample were higher than is typically reported for the general population, whether with convenience- or population-based sampling. Approximately 22% of women reported moderate to severe depressive symptoms (indicative of clinically significant depression) when their infant was 6 months old, declining to about 14% when the infant was 12 months of age. Putnick et al. (2020) identified varied trajectories of PPD symptoms over time in a large, population-based birth cohort: (1) high, persistent symptoms, (2) low stable symptoms, (3) initially low but increasing symptoms over time, and (4) initially moderate symptoms that decreased over time. They found the largest group of women to have persistently low stable symptoms. As a whole, women in our sample appeared to reflect a trajectory involving mild to moderate symptoms that decreased from 6 to 12 months postpartum. However, we did observe a subgroup of about 7.7% of women in our sample who had more severe symptoms that appeared to persist through 12 months.
Overall, mothers’ interaction with their infants showed relatively high levels of sensitivity and positive regard, moderate levels of developmental stimulation, and low intrusiveness, detachment, and depressed or anxious mood. Our descriptive finding that mothers’ interactions were relatively high on positive qualities and relatively low on negative qualities may be explained in several ways. First, although our samples of mothers were all at high risk for PPD, they were, on average, low in sociodemographic risk. Being relatively well-resourced may enhance positive parenting directly or indirectly, protecting against negative effects of PPD on mother–infant interaction (e.g., Martinez-Torteya et al., 2014). Second, this pattern of findings is consistent with other research demonstrating that not all mothers at risk for PPD have poor quality interaction with their infants (e.g., Goodman et al., 2017; Weiss and Leung, 2021). Interactions with infants are not determined by any single factor, such as risk for PPD, but by multiple factors, including the mother’s personal psychological resources, children’s characteristics, and contextual factors (Belsky and Jaffee, 2006). Third, women with mild to moderate depressed states, the majority of our sample, may be more able to readily engage in positive interactions with their infants (Pechtel et al., 2013). This hypothesis was supported by our finding that more severely depressed mothers, relative to mothers with lower symptom levels, had less positive engagement and more negative intrusiveness when interacting with their infants.
In contrast to our findings showing relatively high positive qualities and relatively low negative qualities of maternal interaction, the women in our sample provided, on average, only a moderate degree of cognitive stimulation with their infants. We found that cognitive stimulation, characterized by engagement in activities that can facilitate learning, such as focusing the infant’s attention on perceptual qualities (sounds, colors, movement), was significantly, inversely associated with ratings of mothers on depressed mood during their interactions with infants. This is consistent with Hakanen et al.’s (2019) finding that mothers’ depressive symptoms were associated with lower structuring when interacting with their 6-month-old infants. These findings are also consistent with other studies showing that non-postpartum adult populations with depression show cognitive impairment even when in remission (Listunova et al., 2018). Although we demonstrated a link between reduced cognitive stimulation and depressed mood, we need to interpret findings for the entire sample with caution since women in our study experienced a spectrum of depression, from no symptoms to severe symptoms.
From among the individual qualities of maternal interaction just described, we found support for two overarching factors. One represented positive behavior (higher sensitivity, positive regard and cognitive stimulation, and lower detachment and depressed mood), and the other represented negative behavior (intrusiveness and negative regard). Given that the strongest loadings on our first factor were for a low degree of detachment and a high degree of positive regard, we named it Positive Engagement. We named our second-factor Negative Intrusiveness. Although the strength of specific items and the resulting names given the factors vary, our identification of two key factors (Positive Engagement and Negative Intrusiveness) is congruent with findings from general population samples that have used the NICHD SECCYD rating system (Mills-Koonce et al., 2007; Burchinal et al., 2008; Hibel et al., 2011; Willoughby et al., 2013).
Our Positive Engagement factor has similar items to the Positive Sensitivity factor in these previous studies, consisting of sensitivity/responsiveness, detachment [reverse scored], positive regard, animation, and stimulation of development. However, positive regard and a strong degree of engagement with the infant were the items carrying the strongest weights in our first factor, rather than sensitivity per se. Also, our unique inclusion of the item on depressed mood enabled us to show that mothers’ ability to regulate or manage any depressed affect/behavior in their interactions with infants may be a key component of the Positive Engagement factor. With women at elevated risk for PPD, this depressed mood item may be particularly informative, tapping qualities such as blunted or restricted affect and apathetic, listless behavior when interacting with the infant. The item, animation (energy level), included in some studies of general populations, may assess one dimension of depressed affect and behavior, but not its affective complexity.
Our second factor, Negative Intrusiveness, in line with Hibel et al. (2011) conceptualization, provides strong support for intrusiveness and negative regard as behaviors constituting a second higher-order construct in mother–infant interactions among women at risk for PPD. For our sample of women at elevated risk, the strong factor loadings for intrusiveness at both 6 and 12 months indicate its central importance as a construct within this population, in contrast to some studies of community samples where intrusiveness did not load on any factor (Mills-Koonce et al., 2015; Nordahl et al., 2020).
The rating item anxious mood did not load significantly on either of the two factors we identified. This finding is somewhat surprising in light of the recognized comorbidity of depression and anxiety, including in postpartum women (Goodman and Tully, 2009; Flynn et al., 2018; Weiss et al., 2021) and the related potential for their synchronous effects on interaction. However, we observed generally low levels of anxious behavior at both time points. We hypothesize that women’s potential comorbid anxiety may have presented itself through other interaction items, both in our first factor where disengagement was a central maternal behavior and in our second factor of negative intrusiveness. Further study is needed to understand the role of observed anxiety in mother–infant interactions among women at high risk for PPD.
Our factor analyses showed overall support for the same two factors for mothers’ interactions with their 6- and 12-month-old infants. The maternal behavior of negative regard was the only one that seemed questionable. It cross-loaded on the factors at both time points but loaded a bit more strongly on the negative intrusiveness factor at 6 months and on the positive engagement factor (reverse scored) at 12 months. However, the loadings were both significant and their strength was very similar. Conceptually, negative regard is more congruent with the negative intrusiveness factor, as we more clearly found in the 6-month factor solution. The pattern of coefficients across factor solutions at 6 and 12 months of infant age as well as their valences were very consistent across the two time points.
Our results showed significantly higher levels of negative intrusiveness and lower levels of positive regard with 6-month-old infants among women with concurrent severe depressive symptoms than for women with moderate or fewer depressive symptoms. These findings are consistent with previous research (Slomian et al., 2019) and suggest a certain threshold or tipping point at which mothers have more difficulty managing their symptoms during interactions with their infants, ultimately interfering with the quality of their care. It is noteworthy, however, that the potential effect of more severe depressive symptoms on mothers’ interaction was no longer evident with the 12-month-old infants. Mothers who are more severely depressed may develop improved coping strategies over time, a hypothesis needing examination in future research. Alternatively, although the proportion of women with severe symptoms did not change from 6 months (7.6%) to 12 months (7.4%), our decreased overall sample size at 12 months may have reduced the power to detect significant differences observed at 6 months of infant age.
Overall, our findings should be interpreted within the context of certain limitations. First, although about a third of the sample was not White, most women were married or cohabiting, and college educated. Only 17% were living in poverty. In addition, we recognize that the risk groups we studied are not the only ones at risk of depression. As noted in the introduction, there are many other populations of women at risk of PPD who may have unique mother–infant interactions, including women with minimal or no social support, those with significant socioeconomic disadvantage, or women who are immigrants and have high levels of acculturative stress. Thus, findings may not generalize to women at elevated risk of depression for other reasons. Second, mean levels of observed depressed and anxious mood during mothers’ interactions with infants were low, even in these samples of women at high risk for PPD. Nevertheless, approximately 42% of the women had mild, moderate, or severe depression symptoms. Future studies might consider observing maternal behavior in situations other than free play (e.g., involving stressor paradigms), which may be more challenging to women at risk for PPD, and, thus, more likely to elicit signs of depressed or anxious mood. Third, our use of video recordings of interactions that were collected for previous studies resulted in varied conditions under which interactions were recorded. However, as noted earlier, we examined the effects of the context in which recordings were made as well as the effect of project site and found that they did not influence mothers’ interaction at either 6 or 12 months postpartum. In addition, Lovejoy et al.’s (2000) meta-analytic review found that type of observation (whether structured vs. unstructured or lab vs. home) does not significantly moderate the association between mothers’ depression severity and their interaction with infants.
Despite its limitations, the study has numerous strengths. We leveraged data and video records already available from previous research, applying a common metric and standardized approach. The merging and standardization of our data enabled a much larger and more diverse sample for examining our aims than is typically available in a single study. In addition, we relied on widely used and well-established rating scale items. One of the rating scale’s original authors served as the core trainer for this research and her ratings were used as the “gold standard” for interactions evaluated in the training and reliability process. Another strength was our broad definition of “elevated risk for PPD,” which enhances the external validity of our findings. Finally, we were able to test longitudinal consistency by studying interactions at two infant ages, 6 and 12 months.
Our findings suggest important areas for further research. First, there is a need to determine whether the maternal interactions we identified among our sample of women will generalize to women from other groups of elevated depression risk (e.g., mothers of infants with congenital disorders or women with varied medical problems). Second, we found that cognitive stimulation of infants was quite limited in this sample of mothers and that it was inversely related to depressed mood. More in depth research is needed to understand how mothers’ depressed mood may undermine the ability to enhance their infant’s cognitive development, including both biological and psychological mechanisms. Lastly, identification of factors that may moderate the relationship between more severe depression and mothers’ interactions with infants is critical. Such moderators could represent potential targets for early intervention to prevent adverse effects.
Our findings support the value of screening mothers’ interactions with their infants in ongoing clinical care, using psychometrically sound measures (Weiss and Quides, 2012; Zalewski et al., 2017; Fagan et al., 2019). Such assessments could have profound utility in preventing later developmental and mental health problems for children. Interventions could then be designed that integrate prevention or treatment of women’s depression with enhanced parenting skills, directed especially to women at elevated risk for PPD and the ultimate goal of healthy child development (Muzik et al., 2009; Goodman et al., 2017).
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by University of California, San Francisco; University of Michigan; and Emory University. The participants provided their written informed consent to participate in this study.
SG, MM, and SW designed the study and had oversight of all study components at their respective Universities. SG, SK, CK, and MO had responsibility for procedures related to coding of video-records. BC, SK, and SW were responsible for harmonizing all study data and for statistical analyses to examine research aims. All authors contributed to interpretation of the findings, writing, reviewing and approval of the manuscript.
This research was funded by NICHD, R01 HD084813 [MPIs: SW (Contact), SG, MM]. Other supports to the research include the following: NIMH (MH080147, PI: MM); the Michigan Institute for Clinical and Health Research (UL1TR000433, PI: MM); NIMH (MH065062, PI: Vazquez); NIMH University of Michigan GCRC (M01 RR00042); NICHD (R01 HD081188, PI: SW); NINR (R01 NR002698, PI: SW); Robert C. and Delphine Wentland Eschbach Endowment (PI: SW); NINR (T32 NR016920, PI: SW), NIMH (1P50MH58922-01A1, PI: Nemeroff); NIMH (1 P50 MH077928-01A1, PI: Stowe), NIMH (K23MH096042, PI: DS); Brain & Behavior Research Foundation (PI: DS).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahmad, H. A., Alkhatib, A., and Luo, J. (2021). Prevalence and risk factors of postpartum depression in the Middle East: a systematic review and meta-analysis. BMC Pregnancy Childbirth 21:542. doi: 10.1186/s12884-021-04016-9
Anke, T. M. S., Slinning, K., Moe, V., Brunborg, C., Siqveland, T. S., and Skjelstad, D. V. (2019). Mothers with and without bipolar disorder and their infants: group differences in mother-infant interaction patterns at three months postpartum. BMC Psychiatry 19:292. doi: 10.1186/s12888-019-2275-4
Bakeman, R., and Goodman, S. H. (2019). Inter-observer reliability in clinical research: current issues and discussion of how to establish best practices. J. Abnorm. Psychol. 129, 5–13. doi: 10.1037/abn0000487
Bauman, B. L., Ko, J. Y., Cox, S., D’Angelo, D. V., Warner, L., Folger, S., et al. (2020). Vital signs: postpartum depressive symptoms and provider discussions about perinatal depression — United States, 2018. Morb. Mortal. Wkly. Rep. 69, 575–581. doi: 10.15585/mmwr.mm6919a2
Beck, C. T., and Gable, R. K. (2000). Postpartum depression screening scale: development and psychometric testing. Nurs. Res. 49, 272–282. doi: 10.1097/00006199-200009000-00006
Beck, C., and Gable, R. (2001). Further validation of the postpartum depression screening scale. Nurs. Res. 50, 155–164. doi: 10.1097/00006199-200105000-00005
Beck, A. T., Steer, R. A., and Brown, G. K. (1997). Beck Depression Inventory : 2nd Edn. San Antonio, Texas: The Psychological Corporation.
Beck, A. T., Steer, R. A., and Garbin, M. (1988). Psychometric properties of the beck depression inventory: a review. Clin. Psychol. Rev. 8, 77–100. doi: 10.1016/0272-7358(88)90050-5
Belsky, J., and Jaffee, S. R. (2006). “The multiple determinants of parenting,” in Developmental Psychopathology: Risk, Disorder, and Adaptation. eds. D. Cicchetti and D. J. Cohen (United States: John Wiley & Sons, Inc.), 38–85.
Booth-LaForce, C., and Oxford, M. L. (2008). Trajectories of social withdrawal from grades 1 to 6: prediction from early parenting, attachment, and temperament. Dev. Psychol. 44, 1298–1313. doi: 10.1037/a0012954
Bornstein, M. H., Hahn, C. S., Putnick, D. L., and Esposito, G. (2020). Infant behaviors and maternal parenting practices: short-term reliability assessments. Infant Behav. Dev. 58:101408. doi: 10.1016/j.infbeh.2019.101408
Buckman, J., Underwood, A., Clarke, K., Saunders, R., Hollon, S., Fearon, P., et al. (2018). Risk factors for relapse and recurrence of depression in adults and how they operate: a four-phase systematic review and meta-synthesis. Clin. Psychol. Rev. 64, 13–38. doi: 10.1016/j.cpr.2018.07.005
Bukh, J., Andersen, P., and Kessing, L. (2016). Rates and predictors of remission, recurrence and conversion to bipolar disorder after the first lifetime episode of depression--a prospective 5-year follow-up study. Psychol. Med. 46, 1151–1161. doi: 10.1017/S0033291715002676
Burchinal, M., Vernon-Feagans, L., and Cox, M., Key Family Life Project Investigators (2008). Cumulative social risk, parenting, and infant development in rural low-income communities. Parent. Sci. Pract. 8, 41–69. doi: 10.1080/15295190701830672
Campbell, S. B., Brownell, C. A., Hungerford, A., Spieker, S. J., Mohan, R., and Blessing, J. S. (2004). The course of maternal depressive symptoms and maternal sensitivity as predictors of attachment security at 36 months. Dev. Psychopathol. 16, 231–252. doi: 10.1017/S0954579404044499
Carson, C., Redshaw, M., Gray, R., and Quigley, M. (2015). Risk of psychological distress in parents of preterm children in the first year: evidence from the UK millennium cohort study. BMJ Open 5:e007942. doi: 10.1136/bmjopen-2015-007942
Centers for Disease Control and Prevention (CDC) (2020). Symptoms of depression among adults: United States. National Center for Health Statistics Data Brief No. 379 - September 2020.
Chen, J., Cross, W., Plummer, V., Lam, L., and Tang, S. (2019). A systematic review of prevalence and risk factors of postpartum depression in Chinese immigrant women. Women Birth 32, 487–492. doi: 10.1016/j.wombi.2018.11.019
Choi, K., Sikkema, K., Vythilingum, B., Geerts, L., Faure, S., Watt, M., et al. (2017). Maternal childhood trauma, postpartum depression, and infant outcomes: avoidant affective processing as a potential mechanism. J. Affect. Disord. 211, 107–115. doi: 10.1016/j.jad.2017.01.004
Clark, R. (1985). The Parent-Child Early Relational Assessment: Instrument and Manual. Madison: University of Wisconsin Medical School, Department of Psychiatry.
Clark, R. (1999). The parent-child early relational assessment: A factorial validity study. Educ. Psychol. Meas. 59, 821–846. doi: 10.1177/00131649921970161
Clark, R., Tluczek, A., and Brown, R. (2008). A mother-infant therapy group model for postpartum depression. Infant Ment. Health J. 29, 514–536. doi: 10.1002/imhj.20189
de Paula Eduardo, J., de Rezende, M., Menezes, P., and Del-Ben, C. (2019). Preterm birth as a risk factor for postpartum depression: a systematic review and meta-analysis. J. Affect. Disord. 259, 392–403. doi: 10.1016/j.jad.2019.08.069
Fagan, M. A., Frosch, C. A., Middlemiss, W., LaCoursiere, J. N., Owen, M. T., Hane, A. A., et al. (2019). The practical utility of the welch emotional connection screen for rating parent–infant relational health. Infancy 24, 881–892. doi: 10.1111/infa.12311
Flynn, H., Spino, C., Guille, C., Deligiannidis, K., Maki, P., Jahnke, J., et al. (2018). A collaborative, network-based approach to advance women’s depression research in the US. J. Women Health 27, 51–57. doi: 10.1089/jwh.2016.6261
Frey, H. A., and Klebanoff, M. A. (2016). The epidemiology, etiology, and costs of preterm birth. Semin. Fetal Neonatal Med. 21, 68–73. doi: 10.1016/j.siny.2015.12.011
Fuchs, A., Moehler, E., Resch, F., and Kaess, M. (2017). The effect of a maternal history of childhood abuse on adrenocortical attunement in mothers and their toddlers. Dev. Psychobiol. 59, 639–652. doi: 10.1002/dev.21531
Fuligni, A. S., and Brooks-Gunn, J. (2013). Mother–child interactions in early head start: age and ethnic differences in low-income dyads. Parent. Sci. Pract. 13, 1–26. doi: 10.1080/15295192.2013.732422
Ghaedrahmati, M., Kazemi, A., Kheirabadi, G., Ebrahimi, A., and Bahrami, M. (2017). Postpartum depression risk factors: a narrative review. J. Educ. Health Promot. 6:60. doi: 10.4103/jehp.jehp_9_16
Goodman, S. H., Bakeman, R., McCallum, M., Rouse, M. H., and Thompson, S. F. (2017). Extending models of sensitive parenting of infants to women at risk for perinatal depression. Parenting 17, 30–50. doi: 10.1080/15295192.2017.1262181
Goodman, S. H., and Lusby, C. M. (2014). “Early adverse experiences and depression,” in Handbook of Depression. 3rd Edn. eds. I. H. Gotlib and C. L. Hammen (Guilford).
Goodman, S. H., Simon, H. F. M., Shamblaw, A. L., and Kim, C. Y. (2020). Parenting as a mediator of associations between depression in mothers and Children’s functioning: A systematic review and meta-analysis. Clin. Child. Fam. Psychol. Rev. 23, 427–460. doi: 10.1007/s10567-020-00322-4
Goodman, S. H., and Tully, E. C. (2009). Recurrence of depression during pregnancy: psychosocial and personal functioning correlates. Depress. Anxiety 26, 557–567. doi: 10.1002/da.20421
Gueron-Sela, N., Atzaba-, N., Meiri, G., and Marks, K. (2015). The caregiving environment and developmental outcomes of preterm infants: diathesis stress or differential susceptibility effects? Child Dev. 86, 1014–1030. doi: 10.1111/cdev.12359
Hakanen, H., Flykt, M., Sinervä, E., Nolvi, S., Kataja, E., Pelto, J., et al. (2019). How maternal pre- and postnatal symptoms of depression and anxiety affect early mother-infant interaction. J. Affect. Disord. 257, 83–90. doi: 10.1016/j.jad.2019.06.048
Hawes, K., McGowan, E., O’Donnell, M., Tucker, R., and Vohr, B. (2016). Social emotional factors increase risk of postpartum depression in mothers of preterm infants. J. Pediatr. 179, 61–67. doi: 10.1016/j.jpeds.2016.07.008
Hibel, L. C., Granger, D. A., Blair, C., Cox, M. J., and Family Life Project Key, I. (2011). Maternal sensitivity buffers the adrenocortical implications of intimate partner violence exposure during early childhood. Dev Psychopathol. 23, 689–701. doi: 10.1017/S0954579411000010
Hirsh-Pasek, K., Adamson, L. B., Bakeman, R., Owen, M. T., Golinkoff, R. M., Pace, A., et al. (2015). The contribution of early communication quality to low-income children’s language success. Psychol. Sci. 26, 1071–1083. doi: 10.1177/0956797615581493
Humphreys, K. L., LeMoult, J., Wear, J. G., Piersiak, H. A., Lee, A., and Gotlib, I. (2020). Child maltreatment and depression: a meta-analysis of studies using the childhood trauma questionnaire. Child Abuse Negl. 102:104361. doi: 10.1016/j.chiabu.2020.104361
Hutchens, B., and Kearney, J. (2020). Risk factors for postpartum depression: an umbrella review. J. Midwifery Womens Health 65, 96–108. doi: 10.1111/jmwh.13067
Hutchens, B. F., Kearney, J., and Kennedy, H. P. (2017). Survivors of child maltreatment and postpartum depression: an integrative review. J. Midwifery Womens Health 62, 706–722. doi: 10.1111/jmwh.12680
Jones, D., Letourneau, N., and Leger, L. (2019). Predictors of infant care competence among mothers with postpartum depression. Clin. Med. Insights Reprod. Health 13:1179558119834910. doi: 10.1177/1179558119834910
Keiser, A., Salinas, Y., DeWan, A., Hawley, N., Donohue, P., and Strobino, D. (2019). Risks of preterm birth among non-Hispanic black and non-Hispanic white women: effect modification by maternal age. Paediatr. Perinat. Epidemiol. 33, 346–356. doi: 10.1111/ppe.12572
Kleine, G., Vamvakas, A., Lautarescu, S., Falconer, A., Chew, S., Counsell, A., et al. (2021). Postnatal maternal depressive symptoms and behavioura outcomes in term and preterm - born toddlers. medRxi. doi: 10.1101/2021.09.21.21263881 [Epub ahead of print]
Kluczniok, D., Boedeker, K., Fuchs, A., Hindi Attar, C., Fydrich, T., Fuehrer, D., et al. (2016). Emotional availability in mother–child interaction: the effects of maternal depression in remission and additional history of childhood abuse. Depress. Anxiety 33, 648–657. doi: 10.1002/da.22462
Kroenke, K., Spitzer, R., and Williams, J. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lau, P., Hawes, D., Hunt, C., Frankland, A., Roberts, G., and Mitchell, P. (2018). Prevalence of psychopathology in bipolar high-risk offspring and siblings: a meta-analysis. Eur. Child Adolesc. Psychiatry 27, 823–837. doi: 10.1007/s00787-017-1050-7
Listunova, L., Roth, C., Bartolovic, M., Kienzle, J., Bach, C., Weisbrod, M., et al. (2018). Cognitive impairment along the course of depression: non-pharmacological treatment options. Psychopathology 51, 295–305. doi: 10.1159/000492620
Liu, X., Wang, S., and Wang, G. (2021). Prevalence and risk factors of postpartum depression in women: a systematic review and meta-analysis. J. Clini. Nurs. doi: 10.1111/jocn.16121 [Epub ahead of print]
Lovejoy, M. C., Graczyk, P. A., O’Hare, E., and Neuman, G. (2000). Maternal depression and parenting behavior: a meta-analytic review. Clin. Psychol. Rev. 20, 561–592. doi: 10.1016/S0272-7358(98)00100-7
Mandelli, L., Souery, D., Bartova, L., Kasper, S., Montgomery, S., Zohar, J., et al. (2016). Bipolar II disorder as a risk factor for postpartum depression. J. Affect. Disord. 204, 54–58. doi: 10.1016/j.jad.2016.06.025
Martinez-Torteya, C., Dayton, C. J., Beeghly, M., Seng, J. S., McGinnis, E., Broderick, A., et al. (2014). Maternal parenting predicts infant biobehavioral regulation among women with a history of childhood maltreatment. Dev. Psychopathol. 26, 379–392. doi: 10.1017/S0954579414000017
Mills-Koonce, W. R., Gariépy, J.-L., Propper, C., Sutton, K., Calkins, S., Moore, G., et al. (2007). Infant and parent factors associated with early maternal sensitivity: a caregiver-attachment systems approach. Infant Behav. Dev. 30, 114–126. doi: 10.1016/j.infbeh.2006.11.010
Mills-Koonce, W. R., Willoughby, M. T., Zvara, B., Barnett, M., Gustafsson, H., Cox, M. J., et al. (2015). Mothers’ and fathers’ sensitivity and children’s cognitive development in low-income, rural families. J. Appl. Dev. Psychol. 38, 1–10. doi: 10.1016/j.appdev.2015.01.001
Moody, G., Cannings-John, R., Hood, K., Kemp, A., and Robling, M. (2018). Establishing the international prevalence of self-reported child maltreatment: a systematic review by maltreatment type and gender. BMC Public Health 18:1164. doi: 10.1186/s12889-018-6044-y
Murray, L., Fearon, P., and Cooper, P. (2015). “Postnatal depression, mother-infant interactions, and child development: prospects for screening and treatment,” in Identifying Perinatal Depression and Anxiety: Evidence-Based Practice in Screening, Psychosocial Assessment, and Management. eds. J. Milgrom and A. W. Gemmill (United States: Wiley Blackwell), 139–164.
Muzik, M., Marcus, S. M., and Flynn, H. A. (2009). Psychotherapeutic treatment options for perinatal depression: emphasis on maternal-infant dyadic outcomes. J. Clin. Psychiatry 70, 1318–1319. doi: 10.4088/JCP.09com05451
Neri, E., Agostini, F., Salvatori, P., Biasini, A., and Monti, F. (2015). Mother-preterm infant interactions at 3 months of corrected age: influence of maternal depression, anxiety and neonatal birth weight. Front. Psychol. 6:1234. doi: 10.3389/fpsyg.2015.01234
NICHD Early Child Care Research Network (1999). Child care and mother-child interaction in the first 3 years of life. Dev. Psychol. 35, 1399–1413. doi: 10.1037/0012-1649.35.6.1399
Norcross, P. L., Leerkes, E. M., and Zhou, N. (2017). Examining pathways linking maternal depressive symptoms in infancy to children’s behavior problems: The role of maternal unresponsiveness and negative behaviors. Infant Behav. Dev. 49, 238–247. doi: 10.1016/j.infbeh.2017.09.009
Nordahl, K. B., Owen, M. T., Ribeiro, L. A., and Zachrisson, H. D. (2020). Parenting quality from observational ratings at age 2: validation from Norwegian and US samples. Early Child. Res. Q. 53, 379–390. doi: 10.1016/j.ecresq.2020.05.010
Norhayati, M., Nik Hazlina, N., Asrenee, A., and Wan Emilin, W. (2015). Magnitude and risk factors for postpartum symptoms: a literature review. J. Affect. Disord. 175, 34–52. doi: 10.1016/j.jad.2014.12.041
Owen, M. T. (2006). Qualitative Ratings for Parent-Child Interaction: 3–15 Months of Age: Coding Manual. Richardson, TX: University of Texas at Dallas.
Pechtel, P., Murray, L. M., Brumariu, L. E., and Lyons-Ruth, K. (2013). Reactivity, regulation, and reward responses to infant cues among mothers with and without psychopathology: an fMRI review. Trans. Dev. Psychiat. 1:19673. doi: 10.3402/tdp.v1i0.19673
Pelham, W., West, S., Lemery-Chalfant, K., Goodman, S., Wilson, M., Dishion, T., et al. (2021). Depression in mothers and the externalizing and internalizing behavior of children: An attempt to go beyond association. J. Abnorm. Psychol. 130, 60–77. doi: 10.1037/abn0000640
Perry, A., Gordon-Smith, K., Di Florio, A., Fraser, C., Craddock, N., Jones, L., et al. (2020). Adverse childhood experiences and postpartum depression in bipolar disorder. J. Affect. Disord. 263, 661–666. doi: 10.1016/j.jad.2019.11.042
Plant, D., Jones, F., Pariante, C., and Pawlby, S. (2017). Association between maternal childhood trauma and offspring childhood psychopathology: mediation analysis from the ALSPAC cohort. Br. J. Psychiatry 211, 144–150. doi: 10.1192/bjp.bp.117.198721
Putnick, D., Sundaram, R., Bell, E., Ghassabian, A., Goldstein, R., Robinson, S., et al. (2020). Trajectories of maternal postpartum depressive symptoms. Pediatrics 146:e20200857. doi: 10.1542/peds.2020-0857
Sandstrom, A., Sahiti, Q., Pavlova, B., and Uher, R. (2019). Offspring of parents with schizophrenia, bipolar disorder, and depression: A review of familial high-risk and molecular genetics studies. Psychiatr. Genet. 29, 160–169. doi: 10.1097/YPG.0000000000000240
Schaaf, J., Liem, S., Mol, B., Abu-Hanna, A., and Ravelli, A. (2013). Ethnic and racial disparities in the risk of preterm birth: a systematic review and meta-analysis. Am. J. Perinatol. 30, 433–450. doi: 10.1055/s-0032-1326988
Shlomi Polachek, I., Dulitzky, M., Margolis-Dorfman, L., and Simchen, M. (2016). A simple model for prediction of postpartum PTSD in high-risk pregnancies. Arch. Womens Mental Health 19, 483–490. doi: 10.1007/s00737-015-0582-4
Silverman, M., Reichenberg, A., Savitz, D., Cnattingius, S., Lichtenstein, P., Hultman, C., et al. (2017). The risk factors for postpartum depression: a population-based study. Depress. Anxiety 34, 178–187. doi: 10.1002/da.22597
Slomian, J., Honvo, G., Emonts, P., Reginster, J., and Bruyère, O. (2019). Consequences of maternal postpartum depression: a systematic review of maternal and infant outcomes. Womens Health 15, 174550651984404–174550651984455. doi: 10.1177/1745506519844044
Stein, A., Pearson, R. M., Goodman, S. H., Rapa, E., Rahman, A., McCallum, M., et al. (2014). Effects of perinatal mental disorders on the fetus and child. Lancet 384, 1800–1819. doi: 10.1016/S0140-6736(14)61277-0
Stoltenborgh, M., Bakermans-Kranenburg, M. J., Alink, L. R., and van IJzendoorn, M. H. (2015). The prevalence of child maltreatment across the globe: review of a series of meta-analyses. Child Abuse Rev. 24, 37–50. doi: 10.1002/car.2353
Tryphonopoulos, P., Letourneau, N., and DiTommaso, E. (2016). Caregiver-infant interaction quality: A review of observational assessment tools. Comprehens. Child Adoles. Nurs. 39, 107–138. doi: 10.3109/01460862.2015.1134720
Unternaehrer, E., Cost, K. T., Bouvette-Turcot, A.-A., Gaudreau, H., Massicotte, R., Dhir, S. K., et al. (2019). Dissecting maternal care: patterns of maternal parenting in a prospective cohort study. J. Neuroendocrinol. 31:e12784. doi: 10.1111/jne.12784
Weiss, S. J., Flynn, H., Christian, L., Hantsoo, L., Lanza Di Scalea, T., Kornfield, S., et al. (2021). Symptom profiles of women at risk of mood disorders: a latent class analysis. J. Affect. Disord. 295, 139–147. doi: 10.1016/j.jad.2021.08.013
Weiss, S. J., and Leung, C. (2021). Maternal depressive symptoms, poverty, and young motherhood increase the odds of early depressive and anxiety disorders for children born prematurely. Infant Ment. Health J. 42, 586–602. doi: 10.1002/imhj.21924
Weiss, S. J., and Quides, C. (2012). “Assessment and treatment of mental disorders specific to infants and young children,” in Child and Adolescent Behavioral Health: A Resource for Advanced Practice Psychiatric and Primary Care Nurse Practitioners. eds. E. Yearwood, G. Pearson, and J. Newland (Oxford: Wiley-Blackwell), 335–354.
Wescott, D., Morash-Conway, J., Zwicker, A., Cumby, J., Uher, R., and Rusak, B. (2019). Sleep in offspring of parents with mood disorders. Front. Psych. 10:225. doi: 10.3389/fpsyt.2019.00225
Willoughby, M. T., Mills-Koonce, R., Propper, C. B., and Waschbusch, D. A. (2013). Observed parenting behaviors interact with a polymorphism of the brain-derived neurotrophic factor gene to predict the emergence of oppositional defiant and callous–unemotional behaviors at age 3 years. Dev. Psychopathol. 25, 903–917. doi: 10.1017/S0954579413000266
Zalewski, M., Goodman, S. H., Cole, P. M., and McLaughlin, K. A. (2017). Clinical considerations when treating adults who are parents. Clin. Psychol. Sci. Pract. 24, 370–388. doi: 10.1111/cpsp.12209
Keywords: postpartum, depression, infant, interaction, maternal
Citation: Goodman SH, Muzik M, Simeonova DI, Kidd SA, Owen MT, Cooper B, Kim CY, Rosenblum KL and Weiss SJ (2022) Maternal Interaction With Infants Among Women at Elevated Risk for Postpartum Depression. Front. Psychol. 13:737513. doi: 10.3389/fpsyg.2022.737513
Received: 08 July 2021; Accepted: 27 January 2022;
Published: 03 March 2022.
Edited by:
Sara Calderoni, Stella Maris Foundation (IRCCS), ItalyReviewed by:
Sara Sylvén, Uppsala University, SwedenCopyright © 2022 Goodman, Muzik, Simeonova, Kidd, Owen, Cooper, Kim, Rosenblum and Weiss. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sandra J. Weiss, c2FuZHJhLndlaXNzQHVjc2YuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.