- 1Department of Nursing, Jinzhou Medical University, Jinzhou, China
- 2Department of Dermatology, Shengjing Hospital of China Medical University, Shenyang, China
- 3Department of Neurosurgery, The First Affiliated Hospital of China Medical University, Shenyang, China
Background: In China, some patients avoid seeking medical care and are highly sensitive to subsequent medical care because of fear of possible hospitalization after a diagnosis has been established. Early identification of fear of hospitalization is essential for clinical staff to develop targeted education and interventions. However, there are currently no tools to assess outpatients’ fear of hospitalization in mainland China. This study aimed to translate the Fear of Hospitalization (FH) scale into Chinese and verify its reliability and validity in outpatients.
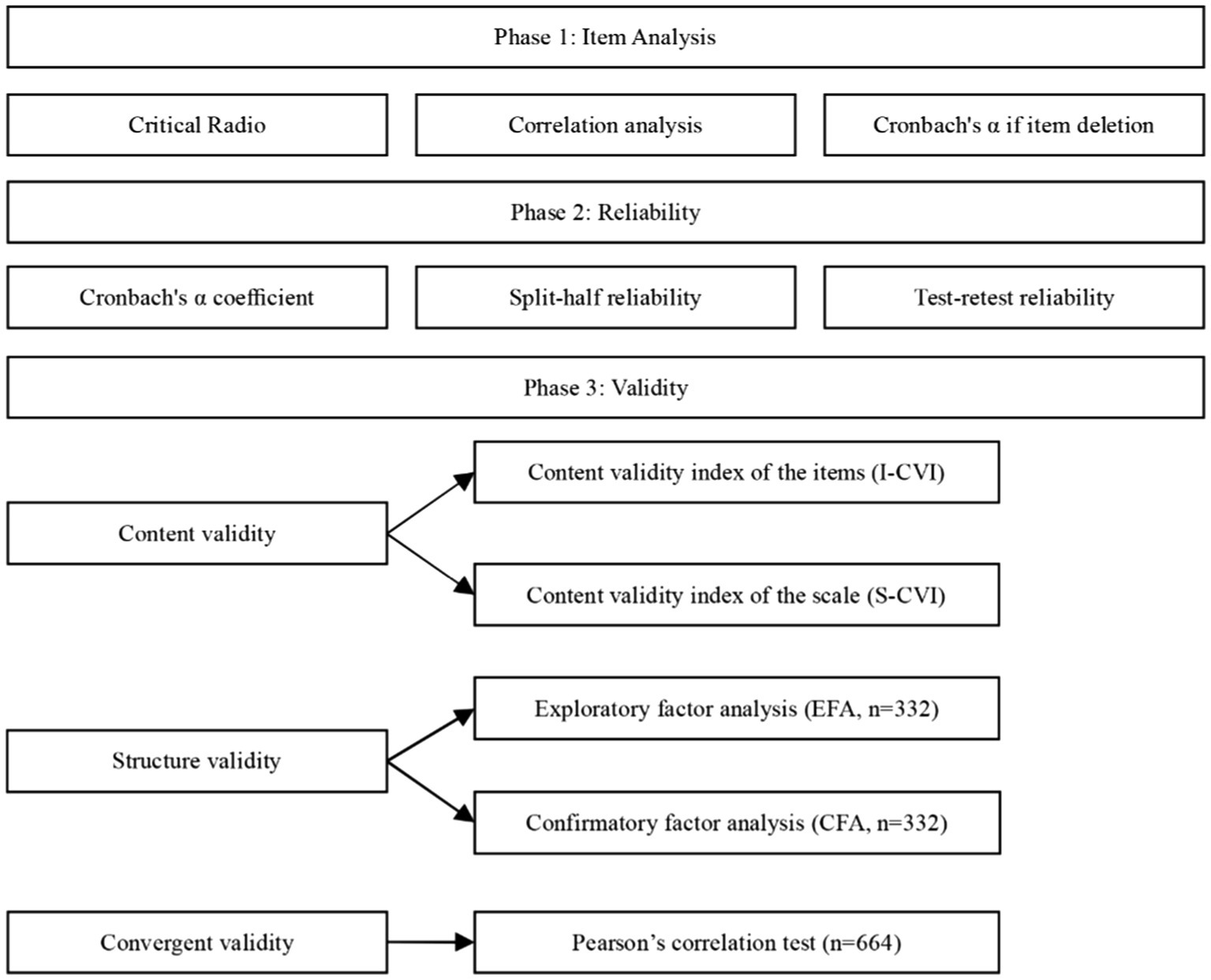
Methods: Through convenience sampling, 664 outpatients who required hospitalization were recruited from two cities in Liaoning Province, China. The reliability of the translated scale was measured by internal consistency, split-half reliability, and test–retest reliability. The validity of the translated scale was evaluated by expert consultation, exploratory factor analysis, and confirmatory factor analysis. Data were analyzed using SPSS 25.0 (IBM Corp., Armonk, NY, United States) and AMOS 23.0 (IBM Corp., Armonk, NY, United States).
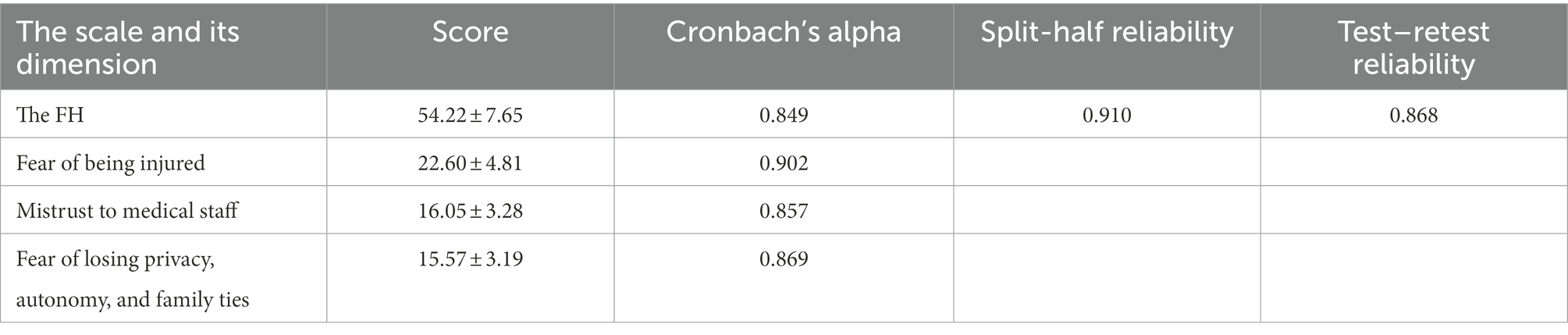
Results: The Cronbach’s α value of the Chinese version of the FH scale was 0.849, and the Cronbach’s α value of the dimensions ranged from 0.857 to 0.902. The test–retest reliability value of 0.868 shows good temporal stability. The split-half reliability value of 0.910 indicates a high degree of measuring the same content. The content validity index of the scale (S-CVI) was 0.924, indicating a good level of content validity. The 3-factor structure supported by eigenvalues, total variance explained, and scree plot was obtained using exploratory factor analysis. In addition, all recommended fit indicators were within the acceptable range by confirmatory factor analysis.
Conclusion: The Chinese version of the FH scale is valid and reliable in outpatients. The developed three-factor structured scale will help identify outpatients with a high fear of hospitalization and can inform the development of educational intervention plans for care managers, physicians, and nurses. In addition, it helps clinicians and nurses take action to reduce this fear of hospitalization in patients and prevent avoidance of using health care services due to fear of hospitalization.
Introduction
Hospitalization is a stressful event for patients of every age and can lead to a vicious cycle of patients delaying treatment and seeking alternative therapies out of fear of hospitalization, and only agreeing to be hospitalized for treatment when their disease escalates (Lowey et al., 2014; Raju and Reddy, 2017; Zvonareva et al., 2021; Correale et al., 2022). Fear of medical treatment is defined as the emotional and psychological response to a medical event experienced by a person in a hospital environment and is a common stress reaction during outpatient clinic visits (Steward and Steward, 1981; Lyu et al., 2020). Studies have shown that patients’ perceptions of pain, threat, and unknown prognostic risks associated with medical events can lead to medical fear, often accompanied by motor agitation and somatic autonomic dysfunction, resulting in anxiety, fear, panic, panic attacks, excessive sweating, and trembling of the hands and feet (Cornelius et al., 2018; Chang, 2019; Hadasik et al., 2021). During hospitalization, patients may feel a lack of privacy and severe limitations on self-direction, loss of personal space, and freedom to move around because they can no longer do anything for themselves and others (Weltens et al., 2021; Huang et al., 2022). They also feel helpless, angry, and insecure because of separation from their loved ones (Hall et al., 2022; Tavakoli et al., 2022). Outpatients are well aware that hospitalization means they will undergo previously unanticipated investigations, procedures, and treatments, some of which may be invasive, painful, or invasive of personal dignity, or even pose a threat to safety, creating a fear of hospitalization and possibly leading to delayed admission or rejection of hospital care. Therefore, assessing patients’ fear of hospitalization in a clinical setting is interesting and necessary.
Patient fear is a normal and complex emotional response, often caused by patient speculation about whether surgery will be successful and how well they will recover from hospitalization, and is essentially a fear of physical harm and death (Ji et al., 2022). The fear of surgery often presents as an emotional state before surgery, and it is recognized as one of surgery’s most significant psychological and socioeconomic risks (Celik and Edipoglu, 2018; Wu et al., 2019). Surgical fear has adversely affected patients’ psychosocial and physical recovery, such as increased pain after surgery, poor physical function, or mental health issues (Wilson et al., 2016; Theunissen et al., 2018). In addition to the surgery, people fear undergoing anesthesia, blood transfusions, being pricked by needles, and even losing their dignity (Kilinc and Ozer, 2017; Mohan et al., 2017). In a study investigating fear of anesthesia, it was shown that the primary sources of fear were fear of postoperative pain (84%), fear of not being able to wake up after surgery (64.8%), fear of nausea or vomiting (60.2%), and fear of drains and needles (59.5%). Patients were less concerned about being paralyzed by anesthesia (33.5%) or exposing personal problems (18.8%). In addition, the study also showed that gender influenced fear of anesthesia, with women being more fearful than men (Mavridou et al., 2013). In addition to patient concerns about surgery and anesthesia, patients experience fear due to a lack of communication and contact with hospital staff and information about various tests, medications, and therapeutic care operations (Tiwary et al., 2019). Conflicting instructions and plans from different healthcare providers can also cause patients to feel confused, fearful, and uncertain of correct statements (Nikitara et al., 2020). The closed management of wards during the prevention and control of the new coronary pneumonia epidemic is an effective means of preventing infection, cutting off transmission routes, and ensuring the health of hospitalized patients. Still, separation from friends and family may negatively impact hospitalized patients, leading to a significantly increased incidence of anxiety and depression (Ma et al., 2020). Thus, the concept of fear of hospitalization can be further applied to multicomponent fears, consisting of the following components: fear of injury (physical or mental) inevitably associated with appropriate diagnostics or treatment, fear of injury caused by diagnostic or treatment errors, fear of being humiliated as a person due to loss of privacy and autonomy in making decisions, and fear to be isolated from the persons with whom they have strong emotional ties. Fear of harm and medical procedures may prevent patients from seeking medical care when they are ill (Cavallo and Forman, 2020; Tesfaw et al., 2020; Kim et al., 2022). It is a severe public health problem that patients often avoid hospitalization despite physician recommendations (Pan et al., 2016).
Currently, there is only one scale to assess medical fear in children in China: the CMFS (Children’s Medical Fear Scale; Broome et al., 1988). Therefore, in many studies, non-specific questionnaires have been used to assess patients’ psychiatric problems related to hospitalization, such as the State–Trait Anxiety Inventory (STAI), Beck Anxiety Inventory (BAI), Hamilton Anxiety Rating Scale (HAM-A), Zung Self-Rating Anxiety Scale (SAS), Depression Anxiety Stress Scale (DASS), and Surgical Fear Questionnaire (SFQ; Hamilton, 1959; Zung, 1971; Beck et al., 1988; Spielberger, 1989; Lovibond and Lovibond, 1995; Theunissen et al., 2014). However, existing instruments for assessing fear of hospitalization are either limited in their target population or too general, and there is currently no scale that comprehensively assesses fear of hospitalization in outpatients in China. Based on the above, there is a need for reliable instruments to assess patients’ fear of hospitalization in China objectively. Professor Slobodan M. Jankovic developed and validated the FH scale (Jankovic et al., 2018) based on the guidelines developed by DeVellis (1991). Therefore, this study aimed to translate the FH scale into Chinese and validate its psychometric properties. This study also provides an instrument to quickly and accurately measure the fear of hospitalization among Chinese outpatients.
Materials and methods
Study design
This study was a cross-sectional and observational survey designed to test the reliability and validity of the new Chinese version of the Fear of Hospitalization scale, also known as the FH scale.
Participants
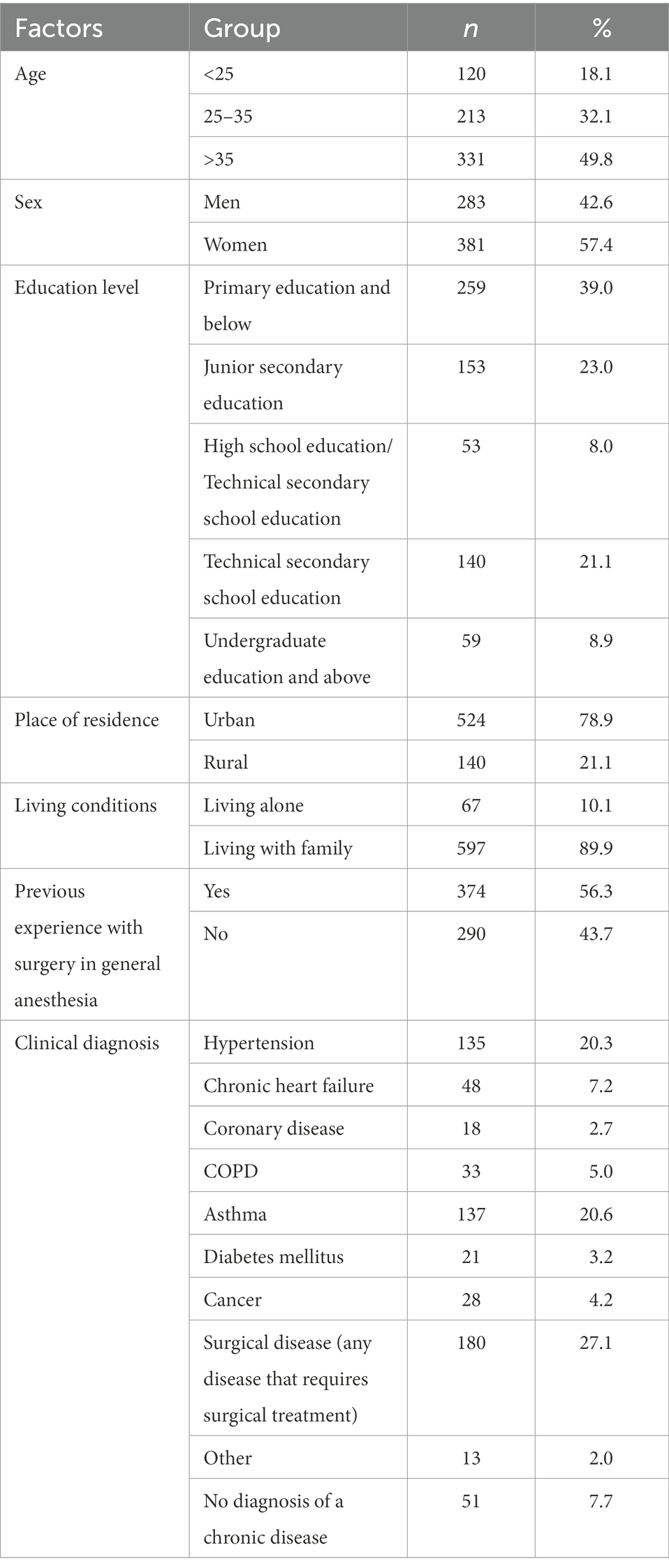
Convenience sampling was conducted from March to July 2022 in the two Chinese cities of Shenyang and Jinzhou to recruit eligible outpatients. Inclusion criteria were outpatients who were literate, over 18 years of age, and had obtained informed consent. Exclusion criteria were outpatients who were pregnant, lactating, cognitively impaired, emotionally disturbed, mentally retarded, and had incomplete patient records. Ultimately, 664 outpatients were recruited from the hospital through convenience sampling with the assistance of the Director of Nursing based on available conditions. We collected basic information about the socio-demographic characteristics of the participants (including age, sex, education level, place of residence, living conditions, previous experience with surgery in general anesthesia, and clinical diagnosis).
Translation, back-translation, and transcultural adaptation of the FH scale
Our translation work has obtained Professor Slobodan M. Jankovic’s permission. The Brislin double back-translation method was adopted to translate the FH scale (Brislin, 1970). First, two Chinese professors majoring in English translated the FH scale into Chinese. Then, two foreign teachers who were native English speakers did the reverse translation. In addition, psychological experts were invited to make cultural adjustments to the translated scale to make the items more compatible with Chinese expressions habits. The draft of the Chinese version of the FH scale was finally formed.
Some modifications have been made to the items in the scale to fit the Chinese cultural context, known as cultural adaptation. (1) Expert consultation: two psychiatrists, two psychologists, one clinical care manager, one English language specialist, and one nurse researcher with experience in acculturation and validation studies for quality life instruments, all with graduate degrees and above. The final version was generated after adapting and modifying each item in the first draft of the Chinese version according to Chinese cultural and linguistic habits. (2) Pretest: A convenience sampling method was used to select 10 outpatients for a preliminary survey, and each participant was invited to evaluate the layout design and understanding of each item. It is important to note that the researchers explained the purpose and significance of the study to respondents before sending the scales and obtaining their informed consent. Outpatients reported that items on the scale were easy to understand, and the scale structure was clear. Finally, the Chinese version of the FH scale was completed.
Questionnaire design
Background characteristics
Our general demographic characteristics questionnaire was developed following a systematic literature review and rigorous team negotiation. Seven variables were included in the questionnaire: age, gender, education level, place of residence, living conditions, previous experience with surgery in general anesthesia, and clinical diagnosis.
The FH scale
The FH scale is a 17-item scale developed by Dr. Slobodan M. Jankovic et al. to comprehensively measure the fear of hospitalization experienced among outpatients (Jankovic et al., 2018). The FH scale includes three dimensions: Factor 1: Fear of being injured (7 items), Factor 2: Mistrust to the medical staff (5 items), and Factor 3: Fear of losing privacy, autonomy, and family ties (5 items). In addition to positive wording, there is also negative wording (items 2, 9, 10, and 11 are reverse scored, while the rest are forward scored). Based on a five-point Likert scale, each item is rated (5 = disagree; 4 = partially disagree; 3 = Neither agree nor disagree; 2 = partially agree; 1 = completely agree). The total and dimension scores are the sum of each item’s scores, with the total score ranging from 17 to 85. A higher score indicates a weaker degree of fear of hospitalization experienced by outpatients. According to the investigators (Cronbach’s alpha 0.799), there is acceptable internal consistency in the original scale and the patients themselves (Cronbach’s alpha 0.760).
The surgical fear questionnaire
Several questionnaires like Hospital Anxiety and Depression Scale (HADS), Hamilton depression scale (HAMD), Hamilton Anxiety Scale (HAMA), Self-rating Anxiety Scales (SAS), Self-rating Depression Scale (SDS), Generalized Anxiety Disorder 7-item Scale (GAD-7), Patient Health Questionnaire 9-item Scale (PHQ-9), and many others have been developed to evaluate specific components of mental problems among patients related to hospitalization. Most outpatients refuse to be hospitalized for treatment because of their fear of surgery, and surgical procedures can cause anxiety and fear in patients who believe they will threaten their physical changes and psychological and social reactions to hospitalization (Garcia et al., 2018). Due to its close relationship to hospitalization fear, the SFQ was used in this study to assess criterion validity, which was developed to evaluate the level of fear of surgical intervention. In 2019, Wu Jun translated and localized the Chinese version of the scale, which was verified to have good reliability and validity (Wu and Zhu, 2019). This scale is a self-rating scale consisting of 2 dimensions with eight items. A Likert 10-point scoring system (not at all afraid to very afraid) was used to collect responses from outpatients. The score ranges from 8 to 80. Generally, the higher the score, the stronger fear of undergoing surgery among patients. The Cronbach’s α value was 0.968, with domains ranging from 0.56 to 0.82.
Data collection
With the assistance of the director of nursing, the researcher explained the study’s purpose and significance and recruited participants. The nursing director arranged a quiet classroom for participants to complete the translated scales anonymously. Seven hundred ten outpatients were recruited to participate in the survey, and 679 outpatients agreed. It was finally decided to retain 664 questionnaires after removing those with missing data from the sample. We asked 50 outpatients to complete the translated scale again after 2 weeks to assess the test’s reliability.
Statistical analysis
SPSS 25.0 (IBM Corp., Armonk, NY, United States) and AMOS 23.0 (IBM Corp., Armonk, NY, United States) was used to complete the statistical analysis. Frequency and composition ratios were used to describe the general demographic characteristics of outpatients. We evaluated the items’ quality using item analysis and the content validity of the scales using expert consultation. Exploratory factor analysis (EFA) was performed using the principal axis factoring method to explore the underlying factor structure of the translation scales. A confirmatory factor analysis was conducted using AMOS 23.0 to examine the structural validity of the scale. Internal consistency analysis and test–retest reliability analysis were conducted to determine the scale’s homogeneity and stability.
Item analysis
We used the critical ratio, correlation coefficient, and Cronbach’s α if item deletion method to evaluate each item’s suitability. A t-test was performed between the high group (highest 27%) and the low group (lowest 27%; McCowan and McCowan, 1999) to determine whether the item discriminated between the high and low groups. The absolute t-values were generally removed if they were below 3 (Raykov and Marcoulides, 2016). In addition, we calculated item-total correlation coefficients to determine item homogeneity, and item-total correlation coefficients ≥ 0.4 are considered appropriate for item homogeneity (Raykov and Marcoulides, 2016). The Cronbach’s α coefficient was calculated after removing each item to determine the items’ quality. It is suggested that you delete an item if its Cronbach’s coefficient increases significantly after its deletion, meaning the item decreases internal correlation and should be removed (Raykov and Marcoulides, 2016). It was done to determine if the items of the translated scale could be retained.
Reliability analysis
Our test–retest reliability and internal consistency analyses were conducted on the translated Chinese FH scale. For the internal consistency analysis, Cronbach’s coefficient and split-half reliability coefficients were calculated for the translated scale and its dimensions to evaluate the homogeneity of the items. The split-half reliability of the translated scale was assessed by dividing the items into two parts in odd and even order, and the correlation between the results of both sides of the scale was calculated (Ren et al., 2021). After 2 weeks, 50 previously diagnosed outpatients were remeasured with the translated scale, and correlation coefficients were calculated to evaluate how stable the scale had become. All three Cronbach’s coefficients, the split-half reliability coefficient, and the test–retest reliability coefficient had to be at least 0.7 to satisfy our requirements (Chang et al., 2018).
Validity analysis
A panel of experts consisting of three psychiatrists, two psychologists, one surgeon, and one internist assessed the content validity of the translated scales. These experts were selected based on: (i) their extensive expertise in psychiatry, psychology, and clinical medicine; (ii) their familiarity with the manual steps of the scale and psychometric measures; (iii) their bachelor’s degree or higher and least 10 years of experience in the field; (iv) their rigorous and pragmatic approach to research; and (v) their volunteers to participate in this study. The experts’ answers were collected using a four-point Likert scale (1 = not relevant, 2 = weakly relevant, 3 = strongly relevant, 4 = highly relevant). Not relevant and weakly relevant are assigned 0 points, and strongly relevant and highly relevant are assigned 1 point. An item’s content validity index (I-CVI) is determined by the percentage of experts who scored three or four out of the total number of participants. S-CVI is the content validity index of the scale, which is the average of the I-CVI of each item in the scale. There has been an indication of good content validity when the I-CVI ≥ 0.78 and the S-CVI ≥ 0.90, indicating that the overall content validity of the scale is good (Shi et al., 2012).
The underlying factor structure of the translation scale was evaluated using exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). We randomly divided the sample of 664 cases into two groups, one group (n = 332) for the EFA and the other group (n = 332) for the CFA. In general, the characteristics of the two groups were similar. Principal axis factorization of EFA was completed, and the dataset was considered suitable for EFA only if the Bartlett test for sphericity was significant (p < 0.05; Bartlett, 1954) and the KMO > 0.60 (Kaiser H. F., 1970; Kaiser H. F. J. P., 1974) to explore the underlying factor structure of the scale. In addition, principal component analysis (PCA) with varimax rotation was used in EFA to estimate the principal components of the analysis. It was recommended that each item should have a factor loading of 0.40 or higher and no cross-loadings (Alavi et al., 2020; Schreiber, 2021). The corresponding items would be deleted if these requirements were not met (Gorsuch, 1997). Generally, contributions over 50% are considered acceptable, and contributions over 70% are deemed suitable (Diamond et al., 2014). The model fitting index for the translation scale was examined using an Analysis of Moment Structure (AMOS). The following metrics must be good to confirm the replicability of the first-order three-factor structure of the FH scale: χ2/DF, the goodness-of-fit index (GFI), the adjusted goodness-of-fit index (AGFI), the incremental fit index (IFI), the Tucker Lewis index (TLI), and the comparative fit index (CFI). Typically, χ2/DF is required to be <3, while all other values are required to be >0.9, indicating good fit of the model (Bentler and Bonett, 1980; Gorsuch, 1997). Furthermore, the root means a square error of approximation (RMSEA) should be <0.08, indicating a good fit and a good model fit (Schreiber et al., 2006). Additionally, convergent and discriminant validity tests were performed to determine the scale’s structural validity. We used the average variance extracted (AVE) values and the composite reliability (CR) values to measure convergent validity. An acceptable model should have a CR > 0.7 and an AVE > 0.45 (Kline, 2015). For assessing discriminant validity, we calculated the square root of the AVE value and the correlation coefficient for each factor. Our requirement was that the square root of the AVE value exceed the correlation coefficient between the corresponding factors (Fornell and Larcker, 1981).
Convergent validity
The calibration correlation is calculated to measure the degree of correlation between the measuring and standard scales using a recognized valid scale as a standard. This study used the SFQ as its calibration standard. A Pearson correlation analysis was conducted to determine whether the Chinese version of the FH scale was correlated with the SFQ. The test has high validity when the correlation coefficient r > 0.70. The validity of the test is moderate when 0.4 < r < 0.7. When r < 0.4, the validity of the test is low (Wang and Sun, 2011). Figure 1 illustrates the steps for the statistical analysis of the data.
Ethical considerations
The Jinzhou Medical University Ethics Committee approved the study protocol (Ref: JZMULL2022025). The authors of the original study authorized the use of the FH scale. Before taking part in the survey, participants received an explanation of the purpose and significance of the study and were asked to sign an informed consent form. The questionnaires returned were all anonymous. The survey was conducted confidentially to ensure the confidentiality of the data.
Results
The general demographic characteristics
This study included 664 outpatients: 283 men (42.6%) and 381 women (57.4%). Participants aged > 35 years accounted for 49.8%. More than half (78.9%) of the participants lived in urban areas; 39% had primary education or below; the largest proportion of the participants lived with their families (89.9%). The following Table 1 provides additional sociodemographic information.
The translation and revision of the FH scale
The original Chinese version of the FH scale was developed through translation, back translation, and cultural adaptation. Seven experts were invited to conduct an expert consultation on the draft Chinese version of the FH scale. The scale included three dimensions (Fear of being injured, Mistrust of the medical staff, Fear of losing privacy, autonomy, and family ties) and 17 items. According to all 10 outpatients in the initial survey, the revised draft of the Chinese version of the FH scale was easy to understand and answer. Eventually, 17 items were developed as a pretest version of the Chinese version of the FH scale.
The exploration and analysis of the item
The item’s quality was estimated based on the critical ratio, the item-scale correlation coefficient, and Cronbach’s coefficient. A critical ratio (CR) > 3.000 indicates a high discriminability of items. The critical ratios of items in the translation scale range from 11.459 to 20.375 (p < 0.001), indicating good discriminability of each item. This study’s item-total correlation coefficients ranged from 0.446 to 0.588 (p < 0.001). Taking the translated scale and removing each item, we found that Cronbach’s coefficient for the translated scale was 0.835–0.847, not more than Cronbach’s coefficient for the scale itself (0.849). Therefore, each item can be accepted without deletion.
The psychometric evaluation of the FH scale
Content validity
Seven qualified experts were invited to assess the content validity of the translation scales (I-CVI and S-CVI), and the results showed a range of 0.857 to 1.000 for I-CVI and 0.924 for S-CVI on the translation scale. The results suggested an adequate content validity of the questionnaire.
Construct validity
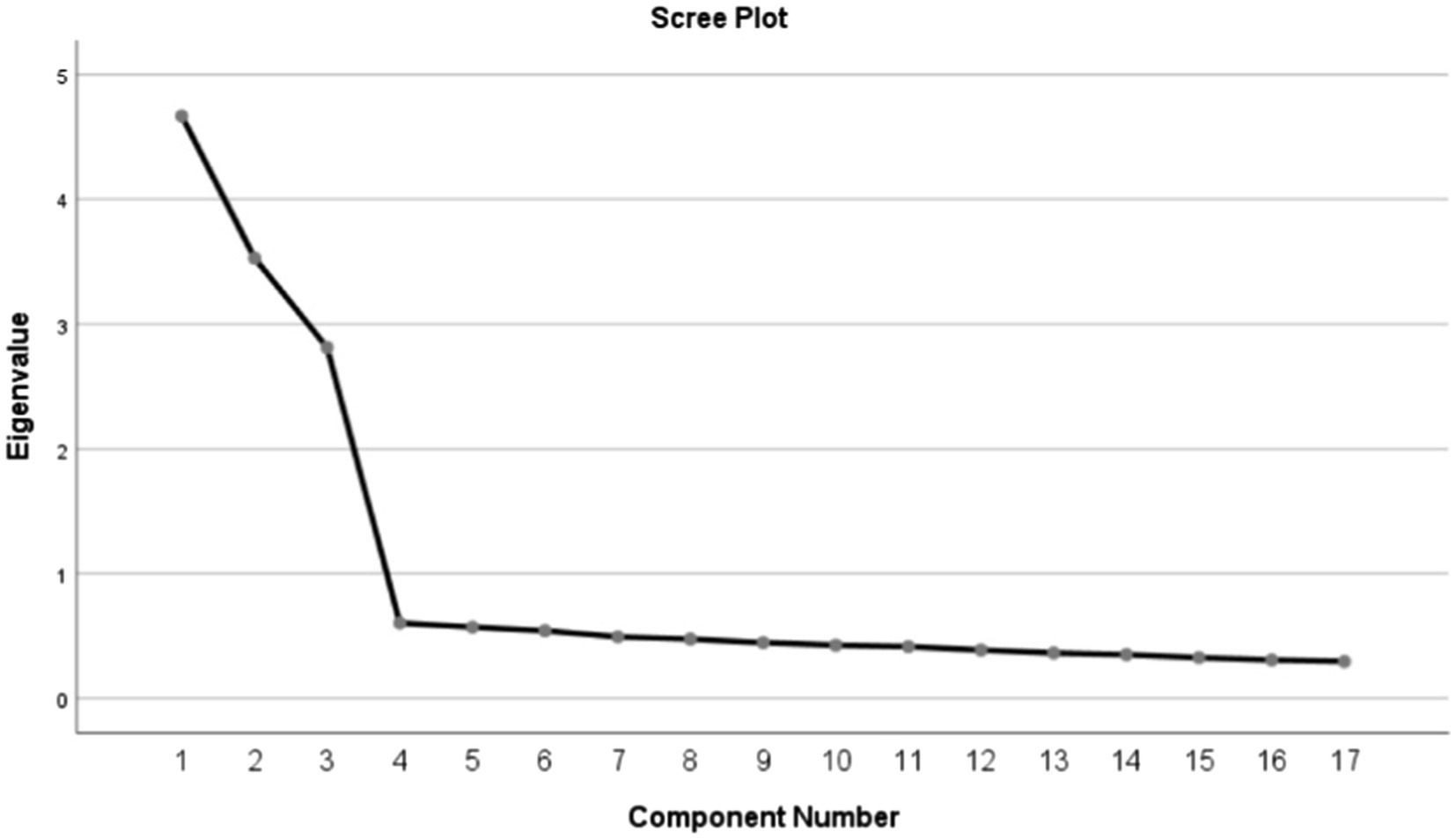
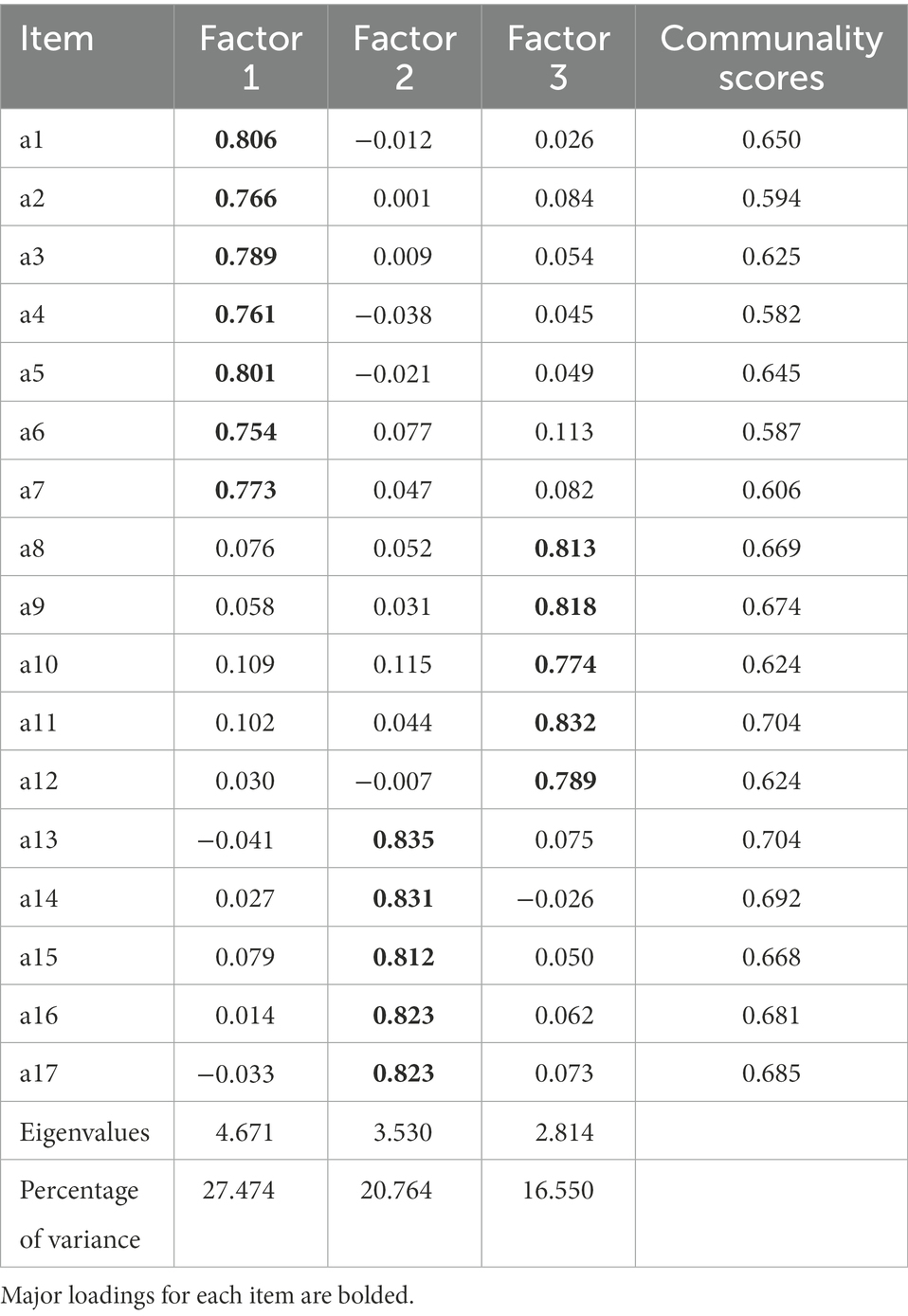
In the EFA, the Kaiser–Meyer–Olkin value was 0.887, and the Bartlett sphericity test was significant (χ2 = 2725.797; p < 0.001). Due to this, the matrix is not an identity matrix, and factor extraction can be performed with it. Kaiser’s rule showed that the three-factor model explained 64.788% of the total variance with initial eigenvalues > 1 each. A scree plot further confirmed the three-factor structure within the original scale, showing that the descending tendency weakened after the third point (Figure 2). Based on the results of the varimax rotation, three factors were identified which could explain 27.474%, 20.764%, and 16.550% of the variance, respectively. Furthermore, the factor loadings of the factors are also satisfactory and are displayed in Table 2.
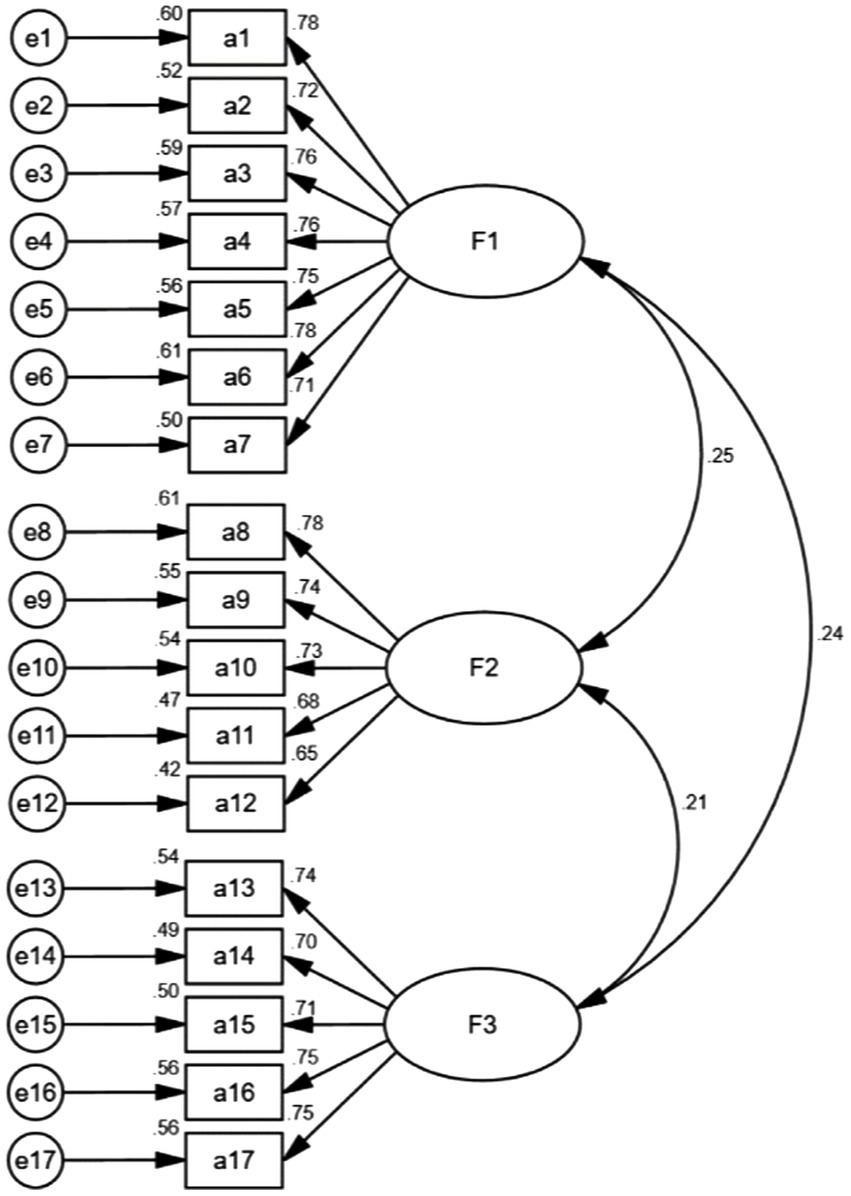
According to the CFA analysis, the three-factor model was fitted using the maximum likelihood SEM (Figure 3). In terms of the CFA results, χ2/DF = 1.764, GFI = 0.932, AGFI = 0.910, RMSEA = 0.048, TLI = 0.958, CFI = 0.964, IFI = 0.965, PGFI = 0.707, and PNFI = 0.787. There is no doubt that the three-factor model fits appropriately based on the fit indices selected. According to the convergent validity analysis, the AVE values ranged from 0.516 to 0.564, and the CR values ranged from 0.841 to 0.900. A discriminant validity analysis revealed that the square root values of AVE ranged from 0.718 to 0.751, greater than the correlation coefficients between the corresponding factors in Table 3.
Criterion validity
We used the Chinese version of the SFQ as the criterion scale to measure the FH scale’s criterion validity. As a result of the correlation analysis, the total scores of the two scales were negatively correlated (r = −0.649, p < 0.001). The significant correlation coefficients for the different dimensions and the SFQ were −0.481, −0.416, and −0.401, respectively (p < 0.001).
Internal consistency, split-half reliability, and test–retest reliability
An analysis of the stability and homogeneity of the Chinese version of the FH scale was conducted based on internal consistency, split-half reliability, and test–retest reliability. The translated scale had a Cronbach’s alpha value of 0.849, while Cronbach’s α values of the dimensions ranged from 0.857 to 0.902. The split-half reliability of the scale was 0.910. A random sample of 50 outpatients was selected for retesting after 2 weeks, and the test–retest reliability was 0.868 (Table 4).
Discussion
The FH scale was adapted cross-culturally to measure outpatients’ fear of hospitalization, and its reliability and validity were tested on 664 outpatients in this study. The FH scale was first applied to a Chinese population and has good construct validity, discriminant validity, and reliability. It can be used to predict the fear of hospitalization and to identify and screen patients diagnosed by physicians or who need to be hospitalized for treatment purposes but avoid hospitalization because of fear. It also facilitates the development of health education interventions by healthcare professionals, essential to reduce or eliminate patients’ fear of hospitalization and increase their acceptance of hospitalization.
This study’s FH scale was translated into Chinese and cross-culturally adapted according to the Brislin translation principle (Brislin, 1970). Seven experts adjusted the first translation based on their professional knowledge, clinical experience, and language expression habits, and eventually, the Chinese version of the FH scale was developed. The Chinese and original scales were fully demonstrated to be equivalent in terms of equivalence.
There has been an extensive review of the content validity of the items by seven experts, and the experts have agreed that the scale, in its original configuration, showed good content validity, with all experts agreeing on the scale items. In the preliminary survey, 50 outpatients indicated that the structure of the Chinese version of the FH scale was simple and reasonable, with clear semantic expressions and easy-to-understand content. The final Chinese version of the FH scale was divided into three dimensions and contained 17 items. The CR values in the item analysis were much higher than the standard values. In addition, the items of the questionnaire were well distinguished, and the scores of each item had a moderate to high correlation with the scale’s total score (Huang et al., 2020). In addition, after deleting each item, Cronbach’s α value did not exceed the original values of the translated scale. In conclusion, the content and structure of the Chinese version of the FH scale are reasonable, 17 items can be retained, and no further items need to be added or reduced.
As part of the reliability analysis conducted in this study, the internal consistency reliability, split-half reliability, and test–retest for reliability analysis were measured to assess the consistency and stability of the Chinese version of the scale. Cronbach’s α coefficient can reflect the homogeneity between all items in the scale (Tavşancıl, 2002; Şencan, 2005). The results showed that the Cronbach’s α coefficient of the Chinese version of the scale was 0.849, and the Cronbach’s α coefficient of each dimension was 0.857 to 0.902, slightly higher than the results of the original scale (Celik and Edipoglu, 2018), indicating that the Chinese version of the scale had a higher internal consistency of the items. Similarly, it was found that the split-half reliability coefficient was 0.910, confirming the previous conclusion. The test–retest reliability is the consistency of results produced by repeating measurements on the same group of subjects using the same research instrument, which can represent the test’s stability and consistency over time (Leppink and Pérez-Fuster, 2017). According to the results, the test–retest reliability of the Chinese version of the scale was 0.868, indicating that the Chinese version of the FH scale has good stability and can be used to measure the fear of hospitalization behavior in outpatients. Overall, the Chinese version of the FH scale has shown good reliability among outpatients.
The validity of the Chinese version of the FH scale was evaluated based on its content validity, construct validity, and calibration validity. Seven experts evaluated the Chinese version of the questionnaire for its content validity. The results showed that the I-CVI was 0.857 to 1.000 and the S-CVI was 0.924, better than the standard values of 0.78 and 0.9, respectively (Lenz, 2010). Thus, the scale showed good content validity. Construct validity, also known as conceptual validity, reflects the extent to which a scale is integrated with the theoretical or conceptual framework on which it is based. The evaluation of outcome validity is mainly based on factor analysis, which can be divided into exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). When evaluating the structural validity of a questionnaire using EFA, the structural validity of the questionnaire is satisfactory if the cumulative variance contribution of the common factors extracted from the scale is >60% and the loadings of the items on their imputation factors are >0.4 (Carlsson et al., 2016; van Bruggen et al., 2018). In this study, the EFA results showed that the three-factor structure extracted from the Chinese version could explain the total variation well, explaining 64.788% of the total variance, the factor loadings of all items in the questionnaire were >0.4, and the factor attributions of every item were consistent with the original version (Celik and Edipoglu, 2018). The results suggested that the Chinese version was conceptually adequate and had appropriate construct validity. It indicates that the items have a strong explanatory power for assessing the fear of hospitalization among outpatients. Meanwhile, the fit index of the Chinese version of the scale was within the acceptable range and stronger than the original version in CFA (Celik and Edipoglu, 2018), indicating that the Chinese version of the FH scale has a good overall fit. In terms of calibration validity, the high correlation between the FH scale and the SFQ (r = −0.649, p < 0.001) also indicated that the scale had appropriate calibration validity. In conclusion, we believe that the Chinese version of the FH scale has appropriate validity among outpatients.
Limitation and perspectives
In this study, we considered several limitations that need attention and discussion. First, despite the study’s sample size meeting the criteria, a large multi-center sample should be considered for improved sample representation and to investigate cultural differences across regions. Second, this study relied on self-reported questionnaires, and bias is inevitable. Finally, although we have adequately validated the psychometric characteristics of the Chinese version of the FH scale in outpatients, we have not yet explored the factors that influence fear of hospitalization behavior. Therefore, this will serve as the focus of our future work, which will be very important for our next steps.
Conclusion
After translation and cultural adaptation, the FH scale was successfully introduced into China, and its psychometric properties have been validated. In response to the serious public health problem of patients avoiding hospitalization despite physician advice, the developed questionnaire can provide a reference for care managers, physicians, and nurses to identify patients at high risk for fear of hospitalization and to develop educational programs and interventions to improve behaviors to prevent fear of hospitalization among outpatients, as well as a basis and prerequisite for research related to fear of hospitalization among outpatients.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Jinzhou Medical University Ethics Committee (Ref: JZMULL2022025). The patients/participants provided their written informed consent to participate in this study.
Author contributions
WL, HY, YZ, BL, and MF were involved in the study route design and data collection. After data collection and analysis, WL wrote the draft. HY and BL made essential revisions to the draft to identify important intellectual content. YZ and MF performed data collection and statistical analysis. All authors contributed to the article and approved the submitted version.
Acknowledgments
The authors would like to thank the outpatients who participated in this study and the nurse directors for their strong support in collecting the samples. In addition, Slobodan M. Jankovic, University of Kragujevac, one of the developers of the FH scale, provided helpful feedback and valuable editorial suggestions.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alavi, M., Visentin, D. C., Thapa, D. K., Hunt, G. E., Watson, R., and Cleary, M. (2020). Exploratory factor analysis and principal component analysis in clinical studies: which one should you use? J. Adv. Nurs. doi: 10.1111/jan.14377. [Epub ahead of print].
Bartlett, M. S. (1954). A note on the multiplying factors for various χ2 approximations. J. R. Stat. Soc. Series B. 16, 296–298. doi: 10.1111/j.2517-6161.1954.tb00174.x
Beck, A. T., Epstein, N., Brown, G., and Steer, R. A. (1988). An inventory for measuring clinical anxiety: psychometric properties. J. Consult. Clin. Psychol. 56, 893–897. doi: 10.1037/0022-006X.56.6.893
Bentler, P. M., and Bonett, D. G. J. P. B. (1980). Significance tests and goodness of fit in the analysis of covariance structures. Psychol. Bull. 88, 588–606. doi: 10.1037/0033-2909.88.3.588
Brislin, R. W. (1970). Back-translation for Cross-Cultural. Cross-Cult. Res. 1, 185–216. doi: 10.1177/135910457000100301
Broome, M. E., Hellier, A., Wilson, T., Dale, S., and Glanville, C. (1988). “Development and testing of an instrument to measure children’s fears of medical experiences,” in Measurement of nursing outcome. eds. C. Waltz and O. Strickland (New York: Springer), 201–214.
Carlsson, E., Pettersson, M., Öhlén, J., Sawatzky, R., Smith, F., and Friberg, F. (2016). Development and validation of the preparedness for colorectal cancer surgery questionnaire: PCSQ-pre 24. Eur. J. Oncol. Nurs. 25, 24–32. doi: 10.1016/j.ejon.2016.09.002
Cavallo, J. J., and Forman, H. P. (2020). The economic impact of the COVID-19 pandemic on radiology practices. Radiology 296, E141–E144. doi: 10.1148/radiol.2020201495
Celik, F., and Edipoglu, I. S. (2018). Evaluation of preoperative anxiety and fear of anesthesia using APAIS score. Eur. J. Med. Res. 23:41. doi: 10.1186/s40001-018-0339-4
Chang, B. P. (2019). Can hospitalization be hazardous to your health? A nosocomial based stress model for hospitalization. Gen. Hosp. Psychiatry 60, 83–89. doi: 10.1016/j.genhosppsych.2019.07.014
Chang, Q., Sha, F., Chan, C. H., and Yip, P. S. F. (2018). Validation of an abbreviated version of the Lubben social network scale ("LSNS-6") and its associations with suicidality among older adults in China. PLoS One 13:e0201612. doi: 10.1371/journal.pone.0201612
Cornelius, T., Agarwal, S., Garcia, O., Chaplin, W., Edmondson, D., and Chang, B. P. (2018). Development and validation of a measure to assess Patients' threat perceptions in the emergency department. Acad. Emerg. Med. 25, 1098–1106. doi: 10.1111/acem.13513
Correale, C., Borgi, M., Collacchi, B., Falamesca, C., Gentile, S., Vigevano, F., et al. (2022). Improving the emotional distress and the experience of hospitalization in children and adolescent patients through animal assisted interventions: a systematic review. Front. Psychol. 13:840107. doi: 10.3389/fpsyg.2022.840107
DeVellis, R. F. (1991). Scale development: Theory and applications. Thousand Oaks, CA, US: Sage Publications, Inc.
Diamond, I. R., Grant, R. C., Feldman, B. M., Pencharz, P. B., Ling, S. C., Moore, A. M., et al. (2014). Defining consensus: a systematic review recommends methodologic criteria for reporting of Delphi studies. J. Clin. Epidemiol. 67, 401–409. doi: 10.1016/j.jclinepi.2013.12.002
Fornell, C., and Larcker, D. F. (1981). "Structural equation models with unobservable variables and measurement error: Algebra and statistics ". Sage Publications Sage CA Los Angeles, CA).
Garcia, A. C. M., Simão-Miranda, T. P., Carvalho, A. M. P., Elias, P. C. L., Pereira, M. D. G., and Carvalho, E. C. D. (2018). The effect of therapeutic listening on anxiety and fear among surgical patients: randomized controlled trial. Rev. Lat. Am. Enfermagem 26:e3027. doi: 10.1590/1518-8345.2438.3027
Gorsuch, R. L. (1997). Exploratory factor analysis: its role in item analysis. J. Pers. Assess. 68, 532–560. doi: 10.1207/s15327752jpa6803_5
Hadasik, K., Arasiewicz, H., and Brzezińska-Wcisło, L. (2021). Assessment of the anxiety and depression among patients with idiopathic pruritus ani. Postepy Dermatologii I Alergologii 38, 689–693. doi: 10.5114/ada.2021.108906
Hall, H., Dhuga, Y., Yan Zheng, C., Clunie, G., Joyce, E., McNair, H., et al. (2022). Patient and practitioner perspectives on the design of a simulated affective touch device to reduce procedural anxiety associated with radiotherapy: a qualitative study. BMJ Open 12:e050288. doi: 10.1136/bmjopen-2021-050288
Hamilton, M. (1959). The assessment of anxiety states by rating. Br. J. Med. Psychol. 32, 50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x
Huang, F., Wang, H., Wang, Z., Zhang, J., Du, W., Su, C., et al. (2020). Psychometric properties of the perceived stress scale in a community sample of Chinese. BMC Psychiatry 20:130. doi: 10.1186/s12888-020-02520-4
Huang, Y., Zhou, Y., Wong, T. K. S., Luo, D., Zhang, G., Chen, J., et al. (2022). Inpatient dignity scale: mandarin translation and psychometric characteristics evaluation. Nurs. Open 9, 500–512. doi: 10.1002/nop2.1088
Jankovic, S. M., Antonijevic, G. V., Vasic, I. R., Zivkovic-Radojevic, M. N., Mirkovic, S. N., Nikolic, B. V., et al. (2018). A rating instrument for fear of hospitalisation. J. Clin. Nurs. 27, 1431–1439. doi: 10.1111/jocn.14295
Ji, W., Sang, C., Zhang, X., Zhu, K., and Bo, L. (2022). Personality, preoperative anxiety, and postoperative outcomes: a review. Int. J. Environ. Res. Public Health 19:12162. doi: 10.3390/ijerph191912162
Kaiser, H. F. (1970). A second generation little jiffy. Psychometrika 35, 401–415. doi: 10.1007/BF02291817
Kaiser, H. F. J. P. (1974). An index of factorial simplicity. Psychometrika 39, 31–36. doi: 10.1007/BF02291575
Kilinc, M., and Ozer, A. B. (2017). Fear of going under general anesthesia: a cross-sectional study. Saudi J. Anaesth. 11, 128–129. doi: 10.4103/1658-354X.197361
Kim, M., Park, J.-A., Cha, H., Lee, W. H., Hong, S.-N., and Kim, D. W. (2022). Impact of the COVID-19 and socioeconomic status on access to Care for Otorhinolaryngology Patients. Int. J. Environ. Res. Public Health 19:11875. doi: 10.3390/ijerph191911875
Kline, R. B. (2015). Principles and practice of structural equation modeling. New York: Guilford publications.
Lenz, E. R. (2010). Measurement in nursing and health research. New York: Springer publishing company.
Leppink, J., and Pérez-Fuster, P. (2017). We need more replication research - a case for test-retest reliability. Pers. Med. Educ. 6, 158–164. doi: 10.1007/s40037-017-0347-z
Lovibond, P. F., and Lovibond, S. H. (1995). The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav. Res. Ther. 33, 335–343. doi: 10.1016/0005-7967(94)00075-U
Lowey, S. E., Norton, S. A., Quinn, J. R., and Quill, T. E. (2014). A place to get worse: perspectives on avoiding hospitalization from patients with end-Stage cardiopulmonary disease. J. Hosp. Palliat. Nurs. 16, 338–345. doi: 10.1097/NJH.0000000000000081
Lyu, X., Liu, Y., Yu, H., Mi, M., Shang, L., Zhong, Y., et al. (2020). Development and validation of a risk perception scale of medical help-seeking behavior in Chinese adults. Annals Transl. Med. 8:1352. doi: 10.21037/atm-20-1656
Ma, X., Li, S., Yu, S., Ouyang, Y., Zeng, L., Li, X., et al. (2020). Emergency Management of the Prevention and Control of novel coronavirus pneumonia in specialized branches of hospital. Acad. Emerg. Med. 27, 312–316. doi: 10.1111/acem.13958
Mavridou, P., Dimitriou, V., Manataki, A., Arnaoutoglou, E., and Papadopoulos, G. (2013). Patient's anxiety and fear of anesthesia: effect of gender, age, education, and previous experience of anesthesia. A survey of 400 patients. J. Anesth. 27, 104–108. doi: 10.1007/s00540-012-1460-0
McCowan, R. J., and McCowan, S. C. J. O. S. (1999). Item analysis for criterion-referenced tests. Buffalo, New York: Research Foundation of SUNY/Center for Development of Human Services.
Mohan, B., Kumar, R., Attri, J. P., Chatrath, V., and Bala, N. (2017). Anesthesiologist's role in relieving Patient's anxiety. Anesth Essays Res. 11, 449–452. doi: 10.4103/0259-1162.194576
Nikitara, M., Constantinou, C. S., Andreou, E., Latzourakis, E., and Diomidous, M. (2020). Views of people with diabetes regarding their experiences of the facilitators and barriers in type 1 diabetes inpatient care: An interpretative phenomenological analysis. Behav. Sci. 10:120. doi: 10.3390/bs10080120
Pan, B., Yuan, Z., Zou, J., Cook, D. M., and Yang, W. (2016). Elderly hospitalization and the new-type rural cooperative medical scheme (NCMS) in China: multi-stage cross-sectional surveys of Jiangxi province. BMC Health Serv. Res. 16:436. doi: 10.1186/s12913-016-1638-5
Raju, B., and Reddy, K. (2017). Are counseling services necessary for the surgical patients and their family members during hospitalization? J. Neurosci. Rural Pract. 8, 114–117. doi: 10.4103/0976-3147.193551
Raykov, T., and Marcoulides, G. A. (2016). On the Relationship Between Classical Test Theory and Item Response Theory:From One to the Other and Back. Educ. Psychol. Meas. 76, 325–338. doi: 10.1177/0013164415576958
Ren, J., Han, D., Zhang, J., Wang, Y., Huang, Q., Tian, T., et al. (2021). Development and psychometric testing of the supportive care needs scale for patients with tuberculosis (SCN-TB). Patient Prefer. Adherence 15, 2267–2278. doi: 10.2147/PPA.S330225
Schreiber, J. B. (2021). Issues and recommendations for exploratory factor analysis and principal component analysis. Res. Soc. Admin. Pharmacy 17, 1004–1011. doi: 10.1016/j.sapharm.2020.07.027
Schreiber, J. B., Nora, A., Stage, F. K., Barlow, E. A., and King, J. (2006). Reporting structural equation modeling and confirmatory factor analysis results: a review. J. Educ. Res. 99, 323–338. doi: 10.3200/JOER.99.6.323-338
Şencan, H. J. A. S. P. (2005). Reliability and validity in social and behavioral measurements. 1st edn. Seçkin Publishing Industry and Trade Inc.
Shi, J., Mo, X., and Sun, Z. (2012). Content validity index in scale development. Zhong Nan Da Xue Xue Bao Yi Xue Ban 37, 152–155. doi: 10.3969/j.issn.1672-7347.2012.02.007
Spielberger, C. J. P. A. (1989). State-Trait Anxiety Inventory: Bibliography. 2nd edn. Palo Alto, CA: Consulting Psychologists Press.
Steward, M. S., and Steward, D. S. J. N. D. (1981). “Children’s conceptions of medical procedures,” in Children’s conceptions of health, illness, and bodily functions: New directions for child development. eds. R. Bibace and M. E. Walsh (San Francisco, CA: Jossey-Bass), 67–84.
Tavakoli, P., Cheraghi, M. A., Jahani, S., and Asadizaker, M. (2022). Experience of discomfort and its self-management strategies in ICU patients. J. Fam. Med. Primary Care 11, 269–276. doi: 10.4103/jfmpc.jfmpc_481_21
Tesfaw, A., Alebachew, W., and Tiruneh, M. (2020). Why women with breast cancer presented late to health care facility in north-West Ethiopia? A qualitative study. PLoS One 15:e0243551. doi: 10.1371/journal.pone.0243551
Theunissen, M., Jonker, S., Schepers, J., Nicolson, N. A., Nuijts, R., Gramke, H.-F., et al. (2018). Validity and time course of surgical fear as measured with the surgical fear questionnaire in patients undergoing cataract surgery. PLoS One 13:e0201511. doi: 10.1371/journal.pone.0201511
Theunissen, M., Peters, M. L., Schouten, E. G. W., Fiddelers, A. A. A., Willemsen, M. G. A., Pinto, P. R., et al. (2014). Validation of the surgical fear questionnaire in adult patients waiting for elective surgery. PLoS One 9:e100225. doi: 10.1371/journal.pone.0100225
Tiwary, A., Rimal, A., Paudyal, B., Sigdel, K. R., and Basnyat, B. (2019). Poor communication by health care professionals may lead to life-threatening complications: examples from two case reports. Wellcome Open Res. 4:7. doi: 10.12688/wellcomeopenres.15042.1
van Bruggen, V., Ten Klooster, P. M., van der Aa, N., Smith, A. J. M., Westerhof, G. J., and Glas, G. (2018). Structural validity of the world assumption scale. J. Trauma. Stress 31, 816–825. doi: 10.1002/jts.22348
Wang, Y., and Sun, A. J. C. M. G. (2011). Statistical estimation of correlation validity of test criteria. Chin. Med. Guide 9, 234–235. doi: 10.15912/j.cnki.gocm.2011.31.025
Weltens, I., Bak, M., Verhagen, S., Vandenberk, E., Domen, P., van Amelsvoort, T., et al. (2021). Aggression on the psychiatric ward: prevalence and risk factors. A systematic review of the literature. PLoS One 16:e0258346. doi: 10.1371/journal.pone.0258346
Wilson, C. J., Mitchelson, A. J., Tzeng, T. H., El-Othmani, M. M., Saleh, J., Vasdev, S., et al. (2016). Caring for the surgically anxious patient: a review of the interventions and a guide to optimizing surgical outcomes. Am. J. Surg. 212, 151–159. doi: 10.1016/j.amjsurg.2015.03.023
Wu, X.-F., Kong, W.-F., Wang, W.-H., Yuan, L.-X., Xu, H.-Q., Qi, M., et al. (2019). Enhanced recovery after surgery protocols in functional endoscopic sinus surgery for patients with chronic rhinosinusitis with nasal polyps: a randomized clinical trial. Chin Med J (Engl) 132, 253–258. doi: 10.1097/CM9.0000000000000060
Wu, J., and Zhu, J. (2019). Validity and reliability of the Sinicization of the surgical fear questionnaire in breast and thyroid surgery patients undergoing elective surgery in a tertiary Hospitial in Wuhan. Med. Soc. 32, 65–68. doi: 10.13723/j.yxysh.2019.11.016
Zung, W. W. (1971). A rating instrument for anxiety disorders. Psychosomatics 12, 371–379. doi: 10.1016/S0033-3182(71)71479-0
Keywords: fear, hospitalization, outpatients, psychometric validation, cross-cultural adaptation, factor analysis
Citation: Li W, Yu H, Zhang Y, Li B and Fu M (2023) Psychometric evaluation of the Chinese version of fear of hospitalization scale among outpatients: A validation study. Front. Psychol. 13:1095905. doi: 10.3389/fpsyg.2022.1095905
Edited by:
André Luiz Monezi Andrade, Pontifical Catholic University of Campinas, BrazilReviewed by:
Maryam Rassouli, Shahid Beheshti University of Medical Sciences, IranHamid Sharif Nia, Mazandaran University of Medical Sciences, Iran
Mahmut Akbolat, Sakarya University, Turkey
Copyright © 2023 Li, Yu, Zhang, Li and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hongyu Yu, ✉ MTU4NDAwNDAwNTNAMTYzLmNvbQ==
 Wenbo Li
Wenbo Li Hongyu Yu
Hongyu Yu Yanli Zhang
Yanli Zhang Bing Li
Bing Li Mingshu Fu
Mingshu Fu