
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 16 January 2023
Sec. Developmental Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.1095030
 Maria C. Gioia1,2
Maria C. Gioia1,2 Antonio Cerasa3,4,5*
Antonio Cerasa3,4,5* Vito M. R. Muggeo6
Vito M. R. Muggeo6 Paolo Tonin5
Paolo Tonin5 Juanita Cajiao7
Juanita Cajiao7 Alessia Aloi2
Alessia Aloi2 Iolanda Martino8
Iolanda Martino8 Flaviana Tenuta9
Flaviana Tenuta9 Angela Costabile9
Angela Costabile9 Francesco Craig9,10
Francesco Craig9,10Maternal-Fetal Attachment (MFA) delineates the emotional, cognitive, and behavioral aspects that mothers develop toward the unborn baby during pregnancy. The literature indicates that optimal attachment in pregnancy represents a protective factor for the mother-child attachment bond after birth and child development outcomes. To date, there are few studies that have investigated associated factors of MFA. This study sets out to explore the association between perceived parental bonds and maternal-fetal bonding in pregnant women, accounting for factors such as psychological distress, socio-demographic and obstetric characteristics.
Methods: In this cross-sectional study, 1,177 pregnant women answered the Parental Bonding Instrument, the Maternal-Fetal Attachment Scale, State-Trait Anxiety Inventory (STAI-Y), and Beck-Depression Inventory (BDI-II).
Results: We found out that perceived maternal and paternal care had significant direct effects on maternal-infant bonding during the pregnancy period when controlling for some confounders, including gestational age and mother age among others. Such maternal and paternal perceived care effects were not mediated by levels of psychological distress, which in turn resulted to be a “borderline” significant predictor of prenatal attachment. Interestingly, the gestational age and the mother age emerged to have a significant and synergic nonlinear effect, suggesting the influence on the MFAS of the gestational age depends on the values of the mother age, and likewise, the effect of mother age on MFAS depends on the gestational week.
Conclusion: This study expands our knowledge of the intergenerational transmission of attachment pointing out the effects of a woman’s perceived bond in relation to her parental figures during the development of the prenatal attachment process. Findings also suggests that parenting support interventions may have benefits that are realized across generations.
The experience of pregnancy has a strong impact on women’s lives. It is a unique period that might produce specific difficulties for the future mothers, adapting to this challenge through positive and negative reactions (Walsh, 2010; Su et al., 2015; Copeland and Harbaugh, 2019). Considering the importance of the child’s representation in the early developmental stages of pregnancies, some authors have studied the internal emotional representation of the future newborn and the maternal-fetus prenatal relationship as a unique experience (Atashi et al., 2018). Some authors have used the term “maternal–fetal attachment” (MFA) to define the emotional attachment between the mother and fetus as an indicator of their health and the mother’s efficiency in the postnatal period (Ckanley, 1981; Alhusen, 2008). Similarly, some researchers used the term “prenatal attachment”, referring to an emotional relationship that parents develop toward the unborn baby during the gestation period (Brandon et al., 2009; Atashi et al., 2018). The extensive literature on prenatal attachment has demonstrated that maternal prenatal attachment contributes to structuring the perception of the child as a human being and future developments of the attachment between the mother and the baby (Akbarzadeh et al., 2016; McNamara et al., 2019; Howland et al., 2020). Through this relationship, during the gestation period the woman expresses to the fetus concerns, affections, and expectations, influencing the postnatal maternal-child attachment and the adequacy of the care (McNamara et al., 2019; Salehi et al., 2019; Howland et al., 2020). In a recent systematic review of 41 studies, Rollè et al. (2020) reported that poor prenatal attachment is linked with low prenatal maternal fetus representations and self-care, low postnatal attachment until 24 months postpartum and early child development problems such as emotional self-regulation, behavioral and cognitive difficulties (Alhusen et al., 2012b; Maddahi et al., 2016; Rossen et al., 2016; Daglar and Nur, 2018; Arguz Cildir et al., 2020). Therefore, it is important to be aware of the factors that may have an influence on a prenatal attachment process and attachment-related behavior.
A key element that might be associated with prenatal attachment is the woman’s perceived bond in relation to own parental figures during her childhood and adolescence, denominated parental bond. Bowlby states that the mother’s psychological state during parenting is related to “a long history of interpersonal relations within her family of origin” (Bowlby, 1982), suggesting that parental bonding is the perception of established bonds that a person has toward his/her parents. Therefore, the parenting of grandparents could regulate the behaviors and emotions of mothers toward their children. These attitudes in future mothers are associated with better quality of maternal-fetus prenatal attachment since positive past parental behaviors contribute to consolidating levels of care and protection and positive interactions between the mother and her fetus (Handelzalts et al., 2018). Care and protection are two important components in child-rearing and adequate parenting is attributed to high care and low protection (Parker, 1990). One study by Reed (2014) suggests that the combination of high parental overprotection and low care during a woman’s childhood presents a risk factor for weakened prenatal attachment levels and potentially low levels of attachment after birth. In contrast, a previous study detected a positive correlation between paternal overprotection and the intensity of maternal concern, particularly in the second gestational trimester (Van Bussel et al., 2010). da Rosa and colleagues, in a recent large-sample longitudinal study, detected the importance of the father’s role in the women’s life, showing that the gestational women who perceived paternal overprotection during their development reported better prenatal attachment (da Rosa et al., 2021). Thus, empirical data regarding the potential relationship between perceived parental bonding and the relationship between a pregnant woman and her fetus are scarce and inconclusive. Moreover, the literature shows that the quality of the mother’s attachment and maternal behaviors to her fetus has important implications in the postnatal period, influencing the postnatal attachment and the adequacy of the care (Tambelli et al., 2014; Ana Luisa et al., 2019; McNamara et al., 2019; Howland et al., 2020; Lutkiewicz and Bidzan, 2022). Considering the above mentioned findings, it is evident the importance of identifying associated factors of the prenatal attachment process, such as a parental bond, since it is implicated with negative outcomes for the infant-mother dyad.
Furthermore, during the transition to parenthood, which is a time of intense psychological change, women are also at risk for the onset of psychological distress. The World Health Organization reports that about 10% of pregnant women experience psychological distress, especially anxiety and depression that generally leads to adverse outcomes for early mother-child bonding (WHO). Prenatal anxiety, depression, and stress can result in pregnancy complications, as well as difficulties in the establishment of the mother-infant bond, which adversely affects the pregnant women’s attachment process, which is essential to the baby’s psychological development. Some authors suggested that psychological distress may compromise capacity to feel adequate in her new role as mother or be related with a general state of detachment that also affects her ability to bond with the fetus (Isgut et al., 2017; Tokuda et al., 2021). Additionally, a noteworthy number of studies have looked at the relationship between psychological distress and parental bonding, showing that the clinical population reported lower parental care than the general population (Røhder et al., 2020). Previous studies, using the Parental Bonding Instrument (PBI), showed that poor parenting styles, characterized by “low care” or “high overprotection” are also associated with anxiety and depressive symptoms in women in the perinatal period (McMahon et al., 2005; Fukui et al., 2021). So far, however, the associations between prenatal parental reflective functioning, psychological distress, and specific dimensions and risk profiles of maternal-fetal bonding in pregnant women have not been closely examined. It has been reported that several socio-demographic and obstetric characteristics such as socioeconomic status, pregnancy age, education level, unplanned pregnancy, being primigravida, social support quality and quantity, may be associated with worse MFA or onset of bonding disorder (Alhusen et al., 2012a; Jamshidimanesh et al., 2013; Lau et al., 2018; Sacchi et al., 2021). Thus, the identification of several risk factors in this regard is a pressing research topic.
The study’s aim is to examine how parental bonding and psychological distress are associated with maternal fetal attachment in a broad sample of pregnant women. Our pre-analyses conjectures are reported in Figure 1: first, parental perceived bonds could predict maternal–fetal attachment quality in the perinatal period; second, psychological distress would mediate the relationship between parental bonding and maternal–fetal attachment. Other socio-demographic and obstetric characteristics have been evaluated as possible confounders.
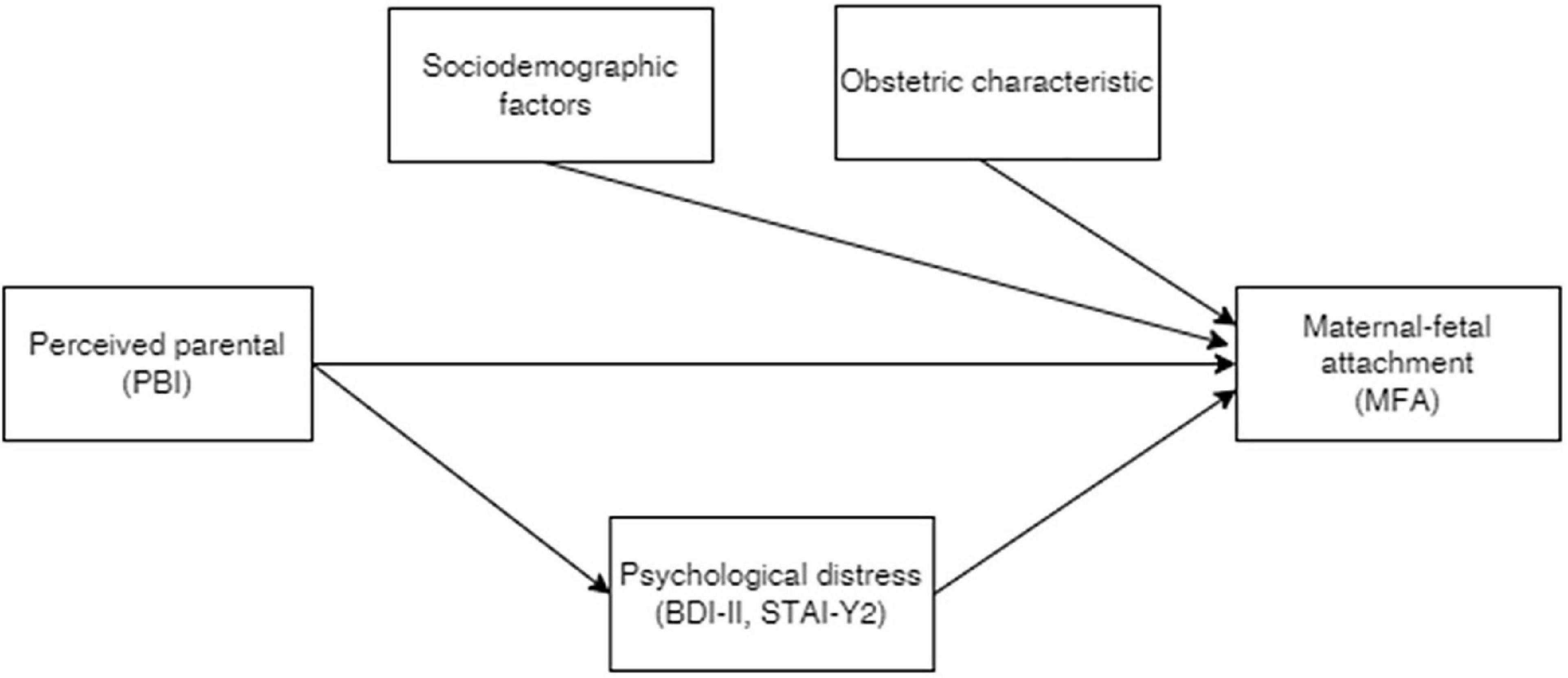
Figure 1. The conjectured relationships between the response maternal–fetal attachment (MFA), parental bonding instrument (PBI), and psychological distress.
The study was authorized by the University of Calabria Ethics Committee (Protocol number: 0013005). The study was conducted in accordance with the Declaration of Helsinki. Data collection took place from 14 March and 25 April 2020 among pregnant Italian women. The study was conducted through an anonymous, web-based, cross-sectional survey developed with Google Forms, and was supported by two local non-governmental associations, the “Associazione di Volontariato Mammachemamme” and the “Movimento di Psicologia Perinatale”. The survey’s URL was sent to the participants through social media, emails, and advertisements in Italian prenatal and natal clinics. The inclusion criteria were as follows: willing to participate, having reading skills and language comprehension to complete the self-report questionnaire, no history of mental disorders or substance abuse and drug addiction. The intent of the study was explained to the participants, who gave formal consent and did not receive any reward.
A questionnaire containing items about the mother’s age, civil status, educational level, disease history, number of children, gestational age, history of abortion, pregnancy complication was used to collect the socio-demographic and obstetrics data.
Maternal–fetal attachment in pregnant women were measured through the Maternal–Fetal Attachment Scale (MFAS) (Ckanley, 1981). The MFAS is a 24-item self-report questionnaire developed to measure the extent of the attachment between a mother and her unborn child. Each item is scored from 1 (Definitely No) to 5 (Definitely yes). The total score ranges from 24 to 120 and higher scores indicate greater attachment between mother and fetus. Negative items namely item numbers 9 and 24 will be reverse scored. MFAS contains five subscales: Differentiation of self; Interaction with the fetus; Attributing characteristics and intentions; Giving of Self; Role taking. The reliability (internal consistency) of the scale was assessed and reported as α = 0.85 by its developer (Ckanley, 1981). Busonera and colleagues (Busonera et al., 2016) evaluated the validity and reliability of the Italian version of this tool and calculated Cronbach α coefficient. The total MFAS scale showed a good internal consistency, with α of 0.77. Item–scale correlations ranged from 0.22 to 0.44.
Prenatal bonding was measured through the PBI (Parker, 1990). The PBI is a 25-item self-report measure of two parenting styles, “Care” and “Overprotection/Control.” The instrument assesses these self-perceived relationships separately for the mother and the father. The care dimension measures positive parenting, including parental warmth and affection. The Control dimension measures negative parenting, including parental control and constraint. We chose the PBI because it is a widely used tool for examining the relationship between parental attitudes and mental-physical health in different populations such as pregnant women. A test-retest reliability study yielded a Pearson correlation coefficient for the care scale of 0.761 and a Pearson correlation coefficient for the overprotection scale of 0.628 (Parker, 1990).
To estimate levels of state and trait anxiety, the survey used is the State-Trait Anxiety Inventory (STAI-Y) (Spielberger and Sydeman, 1994). The items investigating state anxiety are 20 (STAI Form Y-1), exploring feelings of tension, anxiety, and nervousness. Trait anxiety levels are explored with the 20 items of the trait anxiety scale (STAI FORM Y-2), estimating anxiety levels, with a four-point Likert scale. For both scales, scores ranged from a minimum of 20 to a maximum of 80. Mild anxiety is indicated by a cutoff score of 40–50, while 50–60 indicates moderate anxiety, and over 60 indicates severe anxiety. Internal consistency of the scale ranges from 0.86 to 0.95; test-retest reliability ranges from 0.65 to 0.75 in a 2-month interval. In the present study, test-retest coefficients ranged from 0.60 to 0.89.
Depression levels were measured through the Beck-Depression Inventory (BDI-II), consisting of 21 self-report items (Beck et al., 1996). This scale is very effective for the assessment of depression symptoms and of their severity in the population. The items have a rating from zero to three and are summed to obtain a global score of 0–63, with higher scores associated to higher levels of depression. In the range 0–13 the score indicates minimal depression, 14–19 mild depression, 20–28 moderate depression, and 29–63 severe depression. Internal consistency of the test was around 0.92 and test-retest reliability is 0.93.
Symmetric relationships among numeric variables were investigated by means of the Pearson correlation coefficients. The parental perceived bonds are represented by two pairs of variables for both mother and father, namely: the maternal/paternal perceived care (MPC and PPC) and the maternal/paternal perceived over-protection (MPO and PPO). To quantify their effects on the maternal-fetus attachment (MFAS), we ran a regression model for the expected value of MFAS as a function of MPC, PPC, MPO, and PPO, also including additional variables such as mother age, previous childbirth, gestational age and psychological distress (STAI-2 and BDI). Moreover, to assess if the parental bonds effects on MFAS were also partially “mediated” by the psychological distress, specifically the STAI-2 and BDI-II variables, we fitted a second regression model having the STAI-2 and BDI-II as a response and the same aforementioned factors as covariates. Taking the two fitted regression models as input, we carried out mediation analysis (Mackinnon, 2012) to estimate the average direct effects (ADE) and the average conditional mediated effects (ACME).
The statistically significant P-value was set at 0.05. All statistical analyses were done using the software R (version 4.0.5) and packages mediation (Imai et al., 2010) and betareg (Cribari-Neto and Zeileis, 2010).
Table 1 shows the socio-demographic, obstetric, and clinical characteristics of the participants of the n = 1,179 pregnant women enrolled in the study. The age ranging from 18 to 56 years (32.83 ± 4.3 years), and the mean gestational age ranging from 5 to 41 weeks 26.28 ± 8.9. Most of the participants were married (63,2%) and nearly half of them had University degrees (46.6%). With respect to pregnancy aspects, the 42,7% had previous pregnancies, the 26,6% reported history of abortion, and the 13,2% had pregnancy complication.
The mean total score on the MFAS was 91.8, and the mean subscale score were: 16.6 (Differentiation of self), 19.2 (Interaction with the fetus), 20.4 (Attributing characteristics and intentions), 17.9 (Giving of Self), 17.7 (Role taking). The mean total score for STAI Form Y-2 and BDI-II was 43.9 and 12.4, respectively. 63.4% of women had no depressive symptoms, 18.9% had mild depressive symptoms, 14.2% had moderate symptoms and only 3.5% severe symptoms. On the Trait-Anxiety scores, 23.2% had mild trait anxiety levels, 31.1% had moderate levels and 28% had severe levels. Among the anxiety levels, out of 1,179 women 36.6% had mild state anxiety levels, 20.4% had moderate levels, and 7% had severe levels.
We fit a regression model including the MFAS score as the outcome variable and the parental bonds scores, namely MPC, MPO, PPC, and PPO. Also, socio-demographic/obstetric characteristics, depression symptoms, and trait anxiety were entered simultaneously as explanatory variables. Results reported in Table 2 indicated that both maternal (p = 0.022) and paternal (p = 0.004) perceived care is significatively and positively associated with MFAS, sharing a somewhat similar effect on the response; on the other hand, no significant effect was found for the overprotection scores, i.e., MPO and PPO. Moreover, we found no evidence against linearity in the effects of MPC/MPO and PPC/PPO on the MFAS and also no relevant interaction terms between such variables were deemed to be significant, suggesting no synergic effect on the response.
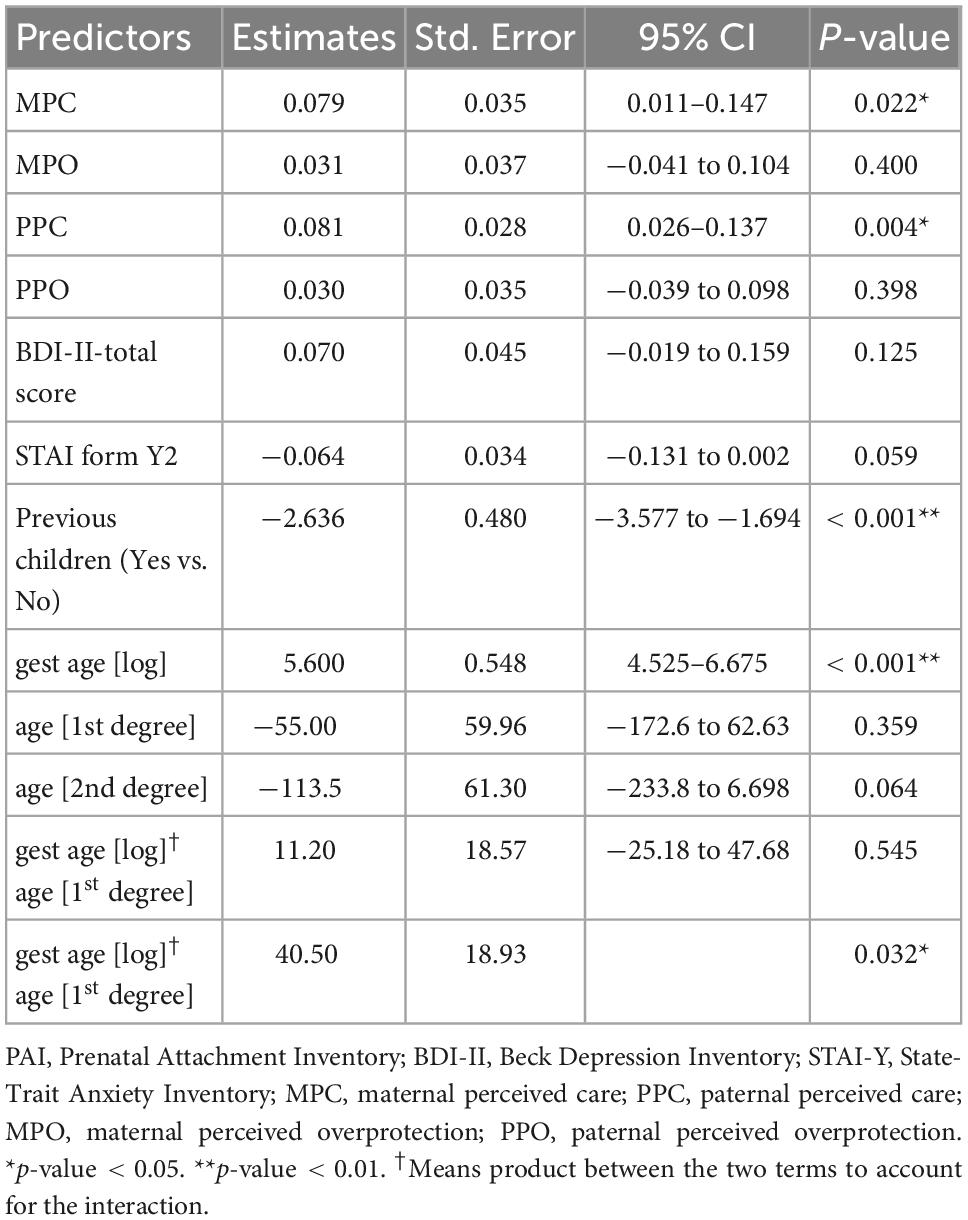
Table 2. Parameter estimates for the outcome regression model having Maternal–Fetal Attachment Scale (MFAS) a response.
Significant effects on the fetus attachment were also obtained for the “previous childbirth” and the psychological distress as measured by trait anxiety (“STAI-form Y2”) exhibiting a somewhat borderline but noteworthy p-value (p = 0.059). Depression level (BDI-II score) appears not to be related to the fetus stimulus. To investigate the mediating role of STAI-form Y2 in the relationships between MFAS and MPC/PPC we ran a mediation analysis by fitting the “mediator” regression model having the STAI-form-2 as response and the same covariates of the outcome model (Table 3): results of mediation analysis suggest that the effect of parental perceived cares, both MPC and PPC, on MFAS are entirely direct with no mediating role of STAI form 2.
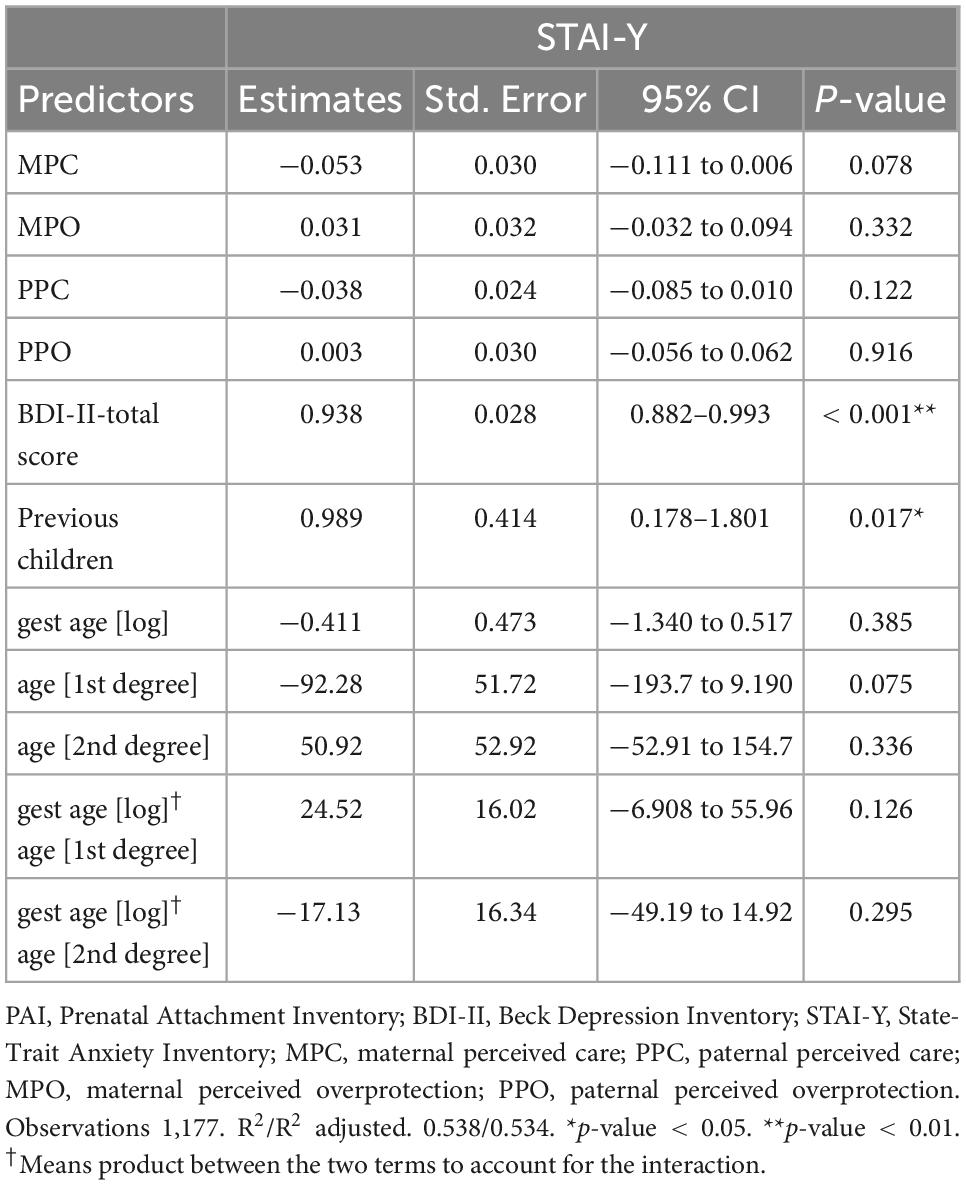
Table 3. Parameter estimates for the mediator regression model having State-Trait Anxiety Inventory (STAI) form Y2 as a response.
We found strong evidence that both MPC and PPC have a significant effect on fetus attachment. As a sensitivity analysis, we also checked for possible non-linear and synergic effects, but no evidence was found.
In addition, we repeated the regression analysis with all five MFAS subscales as outcome variables. Results showed that MPC is a significant predictor of Role Taking (p = 0.038), Differentiation of self from fetus (p = 0.044), and Interaction with fetus (p = 0.009); while PPC is a significant predictor of Role Taking (p = < 0.001) and Attributing characteristics to fetus (p = 0.024). Results are summarized in Table 4.

Table 4. Estimated total effect, relevant p-value and proportion of the effect mediated by STAI2 for the variables maternal perceived care (MPC) and paternal perceived care (PPC) on different outcomes.
Interestingly, the gestational age and the mother age emerged to have a significant and synergic non-linear effect, suggesting the influence on the MFAS of the gestational age depends on the values of the mother age, and likewise, the effect of mother age depends on the gestational week. Non-linearity in both covariates was modeled via a quadratic polynomial (for the mother age) and the log transformation for the gestational age. Figure 2 depicts such non-linear and synergic effects.
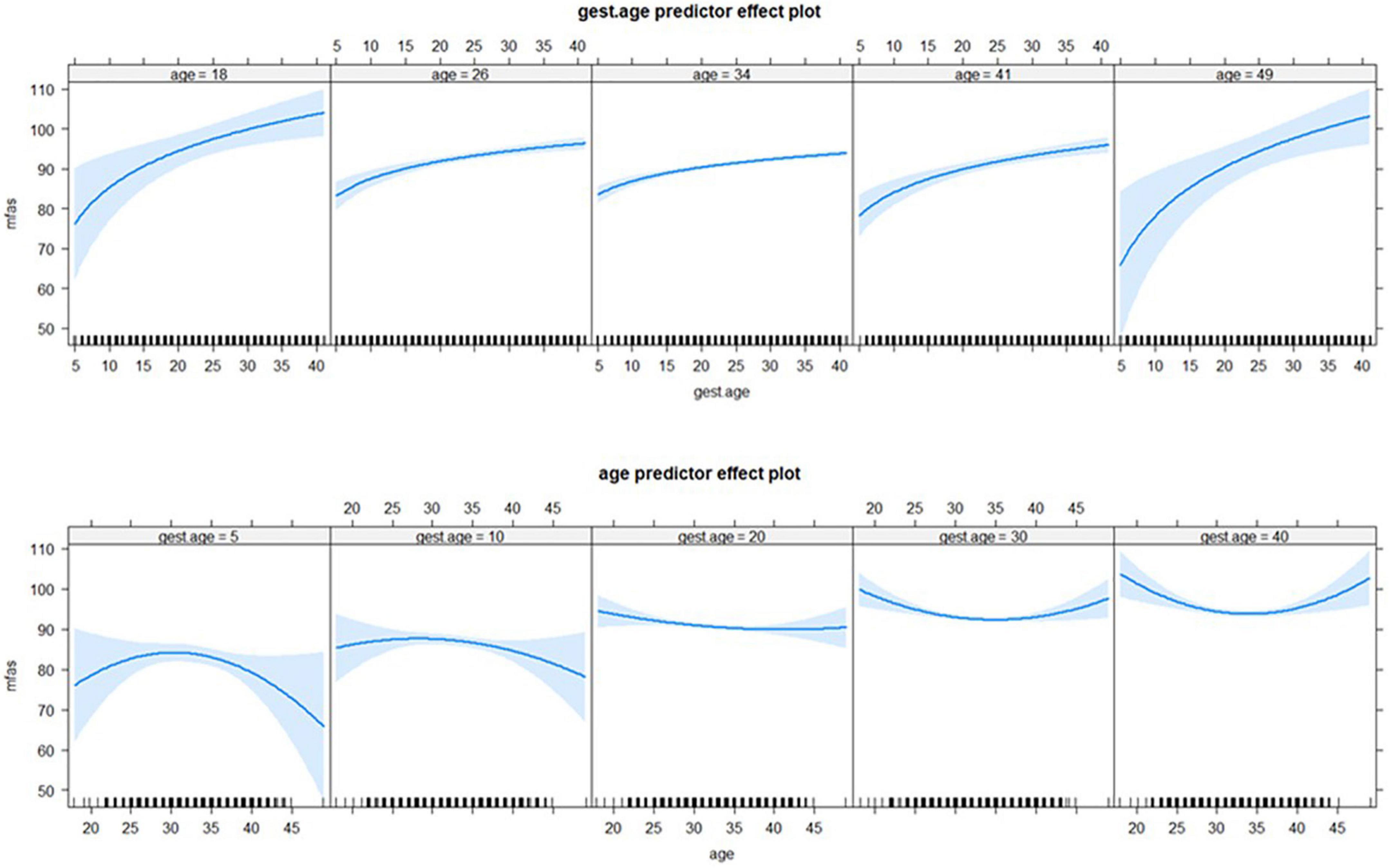
Figure 2. The synergic non-linear effect of mother age and gestational age on MFAS: The top panels portray the effect of gestational age by different values of mother age (18, 26, 34, 41, and 49 years). Specularly, the bottom panels show the effect of mother age by specific values of gestational age i.e., at 5, 10, 20, 30, and 40 weeks.
The objective of this study was to evaluate the effects of perceived parental bonding on maternal prenatal attachment, after controlling for relevant psychological distress symptoms, and socio-demographic and obstetric variables. The main findings revealed that perceived maternal and paternal care both had significant direct effects on maternal–infant bonding during the pregnancy period, indicating that the pregnant women who perceived high parental care during their childhood and adolescence had positive maternal-fetal relationships. Psychological distress was considered as the observed variable that acts as a mediator in the model, however, the effect of parental care on MFA is not mediated by levels of anxiety or depression. Further, no significant relations were found between the perceived maternal/paternal control and MFAS scores. These findings accord with that of Fukui et al. (2021) who found that perceived care for maternal and paternal parenting is a predictor of the attachment process during the pregnancy period. However, the current result is not unexpected given that positive parental or caregivers care represents a protective factor for child cognitive-emotional-social development, and resilience and self-esteem in adulthood (Enns et al., 2002; Tian et al., 2018; Sameshima et al., 2021); while excessive parental control or intrusive behavior hinders the ability to be independent and increases the risk of insecure attachments, and emotional and behavioral problems (Festa and Ginsburg, 2011; Sameshima et al., 2021; Kidd et al., 2022). Hence, the current result suggests that women who receive adequate care from their father or mother before adolescence establish sufficient bonding with their infants in the perinatal period. This is in line with the developmental perspective of intergenerational transmission of parenting style, indicating continuity in the style across generations (Van Ijzendoorn, 1992). Intergenerational transmission is considered the influence of parents’ own experiences as a child on their later childrearing practices (Jarnecke and South, 2013; de Cock et al., 2016; Taccini et al., 2021). Although the majority of studies have focused on the intergenerational continuity of trauma transmission or aggressive-intrusive parenting (Belsky et al., 2009; Ahlfs-Dunn et al., 2022), there is a body of research suggesting such transmission exists also true for warm and supportive parenting (Kretchmar and Jacobvitz, 2002; Madden et al., 2015). Intergenerational transmission of parenting can be explained by genetic and environmental factors (Branje et al., 2020; Craig et al., 2021). First, recent developments in epigenetic research have led to a growing interest in the effects of parental care on the role of biological mechanisms (e.g., DNA methylation) in mediating environmentally induced changes in parental care that are transmitted across generations (Champagne, 2008; Montirosso et al., 2020; Craig et al., 2021). Hence, understanding whether the relationship between perceived parental care and maternal-fetal attachment would be mediated by epigenetic mechanisms could be a key issue in future studies. Second, a direct mechanism is a child observes the behavior of his/her parents and reproduces this parental style when becoming a parent or a child develops an attachment style because of parent-infant interaction, which is replicated when the child becomes a parent (Madden et al., 2015), probably already during the pregnancy period when the prenatal attachment is developing. In support of this possibility, we have found a significant direct effect of perceived both maternal and paternal bonding on the MFAS subscales, in particular the role-taking scale, attributing characteristics to fetus, differentiation of self from fetus, and interaction with fetus. These findings suggest that women who receive adequate care from their father or mother reported mostly positive feelings toward their pregnancy with greater pregnancy acceptability, and they can more easily establish a relationship with their fetus and attribute emotions or behaviors to it. Adjusting to parenthood during pregnancy brings with it lots of biological, physical, and psychological changes that make them particularly vulnerable to psychological distress. Thus, high perceived parental care could be a protective factor for adjusting to the idea of pregnancy and motherhood leading to a decrease in distress, and better antenatal bonding. However, this hypothesis must be interpreted with caution because of several confounding factors not included in this study such as the role of gender, relationship quality, and social support (della Vedova et al., 2019; Göbel et al., 2019; Sacchi et al., 2021).
Another important finding was that state anxiety resulted to be a “borderline” significant predictor of prenatal attachment after adjusting for the other socio-demographic and obstetric information. We found that women who have a higher state of anxiety may experience a lower quality of maternal-fetal attachment. In accordance with the present results, previous studies have demonstrated that anxiety is one of the strongest predictors of poor psychological well-being in pregnant women and of lower quality of MFA (Allison et al., 2011; Mazzeschi et al., 2015; Napoli et al., 2020). It is possible, that elevated state anxiety during pregnancy influences the quality of prenatal attachment, meaning less time on attachment-related behavior (e.g., palpating, talking, and thinking to the fetus) or may result in less pre-occupation with the pregnancy and the fetus (i.e., as reflected in lower maternal-fetal attachment scores). Thus, the results from our study expand prior findings by suggesting that pregnant women who experienced anxiety during pregnancy may be at an elevated risk of reporting a decreased amount of interaction with their fetus (Shahhosseini et al., 2015; Napoli et al., 2020). In contrast to expectations (Rollè et al., 2020), this study did not find a significant association between depression and MFAS scores. However, it is necessary to interpret these results with caution due to the many studies that did not confirm these results. The absence of a significant association, also in the current study, could be due to methodological issues such as assessment time, type of target population or confounding variables that were controlled for and that consequently hid the effect of prenatal depression symptoms on prenatal attachment (e.g., disease history, number of children, gestational age, history of abortion, pregnancy complication).
In the multivariable analysis, gestational age and the age of the woman appear to influence prenatal attachment. As expected, gestational age showed a positive association with MFA. These results corroborate the findings of a great deal of the previous works. It has been demonstrated that prenatal attachment behaviors increase with advancing gestational age and the latter is associated with a positive effect on the fetus such as thinking about her involvement in the dyadic interaction, and interaction and maternal planning (Barone et al., 2014). Hence, it is possible to assume that the women can perceive the new movements of the baby during pregnancy, which makes the experience more corporeal for them and may lead them to interact more adequately with the fetus. In addition, previous studies also detected that MFA intensity may be affected by factors such as maternal age (Čėsnaitė et al., 2019; McNamara et al., 2019). Pregnant women who were younger than 20 years shows the lowest levels of prenatal attachment compared to women who were older (Ossa et al., 2012; Canlı and Demirtaş, 2022). It may be that younger women may experience ambiguous and mixed feelings about the physical and psychological changes during pregnancy and may not feel ready to be mothers (Crozier et al., 2009; Wilson-Mitchell et al., 2014), all of which may blunt their prenatal attachment levels. In contrast, other studies detected no association between participants’ ages and prenatal attachment (Daglar and Nur, 2018; Ulu and Bayraktar, 2018). We found that the relationship between MFA and the mother’s age is quadratic. Prenatal attachment is greater for both younger and older women and reaches a minimum of around 34 years of age. Interestingly, the finding showed the synergic non-linear effect of mother age and gestational age on MFAS. The maternal prenatal attachment is higher for women around 30–35 years old in the early weeks (within 10, say) of the gestational period, but in the late gestational period (after 30 weeks, say) the relationship is the opposite and the maternal prenatal attachment is higher for younger or older women rather than the middle women aged 30–35 years. Most of the studies considered a diverse range of individual and obstetrics variables as potential risk or protective factors, but no one has yet evaluated the interaction between them. Elucidating the role of a combination of the mother’s age together with gestational age in a prenatal attachment will be a new direction for future studies.
Some limitations deserve mention. The first limitation of the study is the lack of a representative group of at-risk pregnant women. The inclusion/exclusion criteria precluded some at-risk pregnant women from participating in the study as women with psychopathological disorders or women with a history of mental disorders or adverse experiences during the past years. Several studies detected that a history of mental health problems or adverse experiences prior to pregnancy is associated with a decreased quality of mother-fetus interaction (Aktar et al., 2019; Smorti et al., 2020). Thus, further studies need to be carried out because the history of the pregnant women may interfere with biological and psychological mechanisms underpinning the mother-infant bond. Second, there is the risk of a memory bias, since the PBI is a measure that examines the perception of the past. In addition, limitations of the use of self-administered questionnaires like the PBI compared to other forms of assessment such as interviews, semi-structured interviews, or grids should be considered. Third, we did not have data on additional factors such as the sex of the infants, resilience and coping strategies of parents, and social support of pregnant women that might have an impact on the prenatal attachment process. Four, due to the cross-sectional design of the study, we cannot directly draw conclusions about cause and effect. Still, to our knowledge, the current study is the first report to include measures of parental bonding, psychological distress, and maternal-fetal attachment during pregnancy. An additional uncontrolled factor is the paternal-fetal attachment. Previous studies revealed that partners have lower fetal attachment scores than pregnant women (Dayton et al., 2019), thus clinical perinatal psychologists, midwives, and nurses have a great responsibility in terms of assessing and promoting attachment behaviors also in partners.
Intergenerational transmission of parenting has been documented in different samples population studies and countries. However, previous studies have mainly focused on the mother-child attachment bond after birth. This study expands our knowledge on the effects of a woman’s perceived bond in relation to her parental figures during childhood and adolescence on the prenatal attachment process in a large population cohort of pregnant women. The results of this study indicate that maternal and paternal care parenting may affect the maternal-fetal bonding of the expectant mother positively. This heightens the hypothesis that parenting support and treatment may have advantages that are realized across generations. Further, by determining mothers’ attachment style and the status of maternal-fetal attachment during pregnancy, in time interventions and education could be planned for improving these interactions and consequently improve the mother-child attachment during and after pregnancy.
Dataset will be shared in accordance with explicit external requirements. Requests to access these datasets should be directed to ZnJhbmNlc2NvLmNyYWlnQHVuaWNhbC5pdA==.
FC substantial contributions to the conception, interpretation of data for the work, and revising it critically for important intellectual content, and drafting the work. MG substantial contributions to the conception, interpretation of data for the work, and revising it critically for important intellectual content. PT final approval of the version to be published. VM performed the statistical analysis, interpretation of data for the work, and drafting the work. JC design of the work and drafting the work. AA and IM design of the work and acquisition of data. FT revising it critically for important intellectual content. ACe and ACo final approval of the version to be published. All authors contributed to the article and approved the submitted version.
We are particularly grateful for the assistance given by “Associazione di Volontariato Mammachemamme” and “Movimento di Psicologia Perinatale (MIPPE)”.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Ahlfs-Dunn, S. M., Benoit, D., and Huth-Bocks, A. C. (2022). Intergenerational transmission of trauma from mother to infant: The mediating role of disrupted prenatal maternal representations of the child. Attach. Hum. Dev. 24, 229–251. doi: 10.1080/14616734.2021.1933769
Akbarzadeh, M., Dokuhaki, A., Joker, A., Pishva, N., and Zare, N. (2016). Teaching attachment behaviors to pregnant women: A randomized controlled trial of effects on infant mental health from birth to the age of three months. Ann. Saudi Med. 36, 175–183. doi: 10.5144/0256-4947.2016.175
Aktar, E., Qu, J., Lawrence, P. J., Tollenaar, M. S., Elzinga, B. M., and Bögels, S. M. (2019). Fetal and infant outcomes in the offspring of parents with perinatal mental disorders: Earliest influences. Front. Psychiatry 10:391. doi: 10.3389/fpsyt.2019.00391
Alhusen, J. L. (2008). A literature update on maternal-fetal attachment. J. Obstet. Gynecol. Neonatal Nurs. 37, 315–328. doi: 10.1111/j.1552-6909.2008.00241.x
Alhusen, J. L., Gross, D., Hayat, M. J., Woods, A. B., and Sharps, P. W. (2012b). The influence of maternal-fetal attachment and health practices on neonatal outcomes in low-income, urban women. Res. Nurs. Health 35, 112–120. doi: 10.1002/nur.21464
Alhusen, J. L., Gross, D., Hayat, M. J., Rose, L., and Sharps, P. (2012a). The role of mental health on maternal-fetal attachment in low-income women. J. Obstet. Gynecol. Neonatal Nurs. 41, E71–E81. doi: 10.1111/j.1552-6909.2012.01385.x
Allison, S. J., Stafford, J., and Anumba, D. O. C. (2011). The effect of stress and anxiety associated with maternal prenatal diagnosis on feto-maternal attachment. BMC Womens Health 11:33. doi: 10.1186/1472-6874-11-33
Ana Luisa, A. L. B. T., Callinan, L. S., and Smith, M. V. (2019). An examination of the impact of maternal fetal attachment, postpartum depressive symptoms and parenting stress on maternal sensitivity. Infant Behav. Dev. 54, 99–107. doi: 10.1016/j.infbeh.2019.01.001
Arguz Cildir, D., Ozbek, A., Topuzoglu, A., Orcin, E., and Janbakhishov, C. E. (2020). Association of prenatal attachment and early childhood emotional, behavioral, and developmental characteristics: A longitudinal study. Infant Ment. Health J. 41, 517–529. doi: 10.1002/imhj.21822
Atashi, V., Kohan, S., Salehi, Z., and Salehi, K. (2018). Maternal-fetal emotional relationship during pregnancy, its related factors and outcomes in Iranian pregnant women: A panel study protocol 11 medical and health sciences 1117 public health and health services 11 medical and health sciences 1114 paediatric. Reprod. Health 15:176. doi: 10.1186/s12978-018-0620-6
Barone, L., Lionetti, F., and Dellagiulia, A. (2014). Maternal-fetal attachment and its correlates in a sample of Italian women: A study using the prenatal attachment inventory. J. Reprod. Infant Psychol. 32, 230–239. doi: 10.1080/02646838.2014.883596
Beck, A. T., Steer, R. A., Ball, R., and Ranieri, W. F. (1996). Comparison of beck depression inventories -IA and -II in psychiatric outpatients. J. Pers. Assess. 67, 588–597. doi: 10.1207/s15327752jpa6703_13
Belsky, J., Conger, R., and Capaldi, D. M. (2009). The intergenerational transmission of parenting: Introduction to the special section. Dev. Psychol. 45, 1201–1204. doi: 10.1037/a0016245
Bowlby, J. (1982). ATTACHMENT AND LOSS: Retrospect and prospect. Am. J. Orthopsychiatry 52, 664–678. doi: 10.1111/j.1939-0025.1982.tb01456.x
Brandon, A. R., Pitts, S., Denton, W. H., Stringer, C. A., and Evans, H. M. (2009). A history of the theory of prenatal attachment. J. Prenat. Perinat. Psychol. Health 23, 201–222.
Branje, S., Geeraerts, S., de Zeeuw, E. L., Oerlemans, A. M., Koopman-Verhoeff, M. E., Schulz, S., et al. (2020). Intergenerational transmission: Theoretical and methodological issues and an introduction to four Dutch cohorts. Dev. Cogn. Neurosci. 45:100835. doi: 10.1016/j.dcn.2020.100835
Busonera, A., Cataudella, S., Lampis, J., Tommasi, M., and Zavattini, G. C. (2016). Psychometric properties of a 20-item version of the maternal-fetal attachment scale in a sample of Italian expectant women. Midwifery 34, 79–87. doi: 10.1016/j.midw.2015.12.012
Canlı, A., and Demirtaş, B. (2022). Prenatal attachment and the relationship with body self-perception. J. Obstet. Gynecol. Neonatal Nurs. 51, e1–e12. doi: 10.1016/j.jogn.2021.09.003
Čėsnaitė, G., Domža, G., Ramašauskaitė, D., Volochovič, J., and Bužinskienė, D. (2019). Factors affecting the maternal-foetal relationship. Acta Med. Litu. 26, 118–124. doi: 10.6001/actamedica.v26i2.4032
Champagne, F. A. (2008). Epigenetic mechanisms and the transgenerational effects of maternal care. Front. Neuroendocrinol. 29, 386–397. doi: 10.1016/j.yfrne.2008.03.003
Ckanley, M. S. (1981). Development of a tool for the measurement of maternal attachment during pregnancy. Nurs. Res. 30, 281–284. doi: 10.1097/00006199-198109000-00008
Copeland, D. B., and Harbaugh, B. L. (2019). “It’s hard being a mama”: Validation of the maternal distress concept in becoming a mother. J. Perinat. Educ. 28, 28–42. doi: 10.1891/1058-1243.28.1.28
Craig, F., Gioia, M. C., Muggeo, V., Cajiao, J., Aloi, A., Martino, I., et al. (2021). Effects of maternal psychological distress and perception of COVID-19 on prenatal attachment in a large sample of Italian pregnant women. J. Affect. Disord. 295, 665–672. doi: 10.1016/j.jad.2021.08.102
Cribari-Neto, F., and Zeileis, A. (2010). Beta regression in R. J. Stat. Softw. 34, 1–24. doi: 10.18637/jss.v034.i02
Crozier, S. R., Robinson, S. M., Borland, S. E., Godfrey, K. M., Cooper, C., and Inskip, H. M. (2009). Do women change their health behaviours in pregnancy? Findings from the Southampton Women’s Survey. Paediatr. Perinat. Epidemiol. 23, 446–453. doi: 10.1111/j.1365-3016.2009.01036.x
da Rosa, K. M., Scholl, C. C., Ferreira, L. A., Trettim, J. P., da Cunha, G. K., Rubin, B. B., et al. (2021). Maternal-fetal attachment and perceived parental bonds of pregnant women. Early Hum. Dev. 154:105310. doi: 10.1016/j.earlhumdev.2021.105310
Daglar, G., and Nur, N. (2018). Level of mother-baby bonding and influencing factors during pregnancy and postpartum period. Psychiatr. Danub. 30, 433–440. doi: 10.24869/psyd.2018.433
Dayton, C. J., Brown, S., Goletz, J., Hicks, L., Barron, C., Sperlich, M., et al. (2019). Pathways to parenting: Predictors of prenatal bonding in a sample of expectant mothers and fathers exposed to contextual risk. J. Child Fam. Stud. 28, 1134–1144. doi: 10.1007/s10826-019-01343-6
de Cock, E. S. A., Henrichs, J., Vreeswijk, C. M. J. M., Maas, A. J. B. M., Rijk, C. H. A. M., and van Bakel, H. J. A. (2016). Continuous feelings of love? The parental bond from pregnancy to toddlerhood. J. Fam. Psychol. 30, 125–134. doi: 10.1037/fam0000138
della Vedova, A. M., Cristini, C., and Bizzi, F. (2019). Prenatal attachment, distress symptoms and psychosocial variables in a sample of Italian first-time parents. Life Span Disabil. 22, 255–285.
Enns, M. W., Cox, B. J., and Clara, I. (2002). Adaptive and maladaptive perfectionism: Developmental origins and association with depression proneness. Pers. Individ. Differ. 33, 921–935. doi: 10.1016/S0191-8869(01)00202-1
Festa, C. C., and Ginsburg, G. S. (2011). Parental and peer predictors of social anxiety in youth. Child Psychiatry Hum. Dev. 42, 291–306. doi: 10.1007/s10578-011-0215-8
Fukui, N., Motegi, T., Watanabe, Y., Hashijiri, K., Tsuboya, R., Ogawa, M., et al. (2021). Perceived parenting before adolescence and parity have direct and indirect effects via depression and anxiety on maternal–infant bonding in the perinatal period. Psychiatry Clin. Neurosci. 75, 312–317. doi: 10.1111/pcn.13289
Göbel, A., Barkmann, C., Arck, P., Hecher, K., Schulte-Markwort, M., Diemert, A., et al. (2019). Couples’ prenatal bonding to the fetus and the association with one’s own and partner’s emotional well-being and adult romantic attachment style. Midwifery 79:102549. doi: 10.1016/j.midw.2019.102549
Handelzalts, J. E., Preis, H., Rosenbaum, M., Gozlan, M., and Benyamini, Y. (2018). Pregnant women’s recollections of early maternal bonding: Associations with maternal–fetal attachment and birth choices. Infant Ment. Health J. 39, 511–521. doi: 10.1002/imhj.21731
Howland, M. A., Sandman, C. A., Davis, E. P., and Glynn, L. M. (2020). Prenatal maternal psychological distress and fetal developmental trajectories: Associations with infant temperament. Dev. Psychopathol. 32, 1685–1695. doi: 10.1017/S095457942000142X
Imai, K., Keele, L., and Tingley, D. (2010). A general approach to causal mediation analysis. Psychol. Methods 15, 309–334. doi: 10.1037/a0020761
Isgut, M., Smith, A. K., Reimann, E. S., Kucuk, O., and Ryan, J. (2017). The impact of psychological distress during pregnancy on the developing fetus: Biological mechanisms and the potential benefits of mindfulness interventions. J. Perinat. Med. 45, 999–1011. doi: 10.1515/jpm-2016-0189
Jamshidimanesh, M., Astaraki, L., Moghadam, Z. B., Taghizadeh, Z., and Haghani, H. (2013). Maternal-fetal attachment and its associated factors. HAYAT 18, 33–45.
Jarnecke, A. M., and South, S. C. (2013). Attachment orientations as mediators in the intergenerational transmission of marital satisfaction. J. Fam. Psychol. 27, 550–559. doi: 10.1037/a0033340
Kidd, K. N., Prasad, D., Cunningham, J. E. A., de Azevedo Cardoso, T., and Frey, B. N. (2022). The relationship between parental bonding and mood, anxiety and related disorders in adulthood: A systematic review and meta-analysis. J. Affect. Disord. 307, 221–236. doi: 10.1016/j.jad.2022.03.069
Kretchmar, M. D., and Jacobvitz, D. B. (2002). Observing mother-child relationships across generations: Boundary patterns, attachment, and the transmission of caregiving. Fam. Process 41, 351–374. doi: 10.1111/j.1545-5300.2002.41306.x
Lau, Y., Htun, T. P., and Kwong, H. K. D. (2018). Sociodemographic, obstetric characteristics, antenatal morbidities, and perinatal depressive symptoms: A three-wave prospective study. PLoS One 13:e0188365. doi: 10.1371/journal.pone.0188365
Lutkiewicz, K., and Bidzan, M. (2022). Maternal adult attachment and maternal-fetal attachment in the context of romantic relationship quality after premature birth-A cross sectional study. Front. Psychiatry 13:935871. doi: 10.3389/fpsyt.2022.935871
Mackinnon, D. P. (2012). Introduction to statistical mediation analysis. New York, NY: Routledge. doi: 10.4324/9780203809556
Maddahi, M. S., Dolatian, M., Khoramabadi, M., and Talebi, A. (2016). Correlation of maternal-fetal attachment and health practices during pregnancy with neonatal outcomes. Electron. Physician 8, 2639–2644. doi: 10.19082/2639
Madden, V., Domoney, J., Aumayer, K., Sethna, V., Iles, J., Hubbard, I., et al. (2015). Intergenerational transmission of parenting: Findings from a UK longitudinal study. Eur. J. Public Health 25, 1030–1035. doi: 10.1093/eurpub/ckv093
Mazzeschi, C., Pazzagli, C., Radi, G., Raspa, V., and Buratta, L. (2015). Antecedents of maternal parenting stress: The role of attachment style, prenatal attachment, and dyadic adjustment in first-time mothers. Front. Psychol. 6:1443. doi: 10.3389/fpsyg.2015.01443
McMahon, C., Barnett, B., Kowalenko, N., and Tennant, C. (2005). Psychological factors associated with persistent postnatal depression: Past and current relationships, defence styles and the mediating role of insecure attachment style. J. Affect. Disord. 84, 15–24. doi: 10.1016/j.jad.2004.05.005
McNamara, J., Townsend, M. L., and Herbert, J. S. (2019). A systemic review of maternal wellbeing and its relationship with maternal fetal attachment and early postpartum bonding. PLoS One 14:e0220032. doi: 10.1371/journal.pone.0220032
Montirosso, R., Provenzi, L., and Mascheroni, E. (2020). “The role of protective caregiving in epigenetic regulation in human infants,” in Developmental human behavioral epigenetics: Principles, methods, evidence, and future directions, ed. T. Tollefsbol (London: Elsevier). doi: 10.1016/B978-0-12-819262-7.00008-8
Napoli, A., Lamis, D. A., Berardelli, I., Canzonetta, V., Sarubbi, S., Rogante, E., et al. (2020). Anxiety, prenatal attachment, and depressive symptoms in women with diabetes in pregnancy. Int. J. Environ. Res. Public Health 17:425. doi: 10.3390/ijerph17020425
Ossa, X., Bustos, L., and Fernandez, L. (2012). Prenatal attachment and associated factors during the third trimester of pregnancy in Temuco, Chile. Midwifery 28, e689–e696. doi: 10.1016/j.midw.2011.08.015
Parker, G. (1990). The parental bonding instrument. A decade of research. Soc. Psychiatry Psychiatr. Epidemiol. 25, 281–282. doi: 10.1007/bf00782881
Reed, O. (2014). The effect of maternal factors on prenatal attachment. Undergraduate honors thesis. Redlands, CA: University of Redlands.
Røhder, K., Væver, M. S., Aarestrup, A. K., Jacobsen, R. K., Smith-Nielsen, J., and Schiøtz, M. L. (2020). Maternal-fetal bonding among pregnant women at psychosocial risk: The roles of adult attachment style, prenatal parental reflective functioning, and depressive symptoms. PLoS One 15:e0239208. doi: 10.1371/journal.pone.0239208
Rollè, L., Giordano, M., Santoniccolo, F., and Trombetta, T. (2020). Prenatal attachment and perinatal depression: A systematic review. Int. J. Environ. Res. Public Health 17:2644. doi: 10.3390/ijerph17082644
Rossen, L., Hutchinson, D., Wilson, J., Burns, L., Olsson, C., Allsop, S., et al. (2016). Predictors of postnatal mother-infant bonding: The role of antenatal bonding, maternal substance use and mental health. Arch. Womens Ment. Health 19, 609–622. doi: 10.1007/s00737-016-0602-z
Sacchi, C., Miscioscia, M., Visentin, S., and Simonelli, A. (2021). Maternal–fetal attachment in pregnant Italian women: Multidimensional influences and the association with maternal caregiving in the infant’s first year of life. BMC Pregnancy Childbirth 21:488. doi: 10.1186/s12884-021-03964-6
Salehi, K., Taleghani, F., and Kohan, S. (2019). Effect of attachment-based interventions on prenatal attachment: A protocol for systematic review. Reprod. Health 16:42. doi: 10.1186/s12978-019-0704-y
Sameshima, H., Shimura, A., Ono, K., Masuya, J., Ichiki, M., Nakajima, S., et al. (2021). Corrigendum: Combined effects of parenting in childhood and resilience on work stress in nonclinical adult workers from the community. Front. Psychiatry 12:742812. doi: 10.3389/fpsyt.2021.742812
Shahhosseini, Z., Pourasghar, M., Khalilian, A., and Salehi, F. (2015). A review of the effects of anxiety during pregnancy on children’s health. Mater. Soc. Med. 27, 200–202. doi: 10.5455/msm.2015.27.200-202
Smorti, M., Ponti, L., Ghinassi, S., and Rapisardi, G. (2020). The mother-child attachment bond before and after birth: The role of maternal perception of traumatic childbirth. Early Hum. Dev. 142:104956. doi: 10.1016/j.earlhumdev.2020.104956
Spielberger, C. D., and Sydeman, S. J. (1994). “State-trait anxiety inventory and state-trait anger expression inventory,” in The use of psychological testing for treatment planning and outcome assessment, ed. M. E. Maruish (Hillsdale, MI: Lawrence Erlbaum Associates, Inc).
Su, Q., Zhang, H., Zhang, Y., Zhang, H., Ding, D., Zeng, J., et al. (2015). Maternal stress in gestation: Birth outcomes and stress-related hormone response of the neonates. Pediatr. Neonatol. 56, 376–381. doi: 10.1016/j.pedneo.2015.02.002
Taccini, F., Rossi, A. A., and Mannarini, S. (2021). Intergenerational transmission of relational styles: Current considerations. Front. Psychol. 12:672961. doi: 10.3389/fpsyg.2021.672961
Tambelli, R., Odorisio, F., and Lucarelli, L. (2014). Prenatal and postnatal maternal representations in nonrisk and at-risk parenting: Exploring the influences on mother-infant feeding interactions. Infant Ment. Health J. 35, 376–388. doi: 10.1002/imhj.21448
Tian, L., Liu, L., and Shan, N. (2018). Parent-child relationships and resilience among Chinese adolescents: The mediating role of self-esteem. Front. Psychol. 9:1030. doi: 10.3389/fpsyg.2018.01030
Tokuda, N., Kobayashi, Y., Tanaka, H., Sawai, H., Shibahara, H., Takeshima, Y., et al. (2021). Feelings about pregnancy and mother-infant bonding as predictors of persistent psychological distress in the perinatal period: The Japan environment and children’s study. J. Psychiatr. Res. 140, 132–140. doi: 10.1016/j.jpsychires.2021.05.056
Ulu, P. G., and Bayraktar, S. (2018). Investigation of variables related to prenatal bonding levels in pregnant women. Yeni Symp. 56, 2–8. doi: 10.5455/NYS.20180629015333
Van Bussel, J. C. H., Spitz, B., and Demyttenaere, K. (2010). Reliability and validity of the Dutch version of the maternal antenatal attachment scale. Arch. Womens Ment. Health 13, 267–277. doi: 10.1007/s00737-009-0127-9
Van Ijzendoorn, M. H. (1992). Intergenerational transmission of parenting: A review of studies in nonclinical populations. Dev. Rev. 12, 76–99. doi: 10.1016/0273-2297(92)90004-L
Walsh, J. (2010). Definitions matter: If maternal-fetal relationships are not attachment, what are they? Arch. Womens Ment. Health 13, 449–451. doi: 10.1007/s00737-010-0152-8
Keywords: prenatal attachment, maternal-fetal attachment, parental bonding, maternal care, paternal care
Citation: Gioia MC, Cerasa A, Muggeo VMR, Tonin P, Cajiao J, Aloi A, Martino I, Tenuta F, Costabile A and Craig F (2023) The relationship between maternal-fetus attachment and perceived parental bonds in pregnant women: Considering a possible mediating role of psychological distress. Front. Psychol. 13:1095030. doi: 10.3389/fpsyg.2022.1095030
Received: 10 November 2022; Accepted: 19 December 2022;
Published: 16 January 2023.
Edited by:
Jens Henrichs, VU Medical Center, NetherlandsReviewed by:
Julian David Gardiner, University of Oxford, United KingdomCopyright © 2023 Gioia, Cerasa, Muggeo, Tonin, Cajiao, Aloi, Martino, Tenuta, Costabile and Craig. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Antonio Cerasa,  YW50b25pby5jZXJhc2FAaXJpYi5jbnIuaXQ=
YW50b25pby5jZXJhc2FAaXJpYi5jbnIuaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.