
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
MINI REVIEW article
Front. Psychol. , 18 January 2023
Sec. Psychology for Clinical Settings
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.1070975
This article is part of the Research Topic Towards a Complex Approach to Psychotherapy, Psychopathology and Learning Processes: Process Analysis and Evaluation of the Clinical Efficacy of Therapeutic and Pedagogical Paths View all 6 articles
Exposure therapy (ET), which follows the Pavlovian extinction model, is regarded as the gold-standard treatment for social anxiety disorder (SAD). The prospect of virtual reality in lieu of a traditional laboratory setting for the treatment of SAD has not been rigorously explored. The aim of the review was to summarize, find gaps in the current literature, and formulate future research direction by identifying two broad research questions: the comparative efficacy between in vivo ET and virtual reality exposure therapy (VRET) and the effectiveness of the Pavlovian extinction model in treating SAD. The criteria for effectiveness were effect size, relapse prevention, attrition rate and ecological validity. A literature search on recent randomized controlled trials yielded a total of 6 original studies (N=358), excluding duplication and overlapping participants. All studies supported that VRET was as effective as in vivo ET. Behavioral therapy that follows classical conditioning principles has a high attrition and relapse rate. Comparisons were drawn between the efficacy of the Pavlovian extinction model and other existing models, including third-wave approaches. The neural markers are suggested to be included as efficacy measures in treating SAD. The gold-standard treatment for SAD requires a paradigm shift through rigorous longitudinal comparative studies.
Social anxiety disorder (SAD), a clinically diagnosed condition that leads to impairments in interpersonal settings due to fear of being judged (McKay and McKiernan, 2018), is the world’s sixth leading cause of disability (Baxter et al., 2014). The fear response is essential for survival, as it enables us to predict danger on cued signals and adapt to external environments (Krause and Domjan, 2017). However, the neural threat circuitry that enables us to regulate our emotions and behavior in changing environments is disrupted in a person with SAD (Kredlow et al., 2022). The development of social anxiety disorders could be explained by classical conditioning theory, attributed to Pavlov (Lilienfeld et al., 2019). Classical conditioning is an involuntary learning process of an association between two or more stimuli (Pavlov, 1897). A repetitive pairing of a neutral stimulus (e.g., people) with a biological stimulus (e.g., scream) elicits a conditioned response (e.g., avoidance) that was initially a reflex response to the biological stimulus (UCS) but is now displayed when the neutral stimulus presents alone (Pavlov, 1897). The benchmark treatments for SAD include exposure therapy (Steinman et al., 2016) and drug intervention (Klinger et al., 2005). Exposure therapy is an alternative to pharmacological interventions that produce undesirable side effects (Hindmarch, 2009). Exposure therapy (ET) follows the extinction principle (Pavlov, 1927) of classical conditioning, which repeatedly exposes the patients to the feared stimulus (CS) without the presence of UCS in a lab setting until the association between the UCS and CS is weakened, and the anxiety subsides (Hofmann, 2008). The digital revolution has brought about a change of modality from laboratory-based therapy to virtual reality exposure therapy (Bucci et al., 2019). Virtual reality is a 3D and 360-degree simulation of environments in which one can immerse and interact.
Can virtual reality treat social anxiety disorder using the principles of classical conditioning? The aim of this mini-review was to summarize, find gaps in the current literature, and formulate future research direction by identifying two broad research questions as follows:
• Is virtual reality exposure therapy (VRET) as effective as in vivo ET?
• Is ET based on the Pavlovian extinction model as effective as other ET or other therapy that use different principles or procedures in treating SAD?
The criteria of effectiveness were effect size, relapse prevention, attrition rate and ecological validity. A broader meta-analyses search was made in the scoping review to find the answer to the first research question (see Figure 1). Nine meta-analyses (Parsons and Rizzo, 2008; Opriş et al., 2012; Chesham et al., 2018; Carl et al., 2019; Wechsler et al., 2019; Horigome et al., 2020; Freitas et al., 2021; Morina et al., 2021; Lim et al., 2022), which included randomized control trials, provided effect sizes between the comparison groups, were published in the last decade and the English language were selected for the review. The meta-analyses covered substantially overlapping studies. Any duplication or studies with less than 10 participants in the experimental (i.e., SAD) group were excluded from this review. A total of 6 studies (N = 358) fitted the eligibility criteria. Table 1 represents all randomized controlled comparative studies on SAD, which were included in the seven meta-analyses. The control groups (nC = 108) and participants in the VRET (nVRET = 121) and in vivo ET (nIVET = 129) studies in Table 1 were unique individuals. Overlapping participants, including follow-up studies, were excluded to avoid depicting a larger sample in a misleading way. For example, Safir et al. (2012) conducted a study with the same set of participants that initially participated in Wallach et al.’s (2009) study; hence, they were not duplicated in the table; and Anderson et al.’s (2017) follow-up study comprising the same group of original participants in a past study (Anderson et al., 2013) was excluded from the table. Two studies (Wallach et al., 2009; Anderson et al., 2013) listed in the table focused on fear of public speaking, which is a subset of SAD.
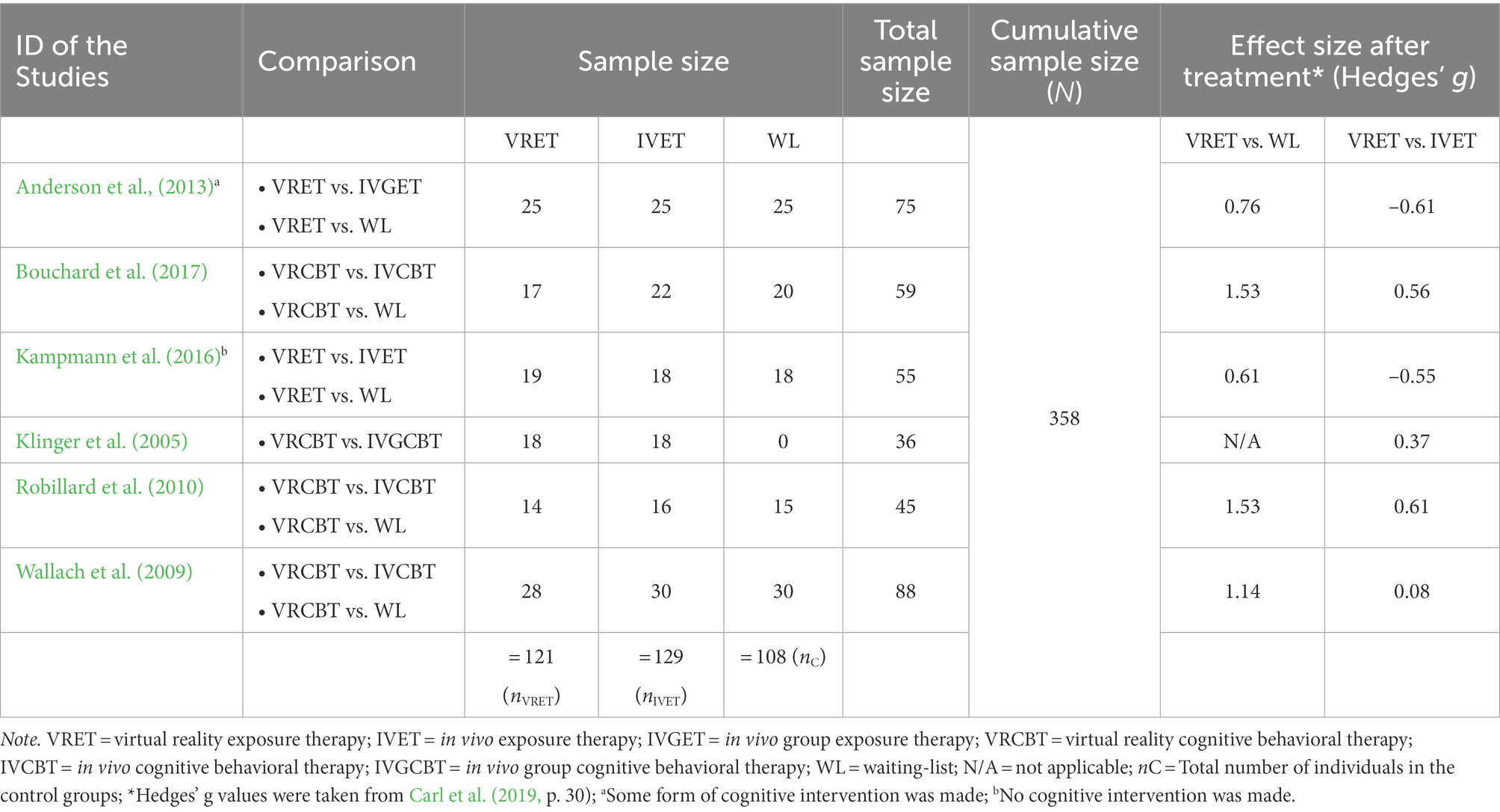
Table 1. Virtual reality exposure therapy (VRET) for the treatment of social anxiety disorder (SAD): randomized controlled comparative studies.
All studies, except for Kampmann et al.’s (2016) study (to be discussed later in this review), in Table 1 unequivocally suggest that the efficacy of VRET in treating SAD is clinically significant (i.e., Hedges’ g = 0.80–1.53) compared to control groups. Furthermore, none of them shows evidence that the effectiveness of VRET is inferior to in vivo ET. To date, only one longitudinal study has been done on the comparative efficacy between VRET and in vivo ET (Anderson et al., 2017). The 6-year longitudinal study (N = 28) that Anderson et al. (2017) investigated showed no difference between VRET and in vivo ET. The effect size that compared the self-rating scores between the two groups of participants, using the ‘fear of native evaluation’ (FNE) scale, was clinically non-significant (i.e., hedges’ g = −0.15). This finding favors VRET over in vivo ET from an ecological standpoint. Extinction trials in ET are required to be conducted in multiple contexts and settings to prevent a relapse of SAD (Vervliet et al., 2013). The delivery of in vivo ET in different settings and contexts is expensive. VRET serves as an ecologically valid option for treating SAD.
Questions may arise about the intensity and frequency of VRET sessions being appropriate for patients with SAD. All VRET studies included in this literature review tailored the virtual environments according to the pace and fear hierarchy of each participant during the VR therapy sessions in the presence of professional therapists (Klinger et al., 2005; Wallach et al., 2009; Robillard et al., 2010; Anderson et al., 2013; Kampmann et al., 2016; Bouchard et al., 2017). The therapists could see the participant’s field of view in real-time and simultaneously observe his or her responses (Kampmann et al., 2016). All VRET sessions were conducted in lab settings to avoid confounding variables, as the in-vivo ET studies took place in lab settings (Klinger et al., 2005; Wallach et al., 2009; Robillard et al., 2010; Anderson et al., 2013; Kampmann et al., 2016; Bouchard et al., 2017). However, VRET sessions can also be conducted in the comfort of one’s home (Hartanto et al., 2015; Emmelkamp et al., 2020; Miloff et al., 2020; Stefaniak et al., 2022). Home-based, self-guided VRET yields an additional advantage over in-vivo ET in that some patients with severe SAD may find direct interaction with the therapist intimidating (Hartanto et al., 2015). Systematic studies are required, however, to investigate the transferability of skills acquired during home-based VRET sessions to real-life scenarios. One study found that the closer the VR environment mimicked the real-life environment in terms of the cultural setting and grooming of VR characters, the more effective the therapy was (Wallach et al., 2009).
The dropout rate is another critical indicator of the efficacy of a treatment. Two studies show that the attrition rate from in vivo ET was more than twice as much as that from the VRET (Safir et al., 2012; Anderson et al., 2013), suggesting VRET’s efficacy over in vivo ET for the treatment of SAD. Nonetheless, a 9–35% attrition rate (Bentley et al., 2021) calls the effectiveness of ET that employs the Pavlovian extinction model into question. Additionally, classical conditioning fails to prevent relapse in SAD patients (Pavlov, 1897; Pittig et al., 2018; Levy et al., 2022).
Relapse prevention is a predictive marker of efficacy. A recent study shows that 21.8% of SAD patients relapse after achieving successful extinction through Pavlovian ET (Scholten et al., 2021). There is a knowledge gap on the efficacy of classical conditioning in relapse prevention due to a dearth of longitudinal studies. One 3-month follow-up study (Mattick et al., 1989) revealed the superiority of cognitive restructuring over the sole Pavlovian extinction model. Likewise, Ougrin’s (2011) meta-analysis showed that the superiority of cognitive intervention strategies over the Pavlovian extinction model was statistically significant at follow-up (6–12 months). The findings are consistent with the findings of Kampmann et al.’s (2016) study (see Table 1) that exclusively administered behavioral therapy and excluded cognitive counterparts from exposure therapy.
In contrast to all VRET studies listed in Table 1, Kampmann et al. (2016) attempted to investigate the sole effects of the Pavlovian extinction model in treating SAD. Compared to the control group, the effect size was not clinically significant (see Table 1). The findings underscore the possible inadequacy of the Pavlovian extinction model in treating SAD. Do other therapies that are not rooted in Pavlovian classical conditioning fare better in relapse prevention in SAD patients?
Acceptance and commitment therapy (ACT) uses the principles of operant conditioning and attempts to shift the focus of SAD patients to holistic well-being from the feared stimulus (Toghiani et al., 2019). Further investigations are needed to compare extinction strategies rooted in operant conditioning with the Pavlovian classical conditioning model. ET strategies that tweaked or deviated from the Pavlovian principles of classical conditioning during the process of extinction show more effectiveness in relapse prevention (Craske et al., 2018). Three studies demonstrated that occasional exposure to UCS, either paired or unpaired with CS during extinction trials, helps prevent relapse compared to Pavlovian classical conditioning (Bouton, 2004; Thompson et al., 2018; Lipp et al., 2021). Craske et al. (2014, p. 11) suggested that during “extinction trials,” a new “inhibitory” learning takes place instead of an unlearning of the previous association. This is supported by Shin and Liberzon’s (2010) study on neurocircuitry during fear conditioning and extinction. The recent advancement in neuroscience has made it possible to pinpoint neural markers of SAD.
Several studies reveal that the difference between the brain activity of the prefrontal cortex of SAD and control groups at baseline is statistically significant (Pittig et al., 2018; Lee et al., 2021; Kredlow et al., 2022). There is a dearth of research pertaining to comparative studies on self-reported scores and neural correlates during VRET in treating SAD. A recent VRET study showed that self-rating scores were consistent with neural correlates in SAD (Lee et al., 2021).
To conclude, recent studies provide strong evidence that VRET is as effective as in vivo ET in treating SAD. VRET has higher ecological validity than in vivo ET. Self-guided VRET in a home setting requires rigorous future investigations on the feasibility of data-driven mechanisms through remote or automated monitoring that ensure optimal intervention and prevent burnout. The future research direction of VRET studies in treating SAD should be geared toward investigating the relationship between the cultural paradigm of the VR environment and the extent of generalization of skills from virtual to real-life environments, and the relevance of designing culturally sensitive VR software. SAD treatment strategies based on classical conditioning have high attrition and relapse rate. There is a gap in the literature estimating the efficacy of therapies based on attrition rate and relapse prevention. Future research should be geared toward comparative longitudinal, relapse-prevention studies between Pavlovian exposure therapy, cognitive therapy, and third-wave approaches, such as therapy based on operant conditioning, and include both self-rating scales and neural markers as efficacy measures in treating SAD.
NC conceived the idea, designed the review protocol, conducted the literature search and drafted the article. AK revised the article and organized the funding. All authors approved the submitted version.
This work was supported by three grants [8474000221; KKJRC- 2019-Health2 (Khandoker), CIRA 2021-051 (8474000408), and HEIC 8474000132] from Khalifa University Abu Dhabi, UAE.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The reviewer MA declared a past co-authorship with the author AK to the handling editor.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Anderson, P. L., Edwards, S. M., and Goodnight, J. R. (2017). Virtual reality and exposure group therapy for social anxiety disorder: results from a 4–6-year follow-up. Cogn. Ther. Res. 41, 230–236. doi: 10.1007/s10608-016-9820-y
Anderson, P. L., Price, M., Edwards, S. M., Obasaju, M. A., Schmertz, S. K., Zimand, E., et al. (2013). Virtual reality exposure therapy for social anxiety disorder: a randomized controlled trial. J. Consult. Clin. Psychol. 81, 751–760. doi: 10.1037/a0033559
Baxter, A. J., Vos, T., Scott, K. M., Ferrari, A. J., and Whiteford, H. A. (2014). The global burden of anxiety disorders in 2010. Psychol. Med. 44, 2363–2374. doi: 10.1017/S0033291713003243
Bentley, K. H., Cohen, Z. D., Kim, T., Bullis, J. R., Nauphal, M., Cassiello-Robbins, C., et al. (2021). The nature, timing, and symptom trajectories of dropout from transdiagnostic and single-diagnosis cognitive-behavioral therapy for anxiety disorders. Behav. Ther. 52, 1364–1376. doi: 10.1016/j.beth.2021.03.007
Bouchard, S., Dumoulin, S., Robillard, G., Guitard, T., Klinger, E., Forget, H., et al. (2017). Virtual reality compared with in vivo exposure in the treatment of social anxiety disorder: a three-arm randomised controlled trial. Br. J. Psychiatry 210, 276–283. doi: 10.1192/bjp.bp.116.184234
Bouton, M. E. (2004). Context and behavioral processes in extinction. Learn. Mem. 11, 485–494. doi: 10.1101/lm.78804
Bucci, S., Schwannauer, M., and Berry, N. (2019). The digital revolution and its impact on mental health care. Psychol. Psychother. Theory Res. Pract. 92, 277–297. doi: 10.1111/papt.12222
Carl, E., Stein, A. T., Levihn-Coon, A., Pogue, J. R., Rothbaum, B., Emmelkamp, P., et al. (2019). Virtual reality exposure therapy for anxiety and related disorders: a meta-analysis of randomized controlled trials. J. Anxiety Disord. 61, 27–36. doi: 10.1016/j.janxdis.2018.08.003
Chesham, R. K., Malouff, J. M., and Schutte, N. S. (2018). Meta-analysis of the efficacy of virtual reality exposure therapy for social anxiety. Behav. Chang. 35, 152–166. doi: 10.1017/bec.2018.15
Craske, M. G., Hermans, D., and Vervliet, B. (2018). State-of-the-art and future directions for extinction as a translational model for fear and anxiety. Phil. Trans. R. Soc. B Biol. Sci. 373:20170025. doi: 10.1098/rstb.2017.0025
Craske, M. G., Treanor, M., Conway, C. C., Zbozinek, T., and Vervliet, B. (2014). Maximizing exposure therapy: an inhibitory learning approach. Behav. Res. Ther. 58, 10–23. doi: 10.1016/j.brat.2014.04.006
Emmelkamp, P. M., Meyerbröker, K., and Morina, N. (2020). Virtual reality therapy in social anxiety disorder. Curr. Psychiatry Rep. 22, 1–9. doi: 10.1007/s11920-020-01156-1
Freitas, J. R. S., Velosa, V. H. S., Abreu, L. T. N., Jardim, R. L., Santos, J. A. V., Peres, B., et al. (2021). Virtual reality exposure treatment in phobias: a systematic review. Psychiatry Q. 92, 1685–1710. doi: 10.1007/s11126-021-09935-6
Hartanto, D., Brinkman, W. P., Kampmann, I. L., Morina, N., Emmelkamp, P. G., and Neerincx, M. A. (2015). “Design and implementation of home-based virtual reality exposure therapy system with a virtual ecoach.” in International Conference on Intelligent Virtual Agents. Springer, Cham, 287–291.
Hindmarch, I. (2009). Cognitive toxicity of pharmacotherapeutic agents used in social anxiety disorder. Int. J. Clin. Pract. 63, 1085–1094. doi: 10.1111/j.1742-1241.2009.02085.x
Hofmann, S. G. (2008). Cognitive processes during fear acquisition and extinction in animals and humans: implications for exposure therapy of anxiety disorders. Clin. Psychol. Rev. 28, 199–210. doi: 10.1016/j.cpr.2007.04.009
Horigome, T., Kurokawa, S., Sawada, K., Kudo, S., Shiga, K., Mimura, M., et al. (2020). Virtual reality exposure therapy for social anxiety disorder: a systematic review and meta-analysis. Psychol. Med. 50, 2487–2497. doi: 10.1017/S0033291720003785
Kampmann, I. L., Emmelkamp, P. M., Hartanto, D., Brinkman, W. P., Zijlstra, B. J., and Morina, N. (2016). Exposure to virtual social interactions in the treatment of social anxiety disorder: a randomized controlled trial. Behav. Res. Ther. 77, 147–156. doi: 10.1016/j.brat.2015.12.016
Klinger, E., Bouchard, S., Légeron, P., Roy, S., Lauer, F., Chemin, I., et al. (2005). Virtual reality therapy versus cognitive behavior therapy for social phobia: a preliminary controlled study. Cyberpsychol. Behav. 8, 76–88. doi: 10.1089/cpb.2005.8.76
Krause, M. A., and Domjan, M. (2017). “Ethological and evolutionary perspectives on Pavlovian conditioning,” in APA Handbook of Comparative Psychology: Perception, Learning, and Cognition. eds. J. Call, G. M. Burghardt, I. M. Pepperberg, C. T. Snowdon, and T. Zentall (Washington, DC: American Psychological Association), 247–266.
Kredlow, A. M., Fenster, R. J., Laurent, E. S., Ressler, K. J., and Phelps, E. A. (2022). Prefrontal cortex, amygdala, and threat processing: implications for PTSD. Neuropsychopharmacology 47, 247–259. doi: 10.1038/s41386-021-01155-7
Lee, H., Choi, J., Jung, D., Hur, J. W., and Cho, C. H. (2021). The effects of virtual reality treatment on prefrontal cortex activity in patients with social anxiety disorder: participatory and interactive virtual reality treatment study. J. Med. Internet Res. 23:e31844. doi: 10.2196/31844
Levy, H. C., Stevens, K. T., and Tolin, D. F. (2022). Research review: a meta-analysis of relapse rates in cognitive behavioral therapy for anxiety and related disorders in youth. J. Child Psychol. Psychiatry 63, 252–260. doi: 10.1111/jcpp.13486
Lilienfeld, S., Lynn, S. J., Namy, L., Woolf, N., Jamieson, G., Marks, A., et al. (2019). Psychology: From inquiry to understanding. Pearson Higher Education Australia.
Lim, M. H., Aryadoust, V., and Esposito, G. (2022). A meta-analysis of the effect of virtual reality on reducing public speaking anxiety. Curr. Psychol. 1–17. doi: 10.1007/s12144-021-02684-6
Lipp, O. V., Ryan, K. M., Luck, C. C., Craske, M. G., and Waters, A. M. (2021). Presentation of unpaired unconditional stimuli during extinction reduces renewal of conditional fear and slows re-acquisition. Psychophysiology 58:e13899. doi: 10.1111/psyp.13899
Mattick, R. P., Peters, L., and Clarke, J. C. (1989). Exposure and cognitive restructuring for social phobia: a controlled study. Behav. Ther. 20, 3–23. doi: 10.1016/S0005-7894(89)80115-7
McKay, D., and McKiernan, K. (2018). Social anxiety disorder. Encyclopedia Britannica. Available at: https://www.britannica.com/science/social-anxiety-disorder (Accessed December 10, 2022).
Miloff, A., Carlbring, P., Hamilton, W., Andersson, G., Reuterskiöld, L., and Lindner, P. (2020). Measuring Alliance toward embodied virtual therapists in the era of automated treatments with the virtual therapist Alliance scale (VTAS): development and psychometric evaluation. J. Med. Internet Res. 22:e16660. doi: 10.2196/16660
Morina, N., Kampmann, I., Emmelkamp, P., Barbui, C., and Hoppen, T. H. (2021). Meta-analysis of virtual reality exposure therapy for social anxiety disorder. Psychol. Med. 50, 1–3. doi: 10.1017/S0033291721001690
Opriş, D., Pintea, S., García-Palacios, A., Botella, C., Szamosközi, Ş., and David, D. (2012). Virtual reality exposure therapy in anxiety disorders: a quantitative meta-analysis. Depress. Anxiety 29, 85–93. doi: 10.1002/da.20910
Ougrin, D. (2011). Efficacy of exposure versus cognitive therapy in anxiety disorders: systematic review and meta-analysis. BMC Psychiatry 11, 1–13. doi: 10.1186/1471-244X-11-200
Parsons, T. D., and Rizzo, A. A. (2008). Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J. Behav. Ther. Exp. Psychiatry 39, 250–261. doi: 10.1016/j.jbtep.2007.07.007
Pavlov, I. P. (1927). Section on “Extinction of conditioned reflexes,” in Conditioned Reflexes: An Investigation of the Physiological Activity of the Cerebral Cortex. Oxford: Oxford University Press.
Pittig, A., Treanor, M., LeBeau, R. T., and Craske, M. G. (2018). The role of associative fear and avoidance learning in anxiety disorders: gaps and directions for future research. Neurosci. Biobehav. Rev. 88, 117–140. doi: 10.1016/j.neubiorev.2018.03.015
Robillard, G., Bouchard, S., Dumoulin, S., Guitard, T., and Klinger, E. (2010). Using virtual humans to alleviate social anxiety: preliminary report from a comparative outcome study. Stud. Health Technol. Inform. 154, 57–60. doi: 10.3233/978-1-60750-561-7-57
Safir, M. P., Wallach, H. S., and Bar-Zvi, M. (2012). Virtual reality cognitive-behavior therapy for public speaking anxiety: one-year follow-up. Behav. Modif. 36, 235–246. doi: 10.1177/0145445511429999
Scholten, W., Ten Have, M., van Geel, C., van Balkom, A., de Graaf, R., and Batelaan, N. (2021). Recurrence of anxiety disorders and its predictors in the general population. Psychol. Med. 1–9. doi: 10.1017/S0033291721002877
Shin, L. M., and Liberzon, I. (2010). The neurocircuitry of fear, stress, and anxiety disorders. Neuropsychopharmacology 35, 169–191. doi: 10.1038/npp.2009.83
Stefaniak, I., Hanusz, K., Mierzejewski, P., Bieńkowski, P., Parnowski, T., and Murawiec, S. (2022). Preliminary study of efficacy and safety of self-administered virtual exposure therapy for social anxiety disorder vs cognitive-behavioral therapy. Brain Sci. 12:1236. doi: 10.3390/brainsci12091236
Steinman, S. A., Wootton, B. M., and Tolin, D. F. (2016). “Exposure therapy for anxiety disorders,” in Encyclopedia of Mental Health. ed. H. S. Friedman (Academic Press), 186–191. doi: 10.1016/b978-0-12-397045-9.00266-4
Thompson, A., McEvoy, P. M., and Lipp, O. V. (2018). Enhancing extinction learning: occasional presentations of the unconditioned stimulus during extinction eliminate spontaneous recovery, but not necessarily reacquisition of fear. Behav. Res. Ther. 108, 29–39. doi: 10.1016/j.brat.2018.07.001
Toghiani, Z., Ghasemi, F., and Samouei, R. (2019). The effectiveness of acceptance and commitment group therapy on social anxiety in female dormitory residents in Isfahan university of medical sciences. J. Educ. Health Promot. 8. doi: 10.4103/jehp.jehp_111_18
Vervliet, B., Craske, M. G., and Hermans, D. (2013). Fear extinction and relapse: state of the art. Annu. Rev. Clin. Psychol. 9, 215–248. doi: 10.1146/annurev-clinpsy-050212-185542
Wallach, H. S., Safir, M. P., and Bar-Zvi, M. (2009). Virtual reality cognitive behavior therapy for public speaking anxiety. Behav. Modif. 33, 314–338. doi: 10.1177/0145445509331926
Wechsler, T. F., Kümpers, F., and Mühlberger, A. (2019). Inferiority or even superiority of virtual reality exposure therapy in phobias?—a systematic review and quantitative meta-analysis on randomized controlled trials specifically comparing the efficacy of virtual reality exposure to gold standard in vivo exposure in agoraphobia, specific phobia, and social phobia. Front. Psychol. 1758. doi: 10.3389/fpsyg.2019.01758
Keywords: social anxiety disorder, classical conditioning, randomized controlled trial, virtual reality, cognitive behavioral therapy, third-wave CBT, operant conditioning, gold-standard treatment
Citation: Chowdhury N and Khandoker AH (2023) The gold-standard treatment for social anxiety disorder: A roadmap for the future. Front. Psychol. 13:1070975. doi: 10.3389/fpsyg.2022.1070975
Received: 15 October 2022; Accepted: 30 November 2022;
Published: 18 January 2023.
Edited by:
Raffaele Sperandeo, University of Basilicata, ItalyReviewed by:
Mohanad Alkhodari, University of Oxford, United KingdomCopyright © 2023 Chowdhury and Khandoker. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nayeefa Chowdhury, ✉ bmF5ZWVmYWNob3dkaHVyeUBnbWFpbC5jb20=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.