- School of Nursing, Hong Kong Polytechnic University, Hong Kong, Hong Kong SAR, China
Background: Spiritual well-being is a strength for childhood cancer patients to cope with cancer. The availability of a valid and reliable instrument for assessing spiritual well-being is crucial. This study translated and adapted the Functional Assessment of Chronic Illness Therapy Spiritual Well-being scale (FACIT-Sp) for Chinese childhood cancer patients and examined the psychometric properties and factor structure in this population.
Methods: This was a methodological study. The FACIT-Sp was translated into Chinese. Adaptation was based on our qualitative study. For psychometric evaluation, a convenience sample of 412 were recruited based on the suggested sample size for the exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). Childhood cancer patients were included if they aged 8–17 years, with parental consent to participate, able to communicate that they were being treated for cancer, and able to communicate and read Chinese. Participants answered the Chinese version of the adapted FACIT-Sp, the Center for Epidemiology Studies Depression Scale for Children (CES-DC), and the Pediatric Quality of Life Inventory 3.0 Cancer Module (PedsQL). Content validity, convergent validity, internal consistency and test–retest reliability were examined. Both EFA and CFA assessed the structural validity of the adapted FACIT-Sp.
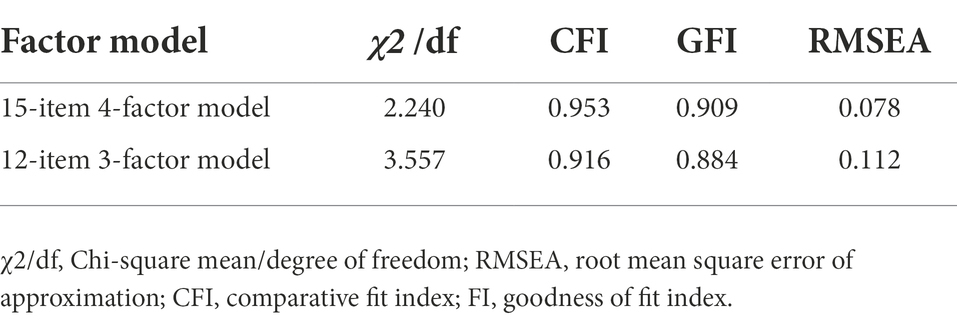
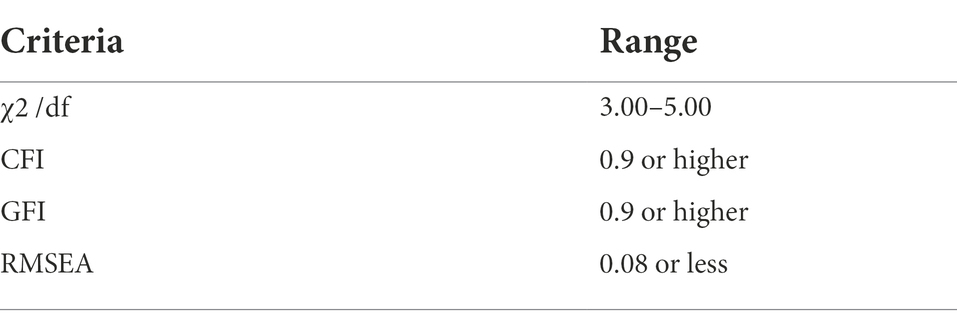
Results: The content validity index values for items ranged 0.8–1.0 and that for the scale was 0.84, indicating appropriate content validity. The scale had good internal consistency, with a Cronbach’s alpha of 0.815. The FACIT-Sp scores positively correlated with the CES-DC scores, and negatively correlated with PedsQL scores, suggesting that the Chinese version of the adapted FACIT-Sp had reasonable convergent validity. EFA yielded a four-factor (meaning, peace, faith, and connection with others) model. The CFA results revealed that the four-factor model achieved a better fit than the original three-factor model (Chi-Square Mean/Degree of Freedom = 2.240 vs. 3.557, Comparative Fit Index = 0.953 vs. 0.916, Goodness of Fit Index = 0.909 vs. 0.884, Root Mean Square Error of Approximation = 0.078 vs. 0.112).
Conclusion: The Chinese version of the adapted FACIT-Sp is a reliable and valid instrument for assessing spiritual well-being among Chinese childhood cancer patients. This instrument can be applied in clinical settings for routine assessment.
Introduction
Cancer is regarded to be a major killer for children worldwide (Steliarova-Foucher et al., 2017). It has been reported that the incidence and mortality rate of childhood cancer in China were 87.1 and 36.3 per million, respectively, after adjusting for age (Zheng et al., 2015). Despite new and advanced treatment options that have improved survival rates, childhood cancer is still regarded as a life-threatening and stressful event (Comas Carbonell et al., 2021). In addition to the physical suffering associated with cancer, the heightened sense of loss and threat of death cause childhood cancer patients to reflect and find meaning in relation to their diagnosis and its impact on their lives (Holge-Hazelton et al., 2016). This ongoing process of reflection and searching throughout the disease trajectory leads to unique spiritual needs among children, which are defined as the needs and expectations of an individual searching for meaning, purpose, and value in their life, and connection with the self, others, the significant, or scared (Murray et al., 2004). Unmet spiritual needs and impaired health status may place childhood cancer patients at increased risk of low spiritual well-being compared with children with other clinical conditions (Taylor et al., 2015).
Spiritual well-being is a fundamental component for the overall quality of life (QoL) of childhood cancer patients (Taylor et al., 2015; Torabi et al., 2018). Spiritual well-being is considered the “fourth domain of well-being,” equally important as physical, mental and social domains (Dhar et al., 2013). It refers to a state of being where an individual is able to handle daily life issues in a way that leads to personal realization of one’s full potential, meaning and purpose of life and fulfilment from within (Aging, 1975). Spiritual well-being is regarded as a source of strength for childhood cancer patients by providing meaning and purpose, and fostering strong relationships with others and with the divine, hence heightening patients’ resistance to the suffering caused by disease (Hendricks-Ferguson, 2008; Foster et al., 2012). Mounting evidence has shown that high spiritual well-being can act as a buffer against depressive symptoms and anxiety in patients with cancer (Chaar et al., 2018; Davis et al., 2018), including those who are adolescent and young adults (Grossoehme et al., 2020). Therefore, healthcare professionals should develop and implement appropriate interventions to improve spiritual well-being among childhood cancer patients. However, before any intervention can be properly designed and evaluated, it is essential to have access to a valid and reliable instrument for assessing spiritual well-being among pediatric cancer patients.
A previous systematic review evaluated the measurements of spirituality in adolescent health outcomes research, and identified five most commonly used scales to assess spiritual well-being, including Brief Multidimensional Measure of Religiousness/Spirituality, Spiritual Well-Being Scale, Religious Coping Questionnaire, Religious Orientation Scale, and Systems of Belief Inventory (Cotton et al., 2010). However, two limitations are needed to be considered when selecting a spiritual scale for childhood cancer patients. Firstly, these scales contained more than half of items on religion, which may not be suitable for non-religious children. Although religion usually links with the spirituality, spiritual well-being can be achieved for both religious population and non-religious population. Patients with religion may attain spiritual well-being via praying to god and finding connections with a supreme being, thus gaining comfort and enhancing their willingness to actively seek treatment (Peteet and Balboni, 2013). While for non-religious patients, like those in China, often rely on other means, such as self-exploration and connections with their loved ones, to identify the meaning of their existence and suffering, giving them the strength to continue their struggle against cancer (Peteet and Balboni, 2013). Hence, it is necessary to identify and select a scale that is appropriate to assess spiritual well-being for both religious and non-religious childhood cancer patients. Secondly, most studies using these five scales did not report the relevant psychometrics in adolescent population (Cotton et al., 2010). Importantly, none of these five scales have been rigorously validated in childhood cancer population.
The Functional Assessment of Chronic Illness Therapy Spiritual Well-being Scale (FACIT-Sp) is the most often employed measure for assessing spiritual well-being in adult cancer patients (Monod et al., 2011). The FACIT-Sp was developed based on interviews with American cancer patients and oncology specialists, and further validated in patients with different religions and in non-religious patients in various contexts, including Brazil, Denmark, Korea, Iran, Jordan, Norway and the United States (Bredle et al., 2011). The scale contains 12 items, and confirmatory factor analysis (CFA) revealed three scale domains: (1) the meaning domain, which assesses meaning and purpose in life; (2) the peace domain, which assesses the feeling of peace and calmness; and (3) the faith domain, which assesses the faith derived from religion or other sources (e.g., supernatural power) (Canada et al., 2008). The FACIT-Sp has been utilized to evaluate spiritual well-being among pediatric patients (Cotton et al., 2009, 2012). Evidence indicates that this instrument is reliable and valid for use with adolescents with chronic illness (de Alvarenga et al., 2019). However, the FACIT-Sp has never been validated for use with childhood cancer patients, including in the Chinese context. Because of the uncertain prognosis, long-term hospitalization, and difficult treatment, childhood cancer patients have unique spiritual needs, which distinct from those with other diseases, according to previous studies (Holge-Hazelton et al., 2016). Importantly, culture plays a significant role in influencing spiritual needs (Conner and Eller, 2004). Due to the aforementioned concerns, it may be premature to directly apply the FACIT-Sp to evaluate the spiritual well-being of childhood cancer patients prior to adaptation and psychometric testing. There is currently no validated instrument for assessing spiritual well-being in children with cancer. As such, the current study aimed to translate and adapt the FACIT-Sp for Chinese children with cancer and examine the psychometric properties and factor structure in this population.
Materials and methods
Study design
This study was a methodological study that was done cross-sectionally. This study was conducted in three stages: translation of the FACIT-SP scale, adaption of the FACIT-Sp scale based on our qualitative results of spiritual needs among Chinese childhood cancer patients, and psychometric evaluation of the adapted scale.
Translation
For the purpose of translation and adaption, an expert panel was established. The translation process followed the method proposed by Bracken and Barona (1991). Initially, the English version of the FACIT-Sp was translated into the Chinese version by two bilingual translators independently. The panel member then compared and reconciled the two translations. The back-translation was completed by two additional independent bilingual translators who were blinded to the original English version of the scale. The panel members checked to see if the original meaning of each item of the scale was preserved in the back translations by comparing them to the original English version. Disagreement were settled at regularly scheduled meetings.
Adaption
The adaptation of the FACIT-Sp was based on a qualitative study which explored the spiritual needs and concerns in Chinese childhood cancer patients aged 8–17 years from a pediatric public hospital. A descriptive phenomenological qualitative was applied. A total of 22 childhood cancer patients recruited by purposive sampling were invited to join an individual semi-structured interview. The semi-structured interview guide covered three aspects of spirituality, including meaning and purpose, relationship, and religion and faith. Example of questions included “Which experience in your cancer journey makes you feel fulfilled?” and “What is the impact of spirituality on your cancer journey?.” The data was analyzed using the thematic analysis. Details of this qualitative study has been previously published in elsewhere (Liu et al., 2022). In brief, patients’ spiritual needs can be divided into four categories: (1) meaning of cancer in their life, (2) personal inner needs, (3) connections with others, and (4) connections with gods, supernatural powers and fictional characters.
Based on the findings of our qualitative research, we found that three identified categories (meaning of cancer in their life, personal inner needs, and connections with gods, supernatural powers and fictional characters) corresponded to the three domains of the FACIT-Sp (meaning, peace, and faith domains). However, the remaining category (connections with others) in our qualitative study was not adequately assessed in the original FACIT-Sp. Thus, in accord with previous literature and our qualitative findings, we added three items to assess the new “connections with others” category: (1) I feel free to express my concerns to others; (2) I can feel the support of others; and (3) I think I am still helpful to others.
Previous evidence suggested that at least five participants are needed to test the comprehension and identify possible ambiguous aspects of scales for children (Halliwell et al., 2017; Llistosella et al., 2019; Riad et al., 2021). Hence, the preliminary version was administered to 10 hospitalized cancer patients (selected based on the same inclusion criteria for the participants in the psychometric evaluation) to test the comprehension of the adapted scale for children.
Psychometric evaluation
Setting
The study was conducted in Hunan Children’s Hospital in South-central China, which provides treatment to all children with cancer in the province. The selection of this study site ensured the representativeness of our participants. The Institutional Review Board of Hong Kong Polytechnic University approved this research (HSEARS20220127001).
Participants
Hospitalized childhood cancer patients were recruited through convenience sampling. The eligibility criteria were as follows: (1) age: 8–17 years old; (2) with parental consent to participate, (3) diagnosed with any cancer and were undergoing treatment at any stage (Grossoehme et al., 2020); (4) ability to communicate that they were having cancer treatment; and (4) ability to communicate and read Chinese. Individuals with identified cognitive and/or behavioral problems that affected communication were excluded. This age range (8–17 years old) was chosen based on the childhood cognitive development. According to the Piaget theory of childhood cognitive developmental stages (Ramesh, 2022), children aged 0–7 years have not developed the mental capacities of logic thought. These immature mental capacities may prevent them from generating an explanation of their own experience, which could impede their understanding of questions in the scale. Thus, only those ≥8 years old were selected because they could comprehend the questionnaire.
Although there are no clear guidelines regarding sample size calculation for factor analysis, ≥200 participants are required for CFA (Gorsuch, 2014). Also ≥200 participants are needed for EFA (Sakaluk and Short, 2017). We therefore determined to recruit 400 hospitalized childhood cancer patients in the current study.
Study instruments
Socio-demographic and clinical characteristics
Participants’ demographic and clinical variables, including age, sex, parental educational attainment, household size, religious affiliation, diagnosis, and treatment type, were documented on an information sheet.
The Chinese version of the adapted FACIT-Sp scale
The adapted FACIT-Sp assessed individuals’ spiritual well-being in the last 7 days. It contains 15 items that can be further categorized into four domains: the meaning domain, peace domain, faith domain, and connections with others domain. All items are scored between 0 (“not at all”) and 4 (“very much”) on a five-point rating scale. The scores are added together to get a total score that ranges from 0 to 60, with higher scores indicating greater spiritual well-being. Previous psychometric testing of the English version of the FACIT-Sp have verified its reliability and validity for measuring spiritual well-being among adult cancer patients (Canada et al., 2008).
The Chinese version of the center for epidemiology studies depression scale for children
The CES-DC was used to record the depressive symptoms experienced by the participants. This questionnaire has 20 items, each of which is rated on a four-point Likert scale based on the last week’s experiences. The range of scores is from 0 to 60, with higher scores indicating more depressive symptoms. The cut-off score is 16, suggesting that children exhibit a considerable number of depressed symptoms. The psychometric properties of the Chinese version of the CES-DC have been reported to show good internal consistency (the Cronbach’s α = 0.82), and appropriate convergent and discriminant validity (Li et al., 2010).
The Chinese version of the pediatric quality of life inventory 3.0 cancer module
Using the PedsQL, the quality of life of the participants was measured. There are a total of 27 questions on this scale, which are divided into eight subscales: pain and hurt, nausea, procedural anxiety, treatment anxiety, worry, cognitive problems, perceived physical appearance, and communication. The PedsQL scores vary from 0 to 100, with higher values indicating a higher quality of life in terms of one’s health. The scale shows good reliability with a Cronbach’s α value of 0.87 and validity in Chinese Children with cancer (Ji et al., 2011).
Data collection
First, a research assistant approached the parents of eligible patients in pediatric wards, and explained the design, method, and potential implications in detail. Parents who consented to their children’s participation were requested to sign a written consent. Both the parents and the children were given the assurance that they could stop participating at any point without penalty. All participants were required to fill in the adapted FACIT-Sp, CES-DC, and PedsQL 3.0 Cancer Module. The Peds-QL and CES-DC were included for examining the convergent validity, since spiritual well-being relates to both quality of life and depressive symptoms (Bai et al., 2015; Chaar et al., 2018). For the purpose of evaluating test–retest reliability, a total of 50 hospitalized pediatric cancer patients were invited (with parental consent) to complete the adapted FACIT-Sp again after 2 weeks (Hopkins, 2000; Li et al., 2010; Carvajal et al., 2011; Ho et al., 2015, 2021).
Data analysis
Semantic equivalence
Semantic equivalence of the translated items was evaluated. A panel of experts was asked to score the translation equivalence between the original English and Chinese versions of the FACIT-SP for each item on a four-point scale (from 1 = not equivalent to 4 = most equivalent). The equivalence rate (the proportion of the total items rated by the experts as either 3 or 4) would next be computed. Any item that received a rating of 1 or 2 from more than 20% of the panel members would be revised.
Content validity
The content validity of the Chinese version of the adapted FACIT-Sp was evaluated using the content validity index (CVI). According to the item relevance to the concept of spiritual well-being, the expert panel graded each item from 1 (entirely irrelevant) to 4 (highly relevant). For each item, the CVI of an item (I-CVI) was determined by dividing the proportion of experts who gave a rating of 3 or 4 of experts who rated the item. Good content validity was indicated by I-CVI ≥ 0.80 (Polit and Beck, 2006). Items rated below 0.8 were discussed and considered for deletion or revision.
Reliability testing
Cronbach’s alpha was used to evaluate the internal consistency reliability of the Chinese versions of the adapted FACIT-Sp, and values over 0.70 were regarded to be satisfactory. The intra-class correlation (ICC) analysis was used and the ICC coefficient was calculated to examine test–retest reliability. ICC values lower than 0.40 were considered weak, values of 0.41–0.59 were considered moderate, values of 0.60–0.75 were considered good or substantial, and values higher than 0.75 were considered very good (Mcdowell, 2006).
Convergent validity
Convergent validity was established by finding correlations between scores on the Chinese versions of the adapted FACIT-Sp and CES-DC, as well as the PedsQL 3.0 Cancer Module using Spearman’s correlation coefficients. On the basis of previous literature (Bai et al., 2015; Chaar et al., 2018), we hypothesized that adapted FACIT-Sp scores would have a positive correlation with PedsQL 3.0 scores and a negative correlation with CES-DC scores.
Exploratory factor analysis and confirmatory factor analysis
To examine the underlying factor structure of the Chinese version of the adapted FACIT-Sp, EFA was first conducted, followed by CFA. These analyses were used to ascertain that the factor structure found in the EFA adequately fit the data. Because the EFA and CFA were needed to be performed on two different datasets, the original dataset (N = 412) was split in half randomly (datasets A and B). EFA and CFA were performed on datasets A (N = 206) and B (N = 206), respectively.
EFA was carried out utilizing the Statistical Package for Social Sciences (SPSS) software, version 26.0 for Windows (SPSS Inc., Chicago, IL, United States). Prior to EFA, data sufficiency was confirmed using Bartlett’s test of sphericity and the Kaiser–Meyer–Olkin test. A principal components analysis was then performed. Coefficients equal or greater than 1.0 according to Kaiser’s criterion were considered (Kline, 2014). For the screen test, all factors above the elbow, or the break in the plot, were kept, since they accounted for a larger portion of the total variance in the data set (Cattell, 1966).
After the EFA analysis, CFA was performed using AMOS for Windows, version 20.0. The overall fit of the three-factor (meaning, peace and faith) and four-factor (meaning, peace, faith, and connection with others) models were examined and compared. The overall fit of the models were examined using goodness of fit indices, including the χ2/degrees of freedom (df) ratio, goodness of fit index (GFI), normed fit index (NFI), adjusted goodness of fit index (AGFI), comparative fit index (CFI), incremental fit index (IFI), and root mean square error of approximation (RMSEA) (Kline, 2014).
Results
Demographic and clinical characteristics
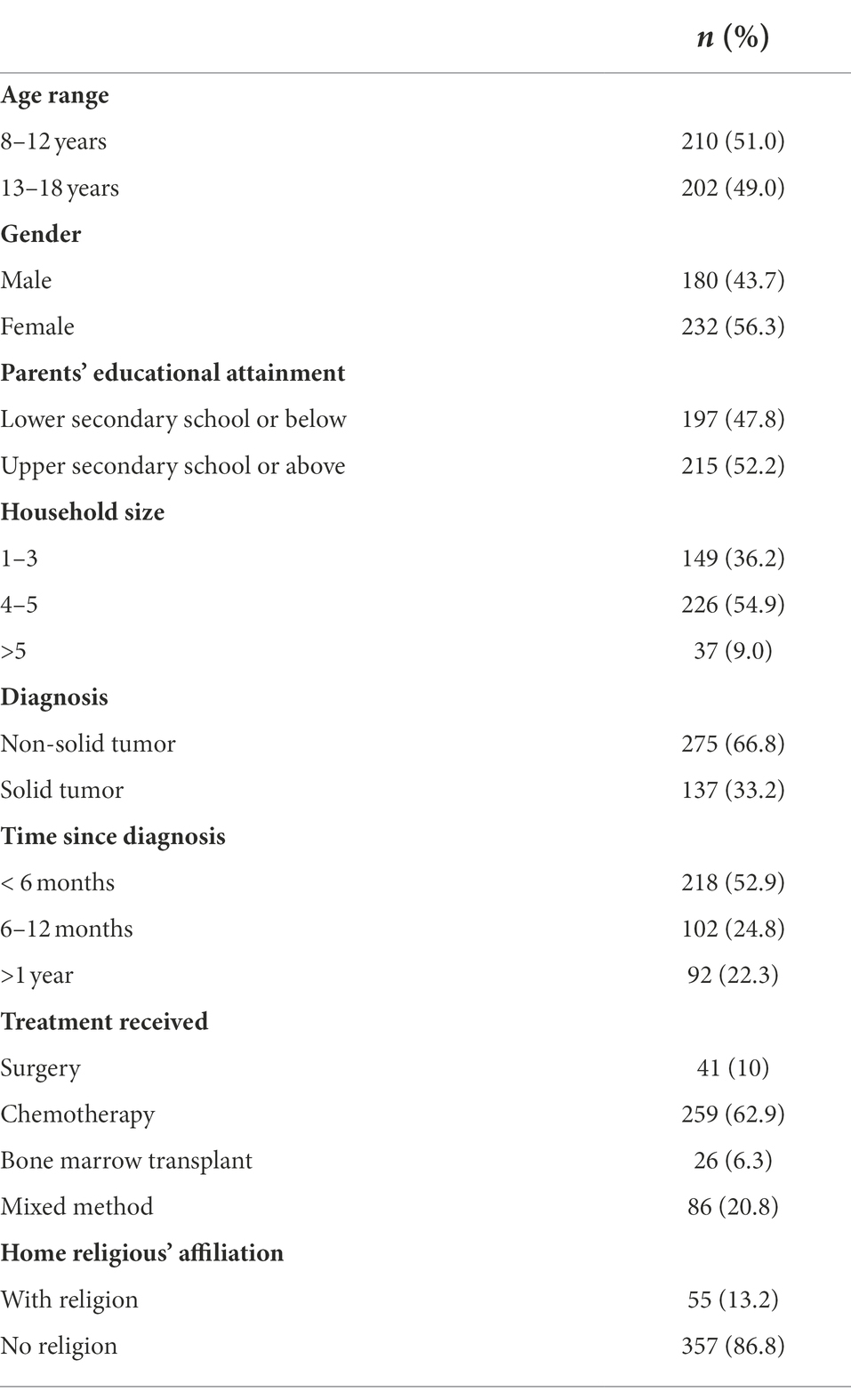
Table 1 presents participants’ demographic and clinical characteristics. Participants’ mean age was 12.3 years (standard deviation [SD] = 2.9) and the mean household size was 4.14 (SD = 1.1). Of the participants, 56.3% (n = 232) were girls, 86.8% (n = 357) were non-religious, 52.2% (n = 215) of parents had attained upper secondary school education, 66.8% (n = 275) were diagnosed with non-solid tumor, 52.9% (n = 232) were diagnosed within 6 months, and 20.8% (n = 86) had received multiple treatments for cancer.
Semantic equivalence
For the translated items, the semantic equivalence ranged from 0.8 to 1.0. The overall rate was 0.83, indicating that each item of the Chinese version of the FACIT-Sp was equivalent to those in the English version in both conceptual and idiomatic terms.
Content validity
For the Chinese version of the adapted FACIT-Sp scale, the I-CVIs values ranged from 0.8 to 1, and the S-CVI was 0.84 for the overall scale, indicating that the adapted scale had satisfactory content validity.
Reliability
The internal consistency of the adapted scale was measured using a Cronbach’s alpha of 0.815. The corrected item–total correlations ranged from 0.29 to 0.70, indicating acceptable internal consistency. At the 2-week interval, the test–retest reliability coefficient was 0.79 (p < 0.001).
Convergent validity
Spearman’s correlation coefficients of 0.64 and 0.47 were found between the scores of FACIT-Sp and CES-DC, and between the scores of FACIT-Sp and PedsQL, respectively. The results indicated that the translated and adapted version of the FACIT-Sp had appropriate construct validity.
Exploratory factor analysis
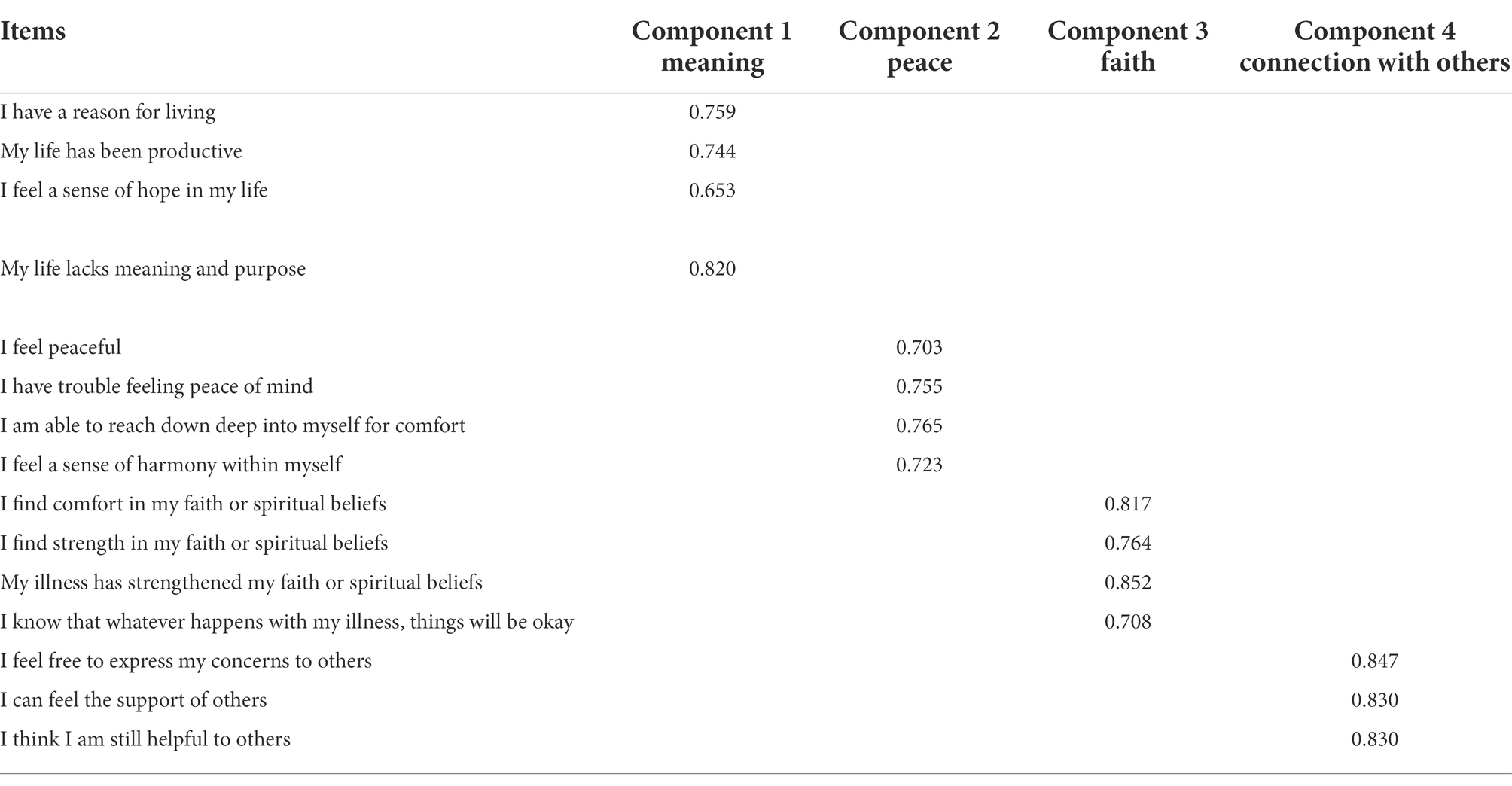
The Kaiser–Meyer–Olkin value was 0.807, and the results of Bartlett’s test of sphericity were significant (p < 0.001), revealing that the dataset met was suitable for factor analysis. Four factors with an eigenvalue higher than 1 were identified using principal components analysis, which explained 72.72% of the total variance. Factor 1 (“meaning”) explained 17.66% of the variance, factor 2 (“peace”) explained 22.25% of the variance, factor 3 (“faith”) explained 17.52% of the variance, and factor 4 (“connection with others”) explained 15.29% of the variance. All items were loaded on a single dominating factor and had factor loadings greater than 0.4. The interpretation of three components (meaning, peace, and faith) was consistent with the proposed factor structures of the original English version of the FACIT-Sp. Three newly added items successfully loaded on the “connection with others” factor (Table 2).
Confirmatory factor analysis
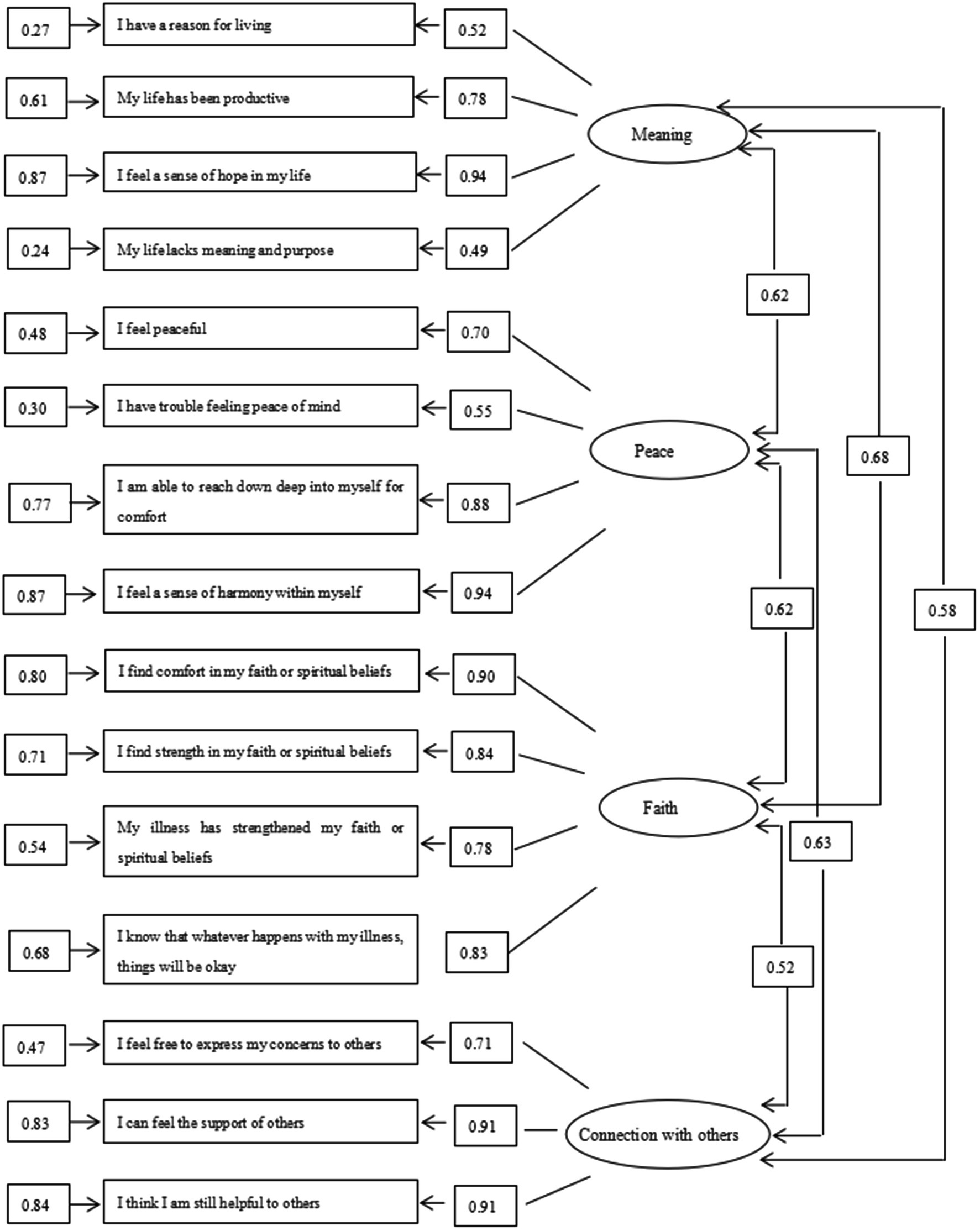
The parameter estimates of the four-factor model are displayed in Figure 1. All correlation matrices were positively definite and were less than 1, indicating that the parameter estimates were appropriate. The observed variables all had high factor loadings, ranging from 0.49 to 0.94. The t-values of all variables were higher than 1.96, indicating that the loadings on the variables were significant.
The overall fit of the three-factor model based on 12 items of the original FACIT-Sp, and the four-factor model based on 15 items of the adapted version were tested by a variety of fit indices. The results suggested that the four-factor model based on 15 items was better than the three-factor model based on 12 items (Tables 3, 4).
Discussion
Spiritual well-being was recently recognized as the fourth dimension of health by the World Health Organization (Dhar et al., 2013), and it is reported to be closely linked to physical and psychosocial well-being in patients with childhood cancer (Grossoehme et al., 2020). Nevertheless, there is currently no validated instrument for assessing spiritual well-being in children with cancer. To address this gap in existing literature, we translated and adapted the FACIT-Sp, a widely used instrument for assessing spiritual well-being in adult cancer patients. Additionally, the psychometric properties of the adapted Chinese version were tested in Chinese children who were hospitalized with cancer in China.
In accord with previous validation studies of adolescents with chronic diseases and young adults with cancer (de Alvarenga et al., 2019; Grossoehme et al., 2020), the Chinese version of the adapted FACIT-Sp showed satisfactory internal consistency. Specifically, all items of the adapted FACIT-Sp appeared to measure the same construct, spiritual well-being, with the corrected item-total correlations ranging from 0.29 to 0.70. In addition, the ICC at 2 weeks was high, indicating good test–retest reliability.
Regarding content validity, most items in the adapted Chinese version of the FACIT-Sp were found to be reflective of the underlying construct (spiritual well-being). However, when we piloted the prototype scale in Chinese children with cancer, few respondents reported (n = 2) that item 5 (“I feel a sense of purpose in life”) was difficult to answer. These two respondents felt that the purpose of life was an ambiguous concept for them to consider, particularly because they were very young to be thinking about this issue. Hence, even if participants responded “not at all,” this did not necessarily indicate that they thought their life was purposeless. Interestingly, these two respondents also stated that they were on a path of searching for their purpose in life, and that the journey of combatting cancer provided them with an opportunity to think and identify their life purpose. Thus, cancer appeared to serve as a catalyst for some children to find purpose, although they still felt unsure of their specific purpose in life. Given the importance of life purpose in the concept of spiritual well-being (Lormans et al., 2021), the panel members decided, after thorough discussion, to retain this item for validation. This item also showed satisfactory factor loadings in both EFA and CFA. However, future research will be required to determine whether refinement of the item wording is necessary to improve clarity for children.
A negative correlation was found between the adapted FACIT-Sp and the CES-DC scores, providing evidence for the convergent validity. These findings were in accord with previous studies reporting that childhood cancer patients with higher levels of spiritual well-being presented fewer depressive symptoms and had better QoL (Bai et al., 2015; Chaar et al., 2018).
The EFA findings indicated that the four-factor model explained 72.72% of the total variance, which was over the Streiner-suggested threshold of 50% (Streiner, 1994). In addition, the CFA results revealed that the four-factor model provided a better fit than the original three-factor model. This result suggests that the four-factor model with the inclusion of “connection to others” domain better captures the concept of spiritual well-being of Chinese childhood cancer patients than the original three-factor model. Unlike adult cancer patients who require room for self-reflection on life goals and values (Van Gurp et al., 2020), children with cancer are more likely to rely on family and friends to establish normalcy in their disease trajectory (Hay and Nye, 2006). The intimate relationships between children and their families as well as their friends serve as a source of love, compassion, distraction, and support to motivate them to combat the disease (Petersen, 2014). Furthermore, in contrast to children in Western countries who relieve their spiritual distress by finding a connection with God via engaging in religious practices, Chinese children count more on the connection with people surrounding them (Moore et al., 2020). This could be because most Chinese are not religious, with only 15% of Chinese having religious affiliations (Zhang and Lu, 2020). The results from our previous qualitative study indicated that there were three ways adopted by Chinese childhood cancer patients to establish the connection with others. The three ways included expressing their suffering and emotional distress to their loved ones, feeling of being supported by others, and being helpful to others (Liu et al., 2022). Expressing suffering to their loved ones help them to share and manage their losses, concerns and feelings, thus alleviating their spiritual suffering (Petersen, 2014; Liu et al., 2022). Feeling of being supported by others can serve as a spiritual support to motivate them to continue the treatment, notwithstanding the suffering caused by cancer (Petersen, 2014; Liu et al., 2022). Being helpful to others allows them to gain appreciations from others, so that they can find their self-value even in this difficult journey (Liu et al., 2022). These three ways of “connection with others” can assist them to overcome an existential crisis, ultimately improving their spiritual well-being. Hence, adding the new domain “connection with others” with its three items in the FACIT-Sp can greatly enhance its structural validity to capture spiritual well-being of children with cancer in the Chinese context.
Most items had significant factor loadings in the four-factor model, as indicated by the CFA results, with the exception of item 4 (“My life lacks meaning and purpose”) that attained a factor loading of 0.49. This is accords with the results of previous validation studies of the FACIT-Sp in adult populations (Canada et al., 2008; Murphy et al., 2010; Lazenby et al., 2013). The low factor loading for item 4 may have been caused by this item being negatively worded. Increasing evidence suggests that negatively worded items do not match the overall logic of other items that are positively worded, and hence people may respond incorrectly if they do not pay sufficient attention to distinguishing negatively worded items from positively worded items (Sonderen et al., 2013; Salazar, 2015). Indeed, “careless responses” and “difficulty in understanding” have been persistently acknowledged as the major reasons for low factor loadings for negatively worded items in previous studies (Salazar, 2015). Although some researchers have suggested switching out negatively worded items on the FACIT-Sp for positively worded ones (Murphy et al., 2010; Lazenby et al., 2013), caution must be taken because negatively worded items can reduce response set bias, which is defined as the tendency of respondents to answer similarly to all or many items (Van Herk et al., 2004). The think-aloud approach suggested by Lewis could be adopted in further studies to give recommendations regarding if the negatively phrased items in the FACIT-Sp should be retained or replaced (Güss, 2018). In particular, respondents can be asked to verbalize or write down their thoughts when answering each item (Güss, 2018). Researchers can then make use of these think-aloud data to specify questions that are easily misinterpreted and even develop further questions for clarification, thus obtaining more accurate responses (Güss, 2018).
Implications for future practice
Increasing evidence indicates that low levels of spiritual well-being are strongly related to the development of various psychological symptoms, such as depression and anxiety, in children with different clinical conditions including cancer (Taylor et al., 2015; Pratiwi et al., 2018). Given the importance of spiritual well-being in the disease trajectory, the Chinese version of the adapted FACIT-Sp can be used as a standard evaluation instrument, and early intervention can be provided to minimize its associated healthcare costs. Additionally, previous studies have developed interventions that can improve spiritual well-being for adult cancer patients (Kruizinga et al., 2016). However, due to the lack of a reliable instrument to evaluate spiritual well-being for children with cancer, including those in China, the development of spiritual interventions is lagging far behind. Hence, to advance clinical practice, the adapted FACIT-Sp may be useful for evaluating the effectiveness of existing spiritual interventions, improving the spiritual well-being of Chinese children hospitalized with cancer.
Limitations
There are several limitations should be noted in the current study. First, the generalizability of the results may restrict by the using of convenience sampling. Second, because of ethical considerations, childhood cancer patients who were terminally ill were not recruited in this study. It is therefore unclear whether this adapted scale can be used to evaluate the spiritual well-being of Chinese children with terminal cancer.
Conclusion
The current study addressed a gap in the literature by translating and adapting the FACIT-Sp for Chinese children with cancer. Statistical analyses confirmed that the adapted FACIT-Sp is a reliable and valid instrument for assessing spiritual well-being in this population.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving human participants were reviewed and approved by the Institutional Review Board, Hong Kong Polytechnic University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author contributions
QL: conceptualization, methodology, data collection, and draft preparation. K-YH: conceptualization, methodology, draft preparation, and supervision. GB: revising and editing. K-K-WL: conceptualization, methodology, and writing. E-H-LC: writing—review and editing. S-S-YC: conceptualization, writing—review and editing. F-K-YW: writing—review and editing. WL: writing—review and editing. All authors contributed to the article and approved the submitted version.
Acknowledgments
We thank the patients for spending their time in this study. We also thank Benjamin Knight, MSc., from Edanz (www.edanz.com/ac) for editing a draft of this manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bai, M., Lazenby, M., Jeon, S., Dixon, J., and Mccorkle, R. (2015). Exploring the relationship between spiritual well-being and quality of life among patients newly diagnosed with advanced cancer. Palliat. Support. Care 13, 927–935. doi: 10.1017/S1478951514000820
Bracken, B. A., and Barona, A. (1991). State of the art procedures for translating, validating and using psychoeducational tests in cross-cultural assessment. Sch. Psychol. Int. 12, 119–132. doi: 10.1177/0143034391121010
Bredle, J. M., Salsman, J. M., Debb, S. M., Arnold, B. J., and Cella, D. (2011). Spiritual well-being as a component of health-related quality of life: the functional assessment of chronic illness therapy—spiritual well-being scale (FACIT-Sp). Religions 2, 77–94. doi: 10.3390/rel2010077
Canada, A. L., Murphy, P. E., Fitchett, G., Peterman, A. H., and Schover, L. R. (2008). A 3-factor model for the FACIT-Sp. Psychooncology 17, 908–916. doi: 10.1002/pon.1307
Carvajal, A., Centeno, C., Watson, R., and Bruera, E. (2011). A comprehensive study of psychometric properties of the Edmonton symptom assessment system (ESAS) in Spanish advanced cancer patients. Eur. J. Cancer 47, 1863–1872. doi: 10.1016/j.ejca.2011.03.027
Cattell, R. B. (1966). The screen test for the number of factors. Multivar. Behav. Res. 1, 245–276. doi: 10.1207/s15327906mbr0102_10
Chaar, E. A., Hallit, S., Hajj, A., Aaraj, R., Kattan, J., Jabbour, H., et al. (2018). Evaluating the impact of spirituality on the quality of life, anxiety, and depression among patients with cancer: an observational transversal study. Support. Care Cancer 26, 2581–2590. doi: 10.1007/s00520-018-4089-1
Comas Carbonell, E., Mateo-Ortega, D., and Busquets-Alibes, E. (2021). The psychological experience of pediatric oncology patients facing life-threatening situations: a systematic review with narrative synthesis. Palliat. Support. Care 19, 733–743. doi: 10.1017/S1478951521000031
Conner, N. E., and Eller, L. S. (2004). Spiritual perspectives, needs and nursing interventions of Christian African–Americans. J. Adv. Nurs. 46, 624–632. doi: 10.1111/j.1365-2648.2004.03053.x
Cotton, S., Kudel, I., Roberts, Y. H., Pallerla, H., Tsevat, J., Succop, P., et al. (2009). Spiritual well-being and mental health outcomes in adolescents with or without inflammatory bowel disease. J. Adolesc. Health 44, 485–492. doi: 10.1016/j.jadohealth.2008.09.013
Cotton, S., Mcgrady, M. E., and Rosenthal, S. L. (2010). Measurement of religiosity/spirituality in adolescent health outcomes research: trends and recommendations. J. Relig. Health 49, 414–444. doi: 10.1007/s10943-010-9324-0
Cotton, S., Weekes, J. C., Mcgrady, M. E., Rosenthal, S. L., Yi, M. S., Pargament, K., et al. (2012). Spirituality and religiosity in urban adolescents with asthma. J. Relig. Health 51, 118–131. doi: 10.1007/s10943-010-9408-x
Davis, L. Z., Cuneo, M., Thaker, P. H., Goodheart, M. J., Bender, D., and Lutgendorf, S. K. (2018). Changes in spiritual well-being and psychological outcomes in ovarian cancer survivors. Psychooncology 27, 477–483. doi: 10.1002/pon.4485
De Alvarenga, W. A., Nascimento, L. C., Dos Santos, C. B., Leite, A., Mühlan, H., Schmidt, S., et al. (2019). Measuring spiritual well-being in Brazilian adolescents with chronic illness using the FACIT-Sp-12: age adaptation of the self-report version, development of the parental-report version, and validation. J. Relig. Health 58, 2219–2240. doi: 10.1007/s10943-019-00901-y
Dhar, N., Chaturvedi, S. K., and Nandan, D. (2013). Spiritual health, the fourth dimension: a public health perspective. WHO South-East Asia J. Pub. Health 2, 3–5. doi: 10.4103/2224-3151.115826
Foster, T. L., Bell, C. J., and Gilmer, M. J. (2012). Symptom Management of Spiritual Suffering in Pediatric palliative care. J. Hosp. Palliat. Nurs. 14, 109–115. doi: 10.1097/NJH.0b013e3182491f4b
Grossoehme, D. H., Friebert, S., Baker, J. N., Tweddle, M., Needle, J., Chrastek, J., et al. (2020). Association of religious and spiritual factors with patient-reported outcomes of anxiety, depressive symptoms, fatigue, and pain interference among adolescents and young adults with cancer. JAMA Netw. Open 3:e206696. doi: 10.1001/jamanetworkopen.2020.6696
Güss, C. D. (2018). What is going through your mind? Thinking aloud as a method in cross-cultural psychology. Front. Psychol. 9:1292. doi: 10.3389/fpsyg.2018.01292
Halliwell, E., Jarman, H., Tylka, T., and Slater, A. (2017). Adapting the body appreciation Scale-2 for children: a psychometric analysis of the BAS-2C. Body Image 21, 97–102. doi: 10.1016/j.bodyim.2017.03.005
Hendricks-Ferguson, V. (2008). Hope and spiritual well-being in adolescents with cancer. West. J. Nurs. Res. 30, 385–401. doi: 10.1177/0193945907303045
Ho, K. Y., Lam, K. K., Xia, W., Chung, J., Cheung, A. T., Ho, L. L., et al. (2021). Psychometric properties of the Chinese version of the Pittsburgh sleep quality index (PSQI) among Hong Kong Chinese childhood cancer survivors. Health Qual. Life Outcomes 19, 1–11. doi: 10.1186/s12955-021-01803-y
Ho, K. Y., Li, W. H. C., Lam, K. W. K., Chui, S. Y., and Chan, C.-F. G. (2015). Psychometric properties of the Chinese version of the fatigue scale-adolescent. BMC Cancer 15:938. doi: 10.1186/s12885-015-1945-y
Holge-Hazelton, B., Timm, H. U., Graugaard, C., Boisen, K. A., and Sperling, C. D. (2016). “perhaps I will die young.” fears and worries regarding disease and death among Danish adolescents and young adults with cancer. A mixed method study. Support Care Cancer 24, 4727–4737. doi: 10.1007/s00520-016-3322-z
Hopkins, W. G. (2000). Measures of reliability in sports medicine and science. Sports Med. 30, 1–15. doi: 10.2165/00007256-200030010-00001
Ji, Y., Chen, S., Li, K., Xiao, N., Yang, X., Zheng, S., et al. (2011). Measuring health-related quality of life in children with cancer living in mainland China: feasibility, reliability and validity of the Chinese mandarin version of PedsQL 4.0 generic Core scales and 3.0 cancer module. Health Qual. Life Outcomes 9, 1–13. doi: 10.1186/1477-7525-9-103
Kruizinga, R., Hartog, I. D., Jacobs, M., Daams, J. G., Scherer-Rath, M., Schilderman, J. B., et al. (2016). The effect of spiritual interventions addressing existential themes using a narrative approach on quality of life of cancer patients: a systematic review and meta-analysis. Psychooncology 25, 253–265. doi: 10.1002/pon.3910
Lazenby, M., Khatib, J., Al-Khair, F., and Neamat, M. (2013). Psychometric properties of the functional assessment of chronic illness therapy—spiritual well-being (FACIT-Sp) in an Arabic-speaking, predominantly Muslim population. Psycho-Oncology 22, 220–227. doi: 10.1002/pon.2062
Li, H. C., Chung, O. K., and Ho, K. Y. (2010). Center for Epidemiologic Studies Depression Scale for children: psychometric testing of the Chinese version. J. Adv. Nurs. 66, 2582–2591. doi: 10.1111/j.1365-2648.2010.05440.x
Liu, Q., Ho, K.-Y., Lam, K.-K.-W., Lam, W.-Y.-Y., Cheng, E.-H.-L., Ching, S.-S.-Y., et al. (2022). A descriptive and phenomenological exploration of the spiritual needs of Chinese children hospitalized with cancer. Int. J. Environ. Res. Public Health 19:13217. doi: 10.3390/ijerph192013217
Llistosella, M., Gutiérrez-Rosado, T., Rodríguez-Rey, R., Liebenberg, L., Bejarano, Á., Gómez-Benito, J., et al. (2019). Adaptation and psychometric properties of the Spanish version of child and youth resilience measure (CYRM-32). Front. Psychol. 10:1410. doi: 10.3389/fpsyg.2019.01410
Lormans, T., De Graaf, E., Van De Geer, J., Van Der Baan, F., Leget, C., and Teunissen, S. (2021). Toward a socio-spiritual approach? A mixed-methods systematic review on the social and spiritual needs of patients in the palliative phase of their illness. Palliat. Med. 35, 1071–1098. doi: 10.1177/02692163211010384
Mcdowell, I. (2006). Measuring Health: A Guide to Rating Scales and Questionnaires. Oxford University Press. United States.
Monod, S., Brennan, M., Rochat, E., Martin, E., Rochat, S., and Büla, C. J. (2011). Instruments measuring spirituality in clinical research: a systematic review. J. Gen. Intern. Med. 26, 1345–1357. doi: 10.1007/s11606-011-1769-7
Moore, K., Talwar, V., Gomez-Garibello, C., Bosacki, S., and Moxley-Haegert, L. (2020). Children’s spirituality: exploring spirituality in the lives of cancer survivors and a healthy comparison group. J. Health Psychol. 25, 888–899. doi: 10.1177/1359105317737605
Murphy, P. E., Canada, A. L., Fitchett, G., Stein, K., Portier, K., Crammer, C., et al. (2010). An examination of the 3-factor model and structural invariance across racial/ethnic groups for the FACIT-Sp: a report from the American Cancer Society's study of cancer survivors-II (SCS-II). Psycho-oncology: journal of the psychological. Soc. Behav. Dimen. Cancer 19, 264–272. doi: 10.1002/pon.1559
Murray, S. A., Kendall, M., Boyd, K., Worth, A., and Benton, T. F. (2004). Exploring the spiritual needs of people dying of lung cancer or heart failure: a prospective qualitative interview study of patients and their carriers. Palliat. Med. 18, 39–45. doi: 10.1191/0269216304pm837oa
Peteet, J. R., and Balboni, M. J. (2013). Spirituality and religion in oncology. CA Cancer J. Clin. 63, 280–289. doi: 10.3322/caac.21187
Petersen, C. L. (2014). Spiritual care of the child with cancer at the end of life: a concept analysis. J. Adv. Nurs. 70, 1243–1253. doi: 10.1111/jan.12257
Polit, D. F., and Beck, C. T. (2006). The content validity index: are you sure you know what's being reported? Critique and recommendations. Res. Nurs. Health 29, 489–497. doi: 10.1002/nur.20147
Pratiwi, E., Mulatsih, S., and Setiyarini, S. (2018). Spirituality relationship to the quality of life of children with cancer. Dr. Sardjito General Hospital, Indonesia: International Journal of Community Medicine and Public Health, 5.
Ramesh, S. (2022). The Theories of Cognitive Development. The Political Economy of Human Behaviour and Economic Development. Springer.
Riad, R., Allodi, M. W., Siljehag, E., Wikman, C., Ford, T., and Bölte, S. (2021). How I feel about my school-adaptation and validation of an educational well-being measure among young children in Sweden. Int. J. Environ. Res. Public Health 18:5075. doi: 10.3390/ijerph18105075
Sakaluk, J. K., and Short, S. D. (2017). A methodological review of exploratory factor analysis in sexuality research: used practices, best practices, and data analysis resources. J. Sex Res. 54, 1–9. doi: 10.1080/00224499.2015.1137538
Salazar, M. S. (2015). The dilemma of combining positive and negative items in scales. Psicothema 27, 192–199. doi: 10.7334/psicothema2014.266
Sonderen, E. V., Sanderman, R., and Coyne, J. C. (2013). Ineffectiveness of reverse wording of questionnaire items: Let’s learn from cows in the rain. PLoS One 8:e68967. doi: 10.1371/journal.pone.0068967
Steliarova-Foucher, E., Colombet, M., Ries, L. A. G., Moreno, F., Dolya, A., Bray, F., et al. (2017). International incidence of childhood cancer, 2001-10: a population-based registry study. Lancet Oncol. 18, 719–731. doi: 10.1016/S1470-2045(17)30186-9
Streiner, D. L. (1994). Figuring out factors: the use and misuse of factor analysis. Can. J. Psychiatry 39, 135–140. doi: 10.1177/070674379403900303
Taylor, E. J., Petersen, C., Oyedele, O., and Haase, J. (2015). Spirituality and spiritual Care of Adolescents and Young Adults with cancer. Semin. Oncol. Nurs. 31, 227–241. doi: 10.1016/j.soncn.2015.06.002
Torabi, F., Rassouli, M., Nourian, M., Borumandnia, N., Shirinabadi Farahani, A., and Nikseresht, F. (2018). The effect of spiritual care on adolescents coping with cancer. Holist. Nurs. Pract. 32, 149–159. doi: 10.1097/HNP.0000000000000263
Van Gurp, J. L., Ebenau, A., Van Der Burg, S., and Hasselaar, J. (2020). Living and dying with incurable cancer: a qualitative study on older patients’ life values and healthcare professionals’ responsivity. BMC Palliat. Care 19, 1–11. doi: 10.1186/s12904-020-00618-w
Van Herk, H., Poortinga, Y. H., and Verhallen, T. M. M. (2004). Response Styles in Rating Scales: Evidence of Method Bias in Data From Six EU Countries. Journal of Cross-Cultural Psychology 35:346.
Zhang, C., and Lu, Y. (2020). The measure of Chinese religions: denomination-based or deity-based? Chin. J. Sociol. 6, 410–426. doi: 10.1177/2057150X20925312
Keywords: child, neoplasm, pediatric nursing, spirituality, psychometrics
Citation: Liu Q, Ho K-Y, Lam K-K-W, Lam W, Cheng E-H-L, Ching S-S-Y, Belay GM and Wong F-K-Y (2022) Adaptation and psychometric evaluation of the Chinese version of the functional assessment of chronic illness therapy spiritual well-being scale among Chinese childhood cancer patients in China. Front. Psychol. 13:1065854. doi: 10.3389/fpsyg.2022.1065854
Edited by:
Maryam Rassouli, Shahid Beheshti University of Medical Sciences, IranReviewed by:
Azam Shirinabadi Farahani, Shahid Beheshti University of Medical Sciences, IranHanieh Gholamnejad, Iran University of Medical Sciences, Iran
Copyright © 2022 Liu, Ho, Lam, Lam, Cheng, Ching, Belay and Wong. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ka-Yan Ho, a3lhbmhvQHBvbHl1LmVkdS5oaw==
 Qi Liu
Qi Liu Ka-Yan Ho
Ka-Yan Ho Katherine-Ka-Wai Lam
Katherine-Ka-Wai Lam Winsome Lam
Winsome Lam