- 1School of Nursing, Nanjing Medical University, Jiangsu, China
- 2Women’s Hospital of Nanjing Medical University (Nanjing Maternity and Child Health Care Hospital), Jiangsu, China
- 3School of Nursing, Suzhou University, Jiangsu, China
Aim: To define and analyze the concept of psychological birth trauma.
Design: The concept analysis method of Walker and Avant was used.
Method: Eight databases (PubMed, CINAHL Complete, Cochrane Library, Web of Science, China National Knowledge Infrastructure, Wanfang, VIP Information Chinese Journal Service Platform, and Chinese BioMedicine Literature Database) were searched from inception to July 2022 for studies focused on psychological birth trauma.
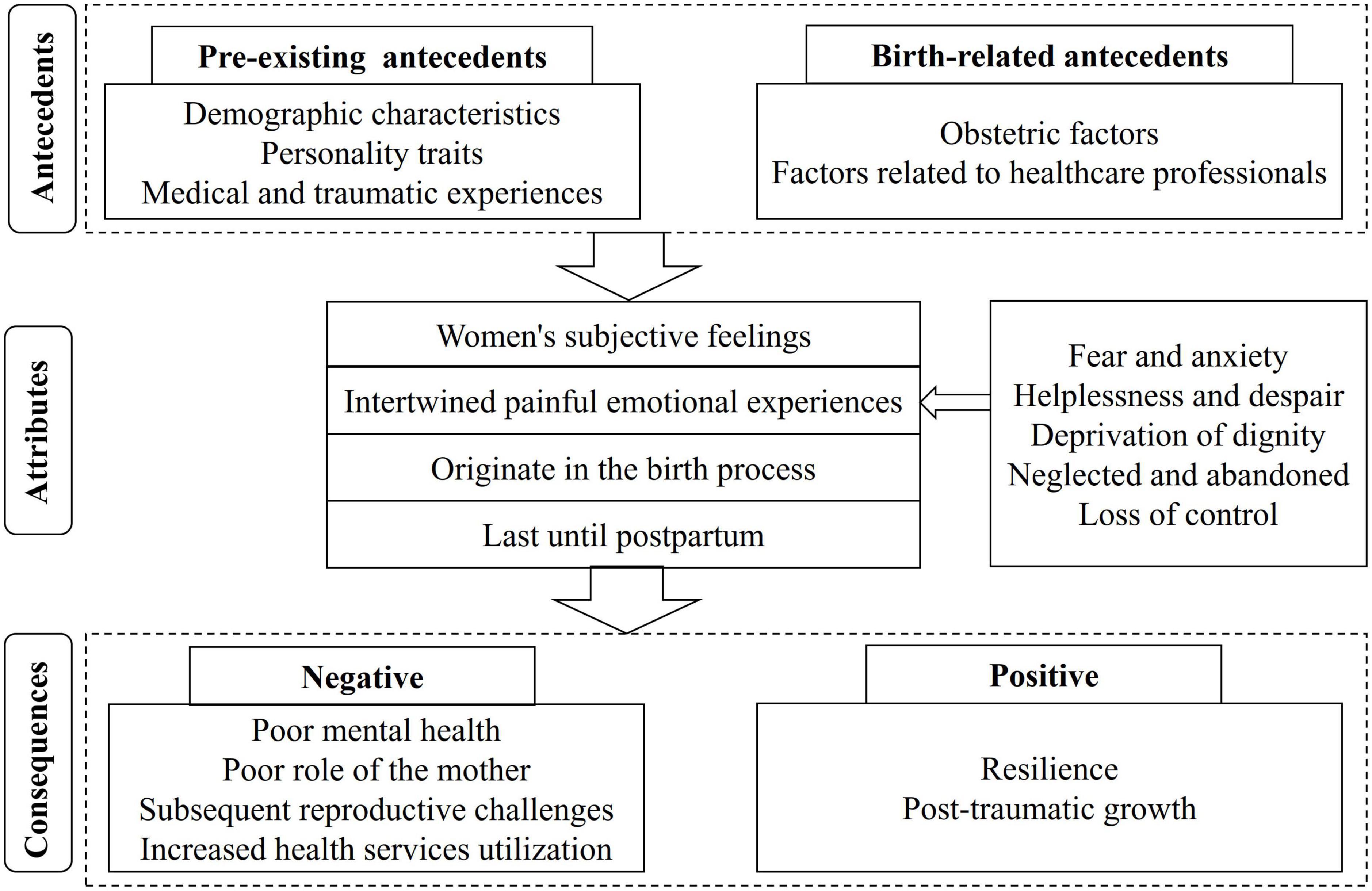
Results: Of the 5,372 studies identified, 44 ultimately met the inclusion criteria. The attributes identified were (1) women’s subjective feelings, (2) intertwined painful emotional experiences, (3) originating in the birth process, and (4) lasting until postpartum. Antecedents were divided into two groups: pre-existing antecedents and birth-related antecedents. Consequences were identified as negative and positive.
Conclusion: Psychological birth trauma is a more complex and comprehensive concept than previously thought, and should be regarded as a separate postpartum mental health problem. This study deepens the understanding of psychological birth trauma through a comprehensive concept analysis and also puts forward some suggestions for the prevention, identification, and intervention of psychological birth trauma, which provides a basis for assisting in the identification of psychological birth trauma and provides a reference for the development of rigorous assessment tools and the design of appropriate interventions in the future. Further research is needed to update and refine this concept.
1. Introduction
Childbirth, a major event in a woman’s life, is of a profound and complex nature (Shorey and Wong, 2022). Not only does it involve huge physical changes, but it is also accompanied by significant psychological fluctuations (Fenech and Thomson, 2015; Shorey and Wong, 2022). Negative birth experiences can even cause terrible psychological trauma to women (Fenech and Thomson, 2015; Shorey and Wong, 2022). Studies indicated that the incidence of traumatic birth ranges from 20 to 68.6 percent in different countries (Uotila et al., 2005; Türkmen et al., 2020; Bay and Sayiner, 2021). Professor Beck used the word “ripple effect” to describe the negative impacts of psychological birth trauma (Beck, 2015). These impacts appear to be centered on the poor mental health of women themselves (Beck, 2006; Taghizadeh et al., 2013), and then expand like ripples, affecting mother-infant relationships (Taghizadeh et al., 2013; Beck and Watson, 2019), breastfeeding behavior (Beck and Watson, 2008; Fenech and Thomson, 2014), marital relationships (Taghizadeh et al., 2013; Fenech and Thomson, 2014), and future reproductive decisions (Gottvall and Waldenström, 2002; Taghizadeh et al., 2013; Holopainen et al., 2020), etc. The further impact of psychological birth trauma is associated with post-traumatic stress disorder (PTSD) (Taghizadeh et al., 2013; Türkmen et al., 2020; McKelvin et al., 2021), a widely known term. According to DSM-IV criteria, PTSD is categorized as a disorder related to trauma and stress, which is mainly manifested in four symptom clusters: re-experience, avoidance, hyperarousal, and negative cognition and mood, and these symptoms should exist for more than a month (American Psychiatric Association, 2000). These symptoms can appear directly after experiencing a traumatic event, but can also occur later in life (American Psychiatric Association, 2000). A meta-analysis suggested that 4% of postpartum women in community samples developed PTSD following a traumatic birth experience, compared with 18.5% in high-risk samples (such as women with complications of pregnancy or childbirth) (Yildiz et al., 2017). This means that more postpartum women who have experienced psychological trauma are not reaching the threshold of PTSD and are therefore unidentified, but they are struggling with the trauma.
Some studies have focused on investigating the risk factors of psychological birth trauma, and multiple factors have been found, including some objective factors, such as preterm delivery (Chabbert et al., 2021; Sommerlad et al., 2021), as well as some subjective factors, such as women feeling disrespected by healthcare professionals during birth (Zhang et al., 2020; McKelvin et al., 2021; Watson et al., 2021; Liu et al., 2022). Notably, the ongoing COVID-19 seems to have made this phenomenon more complicated. A study conducted in the United States confirmed that women who gave birth during the outbreak of COVID-19 experienced more traumatic births and subsequent mother-infant bonding problems than those who gave birth before the pandemic (Mayopoulos et al., 2021). Another study investigated the impact of unaccompanied birth caused by COVID-19-related visiting bans on mothers’ mental health, and found that mothers who gave birth unaccompanied had higher psychological distress than those who gave birth accompanied (Oddo-Sommerfeld et al., 2022).
Regrettably, not enough attention has been paid to the psychological birth trauma itself, and more attention seems to be focused on the diagnosable postpartum psychological problems, such as postpartum PTSD mentioned above. An international knowledge mapping exercise aimed at examining policies, services, and training provisions for women following traumatic birth showed that of the 18 European countries that participated, only the Netherlands has national policies on screening, treatment, and prevention of traumatic birth experiences (Thomson et al., 2021). Adding to the dilemma is the fact that there is no consistent definition, terminology, or detailed description of this concept in the literature. Instead, various terms such as “birth/childbirth trauma,” “traumatic birth/childbirth,” “traumatic birth/childbirth experience,” or “psychological birth/childbirth trauma” are used, with almost the same meaning. Additionally, widely validated tools to assess psychological birth trauma are lacking. In conclusion, there is a long way to go in the management of psychological birth trauma.
A clear concept is the first key step to fully understanding this phenomenon and the basis for theoretical development (Walker and Avant, 2019). Therefore, this study aims to provide a comprehensive analysis of the concept of psychological birth trauma, in order to clarify this definition and provide a basis for the development of rigorous assessment tools, and then provide a reference for subsequent screening and interventional research and practice. We hope this work can make some contribution to the promotion of women’s health and well-being and social development.
2. Materials and methods
2.1. Concept analysis
Concept analysis is a systematic process of developing, clarifying, and refining the phenomenon under analysis (Walker and Avant, 2019). This study adopted the concept analysis method of Walker and Avant (2019), which has been widely used in the field of nursing. It consists of eight steps intended to guide the process (Table 1). Of these, the first and second steps have been described in the introduction section of this study.
2.2. Data sources
A comprehensive search of PubMed, CINAHL Complete, Cochrane Library, Web of Science, China National Knowledge Infrastructure, Wanfang, VIP Information Chinese Journal Service Platform, and Chinese BioMedicine Literature Database was conducted from inception to July 2022. The following medical subject heading (MeSH) terms and text words were used: “traumatic childbirth,” “traumatic birth,” “traumatic labor,” “traumatic delivery,” “childbirth trauma,” “birth trauma,” “labor trauma,” “labor trauma,” “delivery trauma,” “psychological trauma” AND (“parturition” OR “delivery, obstetric” OR “childbirth” OR “labor” OR “birth-giving” OR “birth” OR “delivery” OR “deliver” OR “partus” OR “labor”). The search was limited to studies published in English or Chinese. Specific details of the retrieval strategy are shown in Supplementary material.
Studies that explicitly investigated or discussed psychological trauma following birth from the perspective of postpartum women were included in this concept analysis. The following studies would be excluded: (1) investigating the intervention effects of certain measures on psychological birth trauma; (2) examining physical birth trauma only; (3) only exploring psychological trauma of bystanders during the birthing process, primarily women’s partners and healthcare professionals; (4) only testing the reliability and validity of the scale. Furthermore, to improve the precision of the concept of psychological birth trauma, we excluded studies that aimed to explore postpartum PTSD and its similar themes, including postpartum post-traumatic stress symptoms and post-traumatic stress. Studies on broader topics such as negative birth experiences were also excluded.
3. Results
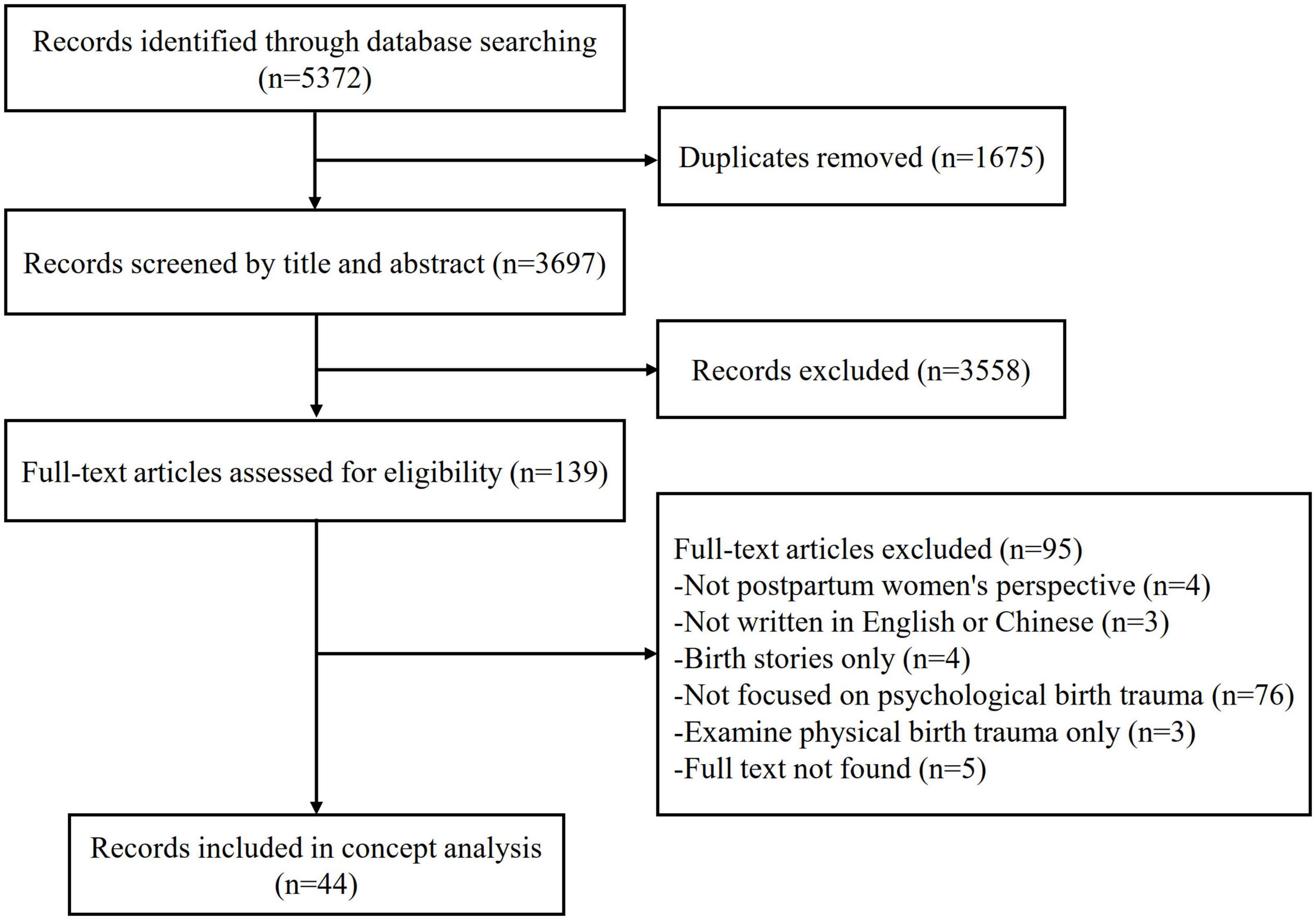
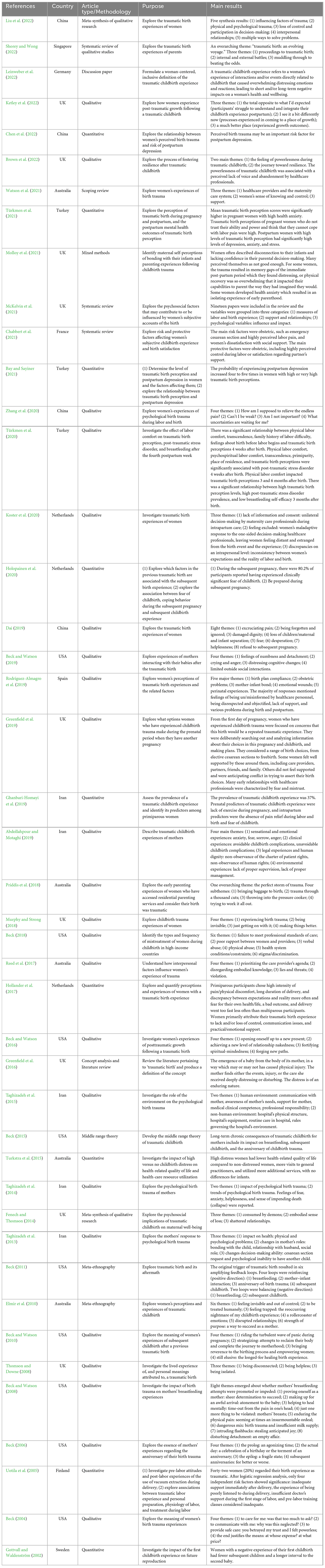
A total of 5,372 studies were identified, then 1,675 duplicated studies were excluded. After screening the titles and abstracts of the remaining studies, 3,558 studies were further excluded. After reading the full texts of 139 studies, 95 studies were excluded for a variety of reasons. Finally, a total of 44 studies were included in the concept analysis. The search process is presented in Figure 1. The specific characteristics of the included studies are presented in Table 2. The years of publication ranged from 2002 to 2022. Of the 44 studies, 10 were from the USA, nine from the UK, five from Iran, four from China, four from Australia, three from the Netherlands, three from Turkey, and one from each of the following countries: Sweden, Singapore, Germany, France, Spain, and Finland. In terms of article type, qualitative studies (n = 25) were the most, followed by quantitative studies (n = 9), and the remaining included systematic reviews (n = 5), mixed methods study (n = 1), scope review (n = 1), concept analysis (n = 1), discussion paper (n = 1), and middle range theory (n = 1).
3.1. Uses of the concept
Walker and Avant’s (2019) method involves identifying defining attributes used to describe the concept. This means that as many concept examples as possible need to be evaluated, and repeated features need to be recorded (Walker and Avant, 2019). Results of the literature showed that earlier birth trauma almost exclusively refers to maternal or neonatal physical trauma during birth, i.e., tissue and organ damage, such as maternal damaged pelvic floor function, neonatal cephalohematoma, clavicular fracture, and brachial plexus injury (Perlow et al., 1996; Meyer et al., 2000). The term further covers the long-term adverse effects of neonatal brain or skull injuries, which are usually presented in cognition (Geirsson, 1988). With the deepening of research, there is increasing evidence that childbirth can cause not only physical trauma but also psychological disturbances (Pantlen and Rohde, 2001). Professor Beck defined birth trauma in 2004 as an event that occurs during the labor and delivery process involving actual or threatened serious injury or death to the mother or her baby, in which women experience intense feelings of fear, helplessness, loss of control, and horror (Beck, 2004). This definition emphasizes the psychological experience of birth. In 2015, professor Beck integrated a series of studies on the topic of birth trauma into a whole, thereby establishing a higher and more abstract middle range theory of birth trauma, in which he clearly proposed that birth trauma can be both psychological and physical (Beck, 2015). Greenfield et al. (2016) conducted a concept analysis of traumatic birth, stating that the term can be defined as: the emergence of a baby from the mother in a way that involves events or care that cause psychological disturbance or deep distress, which may or may not involve physical injury, but leading to enduring psychological distress. A recent discussion paper developed an inclusive and woman-centered definition of the traumatic childbirth experience, which refers to a woman’s experience of interactions and/or events directly related to childbirth that caused overwhelming distressing emotions and reactions; leading to short and/or long-term negative impacts on a woman’s health and wellbeing (Leinweber et al., 2022). Apart from the three definitions above, there is no further conceptual or operational understanding.
3.2. Defining attributes
Defining attributes can be used to identify, understand, and differentiate a concept from other concepts (Walker and Avant, 2019). Analysis of the literature led to the identification of the most common features related to psychological birth trauma. After identifying these features, it was possible to identify key defining attributes. Thus, the attributes of psychological birth trauma are summarized as follows:
(1) Women’s subjective feelings
(2) Intertwined painful emotional experiences
(3) Originate in the birth process
(4) Last until postpartum.
3.2.1. Women’s subjective feeling
Women’s perception of psychological birth trauma is highly subjective (Taghizadeh et al., 2014). Each birth experience is unique to every woman, indeed, even the same events that occur during birth are perceived differently by every woman (Shorey and Wong, 2022). Studies showed that childbirth that appears normal and straightforward to healthcare professionals and is medically uneventful can be perceived as traumatic by the woman (Holopainen et al., 2020; Leinweber et al., 2022). Conversely, not all women with complications will have traumatic experiences (Leinweber et al., 2022). Notably, many studies used self-perceived psychological trauma during birth as the criteria for the recruitment and selection of research subjects (Thomson and Downe, 2008; Beck and Watson, 2019; Dai, 2019; Zhang et al., 2020). In conclusion, psychological birth trauma emphasizes the subjective feeling of women rather than objective aspects of the birth process.
3.2.2. Intertwined painful emotional experiences
3.2.2.1. Fear and anxiety
Faced with an unfamiliar environment and care providers, as well as an unknown birth process, women don’t know if an event will occur that threatens their own or their baby’s safety, which makes them fearful and anxious (Taghizadeh et al., 2014; Hollander et al., 2017; Dai, 2019; Holopainen et al., 2020; Zhang et al., 2020; Shorey and Wong, 2022).
3.2.2.2. Helplessness and despair
During birth, women have to bear severe labor pain and face all the actual or potential risks, they do not know what to do, and the cruel reality makes them feel helpless or even despairing (Beck, 2004; Thomson and Downe, 2008; Taghizadeh et al., 2014; Dai, 2019; Zhang et al., 2020).
3.2.2.3. Deprivation of dignity
Women feel verbally and physically abused and discriminated against by care providers and their privacy is violated, which deprives them of their dignity (Beck, 2015, 2018; Taghizadeh et al., 2015; Reed et al., 2017; Abdollahpour and Motaghi, 2019; Dai, 2019; Holopainen et al., 2020; Chabbert et al., 2021; Shorey and Wong, 2022).
3.2.2.4. Neglected and abandoned
Women feel that they are not receiving adequate communication, explanation, emotional and practical support, and attention, they lose the power to express their thoughts and feelings as if they are a machine rather than a human, which makes them feel neglected and abandoned (Beck, 2004, 2015, 2018; Uotila et al., 2005; Elmir et al., 2010; Hollander et al., 2017; Murphy and Strong, 2018; Priddis et al., 2018; Abdollahpour and Motaghi, 2019; Dai, 2019; Rodríguez-Almagro et al., 2019; Holopainen et al., 2020; Koster et al., 2020; Zhang et al., 2020; Chabbert et al., 2021).
3.2.2.5. Loss of control
Women feel deprived of decision-making and informed consent, their birth process is completely in the hands of care providers, and reality is not moving toward their expectations, which makes them feel out of control (Beck, 2004, 2015; Elmir et al., 2010; Taghizadeh et al., 2015; Hollander et al., 2017; Abdollahpour and Motaghi, 2019; Holopainen et al., 2020; Koster et al., 2020; Zhang et al., 2020; Chabbert et al., 2021; Watson et al., 2021; Liu et al., 2022).
3.2.3. Originate in the birth process
Childbirth is a complex process involving medical acts and during which events that endanger the safety of the mother and baby may occur, which can be traumatic for women, especially when they believe that these events could have been avoided (Leinweber et al., 2022). In addition, the quality of women’s interactions with healthcare professionals during birth was highlighted as a major factor influencing women’s feelings about childbirth, as women used emotional language to describe their negative interaction experiences, including feeling like they were at the “bottom of the hierarch,” “persecuted,” etc. (Greenfield et al., 2019; Leinweber et al., 2022). Furthermore, psychological birth trauma may stem from events that occurred during birth that triggered women’s traumatic memories, such as sexual abuse (Watson et al., 2021).
3.2.4. Last until postpartum
Persistence is a key attribute of psychological birth trauma (Greenfield et al., 2016). However, it is not entirely clear how long it lasts postpartum. In fact, many studies investigated the prevalence or effects of psychological birth trauma at 5 days (Uotila et al., 2005), 3–6 weeks (Türkmen et al., 2021), 1 month (Bay and Sayiner, 2021), and 1–4 months postpartum (Ghanbari-Homayi et al., 2019), etc., while only a few studies conducted longitudinal surveys (Türkmen et al., 2020). One study investigated the incidence of psychological birth trauma at 4 weeks, 3 months, and 6 months postpartum, unfortunately, there was no further longitudinal extension (Türkmen et al., 2020). Studies have vividly described the horrific torment of birth anniversaries that women experienced at least once (Beck, 2006, 2011, 2015). One study reported that women were formally diagnosed with postpartum PTSD 5 months to 19 years after experiencing psychological birth trauma (Beck and Watson, 2016). And even without being diagnosed with PTSD, these women are still tormented by ghosts from psychological birth trauma (Fenech and Thomson, 2014). It was indicated that there are women who still define the birth experience as psychologically traumatic even 32 years after giving birth (Taghizadeh et al., 2015).
3.3. Model case
A model case is designed to demonstrate all defining attributes of the concept (Walker and Avant, 2019). The model case in this study was adapted from a qualitative study aimed at investigating women’s experiences of psychological birth trauma (Beck, 2004).
Mrs. M has been having regular uterine contractions for over 5 h. A midwife asked Mrs. M to take off the pants and she would do a vaginal examination to determine the extent of cervical dilation. At this time, several students suddenly entered the room. Mrs. M tried to cover her bottom with her gown, but a midwife took her hand away from the gown. The students also performed vaginal examinations without Mrs. M’s permission, and no explanation was given afterward. Mrs. M immediately recalled the scene of being sexually assaulted when she was a child. She felt that she had been raped again, which brought her overwhelming pain. Everything seemed to be normal during the whole birth process, and finally, Mrs. M gave birth to the baby successfully, which made the midwife satisfied. All the family members surrounded the baby, leaving Mrs. M in bed alone, no one asked how she was feeling. In the days that followed, Mrs. M still felt very distressed. She was reluctant to interact with her husband and baby, refused to breastfeed, and did not trust medical staff. When the child was 3 years old, Mrs. M became pregnant again. During the pregnancy, she was surrounded by fear that this birth would repeat the previous one, and she visited a psychotherapist several times.
3.4. Borderline case
The authors constructed the borderline case to provide an example that embraces most of the attributes of psychological birth trauma. Mrs. N longed for a vaginal delivery and believed she could do it. Unfortunately, signs of fetal distress appeared at the beginning of the first stage of labor. Doctors told her that the prolonged labor process was dangerous to the fetus and that a cesarean section was needed as soon as possible. Mrs. N had never thought about a cesarean section, she was very scared. The doctor and midwife patiently explained to her again and gave her support and encouragement, which made Mrs. N relax. Subsequently, Mrs. N underwent an emergency cesarean section, and both mother and baby were safe. Although failed to achieve delivery vaginally as expected, Mrs. N was satisfied with the outcomes. When looking back on her birth experience, she feels supported by the healthcare providers and that she was doing the right thing.
3.5. Antecedents
Antecedents are those events or incidents that must occur before or be in place prior to the occurrence of the concept (Walker and Avant, 2019). Hence, in this concept analysis, antecedents refer to the precursive elements of psychological birth trauma. After reviewing the literature, considering the complexity of psychological birth trauma, antecedents are grouped according to either pre-existing or birth-related antecedents. Pre-existing antecedents refer to factors that exist prior to childbirth. These mainly include women’s demographic characteristics, personality traits, and medical and traumatic experiences. Specifically, demographic characteristics include single (Chabbert et al., 2021), low income (Bay and Sayiner, 2021), primipara (Türkmen et al., 2020; Chabbert et al., 2021), and living in the city center (Türkmen et al., 2020). Personality traits encompass insecure attachment style (Chabbert et al., 2021), high health anxiety (Türkmen et al., 2021), fear of childbirth (Ghanbari-Homayi et al., 2019; Chabbert et al., 2021), and disbelief in one’s ability to cope with labor pain (Türkmen et al., 2021). Medical and traumatic experiences encompass a history of sexual trauma (Chabbert et al., 2021), previous mental or physical health problems (Priddis et al., 2018), existing symptoms of depression or anxiety (Chabbert et al., 2021), fertility or complex pregnancy issues (Priddis et al., 2018) and a family history of labor difficulty (Türkmen et al., 2020). Furthermore, several studies reported unplanned pregnancy (Bay and Sayiner, 2021), insufficient prenatal care and training (Uotila et al., 2005; Bay and Sayiner, 2021; Chabbert et al., 2021), society stereotyped pressure on motherhood (Zhang et al., 2020), and lack of exercise during pregnancy (Ghanbari-Homayi et al., 2019) are related to psychological birth trauma.
Birth-related antecedents are key contributors to the occurrence of psychological birth trauma. These include obstetric factors and factors related to healthcare professionals. Specifically, obstetric factors encompass severe pain or physical discomfort (Uotila et al., 2005; Hollander et al., 2017; Murphy and Strong, 2018; Abdollahpour and Motaghi, 2019; Dai, 2019; Zhang et al., 2020; Chabbert et al., 2021), long duration of labor (Hollander et al., 2017; Holopainen et al., 2020; Chabbert et al., 2021), too rapid birth process (Hollander et al., 2017; Holopainen et al., 2020), unnecessary medical intervention (Reed et al., 2017; Priddis et al., 2018; Watson et al., 2021), physical restraint during birth (Shorey and Wong, 2022), cesarean section (Bay and Sayiner, 2021) or emergency cesarean section (Rodríguez-Almagro et al., 2019; Chabbert et al., 2021; Shorey and Wong, 2022), instrumental vaginal delivery (Priddis et al., 2018; Rodríguez-Almagro et al., 2019; Chabbert et al., 2021; Shorey and Wong, 2022), separation from the baby (Priddis et al., 2018; Abdollahpour and Motaghi, 2019; Dai, 2019), medical complications in infant (Holopainen et al., 2020; Liu et al., 2022) or mother (Priddis et al., 2018; Holopainen et al., 2020; Chabbert et al., 2021), dissatisfied neonatal gender (Zhang et al., 2020), preterm delivery (Chabbert et al., 2021), neonatal admission to neonatal intensive care unit (Priddis et al., 2018; Chabbert et al., 2021), neonatal death (Murphy and Strong, 2018; Dai, 2019), partner’s absence and lack of support (Holopainen et al., 2020; Chabbert et al., 2021), unpleasant birthing physical environment, equipment and rules (Taghizadeh et al., 2015; Beck, 2018; Abdollahpour and Motaghi, 2019; Watson et al., 2021; Liu et al., 2022; Shorey and Wong, 2022), and tense atmosphere during birth (Zhang et al., 2020). As for factors associated with healthcare professionals, studies have documented that the following factors are linked to psychological birth trauma: poor communication and explanation (Taghizadeh et al., 2015; Hollander et al., 2017; Beck, 2018; Priddis et al., 2018; Chabbert et al., 2021; Watson et al., 2021; Liu et al., 2022; Shorey and Wong, 2022), insufficient medical clinical competence (Taghizadeh et al., 2015; Abdollahpour and Motaghi, 2019; Rodríguez-Almagro et al., 2019), negative attitudes and words (Priddis et al., 2018), using mothers as learning resources for hospital staff (Reed et al., 2017; Watson et al., 2021), and prioritizing work agendas rather than the thoughts of women in childbirth (Reed et al., 2017; Watson et al., 2021).
3.6. Consequences
Consequences are those events or incidents that appear as results of the concept (Walker and Avant, 2019). Thus, in this concept analysis, consequences refer to the negative or positive effects of psychological birth trauma on women’s well-being. Firstly, there is a definite relationship between psychological birth trauma and consequences that directly affect the mental health of the mother. Following the psychological birth trauma, mothers experience heightened levels of panic, grief, anger, anxiety (Elmir et al., 2010; Fenech and Thomson, 2014), and even suicidal thoughts (Elmir et al., 2010). They are trapped in memories of the traumatic birth (Elmir et al., 2010; Shorey and Wong, 2022) and bombarded with flashbacks and nightmares (Elmir et al., 2010; Fenech and Thomson, 2014). These symptoms can last for years (Fenech and Thomson, 2014). A study described in detail their painful experiences during the subsequent birth anniversary (Beck, 2006). Additionally, these women are more likely to suffer from postpartum depression (Taghizadeh et al., 2013; Bay and Sayiner, 2021; McKelvin et al., 2021; Türkmen et al., 2021; Chen et al., 2022), anxiety (Taghizadeh et al., 2013; McKelvin et al., 2021; Türkmen et al., 2021), PTSD (Taghizadeh et al., 2013; Türkmen et al., 2020; McKelvin et al., 2021), and even psychosis (Taghizadeh et al., 2013).
Secondly, psychological birth trauma leads to changes in the mother’s roles. Several studies reported negative mother-infant interactions, with women expressing feelings of disengagement or feeble attachment to their children (Beck, 2011; Taghizadeh et al., 2013; Fenech and Thomson, 2014; Molloy et al., 2021), and feelings of incompetence as mothers (Taghizadeh et al., 2013; Fenech and Thomson, 2014; Priddis et al., 2018; Molloy et al., 2021), such as low breastfeeding self-efficacy (Türkmen et al., 2020). Mothers may experience excessive fear and anxiety about the health of their children (Molloy et al., 2021). While others described the overprotection of their children (Fenech and Thomson, 2014). Some studies reported that women experience distress while breastfeeding and therefore refuse to continue (Beck and Watson, 2008; Taghizadeh et al., 2013). Other mothers, however, insist on breastfeeding to prove that they are a mother, to help their spiritual recovery, or to atone for the baby (Beck and Watson, 2008). In addition, several studies suggested that psychological birth trauma can lead to difficulties or disruptions in couples’ emotional and sexual relationships (Taghizadeh et al., 2013; Fenech and Thomson, 2014). Moreover, some mothers display social conflicts, such as blame and aggression toward others (Taghizadeh et al., 2013; Fenech and Thomson, 2014; Watson et al., 2021), distrust and anger toward healthcare professionals (Fenech and Thomson, 2014), and a preference to remain shy and isolated (Taghizadeh et al., 2013; Fenech and Thomson, 2014).
Thirdly, psychological birth trauma affects the subsequent reproductive decisions, experiences, and coping behaviors. Women who have experienced psychological birth trauma are often fearful of future pregnancies (Fenech and Thomson, 2014; Greenfield et al., 2019; Holopainen et al., 2020; McKelvin et al., 2021), and some refuse to be pregnant again (Taghizadeh et al., 2013; Fenech and Thomson, 2014; Dai, 2019). In fact, findings suggested that women with psychological birth trauma have fewer subsequent children, as well as a longer interval to their second child (Gottvall and Waldenström, 2002). Additionally, some women who become pregnant again are surrounded by fearful thoughts that subsequent childbirth will be a repeated traumatic experience (Beck and Watson, 2010; Taghizadeh et al., 2013; Greenfield et al., 2019). And, they tend to choose a planned cesarean section (Greenfield et al., 2019; Holopainen et al., 2020), a home delivery (Holopainen et al., 2020), or a freebirth (Greenfield et al., 2019).
Fourthly, psychological birth trauma leads to more health services utilization. Women with psychological birth trauma have longer postpartum hospital stays (Turkstra et al., 2015). In addition, studies showed that they have more general practitioner visits and additional services utilization, such as psychological treatment, lactation support, child health clinic visits, and midwife home visits (Turkstra et al., 2015).
While most of the consequences of psychological birth trauma found in the literature are negative, it can also have positive outcomes. One study explored how women who have experienced psychological birth trauma rely on external and internal resources to move toward resilience (Brown et al., 2022). Moreover, several studies confirmed post-traumatic growth following psychological birth trauma (Beck and Watson, 2016; Ketley et al., 2022), including increased self-confidence and pride (Beck and Watson, 2016; Ketley et al., 2022), better relationship with partners, friends, children, and others (Beck and Watson, 2016; Ketley et al., 2022), stronger faith and a better understanding of spiritual and religious matters (Beck and Watson, 2016). Some women also established new professional and personal goals, such as completing a university degree (Beck and Watson, 2016), and actively participating in volunteer work aimed at preventing other women from psychological birth trauma (Beck and Watson, 2016; Ketley et al., 2022).
3.7. Empirical referents
According to Walker and Avant’s (2019) concept analysis method, the final step is to determine empirical referents of psychological birth trauma, which permits us to know how to measure or identify the defining attributes of a concept.
The Traumatic Childbirth Perception Scale (STCP) (Türkmen et al., 2021) was developed by Yalnız et al. (2016) as a self-report scale to assess women’s perception of traumatic childbirth. The STCP contains information on physical, emotional, and mental trauma associated with childbirth. It includes 13 items. Each item is scored between 0 (positive) and 10 (negative), and the total scale score ranges between 0 and 130. The total mean scores of 0–26, 27–52, 53–78, 79–104, and 105–130 correspond to very low, low, moderate, high, and very high levels of traumatic childbirth perception, respectively. In the study of Yalnız et al. (2016), the Cronbach’s alpha internal consistency coefficient of STCP was 0.895.
The Psychological Birth Trauma Questionnaire (QPBT) (Hajarian Abhari et al., 2022) was developed by Taghizadeh et al. (2013) to assess the level of psychological birth trauma. It includes 30 items and five constructs, namely: anxiety and eternal suffering of birth/labor, psychological manifestations, helplessness, collapse and sensation of death, and somatic manifestations. Each item is scored from 1 to 5 points, with a total score of 30–150 points. A higher score indicates a higher level of psychological birth trauma. The validity and reliability of QPBT have been confirmed in the study by Taghizadeh et al. (2013), the Cronbach’s alpha internal consistency coefficient was 0.949.
Notably, these two scales have not been used in studies in other countries, their English versions have not been identified yet.
3.8. Definition of the concept
Based on an analysis of the literature, the concept of psychological birth trauma is clearly defined as follows:
Psychological birth trauma refers to the woman’s subjective feeling caused by events directly or indirectly related to childbirth, which is manifested as intertwined painful emotional experiences that originate in the birth process and last until postpartum. It has a wide range of negative and, in some cases, positive effects on women. The conceptual model including the antecedents, attributes, and consequences of psychological birth trauma is shown in Figure 2.
4. Discussion
Based on a systematic search of the literature and the method of Walker and Avant (2019), we provided a comprehensive analysis of the concept of psychological birth trauma. Four defining attributes were identified: women’s subjective feelings; intertwined painful emotional experiences; originate in the birth process and last until postpartum. Currently, maternal and neonatal safety is often regarded as the bottom line for successful and satisfying childbirth (Beck, 2004), while the subjective feeling of the mother appears to be ignored. It is worth highlighting whether women in childbirth are experiencing intertwined painful emotional experiences. Additionally, researchers and healthcare professionals should be aware that a proportion of women who have experienced psychological birth trauma are concerned by being diagnosed with postpartum PTSD, while more women who do not meet the diagnostic threshold are still in “dire straits.” Therefore, it is time to raise awareness of psychological birth trauma. Specifically, psychological birth trauma should be considered as a separate postpartum mental health problem.
Antecedents in this concept analysis suggest that women in childbirth are vulnerable to a range of pre-existing factors that may contribute to psychological trauma. Identification of these factors, including demographic characteristics, personality traits, and medical and trauma experiences can help healthcare professionals to be more vigilant and thus aid in prevention. However, the prevention of birth-related antecedents appears to be more promising. The first is to emphasize professional management of labor, such as avoiding unnecessary medical intervention, adequately relieving labor pain, and improving medical clinical competence to reduce maternal and neonatal complications. In addition, obstetric management should aim to reduce psychological birth trauma, including creating a comfortable environment and allowing the woman’s partner to accompany her during birth, etc. Furthermore, it is imperative to improve the quality of women’s interactions with healthcare professionals during birth, which may be achieved by adequately communicating and explaining what happens, listening to women, and seeking to meet their expectations. Notably, further studies are needed to systematically assess these antecedents and to determine their magnitude and interrelationships.
After examining the consequences of included studies, this concept analysis identified the profound negative effects of psychological birth trauma on women, including poor mental health, poor role of the mother, subsequent reproductive challenges, and increased health services utilization. Therefore, early identification and intervention of these women is crucial. In terms of identification, during the postpartum hospital stay, healthcare professionals are advised to be wary of symptoms that may indicate a woman has suffered psychological birth trauma, such as a dazed appearance, withdrawal, temporary amnesia, and detachment from the baby (Church and Scanlan, 2002; Beck and Watson, 2008). If a mother has experienced complex childbirth, such as maternal and neonatal complications, she should be alerted to any psychological trauma as well (Hayden, 2022). Before discharge, healthcare professionals should proactively discuss with mothers whether they perceive their childbirth to be traumatic (Beck and Watson, 2008), as new mothers may not voluntarily express their feelings about the birth experience for fear that doctors will judge their parenting or involve social services (Hayden, 2022). Try asking open-ended questions to get more information about what women might be saying (Hayden, 2022). Beck and Watson (2016) and Beck et al. (2018) recommend that healthcare professionals be wary of the metaphors women use to help describe their experiences of post-traumatic stress. In addition, at infants’ well-baby checkups and yearly physical exams, healthcare professionals are recommended to ask mothers how they are doing and how they evaluate their birth experiences (Beck, 2015). Pediatric clinicians may be in an ideal position to identify women with elevated posttraumatic stress symptoms and to make those critical referrals for mental health care (Beck, 2015).
Furthermore, a limited number of studies have discussed interventions to reduce the negative effects of psychological birth trauma. A recent systematic review examined interventions to prevent women with recent traumatic birth from developing postpartum PTSD, including debriefing, encouraging skin-to-skin contact with healthy babies directly postpartum, structured psychological interventions, expressive writing, and seeing or holding the baby after stillbirth (de Graaff et al., 2018). The results showed that there was great heterogeneity in the study characteristics, and the effectiveness of interventions was different. Possible effective interventions were encouraging skin-to-skin contact with healthy babies directly postpartum, structured psychological interventions, and expressive writing, but the evidence was insufficient (de Graaff et al., 2018). A discussion article detailed how to use an emotion-focused approach to prevent psychological birth trauma (Gökçe İsbir et al., 2022). However, this approach has not yet been applied in clinical practice. A recent study (Hajarian Abhari et al., 2022) supported the effectiveness of counseling based on Gamble’s approach, originally proposed by Gamble et al. (2005), in preventing psychological birth trauma in primiparas. The counseling approach is cost-effective, easy to implement, and can be implemented by midwives, thus it could be valuable to integrate it into healthcare programs. However, due to the huge differences among existing interventions, we cannot make wise recommendations on specific implementation programs. However, some considerations seem to be meaningful. Firstly, it is necessary to strengthen the knowledge and skills training of the interveners, which is the premise to ensure the effectiveness of the intervention. Secondly, the content, duration, frequency and timing of intervention are the key factors affecting the effectiveness, and further studies are needed to determine the optimal programs. Finally, women’s personal preferences should also be considered. Notably, the effectiveness of these interventions is mainly focused on the mental health status of women. Future studies should also examine the effectiveness of interventions on other negative effects of psychological birth trauma, such as mother-infant and marital relationships.
Reassuringly, this concept analysis found that while some women experienced some negative effects of psychological birth trauma, they gained some positive aspects that had not been mentioned in previous related concepts. Studies showed that some mothers who have experienced psychological birth trauma build resilience by using both external resources (such as faith and supportive relationships) and internal resources (such as recognizing the power of their own motherhood) (Brown et al., 2022). And, some women are able to use their inner resources to develop the resilience they need as mothers, which empowers them and allows them to experience post-traumatic growth such as an increased sense of self-worth and competence (Brown et al., 2022; Ketley et al., 2022). Thus, healthcare professionals may play an important role in facilitating this by encouraging mothers to explore their faith and use their social support networks, and informing mothers about organizations and resources that provide niche support after traumatic birth (Brown et al., 2022). In addition, healthcare professionals can provide some hope to women who have experienced psychological birth trauma by sharing the possibility of post-traumatic growth (Beck and Watson, 2016; Beck et al., 2018). Notably, the possibility of positive effects does not diminish the importance of preventing psychological birth trauma (Ketley et al., 2022).
5. Limitations
Some limitations exist in this concept analysis. Firstly, studies were limited to English or Chinese, which restricts the scope of the review. Secondly, the studies included in this concept analysis were mostly qualitative, and quantitative studies were lacking due to the lack of widely validated tools for assessing psychological birth trauma. Thirdly, we excluded studies on postpartum PTSD, postpartum post-traumatic stress symptoms, postpartum post-traumatic stress, and negative birth experiences, which may contain content related to psychological birth trauma. Finally, we excluded studies that explored the feelings of bystanders (especially healthcare professionals and women’s partners) who may also experience psychological trauma as a result of witnessing the birth process. We, therefore, recognize that this definition may be subject to further development and adjustment.
6. Conclusion
This concept analysis provides a comprehensive insight into psychological birth trauma, which is a more complex and comprehensive phenomenon than previously thought and should be considered as a separate postpartum mental health problem. Given the high incidence and far-reaching effects of psychological birth trauma, its prevention, identification and intervention are crucial, but relevant studies are insufficient and need to be further explored. This study provides a starting point for future theory and research, and provides researchers and healthcare professionals with information that can serve as the foundation for assisting in the identification of psychological birth trauma, and as the reference for developing rigorous assessment tools as well as designing appropriate interventions. In addition, further research is needed to expand the definition of psychological birth trauma from the perspective of bystanders during birth. We expect that this concept will continue to be updated and refined as knowledge on the subject develops.
Author contributions
XS, XF, SC, RW, LS, HX, JH, ZZ, and AZ designed the study, critically revised the manuscript, and approved the final version. XS and XF conducted the literature retrieval, literature selection, data extraction, data analysis, and drafted the manuscript. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China Youth Program (grant number: 72204123) and the Nanjing Health Science and Technology Development Special Fund Project (grant number: YKK21162).
Acknowledgments
We acknowledge the support of the National Natural Science Foundation of China and the Nanjing Health Commission.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2022.1065612/full#supplementary-material
References
Abdollahpour, S., and Motaghi, Z. (2019). Lived traumatic childbirth experiences of newly delivered mothers admitted to the postpartum ward: A phenomenological study. J. Caring Sci. 8, 23–31. doi: 10.15171/jcs.2019.004
American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders, 4th Edn. Washington, DC: American Psychiatric Pub.
Bay, F., and Sayiner, F. D. (2021). Perception of traumatic childbirth of women and its relationship with postpartum depression. Women Health 61, 479–489. doi: 10.1080/03630242.2021.1927287
Beck, C. T. (2004). Birth trauma: In the eye of the beholder. Nurs. Res. 53, 28–35. doi: 10.1097/00006199-200401000-00005
Beck, C. T. (2006). The anniversary of birth trauma: Failure to rescue. Nurs. Res. 55, 381–390. doi: 10.1097/00006199-200611000-00002
Beck, C. T. (2011). A metaethnography of traumatic childbirth and its aftermath: Amplifying causal looping. Qual. Health Res. 21, 301–311.
Beck, C. T. (2015). Middle range theory of traumatic childbirth: The ever-widening ripple effect. Glob. Qual. Nurs. Res. 2:2333393615575313. doi: 10.1177/2333393615575313
Beck, C. T. (2018). A secondary analysis of mistreatment of women during childbirth in health care facilities. J. Obstetr. Gynecol. Neonatal Nurs. 47, 94–104. doi: 10.1016/j.jogn.2016.08.015
Beck, C. T., and Watson, S. (2008). Impact of birth trauma on breast-feeding: A tale of two pathways. Nurs. Res. 57, 228–236. doi: 10.1097/01.NNR.0000313494.87282.90
Beck, C. T., and Watson, S. (2010). Subsequent childbirth after a previous traumatic birth. Nurs. Res. 59, 241–249. doi: 10.1097/NNR.0b013e3181e501fd
Beck, C. T., and Watson, S. (2016). Posttraumatic growth after birth trauma: “I was broken. MCN Am. J. Matern. Child Nurs. 41, 264–271. doi: 10.1097/NMC.0000000000000259
Beck, C. T., and Watson, S. (2019). Mothers’ experiences interacting with infants after traumatic childbirth. MCN Am. J. Matern. Child Nurs. 44, 338–344. doi: 10.1097/NMC.0000000000000565
Beck, C. T., Watson, S., and Gable, R. K. (2018). Traumatic childbirth and its aftermath: Is there anything positive? J. Perinat. Educ. 27, 175–184. doi: 10.1891/1058-1243.27.3.175
Brown, A., Nielsen, J. D. J., Russo, K., Ayers, S., and Webb, R. (2022). The journey towards resilience following a traumatic birth: A grounded theory. Midwifery 104:103204. doi: 10.1016/j.midw.2021.103204
Chabbert, M., Panagiotou, D., and Wendland, J. (2021). Predictive factors of women’s subjective perception of childbirth experience: A systematic review of the literature. J. Reprod. Infant Psychol. 39, 43–66. doi: 10.1080/02646838.2020.1748582
Chen, Y., Ismail, F., Xiong, Z., Li, M., Chen, I., Wen, S. W., et al. (2022). Association between perceived birth trauma and postpartum depression: A prospective cohort study in China. Int. J. Gynaecol. Obstetr. 157, 598–603. doi: 10.1002/ijgo.13845
Church, S., and Scanlan, M. (2002). Post-traumatic stress disorder after childbirth. Do midwives have a preventative role? Practis. Midwife 5, 10–13.
Dai, L. (2019). Research on the experience of birth trauma and its influencing factors. Ph.D. thesis. Wuhan: Huazhong University of Science and Technology.
de Graaff, L. F., Honig, A., van Pampus, M. G., and Stramrood, C. A. I. (2018). Preventing post-traumatic stress disorder following childbirth and traumatic birth experiences: A systematic review. Acta Obstetr. Gynecol. Scand. 97, 648–656. doi: 10.1111/aogs.13291
Elmir, R., Schmied, V., Wilkes, L., and Jackson, D. (2010). Women’s perceptions and experiences of a traumatic birth: A meta-ethnography. J. Adv. Nurs. 66, 2142–2153. doi: 10.1111/j.1365-2648.2010.05391.x
Fenech, G., and Thomson, G. (2014). Tormented by ghosts from their past’: A meta-synthesis to explore the psychosocial implications of a traumatic birth on maternal well-being. Midwifery 30, 185–193. doi: 10.1016/j.midw.2013.12.004
Fenech, G., and Thomson, G. (2015). Defence against trauma: Women’s use of defence mechanisms following childbirth-related trauma. J. Reprod. Infant Psychol. 33, 268–281. doi: 10.1080/02646838.2015.1030731
Gamble, J., Creedy, D., Moyle, W., Webster, J., McAllister, M., and Dickson, P. (2005). Effectiveness of a counseling intervention after a traumatic childbirth: A randomized controlled trial. Birth 32, 11–19. doi: 10.1111/j.0730-7659.2005.00340.x
Geirsson, R. T. (1988). Birth trauma and brain damage. Baillieres Clin. Obstetr. Gynaecol. 2, 195–212. doi: 10.1016/s0950-3552(88)80072-5
Ghanbari-Homayi, S., Fardiazar, Z., Meedya, S., Mohammad-Alizadeh-Charandabi, S., Asghari-Jafarabadi, M., Mohammadi, E., et al. (2019). Predictors of traumatic birth experience among a group of Iranian primipara women: A cross sectional study. BMC Pregnancy Childbirth 19:182. doi: 10.1186/s12884-019-2333-4
Gökçe İsbir, G., Yılmaz, M., and Thomson, G. (2022). Using an emotion-focused approach in preventing psychological birth trauma. Perspect. Psychiatr. Care 58, 1170–1176. doi: 10.1111/ppc.12867
Gottvall, K., and Waldenström, U. (2002). Does a traumatic birth experience have an impact on future reproduction? BJOG Int. J. Obstetr. Gynaecol. 109, 254–260. doi: 10.1111/j.1471-0528.2002.01200.x
Greenfield, M., Jomeen, J., and Glover, L. (2016). What is traumatic birth? A concept analysis and literature review. Br. J. Midwifery 24, 254–267. doi: 10.12968/bjom.2016.24.4.254
Greenfield, M., Jomeen, J., and Glover, L. (2019). “It can’t be like last time”–choices made in early pregnancy by women who have previously experienced a traumatic birth. Front. Psychol. 10:56. doi: 10.3389/fpsyg.2019.00056
Hajarian Abhari, Z., Karimi, F. Z., Taghizdeh, Z., Mazloum, S. R., and Asghari Nekah, S. M. (2022). Effects of counseling based on Gamble’s approach on psychological birth trauma in primiparous women: A randomized clinical trial. J. Matern. Fetal Neonatal Med. 35, 668–676. doi: 10.1080/14767058.2020.1730799
Hayden, E. (2022). It felt like my birth trauma had been forgotten. BMJ (Clin. Res. Ed.) 377:o1006. doi: 10.1136/bmj.o1006
Hollander, M., Hastenberg, E., Dillen, J., Pampus, M., Miranda, E., and Stramrood, C. (2017). Preventing traumatic childbirth experiences: 2192 women’s perceptions and views. Arch. Womens Mental Health 20, 515–523. doi: 10.1007/s00737-017-0729-6
Holopainen, A., Stramrood, C., van Pampus, M. G., Hollander, M., and Schuengel, C. (2020). Subsequent childbirth after previous traumatic birth experience: Women’s choices and evaluations. Br. J. Midwifery 28, 488–496. doi: 10.12968/bjom.2020.28.8.488
Ketley, R., Darwin, Z., Masterson, C., and McGowan, L. (2022). Women’s experience of post-traumatic growth following a traumatic birth: An interpretive phenomenological analysis. J. Reprod. Infant Psychol. 27, 1–12. doi: 10.1080/02646838.2022.2070608
Koster, D., Romijn, C., Sakko, E., Stam, C., Steenhuis, N., de Vries, D., et al. (2020). Traumatic childbirth experiences: Practice-based implications for maternity care professionals from the woman’s perspective. Scand. J. Caring Sci. 34, 792–799. doi: 10.1111/scs.12786
Leinweber, J., Fontein-Kuipers, Y., Thomson, G., Karlsdottir, S. I., Nilsson, C., Ekström-Bergström, A., et al. (2022). Developing a woman-centered, inclusive definition of traumatic childbirth experiences: A discussion paper. Birth 49, 687–696. doi: 10.1111/birt.12634
Liu, J., Qiao, J. H., Zhou, S. J., Lv, J., Liu, R. S., Wen, H., et al. (2022). Meta synthesis of qualitative research on women’s real experience of childbirth trauma. Chin. J. Modern Nurs. 28, 2–8. doi: 10.3760/cma.j.cn115682-20210813-03598
Mayopoulos, G. A., Ein-Dor, T., Dishy, G. A., Nandru, R., Chan, S. J., Hanley, L. E., et al. (2021). COVID-19 is associated with traumatic childbirth and subsequent mother-infant bonding problems. J. Affect. Disord. 282, 122–125. doi: 10.1016/j.jad.2020.12.101
McKelvin, G., Thomson, G., and Downe, S. (2021). The childbirth experience: A systematic review of predictors and outcomes. Women Birth 34, 407–416. doi: 10.1016/j.wombi.2020.09.021
Meyer, S., Hohlfeld, P., Achtari, C., Russolo, A., and De Grandi, P. (2000). Birth trauma: Short and long term effects of forceps delivery compared with spontaneous delivery on various pelvic floor parameters. BJOG 107, 1360–1365. doi: 10.1111/j.1471-0528.2000.tb11648.x
Molloy, E., Biggerstaff, D. L., and Sidebotham, P. (2021). A phenomenological exploration of parenting after birth trauma: Mothers perceptions of the first year. Women birth 34, 278–287. doi: 10.1016/j.wombi.2020.03.004
Murphy, H., and Strong, J. (2018). Just another ordinary bad birth? A narrative analysis of first time mothers’ traumatic birth experiences. Health Care Women Int. 39, 619–643. doi: 10.1080/07399332.2018.1442838
Oddo-Sommerfeld, S., Schermelleh-Engel, K., Konopka, M., La Rosa, V. L., Louwen, F., and Sommerlad, S. (2022). Giving birth alone due to COVID-19-related hospital restrictions compared to accompanied birth: Psychological distress in women with caesarean section or vaginal birth - a cross-sectional study. J. Perinat. Med. 50, 539–548. doi: 10.1515/jpm-2021-0368
Pantlen, A., and Rohde, A. (2001). Psychologic effects of traumatic live deliveries. Zentralbl. Gynakol. 123, 42–47. doi: 10.1055/s-2001-12025
Perlow, J. H., Wigton, T., Hart, J., Strassner, H. T., Nageotte, M. P., and Wolk, B. M. (1996). Birth trauma. A five-year review of incidence and associated perinatal factors. J. Reprod. Med. 41, 754–760.
Priddis, H. S., Keedle, H., and Dahlen, H. (2018). The perfect storm of trauma: The experiences of women who have experienced birth trauma and subsequently accessed residential parenting services in Australia. Women Birth 31, 17–24. doi: 10.1016/j.wombi.2017.06.007
Reed, R., Sharman, R., and Inglis, C. (2017). Women’s descriptions of childbirth trauma relating to care provider actions and interactions. BMC Pregnancy Childbirth 17:21. doi: 10.1186/s12884-016-1197-0
Rodríguez-Almagro, J., Hernández-Martínez, A., Rodríguez-Almagro, D., Quirós-García, J. M., Martínez-Galiano, J. M., and Gómez-Salgado, J. (2019). Women’s perceptions of living a traumatic childbirth experience and factors related to a birth experience. Int. J. Environ. Res. Public Health 16:1654. doi: 10.3390/ijerph16091654
Shorey, S., and Wong, P. Z. E. (2022). Traumatic childbirth experiences of new parents: A meta-synthesis. Trauma Violence Abuse 23, 748–763. doi: 10.1177/1524838020977161
Sommerlad, S., Schermelleh-Engel, K., La Rosa, V. L., Louwen, F., and Oddo-Sommerfeld, S. (2021). Trait anxiety and unplanned delivery mode enhance the risk for childbirth-related post-traumatic stress disorder symptoms in women with and without risk of preterm birth: A multi sample path analysis. PLoS One 16:e0256681. doi: 10.1371/journal.pone.0256681
Taghizadeh, Z., Arbabi, M., Kazemnejad, A., Irajpour, A., and Lopez, V. (2015). Iranian mothers’ perceptions of the impact of the environment on psychological birth trauma: A qualitative study. Int. J. Nurs. Pract. 21(Suppl. 2), 58–66. doi: 10.1111/ijn.12286
Taghizadeh, Z., Irajpour, A., and Arbabi, M. (2013). Mothers’ response to psychological birth trauma: A qualitative study. Iran. Red Crescent Med. J. 15:e10572. doi: 10.5812/ircmj.10572
Taghizadeh, Z., Irajpour, A., Nedjat, S., Arbabi, M., and Lopez, V. (2014). Iranian mothers’ perception of the psychological birth trauma: A qualitative study. Iran. J. Psychiatry 9, 31–36.
Thomson, G., and Downe, S. (2008). Widening the trauma discourse: The link between childbirth and experiences of abuse. J. Psychosom. Obstetr. Gynaecol. 29, 268–273. doi: 10.1080/01674820802545453
Thomson, G., Diop, M. Q., Stuijfzand, S., and Horsch, A. (2021). Policy, service, and training provision for women following a traumatic birth: An international knowledge mapping exercise. BMC Health Serv. Res. 21:1206. doi: 10.1186/s12913-021-07238-x
Türkmen, H., Yalniz Dilcen, H., and Akin, B. (2020). The effect of labor comfort on traumatic childbirth perception, post-traumatic stress disorder, and breastfeeding. Breastfeed. Med. 15, 779–788. doi: 10.1089/bfm.2020.0138
Türkmen, H., Yalniz Dilcen, H., and Ozcoban, F. A. (2021). Traumatic childbirth perception during pregnancy and the postpartum period and its postnatal mental health outcomes: A prospective longitudinal study. J. Reprod. Infant Psychol. 39, 422–434. doi: 10.1080/02646838.2020.1792429
Turkstra, E., Creedy, D. K., Fenwick, J., Buist, A., Scuffham, P. A., and Gamble, J. (2015). Health services utilization of women following a traumatic birth. Arch. Womens Mental Health 18, 829–832. doi: 10.1007/s00737-014-0495-7
Uotila, J. T., Taurio, K., Salmelin, R., and Kirkinen, P. (2005). Traumatic experience with vacuum extraction–influence of personal preparation, physiology, and treatment during labor. J. Perinat. Med. 33, 373–378. doi: 10.1515/jpm.2005.068
Walker, L. O., and Avant, K. C. (2019). Strategies for theory construction in nursing, 6th Edn. Upper Saddle River, NJ: Pearson.
Watson, K., White, C., Hall, H., and Hewitt, A. (2021). Women’s experiences of birth trauma: A scoping review. Women and Birth 34, 417–424.
Yalnız, H., Canan, F., Genç, R. E., Kuloğlu, M. M., and Gecici, Ö (2016). Development of a scale of traumatic childbirth perception. Turk. J. Med. Sci. 8, 81–88. doi: 10.5505/ttd.2016.40427
Yildiz, P. D., Ayers, S., and Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: A systematic review and meta-analysis. J. Affect. Disord. 208, 634–645. doi: 10.1016/j.jad.2016.10.009
Keywords: birth, psychological birth trauma, concept analysis, perinatal mental health, obstetric, psychological, trauma
Citation: Sun X, Fan X, Cong S, Wang R, Sha L, Xie H, Han J, Zhu Z and Zhang A (2023) Psychological birth trauma: A concept analysis. Front. Psychol. 13:1065612. doi: 10.3389/fpsyg.2022.1065612
Received: 10 October 2022; Accepted: 28 December 2022;
Published: 13 January 2023.
Edited by:
Dian Veronika Sakti Kaloeti, Diponegoro University, IndonesiaReviewed by:
Elena Commodari, University of Catania, ItalyConcetta Polizzi, University of Palermo, Italy
Copyright © 2023 Sun, Fan, Cong, Wang, Sha, Xie, Han, Zhu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhu Zhu,  enpfbmpmeUBzaW5hLmNvbQ==; Aixia Zhang,
enpfbmpmeUBzaW5hLmNvbQ==; Aixia Zhang,  emhhbmdhaXhpYUBuam11LmVkdS5jbg==
emhhbmdhaXhpYUBuam11LmVkdS5jbg==
†These authors have contributed equally to this work and share first authorship
 Xiaoqing Sun1†
Xiaoqing Sun1† Shengnan Cong
Shengnan Cong Zhu Zhu
Zhu Zhu Aixia Zhang
Aixia Zhang