
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 11 January 2023
Sec. Health Psychology
Volume 13 - 2022 | https://doi.org/10.3389/fpsyg.2022.1035458
 Xiaojun Deng1
Xiaojun Deng1 Huiting Zhang2*
Huiting Zhang2*The coronavirus disease-2019 (COVID-19) pandemic has brought huge and continuous damage to mental health. The mental health of non-medical college students after returning to school remains largely unknown and the influencing factors were awaited to be deciphered. This cross-sectional study was launched among 1,083 non-medical students in Zhanjiang city by means of online survey (WeChat App) from August 1st, 2022 to August 7th, 2022. Knowledge about COVID-19 and attitude toward COVID-19 were assessed by using 7-items and 5-items questionnaires, respectively. Sleep quality, anxiety and depression symptoms were evaluated by Pittsburgh sleep quality index (PSQI), Hamilton depression rating scale-17 (HDRS-17) and self-rating anxiety scale (SAS), respectively. The results showed that more than half of the participants were knowledgeable about COVID-19. The majority of the participants held positive attitude toward COVID-19. The data demonstrated that 6.8% students had poor sleep quality, and 1.86, 0.37 and 0.37% students had mild, moderate and severe anxiety, respectively. About 26.7, 4.7 and 1.7% students had minimal, mild–moderate and severe depression. Female students showed higher proportions of anxiety (p = 0.02) and depression (p < 0.0001) than male students. Students with monthly household income below 3,000 RMB were more vulnerable to anxiety (p = 0.017) and depression (p = 0.004). Correlation analysis and Multivariate logistic regression analysis results showed that lower grade was positively related with anxiety and depression. Female students, income lower than 3,000 RMB/month, poor knowledge about COVID-19 and negative attitude toward COVID-19 were associated with insomnia, anxiety and depression. This study indicated that during the COVID-19 pandemic, a majority of non-medical students returning to school remained good sleep quality and a small number of students suffered from depression and anxiety. To our knowledge, this is a novel study revealing the mental health of non-medical college students concerning COVID-19 in Zhanjiang.
2019 coronavirus disease (COVID-19) was first reported in Wuhan, China in December 2019. COVID-19 was an infectious disease which mainly transmitted through respiratory droplets and direct contact. As of October 15th, 2021, a total of more than 239.4 million person diagnosed with COVID-19 and 4.8 million died of this life-threatening infectious disease (Zheng et al., 2022). Apart from the negative influences of COVID-19 pandemic on physical health, it also causes continuous impacts on mental health including depression and anxiety among individuals (Cao et al., 2020; Wang et al., 2020).
Several retrospective studies have suggested that infection was closely related with subsequent mood deterioration, including depression (Gunaratne et al., 2013; Rahim et al., 2022; Shokri et al., 2022). College students appear to be particularly susceptible to experiencing mental disorder and their mental state is a key concern during the pandemic (Wang X. et al., 2020). With social restriction during COVID-19, factors like decreased physical activity, prolonged sedentary behavior and poor dietary behaviors might put mental health at greater risk (Rahim et al., 2022; Sheedy O’Sullivan et al., 2022). Mental health problems would influence students’ academic performance, overall quality of life, increase suicidal ideation and suicidal behavior (Gao et al., 2022; Zhao et al., 2022). It is of great importance to pay attention to the mental health of college students. Increased incidence of mental health problems experienced by college students have been shown in various countries, including China, France, Iran and America (Lin et al., 2020; Husky et al., 2021; Oh et al., 2021; Abdolkarimi et al., 2022). In the early stage of the COVID-19 outbreak, there are 15.4–24.9% Chinese university students suffered from anxiety (Cao et al., 2020; Wang and Zhao, 2020). Another study revealed that about two-thirds of the 549 medical students experienced anxiety, depression, insomnia and distress (Essangri et al., 2021). Mental illness secondary to the infectious diseases was associated with the restriction of social activities, feelings of loneliness and inferior knowledge about the diseases (Wang et al., 2020b, 2021). After 2 years of suffering from COVID-19 epidemic, most cities in China and other countries have achieved great success in controlling COVID-19 and many students were allowed to return to school. To be note, severe acute respiratory syndrome (SARS) outbreak in 2003 and other previous pandemics have been shown to have long-term effects on mental health (Zhuo et al., 2021). The current COVID-19 pandemic might also have persistent psychological impact on college students. Several studies have devoted attention to the changes in college students’ mental health before and amidst the pandemic, while the findings yielded from these studies were controversial (Elmer et al., 2020; Wang et al., 2020b; Amendola et al., 2021). These preliminary studies motivated us to further investigate the mental health of college students under the control of the pandemic. Non-medical college students have lower understanding of COVID-19 than medical staff and medical students, making them more vulnerable to mental health issues (Lasheras et al., 2020). The mental health status among non-medical college students after returning to school remains largely unclear and the influencing factors were awaited to be explored. Large-scale studies are needed to better understand the impact of COVID-19 and associated factors on the mental health of non-medical college students, and to develop effective intervention strategies.
The aim of this study was to evaluate the mental health status among non-medical college students returning to school during the COVID-19 pandemic in Zhanjiang city. Hopefully, this study could contribute to understanding the mental health of university students in other areas of the world and might provide foundation for the strategies to protect the mental health of non-medical college students from COVID-19 damage.
The sample size was calculated using Power Analysis and Sample Size (PASS) 11.0. The calculation formula was as follows:
The PASS operating parameters were as follows: “Proportions” --- “one proportion” --- “Confidence Intervals for one proportion.” With reference to previous studies, the prevalence of anxiety in college students was 23.8% (Naser et al., 2020), we defined Proportion (P) = 0.238. The other parameters were set as follows: confidence level (1-α) = 0.95, confidence interval width = 0.1, and confidence interval was calculated by Exact (Clopper-Pearson) method and the interval type was “two-sided.” Results showed that at least 297 people were required to meet statistical differences. Considering the 10% drop-out rate, we should at least enroll 327 students. In this study, we totally enrolled 1,083 students and the number met the requirements of the trial.
This cross-sectional study was conducted through a comprehensive social media WeChat (called Weixin in China; Tencent Inc.) from August 1st, 2022 to August 7th, 2022 (Ye et al., 2022). WeChat is the most frequently used APP in China and has been widely applied to collect mental health data (Jiang et al., 2021). Participants entered the survey by scanning a quick response (QR) code presented in the WeChat, which directed them to a survey website hosted by WenJuanXing (Changsha Haoxing Information Technology Co., Ltd., China). The inclusion criteria were as follows: non-medical college students aged 18–25 years old and voluntarily participate in this study. Exclusion criteria were as follows: students with no capacity or visual impairment or history of mental illness. The validity of the questionnaires for each participant was limited to 1 week as longer period might affect the psychological condition of the participants. The study was complied with the criteria of Strengthening the Reporting of Observation Studies in Epidemiology (STROBE), and was in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. The ethics committee of the Affiliated Hospital of Guangdong Medical University approved and supervised this study (Human Investigation Committee PJKT2022-072). This study was registered in the Chinese clinical trial center, and the trial registration number is ChiCTR2200062191.1
Demographic, knowledge about COVID-19, attitude toward COVID-19, mental health status including insomnia, depression and anxiety were collected from all participants.
Knowledge of COVID-19 was assessed by 7 items developed using the World Health Organization’s COVID-19 advice for the public (Wang et al., 2020b). The contents were as follows: (1) the symptoms after contracting COVID-19, (2) the signs indicating seeking health care immediately, (3) the outcomes caused by COVID-19, (4) transmission routes, (5) prevention strategies, (6) quarantine period, (7) availability of specific drug or vaccine. For each item, 0 indicated an incorrect answer and 1 indicated a correct answer, and the total score ranged from 0 to 7. A higher score suggested better knowledge of COVID-19. Poor, moderate and good knowledge of COVID-19 was defined as scores of 0–3, 4–5, and 6–7, respectively. In this study, the Cronbach’s alpha for the scale was 0.73.
A 5-items questionnaire was applied to measure the attitude toward the COVID-19 pandemic among college students as previously recommended with minor modification (Wang et al., 2020b). The contents were as follows: (1) being confident of knowing how to protect yourself from COVID-19, (2) do not worry about contracting COVID-19, (3) do not worry about loved ones/friends contracting COVID-19, (4) feeling hopeful to prevent COVID-19, (5) being confident that the COVID-19 will finish soon. For each item, 0 indicated disagree and 1 indicated agree, and the total score ranged from 0 to 5. A higher score indicated a more positive attitude toward COVID-19 prevention and control. Scores of 0–2, 3, and 4–5 were regarded as negative, neutral and positive attitude toward COVID-19, respectively. The Cronbach’s alpha for the scale in this study was 0.82.
Insomnia was assessed by Pittsburgh sleep quality index (PSQI). Depression and anxiety were evaluated by Hamilton depression rating scale-17 (HDRS-17) and self-rating anxiety scale (SAS), respectively. These scales were considered as valuable screening instruments for insomnia, depression and anxiety in different populations (Huang et al., 2018; Liu et al., 2020; Han et al., 2021). On the basis of previous studies and considering that the study was conducted on Chinese students, Chinese version of these scales were applied in this study (Jiang et al., 2021). In furtherance, the demographics information including age, gender, grade and household income were collected.
As for PSQI, there were 19 questions in this scale with seven components: duration of sleep, sleep disturbance, sleep latency, subjective sleep quality, sleep efficiency, daytime dysfunction and sleep medicine intake. The score for each component is 3 points and the total PSQI scale is 21 points. Higher score implied worse sleep quality. PSQI score > 5 and ≤ 5 were considered as poor and good sleep quality, respectively (Benítez et al., 2022). Cronbach’s α was 0.83 for this scale. The contents of HDRS-17 included depressed mood, feelings of guilt, suicide, insomnia (early in the night/middle of the night/early hours of the morning), work and activities, retardation, agitation, anxiety psychic, anxiety somatic, somatic symptoms gastro-intestinal, general somatic symptoms, genital symptoms, hypochondriasis, loss of weight and insight. HDRS-17 score < 8 indicated no depression (Huang et al., 2018), score 8–16 indicated minimal depression, score 17–24 indicated mild–moderate depression (Sampaio-Junior et al., 2018), score ≥ 25 indicated severe depression (Versiani et al., 2005). Cronbach’s α was 0.86 for this scale. SAS was applied to assess anxiety. The SAS questionnaire consist of 20 questions, and each question ranged from 1 to 4 according to the frequency of symptoms. The score for each item was calculated to obtain the raw score, and the standard score was calculated via the raw score multiplied by 1.25. Anxiety was classified into four different levels: normal (≤49), mild (50–59), moderate (60–70) and severe anxiety (≥70) (Liu et al., 2020). Cronbach’s α was 0.84 for this scale.
The informed consent of each study population was obtained and the answers to the specific demographic questions and insomnia, depression and anxiety scales were collected electronically. The questionnaires mentioned above all showed good reliability and validity in the surveys among college students (Huang et al., 2018; Raniti et al., 2018; Wang and Zhao, 2020; Wang et al., 2020a).
Statistical analysis was performed by using GraphPad Prism 7.0 and SPSS 22.0 (SPSS Inc., Chicago IL, United States). D’Agostino-Pearson omnibus test was used to determine normal distribution. Statistical description was expressed as median ± inter-quartile range (IQR) for the variables with non-normal distribution. The chi-square test or Fisher’s exact test was used to compare anxiety and depression among different gender and household income. Spearman’s analysis was conducted to examine the correlations between insomnia, anxiety, depression and related parameters like gender, age, income, knowledge about COVID-19 and attitude toward COVID-19. The significant factors were included in the stepwise multivariate logistic regression analysis to study their association with insomnia, anxiety and depression (Wang et al., 2022). Raw Cronbach’s αs for total and subscale scores and raw corrected item-total, item-component, and component-total Spearman’s rho (rs) correlations were calculated to assess the questionnaires’ internal consistency. Cronbach’s α ≥ 0.70 and corrected correlations (rs) ≥ 0.30 were recognized to have adequate internal consistency (Spira et al., 2012). Results were expressed as adjusted odds ratios (OR) with the corresponding 95% confidence intervals (95%CI). Differences with p < 0.05 were considered statistically significant.
A total of 1,083 non-medical students were enrolled in this study (Figure 1). As shown in Table 1, the majority of participants were females (n = 681, 62.9%). There were 475 participants (43.9%) aged between 18 and 19 years old and 608 participants (56.1%) aged between 20 and 25 years old. Around half of the participants were freshman (n = 525, 48.5%), and the rest were sophomore (42.6%) and junior or above (8.9%). There were 294 participants (27.1%) owned a monthly household income of less than 3,000 RMB and 789 participants (72.9%) had more than 3,000 RMB each month.
As shown in Table 2, most individuals had a correct understanding of the COVID-19. The correct answers for the 7 items of COVID-19 knowledge ranged from 65.2–77.6%. There were 66.8% (723/1083) and 70.4% (762/1083) students had good knowledge about the symptoms after contracting COVID-19 and the signs of indicating seeking health care immediately. More than half of the participants were familiar with the outcomes caused by COVID-19 (74.3%, 805/1083), transmission routes (74.9%, 811/1083) and prevention strategies of COVID-19 (77.6%, 840/1083), quarantine period (65.2%, 706/1083) and availability of specific drug or vaccine of COVID-19 (72.4%, 784/1083).
A majority of individuals reported being confident in knowing how to protect themselves from COVID-19 (96.1%, 1041/1083), being confident that the COVID-19 will end soon (93.4%, 1011/1083), feeling hopeful to prevent COVID-19 (91.6%, 992/1083). There were 49.7 and 39.9% participants worried about loved ones/friends and themselves contracting COVID-19, respectively (Table 3).
As presented in Table 4, most participants had good sleep quality (93.2%, 1010/1083), and very few students (6.8%, 73/1083) suffered from insomnia. The prevalence of anxiety among the participants were as follows: no anxiety (97.4%, 1055/1083), mild anxiety (1.86%, 20/1083), moderate anxiety (0.37%, 4/1083) and severe anxiety (0.37%, 4/1083). The proportions of no, minimal, mild–moderate and severe depression were 66.9, 26.7, 4.7 and 1.7%, respectively.
Female students obviously represented with more anxiety and depression than male students (anxiety: Fisher’s exact test, p = 0.02, Figure 2A; depression: Chi-square test, p < 0.0001, Figure 2B). Subjects with household income below 3,000 RMB per month showed significantly higher anxiety and depression than those with monthly income above 3,000 RMB (anxiety: Fisher’s exact test, p = 0.017, Figure 3A; depression: Fisher’s exact test, p = 0.004, Figure 3B).
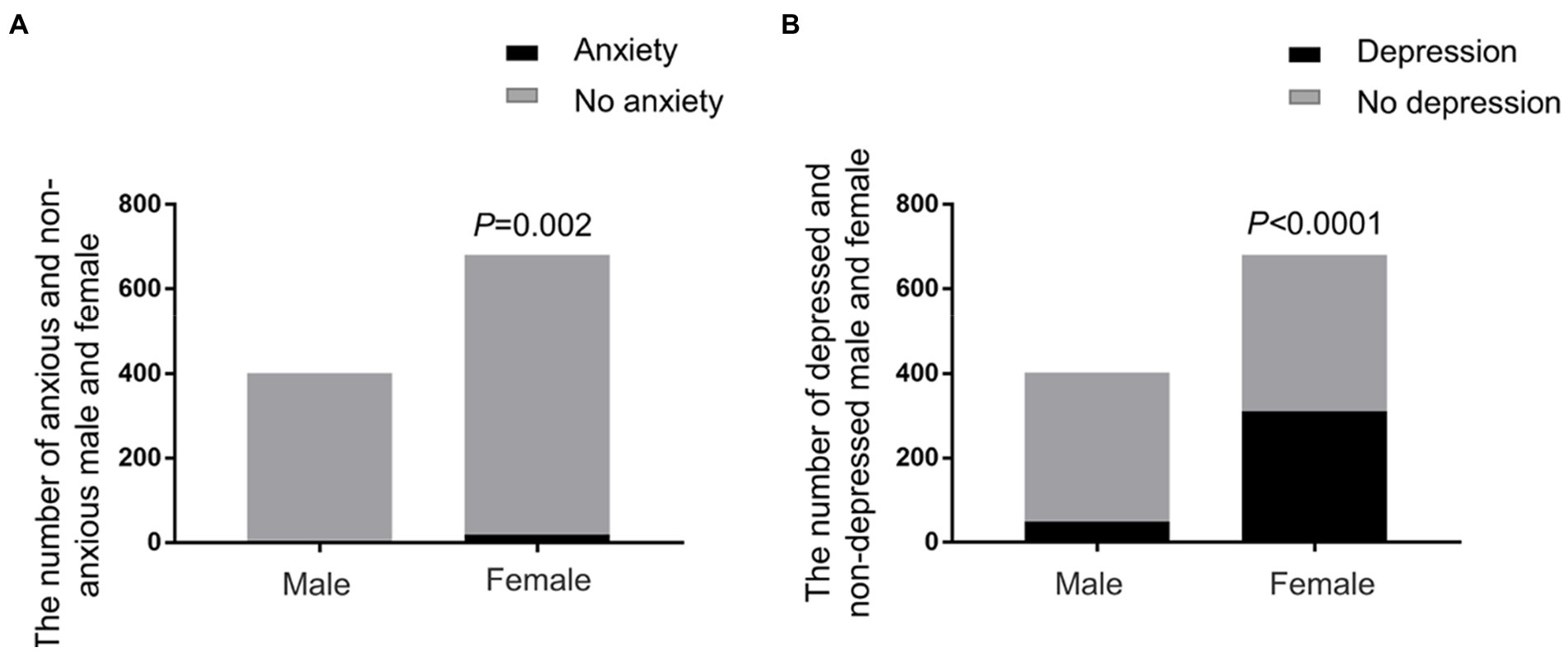
Figure 2. Anxiety and depression of students of different genders. (A) The prevalence of anxiety in male and female students. Female students showed significantly higher proportion of anxiety than male students (Fisher’s exact test, p = 0.02). (B) The prevalence of depression in male and female students. Female students represented more depressive emotion than male students (Chi-square test, p < 0.0001).
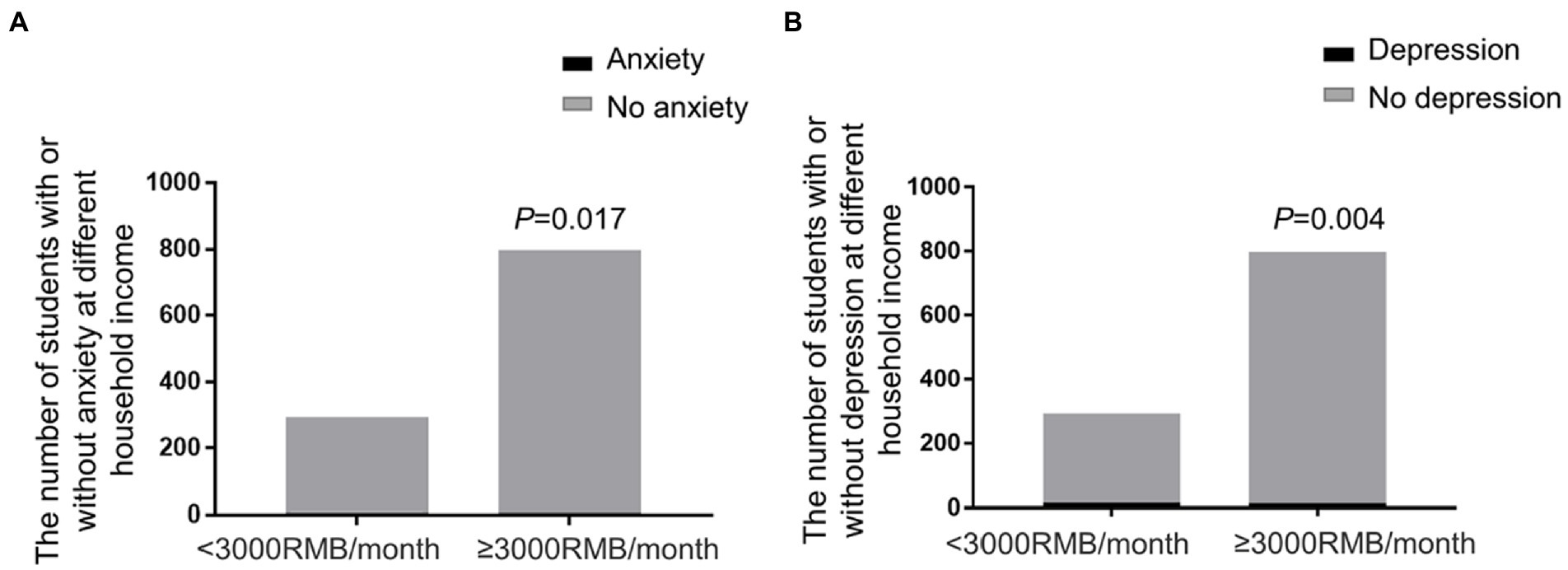
Figure 3. Anxiety and depression of students of different household income. (A) The prevalence of anxiety in different household income. The students with household income below 3,000 RMB/month showed significantly higher anxiety (Fisher’s exact test, p = 0.017). (B) The prevalence of depression in different household income. The students with household income below 3,000 RMB/month had higher rate of depression (Fisher’s exact test, p = 0.004).
Correlation analysis results showed that female and low monthly income were positively associated with insomnia (female: r = 0.17, p < 0.001; income: r = −0.11, p < 0.001, Table 5). Grades were related with anxiety and depression (anxiety: r = −0.092, p = 0.02; depression: r = −0.14, p < 0.001, Tables 6, 7). Good knowledge about COVID-19 and positive attitude toward COVID-19 were negatively associated with insomnia, anxiety and depression (Tables 5–7). Age was not correlated with insomnia, anxiety and depression (Tables 5–7).
We further performed multivariate logistic regression analysis to explore the risk factors associated with insomnia, anxiety and depression. Gender, grade, income, knowledge about COVID-19 and attitude toward COVID-19 were included in the multiple logistic regression analysis. As the data shown in Table 8, female (OR = 0.02, 95%CI: 0.008–0.061), household income lower than 3,000 RMB per month (OR = 13.78, 95%CI: 7.459–25.45), poor knowledge about COVID-19 (OR = 0.82, 95%CI: 0.728–0.915) and negative attitude toward COVID-19 (OR = 0.69, 95%CI: 0.538–0.872) were positively associated with the presence of insomnia. Female (OR = 4.02, 95%CI: 1.216–10.834), low income (OR = 4.08, 95%CI: 1.412–12.081), poor knowledge about COVID-19 (OR = 0.48, 95%CI: 0.370–0.612) and negative attitude toward COVID-19 (OR = 0.52, 95%CI: 0.347–0.788) were positively correlated with the presence of anxiety. Female (OR = 1.08, 95%CI: 1.015–1.161), freshman (OR = 1.87, 95%CI: 1.074–3.266), low monthly income (OR = 2.76, 95%CI: 1.506–5.473), poor knowledge about COVID-19 (OR = 0.85, 95%CI: 0.795–0.898) and negative attitude toward COVID-19 (OR = 0.79, 95%CI: 0.703–0.898) were positively associated with the presence of depression.
This study investigated the COVID-19 pandemic on mental health of 1,083 non-medical college students returning to school in Zhanjiang, China. The research found that most students acquired good knowledge about COVID-19 and held positive attitude toward COVID-19. There were 6.8% students suffered from insomnia, 2.6% students had mild–severe anxiety, and approximately 33.1% students had different degrees of depression. Female students, household income lower than 3,000 RMB per month, poor knowledge about COVID-19 and negative attitude toward COVID-19 were associated with insomnia, anxiety and depression, and freshmen were more vulnerable to depression.
COVID-19 seemed to have adverse impact on the long-term consequences of mental health (Zhuo et al., 2021). A national mental health study conducted in February and April 2020 among Chinese adolescents showed that the prevalence of depression and anxiety increased over time evidently (Chen et al., 2021). The prevalence of depressive and anxiety symptoms among back-to-school children was elevated in comparison to that during the home quarantine period (Xie et al., 2022). The prevalence of insomnia, anxiety and depression among high school students after reopening schools during the COVID-19 was 42.7 to 63.4% (Puteikis et al., 2022). A survey of 5,285 adults in the United States demonstrated that the incidence of adverse mental health symptoms during the later phase of the COVID-19 pandemic (September 2020) was higher than that in June 2020 (Czeisler et al., 2021). Some studies depicted that mental health of college students deteriorated in the few months following the COVID-19 pandemic (Lipson et al., 2022; Shiratori et al., 2022; von Keyserlingk et al., 2022). Some other evidence indicated a decrease in anxiety symptoms with time among university students (Amendola et al., 2021), and some data shown that college students just experienced minor changes during the pandemic outbreak (Pieh et al., 2021; Stamatis et al., 2022). These inconsistent findings highlighted the need for sustained attention to the dynamics of college students’ mental health across time and space. Our study focused on the psychological symptoms in non-medical college students who have experienced long-term home quarantine and have now back to school. During the prevalence of COVID-19, the students accepted online learning instead of face-to-face classes, and the activities of students in public places were restricted (Qin et al., 2021; Regmi and Lwin, 2021). We suggested that these altered lifestyle and social patterns might contribute to the development of mental illness (Wang et al., 2021; Zhuo et al., 2021). Mental disorder could lead to reduced quality of life and higher healthcare burden (Rodrigues et al., 2015). Therefore, providing early recognition of mental illness and support for the vulnerable students is a vital need. It is reported that the incidence of depression among general university students was 12.2–56.8% (Wang et al., 2020; Yu et al., 2021), and approximately 22.4–35.5% medical students represented with depressive symptoms during the COVID-19 pandemic (Xiao et al., 2020; Xie et al., 2020). The prevalence of depression among non-medical students in this study (33.1%) seemed to have no difference from previously published data on medical students and was lower than that of returning high school students. Previous studies pointed out that the incidence of anxiety among general university students and medical students were 7.7–15.43% (Wang et al., 2020; Wang and Zhao, 2020) and 22.1–28% (Lasheras et al., 2020; Xiao et al., 2020), respectively. A recent meta-analysis revealed that the prevalence of anxiety in general population during the COVID-19 pandemic was 31.9% (Salari et al., 2020). The prevalence of anxiety and insomnia among back-to-Wuhan university students was 44 and 37.5%, respectively (Wu et al., 2022). In this study, the incidence of anxiety (2.6%) was lower than previously reported in general university students and medical students, and was particularly lower than the data reported in the general population and the university students returning to school. Besides, a majority of non-medical students showed good sleep quality in this study. The mental health improvements shown in this study might be due to the emphasis placed by schools and government on enhancing COVID-19 knowledge among college students. For the general population, they obtained information from a variety of sources and probably lacked the ability to distinguish information accurately (Xiong et al., 2021). Poor COVID-19 knowledge was correlated with negative emotions like tension and depression (Lee et al., 2021). In addition, optimistic perception and familiarity with COVID-19 might help control the rapid spread of COVID-19 and decrease the incidence of mental illness (Zhong et al., 2020; Yin et al., 2022). Our data revealed that most participants had good knowledge about COVID-19 and held positive attitude toward COVID-19, with the exception of a minority of students who were concerned about contracting COVID-19 for themselves and their loved ones/friends. Our results indicate that the non-medical schools and government of Zhanjiang provide adequate COVID-19 knowledge and implement stringent policies promptly during the pandemic. Positive mental health attitudes can be improved by the popularization of mental health literacy, public awareness of COVID-19 prevention and control, and social support (Zhong et al., 2020).
In addition to evaluating the influences of participants’ knowledge about COVID-19 and attitude toward COVID-19 on their mental health, our study also investigated other potential factors for the development of depression, anxiety and insomnia. One research revealed that students in higher grades had lower prevalence of sleep disturbance compared with those in the lower grades (Li et al., 2020). The sleep quality among different grades in this study did not show statistical difference, indicating that the freshmen enrolled were adaptable to the new circumstances during the COVID-19 pandemic. Age was not correlated with insomnia, anxiety and depression in this study, probably owning to the students enrolled were very similar in age. We found that female students were more prone to sleep disorder, anxiety and depression. The results were in accordance with the previous study demonstrating that women were approximately twice as likely to experience mood disturbance as men, including sleep problems, anxiety and depression (Mong and Cusmano, 2016; Serpytis et al., 2018). This sexual discrepancy might result from different sex steroids levels. For example, testosterone has been regarded as an important sex steroid to resist anxiety and depression (Zarrouf et al., 2009). In furtherance, the influence of economic status of the participants on anxiety and depression should be noted. It is demonstrated that the diabetic patients of higher-income showed a significant decline for anxiety (Al-Ayed et al., 2021). People with low socioeconomic status had high incidences of anxiety and depression (Linder et al., 2020). Similarly, our result also revealed that subjects with higher household incomes had lower rates of anxiety and depression.
To the best of our knowledge, this is the first and largest study that explore the prevalence of depression, anxiety and insomnia among non-medical college students returning to school during COVID-19 pandemic in Zhanjiang city. Our study can provide information on risk factors associated with psychological effects in the countries such as China where the pandemic is under control. The results of the study might be helpful for future research in other countries. There are a few limitations that should be acknowledged. Given the use of an online survey, there might exist some response bias. Though our data are in line with many previous studies, it is hard to establish a causal relationship between pandemic context and mental health disorders in a cross-sectional study. The study might be improved in the future by increasing the correlation analysis between mental health and other factors such as perceived social support, living environment (urban or rural area), physical activity, sedentary time, and dietary behaviors (Ivbijaro et al., 2021; Shibata et al., 2021; Rahim et al., 2022; Silva et al., 2022; Zhao et al., 2022). Furthermore, mood disturbance has been reported to be associated with inflammatory processes (Beurel et al., 2020). We suggest that it would be interesting to study the immunological changes of the participants in the next study.
During the COVID-19 prevalence, non-medical college students returning to school in Zhanjiang experienced no higher levels of anxiety and depression, and most students represented with good sleep quality. The results from this study might help in guiding healthcare practitioners and policymakers to work out appropriate and feasible interventions to recognize and treat the students with mental disorders. Most importantly, universities may be able to apply these results to build mental health profiles of students, which could help identify more ‘at risk’ students in the face of COVID-19.
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
The studies involving human participants were reviewed and approved by the ethics committee of the Affiliated Hospital of Guangdong Medical University. The patients/participants provided their written informed consent to participate in this study.
XD and HZ designed the study. XD developed the questionnaire, recruited the participants, and wrote the main manuscript text. HZ revised the manuscript, analyzed the data, and had full access to all the data in the study and final responsibility for the decision to submit for publication. All authors reviewed and approved the final manuscript.
This work was supported by Guangdong Medical Research Foundation, Grant/Award Number: B2018048; Science and technology research project of Zhanjiang City, Grant/Award Number: 2018B01012; Research Foundation of Guangdong Medical University, Grant/Award Number: GDMUM201807; and Scientific research project of Zhanjiang Preschool Education College (Research center for rural preschool education in Western Guangdong, Guangdong Province), Grant/Award Number: ZY2022XJZX10.
We would like to thank the participants who voluntarily participated and professor Jia-Yuan Wu for his support in statistics.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abdolkarimi, M., Masoomi, M., Lotfipur, S. S., and Zakeri, M. A. (2022). The relationship between spiritual health and happiness in medical students during the COVID-19 outbreak: a survey in southeastern Iran. Front. Psychol. 13:974697. doi: 10.3389/fpsyg.2022.974697
Al-Ayed, M., Moosa, S., Robert, A., and Al Dawish, M. (2021). Anxiety, depression and their associated risk factors among patients with diabetic foot ulcer: a two center cross-sectional study in Jordan and Saudi Arabia. Diabetes Metab. Syndr. 15, 237–242. doi: 10.1016/j.dsx.2020.12.034
Amendola, S., von Wyl, A., Volken, T., Zysset, A., Huber, M., and Dratva, J. (2021). A longitudinal study on generalized anxiety among university students during the first wave of the COVID-19 pandemic in Switzerland. Front. Psychol. 12:643171. doi: 10.3389/fpsyg.2021.643171
Benítez, I., Moncusí-Moix, A., Vaca, R., Gort-Paniello, C., Minguez, O., Santisteve, S., et al. (2022). Sleep and circadian health of critical COVID-19 survivors 3 months after hospital discharge. Crit. Care Med. 50, 945–954. doi: 10.1097/ccm.0000000000005476
Beurel, E., Toups, M., and Nemeroff, C. (2020). The bidirectional relationship of depression and inflammation: double trouble. Neuron 107, 234–256. doi: 10.1016/j.neuron.2020.06.002
Cao, W., Fang, Z., Hou, G., Han, M., Xu, X., Dong, J., et al. (2020). The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res. 287:112934. doi: 10.1016/j.psychres.2020.112934
Chen, X., Qi, H., Liu, R., Feng, Y., Li, W., Xiang, M., et al. (2021). Depression, anxiety and associated factors among Chinese adolescents during the COVID-19 outbreak: a comparison of two cross-sectional studies. Transl. Psychiatry 11:148. doi: 10.1038/s41398-021-01271-4
Czeisler, M., Lane, R., Wiley, J., Czeisler, C., Howard, M., and Rajaratnam, S. (2021). Follow-up survey of US adult reports of mental health, substance use, and suicidal ideation during the COVID-19 pandemic, September 2020. JAMA Netw. Open 4:e2037665. doi: 10.1001/jamanetworkopen.2020.37665
Elmer, T., Mepham, K., and Stadtfeld, C. (2020). Students under lockdown: comparisons of students' social networks and mental health before and during the COVID-19 crisis in Switzerland. PLoS One 15:e0236337. doi: 10.1371/journal.pone.0236337
Essangri, H., Sabir, M., Benkabbou, A., Majbar, M., Amrani, L., Ghannam, A., et al. (2021). Predictive factors for impaired mental health among medical students during the early stage of the COVID-19 pandemic in Morocco. Am. J. Trop. Med. Hyg. 104, 95–102. doi: 10.4269/ajtmh.20-1302
Gao, M., Li, X., Lee, C., Ma, H., Chen, T., Zhang, S., et al. (2022). Sleep duration and depression among adolescents: mediation effect of collective integration. Front. Psychol. 13:1015089. doi: 10.3389/fpsyg.2022.1015089
Gunaratne, P., Lloyd, A., and Vollmer-Conna, U. (2013). Mood disturbance after infection. Aust. N. Z. J. Psychiatry 47, 1152–1164. doi: 10.1177/0004867413503718
Han, Q., Liu, B., Lin, S., Li, J., Liang, P., Fu, S., et al. (2021). Pittsburgh sleep quality index score predicts all-cause mortality in Chinese dialysis patients. Int. Urol. Nephrol. 53, 2369–2376. doi: 10.1007/s11255-021-02842-6
Huang, J., Zhou, F., Guan, B., Zhang, N., Wang, A., Yu, P., et al. (2018). Predictors of remission of early-onset poststroke depression and the interaction between depression and cognition during follow-up. Front. Psych. 9:738. doi: 10.3389/fpsyt.2018.00738
Husky, M., Kovess-Masfety, V., Gobin-Bourdet, C., and Swendsen, J. (2021). Prior depression predicts greater stress during Covid-19 mandatory lockdown among college students in France. Compr. Psychiatry 107:152234. doi: 10.1016/j.comppsych.2021.152234
Ivbijaro, G., Kolkiewicz, L., Goldberg, D., Njie, I., Edwards, T., Riba, M., et al. (2021). Suicide prevention and COVID-19. Asia Pac. Psychiatry 13:e12482. doi: 10.1111/appy.12482
Jiang, H., Jin, L., Qian, X., Xiong, X., La, X., Chen, W., et al. (2021). Maternal mental health status and approaches for accessing antenatal care information during the COVID-19 epidemic in China: cross-sectional study. J. Med. Internet Res. 23:e18722. doi: 10.2196/18722
Lasheras, I., Gracia-García, P., Lipnicki, D., Bueno-Notivol, J., López-Antón, R., de la Cámara, C., et al. (2020). Prevalence of anxiety in medical students during the COVID-19 pandemic: a rapid systematic review with meta-analysis. Int. J. Environ. Res. Public Health 17:6603. doi: 10.3390/ijerph17186603
Lee, Y., Lui, L., Chen-Li, D., Liao, Y., Mansur, R., Brietzke, E., et al. (2021). Government response moderates the mental health impact of COVID-19: a systematic review and meta-analysis of depression outcomes across countries. J. Affect. Disord. 290, 364–377. doi: 10.1016/j.jad.2021.04.050
Li, Y., Bai, W., Zhu, B., Duan, R., Yu, X., Xu, W., et al. (2020). Prevalence and correlates of poor sleep quality among college students: a cross-sectional survey. Health Qual. Life Outcomes 18:210. doi: 10.1186/s12955-020-01465-2
Lin, Y., Hu, Z., Alias, H., and Wong, L. (2020). Influence of mass and social media on psychobehavioral responses among medical students during the downward trend of COVID-19 in Fujian, China: cross-sectional study. J. Med. Internet Res. 22:e19982. doi: 10.2196/19982
Linder, A., Gerdtham, U., Trygg, N., Fritzell, S., and Saha, S. (2020). Inequalities in the economic consequences of depression and anxiety in Europe: a systematic scoping review. Eur. J. Pub. Health 30, 767–777. doi: 10.1093/eurpub/ckz127
Lipson, S., Zhou, S., Abelson, S., Heinze, J., Jirsa, M., Morigney, J., et al. (2022). Trends in college student mental health and help-seeking by race/ethnicity: findings from the national healthy minds study, 2013-2021. J. Affect. Disord. 306, 138–147. doi: 10.1016/j.jad.2022.03.038
Liu, C., Yang, Y., Zhang, X., Xu, X., Dou, Q., Zhang, W., et al. (2020). The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol. Infect. 148:e98. doi: 10.1017/s0950268820001107
Mong, J., and Cusmano, D. (2016). Sex differences in sleep: impact of biological sex and sex steroids. Philos. Trans. R. Soc. Lond. Ser. B Biol. Sci. 371:20150110. doi: 10.1098/rstb.2015.0110
Naser, A., Dahmash, E., Al-Rousan, R., Alwafi, H., Alrawashdeh, H., Ghoul, I., et al. (2020). Mental health status of the general population, healthcare professionals, and university students during 2019 coronavirus disease outbreak in Jordan: a cross-sectional study. Brain Behav. 10:e01730. doi: 10.1002/brb3.1730
Oh, H., Marinovich, C., Rajkumar, R., Besecker, M., Zhou, S., Jacob, L., et al. (2021). COVID-19 dimensions are related to depression and anxiety among US college students: findings from the healthy minds survey 2020. J. Affect. Disord. 292, 270–275. doi: 10.1016/j.jad.2021.05.121
Pieh, C., Budimir, S., Humer, E., and Probst, T. (2021). Comparing mental health during the COVID-19 lockdown and 6 months after the lockdown in Austria: a longitudinal study. Front. Psych. 12:625973. doi: 10.3389/fpsyt.2021.625973
Puteikis, K., Mameniškytė, A., and Mameniškienė, R. (2022). Sleep quality, mental health and learning among high school students after reopening schools during the COVID-19 pandemic: results of a cross-sectional online survey. Int. J. Environ. Res. Public Health 19:2553. doi: 10.3390/ijerph19052553
Qin, Z., Shi, L., Xue, Y., Lin, H., Zhang, J., Liang, P., et al. (2021). Prevalence and risk factors associated with self-reported psychological distress among children and adolescents during the COVID-19 pandemic in China. JAMA Netw. Open 4:e2035487. doi: 10.1001/jamanetworkopen.2020.35487
Rahim, N. A., Abidin, M. Z. A. Z., Shalan, N. A. A. M., Karim, Z. B., Aziz, N. U. A., and Avin, F. A. (2022). COVID-19 lockdown: physical activity, sedentary behaviour, and academic motivation among undergraduates university students in Malaysia. Ann Appl Sport Sci 9:1047. doi: 10.52547/aassjournal.1047
Raniti, M., Waloszek, J., Schwartz, O., Allen, N., and Trinder, J. (2018). Factor structure and psychometric properties of the Pittsburgh sleep quality index in community-based adolescents. Sleep 41:66. doi: 10.1093/sleep/zsy066
Regmi, K., and Lwin, C. (2021). Factors associated with the implementation of non-pharmaceutical interventions for reducing coronavirus disease 2019 (COVID-19): a systematic review. Int. J. Environ. Res. Public Health 18:4274. doi: 10.3390/ijerph18084274
Rodrigues, G., Gebara, O., Gerbi, C., Pierri, H., and Wajngarten, M. (2015). Depression as a clinical determinant of dependence and low quality of life in elderly patients with cardiovascular disease. Arq. Bras. Cardiol. 104, 443–449. doi: 10.5935/abc.20150034
Salari, N., Hosseinian-Far, A., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Mohammadi, M., et al. (2020). Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob. Health 16:57. doi: 10.1186/s12992-020-00589-w
Sampaio-Junior, B., Tortella, G., Borrione, L., Moffa, A., Machado-Vieira, R., Cretaz, E., et al. (2018). Efficacy and safety of transcranial direct current stimulation as an add-on treatment for bipolar depression: a randomized clinical trial. JAMA Psychiat. 75, 158–166. doi: 10.1001/jamapsychiatry.2017.4040
Serpytis, P., Navickas, P., Lukaviciute, L., Navickas, A., Aranauskas, R., Serpytis, R., et al. (2018). Gender-based differences in anxiety and depression following acute myocardial infarction. Arq. Bras. Cardiol. 111, 676–683. doi: 10.5935/abc.20180161
Sheedy O’Sullivan, E., McCarthy, K. M., O'Neill, C., Walton, J., Bolger, L., and Bickerdike, A. (2022). The impact of COVID-19 on the health-related behaviours, mental well-being, and academic engagement of a cohort of undergraduate students in an Irish university setting. Int. J. Environ. Res. Public Health 19:16096. doi: 10.3390/ijerph192316096
Shibata, M., Burkauskas, J., Dores, A., Kobayashi, K., Yoshimura, S., Simonato, P., et al. (2021). Exploring the relationship between mental well-being, exercise routines, and the intake of image and performance enhancing drugs during the coronavirus disease 2019 pandemic: a comparison across sport disciplines. Front. Psychol. 12:689058. doi: 10.3389/fpsyg.2021.689058
Shiratori, Y., Ogawa, T., Ota, M., Sodeyama, N., Sakamoto, T., Arai, T., et al. (2022). A longitudinal comparison of college student mental health under the COVID-19 self-restraint policy in Japan. J. Affect. Disord. Rep. 8:100314. doi: 10.1016/j.jadr.2022.100314
Shokri, F., Taheri, M., Irandoust, K., and Mirmoezzi, M. (2022). Effects of the COVID -19 pandemic on physical activity, mood status, and eating patterns of Iranian elite athletes and non-athletes. Zahedan J. Res. Med. Sci. 24:120049. doi: 10.5812/zjrms-120049
Silva, R. R., Rufino, C. R., Galvão, L. L, Vancini, R. L., Santos, D., and Lira, C. A. B.De.,, et al. (2022). Motivation for Brazilian older adult women to join a community physical activity program before COVID-19 pandemic. Int. J. Sport Stud. Health, 5,:e128560. doi: 10.5812/intjssh-128560
Spira, A. P., Beaudreau, S. A., Stone, K. L., Kezirian, E. J., Lui, L. Y., Redline, S., et al. (2012). Reliability and validity of the Pittsburgh sleep quality index and the Epworth sleepiness scale in older men. J. Gerontol. A Biol. Sci. Med. Sci. 67, 433–439. doi: 10.1093/gerona/glr172
Stamatis, C., Broos, H., Hudiburgh, S., Dale, S., and Timpano, K. (2022). A longitudinal investigation of COVID-19 pandemic experiences and mental health among university students. Br. J. Clin. Psychol. 61, 385–404. doi: 10.1111/bjc.12351
Versiani, M., Moreno, R., Ramakers-van Moorsel, C., and Schutte, A. (2005). Comparison of the effects of mirtazapine and fluoxetine in severely depressed patients. CNS Drugs 19, 137–146. doi: 10.2165/00023210-200519020-00004
von Keyserlingk, L., Yamaguchi-Pedroza, K., Arum, R., and Eccles, J. S. (2022). Stress of university students before and after campus closure in response to COVID-19. J. Community Psychol. 50, 285–301. doi: 10.1002/jcop.22561
Wang, D., Chen, H., Zhai, S., Zhu, Z., Huang, S., Zhou, X., et al. (2021). Is returning to school during the COVID-19 pandemic stressful? A study on immediate mental health status of Chinese college students. J. Affect. Disord. 287, 261–267. doi: 10.1016/j.jad.2021.03.035
Wang, L., Dong, J., Xu, M., Li, L., Yang, N., and Qian, G. (2022). Association between monocyte to high-density lipoprotein cholesterol ratio and risk of non-alcoholic fatty liver disease: a cross-sectional study. Front. Med. 9:898931. doi: 10.3389/fmed.2022.898931
Wang, X., Hegde, S., Son, C., Keller, B., Smith, A., and Sasangohar, F. (2020). Investigating mental health of US College students during the COVID-19 pandemic: cross-sectional survey study. J. Med. Internet Res. 22:e22817. doi: 10.2196/22817
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., McIntyre, R. S., et al. (2020a). A longitudinal study on the mental health of general population during the COVID-19 epidemic in China. Brain Behav. Immun. 87, 40–48. doi: 10.1016/j.bbi.2020.04.028
Wang, C., Tian, Q., Zhao, P., Xiong, M., Latkin, C., Gan, Y., et al. (2020b). Disease knowledge and attitudes during the COVID-19 epidemic among international migrants in China: a national cross-sectional study. Int. J. Biol. Sci. 16, 2895–2905. doi: 10.7150/ijbs.47075
Wang, Z., Yang, H., Yang, Y., Liu, D., Li, Z., Zhang, X., et al. (2020). Prevalence of anxiety and depression symptom, and the demands for psychological knowledge and interventions in college students during COVID-19 epidemic: a large cross-sectional study. J. Affect. Disord. 275, 188–193. doi: 10.1016/j.jad.2020.06.034
Wang, C., and Zhao, H. (2020). The impact of COVID-19 on anxiety in Chinese university students. Front. Psychol. 11:1168. doi: 10.3389/fpsyg.2020.01168
Wu, Q., Zhuo, L., Li, H., Zheng, L., Ma, G., and Tao, H. (2022). Factors associated with the mental health of back-to-Wuhan university students based on quantile regression model during the COVID-19 period. BMC Psychiatry 22:284. doi: 10.1186/s12888-022-03828-z
Xiao, H., Shu, W., Li, M., Li, Z., Tao, F., Wu, X., et al. (2020). Social distancing among medical students during the 2019 coronavirus disease pandemic in China: disease awareness, anxiety disorder, depression, and Behavioral activities. Int. J. Environ. Res. Public Health 17:5047. doi: 10.3390/ijerph17145047
Xie, J., Li, X., Luo, H., He, L., Bai, Y., Zheng, F., et al. (2020). Depressive symptoms, sleep quality and diet during the 2019 novel coronavirus epidemic in China: a survey of medical students. Front. Public Health 8:588578. doi: 10.3389/fpubh.2020.588578
Xie, X., Liu, Q., Zhu, K., Jiang, Q., Feng, Y., Xiao, P., et al. (2022). Psychological symptom progression in school-aged children after COVID-19 home confinement: a longitudinal study. Front. Psych. 13:809107. doi: 10.3389/fpsyt.2022.809107
Xiong, P., Ming, W. K., Zhang, C., Bai, J., Luo, C., Cao, W., et al. (2021). Factors influencing mental health among Chinese medical and non-medical students in the early stage of the COVID-19 pandemic. Front. Public Health 9:603331. doi: 10.3389/fpubh.2021.603331
Ye, J. H., Wu, Y. T., Wu, Y. F., Chen, M. Y., and Ye, J. N. (2022). Effects of short video addiction on the motivation and well-being of Chinese vocational college students. Front. Public Health 10:847672. doi: 10.3389/fpubh.2022.847672
Yin, R., Tian, R., Wu, J., and Gan, F. (2022). Exploring the factors associated with mental health attitude in China: a structural topic Modeling approach. Int. J. Environ. Res. Public Health 19:12579. doi: 10.3390/ijerph191912579
Yu, M., Tian, F., Cui, Q., and Wu, H. (2021). Prevalence and its associated factors of depressive symptoms among Chinese college students during the COVID-19 pandemic. BMC Psychiatry 21:66. doi: 10.1186/s12888-021-03066-9
Zarrouf, F., Artz, S., Griffith, J., Sirbu, C., and Kommor, M. (2009). Testosterone and depression: systematic review and meta-analysis. J. Psychiatr. Pract. 15, 289–305. doi: 10.1097/01.pra.0000358315.88931.fc
Zhao, J., Chapman, E., and Houghton, S. (2022). Key predictive factors in the mental health of Chinese university students at home and abroad. Int. J. Environ. Res. Public Health 19:16103. doi: 10.3390/ijerph192316103
Zhao, G., Xie, F., Li, S., Ding, Y., Li, X., and Liu, H. (2022). The relationship between perceived social support with anxiety, depression, and insomnia among Chinese college students during the COVID-19 pandemic: the mediating role of self-control. Front. Psych. 13:994376. doi: 10.3389/fpsyt.2022.994376
Zheng, C., Shao, W., Chen, X., Zhang, B., Wang, G., and Zhang, W. (2022). Real-world effectiveness of COVID-19 vaccines: a literature review and meta-analysis. Int. J. Infect. Dis. 114, 252–260. doi: 10.1016/j.ijid.2021.11.009
Zhong, B., Luo, W., Li, H., Zhang, Q., Liu, X., Li, W., et al. (2020). Knowledge, attitudes, and practices towards COVID-19 among Chinese residents during the rapid rise period of the COVID-19 outbreak: a quick online cross-sectional survey. Int. J. Biol. Sci. 16, 1745–1752. doi: 10.7150/ijbs.45221
Keywords: COVID-19 pandemic, non-medical students, mental health, insomnia, anxiety, depression, Zhanjiang city
Citation: Deng X and Zhang H (2023) Mental health status among non-medical college students returning to school during the COVID-19 pandemic in Zhanjiang city: A cross-sectional study. Front. Psychol. 13:1035458. doi: 10.3389/fpsyg.2022.1035458
Received: 02 September 2022; Accepted: 22 December 2022;
Published: 11 January 2023.
Edited by:
Padraic James Dunne, Royal College of Surgeons in Ireland, IrelandReviewed by:
Manh Van Pham, Hai Duong Medical Technical University, VietnamCopyright © 2023 Deng and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huiting Zhang, ✉ YmFyYmFyYTMzNjc3MjNAMTI2LmNvbQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.