- 1Key Laboratory of Public Health Safety, NHC Key Laboratory of Health Technology Assessment, School of Public Health, Fudan University, Shanghai, China
- 2Taizhou City Center for Disease Prevention and Control, Taizhou, China
- 3Songjiang District Center for Disease Prevention and Control, Shanghai, China
Background: Most studies on mental health problems caused by COVID-19 crisis in children were limited to the period of home quarantine. It remained unclear what adverse impact of the psychosocial stressors caused by school reopening, as well as the transitions in daily activities and social interactions had on mental health in children.
Methods: A total of 6400 students in primary schools were enrolled in a cross-sectional study conducted in East China, between June 26 and July 6, 2020, when schools reopened. Children’s mental health status was assessed by the parent version of Strengths and Difficulties Questionnaire (SDQ). Ultimately, data on a total of 6017 children with completed information on mental health, psychosocial stressors, daily activities, and social interactions were eligible for analysis. The associations of mental health with psychosocial stressors, daily activities, and social interactions were determined by ordinal logistic regression models. Stratified analyses were conducted according to grade, gender, school level, area, and caregiver–child relationship to further observe the effects of stressors on mental status.
Results: The prevalence of borderline, moderately abnormal, and prominently abnormal scores were 7.16, 3.34, and 1.96% for total difficulties, and 13.83, 13.45, and 17.85% for prosocial behavior, respectively. Children with psychological stressors had a significantly higher risk of being in a worse category of mental health status, with the maximum adjusted OR of 7.90 (95% CI 3.33–18.75) in those definitely afraid of inadaptation to study and life styles. Time used in home work and computer games was positively related to mental health problems, while physical exercises and frequency of communication with others was negatively related. The effects of psychological stressors on total difficulties were more evident in middle-high grade students (OR = 7.52, 95% CI 4.16–8.61), boys (OR = 6.95, 95% CI 4.83–8.55), those who lived in Taizhou (OR = 7.62, 95% CI 4.72–8.61) and with poor caregiver–child relationship (OR = 7.79, 95% CI 2.26–8.65).
Conclusion: Emotional and behavioral difficulties, especially less prosocial behavior, were prevalent in primary school children after schools reopened. The Chinese government, communities, schools, and families need to provide more effective support for students’ transition back into the school building and address emotional and behavioral problems for children with difficulties.
Introduction
The pandemic of COVID-19, which was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) (Zhu et al., 2020), has been declared as an international public health emergency by the World Health Organization (WHO), 2021. The Chinese government had implemented a nationwide school closure in response to the outbreak in order to protect the students through reducing contacts with others since early February, 2020. More than 220 million children and adolescents in China were restricted to their homes, including 180 million primary students and 47 million preschool children (CCTV News, 2021). The dates of primary schools reopening across provinces in China were inconsistent, progressively from March 23, 2020, in Xinjiang Province (People’s Daily Online, 2021b), to June 15, 2020, in Hebei Province (People’s Daily Online, 2021a), according to the local epidemic situation and prevention and control strategies.
This emergency measure has brought remarkable benefit of preventing the transmission of COVID-19 (Zhang et al., 2020), but children and adolescents, as the vulnerable groups, had been affected by the adverse impacts of prolonged COVID-19-related school closure and home confinement on physical and mental health (Saurabh and Ranjan, 2020; Xie et al., 2020; Li et al., 2021). They had encountered a series of difficult transitions in daily activities (e.g., irregular rest timetable, lack of personal space at home, less outdoor activities, and more time used on electronic equipment), and social interactions (e.g., more dependence on social media instead of face-to-face contact with peers, teachers, and others) (Ezpeleta et al., 2020). Some mental health threats were generated during the transitional period, such as loneliness (Guessoum et al., 2020) and intensified caregiver–child relationship (Cusinato et al., 2020). A study investigated the psychological responses of children to pandemic disasters and reported that children who experienced isolation or quarantine were more likely to meet the clinical cutoff score for post-traumatic stress disorder (PTSD) than those who did not (30 vs. 1.1%) (Sprang and Silman, 2013). However, it remains unclear what mental status was in children after schools reopened and what influence the transitions in daily activities and social interactions had on mental health in children during COVID-19 post-pandemic period.
Furthermore, the dates of school reopening had been repeatedly postponed, although all the subjects were taught online, including language, math, science, even gym, and art (Wang et al., 2020). As a result of lack of school rhythm and routines, group study atmosphere and effective monitoring, students may fail to adapt to online learning at home, lose interest in studying, and have diminished attention and academic performance (Zhao et al., 2020). After the lockdown period ended and schools reopened, children returned to a new studying lifestyle with restrictive measures for COVID-19. They had to wear facemasks, adhere to hand hygiene, and keep physical distance. The joint effects of the disruption in normal classroom schooling and concerns of social distancing could be considered as psychosocial stressors which may lead to maladjustment and make children vulnerable to mental health problems, including fear (Jiao et al., 2020), anxiety (Duan et al., 2020), and depression (Zhou et al., 2020). Therefore, further studies are warranted to investigate the degrees of psychological stressors and their adverse effects on mental health in children when schools reopened.
Although the knowledge regarding children’s reactions to this unprecedented COVID-19 crisis has been expanded, the majority of studies were limited to the duration of school closure and home quarantine (Guessoum et al., 2020; Khan et al., 2020; Xie et al., 2020), and further observations after school reopening should be continued. The feasibility and effectiveness of school closure policies on mitigating the epidemics of infectious diseases were well-known (Fumanelli et al., 2016), but it remains unclear what the negative impact of long-term school closures have on psychological and behavioral problems in children, especially when they return to schools and face school life again. Therefore, the aim of this study was to investigate the prevalence of mental health problems among primary school students after schools reopened. We also aimed to evaluate the associations between psychological stressors, daily activities, social interactions, and mental health status, in order to provide suggestions for mental health promotion in school-aged children.
Materials and Methods
Study Design and Subject Selection
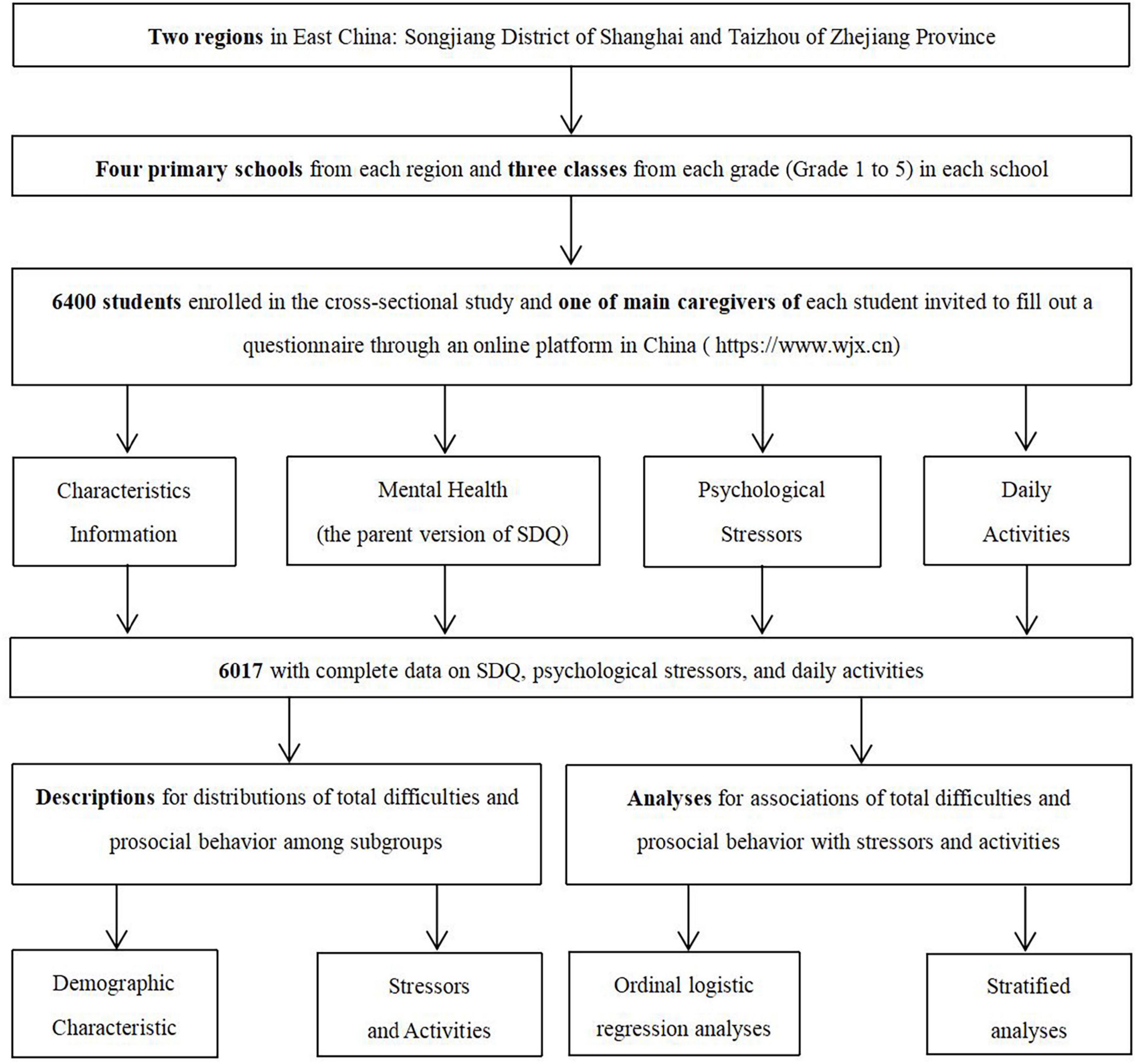
A cross-sectional study was conducted by using a cluster sampling method among primary school students in Songjiang District of Shanghai and Taizhou of Zhejiang Province, with different levels of education and economic development in East China, between June 26 and July 6, 2020, when primary schools in these regions have been reopened. Primary schools in Shanghai reopened on May 18, 2020 for Grade 4 and 5 and June 2, 2020 for Grade 1–3, while primary schools in Taizhou reopened on April 20, 2020 for Grade 4–6 and April 26, 2020 for Grade 1–3. Four primary schools of different characteristics, including key schools and non-key schools, were randomly sampled from each region, and three classes from each grade (Grade 1–5) were randomly selected in each school. A total of 6400 students from these classes were enrolled in the study after excluding 204 individuals who refused to participate. One of main caregivers of each student was invited to fill out a questionnaire through an online platform in China1 to report information about their child. Ultimately, data on a total of 6017 students with complete information on scores of the parent version of the Strengths and Difficulties Questionnaire (SDQ), psychological stressors, daily activities, and social communication ways were used in statistical analyses after removing those with invalid questionnaires. The response rate was 94.02%. A flow chart was shown in Figure 1. Informed written consents were obtained from all subjects and their caregivers, and this study was approved by the ethical review board of the School of Public Health of Fudan University (IRB#2020040817).
Information Collection for Sociodemographic Characteristics
Information on characteristics of children was collected, including age, grade, gender, school level (“non-key school” and “key school.” Teaching equipment, students’ academic performance, and quality of teachers in key schools are generally better than those in non-key schools), child medical conditions (hypertension, diabetes, cardiovascular diseases, pulmonary diseases, cancers, other chronic physical diseases, anxiety, depression, other psychiatric illnesses, attention-deficit disorder/attention-deficit hyperactivity disorder, autism spectrum disorder, lack of outdoor activities due to disability and any other disability), knowledge, and precaution (preventive behaviors) levels on COVID-19 (score 1–7). Information on characteristics of their families was also recorded, including area, number of household rooms, family economic status (“low,” “middle,” and “high”), caregiver education level (“primary school or below,” “middle or high school,” and “college or above”), and caregiver medical conditions (pregnancy, hypertension, diabetes, cardiovascular diseases, pulmonary diseases, cancers, other chronic physical diseases, anxiety, depression, other psychiatric illnesses, lack of outdoor activities due to disability and any other disability), as well as caregiver–child relationship (the question was “Do you agree with the statement that you have a good relationship with your child?” The corresponding responses were “Strongly disagree,” “Disagree,” “Agree,” and “Strongly agree.” Finally, the responses were categorized into two groups: “poor” and “good”) (Table 1).
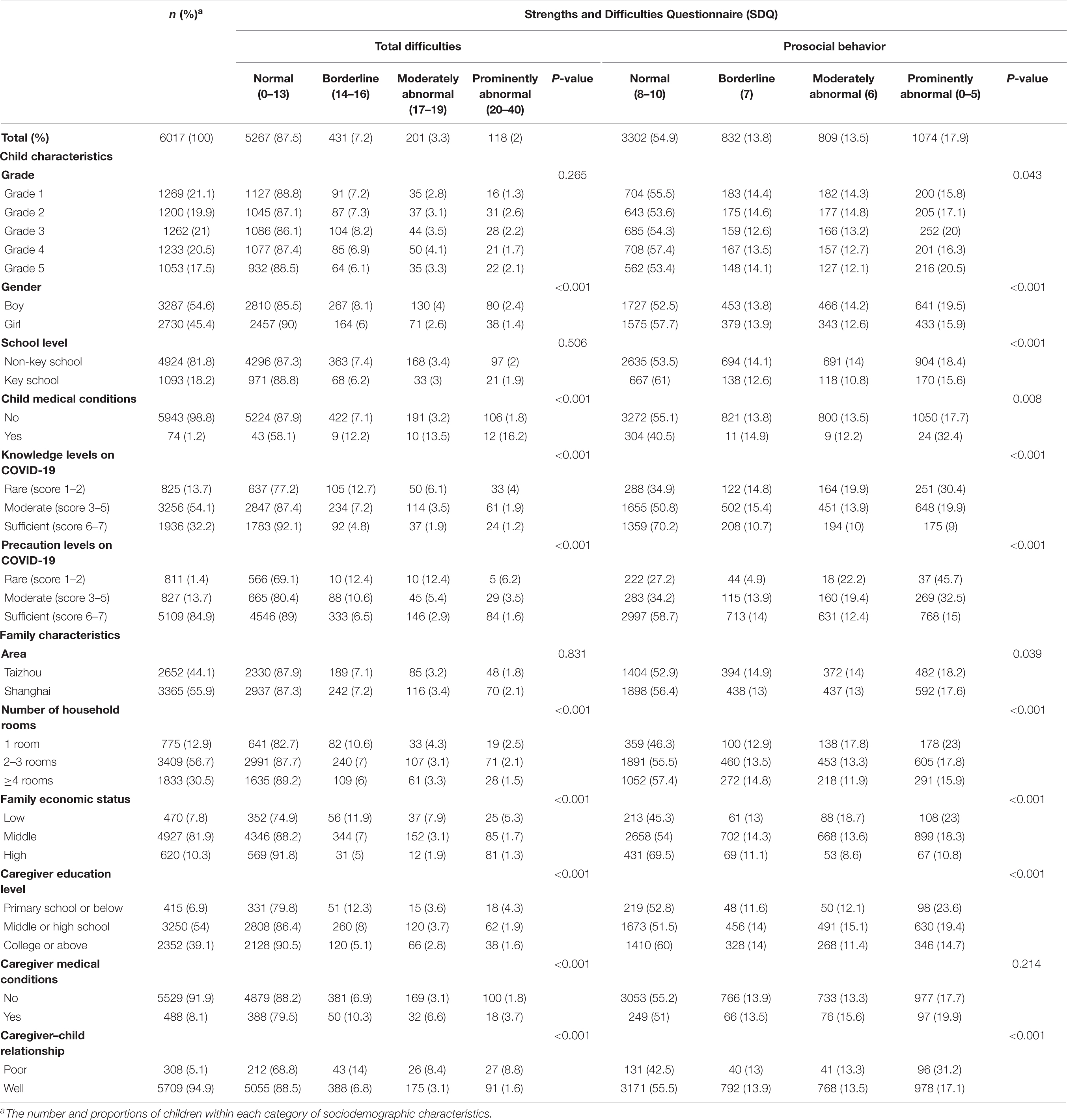
Table 1. Distributions of total difficulties scores and prosocial behavior scores by different characteristics.
Information Collection for Psychological Stressors, Daily Activities, and Social Interactions
Psychological stressors for children were obtained through a self-made questionnaire, regarding the degree to which a child was afraid of each situation after school reopened (1) going to school, (2) lagging behind in school lessons, (3) inadaptation to study and life styles, (4) keeping social distance with others, and (5) changes in relationship with schoolmates. The responses were defined into four levels (“completely not,” “slightly,” “moderately,” and “definitely”). Children’s daily activities and social interactions were also collected, in terms of length of time or frequency a child conducting each in the last week (1) online learning, (2) homework, (3) computer games, (4) physical exercises, (5) telephone or video calling, (6) text messaging or social media communication, and (7) meeting with friends or relatives. The responses were defined into three levels (“≤1,” “1–3,” and “>3 h” for the first three items, “none,” “≤30 min,” and “>30 min” for the fourth item, and “none,” “≤1 time,” and “>1 time” for the last three items) and were presented in Table 2.
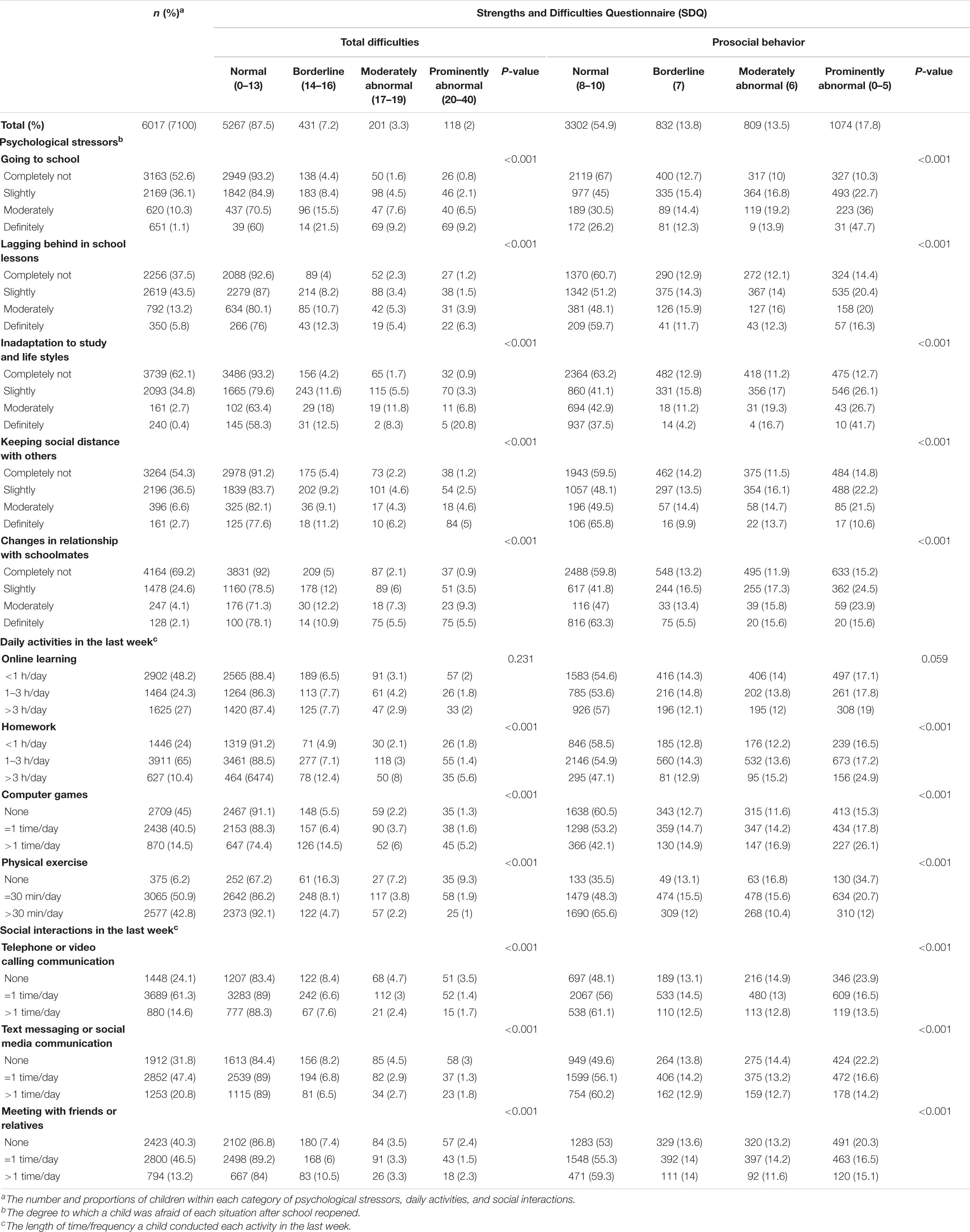
Table 2. Distributions of total difficulties score and prosocial behavior score by psychological stressors, daily activities, and social interactions.
Assessments of Children’s Mental Health
The parent version of the SDQ was adopted to assess mental health of children according to caregivers’ observations (Stone et al., 2010). Five subscales included in SDQ were designed for evaluating emotional symptoms, conduct problems, hyperactivity/inattention, peer relationship problems, and prosocial behavior, respectively. Each subscale includes five items and each item is scored on a 3-point scale (0 = not true, 1 = somewhat true, 2 = certainly true). SDQ is a useful screening tool for identifying mental health difficulties and strengths in children. Total difficulties scores, reflecting emotional, and behavioral difficulties, were calculated by summing the first four of the subscale scores, with higher scores representing greater difficulties. The prosocial behavior scores were calculated by the last subscale, with lower scores indicating less prosocial behavior. Four degrees of total difficulties were defined according to total difficulties subscale scores (“Normal,” score 0–13; “Borderline,” score 14–16; “Moderately abnormal,” score 17–19; and “Prominently abnormal,” score 20–40). Four degrees of prosocial behavior were classified based on prosocial behavior subscale scores (“Normal,” score 8–10; “Borderline,” score 7; “Moderately abnormal,” score 6; and “Prominently abnormal,” score 0–5) (Du et al., 2008). The Chinese version of parent-reported SDQ showed strong internal consistency (Cronbach’s alpha coefficients for the total difficulties scale and the prosocial behavior subscale were 0.81 and 0.87, respectively), and moderate test-retest reliability (Pearson’s correlation coefficients for the total difficulties scale and the prosocial behavior subscale were 0.71 and 0.61, respectively, over a 2-month interval) (Yao et al., 2009). It also had a good parallel validity with Conners Parent Questionnaire in behavioral and emotional problems of Chinese children and adolescents (Kou et al., 2005).
Statistical Analysis
Continuous variables were represented as mean (standard deviation, SD), while categorical variables as frequency (percentage, %). Chi-square test was utilized to compare the prevalence of normal, borderline, moderately abnormal, and prominently abnormal scores for total difficulties and prosocial behavior, respectively, among children with different characteristics. Grade (1–5) and age (5–13 years) were highly correlated (Spearman correlation coefficients: 0.963), and grade variable was selected for further analysis because there were several missing values for age. Ordinal logistic regression analyses were used to evaluate the impact of psychological stressors, daily activities, and social interactions on total difficulties and prosocial behavior according to the four categories of SDQ scores, based on the crude model (Model 1) and the adjusted model (Model 2). Model 2 adjusted for child characteristics (grade, gender, school level, child medical conditions, knowledge levels on COVID-19, and precaution levels on COVID-19) and family characteristics (including area, number of household rooms, economic status, education of caregiver, caregiver medical conditions, and caregiver–child relationship). The Brant test showed that the proportional odds assumption was met. The results were presented as odds ratios (ORs) and 95% confidence intervals (CIs). Interactions between psychological stressors and sociodemographic characteristics were tested. Stratified analyses were conducted according to grade, gender, school level, area, and caregiver–child relationship with interaction terms in the regression models to further observe the associations of total difficulties and prosocial behavior with the number of psychological stressors. The level of statistical significance was defined as α = 0.05 of two-side probability. All analyses were performed by R program (version 4.0.4, R Foundation for Statistical Computing, Vienna, Austria), and all figures were performed by GraphPad Prism software (version 7, GraphPad Prism, CA, United States).
Results
Distributions of Total Difficulties Scores and Prosocial Behavior Scores
Of those eligible participants (n = 6017), the mean score of SDQ on total difficulties and prosocial behavior was 8.08 (±4.51) and 7.59 (±1.99), respectively. The prevalence of borderline, moderately abnormal and prominently abnormal scores were 7.16% (n = 431), 3.34% (n = 201), and 1.96% (n = 118) for total difficulties and 13.83% (n = 832), 13.45% (n = 809), and 17.85% (n = 1074) for prosocial behavior, respectively (Table 1). Boys, children with medical conditions (acute or chronic illnesses or mental disorders), children with less knowledge and precautionary measures toward COVID-19, fewer household rooms, lower family economic status, lower caregiver education level and poor caregiver–child relationship were more likely to have both abnormal total difficulties scores and prosocial behavior scores, compared with the counterparts (P < 0.05). In addition, children in Grade 5, from non-key school, from Taizhou may have less prosocial behavior than their counterparts (P < 0.05). Parents having medical conditions potentially increased their child’s total difficulties (P < 0.05).
Status of Psychological Stressors, Daily Activities, and Social Interactions
When schools reopened, most of children (62.51%, n = 3761) were afraid of, to varying degrees, lagging behind in school lessons. Over 30% of participants were, to some extent, afraid of going to school (47.43%, n = 2854), keeping social distance with others (45.75%, n = 2753), inadaptation to study and life styles (37.86%, n = 2278), and changes in relationship with schoolmates (30.8%, n = 1853). Above 27% (n = 1625) of participants had online learning and 10.42% (n = 627) did homework more than 3 h daily in the last week. The majority did physical exercises (93.77%, n = 5462) and had some types of communication with friends or relatives in the last week, including telephone or video calling (75.93%, n = 4569), text messaging or social media communication (68.22%, n = 4105), and face-to-face meeting (59.73%, n = 3594). More than half of children (54.98%, n = 3308) played computer games in the past week. All these psychological stressors, daily activities, and social interactions, except online learning, had an impact on total difficulties and prosocial behavior scores (P < 0.001) (Table 2).
Associations Between Psychological Stressors, Daily Activities, Social Interactions, and Strengths and Difficulties Questionnaire Scores
Results of ordinal logistic regression analyses were shown in Table 3. Compared with children without psychological stressors, those with concerns had a significantly higher risk of being in a worse category of mental health status after schools reopened. The associations between psychological stressors and total difficulties were progressively stronger in children with increased degrees of concerns, with the maximum adjusted OR of 7.90 (95% CI 3.33–18.75) observed in those who were definitely afraid of inadaptation to study and life styles. The associations for prosocial behavior were more moderate, with the maximum adjusted OR of 4.54 (95% CI 2.80–7.34) observed in those who were definitely afraid of going to school. Time used in home work and computer games was positively related to mental health problems, while frequency of communication with others was negatively related. Children who did physical exercises at least half an hour daily in the last week were less likely to be in a worse category of total difficulties (OR = 0.27, 95% CI 0.21–0.36) and of prosocial behavior (OR = 0.41, 95% CI 0.34–0.51), compared with those who did not.
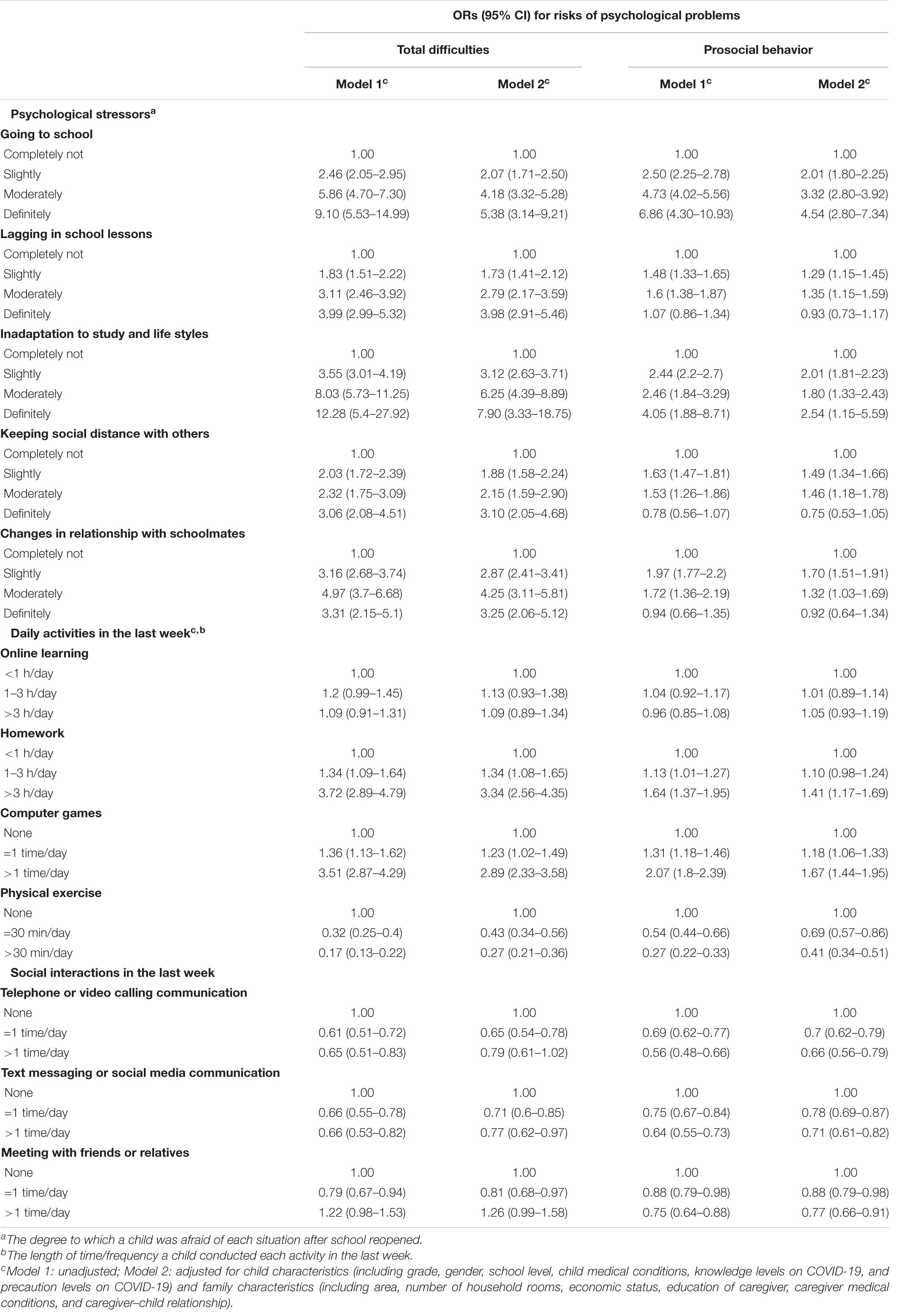
Table 3. Associations of total difficulties and prosocial behavior with psychological stressors, daily activities, and social interactions by ordinal logistic regression models.
Associations Between Psychological Stressors and Strengths and Difficulties Questionnaire Scores Stratified by Sociodemographic Characteristics
There was an accumulative effect of the number of psychological stressors on total difficulties and prosocial behavior. The magnitude of risk to total difficulties varied in children with different characteristics in stratified analyses (Figure 2). Compared with children without psychological stressors, those with two or more stressors were more likely to be in a worse category of total difficulties, and the results were more evident in middle-high grade (Grade 3–5) students (OR = 7.52, 95% CI 4.16–8.61), boys (OR = 6.95, 95% CI 4.83–8.55), those who lived in Taizhou (OR = 7.62, 95% CI 4.72–8.61) and with poor caregiver–child relationship (OR = 7.79, 95% CI 2.26–8.65) (Figure 2A). Key school students and those with poor caregiver–child relationship were more vulnerable to the effects of psychological stressors on prosocial behavior, with the corresponding adjusted ORs of 2.75 (95% CI 1.81–4.18) and 3.29 (95% CI 1.38–7.86), respectively (Figure 2B).
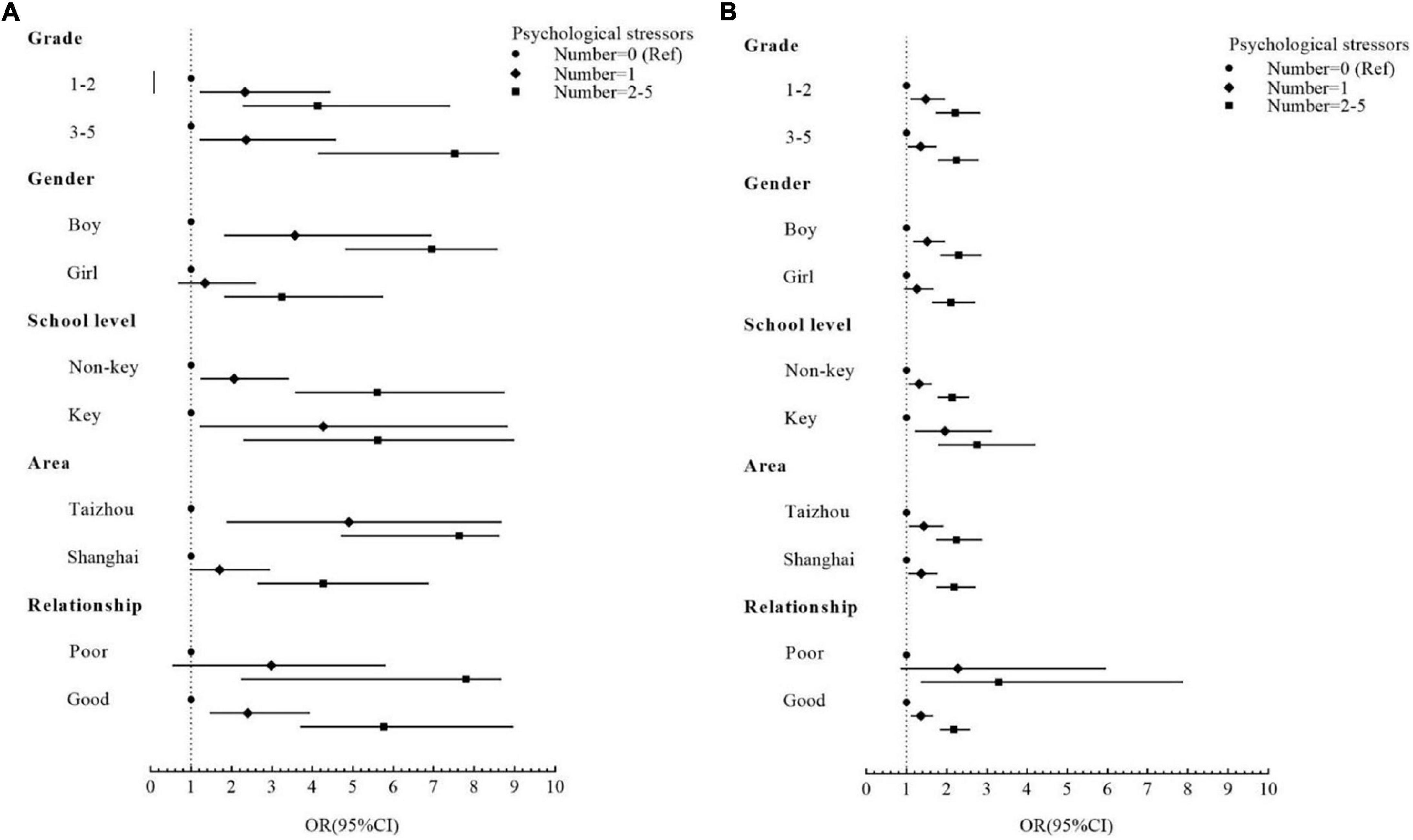
Figure 2. Odds ratio (ORs) and 95% confidence intervals (95% CIs) for risk of (A) total difficulties and (B) prosocial behavior by the effects of the number of psychological stressors after being stratified by grade, gender, school level, area, and caregiver–child relationship based on Model 2.
Discussion
In this current study, we observed that the prevalence of borderline to prominently abnormal scores was 12.46% for total difficulties and 45.12% for prosocial behavior, respectively, among primary school students after schools reopened. In addition, the prevalence of prominently abnormal scores was 1.96% for total difficulties and 17.85% for prosocial behavior. Psychological stressors caused by school reopening and social distancing measures, and longer time involved in homework and computer games were related to increased risks of mental health problems. In contrast, more physical exercise and more social interactions may have beneficial effects on mental health. Moreover, boys, middle-high grade (Grade 3–5) or key school students, those living in Taizhou and those with poor caregiver–child relationship were more sensitive to the effect of psychological stressors on mental health status.
The mean score of total difficulties was 8.08 (±4.51) among 6017 students (aged 5–13 years) in this study, which was lower than that of 9.63 (±4.79) among the 1264 students (aged 7–12 years) in a study conducted in Hubei Province, China, between February 25 and March 8, 2020 (the total difficulties were measured using the Chinese version of parent-reported SDQ for grades 2–3 and the Chinese version of self-reported SDQ for grades 4–6) (Liu et al., 2020), and much lower than that of 11.59 (±5.57) among 17,029 children (aged 6–12 years) in a study conducted in Hong Kong, China, in late March 2020 (using the Chinese version of parent-reported SDQ) (Tso et al., 2020). These findings suggested that, compared with children under school closure and home confinement, those who returned to school may experience less mental health difficulties. School routine consists an important coping mechanism for children to maintain mental health, allowing them to have a regular schedule, interact with their peers, and focus on achieving meaningful goals (Lee, 2020). In addition, we did not observe a higher mean score of total difficulties in the current study than that of children (10.89 ± 4.84, aged 3–10 years) in Shanghai prior to COVID-19 (using the Chinese version of parent-reported SDQ) (Du et al., 2008). There is a cumulative risk theory that short term exposure to trauma and adversities may not obviously affect children’s emotional and behavioral problems, but make them more vulnerable to disadvantages experienced at a later stage (Gutman et al., 2019). Therefore, longitudinal research on children’s mental health is necessary to further understand the long-term effect of the COVID-19 pandemic.
Prosocial behavior typically refers to a large class of voluntary behaviors that share the common intention to benefit another, by helping, sharing, comforting, informing, and cooperating (Dunfield and Kuhlmeier, 2013). In this study, 17.85% children reported having prominently abnormal prosocial behavior scores, the prevalence of which was higher than that of children in Hubei Province during the early period of home quarantine (10.3%) (Liu et al., 2020), and that of children in Shanghai prior to COVID-19 (9.1%) (Du et al., 2008). However, prosocial score ≤4 was used as a cutoff score for prosocial problems in the above studies, while a score ≤5 was considered as prominently abnormal in this study according to a newer 4-band categorization recommended by the inventors of SDQ (Youthinmind, 2021). The mean score of prosocial behavior in our study (7.59 ± 1.99) was comparable to theirs during home confinement (7.24 ± 2.19) (Liu et al., 2020), but higher than that of Chinese children before the pandemic (5.7 ± 2.2–6.6 ± 2.1) (using the Chinese version of parent-reported SDQ) (Gao et al., 2013). It is noteworthy that the prevalence of prosocial behavior problems was high in children during the pandemic period when a set of new norms were created and unique stressors were faced by students (McDonald, 2020).
In this study, children who experienced psychological stressors and who were involved in longtime homework or computer games were less likely to present prosocial behavior. The consequences of 3- to 4-month gap in normal schooling might be extensive with adverse impacts on learning motivation, self-control, and social competence (Fontenelle-Tereshchuk, 1984). We found that more than 30% of children were afraid of inadaptation to social activities after schools reopened, such as keeping social distance with others (45.75%) and changes in relationship with schoolmates (30.8%). Some children might be unwilling to be close to others due to concerns over the spread of coronavirus and thus expressed less prosocial behaviors. Chronic stress has also been reported to reduce social motivation and social interactions, while social stressors such as social isolation may increase aggressiveness (Sandi and Haller, 2015). Although these students have returned to the campus, some children might fail to complete the transition to normal lives. Long exposure to digital screens and addiction to computer games may cause reduced vision and sedentary lifestyle (Mittal et al., 2020), leading to physical and mental health problems (Lemola et al., 2015; Alhassan et al., 2018). Therefore, the chronic stress children experienced and the long-time isolated lives before the schools reopened were detrimental to their prosocial behaviors. In addition, our findings showed that physical exercises and social interactions were protective factors for prosocial behavior. Consistent with our study, a research conducted in the United States found a significant relationship between prosocial behavior and moderate-intensity physical exercise (Moore et al., 2020). In terms of social interactions, Barry and Wentzel reported that the quantity and quality of social contact moderated relations between a friend’s prosocial behavior and an individual’s prosocial goal pursuit, which in turn, affected the individual’s prosocial behavior (Barry and Wentzel, 2006).
The magnitude of the risk of psychological stressors to emotional and behavioral problems was different across participants, and was larger in boys, middle-high grade or key school students, children with poor caregiver–child relationship and living in Taizhou. During the long-time period of schooling at home, children had limited interaction with teachers and classmates, and largely relied on their parents or other main caregivers for emotional and academic support (Fontenelle-Tereshchuk, 1984). Parenthood is a demanding role, particularly under the influence of COVID-19 pandemic. Parents had to manage multiple tasks and spend much more time with their children, thus increasing the risk of conflict between them. A study conducted in Taizhou reported that when students had study problems due to school closures, those with poor parent–child relationship were particularly vulnerable to depressive symptoms (Wang et al., 2021). On the contrary, harmonious parent–child relationship, especially parental supportive behaviors and responsive parenting, tend to alleviate the effects of stressors on children’s mental health and promote their prosocial behavior (Eisenberg et al., 2019; Tang et al., 2020). Boys in childhood may have more hyperactivity issues, more conduct problems and poorer self-discipline than girls (Gao et al., 2013), and thus they may experience higher levels of stress and anxiety after returning to campus (Duckworth and Seligman, 2006). Students in higher grade and key schools tend to have more academic pressure and achievement expectation than the others. Schooling at home for a long time may take a toll on their study progress and is especially a stressor to these students (Tang et al., 2020). The safety measures on campus for pandemic control after school reopening, to some degree, restricted physical activities and social interactions for children, and included repeated nucleic acid testing which may lead to a new round of psychological anxiety and emotional distress (Wu, 2020). The time of school reopening in Taizhou was approximately 1 month earlier than in Shanghai, and thus children living in Taizhou might be more greatly affected by stricter safety measures. In the current study, 85.7% children in Taizhou experienced psychological stressors, while 82.5% in Shanghai. In addition, the percentages of boys (56.7 vs. 43.3%, P = 0.003) and those who studied in key schools (30.9 vs. 8.1%, P < 0.001) were significantly larger in Taizhou than those in Shanghai, which may in part explain the regional difference in the results.
To our knowledge, this is the first study to evaluate the mental health status of primary school students after schools reopened during the COVID-19 post-pandemic in China, with a large sample size and a hot issue warranted to be paid more attention in the current society. Understanding children’s reactions and resilience to great changes in their lives in difficult times is essential to properly address their needs and promote their mental well-being. Our study provides a preliminary understanding of behavioral and emotional problems, as well as their related factors of primary school students in two regions in east China after a period of school reopening. It is noteworthy that school reopening could be a psychological stressor per se. Students need to face inadaptation to lifestyle changes again and social distance requirements. School psychologists need to increase their level of service to support students’ transition back into the school building and address emotional and behavioral problems.
The results of this study should be interpreted with a number of limitations. First, this was a cross-sectional study, so we were unable to collect detailed information on the mental health status of children before schools reopened. However, we had a question of child medical conditions which included psychiatric illnesses, and we adjusted for this variable in the regression models. Future longitudinal studies will allow a better understanding of the long-term effects of the COVID-19 outbreak on children’s psychological adjustment. Second, subjects in this study were residing in two regions in east China, and the findings may not be fully applicable to children living in other areas. Third, the information of children was collected from their caregivers, and the potential bias inherent in this study should be noted. Although our study has some limitations, the results could help to inform future research to enable children’s mental well-being and minimize their distress. More focused research should be performed directly on testimony to children’s experience during the pandemic apart from indirect information collected from their caregivers. Qualitative research could be considered to fully understand children’s feelings and identify approaches in which the negative impact of COVID-19 might be alleviated. Future research should also endeavor to ascertain the longer-term consequences of the pandemic on psychological well-being for children, determine the mechanisms which explain the prevalence of emotional and behavioral difficulties, and develop novel interventions to improve mental health such as those based on altruism and prosocial behavior (Holmes et al., 2020).
The present study has some important implications. The Chinese government, community, school, and family need to provide more effective support for children after school reopened. The government needs to recognize the public health challenge of children’s mental health, ensure multifaceted and coordinated actions between schools, local health professionals, and other organizations, and provide sufficient funding to support relevant research and practice. Communities can collaborate with mental health professionals in providing online and offline psychological services for high-risk individuals, and specialized psychoeducation for children and their caregivers to improve coping strategies and resilience for stressful life changes and negative situations. Schools should try to alleviate students’ academic pressure by reducing non-essential homework and class ranking, and set up some engaging lessons related to emotion management, positive psychology, and so on. Teachers should pay more attention to students’ emotional and behavioral problems, and refer students with difficulties to school psychologists. Caregivers need to provide consistent and sensitive care as well as age-appropriate information about the pandemic, and opportunities for kids to talk about their concerns (Dalton et al., 2020). Furthermore, caregivers and teachers should foster children’s prosocial tendency, as helping others might distract an individual from stressors and increase one’s sense of meaning, purpose, and self-efficacy (Raposa et al., 2016). Prosocial behavior has also been identified as an important contributor to resilience for kids experiencing hardship (Daud et al., 2008). Evidence suggested that keeping in touch with friends and family can ease mental distresses (Feng and Astell-Burt, 2016), and the similar results were also indicated in this study. During the pandemic, adults should help children find effective approaches to staying connected such as online video chats. It is also important to encourage children to engage in restorative activities that help them self-regulate, e.g., physical exercise and outdoor activities which may lead to reduced anxiety, improvements in self-esteem, and cognitive performance (Biddle and Asare, 2011).
Conclusion
Emotional and behavioral difficulties, especially prosocial behavior problems, existed in primary school children after schools reopened, which may be aggravated by psychological stressors, longtime home work, and excessive computer games. Conversely, more physical exercise and social interactions may alleviate these mental health problems. Boys, middle-high grade or key school students, and those with poor caregiver–child relationship may be especially vulnerable to psychological stressors during their transition back to school.
Data Availability Statement
The datasets for this manuscript will be made available upon request pending, further inquiries can be directed to the corresponding author CF, ZmN3QGZ1ZGFuLmVkdS5jbg==.
Ethics Statement
The studies involving human participants were reviewed and approved by the Ethical Review Board of School of Public Health of Fudan University. Written informed consent to participate in this study was provided by the participants’ legal guardian/next of kin.
Author Contributions
CF, XG, XC, and HJL designed the study. HW, HJL, and HBL were involved in data collection and assembly. JW and YW analyzed and interpreted the data, and drafted the manuscript as co-first authors. CF and XG reviewed and revised the manuscript. All authors contributed to manuscript writing and approved the final manuscript.
Funding
This work was supported by the Shanghai Leading Academic Discipline Project of Public Health (Grant Numbers GWV-10.1-XK18 and GWV-10.1-XK14).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to thank the study members for their participation. We are grateful to the Taizhou City Center of Disease Prevention and Control (CDC) and Songjiang District Center of Disease Prevention and Control (CDC) for their dedication and hard work.
Footnotes
References
Alhassan, A. A., Alqadhib, E. M., Taha, N. W., Alahmari, R. A., Salam, M., and Almutairi, A. F. (2018). The relationship between addiction to smartphone usage and depression among adults: a cross sectional study. BMC Psychiatry 2018:18.
Barry, C. M., and Wentzel, K. R. (2006). Friend influence on prosocial behavior: The role of motivational factors and friendship characteristics. Dev. Psychol. 42, 153–163. doi: 10.1037/0012-1649.42.1.15
Biddle, S. J. H., and Asare, M. (2011). Physical activity and mental health in children and adolescents: a review of reviews. Br. J. Sports Med. 45, 886–895. doi: 10.1136/bjsports-2011-090185
CCTV News (2021). Ministry of Education: national elementary and middle school network cloud platform opens for free use today. Feb 17, 2020. Available online at: http://www.chinanews.com/sh/2020/02-17/9094648.shtml (accessed January 29, 2021).
Cusinato, M., Iannattone, S., Spoto, A., Poli, M., Moretti, C., Gatta, M., et al. (2020). Stress, Resilience, and Well-Being in Italian Children and Their Parents during the COVID-19 Pandemic. Int. J. Env. Res. Public Health 17:22.
Dalton, L., Rapa, E., and Stein, A. (2020). Protecting the psychological health of children through effective communication about COVID-19. Lancet Child Adolescent Health. 4, 346–347. doi: 10.1016/s2352-4642(20)30097-3
Daud, A., Klinteberg, B., and Rydelius, P. A. (2008). Resilience and vulnerability among refugee children of traumatized and non-traumatized parents. Child Adolesc Psychiatry Ment Health. 2:7. doi: 10.1186/1753-2000-2-7
Du, Y., Kou, J., and Coghill, D. (2008). The validity, reliability and normative scores of the parent, teacher and self report versions of the Strengths and Difficulties Questionnaire in China. Child Adol. Psych. Men. 2, 8–8. doi: 10.1186/1753-2000-2-8
Duan, L., Shao, X., Wang, Y., Huang, Y., Miao, J., Yang, X., et al. (2020). An investigation of mental health status of children and adolescents in china during the outbreak of COVID-19. J. Affect Disord. 275, 112–118. doi: 10.1016/j.jad.2020.06.029
Duckworth, A. L., and Seligman, M. E. P. (2006). Self-discipline gives girls the edge: Gender in self-discipline, grades, and achievement test scores. J. Educ. Psychol. 98, 198–208. doi: 10.1037/0022-0663.98.1.198
Dunfield, K. A., and Kuhlmeier, V. A. (2013). Classifying prosocial behavior: children’s responses to instrumental need, emotional distress, and material desire. Child Dev. 84, 1766–1776. doi: 10.1111/cdev.12075
Eisenberg, N., Spinrad, T. L., Taylor, Z. E., and Liew, J. (2019). Relations of Inhibition and Emotion-Related Parenting to Young Children’s Prosocial and Vicariously Induced Distress Behavior. Child Dev. 90, 846–858. doi: 10.1111/cdev.12934
Ezpeleta, L., Navarro, J. B., de la Osa, N., Trepat, E., and Penelo, E. (2020). Life Conditions during COVID-19 Lockdown and Mental Health in Spanish Adolescents. Int. J. Env. Res. Public Health 17:19.
Feng, X., and Astell-Burt, T. (2016). What types of social interactions reduce the risk of psychological distress? Fixed effects longitudinal analysis of a cohort of 30,271 middle-to-older aged Australians. J. Affect Disord. 204, 99–102. doi: 10.1016/j.jad.2016.06.041
Fontenelle-Tereshchuk, D. (1984). Mental Health and the COVID-19 Crisis: The Hopes and Concerns for Children as Schools Re-open. Interchange 2020, 1–16. doi: 10.1007/s10780-020-09413-1
Fumanelli, L., Ajelli, M., Merler, S., Ferguson, N. M., and Cauchemez, S. (2016). Model-Based Comprehensive Analysis of School Closure Policies for Mitigating Influenza Epidemics and Pandemics. PLoS Comp. Biol. 12:e1004681. doi: 10.1371/journal.pcbi.1004681
Gao, X., Shi, W., Zhai, Y., He, L., and Shi, X. (2013). Results of the parent-rated Strengths and Difficulties Questionnaire in 22,108 primary school students from 8 provinces of China. Shanghai Arch Psychiatry. 25, 364–374. doi: 10.3969/j.issn.1002-0829.2013.06.005
Guessoum, S. B., Lachal, J., Radjack, R., Carretier, E., Minassian, S., Benoit, L., et al. (2020). Adolescent psychiatric disorders during the COVID-19 pandemic and lockdown. Psychiatry Res. 291:113264.
Gutman, L. M., Joshi, H., and Schoon, I. (2019). Developmental Trajectories of Conduct Problems and Cumulative Risk from Early Childhood to Adolescence. J. Youth Adolesc. 48, 181–198. doi: 10.1007/s10964-018-0971-x
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7, 547–560. doi: 10.1016/S2215-0366(20)30168-1
Jiao, W. Y., Wang, L. N., Liu, J., Fang, S. F., Jiao, F. Y., Pettoello-Mantovani, M., et al. (2020). Behavioral and Emotional Disorders in Children during the COVID-19 Epidemic. J. Pediatr. 221:264. doi: 10.1016/j.jpeds.2020.03.013
Khan, A. H., Sultana, M. S., Hossain, S., Hasan, M. T., Ahmed, H. U., and Sikder, M. T. (2020). The impact of COVID-19 pandemic on mental health & wellbeing among home-quarantined Bangladeshi students: A cross-sectional pilot study. J. Affect Disord. 277, 121–128.
Kou, J., Du, Y., and Xia, L. (2005). Reliability and validity of “children strengths and difficulties questionnaire” in Shanghai norm. Shanghai Archiv. Psychiatry 17, 25–28.
Lee, J. (2020). Mental health effects of school closures during COVID-19. Lancet Child Adolesc. Health 4:421.
Lemola, S., Perkinson-Gloor, N., Brand, S., Dewald-Kaufmann, J. F., and Grob, A. (2015). Adolescents’ Electronic Media Use at Night, Sleep Disturbance, and Depressive Symptoms in the Smartphone Age. J. Youth Adolesc. 44, 405–418.
Li, W., Zhang, Y., Wang, J., Ozaki, A., Wang, Q., Chen, Y., et al. (2021). Association of Home Quarantine and Mental Health Among Teenagers in Wuhan, China, During the COVID-19 Pandemic. JAMA Pediatr. 2021:2021.
Liu, Q., Zhou, Y., Xie, X., Xue, Q., et al. (2020). The prevalence of behavioral problems among school-aged children in home quarantine during the COVID-19 pandemic in china. J. Affect Disord. 279, 412–416. doi: 10.1016/j.jad.2020.10.008
McDonald, C. C. (2020). Reopening Schools in the Time of Pandemic: Look to the School Nurses. J. Sch. Nurs. 36, 239–240. doi: 10.1177/1059840520937853
Mittal, V. A., Firth, J., and Kimhy, D. (2020). Combating the Dangers of Sedentary Activity on Child and Adolescent Mental Health During the Time of COVID-19. J. Am. Acad. Child Adolesc. Psychiatry 59, 1197–1198. doi: 10.1016/j.jaac.2020.08.003
Moore, Q. L., Kulesza, C., Kimbro, R., Flores, D., and Jackson, F. (2020). The Role of Prosocial Behavior in Promoting Physical Activity, as an Indicator of Resilience, in a Low-Income Neighborhood. Behav. Med 46, 353–365. doi: 10.1080/08964289.2020.1712647
People’s Daily Online (2021b). The safe and orderly schools reopening has been ensured for students from schools at all levels and all types in Xinjiang Province. Available online at: http://xj.people.com.cn/n2/2020/0315/c186332-33877428.html (accessed January 29, 2021)
People’s Daily Online (2021a). The reopening dates for schools at all levels and all types in Hebei Province has been announced. Available online at: http://he.people.com.cn/n2/2020/0516/c192235-34022234.html (accessed January 29, 2021)
Raposa, E. B., Laws, H. B., and Ansell, E. B. (2016). Prosocial Behavior Mitigates the Negative Effects of Stress in Everyday Life. Clin. Psychol. Sci. 4, 691–698. doi: 10.1177/2167702615611073
Sandi, C., and Haller, J. (2015). Stress and the social brain: behavioural effects and neurobiological mechanisms. Nat. Rev. Neurosci. 16, 290–304. doi: 10.1038/nrn3918
Saurabh, K., and Ranjan, S. (2020). Compliance and Psychological Impact of Quarantine in Children and Adolescents due to Covid-19 Pandemic. Indian J. Pediatr. 87, 532–536. doi: 10.1007/s12098-020-03347-3
Sprang, G., and Silman, M. (2013). Posttraumatic Stress Disorder in Parents and Youth After Health-Related Disasters. Disaster Med. Public Health Prep. 7, 105–110. doi: 10.1017/dmp.2013.22
Stone, L. L., Otten, R., Engels, R., Vermulst, A. A., and Janssens, J. (2010). Psychometric Properties of the Parent and Teacher Versions of the Strengths and Difficulties Questionnaire for 4-to 12-Year-Olds: A Review. Clin. Child Fam. Psychol. Rev. 13, 254–274. doi: 10.1007/s10567-010-0071-2
Tang, S., Xiang, M., Cheung, T., and Xiang, Y.-T. (2020). Mental health and its correlates among children and adolescents during COVID-19 school closure: The importance of parent-child discussion. J. Affect. Disord. 279, 353–360. doi: 10.1016/j.jad.2020.10.016
Tso, W. W. Y., Wong, R. S., Tung, K. T. S., Rao, N., Fu, K. W., Yam, J. C. S., et al. (2020). Vulnerability and resilience in children during the COVID-19 pandemic. Eur. Child Adolesc. Psych. 2020, 1–16.
Wang, G., Zhang, Y., Zhao, J., Zhang, J., and Jiang, F. (2020). Mitigate the effects of home confinement on children during the COVID-19 outbreak. Lancet 395, 945–947. doi: 10.1016/s0140-6736(20)30547-x
Wang, J., Wang, H., and Lin, H. (2021). Study problems and depressive symptoms in adolescents during the COVID-19 outbreak: poor parent-child relationship as a vulnerability. Global Health. 17:40. doi: 10.1186/s12992-021-00693-5
World Health Organization (WHO) (2021). Coronavirus disease 2019 (COVID-19) Situation Report – 77. Available online at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200406-sitrep-77-covid-19.pdf. (accessed January 29, 2021)
Wu, X. (2020). Thinking on the Integration of Students’ Psychological Counseling and Campus Safety Management under the Situation of Epidemic Prevention and Control——Comment on Safety Management of Primary and Secondary Schools. China Safety Sci. J. 30, 191–192.
Xie, X., Xue, Q., Zhou, Y., Zhu, K., Liu, Q., Zhang, J., et al. (2020). Mental Health Status Among Children in Home Confinement During the Coronavirus Disease 2019 Outbreak in Hubei Province, China. JAMA Pediatr. 174, 898–900. doi: 10.1001/jamapediatrics.2020.1619
Yao, S., Zhang, C., Zhu, X., Jing, X., McWhinnie, C. M., and Abela, J. R. (2009). Measuring adolescent psychopathology: psychometric properties of the self-report strengths and difficulties questionnaire in a sample of Chinese adolescents. J Adolesc Health. 45, 55–62. doi: 10.1016/j.jadohealth.2008.11.006
Youthinmind (2021). The Strengths & Difficulties Questionnaire English (UK). Available online at: https://www.sdqinfo.org/py/sdqinfo/b3.py?language=Englishqz(UK). (accessed May 23, 2021)
Zhang, J., Litvinova, M., Liang, Y., Wang, Y., Wang, W., Zhao, S., et al. (2020). Changes in contact patterns shape the dynamics of the COVID-19 outbreak in China. Science 368:1481.
Zhao, Y., Guo, Y., Xiao, Y., Zhu, R., Sun, W., Huang, W., et al. (2020). The Effects of Online Homeschooling on Children, Parents, and Teachers of Grades 1-9 During the COVID-19 Pandemic. Med. Sci. Monit. 26:e925591. doi: 10.12659/MSM.925591
Zhou, S., Zhang, L., Wang, L., Guo, Z. C., Wang, J. Q., Chen, J. C., et al. (2020). Prevalence and socio-demographic correlates of psychological health problems in Chinese adolescents during the outbreak of COVID-19. Eur. Child Adoles. Psy. 29, 749–758.
Keywords: mental health, psychological stressors, children, school reopening, COVID-19
Citation: Wang J, Wang Y, Lin H, Chen X, Wang H, Liang H, Guo X and Fu C (2021) Mental Health Problems Among School-Aged Children After School Reopening: A Cross-Sectional Study During the COVID-19 Post-pandemic in East China. Front. Psychol. 12:773134. doi: 10.3389/fpsyg.2021.773134
Received: 09 September 2021; Accepted: 18 October 2021;
Published: 11 November 2021.
Edited by:
Stefano Triberti, University of Milan, ItalyReviewed by:
Manuela Altieri, University of Campania “Luigi Vanvitelli”, ItalyHeba Saadeh, The University of Jordan, Jordan
Copyright © 2021 Wang, Wang, Lin, Chen, Wang, Liang, Guo and Fu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chaowei Fu, ZmN3QGZ1ZGFuLmVkdS5jbg==; Xiaoqin Guo, Z3VveGlhb3FpbjExMDJAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Jingyi Wang
Jingyi Wang Yingying Wang
Yingying Wang Haijiang Lin2
Haijiang Lin2 Xiaoxiao Chen
Xiaoxiao Chen Hao Wang
Hao Wang Xiaoqin Guo
Xiaoqin Guo Chaowei Fu
Chaowei Fu