
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychol. , 02 December 2021
Sec. Health Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.748133
Introduction: High rates of burnout, depression, anxiety, and insomnia in healthcare workers responding to the COVID-19 pandemic have been reported globally.
Methods: Responding to the crisis, the Foundation for Professional Development (FPD) developed an e-learning course to support healthcare worker well-being and resilience. A self-paced, asynchronous learning model was used as the training intervention. Each module included practical, skill-building activities. An outcome evaluation was conducted to determine if completing the course improved healthcare worker knowledge of and confidence in the learning outcomes of the course, their use of resilience-building behaviours, their resilience, and their well-being. A secondary objective was to explore if there were any associations between behaviours, resilience, and well-being. Participants completed pre- and post-course questionnaires to measure knowledge of and confidence in the learning outcomes, y, frequency of self-reported resilience-building behaviours, and levels of resilience (CD-RISC) and well-being (WHO-5). Results were analysed in STATA using paired T-tests, univariate and multivariate linear regression models.
Results: Participants (n = 474; 77.6% female; 55.7% primary care) exhibited significant increases in knowledge, confidence, resilience-building behaviour, resilience, and well-being scores. Statistically significant improvements in the frequency of resilience-building behaviours led to significant improvements in resilience (0.25 points; 95% CI: 0.06, 0.43) and well-being (0.21 points; 95% CI: 0.05, 0.36). Increasing changes in well-being scores had a positive effect on change in resilience scores (β = 0.20; 95% CI: 0.11, 0.29), and vice versa (β = 0.28; 95% CI: 0.14, 0.41).
Conclusion: A healthcare worker e-learning course can build knowledge and skills that may prompt changes in resilience-building behaviours and improvements in well-being and resilience scores. The findings suggest that e-learning courses may improve more than competency-based outcomes alone but further research is warranted to further explore these relationships.
Healthcare workers (HCWs) are at high-risk of experiencing mental health problems. Exacerbating this issue is the additional stress and trauma brought on by the COVID-19 pandemic. Several factors contribute to the additional stress experienced by frontline HCWs during a pandemic, including longer working hours under difficult conditions; fear of being infected; and making critical decisions regarding the life and death of patients (Huang et al., 2020; Lai et al., 2020; Pfefferbaum, 2020; Senni, 2020). Studies conducted across the world have shown high rates of burnout, depression, anxiety, and insomnia in HCWs responding to the virus (Kang et al., 2020; Lai et al., 2020; Robertson et al., 2020; Senni, 2020). A cross-sectional study conducted in Wuhan, China found high levels of psychological distress in response to the trauma experienced by HCWs working in COVID-19 hospitals (Lai et al., 2020). This finding is consistent with parallel studies which found symptoms of post-traumatic stress disorder (PTSD) among HCWs who were involved in the SARS outbreak (Wu et al., 2009; Brooks et al., 2018).
The work-related consequences of high levels of stress, burnout and fatigue in frontline HCWs has been well-researched in studies conducted after similar pandemics. Burnout is a state of mental, emotional, or physical exhaustion resulting from workplace stressors (World Health Organization [WHO], 2019). The consequences of burnout can include increases in absenteeism, increases in clinical errors, reduced productivity, breaches in infection control, and poorer quality of care (Gray et al., 2019; Robertson et al., 2020). It is important to acknowledge that systemic efforts are necessary to protect HCWs and reduce their exposure to work-related stressors. However, the role of a healthcare worker is inherently stressful, and it is not always feasible to completely remove all work-related stressors. Research has shown that resilience can act as a “buffer” during high periods of stress and is a protective factor against post-traumatic stress disorder and burnout (Mealer et al., 2012; McCann et al., 2013; Arrogante and Aparicio-Zaldivar, 2017). In addition to efforts to reduce external stressors, there is an opportunity to improve HCWs’ ability to cope with and manage stress by building their resilience as a complementary approach to the necessary systemic efforts required.
It is of critical importance that the mental health of frontline HCWs be prioritised within the COVID-19 response planning and implementation. Several strategies which can be implemented in resource constrained settings have been documented and include training and education of HCWs in mental health literacy, self-help, and mindfulness skills; provision of locally relevant educational material; and creating awareness of available resources and how to access them (Gray et al., 2019; Robertson et al., 2020).
In direct response to the immediate needs of HCWs, the Foundation for Professional Development (FPD) developed a short online five-module course for frontline HCWs on resilience and well-being during COVID-19 in order to minimise the personal and work-related consequences of being on the frontline during a crisis. While the primary objective was to meet the needs of the community, researchers noted that evidence of the impact of e-learning on behaviour and quality of care is often lacking (Maunder et al., 2010; Cook et al., 2011; Ruggeri and Brayne, 2013; Lawn et al., 2017). According to Ruggeri and Brayne (2013), “Health education almost always has a social element, and it is important to evaluate more than just learning and skills to fully understand the benefits of a program.” Researchers in this field highlight the importance of assessing behaviour change using pre- and post-training measures that are objective and reliable (Wutoh et al., 2004; Cook et al., 2011; Ruggeri and Brayne, 2013; Lawn et al., 2017). One particular framework proposed by Kirkpatrick identified four levels for evaluating training effectiveness, namely (1) participant reaction to the training experience; (2) learning outcomes; (3) participant’s behaviour change; and (4) impact on system or organisation (Kirkpatrick, 1994).
Therefore, the secondary objective of this programme implementation, was to explore whether the benefit of the e-learning course could be observed across several levels of Kirkpatrick’s framework (Kirkpatrick, 1994). An outcome evaluation was designed to measure HCW resilience-building behaviours, resilience and wellbeing, and exploratory analyses conducted to inform future course evaluation efforts.
The course content focused on improving HCWs’ knowledge of stress in the workplace, how it has been exacerbated by COVID-19, and improving their ability to manage stress, trauma, and distress using practical strategies. The content was delivered online through narrated presentation slides and additional resources such as journal articles and websites. The training intervention used an asynchronous learning model allowing the HCWs to work through the modules at their own pace when they had time, however, content needed to be completed within a month. The five modules were delivered in brief “knowledge bites” to prevent HCWs being overloaded with information.
The course was designed by a medical doctor with an educational diploma and several years of experience in developing content for training interventions, both online and for contact workshops, and who has developed content for psycho-social rehabilitation, Tuberculosis training for HCWs and other clinical online short courses for General Practitioners. The content of the course was informed by well-known, open source, evidence-based resources that were accessible online (for example resources from the South African Depression and Anxiety Group). Key elements of e-learning interventions, which have been shown to influence learning outcomes include interactivity, skill development, action planning future use of skills, provision of tools for future use, opportunity to practice, repetition, adopting mixed learning approaches, and educational support (Maunder et al., 2010; Lawn et al., 2017; Davies et al., 2018; Regmi and Jones, 2020). As such, the course was designed to be interactive, incorporating quizzes, discussion boards, and practical activities to engage the user and strengthen learning (Figure 1). These activities included self-assessments of burnout and psychological well-being, practicing mindfulness and meditation, and developing a self-care plan. The self-care plan was intended to be used by the HCWs beyond the training and required them to list the self-care practices that they will start engaging in across six categories: Physical (e.g., eat regular and healthy meals, good sleep habits, regular exercise, medical check-ups); Mind/spiritual (e.g., take time for yourself, disconnect from electronic devices, journal, pursue new interests, learn new skills, meditation, access psychotherapy, life coaching, or counselling support); Relationships (e.g., healthy relationships, make time for family/friends, schedule dates with partner/spouse, ask for support from family and friends); Emotions (e.g., engage in positive activities, acknowledge my own accomplishments, express emotions in a healthy way); and Work (e.g., maintain work-life balance, positive relationships with co-workers, time management skills).
The sampling method used for this evaluation was non-probability convenience sampling. The sample included all HCWs who had completed the course by December 2020 and who had completed both the pre- and post-training assessments.
At the time of analysis, 2449 HCWs were enrolled in this course and 750 had completed it. Of the 750 completions, 474 HCWs completed both the pre- and post-training assessments and were included in the analysis (Figure 1).
The evaluation methodology and resultant data collection was based on the first three levels of Kirkpatrick’s framework for evaluating training effectiveness; (1) participant reaction to the training experience; (2) learning outcomes; (3) participant’s behaviour change (Kirkpatrick, 1994). Level 4 data collection and analyses (impact on system or organisation) was out of scope for this evaluation.
The objective of the evaluation was to explore whether the benefit of the e-learning course could be observed across the three levels of Kirkpatrick’s framework. Namely reaction to the training or participant satisfaction (level 1), HCW knowledge of and confidence in the learning outcomes of the course (level 2), and resilience-building behaviours, resilience, and wellbeing (level 3). An exploratory objective was to identify any associations between resilience building behaviours, resilience, and well-being. Data were collected using a satisfaction survey and pre- and post-training assessment that participants completed on the online training portal (Figure 1).
Pre- and post-training knowledge scores were measured using a multiple-choice questionnaire based on the contents of the course (total score of 10). Confidence scores were also measured using a rating scale linked to the learning outcomes of the course (total score of 12). As behaviour could not be directly observed or measured, HCWs were asked to self-report the frequency of engagement in five resilience-building behaviours (total score of 25). These resilience-building behaviours included: using coping mechanisms to deal with stress, engaging in mindfulness and relaxation activities, engaging in self-care behaviours, connecting with a social support network, and discussing the impact of COVID-19 on mental health. Resilience was measured using the validated 10-item Connor-Davidson Resilience Scale (10-item CD-RISC) (Connor and Davidson, 2003). The scale is comprised of 10 items, each rated on a 5-point scale (0–4), with higher scores reflecting greater resilience (total score of 40). The CD-RISC has been validated in the South African context (Jorgensen and Seedat, 2008), specifically in populations that include HCWs (Rogers, 2016a). Well-being was measured using the World Health Organisation-5 well-being index (WHO-5) (World Health Organization [WHO], 1998). The measure comprises of 5 items, each rated on a 6-point scale (0–5), with higher scores suggesting better well-being (total score of 25). The WHO-5 has been used extensively worldwide, including in South Africa (Soares et al., 2009). Demographic data were collected from participants’ registration forms.
Mean pre- and post-training scores were calculated and statistically compared using paired sample t-test. Crude linear regressions were used to estimate associations between the change (from pre- to post-training) in well-being and resilience and the change in knowledge, confidence, resilience-building behaviours, or socio-demographics individually. Pre-training well-being and resilience scores were included regardless of the P-value to account for varying baseline levels. Factors with a P-value ≤ 0.05 were included together in a multivariable linear regression model to adjust for potential confounding variables. All model coefficients were interpreted as the mean change of well-being or resilience scores for every one-point increase in the change of each factor of interest, adjusting for other covariates in the model such as socio-demographics, baseline scores, and resilience-building behaviours. Descriptive and multivariable analyses were performed with STATA 13.1 software (StataCorp, College Station, TX, United States).
Of the 750 HCWs who had completed the course as of December 2020, 474 completed both the pre- and post-training assessments and were included in the analysis. Most participants were female (77.6%), from South Africa (96.4%), working with outpatients (37.1%), in an urban setting (64.5%), in the public sector (51.1%) (Table 1). A variety of occupations participated and completed the course with the top three being: (1) medical practitioners (16.1%), (2) Physio, Chiro, Dietician, Biokineticist, Podiatry (14.0%), and (3) Registered counsellor, psychologist, social worker (14.0%) (Table 1).
The HCWs who participated in the course reported high levels of satisfaction with their experience, providing an overall average satisfaction rating of 4.4 out of 5 (on a Likert scale from 1: very poor to 5: excellent) for the e-learning course.
In the pre-training questionnaire, most participants were found to have high levels of knowledge (71%) and moderate levels of confidence (50%) in the learning outcomes. The post-training assessment provided evidence of statistically significant increases in the knowledge (mean increase: 1.52 points, P-value: 0.00) and confidence (mean increase: 4.94 points, P-value: 0.00) of HCWs (Figure 2).
Statistical analyses of the mean pre- and post-training scores revealed significant increases in self-reported resilience-building behaviours (mean increase: 3.06 points; P-value: 0.00), resilience (mean increase: 3.31 points; P-value: 0.00), and wellbeing (mean increase: 2.58; P-value: 0.00) of HCWs (Figure 2).
Increases in changes of behaviour and resilience scores had a significant, positive effect on change in well-being, when adjusting for the other course domains. Further analysis revealed that changes in specific behaviours influenced well-being scores (Table 2). Increasing the use of coping mechanisms for stress was associated with a 0.48-point increase in the change in well-being scores (95% CI: 0.10, 0.86) while increasing the use of self-care behaviours was associated with a 0.46-point increase change in well-being scores when adjusting for other significant factors (95% CI: 0.11, 0.80). Increasing changes in resilience scores had a positive effect on well-being scores, when adjusting for significant covariates (β = 0.20; 95% CI: 0.11, 0.29). No sociodemographic factors were statistically associated with changes in well-being score when adjusting for other covariates.
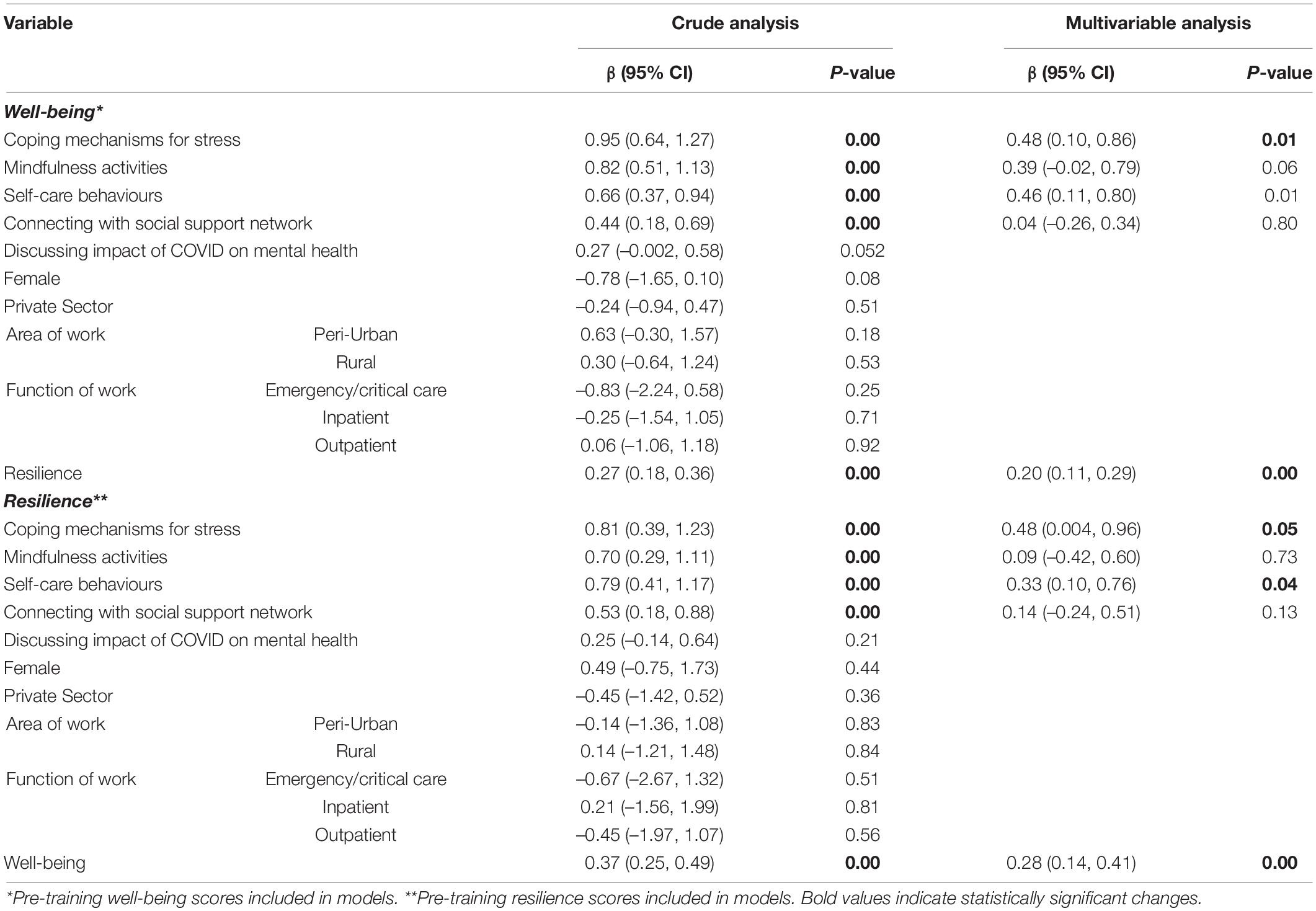
Table 2. Changes in specific behaviours and socio-demographics predicting well-being or resilience (crude and multivariable analysis).
Increases in changes in behaviour and well-being scores had a significant, positive effect on change in resilience scores, when adjusting for the other course domains. Increasing the use of specific behaviours influenced resilience scores when adjusting for other factors (Table 2). Specifically, increasing the use of coping mechanisms for stress and self-care behaviours were associated with increased changes of resilience scores (coping mechanisms for stress increase: 0.48; 95% CI: 0.004, 0.96; self-care behaviours increase: 0.33; 95% CI: 0.10, 0.76). Increasing changes in well-being scores had a positive effect on changes of resilience scores, when adjusting for significant covariates (β = 0.28; 95% CI: 0.14, 0.41). No sociodemographic factors were statistically associated with changes in resilience score when adjusting for other covariates.
E-learning has become an accepted approach to continuing professional development (CPD) within health profession education as the nature of e-learning is suited to the rapidly changing field and HCWs’ need for flexible delivery (Regmi and Jones, 2020). There is evidence to support the value of technology-enhanced e-learning for healthcare worker CPD (Wutoh et al., 2004; Ruiz et al., 2006; Davis et al., 2007; Cook et al., 2011; Kuiler et al., 2012; Lawn et al., 2017) and previous research has shown that technology-enhanced education is associated with improved outcomes when compared to no intervention, including effects on HCW behaviour and patient care (Cook et al., 2011).
The evaluation of this course suggests that the benefit of e-learning interventions may be observed across the first three levels of Kirkpatrick’s framework including knowledge, confidence, resilience-building behaviours, well-being, and resilience. The framework used for this evaluation is similar to the evaluation model set out by Ruggeri and Brayne (2013) which assesses the following elements of e-learning in health; baseline participant characteristics, programme outcomes and benefits, appropriateness of content for e-learning, and the cost of implementing the programme.
As expected, participants’ knowledge of stress and how to manage it improved after the course (by 1.52 points), which is comparable to the 1-point pooled effect size in the meta-analysis conducted by Cook et al. (2011). The results suggest that the training intervention contributed to an improvement in participants’ knowledge and confidence in discussing concepts related to resilience and well-being, as well as their self-reported use of resilience-building behaviours. The increase of 3.06-points found in this study is higher than pooled effect sizes reported by previous studies potentially due to the self-report nature of this study (Cook et al., 2011).
Our results are comparable to the work of Raj (2016) who found that interventions focusing on health and coping skills appear to improve well-being. This study found that increased use of coping mechanisms for stress was associated with approximately the same magnitude of change in both well-being and resilience. However, the increased use of self-care behaviours was associated with a larger change in well-being than in resilience. This finding highlights the complex relationship between resilience and well-being. Several studies have shown that resilience is positively correlated with psychological well-being and vice versa, however, the directional causality of resilience and well-being has not been clearly explored (Fredrickson and Joiner, 2002; Mak et al., 2011; Souri and Hasanirad, 2011; Rodriguez-Fernandez et al., 2018; Liu et al., 2020; Wu et al., 2020). A study conducted with Chinese college students found further support for the reciprocal relationship between resilience and mental health status, indicating that resilience predicted the level of mental health and vice versa within 1 year from baseline. In the longer term, within 2 years from baseline, mental health was found to predict the level of resilience (Wu et al., 2020). Further research needs to be conducted on the directional relationship between resilience and subjective well-being. The second phase of this study will re-assess the sample on the same domains 3 months after completion and may provide further insight into this relationship.
We observed an association between improvements in both well-being and resilience outcomes after completing the course and self-reported use of resilience-building behaviours. In our study, two specific behaviours were associated with larger changes in well-being and resilience scores: the increased use of coping mechanisms and self-care behaviours (e.g., getting adequate sleep, eating healthily, and engaging in physical activity). This is in line with previous research that suggests engaging in mindfulness and relaxation practices (Yung et al., 2004; McDonald et al., 2012; Foureur et al., 2013; Rogers, 2016b; Liu et al., 2020), getting enough sleep (Rosen et al., 2006; Kemper et al., 2015; Raj, 2016), and physical activity (Cameron and Brownie, 2010; Hart et al., 2014; Bergouignan et al., 2016) are associated with greater well-being and resilience. Although positive social relationships are also found to be associated with greater well-being (Glass, 2009; Cameron and Brownie, 2010; Hart et al., 2014; Raj, 2016; Powell, 2018; Liu et al., 2020), and this was communicated within the e-learning course, in our evaluation, connecting with social support networks did not significantly influence well-being or resilience. We posit that this may be due to the intervention taking place during the COVID-19 pandemic, under restricted social contact, limiting the ability of course attendees to “action” upon this behaviour. Behaviours related to diet, sleep and exercise may have been more within the control of participants during this time, thus more likely to be engaged with.
In our study no sociodemographic factors were statistically associated with changes in well-being or resilience scores when adjusting for other covariates. This finding suggests that HCWs from different disciplines, levels, and sectors (private vs. public) can benefit from training interventions such as this. However, research has shown that resilience is a product of complex interactions between individuals and socio ecological determinants (Liu et al., 2020). Conditions that facilitate resilience vary based on circumstances or stressors, access to available resources and socio-cultural differences (Ungar, 2017). The authors encourage future researchers to measure these for more in-depth analyses as mediators or moderators of the associations we found, alongside the inclusion of a wait-list control group.
Overall, these findings may be of particular importance to health systems and organisations interested in designing e-learning programmes to improve HCW well-being and resilience as protective factors against burnout, particularly during crises care. However, future research should focus on all level four of Kirkpatrick’s framework and rigourous evaluation methods so that the effectiveness of e-learning interventions on patient outcomes and health systems can be better understood.
As the primary objective of this e-learning course was to meet the immediate needs of the community, a wait-control list for research purposes was not deemed appropriate. Therefore, several limitations of the study that should be considered when interpreting the results. Convenience sampling was used as participants were included based on their willingness to participate, and there was no control group. Approximately half of the participants that completed pre-course questionnaire also completed the post-course questionnaire. This selection bias may positively skew the results as those who decided to complete the post-questionnaire may have found more benefit from the course. The results rely on self-reported data from the participants which may be susceptible to social desirability and acquiescent effects (Kreitchmann et al., 2019). However, the use of validated screening tools (CD-RISC and WHO-5) should minimise this. As the HCWs were asked to recall their behaviours and emotions over a period of 1 month, recall bias may have occurred. We recommend that future studies make use of validated tools, or objective measures where possible, to measure behaviour. The collection of post-course data was collected immediately after the course was completed; larger effects may have been seen if the participants had had more time to work on the new behaviours learnt. The second phase of the programme implementation includes another course and a follow-up survey for those that have completed the first course to assess the same domains 1–3 months after the first course. This may facilitate exploration of maintenance and comparisons between groups that have completed none, one or all of the courses.
Our findings suggest that e-learning courses may improve more than competency-based outcomes alone. To fully assess the impact of an e-learning course, community programme implementors, designers, and funders, should be encouraged to build and support robust evaluation strategies that not only measure whether an improvement in knowledge and skill is achieved but also whether that knowledge and skill is applied and actioned. Finally, short- and longer-term evaluation strategies should also be considered to explore potential sustained effects of e-learning courses.
The datasets generated and/or analysed during the current study are not publicly available as individual privacy could be compromised but are available from the corresponding author on reasonable request.
The study was reviewed and approved by the FPD Research Ethics Committee (certificate number: 19/2020). The FPD REC is registered with the National Health Research Ethics Council for consideration of research projects that involve minimal risk to human participants (Registration No. REC-03711-033-RA). The patients/participants provided their written informed consent to participate in this study.
FK designed the study, managed data collection, and drafted the manuscript. DB conducted the statistical analysis. MU designed the course. SM and CB provided supervisory support. All authors contributed to the article and approved the submitted version.
This study was funded by the Johnson & Johnson Foundation. The funders contributed to critical review of the manuscript and decision to submit the paper for publication (grant number: 61468813).
CB was employed by Johnson and Johnson Global Community Impact and SM was employed by Johnson and Johnson Health and Wellness Solutions.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Johnson & Johnson for their support for this project and the evaluation thereof. We would also like to thank the participants for their time and participation in the study.
Arrogante, O., and Aparicio-Zaldivar, E. (2017). Burnout and health among critical care professionals: the mediational role of resilience. Intensive. Crit. Care Nurs. 42, 110–115. doi: 10.1016/j.iccn.2017.04.010
Bergouignan, A., Legget, K. T., and De Jong, N. (2016). Effect of frequent interruptions of prolonged sitting on self-perceived levels of energy, mood, food cravings and cognitive function. Int. J. Behav. Nutr. Phys. Activity 13:13. doi: 10.1186/s12966-016-0437
Brooks, S. K., Dunn, R., Amlot, R., Rubin, G. J., and Greenberg, N. (2018). Systematic, Thematic Review of Social and Occupational Factors Associated With Psychological Outcomes in Healthcare Employees During an Infectious Disease Outbreak. J. Occup. Environ. Med. 60, 248–257. doi: 10.1097/JOM.0000000000001235
Cameron, F., and Brownie, S. (2010). Enhancing resilience in registered aged care nurses. Austr. J. Ageing 29, 66–71. doi: 10.1111/j.1741-6612.2009.00416.x
Connor, K. M., and Davidson, J. R. (2003). Development of a New Resilience Scale: the Connor-Davidson Resilience Scale (CD-RISC). Depr. Anxiety 18, 76–82. doi: 10.1002/da.10113
Cook, D. A., Hatala, R., Brydges, R., Zendejas, B., Szostek, J. H., and Wang, A. T. (2011). Technology-Enhanced Simulation for Health Professions Education: a Systematic Review and Meta-analysis. JAMA Netw. 306, 978–988. doi: 10.1001/jama.2011.1234
Davies, E. B., Beever, E., and Glazebrook, C. (2018). A pilot randomised controlled study of the Mental Health First Aid eLearning course with UK medical students. BMC Med. Educ. 18:45. doi: 10.1186/s12909-018-1154-x
Davis, J., Chryssafidou, E., Zamora, J., Davies, D., Kahn, K., and Coomarasamy, A. (2007). Computer-based teaching is as good as face to face lecture-based teaching of evidence based medicine: a randomised controlled trial. BMC Med. Educ. 30, 302–7. doi: 10.1186/1472-6920-7-23
Foureur, M., Besley, K., Burton, G., Yu, N., and Crisp, J. (2013). Enhancing the resilience of nurses and midwives: pilot of a mindfulness based program for increased health, sense of coherence and decreased depression, anxiety and stress. Contemp. Nurse 45, 114–25. doi: 10.5172/conu.2013.45.1.114
Fredrickson, B. L., and Joiner, T. (2002). Positive emotions trigger upward spirals toward emotional well-being. Psychol. Sci. 13, 172–175. doi: 10.1111/1467-9280.00431
Glass, N. (2009). An investigation of nurses’ and midwives’ academic/clinical workplaces. Holistic Nurs. Pract. 23, 158–170. doi: 10.1097/HNP.0b013e3181a056c4
Gray, P., Senabe, S., Naicker, N., Kgalamono, S., Yassi, A., and Speigel, J. (2019). Workplace-Based Organizational Interventions Promoting Mental Health and Happiness among healthcare workers: a realist review. Int. J. Environ. Res. Public Health 16:4396. doi: 10.3390/ijerph16224396
Hart, P. L., Brannan, J. D., and De Chesnay, M. (2014). Resilience in nurses: an integrative review. J. Nurs. Manag. 22, 720–734. doi: 10.1111/j.1365-2834.2012.01485.x
Huang, J., Lui, F., Teng, Z., Zhao, J., and Wang, X. (2020). Care for the Psychological Status of Frontline Medical Staff Fighting Against Coronavirus Disease 2019. 71(12):3268 - 3269. Clin. Infect. Dis. 12, 3268–3269. doi: 10.1093/cid/ciaa385
Jorgensen, I. E., and Seedat, S. (2008). Factor structure of the Connor-Davidson Resilience Scale in South African adolescents. Int. J. Adolesc. Med. Health 20, 23–32. doi: 10.1515/ijamh.2008.20.1.23
Kang, L., Simeng, M., Chen, M., Yang, J., Wang, Y., and Li, R. (2020). Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: a cross-sectional study. Brain Behav. Immunity 87, 11–17. doi: 10.1016/j.bbi.2020.03.028
Kemper, K. J., Mo, X., and Khayat, R. (2015). Are mindfulness and self-compassion associated with sleep and resilience in health professionals? J. Altern. Compl. Med. 21, 496–503. doi: 10.1089/acm.2014.0281
Kirkpatrick, D. L. (1994). Evaluating Training Programs: the Four Levels. California: Berrett-Koehler.
Kreitchmann, R. S., Abad, F. J., Ponsoda, V., Nieto, M. D., and Morillo, D. (2019). Controlling for Response Biases in Self-Report Scales: forced-Choice vs. Psychometric Modeling of Likert Items. Front. Psychol. 10:2309. doi: 10.3389/fpsyg.2019.02309
Kuiler, R., Gulmezoglu, A. M., and Zamora, J. (2012). Effectiveness of a Clinically Integrated e-Learning Course in Evidence-Based Medicine for Reproductive Health Training: a randomized trial. JAMA 308, 2218–2225. doi: 10.1001/jama.2012.33640
Lai, J., Ma, S., Wang, Y., Cai, Z., Hu, J., and Wei, N. (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Open Netw. 3:e203976. doi: 10.1001/jamanetworkopen.2020.3976
Lawn, S., Zhi, X., and Morello, A. (2017). An integrative review of e-learning in the delivery of self-management support training for health professionals. BMC Med. Educ. 17:183. doi: 10.1186/s12909-017-1022-0
Liu, J. W., Ein, N., Gervasio, J., Battaion, M., Reed, M., and Vickers, K. (2020). Comprehensive meta-analysis of resilience interventions. Clin. Psychol. Rev. 82:101919. doi: 10.1016/j.cpr.2020.101919
Mak, W. S., Ng, I. W., and Wong, C. Y. (2011). Resilience: enhancing well-being through the positive cognitive triad. J. Counsel. Psychol. 58, 610–617. doi: 10.1037/a0025195
Maunder, R. G., Lance, W. J., Mae, R., Vincent, L., Peladeau, N., and Beduz, M. A. (2010). Computer-assisted resilience training to prepare healthcare workers for pandemic influenza: a randomized trial of the optimal dose of training. BMC Health Serv. Res. 10:72. doi: 10.1186/1472-6963-10-72
McCann, C. M., Beddoe, E., McCormick, K., Huggard, P., Kedge, S., Adamson, C., et al. (2013). Resilience in the health professions: a review of recent literature. Int. J. Wellbeing 3:1. doi: 10.5502/ijw.v3i1.4
McDonald, G., Jackson, D., Wilkes, L., and Vickers, M. H. (2012). A work-based educational intervention to support the development of personal resilience in nurses and midwives. Nurse Education Today. 32, 378–384. doi: 10.1016/j.nedt.2011.04.012
Mealer, M., Jones, J., and Moss, M. (2012). A qualitative study of resilience and posttraumatic stress disorder in United States ICU nurses. Intensive Care Med. 38, 1445–1451. doi: 10.1007/s00134-012-2600-6
Pfefferbaum, B. (2020). Mental Health and the Covid-19 Pandemic. New Engl. J. Med. 6, 510–212. doi: 10.1056/NEJMp2008017
Powell, S. K. (2018). Work–Life BALANCE: how Some Case Managers Do It! Prof. Case Manag. 23, 235–239. doi: 10.1097/ncm.0000000000000317
Raj, K. S. (2016). Well-being in residency: a systematic Review. J. Graduate Med. Educ. 8, 674–684. doi: 10.4300/JGME-D-15-00764.1
Regmi, K., and Jones, L. (2020). A systematic review of the factors – enablers and barriers - affecting e-learning in health sciences education. BMC Med. Educ. 20:91. doi: 10.1186/s12909-020-02007-6
Robertson, L. J., Maposa, I., Somaroo, H., and Johnson, O. (2020). Mental health of healthcare workers during the COVID-19 outbreak: a rapid scoping review to inform provincial guidelines in South Africa. S. Afr. Med. J. 110, 1010–1019. doi: 10.7196/SAMJ.2020.v110i10.15022
Rodriguez-Fernandez, A., Ramos-Diaz, E., and Axpe-Saez, I. (2018). “The Role of Resilience and Psychological Well-Being in School Engagement and Perceived Academic Performance: an Exploratory Model to Improve Academic Achievement, Health and Academic Achievement” in Health and Academic Achievement. ed. B. Bernal-Morales (London: IntechOpen).
Rogers, D. (2016a). Does a brief workshop change clinical associate students’ resilience? Afr. J. Prim. Health Care Fam. Med. 8:1183. doi: 10.4102/phcfm.v8i1.1183
Rogers, D. (2016b). Which educational interventions improve healthcare professionals’ resilience? Med. Teach. 38, 1236–1241. doi: 10.1080/0142159X.2016.1210111
Rosen, I. M., Gimotty, P. A., Shea, J. A., and Bellini, L. M. (2006). Evolution of sleep quantity, sleep deprivation, mood disturbances, empathy, and burnout among interns. Acad. Med. 81, 82–85. doi: 10.1097/00001888-200601000-00020
Ruggeri, K., and Brayne, C. (2013). Global Model for Effective Use and Evaluation of e-Learning in Health. Telemed. E Health 19, 312–321. doi: 10.1089/tmj.2012.0175
Ruiz, J. G., Mintzer, M. J., and Leipzig, R. M. (2006). The Impact of E-Learning in Medical Education. Acad. Med. Educ. 81, 207–12. doi: 10.1097/00001888-200603000-00002
Senni, M. (2020). COVID-19 experience in Bergamo, Italy. Eur. Heart J. 41, 1783–1784. doi: 10.1093/eurheartj/ehaa279
Soares, C. N., Kornstein, S. G., Thase, M. E., Jiang, Q., and Guico-Pabia, C. J. (2009). Assessing the efficacy of desvenlafaxine for improving functioning and well-being outcome measures in patients with major depressive disorder: a pooled analysis of 9 double-blind, placebo-controlled, 8-week clinical trials. J. Clin. Psychiatry 70, 1365–1371. doi: 10.4088/JCP.09m05133blu
Souri, H., and Hasanirad, T. (2011). Relationship between resilience, optimism, and psychological Well-being in students. Soc. Behav. Sci. 30, 1541–1544. doi: 10.1016/j.sbspro.2011.10.299
Ungar, M. (2017). Which counts more: differential impact of the environment or differential susceptibility of the individual. Br. Soc. Work 47, 1279–1289. doi: 10.1093/bjsw/bcw109
World Health Organization [WHO] (1998). Well-being Measures in Primary Health Care/The Depcare Project. Switzerland: World Health Organization.
World Health Organization [WHO] (2019). Burn-out an “Occupational Phenomenon”: international Classification of Diseases. Switzerland: World Health Organization.
Wu, P., Fang, Y., and Guan, Z. (2009). The Psychological Impact of the SARS Epidemic on Hospital Employees in China: exposure, Risk Perception, and Altruistic Acceptance of Risk. Can. J. Psychiatry 54, 302–11. doi: 10.1177/070674370905400504
Wu, Y., Sang, Z., Zhang, X., and Margraf, J. (2020). The Relationship Between Resilience and Mental Health in Chinese College Students: a Longitudinal Cross-Lagged Analysis. Front. Psychol. 11:108. doi: 10.3389/fpsyg.2020.00108
Wutoh, R., Boren, S. A., and Balas, E. A. (2004). eLearning: a review of Internet-based continuing medical education. J. Contin. Educ. Health Profess. 24, 20–30. doi: 10.1002/chp.1340240105
Keywords: e-learning, healthcare worker, resilience, wellbeing, mental health, COVID-19, continuing professional development
Citation: Kelly F, Uys M, Bezuidenhout D, Mullane SL and Bristol C (2021) Improving Healthcare Worker Resilience and Well-Being During COVID-19 Using a Self-Directed E-Learning Intervention. Front. Psychol. 12:748133. doi: 10.3389/fpsyg.2021.748133
Received: 27 July 2021; Accepted: 03 November 2021;
Published: 02 December 2021.
Edited by:
Judith Andersen, University of Toronto Mississauga, CanadaReviewed by:
Laura Lacomba-Trejo, University of Valencia, SpainCopyright © 2021 Kelly, Uys, Bezuidenhout, Mullane and Bristol. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Frances Kelly, ZnJhbmNlc2tAZm91bmRhdGlvbi5jby56YQ==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.