
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol., 25 November 2021
Sec. Organizational Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.736809
This article is part of the Research TopicCommunication, Emotions, and Well-Being in Emotionally Charged WorkersView all 12 articles
Communication is essential to the quality of care and patient satisfaction. It has been linked to positive patient outcomes, increased engagement, improved health outcomes, and safe practices. Given these benefits and the association between attitudes and behaviors, as behaviors can be predicted by studying attitudes, assessing attitudes of nursing students toward patient communication is critical for future nursing professionals. For this purpose, the main aim of this study was to adapt and validate an instrument to measure nurses’ attitudes toward communication (ACO) for nursing students. The ACO with patients was analyzed. Then, differences in the dimensions of the instrument (ACO) for nursing students according to an academic course and the correlations were calculated. A cross-sectional study was carried out in a convenience sample of 1,417 nursing students from five universities in the Valencian Community (Spain) during the 2018/2019 academic year and 83.8% (1,187) were women. The reliability was analyzed by using Cronbach’s alpha and composite reliability (CR). Analysis of construct validity was performed with exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The instrument adapted from nurses to nursing students was composed of 25 items grouped in three dimensions: affective, cognitive, and behavioral. The psychometric properties suggested that the instrument ACO for nursing students was reliable and valid. The ACO of nursing students was positive with high levels in cognitive and behavioral dimensions, while scores were worst in the affective component. The second-year nursing students showed more positive attitudes in the affective dimension, while in the cognitive and behavioral dimensions, the most positive attitudes were found in the first year. In the correlations, the behavioral and cognitive dimensions showed a significant, positive, and very high correlation. These findings should be considered in developing academic plans to improve the effectiveness of the communication education process of the students to increase the quality of patient care and well-being of nursing students.
The importance of communication is reflected in the theories and models of nursing that support the professional practice; in this sense, the Theory of Human Caring proposed by Jean Watson (Watson, 2018) highlights the importance of open communication with the patient and his/her family in the care process. In the care process according to Watson, the nurse should interact with “the person” rather than with “the patient,” understand their beliefs, emotions, feelings, and fears, without forgetting their individuality and knowledge (Foronda et al., 2016; Wei and Watson, 2019). Communication is vital in all the areas of nursing care: prevention, treatment, rehabilitation, education, and health promotion (Kourkouta and Papathanasiou, 2014); it is a process by which information is exchanged and shared during interventions performed with the patient (Hannawa et al., 2015). In short, it is the essence of the relationship with the patient to create a positive interpersonal relationship, exchange information and make appropriate decisions related to treatment and care (Grassi et al., 2015), and sharing of ideas, thoughts, feelings, and needs with another person (Xie et al., 2013). All the nurses are expected to be competent in communication (Mullan and Kothe, 2010), i.e., able to communicate effectively with patients, their families, and other members of the healthcare team (Claramita et al., 2016).
Nurse-patient communication is ultimately an interpersonal communication in which an exchange of information is carried out between the patient and the professional from a comprehensive and holistic view of the person, which allows knowing their real needs and, therefore, to establish a therapeutic relationship. Therapeutic communication between nurse and patient is considered the basis of nursing care (Abdolrahimi et al., 2017a); it is patient-centered and involves physiological, psychological, environmental, and spiritual aspects of the patient (Peplau, 1991). It is based on understanding and addressing the situation of the patient, including relevant life circumstances, beliefs, perspectives, concerns, and needs in order to plan appropriate patient care (Cusatis et al., 2020). Therapeutic communication is essential to the quality of care and satisfaction of the patient (Finke et al., 2008; Kourkouta and Papathanasiou, 2014; Finney Rutten et al., 2015; Banerjee et al., 2016; Gillett et al., 2016; Howick et al., 2018). It has been linked to positive patient outcomes, increased engagement, improved health outcomes (Kitson et al., 2014; Burgener, 2020), safe practices (Lin et al., 2017), and decrease the emotional burden on both the nurses and families (Charlton et al., 2008; Wittenberg et al., 2017). From the perspective of patients, it enhances the trusting relationship that can be built with nurses and facilitates decision-making (Rosemond et al., 2017). In addition, effective communication among multidisciplinary team members is critical to the effectiveness of healthcare teams and can be related to the quality of care and job satisfaction of the nurses (Gausvik et al., 2015). Communication errors can increase the incidence of adverse events and cause various harm to patients (Li et al., 2019). World Health Organization (2017) identifies communication as an essential tool of patient safety culture and a cause of delay in treatment, medication errors, and incorrect procedures (The Joint Commission, 2016).
Given the benefits of therapeutic communication for good care, for safe, and quality practice (Boschma et al., 2010; Finney Rutten et al., 2015), it is critical to address these issues in nursing students as future nursing professionals (Grant and Jenkins, 2014). Literature shows that communication can be a challenge for nurses and nursing students (Suzuki et al., 2014), as studies assess communication skills showing that these skills are poor among nurses (Hemsley et al., 2012; Shorey et al., 2018). Other studies have shown that communication skills are also deficient among nursing students such that they are a problem for their well-being (Satu et al., 2013). Students identified numerous barriers to effective communication, including reluctance to engage with patients or families, difficulty in initiating or sustaining conversation, feeling devalued, frightened, fearful, or anxious, and continuing to worry about their performance after the interaction is over (Beckstrand et al., 2012; Banerjee et al., 2016; Lin et al., 2017). Previous studies indicate that interventions to teach nurse-patient communication skills focus on more difficult clinical interactions (MacLean et al., 2017), mental health patients (Sarikoc et al., 2017), palliative care (Coyle et al., 2015), hence these are more studied areas. However, communication skills in general care settings with patients are equally important (Chan, 2014).
Therapeutic communication is based on the knowledge, attitudes, and skills of the patient and nurse that lead to patient understanding and participation (Abdolrahimi et al., 2017b). Despite this, most studies have focused on communication skills, communication knowledge, and medical students (Epstein et al., 2010; Škodová et al., 2018). There is not a comprehensive assessment of attitudes in the communication of nursing students before they are exposed to real human interactions during their clinical practice (Foronda et al., 2016). Therefore, studying attitude toward communication (ACO) in nursing students is important based on the “Theory of Reasoned Action” (Ajzen and Fishbein, 1980) because of the relationship between attitudes and the behavior of individuals. According to this theory, a change in behavior can be induced by a change in the attitude of the person and can predict behaviors by studying attitudes (Ajzen, 1991). The behavioral component of attitudes is a manifestation of the underlying cognitive and affective components (Anvik et al., 2007). This aspect is very important in nursing students because assessment of ACO allows identification of negative attitudes and perception of communication is an unimportant part of effective healthcare, which could negatively influence the effectiveness of the educational process (Škodová et al., 2018) in the integration of communicative knowledge and skills in nursing students (Fukada, 2018). In addition, studying ACO within the care process helps to evaluate the interpersonal communication of the nurse with the patient (Chan, 2017) in order to be able to adapt strategies and their effectiveness (Grant and Jenkins, 2014) to increase the quality of patient care and well-being of nursing students (Satu et al., 2013). Considering the importance of ACO in nursing students and there are no instruments for its assessment, it would be important to develop validated instruments to evaluate ACO with the patient (MacLean et al., 2017; Levett-Jones et al., 2019).
The literature provides scarce studies on the reliability and validity of the instruments used (Grant and Jenkins, 2014; Gutiérrez-Puertas et al., 2020) on ACO skills in nursing students; the Communication Skills Attitude Scale (CSAS) (Škodová et al., 2018) was originally developed to measure the ACO skills in medical students (Rees et al., 2002). Others measure communication competencies of nursing students such as the Interpersonal Communication Assessment Scale (ICAS) (Klakovich and dela Cruz, 2006) and the ACO of the nurses with patients (Giménez-Espert and Prado-Gascó, 2018), with adequate psychometric properties. So, in this study, the main aim of an adaptation and validation of this instrument in nursing students was performed. Thus, the ACO with patients in a sample of nursing students was analyzed. Finally, differences in the dimensions of the instrument (ACO) for nursing students according to an academic course and the correlations were calculated.
A cross-sectional study was carried out in a convenience sample of 1,417 nursing students from five universities in the Valencian Community (Spain). The nursing degree in Spain includes four full-time academic years with 240 European Credit Transfer System (ECTS) at 60 ECTS per year (1 credit representing between 25 and 30 h of student work). After completing the program, the student obtains a degree in nursing and can practice in Spain and in the European Union countries.
The inclusion criteria were students enrolled in the nursing degree of the universities participating who gave their consent for participation after receiving information about this study. The anonymity and confidentiality of the information provided were indicated. The self-report instrument was completed in the classroom by the participants, which lasted around 10 min. The data collection phase was developed during the 2018/2019 academic year.
Attitudes Toward Communication of Nurses with the patient (ACO) (Giménez-Espert and Prado-Gascó, 2018) to measure the ACO of the nurses with the patient (intellectual property registered at the University of Valencia on 08/04/2019, registration number: UV-MET-201917R). The instrument is based on Rosenberg and Hovland’s (1960) three-dimensional model of attitude: affective, cognitive, and behavioral. The attitude components were related to the most important communicative moments of the hospitalization process (Duhamel and Talbot, 2004): admission, procedure, and discharge. The three communicative moments were related to the nursing interventions according to the Nursing Interventions Classification (NIC) (Bulechek, 2009). Finally, from this classification, the following interventions with their corresponding activities were selected and related to the three components of the attitude: nursing care at admission (7,310), teaching: procedure/treatment (5,618), and discharge planning (7,370). The instrument was composed of 25 items, grouped in three dimensions: Affective, related to situations and to admission, procedure, and discharge of the patient that generate anxiety in nurses (12 items, Cronbach’s α = 0.95, e.g., “I’m nervous when I inform the patient and/or family about how they can help in recovery”); behavioral, related to what nurses usually do with respect to the patient and/or family member regarding checking to understand information on admission, encouraging questions, aspects related to orientation in the unit (visiting hours, routines), reinforcing, facilitating and clarifying information to the patient to obtain informed consent, checking to understand information on discharge and its implementation, allowing time for questions, and how to collaborate during the procedure. It is that which we can observe and allows us to deduce the other two (9 items, Cronbach’s α = 0.92, e.g., “I usually encourage the patient and/or family ask me when I provide information at the time of admission to the unit”); and cognitive, refers to the importance for nurses: orientation of the patient and/or family in the unit, information that can help in recovery, information on discharge care, and finally collaboration with other members of the healthcare team (4 items, Cronbach’s α = 0.85, e.g., “It is necessary to inform the patient and/or family about how they can help in recovery”). A five-point Likert scale was used ranging from 1 = strongly disagree to 5 = strongly agree. High scores in all the dimensions correspond to positive ACO, except in the affective dimension where lower scores indicate more positive ACO, as it is an inverted dimension when considering the stress produced by communication. The original instrument showed adequate psychometric properties (Giménez-Espert and Prado-Gascó, 2018) and was modified for nursing students “Although I am a student now, I believe that when I practice as a nurse.” In this study, the student-adapted version of the instrument had acceptable reliability (Cronbach’s α = 0.84) (intellectual property registered at the University of Valencia on 30/07/2020, registration number: UV-MET-202044R).
The instrument adaptation process was performed in three stages:
Stage 1: adaptation
The international methodological standards for the adaptation of an instrument established by the International Test Commission (2017) were followed in the adaptation of the ACO of the nurses with the patient instrument for nursing students.
Stage 2: content validity process
The items were evaluated by a panel of experts and in a pilot sample of 100 nursing students to assess content validity, according to the accuracy, clarity, legibility, and relevance of each item of the instrument (Polit and Beck, 2008). The experts were five nurses with at least 10 years of clinical experience, training and research in the field (Polit and Beck, 2008). The content validity index (CVI) was calculated, and the criteria for inclusion of the item were that the CVI was larger than 0.80 (Lynn, 1986). Moreover, the comments of the nursing students and the experts were analyzed, and there were no items unclear or controversial. According to these results, the 25 items were maintained in the final version of the instrument.
Stage 3: statistical analyses and psychometric properties
The Statistical Package for the Social Sciences (SPSS) software (version 22), the EQS software (Structural Equation Modeling software, version 6.2) (Bentler, 2004), and the FACTOR software (Lorenzo-Seva and Ferrando, 2006) were used to perform the statistical analyses of this study. First, descriptive analysis of every item (mean and SD) and observations of the item-total correlation coefficients. The reliability was also analyzed by using Cronbach’s alpha and composite reliability (CR). Analysis of construct validity was performed with exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The convergent validity was assessed by using the results of the CFA, while for discriminant validity, the average variance extracted (AVE) test was used (Fornell and Larcker, 1981).
The adequacy of the proposed models by CFA was tested with the significance of χ2 (Bentler, 2004). The coefficients of the goodness of fit, the non-normed fit index (NNFI), the comparative fit index (CFI), and the incremental fit fix (IFI) values > 0.90 were considered as a good fit (McCallum and Austin, 2000). Finally, the root mean square error of approximation (RMSEA) was calculated, and it was required to be <0.08 to considered as a good fit (Browne and Cudeck, 1993).
The ANOVA was calculated to search for differences between academic year and the ACO dimensions for nursing students. The correlations were analyzed by using Pearson’s correlation coefficient.
The age of the participants ranges from 18 to 55 years (M = 21.80, SD = 5.34). According to the distribution by sex, 83.8% are women (n = 1,187) and 16.2% are men (n = 230). According to the course of study, the distribution observed is as follows: 29.6% first, 25% second, 23.8% third, and 21.6% fourth.
The attitudes toward communication instrument for nursing students is composed of 25 items distributed in three dimensions. Table 1 shows items grouped according to the dimension. In addition, the table collects for all the items such as the mean (M), SD, item-total correlation (rjx), and Cronbach’s alpha, if that item is eliminated (α-x). The ACO instrument for nursing students as a whole shows acceptable reliability (α = 0.84).
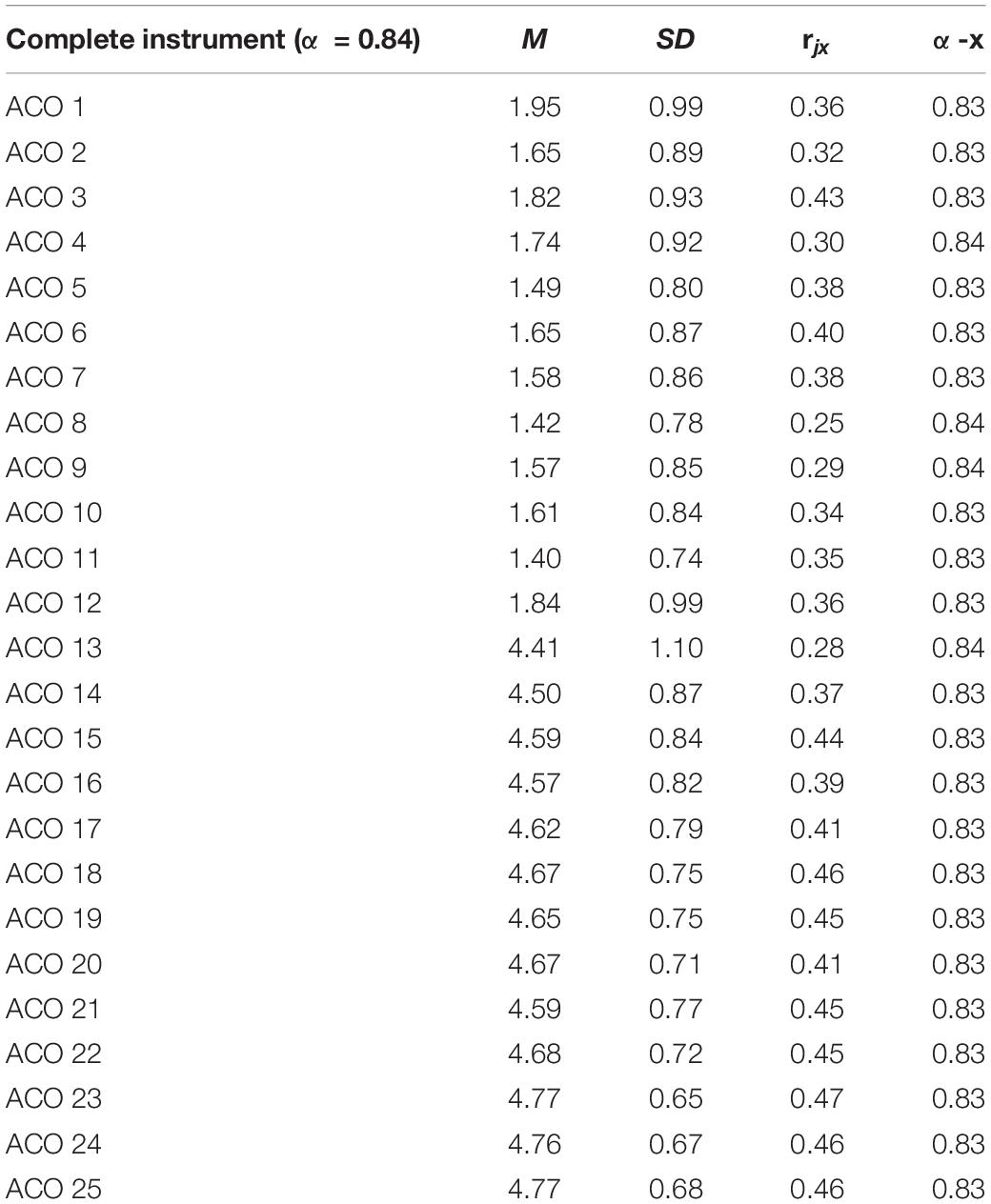
Table 1. Analysis of the attitudes toward communication (ACO) for nursing students items: Mean (M), SD, item-total correlation (rjx), and Cronbach’s alpha if it eliminates the element (α-x).
An EFA was performed to examine how the items are distributed without any restriction. An EFA was performed following the process recommended by Lloret-Segura et al. (2014) by using the unweighted least squares method and normalized direct oblimin rotation. To determine the number of common factors in which the items are grouped, parallel analysis was used.
The EFA performed by using the FACTOR program (Lorenzo-Seva and Ferrando, 2006) with the 25 items of the ACO instrument for nursing students recommended the grouping of the items into two common factors. It was decided to check the fit of the factorial structure set on the three dimensions since it was difficult to interpret the two-factor factorial solution theoretically. After the application of the EFA fixed to three factors, it was not necessary to suppress any item since the saturations were higher than 0.40, maintaining the scale at 25 items. The fit of this solution was adequate with an RMSR value of 0.03 (<0.50; Harman, 1980) and a goodness of fit index (GFI) index of 0.99 (>0.95; Tanaka and Huba, 1989). The Kaiser–Meyer–Olkin (KMO) index of sampling adequacy also presented an optimal value (KMO = 0.93; 95% CI 0.918–0.920) and Bartlett’s test of sphericity was significant (χ2 = 13836.6; df = 300; p ≤ 0.001). The variance explained by the three factors was 78%.
Once the EFA was performed, CFA was completed to check the factor structure extracted by the EFA. This model presents adequate fit (χ2 = 2347.59; df = 272; p < 0.05; NNFI = 0.91; CFI = 0.92; IFI = 0.92; and RMSEA = 0.07 (95% CI = 0.076–0.082). Convergent validity showed that the items of the instrument were correlated with the latent variables (affective, behavioral, and cognitive). The loadings of each item were higher (>0.70; Anderson and Gerbing, 1988) except in items (ACO4 λ = 0.67, ACO8 λ = 0.66, ACO12 λ = 0.61, and ACO13 λ = 0.58). In every case, the T values for the variables ranged from 20.13 to 48.81 (t > 1.96) and were significant at the 0.05 level. The CR and the AVE for each dimension: affective CR = 0.98; AVE = 0.58, behavioral CR = 0.97; AVE = 0.53, and cognitive CR = 0.96, AVE = 0.82; CR (>0.70; Nunnally, 1978) and AVE (≥0.50; Fornell and Larcker, 1981; Table 2).
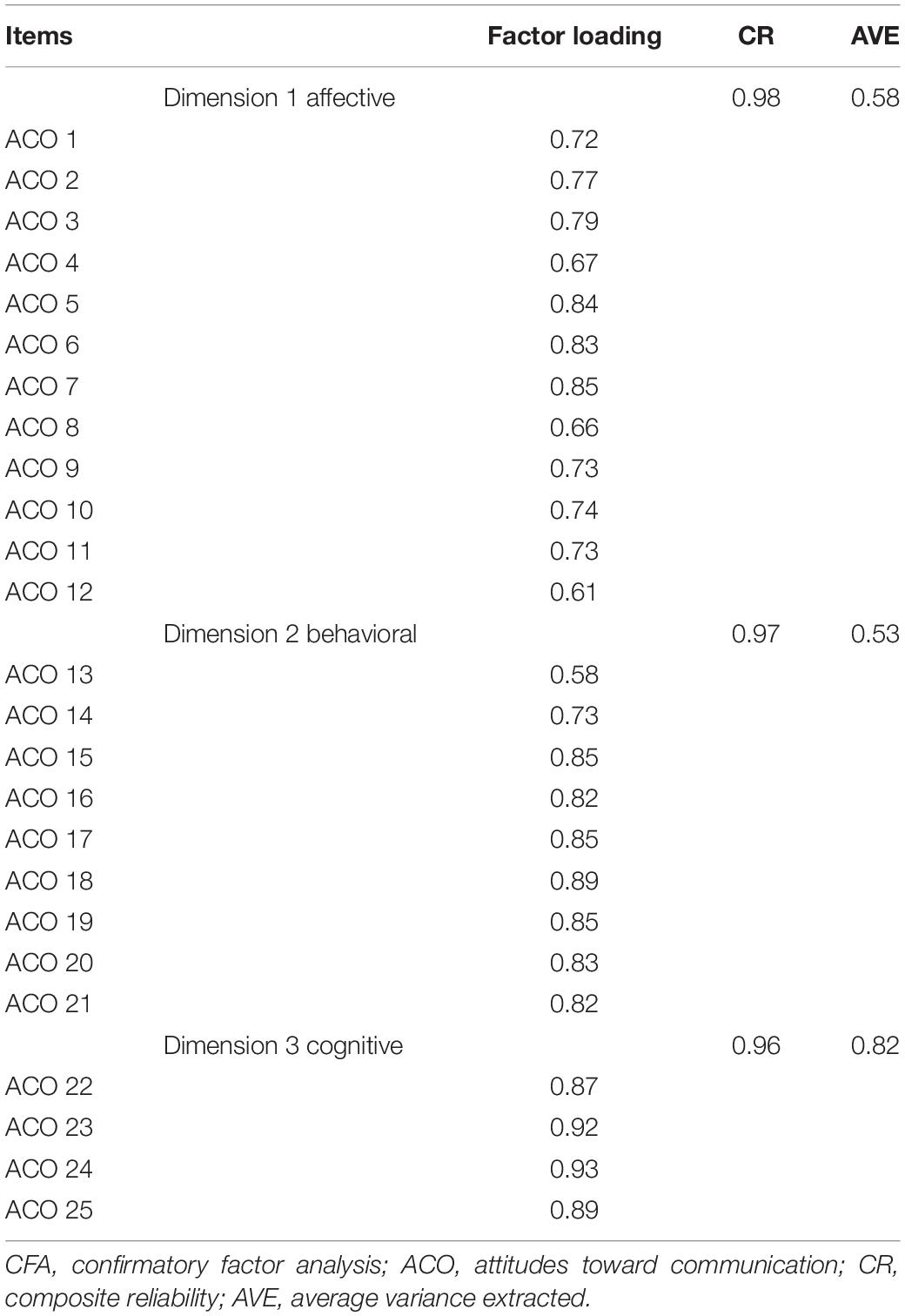
Table 2. Results of the CFA with factor loadings, composite reliability, and average variance extracted from ACO for nursing students.
Analysis of attitudes toward patient communication of nursing students provided the following results: behavioral (M = 4.56; SD = 0.69) and cognitive (M = 4.73; SD = 0.47) showed the highest scores, meanwhile the dimension related to affective communication (M = 1.65; SD = 0.77) had the lowest average score.
Then, we analyzed the relationships between the academic course and the ACO dimensions by using the ANOVA analyses with the Bonferroni post hoc test to determine the differences between the variables.
In relation to the academic course (first, second, third, and fourth courses), the results of the ANOVA statistically significant differences in all the dimensions of the ACO instrument for nursing students were observed (Table 3). Statistically significant differences in the Bonferroni post hoc tests in the affective dimension were reported between the second and the other courses, with higher differences in the second-year students. With respect to the cognitive and behavioral dimensions, statistically significant differences were shown between first-, second-, and fourth-year students, with the highest values in first-year students.
Finally, correlations between the different dimensions of the ACO instrument for nursing students were tested. In the case of the affective dimension, statistically significant, negative and low correlations were observed with the behavioral (r = −0.32; *p ≤ 0.05) and cognitive (r = −0.36; *p ≤ 0.05) dimensions. The behavioral and cognitive dimensions showed a significant, positive, and very high correlation (r = 0.90; *p ≤ 0.05).
This study showed the adaptation and validation of the instrument to measure the ACO of nursing students. Analysis of the 25 items demonstrated an adequate contribution to the overall scale. The reliability of the construct showed an acceptable coefficient (Cronbach’s α = 0.84) above the minimum value (>0.70) indicated in the literature (Nunnally, 1978) and did not appear to be improved by removing any of the items. As for the construct validity of the scale, the EFA results showed that the 25 items of the variance explained by the three factors was 78%, RMSR value of 0.03 (<0.50; Harman, 1980), and a GFI index of 0.99 (>0.95; Tanaka and Huba, 1989). This indicated an adequate fit, CFA also replicated that structure, and presented an adequate fit (χ2 = 2347.59; df = 272; p < 0.05; NNFI = 0.91; CFI = 0.92; IFI = 0.92; and RMSEA = 0.07). The RMSEA was 0.07, which agrees with the optimal values fit criteria (≤ 0.08) (Browne and Cudeck, 1993). Similarly, the remaining indices showed a good fit: NNFI = 0.91; CFI = 0.92; and IFI = 0.92 (values over 0.90 indicate an adequate fit) (McCallum and Austin, 2000). Overall, the obtained psychometric properties suggest that the instrument is reliable and valid, which justifies its use to assess ACO in nursing students. These results are relevant because communication is a core competence in nursing students (Chang and Chang, 2021) and behaviors can be predicted by studying attitudes. Then, assessing the ACO for nursing students with the patient is critical as future nursing professionals. Studying the development and modification of attitudes involve exposure to new information (theory lessons, the importance of communication, benefits, and communicative moments), imposed behavioral change (experiential lessons, communication behavioral, and role play), and an increase in self-knowledge (answering an instrument increasing the awareness of the students of their attitudes). Increased knowledge and awareness of their attitudes and behaviors may have already contributed to changing attitudes in nursing students (Koponen et al., 2012). Despite the importance of attitudes in predicting behaviors, no studies have been found assessing ACO in nursing students (MacLean et al., 2017; Levett-Jones et al., 2019), but on communication skills, communication knowledge, and in medical students (Epstein et al., 2010; Škodová et al., 2018; Givron and Desseilles, 2021). Therefore, it is essential to have instruments with adequate psychometric properties to be aware of the attitudes in order to improve negative attitudes and contribute to the development of training programs adapted to the real needs of nursing students.
With respect to the attitudes of nursing students, it seems to indicate positive ACO with the patient. The dimensions with the highest scores were cognitive and behavioral, while scores were worst in the affective component. The affective component showed an inverted dimension when subjects were asked about communication anxiety. These results were in the same line as the Giménez-Espert and Prado-Gascó (2018) study carried out with a sample of the nurse. This can be explained by the fact that the three attitude components are related, since the experienced feeling (emotional dimension) is mainly based on knowledge (cognitive dimension) and actions are guided by feelings and by knowledge (behavioral dimension) (Fishbein and Cappella, 2006; Ertz et al., 2016).
According to the academic course of nursing students, the ANOVA statistically significant differences in all the dimensions of instrument ACO were found. The second-year nursing students showed more positive attitudes in the affective dimension, while in the cognitive and behavioral dimension, the most positive attitudes were found in the first-year students. These findings are consistent with previous studies, showing that communicative attitudes become more negative over time because students may be exposed to more negative communicative experiences, as they get older and may also experience difficulties with increasingly demanding communicative situations (Clark et al., 2012). Due to the curriculum demands and time constraints, it leads to prioritizing clinical skills over interpersonal skills (Cusatis et al., 2020). In addition, the upper class nursing students have already had experiences with the professional world during their clinical practice, which implies exposure to communicate complex situations, human suffering, without adequate educational preparation and support (Ward et al., 2012).
Finally, in the correlations, the behavioral and cognitive dimensions showed a significant, positive, and very high correlation, according to the literature (Rosenberg and Hovland, 1960; Ajzen, 1991). Communication is essential for the quality of care and satisfaction of the patient (Finke et al., 2008; Kourkouta and Papathanasiou, 2014; Finney Rutten et al., 2015; Banerjee et al., 2016; Gillett et al., 2016; Howick et al., 2018) and for the effectiveness of healthcare teams, it can be related to the quality of care and job satisfaction of healthcare workers, such as nurses (Gausvik et al., 2015). Moreover, the influence of knowledge and attitudes on communication is evident (Mullan and Kothe, 2010); therefore, it is necessary to deepen the study of the ACO of nursing students.
In spite of the advantages of this study, several limitations were present. Nevertheless, because the sampling was not probabilistic and the subjects were exclusively from Valencian Community, the results should be generalized with caution. A large sample of nursing students was used in this study. Future studies would be interesting to extend this study to other populations in Spain and in other Spanish-speaking countries. Another limitation is related to the use of self-reports to collect data, and they can introduce bias through the phenomenon of social desirability (Rammstedt et al., 2017). In future research, it would be advisable to combine the results on another type of instrument completed by others and/or with external objective measures, perform a comparison to another measure gold standard, and potential outcome to nursing students’ attitude to communication with patients.
Hence, the importance of analyzing the ACO in nursing students generates a need for reliable and validated instruments. In conclusion, the existence of appropriate instruments allows the measurement of the ACO, evaluating educational needs, developing interventions adapted to real needs, and assessing the interventions developed to improve the ACO in nursing students. These findings should be considered in developing academic plans to improve the effectiveness of the communication education process of the students to increase the quality of patient care and well-being of the nursing students.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the Human Research Ethics Committee of the University of Valencia H1529396558647. The patients/participants provided their written informed consent to participate in this study.
MCG-E, SM, DP, and VP-G made a substantial contribution to the concept, design of the work, acquisition, analysis, and interpretation of data, drafted the manuscript and revised it critically for important intellectual content, and participated sufficiently in the work to take public responsibility for appropriate portions of the content. All authors contributed to the manuscript and approved the submitted version.
This study was funded by the Conselleria de Innovación, Universidades, Ciencia y Sociedad Digital, Generalitat Valenciana (GV/2020/014).
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We thank the students who participated in this study by completing the instrument.
Abdolrahimi, M., Ghiyasvandian, S., Zakerimoghadam, M., and Ebadi, A. (2017a). Antecedents and consequences of therapeutic communication in Iranian nursing students: a qualitative research. Nurs. Res. Pract. 2017:4823723. doi: 10.1155/2017/4823723
Abdolrahimi, M., Ghiyasvandian, S., Zakerimoghadam, M., and Ebadi, A. (2017b). Therapeutic communication in nursing students: a Walker & Avant concept analysis. Electron. Physician 9, 4968–4977. doi: 10.19082/4968
Ajzen, I., and Fishbein, M. (1980). “Predicting and understandingconsumer behavior: attitude-behavior correspondence,” in Under-standing Attitudes and Predicting Social Behavior, eds I. Ajzen and M. Fishbein (Hoboken, NJ: Prentice Hall), 148–172.
Anderson, J. C., and Gerbing, D. W. (1988). Structural equation modeling in practice: a review and recommended two-step approach. Psychol. Bull. 103, 411–423. doi: 10.1037/0033-2909.103.3.411
Anvik, T., Gude, T., Grimstad, H., Baerheim, A., Fasmer, O. B., Hjortdahl, P., et al. (2007). Assessing medical students’ attitudes towards learning communication skills–which components of attitudes do we measure? BMC Med. Educ. 7:4. doi: 10.1186/1472-6920-7-4
Banerjee, S. C., Manna, R., Coyle, N., Shen, M. J., Pehrson, C., Zaider, T., et al. (2016). Oncology Nurses’. Nurse Educ. Pract. 16, 193–201. doi: 10.1016/j.nepr.2015.07.007
Beckstrand, R. L., Collette, J., Callister, L., and Luthy, K. E. (2012). Oncology nurses’ obstacles and supportive behaviors in end-of-life care: providing vital family care. Oncol. Nurs. Forum 39, E398–E406. doi: 10.1188/12.ONF.E398-E406
Boschma, G., Einboden, R., Groening, M., Jackson, C., MacPhee, M., Marshall, H., et al. (2010). Strengthening communication education in an undergraduate nursing curriculum. Int. J. Nurs. Educ. Scholarsh. 7:28. doi: 10.2202/1548-923X.2043
Browne, M. W., and Cudeck, R. (1993). “Alternative ways of assessing model fit,” in Testing Structural Equation Models, eds K. A. Bollen and J. S. Long (Newbury Park, CA: Sage), 136–162.
Bulechek, G. M. (2009). Clasificación de Intervenciones de Enfermería (NIC). [Nursing Intervention Classification (NIC)]. Barcelona: Elsevier Health Sciences.
Burgener, A. M. (2020). Enhancing communication to improve patient safety and to increase patient satisfaction. Health Care Manag. 39, 128–132. doi: 10.1097/HCM.0000000000000298
Chan, E. A. (2014). Cue-responding during simulated routine nursing care: a mixed method study. Nurse Educ. Today 34, 1057–1061. doi: 10.1016/j.nedt.2014.02.010
Chan, Z. C. (2017). A qualitative study on communication between nursing students and the family members of patients. Nurse Educ. Today 59, 33–37. doi: 10.1016/j.nedt.2017.08.017
Chang, H. Y., and Chang, H. L. (2021). A virtual simulation-based educational application about complementary and alternative medicine: a pilot study of nurses’ attitudes and communication competency. Nurse Educ. Today 97:104713. doi: 10.1016/j.nedt.2020.104713
Charlton, C. R., Dearing, K. S., Berry, J. A., and Johnson, M. J. (2008). Nurse practitioners’ communication styles and their impact on patient outcomes: an integrated literature review. J. Am. Acad. Nurse Pract. 20, 382–388. doi: 10.1111/j.1745-7599.2008.00336.x
Claramita, M., Tuah, R., Riskione, P., Prabandari, Y. S., and Effendy, C. (2016). Comparison of communication skills between trained and untrained students using a culturally sensitive nurse-client communication guideline in Indonesia. Nurse Educ. Today 36, 236–241. doi: 10.1016/j.nedt.2015.10.022
Clark, C. E., Conture, E. G., Frankel, C. B., and Walden, T. A. (2012). Communicative and psychological dimensions of the KiddyCAT. J. Commun. Disord. 45, 223–234. doi: 10.1016/j.jcomdis.2012.01.002
Coyle, N., Manna, R., Shen, M. J., Banerjee, S. C., Penn, S., Pehrson, C., et al. (2015). Discussing death, dying, and end-of-life goals of care: a communication skills training module for oncology nurses. Clin. J. Oncol. Nurs. 19, 697–702. doi: 10.1188/15.CJON.697-702
Cusatis, R., Holt, J. M., Williams, J., Nukuna, S., Asan, O., Flynn, K. E., et al. (2020). The impact of patient-generated contextual data on communication in clinical practice: a qualitative assessment of patient and clinician perspectives. Patient Educ. Couns. 103, 734–740. doi: 10.1016/j.pec.2019.10.020
Duhamel, F., and Talbot, L. R. (2004). A constructivist evaluation of family systems nursing interventions with families experiencing cardiovascular and cerebrovascular illness. J. Fam. Nurs. 10, 12–32. doi: 10.1177/1074840703260906
Epstein, R. M., Fiscella, K., Lesser, C. S., and Stange, K. C. (2010). Why the nation needs a policy push on patient-centered health care. Health Aff. 29, 1489–1495. doi: 10.1377/hlthaff.2009.0888
Ertz, M., Karakas, F., and Sarigöllü, E. (2016). Exploring pro-environmental behaviors of consumers: an analysis of contextual factors, attitude, and behaviors. J. Bus. Res. 69, 3971–3980. doi: 10.1016/j.jbusres.2016.06.010
Finke, E. H., Light, J., and Kitko, L. (2008). A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J. Clin. Nurs. 17, 2102–2115. doi: 10.1111/j.1365-2702.2008.02373.x
Finney Rutten, L. J., Agunwamba, A. A., Beckjord, E., Hesse, B. W., Moser, R. P., and Arora, N. K. (2015). The relation between having a usual source of care and ratings of care quality: does patient-centered communication play a role? J. Health Commun. 20, 759–765. doi: 10.1080/10810730.2015.1018592
Fishbein, M., and Cappella, J. N. (2006). The role of theory in developing effective health communications. J. Commun. 56, S1–S17. doi: 10.1111/j.1460-2466.2006.00280.x
Fornell, C., and Larcker, D. F. (1981). Evaluating structural equation models with unobservable variables and measurement error. J. Mark. Res. 18, 39–50. doi: 10.2307/3151312
Foronda, C., MacWilliams, B., and McArthur, E. (2016). Interprofessional communication in healthcare: an integrative review. Nurse Educ. Pract. 19, 36–40. doi: 10.1016/j.nepr.2016.04.005
Fukada, M. (2018). Nursing competency: definition, structure anddevelopment. Yonago Acta Med. 61, 1–7. doi: 10.33160/yam.2018.03.001
Gausvik, C., Lautar, A., Miller, L., Pallerla, H., and Schlaudecker, J. (2015). Structured nursing communication on interdisciplinary acute care teams improves perceptions of safety, efficiency, understanding of care plan and teamwork as well as job satisfaction. J. Multidiscip. Healthc. 8, 33–37. doi: 10.2147/JMDH.S72623
Gillett, K., O’Neill, B., and Bloomfield, J. G. (2016). Factors influencing the development of end-of-life communication skills: a focus group study of nursing and medical students. Nurse Educ. Today 36, 395–400. doi: 10.1016/j.nedt.2015.10.015
Giménez-Espert, M. C., and Prado-Gascó, V. J. (2018). The development and psychometric validation of an instrument to evaluate nurses’ attitudes towards communication with the patient (ACO). Nurse Educ. Today 64, 27–32. doi: 10.1016/j.nedt.2018.01.031
Givron, H., and Desseilles, M. (2021). Longitudinal study: impact of communication skills training and a traineeship on medical students’ attitudes toward communication skills. Patient Educ. Couns. 104, 785–791. doi: 10.1016/j.pec.2020.09.010
Grant, M. S., and Jenkins, L. S. (2014). Communication education for pre-licensure nursing students: literature review 2002-2013. Nurse Educ. Today 34, 1375–1381. doi: 10.1016/j.nedt.2014.07.009
Grassi, L., Caruso, R., and Costantini, A. (2015). Communication with patients suffering from serious physical illness. Adv. Psychosom. Med. 34, 10–23. doi: 10.1159/000369050
Gutiérrez-Puertas, L., Márquez-Hernández, V. V., Gutiérrez-Puertas, V., Granados-Gámez, G., and Aguilera-Manrique, G. (2020). Educational interventions for nursing students to develop communication skills with patients: a systematic review. Int. J. Environ. Res. Public Health 17:2241. doi: 10.3390/ijerph17072241
Hannawa, A. F., García-Jiménez, L., Candrian, C., Rossmann, C., and Schulz, P. J. (2015). Identifying the field of health communication. J. Health Commun. 20, 521–530. doi: 10.1080/10810730.2014.999891
Harman, H. H. (1980). Análisis factorial moderno [Modern factor analysis]. Chicago, IL: The University Of Chicago Press.
Hemsley, B., Balandin, S., and Worrall, L. (2012). Nursing the patient with complex communication needs: time as a barrier and a facilitator to successful communication in hospital. J. Adv. Nurs. 68, 116–126. doi: 10.1111/j.1365-2648.2011.05722.x
Howick, J., Moscrop, A., Mebius, A., Fanshawe, T. R., Lewith, G., Bishop, F. L., et al. (2018). Effects of empathic and positive communication in healthcare consultations: a systematic review and meta-analysis. J. R. Soc. Med. 111, 240–252. doi: 10.1177/0141076818769477
International Test Commission (2017). The ITC Guidelines for Translating and Adapting Tests (Second edition). Available online at: www.InTestCom.org (accessed February 21, 2021).
Kitson, A. L., Muntlin Athlin, Å, and Conroy, T., and International Learning Collaborative (2014). Anything but basic: nursing’s challenge in meeting patients’ fundamental care needs. J. Nurs. Scholarsh. 46, 331–339. doi: 10.1111/jnu.12081
Klakovich, M. D., and dela Cruz, F. A. (2006). Validating the interpersonal communication assessment scale. J. Prof. Nurs. 22, 60–67. doi: 10.1016/j.profnurs.2005.12.005
Koponen, J., Pyörälä, E., and Isotalus, P. (2012). Comparing three experiential learning methods and their effect on medical students’ attitudes to learning communication skills. Med. Teach. 34, e198–e207. doi: 10.3109/0142159X.2012.642828
Kourkouta, L., and Papathanasiou, I. (2014). Communication in nursing practice. Mater. Sociomed. 26, 65–67. doi: 10.5455/msm.2014.26.65-67
Levett-Jones, T., Cant, R., and Lapkin, S. (2019). A systematic review of the effectiveness of empathy education for undergraduate nursing students. Nurse Educ. Today 75, 80–94. doi: 10.1016/j.nedt.2019.01.006
Li, Y., Wang, X., Zhu, X. R., Zhu, Y. X., and Sun, J. (2019). Effectiveness of problem-based learning on the professional communication competencies of nursing students and nurses: a systematic review. Nurse Educ. Pract. 37, 45–55. doi: 10.1016/j.nepr.2019.04.015
Lin, M. F., Hsu, W. S., Huang, M. C., Su, Y. H., Crawford, P., and Tang, C. C. (2017). I couldn’t even talk to the patient’: barriers to communicating with cancer patients as perceived by nursing students. Eur. J. Cancer Care 26:e12648. doi: 10.1111/ecc.12648
Lloret-Segura, S., Ferreres-Traver, A., Hernández-Baeza, A., and Tomás-Marco, I. (2014). El análisis factorial exploratorio de los ítems: una guía práctica, revisada y actualizada. [Exploratory item factor analysis: a practical guide revised and updated]. Anales de Psicología 30, 1151–1169. doi: 10.6018/analesps.30.3.199361
Lorenzo-Seva, U., and Ferrando, P. J. (2006). FACTOR: a computer program to fit the exploratory factor analysis model. Behav. Res. Methods 38, 88–91. doi: 10.3758/BF03192753
MacLean, S., Kelly, M., Geddes, F., and Della, P. (2017). Use of simulated patients to develop communication skills in nursing education: an integrative review. Nurse Educ. Today 48, 90–98. doi: 10.1016/j.nedt.2016.09.018
McCallum, R. C., and Austin, J. T. (2000). Applications of structural equation modeling in psychological research. Annu. Rev. Psychol. 51, 201–226. doi: 10.1146/annurev.psych.51.1.201
Mullan, B. A., and Kothe, E. J. (2010). Evaluating a nursing communication skills training course: the relationships between self-rated ability, satisfaction, and actual performance. Nurse Educ. Pract. 10, 374–378. doi: 10.1016/j.nepr.2010.05.007
Peplau, H. E. (1991). Interpersonal Relations in Nursing: A Conceptual Frame of Reference for Psychodynamic Nursing. New York, NY: Springer Publishing Company.
Polit, D. F., and Beck, C. T. (2008). Nursing Research: Generating and Assessing Evidence for Nursing Practice, 8th Edn. Philadelphia: Lippincott Williams and Wilkins.
Rammstedt, B., Danner, D., and Bosnjak, M. (2017). Acquiescence response styles: a multilevel model explaining individual-level and country-level differences. Pers. Individ. Dif. 107, 190–194. doi: 10.1016/j.paid.2016.11.038
Rees, C., Sheard, C., and Davies, S. (2002). The development of a scale to measure medical students’ attitudes towards communication skills learning: the communication skills attitude scale (CSAS). Med. Educ. 36, 141–147. doi: 10.1046/j.1365-2923.2002.01072.x
Rosemond, C., Hanson, L. C., and Zimmerman, S. (2017). Goals of care or goals of trust? how family members perceive goals for dying nursing home residents. J. Palliat. Med. 20, 360–365. doi: 10.1089/jpm.2016.0271
Rosenberg, M. J., and Hovland, C. I. (1960). “Cognitive, affective and behavioral components of attitudes,” in Attitude Organization and Change: An Analysis of Consistency Among Attitude Components, eds M. J. Rosenberg and C. I. Hovland (New Haven: Yale University Press).
Sarikoc, G., Ozcan, C. T., and Elcin, M. (2017). The impact of using standardized patients in psychiatric cases on the levels of motivation and perceived learning of the nursing students. Nurse Educ. Today 51, 15–22. doi: 10.1016/j.nedt.2017.01.001
Satu, K. U., Leena, S., Mikko, S., Riitta, S., and Helena, L. K. (2013). Competence areas of nursing students in Europe. Nurse Educ. Today 33, 625–632. doi: 10.1016/j.nedt.2013.01.017
Shorey, S., Kowitlawakul, Y., Devi, M. K., Chen, H. C., Soong, S. K. A., and Ang, E. (2018). Blended learning pedagogy designed for communication module among undergraduate nursing students: a quasi-experimental study. Nurse Educ. Today 61, 120–126. doi: 10.1016/j.nedt.2017.11.011
Škodová, Z., Bánovèinová, L., and Bánovèinová, A. (2018). Attitudes towards communication skills among nursing students and its association with sense of coherence. Kontakt 20, e17–e22.
Suzuki, E., Azuma, T., Kobiyama, A., Takayama, Y., Sato, Y., Maruyama, A., et al. (2014). Situations Among Novice Nurses and Preceptor: They Cannot Be Assertive. Available online at: https://sigma.nursingrepository.org/handle/10755/335454 (accessed February 1, 2021).
Tanaka, J. S., and Huba, G. H. (1989). A general coefficient of determination for covariance structure models under arbitrary GLS estimation. Br. J. Math. Stat. Psychol. 42, 233–239. doi: 10.1111/j.2044-8317.1989.tb00912.x
The Joint Commission (2016). Sentinel Event Statistics Data – Event Type by Year (1995–Q2−2016). Available online at: https://www.jointcommission.org/se_data_event_type_by_year_/ (accessed January 15, 2021).
Ward, J., Cody, J., Schaal, M., and Hojat, M. (2012). The empathy enigma: an empirical study of decline in empathy among undergraduate nursing students. J. Prof. Nurs. 28, 34–40. doi: 10.1016/j.profnurs.2011.10.007
Watson, J. (2018). Unitary caring science: Philosophy and Praxis of Nursing. Boulder, CO: University Press of Colorado.
Wei, H., and Watson, J. (2019). Healthcare interprofessional team members’. Int. J. Nurs. Sci. 6, 17–23. doi: 10.1016/j.ijnss.2018.12.001
Wittenberg, E., Ragan, S. L., and Ferrell, B. (2017). Exploring nurse communication about spirituality. Am. J. Hosp. Palliat. Care 34, 566–571. doi: 10.1177/1049909116641630
World Health Organization (2017). Patient Safety: Making Healthcare Safer. Licence: CC, BY-NC-SA3.0, IGO. Available online at: https://apps.who.int/iris/handle/10665/255507 (accessed January 27, 2021).
World Medical Association (2013). “Ethical principles for medical research involving human subjects,” in Proceedings of the 64th WMA General Assembly October 2013, Fortaleza.
Keywords: attitude, communication, construct validation, nursing students, psychometric properties
Citation: Giménez-Espert MdC, Maldonado S, Pinazo D and Prado-Gascó V (2021) Adaptation and Validation of the Spanish Version of the Instrument to Evaluate Nurses’ Attitudes Toward Communication With the Patient for Nursing Students. Front. Psychol. 12:736809. doi: 10.3389/fpsyg.2021.736809
Received: 05 July 2021; Accepted: 19 October 2021;
Published: 25 November 2021.
Edited by:
Ernesto Lodi, University of Sassari, ItalyReviewed by:
Einav Srulovici, University of Haifa, IsraelCopyright © 2021 Giménez-Espert, Maldonado, Pinazo and Prado-Gascó. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: María del Carmen Giménez-Espert, bWFyaWEuYy5naW1lbmV6QHV2LmVz
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.