
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 26 October 2021
Sec. Psychopathology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.708579
Background: The symptoms of attention-deficit hyperactivity disorder (ADHD) are known to exacerbate the effect of cognitive-behavioral impairments on emotional burden. Although adults with ADHD frequently experience procrastination and internalizing symptoms such as depression and anxiety, few studies have examined whether the association between procrastination and internalizing symptoms differs by ADHD symptoms.
Objective: This study aimed to examine the moderating effect of ADHD symptoms on the association between procrastination and internalizing symptoms.
Method: A cross-sectional survey was conducted among 470 adults (mean age=26.57, standard deviation=2.93) using self-reported questionnaires: Adult ADHD Self-Report Scale, General Procrastination Scales, Patient Health Questionnaire-9, and State–Trait Anxiety Inventory.
Conclusion: Participants with more substantial ADHD symptoms experienced more procrastination and internalizing symptoms than those with the less substantial ADHD symptoms. Therefore, procrastination constitutes the treatment target for those suffering from ADHD and comorbid internalizing symptoms. Alternatively, there was no enhancing effect of ADHD symptoms on the association between procrastination and internalizing symptoms. It is necessary to examine more precise and valid hypotheses and underlying mechanisms of procrastination in high and low ADHD symptom groups.
Attention-deficit hyperactivity disorder (ADHD), which persists in 2.5–5% of adults (McCarthy et al., 2012; Polanczyk et al., 2014), is characterized by inattention and hyperactivity/impulsivity (American Psychiatric Association, 2013). People diagnosed with ADHD are likely to suffer from comorbid emotional conditions such as depression and anxiety (Chen et al., 2018). Severe depressive symptoms are commonly experienced by adults (Kessler et al., 2006; Torgersen et al., 2006) and emerging adults (aged 18–24years; Arnett et al., 2014) with ADHD (Biederman et al., 2010; Hinshaw et al., 2012; Meinzer et al., 2013). Adults with ADHD are also at a higher risk for developing anxiety disorders than the general population (Kessler et al., 2006). These emotional symptoms, usually summarized as “internalizing symptoms” (McElroy and Patalay, 2019), affect the life satisfaction of adults with ADHD (Yang et al., 2013).
To improve internalizing symptoms, it is necessary to approach the associated symptoms of ADHD as well as decreasing the cardinal symptoms (Safren et al., 2004, 2005; Knouse et al., 2013a). The associated symptoms occur because of a lack of skills for managing the cardinal symptoms of ADHD. Adult ADHD patients have such associated symptoms as procrastination, low frustration tolerance, severe mood swings, and low motivation, leading to various problems in daily life (Weiss and Weiss, 2004). Among these associated symptoms, adult ADHD patients experience procrastination frequently in their daily lives (Young and Bramham, 2007; Ramsay, 2017). Procrastination has been categorized as one of the functional disorders associated with the inattention symptom cluster of ADHD (Young and Bramham, 2007). According to the DSM-5 criteria, inattentive symptoms are associated with procrastination: “often does not follow through on instructions and fails to finish schoolwork, chores, or duties in the workplace (e.g., loses focus, side-tracked)”; “often has trouble organizing tasks and activities”; and “often avoids, dislikes, or is reluctant to do tasks that require mental effort over a long period of time (such as schoolwork or homework).” In a cross-sectional study of college students without an ADHD diagnosis, only inattentive symptoms were positively associated with procrastination after controlling for impulsivity/hyperactivity, while the correlation between impulsivity/hyperactivity and procrastination disappeared by controlling for inattention as measured by a questionnaire (Niermann and Scheres, 2014).
Procrastination has two aspects: maladaptive and adaptive. Maladaptive procrastination is defined as “voluntarily delay in an intended course of action despite expecting to be worse off due to the delay” (Steel, 2007). Several studies have found that procrastination is associated with high levels of depression and anxiety symptoms among emerging adults (van Eerde, 2003; Beutel et al., 2016). This maladaptive behavior also causes low work efficiency, financial difficulties, and poor academic achievement (Stead et al., 2010). In the general population, procrastination not only has maladaptive behaviors, but also adaptive aspects. The positive forms of delay (e.g., active procrastination; Chu and Choi, 2005) refer to self-managed time-management strategy for working under pressure and successfully meeting deadlines. The common element for both aspects of procrastination is the intentional delay, which is a personally important action (Klingsieck, 2013). Alternatively, the difference between both concepts is that maladaptive procrastination includes unnecessary and unreasonable delay (Steel, 2010). For example, college students who showed more adaptive procrastination had higher grades (Choi and Moran, 2009; Kim et al., 2017), and adaptive procrastination was positively correlated with intrinsic motivation, well-being (Habelrih and Hicks, 2015), self-efficacy, and self-regulation (Taura et al., 2015). In contrast to maladaptive procrastination, adaptive procrastination has positive psychosocial consequences due to the delay.
Procrastination, which can cause maladaptive problems, frequently appears in ADHD adults’ daily lives (Ramsay, 2020). Clinically, adults with ADHD experience procrastination as the most common functional impairment (Solanto et al., 2010; Ramsay, 2020). Chronic procrastination occurred more frequently in ADHD patients than those without ADHD regardless of gender (Ferrari and Sanders, 2006). Those with chronic procrastination were particularly prone to procrastination with thrill-seeking and avoidance functions. Furthermore, adults with ADHD procrastinate as a maladaptive compensatory strategy to avoid negative or stressful situations when faced with them (Ramsay and Rostain, 2008). Therefore, adults with ADHD might have more maladaptive procrastination compared to those without. These avoidant behaviors are major maintenance and aggravation factors common to depressive and anxiety symptoms (Ehrenreich-May and Chu, 2013). Similarly, in adult ADHD, avoidance behavior leads to internalizing symptoms (Bodalski et al., 2019). Previous studies have suggested that adults with ADHD might experience procrastination as more maladaptive and show a stronger relationship between procrastination and internalizing symptoms than healthy controls. However, principally, the relationship between procrastination and internalizing symptoms has only been studied in the general population, and little is known in the clinical population, such as people with ADHD.
The presence of ADHD tendencies may explain the inconsistent research on the effects of procrastination on psychiatric symptoms. These inconsistent findings show that effects of procrastination differ depending on the presence of ADHD tendencies. For instance, the adaptive aspects of procrastination require executive functional skills such as time management and planning strategies (van Eerde et al., 2015). Additionally, strategic putting off also demands skills related to reward sensitivity, assessing the consequences of behavior in terms of their long-term advantage or disadvantage, and engaging in or waiting to acquire the long-term advantages and avoid the disadvantages (Safren et al., 2004; Rozental and Carlbring, 2014). However, since ADHD symptoms display deficits in executive function and delayed reward aversion (Sonuga-Barke et al., 2010), these impairments prevent the skill of putting off adaptively. In addition to children, adult ADHD patients have diminished performance on executive function tasks, such as response inhibition and planning/organization, compared to the control group (Fabio and Caprì, 2017; Martino et al., 2017). Additionally, children with ADHD indicate difficulty waiting for delayed rewards and tendencies to choose immediate rewards when memory load is heavier (Fabio et al., 2020). Those adult ADHD patients with more executive dysfunction and reward impairments tend to display the greatest impairment in daily life functioning. Therefore, adaptive procrastination is reduced in cases with high ADHD tendencies, which may exacerbate the relationship between procrastination and clinical symptoms such as depression and anxiety. In the clinical practice, adult ADHD patients have been reported to experience more of maladaptive procrastination (Ramsay and Rostain, 2008). Furthermore, people with ADHD in emerging adulthood struggle with demands for autonomy and self-regulation, which overwhelm their cognitive capacities (Knouse and Fleming, 2016). Nonetheless, the synergistic effects of ADHD and procrastination on internalizing symptoms remain unclear. Procrastination is one of the most prevalent difficulties faced by adults with ADHD and may further exacerbate their internalizing symptoms.
Therefore, the current study aimed to investigate the moderating effect of ADHD symptoms on the association between procrastination and internalizing symptoms. Based on the literature regarding ADHD, procrastination, and internalizing symptoms, this study proposed the following three hypotheses: (a) People with ADHD exhibit more procrastination, (b) procrastination is positively correlated with depression and anxiety symptoms, and (c) ADHD symptoms strengthen this correlation.
All procedures of this study were approved by the institutional Ethics Review Committee on Research with Human Subjects of the first author’s affiliation (2018-282).
The online questionnaire survey was conducted among participants who had registered on an online survey company in Japan. It was executed during February and March 2019. Before completing the questionnaire, participants read an onscreen explanation about responding without compulsion as an ethical consideration. This study recruited 500 participants who were grouped according to their Adult ADHD Self-Report Scale-v1.1 (ASRS) score. The higher-level ADHD symptoms group (ADHD-H) were those who scored above the cutoff point of the ASRS Part A (Kessler et al., 2005), while the lower-level ADHD symptoms group (ADHD-L) included those with scores below the cutoff point; both groups had 250 participants each. The sample size was calculated using G power 3.1.9.4 with 0.01 alpha and 0.95 statistical power. The effect size was determined using recent reports on the correlation between the status of ADHD symptoms and procrastination (r=0.21, Ozel-Kizil et al., 2016; r=0.43, Niermann and Scheres, 2014) and between procrastination and depression/anxiety (r=0.36, Beutel et al., 2016; r=0.27, Hernández et al., 2019). The average effect size was r=0.25, which resulted in an estimated sample size of 240. As a reward, respondents received points that could redeem for goods within the system of the survey company.
To ensure the quality of the online survey, data from 10 of the 500 participants were excluded because their answers showed patterns of straightlining for all scales. Straightlining is defined as giving the same answer for all items in each scale (Simon, 1956; Schonlau and Toepoel, 2015); it is a type of satisficing response that has been used as an indicator of poor answer quality (Zhang and Conrad, 2013). Of the five measures in the current study, 339 (67.8%) participants did not show straightlining in any measure. Further, 88 (17.6%) participants showed straightlining in at least one measure, 36 (7.2%) in two, 17 (3.4%) in three, and 10 (2%) in four. The remaining 10 participants with straightlining in all five measures were excluded from the analyses for their refusal to answer. The final sample consisted of 490 participants (244 men; age: mean=26.56, standard deviation=2.91).
Attention-deficit hyperactivity disorder symptom status was assessed using the ASRS (Kessler et al., 2005). The first six items of this scale (Part A) are used for brief screening of ADHD symptoms in people aged 18years or older. This scale was scored using a 5-point Likert scale from 0 (never) to 4 (very often) to indicate ADHD symptoms. Responses like “often” and “very often” in all items were regarded as positive ADHD symptomatology. In the case of items 1, 2, and 3, a response of “sometimes” was also considered positive. This study defined ADHD-H as those who showed four or more positive responses for the first six items of the ASRS (Part A), which predicts an adult ADHD diagnosis based on the DSM-IV criteria (Kessler et al., 2007). This scale has high validity regarding the clinical diagnosis of ADHD as well as internal consistency reliability (Cronbach’s α=0.63–0.72) and test–retest reliability (r=0.58–0.77), and the area under the receiver operating characteristics curve (AUC) was 0.90 (Kessler et al., 2007).
Self-reported difficulties related to procrastination were determined using the General Procrastination Scale (GPS; Lay, 1986). The original English version of the GPS consists of 20 items, scored using a 5-point Likert scale from 1 (extremely uncharacteristic) to 5 (very characteristic). However, the Japanese version of the GPS (J-GPS; Hayashi, 2007) includes only 13 items, since seven were excluded during the translation and validation process. Higher scores indicate greater difficulties in everyday tasks, for example, “I often find myself performing tasks that I had intended to do the day before.” The Japanese version of the GPS has good construct validity and internal consistency reliability (Cronbach’s α=0.87) according to Hayashi (2007).
The Patient Health Questionnaire (PHQ-9; Kroenke et al., 2001) consists of nine items, scored using a 4-point Likert scale from 0 (not at all) to 3 (nearly every day). Higher scores indicate greater severity of depressive symptoms over the past 2weeks. The total score ranges from 0 to 27; scores over 20 indicate clinical severity. Internal consistency of the PHQ-9 has been shown to be high (Cronbach’s α=0.89; Kroenke et al., 2001, 2010). The reliability and validity of the Japanese version of the PHQ-9 were confirmed by Muramatsu et al. (2007).
The Japanese version of the State–Trait Anxiety Inventory (Hidano et al., 2000) is scored using a 4-point Likert scale from 1 (almost never) to 4 (almost always). The inventory consists of two subscales (state and trait anxiety) with 20 items each. However, this study used only the trait anxiety items to investigate the frequency anxiety which a person experiences anxiety with the highest stability over time. Higher scores indicate greater severity of anxiety symptoms. The total score ranges from 20 to 80, and the clinical significance level is over 55. The reliability and validity of the Japanese version of the State–Trait Anxiety Inventory were confirmed by Hidano et al. (2000): internal consistency reliability (Cronbach’s α=0.896 in men and α=0.904 in women) and test–retest reliability (r=0.58 in men and r=0.77 in women).
All statistical analyses were conducted using IBM SPSS Statistics 26.0 software (SPSS Inc., 2017). The analyses included the following four steps. First, descriptive statistics were calculated to check for data normality where skewness within −1.00 to +1.00 indicated a normal distribution. Second, each scale’s scores were compared between groups by t tests to examine the first hypothesis. Third, Pearson’s correlation coefficients were calculated between all variables to test the second hypothesis. Finally, two hierarchical multiple regression analyses using depression and anxiety symptoms as outcome variables were conducted to examine the last hypothesis. Four variables (gender, age, ADHD symptom status, and procrastination) were used as predictors in the first step. In the second step, the interaction variable (ADHD symptom status and procrastination) was added. The interaction term was calculated using ADHD symptom status and the centering procrastination score. It aimed to establish the moderating effect of ASRS Part A on the association between procrastination and symptoms of depression and anxiety. The model fit was assessed using the Akaike information criterion (AIC) and Bayesian information criterion (BIC).
An acceptable level of skewness was observed for all scales, indicating a normal distribution. The descriptive characteristics and t test for all variables are presented in Table 1 including mean, standard deviation, kurtosis, skewness, Cronbach’s alpha, t ratio, value of p, and Cohen’s d. The number of participants with clinical-level depression and anxiety in the ADHD-H group was 24 (9.68%) and 90 (36.29%), respectively, and 13 (5.37%) and 43 (17.77%), in the ADHD-L group, respectively.
Our analyses revealed significant differences between the two groups for all assessments (Table 1). Participants with more ADHD symptoms reported higher levels of procrastination, depression, and anxiety compared to those with fewer ADHD symptoms.
Table 2 shows the correlations among total ASRS Part A score, procrastination, depression, and anxiety. Pearson’s correlations revealed significantly positive correlations among procrastination and depression and anxiety.
Hierarchical multiple regression analyses using depressive and anxiety symptoms as outcome variables were conducted using all variables as predictors in the first step and adding the interaction of ADHD symptom status and procrastination as a predictor in the second step. These analyses allowed the examination of whether procrastination predicted internalizing symptom and if this relation is strengthened by ADHD symptom status as a moderator.
The results for depressive symptoms are presented in Table 3 and for anxiety symptoms are presented in Table 4. These analyses revealed that, in the first step, both ADHD symptom status [β=−0.121, B=−1.675, SE=0.651, p=0.010, CI (−2.953, −0.397)] and procrastination [β=0.232, B=0.182, SE=0.037, p<0.001, CI (0.109, 0.254)] had a statistically significant effect on depression after controlling for participants’ sex and age. ADHD symptom status [β=−0.152, B=−3.085, SE=0.909, p=0.001, CI (−4.871, −1.300)] and procrastination [β=0.341, B=0.392, SE=0.052, p<0.001, CI (0.290, 0.493)] also had a significant effect on trait anxiety. In contrast, in the second step, the interaction effect of ADHD symptom status and procrastination was not significantly associated with depression [β=−0.010, B=−0.017, SE=0.074, p=0.813, CI (−0.162, 0.128)] or trait anxiety [β=0.004, B=0.010, SE=0.103, p=0.919, CI (−0.192, 0.213)]. This interaction did not improve the prediction of depression (ΔR2<0.000, p=0.813, AIC=1862.159, BIC=1887.325) and anxiety symptoms (ΔR2<0.000, p=0.919, AIC=2189.647, BIC=2214.813) compared to first step in depression (AIC=1860.215, BIC=1881.187) and anxiety symptoms (AIC=2187.657, BIC=2208.629).
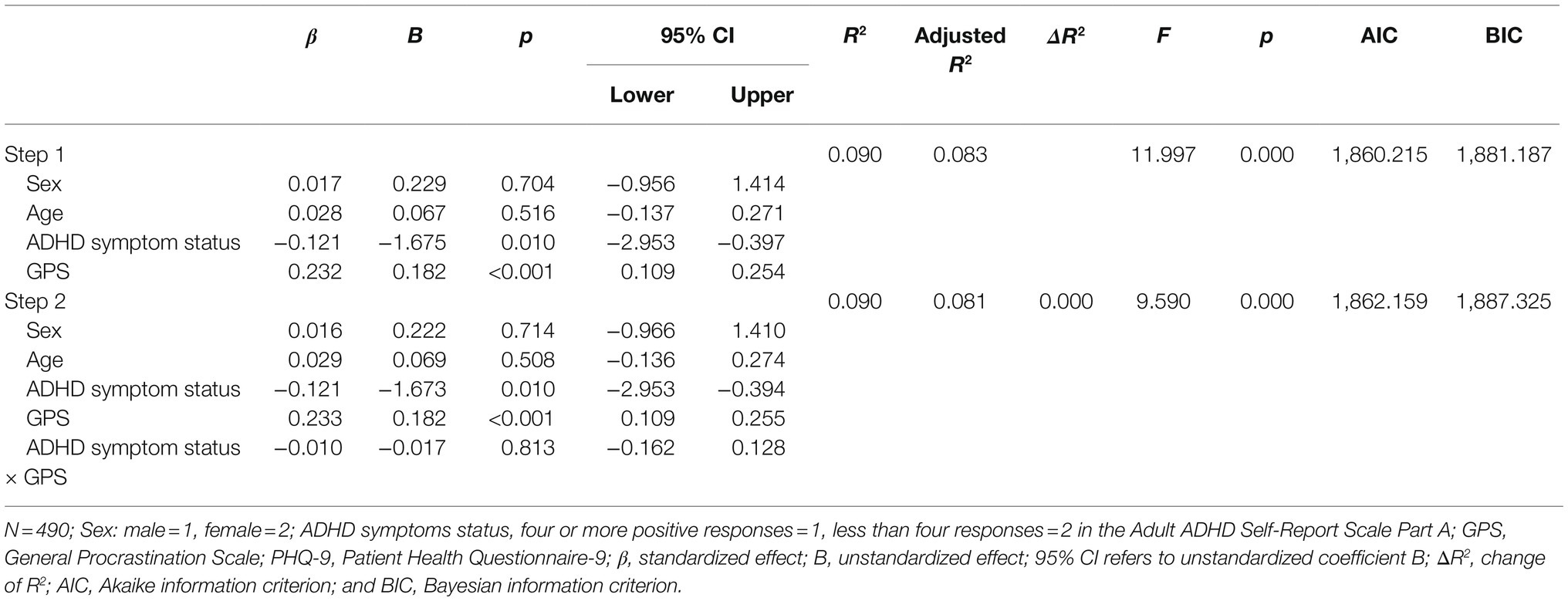
Table 3. Attention-deficit hyperactivity disorder symptom status, procrastination, and their interactions with PHQ.
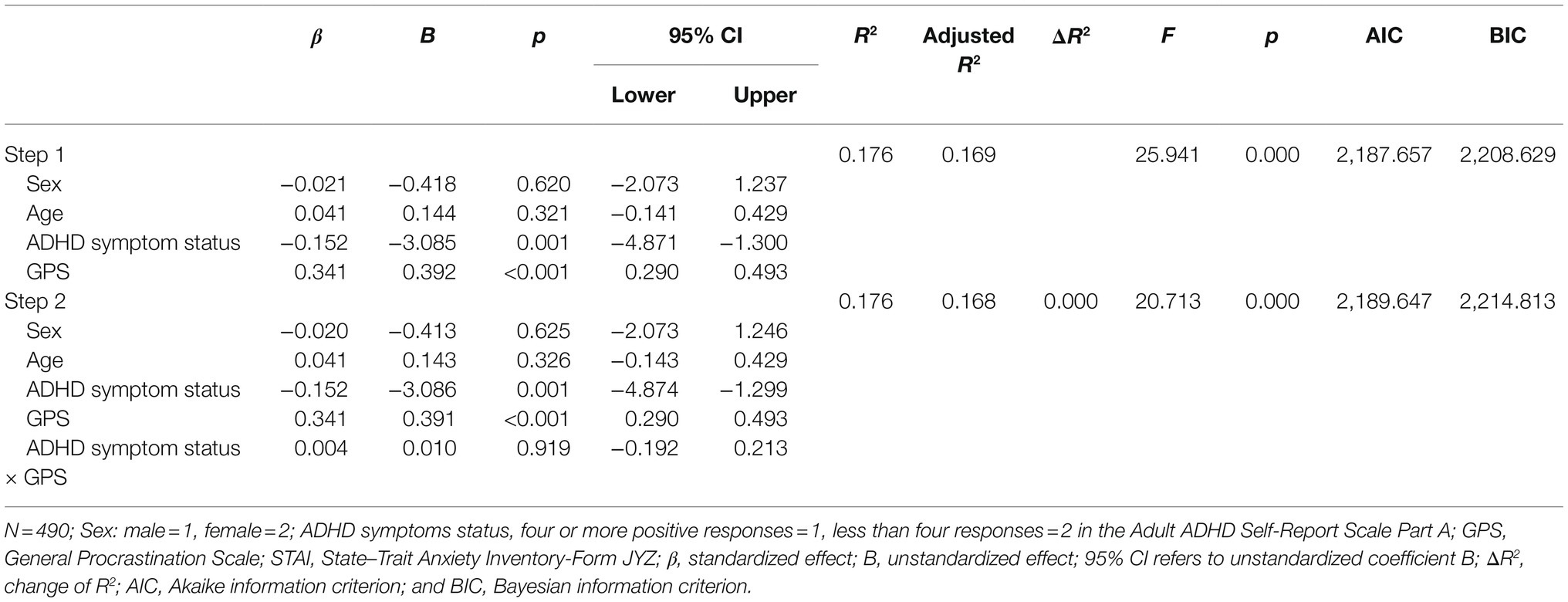
Table 4. Attention-deficit hyperactivity disorder symptom status, procrastination, and their interactions with STAI-T.
The present study aimed to examine the moderating effects of ADHD symptom status on the association between procrastination and internalizing symptoms. First, our analysis confirmed that adults with a higher ADHD symptom status showed more frequent procrastination than those with a lower ADHD symptom status. Participants in the ADHD-H group had higher scores for procrastination than those in the ADHD-L group, indicating a non-negligible effect size of Cohen’s d (0.83). This result is consistent with a previous study that compared academic procrastination in undergraduate students with or without ADHD symptoms status (Cohen’s d=0.65; Wood et al., 2019). Furthermore, the results of this study regarding participants with nonclinical ADHD symptoms are in line with previous findings that adults with ADHD diagnosis exhibit more procrastination (Ramsay, 2020). This suggests that procrastination constitutes an essential treatment target even for adults who are not diagnosed with but exhibit subthreshold ADHD symptoms. Second, the present study further confirmed the association between procrastination and symptoms of depression and anxiety, as observed in earlier studies (Solomon and Rothblum, 1984; van Eerde, 2003). This study observed a positive correlation between procrastination and depression and anxiety. Procrastination causes impairments in several daily life domains (Stead et al., 2010), which may, in turn, lead to internalizing symptoms.
Third, contrary to our hypothesis, ADHD symptom status had no moderating effect – that is, the association between procrastination and internalizing symptoms did not depend on the severity of ADHD symptoms. Although clinical perspectives have indicated that adults with ADHD are more likely to experience maladaptive procrastination in their daily lives (Ramsay and Rostain, 2008; Ramsay, 2020), our result did not provide any positive evidence to support it. The present study revealed that maladaptive procrastination is not a categorical problem due to ADHD symptoms. This result, which focused on procrastination as a behavioral impairment, is inconsistent with an earlier finding suggesting that ADHD exacerbates the association between cognitive burden and stress responses (Hirvikoski et al., 2009) and job functioning and conduct problems in young ADHD (Babinski et al., 2017).
Although this study did not support the hypothesis, its findings can be regarded as a significant step in understanding the role of ADHD in the onset of the procrastination. The current result suggested that association between procrastination and internalizing symptoms was not moderated by ADHD symptomatology, inattention, hyperactivity, and impulsivity. However, among the ADHD core symptoms, inattentiveness was found to be positively associated with elevated neuroticism (Knouse et al., 2013b), which predicts more frequent maladaptive procrastinations (Kim et al., 2017). Contrastingly, hyperactivity is positively associated with higher extroversion (Knouse et al., 2013a), which predicts more frequent adaptive procrastinations (Kim et al., 2017). Different ADHD symptoms may be associated with different aspects of procrastination. The ASRS used in this study was developed for screening ADHD and is unsuitable for measuring levels of different ADHD symptoms. Future studies should include scales that measure the different core symptoms of ADHD.
The present study has several limitations. First, all measurements were self-reported, meaning that the correlations observed here may be explained by the common method variance (Lindell and Whitney, 2001). Although many validated self-report questionnaires are available (Lay, 1986; Steel, 2010), the nature of procrastination should be captured using hierarchical multiple methods, such as observation from others (Rotenstein et al., 2009), laboratory tasks (Ferrari and Tice, 2000), and ecological momentary assessments (Wieland et al., 2018). Therefore, future research should use an objective indicator to measure procrastination.
Second, this study was a cross-sectional survey. Therefore, the direction of causality between procrastination and internalizing symptoms is unclear. In the case of depression, symptoms of sluggish activity might cause procrastination (Beutel et al., 2016). Regarding anxiety, previous studies have indicated that anxiety might increase procrastination (Steel, 2007). As an exception, Rozental et al. (2017) conducted a randomized clinical trial and reported that procrastination interventions reduced anxiety symptoms. Therefore, future studies should reveal the causal relationship between procrastination and internalizing symptoms using longitudinal or intervention studies.
Third, one of the six items of the ASRS Part A represents procrastination: “When you have a task that requires a lot of thought, how often do you avoid or delay getting started?” (Ustun et al., 2017) This overlap between measurement of ASRS and GPS may cause underestimation of the effect of procrastination. This measurement contamination could be avoided by utilizing the severity measure of ADHD excluding the procrastination item.
Finally, data for socioeconomic status, education level, intelligence quotient, or any other confounders were not collected. For instance, internalizing symptoms are known to be associated with the absence of partners (Roohafza et al., 2014), which may play an important role in coping with procrastination (Ferrari et al., 1999). Furthermore, the proportion of models in which procrastination explained internalizing symptoms was low, R2=0.090 for depressive symptoms and R2=0.176 for anxiety symptoms. The reason for this low explanatory rate results might be related to the attributes of the sample selected for this study. The attributes such as younger age and being a student affect procrastination (Beutel et al., 2016), which are inconsistent with the characteristics of the current participants. The present study focused on participants on the cusp of adulthood (18–30years old). The age group of 30 was the most frequently reported age group in low and high ADHD groups (17.4–18.1%). The largest age group of candidates enrolling and entering university/junior college in Japan is 18–22years. However, the proportion of 18–22years old in this sample is small: 14 (14.9% in ADHD high group) and 11 (8.3% in ADHD low group). Considering that 58.1% of students in Japan enter junior college/university (Ministry of Education, Culture Sports, Science and Technology, 2020), the proportion of students in this sample is relatively low. Since the sample’s age range in this study was different from those of the previous studies, the R2 of this model in the hierarchical multiple regression analysis might be low. Thus, confounding factors such as annual income, education, and other psychiatric disorders should be considered in future studies.
This study revealed that people with higher ADHD symptom levels exhibited procrastination more frequently and showed more internalizing symptoms such as depression and anxiety. Focusing on procrastination would be helpful for those who suffer from ADHD and internalizing symptoms. However, there was no moderating effect of ADHD symptoms on the association between procrastination and internalizing symptoms. We should examine more precise and valid hypotheses and underlying mechanisms of procrastination in high and low ADHD symptom groups.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
The studies involving human participants were reviewed and approved by the institutional Ethics Review Committee on Research with Human Subjects of the first author’s affiliation (2018-282). Written informed consent for participation was not required for this study in accordance with the national legislation and the institutional requirements.
MO designed and conducted the survey, undertook the statistical analyses, and wrote the draft manuscript. TT, YN, and HK managed the survey and all other issues related to conducting the research. MO, TT, YN, and HK contributed to the critical revision and have approved the final version of the manuscript. All authors contributed to the article and approved the submitted version.
This study was supported by grants from the Ibuka fund and JSPS KAKENHI grant Number 202023103.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
We would like to thank Editage (www.editage.com) for English language editing.
ADHD, Attention-deficit hyperactivity disorder; ASRS, Adult ADHD Self-Report Scale; ADHD-H, Higher-level ADHD symptoms group; ADHD-L, Lower-level ADHD symptoms group; AIC, Akaike information criterion; BIC, Bayesian information criterion; GPS, General Procrastination Scale; STAI-JYZ, Japanese version of the State–Trait Anxiety Inventory; PHQ-9, Patient Health Questionnaire.
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders. 5th Edn. Washington, DC: American Psychiatric Publishing.
Arnett, J. J., Žukauskienė, R., and Sugimura, K. (2014). The new life stage of emerging adulthood at ages 18–29 years: implications for mental health. Lancet Psychiatry 1, 569–176. doi: 10.1016/S2215-0366(14)00080-7
Babinski, D. E., Neely, K. A., Kunselman, A., and Waschbusch, D. A. (2017). Attention-deficit/hyperactivity disorder and callous-unemotional traits as moderators of conduct problems when examining impairment in emerging adults. Psychiatry Res. 258, 525–530. doi: 10.1016/j.psychres.2017.09.001
Beutel, M. E., Klein, E. M., Aufenanger, S., Brähler, E., Dreier, M., Müller, K. W., et al. (2016). Procrastination, distress and life satisfaction across the age range – a German representative community study. PLoS One 11:e0148054. doi: 10.1371/journal.pone.0148054
Biederman, J., Petty, C. R., Evans, M., Small, J., and Faraone, S. V. (2010). How persistent is ADHD? A controlled 10-year follow-up study of boys with ADHD. Psychiatry Res. 177, 299–304. doi: 10.1016/j.psychres.2009.12.010
Bodalski, E. A., Knouse, L. E., and Kovalev, D. (2019). Adult ADHD, emotion dysregulation, and functional outcomes: examining the role of emotion regulation strategies. J. Psychopathol. Behav. Assess. 41, 81–92. doi: 10.1007/s10862-018-9695-1
Chen, Q., Hartman, C. A., Haavik, J., Harro, J., Klungsøyr, K., Hegvik, T., et al. (2018). Common psychiatric and metabolic comorbidity of adult attention-deficit/hyperactivity disorder: a population-based cross-sectional study. PLoS One 13:e0204516. doi: 10.1371/journal.pone.0204516
Choi, J. N., and Moran, S. V. (2009). Why not procrastinate? Development and validation of a new active procrastination scale. J. Soc. Psychol. 149, 195–211. doi: 10.3200/SOCP.149.2.195-212
Chu, A. H. C., and Choi, J. N. (2005). Rethinking procrastination: positive effects of “active” procrastination behavior on attitudes and performance. J. Soc. Psychol. 145, 245–264. doi: 10.3200/SOCP.145.3.245-264
Ehrenreich-May, J., and Chu, B. C. (eds.) (2013). Transdiagnostic Treatments for Children and Adolescents: Principles and Practice. New York, NY: The Guilford Press.
Fabio, R., Bianco, M., Caprì, T., Marino, F., Ruta, L., Vagni, D., et al. (2020). Working memory and decision making in children with ADHD: an analysis of delay discounting with the use of the dual-task paradigm. BMC Psychiatry 20:272. doi: 10.1186/s12888-020-02677-y
Fabio, R. A., and Caprì, T. (2017). The executive functions in a sample of Italian adults with ADHD: attention, response inhibition and planning/organization. Mediterr. J. Clin. Psychol. 5, 1–17. doi: 10.6092/2282-1619/2017.5.1636
Ferrari, J. R., Harriott, J. S., and Zimmerman, M. (1999). The social support networks of procrastinators: friends or family in times of trouble? Personal. Individ. Differ. 26, 321–331. doi: 10.1016/S0191-8869(98)00141-X
Ferrari, J. R., and Sanders, S. R. (2006). Procrastination rates among adults with and without AD/HD: a pilot study. Couns. Clin. Psychol. J. 3, 2–9.
Ferrari, J. R., and Tice, D. M. (2000). Procrastination as a self-handicap for men and women: a task-avoidance strategy in a laboratory setting. J. Res. Pers. 34, 73–83. doi: 10.1006/jrpe.1999.2261
Habelrih, E. A., and Hicks, R. E. (2015). Psychological well-being and its relationships with active and passive procrastination. Int. J. Psychol. Stud. 7, 25–34. doi: 10.5539/ijps.v7n3p25
Hayashi, J. (2007). Development of Japanese version of General Procrastination Scale. Jpn. J. Pers. 15, 246–248. doi: 10.2132/personality.15.246
Hernández, C., Ottenberger, D. R., Moessner, M., Crosby, R. D., and Ditzen, B. (2019). Depressed and swiping my problems for later: the moderation effect between procrastination and depressive symptomatology on internet addiction. Comput. Hum. Behav. 97, 1–9. doi: 10.1016/j.chb.2019.02.027
Hidano, T., Fukuhara, M., Iwawaki, S., Soga, S., and Spielberger, C. D. (2000). Shin-ban STAI Manyuaru [New STAI Manual State-Trait Anxiety Inventory-Form JYZ]. Tokyo, Japan: Jitsumu Kyoiku Shuppan.
Hinshaw, S. P., Owens, E. B., Zalecki, C., Huggins, S. P., Montenegro-Nevado, A. J., Schrodek, E., et al. (2012). Prospective follow-up of girls with attention-deficit/hyperactivity disorder into early adulthood: continuing impairment includes elevated risk for suicide attempts and self-injury. J. Consult. Clin. Psychol. 80, 1041–1051. doi: 10.1037/a0029451
Hirvikoski, T., Lindholm, T., Nordenström, A., Nordström, A., and Lajic, S. (2009). High self-perceived stress and many stressors, but normal diurnal cortisol rhythm, in adults with ADHD (attention-deficit/hyperactivity disorder). Horm. Behav. 55, 418–424. doi: 10.1016/j.yhbeh.2008.12.004
Kessler, R. C., Adler, L., Ames, M., Demler, O., Faraone, S., Hiripi, E., et al. (2005). The World Health Organization adult ADHD Self-Report Scale (ASRS): a short screening scale for use in the general population. Psychol. Med. 35, 245–256. doi: 10.1017/S0033291704002892
Kessler, R. C., Adler, L., Barkley, R., Biederman, J., Conners, C. K., Demler, L., et al. (2006). The prevalence and correlates of adult ADHD in the United States: results from the national comorbidity survey replication. Am. J. Psychiatry 163, 716–723. doi: 10.1176/ajp.2006.163.4.716
Kessler, R. C., Adler, L. A., Gruber, M. J., Sarawate, C. A., Spencer, T., and Van Brunt, D. L. (2007). Validity of the World Health Organization adult ADHD Self-Report Scale (ASRS) screener in a representative sample of health plan members. Int. J. Methods Psychiatr. Res. 16, 52–65. doi: 10.1002/mpr.208
Kim, S., Fernandez, S., and Terrier, L. (2017). Procrastination, personality traits, and academic performance: when active and passive procrastination tell a different story. Personal. Individ. Differ. 108, 154–157. doi: 10.1016/j.paid.2016.12.021
Klingsieck, K. B. (2013). Procrastination: when good things don’t come to those who wait. Eur. Psychol. 18, 24–34. doi: 10.1027/1016-9040/a000138
Knouse, L. E., and Fleming, A. P. (2016). Applying cognitive-behavioral therapy for ADHD to emerging adults. Cogn. Behav. Pract. 23, 300–315. doi: 10.1016/j.cbpra.2016.03.008
Knouse, L. E., Traeger, L., O’Cleirigh, C., and Safren, S. A. (2013a). Adult attention deficit hyperactivity disorder symptoms and five-factor model traits in a clinical sample: a structural equation modeling approach. J. Nerv. Ment. Dis. 201, 848–854. doi: 10.1097/NMD.0b013e3182a5bf33
Knouse, L. E., Zvorsky, I., and Safren, S. A. (2013b). Depression in adults with attention-deficit/hyperactivity disorder (ADHD): the mediating role of cognitive-behavioral factors. Cognit. Ther. Res. 37, 1220–1232. doi: 10.1007/s10608-013-9569-5
Kroenke, K., Spitzer, R. L., and Williams, J. B. W. (2001). The PHQ-9. Validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Kroenke, K., Spitzer, R. L., Williams, J. B., and Löwe, B. (2010). The Patient Health Questionnaire somatic, anxiety, and depressive symptom scales: a systematic review. Gen. Hosp. Psychiatry 32, 345–359. doi: 10.1016/j.genhosppsych.2010.03.006
Lay, C. H. (1986). At last, my research article on procrastination. J. Res. Pers. 20, 474–495. doi: 10.1016/0092-6566(86)90127-3
Lindell, M. K., and Whitney, D. J. (2001). Accounting for common method variance in cross-sectional research designs. J. Appl. Psychol. 86, 114–121. doi: 10.1037/0021-9010.86.1.114
Martino, G., Caprì, T., Castriciano, C., and Fabio, R. A. (2017). Automatic deficits can lead to executive deficits in ADHD. Mediterr. J. Clin. Psychol. 5, 1–32. doi: 10.6092/2282-1619/2017.5.1669
McCarthy, S., Wilton, L., Murray, M. L., Hodgkins, P., Asherson, P., and Wong, I. C. (2012). The epidemiology of pharmacologically treated attention deficit hyperactivity disorder (ADHD) in children, adolescents, and adults in UK primary care. BMC Pediatr. 12:78. doi: 10.1186/1471-2431-12-78
McElroy, E., and Patalay, P. (2019). In search of disorders: internalizing symptom networks in a large clinical sample. J. Child Psychol. Psychiatry 60, 897–906. doi: 10.1111/jcpp.13044
Meinzer, M. C., Lewinsohn, P. M., Pettit, J. W., Seeley, J. R., Gau, J. M., Chronis-Tuscano, A., et al. (2013). Attention-deficit hyperactivity disorder in adolescence predicts onset of major depressive disorder through early adulthood. Depress. Anxiety 30, 546–553. doi: 10.1002/da.22082
Ministry of Education, Culture Sports, Science and Technology (2020). The school basic survey (in Japanese). Available at: https://www.mext.go.jp/content/20200825-mxt_chousa01-1419591_8.pdf (Accessed September 15, 2021).
Muramatsu, K., Kamijima, K., Yoshida, M., Otsubo, T., Miyaoka, H., Muramatsu, Y., et al. (2007). The Patient Health Questionnaire, Japanese version: validity according to the mini-international neuropsychiatric interview-plus. Psychol. Rep. 101, 952–960. doi: 10.2466/pr0.101.3.952-960
Niermann, H. C. M., and Scheres, A. (2014). The relation between procrastination and symptoms of attention-deficit hyperactivity disorder (ADHD) in undergraduate students. Int. J. Methods Psychiatr. Res. 23, 411–421. doi: 10.1002/mpr.1440
Ozel-Kizil, E. T., Kokurcan, A., Aksoy, U. M., Kanat, B. B., Sakarya, D., Bastug, G., et al. (2016). Hyperfocusing as a dimension of adult attention deficit hyperactivity disorder. Res. Dev. Disabil. 59, 351–358. doi: 10.1016/j.ridd.2016.09.016
Polanczyk, G. V., Willcutt, E. G., Salum, G. A., Kieling, C., and Rohde, L. A. (2014). ADHD prevalence estimates across three decades: an updated systematic review and meta-regression analysis. Int. J. Epidemiol. 43, 434–442. doi: 10.1093/ije/dyt261
Ramsay, J. R. (2017). The relevance of cognitive distortions in the psychosocial treatment of adult ADHD. Prof. Psychol. Res. Pract. 48, 62–69. doi: 10.1037/pro0000101
Ramsay, J. R. (2020). Rethinking Adult ADHD. Helping Clients Turn Intentions into Actions. Washington, DC: American Psychological Association.
Ramsay, J. R., and Rostain, A. L. (2008). Cognitive-Behavioral Therapy for Adult ADHD: An Integrative Psychosocial and Medical Approach Routledge/Taylor & Francis Group.
Roohafza, H. R., Afshar, H., Keshteli, A. H., Mohammadi, N., Feizi, A., Taslimi, M., et al. (2014). What’s the role of perceived social support and coping styles in depression and anxiety? J. Res. Med. Sci. 19, 944–949.
Rotenstein, A., Davis, H. Z., and Tatum, L. (2009). Early birds versus juts-in-timers: the effect of procrastination on academic performance of accounting students. J. Account. Educ. 27, 223–232. doi: 10.1016/j.jaccedu.2010.08.001
Rozental, A., and Carlbring, P. (2014). Understanding and treating procrastination: a review of a common self-regulatory failure. Psychology 5, 1488–1502. doi: 10.4236/psych.2014.513160
Rozental, A., Forsell, E., Svensson, A., Andersson, G., and Carlbring, P. (2017). Overcoming procrastination: one-year follow-up and predictors of change in a randomized controlled trial of internet-based cognitive behavior therapy. Cogn. Behav. Ther. 46, 177–195. doi: 10.1080/16506073.2016.1236287
Safren, S. A., Otto, M. W., Sprich, S., Winett, C. L., Wilens, T. E., and Biederman, J. (2005). Cognitive-behavioral therapy for ADHD in medication-treated adults with continued symptoms. Behav. Res. Ther. 43, 831–842. doi: 10.1016/j.brat.2004.07.001
Safren, S. A., Sprich, S., Chulvick, S., and Otto, M. W. (2004). Psychosocial treatments for adults with attention-deficit/hyperactivity disorder. Psychiatr. Clin. N. Am. 27, 349–360. doi: 10.1016/S0193-953X(03)00089-3
Schonlau, M., and Toepoel, V. (2015). Straightlining in web survey panels over time. Survey Res. Meth. 9, 125–137. doi: 10.18148/srm/2015.v9i2.6128
Simon, H. (1956). Rational choice and the structure of the environment. Psychol. Rev. 63, 129–138. doi: 10.1037/h0042769
Solanto, M. V., Marks, D. J., Wasserstein, J., Mitchell, K., Abikoff, H., Alvir, J. M. J., et al. (2010). Efficacy of meta-cognitive therapy (MCT) for adult ADHD. Am. J. Psychiatry 167, 958–968. doi: 10.1176/appi.ajp.2009.09081123
Solomon, L. J., and Rothblum, E. D. (1984). Academic procrastination: frequency and cognitive-behavioral correlates. J. Couns. Psychol. 31, 503–509. doi: 10.1037/0022-0167.31.4.503
Sonuga-Barke, E., Bitsakou, P., and Thompson, M. (2010). Beyond the dual pathway model: evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. J. Am. Acad. Child Adolesc. Psychiatry 49, 345–355. doi: 10.1016/j.jaac.2009.12.018
SPSS Statistics 26.0 software (SPSS Inc. 2017). Version 26.0, SPSS Inc, Japan, Armonk, NY: IBM Corp.
Stead, R., Shanahan, M. J., and Neufeld, R. W. J. (2010). “I’ll go to therapy, eventually”: procrastination, stress and mental health. Personal. Individ. Differ. 49, 175–180. doi: 10.1016/j.paid.2010.03.028
Steel, P. (2007). The nature of procrastination: a meta-analytic and theoretical review of quintessential self-regulatory failure. Psychol. Bull. 133, 65–94. doi: 10.1037/0033-2909.133.1.65
Steel, P. (2010). Arousal, avoidant and decisional procrastinators: do they exist? Personal. Individ. Differ. 48, 926–934. doi: 10.1016/j.paid.2010.02.025
Taura, A. A., Abdullah, M. C., Roslan, S., and Omar, Z. (2015). Relationship between self-efficacy, task value, self-regulation strategies and active procrastination among pre-service teachers in colleges of education. Int. J. Psychol. Couns. 7, 11–17.
Torgersen, T., Gjervan, B., Polit, C., and Rasmussen, K. (2006). ADHD in adults: a study of clinical characteristics, impairment and comorbidity. Nord. J. Psychiatry 60, 38–43. doi: 10.1080/08039480500520665
Ustun, B., Adler, L. A., Rudin, C., Faraone, S. V., Spencer, T. J., Berglund, P., et al. (2017). The World Health Organization adult attention-deficit/hyperactivity disorder self-report screening scale for DSM-5. JAMA Psychiatry 74, 520–526. doi: 10.1001/jamapsychiatry.2017.0298
van Eerde, W. (2003). A meta-analytically derived nomological network of procrastination. Personal. Individ. Differ. 35, 1401–1418. doi: 10.1016/S0191-8869(02)00358-6
van Eerde, W. (2015). Time management and procrastination. in The psychology of planning in organizations: Research and applications 35, 312–333. eds M. D. Mumford and M. Frese Routledge/Taylor & Francis Group.
Weiss, M. D., and Weiss, J. R. (2004). A guide to the treatment of adults with ADHD. J. Clin. Psychiatry 65, 27–37.
Wieland, L. M., Grunschel, C., Limberger, M. F., Schlotz, W., Ferrari, J. R., and Ebner-Priemer, U. (2018). The ecological momentary assessment of procrastination in daily life: psychometric properties of a five-item short scale. N. Am. J. Psychol. 20, 315–340.
Wood, W. L. M., Lewandowski, L. J., and Lovett, B. J. (2019). Profiles of diagnosed and undiagnosed college students meeting ADHD symptom criteria. J. Atten. Disord. 25, 646–656. doi: 10.1177/1087054718824991
Yang, H., Tai, Y., Yang, L., and Gau, S. S. (2013). Prediction of childhood ADHD symptoms to quality of life in young adults: adult ADHD and anxiety/depression as mediators. Res. Dev. Disabil. 34, 3168–3181. doi: 10.1016/j.ridd.2013.06.011
Young, S., and Bramham, J. (2007). ADHD in Adults: A Psychological Guide to Practice. Chichester: John Wiley & Sons.
Keywords: attention-deficit hyperactivity disorder, procrastination, depression, anxiety, emerging adulthood
Citation: Oguchi M, Takahashi T, Nitta Y and Kumano H (2021) The Moderating Effect of Attention-Deficit Hyperactivity Disorder Symptoms on the Relationship Between Procrastination and Internalizing Symptoms in the General Adult Population. Front. Psychol. 12:708579. doi: 10.3389/fpsyg.2021.708579
Received: 13 May 2021; Accepted: 23 September 2021;
Published: 26 October 2021.
Edited by:
Henry W. Chase, University of Pittsburgh, United StatesReviewed by:
Rosa Angela Fabio, University of Messina, ItalyCopyright © 2021 Oguchi, Takahashi, Nitta and Kumano. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mana Oguchi, b2d1Y2hpbWEzOTRAZ21haWwuY29t
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.