
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
SYSTEMATIC REVIEW article
Front. Psychol. , 11 June 2021
Sec. Health Psychology
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.661078
This article is part of the Research Topic Psychosocial Effects of Isolation and Fear of Contagion of COVID-19 on the Mental Health of Different Population Groups View all 32 articles
Background: Due to lack of preparedness of health systems, fast spread of the new virus, high mortality rates, and lack of a definite treatment, the outbreak of Coronavirus disease (COVID-19) led to high levels of fear and anxiety in different populations. In addition, isolation, mental disorders, and limitations in social interactions as a result of lockdown and travel ban increased the fear of the new coronavirus.
Methods: International databases, including Scopus, PubMed, Web of Science, and Google scholar, were searched without any time limitation, and all observational studies published in English reporting the mean of fear of COVID-19 based on the Fear of COVID-19 scale (FCV-19S) were included in the analysis. Methodological quality was assessed using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines. Random effects model, subgroup analysis, and meta-regression analysis were used to analyze the data. Heterogeneity across studies was examined using Cochran's Q test and I2 statistic. All the statistical analyses were conducted using R software v4.0.3.
Results: A total of 44 articles with a sample size of 52,462 were reviewed. A pooled mean of 18.57 was found for fear of COVID-19. The mean of fear of COVID-19 was higher in women than in men (20.67 vs. 18.21). The highest and lowest means of fear of COVID-19 had been found in Asia (18.36) and Australia (17.43) based on continent, and in hospital staff (19.51) and college students (17.95) based on target population, respectively. In addition, the highest and lowest means of fear of COVID-19 were related to items #1 and #3 of the scale, respectively. According to the results of meta-regression analysis, there was no significant association between the mean of fear of COVID-19 and sample size and participants' age. In addition, publication error was not significant (P = 0.721).
Conclusion: The mean of fear of COVID-19 was high around the world; therefore, it seems necessary to pay more attention to the negative effects of the COVID-19 pandemic on mental health.
The Coronavirus disease (COVID-19) pandemic was first reported in Hubei, China, in December 2019. So far, it has affected about six million people and has led to the death of more than 360,000 people around the world mostly due to severe acute respiratory illness (Ashamalla et al., 2020). Given the lack of an effective treatment for COVID-19, different countries around the world focused their efforts on reducing the risk of transmission through implementing public health measures, such as social distancing, self-isolation, and regular hand washing. In addition, unprecedented measures, such as controlling borders, contact tracing, and lockdown were taken (Ahorsu et al., 2020a; Alyami et al., 2020). These measures led to widespread fear so that in some countries people started to stockpile staple foods, toilet paper, and even guns (Bakioğlu et al., 2020; Skoda et al., 2020). As the prevalence of COVID-19 increased, people started to isolate themselves, limit their social interactions, and avoid others for fear of getting the virus (Abuhammad et al., 2020). Fear is an adaptive response to one's environment and a defense mechanism to increase the chance of one's survival; however, it can be maladaptive when it is not proportionate to the actual threat (Steimer, 2002).
During the Severe Acute Respiratory Syndrome (SARS) and Ebola outbreaks, public fear worsened the negative effects of the actual illness; therefore, one of the most important challenges in the face of outbreaks is to control social reactions (García-Reyna et al., 2020). In order to reduce possible psychological problems, researchers recommend that the level of fear, worry, and helplessness associated with COVID-19 should be examined, because high levels of stress may prevent one from making logical decisions to protect themselves (Ahorsu et al., 2020a). For example, some patients who need medical care may refuse to go to the hospital due to experiencing illogical levels of fear (WongLaura et al., 2020). Some patients may postpone their surgical treatment for fear of contracting the virus (Vanni et al., 2020). In some cases, fear of COVID-19 can lead to hypochondriasis, so that some people may misinterpret their bodily sensations and attribute them to COVID-19 (Coelho et al., 2020). Some people may also excessively use medications recommended in COVID-19 treatment guidelines, such as hydroxychloroquine (Banerjee, 2020). On the other hand, fear can act as a motivator of behavioral change in the face of COVID-19 (Harper et al., 2020; Pakpour and Griffiths, 2020). The experience of fear can increase risk perception and reinforce protective behaviors, such as washing of hands and keeping physical distance (Broche-Pérez et al., 2020). When people take a threat seriously, they can perform preventive measures more efficiently, and perception of threat as a motivator facilitates the prevention of COVID-19. Harper et al. found that fear of COVID-19 strongly predicted improved social distancing and hand washing and had an important role in adherence to public health measures related to COVID-19 (Harper et al., 2020).
The COVID-19 pandemic has led to fear and negative emotions; however, it has also had positive consequences, such as encouraging people to engage in ethical behavior (Jian et al., 2020). According to what was explained above, measuring fear of COVID-19 has an important role in understating the implications of the pandemic for mental health and in designing interventions to reduce COVID-19 fear and anxiety. One of the most important instruments available to assess fear of COVID-19 is the Fear of COVID-19 Scale (FCV-19S) that has been translated to many languages. Studies form different parts of the world examining fear of COVID-19 have led to different results. Therefore, the goal of the present systematic review and meta-analysis is to estimate the pooled mean of fear of COVID-19 around the world.
The present systematic review and meta-analysis aimed to estimate the pooled mean of fear of COVID-19 based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2009).
Search for articles was conducted in September 20, 2020, in databases of Web of science/ISI, PubMed, and Scopus using the following keywords: Wuhan Coronavirus, Sars-cov-2, 2019 Novel Coronavirus, COVID-19 Virus, Coronavirus Disease 2019 Virus, Wuhan Seafood Market Pneumonia Virus, Fear, and all possible combination to increase search sensitivity. In addition, references of the selected articles were reviewed to access more related articles.
All observational studies published in English examining the state of fear of COVID-19 using the FCV-19S were analyzed. This scale developed by Ahorsu et al. assesses fear of COVID-19 using seven items that are rated on a Likert-type scale ranging from 5 (totally agree) to 1 (totally disagree). Total score on this scale ranges from 7 to 35, and higher scores indicate stronger fear of COVID-19 (Ahorsu et al., 2020a). The inclusion criteria were as follows: participants aged at least 18 years and reporting the mean and standard deviation of fear of COVID-19 score. Articles with unavailable full texts, preprinted articles, and articles not reporting the fear of COVID-19 score were excluded from the analysis.
In the first step, two independent authors screened the articles and selected those having the aforementioned keywords in their titles or abstracts. Then, they extracted the article information and recorded it in a predesigned Excel sheet. This information included first author's name, publication year, mean age of patients, target population, mean and standard deviations of fear of COVID-19 (total score and score by gender). Because all the selected articles had been published in 2020, publication year was not included in the table presenting article information.
The two researchers independently evaluated the quality of the articles based on 10 items of Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (title and abstract, study environment, objectives and hypotheses, sample size, inclusion criteria, statistical methods, descriptive data, interpretation of findings, limitations, and funding). Higher scores indicate better methodological quality. In terms of methodological quality, articles were divided into three categories: poor (4 or below), moderate (4 to 7), and good (over 7) (Vandenbroucke et al., 2007).
Random effects model was used to estimate the pooled raw mean of fear of COVID-19. A forest plot was used to visually depict heterogeneity across studies in which the mean of fear of COVID-19 with a 95% confidence interval and also the pooled raw mean of the selected studies are reported. Heterogeneity across studies was assessed using I2 statistic and Cochran's Q test. I2 percentages of 25%, 50%, and 75% show low, average, and high heterogeneity, respectively, and in Cochran's Q test, P < 0.1 indicates significant heterogeneity (Higgins et al., 2003). Source of heterogeneity across studies was examined using subgroup analysis by gender, continent (Asia/America/Europe/Australia/multi-countries), and target population (general population, college students, pregnant women, and medical staff).
The association of the mean of fear of COVID-19 with sample size and mean age of participants was assessed using meta-regression analysis. To ensure that the meta-regression results were not affected by one or several articles, leave-one-out sensitivity analysis method was used that involved performing the analysis on the data by leaving out one study at a time. For studies reporting scores by drop out one study at a time and estimate the pooled raw mean of remained studies. In addition, the potential effect of small studies was assessed using a funnel plot based on Egger's regression test (Egger et al., 1997). It is worthwhile to note that all analyses were performed based on random effects model using R software, version 4.0.3, and that all statistical tests were two-tailed ones. In addition, the significance level for all tests except for examination of heterogeneity across studies was set at P < 0.05.
In the primary search, a total of 634 articles were found, of which 320 duplicate articles were excluded, and titles and abstracts of the remaining articles were reviewed. In addition, 270 articles focused on unrelated subjects were removed from the analysis. Figure 1 shows the flowchart of selecting and screening articles based on the PRISMA guidelines.
A total of 44 articles with a sample size of 52,462 were included in the final analysis. As shown in Table 1, among the 44 articles, 33 reported the total score of fear of COVID-19, 8 reported this score by gender, and 17 reported the mean scores by item (Abuhammad et al., 2020; Alyami et al., 2020; Bitan et al., 2020; Cavalheiro and Sticca, 2020; Caycho-Rodríguez et al., 2020; Elemo et al., 2020; Giordani et al., 2020; Huarcaya-Victoria et al., 2020; Martínez-Lorca et al., 2020; Masuyama et al., 2020; Pang et al., 2020; Sakib et al., 2020; Satici et al., 2020a; Soraci et al., 2020; Winter et al., 2020; Zolotov et al., 2020). There were two groups of participants in the Winter et al. study; therefore, results were reported separately for each group. In eight studies, the mean of fear of COVID-19 was reported by gender (Abad et al., 2020; Bakioğlu et al., 2020; Broche-Pérez et al., 2020; Haktanir et al., 2020; Hossain et al., 2020; Mertens et al., 2020; Nguyen et al., 2020a; Sakib et al., 2020). These studies had been conducted with the general population, college students, pregnant women, and medical staff. Detailed information on selection of articles is provided in Table 1. In terms of methodological quality, eight studies had medium quality, and the remaining articles had excellent quality.
According to the level of heterogeneity across studies, random effects model was used to combine the studies (P < 0.0001; Q = 8243.69, df = 32, P < 0.0001, τ2 = 7.9730, and I2= 99.6%). In the present study, the pooled mean of fear of COVID-19 was found to be 18.57 (95% CI: 17.60–19.54). In addition, the prediction interval for the pooled mean of fear of COVID-19 was found to be 12.72–24.42 (Figure 2). Among the selected studies, 17 reported the mean of fear of COVID-19 by item; the highest and lowest mean scores were related to items #1 (3.32) and #3 (1.78), respectively. It is worthwhile to note that the mean of fear of COVD-19 for all items was higher in Asian studies compared to those conducted in other continents. The lowest scores on items #1, #3, #5, and #6 were reported by the American studies, the lowest scores on items #4 and #7 were reported by Australian studies, and the lowest scores on item #2 were reported by European studies. In addition, the mean of fear of COVD-19 on all items except for items #1 and #4 was higher in the general population than in college students. The pooled mean of fear of COVD-19 by item is presented in Table 2 (Supplementary Figures 1–7).
The pooled raw mean of fear of COVID-19 was examined using random effects model. According to the results of subgroup analysis, the highest and lowest pooled means of fear of COVID-19 were reported in the studies conducted in Asia (18.36, 95% CI: 16.88–19.84) and Australia (17.43, 95% CI: 15.51–19.34), respectively (Supplementary Figure 8). In addition, the pooled raw mean of fear of COVID-19 was higher in medical staff than in other groups (Supplementary Figure 9).
According to the results of subgroup difference test reported in Table 3, there was a significant difference in the mean of fear of COVID-19 in different continents (P = 0.0347), but there was no significant difference between different target populations (P = 0.0773). In addition, eight articles reported the mean of fear of COVID-19 by gender that was lower in men (18.21, 95% CI: 15.99–20.42) than in women (20.67, 95% CI: 18.62–22.73) (Supplementary Figures 10, 11). Moreover, the mean fear of COVID-19 was 17.68 and 19.70 in Asian men and women and 16.15 and 20.39 in American men and women, respectively (Supplementary Figures 12, 13).
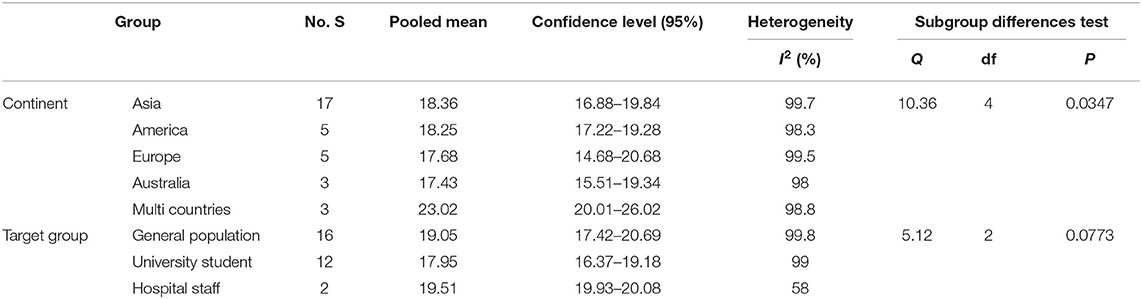
Table 3. Subgroup analysis of the pooled mean of fear of COVID-19 by continent and target population.
The results of meta-regression analysis showed that mean score of fear of COVID-19 increased with mean age, but the relationship was not statistically significant (P = 0.797) (Figure 3 and Table 4).
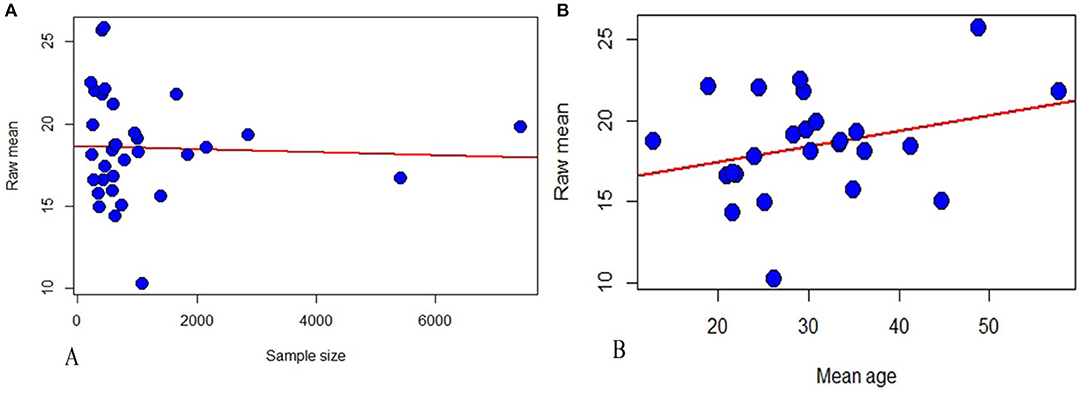
Figure 3. Meta-regression analysis of the relationship between mean of fear of COVID-19 and sample size (A) and mean age of participants (B).
Results of sensitivity analysis based on random effects model showed that none of the studies alone had a substantial impact on the pooled raw mean of fear of COVID-19 (Supplementary Figure 14). Results of Egger's regression test also indicated that publication bias was not statistically significant (P = 0.721) (Supplementary Figure 15).
Examination of the pooled mean by continent and target population showed that on all items, it was higher in the studies conducted in Asia compared to those conducted in other continents. In addition, the pooled mean of fear of COVID-19 on all items except for items #1 and #4 was higher in the general population than in college students (Table 5). Moreover, a significant difference was observed between studies conducted in different continents in terms of scores on item #2 of the scale (P < 0.0001), but there was no significant difference between different continents in terms of scores on other items. In addition, a significant difference was observed between different target populations in scores on items #6 and #7 (P < 0.05).
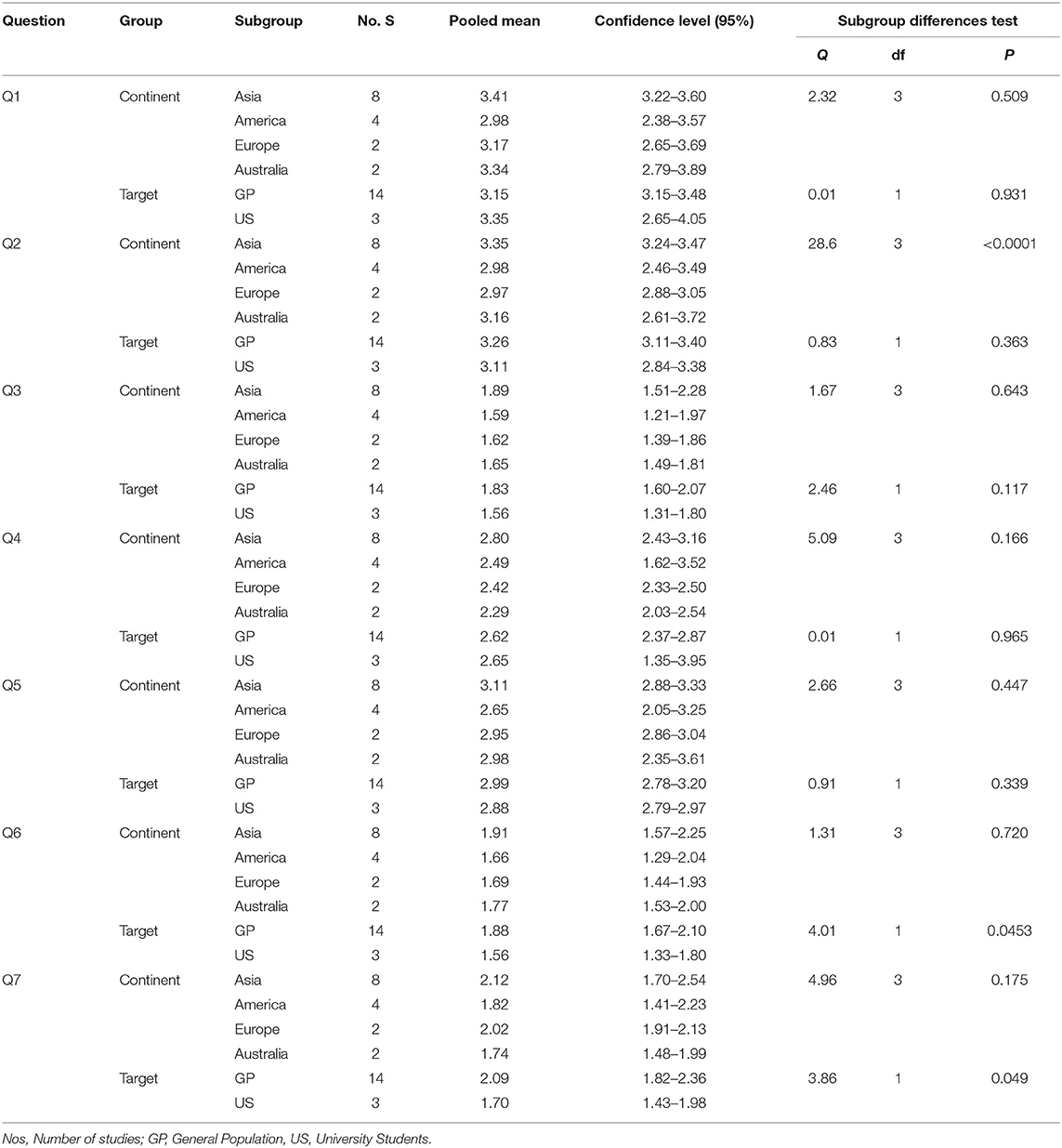
Table 5. Subgroup analysis of the mean of different items of the FCV-19s by continent and target population.
The present systematic review and meta-analysis aimed to estimate the pooled mean of fear of COVID-19. The results showed that the participants in the reviewed studies had obtained 41% of the total score on the the FCV-19s. Fear of COVID-19 leads to stigmatization and social exclusion of patients and their families, and makes them vulnerable to adjustment problems, depression, irritability, anxiety, and anger (Abad et al., 2020; Satici et al., 2020b; Zhang et al., 2020). Therefore, it is important to pay attention to implications of COVID-19 for psychological health, because pandemics can lead to crisis in psychological, social, and economic domains (Xiang et al., 2020). Fear is not limited to the COVID-19 pandemic and has been observed in other outbreaks, including those of HIV and SARS (Ho et al., 2005). The pooled mean of fear of COVID-19 was higher in women than in men. This finding can be attributed to the fact that women are more delicate and vulnerable than men. In addition, Bakioğlu et al. (2020) found that it was more acceptable for women to express their fears of illness. On the other hand, it is more acceptable for men to be strong and brave. In addition, because men are less likely than women to become ill, they tend to be less afraid of COVID-19. The results of the present study showed that the highest and lowest fears of COVID-19 scores were in studies conducted in Asia and Australia, respectively. This finding can be attributed to the fact that before spreading to other countries, COVID-19 was reported in China as an Asian country; therefore, people in China and other Asian countries experienced higher levels of fear of the new virus. Overall, different rates of fear of COVID-19 in different countries can be attributed to contextual and cultural factors and different levels of access to medical services. Isolation as a result of the COVID-19 pandemic led to increased rates of mental problems, such as anxiety, anger, PTSD, confusion, and even suicide (Giordani et al., 2020; Haktanir et al., 2020; Mamun and Griffiths, 2020a). For example, a Bangladeshi man killed himself because he thought that he had the new virus, but the autopsy showed that he actually did not (Mamun and Griffiths, 2020b). Therefore, misconceptions about COVID-19 can lead to increased xenophobia and suicide ideation. The same pattern had been observed during the SARS outbreak in Asia (Hong Kong) (Cheung et al., 2008).
The pooled mean of fear of COVID-19 was higher in medical staff than in other target groups. This group became involved in fighting the new virus when health systems were not adequately prepared to respond to the pandemic (1). Long-term exposure to confirmed and also unrecognized COVID-19 patients, insufficient training on prevention and control of infectious diseases, and shortage of protective equipment were factors putting healthcare providers at higher risk of COVID-19 and, as a result, fear of the pandemic (Wang et al., 2020; Zhou et al., 2020). Nguyen et al. showed that the risk of testing positive for COVID-19 was three times higher in healthcare workers than in the general population (Nguyen et al., 2020b). Fear in healthcare providers is not limited to COVID-19 and has been reported during other outbreaks, including those of HIV (Montgomery and Lewis, 1995) and SARS (Ho et al., 2005). The highest and lowest pooled means were related to items #1 and #3 of the scale, respectively. This finding can be attributed to what the items assess. Item #1 directly assesses fear of COVID-19, while item #3 asks about symptoms of fear of COVID-19. One of the limitations of this study was the exclusion of preprint studies. Due to the large number of studies, it was not possible to review this type of articles in this meta-analysis and it is suggested that this type of articles be reviewed in future studies.
The excessive fear observed in previous outbreaks, including those of HIV and Ebola, has also been reported in the current COVID-19 pandemic and can be observed in the future. Excessive fear can negatively impact one's life in personal (e.g., mental health problems) and social (panic shopping and xenophobia) domains, while a normal (logical) level of fear can help one pay more attention to government measures aimed at reducing the spread of COVID-19 (33). The results of the present study showed that a moderate level of fear is required to reduce the risk of contracting COVID-19 and that fear of COVID-19 can be controlled and prevented from turning into excessive fear through providing effective training programs for different populations.
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the Corresponding author.
FL and RGG: data collection and manuscript preparation. RGG: manuscript preparation and study conceptualization. QL: study design. SS and RGG: search strategy. QL and FL: final revision and grammar editing. SD: statistical analysis.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.661078/full#supplementary-material
Abad, A., da Silva, J. A., de Paiva Teixeira, L. E., Antonelli-Ponti, M., Bastos, S., Mármora, C. H., et al. (2020). Evaluation of fear and peritraumatic distress during COVID-19 pandemic in brazil. Adv. Infect. Dis. 10:184. doi: 10.4236/aid.2020.103019
Abuhammad, S., Alzoubi, K., and Khabour, O. (2020). Fear of COVID-19 and stigmatization toward infected people among jordanian people. Int. J. Clin. Pract. 75:e13899. doi: 10.1111/ijcp.13899
Ahorsu, D. K., Imani, V., Lin, C. Y., Timpka, T., Broström, A., Updegraff, J. A., et al. (2020c). Associations between fear of COVID-19, mental health, and preventive behaviours across pregnant women and husbands: an actor-Partner interdependence modelling. Int. J. Ment. Health Addict. 1–15. doi: 10.1007/s11469-020-00340-x
Ahorsu, D. K., Lin, C. Y., Imani, V., Saffari, M., Griffiths, M. D., and Pakpour, A. H. (2020a). The fear of COVID-19 scale: development and initial validation. Int. J. Mental Health Addict. 27, 1–9. doi: 10.1007/s11469-020-00270-8
Ahorsu, D. K., Lin, C. Y., and Pakpour, A. H. (2020b). The association between health status and insomnia, mental health, and preventive behaviors: the mediating role of fear of COVID-19. Gerontol. Geriatr. Med. 6:2333721420966081. doi: 10.1177/2333721420966081
Alyami, M., Henning, M., Krägeloh, C. U., and Alyami, H. (2020). Psychometric evaluation of the arabic version of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00316-x
Ashamalla, M., Chaudhary, H., Hevroni, G., Salifu, M. O., and McFarlane, S. I. (2020). Acute cord compression left untreated for fear of contracting COVID-19: a Case report and a call for health care plans for oncologic emergencies during crisis. Am. J. Med. Case Rep. 8, 397–399. doi: 10.12691/ajmcr-8-11-5
Bakioğlu, F., Korkmaz, O., and Ercan, H. (2020). Fear of COVID-19 and positivity: mediating role of intolerance of uncertainty, depression, anxiety, and stress. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00331-y
Banerjee, D. (2020). The other side of COVID-19: impact on obsessive compulsive disorder (OCD) and hoarding. Psychiatry Res. 288:112966. doi: 10.1016/j.psychres.2020.112966
Bitan, D. T., Grossman-Giron, A., Bloch, Y., Mayer, Y., Shiffman, N., and Mendlovic, S. (2020). Fear of COVID-19 scale: psychometric characteristics, reliability and validity in the israeli population. Psychiatry Res. 289:113100. doi: 10.1016/j.psychres.2020.113100
Broche-Pérez, Y., Fernández-Fleites, Z., Jiménez-Puig, E., Fernández-Castillo, E., and Rodríguez-Martin, B. C. (2020). Gender and fear of COVID-19 in a cuban population sample. Int. J. Ment. Health Addict. 1–9. doi: 10.1007/s11469-020-00343-8
Cavalheiro, F. R. S., and Sticca, M. G. (2020). Adaptation and validation of the brazilian version of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 1–9. doi: 10.1007/s11469-020-00415-9
Caycho-Rodríguez, T., Vilca, L. W., Cervigni, M., Gallegos, M., Martino, P., Portillo, N., et al. (2020). Fear of COVID-19 scale: validity, reliability and factorial invariance in argentina's general population. Death Stud. 28, 1–10. doi: 10.1080/07481187.2020.1836071
Cheung, Y. T., Chau, P. H., and P. S. Y.. (2008). A revisit on older adults suicides and severe acute respiratory syndrome (SARS) epidemic in hong kong. Int. J. Geriatr. Psychiatry 23, 1231–1238. doi: 10.1002/gps.2056
Coelho, C. M., Suttiwan, P., Arato, N., and Zsido, A. N. (2020). On the nature of fear and anxiety triggered by COVID-19. Front Psychol. 11:3109. doi: 10.3389/fpsyg.2020.581314
Egger, M., Smith, G. D., Schneider, M., and Minder, C. J. B. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ. 315, 629–634. doi: 10.1136/bmj.315.7109.629
Elemo, A. S., Satici, S. A., and Griffiths, M. D. (2020). The fear of COVID-19 scale: psychometric properties of the ethiopian amharic version. Int. J. Ment. Health Addict. 3, 1–2. doi: 10.1007/s11469-020-00448-0
García-Reyna, B., Castillo-García, G. D., Barbosa-Camacho, F. J., Cervantes-Cardona, G. A., Cervantes-Pérez, E., Torres-Mendoza, B. M., et al. (2020). Fear of COVID-19 scale for hospital staff in regional hospitals in mexico: a brief report. Int. J. Ment. Health Addict. 1–12. doi: 10.1007/s11469-020-00413-x
Gasparro, R., Scandurra, C., Maldonato, N. M., Dolce, P., Bochicchio, V., Valletta, A., et al. (2020). Perceived job insecurity and depressive symptoms among italian dentists: the moderating role of fear of cOVID-19. Int. J. Environ. Res. Public Health 17:5338. doi: 10.3390/ijerph17155338
Giordani, R. C., Zanoni da Silva, M., Muhl, C., and Giolo, S. R. (2020). Fear of cOVID-19 scale: assessing fear of the coronavirus pandemic in brazil. J. Health Psychol. 16:1359105320982035. doi: 10.1177/1359105320982035
Haktanir, A., Seki, T., and Dilmaç, B. (2020). Adaptation and evaluation of turkish version of the fear of COVID-19 scale. Death Stud. 28, 1–9. doi: 10.1080/07481187.2020.1773026
Harper, C. A., Satchell, L. P., Fido, D., and Latzman, R. D. (2020). Functional fear predicts public health compliance in the COVID-19 pandemic. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00281-5
Higgins, J. P., Thompson, S. G., Deeks, J. J., and Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ 327, 557–560. doi: 10.1136/bmj.327.7414.557
Ho, S. M., Kwong-Lo, R. S., Mak, C. W., and Wong, J. S. (2005). Fear of severe acute respiratory syndrome (SARS) among health care workers. J. Consult. Clin. Psychol. 73:344. doi: 10.1037/0022-006X.73.2.344
Hossain, M. A., Jahid, M. I. K., Hossain, K. M. A., Walton, L. M., Uddin, Z., Haque, M. O., et al. (2020). Knowledge, attitudes, and fear of COVID-19 during the rapid rise period in bangladesh. PLoS ONE 15:e0239646. doi: 10.1371/journal.pone.0239646
Huarcaya-Victoria, J., Villarreal-Zegarra, D., Podestà, A., and Luna-Cuadros, M. A. (2020). Psychometric properties of a spanish version of the fear of COVID-19 scale in general population of lima, peru. Int. J. Ment. Health Addict. 1–14. doi: 10.1007/s11469-020-00354-5
Isralowitz, R., Khamenka, N., Konstantinov, V., Gritsenko, V., and Reznik, A. (2020). Fear, depression, substance misuse and related conditions among multi-national medical students at the peak of the COVID-19 epidemic. J. Loss Trauma 1–4. doi: 10.1080/15325024.2020.1799521
Jaspal, R., Lopes, B., and Lopes, P. (2020). Fear, social isolation and compulsive buying in response to COVID-19 in a religiously diverse UK sample. Ment. Health Relig Cult. 23, 427–442. doi: 10.1080/13674676.2020.1784119
Jian, Y. F., Yu, I. Y., Yang, M. X., and Zeng, K. J. (2020). The impacts of fear and uncertainty of COVID-19 on environmental concerns, brand trust, and behavioral intentions toward green hotels. Sustainability 12:8688. doi: 10.3390/su12208688
Kaya, S., Uzdil, Z., and Cakiroğlu, F. P. (2020). Evaluation of the effects of fear and anxiety on nutrition during the COVID-19 pandemic in turkey. Public Health Nutr. 25, 1–8. doi: 10.1017/S1368980020003845
Konstantinov, V., Berdenova, S., Satkangulova, G., Reznik, A., and Isralowitz, R. (2020). COVID-19 impact on kazakhstan University student fear, mental health, and substance use. Int. J. Ment. Health Addict. 1–7. doi: 10.1007/s11469-020-00412-y
Labrague, L. J., and de Los Santos, J. A. (2020). Fear of covid-19, psychological distress, work satisfaction and turnover intention among frontline nurses. J. Nurs. Manag. 29, 395–403. doi: 10.1111/jonm.13168
Lin, C. Y., Broström, A., Griffiths, M. D., and Pakpour, A. H. (2020). Investigating mediated effects of fear of COVID-19 and COVID-19 misunderstanding in the association between problematic social media use, psychological distress, and insomnia. Internet Interven. 21:100345. doi: 10.1016/j.invent.2020.100345
Mamun, M. A., and Griffiths, M. D. (2020a). A rare case of bangladeshi student suicide by gunshot due to unusual multiple causalities. Asian J. Psychiatry. 49:101951. doi: 10.1016/j.ajp.2020.101951
Mamun, M. A., and Griffiths, M. D. (2020b). First COVID-19 suicide case in bangladesh due to fear of COVID-19 and xenophobia: possible suicide prevention strategies. Asian J. Psychiatry. 51:102073. doi: 10.1016/j.ajp.2020.102073
Martínez-Lorca, M., Martínez-Lorca, A., Criado-Álvarez, J. J., and Armesilla, M. D. (2020). The fear of COVID-19 scale: validation in spanish University students. Psychiatry Res. 2:113350. doi: 10.1016/j.psychres.2020.113350
Masuyama, A., Shinkawa, H., and Kubo, T. (2020). Validation and psychometric properties of the Japanese version of the fear of COVID-19 scale among adolescents. Int. J. Ment. Health Addict. 1–11. doi: 10.1007/s11469-020-00368-z
Mertens, G., Gerritsen, L., Duijndam, S., Salemink, E., and Engelhard, I. M. (2020). Fear of the coronavirus (COVID-19): predictors in an online study conducted in march. J. Anxiety Disord. 74:102258. doi: 10.1016/j.janxdis.2020.102258
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., and med, PGJP. (2009). Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Montgomery, K., and Lewis, C. E. (1995). Fear of HIV contagion as workplace stress: behavioral consequences and buffers. J. Healthcare Manag. 40:439.
Nguyen, H. T., Do, B. N., Pham, K. M., Kim, G. B., Dam, H. T. B., Nguyen, T. T., et al. (2020a). Fear of COVID-19 scale—associations of its scores with health literacy and health-related behaviors among medical students. Int. J. Environ. Res. Public Health 17, 1–14. doi: 10.3390/ijerph17114164
Nguyen, L. H., Drew, D. A., Graham, M. S., Joshi, A. D., Guo, C.-G., Ma, W., et al. (2020b). Risk of cOVID-19 among front-line health-care workers and the general community: a prospective cohort study. medRxiv 5:e475–e483. doi: 10.1101/2020.04.29.20084111
Pakpour, A. H., and Griffiths, M. D. (2020). The fear of COVID-19 and its role in preventive behaviors. J. Concurrent Disord. 2, 58–63.
Pang, N. T., Kamu, A., Hambali, N. L., Mun, H. C., Kassim, M. A., Mohamed, N. H., et al. (2020). Malay version of the fear of cOVID-19 scale: validity and reliability. Int. J. Ment. Health Addict. 3, 1–0. doi: 10.1007/s11469-020-00373-2
Perz, C. A., Lang, B. A., and Harrington, R. (2020). Validation of the fear of COVID-19 scale in a US college sample. Int. J. Ment. Health Addict. 1–11. doi: 10.1007/s11469-020-00356-3
Rahman, M. A., Hoque, N., Alif, S. M., Salehin, M., Islam, S. M. S., Banik, B., et al. (2020). Factors associated with psychological distress, fear and coping strategies during the cOVID-19 pandemic in australia. Global. Health. 16:95. doi: 10.1186/s12992-020-00624-w
Reznik, A., Gritsenko, V., Konstantinov, V., Khamenka, N., and Isralowitz, R. (2020). COVID-19 fear in eastern europe: validation of the fear of COVID-19 [0mm][3mm]scale. Int. J. Ment. Health Addict. 1–6. doi: 10.1007/s11469-020-00283-3
Rodríguez-Hidalgo, A. J., Pantaleón, Y., Dios, I., and Falla, D. (2020). Fear of cOVID-19, stress, and anxiety in University undergraduate students: a predictive model for depression. Front. Psychol. 11:591797. doi: 10.3389/fpsyg.2020.591797
Sakib, N., Bhuiyan, A. I., Hossain, S., Al Mamun, F., Hosen, I., Abdullah, A. H., et al. (2020). Psychometric validation of the bangla fear of COVID-19 scale: confirmatory factor analysis and rasch analysis. Int. J. Ment. Health Addict. 11, 1–2. doi: 10.1007/s11469-020-00289-x
Salehi, L., Rahimzadeh, M., Molaei, E., Zaheri, H., and Esmaelzadeh-Saeieh, S. (2020). The relationship among fear and anxiety of COVID-19, pregnancy experience, and mental health disorder in pregnant women: a structural equation model. Brain Behav. 10:e01835. doi: 10.1002/brb3.1835
Saravanan, C., Mahmoud, I., Elshami, W., and Taha, M. H. (2020). Knowledge, anxiety, fear, and psychological distress about COVID-19 among University students in the united arab emirates. Front Psychiatry. 11:582189. doi: 10.3389/fpsyt.2020.582189
Saricali, M., Satici, S. A., Satici, B., Gocet-Tekin, E., and Griffiths, M. D. (2020). Fear of COVID-19, mindfulness, humor, and hopelessness: a multiple mediation analysis. Int J. Ment Health Addict. 1–14. doi: 10.1007/s11469-020-00419-5
Satici, B., Gocet-Tekin, E., Deniz, M. E., and Satici, S. A. (2020a). Adaptation of the fear of COVID-19 scale: its association with psychological distress and life satisfaction in Turkey. Int. J. Ment. Health Addict. 1–9. doi: 10.1007/s11469-020-00294-0
Satici, B., Saricali, M., Satici, S. A., and Griffiths, M. D. (2020b). Intolerance of uncertainty and mental wellbeing: serial mediation by rumination and fear of COVID-19. Int. J. Ment. Health Addict. 1–12. doi: 10.1007/s11469-020-00305-0
Seyed Hashemi, S. G., Hosseinnezhad, S., Dini, S., Griffiths, M. D., Lin, C. Y., and Pakpour, A. H. (2020). The mediating effect of the cyberchondria and anxiety sensitivity in the association between problematic internet use, metacognition beliefs, and fear of COVID-19 among iranian online population. Heliyon 6:e05135. doi: 10.1016/j.heliyon.2020.e05135
Skoda, E. M., Bäuerle, A., Schweda, A., Dörrie, N., Musche, V., Hetkamp, M., et al. (2020). Severely increased generalized anxiety, but not COVID-19-related fear in individuals with mental illnesses: a population based cross-sectional study in germany. Int. J. Soc. Psychiatry. 20764020960773. doi: 10.1177/0020764020960773
Soraci, P., Ferrari, A., Abbiati, F. A., Del Fante, E., De Pace, R., Urso, A., et al. (2020). Validation and psychometric evaluation of the italian version of the fear of COVID-19 scale. Int. J. Ment. Health Addict. 4, 1–10. doi: 10.1007/s11469-020-00277-1
Steimer, T. (2002). The biology of fear-and anxiety-related behaviors. Dialogues Clin. Neurosci. 4:231. doi: 10.31887/DCNS.2002.4.3/tsteimer
Vandenbroucke, J. P., Von Elm, E., Altman, D. G., Gøtzsche, P. C., Mulrow, C. D., Pocock, S. J., et al. (2007). Strengthening the reporting of observational studies in epidemiology (STROBE): explanation and elaboration. PLoS Med. 4:e297. doi: 10.1371/journal.pmed.0040297
Vanni, G., Materazzo, M., Pellicciaro, M., Ingallinella, S., Rho, M., Santori, F., et al. (2020). Breast cancer and cOVID-19: the effect of fear on patients' decision-making process. In Vivo. 34, 1651–1659. doi: 10.21873/invivo.11957
Wang, J., Zhou, M., and Liu, F. (2020). Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hosp. Infect. 105, 100–101. doi: 10.1016/j.jhin.2020.03.002
Winter, T., Riordan, B. C., Pakpour, A. H., Griffiths, M. D., Mason, A., Poulgrain, J. W., et al. (2020). Evaluation of the english version of the fear of cOVID-19 scale and its relationship with behavior change and political beliefs. Int. J. Ment. Health Addict. 1–11. doi: 10.1007/s11469-020-00342-9
WongLaura, E., HawkinsJessica, E., and MurrellKaren, L. (2020). Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catalyst Innovations Care Deliv. 14, 1–12.
Xiang, Y. T., Yang, Y., Li, W., Zhang, L., Zhang, Q., Cheung, T., et al. (2020). Timely mental health care for the 2019 novel coronavirus outbreak is urgently needed. Lancet Psychiatry 7, 228–229. doi: 10.1016/S2215-0366(20)30046-8
Yehudai, M., Bender, S., Gritsenko, V., Konstantinov, V., Reznik, A., and Isralowitz, R. (2020). COVID-19 fear, mental health, and substance misuse conditions among University social work students in israel and russia. Int. J. Ment. Health Addict. 6, 1–8. doi: 10.1007/s11469-020-00360-7
Zhang, J., Wu, W., Zhao, X., and Zhang, W. (2020). Recommended psychological crisis intervention response to the 2019 novel coronavirus pneumonia outbreak in china: a model of West China hospital. Precis. Clin. Med. 3, 3–8. doi: 10.1093/pcmedi/pbaa006
Zhou, P., Huang, Z., Xiao, Y., Huang, X., and Fan, X. G. (2020). Protecting chinese healthcare workers while combating the 2019 novel coronavirus. Infect. Control Hospital Epidemiol. 41, 745–746. doi: 10.1017/ice.2020.60
Keywords: fear, COVID-19, systematic review, meta-analysis, fear of COVID-19
Citation: Luo F, Ghanei Gheshlagh R, Dalvand S, Saedmoucheshi S and Li Q (2021) Systematic Review and Meta-Analysis of Fear of COVID-19. Front. Psychol. 12:661078. doi: 10.3389/fpsyg.2021.661078
Received: 30 January 2021; Accepted: 24 March 2021;
Published: 11 June 2021.
Edited by:
María Cristina Richaud, Consejo Nacional de Investigaciones Científicas y Técnicas (CONICET), ArgentinaReviewed by:
Stephen Zhang, University of Adelaide, AustraliaCopyright © 2021 Luo, Ghanei Gheshlagh, Dalvand, Saedmoucheshi and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qingyun Li, bGlxaW5neXVuOTQzQGdtYWlsLmNvbQ==
†ORCID: Reza Ghanei Gheshlagh orcid.org/0000-0002-7414-8134
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.