- 1Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy
- 2Department of Neonatal and Pediatric Critical Care, Verona University Hospital, Verona, Italy
- 3Department of Psychology and Neuroscience, University of North Carolina at Chapel Hill, Chapel Hill, NC, United States
- 4Department of Human Sciences, University of Verona, Verona, Italy
The ongoing Coronavirus disease 2019 (COVID-19) pandemic is disrupting most specialized healthcare services worldwide, including those for high-risk newborns and their families. Due to the risk of contagion, critically ill infants, relatives and professionals attending neonatal intensive care units (NICUs) are undergoing a profound remodeling of the organization and quality of care. In particular, mitigation strategies adopted to combat the COVID-19 pandemic may hinder the implementation of family-centered care within the NICU. This may put newborns at risk for several adverse effects, e.g., less weight gain, more nosocomial infections, increased length of NICU stay as well as long-term worse cognitive, emotional, and social development. This article aims to contribute to deepening the knowledge on the psychological impact of COVID-19 on parents and NICU staff members based on empirical data from the literature. We also provided evidence-based indications on how to safely empower families and support NICU staff facing such a threatening emergency, while preserving the crucial role of family-centered developmental care practices.
Introduction
The ongoing pandemic of Coronavirus disease 2019 (COVID-19) has infected, at the time of writing this article, tens of millions of people and contributed to over one and a half million deaths globally (see https://covid19.who.int/). Many governments have imposed regional or national mobility restriction measures in an effort to inhibit its spread. During this global health emergency, special attention has been given to the potential impact of both the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and the measures taken to prevent the virus from spreading to vulnerable populations such as people with serious mental illness (Druss, 2020; Stefana et al., 2020b) and frontline health workers (Chen Q. et al., 2020; Wang J. et al., 2020). However, another vulnerable population, those who are treated, visit or work in the orbit of neonatal intensive care units (NICUs), is receiving less attention than it deserves. Infants who require NICU admission are exposed to a range of intrinsic and environmental factors that can lead, as in the case of pre-term birth, to an increased risk of neurodevelopmental disorders, psychiatric disorders, and chronic disorders involving various organ systems, which can persist from childhood into adulthood or sometimes first manifest in adolescence or adulthood (Saigal and Doyle, 2008; Crump, 2020). However, NICU infants are not the only susceptible population. Indeed, NICU staff members and parents also are vulnerable from a psychological perspective. The NICU staff members frequently encounter work-related stressors that make them prone to burnout and mental health problems (Tawfik et al., 2017; Favrod et al., 2018), whereas parents who have a child being treated in the NICU (i.e., having a critically ill infant and being physically separated from her/him) often perceive this experience as psychologically traumatic (Ionio et al., 2016; Janvier et al., 2016; Sabnis et al., 2019). These issues are likely to be exacerbated by the added burden of the ongoing COVID-19 pandemic, which also hinders the implementation of family-centered care in the NICU, with several negative consequences for the infants. This article aims to provide medical, psychological, and allied health communities with empirical data from the literature on the impact of the COVID-19 pandemic on NICUs' and families. We have also developed evidence-based recommendations for caring family, infant, and NICU staff amid such a challenging pandemic.
COVID-19 in Fetuses and Newborns
To date, no empirical study has clearly demonstrated the occurrence of intrauterine infection by vertical transmission of SARS-CoV-2 from pregnant women to their fetuses (Karimi-Zarchi et al., 2020; Kimberlin and Stagno, 2020; Schwartz, 2020). However, emerging evidence based on the presence of SARS-CoV-2 specific IgM antibodies in neonates suggests that vertical or peripartum transmission from a woman to her fetus is probable (Shek et al., 2003; Dong L. et al., 2020; Rodrigues et al., 2020; Zeng H. et al., 2020). These results are based on small numbers of cases, thus the proportion of pregnancies affected (which seems to be low; Parazzini et al., 2020) is yet to be determined, and the short- and long-term consequences for babies born to mothers with COVID-19 are still unclear. With regard to COVID-19 post-natal infection in newborns, some studies report cases of neonatal early-onset infection confirmed by nasopharyngeal and anal swabs positive for SARS-CoV-2 assay 36-to-48 h after birth (Wang S. et al., 2020; Zeng L. et al., 2020). Although the majority of infected infants aged <1 year at diagnosis are asymptomatic or have mild-to-moderate symptoms, the prevalence of severe-to-critical symptoms requiring NICU admission is about 10% (Dong Y. et al., 2020). Furthermore, although having COVID-19 during pregnancy may cause some pre-natal problems (Zhu et al., 2020), including pre-term delivery in about one out of four infected pregnant women (Rodrigues et al., 2020), it did not considerably increase the immediate adverse outcome of neonates (Dubey et al., 2020; Parazzini et al., 2020; Rawat et al., 2020; Yee et al., 2020).
The Psychological Impact of COVID-19
Infections, deaths, and uncertainty about the future as well as the economic and social consequences of essential public health measures used to contain the spread of the virus (i.e., shelter-at-home, quarantine, isolation and lockdown) are playing key roles in the short- and long-term social and psychological impacts of the COVID-19 pandemic (Osofsky et al., 2020; Provenzi and Tronick, 2020). Sheltering in place entails the loss of daily routines and a reduction in social activities and in-person interactions (which, among other things, provide emotional support). In other words, the current pandemic is reducing the quality of individual, family, and social life intrapersonally and interpersonally. Epidemiological studies of the COVID-19 impacts have shown a high burden of psychological distress (anxiety, depression, and stress) among uninfected individuals, particularly among females (Gao et al., 2020; Wang C. et al., 2020). Furthermore, growing evidence indicates that longer duration of externally-imposed social isolation and an inadequate home environment (characterized by small size, low levels of natural luminosity, or limited possibility of privacy) can lead to a wide range of adverse psychological effects, including alienation, diminished self-esteem, helplessness, insomnia, and panic (Brooks et al., 2020; Pancani et al., 2020; Sim et al., 2020), in addition to the aforementioned distress. Moreover, anxiety, anger, and post-traumatic stress disorder can endure for months to years after the end of such mobility restrictions (Brooks et al., 2020).
Psychological Impact on Parents (and Their Infants)
Though COVID-19 seems to be a less severe illness during pregnancy than previous coronavirus diseases, i.e., Severe Acute Respiratory Syndrome-related coronavirus (SARS) and Middle East Respiratory Syndrome-related coronavirus (MERS), it remains a serious disease as a small number of new mothers may require critical care. There have been few reported cases of both mother and infant deaths in association with COVID-19 (Abou Ghayda et al., 2020; Thornton, 2020), and the factors determining the neonatal mortality seem to be a consequence of pre-term birth rather than of infection with SARS-CoV-2 (Hessami et al., 2020). Pregnant women fear that they may be infected and transmit the harmful infection to their baby, damaging or causing him/her physical pain, whereas fathers are primarily (but probably not exclusively; Stefana and Lavelli, 2018) worried about the risks for both their partners and their babies.
Given the current coronavirus-related restrictions, fathers often are kept out of the delivery room and/or the obstetrics and gynecology ward during delivery in an effort to protect patients and staff from infection (Carroll et al., 2020; Gressier et al., 2020). Mothers with suspected, probable, or confirmed COVID-19 who must take care of their infants by themselves (due to their partners being kept from the ward) must apply standard precautions (e.g., hand hygiene before and after contact with the baby, use a medical mask when near the baby, and routine disinfection of surfaces and objects used) to preserve physical health. Such precautions could be psychologically demanding and complicate the mother's relationship with her baby. The first contacts between mother and newborn are crucial to start the bonding process (Johnson, 2013; Widström et al., 2019). Immediate skin-to-skin contact and breastfeeding within 2 h following delivery make new mothers more sensitive to the infant's needs, and the infant's innate interest toward social stimuli meets a constellation of species-specific caregiving bonding-related behaviors such as looking, vocalizing, positive facial affect and affectionate touch that appear soon after birth (Feldman and Eidelman, 2007; O'Higgins et al., 2013). In contrast, post-natal separation disrupts the establishment of the early parent-infant physiological/emotional connection (Flacking et al., 2012; Welch and Ludwig, 2017) and leads to inadequate mother-infant relationships that can result in long-term negative consequences for the child's cognitive, socio-emotional, and physical development, as well as interpersonal relationships (Johnson, 2013). Adhering to the coronavirus-related restrictions, despite the World Health Organization recommendation that “mothers with suspected or confirmed COVID-19 should not be separated from their infants” (WHO, 2020), means that mothers who are suspected or confirmed to have an infection but are generally in good health are not allowed to care for and feed for their babies according to standard guidelines in some countries and hospitals (WHO, 2002), even when applying necessary precautions for infection prevention and control (Davanzo et al., 2020; Stuebe, 2020). Furthermore, in some countries, these mothers are not allowed skin-to-skin contact in the delivery room or in the ward (this is a pivotal aspect because the early experience of skin-to-skin contact can lead to decreased nosocomial infections and pain perception and to improved breastfeeding, sleeping patterns and neurodevelopmental outcomes; Holditch-Davis et al., 2014; Lumbanraja, 2016; Johnston et al., 2017; Casper et al., 2018; Karimi et al., 2019). These restrictions adversely impact mothers' mood, self-esteem, self-confidence, and confidence in their abilities to care for their infant (Morelius et al., 2005; Bigelow et al., 2014; Krol and Grossmann, 2018; Pineda et al., 2018).
This situation is even more complex and critical in the case of high-risk infants. Even in a non-pandemic period, having a child admitted to a NICU is a traumatic and stressful experience for most parents (Stefana and Lavelli, 2016; Sabnis et al., 2019), mainly because of the unfamiliarity and intimidating intensive care unit environment, the limited ability to provide care for their child, and the uncertainties and worries about their child's outcomes (Obeidat et al., 2009; Stefana et al., 2018). Parents of infants hospitalized in a NICU are at high risk for developing anxiety and depressive symptoms or disorders (Mendelson et al., 2017). They need and desire comprehensive, timely, and clear information about their baby as well as emotional support (Franck and Spencer, 2003). Furthermore, these parents are likely to develop high levels of stress and feelings of guilt and shame, e.g., for not being able to provide care for their hospitalized child in the way they want to or from the sense that they are responsible for their infant's pre-term birth (Flacking et al., 2007; Roque et al., 2017; Stefana et al., under review). During the ongoing pandemic, infants are admitted in an isolated room of the NICU, and mothers with suspected or confirmed COVID-19 sometimes may be totally separated from their child for days or even weeks. In cases where the other parent is also infected, they cannot visit the infant until the test results return negative. Furthermore, in an effort to reduce the risk of SARS-CoV-2 transmission, many NICUs have reduced parental (especially paternal) and family visitation privileges (Cavicchiolo et al., 2020a; Murray and Swanson, 2020) regardless of the other parent's chance of being infected. Despite parents' understanding of the need for visitation restrictions, they are seriously concerned about their ability to visit, care for, and bond with their hospitalized infants (Muniraman et al., 2020).
Forcing a parent to be separated from their newborn child is a devastating experience that adds much to the distress of NICU admission (Bembich et al., 2020), and could negatively impact child development and family well-being in the long term (Erdei and Liu, 2020). Adverse consequences include reduced opportunities for breastfeeding and skin-to-skin touch and holding (Furlow, 2020), delayed and reduced parent–infant interactions (which play a crucial role in early regulation of the stress response and provide the foundations for the development of mutual regulation; Stefana and Lavelli, 2017; Stefana et al., 2020a; Lavelli et al., under review), reduced maternal bonding and infant attachment, parental emotional issues (Franck and Spencer, 2003; Latva et al., 2004; Mäkelä et al., 2018), later parental mental well-being (Lean et al., 2018), and worse infant/child developmental outcomes (Turpin et al., 2019; Cheong et al., 2020). For these reasons, the United States Centers for Disease Control and Prevention (2020) suggest that “the risks and benefits of temporary separation should be discussed by the healthcare team.”
Likely, the adverse effects experienced by parents following their infant's admission to the NICU are more severe and long-lasting during the COVID-19 crisis because many traumatic experiences could have a cumulative effect (Khan, 1963; Sacchi et al., 2020). A recent systematic review and meta-analysis, aimed to estimate the effect of the COVID-19 pandemic on both pregnant and post-partum women's mental health, found that pregnant women and new mothers of full-term and healthy infants report substantially higher levels of anxiety and depression symptoms compared to similar pre-pandemic cohorts (Yan et al., 2020). More specifically, the authors found that the prevalence rates of anxiety and depression among pregnant women during the pandemic were, respectively 37 and 31%, whereas the prevalence of post-partum depression was 22% (the pooled prevalence rate of post-partum anxiety was not evaluated due to the limited data available). Before the COVID-19 pandemic, the estimated prevalence of anxiety symptoms among pregnant women was between 18 and 25% (Dennis et al., 2017; Cena et al., 2020a), while the pooled prevalence of depression among new mothers was between 18 and 20% (Woody et al., 2017; Cena et al., 2021). Furthermore, the levels of anxiety and depression of parents of children who are not infected but are hospitalized during the COVID-19 pandemic are more serious than that of parents of children hospitalized during non-pandemic periods (Yuan et al., 2020). Under such distress, previous evidence suggests that some of these parents may also develop post-traumatic stress disorder (Ursano et al., 2009; Cukor et al., 2011). Finally, reduced maternal and paternal mental health may also lead to additional risk factors for child neurodevelopmental disorders (Giallo et al., 2014; Cena et al., 2020b). For example, two recent systematic reviews found that maternal pre-natal stress is associated with an increased risk of poor socio-emotional development (e.g., difficult temperament, behavioral dysregulation; Madigan et al., 2018) as well as of autism spectrum disorder and attention-deficit hyperactivity disorder in the offspring (Manzari et al., 2019). Furthermore, a longitudinal study involving 3,741 father-child dyads found that fathers' high post-natal distress and low parenting self-efficacy were associated with lower parenting consistency and higher levels of hostile parenting when offspring were aged 4–5 years, and poorer child emotional-behavioral outcomes at 8–9 years (Rominov et al., 2016).
Psychological Impact on NICU Staff Members
NICU staff members are the key players in the provision of infant health care and family-centered care. Efforts to maintain high-quality care can be emotionally demanding, due to factors such as frequent changes in technology and guidelines as well as recurrent occupational exposure to the pain and distress of high-risk neonates and their families; this can negatively impact both personal and professional well-being and performance (Van Mol et al., 2015; Weintraub et al., 2016; Tawfik et al., 2017). Thus it is not surprising that even in normal conditions, burnout (defined as a state of fatigue, detachment, and cynicism) affects 25–50% of NICU professionals (Profit et al., 2014; Tawfik et al., 2017; Barr, 2020).
The ongoing global health emergency is a stressful situation for NICU staff both personally as people and professionally as clinicians. Pandemic-related factors such as (i) over-work or work with long shifts, (ii) wearing additional personal protective equipment, which has been described as necessary but time-consuming and disruptive to clear communication with parents (Semaan et al., 2020; Cena et al., under review), (iii) being unable to act according to their own values, the values of the patient's family, or the values of the family-centered care model (i.e., because of pandemic-related policies enforcing social distancing and other measures that are not typical in NICU patient care), (iv) difficulties in meeting the emotional needs of hospitalized infants and their families while also safeguarding their own health, (v) anxiety and fear about their personal physical safety (Chang et al., 2020) as well as that of friends and family members (whom they could infect while asymptomatic), (vi) emotional pain for the loss of infected friends/relatives/colleagues, and (vii) restrictions on personal and social activities are contributing to increased psychological stress in these people. It follows that these professionals are at higher than average risk for burnout (Profit et al., 2014; Crowe et al., 2020), a condition that poses additional challenges for family-centered care. Thus, NICU staff members are in a continuously stressful situation both in the workplace and in their personal lives.
Supporting Persons and Strengthening NICUs
Next we offer suggestions on how to support and empower both NICU parents and staff, and strengthen NICU systems, while emphasizing the role of Family-Centered Care in the NICU during the COVID-19.
Family-Centered Care
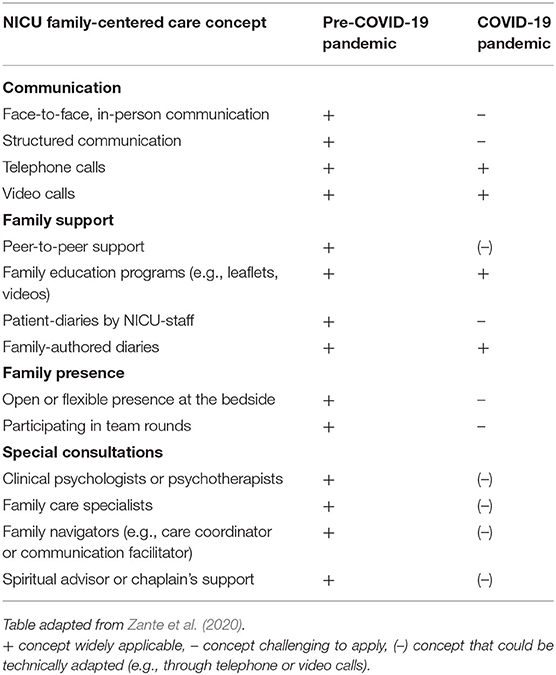
Family-centered care in the NICU requires as primary components the family's presence in the ward, family support, communication with family members, use of specific consultations and NICU team members, and operational and environmental issues (Davidson et al., 2017). Despite the fact that family-centered care is challenged by the current COVID-19 pandemic, leading to visitation restrictions and indications for physical distancing, its goals must remain the same, though adapted to and focused on maintaining family integrity and respecting the role of family members as care partners with whom to collaborate (Papadimos et al., 2018; Hart et al., 2020). Given that several important practices in typical family-centered care may not be feasible in times of pandemic, family-centered care in the NICU must undergo specific adaptations in order to be accomplished in the midst of the COVID-19 pandemic (see Table 1).
Supporting Parents
When parents' visitation is limited or denied, communication between them and the NICU team should include a video component. Real-time videoconferencing is a means for parents to communicate (and collaborate) with NICU staff and to see their infant (Lindberg et al., 2009; Gund et al., 2013; Epstein et al., 2015; Joshi et al., 2016). It is essential in the current health emergency that parents can see their baby via video when they cannot be or stay with them in the NICU (Epstein et al., 2017), as viewing their newborn on a camera reduces parental stress and anxiety (Rhoads et al., 2015a,b).
A further consequence of visitation restrictions and rules for social distancing is the loss of in-person, peer-to-peer support for NICU parents (Hall et al., 2015). Support groups have a beneficial, normalizing effect on the parental role, emotions, control, trust, coping, and adaptation to parenthood reality (Dahan et al., 2020). More generally, offering peer support is recommended as an integral and crucial component of family-centered care and comprehensive family support (Hall et al., 2015, 2016). Although meeting in-person appears to be preferable, both individual and group peer support interventions offered by telephone or via the internet appear to be beneficial (Hall et al., 2015) when the communications are managed by the same staff who would normally deliver that information personally inside the NICU (i.e., when not managed by a “stranger”). Thus, the best solution in the time of COVID-19 seems to be providing peer support by video and voice calls. NICUs should develop or implement internet-based peer support programs, and offer a comprehensive training program to both veteran parents (i.e., parents who have had previous experience with their own infant in a NICU, have participated in the family-integrated care program, and now provide peer-to-peer support) and NICU staff members who facilitate the support.
In order to ensure that support by mental health professionals continues to function, perinatal psychiatric and psychological services should be implemented through telepsychiatry (see www.psychiatry.org/psychiatrists/practice/telepsychiatry) and telepsychology (see www.apa.org/practice/guidelines/telepsychology and https://w.wiki/NYz) (Hermann et al., 2020; Perrin et al., 2020; Zork et al., 2020). This might include the development of telephone helplines manned by mental health specialists, specifically addressing the needs of parents with hospitalized infants.
Finally, it is crucial that when parents are allowed to visit in the NICU, the healthcare team put in place all the interdisciplinary recommendations for educational and emotional support (Hynan et al., 2015) and for encouraging and involving them in the care of their baby (Craig et al., 2015). Regarding emotional support, the implementation of evidence-based assessment (EBA) and treatment appear to be essential to reduce parents' burden at individual and public health levels. An EBA model that could be usefully adopted by NICU mental health professionals is that devised by Youngstrom and colleagues (Youngstrom, 2013, 2014; Youngstrom et al., 2015, 2017, 2018; Youngstrom and Van Meter, 2016, 2018; Youngstrom and Prinstein, 2020). This EBA 2.0 model (see Table 2) combines empirical research and pragmatism of application to identify the most appropriate measurements and sequence their order to minimize redundancy and unnecessary testing. Such an effective and efficient assessment process is crucial because it leads to more accurate diagnosis, appropriate intervention, better treatment matching, and enhanced outcomes.
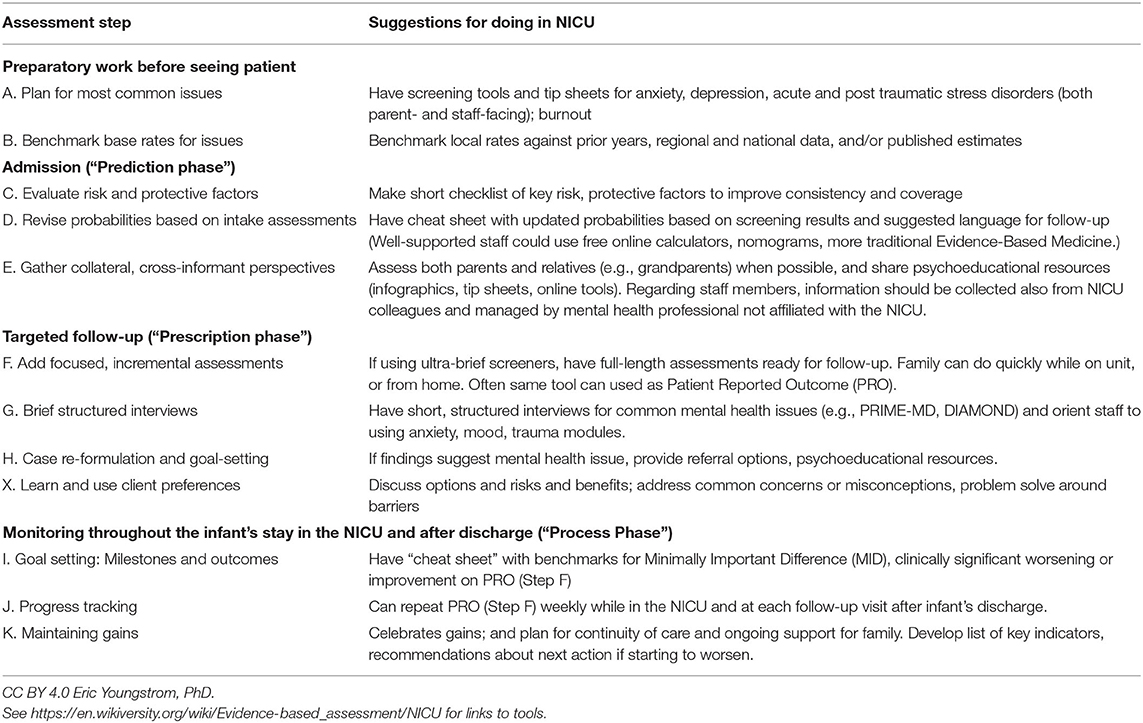
Table 2. Strategies for adding Evidence-Based Assessment techniques for mental health issues to the NICU (adapted from Youngstrom et al., 2017).
Supporting and Empowering NICU Staffs
From the above, it follows that it is vital to adequately support NICU staff members in maintaining their security and safety (e.g., personal protective equipment to protect themselves) and, more generally, that hospital institutions make them feel cared for. At the same time, being on the front line to cure and care for the most vulnerable (especially newborns and their families) and being a member of a highly specialized team who bravely faces this threat while continuing to do their jobs are elements that can encourage and even make healthcare providers fittingly proud of themselves and their efforts (Barello et al., 2020a,b). In addition to the above responsibilities, usually NICU staff are also the primary point of contact with the general health system for the parents of hospitalized infants, and as such could (and should) also be the first observer/responder for both SARS-CoV-2 and mental health conditions for many of these parents. Thus, NICU staff need specific training to recognize the signs and symptoms of both COVID-19 and the most common post-partum mental disorders (i.e., anxiety, depression, and psychological distress). Additionally, in this scenario, NICU staff would ideally have (i) accurate and clear guidelines, (ii) access to online screening tools to explore their own mental health status and determine whether they should contact a mental health professional (e.g., www.hgaps.org/assessment-center.html and www.dbsalliance.org/education/mental-health-screening-center/), (iii) the provision of a dedicated psychological help service for healthcare professionals located in the hospital or through a telephone helpline staffed by mental health professionals not affiliated with the NICU, (iv) training on COVID-19 management, (v) training on the use of mobile and web technologies needed to provide support at a distance to parents, (vi) training and access to brief anxiety and depression scales to use for monitoring families' distress (e.g., www.hgaps.org/assessment-center.html and www.dbsalliance.org/education/mental-health-screening-center/), and (vii) a forum for discussion, advice and support from colleagues. These support and training measures are essential and must be developed and implemented, particularly if the pandemic and its aftermath will continue for a long time. If professionals do not have accessible resources and support to take care of their physical and mental health, they will not be able to deliver the appropriate care and critical services to the most vulnerable populations, including infants and NICU families, during this pandemic.
Strengthening NICU Systems
The COVID-19 global health crisis is a disaster; however, it can also be an opportunity (Stefana et al., 2020c; Youngstrom et al., 2020) to improve health care systems and services by including an increased number of NICU staff members, adequate resources and training, and improved visitation policies for family members of hospitalized infants. Before the COVID-19 pandemic, there was a widespread and substantial shortage of NICU medical and nursing staff (Rogowski et al., 2013; Gagliardi et al., 2016; Bliss, 2017) the current crisis has highlighted. Indeed, three of ten NICUs were already understaffed compared to national guidelines (Rogowski et al., 2013). This is particularly important in pandemic times because understaffing is associated with children's adverse outcomes, including a heightened risk of nosocomial infection on very-low-birth-weight infants (Rogowski et al., 2013). Despite understaffing being a significant risk factor for poor patient outcomes, it is infrequently addressed by interventions (Stapleton et al., 2016).
In many cases, the needed restrictions and containment measures (Cavicchiolo et al., 2020a,b; De Rose et al., 2020) that are in place to deal with the COVID-19 emergency are exacerbating the problems associated with meager adoption of family-centered care principles in NICUs. During these months, it has been common to hear colleagues say that “COVID has made us go back decades in the quality of family support we provide.” This is a serious negative development because care should be all the more humane and person-centered during the COVID-19 pandemic; a goal that becomes fully achievable only through a strengthened involvement of patients' families (Coulter and Richards, 2020) and the support and empowerment of frontline healthcare workers. The development of online support groups, video and messaging platforms to increase communication between families and providers, as well as peer support, all are innovations that should continue even after the pandemic ends. As such, the present healthcare crisis can increase the awareness of healthcare specialists about the critical need to enable open access of families to the intensive care unit environment, and an active engagement of parents in the primary care of hospitalized newborns and infants at risk. The tools and techniques developed in response to the disruption of the system can ratchet practice forward.
Conclusions
The COVID-19 pandemic has dramatically changed the lifestyle of people worldwide, while disrupting healthcare services and systems, including NICUs. The mitigation strategies adopted to manage the pandemic have upset care delivery for high-risk newborns and their families, and the mental health legacy of the pandemic will likely endure – for both NICU staff and family members – long after the acute phase (Erdei and Liu, 2020; Lemmon et al., 2020). It is vital to deepen the understanding of how the pandemic has influenced family-centered care practices and dynamics in NICUs, gauging the psychological impact of COVID-19 on parents and frontline professionals. This article provides evidence-based strategies to aid NICU staff members engaged in ensuring high-quality care and supporting critically ill newborns and their families (Tscherning et al., 2020). We proposed several ways to safely support and empower NICU staff and enhance family-centered developmental care practices, without increasing the risk of contagion. Apart from evidence-based training on cutting-edge COVID-19 management tools, high priority should be given to the preservation of family-centered care principles, including parents' presence in the NICU, parent-infant physical and emotional closeness, and parental involvement in the infant's care. Furthermore, NICU systems should implement evidence-based assessment and treatment for parental distress while providing peer support for parents by video and voice calls. Finally, NICU systems should ensure dedicated psychological help services for healthcare professionals, being particularly exposed to a higher risk of burnout COVID-19 related.
Author Contributions
AS designed the study. AS, EAY, PB, JJ, ML, JL, AT, and LC contributed to the manuscript writing. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abou Ghayda, R., Li, H., Lee, K. H., Lee, H. W., Hong, S. H., Kwak, M., et al. (2020). COVID-19 and adverse pregnancy outcome: a systematic review of 104 cases. J. Clin. Med. 9:3441. doi: 10.3390/jcm9113441
Barello, S., Palamenghi, L., and Graffigna, G. (2020a). Burnout and somatic symptoms among frontline healthcare professionals at the peak of the Italian COVID-19 pandemic. Psychiatry Res. 290:113129. doi: 10.1016/j.psychres.2020.113129
Barello, S., Palamenghi, L., and Graffigna, G. (2020b). Empathic communication as a “risky strength” for health during the COVID-19 pandemic: the case of frontline italian healthcare workers. Patient Educ. Couns. 103, 2200–2202. doi: 10.1016/j.pec.2020.06.027
Barr, P. (2020). Burnout in neonatal intensive care unit nurses: relationships with moral distress, adult attachment insecurities, and proneness to guilt and shame. J. Perinat. Med. 48, 416–422. doi: 10.1515/jpm-2019-0323
Bembich, S., Tripani, A., Mastromarino, S., Di Risio, G., Castelpietra, E., and Risso, F. M. (2020). Parents experiencing NICU visit restrictions due to COVID-19 pandemic. Acta Paediatr. 1–2. doi: 10.1111/apa.15620
Bigelow, A. E., Power, M., Gillis, D. E., Maclellan-Peters, J., Alex, M., and McDonald, C. (2014). Breastfeeding, skin-to-skin contact, and mother–infant interactions over infants' first three months. Infant Mental Health J. 35, 51–62. doi: 10.1002/imhj.21424
Bliss (2017). Bliss Scotland Baby Report 2017: An Opportunity to Deliver Improvements in Neonatal Care.
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Carroll, W. D., Strenger, V., Eber, E., Porcaro, F., Cutrera, R., Fitzgerald, D. A., et al. (2020). European and United Kingdom COVID-19 pandemic experience: the same but different. Paediatr. Respir. Rev. 35, 50–56. doi: 10.1016/j.prrv.2020.06.012
Casper, C., Sarapuk, I., and Pavlyshyn, H. (2018). Regular and prolonged skin-to-skin contact improves short-term outcomes for very preterm infants: a dose-dependent intervention. Arch. Pediatr. 25, 469–475. doi: 10.1016/j.arcped.2018.09.008
Cavicchiolo, M. E., Lolli, E., Trevisanuto, D., and Baraldi, E. (2020a). Managing a tertiary-level NICU in the time of COVID-19: lessons learned from a high-risk zone. Pediatr. Pulmonol. 55, 1308–1310. doi: 10.1002/ppul.24788
Cavicchiolo, M. E., Trevisanuto, D., Lolli, E., Mardegan, V., Saieva, A. M., Franchin, E., et al. (2020b). Universal screening of high-risk neonates, parents, and staff at a neonatal intensive care unit during the SARS-CoV-2 pandemic. Eur. J. Pediatr. 179, 1949–1955. doi: 10.1007/s00431-020-03765-7
Cena, L., Mirabella, F., Palumbo, G., Gigantesco, A., Trainini, A., and Stefana, A. (2020a). Prevalence of maternal antenatal anxiety and its association with demographic and socioeconomic factors: a multicentre study in Italy. Eur. Psychiatry 63:E84. doi: 10.1192/j.eurpsy.2020.82
Cena, L., Mirabella, F., Palumbo, G., Gigantesco, A., Trainini, A., and Stefana, A. (2021). Prevalence of maternal antenatal and postnatal depression and their association with sociodemographic and socioeconomic factors: a multicentre study in Italy. J. Affect. Disord. 279, 217–221. doi: 10.1016/j.jad.2020.09.136
Cena, L., Palumbo, G., Mirabella, F., Gigantesco, A., Stefana, A., Trainini, A., et al. (2020b). Perspectives on early screening and prompt intervention to identify and treat maternal perinatal mental health. Protocol for a prospective multicentre study in Italy. Frontiers in Psychology, 11: 365. doi: 10.3389/fpsyg.2020.00365
Centers for Disease Control and Prevention (2020). Interim Considerations for Infection Prevention and Control of Coronavirus Disease 2019 (COVID-19) in Inpatient Obstetric Healthcare Settings. Centers for Disease Control and Prevention.
Chang, D., Xu, H., Rebaza, A., Sharma, L., and Cruz, C. S. D. (2020). Protecting health-care workers from subclinical coronavirus infection. Lancet Respir. Med. 8:e13. doi: 10.1016/S2213-2600(20)30066-7
Chen, Q., Liang, M., Li, Y., Guo, J., Fei, D., Wang, L., et al. (2020). Mental health care for medical staff in China during the COVID-19 outbreak. Lancet Psychiatry 7, e15–e16. doi: 10.1016/S2215-0366(20)30078-X
Cheong, J. L., Burnett, A. C., Treyvaud, K., and Spittle, A. J. (2020). Early environment and long-term outcomes of preterm infants. J. Neural Transm. 127, 1–8. doi: 10.1007/s00702-019-02121-w
Coulter, A., and Richards, T. (2020). Care during covid-19 must be humane and person centred. BMJ 370:m3483. doi: 10.1136/bmj.m3483
Craig, J. W., Glick, C., Phillips, R., Hall, S. L., Smith, J., and Browne, J. (2015). Recommendations for involving the family in developmental care of the NICU baby. J. Perinatol. 35, S5–S8. doi: 10.1038/jp.2015.142
Crowe, R. P., Fernandez, A. R., Pepe, P. E., Cash, R. E., Rivard, M. K., Wronski, R., et al. (2020). The association of job demands and resources with burnout among emergency medical services professionals. J. Am. College Emerg. Phys. Open 1, 6–16. doi: 10.1002/emp2.12014
Crump, C. (2020). An overview of adult health outcomes after preterm birth. Early Hum. Dev. 150:105187. doi: 10.1016/j.earlhumdev.2020.105187
Cukor, J., Wyka, K., Jayasinghe, N., Weathers, F., Giosan, C., Leck, P., et al. (2011). Prevalence and predictors of posttraumatic stress symptoms in utility workers deployed to the World Trade Center following the attacks of September 11, 2001. Depress. Anxiety 28, 210–217. doi: 10.1002/da.20776
Dahan, S., Bourque, C. J., Reichherzer, M., Prince, J., Mantha, G., Savaria, M., et al. (2020). Peer-support groups for families in neonatology: why and how to get started? Acta Paediatr. 109, 2525–2531. doi: 10.1111/apa.15312
Davanzo, R., Moro, G., Sandri, F., Agosti, M., Moretti, C., and Mosca, F. (2020). Breastfeeding and coronavirus disease-2019. Ad interim indications of the Italian society of neonatology endorsed by the Union of European neonatal and perinatal societies. Matern. Child Nutr. 16:e13010. doi: 10.1111/mcn.13010
Davidson, J. E., Aslakson, R. A., Long, A. C., Puntillo, K. A., Kross, E. K., Hart, J., et al. (2017). Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit. Care Med. 45, 103–128. doi: 10.1097/CCM.0000000000002169
De Rose, D. U., Auriti, C., Landolfo, F., Capolupo, I., Salvatori, G., Ranno, S., et al. (2020). Reshaping neonatal intensive care units (NICUs) to avoid the spread of severe acute respiratory coronavirus virus 2 (SARS-CoV-2) to high-risk infants. Infect. Control Hospital Epidemiol. 1–2. doi: 10.1017/ice.2020.310
Dennis, C. L., Falah-Hassani, K., and Shiri, R. (2017). Prevalence of antenatal and postnatal anxiety: systematic review and meta-analysis. Br. J. Psychiatry 210, 315–323. doi: 10.1192/bjp.bp.116.187179
Dong, L., Tian, J., He, S., Zhu, C., Wang, J., Liu, C., et al. (2020). Possible vertical transmission of SARS-CoV-2 from an infected mother to her newborn. JAMA 323, 1846–1848. doi: 10.1001/jama.2020.4621
Dong, Y., Mo, X., Hu, Y., Qi, X., Jiang, F., Jiang, Z., et al. (2020). Epidemiological characteristics of 2143 pediatric patients with 2019 coronavirus disease in China. Pediatrics 16:16. doi: 10.1542/peds.2020-0702
Druss, B. G. (2020). Addressing the COVID-19 pandemic in populations with serious mental illness. JAMA Psychiatry 77, 891–892. doi: 10.1001/jamapsychiatry.2020.0894
Dubey, P., Reddy, S., Manuel, S., and Dwivedi, A. K. (2020). Maternal and neonatal characteristics and outcomes among COVID-19 infected women: an updated systematic review and meta-analysis. Eur. J. Obstetr. Gynecol. Reprod. Biol. 252, 490–501. doi: 10.1016/j.ejogrb.2020.07.034
Epstein, E. G., Arechiga, J., Dancy, M., Simon, J., Wilson, D., and Alhusen, J. L. (2017). Integrative review of technology to support communication with parents of infants in the NICU. J. Obstetr. Gynecol. Neonatal Nurs. 46, 357–366. doi: 10.1016/j.jogn.2016.11.019
Epstein, E. G., Sherman, J., Blackman, A., and Sinkin, R. A. (2015). Testing the feasibility of Skype and FaceTime updates with parents in the neonatal intensive care unit. Am. J. Crit. Care 24, 290–296. doi: 10.4037/ajcc2015828
Erdei, C., and Liu, C. H. (2020). The downstream effects of COVID-19: a call for supporting family wellbeing in the NICU. J. Perinatol. 40, 1283–1285. doi: 10.1038/s41372-020-0745-7
Favrod, C., Jan du Chêne, L., Martin Soelch, C., Garthus-Niegel, S., Tolsa, J. F., Legault, F., et al. (2018). Mental health symptoms and work-related stressors in hospital midwives and NICU nurses: a mixed methods study. Front. Psychiatry 9:364. doi: 10.3389/fpsyt.2018.00364
Feldman, R., and Eidelman, A. I. (2007). Maternal postpartum behavior and the emergence of infant-mother and infant-father synchrony in preterm and full-term infants: the role of neonatal vagal tone. Dev. Psychobiol. 49, 290–302. doi: 10.1002/dev.20220
Flacking, R., Ewald, U., and Starrin, B. (2007). “I wanted to do a good job”: experiences of “becoming a mother” and breastfeeding in mothers of very preterm infants after discharge from a neonatal unit. Soc. Sci. Med. 64, 2405–2416. doi: 10.1016/j.socscimed.2007.03.008
Flacking, R., Lehtonen, L., Thomson, G., Axelin, A., Ahlqvist, S., Moran, V. H., et al. (2012). Closeness and separation in neonatal intensive care. Acta Paediatr. 101, 1032–1037. doi: 10.1111/j.1651-2227.2012.02787.x
Franck, L. S., and Spencer, C. (2003). Parent visiting and participation in infant caregiving activities in a neonatal unit. Birth 30, 31–35. doi: 10.1046/j.1523-536X.2003.00214.x
Furlow, B. (2020). US NICUs and donor milk banks brace for COVID-19. Lancet Child Adolesc. Health 4:355. doi: 10.1016/S2352-4642(20)30103-6
Gagliardi, L., Corchia, C., Bellù, R., Coscia, A., Zangrandi, A., Zanini, R., et al. (2016). What we talk about when we talk about NICUs: infants' acuity and nurse staffing. J. Matern. Fetal Neonatal Med. 29, 2934–2939. doi: 10.3109/14767058.2015.1109618
Gao, J., Zheng, P., Jia, Y., Chen, H., Mao, Y., Chen, S., et al. (2020). Mental health problems and social media exposure during COVID-19 outbreak. PLoS ONE 15:e0231924. doi: 10.1371/journal.pone.0231924
Giallo, R., Cooklin, A., Wade, C., D'Esposito, F., and Nicholson, J. M. (2014). Fathers' postnatal mental health and child well-being at age five: the mediating role of parenting behavior. J. Fam. Issues 35, 1543–1562. doi: 10.1177/0192513X13477411
Gressier, F., Mezzacappa, A., Lasica, P. A., Fourcade, C., and Corruble, E. (2020). COVID outbreak is changing our practices of perinatal psychiatry. Arch. Womens Ment. Health 23, 791–792. doi: 10.1007/s00737-020-01039-7
Gund, A., Sjöqvist, B. A., Wigert, H., Hentz, E., Lindecrantz, K., and Bry, K. (2013). A randomized controlled study about the use of eHealth in the home health care of premature infants. BMC Med. Inform. Decis. Mak. 13:22. doi: 10.1186/1472-6947-13-22
Hall, S. L., Phillips, R., and Hynan, M. T. (2016). Transforming NICU care to provide comprehensive family support. Newborn Infant Nurs. Rev. 16, 69–73. doi: 10.1053/j.nainr.2016.03.008
Hall, S. L., Ryan, D. J., Beatty, J., and Grubbs, L. (2015). Recommendations for peer-to-peer support for NICU parents. J. Perinatol. 35, S9–S13. doi: 10.1038/jp.2015.143
Hart, J. L., Turnbull, A. E., Oppenheim, I. M., and Courtright, K. R. (2020). Family-centered care during the COVID-19 era. J. Pain Symptom Manage 60, 93–97. doi: 10.1016/j.jpainsymman.2020.04.017
Hermann, A., Fitelson, E. M., and Bergink, V. (2020). Meeting maternal mental health needs during the COVID-19 pandemic. JAMA Psychiatry 78, 123–124. doi: 10.1001/jamapsychiatry.2020.1947
Hessami, K., Homayoon, N., Hashemi, A., Vafaei, H., Kasraeian, M., and Asadi, N. (2020). COVID-19 and maternal, fetal and neonatal mortality: a systematic review. J. Matern. Fetal Neonatal Med. 1–6. doi: 10.1080/14767058.2020.1806817
Holditch-Davis, D., White-Traut, R. C., Levy, J. A., O'Shea, T. M., Geraldo, V., and David, R. J. (2014). Maternally administered interventions for preterm infants in the NICU: effects on maternal psychological distress and mother–infant relationship. Infant Behav. Dev. 37, 695–710. doi: 10.1016/j.infbeh.2014.08.005
Hynan, M. T., Steinberg, Z., Baker, L., Cicco, R., Geller, P. A., Lassen, S., et al. (2015). Recommendations for mental health professionals in the NICU. J. Perinatol. 35, S14–S18. doi: 10.1038/jp.2015.144
Ionio, C., Colombo, C., Brazzoduro, V., Mascheroni, E., Confalonieri, E., Castoldi, F., et al. (2016). Mothers and fathers in NICU: the impact of preterm birth on parental distress. Eur. J. Psychol. 12, 604–621. doi: 10.5964/ejop.v12i4.1093
Janvier, A., Lantos, J., Aschner, J., Barrington, K., Batton, B., Batton, D., et al. (2016). Stronger and more vulnerable: a balanced view of the impacts of the NICU experience on parents. Pediatrics 138:e20160655. doi: 10.1542/peds.2016-0655
Johnson, K. (2013). Maternal-infant bonding: a review of literature. Int. J. Childbirth Educ. 28, 17–22.
Johnston, C., Campbell-Yeo, M., Disher, T., Benoit, B., Fernandes, A., Streiner, D., et al. (2017). Skin-to-skin care for procedural pain in neonates. Cochrane Database Syst. Rev. 2:CD008435. doi: 10.1002/14651858.CD008435.pub3
Joshi, A., Chyou, P. H., Tirmizi, Z., and Gross, J. (2016). Web camera use in the neonatal intensive care unit: impact on nursing workflow. Clin. Med. Res. 14, 1–6. doi: 10.3121/cmr.2015.1286
Karimi, F. Z., Sadeghi, R., Maleki-Saghooni, N., and Khadivzadeh, T. (2019). The effect of mother-infant skin to skin contact on success and duration of first breastfeeding: a systematic review and meta-analysis. Taiwan. J. Obstetr. Gynecol. 58, 1–9. doi: 10.1016/j.tjog.2018.11.002
Karimi-Zarchi, M., Neamatzadeh, H., Dastgheib, S. A., Abbasi, H., Mirjalili, S. R., Behforouz, A., et al. (2020). Vertical transmission of coronavirus disease 19 (COVID-19) from infected pregnant mothers to neonates: a review. Fetal Pediatr. Pathol. 1, 1–5. doi: 10.1080/15513815.2020.1747120
Khan, M. M. R. (1963). The concept of cumulative trauma. Psychoanal. Study Child 18, 286–306. doi: 10.1080/00797308.1963.11822932
Kimberlin, D. W., and Stagno, S. (2020). Can SARS-CoV-2 infection be acquired in utero? More definitive evidence is needed. JAMA 323, 1788–1789. doi: 10.1001/jama.2020.4868
Krol, K. M., and Grossmann, T. (2018). Psychological effects of breastfeeding on children and mothers. Bundesgesundheitsblatt-Gesundheitsforschung-Gesundheitsschutz 61, 977–985. doi: 10.1007/s00103-018-2769-0
Latva, R., Lehtonen, L., Salmelin, R. K., and Tamminen, T. (2004). Visiting less than every day: a marker for later behavioral problems in Finnish preterm infants. Arch. Pediatr. Adolesc. Med. 158, 1153–1157. doi: 10.1001/archpedi.158.12.1153
Lean, R. E., Rogers, C. E., Paul, R. A., and Gerstein, E. D. (2018). NICU hospitalization: long-term implications on parenting and child behaviors. Curr. Treatment Options Pediatrics 4, 49–69. doi: 10.1007/s40746-018-0112-5
Lemmon, M. E., Chapman, I., Malcolm, W., Kelley, K., Shaw, R. J., Milazzo, A., et al. (2020). Beyond the first wave: consequences of COVID-19 on high-risk infants and families. Am. J. Perinatol. 37, 1283–1288. doi: 10.1055/s-0040-1715839
Lindberg, B., Axelsson, K., and Ohrling, K. (2009). Taking care of their baby at home but with nursing staff as support: the use of videoconferencing in providing neonatal support to parents of preterm infants. J. Neonatal Nurs. 15, 47–55. doi: 10.1016/j.jnn.2009.01.004
Lumbanraja, S. N. (2016). Influence of maternal factors on the successful outcome of kangaroo mother care in low birth-weight infants: a randomized controlled trial. J. Neonatal Perinatal Med. 9, 385–392. doi: 10.3233/NPM-161628
Madigan, S., Oatley, H., Racine, N., Fearon, R. P., Schumacher, L., Akbari, E., et al. (2018). A meta-analysis of maternal prenatal depression and anxiety on child socioemotional development. J. Am. Acad. Child Adolesc. Psychiatry 57, 645–657. doi: 10.1016/j.jaac.2018.06.012
Mäkelä, H., Axelin, A., Feeley, N., and Niela-Vilén, H. (2018). Clinging to closeness: the parental view on developing a close bond with their infants in a NICU. Midwifery 62, 183–188. doi: 10.1016/j.midw.2018.04.003
Manzari, N., Matvienko-Sikar, K., Baldoni, F., O'Keeffe, G. W., and Khashan, A. S. (2019). Prenatal maternal stress and risk of neurodevelopmental disorders in the offspring: a systematic review and meta-analysis. Soc. Psychiatry Psychiatr. Epidemiol. 54, 1299–1309. doi: 10.1007/s00127-019-01745-3
Mendelson, T., Cluxton-Keller, F., Vullo, G. C., Tandon, S. D., and Noazin, S. (2017). NICU-based interventions to reduce maternal depressive and anxiety symptoms: a meta-analysis. Pediatrics 139:e20161870. doi: 10.1542/peds.2016-1870
Morelius, E., Theodorsson, E., and Nelson, N. (2005). Salivary cortisol and mood and pain profiles during skin-to-skin care for an unselected group of mothers and infants in neonatal intensive care. Pediatrics 116, 1105–1113. doi: 10.1542/peds.2004-2440
Muniraman, H., Ali, M., Cawley, P., Hillyer, J., Heathcote, A., Ponnusamy, V., et al. (2020). Parental perceptions of the impact of neonatal unit visitation policies during COVID-19 pandemic. BMJ Paediatrics Open 4:e000899. doi: 10.1136/bmjpo-2020-000899
Murray, P. D., and Swanson, J. R. (2020). Visitation restrictions: is it right and how do we support families in the NICU during COVID-19? J. Perinatol. 40, 1576–1581. doi: 10.1038/s41372-020-00781-1
Obeidat, H. M., Bond, E. A., and Callister, L. C. (2009). The parental experience of having an infant in the newborn intensive care unit. J. Perinatal Educ. 18, 23–29. doi: 10.1624/105812409X461199
O'Higgins, M., Roberts, I. S., Glover, V., and Taylor, A. (2013). Mother-child bonding at 1 year; associations with symptoms of postnatal depression and bonding in the first few weeks. Arch. Women's Ment. Health 16, 381–389. doi: 10.1007/s00737-013-0354-y
Osofsky, J. D., Osofsky, H. J., and Mamon, L. Y. (2020). Psychological and social impact of COVID-19. Psychol. Trauma 12, 468–469. doi: 10.1037/tra0000656
Pancani, L., Marinucci, M., Aureli, N., and Riva, P. (2020). Forced social isolation and mental health: a study on 1006 Italians under COVID-19 quarantine. PsyArXiv. doi: 10.31234/osf.io/uacfj
Papadimos, T. J., Marcolini, E. G., Hadian, M., Hardart, G. E., Ward, N., Levy, M. M., et al. (2018). Ethics of outbreaks position statement. Part 2: family-centered care. Crit. Care Med. 46, 1856–1860. doi: 10.1097/CCM.0000000000003363
Parazzini, F., Bortolus, R., Mauri, P. A., Favilli, A., Gerli, S., and Ferrazzi, E. (2020). Delivery in pregnant women infected with SARS-CoV-2: a fast review. Int. Gynecol. Obstetr. 150, 41–46. doi: 10.1002/ijgo.13166
Perrin, P. B., Rybarczyk, B. D., Pierce, B. S., Jones, H. A., Shaffer, C., and Islam, L. (2020). Rapid telepsychology deployment during the COVID-19 pandemic: a special issue commentary and lessons from primary care psychology training. J. Clin. Psychol. 76, 1173–1185. doi: 10.1002/jclp.22969
Pineda, R., Bender, J., Hall, B., Shabosky, L., Annecca, A., and Smith, J. (2018). Parent participation in the neonatal intensive care unit: predictors and relationships to neurobehavior and developmental outcomes. Early Hum. Dev. 117, 32–38. doi: 10.1016/j.earlhumdev.2017.12.008
Profit, J., Sharek, P. J., Amspoker, A. B., Kowalkowski, M. A., Nisbet, C. C., Thomas, E. J., et al. (2014). Burnout in the NICU setting and its relation to safety culture. BMJ Qual. Safety 23, 806–813. doi: 10.1136/bmjqs-2014-002831
Provenzi, L., and Tronick, E. (2020). The power of disconnection during the COVID-19 emergency: from isolation to reparation. Psychol. Trauma 12, 252–254. doi: 10.1037/tra0000619
Rawat, M., Chandrasekharan, P., Hicar, M. D., and Lakshminrusimha, S. (2020). COVID-19 in newborns and infants—low risk of severe disease: silver lining or dark cloud? Am. J. Perinatol. 37:845. doi: 10.1055/s-0040-1710512
Rhoads, S. J., Green, A., Gauss, C. H., Mitchell, A., Pate, B., and Dowling, D. (2015a). Web camera use of mothers and fathers when viewing their hospitalized neonate. Adv. Neonatal Care 15, 440–446. doi: 10.1097/ANC.0000000000000235
Rhoads, S. J., Green, A., Mitchell, A., and Lynch, C. E. (2015b). Neuroprotective core measure 2: partnering with families-exploratory study on web-camera viewing of hospitalized infants and the effect on parental stress, anxiety, and bonding. Newborn Infant Nurs. Rev. 15, 104–110. doi: 10.1053/j.nainr.2015.06.011
Rodrigues, C., Baia, I., Domingues, R., and Barros, H. (2020). Pregnancy and breastfeeding during COVID-19 pandemic: a systematic review of published pregnancy cases. Front. Public Health 8:558144. doi: 10.3389/fpubh.2020.558144
Rogowski, J. A., Staiger, D., Patrick, T., Horbar, J., Kenny, M., and Lake, E. T. (2013). Nurse staffing and NICU infection rates. JAMA Pediatr. 167, 444–450. doi: 10.1001/jamapediatrics.2013.18
Rominov, H., Giallo, R., and Whelan, T. A. (2016). Fathers' postnatal distress, parenting self-efficacy, later parenting behavior, and children's emotional–behavioral functioning: a longitudinal study. J. Family Psychol. 30, 907–917. doi: 10.1037/fam0000216
Roque, A. T. F., Lasiuk, G. C., Radünz, V., and Hegadoren, K. (2017). Scoping review of the mental health of parents of infants in the NICU. J. Obstetr. Gynecol. Neonatal Nurs. 46, 576–587. doi: 10.1016/j.jogn.2017.02.005
Sabnis, A., Fojo, S., Nayak, S. S., Lopez, E., Tarn, D. M., and Zeltzer, L. (2019). Reducing parental trauma and stress in neonatal intensive care: systematic review and meta-analysis of hospital interventions. J. Perinatol. 39, 375–386. doi: 10.1038/s41372-018-0310-9
Sacchi, L., Merzhvynska, M., and Augsburger, M. (2020). Effects of cumulative trauma load on long-term trajectories of life satisfaction and health in a population-based study. BMC Public Health 20:1612. doi: 10.1186/s12889-020-09663-9
Saigal, S., and Doyle, L. W. (2008). An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet 371, 261–269. doi: 10.1016/S0140-6736(08)60136-1
Schwartz, D. A. (2020). An analysis of 38 pregnant women with COVID-19, their newborn infants, and maternal-fetal transmission of SARS-CoV-2: maternal coronavirus infections and pregnancy outcomes. Arch. Pathol. Lab. Med. 144, 799–805. doi: 10.5858/arpa.2020-0901-SA
Semaan, A. T., Audet, C., Huysmans, E., Afolabi, B. B., Assarag, B., Banke-Thomas, A., et al. (2020). Voices from the frontline: findings from a thematic analysis of a rapid online global survey of maternal and newborn health professionals facing the COVID-19 pandemic. BMJ Global Health 5:e002967. doi: 10.1136/bmjgh-2020-002967
Shek, C. C., Ng, P. C., Fung, G. P., Cheng, F. W., Chan, P. K., Peiris, M. J., et al. (2003). Infants born to mothers with severe acute respiratory syndrome. Pediatrics 112, e254–e254. doi: 10.1542/peds.112.4.e254
Sim, K., Chua, H. C., Vieta, E., and Fernandez, G. (2020). The anatomy of panic buying related to the current COVID-19 pandemic. Psychiatry Res. 288:113015. doi: 10.1016/j.psychres.2020.113015
Stapleton, P. J., Murphy, M., McCallion, N., Brennan, M., Cunney, R., and Drew, R. J. (2016). Outbreaks of extended spectrum beta-lactamase-producing Enterobacteriaceae in neonatal intensive care units: a systematic review. Arch. Dis. Childhood-Fetal Neonatal Ed. 101, 72–78. doi: 10.1136/archdischild-2015-308707
Stefana, A., and Lavelli, M. (2016). I genitori dei bambini prematuri. Una prospettiva psicodinamica. Med. Bambino 35, 327–332. doi: 10.23736/S0026-4946.16.04618-1
Stefana, A., and Lavelli, M. (2017). Parental engagement and early interactions with preterm infants during the stay in the neonatal intensive care unit: protocol of a mixed-method and longitudinal study. BMJ Open 7:e013824. doi: 10.1136/bmjopen-2016-013824
Stefana, A., and Lavelli, M. (2018). What is hindering research on psychological aspects of fathers of premature infants? Minerva Pediatr. 70, 204–206.
Stefana, A., Lavelli, M., Rossi, G., and Beebe, B. (2020a). Interactive sequences between fathers and preterm infants in the neonatal intensive care unit. Early Hum. Dev. 140:104888. doi: 10.1016/j.earlhumdev.2019.104888
Stefana, A., Padovani, E. M., Biban, P., and Lavelli, M. (2018). Fathers' experiences with their preterm babies admitted to neonatal intensive care unit: a multi-method study. J. Adv. Nurs. 74, 1090–1098. doi: 10.1111/jan.13527
Stefana, A., Youngstrom, E. A., Hopwood, C. J., and Dakanalis, A. (2020b). The COVID-19 pandemic brings a second wave of social isolation and disrupted services. Eur. Arch. Psychiatry Clin. Neurosci. 270, 785–786. doi: 10.1007/s00406-020-01137-8
Stefana, A., Youngstrom, E. A., Jun, C., Hinshaw, S., Maxwell, V., Michalak, E., et al. (2020c). The COVID-19 pandemic is a crisis and opportunity for bipolar disorder. Bipolar Disord. 22, 641–643. doi: 10.1111/bdi.12949
Stuebe, A. (2020). Should infants be separated from mothers with COVID-19? First, do no harm. Breastfeed. Med. 15, 351–352. doi: 10.1089/bfm.2020.29153.ams
Tawfik, D. S., Sexton, J. B., Kan, P., Sharek, P. J., Nisbet, C. C., Rigdon, J., et al. (2017). Burnout in the neonatal intensive care unit and its relation to healthcare-associated infections. J. Perinatol. 37, 315–320. doi: 10.1038/jp.2016.211
Tscherning, C., Sizun, J., and Kuhn, P. (2020). Promoting attachment between parents and neonates despite the COVID-19 pandemic. Acta Paediatr. 109, 1937–1943. doi: 10.1111/apa.15455
Turpin, H., Urben, S., Ansermet, F., Borghini, A., Murray, M. M., and Müller-Nix, C. (2019). The interplay between prematurity, maternal stress and children's intelligence quotient at age 11: a longitudinal study. Sci. Rep. 9:450. doi: 10.1038/s41598-018-36465-2
Ursano, R. J., Zhang, L., and Li, H. (2009). PTSD and traumatic stress from gene to community and bench to bedside. Brain Res. 1293, 2–12. doi: 10.1016/j.brainres.2009.03.030
Van Mol, M. M., Kompanje, E. J., Benoit, D. D., Bakker, J., and Nijkamp, M. D. (2015). The prevalence of compassion fatigue and burnout among healthcare professionals in intensive care units: a systematic review. PLoS ONE 10:e0136955. doi: 10.1371/journal.pone.0136955
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020). Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 17:1729. doi: 10.3390/ijerph17051729
Wang, J., Zhou, M., and Liu, F. (2020). Reasons for healthcare workers becoming infected with novel coronavirus disease 2019 (COVID-19) in China. J. Hospital Infect. 105, 100–101. doi: 10.1016/j.jhin.2020.03.002
Wang, S., Guo, L., Chen, L., Liu, W., Cao, Y., Zhang, J., et al. (2020). A case report of neonatal 2019 coronavirus disease in China. Clin. Infect. Dis. 71, 853–857. doi: 10.1093/cid/ciaa225
Weintraub, A. S., Geithner, E. M., Stroustrup, A., and Waldman, E. D. (2016). Compassion fatigue, burnout and compassion satisfaction in neonatologists in the US. J. Perinatol. 36, 1021–1026. doi: 10.1038/jp.2016.121
Welch, M. G., and Ludwig, R. J. (2017). Calming cycle theory and the co-regulation of oxytocin. Psychodyn. Psychiatry 45, 519–540. doi: 10.1521/pdps.2017.45.4.519
Widström, A. M., Brimdyr, K., Svensson, K., Cadwell, K., and Nissen, E. (2019). Skin-to-skin contact the first hour after birth, underlying implications and clinical practice. Acta Paediatr. 108, 1192–1204. doi: 10.1111/apa.14754
Woody, C. A., Ferrari, A. J., Siskind, D. J., Whiteford, H. A., and Harris, M. G. (2017). A systematic review and meta-regression of the prevalence and incidence of perinatal depression. J. Affect. Disord. 219, 86–92. doi: 10.1016/j.jad.2017.05.003
Yan, H., Ding, Y., and Guo, W. (2020). Mental health of pregnant and postpartum women during the coronavirus disease 2019 pandemic: a systematic review and meta-analysis. Front. Psychol. 11:3324. doi: 10.3389/fpsyg.2020.617001
Yee, J., Kim, W., Han, J. M., Yoon, H. Y., Lee, N., Lee, K. E., et al. (2020). Clinical manifestations and perinatal outcomes of pregnant women with COVID-19: a systematic review and meta-analysis. Sci. Rep. 10:18126. doi: 10.1038/s41598-020-75096-4
Youngstrom, E., Hinshaw, S. P., Stefana, A., Chen, J., Michael, K., Van Meter, A., et al. (2020). Working with bipolar disorder during the COVID-19 pandemic: both crisis and opportunity. WikiJ. Med. 7:4. doi: 10.15347/WJM/2020.004
Youngstrom, E. A. (2013). Future directions in psychological assessment: combining evidence-based medicine innovations with psychology's historical strengths to enhance utility. J. Clin. Child Adolesc. Psychol. 42, 139–159. doi: 10.1080/15374416.2012.736358
Youngstrom, E. A. (2014). A primer on receiver operating characteristic analysis and diagnostic efficiency statistics for pediatric psychology: we are ready to ROC. J. Pediatr. Psychol. 39, 204–221. doi: 10.1093/jpepsy/jst062
Youngstrom, E. A., Choukas-Bradley, S., Calhoun, C. D., and Jensen-Doss, A. (2015). Clinical guide to the evidence-based assessment approach to diagnosis and treatment. Cogn. Behav. Pract. 22, 20–35. doi: 10.1016/j.cbpra.2013.12.005
Youngstrom, E. A., Halverson, T. F., Youngstrom, J. K., Lindhiem, O., and Findling, R. L. (2018). Evidence-based assessment from simple clinical judgments to statistical learning: evaluating a range of options using pediatric bipolar disorder as a diagnostic challenge. Clin. Psychol. Sci. 6, 243–265. doi: 10.1177/2167702617741845
Youngstrom, E. A., and Prinstein, M. J. (2020). “Introduction to evidence-based assessment: a recipe for success,” in Assessment of Disorders in Childhood and Adolescence, 5th Edn., eds E. A. Youngstrom, M. J. Prinstein, E. J. Mash, and R. A. Barkley (New York, NY: Guilford Publications), 3–29.
Youngstrom, E. A., and Van Meter, A. (2016). Empirically supported assessment of children and adolescents. Clin. Psychol. 23, 327–347. doi: 10.1111/cpsp.12172
Youngstrom, E. A., and Van Meter, A. (2018). “Advances in evidence-based assessment,” in A Guide to Assessments That Work, 2nd Edn., eds J. Hunsley, and E. J. Mash (New York, NY: Oxford University Press), 32–44. doi: 10.1093/med-psych/9780190492243.003.0003
Youngstrom, E. A., Van Meter, A., Frazier, T. W., Hunsley, J., Prinstein, M. J., Ong, M. L., et al. (2017). Evidence-based assessment as an integrative model for applying psychological science to guide the voyage of treatment. Clin. Psychol. 24, 331–363. doi: 10.1111/cpsp.12207
Yuan, R., Xu, Q. H., Xia, C. C., Lou, C. Y., Xie, Z., Ge, Q. M., et al. (2020). Psychological status of parents of hospitalized children during the COVID-19 epidemic in China. Psychiatry Res. 2020:112953. doi: 10.1016/j.psychres.2020.112953
Zante, B., Camenisch, S. A., Jeitziner, M. M., Jenni-Moser, B., and Schefold, J. C. (2020). Fighting a family tragedy: family-centred care in times of the COVID-19 pandemic. Anaesthesiol. Intens. Ther. 52, 336–338. doi: 10.5114/ait.2020.100501
Zeng, H., Xu, C., Fan, J., Tang, Y., Deng, Q., Zhang, W., et al. (2020). Antibodies in infants born to mothers with COVID-19 pneumonia. JAMA 323, 1848–1849. doi: 10.1001/jama.2020.4861
Zeng, L., Xia, S., Yuan, W., Yan, K., Xiao, F., Shao, J., et al. (2020). Neonatal early-onset infection with SARS-CoV-2 in 33 neonates born to mothers with COVID-19 in Wuhan, China. JAMA Pediatr. 174, 722–725. doi: 10.1001/jamapediatrics.2020.0878
Zhu, H., Wang, L., Fang, C., Peng, S., Zhang, L., Chang, G., et al. (2020). Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatrics 9:51. doi: 10.21037/tp.2020.02.06
Keywords: COVID-19, pre-term infant, neonatal intensive care unit, parents, NICU staff, family-centered care
Citation: Cena L, Biban P, Janos J, Lavelli M, Langfus J, Tsai A, Youngstrom EA and Stefana A (2021) The Collateral Impact of COVID-19 Emergency on Neonatal Intensive Care Units and Family-Centered Care: Challenges and Opportunities. Front. Psychol. 12:630594. doi: 10.3389/fpsyg.2021.630594
Received: 18 November 2020; Accepted: 25 January 2021;
Published: 24 February 2021.
Edited by:
Efrat Neter, Ruppin Academic Center, IsraelReviewed by:
Mariana Amorim, University of Porto, PortugalPamela A. Geller, Drexel University, United States
Alison Hartman, Drexel University, United States, in collaboration with reviewer PG
Copyright © 2021 Cena, Biban, Janos, Lavelli, Langfus, Tsai, Youngstrom and Stefana. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alberto Stefana, YWxiZXJ0by5zdGVmYW5hJiN4MDAwNDA7Z21haWwuY29t
†These authors have contributed equally to this work
 Loredana Cena
Loredana Cena Paolo Biban2†
Paolo Biban2† Jessica Janos
Jessica Janos Manuela Lavelli
Manuela Lavelli Angelina Tsai
Angelina Tsai Eric A. Youngstrom
Eric A. Youngstrom Alberto Stefana
Alberto Stefana