- 1CiaoLapo Foundation for Perinatal Health, Prato, Italy
- 2Perinatal Research Laboratory (PeaRL), University of Florence, Florence, Italy
- 3Section of Pharmacology and Toxicology, Department of Neurosciences, Psychology, Drug Research and Child Health, University of Florence, Florence, Italy
Background: When infertility is diagnosed, physicians have the difficult task to break bad news. Their communication skills play a central role in improving patients' coping abilities and adherence to infertility treatments. However, specific guidelines and training courses on this topic are still lacking. The aim of the present study is to provide some practical advice for improving breaking bad news in infertility diagnosis through a systematic literature review of qualitative and quantitative studies.
Methods: Electronic searches were performed in the MEDLINE, Embase, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Psychology and Behavioral Sciences Collection databases. All articles focusing on the communication of the diagnosis of infertility were included. The main findings of each included article were then summarized.
Results: Literature search identified 11,838 references that were screened for eligibility. Full texts of 81 articles were retrieved, and their analysis led to the inclusion of 4 articles, which treated the theme of communication of infertility only partially. The main addressed aspects concerning the communication of the infertility diagnosis were the following: (i) the value that patients give to healthcare professionals' communication skills; (ii) the importance of giving clear information on diagnostic procedures and treatments in order to decrease patients' anxiety; and (iii) the importance of involving both partners.
Conclusions: This review pointed out that the communication of the infertility diagnosis is still underinvestigated. Specific guidelines are currently not available, but other protocols could be used. Taking into account the principal aspects of communication highlighted with this review, in this study, we suggested an adaptation of the original SPIKES protocol that could be used by healthcare professionals for the communication of the infertility status.
Introduction
Infertility is an extensive problem worldwide. It has been estimated that in 2010, there were 48.5 million infertile couples all over the world. Around 2 out 100 women between 24 and 44 years old suffer from primary infertility, while 10 out 100 women suffer from secondary infertility (Mascarenhas et al., 2012). In Italy, the “Istituto Superiore di Sanità” estimates that around 15% of couples suffer from infertility (Istituto Superiore di Sanità). Most couples begin to fear an infertility issue after a few months of unsuccessful attempts to conceive. The time frame between the decision to have a child and the diagnosis of infertility is very stressful: infertility is a physical condition that has a direct impact on the individual's perception of physical integrity, on the couple functioning, and on the couple's short- and long-term life projects (Ansha Patel and Sharma, 2018). For this reason, the diagnosis of infertility has a strong impact on women' and couples' well-being. In a study of Domar et al., about 500 women with several medical conditions completed the Symptom Checklist-90-Revised (SCL-90R). The results suggest that the psychological impact of stress related to reproductive problems could be comparable to those of other long-term medical conditions such as cancer, undergoing cardiac rehabilitation, and hypertension (Domar et al., 1993).
When infertility is diagnosed, physicians have the difficult task to break bad news. However, little is known about communication in this field. The diagnosis of infertility has a strong impact per se, and it could be defined a “symbolic loss” and is related to an “infertility grief.” The “symbolic loss” related to the diagnosis of infertility is not clear and visible to others, while other life events are clear and identifiable forms of loss, such as the death of a loved one. In other conditions, the loss is publicly recognized, and the bereaved are likely to receive support throughout their mourning. They can openly discuss their feelings of loss, and the grieving process follows cultural norms that include rituals to mitigate the grieving process (McBain and Reeves, 2019). None of this happens following a diagnosis of infertility.
Moreover, infertility diagnosis is related to many other challenges for couples: they have to decide the subsequent steps, and they have to discuss the risks and limitations related to infertility treatments with healthcare professionals. This has a deep impact on their health and quality of life: according to a literature review, women who received a diagnosis of infertility had significantly lower scores on mental health, social functioning, and emotional behavior (Chachamovich et al., 2010). It should be taken into account that infertility treatments have a poor outcome for most couples. In fact, in Italy, the percentage of live births with intrauterine insemination (IUI) over the total of assisted reproductive technology (ART) cycles is 6.9%, while with FIVET or intracytoplasmatic sperm injection (ICSI) is 11.3% (Istituto Superiore di Sanità-ISS, 2017). In this sense, sometimes, the diagnosis of infertility is not the only and last piece of bad news: for instance, people who resort to ART often receive further bad news during the diagnostic workup and the infertility treatment (reiteration of bad news) (Lalos, 1999; Leone et al., 2017). It is useful to remember that bad news following the primary diagnosis of infertility is one of the reasons for patients' dropout before completing infertility treatments; moreover, poor management of psychological aspects is listed among the main causes of treatment discontinuation (Gameiro et al., 2012). Quality of communication is a key point for improving patients' coping abilities, well-being, adherence to infertility treatments, and patient–provider continuity of care. The latter is one of the main factors of patient-centered care (PCC) that could prove essential for treatment compliance (Palmer-Wackerly et al., 2019). However, while patients claim for clear information, honesty, emotional support, and respect (Ussher et al., 2018), healthcare providers should have access to adequate training programs. Some experiences demonstrated that nurses' knowledge of reproductive issues, communication skills, and practice behaviors increased significantly after structured courses (Quinn et al., 2019).
Nowadays, the impact of breaking bad news on healthcare providers and their perceptions in the relationship with the patient are still poorly characterized. The fear of inflicting pain or not to fully understand patients' discomfort, lack of time, and the complex management of patients' expectations are just some of the problems identified (Klitzman, 2018). In addition, more attention must be paid to psychological care after the diagnosis of infertility and after the subsequent bad news due to the failure of ART (e.g., a negative pregnancy test). In particular, the current literature highlights the importance of specific psychological interventions to reduce stress and to improve couples' well-being.
Although there is a proposal of guidelines on how to communicate bad news during ART (based on SPIKES protocol) (Leone et al., 2017), shared protocols and guidelines on how to communicate the diagnosis of infertility are currently not available. The fields of infertility and ART are strongly connected but show different communication issues. As mentioned above, in the context of ART, there is a reiteration of bad news connected to repeated treatment failures and the clinical ineffectiveness of medical treatments (Leone et al., 2017). Meanwhile, infertility diagnosis involves couples before the beginning of the ART path. In this case, they face bad news for the first time and have not dealt with an alternation of hope and despair. For this reason, the aim of the present systematic literature review of qualitative and quantitative studies is to explore existing research focusing on the communication of the diagnosis of infertility and to highlight existing evidence on physician–patient relationship in this field. Starting from this point, the final goal of our research was to provide some practical advice for improving breaking bad news in clinical practice.
Materials and Methods
Search Strategy
Data for the systematic review were obtained through a search strategy based on the intersection of two main domains. The first one was related to infertility, communication, and physician–patient relationship. The second one focused on healthcare professionals vs. patients (women and couples). Electronic searches were performed in the MEDLINE, Embase, PsycINFO, Cumulative Index to Nursing and Allied Health Literature (CINAHL), and Psychology and Behavioral Sciences Collection (PBSC) databases. Complete search strategies for all databases are provided within the Supplementary Material 1.
Inclusion and Exclusion Criteria
We included all studies, posters, and abstracts published in English or Italian in scientific journals between January 2000 and March 5, 2020. We included all qualitative and quantitative studies, independently from their study design, containing information about breaking bad news in infertility. Additional searches in the reference lists of retrieved manuscripts were also performed. We excluded all papers that deal with infertility care but did not mention how to communicate the diagnosis of infertility. We also excluded remaining articles concerning patients' coping strategies and psychological adaptation after receiving the diagnosis of infertility.
Selection Process and Data Extraction
Records were retrieved on the same day from all sources. Two investigators (CR, LM) independently selected the studies (double-blind selection). Discrepancies about inclusion/exclusion were resolved through discussion or in consultation with a third reviewer (AV, GC). CR and LM reviewed the main reports and Supplementary Material and extracted all relevant information for the included studies. In case of doubt or missing information, we contacted the authors of the original paper. For each paper, the following qualitative and/or quantitative data were extracted: country, type of study (i.e., quantitative, qualitative, guidelines), perspective [i.e., patients' or healthcare practitioners' (HCPs')], main results, and parameters used by authors for their evaluation (i.e., theme for qualitative studies, scores for quantitative studies), and main results concerning communication and relationship with the staff.
Quality of Included Studies
Quality of included studies was evaluated using the Checklist for Qualitative Research by the Joanna Briggs Institute (JBI) (JBI Critical Appraisal Checklist for Qualitative Research, 2020) and with the Checklist for the Quality Assessment of Guidelines (AGREE II) (Canadian Agency for Drugs and Technologies in Health (CADTH), 2014).
This systematic review was reported in accordance with the preferred reporting items for systematic reviews and meta-analyses (PRISMA) (Moher et al., 2009).
Results
A flow chart describing the results of the selection process is reported in Figure 1. The literature search identified 19,347 references. After removing duplicates (n = 7,509), titles and abstracts of 11,838 references were screened. Of those, 11,757 were excluded. We retrieved the full texts of the remaining 81 references and assessed them for eligibility.
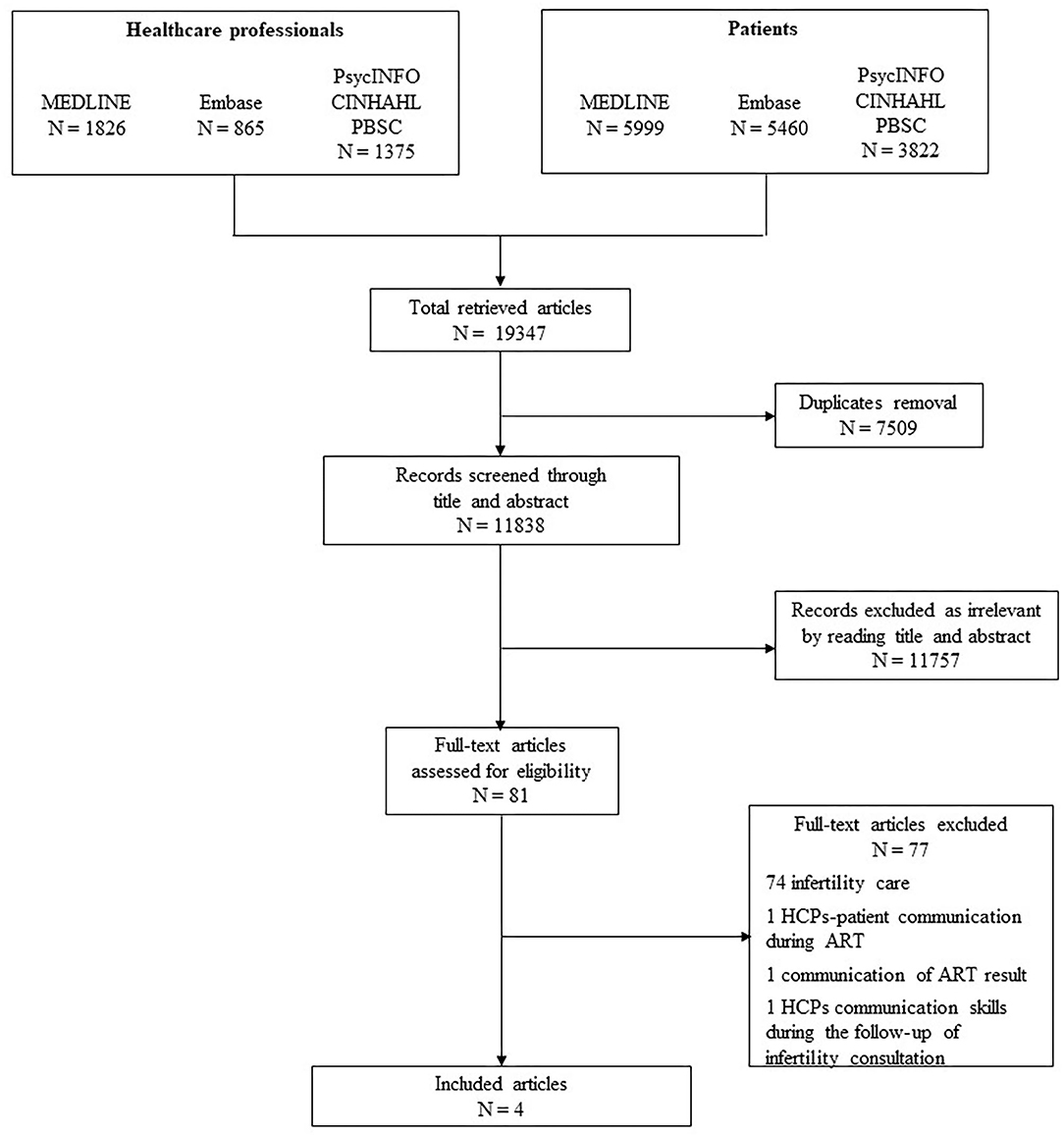
Figure 1. Preferred reporting items for systematic reviews and meta-analyses PRISMA flowchart of search strategy results.
Seventy-seven studies were excluded due to the absence of information about breaking bad news in infertility. These papers deal with infertility care, but there was no reference to the specific topic explored in the present review (communication of the infertility diagnosis). For instance, the paper “Impediments to communication and relationships between infertility care providers and patients” concerns communication issues between ART practitioners and patients that underwent infertility treatment (Klitzman, 2018). However, it does not take into account how to communicate the diagnosis of infertility. Another study concerns the communication of results after the first cycle of ART, but it does not focus on giving bad news specifically and does not deal with the diagnosis of infertility itself (Groh and Wagner, 2005). A paper published in 2005 (Leite et al., 2005) focused on women's satisfaction with physicians' communication skills during a follow-up infertility consultation at the initial phase of the infertility treatment. Although physicians' communication skills are mentioned in the study, there is no advice on how to communicate the diagnosis of infertility. Once again the main focus is on ART and infertility treatment in general.
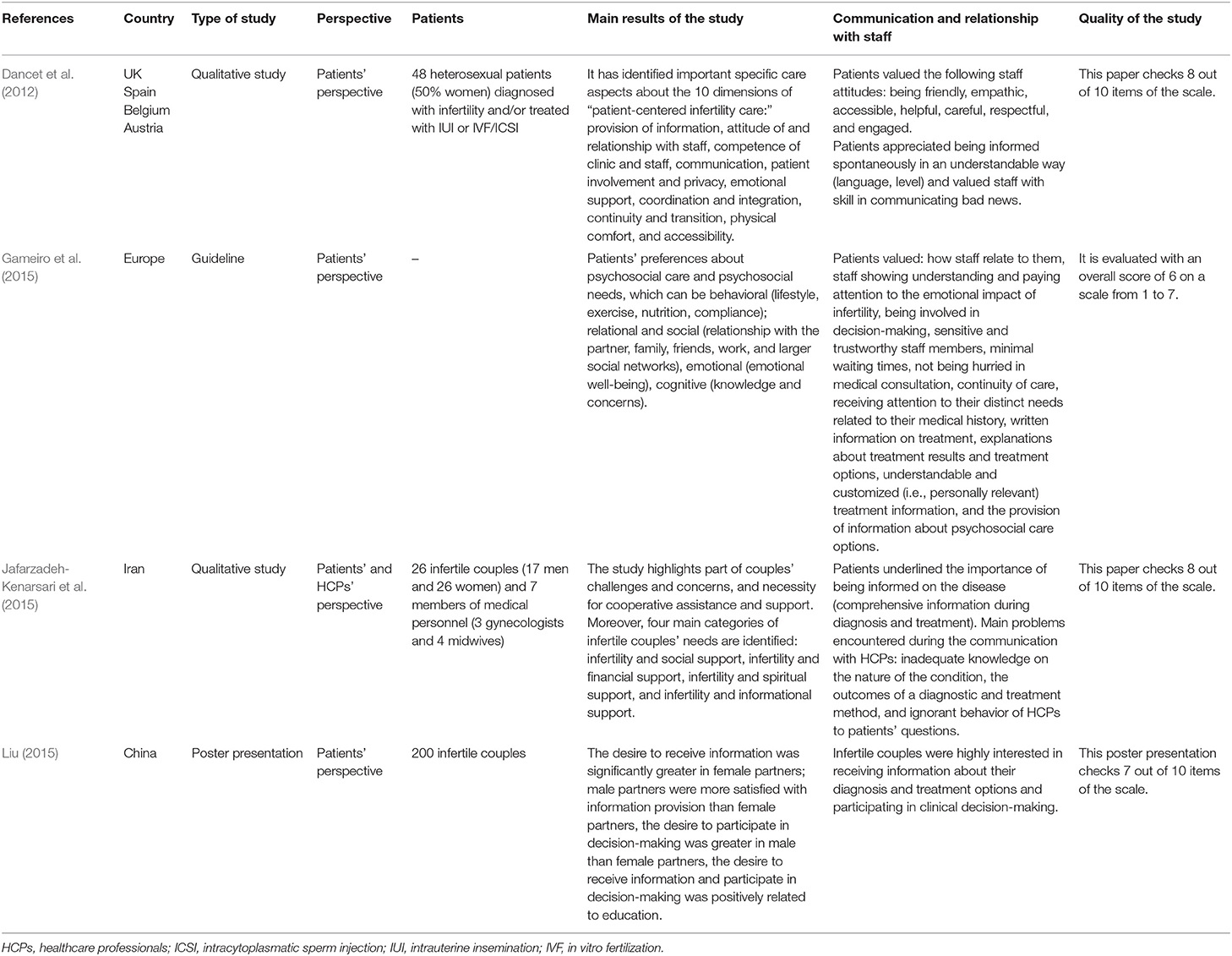
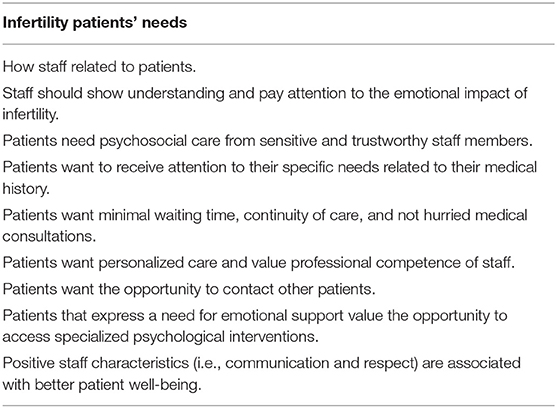
Ultimately, four studies were eligible according to the inclusion criteria (Dancet et al., 2012; Gameiro et al., 2015; Jafarzadeh-Kenarsari et al., 2015; Liu, 2015). Features of the analyzed studies are reported in Table 1. Two of them are qualitative studies, and the others are a poster presentation and a clinical guideline for psychosocial care in infertility and the medically assisted reproduction setting. Apart from one paper that has a mixed perspective of patients and HCPs (Jafarzadeh-Kenarsari et al., 2015), the others take only the patients' perspective. The main results of each paper are highlighted, with particular attention to the aspects of communication and relationship with staff. In particular, Dancet et al. (2012) suggested that patients “valued staff with skill in communicating bad news.” They reported no other advice concerning how to communicate the diagnosis of infertility. The study mainly concerns the “patient centered infertility care” model (PCIC) from the patients' perspective and does not explain its dimensions thoroughly. Authors gave just a brief description of them (Dancet et al., 2012). The European Society of Human Reproduction and Embryology (ESHRE) guidelines (Gameiro et al., 2015) pointed out that fertility staff should provide information about diagnostic procedures to decrease patients' anxiety and stress related to the process itself. Moreover, the authors recommended involving both partners during the diagnosis. These guidelines are a landmark in the infertility care field, but their primary focus is the treatment of infertility. Finally, the poster presentation by Liu (2015) suggested that Chinese patients valued receiving information about their diagnosis (Liu, 2015). Other advice concerned both the diagnosis and the treatment of infertility without a clear separation between the two steps. In particular, authors pointed out that women were more anxious to receive information than their male partners, while the latter dominated in clinical decision-making. Another paper from Iran highlights the patients' need to obtain comprehensive information about diagnosis and fertility treatment (Jafarzadeh-Kenarsari et al., 2015), and this is in line with the poster presentation by Liu (Liu, 2015). Inadequate knowledge about their condition leads to mistrust against HCPs as shown by a couple's words: “We are so unhappy because they refuse to explain what the problem is [...] we have to search the web to find some answers.” 18 Finally, authors of the ESHRE guidelines made a list of general principles of psychosocial care that patients value that could be applied to the communication of bad news (Table 2) (Gameiro et al., 2015). According to JBI's Checklist for the evaluation of the quality of included studies and according to the Checklist for the Quality Assessment of Guidelines (AGREE II), all papers show a good quality. However, the paper by Dancet et al. (2012) and the poster presentation by Liu (2015) do not mention any cultural or theoretical statement from the researchers, and they do not address any influence of the researcher on the research or vice versa. On the other hand, in the paper by Jafarzadeh-Kenarsari et al. (2015), the cultural and theoretical statement from the researchers is unclear, and the evaluation of the influence of the researcher on the research or vice versa are not applicable because it is part of a larger study. Although the poster presentation is not a qualitative study, data reported were evaluated even though we could not assess if the conclusion drawn in the study flowed from the analysis of the data. Moreover, the ESHRE guidelines show a high score in all domains except for the applicability domain where the average score is 4 in a scale from 1 to 7. The evaluation of the domain of “Editorial Independence” is not applicable because the guidelines were funded by the ESHRE group itself. Complete quality evaluation of included studies is available in Supplementary Material 2.
Discussion
Infertility is a very common issue around the world, and it represents a milestone in a couple's life. Coping with the infertility status can be very complicated due to the sudden interruption of the family plan and the lack of acknowledgment of the couple's grief. However, HCPs can avoid further trauma and pain using good communication. How the diagnosis is communicated could improve patients' well-being and the ability to cope with it.
In this literature review, we did not find any protocol or guideline concerning breaking bad news in infertility. Many papers concern infertility treatment care or ART, for instance, the paper of Leone et al. (2017) about a proposal of guidelines about breaking bad news in ART. However, we found some useful information that could help practitioners in their daily practice whenever they face an infertility diagnosis. About this, Dancet et al. (2012) suggested that patients value staff's skills on communicating bad news16. This is in agreement to the ESHRE guidelines (Gameiro et al., 2015), which points out that patients value positive staff characteristics including communication skills, which are linked to the couples' well-being. Moreover, we should consider that some patients report unprofessional communication from HCPs. In fact, they point out that they felt the practitioners' fear during the diagnosis of infertility (Dancet et al., 2011).
Giving information is linked to the staff's communication skills, and it is very important to patients according to the ESHRE guideline (Gameiro et al., 2015), Liu's (2015) and Jafarzadeh-Kenarsari et al. (2015) works. Another important issue is the need for personalized, sensitive, and continuous care from trustworthy staff members who should show an understanding of the emotional impact of infertility (Gameiro et al., 2015). Communication, information, and continuity of care are three dimensions of PCC whose application is linked to the patients' well-being (Gameiro et al., 2013). PCC is usually valued more important by patients than HCPs (Van Empel et al., 2011), and this could be an obstacle to satisfy patients' needs. Moreover, giving poor information could lead to mistrust against HCPs (Jafarzadeh-Kenarsari et al., 2015), and it might result in inadequate care. Also, in this case, there is a different evaluation about the importance of information between patients and providers. The latter ones value providing information less important than patients do (Streisfield et al., 2015). This gap should be removed to improve the quality of care and to move from physician centered care to PCC.
Concerning psychological help and support, patients expect to have the possibility to access professional psychological care, and they want the opportunity to contact other couples (Gameiro et al., 2015). Patients have various counseling needs that HCPs should take into account and that involve several areas: emotional, sexual, marital, and the family one (Jafarzadeh-Kenarsari et al., 2015). Infertility counseling organizations agree that all patients who suffer from infertility should be able to access individual or couple counseling before, during, and after infertility treatment. Infertility counseling has different goals depending on the type of counseling itself: individual, couple, or group approach. Individual counseling allows exploring in greater depth concerns related to the experience and treatment of infertility, as well as coping mechanisms and social implications. Couple counseling enables patients to understand couple dynamics and to learn how to support each other. Finally, group counseling offers couples the opportunity to share their experience with others who are living in a similar situation (Van den Broeck et al., 2010). The literature helps mental health practitioners by showing the key issues that should be considered during infertility counseling (Stammer et al., 2002; Van den Broeck et al., 2010; Peterson et al., 2012). For instance, gender differences involve a diverse coping approach to the issue (Peterson et al., 2012).
Many other psychological approaches appear to be effective to reduce couples' stress and improve well-being. For instance, acceptance and commitment therapy helps patients to reduce stress and to increase couples' intimacy (Taheri et al., 2013). A paper about mindfulness-based cognitive approach points out how this technique can help to improve women's self-acceptance and their relationship with others (Fard et al., 2018).
Implications for Clinical Practice
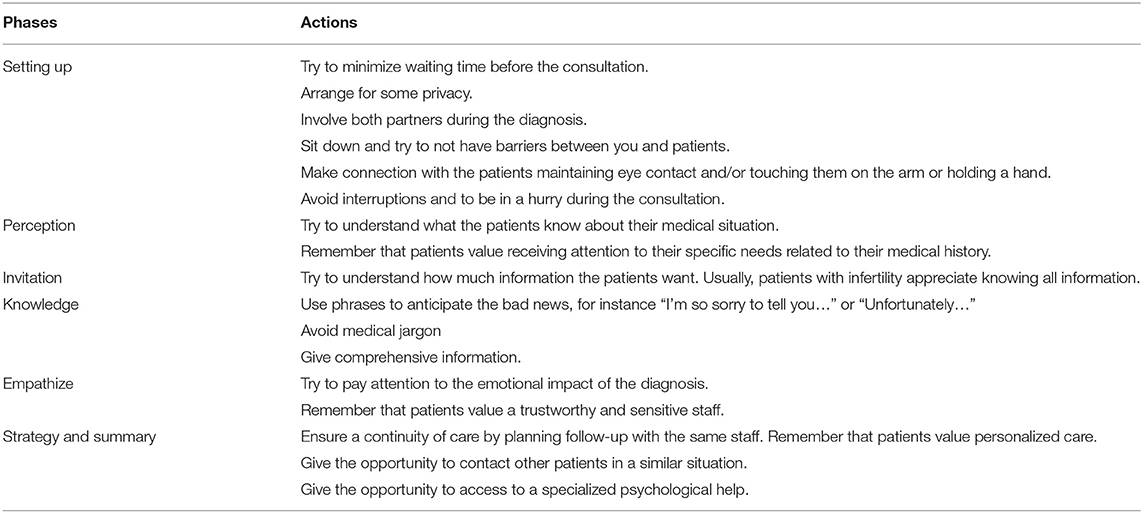
Although there is no specific guideline to communicate the diagnosis of infertility, other protocols currently adopted in daily medical practice could be used. SPIKES is an easy-to-follow protocol that has been used in the oncology setting for 20 years. It is divided in six steps, which help and facilitate HCPs to break bad news (Baile et al., 2000). These steps are identified as “Setting up, Perception, Invitation, Knowledge, Empathize, Strategy, and Summary.” SPIKES has been applied in the area of perinatal grief (Greiner and Conklin, 2015; Mosconi et al., 2019) and ART (Leone et al., 2017) and could be used to communicate the infertility status. In Table 3, we suggest an adaptation of the original SPIKES protocol for the infertility field, taking into account the results of this literature review. In particular, we modified some advice included in the original version of the SPIKES protocol, and we added other recommendations; for instance, we replaced the sentence “Manage time constraints and interruptions” with “Avoid interruptions and to be in a hurry during the consultation.” In fact, patients with infertility appreciate a thorough consultation without rush. These few actions could be very useful in clinical practice due to their easiness to be remembered and to be applied. Moreover, they could be integrated with the professional personal experience of HCPs.
Strengths and Limitations
This review has several points of strength. First, the literature research was performed, retrieving articles from five large databases, and the literature screening was performed double blind, ensuring a rigorous methodology. Second, the extensive analysis of articles allowed us to highlight the lack of investigations focused on this topic and, therefore, to propose a new approach for the communication of infertility diagnosis. Finally, focusing on the importance of HCPs' communication skills in this field, this review may act as a starting point for future investigations and targeted interventions for HCPs.
The main limitation of this review lies in the scarcity of information reported in each of the included studies. In this light, the adaptation of the original SPIKES protocol may not include all aspects of patients' needs other than the few ones reported within the included articles. Further research could identify other areas of interest to be analyzed and included in an updated protocol for the communication of the infertility diagnosis.
Conclusions
Most of the currently available literature is related to infertility treatment care, and its main focus was not the communication of infertility diagnosis, which represents the starting point of infertility grief for many couples. Only a few papers give some advice about breaking bad news, and there are no thorough guidelines about it. Based on the findings of this review, our adapted version of the SPIKES protocol is an easy-to-use guideline, which could be very useful for healthcare professionals and could be easily integrated in routinary clinical practices.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Author Contributions
AV and CR: conceptualization and validation. GC and LM: original draft, methodology, writing, and formal analysis. All authors: writing, review, and editing.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.615699/full#supplementary-material
References
Ansha Patel, P. S. V. N., and Sharma, P. K. (2018). In cycles of dreams, despair, and desperation: research perspectives on infertility specific distress in patients undergoing fertility treatments. J. Hum. Reprod. Sci. 11, 320–328. doi: 10.4103/jhrs.JHRS_42_18
Baile, W. F., Buckman, R., Lenzi, R., Glober, G., Beale, E. A., and Kudelka, A. P. (2000). SPIKES—a six-step protocol for delivering bad news: application to the patient with cancer. Oncologist 5, 302–311. doi: 10.1634/theoncologist.5-4-302
Canadian Agency for Drugs and Technologies in Health (CADTH) (2014). Stepwise Approach for the Prescription of Opiates for Non-Cancer Pain: A Review of Clinical Evidence and Guidelines. Available online at: https://www.ncbi.nlm.nih.gov/books/NBK263404/ (accessed December 01, 2020).
Chachamovich, J. R., Chachamovich, E., Ezer, H., Fleck, M. P., Knauth, D., and Passos, E. P. (2010). Investigating quality of life and health-related quality of life in infertility: a systematic review. J. Psychosom. Obstet. Gynecol. 31, 101–110. doi: 10.3109/0167482X.2010.481337
Dancet, E. A. F., Dhooghe, T. M., Sermeus, W., Van Empel, I., Strohmer, H., Wyns, C., et al. (2012). Patients from across Europe have similar views on patient-centred care: an international multilingual qualitative study in infertility care. Hum. Reprod. 27, 1702–1711. doi: 10.1093/humrep/des061
Dancet, E. A. F., Van Empel, I. W. H., Rober, P., Nelen, W. L. D. M., Kremer, J. A. M., and Dhooghe, T. M. (2011). Patient-centred infertility care: a qualitative study to listen to the patients voice. Hum. Reprod. 26, 827–833. doi: 10.1093/humrep/der022
Domar, A. D., Zuttermeister, P. C., and Friedman, R. (1993). The psychological impact of infertility: a comparison with patients with other medical conditions. J. Psychosom. Obstet. Gynaecol. 14, 45–52.
Fard, T. R., Kalantarkousheh, M., and Faramarzi, M. (2018). Effect of mindfulness-based cognitive infertility stress therapy on psychological well-being of women with infertility. Middle East Fertil. Soc. J. 23, 476–481. doi: 10.1016/j.mefs.2018.06.001
Gameiro, S., Boivin, J., Dancet, E., De Klerk, C., Emery, M., Lewis-Jones, C., et al. (2015). ESHRE guideline: routine psychosocial care in infertility and medically assisted reproduction - a guide for fertility staff. Hum. Reprod. 30, 2476–2485. doi: 10.1093/humrep/dev177
Gameiro, S., Boivin, J., Peronace, L., and Verhaak, C. M. (2012). Why do patients discontinue fertility treatment? A systematic review of reasons and predictors of discontinuation in fertility treatment. Hum. Reprod. Update 18, 652–669. doi: 10.1093/humupd/dms031
Gameiro, S., Canavarro, M., and Boivin, J. (2013). Patient centred care in infertility health care: direct and indirect associations with wellbeing during treatment. Patient Educ. Couns. 93, 646–654. doi: 10.1016/j.pec.2013.08.015
Greiner, A. L., and Conklin, J. (2015). Breaking bad news to a pregnant woman with a fetal abnormality on ultrasound. Obstet. Gynecol. Surv. 70, 39–44. doi: 10.1097/OGX.0000000000000149
Groh, C. J., and Wagner, C. (2005). The art of communicating ART results: an analysis of infertile couples' experience. J. Reprod. Infant Psychol. 23, 333–346. doi: 10.1080/02646830500273533
Istituto Superiore di Sanità-ISS (2017). Available online at: https://www.iss.it/infertilità-e-pma (accessed October 03, 2020).
Jafarzadeh-Kenarsari, F., Ghahiri, A., Habibi, M., and Zargham-Boroujeni, A. (2015). Exploration of infertile couples' support requirements: a qualitative study. Int. J. Fertil. Steril. 9, 81–92. doi: 10.22074/ijfs.2015.4212
JBI Critical Appraisal Checklist for Qualitative Research (2020). Available online at: https://joannabriggs.org/sites/default/files/2020-08/Checklist_for_Qualitative_Research.pdf (accessed December 01, 2020).
Klitzman, R. (2018). Impediments to communication and relationships between infertility care providers and patients. BMC Womens Health. 18:84. doi: 10.1186/s12905-018-0572-6
Lalos, A. (1999). Breaking bad news concerning fertility. Hum. Reprod. 14, 581–585. doi: 10.1093/humrep/14.3.581
Leite, R. C., Makuch, M. Y., Petta, C. A., and Morais, S. S. (2005). Women's satisfaction with physicians' communication skills during an infertility consultation. Patient Educ. Couns. 59, 38–45. doi: 10.1016/j.pec.2004.09.006
Leone, D., Menichetti, J., Barusi, L., Chelo, E., Costa, M., De Lauretis, L., et al. (2017). Breaking bad news in assisted reproductive technology: a proposal for guidelines. Reprod. Health. 14:87. doi: 10.1186/s12978-017-0350-1
Liu, W. (2015). Infertile patients' preference for receiving clinical information and participating in decision-making in China. Hum. Reprod. 30:347.
Mascarenhas, M. N., Flaxman, S. R., Boerma, T., Vanderpoel, S., and Stevens, G. A. (2012). National, regional, and global trends in infertility prevalence since 1990: a systematic analysis of 277 health surveys. PLoS Med. 9:e1001356. doi: 10.1371/journal.pmed.1001356
McBain, T. D., and Reeves, P. (2019). Women's experience of infertility and disenfranchised grief. Fam. J. 27, 156–166 doi: 10.1177/1066480719833418
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G., Altman, D., Antes, G., et al. (2009). Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6:e1000097. doi: 10.1371/journal.pmed.1000097
Mosconi, L., Ravaldi, C., and Vannacci, A. (2019). “A guideline to breaking bad news in prenatal ultrasound screening,” in International Stillbirth Alliance, Annual Conference on Perinatal Mortality and Bereavement Care (Madrid). Available online at: https://www.isa2019madrid.com/breaking-bad-news-during-prenatal-ultrasound-screening/ (accessed December 1, 2020).
Palmer-Wackerly, A. L., Voorhees, H. L., D'Souza, S., and Weeks, E. (2019). Infertility patient-provider communication and (dis)continuity of care: An exploration of illness identity transitions. Patient Educ. Couns. 102, 804–809. doi: 10.1016/j.pec.2018.12.003
Peterson, B., Boivin, J., Norré, J., Smith, C., Thorn, P., and Wischmann, T. (2012). An introduction to infertility counseling: A guide for mental health and medical professionals. J. Assist. Reprod. Genet. 29, 243–248. doi: 10.1007/s10815-011-9701-y
Quinn, G. P., Bowman Curci, M., Reich, R. R., Gwede, C. K., Meade, C. D., and Vadaparampil, S. T. (2019). Impact of a web-based reproductive health training program: ENRICH (educating nurses about reproductive issues in cancer healthcare). Psychooncology 28, 1096–1101. doi: 10.1002/pon.5063
Stammer, H., Wischmann, T., and Verres, R. (2002). Counseling and couple therapy for infertile couples. Fam. Process. 41, 111–122. doi: 10.1111/j.1545-5300.2002.40102000111.x
Streisfield, A., Chowdhury, N., Cherniak, R., and Shapiro, H. (2015). Patient centered infertility care: The health care provider's perspective. Patient Exp. J. 2, 93–97 doi: 10.35680/2372-0247.1062
Taheri, Z., Zeinalzadeh, M., Ghanbarpour, F., and Taheri, M. (2013). Effect of psychotherapy with acceptance and commitment therapy approach on reduction of infertility stress and increase of infertile couples' intimacy. Int. J. Fertil. Steril. 7(Suppl. 1), 157–158.
Ussher, J. M., Parton, C., and Perz, J. (2018). Need for information, honesty and respect: patient perspectives on health care professionals communication about cancer and fertility. Reprod. Health 15:2. doi: 10.1186/s12978-017-0441-z
Van den Broeck, U., Emery, M., Wischmann, T., and Thorn, P. (2010). Counselling in infertility: Individual, couple and group interventions. Patient Educ. Couns. 81, 422–428. doi: 10.1016/j.pec.2010.10.009
Keywords: infertility, care, communication, counseling, prenatal care, perinatal care
Citation: Mosconi L, Crescioli G, Vannacci A and Ravaldi C (2021) Communication of Diagnosis of Infertility: A Systematic Review. Front. Psychol. 12:615699. doi: 10.3389/fpsyg.2021.615699
Received: 09 October 2020; Accepted: 02 February 2021;
Published: 18 March 2021.
Edited by:
Lidia Borghi, University of Milan, ItalyReviewed by:
Isolde Martina Busch, University of Verona, ItalyDaniela Leone, University of Milan, Italy
Copyright © 2021 Mosconi, Crescioli, Vannacci and Ravaldi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alfredo Vannacci, YWxmcmVkby52YW5uYWNjaUB1bmlmaS5pdA==
 Laura Mosconi
Laura Mosconi Giada Crescioli
Giada Crescioli Alfredo Vannacci
Alfredo Vannacci Claudia Ravaldi
Claudia Ravaldi