
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 19 February 2021
Sec. Psychology for Clinical Settings
Volume 12 - 2021 | https://doi.org/10.3389/fpsyg.2021.588767
 Federica Scarpina1,2*
Federica Scarpina1,2* Ilaria Bastoni3
Ilaria Bastoni3 Simone Cappelli3
Simone Cappelli3 Lorenzo Priano1,2*
Lorenzo Priano1,2* Emanuela Giacomotti1
Emanuela Giacomotti1 Gianluca Castelnuovo3,4
Gianluca Castelnuovo3,4 Enrico Molinari3,4
Enrico Molinari3,4 Ilaria Maria Angela Tovaglieri5
Ilaria Maria Angela Tovaglieri5 Mauro Cornacchia5
Mauro Cornacchia5 Paolo Fanari5
Paolo Fanari5 Alessandro Mauro1,2
Alessandro Mauro1,2Obstructive sleep apnea (OSA) syndrome severely affects psychological well-being. This syndrome frequently occurs in obesity; however, no previous study has investigated the level of psychological well-being in the case of OSA syndrome associated with obesity. In this work, we assessed the level of psychological well-being in fifty-two individuals affected by OSA syndrome and obesity through the Psychological General Well-Being Index. Moreover, we investigated the role of personality, cognitive functioning and attentional capabilities, subjective perception and objective measurement about sleeping, on the subjective perception of psychological well-being. Our sample reported a lower level of psychological well-being; the participants’ scores were below the normative cut-off in all components, except for depression symptoms. A lower expression of harm avoidance temperament and a lower level of daily sleepiness predicted a higher level of psychological well-being. Psychological well-being seemed to be severely affected in individuals affected by OSA syndrome and obesity. The temperament and subjective perception of daily alertness and sleepiness, rather than the syndrome severity, seemed to play a crucial role in the individual perception of the psychological well-being.
Obstructive Sleep Apnea (OSA) syndrome is a clinical condition characterized by periodic reductions (i.e., hypopnea) or cessations (i.e., apnea) of airflow due to narrowing of the upper airway during sleep. Also, frequent awakenings, episodes of oxyhemoglobin desaturation, and fluctuations of heart-rate, systemic and pulmonary artery pressure are observed. Affected individuals generally report to suffering from excessive daytime sleepiness, sleep fragmentation, and drowsiness, together with decreased energy, reduced level of concentration and alertness, and overall cognitive difficulties (i.e., Akashiba et al., 2002; Zhou et al., 2016; Simões et al., 2018; Angelelli et al., 2020). Crucially, these symptoms impact negatively on individuals’ efficacy in daily-life activities, such as working, driving, social interaction, and they increase the risk of (work- or road-) accidents (Vaessen et al., 2015). Consequently, in OSA syndrome, individuals generally experience a lower level of psychological well-being (Ohayon, 2003; Naismith et al., 2004; Saunamäki and Jehkonen, 2007; Harris et al., 2009; Sanchez et al., 2009; Iacono Isidoro et al., 2013; Hobzova et al., 2017), because of their difficulties about having a good and restorative sleeping (Hamilton et al., 2007; Weinberg et al., 2016) or because of the associated cognitive difficulties (Llewellyn et al., 2008; Wilson et al., 2013). Higher levels of anxiety and depressive symptoms (i.e., Ohayon, 2003; Naismith et al., 2004; Saunamäki and Jehkonen, 2007; Harris et al., 2009; Sanchez et al., 2009; Hobzova et al., 2017) are also registered. However, some of these symptoms (especially those related to a depressive mood) seem to be more related to the degree of daytime sleepiness, that is an effect of the disease, than to the degree of nocturnal hypoxemia, which expresses the severity of the disease (Naismith et al., 2004; Karkoulias et al., 2013). Moreover, Iacono Isidoro et al. (2013) highlighted that some individual factors might play a crucial role in the subjective perception of the psychological impact of OSA syndrome symptoms on psychological well-being, in line with evidence about beliefs and coping strategies (Dodge et al., 2012) as well as personality traits (Ryff, 2014).
OSA syndrome occurs frequently in obesity, as well as obesity is a high-risk factor for the development and progression of sleep apnea, even though the mechanisms linking obesity to the development and progression of OSA syndrome is still unclear (Schwartz et al., 2008). Obesity is a complex, multifactorial disease that develops from the interaction of genetic, metabolic, social, behavioral, and cultural factors. Thus, it might be expected that OSA syndrome in the context of obesity impacts severely individuals’ health (Veale et al., 2002; Iacono Isidoro et al., 2013). However, as in our knowledge, no study has investigated psychological well-being in individuals with both OSA syndrome and obesity. Indeed, studies focusing on OSA syndrome did not generally assess the participants’ level of obesity (i.e., Saunamäki and Jehkonen, 2007), as well as those studies in which psychological well-being (i.e., Carr and Friedman, 2005; Dierk et al., 2006; Heo et al., 2006; Simon et al., 2006; Manzoni et al., 2010; Jackson et al., 2015) was investigated in the case of obesity, did not generally assess sleeping quality or respiratory distress.
The present work aimed to describe the level of psychological well-being in a sample of individuals affected by OSA syndrome and obesity. To this aim, we used the Psychological General Well Being Index (Dupuy, 1984): it scores the psychological well-being as resulting from the components of anxiety, depressed mood, positive well-being, self-control, general health, and vitality. Moreover, because of the previous evidence about the impact of sleeping quality, cognition, and personality on the individual perception of psychological well-being (i.e., Ryff, 2014; Hamilton et al., 2007; Llewellyn et al., 2008; Dodge et al., 2012; Wilson et al., 2013; Weinberg et al., 2016), we explored the predictive role of these components in our sample’s experience. We assessed sleeping efficacy quantitatively, performing polysomnography, and qualitatively, through traditional self-report questionnaires. Neuropsychological tests focusing on the global functioning were administered to our participants to assess the cognitive efficiency; moreover, we investigated attentional abilities through a computerized task (Mueller and Piper, 2014; Scarpina et al., 2020). Finally, we profiled our participants’ personality referring to Cloninger et al. (1993)’s model, which postulates four temperamental traits: (i) novelty seeking, that defines the tendency to respond actively to novel stimuli leading to pursue rewards and escape from punishment; (ii) harm avoidance, corresponding to the tendency toward an inhibitory response to signals of aversive stimuli that lead to avoidance of punishment and non-reward; (iii) reward dependence, that is the tendency for a positive response to signals of reward to maintain or resist behavioral extinction; and, (iv) persistence, represented by the tendency to persevere in behavior, despite fatigue or frustration. The model also postulates three types of character, meaning self-concepts and individual differences in goals and values: (i) self-directedness, that is the ability to control, regulate and adapt behavior to fit the situation in accordance with individually chosen goals and values; (ii) cooperativeness, that accounts for individual differences in identification with and acceptance of other people; and, (iii) self-transcendence, which refers generally to the identification with everything conceived as essential and consequential part of a united whole. In our study, we used the Temperament and Character Inventory (Cloninger et al., 1993) to describe the level of expression for each temperament and character in our sample.
This study was approved by the Ethics Committee of the I.R.C.C.S. Istituto Auxologico Italiano (Reference number: 21C924_2019). All participants were volunteers who gave informed written consent before participating in the study; they were free to withdraw at any time.
Fifty-two individuals (32 females; 20 males; mean age in years = 54.61; SD = 9.52; range = 34–75; mean education in years = 11.88; SD = 3.82; range = 5–23) participated at this study. They were in-patients consecutively recruited at their admission to the institute, before an intensive hospital-based and medically managed rehabilitation program for weight reduction. Individuals were included in this study if at the admission: (i) they were affected by obesity, meaning a body mass index (BMI, defined as weight in kilograms divided by height in meters squared) over the value of 30; and (ii) they reported symptoms that might be referred to the OSA syndrome, such as: snoring loud enough to disturb their own or relatives’ sleep; waking up gasping or choking; intermittent pauses in breathing during sleep; excessive daytime drowsiness, with falls asleep during working or daily life activities. We excluded individuals who used C-PAP currently or in the past. Also, we excluded: smokers; individuals with a history of alcohol abuse; individuals with a history of gastrointestinal, cardiovascular, psychiatric, neurological disorders or any concurrent medical condition not related to obesity.
Overall, our sample of participants reported a mean BMI of 44.99 kg/m2 (SD = 9.33; range = 24.97–59.14).
The Psychological General Well Being Index (PGWBI) (Dupuy, 1984; Grossi et al., 2006) was used to assess six dimensions (anxiety, depressed mood, positive well-being, self-control, general health, and vitality) of the psychological well-being. We profiled the temperament and the character of our sample through the Temperament and Character Inventory (TCI) (Cloninger et al., 1994; Martinotti et al., 2008). We assessed the participants’ global cognitive functioning through the Mini-Mental State Examination (Folstein et al., 1975; Magni et al., 1996), the Clock Drawing Test (Rouleau et al., 1992; Siciliano et al., 2016), and the Frontal Assessment Battery (Dubois et al., 2000; Appollonio et al., 2005). Also, the attentional resources and cognitive inhibition were measured through the Flanker’s Test from the PEBL Psychological Test Battery (Mueller and Piper, 2014; Scarpina et al., 2020).
Three questionnaires were used to rate the subjective perception of sleeping efficacy: the Epworth Sleepiness Scale (Johns, 1991; Manni et al., 1999) which focuses on the pathological daily sleepiness; the Pittsburgh Sleep Quality Index (Buysse et al., 2005; Curcio et al., 2013), which assesses sleep quality; and the Stanford Sleepiness Scale (Hoddes, 1972; Romigi et al., 2015), which quantifies the subjective level of alertness and sleepiness throughout the day. Finally, all participants underwent a full-night polysomnography, which is routinely performed in our institute (i.e., Zibetti et al., 2017). The Apnoea–Hypopnoea Index (AHI), computed according to the number of apnea and hypopnea events per hour of sleep, was used as index of sleep apnea severity. Following the standard criteria (Ruehland et al., 2009), a value below of the cut-off of 5 was considered in the range of normality; values between the range 5 ≤ AHI < 15 defined a mild sleep apnea; the range 15 ≤ AHI < 30, a moderate apnea; values of AHI ≥ 30 defined a severe apnea. Details about all the measurements are reported in the Supplementary Material.
Preliminary, psychological questionnaires and neuropsychological tests were scored accordingly to the seminal works and compared to the normative data. About the computerized test of PEBL Flanker’s Test (Mueller and Piper, 2014), we computed behavioral indexes suggesting the presence of attentional difficulties (Scarpina et al., 2020). For details, consult the Supplementary Material.
To describe the level of the psychological well-being in our sample, an independent sample t-test was performed for each subscale of the PGWBI in order to compare the scores reported by our sample and the normative score for the Italian population reported in Grossi et al. (2006).
Successively, we performed a linear regression analyses to verify the role of temperament, cognitive functioning, and sleep characteristics on the level of psychological well-being in our sample. Thus, we preliminary analyzed the correlation and directionality of the data to formulate the statistical model: the Spearman’s correlation coefficient was computed between the PGWBI total score and those factors which would be included in the statistical model, that were: (i) the demographical characteristics of Age and Education, as well as the BMI; (ii) the scores relative to the four temperamental traits from the Temperament and Character Inventory; (iii) the score at the neuropsychological tests (Mini Mental State Examination, Clock Drawing Test, Frontal Assessment Battery, and Flanker’s Test - RT index and Accuracy index); (iv) the polysomnographic components; and (v) the scores at the questionnaires of Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index and Stanford Sleepiness Scale. A nonparametric measure (i.e., the Spearman’s correlation) was used since most of the factors were not normally distributed, as usually observed in the case of questionnaires’ scores. Those factors significantly associated with the PGWBI total score (p ≤ 0.05) were further investigated with the linear regression model, about which we reported the R-squared as a goodness-of-fit measure; also, we evaluated the significance of the model through F-value and the p-value. Finally, we verified the relative contribution of the factors included in the statistical model with the independent variable (i.e., the PGWBI total score). About each of them, we reported the variance inflation factor (VIF) as measure of multicollinearity.
Further analyses focused on the OSA syndrome severity (Supplementary Table 1) and the obesity severity (Supplementary Table 2), as well as those analyses investigating possible differences in the individual factors between the different levels of OSA syndrome severity (Ruehland et al., 2009; Supplementary Table 3) are reported in the Supplementary Material.
In Table 1, mean, standard deviation, and range for all the measurements were reported.
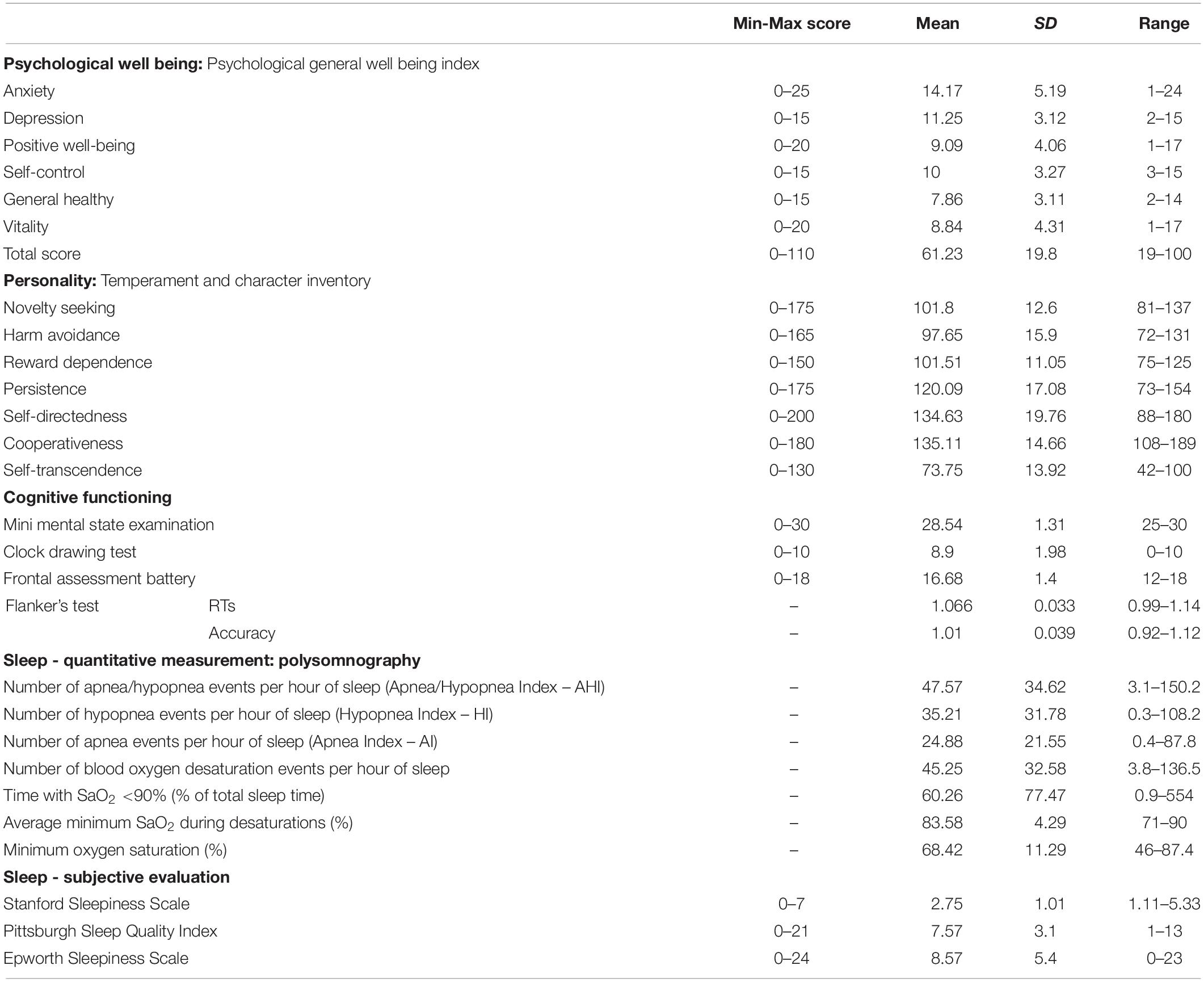
Table 1. Minimum (Min) and maximum (Max) score, mean, standard deviation (SD), and values range are reported for all the measurements.
Focusing on the PGWBI, in all subscales, except for the level of depression, our sample reported lower scores in comparison with the normative sample (N = 76; age range = 50–54) (Grossi et al., 2006), as show in Figure 1. Thus, as suggested by the global score, our sample described a lower level of psychological well-being.
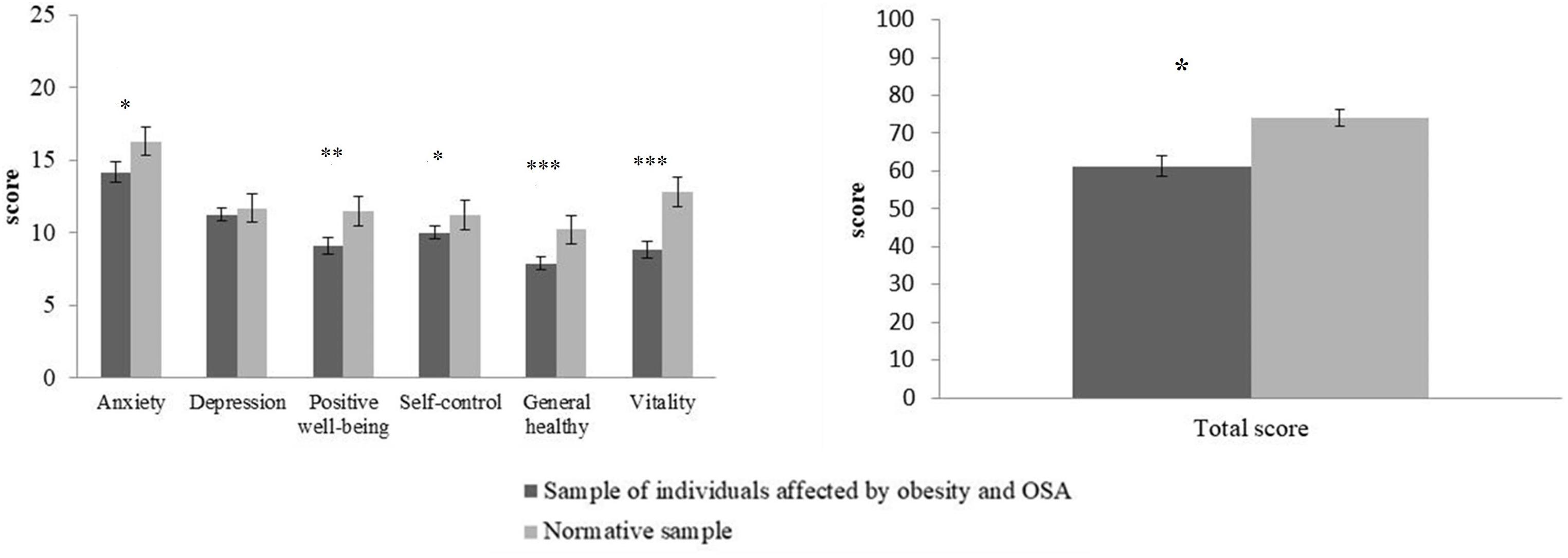
Figure 1. For each subscale (right panel) and the total score (left panel) relative to the Psychological General Well Being Index (Dupuy, 1984), mean (y axis) and standard deviation (vertical lines) are shown about the sample of individuals affected by OSA syndrome and obesity (dark gray bars) and the normative sample (light gray bars; data from Grossi et al., 2006).* indicates a p-value < 0.05; **p-value = 0.001; ***p-value < 0.001.
No significant relationship emerged between the PGWBI global score and the demographical characteristics of Age [ρ(52) = 0.05; p = 0.68] and Education [ρ(52) = 0.06; p = 0.66], or with the level of BMI [ρ(52) = −0.04; p = 0.75].
In Table 2, the results relative to the relationship between the PGWBI total score and the scores relative to the temperament, cognitive functioning, subjective perception and objective measurement of sleeping were reported.
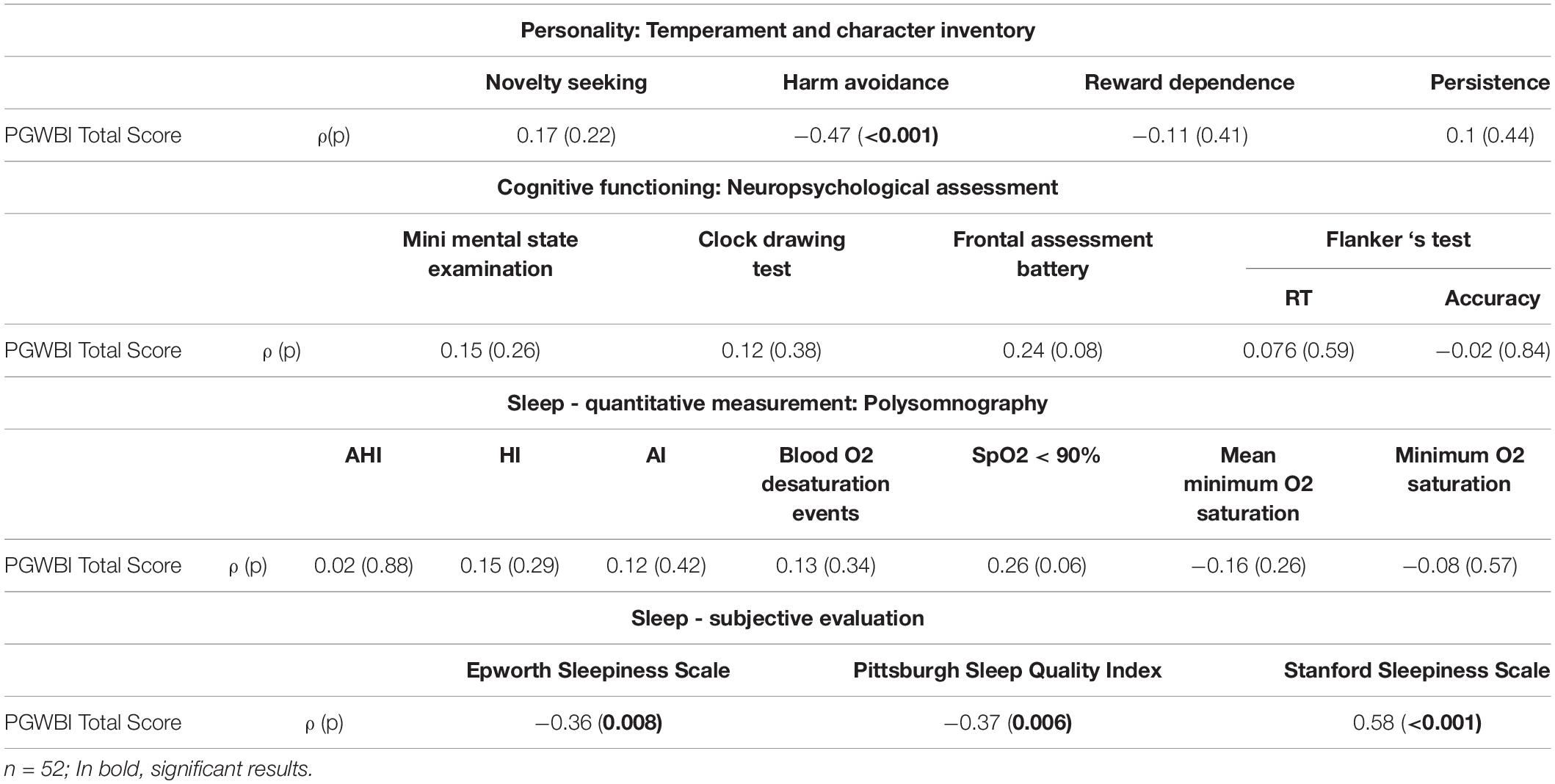
Table 2. Results relative to the relationship between the PGWBI total score and the scores relative to the personality (Temperament and Character Inventory), the cognitive functioning (the neuropsychological assessment), the objective assessment of sleeping (polysomnography) and the subjective sleeping functionality (sleep – subjective evaluation: questionnaires).
We observed a significant negative relationship only with the score relative to the harm avoidance temperament, while no significant relationship emerged with the scores relative to the other temperamental traits (p ≥ 0.22). Thus, those participants affected by OSA syndrome and obesity with a lower expression of harm avoidance temperament reported a higher level of psychological well-being. No significant relationship between the PGWBI total score and the scores relative to the neuropsychological tests emerged (p ≥ 0.08). However, the role of a possible ceiling effect, as suggested by the data reported in Table 1, should be considered. No significant relationship emerged with any of the neurophysiological parameters from the polysomnography (p ≥ 0.06). Instead, all the subjective measures about the sleep efficacy were significantly related to the PGWBI total score (p ≤ 0.008). Thus, in the linear regression model we included the scores relative to the subjective sleeping questionnaires (Epworth Sleepiness Scale, Pittsburgh Sleep Quality Index, and Stanford Sleepiness Scale) and the score relative to the harm avoidance temperament, as predictors of the PGWBI total score. According to the results reported in Table 3, a higher global score at PGWBI, suggesting a higher level of psychological well-being, was significantly predicted by a lower score relative to the harm avoidance temperament, and a lower perception of daily sleepiness measured through the Stanford Sleepiness Scale. The other factors included in the model were not statistically significant.
We aimed to describe the psychological well-being of individuals affected by OSA syndrome and obesity, and to assess the role of temperament, cognitive functioning, and subjective and objective sleeping efficacy on its perception.
We observed a lower level of psychological well-being, measured through the Psychological General Well Being Index (Dupuy, 1984), when our sample’s scores were compared with the Italian normative data (Grossi et al., 2006). This result seemed in agreement with Iacono Isidoro et al. (2013)’s study, in which the same questionnaire was used in the case of Italian individuals affected by OSA syndrome. The authors described their sample as suffering from moderate distress, since they reported a total score mean of 70.9 (SD = 16), ranging from 20 to 101, at the Psychological General Well Being Index (Dupuy, 1984). This score seemed to be higher in comparison with our sample’ score. However, it should be considered the role of obesity. Indeed, a level of BMI higher than 30 was an inclusion criterion in our study; according to the BMI range, individuals from severe obesity – Class II to very severe obesity – Class III (WHO, 1995) were included in our sample. Instead, Iacono Isidoro et al. (2013) did not specify the BMI as an inclusion/exclusion criterion in their study. As results, their sample’s BMI ranged from 17.3 to 57.8. Thus, not only individuals affected by different levels of obesity, but also individuals with healthy-weight as well as underweight individuals might have been included in the sample. Interestingly, we did not report any significant relationship between the level of psychological well-being and the level of obesity, as registered in other studies (i.e., Dierk et al., 2006; Manzoni et al., 2010; Iacono Isidoro et al., 2013), but in disagreement with other ones, in which psychological difficulties were reported to be higher for higher levels of obesity (i.e., Carr and Friedman, 2005; Heo et al., 2006; Simon et al., 2006; Jackson et al., 2015). Nevertheless, some cautions should be taken in confronting different studies, because the role played by social and cultural factors, which may, in turn, affect the perception of psychological well-being (Dierk et al., 2006). On the other hand, an ongoing debate is still in the literature about the meaningful and useful of the individual’s BMI as an index of level of obesity severity in the context of psychological and social studies (Schwartz and Brownell, 2004; Vieira et al., 2012). Our sample reported a lower score in almost all components of the Psychological General Well Being Index (Dupuy, 1984), except for the number of depressive symptoms, about which we observed a score in line with the normative sample (Grossi et al., 2006). This result seemed in agreement with previous evidence, such as Pillar and Lavie (1998), but in disagreement with other ones (i.e., Harris et al., 2009) about OSA syndrome and depression. Nevertheless, it should be considered that some of the symptoms typically observed in this clinical condition, such as physical fatigue, cognitive slowness and memory loss, headaches, restless sleep, mood changes, decreased sexual interest, may resemble symptoms associated with the depressive condition, challenging clinicians in diagnosing the presence of the psychiatric disease (Harris et al., 2009).
In our study, we also registered that a lower level of daily sleepiness and a lower expression of harm avoidance temperament predicted a higher level of psychological well-being in individuals affected by OSA syndrome and obesity. About the first component, our results, which relied on the score reported by participants at the Stanford Sleepiness Scale (Hoddes, 1972), were globally in line with the Iacono Isidoro et al. (2013): the authors observed that higher scores registered at the Epworth Sleepiness Scale (Johns, 1991), were related to the lower level of psychological well-being, as registered in our analyses. However, the authors did not report statistical results about the predictive role of the score at the Epworth Sleepiness Scale on the PGWBI score. Moreover, Iacono Isidoro et al. (2013) reported that the AHI index from the polysomnography, which represents an objective measurement about sleep quality and efficacy, did not predict the subjective perception of the psychological well-being, in line with our results. Also, our results and those provided by Iacono Isidoro et al. (2013) were in agreement in reporting no difference in the psychological well-being between different levels of sleep apnea severity (Ruehland et al., 2009). Finally, we also observed no significant relationship between the scores relative to the three questionnaires - measuring the subjective perception of daily sleeping and sleeping efficacy – and the Apnea/Hypopnea Index registered in the polysomnography (see Supplementary Material). Overall, all these results seem to confirm that lower psychological well-being might be not strictly related to the OSA severity. Instead, how individuals perceive the impact of syndrome on their sleeping and daily functioning may play a significantly crucial role. Thus, in this vein, objective measurements about sleeping quality, as reported in the present study as well as in Iacono Isidoro et al. (2013), might be mandatory not only when individuals spontaneously recognize and report to suffer from daily sleeping and decreased alertness, suggesting possibly OSA syndrome, but also in all these conditions in which such difficulties might emerge due to other clinical conditions, such as obesity.
The second component that predicted higher levels of psychological well-being was a lower level of harm avoidance. In other words, those affected individuals showing a carefree, courageous, and optimistic way to approach their health-related condition, might experience a higher level of psychological well-being. Within the sample, we observed that the majority of our participants reported a higher score in the scale relative to the persistence trait, although the other three temperamental traits seemed to be under-expressed. It was reported that a high level of persistence may play a protective effect on the emotional functioning, reducing negative emotions and increasing positive ones, especially in the case of lower expressions of harm avoidance (Cloninger et al., 2012). We assessed our participants before to start an intensive hospital-based and medically managed rehabilitation program for weight reduction. This medical choice may be embraced especially by those individuals who are highly persistent despite the perceived distress and more prone to pro-health activities. Also, it may depend on external solicitations, such as general practitioners and/or relatives, suggesting a rewards-dependent temperament. Nevertheless, about the high expression of persistence, “its value depends on a complex set of adaptive processes, both internal and external, and how well these forces that push and pull on the person are integrated and balanced. Being highly persistent is likely to lead to intense mixtures of positive and negative emotions, which can lead to high achievement, much anxiety, or both” (Cloninger et al., 2012; p. 8). Indeed, our participants reported higher levels of anxious (and not of depressive) symptoms: this result, which was in line with previous evidence (Saunamäki and Jehkonen, 2007; Gupta and Simpson, 2015), might be related to the higher expression of the persistence as temperamental trait. As in our knowledge, two previous studies (Sforza et al., 2002; Fìdan et al., 2013) described the personality according to Cloninger et al. (1993)’s model in individuals affected by OSA syndrome. Other studies described personality in individuals affected by this syndrome referring to other psychological models, such as the Eysenck and Eysenck (1975)’ model in So et al. (2015), and the behavioral inhibition system/behavioral activation system (BIS/BAS) model (Carver and White, 1994) in Moran et al. (2011). The two studies in which Cloninger et al. (1993)’s model was used reported heterogeneous results: Sforza et al. (2002) observed that individuals with OSA syndrome mostly showed a higher expression of novelty-seeking behavior in comparison with healthy adults, but no difference emerged in comparison with snoring individuals; instead, Fìdan et al. (2013) registered no difference in the four temperamental traits between individuals affected by OSA syndrome and healthy individuals. However, focusing on the obesity, we might observe that Sforza et al. (2002) assessed individuals with a level of BMI of 30.4 (SD = 0.7); similarly, Fìdan et al. (2013) reported a level of BMI of 30.9 (SD = 4.9) about their sample. Thus, in both these studies, individuals with low-risk obesity were assessed. Instead, we enrolled individuals with high-risk obesity.
In our work, we performed a global assessment of cognitive functioning. Our sample did not show pervasive cognitive difficulties or dementia. However, as reported in the Supplementary Material, we verified the presence of attentional difficulties, in accordance with previous evidence (Akashiba et al., 2002; Vaessen et al., 2015; Zhou et al., 2016; Simões et al., 2018; Angelelli et al., 2020) about OSA syndrome. It is worthy to note that overall cognitive difficulties were not assessed extensively in the literature. However, we would emphasize the importance to adopt neuropsychological tests to measure cognitive functioning, since a mismatch between the subjective perception (i.e., an efficient attentional functioning in daily-life) and the objective assessment (i.e., lower attentional capabilities measured through neuropsychological tests) might be observed.
In this article, we described the level of psychological well-being in the case of OSA syndrome and obesity, which was found to be severely decreased in the assessed sample. Specifically, we reported that the temperament and the subjective perception of daily alertness and sleepiness, rather than the syndrome severity, seemed to play a crucial role in the individual perception of the psychological well-being. However, since we performed an observational cross-sectional study, we cannot furnish any conclusive information about the relationship between OSA syndrome and obesity, as well as their specific role on the individuals’ psychological well-being perception. Indeed, to this aim, future studies in which different levels of obesity will be compared with healthy-weight condition with and without OSA syndrome should be performed. Moreover, it should be considered that in our study, because of the clinical procedure described in the Supplementary Material, participants were enrolled based on the suspicion of OSA syndrome according to the subjective symptoms, rather than its objective diagnosis, which grounds on the AHI registered at the polysomnography, Our findings might extend our understanding about how personality, subjective and objective measures of sleep quality, and cognitive functioning interact with the psychological well-being of affected individuals.
The datasets presented in this article are not readily available because the data are restricted according to the Ethical Commission’s indications. Requests to access the datasets should be directed to corresponding author (FS).
The studies involving human participants were reviewed and approved by the IRCCS Istituto Auxologico Italiano. The patients/participants provided their written informed consent to participate in this study.
FS and AM conceived the study. FS supervised the entire study, performed the statistical analyses, and wrote the manuscript. IB and SC performed the data collection. LP, EG, IMAT, and MC selected the participants and performed the clinical assessment. GC and EM supervised the psychological assessment. PF and AM supervised the clinical assessment. All authors revised the manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2021.588767/full#supplementary-material
Supplementary Figure 1 | About the Stanford Sleepiness Scale, we report mean and standard deviation for each time hour; vertical lines represent standard deviation. a.m., ante meridiem; p.m., post meridiem.
Supplementary Figure 2 | About the Flanker’s Test, we report mean and standard error (vertical lines) for each experimental condition (x-axis) for the Reaction Time (RT) expressed in milliseconds (left panel) and the Accuracy in percentage (right panel). * indicates a significant difference (p < 0.05), according to the post hoc analyses.
Supplementary Table 1 | The relationship between the AHI index and BMI, the scores relative to the personality (i.e., Temperament and Character Inventory), cognitive functioning (i.e., neuropsychological tests), and the subjective characteristics (self-report questionnaires) about sleeping; n = 52.
Supplementary Table 2 | The relationship between the BMI and the scores relative to the personality (i.e., Temperament and Character Inventory), cognitive functioning (i.e., neuropsychological tests), and the subjective characteristics (self-report questionnaires) about sleeping. We report again the relationship with the AHI index, as shown in Supplementary Table 1. n = 52. In bold, significant relationships.
Supplementary Table 3 | Mean and standard deviation (SD) for each assessed factors are reported for the different levels of sleep apnea, along with the statistical results.
Akashiba, T., Kawahara, S., Akahoshi, T., Chiharu, O., Osamu, S., Tohru, M., et al. (2002). Relationship between quality of life and mood or depression in patients with severe obstructive sleep apnea syndrome. Chest 122, 861–865. doi: 10.1378/chest.122.3.861
Angelelli, P., Macchitella, L., Toraldo, D. M., Abbate, E., Marinelli, C. V., Arigliani, M., et al. (2020). The neuropsychological profile of attention deficits of patients with obstructive sleep apnea: an update on the daytime attentional impairment. Brain Sci. 10:325. doi: 10.3390/brainsci10060325
Appollonio, I., Leone, M., Isella, V., Piamarta, F., Consoli, T., Villa, M. L., et al. (2005). The frontal assessment battery (FAB): normative values in an Italian population sample. Neurol. Sci. 26, 108–116. doi: 10.1007/s10072-005-0443-4
Buysse, D. J., Germain, A., Moul, D., and Nofzinger, E. A. (2005). “Insomnia,” in Sleep Disorders and Psychiatry, ed. D. J. Buysse (Arlington: American Psychiatric Publishing Inc), 29–75. doi: 10.2307/j.ctt5hjqd5.18
Carr, D. S., and Friedman, M. A. (2005). Is obesity stigmatizing? Body weight, perceived discrimination, and psychological well-being in the United States. J. Health Soc. Behav. 46, 244–259. doi: 10.1177/002214650504600303
Carver, C. S., and White, T. L. (1994). Behavioral-inhibition, behavioral activation, and affective responses to impending reward and punishment—the BIS BAS scales. J. Pers. Soc. Psychol. 67, 319–333. doi: 10.1037/0022-3514.67.2.319
Cloninger, C. R., Przybeck, T. R., Svrakic, D. M., and Wetzel, R. D. (1994). The Temperament and Character Inventory (TCI) a Guide to its Development and use. St Louis, MO: Washington University.
Cloninger, C. R., Svrakic, D. M., and Przybeck, T. R. (1993). A psychobiological model of temperament and character. Arch. Gen. Psychiatry 50, 975–990. doi: 10.1001/archpsyc.1993.01820240059008
Cloninger, C. R., Zohar, A. H., Hirschmann, S., and Dahan, D. (2012). The psychological costs and benefits of being highly persistent: personality profiles distinguish mood disorders from anxiety disorders. J. Affect. Disord. 136, 758–766. doi: 10.1016/j.jad.2011.09.046
Curcio, G., Tempesta, D., Scarlata, S., Marzano, C., Moroni, F., Rossini, P. M., et al. (2013). Validity of the Italian version of the pittsburgh sleep quality index (PSQI). Neurol. Sci. 34, 511–519. doi: 10.1007/s10072-012-1085-y
Dierk, J. M., Conradt, M., Rauh, E., Schlumberger, P., Hebebrand, J., and Rief, W. (2006). What determines well-being in obesity? Associations with BMI, social skills, and social support. J. Psychosom. Res. 60, 219–227. doi: 10.1016/j.jpsychores.2005.06.083
Dodge, R., Daly, A., Huyton, J., and Sanders, L. (2012). The challenge of defining wellbeing. Int. J. Wellbeing 2, 222–235. doi: 10.5502/ijw.v2i3.4
Dubois, B., Slachevsky, A., Litvan, I., and Pillon, B. (2000). The FAB: a frontal assessment battery at bedside. Neurology 55, 1621–1626. doi: 10.1212/wnl.55.11.1621
Dupuy, H. J. (1984). “The psychological general well-being (PGWB) Index,” in Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies, ed. N. Wenger (New York, NY: Le Jacq), 170–183.
Eysenck, H. Y., and Eysenck, S. B. (1975). Manual of the Eysenck Personality Questionnaire. London: Hodder and Stoughton.
Fìdan, F., Ozbulut, O., Aycicek, A., Hakki Asik, A., and Unlu, E. (2013). Effects of obstructive sleep apnea syndrome on temperament and character. Turk. J. Med. Sci 43, 138–143. doi: 10.3906/sag-1206-65
Folstein, M. F., Folstein, S. E., and McHugh, P. R. (1975). “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J. Psychiatr. Res. 12, 189–198. doi: 10.1016/0022-3956(75)90026-6
Grossi, E., Groth, N., Mosconi, P., Cerutti, R., Pace, F., Compare, A., et al. (2006). Development and validation of the short version of the psychological general well-being index (PGWB-S). Health Qual. Life Out. 4:88. doi: 10.1186/1477-7525-4-88
Gupta, M. A., and Simpson, F. C. (2015). Obstructive sleep apnea and psychiatric disorders: a systematic review. J. Clin. Sleep Med. 11, 165–175. doi: 10.5664/jcsm.4466
Hamilton, N. A., Gallagher, M. W., Preacher, K. J., Stevens, N., Nelson, C. A., Karlson, C., et al. (2007). Insomnia and well-being. J. Consult. Clin. Psychol. 75, 939–946. doi: 10.1037/0022-006X.75.6.939
Harris, M., Glozier, N., Ratnavadivel, R., and Grunstein, R. R. (2009). Obstructive sleep apnea and depression. Sleep Med. Rev. 13, 437–444. doi: 10.1016/j.smrv.2009.04.001
Heo, M., Pietrobelli, A., Fontaine, K. R., Sirey, J. A., and Faith, M. S. (2006). Depressive mood and obesity in US adults: comparison and moderation by age, sex, and race. Inter. J. Ob. 30, 513–519. doi: 10.1038/sj.ijo.0803122
Hobzova, M., Prasko, J., Vanek, J., Ociskova, M., Genzor, S., Holubova, M., et al. (2017). Depression and obstructive sleep apnea. Neuro Endocrinol. Lett. 38, 343–352.
Hoddes, E. (1972). The development and use of the stanford sleepiness scale (SSS). Psychophysiology 9:150.
Iacono Isidoro, S., Salvaggio, A., Lo Bue, A., Romano, S., Marrone, O., and Insalaco, G. (2013). Quality of life in patients at first time visit for sleep disorders of breathing at a sleep centre. Health Qual. Life Out. 11:207. doi: 10.1186/1477-7525-11-207
Jackson, S. E., Beeken, R. J., and Wardle, J. (2015). Obesity, perceived weight discrimination, and psychological well-being in older adults in England. Obesity 23, 1105–1111. doi: 10.1002/oby.21052
Johns, M. W. (1991). A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14, 540–545. doi: 10.1093/sleep/14.6.540
Karkoulias, K., Lykouras, D., Samsonas, F., Karaivazoglou, K., Sargianou, M., Drakatos, P., et al. (2013). The impact of obstructive sleep apnea syndrome severity on physical performance and mental health. The use of SF-36 questionnaire in sleep apnea. Eur. Rev. Med. Pharmacol. Sci. 17, 531–553.
Llewellyn, D. J., Lang, I. A., Langa, K. M., and Huppert, F. A. (2008). Cognitive function and psychological well-being: findings from a population-based cohort. Age Ageing 37, 685–689. doi: 10.1093/ageing/afn194
Magni, E., Binetti, G., Bianchetti, A., Rozzini, R., and Trabucchi, M. (1996). Mini-Mental State Examination: a normative study in Italian elderly population. Eur. J. Neurol. 3, 198–202. doi: 10.1111/j.1468-1331.1996.tb00423.x
Manni, R., Politini, L., Ratti, M. T., and Tartara, A. (1999). Sleepiness in obstructive sleep apnea syndrome and simple snoring evaluated by the Epworth Sleepiness Scale. J. Sleep Res. 8, 319–320. doi: 10.1046/j.1365-2869.1999.00166.x
Manzoni, G. M., Cribbie, R. A., Villa, V., Arpin-Cribbie, C. A., Gondoni, L., and Castelnuovo, G. (2010). Psychological well-being in obese inpatients with ischemic heart disease at entry and at discharge from a four-week cardiac rehabilitation program. Front. Psychol. 1:38. doi: 10.3389/fpsyg.2010.00038
Martinotti, G., Mandelli, L., Di Nicola, M., Serretti, A., Fossati, A., Borroni, S., et al. (2008). Psychometric characteristic of the Italian version of the temperament and character inventory–revised, personality, psychopathology, and attachment styles. Compr. Psychiatry 49, 514–522. doi: 10.1016/j.comppsych.2007.11.002
Moran, A. M., Everhart, D. E., Davis, C. E., Wuensch, K. L., Lee, D. O., and Demaree, H. A. (2011). Personality correlates of adherence with continuous positive airway pressure (CPAP). Sleep Breath 15, 687–694. doi: 10.1007/s11325-010-0422-8
Mueller, S. T., and Piper, B. J. (2014). The psychology experiment building language (PEBL) and PEBL test battery. J. Neurosci. Methods 222, 250–259. doi: 10.1016/j.jneumeth.2013.10.024
Naismith, S., Winter, V., Gotsopoulos, H., Hickie, I., and Cistulli, P. (2004). Neurobehavioral functioning in obstructive sleep apnea: differential effects of sleep quality, hypoxemia and subjective sleepiness. J. Clin. Exp. Neuropsychol. 26, 43–54. doi: 10.1076/jcen.26.1.43.23929
Ohayon, M. M. (2003). The effects of breathing-related sleep disorders on mood disturbances in the general population. J. Clin. Psychiatry 64, 1195–1200. doi: 10.4088/jcp.v64n1009
Pillar, G., and Lavie, P. (1998). Psychiatric symptoms in sleep apnea syndrome: effects of gender and respiratory disturbance index. Chest 114, 697–703. doi: 10.1378/chest.114.3.697
Romigi, A., Pierantozzi, M., Placidi, F., Evangelista, E., Albanese, M., Liguori, C., et al. (2015). Restless legs syndrome and post polio syndrome: a case-control study. Eur. J. Neurol. 22, 472–478. doi: 10.1111/ene.12593
Rouleau, I., Salmon, D. P., Butters, N., Kennedy, C., and McGuire, K. (1992). Quantitative and qualitative analyses of clock drawings in Alzheimer’s and Huntington’s disease. Brain Cogn. 18, 70–87. doi: 10.1016/0278-2626(92)90112-Y
Ruehland, W. R., Rochford, P. D., O’Donoghue, F. J., Pierce, R. J., Singh, P., and Thornton, A. T. (2009). The new AASM criteria for scoring hypopneas: impact on the apnea hypopnea index. Sleep 32, 150–157. doi: 10.1093/sleep/32.2.150
Ryff, C. D. (2014). Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother. Psychosom. 83, 10–28. doi: 10.1159/000353263
Sanchez, A. I., Martnez, P., Miro, E., Baedwell, W. A., and Buela-Casal, G. (2009). CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med. Rev. 13, 223–233. doi: 10.1016/j.smrv.2008.07.002
Saunamäki, T., and Jehkonen, M. (2007). Depression and anxiety in obstructive sleep apnea syndrome: a review. Acta Psychol. Scand. 116, 277–288. doi: 10.1111/j.1600-0404.2007.00901.x
Scarpina, F., D’Agata, F., Priano, L., and Mauro, A. (2020). Difference between young and old adults’ performance on the psychology experiment building language (PEBL) test battery: what is the role of familiarity with technology in cognitive performance? Assessment 21:1073191120918010. doi: 10.1177/1073191120918010
Schwartz, A. R., Patil, S. P., Laffan, A. M., Vsevolod Polotsky, V., Schneider, H., and Smith, P. L. (2008). Obesity and obstructive sleep apnea: pathogenic mechanisms and therapeutic approaches. Proc. Am. Thorac. Soc. 5, 185–192. doi: 10.1513/pats.200708-137MG
Schwartz, M. B., and Brownell, K. D. (2004). Obesity and body image. Body Image 1, 43–56. doi: 10.1016/S1740-1445(03)00007-X
Sforza, E., de Saint Hilaire, Z., Pelissolo, A., Rochat, T., and Ibanez, V. (2002). Personality, anxiety and mood traits in patients with sleep-related breathing disorders: effect of reduced daytime alertness. Sleep Med. 3, 139–145. doi: 10.1016/s1389-9457(01)00128-9
Siciliano, M., Santangelo, G., D’Iorio, A., Basile, A., Piscopo, F., Grossi, D., et al. (2016). Rouleau version of the clock drawing test: age- and education-adjusted normative data from a wide Italian sample. Clin. Neuropsychol. 30, 1501–1516. doi: 10.1080/13854046.2016.1241893
Simões, E. N., Padilla, C. S., Bezerra, M. S., and Schmidt, S. L. (2018). Analysis of attention subdomains in obstructive sleep apnea patients. Front. Psychiatr. 9:435. doi: 10.3389/fpsyt.2018.00435
Simon, G. E., Von Korff, M., Saunders, K., Miglioretti, D. L., Crane, P. K., Van Belle, G., et al. (2006). Association between obesity and psychiatric disorders in the US adult population. Arch. Gen. Psychiatry 63, 824–830. doi: 10.1001/archpsyc.63.7.824
So, S. J., Lee, H. J., Kang, S. G., Cho, C. H., Yoon, H. K., and Kim, L. (2015). A comparison of personality characteristics and psychiatric symptomatology between upper airway resistance syndrome and obstructive sleep apnea syndrome. Psychiatry Investig 12, 183–189. doi: 10.4306/pi.2015.12.2.183
Vaessen, T. J., Overeem, S., and Sitskoorn, M. M. (2015). Cognitive complaints in obstructive sleep apnea. Sleep Med. Rev. 19, 51–58. doi: 10.1016/j.smrv.2014.03.008
Veale, D., Poussin, G., Pépin, J. L., and Levy, P. (2002). Identification of quality of life concerns of patients with obstructive sleep apnoea at the time of initiation of continuous positive airway pressure: a discourse analysis. Qual. Life Res. 11, 389–399. doi: 10.1023/a:1015599326110
Vieira, P. N., Palmeira, A. L., Mata, J., Kolotkin, R. L., Silva, M. N., Sardinha, L. B., et al. (2012). Usefulness of standard BMI cut-offs for quality of life and psychological well-being in women. Obes Facts 5, 795–805. doi: 10.1159/000345778
Weinberg, M. K., Noble, J. M., and Hammond, T. G. (2016). Sleep well feel well: An investigation into the protective value of sleep quality on subjective well-being. Aust. J. Psychol. 68, 91–97. doi: 10.1111/ajpy.12098
WHO (1995). Physical Status: The Use and Interpretation of Anthropometry: Report of a World Health Organization (WHO) Expert Committee. Geneva: World Health Organization.
Wilson, R. S., Boyle, P. A., Segawa, E., Yu, L., Begeny, C. T., Anagnos, S. E., et al. (2013). The influence of cognitive decline on well-being in old age. Psychol. Aging 28, 304–313. doi: 10.1037/a0031196
Zhou, J., Camacho, M., Tang, X., and Kushida, C. A. (2016). A review of neurocognitive function and obstructive sleep apnea with or without daytime sleepiness. Sleep Med. 23, 99–108. doi: 10.1016/j.sleep.2016.02.008
Keywords: cognition, psychological well-being, temperament, sleep, obesity, OSA syndrome
Citation: Scarpina F, Bastoni I, Cappelli S, Priano L, Giacomotti E, Castelnuovo G, Molinari E, Tovaglieri IMA, Cornacchia M, Fanari P and Mauro A (2021) Psychological Well-Being in Obstructive Sleep Apnea Syndrome Associated With Obesity: The Relationship With Personality, Cognitive Functioning, and Subjective and Objective Sleep Quality. Front. Psychol. 12:588767. doi: 10.3389/fpsyg.2021.588767
Received: 29 July 2020; Accepted: 01 February 2021;
Published: 19 February 2021.
Edited by:
Edward Callus, University of Milan, ItalyReviewed by:
Sandra Torres, University of Porto, PortugalCopyright © 2021 Scarpina, Bastoni, Cappelli, Priano, Giacomotti, Castelnuovo, Molinari, Tovaglieri, Cornacchia, Fanari and Mauro. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Federica Scarpina, Zi5zY2FycGluYUBhdXhvbG9naWNvLml0; ZmVkZXJpY2Euc2NhcnBpbmFAdW5pdG8uaXQ=; Lorenzo Priano, TG9yZW56by5wcmlhbm9AdW5pdG8uaXQ=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.