
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 09 November 2020
Sec. Psychology for Clinical Settings
Volume 11 - 2020 | https://doi.org/10.3389/fpsyg.2020.574475
This article is part of the Research Topic Coronavirus Disease (COVID-19): Psychological, Behavioral, Interpersonal Effects, and Clinical Implications for Health Systems View all 204 articles
 Christian Franceschini1*
Christian Franceschini1* Alessandro Musetti2
Alessandro Musetti2 Corrado Zenesini3
Corrado Zenesini3 Laura Palagini4
Laura Palagini4 Serena Scarpelli5
Serena Scarpelli5 Maria Catena Quattropani6
Maria Catena Quattropani6 Vittorio Lenzo6
Vittorio Lenzo6 Maria Francesca Freda7
Maria Francesca Freda7 Daniela Lemmo7
Daniela Lemmo7 Elena Vegni8
Elena Vegni8 Lidia Borghi8
Lidia Borghi8 Emanuela Saita9
Emanuela Saita9 Roberto Cattivelli9,10
Roberto Cattivelli9,10 Luigi De Gennaro5
Luigi De Gennaro5 Giuseppe Plazzi3,11
Giuseppe Plazzi3,11 Dieter Riemann12
Dieter Riemann12 Gianluca Castelnuovo9,10
Gianluca Castelnuovo9,10Background: Coronavirus disease 2019 (COVID-19) seriously affected the whole of Italy. The extreme virulence and the speed of propagation resulted in restrictions and home confinement. This change was immediately perceived by people who found themselves exposed to feelings of uncertainty, fear, anger, stress, and a drastic change in the diurnal but above all nocturnal lifestyle. For these reasons, we aimed to study the quality of sleep and its connection to distress levels and to evaluate how lifestyle changed in the Italian population during the lockdown.
Methods: By means of an Internet survey we recruited 6,519 adults during the whole of the COVID-19 lockdown (from March 10–1st phase to May 4–2nd phase). We investigated the sociodemographic and COVID-19-related information and assessed sleep quality using the Medical Outcomes Study–sleep scale (MOS-SS) and mental health with the short form of Depression, Anxiety, and Stress Scales–21 Items (DASS-21). Multiple logistic regression model was used to evaluate the multivariate association between the dependent variable (good sleeper vs. poor sleeper) and all the variables that were significant in the univariate analysis.
Results: A total of 3,562 (55.32%) participants reported poor sleep quality according to the MOS-Sleep Index II score. The multiple binary logistic regression results of poor sleepers revealed several risk factors during the outbreak restrictions: female gender, living in Central Italy, having someone close who died because of COVID-19, markedly changed sleep–wake rhythms characterized by earlier or postponed habitual bedtime, earlier habitual awakening time and reduced number of afternoon naps, and extremely severe levels of stress, anxiety, and depression.
Conclusion: This is the first study designed to understand sleep quality and sleep habits during the whole of the lockdown period in the Italian population that provides more than 6,000 participants in a survey developed specifically for the health emergency related to COVID-19. Our study found that more than half of the Italian population had impaired sleep quality and sleep habits due to elevated psychological distress during the COVID-19 lockdown containment measures. A multidisciplinary action should be undertaken in order to plan appropriate responses to the current crisis caused by the lockdown for the COVID-19 outbreak.
Coronavirus disease 2019 (COVID-19) was first identified as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in December 2019 by healthcare professionals in Wuhan City (China). Since then, it has spread rapidly throughout Hubei Province and other areas in China soon becoming a worldwide health problem affecting over 100 nations. During the same period, the World Health Organization indicated “COVID-19” as the official name to refer to the severe acute respiratory syndrome caused by SARS-CoV-2 (World Health Organization, 2020). Italy was the most seriously impacted country in Europe.
The Italian prime minister introduced the “I stay home” government decree (Italian Ministry of Health, 2020), which concerned the entire country and formally ordered people to stay at home. Travel restrictions, lockdown of schools and workplaces were the key measures of the “I stay home” decree together with the use of protective devices.
It is beyond doubt that this decision helped to prevent the further spread of the virus and was a necessary imposition to limit the number of patients being admitted to hospital. Nevertheless, from a psychological point of view, people undergoing this first form of intervention were exposed to feelings of uncertainty, fear, anger, and frustration that may easily lead to anxiety, boredom, and/or uneasiness (Brooks et al., 2020; De Giorgio, 2020; Holmes et al., 2020; Rubin and Wessely, 2020; Wang et al., 2020a).
This new situation where people were forced to manage work or study at home, with all the burden of worries stemming from almost inevitable health risks and social distancing, has had a strong impact on daily functioning and night-time sleep (Altena et al., 2020).
Sleep and stress have been described in a bidirectional relationship across the life span (Lo Martire et al., 2019) with stressors impacting on sleep quality and vice versa. In particular, high levels of cognitive and physiological arousal in response to stressors have been hypothesized to interfere with sleep according to the hyperarousal model of insomnia within the framework of a self-reinforcing loop (Morin et al., 1993, 2002; Harvey, 2002; Morin and Espie, 2003; Harvey et al., 2005, 2014; Bonnet and Arand, 2010; Riemann et al., 2010, 2015). In this difficult period, vigilance was constantly high: feelings of loss, excessive use of the Internet to seek information or to maintain social relationships, worries about getting infected, impulsive decisions, and rigid expectations were just some of the factors that could have interfered with a good sleep quality in the Italian population. Moreover, quarantine could have reduced the daylight exposure, which is essential for synchronizing the circadian body clock, consequently affecting many processes including sleep and mood (McClung, 2013; Vadnie and McClung, 2017). Hence, the current study aimed to investigate the quality of sleep and the lifestyle changes in the Italian population during the lockdown imposed by the “I stay home” decree-law issued by the Italian government (March 10) to its end (May 4–the so-called 2nd phase) expecting to find disrupted sleep.
In addition, since sleep quality is well known as being a crucial element of psychological health and a disturbed sleep has been related to psychopathology (Hertenstein et al., 2019), we wanted to study levels of anxiety, depression, and stress in the Italian population in relation to the quality of sleep experienced during the lockdown.
We conducted a cross-sectional study using a short sociodemographic and COVID-19-related information chart and self-administered questionnaire delivered by means of an Internet survey. Data were collected from the issue of the “I stay home” Italian government decree-law (“1st phase” –total lockdown) on March 10 to May 4, 2020 (“2nd phase” –end of lockdown).
This study was conducted in accordance with the Declaration of Helsinki, and the study protocol was approved by the Ethics Committee of the Center for Research and Psychological Intervention (CERIP) of the University of Messina. Electronic informed consent was obtained from each participant prior to starting the investigation. Participants could withdraw from the survey at any moment without needing to provide a reason.
The data were collected through an online survey (conducted with Microsoft Azure). On the Microsoft Azure platform, information and consent to the processing of personal data were prepared, and furthermore, consent was requested to provide an email contact; the subject was asked to create an identification code in order to anonymize it. Only after expressing consent the URL of the Google Form (Google Form) was available, and the subject needed to affix the identification code previously created to secure anonymity for all the partners and collaborators involved in this multicenter project. Questionnaires were created on the Google Cloud platform, which was anonymous. The survey study was advertised via university communication systems as well as online forums (e.g., through virtual learning environments and Facebook accounts) or WeChat groups. Our questionnaire was set to proceed only when each option was completed before the final submission.
The study surveyed a convenience sample of 6,519 adults from 18 years old or above who lived in Italy and were recruited via notices in several Italian universities (University of Parma; University of Messina; Catholic University of Milan; University of Milan, La Statale; University of Napoli, Federico II). People who do not live in Italy or participants who do not complete all the questionnaires were excluded (n = 43 and n = 37, respectively).
Data reported in the current study were part of a wider project called “Resilience and the COVID-19: how to react to perceived stress. Effects on sleep quality and diurnal behavior/thoughts.” This multipurpose project was designed to investigate the impact of lockdown in the Italian population.
The variables examined in the sociodemographic section included gender, age, marital status (single or not), education level (secondary education or higher), occupation (employed or unemployed), region of origin, and general information about family and home (having or not children, number of people living in the house, size of the house, presence/absence of garden or balcony).
According to the Italian Institute of Statistics (ISTAT), the Italian territory can be divided into three macro-areas: North (1): Valle D’Aosta, Piedmont, Lombardy, Liguria, Emilia Romagna, Friuli-Venezia Giulia, Trentino-Alto Adige, Veneto; Center (2): Lazio, Marche, Tuscany and Umbria; South (3) Abruzzo, Molise, Campania, Apulia, Basilicata, Calabria, Sardinia, and Sicily.
This section assessed information on participants’ employment data and any changes that occurred following the onset of the lockdown due to the COVID-19 pandemic: occupation, presence/absence of public contacts on workplace, working or not after the onset of COVID-19 pandemic, and information about work changes (at the office or smart working; number of hours: increased/reduced or loss of work).
The classification of occupations is based on an official list (“Nomenclatura e Classificazione delle Unità Professionali–CP2011, ISTAT). Moreover, we added the following categories: unemployed or job-seekers; retired persons; working students or not, and last, we extrapolated the health professions from the ISTAT categories.
We collected data about participants and their relatives/friends’ possible COVID-19 contacts/infection and the effects that the new emergency had on their social relationships (decreases/improvements of face-to-face or online contacts) with ad hoc items according to the Chinese findings (Wang et al., 2020b; Zhang et al., 2020): positivity or not to the COVID-19 virus, having been forced or not to stay in an obligatory quarantine, having people close who tested positive or not, having lost someone close due to COVID-19, and possible changes in psychical or online relationships (from a decrease to an improvement).
The participants’ sleep habits during the lockdown period were assessed. In particular, we evaluated the changes in the habitual bedtime, awakening time, and napping. Answers regarding bedtime and waking time ranged from bringing forward to postponing the usual time. Instead, for the napping time, the answers were aimed at understanding if they were increased or reduced compared to usual.
The sleep quality of the Italian population during the lockdown period was assessed using the Medical Outcomes Study–Sleep Scale (MOS-SS) (Hays and Stewart, 1992). The MOS-SS is a self-administered validated instrument with 12 self-reported questions to determine sleep quality and quantity within a 4-week period. We decided to adopt only the global index of MOS-SS to assess the quality of sleep defined as Sleep Index II (score range from 0 to 100), with higher scores indicating greater sleep problems. A cut-off scoring of 25.8 (Hays et al., 2005; Rejas et al., 2007; Martin et al., 2009) is considered as having poor sleep. The Italian version is available (Palagini and Manni, 2016). In this study, reliability of Sleep Problem II index scales was good, with a Cronbach’s α of 0.85.
Symptoms of common mental health status were assessed using the short form of Depression, Anxiety, and Stress Scales–21 Items (DASS-21) (Lovibond and Lovibond, 1995). The DASS-21 is a self-report measure in which participants rate the frequency and severity of depression, anxiety, and stress (emotional reactions).
As measured by the DASS-21, depression assesses dysphoria, anhedonia, lack of incentive, and low self-esteem; anxiety refers to somatic and subjective symptoms of anxiety and an acute response of fear; and stress evaluates irritability, impatience, tension, and persistent arousal.
Subscale scores are calculated as the sum of the responses to the seven items from each subscale multiplied by 2 to suit the original 42 items. The cutoffs for severe depression, anxiety, and stress are ≥21, ≥15, and ≥26, respectively (Lovibond and Lovibond, 1995).
In the current study, the Italian version of DASS-21 showing excellent psychometric properties was adopted (Bottesi et al., 2015).
Excellent levels of reliability were detected in this sample (depression, α = 0.89; anxiety, α = 0.83; stress, α = 0.90).
Continuous variables were presented as mean and standard deviation (SD), while categorical variables as absolute (n) and relative frequency (%). Chi-square test was used to evaluate the univariate association between MOS-Sleep Index II (sleep disturbance vs. no sleep disturbance) and all the variables described in the section “Materials and Methods.” Multiple logistic regression model was used to evaluate the multivariate association between the dependent variable (good sleeper vs. poor sleeper) and all the variables that were significant in the univariate analysis. The results were presented as odds ratio (OR) with 95% confidence interval (95% CI). The false discovery rate (FDR) correction was applied to adjust the statistical significance to account for multiple comparison (adjusted critic p = 0.008) (Benjamini and Hochberg, 1995).
Cronbach’s alpha was used to evaluate the reliability of the questionnaires used in the survey.
Statistical analysis was performed using the statistical package Stata SE, 14.2.
Our study sample consisted of 6,439 participants: 4,707 (73.1%) females and 1,732 (26.9%) males. The mean age of the sample was 33.9 (SD = 27.6; range 18–82 years), and most of the participants were living in Northern Italy (67.4%). Less than half of the samples had a high school diploma (46.9%) and 28.7% were students. With regard to marital status, 34.9% were unmarried and 28.6% had children.
In Tables 1A,B, we show all the characteristics and differences of the good sleeper and poor sleeper groups in terms of demographic data, living situation during the COVID-19 outbreak, COVID-19 outbreak-related questions, sleep-related data, and mental health in terms of stress, anxiety, and depression. There were 6,439 participants in our study. A total of 3,562 (55.32%) participants reported poor sleep quality according to the MOS-Sleep Index II score. All participants were divided into two groups, poor sleeper (MOS-Sleep Index II total score ≥25.8) and good sleeper (MOS-Sleep Index II total score <25.8). In Figures 1A,B, we show the graphical representation of percentages of poor sleepers stratified for the variables. Also, in Figures 1C,D we show the graphical representation of percentages of good sleepers stratified for the variables.
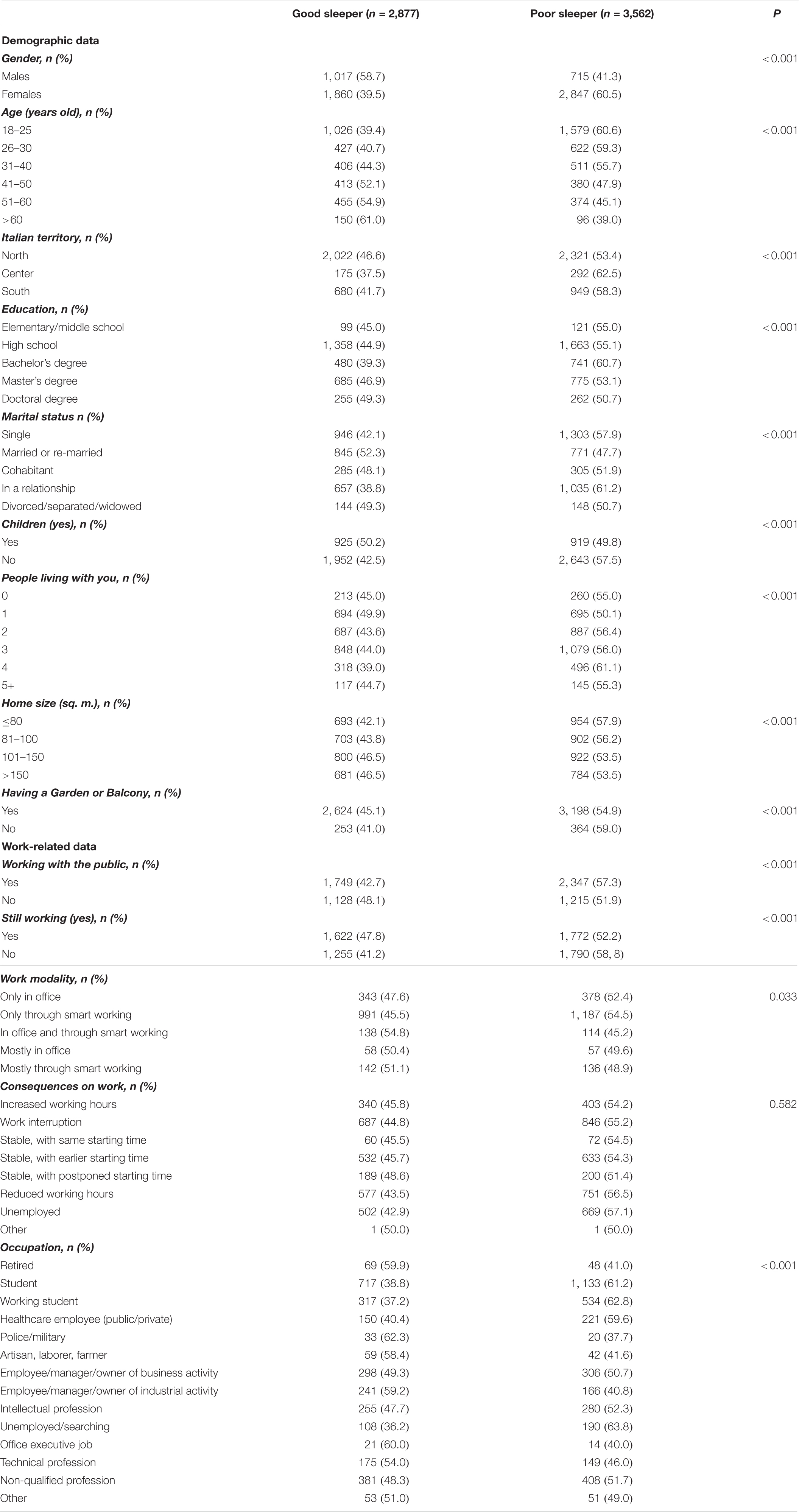
Table 1-A Comparisons between the good sleeper vs. poor sleeper sample with chi-square tests on demographic data and living situations.
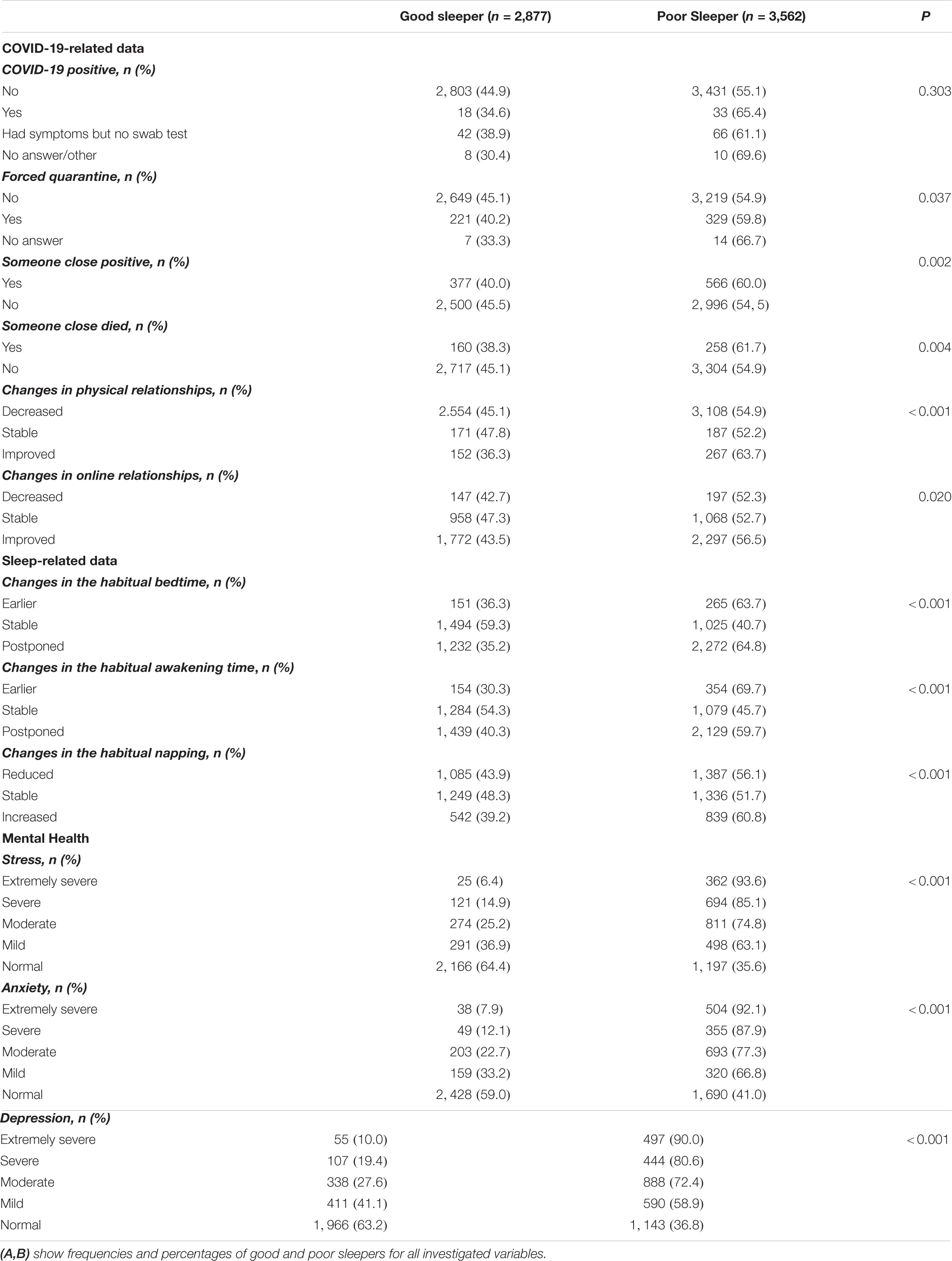
Table 1-B Comparisons between the Good Sleeper vs. Poor Sleeper sample with chi-square tests on COVID-19 related data, sleep habits and mental healths.
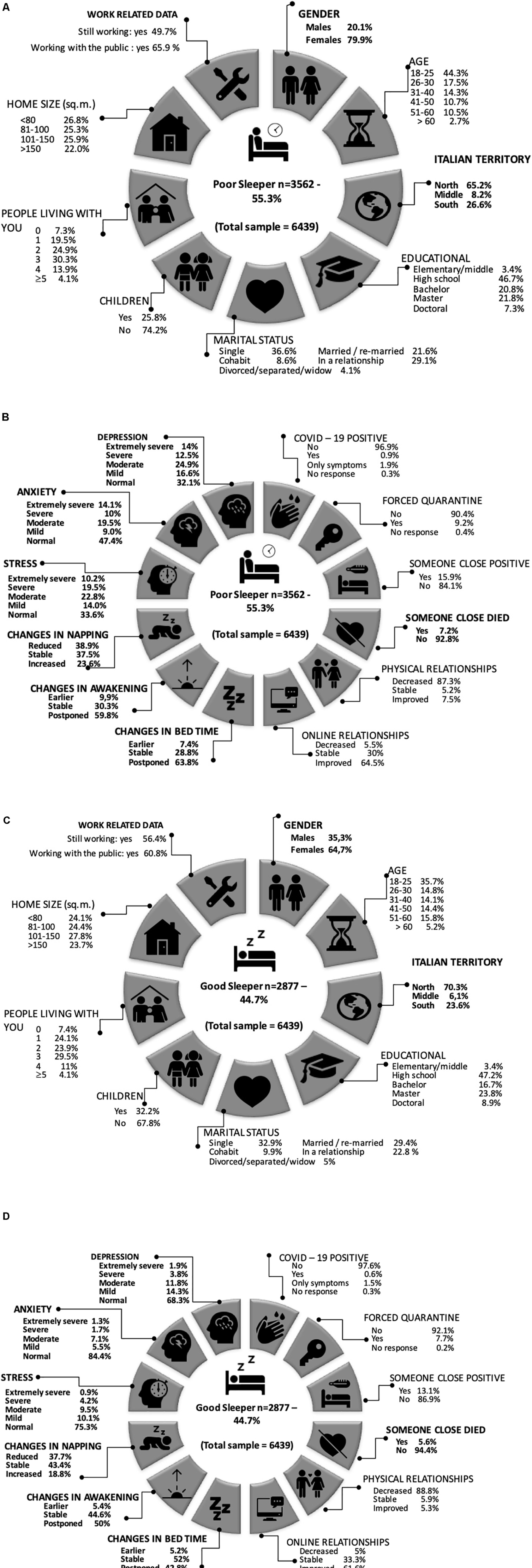
Figure 1. (A) Percentages of poor sleeper stratified for the variables. In bold the significations in the multivariable logistic regression model. The icons are selected from the https://icons8.it. (B) Percentages of poor sleeper stratified for the variables. In bold the significations in the multivariable logistic regression model. The icons are selected from the https://icons8.it. (C) Percentages of good sleeper stratified for the variables. In bold the significations in the multivariable logistic regression model. The icons are selected from the https://icons8.it. (D) Percentages of good sleeper stratified for the variables. In bold the significations in the multivariable logistic regression model. The icons are selected from the https://icons8.it.
Sixty-seven participants who gave no answers to questions about forced quarantine or being positive to COVID-19 were removed to perform the multivariate logistic regression. Table 2 shows the multiple binary logistic regression results of poor sleepers. Significant factors were found in female gender (OR: 1.66; 95% CI: 1.45–1.90), living in Central Italy (OR: 1.39; 95% CI: 1.10–1.76), having someone close who died due to COVID-19 (OR: 1.41; 95% CI: 1.09–1.81), earlier (OR: 1.59; 95% CI: 1.22–2.07) or postponed (OR: 2.10; 95% CI: 1.81–2.41) habitual bedtime, earlier habitual awakening time (OR: 1.47; 95% CI: 1.14–1.90), reduced number of afternoon naps (OR: 1.32; 95% CI: 1.13–1.56), experiencing mild (OR: 2.10; 95% CI: 1.76–2.52), moderate (OR: 2.60;95% CI: 2.16–3.16), severe (OR: 3.37; 95% CI: 2.59–4.39), or extremely severe (OR: 4.83; 95% CI: 2.95–7.92) stress, having mild (OR: 1.61; 95% CI: 1.29–2.02), moderate (OR: 2.39; 95% CI: 1.98–2.89), severe (OR: 3.11; 95% CI: 2.23–4.53), or extremely severe (OR: 3.74; 95% CI: 2.54–5.51) anxiety, and having mild (OR: 1.53; 95% CI: 1.30–1.81), moderate (OR: 1.67; 95% CI: 1.38–1.98), severe (OR: 1.77; 95% CI: 1.32–2.30), or extremely severe (OR: 2.39; 95% CI: 1.69–3.53) depression. Furthermore, being positive to COVID-19 was almost significant (OR: 1.96; p = 0.066).
As far as we know, this is the first study to assess sleep quality and its negative consequences on mental health in the Italian population during the whole of the COVID-19 lockdown (from March 10–1st phase to May 42nd phase). This survey interestingly highlights how quarantine and restriction measures worsened sleep habits, leading to a whole series of consequences on people’s health. In particular, our study found that 55.32% of the sample of 6,439 Italian participants experienced disrupted sleep patterns during the outbreak restrictions.
In our study, the poor sleeper group presented with more negative effects on psychological well-being related to the COVID-19 lockdown. We outlined some risk factors for the development of sleep disturbance: female gender (79.9%), living in Central Italy, losing a loved one due to COVID-19, having markedly changed sleep–wake rhythms (specifically, going to bed earlier or later than the usual time), getting up earlier than usual and having increased the habitual napping time, having moderate to very severe stress (22.8–10.2%), anxiety (19.5–14.1%), and depression levels (25.9–14%).
The prevalence rate of poor sleepers in our population is consistent with 52.4 and 57.1% of two Italian resident surveys [lockdown period: from March 17 to 23 (Cellini et al., 2020) and from March 18 to April 2 (Casagrande et al., 2020)] and higher than in China’s general population (36.38%) (online survey from to February 18 to 25) (Zhao et al., 2020) during the outbreak. In addition, our sample with sleep problems reported a remarkable alteration in their sleep habits: 63.8% reported postponing or bringing forward (7.4%) bedtime; 59.8% reported the need for delayed awakening and an increased napping time in 23.6% during the daytime. All these lifestyle changes seem to be followed by worrying symptoms, such as altered sleep–wake rhythms, which can be interpreted by the negative psychosocial changes observed by Brooks et al. (2020), especially in sleep habits during the COVID-19 outbreak. Evidence (Lo Martire et al., 2019) shows that temporally close excessive and unpredictable stress can impact on the defense system and the central nervous system: stress is modulated by the individual’s psychological responses, which include neuro-endocrine and behavioral components, such as changes in the activity and immune function of the hypothalamic pituitary adrenal (HPA) axis. Consequently, the activation of the HPA system by stress is incompatible with physiological sleep leading to lower sleep quality, longer sleep latency, increased awareness during the night, and more sleep complaints (Tempesta et al., 2013). On the other hand, impairment of sleep quality is a common behavioral consequence of the acute and chronic response to sleep, stress, and trauma (Lo Martire et al., 2019) and determines further increases in the HPA system, thereby promoting a vicious cycle of stress and worsened sleep quality (Lo Martire et al., 2019).
In addition, our results showed that sleep habits affected by quarantine had a strong impact on sleep quality: individuals who go to bed earlier or after the usual time and wake up earlier than usual or have increased habitual napping time have poor sleep quality. Regular schedules also played a role: there is an association between irregular schedules and the complaint of poor sleep (Pilz et al., 2018). Quality sleep requires regular schedules: numerous studies on the deleterious effects of shift work and social jet-lag prove the negative effects of these disturbed rhythms, both metabolically and psychiatrically (Rutters et al., 2014; Levandovski et al., 2011; Sűdy et al., 2019). The biological clock depends on a strong light signal in the morning to update the central clock (Roenneberg et al., 2013). Exposure to intense light in the evening directly stimulates the arousal systems; thus, the individual remains more vigilant and goes to bed later (Phipps-Nelson et al., 2003). In addition, exposure to light in the evening may affect melatonin secretion, resulting in altered night sleep duration (Gooley et al., 2011). This lag may become confusing for the subject once the confinement measures had been lifted: resetting the clock can be difficult, with severe drowsiness and sleeplessness in the evening.
The present study also found a strong association, also recently documented in the Italian population (Casagrande et al., 2020; Cellini et al., 2020), between those who have poor sleep quality and psychological distress. In particular, our study reveals that those who have high levels of stress, anxiety and depression had a higher probability of have sleep problems.
Since quarantine is characterized by self-isolation, social estrangement, separation, loss of freedom, and uncertainty, negative emotions such as fear, anger, and frustration are common and may lead to anxiety, boredom, and/or a feeling of uneasiness (Brooks et al., 2020; Holmes et al., 2020; Qiu et al., 2020; Roychowdhury, 2020). Such feelings endorse negative beliefs about the individual ability to cope. In this context, Brooks et al. (2020) present the main factors that seem to negatively influence our system during the quarantine period: (1) duration of the quarantine; (2) fear of getting infected/spreading the infection; (3) feelings of frustration and boredom; (4) inadequate supply capacity; and (5) lack of sufficient/salient information (Brooks et al., 2020). Moreover, the impossibility to take part in usual day-to-day activities, like outdoor physical activity or physical contact with others, together with dramatic changes in working modalities might encourage a dysregulation of the wake/sleep cycle (Panahi and Tremblay, 2018) as well as increasing psychological distress (Chirico et al., 2020).
According to the cognitive–behavioral model of insomnia, the 3P model, stress is the most common precipitating factor (Spielman et al., 1987). Therefore, all the highlighted COVID stressors seem to trigger elevated cognitive and physiological hyperarousal in a vicious circle that may have impaired sleep quality. Furthermore, when the perceived stress exceeds an individual’s resources, the consequent change in the emotional state (e.g., anxiety) affects wellbeing (Lazarus and Folkman, 1984; Lazarus et al., 1985). Moreover, recent studies underlined how sleep deprivation (Spiegelhalder et al., 2013) significantly reduces the functional connectivity in frontal brain regions, including the ventromedial regions involved in strategies of decision making based on reward and punishment. These alterations have been related with a loss in emotional control and a general tendency to take impulsive and risky decisions that may contribute to maintaining the mood disorder (Kalmbach et al., 2018).
Furthermore, in line with scientific evidence on sleep disturbances (Ohayon and Smirne, 2002; Terzano et al., 2004; Léger et al., 2008) the female gender is more exposed than the male to having problems with sleep. According to other studies on epidemic and quarantine conditions, in nation-wide pandemic catastrophes, sleep disorders are more present in women than in men (Kendler et al., 2001; McLean and Anderson, 2009). Some evidence (Driver et al., 1996; Baker and Driver, 2004; Dzaja et al., 2005; Zhang and Wing, 2006; Davidson, 2009) shows that the changing hormone profile across the reproductive life of a woman, from puberty through the reproductive period to the postmenopausal years, may have a significant influence on sleep leading to sleep alteration or disruption and other vulnerabilities specific to psychological disorders in women (Soni et al., 2013).
Moreover, in our study, the death of someone close due to COVID-19 seems to be a risk factor in the onset of a sleep disorder, as described in the literature (Healey et al., 1981; Morin et al., 2003; Monk et al., 2008). The death of family members or close friends can be very traumatic, especially when the circumstances are unexpected as in this period. Surely, in this dramatic period, not being able to bid farewell and give loved ones a dignified burial have certainly worsened the grief over the loss, with consequences on sleep.
Paradoxically, in our sample, neither age nor the type of occupation seemed to represent a risk factor in developing sleep disorders, as it has been instead described in the Chinese healthcare staff and attributed to the grueling work shifts and the constant witnessing of death and suffering. Most likely, our sample of healthcare professionals was too small (5.7%) compared not only to the other professions but also to the Chinese sample, since our survey was voluntary and did not involve direct administration (Pappa et al., 2020; Xiao et al., 2020; Xue et al., 2020; Zhang et al., 2020) in the front line (hospitals), where these workers were active. In addition, with age, nighttime sleep becomes more fragmented, and total sleep time is reduced (Ohayon et al., 2017). In this stressful condition where COVID induced profound changes in sleep habits, we may all find ourselves, regardless of age differences, experiencing sleep in a problematic way.
Another interesting result that we reported is a risk of sleep problems in Central Italy, although those who live in Northern Italy have been considered the main Italian core of the emergency, due to the greater number of infections and deaths (Istituto Superiore di Sanità, 2020). Perhaps the worries about personal safety, transmitting the disease to family members, stigmatization from being infected, shift work, and interpersonal isolation can manifest by hyperarousal states, as well as problems with anxiety and stimulus control. Stigma can lead to continued fear as people with a disease anticipate discrimination (Audet et al., 2013), and we know at the same time that stigma can be one of the most powerful barriers to delivering prevention, treatment, and care to the most vulnerable, who are at the same time the ones most in need. Moreover, it is possible to hypothesize that another explanation of this result is due to the fact that residents of this area, following the violent L’Aquila earthquake, have developed greater psychological consequences and are more prone to developing posttraumatic stress disorder symptomatology affecting sleep (Tempesta et al., 2013; Ferrara et al., 2016). Finally, the people living in this location perceive themselves to be at higher risk of infection. In fact, some studies (Alexander and Klein, 2001; Cacciaglia et al., 2017) suggested that people who were repeatedly exposed to traumatic events were prone to suffering from many psychological problems and consequently have sleep disorders.
We believe that multidisciplinary action should be taken in order to plan appropriate responses to the current crisis caused by the COVID-19 health emergency. According to Holmes et al. (2020), the consequences of COVID-19 epidemic in the global population are truly unknown and worrying. Therefore, a range wealth of collaborative work is necessary where psychologists, psychiatrists, neurologists, pulmonologists, and virologists cooperate to finalize a policy that will help the population not only to reduce fear and stigma but also to treat mental health and poor quality of sleep caused by the COVID-19 outbreak (Castelnuovo et al., 2020). In particular, as our results highlight, the poor quality of sleep, especially in predisposed subjects, might represent a risk factor for the development of chronic insomnia or other sleep disorders. Moreover, we confirm the negative psychosocial changes observed by Brooks et al. (2020), especially in sleep habits. These are probably caused not only by factors such as poor exposure to sunlight, reduced physical activity, and psychological distress (Altena et al., 2020) but also by the lack of regular and scheduled activities. Moreover, the European Academy for Cognitive–Behavioral Treatment of Insomnia has developed some useful recommendations for the family or single people adapted from the key points of cognitive–behavioral therapy for insomnia to manage the risks attendant to home confinement and to give practical advice about how to handle sleep problems (Altena et al., 2020).
In Italy, the Italian Associations of Sleep Medicine, a multidisciplinary association of specialists on sleep disorders and their treatments, have started an intensive awareness campaign about sleep problems during the lockdown and developed an online help desk1 where the best sleep medicine experts (neurologists, pulmonologists, psychiatrists, and psychologists) respond online to requests of whoever feels the need to improve sleep in this period of time.
As a whole, the results of our study seem to be relevant to outline risk factors for sleep quality in the Italian population during the COVID-19 emergency, but some limitations need to be considered. First, our study is not representative of the sample compared to the Italian population: it was a convenience sample. In addition, the data and results were derived from a cross-sectional design: it was difficult to make cause-and-effect hypotheses. Second, having adopted an online survey limits the generalizability of the results, although it currently represents the only solution for data collection in the time of outbreak. Subsequently, recruitment bias emerged in our sample, which is characterized by a high number of students and women. This aspect should be considered in the interpretation of the results. Third, in this survey we only adopted a self-report questionnaire. Despite the importance of measuring the subjective perception of sleep and distress, semi-objective or objective measures of sleep (such as a sleep diary or actigraphy) and distress would be useful to support our findings.
This is the first study designed to understand sleep quality and lifestyle in the Italian population during the lockdown period that provides more than 6,000 participants in a survey developed specifically for the health emergency related to COVID-19. Our study found that more than half of the Italian population had impaired sleep quality and sleep habits during the COVID-19 lockdown containment measures.
The related factors included female gender, Italian territory, loss of a loved one due to COVID-19 during the lockdown, changes in sleep habits, and elevated psychological distress. A multidisciplinary intervention for sleep disorders and related psychological discomfort is fundamental with a view to taking action to deal with the current crisis caused by the restrictions adopted to reduce the COVID-19 outbreak and to cope with the eventuality of new lockdown periods.
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
This study was conducted in accordance with the Declaration of Helsinki and the study protocol was approved by the Ethics Committee of the Center for Research and Psychological Intervention (CERIP) of the University of Messina. Electronic informed consent was obtained from each participant prior to starting the investigation. Participants could withdraw from the survey at any moment without needing to give a reason.
CF provided substantial contributions to the conception of the work, deep analysis of the literature, study design, development, and final approval of the manuscript. AM contributed in the design of the study, participated in the development and revision of the work, and agreement for final approval of the manuscript. CZ and SS contributed to data analysis and agreement for final approval of the manuscript. MQ, VL, MF, DL, EV, LB, ES, and RC contributed to the revision of the work and agreement for final approval of the manuscript. LP, LD, DR, GP, and GC contributed to deep revision of the work, with literature analysis and agreement for final approval of the manuscript. All authors contributed to the article and approved the submitted version.
GP is a consultant and participated in the advisory board for UCB Pharma, Jazz Pharmaceuticals, Bioprojet, Takeda, and Idorsia outside the submitted work.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor is currently organizing a Research Topic with one of the authors GC.
We wish to thank Cecilia Baroncini and Maria Claudia Folli for their help in editing the English text.
Alexander, D. A., and Klein, S. (2001). Ambulance personnel and critical incidents: impact of accident and emergency work on mental health and emotional well-being. Br. J. Psychiatry 178, 76–81. doi: 10.1192/bjp.178.1.76
Altena, E., Baglioni, C., Espie, C. A., Ellis, J., Gavriloff, D., Holzinger, B., et al. (2020). Dealing with sleep problems during home confinement due to the COVID-19 outbreak: Practical recommendations from a task force of the European CBT-I Academy. J. Sleep Res. 4:e13052. doi: 10.1111/jsr.13052
Audet, C. M., McGowan, C. C., Wallston, K. A., and Kipp, A. M. (2013). Relationship Between HIV Stigma and Self-Isolation Among People Living With HIV in Tennessee. PLoS One. 8:e69564. doi: 10.1371/journal.pone.0069564
Baker, F. C., and Driver, H. S. (2004). Self-reported sleep across the menstrual cycle in young, healthy women. J. Psychosom. Res. 56, 239–243. doi: 10.1016/S0022-3999(03)00067-9
Benjamini, Y., and Hochberg, Y. (1995). Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. Royal Statist. Soc. Ser. B 57, 289–300. doi: 10.1111/j.2517-6161.1995.tb02031.x
Bonnet, M. H., and Arand, D. L. (2010). Hyperarousal and insomnia: state of the science. Sleep Med. Rev. 14, 9–15. doi: 10.1016/j.smrv.2009.05.002
Bottesi, G., Ghisi, M., Altoè, G., Conforti, E., Melli, G., and Sica, C. (2015). The Italian version of the Depression Anxiety Stress Scales-21: Factor structure and psychometric properties on community and clinical samples. Compr. Psychiatry 60, 170–181. doi: 10.1016/j.comppsych.2015.04.005
Brooks, S. K., Webster, R. K., Smith, L. E., Woodland, L., Wessely, S., Greenberg, N., et al. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet 395, 912–920. doi: 10.1016/S0140-6736(20)30460-8
Cacciaglia, R., Nees, F., Grimm, O., Ridder, S., Pohlack, S. T., Diener, S. J., et al. (2017). Trauma exposure relates to heightened stress, altered amygdala morphology and deficient extinction learning: Implications for psychopathology. Psychoneuroendocrinology 76, 19–28. doi: 10.1016/j.psyneuen.2016.11.012
Casagrande, M., Favieri, F., Tambelli, R., and Forte, G. (2020). The enemy who sealed the world: Effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 75, 12–20. doi: 10.1016/j.sleep.2020.05.011
Castelnuovo, G., De Giorgio, A., Manzoni, G. M., Treadway, D. C., and Mohiyeddini, C. (2020). Psychological, Behavioral, and Interpersonal Effects and Clinical Implications for Health Systems of the Coronavirus (COVID-19) Pandemic: A Call for Research. Front. Psychol. 11:2146. doi: 10.3389/fpsyg.2020.02146
Cellini, N., Canale, N., Mioni, G., and Costa, S. (2020). Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J. Sleep Res. 15:e13074. doi: 10.1111/jsr.13074
Chirico, A., Lucidi, F., Galli, F., Giancamilli, F., Vitale, J., Borghi, S., et al. (2020). COVID-19 Outbreak and Physical Activity in the Italian Population: A Cross-Sectional Analysis of the Underlying Psychosocial Mechanisms. Front. Psychol. 11:2100. doi: 10.3389/fpsyg.2020.02100
Davidson, J. R. (2009). Insomnia treatment options for women. Obstet. Gynecol. Clin. North Am. 36, 831–846. doi: 10.1016/j.ogc.2009.10.004
De Giorgio, A. (2020). Global Psychological Implications of Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) and Coronavirus Disease-2019 (COVID-19). What Can Be Learned From Italy. Reflections, Perspectives, Opportunities. Front. Psychol. 11:1836. doi: 10.3389/fpsyg.2020.01836
Driver, H. S., Dijk, D. J., Werth, E., Biedermann, K., and Borbély, A. A. (1996). Sleep and the sleep electroencephalogram across the menstrual cycle in young healthy women. J. Clin. Endocrinol. Metab. 81, 728–735. doi: 10.1210/jcem.81.2.8636295
Dzaja, A., Arber, S., Hislop, J., Kerkhofs, M., Kopp, C., Pollmächer, T., et al. (2005). Women’s sleep in health and disease. J. Psychiatr. Res. 39, 55–76. doi: 10.1016/j.jpsychires.2004.05.008
Ferrara, M., Mazza, M., Curcio, G., Iaria, G., De Gennaro, L., and Tempesta, D. (2016). [Sleep disturbances and spatial memory deficits in post-traumatic stress disorder: the case of L’Aquila (Central Italy)]. Epidemiol. Prev. 40, 45–48. doi: 10.19191/EP16.2S1.P045.047
Gooley, J. J., Chamberlain, K., Smith, K. A., Rajaratnam, S. M. W., Van Reen, E., Zeitzer, J. M., et al. (2011). Exposure to Room Light before Bedtime Suppresses Melatonin Onset and Shortens Melatonin Duration in Humans. J. Clin. Endocrinol. Metab. 96, E463–E472. doi: 10.1210/jc.2010-2098
Harvey, A. G. (2002). A cognitive model of insomnia. Behav. Res. Ther. 40, 869–893. doi: 10.1016/s0005-7967(01)00061-4
Harvey, A. G., Tang, N. K. Y., and Browning, L. (2005). Cognitive approaches to insomnia. Clin. Psychol. Rev. 25, 593–611. doi: 10.1016/j.cpr.2005.04.005
Harvey, C. J., Gehrman, P., and Espie, C. A. (2014). Who is predisposed to insomnia: a review of familial aggregation, stress-reactivity, personality and coping style. Sleep Med. Rev. 18, 237–247. doi: 10.1016/j.smrv.2013.11.004
Hays, R. D., and Stewart, A. L. (1992). “Sleep measures,” in Measuring Functioningand Well-being: The Medical Outcomes Study Approach, eds A. L. Stewart and J. E. Ware (Durham: Duke University Press), 235–259.
Hays, R. D., Martin, S. A., Sesti, A. M., and Spritzer, K. L. (2005). Psychometric properties of the Medical Outcomes Study Sleep measure. Sleep Med. 6, 41–44. doi: 10.1016/j.sleep.2004.07.006
Healey, E. S., Kales, A., Monroe, L. J., Bixler, E. O., Chamberlin, K., and Soldatos, C. R. (1981). Onset of insomnia: role of life-stress events. Psychosom. Med. 43, 439–451. doi: 10.1097/00006842-198110000-00007
Hertenstein, E., Feige, B., Gmeiner, T., Kienzler, C., Spiegelhalder, K., Johann, A., et al. (2019). Insomnia as a predictor of mental disorders: A systematic review and meta-analysis. Sleep Med. Rev. 43, 96–105. doi: 10.1016/j.smrv.2018.10.006
Holmes, E. A., O’Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., et al. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. Lancet Psychiatry 7, 547–560. doi: 10.1016/S2215-0366(20)30168-1
Istituto Superiore di Sanità (2020). EpiCentro Coronavirus Istituto Superiore di Sanità. HYPERLINK “../../../app/fpsyg-11-574475/app/Italy”Italy: Istituto Superiore di Sanità.
Italian Ministry of Health (2020). Covid-19, in GazzettaufficialeilDecreto #Iorestoacasa. March 10, 2020. Available online at: http://www.salute.gov.it/portale/news/p3_2_1_1_1.jsp?lingua=italiano&menu=notizie&p=dalministero&id=4186 (accessed on March 10, 2020)
Kalmbach, D. A., Cuamatzi-Castelan, A. S., Tonnu, C. V., Tran, K. M., Anderson, J. R., Roth, T., et al. (2018). Hyperarousal and sleep reactivity in insomnia: current insights. Nat. Sci. Sleep 10, 193–201. doi: 10.2147/NSS.S138823
Kendler, K. S., Thornton, L. M., and Prescott, C. A. (2001). Gender differences in the rates of exposure to stressful life events and sensitivity to their depressogenic effects. Am. J. Psychiatry 158, 587–593. doi: 10.1176/appi.ajp.158.4.587
Lazarus, R. S., and Folkman, S. (1984). Stress, appraisal, and coping. New York: Springerpublishing company.
Lazarus, R. S., DeLongis, A., Folkman, S., and Gruen, R. (1985). Stress and adaptational outcomes. Problem of confounded measures. Am. Psychol. 40, 770–785. doi: 10.1037/0003-066x.40.7.770
Léger, D., Poursain, B., Neubauer, D., and Uchiyama, M. (2008). An international survey of sleeping problems in the general population. Curr. Med Res. Opin. 24, 307–317. doi: 10.1185/030079907x253771
Levandovski, R., Dantas, G., Fernandes, L. C., Caumo, W., Torres, I., Roenneberg, T., et al. (2011). Depression scores associate with chronotype and social jetlag in a rural population. Chronobiol. Int. 28, 771–778. doi: 10.3109/07420528.2011.602445
Lo Martire, V., Caruso, D., Palagini, L., Zoccoli, G., and Bastianini, S. (2019). Stress & sleep: A relationship lasting a lifetime. Neurosci. Biobehav. Rev. S014, 30149–30146. doi: 10.1016/j.neubiorev.2019.08.024
Lovibond, P. F., and Lovibond, S. H. (1995). Manual for the Depression Anxiety Stress Scales. 2nd. Sydney: Psychology Foundation.
Martin, S., Chandran, A., Zografos, L., and Zlateva, G. (2009). Evaluation of the impact of fibromyalgia on patients’ sleep and the content validity of two sleep scales. Health Qual. Life Outcomes 7:64. doi: 10.1186/1477-7525-7-64
McClung, C. A. (2013). How might circadian rhythms control mood? Let me count the ways. Biol. Psychiatry 74, 242–249. doi: 10.1016/j.biopsych.2013.02.019
McLean, C. P., and Anderson, E. R. (2009). Brave men and timid women? A review of the gender differences in fear and anxiety. Clin. Psychol. Rev. 29, 496–505. doi: 10.1016/j.cpr.2009.05.003
Monk, T. H., Germain, A., and Reynolds, C. F. (2008). Sleep Disturbance in Bereavement. Psychiatr Ann. 38, 671–675. doi: 10.3928/00485713-20081001-06
Morin, C. M., and Espie, C. A. (2003). Insomia: a clinical guide to assessment and treatment. New York: Klewer Academic/Plenum.
Morin, C. M., Blais, F., and Savard, J. (2002). Are changes in beliefs and attitudes about sleep related to sleep improvements in the treatment of insomnia? Behav. Res. Ther. 40, 741–752. doi: 10.1016/s0005-7967(01)00055-9
Morin, C. M., Rodrigue, S., and Ivers, H. (2003). Role of stress, arousal, and coping skills in primary insomnia. Psychosom. Med. 65, 259–267. doi: 10.1097/01.psy.0000030391.09558.a3
Morin, C. M., Stone, J., Trinkle, D., Mercer, J., and Remsberg, S. (1993). Dysfunctionalbeliefs and attitudes about sleep among older adults with and without insomnia complaints. Psychol. Aging 8, 463–467. doi: 10.1037//0882-7974.8.3.463
Ohayon, M. M., and Smirne, S. (2002). Prevalence and consequences of insomnia disorders in the general population of Italy. Sleep Med. 3, 115–120. doi: 10.1016/S1389-9457(01)00158-7
Ohayon, M., Wickwire, E. M., Hirshkowitz, M., Albert, S. M., Avidan, A., Daly, F. J., et al. (2017). National Sleep Foundation’s sleep quality recommendations: first report. Sleep Health 3, 6–19. doi: 10.1016/j.sleh.2016.11.006
Palagini, L., and Manni, R. (2016). Misurare il sonno : repertorio delle scale di valutazione dei disturbi del sonno. Torino: Minerva medica.
Panahi, S., and Tremblay, A. (2018). Sedentariness and Health: Is Sedentary Behavior More Than Just Physical Inactivity? Front. Publ. Health 6:258. doi: 10.3389/fpubh.2018.00258
Pappa, S., Ntella, V., Giannakas, T., Giannakoulis, V. G., Papoutsi, E., and Katsaounou, P. (2020). Prevalence of depression, anxiety, and insomnia among healthcare workers during the COVID-19 pandemic: A systematic review and meta-analysis. Brain Behav. Immun. 88, 901–907. doi: 10.1016/j.bbi.2020.05.026
Phipps-Nelson, J., Redman, J. R., Dijk, D.-J., and Rajaratnam, S. M. W. (2003). Daytime exposure to bright light, as compared to dim light, decreases sleepiness and improves psychomotor vigilance performance. Sleep 26, 695–700. doi: 10.1093/sleep/26.6.695
Pilz, L. K., Keller, L. K., Lenssen, D., and Roenneberg, T. (2018). Time to rethink sleep quality: PSQI scores reflect sleep quality on workdays. Sleep 41:zsy029. doi: 10.1093/sleep/zsy029
Qiu, J., Shen, B., Zhao, M., Wang, Z., Xie, B., and Xu, Y. (2020). A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen. Psychiatr. 33:e100213. doi: 10.1136/gpsych-2020-100213
Rejas, J., Ribera, M. V., Ruiz, M., and Masrramón, X. (2007). Psychometric properties of the MOS (Medical Outcomes Study) Sleep Scale in patients with neuropathic pain. Eur. J. Pain 11, 329–340. doi: 10.1016/j.ejpain.2006.05.002
Riemann, D., Nissen, C., Palagini, L., Otte, A., Perlis, M. L., and Spiegelhalder, K. (2015). The neurobiology, investigation, and treatment of chronic insomnia. Lancet Neurol. 14, 547–558. doi: 10.1016/S1474-4422(15)00021-6
Riemann, D., Spiegelhalder, K., Feige, B., Voderholzer, U., Berger, M., Perlis, M., et al. (2010). The hyperarousal model of insomnia: a review of the concept and its evidence. Sleep Med. Rev. 14, 19–31. doi: 10.1016/j.smrv.2009.04.002
Roenneberg, T., Kantermann, T., Juda, M., Vetter, C., and Allebrandt, K. V. (2013). Light and the human circadian clock. Handb. Exp. Pharmacol. 217, 311–331. doi: 10.1007/978-3-642-25950-0_13
Roychowdhury, D. (2020). 2019 Novel Coronavirus Disease, Crisis, and Isolation. Front. Psychol. 11:1958. doi: 10.3389/fpsyg.2020.01958
Rubin, G. J., and Wessely, S. (2020). The psychological effects of quarantining a city. BMJ 368:m313. doi: 10.1136/bmj.m313
Rutters, F., Lemmens, S. G., Adam, T. C., Bremmer, M. A., Elders, P. J., Nijpels, G., et al. (2014). Is social jetlag associated with an adverse endocrine, behavioral, and cardiovascular risk profile? J. Biol. Rhythms 29, 377–383. doi: 10.1177/0748730414550199
Spiegelhalder, K., Regen, W., Baglioni, C., Riemann, D., and Winkelman, J. W. (2013). Neuroimaging studies in insomnia. Curr. Psychiatry Rep. 15:405. doi: 10.1007/s11920-013-0405-0
Spielman, A. J., Caruso, L. S., and Glovinsky, P. B. (1987). A behavioral perspective on insomnia treatment. Psychiatr. Clin. North Am. 10, 541–553.
Soni, M., Curran, V. H., and Kamboj, S. K. (2013). Identification of a narrow post-ovulatory window of vulnerability to distressing involuntary memories in healthy women. Neurobiol. Learn. Mem. 104, 32–38. doi: 10.1016/j.nlm.2013.04.003
Sűdy, ÁR., Ella, K., Bódizs, R., and Káldi, K. (2019). Association of Social Jetlag With Sleep Quality and Autonomic Cardiac Control During Sleep in Young Healthy Men. Front. Neurosci. 13:950. doi: 10.3389/fnins.2019.00950
Tempesta, D., Curcio, G., De Gennaro, L., and Ferrara, M. (2013). Long-term impact of earthquakes on sleep quality. PLoS One 8:e55936. doi: 10.1371/journal.pone.0055936
Terzano, M. G., Parrino, L., Cirignotta, F., Ferini-Strambi, L., Gigli, G., Rudelli, G., et al. (2004). Studio Morfeo: insomnia in primary care, a survey conducted on the Italian population. Sleep Med. 5, 67–75. doi: 10.1016/j.sleep.2003.09.006
Vadnie, C. A., and McClung, C. A. (2017). Circadian Rhythm Disturbances in Mood Disorders: Insights into the Role of the Suprachiasmatic Nucleus. Neural. Plast. 2017:1504507. doi: 10.1155/2017/1504507
Wang, C., Horby, P. W., Hayden, F. G., and Gao, G. F. (2020a). A novel coronavirus outbreak of global health concern. Lancet 395, 470–473. doi: 10.1016/S0140-6736(20)30185-9
Wang, C., Pan, R., Wan, X., Tan, Y., Xu, L., Ho, C. S., et al. (2020b). Immediate Psychological Responses and Associated Factors during the Initial Stage of the 2019 Coronavirus Disease (COVID-19) Epidemic among the General Population in China. Int. J. Environ. Res. Publ. Health 17:1729. doi: 10.3390/ijerph17051729
World Health Organization (2020). Mental health and psychosocial considerationsduring the COVID-19 outbreak. (No. WHO/2019-nCoV/MentalHealth/2020.1). Geneva: World Health Organization.
Xiao, H., Zhang, Y., Kong, D., Li, S., and Yang, N. (2020). The Effects of Social Support on Sleep Quality of Medical Staff Treating Patients with Coronavirus Disease 2019 (COVID-19) in January and February 2020 in China. Med. Sci. Monit. 26:e923549. doi: 10.12659/MSM.923549
Xue, Z., Lin, L., Zhang, S., Gong, J., Liu, J., and Lu, J. (2020). Sleep problems and medical isolation during the SARS-CoV-2 outbreak. Sleep Med. 70, 112–115. doi: 10.1016/j.sleep.2020.04.014
Zhang, B., and Wing, Y.-K. (2006). Sex differences in insomnia: a meta-analysis. Sleep 29, 85–93. doi: 10.1093/sleep/29.1.85
Zhang, C., Yang, L., Liu, S., Ma, S., Wang, Y., Cai, Z., et al. (2020). Survey of Insomnia and Related Social Psychological Factors Among Medical Staff Involved in the 2019 Novel Coronavirus Disease Outbreak. Front. Psychiatry 11:306. doi: 10.3389/fpsyt.2020.00306
Keywords: sleep quality, sleep habits, COVID-19, Italian lockdown, depression, anxiety, stress, clinical psychology
Citation: Franceschini C, Musetti A, Zenesini C, Palagini L, Scarpelli S, Quattropani MC, Lenzo V, Freda MF, Lemmo D, Vegni E, Borghi L, Saita E, Cattivelli R, De Gennaro L, Plazzi G, Riemann D and Castelnuovo G (2020) Poor Sleep Quality and Its Consequences on Mental Health During the COVID-19 Lockdown in Italy. Front. Psychol. 11:574475. doi: 10.3389/fpsyg.2020.574475
Received: 19 June 2020; Accepted: 15 October 2020;
Published: 09 November 2020.
Edited by:
Antonella Granieri, University of Turin, ItalyReviewed by:
Yiqi Lin, Fujian Provincial Hospital, ChinaCopyright © 2020 Franceschini, Musetti, Zenesini, Palagini, Scarpelli, Quattropani, Lenzo, Freda, Lemmo, Vegni, Borghi, Saita, Cattivelli, De Gennaro, Plazzi, Riemann and Castelnuovo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Christian Franceschini, Y2hyaXN0aWFuLmZyYW5jZXNjaGluaUB1bmlwci5pdA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.