- 1Department of Psychological Medicine, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 2Department of Psychology, Institute of Psychiatry, Psychology and Neuroscience, King’s College London, London, United Kingdom
- 3Child and Adolescent Eating Disorders Service, South London and Maudsley NHS Foundation Trust, London, United Kingdom
- 4Department of Psychology and Human Development, University College London, London, United Kingdom
- 5Department of General Psychology, University of Padova, Padova, Italy
People with eating disorders display a negative interpretation bias towards ambiguous social stimuli. This bias may be particularly relevant to young people with the illness due to the developmental salience of social acceptance and rejection. The overall aim of this study was to systematically develop and validate stimuli for a cognitive bias modification training to reduce a social rejection-related negative interpretation bias in young people with eating disorders. A mixed-methods design was used to achieve this aim. A review of the literature was conducted using EMBASE, MEDLINE, PsycINFO, Web of Science, and PubMed. Six studies were included in the review. Focus groups were held with patients with eating disorders, carers and healthcare professionals. Content analysis was used to identify key themes from the qualitative data. Based on these themes, a total of 339 scenarios were generated by the researchers. Salient themes identified from the focus group data included virtual rejection/exclusion, rejection associated with an aspect of the eating disorder, rejection triggered by ambiguous/benign comments or behaviors of others and rejection perceived when confiding in others. Patients rated these scenarios in terms of their age-relevance and emotional salience and 301 scenarios were included in the final stimulus set. These materials may be used by researchers conducting future experimental research into the potential benefits of interpretation bias training for young people with eating disorders.
Introduction
Mental health disorders place a huge burden on the individuals affected, their families and society (Holmes et al., 2018). Despite the availability of evidence-based psychological treatments, their efficacy is sub-optimal and requires coordinated efforts from researchers and clinicians worldwide to improve (Holmes et al., 2018). The use of evidence-based practice is key to treatment innovation. Evidence-based practice refers to treatment guided by a combined consideration of clinical expertise, research evidence and patient values, preferences and circumstances (American Psychological Association, 2005). Recently, it has been suggested that this approach is particularly suited to improve treatment for conditions characterized by repeated treatment failures and chronicity, such as eating disorders (Peterson et al., 2016; Hilbert et al., 2017). In this study, we will use the evidence-based practice framework to validate the materials for a novel computerized training to improve social functioning in young people with eating disorders.
Eating disorders are psychiatric conditions diagnostically characterized by abnormal eating behaviors and cognitions related to eating, weight and shape (American Psychiatric Association, 2013). These symptoms often appear in adolescence, a time when the pressure for social acceptance is critically high (Somerville, 2013). Among other factors, the onset of abnormal eating behaviors in adolescence has been associated with criticism from others with regards to general aspects of the self, eating, and physical appearance (Jacobi et al., 2011; Copeland et al., 2015; Duarte et al., 2017; Lee and Vaillancourt, 2019; Lie et al., 2019; Okada et al., 2019). Furthermore, the severity of eating disorder symptoms has been linked to greater concerns about appearing nervous or anxious to others (Espel-Huynh et al., 2019). Experimental studies have corroborated the causal role played by interpersonal stress in triggering eating disorder symptoms (Cardi et al., 2018b; Monteleone et al., 2018). For instance, tasks that elicit interpersonal stress increase the desire to binge eat in patients with bulimia nervosa or binge eating disorder (Tuschen-Caffier and Vogele, 1999; Hilbert et al., 2011; Rosenberg et al., 2013), and reduce the liking of food in women with a lifetime diagnosis of anorexia nervosa compared to healthy women (Chami et al., in preparation). The implication of these findings is that decreasing reactivity to interpersonal stress might reduce the severity of eating disorder symptoms.
Recent advances in the field of experimental psychopathology indicate that it is possible to lower patients’ sensitivity to negative social feedback by reducing their tendency to interpret ambiguous social information in a negative way (Cardi et al., 2015, 2019; Turton et al., 2018).
Cognitive Bias Modification for Interpretation (CBM-I) is a computerized training developed with the goal of reducing a negative interpretation bias by exposing participants to benign/neutral interpretations of ambiguous social scenarios. Both adults and adolescents with eating disorders display an interpretation bias towards negative social information and this bias is related to self-reported sensitivity to rejection as well as core eating disorder symptoms, such as fear of weight gain and body image disturbance (Cardi et al., 2017). A recent study also indicated that cognitive biases (attention and interpretation biases) towards negative or ambiguous social information are malleable to change after using five training sessions of combined CBM-I and CBM of attention (CBM-A) and that the use of the training is associated with lower levels of anxiety and higher levels of self-compassion in response to critical feedback from an actor (Cardi et al., 2015).
A common limitation of these studies is that they have not measured changes in core eating disorder symptoms following CBM-I. Procedures for CBM-I in other mental health conditions, such as depression and anxiety disorders, seem to produce only a small effect on clinical symptoms (Krebs et al., 2018). A possible reason to explain the lack of generalization effects on clinical symptoms is that training materials are not systematically developed and validated within the target population. Most existing interpretation bias trainings in eating disorders have been adapted from those originally developed for people with anxiety disorders and have been validated in adults. For example, Cardi et al. (2015) adapted stimuli originally developed by Hirsch et al. (2009) which included scenarios covering common worry topics, and tested these in a feasibility study involving a sample of 28 females with anorexia nervosa. Furthermore, these materials were adapted by researchers without the involvement of key stakeholders including patients, health professionals, and carers. These factors limit the ecological validity of the training for the target population within today’s social context (Hughes et al., 2016). Based on this hypothesis, this study involved the development of stimuli for a novel CBM-I training for adolescents with eating disorders, and piloting the face validity of these stimuli. The three aims were:
1. To conduct a critical review of the literature on interpretation bias assessment and training towards social stimuli in eating disorders.
2. To conduct focus groups with adolescents with eating disorders, carers and professionals to identify salient themes around the topic of social rejection and generate scenarios (interpretation bias training stimuli) reflecting those themes.
3. To pilot the face validity of these materials, focusing on two key aspects (age-relevance and emotional salience) in the target population (adolescents with eating disorders).
Materials and Methods
Aim 1
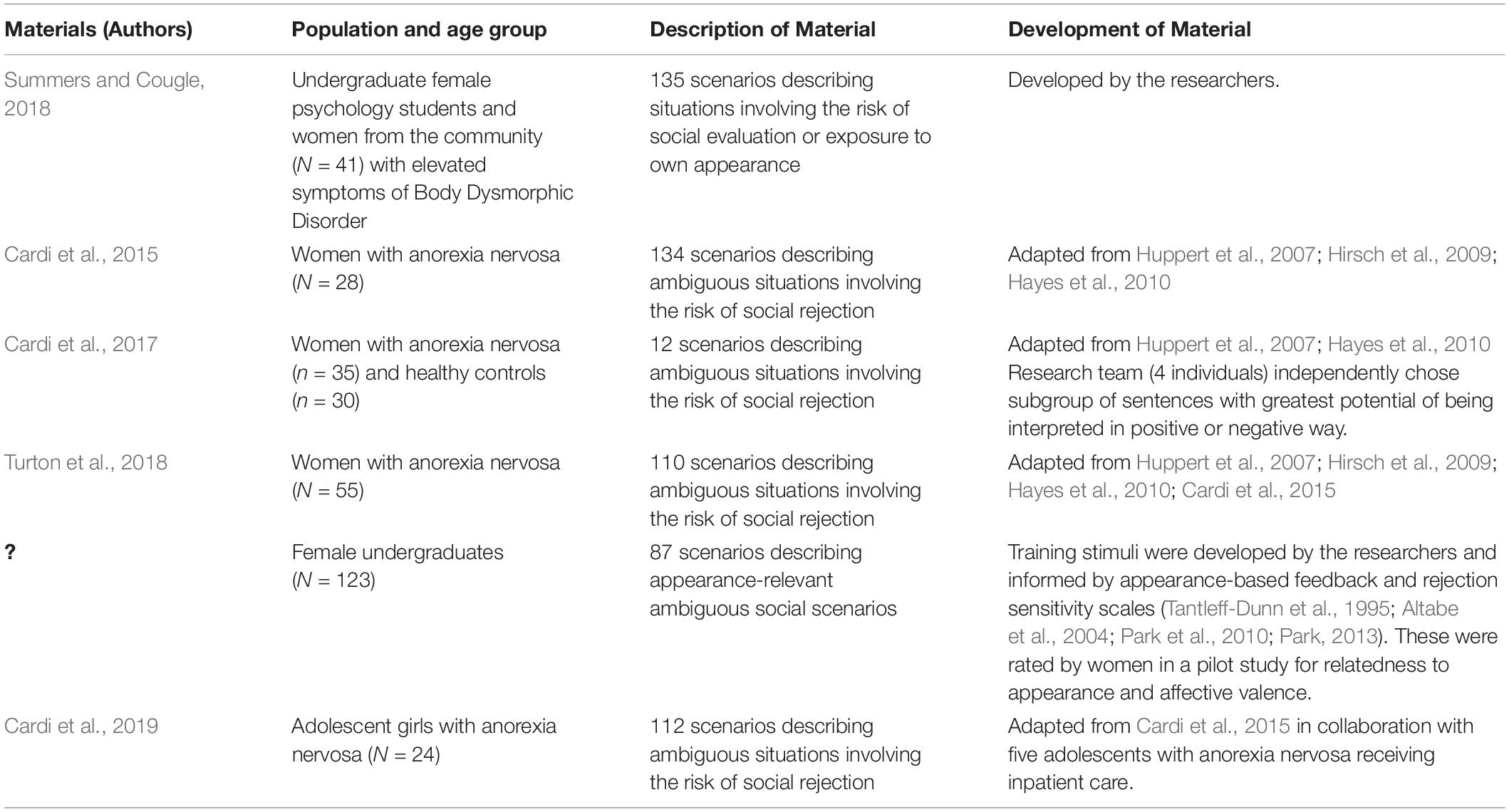
The literature on interpretation bias towards social stimuli in people with eating disorders or studies involving community samples and included a measurement of eating disorder symptoms were reviewed. An online literature search was conducted using EMBASE, MEDLINE, PsycINFO, Web of Science, and PubMed from database inception – October 2019. Search terms included “interpretation bias” or “biased interpretation” in combination with “anorexia nervosa” or “bulimia nervosa” or “eating disorder” in the Title/Abstract or full-text fields. Publications were included if (1) they were published in a peer-reviewed journal and written in English, (2) used an assessment task to measure interpretation bias towards social stimuli or a cognitive bias modification training to reduce negative interpretation bias towards social information and (3) included a sample of children, adolescents or adults with a diagnosis of an eating disorder or included a community sample and a measurement of eating disorder symptoms (Table 1). The materials used for the assessment or training task used within each study are summarized in Table 1.
Aim 2
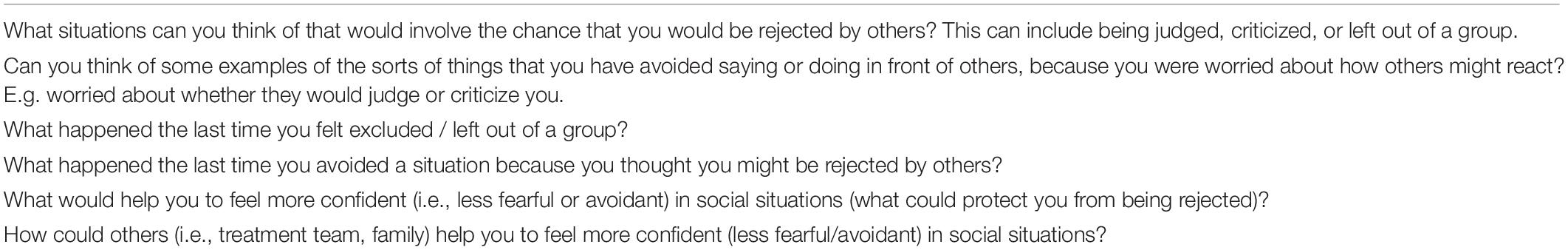
In order to address the main research question, “What situations are likely to trigger fear of being rejected/left out/excluded in adolescents with eating disorders?”, patients with eating disorders, carers and health professionals were invited to participate in separate, live online group forums which were themed around the topic of social rejection. Participants were recruited via opportunity sampling from a specialist eating disorder intensive treatment service and from a departmental database of patients who had previously participated in research and had opted to be contacted about future studies. Participants were required to be fluent in English and have no severe medical or psychiatric comorbidities in order to take part. Patients’ eligibility was assessed by the researcher and the eating disorder diagnosis was confirmed by a Consultant Psychiatrist based on DSM-5 criteria or self-reported by the patient (in three cases). A standard topic guide including questions related to the topic of social rejection was developed (Table 2) and the wording was adapted for patients, carers and health professionals. Two separate groups were held for the professionals to accommodate the availability of participants. The forums were hosted on a bespoke research platform that developed for another study running in the department (created by https://www.mindwaveventures.com/ and funded by the National Institute for Health Research - Health Technology Assessment). The forums were live, text-based groups accessible to participants only. All participants were given a participant screen name (e.g., Participant 1) in order to anonymise them. The researcher led the groups by posting open questions and providing participants with time to respond to each question. Each group lasted for one hour. Ambiguous scenarios related to the risk of rejection from others were then generated with consideration of those previously adapted for adolescents with eating disorders (Cardi et al., 2019) and the data derived from the focus groups. Each scenario consisted of a hypothetical ambiguous social situation which was open to the young person for interpretation (e.g., “It is a classmate’s birthday and your good friend brings in a cake. You aren’t offered a slice and feel awkward. Later you speak to your friend about how this made you feel and they…”).
Aim 3
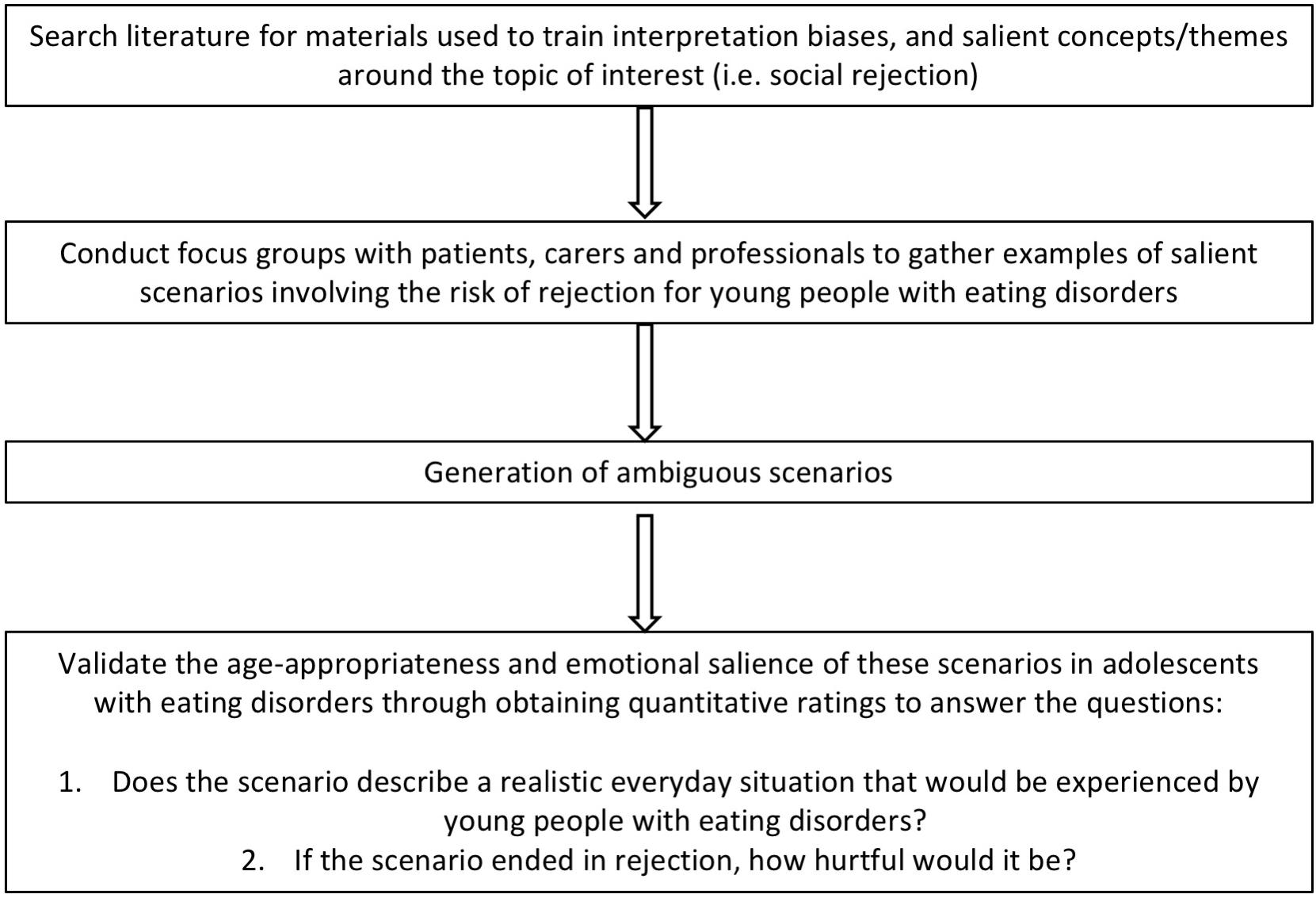
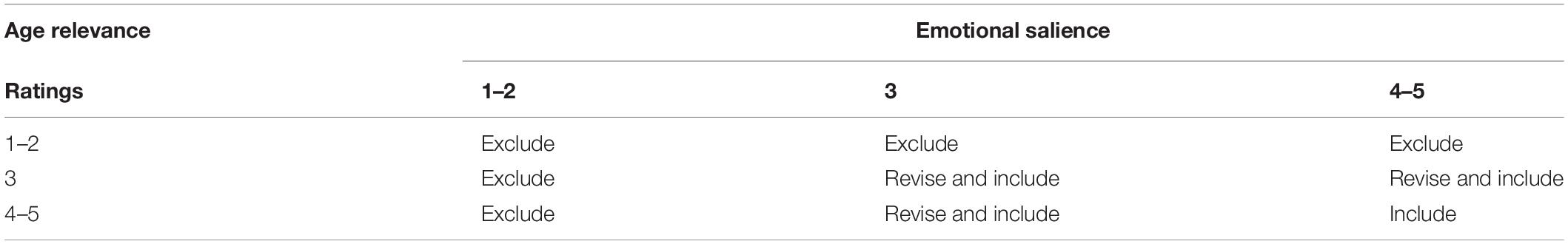
Quantitative methods were used to assess the degree to which the scenarios reflected realistic concerns that were both age appropriate and emotionally salient to young people with eating disorders (see Figure 1). Girls with eating disorders (N = 27) aged 13–17 who participated in the focus groups and girls attending an intensive treatment program who did not participate in the focus groups were invited to rate the scenarios (at this time there were no boys available in the service to rate the scenarios). Participants were provided with paper forms over email, or in person at their treatment center. Each paper form contained a proportion of the scenarios depending on the participants’ time availability, and two 5-point Likert-scales which were used to measure the age-relevance and emotional salience of each scenario. The scales ranged from 0 (not at all realistic) to 5 (very realistic) and 0 (not at all hurtful) to 5 (very hurtful). After discussion with the research team, the matrix (Table 3) was developed to decide whether to include, modify or exclude each of the scenarios. The scenarios that were considered both realistic and hurtful (scenarios scoring 3 or above on both scales) were included in the final selection of scenarios. The data that support the findings of this study are openly available in [repository name e.g., “figshare”] at, reference number [reference number].
Results
Results of Aim 1
Six papers meeting the inclusion criteria were identified and reviewed (see Table 1). Five studies included adults (N = 312) aged 18–65 and one study included adolescents (N = 24) aged 14–18. With the exception of Cardi et al. (2019) that involved adolescents with lived experience of eating disorders in the process of adapting materials for an interpretation bias modification training, all five studies included stimuli adapted by the researchers that were originally designed for other populations. This presents missed opportunities to tap into concerns around social rejection that may be relevant to people with eating disorders in particular, such as fears around being rejected due to the physical or behavioral symptoms that are specific to anorexia nervosa, and to explore concerns that may be predominantly relevant to adolescents with these conditions.
Results of Aim 2
Five focus groups were held in total. The patient group consisted of eight young people (seven females, one male) aged 13–17 (M = 15.50, SD = 1.22) with anorexia nervosa (n = 6) or bulimia nervosa (n = 2). A separate focus group was held for carers (n = 7) who were females aged 40–58 (M = 50.33, SD = 5.59). Only one of the carer participants was related to one of the patient participants in the study. Two separate groups were held for health professionals who were females aged 23–60 (M = 35.67, SD = 12.02) working within specialist eating disorder services. All participants were living in the United Kingdom. One group included two psychiatrists and two psychologists, and one group included a consultant psychologist, an assistant psychologist and a mental health support worker.
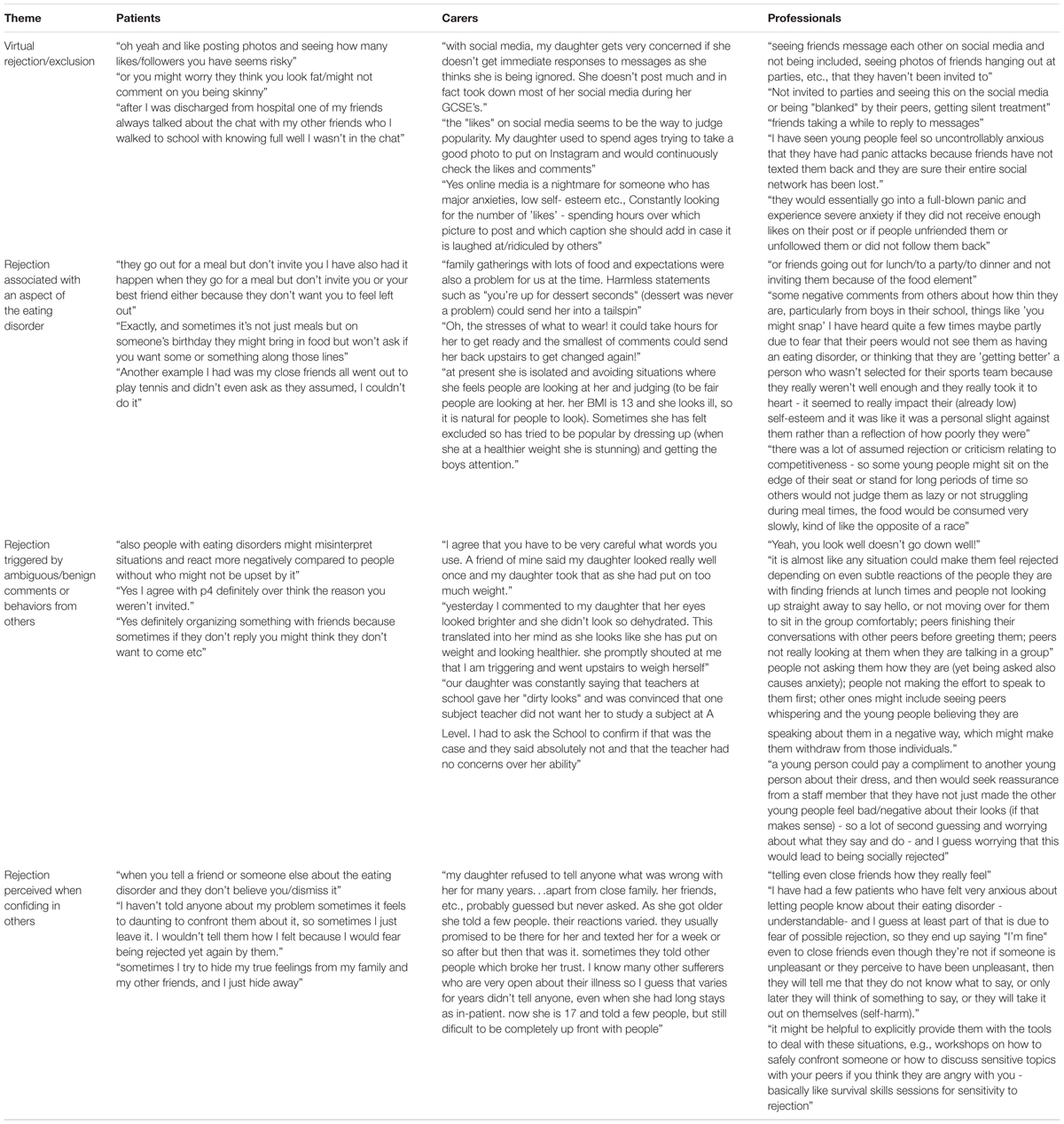
Data collected from the focus group transcripts were analyzed using content analysis to identify recurrent examples of social rejection scenarios (Table 4). Two researchers manually coded the data and used the qualitative data analysis software NVivo (Version 13). First the researchers familiarized themselves with the data through repeatedly reading the text of all transcripts and identifying initial codes (i.e., sentence by sentence coding). The researchers then categorized the examples of social rejection described by patients, carers and health professionals into themes, including virtual rejection/exclusion, rejection associated with an aspect of the eating disorder, rejection triggered by ambiguous/benign comments or behaviors from others and rejection perceived when confiding in others (see Table 4).
Results of Aim 3
Following Aims 1 and 2, 339 scenarios were generated by the research team. Each patient rated a minimum of 19 and a maximum of 264 scenarios depending on their time availability. The scenarios were then categorized using the ratings matrix (Table 3). One-hundred and sixty-six (49%) scenarios were rated high [scoring 4 or 5 on both age-relevance (M = 4.28, SD = 0.71) and emotional salience (M = 4.18, SD = 0.76)] and were automatically included in the final set of stimuli. Thirty-eight (11%) scenarios were rated as low (1 or 2) on one or both measures by at least one patient and automatically excluded. One-hundred thirty-five (40%) scenarios were rated as neutral (3) on both aspects and were then revised to increase their age-relevance and emotional salience by the researchers, so that they could be included in the final set of scenarios. Revisions to the neutral scenarios were made by taking aspects from the scenarios rated as high or feedback from young people rating the scenarios and applying them to the neutral scenario. For example, “Your friends are looking at a magazine over lunch at school. One of them turns the page and makes a comment about a thin model, so you ask if they can change the page” was changed to “your friends are looking at Instagram during the school lunchbreak. One of them starts looking at an Instagram feed and makes comments about a thin model, so you ask if they can look at a different account.”
The final set of stimuli consisted of 301 scenarios. All scenarios, with ratings for each of them presented separately are openly available in [repository name e.g., “figshare”] at, reference number [reference number].
Discussion
This study followed the evidence-based practice framework and a systematic process of adapting experimental paradigms to specific populations (Hughes et al., 2016) to develop and validate stimuli for a cognitive bias modification training to reduce interpretation bias towards negative social stimuli in young people with eating disorders. The first aim was to review existing studies that have used cognitive bias assessment or modification procedures to target an interpretation bias towards negative social stimuli in people with eating disorders. The majority of identified studies included only adults and the majority of materials used within the training protocols had been adapted by the researchers from those originally developed for people with anxiety disorders (Cardi et al., 2015, 2017; Summers and Cougle, 2018; Turton et al., 2018). The second aim was to generate real-life examples of scenarios in which individuals with eating disorders feel exposed to social rejection or exclusion. Focus group discussions were held with young people with lived experience of eating disorders, carers and healthcare professionals with experience working with young people with eating disorders in specialist treatment services. Four key themes were identified from the focus groups including (1) virtual rejection/exclusion (2) rejection associated with an aspect of the eating disorder (3) rejection triggered by ambiguous/benign comments or behaviors of others and (4) rejection perceived when confiding in others. The final aim was to obtain quantitative ratings from young people with eating disorders concerning the age-relevance and emotional salience of the scenarios, and to make final adjustments to the scenarios based on this feedback. A total of 301 scenarios were included in the final stimulus set.
The findings from the focus groups with patients, carers and healthcare professionals in this study support the literature on social functioning in young people with eating disorders (Caglar-Nazali et al., 2014; Cardi et al., 2018a,b). All groups agreed that patients perceive rejection when exposed to ambiguous/benign comments or behaviors from others, such as over-thinking the reason for not being invited to a party or receiving a compliment on their physical appearance. These observations corroborate findings from an earlier qualitative study in which young people with anorexia nervosa described a heightened sensitivity to any form of perceived criticism (Patel et al., 2016) and recent quantitative data, which demonstrated that young people with anorexia nervosa on average produced more negative than benign interpretations of ambiguous social scenarios involving the risk of rejection (Cardi et al., 2019).
Participants also recalled examples of illness-related rejection experiences, such as being excluded from arrangements to have meals out with friends or not being offered food in social contexts. These findings support other qualitative accounts from young people with anorexia nervosa who have described the impact that their eating disorder and treatment regime had on their social functioning (Lindstedt et al., 2018). Furthermore, the risk of rejection perceived by patients when confiding in others, for example a reluctance to disclose their illness to friends due to a fear of being dismissed or disbelieved, supports the interpersonal model of eating disorders which posits that some problems with social functioning in people with eating disorders may originate in part from maladaptive personality traits, such as the tendency to avoid expressing feelings and the tendency towards interpersonal distrust and negative interactions with others (Arcelus et al., 2013).
Participants referred to several examples of virtual rejection, and over-reactions to this experience such as full-blown panic or severe anxiety if a friend did not reply to their message, or if they did not receive enough likes on their social media posts. These findings are novel in the context of the existing literature on interpretation bias, which has lacked the consideration of exposure to rejection in a virtual environment. However, the findings are in line with what is known about the role of online social interactions in eating disorders. For example, one study found that girls and women with a lifetime diagnosis of an eating disorder reported poorer mood after posting or commenting online, a greater frequency of social comparison, and a greater use of online forums and blogs with more focus on eating disorder-related issues in comparison to a group of age-matched controls (Bachner-Melman et al., 2018). In both groups, these online behaviors correlated with eating disorder symptoms and general psychological health. In another study, the frequency of Facebook use was associated with greater disordered eating, and maintenance of weight/shape concerns and state anxiety compared to an alternative online activity (Mabe et al., 2014). Together, these findings suggest that negative interpretations of social cues online may contribute to feelings of rejection and trigger eating disorder symptoms.
Strengths and Limitations
The main strength of this study is that it is the first study to use a systematic approach to the development of stimuli for an interpretation bias training intervention for people with eating disorders. Other strengths include the involvement of different parties, including patients, carers and professionals (Kimber et al., 2019), to identify the type and content of social situations that trigger social evaluative concerns in adolescents with eating disorders, and the incorporation of both qualitative and quantitative methods in the development and validation of the materials. Furthermore, the large pool of materials developed (N = 301) will be made publicly available, in line with the open science framework and may be used for multi-session interpretation bias training protocols, which have shown advantages over single-session trainings in terms of training efficacy on interpretation bias change (Menne-Lothmann et al., 2014; Cristea et al., 2015; Turton et al., 2018). One limitation of this study was that due to the large number of scenarios and limited availability of patients, quantitative feedback was obtained only from a subgroup of adolescents with eating disorders (girls aged 14–18) and might not be generalisable to other groups of individuals, particularly younger girls or boys who may differ in their experiences of social rejection. Furthermore, some scenarios only had one rating from one participant. The scenarios rated by participants as neutral (n = 135) were revised further by the researchers to increase their age-relevance and emotional salience so that they could be included in the final set of scenarios. Although these adapted neutral scenarios were not included in the pilot study, they will be included in a proceeding study, investigating the feasibility and clinical effectiveness of multi-session cognitive bias modification training.
Clinical Implications
There is increasing interest in the use of treatment enhancers in eating disorders due to their potential to improve clinical outcomes. In the United Kingdom, the National Institute for Health and Care Excellence (NICE) guidelines recommend Family Based Treatment as the first-line treatment for adolescents with eating disorders (National Institute for Health and Care Excellence (NICE), 2017). This therapy aims to improve nutrition and mostly focuses on providing information and support to carers to feed their children (Le Grange and Eisler, 2009; Lock and Le Grange, 2019). Whilst this is the most effective treatment available according to the current evidence base, approximately 20% patients offered Family Based Treatment drop-out (Dejong et al., 2012), between 33% and 42% reach remission by the end of treatment (Lock et al., 2010; Agras et al., 2014), and 40% of patients struggle with significant ongoing psychological distress after treatment (Lock et al., 2006; Wufong et al., 2019). CBM could provide a useful ‘treatment enhancer’ by increasing sensitivity to positive social feedback and reducing sensitivity to social criticism from family and peers, and the online nature of the training may appeal to the younger population.
The large set of stimuli described here has been developed and validated by girls with eating disorders. Multi-session studies combined with follow-up assessments allow for an investigation of the acceptability and effectiveness of the training in the long term. In doing so researchers should consider strategies for facilitating participant engagement with the training over time (Zhang et al., 2018) and to assess whether changes observed in interpretation biases are associated with changes in social perceptions and behaviors, as well as key clinical variables. It will also be important to explore potential pathways through which this training can be related to improvements in symptoms, such as through strengthening responsiveness to social acceptance or support. The training may also provide benefits to individuals at ‘high risk’ of psychopathology through boosting resilience to the risk of social rejection/exclusion.
Conclusion
To date, this is the first study to use a systematic approach to the development of a cognitive bias training targeting an interpretation bias towards negative social stimuli in young people with eating disorders. These materials will be made available to aid researchers in conducting experimental studies to assess the acceptability and clinical effectiveness of multi-session cognitive bias modification training protocols in young people with eating disorders.
Data Availability Statement
The datasets generated for this study are available on request to the corresponding author.
Ethics Statement
This study was reviewed and approved by London Riverside – Research Ethics Committee. Written informed consent to participate in this study was provided by the participants’ or their legal guardian/next of kin.
Author Contributions
KR, EW, MS, AH, and VC contributed to the study design. KR and EW performed the data collection and analysis which was supervised by VC. KR, EW, and VC wrote the manuscript with input from MS and AH.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank the patients, carers and healthcare professionals who participated in this study. VC is supported by a grant from MIUR (Dipartimenti di Eccellenza DM 11/05/2017 n. 262) to the Department of General Psychology. AH is supported by the Medical Research Council (MR/S020381/1).
References
Agras, W. S., Lock, J., Brandt, H., Bryson, S. W., Dodge, E., Halmi, K. A., et al. (2014). Comparison of 2 family therapies for adolescent anorexia nervosa: a randomized parallel trial. JAMA Psychiatry 71, 1279–1286. doi: 10.1001/jamapsychiatry.2014.1025
Altabe, M., Wood, K., Herbozo, S., and Thompson, J. K. (2004). The physical appearance ambiguous feedback scale (PAAFS): a measure for indexing body image related cognitive bias. Body Image 1, 299–304. doi: 10.1016/j.bodyim.2004.05.004
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders. Arlington, VA: American Psychiatric Publishing.
American Psychological Association (2005). Policy Statement on Evidence-Based Practice in Psychology. Available online at: http://www.apa.org/practice/guidelines/evidence-based-statement (accessed August, 2005).
Arcelus, J., Haslam, M., Farrow, C., and Meyer, C. (2013). The role of interpersonal functioning in the maintenance of eating psychopathology: a systematic review and testable model. Clin. Psychol. Rev. 33, 156–167. doi: 10.1016/j.cpr.2012.10.009
Bachner-Melman, R., Zontag-Oren, E., Zohar, A. H., and Sher, H. (2018). Lives on the line: the online lives of girls and women with and without a lifetime eating disorder diagnosis. Front. Psychol. 9:2128. doi: 10.3389/fpsyg.2018.02128
Caglar-Nazali, H. P., Corfield, F., Cardi, V., Ambwani, S., Leppanen, J., Olabintan, O., et al. (2014). A systematic review and meta-analysis of ‘Systems for Social Processes’ in eating disorders. Neurosci. Biobehav. Rev. 42, 55–92. doi: 10.1016/j.neubiorev.2013.12.002
Cardi, V., Esposito, M., Bird, G., Rhind, C., Yiend, J., Schifano, S., et al. (2015). A preliminary investigation of a novel training to target cognitive biases towards negative social stimuli in Anorexia Nervosa. J. Affect. Disord. 188, 188–193. doi: 10.1016/j.jad.2015.08.019
Cardi, V., Mallorqui-Bague, N., Albano, G., Monteleone, A. M., Fernandez-Aranda, F., and Treasure, J. (2018a). Social difficulties as risk and maintaining factors in anorexia nervosa: a mixed-method investigation. Front. Psychiatry 9:12. doi: 10.3389/fpsyt.2018.00012
Cardi, V., Tchanturia, K., and Treasure, J. (2018b). Premorbid and illness-related social difficulties in eating disorders: an overview of the literature and treatment developments. Curr. Neuropharmacol. 16, 1122–1130. doi: 10.2174/1570159X16666180118100028
Cardi, V., Turton, R., Brazil, C., Harrison, A., Rowlands, K., Treasure, J., et al. (2019). Training rejection interpretation in eating disorders (TRIER): preliminary findings of a feasibility study in adolescents with anorexia nervosa. Cogn. Ther. Res. 43, 1109–1117. doi: 10.1007/s10608-019-10034-x
Cardi, V., Turton, R., Schifano, S., Leppanen, J., Hirsch, C. R., and Treasure, J. (2017). Biased interpretation of ambiguous social scenarios in anorexia nervosa. Eur. Eat. Disord. Rev. 25, 60–64. doi: 10.1002/erv.2493
Copeland, W. E., Bulik, C. M., Zucker, N., Wolke, D., Lereya, S. T., and Costello, E. J. (2015). Does childhood bullying predict eating disorder symptoms? A prospective, longitudinal analysis. Int. J. Eat. Disord. 48, 1141–1149. doi: 10.1002/eat.22459
Cristea, I. A., Kok, R. N., and Cuijpers, P. (2015). Efficacy of cognitive bias modification interventions in anxiety and depression: meta-analysis. Br. J. Psychiatry 206, 7–16. doi: 10.1192/bjp.bp.114.146761
Dejong, H., Broadbent, H., and Schmidt, U. (2012). A systematic review of dropout from treatment in outpatients with anorexia nervosa. Int. J. Eat. Disord. 45, 635–647. doi: 10.1002/eat.20956
Duarte, C., Pinto-Gouveia, J., and Stubbs, R. (2017). The prospective associations between bullying experiences, body image shame and disordered eating in a sample of adolescent girls. Pers. Individ. Dif. 116, 319–325. doi: 10.1016/j.paid.2017.05.003
Espel-Huynh, H. M., Muratore, A. F., Virzi, N., Brooks, G., and Zandberg, L. J. (2019). Mediating role of experiential avoidance in the relationship between anxiety sensitivity and eating disorder psychopathology: a clinical replication. Eat. Behav. 34:101308. doi: 10.1016/j.eatbeh.2019.101308
Hayes, S., Hirsch, C. R., Krebs, G., and Mathews, A. (2010). The effects of modifying interpretation bias on worry in generalized anxiety disorder. Behav. Res. Ther. 48, 171–178. doi: 10.1016/j.brat.2009.10.006
Hilbert, A., Hoek, H. W., and Schmidt, R. (2017). Evidence-based clinical guidelines for eating disorders: international comparison. Curr. Opin. Psychiatry 30, 423–437. doi: 10.1097/YCO.0000000000000360
Hilbert, A., Vogele, C., Tuschen-Caffier, B., and Hartmann, A. S. (2011). Psychophysiological responses to idiosyncratic stress in bulimia nervosa and binge eating disorder. Physiol. Behav. 104, 770–777. doi: 10.1016/j.physbeh.2011.07.013
Hirsch, C. R., Hayes, S., and Mathews, A. (2009). Looking on the bright side: accessing benign meanings reduces worry. J. Abnorm. Psychol. 118, 44–54. doi: 10.1037/a0013473
Holmes, E. A., Ghaderi, A., Harmer, C. J., Ramchandani, P. G., Cuijpers, P., Morrison, A. P., et al. (2018). The lancet psychiatry commission on psychological treatments research in tomorrow’s science. Lancet Psychiatry 5, 237–286. doi: 10.1016/S2215-0366(17)30513-8
Hughes, A. M., Gordon, R., Chalder, T., Hirsch, C. R., and Moss-Morris, R. (2016). Maximizing potential impact of experimental research into cognitive processes in health psychology: a systematic approach to material development. Br. J. Health Psychol. 21, 764–780. doi: 10.1111/bjhp.12214
Huppert, J. D., Pasupuleti, R. V., Foa, E. B., and Mathews, A. (2007). Interpretation biases in social anxiety: response generation, response selection, and self-appraisals. Behav. Res. Ther. 45, 1505–1515. doi: 10.1016/j.brat.2007.01.006
Jacobi, C., Fittig, E., Bryson, S., Wilfley, D., Kraemer, H., and Taylor, C. B. (2011). Who is really at risk? Identifying risk factors for subthreshold and full syndrome eating disorders in a high-risk sample. Psychol. Med. 41, 1939–1949. doi: 10.1017/S0033291710002631
Kimber, M., Dimitropoulos, G., Williams, E. P., Singh, M., Loeb, K. L., Hughes, E. K., et al. (2019). Tackling mixed messages: practitioner reflections on working with adolescents with atypical anorexia and their families. Eat. Disord. 27, 436–452. doi: 10.1080/10640266.2018.1542888
Krebs, G., Pile, V., Grant, S., Degli Esposti, M., Montgomery, P., and Lau, J. Y. F. (2018). Research review: cognitive bias modification of interpretations in youth and its effect on anxiety: a meta-analysis. J. Child Psychol. Psychiatry 59, 831–844. doi: 10.1111/jcpp.12809
Le Grange, D., and Eisler, I. (2009). Family interventions in adolescent anorexia nervosa. Child Adolesc. Psychiatr. Clin. N. Am. 18, 159–173. doi: 10.1016/j.chc.2008.07.004
Lee, K. S., and Vaillancourt, T. (2019). A four-year prospective study of bullying, anxiety, and disordered eating behavior across early adolescence. Child Psychiatry Hum. Dev. 50, 815–825. doi: 10.1007/s10578-019-00884-7
Lie, S. Ø., Rø, Ø., and Bang, L. (2019). Is bullying and teasing associated with eating disorders? A systematic review and meta-analysis. Int. J. Eat. Disord. 52, 497–514. doi: 10.1002/eat.23035
Lindstedt, K., Neander, K., Kjellin, L., and Gustafsson, S. A. (2018). A life put on hold: adolescents’ experiences of having an eating disorder in relation to social contexts outside the family. J. Multidiscip. Healthc. 11, 425–437. doi: 10.2147/JMDH.S168133
Lock, J., Couturier, J., and Agras, W. S. (2006). Comparison of long-term outcomes in adolescents with anorexia nervosa treated with family therapy. J. Am. Acad. Child Adolesc. Psychiatry 45, 666–672. doi: 10.1097/01.chi.0000215152.61400.ca
Lock, J., and Le Grange, D. (2019). Family-based treatment: where are we and where should we be going to improve recovery in child and adolescent eating disorders. Int. J. Eat. Disord. 52, 481–487. doi: 10.1002/eat.22980
Lock, J., Le Grange, D., Agras, W. S., Moye, A., Bryson, S. W., and Jo, B. (2010). Randomized clinical trial comparing family-based treatment with adolescent-focused individual therapy for adolescents with anorexia nervosa. Arch. Gen. Psychiatry 67, 1025–1032. doi: 10.1001/archgenpsychiatry.2010.128
Mabe, A. G., Forney, K. J., and Keel, P. K. (2014). Do you “like” my photo? Facebook use maintains eating disorder risk. Int. J. Eat. Disord. 47, 516–523. doi: 10.1002/eat.22254
Matheson, E., Wade, T. D., and Yiend, J. (2018). A new cognitive bias modification technique to influence risk factors for eating disorders. Int. J. Eat. Disord. 51, 959–967. doi: 10.1002/eat.22938
Menne-Lothmann, C., Viechtbauer, W., Hohn, P., Kasanova, Z., Haller, S. P., Drukker, M., et al. (2014). How to boost positive interpretations? A meta-analysis of the effectiveness of cognitive bias modification for interpretation. PLoS One 9:e100925. doi: 10.1371/journal.pone.0100925
Monteleone, A. M., Treasure, J., Kan, C., and Cardi, V. (2018). Reactivity to interpersonal stress in patients with eating disorders: a systematic review and meta-analysis of studies using an experimental paradigm. Neurosci. Biobehav. Rev. 87, 133–150. doi: 10.1016/j.neubiorev.2018.02.002
National Institute for Health and Care Excellence (NICE) (2017). Eating Disorders: Recognition, and Treatment. NICE Guideline [NG69]. London: NICE Guideline.
Okada, L. M., Miranda, R. R., das Graças Pena, G., Levy, R. B., and Azeredo, C. M. (2019). Association between exposure to interpersonal violence and social isolation, and the adoption of unhealthy weight control practices. Appetite 142:104384.
Park, L. E. (2013). Appearance-Based Rejection Sensitivity (Appearance-RS) Scale (Long and Short Form). Measurement Instrument Database for the Social Science. Available online at: www.midss.org (accessed February 27, 2020).
Park, L. E., Calogero, R. M., Young, A. F., and Diraddo, A. M. (2010). Appearance-based rejection sensitivity predicts body dysmorphic disorder symptoms and cosmetic surgery acceptance. J. Soc. Clin. Psychol. 29, 489–509. doi: 10.1521/jscp.2010.29.5.489
Patel, K., Tchanturia, K., and Harrison, A. (2016). An exploration of social functioning in young people with eating disorders: a qualitative study. PLoS One 11:e0159910. doi: 10.1371/journal.pone.0159910
Peterson, C. B., Becker, C. B., Treasure, J., Shafran, R., and Bryant-Waugh, R. (2016). The three-legged stool of evidence-based practice in eating disorder treatment: research, clinical, and patient perspectives. BMC Med. 14:69. doi: 10.1186/s12916-016-0615-5
Rosenberg, N., Bloch, M., Ben Avi, I., Rouach, V., Schreiber, S., Stern, N., et al. (2013). Cortisol response and desire to binge following psychological stress: comparison between obese subjects with and without binge eating disorder. Psychiatry Res. 208, 156–161. doi: 10.1016/j.psychres.2012.09.050
Somerville, L. H. (2013). Special issue on the teenage brain: sensitivity to social evaluation. Curr. Dir. Psychol. Sci. 22, 121–127. doi: 10.1177/0963721413476512
Summers, B. J., and Cougle, J. R. (2018). An experimental test of the role of appearance-related safety behaviors in body dysmorphic disorder, social anxiety, and body dissatisfaction. J. Abnorm. Psychol. 127, 770–780. doi: 10.1037/abn0000387
Tantleff-Dunn, S., Thompson, J. K., and Dunn, M. E. (1995). The feedback on physical appearance scale (FOPAS): questionnaire development and psychometric evaluation. Eat. Disord. 3, 332–341. doi: 10.1080/10640269508250063
Turton, R., Cardi, V., Treasure, J., and Hirsch, C. R. (2018). Modifying a negative interpretation bias for ambiguous social scenarios that depict the risk of rejection in women with anorexia nervosa. J. Affect. Disord. 227, 705–712. doi: 10.1016/j.jad.2017.11.089
Tuschen-Caffier, B., and Vogele, C. (1999). Psychological and physiological reactivity to stress: an experimental study on bulimic patients, restrained eaters and controls. Psychother. Psychosom. 68, 333–340. doi: 10.1159/000012352
Wufong, E., Rhodes, P., and Conti, J. (2019). “We don’t really know what else we can do”: parent experiences when adolescent distress persists after the Maudsley and family-based therapies for anorexia nervosa. J. Eat. Disord. 7:5. doi: 10.1186/s40337-019-0235-5
Keywords: interpretation bias, eating disorders, social, interpersonal, cognitive bias modification
Citation: Rowlands K, Wilson E, Simic M, Harrison A and Cardi V (2020) A Critical Review of Studies Assessing Interpretation Bias Towards Social Stimuli in People With Eating Disorders and the Development and Pilot Testing of Novel Stimuli for a Cognitive Bias Modification Training. Front. Psychol. 11:538527. doi: 10.3389/fpsyg.2020.538527
Received: 27 February 2020; Accepted: 21 August 2020;
Published: 29 September 2020.
Edited by:
Andrew Kemp, Swansea University, United KingdomReviewed by:
Daniel Eric Schoth, University of Southampton, United KingdomIoana Roxana Podina, University of Bucharest, Romania
Copyright © 2020 Rowlands, Wilson, Simic, Harrison and Cardi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Katie Rowlands, a2F0aWUucm93bGFuZHNAa2NsLmFjLnVr
 Katie Rowlands
Katie Rowlands Emma Wilson
Emma Wilson Mima Simic
Mima Simic Amy Harrison
Amy Harrison Valentina Cardi
Valentina Cardi