
94% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
CLINICAL TRIAL article
Front. Psychol. , 23 October 2019
Sec. Psychology for Clinical Settings
Volume 10 - 2019 | https://doi.org/10.3389/fpsyg.2019.02373
Background: Individuals who were maltreated during childhood are faced with increased risks for developing various psychological symptoms that are particularly resistant to traditional treatments. This pilot study investigated the effects of a mindfulness based behavioral intervention for young adults with a childhood maltreatment history.
Methods: This study looked at self-report psychological questionnaires from 20 subjects (5 males) before and after a mindfulness-based behavioral intervention, compared to 18 subjects (6 males) in the waiting list control group (age range 22–29); all subjects experienced mild-to-moderate childhood maltreatment. We analyzed changes in stress, anxiety, depression, mindfulness and self-compassion related to the intervention with linear mixed effects models; we also analyzed the relationships among questionnaire score changes with partial correlation analyses and mediation analysis.
Results: Linear mixed effects model analyses revealed significant group by time interaction on stress (p < 0.01), anxiety (p < 0.05), and self-compassion (p < 0.01), with the mindfulness group having significant reduction in stress and anxiety (p < 0.01), and significant increase in mindfulness (p < 0.05) and self-compassion (p < 0.001). Partial correlation analyses showed that among all subjects from both groups, changes in mindfulness positively correlated with changes in self-compassion (r = 0.578, p = 0.001), which negatively correlated with changes in depression (r = −0.374, p = 0.05) and anxiety (r = −0.395, p < 0.05). Changes in self-compassion mediated, in part, the relationship between changes in mindfulness and changes in anxiety (average causal mediation effect = −4.721, p < 0.05). We observed a dose-dependent effect of the treatment, i.e., the number of intervention sessions attended were negatively correlated with changes in stress (r = −0.674, p < 0.01), anxiety (r = −0.580, p < 0.01), and depression (r = −0.544, p < 0.05), after controlling for the individual differences in childhood maltreatment severity.
Conclusion: Our results suggest that, to some extent, the mindfulness-based intervention can be helpful for improving self-compassion and psychological health among young adults with a childhood maltreatment history.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier NCT02447744.
Childhood maltreatment is remarkably prevalent. “Child maltreatment is the abuse and neglect that occurs to children under 18 years of age. It includes all types of physical and/or emotional ill-treatment, sexual abuse, neglect, negligence and commercial or other exploitation, which results in actual or potential harm to the child’s health, survival, development or dignity in the context of a relationship of responsibility, trust or power. Exposure to intimate partner violence is also sometimes included as a form of child maltreatment” (World Health Organization, 2016). In the 1990s, a large scale survey, later known as the Adverse Childhood Experience study, was conducted on 17,337 adult HMO members at a preventative health clinic in California (Felitti et al., 1998). This study indicated that 63% of the participants had experienced at least one category of childhood maltreatment or household dysfunction, and over 20% experienced three or more categories of adverse childhood experience (Felitti et al., 1998). This study also found more adverse childhood experience was associated with increased risks for alcoholism, drug abuse, depression, suicide attempts, and other high risk health conditions (Felitti et al., 1998).
Childhood maltreatment is also associated with increased risks for multiple medical and psychiatric conditions throughout the entire lifespan (Pietrek et al., 2013). Childhood maltreatment also puts individuals at risk for developing borderline personality disorder (Herman et al., 1989) as well as other personality disorders (Johnson et al., 1999). Individuals with a childhood maltreatment history tend to have earlier onset of psychological symptoms, more episodes, more comorbid disorders (Bernet and Stein, 1999), as well as higher likelihood of resistance toward traditional treatments (Nanni et al., 2012).
In recent years, mindfulness-based or mindfulness-informed treatment programs showed promising effects for treating a wide variety of clinical symptoms and disorders, many of which are commonly experienced in individuals with a childhood maltreatment history. For example, mindfulness based cognitive therapy is a highly effective treatment for recurrent depression (Williams et al., 2014; Kuyken et al., 2016; Rodrigues et al., 2019), especially for patients with a childhood maltreatment history (Williams et al., 2014) dialectical behavioral therapy, which has a strong mindfulness element, is a highly effective treatment for borderline personality disorder (Linehan et al., 1999; Verheul et al., 2003; Soler et al., 2012; Moran et al., 2018) mindfulness-based interventions are also useful for treating anxiety disorders (Roemer and Orsillo, 2002; Evans et al., 2008; Goldin and Gross, 2010; McEvoy, 2019), and in particular have shown efficacy for treating symptoms of trauma (Follette et al., 2006; King et al., 2013; Banks et al., 2015). Given that individuals with a childhood maltreatment history typically have symptoms of multiple disorders and are resistant to traditional treatments, the present study aims to investigate the effect of a mindfulness based behavioral intervention program for reducing psychological symptoms in young adults with a history of childhood maltreatment, regardless of the primary psychopathology they currently present.
Mindfulness has been defined as paying attention in a particular way: on purpose, in the present moment, and non-judgmentally, in the service of self-understanding and wisdom (Kabat-Zinn, 1990). Because of the intrinsic “present-centered” nature of mindfulness practice, i.e., it encourages “non-judgment and acceptance of thoughts and emotions as they occur in the present moment” (Boyd et al., 2018, p. 7), its therapeutic value for people with traumatic memories has been recognized in recent years. Several mindfulness-based treatments have also been developed or adapted for treating Post-traumatic Stress Disorder (PTSD), “as an alternative technique for targeting symptoms of avoidance and negative cognitions, including self-blame, shame and guilt among individuals with PTSD” (Follette et al., 2006; Lang et al., 2012; Banks et al., 2015; Boyd et al., 2018, p. 8). Although not all individuals with a childhood maltreatment history demonstrate full scale PTSD per DSM standard, the “self-blame, shame and guilt” components of the symptomology are rather common among childhood maltreatment victims (Hoglund and Nicholas, 1995; Andrews, 1998; Stuewig and McCloskey, 2005; Dorahy and Clearwater, 2012). Therefore, we hypothesized that a mindfulness-based intervention could bring similar therapeutic benefits for individuals with a childhood maltreatment history.
Previous studies have also suggested that childhood maltreatment is associated with low “self-compassion” (Tanaka et al., 2011; Vettese et al., 2011), which has been associated with emotional dysregulation (Vettese et al., 2011), and higher risk of psychological distress and suicidality (Tanaka et al., 2011). Self-compassion “involves feelings of caring and kindness toward oneself in the face of personal suffering and involves the recognition that one’s suffering, failures and inadequacies are part of the human condition” (Neff, 2003, p. 224). The Self-Compassion Scale was developed to evaluate this construct with six subscales: self-kindness vs. self-judgment, which evaluates the tendency to be “gentle, supportive and understanding toward oneself” instead of “harshly judging oneself for personal shortcomings” (Neff, 2016, p. 265), common humanity vs. isolation, which evaluates the recognition for shared human experience in face of failure, mistakes and imperfection, and mindfulness vs. over-identification, which measures the ability to be aware of one’s present moment experience without being caught up with negative narratives (Neff, 2016).
A previous factor analysis found strong positive correlation between mindfulness and self-compassion (Baer et al., 2006), while several clinical trials indicate that participation in a mindfulness based intervention increased self-compassion (Birnie et al., 2010; Gard et al., 2012; Greenberg et al., 2018). Therefore, the present study also investigated the effect of the mindfulness-based intervention on self-compassion, and the possible role of self-compassion in mediating the therapeutic effects of the intervention.
This study has been registered on clinicaltrials.gov, with a clinical trial identifier of NCT02447744; the detailed information of this clinical trial can be publicly accessed at https://clinicaltrials.gov/ct2/show/NCT02447744. This study was approved by the Institutional Review Board (IRB) (IRB#: 2014P000295) of Partners HealthCare, which is the IRB for Massachusetts General Hospital, McLean Hospital, and several other major hospitals in the Boston area.
Forty-three subjects were recruited from the subject pool of a previous study about childhood maltreatment (Khan et al., 2015). Subjects were enrolled into the study if they pass the following inclusion/exclusion criteria: (1) determined to have childhood maltreatment as having a score of at least one in the Adverse Childhood Experience questionnaire (Felitti et al., 1998) or at least one category of childhood maltreatment in the Maltreatment and Abuse Chronology of Exposure (MACE) questionnaire (Teicher and Parigger, 2015); (2) verified age between 21 and 35 years old; (3) no suicidal attempts during the past 6 months; (4) no history of neurological disorders or psychiatric disorders with psychotic features; (5) passing common MRI exclusion criteria; (6) no prior experience with the Mindfulness Based Stress Reduction (MBSR) program (Kabat-Zinn, 1990) or other systematic meditation programs; (7) committed to meeting the requirement of refraining from using illicit drugs throughout the course of the study; (8) provided written informed consent to participate in this study.
The whole trial included three waves of recruitment for three corresponding cohorts of the mindfulness-based intervention programs. Only two cohorts are included in the analysis of this study because the research component of the trial stopped abruptly while participants were still enrolled in the third cohort of intervention, due to reasons unrelated to the trial itself; as a result, there was no research data from the third cohort. During each cohort of recruitment, subjects were enrolled in the mindfulness-based intervention program if they were available to attend the majority of the 9 sessions of meetings in that cohort, and they were administered research questionnaires before the beginning and after the end of the intervention program; if they were not available to attend the majority of sessions on the schedule, they were placed on the waiting list for the intervention program of the next cohort, and they were administered research procedures first at the time of enrolment, then for a second time at least 2 months later, then a third time after they complete the intervention program. The majority of subjects on the waiting list dropped out from the study; only a total of six subjects completed the intervention program after their waiting period and provided research data for three time points, among them, only four subjects completed the research questionnaires analyzed in this paper.
Comprehensive clinical assessment about childhood experience and psychiatric history were completed in the previous study, the subject pool of which we recruited from Khan et al. (2015). When subjects were enrolled in the present study, clinicians administered the Longitudinal Interview Follow-up Evaluation - Psychiatric Status Ratings (LIFE) (Keller et al., 1987) to assess their current mental health condition to determine whether they meet the inclusion/exclusion criteria of the present study. During the structured interview when subjects were first recruited into the previous study (Khan et al., 2015), we collected demographic information such as subjects’ date of birth, ethnicity, biological sex, employment, and marital status. During the LIFE interview when subjected were recruited into this study, we re-evaluated their employment and marital status.
After subjects were consented and enrolled into the study, they completed the following psychological questionnaires online: Perceived Stress Scale (PSS; Cohen et al., 1994), State-Trait Anxiety Inventory-Trait subscale (STAI-t; Spielberger and Sydeman, 1994), Self-Compassion Scale (SCS; Neff, 2003), Beck Depression Inventory (BDI; Beck et al., 1996) and Mindful Attention Awareness Scale (MAAS; Brown and Ryan, 2003). Those online questionnaires were administered with the REDCap electronic data capture tools (Harris et al., 2009). Upon completion of the intervention program, subjects were administered the same questionnaires. Subjects on the waiting lists were administered the same questionnaires at the same time period as the subjects in the corresponding cohort of mindfulness-based intervention. Other research procedures were also administered at the same time, including additional questionnaires, MRI and an episodic memory test, and they will be reported in other publications. Examples of items on MAAS include: “I could be experiencing some emotion and not be conscious of it until some time later.”, “I break or spill things because of carelessness, not paying attention, or thinking of something else.”, and “I rush through activities without being really attentive to them.” Examples of items on SCS include: “(Self-Kindness) I try to be loving toward myself when I’m feeling emotional pain.”, “(Self-Judgment) I’m disapproving and judgmental about my own flaws and inadequacies.”, “(Mindfulness) When I’m feeling down I try to approach my feelings with curiosity and openness.”, “(Over-Identification) When I fail at something important to me I become consumed by feelings of inadequacy.”, “(Common-Humanity)When I’m down and out, I remind myself that there are lots of other people in the world feeling like I am.” and “(Isolation)When I’m feeling down, I tend to feel like most other people are probably happier than I am.”
The mindfulness-based intervention program lasted for eight continuous weeks, which included eight 2.5-hour long weekly meeting sessions that took place on a weekday evening plus one whole-day session on a weekend day. The mindfulness based intervention program was modeled after the Mindfulness-Based Stress Reduction (MBSR) program (Kabat-Zinn, 1990), with several modifications to adapt the program to our study population. The intervention program covered topics such as mindfulness and awareness, perception and perspectives, being present, responding vs. reacting to stress, stress coping strategies, dealing with difficult emotions, handling difficult communications, and using mindfulness in everyday life (Santorelli et al., 2017). Modification to the original MBSR program included: allowing subjects to choose the length of homework meditation practice as they see fit (2, 3, 10, 20 or 30 min, as opposed to the original 45 min); inclusion of the “3-minute breathing space” exercise which was originally a component of the mindfulness based cognitive therapy program and has been shown to be helpful for PTSD patients (King et al., 2013); and general emphasis on empowering the participants by giving them choices on participation (e.g., they could choose to speak or not during group discussions) and practices (e.g., they could choose the type of practice that work better for them during their homework practice, such as body scan meditation, breathing awareness meditation or yoga/mindful movement). Skills taught in the program included body scan meditation during which subjects slowly moved attention to each part of the body, mindful yoga which was a gentle form of yoga that emphasized awareness to body movements instead of the exercise aspect, open awareness meditation during which attention was on anything that came into awareness at each moment, and breath awareness meditation during which the focus of awareness was on breathing, as well as loving-kindness meditation during which mantra were repeated to send kind wishes to people of choice, e.g., “May you/I/my wife be happy, healthy and strong.” Subjects were instructed to keep a daily log of how many minutes they practiced each skill at home. Subjects on the waiting list were instructed to keep a daily log about their stress level and the things they did for stress reduction (e.g., hobbies).
A total of 34 subjects completed both testing time points or the two corresponding time points for the waiting list control. Among them, four subjects completed the mindfulness program after their waiting period, and thus contributed data from three time points: baseline, post-waiting period and post-intervention (Figure 1). Questionnaire data was extracted from the REDCap platform (Harris et al., 2009), and scored with scripts written in MATLAB® R2012a (The MathWorks, Inc.).
Missing data was an issue for some research questionnaires, due to reasons such as subjects did not answer some items in a particular questionnaire or did not submit response to several questionnaires. If a subject did not answer some items in a certain questionnaire, or did not respond to the whole questionnaire, this subject’s data of this questionnaire at this particular assessment time point was discarded (i.e., marked as missing data) from further analysis. We reported the subject number (N) or degree of freedom (df) for each statistical analysis of each research questionnaire.
We first used ANCOVA, with group, age, sex, race and time-interval as covariates, to test whether the two groups had significant difference at baseline before the intervention. Then we used linear mixed effects models (Lindstrom and Bates, 1988) to evaluate the treatment effects on BDI, STAI-t, PSS, MAAS, and SCS. We used the implementation of this method in the “lme” function of the “nlme” package in R. The scores of each of the above-mentioned scales were used as the response/dependent variable for each model, with group (i.e., mindfulness or waiting list) and time point (i.e., before or after the intervention) as independent variables, and group by time interaction was the effect of interest in each model. In all models we used age, sex, ethnicity, and time-interval between the two measurements as covariates. Separate variance for each group and time point was used in all models. “REML” method was chosen in all models to maximize the restricted log-likelihood. We used the “r.squaredGLMM” function of the “MuMIn” package in R to estimate the percentage of variance explained in each linear mixed effects model. To obtain an effect size measure, we used the “ANOVA” function in R to compare each model with the alternative model without the factor of interest, which outputs the likelihood ratio and p-value as measurements of effect size. To test whether there was significant change after the intervention within the mindfulness group, we conducted further analysis with the “lmer” function in the “lme4” package of R, with age, sex, ethnicity and time-interval as covariates.
We used Pearson correlations to evaluate the relationships between variables of interest, and partial correlations to control for certain factors in the correlation analyses; in all correlation analyses we excluded cases with missing data in a “pairwise” manner.
Causal Mediation Analysis package in R (Tingley et al., 2014) was used to further investigate the relationships among score changes of research questionnaires. All subjects in both groups were included in the mediation analyses. The mediation analysis used score change of symptoms (BDI, STAI-t and PSS) as dependent variables, mindfulness (MAAS) score change as independent variable, with self-compassion (SCS) score change as the mediator.
The two groups did not differ significantly in the distribution of sex [χ2(1, N = 38) = 0.320, p = 0.724) and race [χ2(4, N = 38) = 3.611, p = 0.579]. The two groups did not have any significant difference on employment status [χ2(4, N = 38) = 5.911, p = 0.206] or marital status [χ2(2, N = 38) = 0.266, p = 0.876]. The two groups had a marginally significant difference in age with the mindfulness group slightly older [t(36) = −1.755, p = 0.088], and a marginally significant difference in the interval between their two visits [t(36) = −1.764, p = 0.089] with the mindfulness group slightly longer due to the longer time interval of the four subjects from the waiting list. The two groups did not have significant difference in any of the assessments on childhood maltreatment or lifetime DSM diagnoses. Detailed information about subject demographics are listed in Table 1. Detailed childhood maltreatment assessment scores for each group are listed in Table 2. Percentages of DSM diagnoses in each group are listed in Table 3. Compliance of intervention session participation and homework practice in the mindfulness group is summarized in Table 4.
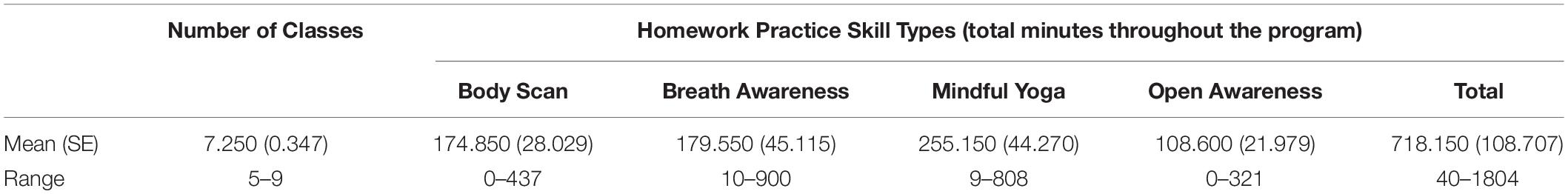
Table 4. Average number of class attended and minutes of homework practice in the mindfulness group.
ANCOVA analyses, with age, sex, race and time-interval as covariates, showed there were no group differences at baseline on any of the questionnaires (p > 0.25). Multivariate ANCOVA analyses, with group, age, sex, race and time-interval as covariates, showed no significant difference related to employment status [F(16,4) = 0.791, p = 0.676) or marital status [F(16,4) = 2.131, p = 0.243).
Fixed effects in the linear mixed effects model of STAI-t explained 19.49% of variance (Likelihood Ratio = 21.172, p = 0.032), and there was a significant group by time interaction effect [F(1,36) = 7.079, p = 0.012), with the mindfulness group having significant score reduction after the intervention [F(1,19) = 8.674, p = 0.008) while the waiting list control group had no significant change; the group by time interaction explained 2.92% of the variance in addition to the demographic covariates that explained 16.57% of the variance. The estimated marginal means for each group at each time point as well as their variance standard error (SE) are plotted in Figure 2A. To test whether history of childhood maltreatment was a moderator, we built another model to evaluate the 3-way interaction effect of “group” by “time” by “MACE-total severity scores of all types of maltreatment”. Fixed effects in this model explained 22.82% of variance (Likelihood Ratio = 30.562, p = 0.01), which was 3.33% more than the original model (Likelihood Ratio = 9.698, p = 0.046); there was a significant 3-way interaction [F(1,32) = 4.842, p = 0.035].
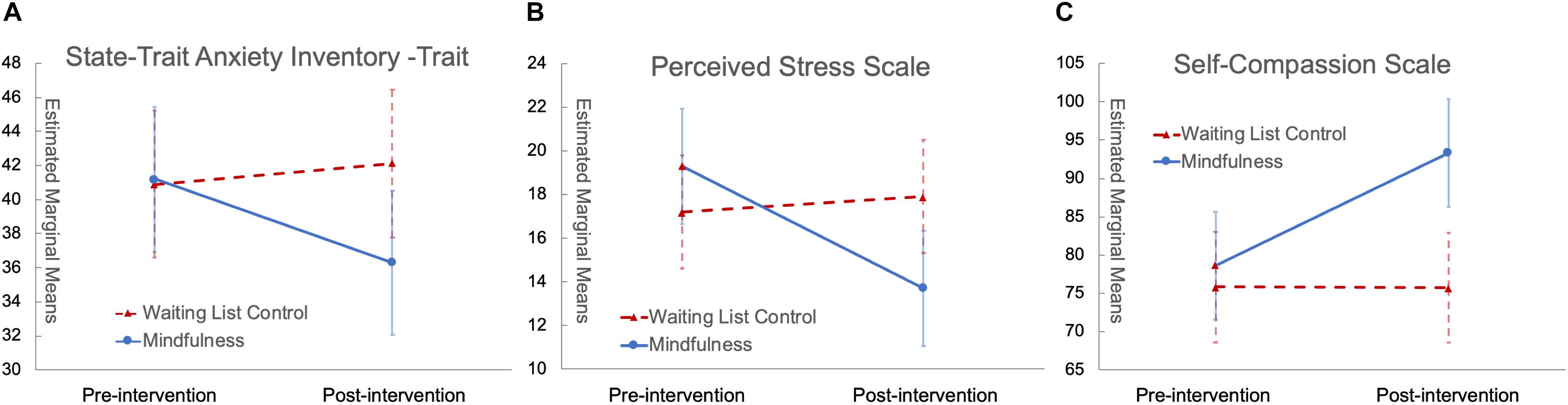
Figure 2. Significant group by time interaction with scores of STAI-t (A), PSS (B), and SCS (C). In all panels, red triangles with dashed red lines represent the control group while blue circles with solid blue lines represent the mindfulness group; error bars are standard errors.
Fixed effects in the linear mixed effects model of PSS explained 16.08% of the variance (Likelihood Ratio = 22.160, p = 0.023), and there was a significant group by time interaction effect [F(1,36) = 9.486, p = 0.004] with the mindfulness group having significant score reduction after the intervention [F(1,18.35) = 12.934, p = 0.002] while the waiting list control group had no significant change; the group by time interaction explained 6.40% of the variance in addition to the demographic covariates that explained 9.68% of the variance. The estimated marginal means for each group at each time point as well as their variance SE are plotted in Figure 2B.
The linear mixed effects models of BDI and MAAS did not reveal any significant group by time interaction effect, although the mindfulness group had significant score increase after the intervention [F(1,16.86) = 4.887, p = 0.041].
Fixed effects in the linear mixed effects model of SCS explained 22.77% variance (Likelihood Ratio = 28.448, p = 0.003), and there was a significant group by time interaction effect in the model [F(1,32) = 11.159, p = 0.002] with the mindfulness group having significant score increase after the intervention [F(1,15.46) = 21.094, p < 0.001] while the waiting list control group had no significant change; the group by time interaction effect explained 11.08% of the variance in addition to the demographic covariates that explained 11.69% of the variance. The estimated marginal means for each group at each time point as well as their variance SE are plotted in Figure 2C. Linear mixed effects models of SCS subscales found significant group by time interaction effects with Self-Kindness, Isolation, and Over-Identification (p < 0.05), with the mindfulness group having significant score increase in Self-Kindness, Common Humanity and Mindfulness and significant decrease in Self-Judgment, Isolation and Over-Identification (p < 0.05), while the waiting list control group had no significant change.
Partial correlation analyses showed that, with group and childhood maltreatment (as measured by MACE total severity of all types of maltreatment) as covariates, changes in mindfulness (as measured by MAAS scores) were significantly correlated with changes in self-compassion (as measured by SCS scores) among all subjects (r = 0.578, p = 0.001, df = 26). Partial correlation analyses in each group showed that after controlling for childhood maltreatment severity, changes in mindfulness and self-compassion were significantly correlated in the control group (r = 0.641, p = 0.018, df = 11) and marginally significantly correlated in the mindfulness group (r = 0.515, p = 0.059, df = 12) (Figure 3).
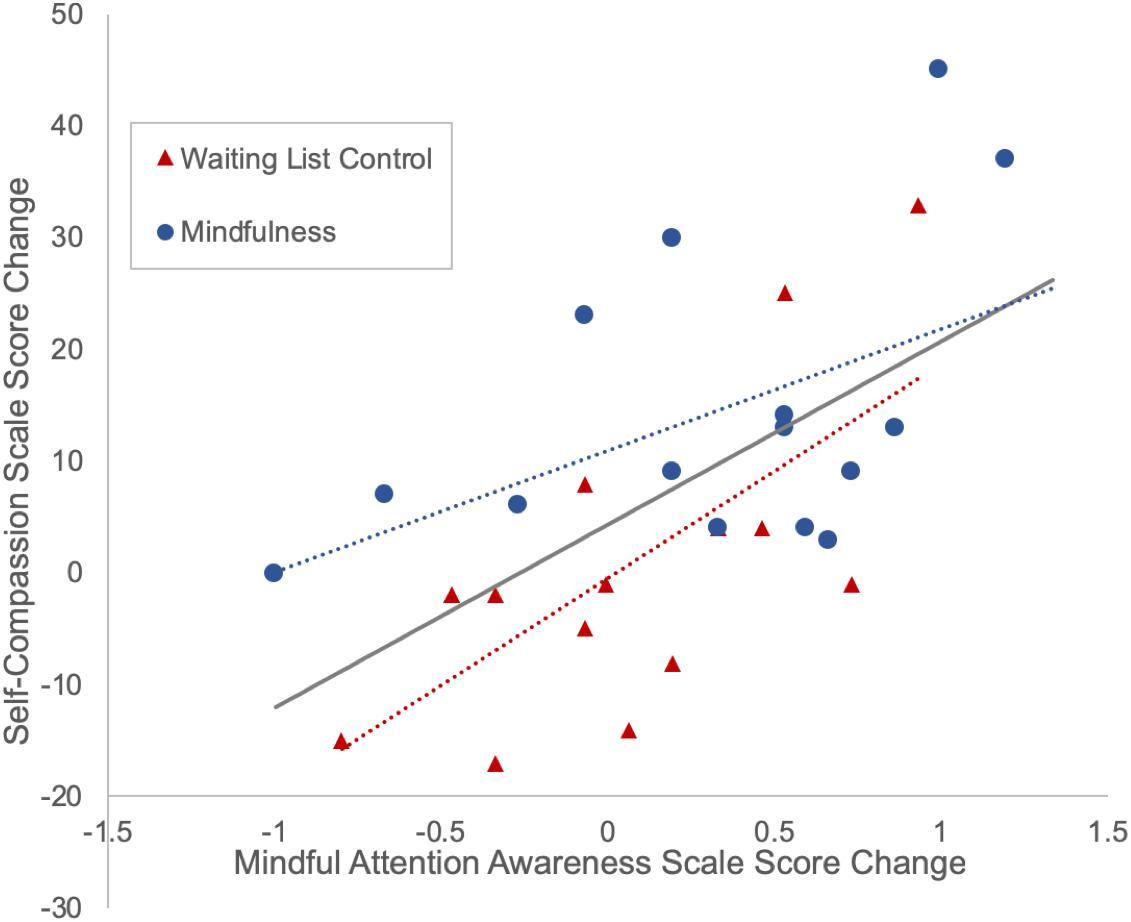
Figure 3. Positive correlation between changes in mindfulness and self-compassion. Subjects with more increase in mindfulness (measured by the Mindful Attention Awareness Scale) tend to have more increase in self-compassion (measured by the Self-Compassion Scale).
Partial correlation analyses, with group and childhood maltreatment as covariates, showed that changes in self-compassion were negatively correlated with changes in depression (SCS and BDI: r = −0.367, p = 0.05, df = 27) and anxiety (SCS and STAI-t: r = −0.395, p = 0.034, df = 27), while changes in perceived stress (as measured by PSS) were positively correlated with changes in depression (PSS and BDI: r = 0.591, p < 0.001, df = 30) and anxiety (PSS and STAI-t: r = 0.643, p < 0.001, df = 30) (Figure 4).
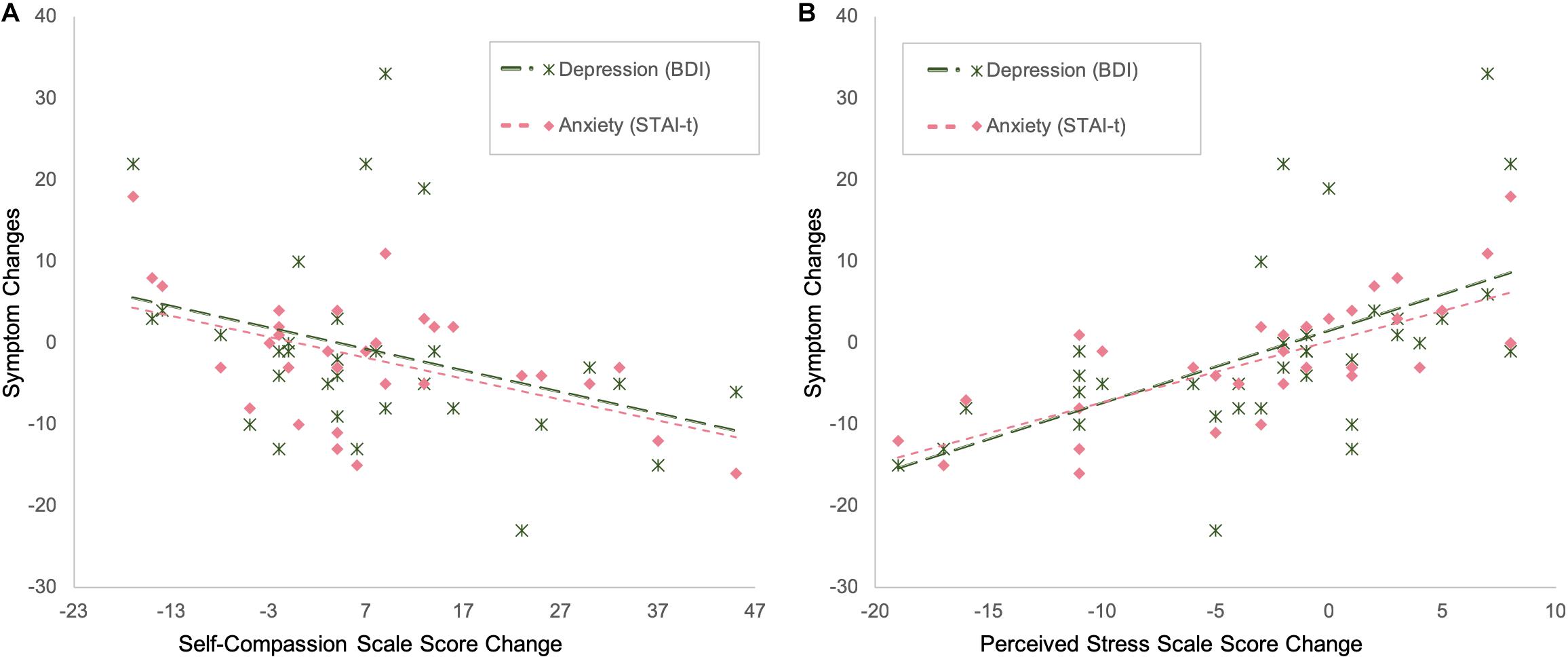
Figure 4. The amount of changes in depression and anxiety severity is negatively correlated with the amount of changes in self-compassion (A) and positively correlated with the amount of changes in stress (B).
The correlations between the score change of SCS subscales and other questionnaires are summarized in Table 5.
Mediation analyses revealed that changes in SCS score had a significant mediating effect between MAAS and STAI-t score changes (Average Causal Mediation Effect ACME = −4.721, p = 0.014) (Figure 5); SCS remained a significant mediator after including group and demographic factors as covariates (ACME) = −3.337, p = 0.05). Mediation analyses revealed that BDI score change was not mediated by SCS. In terms of PSS, there was a marginally significant meditation effect without any covariates in the model (ACME = −2.642, p = 0.057), but the effect was no longer significant after adding any covariate.
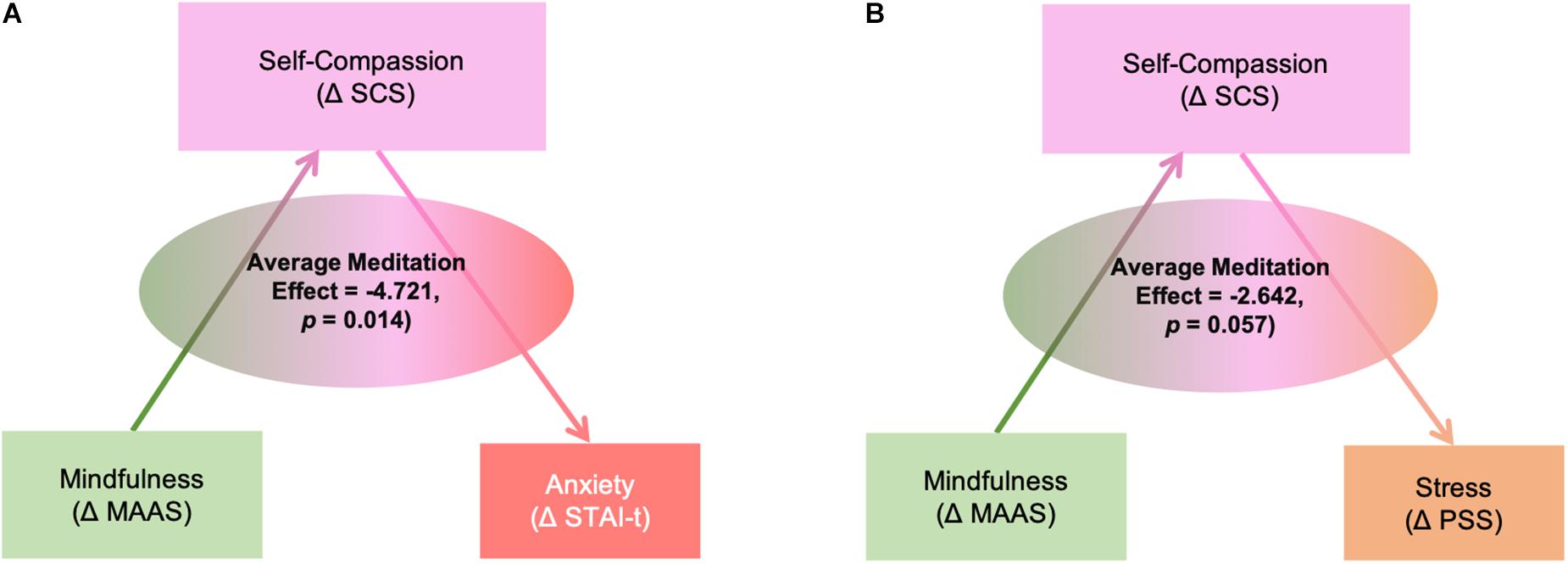
Figure 5. Mediation effects of self-compassion (ΔSCS: the amount of changes in scores of Self-Compassion Scale) between the changes in mindfulness (ΔMAAS: the amount of changes in scores of Mindful Attention Awareness Scale) and changes in anxiety (A) (ΔSTAI-t: the amount of changes in scores of State-Trait Anxiety Inventory-Trait subscale) and stress (B) (ΔPSS: the amount of changes in scores of Perceived Stress Scale).
In the mindfulness group, after controlling for the individual differences in childhood maltreatment severity, the number of intervention sessions attended was significantly associated with reduction in stress (correlation with changes in PSS: r = −0.674, p = 0.002, df = 16), anxiety (correlation with changes in STAI-t: r = −0.580, p = 0.009, df = 17), and depression (correlation with changes in BDI: r = −0.544, p = 0.020, df = 16) (Figure 6A).
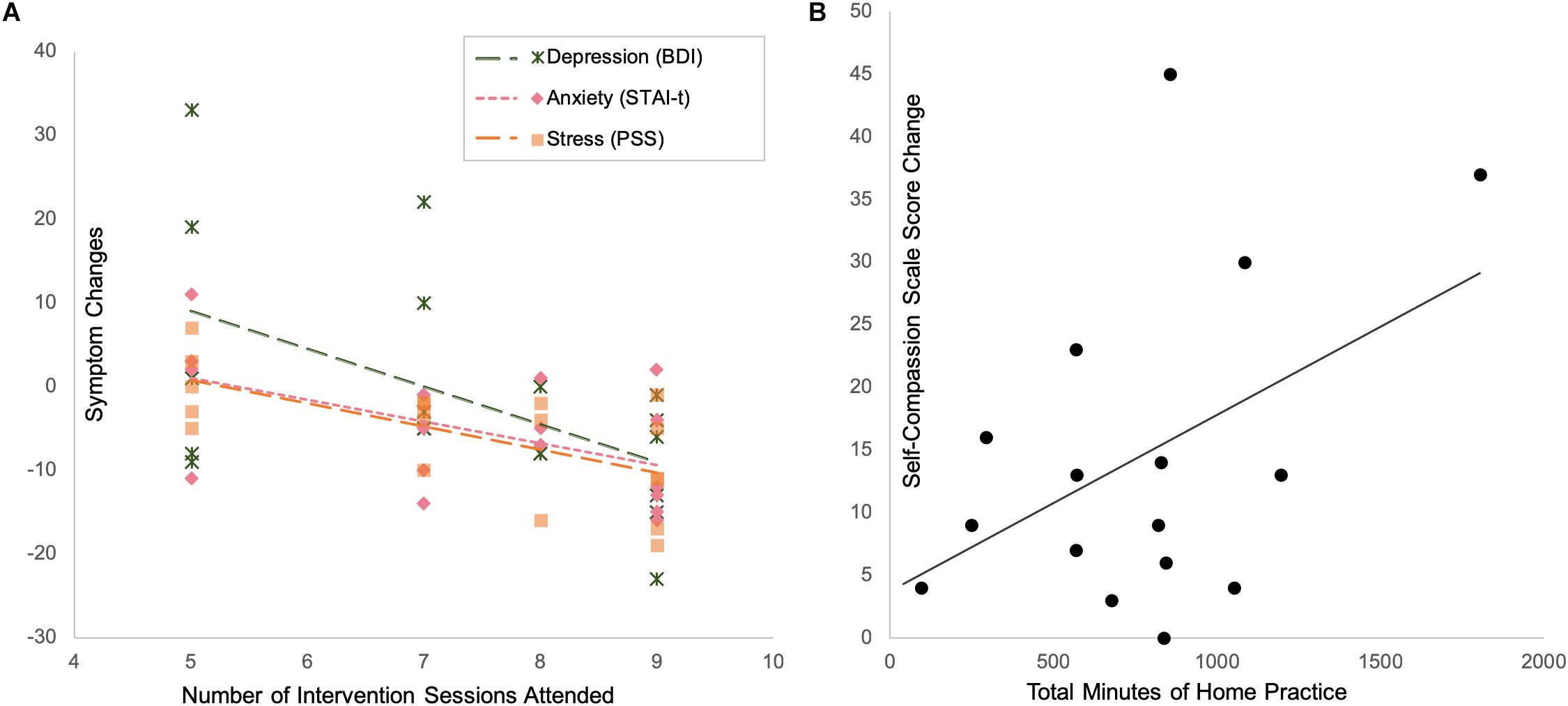
Figure 6. Intervention compliance and treatment effects: subjects who attended more intervention sessions had more reduction in depression, anxiety and stress (A), while subjects who practiced more at home had more increase in self-compassion (B).
With respect to the amount of homework practice, after controlling for the individual differences in childhood maltreatment severity, the reported total minutes of home practice were associated with increase in self-compassion (marginally significant correlation with changes in SCS scores: r = 0.468, p = 0.079, df = 13) (Figure 6B).
Partial correlation analyses, controlling for baseline symptom severity (pre-intervention STAI-t scores) and number of intervention sessions attended, showed that overall childhood maltreatment severity (measured by MACE-total severity scores of all types of maltreatment) negatively impacted the reduction in anxiety symptoms observed in the mindfulness group (positive correlation with changes in STAI-t scores, r = 0.678, p = 0.002, df = 16) (Figure 7A).
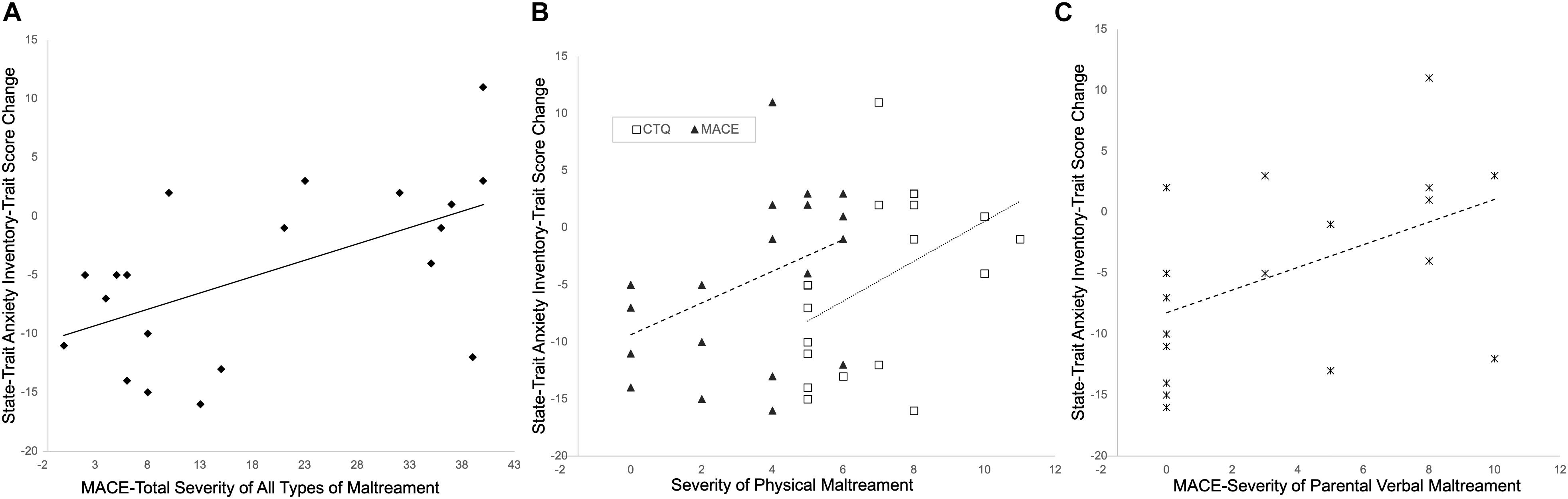
Figure 7. Childhood maltreatment negatively impacts treatment effects. Subjects with more severe maltreatment (A), or more severe physical maltreatment as measured by Childhood Trauma Questionnaire (CTQ) or MACE (B), or more severe parental verbal maltreatment (C), tend to have less reduction in anxiety symptoms.
The specific types of maltreatment most strongly associated with changes in STAI-t scores in the mindfulness group, after controlling for pre-intervention STAI-t scores and number of intervention sessions attended, were physical abuse scores on the CTQ (r = 0.666, p = 0.003, df = 16) and ratings of parental physical maltreatment on the MACE (r = 0.570, p = 0.014, df = 16) (Figure 7B), as well as severity of parental verbal abuse on the MACE (r = 0.653, p = 0.003, df = 16) (Figure 7C).
This pilot study indicates that a mindfulness based behavioral intervention can be helpful for relieving stress, depression and anxiety for young adults with a childhood maltreatment history. Findings from this study also suggest that increase in self-compassion plays an important role in the therapeutic effects of the intervention. Such findings add to the literature about alternative treatments for psychological symptoms among individuals with a history of childhood maltreatment.
Previously mindfulness based interventions have been adapted and applied to treating trauma-related psychopathology such as PTSD (for review see, Banks et al., 2015; Boyd et al., 2018). The theory (Lang et al., 2012) is that mindfulness practices involves purposeful allocation of attention, which helps traumatized individuals to overcome the negative bias in their cognition and the inability to inhibit irrelevant and unwanted information (Lang et al., 2012). The “present-focus” of mindfulness practices also helps to reduce worry and rumination (Greenberg et al., 2018), which is a common contributing factor to negative affect (McLaughlin et al., 2007). The “non-judgmental” aspect of mindfulness practices helps to counteract negative interpretation of internal and external experiences (Lang et al., 2012). Although not all forms of childhood maltreatment meet the DSM definition of trauma, and only a small percentage of young adults with a childhood maltreatment history meet the DSM criteria of PTSD (Teicher et al., 2012), childhood maltreatment affects individuals’ psychological health very similarly, as mentioned above (e.g., attention bias toward negative stimuli, excessive worry and rumination, and negative interpretation of internal and external experiences). Therefore, individuals with a childhood maltreatment history may obtain similar benefits from mindfulness practices.
Previous studies about the effect of mindfulness intervention in the general population rarely report measurements of childhood maltreatment. However, childhood maltreatment is very common and thus likely introduced unknown variability in the outcome measures. One study used “Measure of Parenting Style” as a measurement of childhood experience, and found that subjects with more episodes of depression tend to have more adverse childhood experience, but they did not find significant relationship between childhood maltreatment and treatment response (Ma and Teasdale, 2004). Another study showed a mindfulness based cognitive therapy treatment was particularly helpful for protecting relapse prevention among patients with recurrent depression who had a history of childhood maltreatment (Williams et al., 2014). The present study observed increased mindfulness and reduced stress after the mindfulness based intervention, which is consistent with previous findings on the effect of mindfulness based interventions (Shapiro et al., 2005; Shapiro et al., 2007; Carmody and Baer, 2008; Baer et al., 2012a; Chin et al., 2019). The present study even observed a dose-dependent effect between the number of intervention sessions attended and symptom reduction. These findings confirm the efficacy of the mindfulness-based intervention for reducing stress in this population.
Furthermore, the present study also observed increased self-compassion after the mindfulness intervention. A previous study also found increased self-compassion after the mindfulness based stress reduction program (Birnie et al., 2010), while another study found that self-compassion is a significant predictor of psychological wellbeing among meditators (Baer et al., 2012b). Childhood maltreatment often leads to low self-esteem (Stein et al., 2002; Bungert et al., 2015) and self-criticism (Dunkley et al., 2010), which in turn contributes to other psychological health issues (Stein et al., 2002; Dunkley et al., 2010; Bungert et al., 2015). Therefore, promoting self-compassion seems to be a necessary step toward alleviating psychological symptoms influenced by childhood maltreatment. In the present study, increase in self-compassion is a significant mediator between mindfulness and symptom reduction, which is consistent with a previous study that suggests self-compassion is a better predictor than mindfulness for symptom severity of depression and anxiety among a large community sample (Van Dam et al., 2011). The present finding highlights the importance of self-compassion for treating psychological symptoms of individuals with a childhood maltreatment history.
Although self-compassion was not explicitly taught as part of the mindfulness based intervention program, self-care and self-awareness were emphasized throughout the intervention, and participants were also taught a “loving-kindness” meditation exercise in the later weeks of the program, which included kind wishes to people of choice, e.g., “May you/I be happy, healthy and strong.” These elements might have helped the cultivation of self-compassion. Furthermore, the non-judgmental and present-focused properties of mindfulness practices naturally set the stage for developing self-compassion by encouraging participants to be open and accepting of their inner experience. Future studies may consider investigating whether this population would benefit from interventions that are explicitly focused on improving self-compassion, such as the mindful self-compassion program developed by Neff and Germer (2013).
The severity of childhood maltreatment appeared to have negatively impacted the efficacy of the intervention. Individuals with more severe childhood maltreatment had less reduction in anxiety symptoms, especially individuals with more severe parental physical or verbal maltreatment. Our finding is consistent with the existing literature that individuals with a childhood maltreatment history are difficult to treat (e.g., Shamseddeen et al., 2011; Harkness et al., 2012; Tunnard et al., 2014). Such results bring up the possibility that this mindfulness-based program might have limited benefits for individuals with severe childhood maltreatment, who might require a longer program or multiple treatment approaches, such as a combination of individual psychotherapy, group therapy, mindfulness practice and explicit self-compassion training.
There are several limitations in the present study, including (1) a relatively small sample, which limits the generalizability of the findings; (2) a waiting list control instead of an active control condition, which could have been confounded by placebo effects; (3) subjects were not randomized, but were rather assigned based on their availability to attend the intervention sessions, which could have resulted in the two groups being different, e.g., subjects on the waiting list group might have busier schedules. Although the two groups had no significant difference on their baseline stress levels or any of the psychological instruments used in the present study, they could have been different on some unmeasured factors. Therefore, strict randomization procedures shall be applied on future studies. (4) subjects were not followed up with after they finished the program to observe the long-term effect of the intervention; future studies that include long term follow up assessments can help understand how long the benefits from the intervention can last. (5) subjects were predominantly female, future studies should recruit more male participants. (6) lack of comprehensive information about subjects’ personality and social support system limit our understanding about potential societal factors that could contribute to treatment effects. (7) stress is a multifaceted concept, we only measured subjects’ subjective report of perceived stress, more comprehensive measurement that includes biological markers of stress could reveal more information about the treatment’s effect on stress response. (8) most subjects in this study only had mild to moderate psychological symptoms, which limits the generalizability of the study to more symptomatic patients.
This pilot study provided promising initial findings that young adults with a childhood trauma history can benefit from a mindfulness-based intervention. Given that this population tends to be resistant to traditional treatments, mindfulness-based interventions are worth considering as one of the alternative treatment approaches for psychological symptoms related to childhood maltreatment.
The datasets generated for this study are available on request to the corresponding author.
This study was reviewed and approved by the Institutional Review Board (IRB) (IRB#: 2014P000295) of Partners HealthCare, which is the IRB for Massachusetts General Hospital, McLean Hospital, and several other major hospitals in the Boston area. The patients/participants provided their written informed consent to participate in this study.
DJ and SL planned the experiments and supervised the intervention programs. AK performed clinical screening for all subjects. MT provided subject database with all childhood maltreatment assessments. DJ conducted the experiments and data analyses and drafted the manuscript. All authors contributed to the final version of the manuscript.
This study was partly supported by a Varela award from the Mind and Life Institute. The Athinoula A. Martinos Center for Biomedical Imaging provided discounted MRI time that made the MRI component of the study possible. DJ was supported by funding from NIH (Grant No. 5K01AT009085) while working on this manuscript.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
We thank Zayda Vallejo for assistance with modification of the MBSR program into the trauma-sensitive mindfulness-based intervention used in the current study, and Lauri J. Klein and David Schouela for teaching the intervention sessions. We thank Elizabeth A. Bolger, Cynthia E. McGreenery, Hannah C. McCormack, Laura Doyle, Callum Roberts, and Asama Lekbua for their assistance with the logistics of the study. We also thank the research participants for volunteering in this research study without receiving monetary compensation.
Andrews, B. (1998). “Shame and childhood abuse,” in Shame: Interpersonal Behavior, Psychopathology, and Culture, eds P. Gilbert and B. Andrews (New York, NY: Oxford University Press), 176–190.
Baer, R. A., Carmody, J., and Hunsinger, M. (2012a). Weekly change in mindfulness and perceived stress in a mindfulness-based stress reduction program. J. Clin. Psychol. 68, 755–765. doi: 10.1002/jclp.21865
Baer, R. A., Lykins, E. L., and Peters, J. R. (2012b). Mindfulness and self-compassion as predictors of psychological wellbeing in long-term meditators and matched nonmeditators. J. Posit. Psychol. 7, 230–238. doi: 10.1080/17439760.2012.674548
Baer, R. A., Smith, G. T., Hopkins, J., Krietemeyer, J., and Toney, L. (2006). Using self-report assessment methods to explore facets of mindfulness. Assessment 13, 27–45. doi: 10.1177/1073191105283504
Banks, K., Newman, E., and Saleem, J. (2015). An overview of the research on mindfulness-based interventions for treating symptoms of posttraumatic stress disorder: a systematic review. J. Clin. Psychol. 71, 935–963. doi: 10.1002/jclp.22200
Beck, A. T., Steer, R. A., and Brown, G. K. (1996). Beck depression inventory-II. San Antonio 78, 490–498.
Bernet, C. Z., and Stein, M. B. (1999). Relationship of childhood maltreatment to the onset and course of major depression in adulthood. Depress. Anxiety 9, 169–174. doi: 10.1002/(sici)1520-6394(1999)9:4<169::aid-da4>3.3.co;2-u
Birnie, K., Speca, M., and Carlson, L. E. (2010). Exploring self-compassion and empathy in the context of mindfulness-based stress reduction (MBSR). Stress Health 26, 359–371. doi: 10.1002/smi.1305
Boyd, J. E., Lanius, R. A., and McKinnon, M. C. (2018). Mindfulness-based treatments for posttraumatic stress disorder: a review of the treatment literature and neurobiological evidence. J. Psychiatry Neurosci. 43, 7–25. doi: 10.1503/jpn.170021
Brown, K. W., and Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. J. Pers. Soc. Psychol. 84, 822–848. doi: 10.1037/0022-3514.84.4.822
Bungert, M., Liebke, L., Thome, J., Haeussler, K., Bohus, M., and Lis, S. (2015). Rejection sensitivity and symptom severity in patients with borderline personality disorder: effects of childhood maltreatment and self-esteem. Borderline Personal. Disord. Emot. Dysregul. 2:4. doi: 10.1186/s40479-015-0025-x
Carmody, J., and Baer, R. A. (2008). Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well-being in a mindfulness-based stress reduction program. J. Behav. Med. 31, 23–33. doi: 10.1007/s10865-007-9130-7
Chin, B., Slutsky, J., Raye, J., and Creswell, J. D. (2019). Mindfulness training reduces stress at work: a randomized controlled trial. Mindfulness 10, 627–638. doi: 10.1007/s12671-018-1022-1020
Cohen, S., Kamarck, T., and Mermelstein, R. (1994). “Perceived stress scale,” in Measuring Stress: A Guide for Health and Social Scientists, ed. R. C. Kessler (Oxford: Oxford University Press), 235–283.
Dorahy, M. J., and Clearwater, K. (2012). Shame and guilt in men exposed to childhood sexual abuse: a qualitative investigation. J. Child Sex Abuse 21, 155–175. doi: 10.1080/10538712.2012.659803
Dunkley, D. M., Masheb, R. M., and Grilo, C. M. (2010). Childhood maltreatment, depressive symptoms, and body dissatisfaction in patients with binge eating disorder: the mediating role of self-criticism. In. J. Eat. Disord. 43, 274–281. doi: 10.1002/eat.20796
Evans, S., Ferrando, S., Findler, M., Stowell, C., Smart, C., and Haglin, D. (2008). Mindfulness-based cognitive therapy for generalized anxiety disorder. J. Anxiety Disord. 22, 716–721. doi: 10.1016/j.janxdis.2007.07.005
Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., et al. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: the adverse childhood experiences (ACE) study. Am. J. Prev. Med. 14, 245–258. doi: 10.1016/s0749-3797(98)00017-8
Follette, V., Palm, K. M., and Pearson, A. N. (2006). Mindfulness and trauma: implications for treatment. J. Ration Emot. Cogn. Behav. Ther. 24, 45–61. doi: 10.1007/s10942-006-0025-2
Gard, T., Brach, N., Hölzel, B. K., Noggle, J. J., Conboy, L. A., and Lazar, S. W. (2012). Effects of a yoga-based intervention for young adults on quality of life and perceived stress: the potential mediating roles of mindfulness and self-compassion. J. Posit. Psychol. 7, 165–175. doi: 10.1080/17439760.2012.667144
Goldin, P. R., and Gross, J. J. (2010). Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion 10, 83–91. doi: 10.1037/a0018441
Greenberg, J., Datta, T., Shapero, B. G., Sevinc, G., Mischoulon, D., and Lazar, S. W. (2018). Compassionate hearts protect against wandering minds: self-compassion moderates the effect of mind-wandering on depression. Spiritual. Clin. Pract. 5, 155–169. doi: 10.1037/scp0000168
Harkness, K. L., Bagby, R. M., and Kennedy, S. H. (2012). Childhood maltreatment and differential treatment response and recurrence in adult major depressive disorder. J. Consult Clin. Psychol. 80, 342–353. doi: 10.1037/a0027665
Harris, P. A., Taylor, R., Thielke, R., Payne, J., Gonzalez, N., and Conde, J. G. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J. Biomed. Inform. 42, 377–381. doi: 10.1016/j.jbi.2008.08.010
Herman, J. L., Perry, C., and Van der Kolk, B. A. (1989). Childhood trauma in borderline personality disorder. Am. J. Psychiatry 146, 490–495. doi: 10.1176/ajp.146.4.490
Hoglund, C. L., and Nicholas, K. B. (1995). Shame, guilt, and anger in college students exposed to abusive family environments. J. Fam. Violence 10, 141–157. doi: 10.1007/bf02110597
Johnson, J. G., Cohen, P., Brown, J., Smailes, E. M., and Bernstein, D. P. (1999). Childhood maltreatment increases risk for personality disorders during early adulthood. Arch. Gen. Psychiatry 56, 600–606.
Kabat-Zinn, J. (1990). Full Catastrophe Living: Using the Wisdom of Your Body and Mind in Everyday Life. New York, NY: Delacorte.
Keller, M. B., Lavori, P. W., Friedman, B., Nielsen, E., Endicott, J., McDonald-Scott, P., et al. (1987). The longitudinal interval follow-up evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry 44, 540–548. doi: 10.1001/archpsyc.1987.01800180050009
Khan, A., McCormack, H. C., Bolger, E. A., McGreenery, C. E., Vitaliano, G., Polcari, A., et al. (2015). Childhood maltreatment, depression, and suicidal ideation: critical importance of parental and peer emotional abuse during developmental sensitive periods in males and females. Front. Psychiatry 6:42. doi: 10.3389/fpsyt.2015.00042
King, A. P., Erickson, T. M., Giardino, N. D., Favorite, T., Rauch, S. A., Robinson, E., et al. (2013). A pilot study of group mindfulness-based cognitive therapy (MBCT) for combat veterans with posttraumatic stress disorder (PTSD). Depress. Anxiety 30, 638–645. doi: 10.1002/da.22104
Kuyken, W., Warren, F. C., Taylor, R. S., Whalley, B., Crane, C., Bondolfi, G., et al. (2016). Efficacy of mindfulness-based cognitive therapy in prevention of depressive relapse: an individual patient data meta-analysis from randomized trials. JAMA Psychiatry 73, 565–574. doi: 10.1001/jamapsychiatry.2016.0076
Lang, A. J., Strauss, J. L., Bomyea, J., Bormann, J. E., Hickman, S. D., Good, R. C., et al. (2012). The theoretical and empirical basis for meditation as an intervention for PTSD. Behav. Modif. 36, 759–786. doi: 10.1177/0145445512441200
Lindstrom, M. J., and Bates, D. M. (1988). Newton-Raphson and EM algorithms for linear mixed-effects models for repeated-measures data. J. Am. Stat. Assoc. 83, 1014–1022. doi: 10.1080/01621459.1988.10478693
Linehan, M. M., Schmidt, H., Dimeff, L. A., Craft, J. C., Kanter, J., and Comtois, K. A. (1999). Dialectical behavior therapy for patients with borderline personality disorder and drug-dependence. Am. J. Addict. 8, 279–292. doi: 10.1080/105504999305686
Ma, S. H., and Teasdale, J. D. (2004). Mindfulness-based cognitive therapy for depression: replication and exploration of differential relapse prevention effects. J. Consult. Clin. Psychol. 72, 31–40. doi: 10.1037/0022-006x.72.1.31
McEvoy, P. M. (2019). Metacognitive therapy for anxiety disorders: a review of recent advances and future research directions. Curr. Psychiatry Rep. 21:29. doi: 10.1007/s11920-019-1014-3
McLaughlin, K. A., Borkovec, T. D., and Sibrava, N. J. (2007). The effects of worry and rumination on affect states and cognitive activity. Behav. Ther. 38, 23–38. doi: 10.1016/j.beth.2006.03.003
Moran, L. R., Kaplan, C., Aguirre, B., Galen, G., Stewart, J. G., Tarlow, N., et al. (2018). Treatment effects following residential dialectical behavior therapy for adolescents with borderline personality disorder. Evid. Based Pract. Child Adolesc. Ment. Health 3, 117–128. doi: 10.1080/23794925.2018.1476075
Nanni, V., Uher, R., and Danese, A. (2012). Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am. J. Psychiatry 169, 141–151. doi: 10.1176/appi.ajp.2011.11020335
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self Identity 2, 223–250. doi: 10.1080/15298860309027
Neff, K. D. (2016). The self-compassion scale is a valid and theoretically coherent measure of self-compassion. Mindfulness 7, 264–274. doi: 10.1007/s12671-015-0479-3
Neff, K. D., and Germer, C. K. (2013). A pilot study and randomized controlled trial of the mindful self-compassion program. J. Clin. Psychol. 69, 28–44. doi: 10.1002/jclp.21923
Pietrek, C., Elbert, T., Weierstall, R., Müller, O., and Rockstroh, B. (2013). Childhood adversities in relation to psychiatric disorders. Psychiatry Res. 206, 103–110. doi: 10.1016/j.psychres.2012.11.003
Rodrigues, M. F., Campos, C., Pelucio, L., Barreto, I., Machado, S., Appolinario, J. C., et al. (2019). Patients’ comprehension of mindfulness-based cognitive behavioral therapy in an outpatient clinic for resistant depression: a cross-sectional study. Front. Psychol. 10:271. doi: 10.3389/fpsyg.2019.00271
Roemer, L., and Orsillo, S. M. (2002). Expanding our conceptualization of and treatment for generalized anxiety disorder: integrating mindfulness/acceptance-based approaches with existing cognitive-behavioral models. Clin. Psychol. 9, 54–68. doi: 10.1093/clipsy.9.1.54
Santorelli, S. F., Kabat-Zinn, J., Blacker, M., Meleo-Meyer, F., and Koerbel, L. (2017). “Mindfulness-based stress reduction (MBSR) authorized curriculum guide,” in Center for Mindfulness in Medicine, Health Care, and Society (CFM), (Worcester, MA: University of Massachusetts Medical School).
Shamseddeen, W., Asarnow, J. R., Clarke, G., Vitiello, B., Wagner, K. D., Birmaher, B., et al. (2011). Impact of physical and sexual abuse on treatment response in the treatment of resistant depression in adolescent study (TORDIA). J. Am. Acad. Child Adolesc. Psychiatry 50, 293–301. doi: 10.1016/j.jaac.2010.11.019
Shapiro, S. L., Astin, J. A., Bishop, S. R., and Cordova, M. (2005). Mindfulness-based stress reduction for health care professionals: results from a randomized trial. Int. J. Stress Manag. 12, 164–176. doi: 10.1037/1072-5245.12.2.164
Shapiro, S. L., Brown, K. W., and Biegel, G. M. (2007). Teaching self-care to caregivers: effects of mindfulness-based stress reduction on the mental health of therapists in training. Train. Educ. Prof. Psychol. 1, 105–115. doi: 10.1037/1931-3918.1.2.105
Soler, J., Valdepérez, A., Feliu-Soler, A., Pascual, J. C., Portella, M. J., Martín-Blanco, A., et al. (2012). Effects of the dialectical behavioral therapy-mindfulness module on attention in patients with borderline personality disorder. Behav. Res. Therapy 50, 150–157. doi: 10.1016/j.brat.2011.12.002
Spielberger, C. D., and Sydeman, S. J. (1994). “State-Trait anxiety inventory and state-trait anger expression inventory,” in The Use of Psychological Testing for Treatment Planning and Outcome Assessment, ed. M. Maruish, (Hillsdale, NJ: Lawrence Erlbaum Associates).
Stein, J. A., Leslie, M. B., and Nyamathi, A. (2002). Relative contributions of parent substance use and childhood maltreatment to chronic homelessness, depression, and substance abuse problems among homeless women: mediating roles of self-esteem and abuse in adulthood. Child Abuse Neglect 26, 1011–1027. doi: 10.1016/s0145-2134(02)00382-4
Stuewig, J., and McCloskey, L. A. (2005). The relation of child maltreatment to shame and guilt among adolescents: psychological routes to depression and delinquency. Child Maltreat. 10, 324–336. doi: 10.1177/1077559505279308
Tanaka, M., Wekerle, C., Schmuck, M. L., Paglia-Boak, A., and Team, M. R. (2011). The linkages among childhood maltreatment, adolescent mental health, and self-compassion in child welfare adolescents. Child Abuse Neglect 35, 887–898. doi: 10.1016/j.chiabu.2011.07.003
Teicher, M. H., Anderson, C. M., and Polcari, A. (2012). Childhood maltreatment is associated with reduced volume in the hippocampal subfields CA3, dentate gyrus, and subiculum. Proc. Natl. Acad. Sci. U.S.A. 109, E563–E572. doi: 10.1073/pnas.1115396109
Teicher, M. H., and Parigger, A. (2015). The ‘maltreatment and abuse chronology of exposure’(MACE) scale for the retrospective assessment of abuse and neglect during development. PLoS One 10:e0117423. doi: 10.1371/journal.pone.0117423
Tingley, D., Yamamoto, T., Hirose, K., Keele, L., and Imai, K. (2014). Mediation: R package for causal mediation analysis. J. Stat. Softw. 59. doi: 10.18637/jss.v059.i05
Tunnard, C., Rane, L. J., Wooderson, S. C., Markopoulou, K., Poon, L., Fekadu, A., et al. (2014). The impact of childhood adversity on suicidality and clinical course in treatment-resistant depression. J. Affect. Disord. 152, 122–130. doi: 10.1016/j.jad.2013.06.037
Van Dam, N. T., Sheppard, S. C., Forsyth, J. P., and Earleywine, M. (2011). Self-compassion is a better predictor than mindfulness of symptom severity and quality of life in mixed anxiety and depression. J. Anxiety Disord. 25, 123–130. doi: 10.1016/j.janxdis.2010.08.011
Verheul, R., Van Den Bosch, L. M., Koeter, M. W., De Ridder, M. A., Stijnen, T., and Van Den Brink, W. (2003). Dialectical behaviour therapy for women with borderline personality disorder: 12-month, randomised clinical trial in the Netherlands. Br. J. Psychiatry 182, 135–140. doi: 10.1192/bjp.182.2.135
Vettese, L. C., Dyer, C. E., Li, W. L., and Wekerle, C. (2011). Does self-compassion mitigate the association between childhood maltreatment and later emotion regulation difficulties? a preliminary investigation. Int. J. Ment. Health Addict. 9, 480–491. doi: 10.1007/s11469-011-9340-7
Williams, J. M., Crane, C., Barnhofer, T., Brennan, K., Duggan, D. S., Fennell, M. J., et al. (2014). Mindfulness-based cognitive therapy for preventing relapse in recurrent depression: a randomized dismantling trial. J. Consult Clin. Psychol. 82, 275–286. doi: 10.1037/a0035036
World Health Organization (2016). Child Maltreatment [Online]. Available: https://www.who.int/news-room/fact-sheets/detail/child-maltreatment (accessed July 16, 2019).
Keywords: mindfulness, self-compassion, stress, childhood maltreatment, depression, anxiety
Citation: Joss D, Khan A, Lazar SW and Teicher MH (2019) Effects of a Mindfulness-Based Intervention on Self-Compassion and Psychological Health Among Young Adults With a History of Childhood Maltreatment. Front. Psychol. 10:2373. doi: 10.3389/fpsyg.2019.02373
Received: 15 May 2019; Accepted: 04 October 2019;
Published: 23 October 2019.
Edited by:
Barbara Colombo, Champlain College, United StatesReviewed by:
Jude Uzoma Ohaeri, University of Nigeria, Nsukka, NigeriaCopyright © 2019 Joss, Khan, Lazar and Teicher. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Diane Joss, ZGpvc3NAbWNsZWFuLmhhcnZhcmQuZWR1
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.