
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 23 July 2019
Sec. Health Psychology
Volume 10 - 2019 | https://doi.org/10.3389/fpsyg.2019.01664
The study examined the trajectories of health-related quality of life (HRQoL) and perceived social support (PSS) among people living with HIV (PLWH), with a special focus on gender differences. The participants included 252 PLWH (18% female) undergoing antiretroviral therapy. HRQoL (WHO Quality of Life-BREF; WHOQOL Group, 1998) and PSS (Berlin Social Support Scales; Schulz and Schwarzer, 2003) were measured three times at six-month intervals. Using a univariate approach, three trajectories of HRQoL and four trajectories of PSS were identified. Gender and relationship status were significant covariates for PSS only, with overrepresentation of single women in the increasing trajectory. The dual trajectory approach revealed a match in the decrease of HRQoL and PSS, but only for 31% of the sample. In fact, decreasing PSS co-occurred with increasing as well as stable HRQoL. There was no significant gender effect in this regard. Although a clear correspondence for decreasing trajectories exists, the findings also highlight a discrepancy between HRQoL and PSS changes that are unrelated to gender.
Over the last two decades, cutting-edge progress has occurred in the treatment and prevention of HIV infection, which has not only significantly reduced mortality and morbidity among people living with HIV (PLWH; Samji et al., 2013; Cohen et al., 2016) but has also been attributed to signaling the end of the HIV/AIDS epidemic (Deeks et al., 2013; Carrico, 2019). However, the enormous progress in bio-medical care for PLWH did not directly translate to the improvement of their psychological well-being. More specifically, both in the past (e.g., Bing et al., 2001) and at present, PLWH systematically declare lower levels of well-being and higher psychological distress than the general population (Miners et al., 2014), and especially worse health-related quality of life (HRQoL) with respect to other chronic diseases (Psaros et al., 2013).
Although a large number of studies have been conducted on factors related to the HRQoL of these patients (e.g., Burgoyne and Saunders, 2001; Hansen et al., 2009; Herrmann et al., 2013; Bucciardini et al., 2014; Lifson et al., 2017; Mitchell et al., 2017; Torres et al., 2018), they failed not only to provide a consistent picture of the variables associated with the HRQoL of PLWH but also to produce a convincing answer to the aforementioned issue of low well-being among PLWH, especially at a time when their life expectancies are similar to the general population (Degroote et al., 2014). The only visible trend deals with the fact that clinical factors have been historically considered as the predominant predictor of the well-being of PLWH (Lubeck and Fries, 1997), while there is now a growing recognition of psychosocial factors as the major determinant of their quality of life (Chida and Vedhara, 2009; Cooper et al., 2017). Some authors underline that the plethora of inconclusive results in research on HRQoL among PLWH is derived from methodological shortcomings among most studies on this topic. Notably, the literature is dominated by cross-sectional frameworks using the variable-centered approach, which focuses only on the average values for an entire study sample and neglects the heterogeneity of well-being among PLWH and its relationship with sociodemographic, clinical, and psychological characteristics (Oberjé et al., 2015; Rzeszutek and Gruszczyńska, 2018). Therefore, the present study aims to overcome these methodological drawbacks by applying a longitudinal design accompanied by a person-centered perspective that allows for the identification of subgroups with different levels of HRQoL and their changes during time. Specifically, we aim to enrich the literature by focusing on the relatively understudied issue of gender-based differences in HRQoL among PLWH.
Surprisingly, although the global amount of HIV-infected women is similar to the number of HIV-infected men, both of which continue to grow worldwide (European Centre for Disease Prevention and Control/WHO Regional Office for Europe, 2017), the majority of studies on HRQoL in HIV infection were conducted on male populations only (e.g., Jia et al., 2004; Liu et al., 2006; Song et al., 2016; Emuren et al., 2017). Thus, research on HRQoL among HIV-infected women remains scarce (e.g., McDonnell et al., 2000; Gielen et al., 2001). In addition, authors examining gender differences in HRQoL in this patient group consequently observed lower HRQoL among HIV-infected women than HIV-infected men (e.g., Campsmith et al., 2003; Mrus et al., 2005; Chandra et al., 2009). There are several hypotheses on this consistent finding that have pointed to the limited access to antiretroviral treatment (ART) in some world regions (Penniman et al., 2007; Aziz and Smith, 2011), more intense HIV-related stigma, and an associated higher rate of mental disorders among HIV-infected women than HIV-infected men (Campbell et al., 2006; Machtinger et al., 2012; Geary et al., 2014). On the other hand, several studies have demonstrated that females living with HIV exhibit far greater adherence to treatment than their male counterparts and therefore report better HIV-related clinical outcomes (Collazos et al., 2007; Nicastri et al., 2007; Bor et al., 2015). In considering the aforementioned findings, it seems that no comprehensive explanation for the observed gender differences in HRQoL among PLWH exists to date. As such, the present study examines one variable that may provide important context on this topic – social support (Carvalhal, 2010).
HIV/AIDS is a chronic disease that promotes multidimensional psychological distress among PLWH, which is now primarily associated with persistent HIV-related stigma and social isolation (Rendina et al., 2018). Many studies have observed that social support – particularly perceived social support (PSS) – is one of the most important assets in coping with HIV infection and related distress (e.g., Turner-Cobb et al., 2002; Gonzalez et al., 2004; Earnshaw et al., 2015). More specifically, perceiving a high availability of support may enhance adjustment to HIV infection directly through improved adherence to treatment (e.g., Ashton et al., 2005; Alemu et al., 2012) and also indirectly through buffering the effect of HIV-related stigma on mental functioning and quality of life among these patients (Bekele et al., 2013; Breet et al., 2014).
Although the beneficial effects of perceived support on quality of life of PLWH are widely known, some authors have recently become increasingly skeptical regarding this unambiguously optimistic picture and have highlighted several methodological shortcomings of existing studies conducted using a cross-sectional framework, which is the most common (Qiao et al., 2014). Consequently, it is difficult to solve the egg or chicken dilemma in research on the link between perceived social support and HRQoL among PLWH. Notably, existing studies have been conducted in small samples (since the implementation of a repeated measurement design among PLWH may be challenging; Burgoyne and Renwick, 2004) or using only a baseline assessment of PSS as a predictor for HRQoL changes (Jia et al., 2005). Thus, the current literature has not examined possible heterogeneity of the dual trajectories of HRQoL and PSS. Furthermore, another topic that remains understudied in the literature deals with gender differences in both PSS and HRQoL among PLWH (Gordillo et al., 2009).
In considering the aforementioned research gaps, the aim of our study was three-fold. First, we aimed to examine whether heterogeneity of univariate change of HRQoL and PSS exists among PLWH, and if these trajectories are also gender-related, both with and without other possible sociodemographic and clinical covariates. Then, the probability of following a given pattern of the dual trajectories of HRQoL and PSS was explored. Specifically, we were interested in the co-occurrence of trajectories with the same direction of change, under the assumption of existing cross-sectional studies that a decrease or an increase in HRQoL corresponds to relevant changes in PSS. Finally, we examined whether any gender differences in joint probability for dual trajectories existed, supposing that combinations of changes may not be equally distributed due to gender-related patterns of social exchange as well as the social consequences of being diagnosed with HIV.
The participants were 252 persons with confirmed HIV-positive results undergoing antiretroviral therapy in an outpatient clinic. The majority of them were men, which is typical based on the gender-related prevalence rate of HIV infection in Europe and the United States (Joint United Nations Programme on HIV/AIDS (UNAIDS), 2018). Detailed characteristics of the sample are provided in Table 1.
The study design was longitudinal, with three measurements at 6-month intervals. After written informed consent was obtained from a participant, they filled in the self-descriptive questionnaire provided. For the next two measurements, they were approached during their control visit in the outpatient clinic after establishing the date via phone or email, based on their preference. All longitudinal data were collected by trained research assistants using a “paper-and-pencil” approach. Participation in the study was voluntary. The study was approved by the institutional ethics committee.
Health-related quality of life was assessed using the WHO Quality of Life-BREF (WHOQOL-BREF), developed under a WHO initiative for cross-cultural assessment (WHOQOL Group, 1998). The tool consists of 26 items to measure four domains: physical health, psychological health, social relationships, and environment. Each item is rated on a five-point Likert scale (scores ranged from 1 to 5), and raw scores were used. Since correlations between domains in our study were stable and moderate (from 0.48 to 0.69), and followed the research indicating a possibility of assessing global HRQoL using this tool (Harsha et al., 2016), the overall indicator was obtained by summing and averaging all item scores. Higher values indicate a higher quality of life. The reliability, measured by the Cronbach’s α coefficient, was 0.93, 0.92, and 0.92, from the first to third wave, respectively.
Perceived social support was measured using the relevant subscale of eight items from the Berlin Social Support Scales developed by Schulz and Schwarzer (2003). The answers are provided on a Likert-type scale, from 1 (not true at all) to 4 (entirely true), then summed and averaged. The higher scores indicate higher PSS. The Cronbach’s α coefficient was 0.93, 0.92, and 0.92, for first, second, and third measurement, respectively.
We started the analysis with univariate latent class growth curve models to examine how HRQoL and PSS changed in our sample during the study period. From 1- to 5-class solutions were tested separately for HRQoL and PSS, and error variances and covariances were freely estimated across classes. The optimal solution was identified on the basis of several criteria widely identified in the literature (Nylund et al., 2007). Namely, we used Akaike as well as Bayesian information criterion (AIC and BIC, respectively), including the sample size-adjusted BIC (SABIC). The model with lower values was favored. Next, entropy as a measure of accuracy of classification was taken into consideration; in this case, the model with higher values was favored (Celeux and Soromenho, 1996). Finally, sample proportion per class was analyzed, since classes with very few individuals may be sample-specific and difficult to replicate. The practical rule is to favor a model with a fewer number of classes when at least one class has a frequency of less than 5% of the sample size (Hipp and Bauer, 2006). Time was coded as 0 for the first measurement, 0.5 for the second, and 1 for the third (Biesanz et al., 2004). Both linear and quadratic trends were explored, but we did not present them further since all quadratic terms were revealed as insignificant.
To identify covariates of trajectories, the bias-adjusted three-step analysis (Vermunt and Magidson, 2016) was implemented in order (1) to separate modeling trajectories from their relationship with other variables and (2) to correct for probabilistic classification to classes. Namely, when univariate models were established (e.g., the number, shape, and membership of trajectories were fixed), we examined whether any differences existed in predicting this membership based on sociodemographic and clinical variables. We started with gender and then added other covariates to determine if they would modify the gender effect.
In the next step, joint probabilities were computed since we used two sets of trajectories (one for HRQoL and the other for PSS). Specifically, we were interested in the probability of belonging to a given trajectory of HRQoL when simultaneously being a member of a given trajectory of PSS. Finally, by means of multinomial logistic regression, we assessed whether the probability of being a member of each combination of HRQoL and PSS trajectories was the same for women and men, both with and without additional covariates. All analyses were performed using IBM SPSS Statistics version 25 (IBM Corp, 2016) and LatentGOLD version 5.1 (Vermunt and Magidson, 2016).
Table 2 presents basic descriptive statistics for repeated measures of HRQoL and PSS. The dropout due to longitudinal design was 41% of the sample between the first and last measurements. Missing data analysis suggested that the pattern of missingness can be treated as random (Little’s MCAR test: χ2 = 53.32, df = 54, p = 0.50); therefore, the option that included all available data was chosen, with missing values for indicators being handled by the maximum likelihood function (Vermunt and Magidson, 2016). Furthermore, regarding sociodemographic and clinical variables, there were also no significant differences between completers and non-completers. However, the result for gender was on the edge of significance (χ2 = 3.95, df = 1, p = 0.05), suggesting a tendency of higher dropout among women than men.
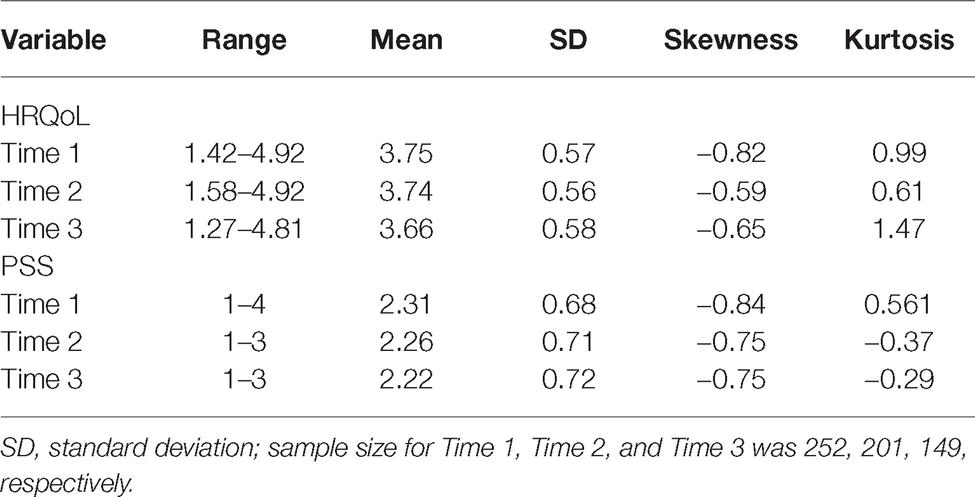
Table 2. Descriptive statistics for health-related quality of life (HRQoL) and perceived social support (PSS).
The model fit criteria indicate that model with three trajectories was the best fitted to the HRQoL data (see Table 3). Specifically, although all the informative criteria indices scored lower with every added class, the drop in value became smaller. For models with more than three classes, the smallest class had only four members, which suggests the existence of outliners. Finally, entropy was relatively stable across all models, indicating that the perfect classification of participants was challenging. Average posterior probabilities were 0.79, 0.93, and 0.81 for classes 1, 2, and 3, respectively. This solution is plotted in Figure 1.
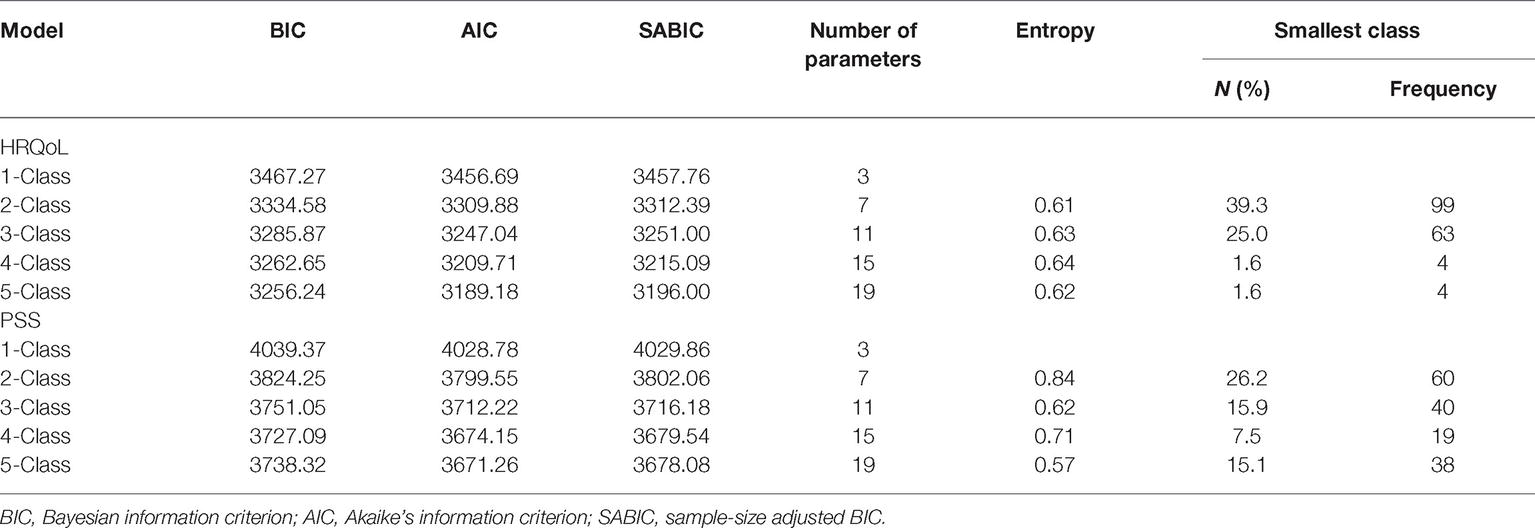
Table 3. Summary of model selection indices of latent class growth curve analysis: Unconditional univariate models for health-related quality of life (HRQoL) and perceived social support (PSS).
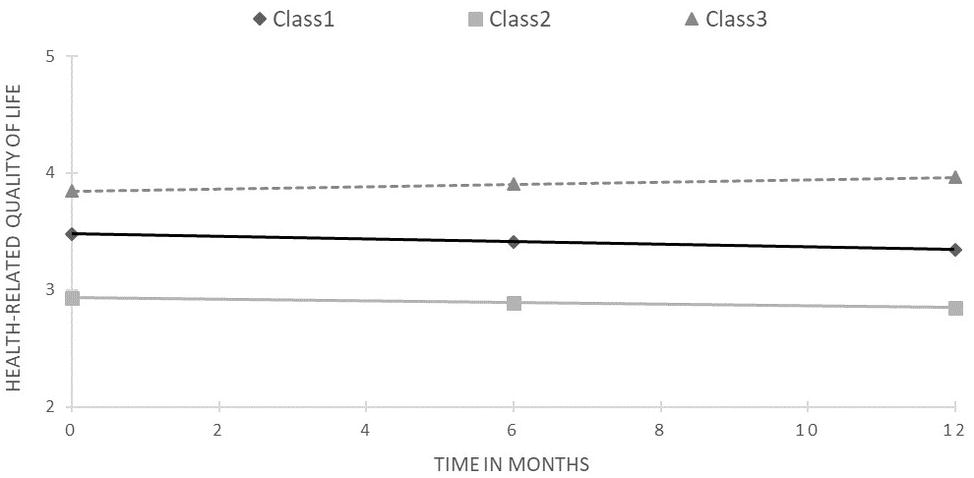
Figure 1. Results of latent class growth curve analysis for health-related quality of life (unconditional model).
The starting points differed significantly across trajectories (overall Wald statistics = 14101.81, p < 0.001; for all pairwise comparisons p < 0.001). The first class was the most numerous, containing 45.6% of the sample, for whom HRQoL significantly decreased during the study period (slope = −0.13, z = 2.55, p < 0.02). The second class, with the lowest and most stable HRQoL (slope = −0.08, z = −0.86, ns), was represented by 29.4% of the sample. Finally, the third class included 25% of PLWH and exhibited the highest and increasing HRQoL (slope = 0.12, z = 1.98, p < 0.05).
For PSS, the 4-class solution was chosen as the best fitted to the data due to the lowest BIC and SABIC values, and highest accuracy of classification, while retaining a reasonable size for the smallest class. Moreover, this decision was supported by visibly worse performance on all these criteria by the 5-class model (see Table 3). Average posterior probabilities ranged from 0.78 for class 2 to 0.89 for class 1. Figure 2 presents the obtained trajectories. The majority of the sample (63.1%) was allocated to the first class and exhibited decreasing PSS trajectory (slope = −0.19, z = −2.21, p < 0.05) with a middle starting point. The second class consisted of PLWH (14.3% of the sample) with a slightly higher starting point and increasing PSS (slope = 0.21, z = 2.36, p < 0.05). The highest and stable trajectory was represented by 15.1% of the sample, identified as class 3. On the other side was the smallest class 4 (7.5% of the sample) with the lowest and stable PSS, albeit with a noticeable tendency to decrease (slope = −0.23, z = −1.08, ns).
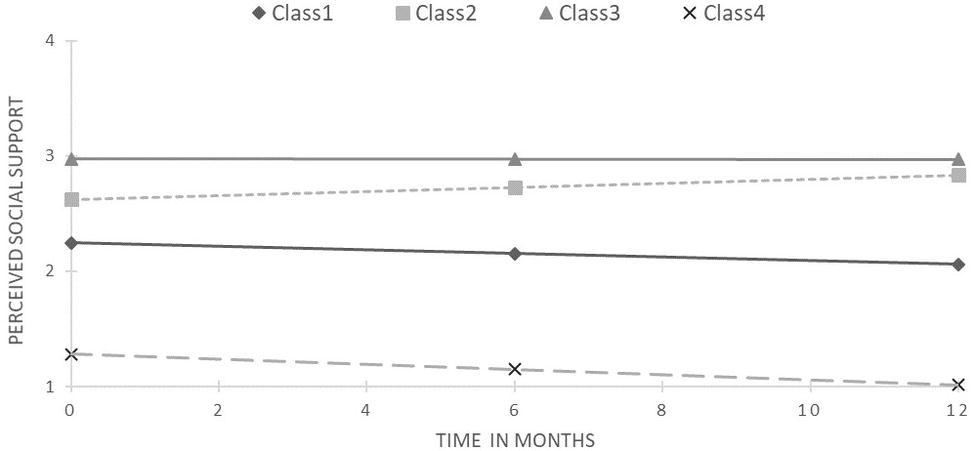
Figure 2. Results of latent class growth curve analysis for perceived social support (unconditional model).
When gender was added to the models as the only predictor of class membership, it was insignificant for both HRQoL (W = 4.71, ns) and PSS (W = 3.25, ns). When all the other covariates were included in the mode (i.e., age, education, relationship status, CD4 count, duration of being diagnosed with HIV infection, duration of antiretroviral therapy and being in the AIDS stage) for HRQoL, trajectories of gender remained insignificant. Significant effects were observed for age (W = 7.11, p < 0.05) and education (W = 8.77, p < 0.02). Specifically, PLWH in the decreasing HRQoL trajectory were older than the other two trajectories (41.2 vs. 36.8 and 37.7 years of age, respectively), and PLWH in the increasing HRQoL trajectory were better educated than those with the stable HRQoL trajectory.
For PSS, both gender (W = 674.39, p < 0.001) and relationship status (W = 9.02, p < 0.05) were significant correlates of PSS trajectories. Thus, an interaction of these variables was examined, revealing a significant effect between classes 1 and 2 (W = 196.56, p < 0.001). Compared to the decreasing trajectory, there was overrepresentation of single women in the increasing PSS trajectory.
Table 4 illustrates joint probability while accounting for both sets of heterogonous trajectories (i.e., for HRQoL and PSS simultaneously). It is evident that no clear correspondence exists between the trajectories of HRQoL and PSS. Although the highest probability was noted for the dual decreasing trajectory (0.31), the relatively high probability also points to the simultaneous membership of stable HRQoL and decreasing PSS. Likewise, approximately 11% of PLWH followed the increasing HRQoL and decreasing PSS trajectories concurrently. However, no members in the lowest and stable PSS reported an increase in HRQoL.
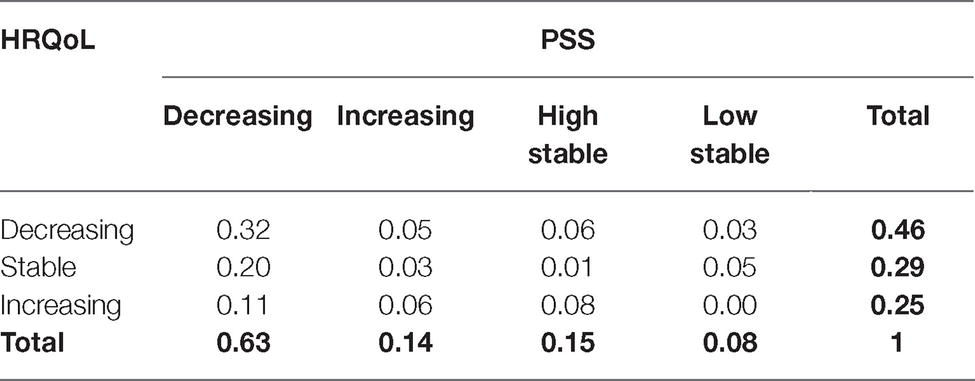
Table 4. Joint probability of membership for dual trajectories of health-related quality of life (HRQoL) and perceived social support (PSS).
Finally, considering joint probability, gender differences were examined with control for all the other sociodemographic and clinical variables. We focused on the dual trajectories combining the decreasing PSS and all HRQoL trajectories, since for all the other combinations the frequency was below 10% of the sample (see Table 4). The results of multinomial logistic regression with dual decreasing trajectories as a reference category showed no significant effect of gender alone (χ2 = 3.88, df = 2, p = 0.14) nor of any of the remaining variables when added to the model (χ2 = 20.12, df = 16, p = 0.22).
The first aim of our study was partly achieved (i.e., we managed to observe the heterogeneity of change in HRQoL and PSS among PLWH), but no systematic gender differences were found with regard to these trajectories. Specifically, we identified three classes of HRQoL, and their members differed in terms of age and education only; therefore, clinical variables did not predict class membership. Thus, our study fits the current trend of HRQoL research, which points to the diminishing role of HIV-related clinical factors as determinants of quality of life for PLWH (Cooper et al., 2017). In a time of great progress in HIV/AIDS treatment and prevention HIV, infection has lost its fatal character and became a chronic and manageable health problem (Deeks et al., 2013). Therefore, it is unsurprising that socially valid resources such as education can be a significant predictor of HRQoL trajectories, which is in line with other studies (albeit cross-sectional and variable-centered; e.g., Degroote et al., 2014; O’Leary et al., 2014). Moreover, we observed that older age was related to decreasing HRQoL trajectories, even if they started from a relatively high level. This corresponds to existing research on elderly PLWH who compared to younger PLWH faced more problems and impediments in their daily functioning due to higher HIV-related stigma (Emlet, 2006) as well as difficulties in distinguishing physical HIV symptoms from those associated with aging (Guaraldi et al., 2011; Morgan et al., 2012).
However, one of the most important (yet null) results deals with the lack of gender differences in HRQoL change among our participants. Specifically, our finding may revise the long-lasting and relatively persistent trend in the literature, which points to lower HRQoL among female PLWH than male PLWH based on cross-sectional data only (e.g., Campsmith et al., 2003; Mrus et al., 2005; Solomon et al., 2008; Chandra et al., 2009). Some authors observed that gender differences in HRQoL within this patient group may be apparent, i.e., they disappeared after careful adjustment of the results with regard to some clinical (e.g., longer illness duration; Ruiz-Perez et al., 2009) or sociodemographic data (worse employment and education status; Rzeszutek, 2017). In other words, lower quality of life among female PLWH does not necessarily reflect their more difficult or different adjustment to HIV/AIDS in comparison to male PLWH but may rather be a result of other factors that have not been carefully controlled for in other studies (Bogart et al., 2011; Rzeszutek, 2017).
However, the results for PSS do not support this explanation. Namely, the null effect for gender became significant only when other covariates were included in the model, resulting in gender and relationship status being identified as correlates of PSS trajectory membership. For a single woman, there was a higher probability of belonging to the increasing PSS trajectory than to the decreasing one, even if the starting points of both trajectories were only slightly different. Notably, this is inconsistent with results concerning female PLWH (Li et al., 2016), but it corresponds to research demonstrating that relationship status may have different consequences for men and women, with men benefiting more from marriage (Nock, 1998). Among PLWH, men also benefit more from social support, while women are more likely to seek it (Gordillo et al., 2009; Bekele et al., 2013). Thus, being a single woman is not necessarily a disadvantageous condition in this context. Such individuals may effectively receive support from other sources that do not require HIV disclosure, and they may also be less prone to abuse from an intimate partner (Machtinger et al., 2012). However, we lack data on the relationship status of these women at the time of diagnosis; therefore, it cannot be excluded that they had been infected by a partner in a heterosexual relationship. The decision to be single could thus be a deliberate consequence of this mode of transmission – the most frequent among women in Europe and the United States (Crepaz et al., 2017; European Centre for Disease Prevention and Control/WHO Regional Office for Europe, 2017). Nonetheless, since no relevant published data exist with which to compare this gender-relationship status interaction, it could represent a sample-specific association. As such, this topic requires further research.
The obtained combinations of dual trajectories added to a complexity of change in HRQoL and PSS among PLWH. Although the probability of being a member of dual decreasing trajectories was the highest, only 31% of the sample could be assigned to this group. Thus, some factors may indeed be responsible for the simultaneous change of both HRQoL and PSS; however, they do not respond in the same manner across the entire sample, since co-occurrence of the matching change direction in both variables was rather modest. This is especially pronounced within decreasing PSS, where we identified three combinations of dual trajectories: (1) congruent decreasing PSS and HRQoL, (2) decreasing PSS and increasing HRQoL, and (3) decreasing PSS with stable HRQoL. Therefore, a few non-exclusive explanations are possible for this mixture of HRQoL and PSS change.
First, it is likely that an interrelation exists between PSS and HRQoL (Burgoyne and Renwick, 2004) causing a downward spiral over time. In this case, some general factors may broadly affect the functioning of PLWH. The natural candidates are those related to sociodemographic resources and clinical characteristics; however, this group did not differ in this respect from the other combinations of trajectories. The primary explanation for this null effect could be that we did not assess the change of these characteristics, only baselines. Nevertheless, this result is congruent with most studies, which show its modest role in the functioning of PLWH after the inception of ART (Torres et al., 2018). Second, for some PLWH, an increase in HRQoL may result in reduced perceived support since it is no longer needed to the same extent. Also, this shift in perception may additionally serve to conserve self-efficacy (Warner et al., 2011), which is of particular importance for patients with chronic diseases that have a stigmatized social reception, thereby further improving quality of life (Li et al., 2011). Finally, in the third case (i.e., for PLWH with decreasing PSS and stable HRQoL), these two processes may have different temporal dynamics, as a change in PSS likely proceeded changes in HRQoL (Jia et al., 2005). It would be rather exceptional to maintain such an incongruent dynamic-static status in light of findings that suggest cross-sectionally lower PSS is related to lower HRQoL among PLWH (Douaihy and Singh, 2001; Burgoyne and Renwick, 2004). Interestingly, being a member of each of these groups remained unrelated not only to gender but also to the other sociodemographic and clinical variables.
There are several strengths of this study, including the longitudinal and person-centered approach with a relatively large clinical sample and three measurement points. However, certain limitations must be noted. First, this is a correlational study based on self-descriptive data; thus, no causal interpretation is allowed. Additionally, the separation of the univariate trajectory classes for HRQoL was only acceptable. Moreover, since the HRQoL measurement covered social domain, significant overlap with social support is likely to occur, which may lead to an overestimation of the relationship between these variables. Even if conceptually relevant, only weak and highly similar correlation has been noted across all the domains1. This indicates already well-recognized difference among perceived social support, satisfaction with social support, and their correlates and outcomes (Vangelisti, 2009). Next, although the sample reflects the gender-related prevalence of HIV infection in Europe and United States, the study could be underpowered to detect gender differences. Furthermore, since there was a tendency for higher dropout among women, a recruitment bias cannot be excluded, though it was not observed in a careful examination of the general pattern of missingness. Finally, it must be underlined that the findings are restricted only to PLWH who are formally diagnosed and under medical treatment, which is a typical characteristic for most studies with clinical samples.
Despite these limitations, our study adds to the HIV/AIDS literature by investigating the heterogeneity of change in HRQoL and PSS with a special emphasis on gender differences. The present study demonstrates the complexity of dual changes and identifies groups of PLWH with mismatched HRQoL and PSS trajectories. The limited role of baseline sociodemographic and clinical characteristics of PLWH in predicting these changes was also highlighted, particularly a lack of significant differences between men and women. In fact, the findings may suggest that gender is no longer a crucial factor beyond their HRQoL and PSS change if after being diagnosed access to treatment is equal.
The datasets for this study will not be made publicly available because although anonymized, it concerns sensitive issues (being infected with HIV). The informed consent did not include the consent to the publication of the data.
All procedures performed in this study were in accordance with the ethical standards of the Research Ethics Committee of the University of Economics and Human Sciences, Warsaw, Poland, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study. The protocol was approved by the Research Ethics Committee of the University of Economics and Human Sciences, Warsaw, Poland.
EG and MR conceived the study, designed the study, supervised the data collection and database organization, conducted the interpretation of the data, drafted, and revised the manuscript. EG conducted the statistical analysis. EG and MR approved the submitted version of the manuscript.
This study was funded by the National Science Center, Poland, research project no. 2016/23/D/HS6/02943. Open access of this article was financed by the Ministry of Science and Higher Education in Poland under the 2019–2022 program “Regional Initiative of Excellence”, project number 012/RID/2018/19.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
1. We would like to thank the anonymous reviewer for this comment. The time-averaged correlations with PSS for each domain of HRQoL were as follows: 0.25 for somatic domain, 0.40 for psychological domain, 0.40 for social domain, and 0.43 for environmental domain.
Alemu, H., Haile, D., Tsui, A., Ahmed, S., and Shewamare, A. (2012). Effect of depressive symptoms and social support on weight and CD4 count increase at HIV clinic in Ethiopia. AIDS Care 24, 866–876. doi: 10.1080/09540121.2011.648160
Ashton, E., Vosvick, M., Chesney, M., Gore-Felton, C., Koopman, C., O’Shea, K., et al. (2005). Social support and maladaptive coping as predictors of the change in physical health symptoms among persons living with HIV/AIDS. AIDS Patient Care STDs 19, 587–598. doi: 10.1089/apc.2005.19.587
Aziz, M., and Smith, K. (2011). Challenges and successes in linking HIV-infected women to care in the United States. Clin. Infect. Dis. 52, 231–237. doi: 10.1093/cid/ciq047
Bekele, T., Rourke, S., Tucker, R., Greene, S., Sobota, M., Koornstra, J., et al. (2013). Direct and indirect effects of perceived social support on health-related quality of life in persons living with HIV/AIDS. AIDS Care 25, 337–346. doi: 10.1080/09540121.2012.701716
Biesanz, J. C., Deeb-Sossa, N., Papadakis, A. A., Bollen, K. A., and Curran, P. J. (2004). The role of coding time in estimating and interpreting growth curve models. Psychol. Methods 9, 30–52. doi: 10.1037/1082-989X.9.1.30
Bing, E. G., Burnam, M. A., Longshore, D., Fleishman, J. A., Sherbourne, C. D., London, A. S., et al. (2001). Psychiatric disorders and drug use among human immunodeficiency virus infected adults in the United States. Arch. Gen. Psychiatry 58, 721–728. doi: 10.1001/archpsyc.58.8.721
Bogart, L. M., Wagner, G. J., Galvan, F. H., Landrine, H., Klein, D. J., and Sticklor, L. A. (2011). Perceived discrimination and mental health symptoms among black men with HIV. Cult. Divers. Ethn. Minor. Psychol. 17, 295–302. doi: 10.1037/a0024056
Bor, J., Rosen, S., Chimbindi, N., Haber, N., Herbst, K., Mutevedzi, T., et al. (2015). Mass HIV treatment and sex disparities in life expectancy: demographic surveillance in rural South Africa. PLoS Med. 12:e1001905. doi: 10.1371/journal.pmed.1001905
Breet, E., Kagee, A., and Seedat, S. (2014). HIV-related stigma and symptoms of post-traumatic stress disorder and depression in HIV-infected individuals: does social support play a mediating or moderating role? AIDS Care 26, 947–951. doi: 10.1080/09540121.2014.901486
Bucciardini, R., Pugliese, K., Weimer, L., Digregorio, M., Fragola, V., and Mancini, M. (2014). Relationship between health-related quality of life measures and high HIV viral load in HIV-infected triple-class-experienced patients. HIV Clin. Trials 15, 176–183. doi: 10.1310/hct1504-176
Burgoyne, R., and Renwick, R. (2004). Social support and quality of life over time among adults living with HIV in the HAART era. Soc. Sci. Med. 58, 1353–1366. doi: 10.1016/S0277-9536(03)00314-9
Burgoyne, R., and Saunders, D. (2001). Quality of life among urban Canadian HIV/AIDS clinic outpatients. Int. J. STD AIDS 12, 505–512. doi: 10.1328/a03564056
Campbell, C., Nair, S., and Maimane, M. (2006). AIDS stigma, sexual moralities and the policing of women and youth in South Africa. Fem. Rev. 83, 132–138. doi: 10.1057/palgrave.fr.9400285
Campsmith, M., Nakashima, A., and Davidson, A. (2003). Self-reported health-related quality of life in persons with HIV infection: results from a multi-site interview project. Health Qual. Life Outcomes 1:12. doi: 10.1186/1477-7525-1-12
Carrico, A. W. (2019). Getting to zero: targeting psychiatric comorbidities as drivers of the HIV/AIDS epidemic. Int. J. Behav. Med. 26, 1–2. doi: 10.1007/s12529-019-09771-w
Carvalhal, A. (2010). Are women a different group of HIV-infected individuals? Arch. Womens Ment. Health 13, 181–183. doi: 10.1007/s00737-010-0167-1
Celeux, G., and Soromenho, G. (1996). An entropy criterion for assessing the number of clusters in a mixture model. J. Classif. 13, 195–212. doi: 10.1007/BF01246098
Chandra, P., Satyanarayana, V., Satishchandra, P., Satish, K., and Kumar, M. (2009). Do men and women with HIV differ in their quality of life? A study from South India. AIDS Behav. 13, 110–117. doi: 10.1007/s10461-008-9434-9
Chida, Y., and Vedhara, K. (2009). Adverse psychosocial factors predict poorer prognosis in HIV disease: a meta-analytic review of prospective investigations. Brain Behav. Immun. 23, 434–445. doi: 10.1016/j.bbi.2009.01.013
Cohen, M. S., Chen, Y. Q., McCauley, M., Gamble, T., Hosseinipour, M. C., Kumarasamy, N., et al. (2016). Antiretroviral therapy for the prevention of HIV-1 transmission. N. Engl. J. Med. 375, 830–839. doi: 10.1056/NEJMoa1600693
Collazos, J., Asensi, V., and Carto, J. (2007). Sex differences in the clinical, immunological and virological parameters of HIV-infected patients treated with HAART. AIDS 21, 835–843. doi: 10.1097/QAD.0b013e3280b0774a
Cooper, V., Clatworthy, J., Harding, R., Whetham, J., and Consortium, E. (2017). Measuring quality of life among people living with HIV: a systematic review of reviews. Health Qual. Life Outcomes 15:220. doi: 10.1186/s12955-017-0778-6
Crepaz, N., Dong, X., Chen, M., and Hall, H. I. (2017). Examination of HIV infection through heterosexual contact with partners who are known to be HIV infected in the United States. AIDS 31, 1641–1644. doi: 10.1097/QAD.0000000000001526
Deeks, S., Lewin, S., and Havlir, D. (2013). The end of AIDS: HIV infection as a chronic disease. Lancet 382, 1525–1533. doi: 10.1016/S0140-6736(13)61809-7
Degroote, S., Vogelaers, D., and Vandijck, D. (2014). What determines health-related quality of life among people living with HIV: an updated review of the literature. Arch. Public Health 72:40. doi: 10.1186/2049-3258-72-40
Douaihy, A., and Singh, N. (2001). Factors affecting quality of life in patients with HIV infection. AIDS Read. 11, 444–449.
Earnshaw, V., Lang, S., Lippitt, M., Jin, H., and Chaudoir, S. (2015). HIV stigma and physical health symptoms: do social support, adaptive coping, and/or identity centrality act as resilience resources? AIDS Behav. 19, 41–49. doi: 10.1007/s10461-014-0758-3
Emlet, C. (2006). A comparison of HIV stigma and disclosure patterns between older and younger adults living with HIV/AIDS. AIDS Patient Care STDs 20, 350–358. doi: 10.1089/apc.2006.20.350
Emuren, L., Welles, S., Evans, A. A., Polansky, M., Okulicz, J. F., Macalino, G., et al. (2017). Health-related quality of life among military HIV patients on antiretroviral therapy. PLoS One. 12:e0178953. doi: 10.1371/journal.pone.0178953
European Centre for Disease Prevention and Control/WHO Regional Office for Europe (2017). HIV/AIDS surveillance in Europe 2017–2016 data. Stockholm: ECDC.
Geary, C., Parker, W., Rogers, S., Haney, E., Njihia, C., and Haile, A. (2014). Gender differences in HIV disclosure, stigma, and perceptions of health. AIDS Care 26, 1419–1425. doi: 10.1080/09540121.2014.921278
Gielen, A., McDonnell, K., Campo, P., and Faden, R. (2001). Quality of life among women living with HIV: the importance violence, social support, and self-care behaviors. Soc. Sci. Med. 52, 315–322. doi: 10.1016/S0277-9536(00)00135-0
Gonzalez, J., Penedo, F., Antoni, M., Dura, R., Pherson-Baker, S., and Ironson, G. (2004). Social support, positive states of mind, and HIV treatment adherence in men and women living with HIV/AIDS. Health Psychol. 23, 413–418. doi: 10.1037/0278-6133.23.4.413
Gordillo, V., Fekete, E., Platteau, T., Antoni, M., Schneiderman, N., and Nostlinger, C. (2009). Emotional support and gender in people living with HIV: effects on psychological well-being. J. Behav. Med. 32, 523–531. doi: 10.1007/s10865-009-9222-7
Guaraldi, G., Orlando, G., and Zona, S. (2011). Premature age-related co-morbidities among HIV-infected persons compared with the general population. Clin. Infect. Dis. 53, 1120–1126. doi: 10.1093/cid/cir627
Hansen, N., Vaughan, E., Cavanaugh, C., Connell, C. M., and Sikkema, K. (2009). Health-related quality of life in bereaved HIV-positive adults: relationships between HIV symptoms, grief, social support, and axis II indication. Health Psychol. 28, 249–257. doi: 10.1037/a0013168
Herrmann, S., McKinnon, E., Hyland, N., Lalanne, C., Mallal, S., Nolan, D., et al. (2013). HIV-related stigma and physical symptoms have a persistent influence on health-related quality of life in Australians with HIV infection. Health Qual. Life Outcomes 11:56. doi: 10.1186/1477-7525-11-56
Hipp, J. R., and Bauer, D. J. (2006). Local solutions in the estimation of growth mixture models. Psychol. Methods 11, 36–53. doi: 10.1037/1082-989X.11.1.36
Jia, H., Uphold, C. R., Wu, S., Chen, G. J., and Duncan, P. W. (2005). Predictors of changes in health-related quality of life among men with HIV infection in the HAART era. AIDS Patient Care STDs 19, 395–405. doi: 10.1089/apc.2005.19.395
Jia, H., Uphold, C., Wu, S., Reid, K., Findley, K., and Duncan, P. (2004). Health-related quality of life among men with HIV infection: effects of social support, coping, and depression. AIDS Patient Care STDs 18, 594–603. doi: 10.1089/apc.2004.18.594
Joint United Nations Programme on HIV/AIDS (UNAIDS) (2018). UNAIDS DATA 2018. Available at: http://www.unaids.org/sites/default/files/media_asset/unaids-data-2018_en.pdf (Accessed March, 19 2019).
Li, X., Huang, L., Wang, H., Fennie, K. P., He, G., and Williams, A. B. (2011). Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS Patient Care STDs 25, 665–671. doi: 10.1089/apc.2011.0174
Li, L., Lin, C., Liang, L. J., and Ji, G. (2016). Exploring coping and social support with gender and education among people living with HIV in China. AIDS Behav. 20, 317–324. doi: 10.1007/s10461-015-1232-6
Lifson, A. R., Grund, B., Gardner, E. M., Kaplan, R., Denning, E., Engen, N., et al. (2017). Improved quality of life with immediate versus deferred initiation of antiretroviral therapy in early asymptomatic HIV infection. AIDS 31, 953–963. doi: 10.1097/QAD.0000000000001417
Liu, C., Ostrow, D., Detels, R., Hu, Z., Johnson, L., Kingsley, L., et al. (2006). Impacts of HIV infection and HAART use on quality of life. Qual. Life Res. 15, 941–949. doi: 10.1007/s11136-005-5913-x
Lubeck, D., and Fries, J. (1997). Assessment of quality of life in early stage HIV-infected persons: data from the AIDS time-oriented health outcome study (ATHOS). Qual. Life Res. 6, 494–506. doi: 10.1023/A:1018404014821
Machtinger, E., Wilson, T., Haberer, J., and Weiss, D. (2012). Psychological trauma and PTSD in HIV-positive women: a meta-analysis. AIDS Behav. 16, 2091–2100. doi: 10.1007/s10461-011-0127-4
McDonnell, K., Gielen, A., Wu, A., Campo, P., and Faden, R. (2000). Measuring health related quality of life among women living with HIV. Qual. Life Res. 9, 931–940. doi: 10.1023/A:1008909919456
Miners, A., Phillips, A., Kreif, N., Rodger, A., Speakman, A., Fisher, M., et al. (2014). Health-related quality-of-life of people with HIV in the era of combination antiretroviral treatment: a cross-sectional comparison with the general population. Lancet HIV 1, e32–e40. doi: 10.1016/S2352-3018(14)70018-9
Mitchell, M., Nguyen, T., Isenberg, S., Maragh-Bass, A., Keruly, J., and Knowlton, A. (2017). Psychosocial and service use correlates of health-related quality of life among a vulnerable population living with HIV/AIDS. AIDS Behav. 21, 1580–1587. doi: 10.1007/s10461-016-1589-1
Morgan, E., Iudicello, J., and Weber, E. (2012). Synergistic effects of HIV infection and older age on daily functioning. J. Acquir. Immune Defic. Syndr. 61, 341–348. doi: 10.1097/QAI.0b013e31826bfc53
Mrus, J., Williams, P., Tsevat, J., Cohn, S., and Wu, A. (2005). Gender differences in health-related quality of life in patients with HIV/AIDS. Qual. Life Res. 14, 479–491. doi: 10.1007/s11136-004-4693-z
Nicastri, E., Leone, S., Angeletti, C., Palmesano, L., Sarmati, L., Chiesi, A., et al. (2007). Sex issues in HIV-1-infected persons during highly active antiretroviral therapy: a systematic review. J. Antimicrob. Chemother. 60, 724–732. doi: 10.1093/jac/dkm302
Nylund, K., Asparouhov, T., and Muthén, B. O. (2007). Deciding on the number of classes in latent class analysis and growth mixture modeling: a Monte Carlo simulation study. Struct. Equ. Model. 14, 535–569. doi: 10.1080/10705510701575396
O’Leary, A., Jemmott, J. B., Stevens, R., Rutledge, S. E., and Icard, L. D. (2014). Optimism and education buffer the effects of syndemic conditions on HIV status among African American men who have sex with men. AIDS Behav. 18, 2080–2088. doi: 10.1007/s10461-014-0708-0
Oberjé, E., Dima, A., van Hulzen, A. W., Prins, J., and de Bruin, M. (2015). Looking beyond health-related quality of life: predictors of subjective well-being among people living with HIV in the Netherlands. AIDS Behav. 19, 1398–1407. doi: 10.1007/s10461-014-0880-2
Penniman, T. V., Taylor, S. L., Bird, C. E., Beckman, R., Collins, R. L., and Cunningham, W. (2007). The associations of gender, sexual identity and competing needs with healthcare utilization among people with HIV/AIDS. J. Natl. Med. Assoc. 99, 419–427.
Psaros, C., O’Cleirigh, C., Bullis, J., Markowitz, S., and Safren, S. (2013). The influence of psychological variables on health related quality of life among HIV positive individuals with a history of intravenous drug use. J. Psychoactive Drugs 45, 304–312. doi: 10.1080/02791072.2013.825030
Qiao, S., Li, X., and Stanton, B. (2014). Social support and HIV-related risk behaviors: a systematic review of the global literature. AIDS Behav. 18, 419–441. doi: 10.1007/s10461-013-0561-6
Rendina, H., Brett, M., and Parsons, J. (2018). The critical role of internalized HIV-related stigma in the daily negative affective experiences of HIV-positive gay and bisexual men. J. Affect. Disord. 227, 289–297. doi: 10.1016/j.jad.2017.11.005
Ruiz-Perez, I., Olry, A., del Castilloc, L., Bano, J., Ruz, M., and Jimeneze, A. (2009). No differences in quality of life between men and women undergoing HIV antiretroviral treatment. Impact of demographic, clinical and psychosocial factors. AIDS Care 21, 943–952. doi: 10.1080/09540120802612840
Rzeszutek, M. (2017). Health-related quality of life and coping strategies among people living with HIV: the moderating role of gender. Arch. Womens Ment. Health 21, 247–257. doi: 10.1007/s00737-017-0801-2
Rzeszutek, M., and Gruszczyńska, E. (2018). Positive and negative affect change among people living with HIV: a one-year prospective study. Int. J. Behav. Med. 26, 28–37. doi: 10.1007/s12529-018-9741-0
Samji, H., Cescon, A., Hogg, R. S., Modur, S. P., Althoff, K. N., Buchacz, K., et al. (2013). Closing the gap: Increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One 18, 144–156. doi: 10.1371/journal.pone.0081355
Schulz, U., and Schwarzer, R. (2003). Soziale Unterstützung bei der Krankheitsbewältigung: Die Berliner Social Support Skalen (BSSS). Diagnostica 49, 73–82. doi: 10.1026//0012-1924.49.2.73
Solomon, S., Venkatesh, K., Brown, L., Verma, P., Cecelia, A., Daly, C., et al. (2008). Gender-related differences in quality of life domains of persons living with HIV/AIDS in South India in the era prior to greater access to antiretroviral therapy. AIDS Patient Care and STDs 22, 999–1005. doi: 10.1089/apc.2008.0040
Song, B., Yan, C., Lin, Y., Fuxiang, W., and Wang, L. (2016). Health-related quality of life in HIV-infected men who have sex with men in China: a Cross-sectional study. Med. Sci. Monit. 22, 2859–2870. doi: 10.12659/MSM.897017
Torres, T. S., Harrison, L. J., La Rosa, A. M., Cardoso, S. W., Zheng, L., Ngongondo, M., et al. (2018). Quality of life improvement in resource-limited settings after one year of second-line antiretroviral therapy use among adult men and women. AIDS 32, 583–593. doi: 10.1097/QAD.0000000000001738
Turner-Cobb, J. M., Gore-Felton, C., Marouf, F., Koopman, C., Kim, P., et al. (2002). Coping, social support, and attachment style as psychosocial correlates of adjustment in men and women with HIV/AIDS. J. Behav. Med. 25, 337–353. doi: 10.1023/A:1015814431481
Vangelisti, A. L. (2009). Challenges in conceptualizing social support. J. Soc. Pers. Relat. 26, 39–51. doi: 10.1177/0265407509105520
Vermunt, J. K., and Magidson, J. (2016). Technical guide for latent GOLD 5.1: Basic, advanced, and syntax. Belmont, CA: Statistical Innovations.
Warner, L., Ziegelmann, J., Schüz, B., Wurm, S., Tesch-Roemer, C., and Schwarzer, R. (2011). Maintaining autonomy despite multimorbidity: self-efficacy and the two faces of social support. Eur. J. Ageing 8, 3–12. doi: 10.1007/s10433-011-0176-6
Keywords: health-related quality of life, perceived social support, people living with HIV, gender differences, latent class growth curve
Citation: Gruszczyńska E and Rzeszutek M (2019) Trajectories of Health-Related Quality of Life and Perceived Social Support Among People Living With HIV Undergoing Antiretroviral Treatment: Does Gender Matter? Front. Psychol. 10:1664. doi: 10.3389/fpsyg.2019.01664
Received: 20 April 2019; Accepted: 02 July 2019;
Published: 23 July 2019.
Edited by:
Sabrina Cipolletta, University of Padova, ItalyReviewed by:
Serena Giunta, University of Palermo, ItalyCopyright © 2019 Gruszczyńska and Rzeszutek. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ewa Gruszczyńska, ZWdydXN6Y3p5bnNrYUBzd3BzLmVkdS5wbA==
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.