- 1Department of Otorhinolaryngology, Radboud University Medical Center, Nijmegen, Netherlands
- 2Donders Institute for Brain, Cognition and Behaviour, Radboud University, Nijmegen, Netherlands
Background: Internalizing and externalizing behavioral problems were frequently reported in profoundly hearing-impaired (HI) children with hearing aids. Due to the positive effect of cochlear implants (CIs) on hearing and language development, a positive effect on behavioral problems was expected. However, there is no consensus about the frequency of behavioral problems in CI children, and studies are often based on one informant with the risk of missing behavioral problems in other contexts.
Aims: The first aim of this study was to investigate the frequency of behavioral problems in children with CIs as compared to a hearing normative sample. The second aim was to measure the agreement between the parents’ and teachers’ rates on the behavioral problem scales. And the third aim was to investigate the relation between speech perception, language skills and the frequencies of reported behavioral problems.
Methods: Of 71 CI children, 51% were girls and 49% were boys, and the mean age was 8.6 (SD = 3.3). Behavior was reported by parents using the Child Behavior Checklist (CBCL) and by teachers using the Teacher Report Form (TRF). Frequencies of behavioral problems of CI children (6–16 years) were compared to a normative sample with the chi square test. Parent-teacher agreement was measured with the intraclass correlation coefficient (ICC 2,1). Next CI children were divided into four ability level categories regarding speech perception and language skills. Frequencies of behavioral problems were compared between the categories with the chi square test.
Results: Parents and teachers of CI children reported similar frequencies of behavioral problems to the normative sample. Fair to low parent-teacher agreements were found on the behavioral problem scales. A significantly higher frequency of behavioral problems was reported in children with low speech perception and receptive vocabulary at school.
Conclusion: Parents and teachers report similar frequencies of behavioral problems children with CIs compared to a hearing normative sample. Children with lower speech perception and language levels are more at risk of developing behavioral problems at school. Adequate speech perception and language levels are found to be protective factors for the development of behavior.
Introduction
Prior to the application of cochlear implants (CIs), profoundly hearing-impaired (HI) children used to have limited to no auditory access to sound and spoken language. The perception of speech and interaction with the environment is required for communication and the development of spoken language (Kuhl and Rivera-Gaxiola, 2008; Kral and O’Donoghue, 2010). Language is known to support emotional self-regulation and social-cognitive competence. The lack of understanding of the auditory and linguistic refinements of social and emotional language, such as intonation, sarcasm, recognizing emotions and the ability to attribute mental states of other people, interferes with the understanding of people, culture, emotions, and social rules (Vaccari and Marschark, 1997; Calderon and Greenberg, 2003; Moeller, 2007). Therefore, profoundly HI children with limited or no access to spoken language are at risk for developing social and emotional problems (Barker et al., 2009; Gentilli and Holwell, 2011). Indeed, enormous percentages reaching approximately 30–50% of profoundly HI children fitted with or without hearing aids were reported to exhibit behavioral problems (Mitchell and Quittner, 1996; Vostanis et al., 1997; van Eldik et al., 2004; van Eldik, 2005; van Gent et al., 2007). Behavioral problems can be divided into externalizing and internalizing behavioral problems. Externalizing behavioral problems in HI children manifest in behavioral symptoms such as conduct problems, aggression and hyperactivity (Mitchell and Quittner, 1996; van Eldik et al., 2004; van Eldik, 2005; van Gent et al., 2007; Stevenson et al., 2010; Theunissen et al., 2014a; Stevenson et al., 2015). Internalizing behavioral problems manifest in emotional symptoms such as depression, anxiety, withdrawal behavior and thought and attention problems (van Eldik et al., 2004; van Eldik, 2005; van Gent et al., 2007; Barker et al., 2009; Stevenson et al., 2010; Theunissen et al., 2011, 2014a). The frequency of behavioral problems in profoundly HI children without CIs is disturbingly higher than in a Dutch normative sample of normal hearing peers, of whom 16% showed behavioral problems (Verhulst et al., 1996; van Eldik et al., 2004). Even more concerning is that only a small proportion of approximately 10% of HI children with emotional or behavioral problems were referred for professional help (van Gent et al., 2007). The guidance of profoundly HI children with behavioral problems therefore requires substantial effort from and skills of the parents and teachers. Especially for children in special educational settings for the deaf, these children show more behavioral problems than those in mainstream education (Theunissen et al., 2014b). Therefore, parents and teachers need more support and training to prevent or remediate emotional and behavioral problems in profoundly HI children (Calderon and Greenberg, 2003).
Currently, CIs can provide children with severe or profound deafness auditory access to sound and often levels of spoken language communication (Svirsky et al., 2004; Niparko et al., 2010; Fulcher et al., 2012; Boons et al., 2013; Geers and Nicholas, 2013). Especially early cochlear implantation before the age of 12 months provides profoundly HI children more abilities to develop sufficient speech recognition and perception to achieve age-appropriate language development (Colletti et al., 2011; Leigh et al., 2013; Dettman et al., 2016). Whereas it has been expected that improved language skills will decrease emotional and behavioral problems in profoundly HI children without CIs (Barker et al., 2009), it is hoped that, based on improved hearing and language development after cochlear implantation, a decrease in the frequency of behavioral problems is also observed in these children.
Indeed, several studies found that better language and communication skills were related to fewer behavioral problems in CI children (Wiefferink et al., 2012; Theunissen et al., 2014a; Netten et al., 2018). In addition, some studies found that children with CIs even show similar levels of behavioral problems to their normal-hearing peers (Khan et al., 2005; Huber and Kipman, 2011; Theunissen et al., 2014a, 2015; Huber et al., 2015). This finding reflects a major improvement for profoundly HI children since the introduction of CIs. However, some studies still report that children with CIs show more externalizing behavioral problems, internalizing behavioral problems and peer problems (Huber and Kipman, 2011; Chao et al., 2015; Huber et al., 2015). Despite much research on social and emotional development in CI children, there is still no consensus about the frequency of behavioral problems. These frequencies range from nine percent (Wong et al., 2017) to 20–30% (Huber and Kipman, 2011; Chao et al., 2015; Theunissen et al., 2015). Studies with young children (M = 5.1 years) with an early age of implantation (M = 16 months) (Wong et al., 2017) reported fewer behavioral problems than studies with an older test age (>11 years) and a later age of implantation (>3.8 years) (Huber and Kipman, 2011; Chao et al., 2015; Theunissen et al., 2015). However, in most studies, the frequencies of behavioral problems were not reported (Khan et al., 2005; Theunissen et al., 2011, 2014b; Huber et al., 2015; Park et al., 2016).
Behavioral problems are often determined by questionnaires. However, questionnaires are highly specific with regard to the context as well as the children’s behavior (Brown et al., 2006; De Los Reyes et al., 2009). Parental questionnaires, especially those completed by the parent with greater exposure and knowledge of the child’s behavior, seem to be representative of the child’s behavior at home (Langberg et al., 2010; Schroeder et al., 2010) but not at school. Therefore, information gathering about behavioral problems in children should be based on multi-informant information from different contexts (De Los Reyes et al., 2009; van der End et al., 2012). In the aforementioned studies on behavioral problems in children with CIs, almost all studies used parental questionnaires only or combined them with self-reported questionnaires for children. Only Huber and Kipman (2011) and Huber et al. (2015) used parental questionnaires combined with teacher questionnaires. Huber and Kipman (2011) found that teachers rated significantly more CI children with peer problems and clinical behavioral problems than did parents, with a parent-teacher agreement correlation of 0.40.
The first aim of this study is to investigate the frequency of behavioral problems in children with CIs. Next we want to compare these frequencies to that of a hearing normative sample. Additionally, agreement between the parents’ and teachers’ rates on the internalizing, externalizing and total behavioral problem scales will be measured. Finally, the relation between speech perception and language skills with the frequencies of reported behavioral problems will be investigated.
Materials and Methods
Participants
Participants were retrospectively included based on consecutive sampling as part of standard CI follow-up between June 2011 and June 2016. The inclusion criteria were as follows: (1) between 2.5 and 16 years old, (2) being able to participate in the speech perception test, (3) being able to participate in the receptive vocabulary test, and (4) parents and teachers both returned the behavioral questionnaires. All children with a bilateral unaided pure tone average of 90 dB or higher averaged over the frequencies of 1000, 2000, and 4000 Hz before cochlear implantation. The parents and teachers of 71 children both returned the behavioral questionnaires. Only these children were included in this study. Of 12 children, only the parents returned the questionnaires, and of 25 children, only the teachers returned the questionnaires. These children were excluded from this study.
The children attended one of three types of educational settings: mainstream education, education for profoundly HI/deaf children (Special HI), and education for children with other special needs (Special Other). Of the three children attending the Special Other educational setting, one child was diagnosed with ADHD and ASS, one child was diagnosed with cerebral palsy and one child was diagnosed with developmental disabilities due to Noonan syndrome.
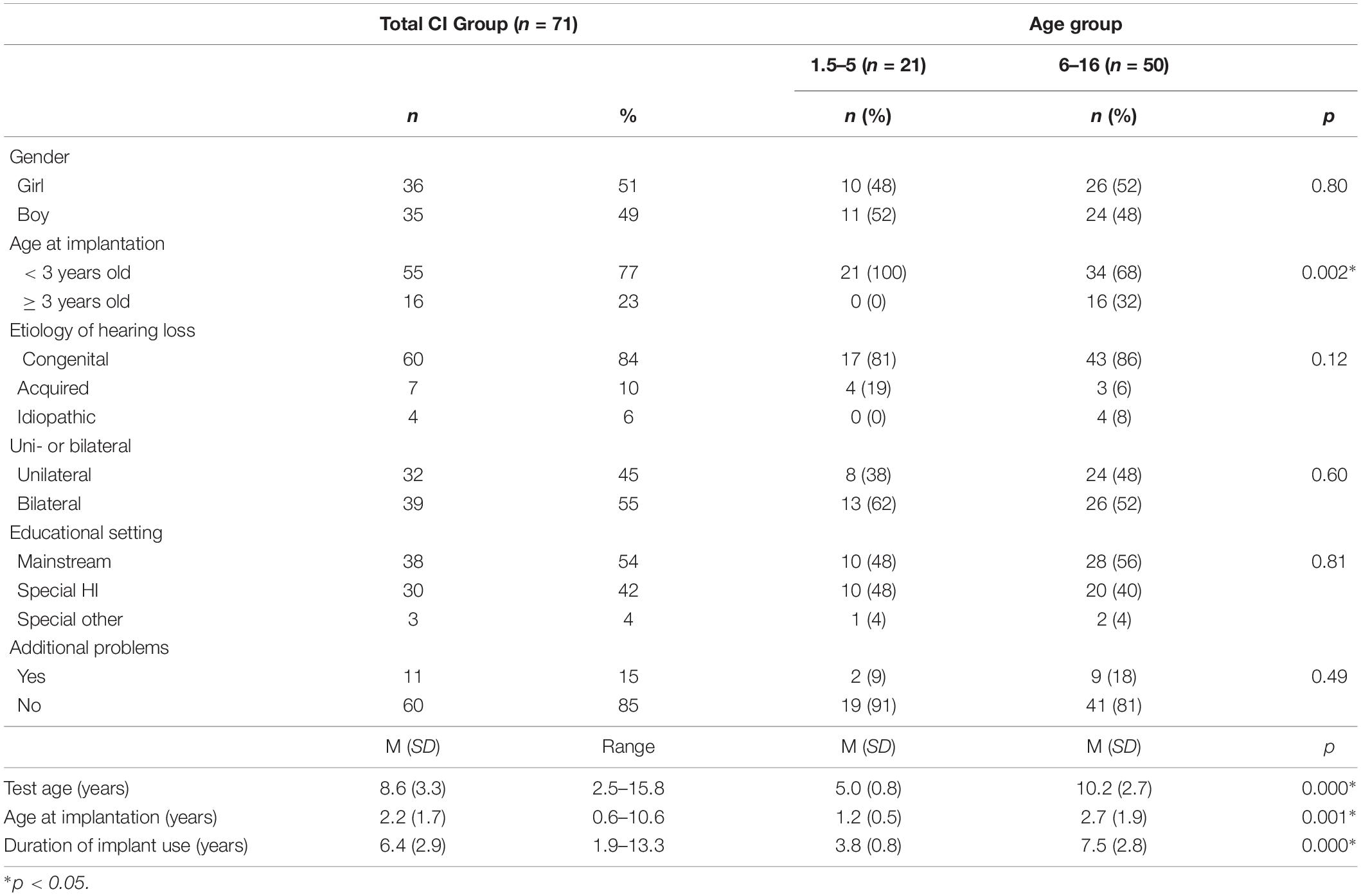
Most of the other children with additional problems in mainstream or special settings were diagnosed with ADHD or ASS or had motor disabilities or learning problems. Descriptive statistics of the CI participant group are listed in Table 1.
The participants were divided in two groups based on age, 1.5–5 years and 6–16 years. Descriptive statistics of both groups are presented in Table 1. The frequencies of behavioral problems in CI participants in the range 6–16 years were compared to a Dutch normative sample of 1,417 children aged from 6 to 16 years, of whom 50% were male and 50% were female. Fifty-four percent of the normative sample were between 6 and 11 years old, and 46% were between 12 and 16 years old (Tick et al., 2007).
Materials
Behavior Questionnaires for Parents and Teachers
The Dutch version of the Child Behavior Checklist (CBCL) and the Teacher Report Form for teachers (TRF) were used (Achenbach and Rescorla, 2000, 2010; Verhulst and Van der Ende, 2013). Children between 1.5 and 5 years old were assed with the CBCL/1½-5 and the caregiver-TRF (C-TRF). The children between 6 and 16 were assessed with the CBCL/6-18 and the TRF. These standardized and validated questionnaires comprise questions about a child’s emotional state and behavior. Response options are: 0 = not at all, 1 = a little or sometimes, 2 = clearly or often. Scores were tallied for the Internalizing, Externalizing and Total Behavior Problem broadband scales. The Internalizing Problem Scale covers anxiety and depressive problems, and the Externalizing Problem Scale covers aggressive and rule-breaking behavior. Raw scores were converted to T-scores after correcting for age and gender; next, the T-scores were classified into two categories: normal or deviant. A T-score ≥ 60 reflects a deviant score. A deviant behavior score indicates a significantly higher prevalence of dysfunctional behavior.
Auditory Speech Perception
Auditory speech perception was assessed using a standard Dutch open-set identification test for children aged up to 16 years old containing the consonant – vowel – consonant words of Bosman and Smoorenburg (1995). This test was carried out in a sound-treated booth by an audiologist. Stimuli were presented in the sound field at a presentation level of 65 dB SPL. Scores are expressed as a percentage of correctly recognized phonemes. Scores at or above 85% are considered good speech-recognition scores clinically by Hicks and Tharpe (2002) as well as in our clinic.
Receptive Vocabulary
Receptive vocabulary was assessed with the Peabody Picture Vocabulary Test-III-NL (PPVT) by Dunn and Dunn (2005). The PPVT is a standardized and validated test for persons aged from 2.3 to 90 years. A series of four pictures per page are presented to the child. The examiner states a word describing one of the pictures; then, the child has to point to the picture the word describes. The outcomes are expressed as a receptive vocabulary quotient. The average age-appropriate quotient is 100 (SD = 15).
Procedure
After a technical inspection of the CI, speech perception assessments were carried out by an audiologist or audiologist assistant. Before or after the technical inspection and speech perception test, the receptive vocabulary test was conducted by a language and speech pathologist or speech therapist. Parents were requested to complete a parent questionnaire about behavior problems at home and were provided a teacher questionnaire with the request to give it to the child’s teacher. They received the questionnaire with standardized instruction information and prepaid return envelopes for both questionnaires. The time period for returning the questionnaires was as soon as possible but within 3 months of the CI follow-up date. The questionnaires were analyzed by a psychologist. Children and their parents received an evaluation report afterward. Data for this study were retrospectively collected by file study.
Ethical Considerations
The study was carried out in accordance with the recommendations of the Committee on Research Involving Human Subjects of the Radboud University Medical Center. All parents of the participants gave written informed consent for the use of the patient’s file data in accordance with the Declaration of Helsinki.
Statistical Analyses
First, we investigated the frequencies of clinical deviant behavioral problems in CI children on the CBCL and TRF Internalizing, Externalizing and Total Behavioral Problem Scales. Next the frequencies of CI children aged 6–16 with normal and deviant behavior reported by parents and teachers were compared to the frequencies of children classified with normal and deviant behavior reported by parents and teachers of the normal hearing Dutch normative sample (Tick et al., 2007) with the chi square test for goodness of fit (p < 0.05). The agreement between the parents’ and teachers’ rates on the internalizing, externalizing, and total behavioral problem scales was tested with the two-way random total agreement intraclass correlation coefficient (ICC 2,1) (p < 0.05). The cutoff scores of Cicchetti (1994) were used. An ICC level below 0.40 is classified as a low parent-teacher agreement; between 0.40 and 0.59, the parent-teacher agreement level is fair; between 0.60 and 0.74, the parent-teacher agreement level is good; and from 0.75 and higher the parent-teacher agreement is excellent.
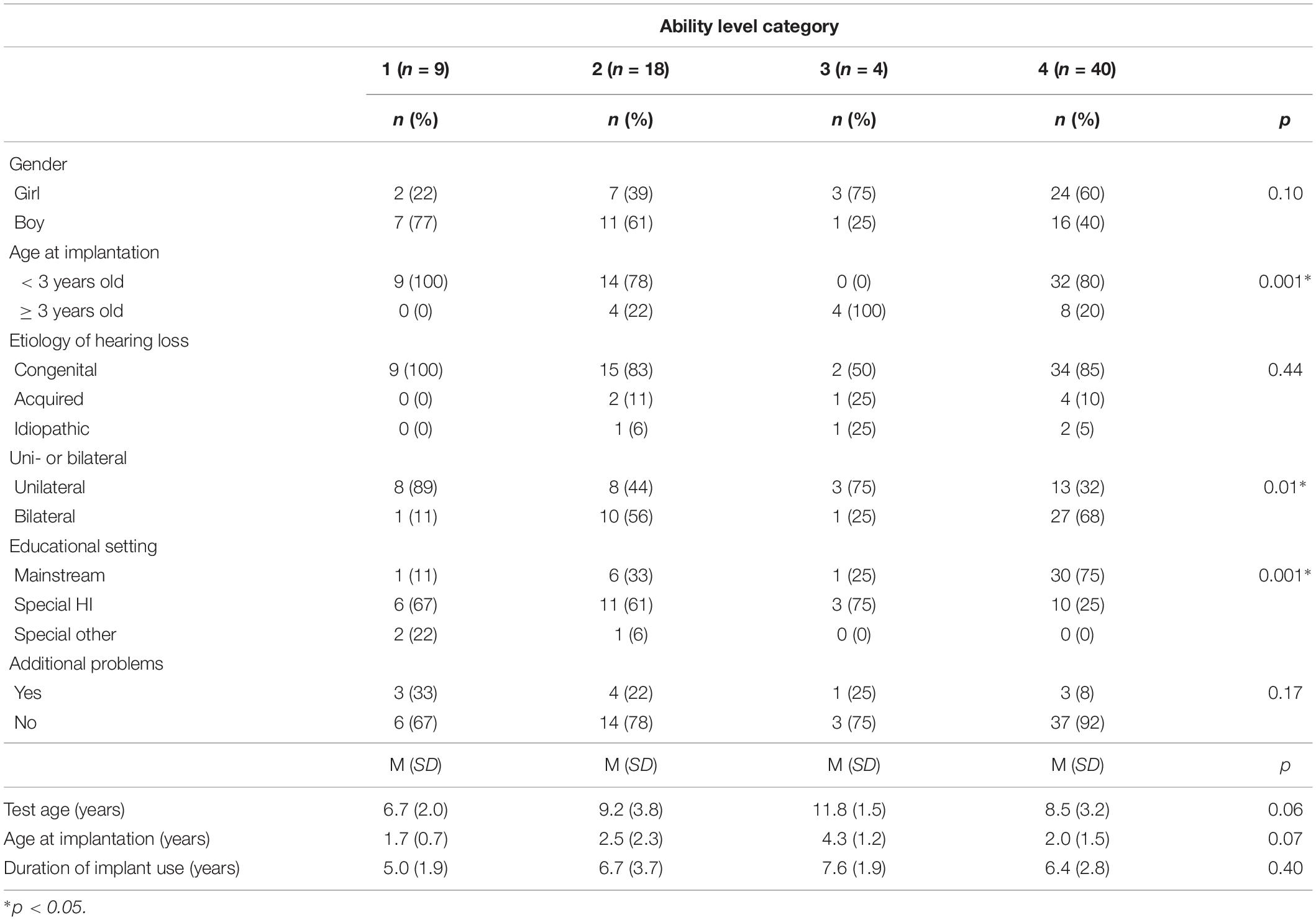
To assess the effects of speech perception and receptive vocabulary on the number of reported behavioral problems, the CI children were divided into four ability level categories. These four ability level categories were based on clinical levels of speech perception and receptive vocabulary. The clinical level for adequate speech perception was set at a phoneme score of ≥85%, and that for adequate receptive vocabulary was set on a receptive vocabulary quotient of ≥85. CI children who obtained low speech perception and low receptive vocabulary scores were classified as ability category 1. Children who obtained adequate speech perception and low receptive vocabulary scores were classified as ability category 2. Children who obtained low speech perception and adequate receptive vocabulary were classified as ability category 3. Children who obtained an adequate speech perception and adequate receptive vocabulary score were classified as ability category 4. Descriptive statistics of the CI children in the four ability level categories are presented in Table 2. The chi-square test of contingencies (p < 0.05), with Cohen’s w as a measure of effect size, was used to assess the differences in the frequencies of behavioral problems between the ability level categories. Ability category 3 was excluded from the analyses due to the small sample size of four participants. Post hoc analyses were performed using the chi square test for goodness of fit (p < 0.01).
All statistical analyses were performed using IBM SPSS Statistics 25.
Results
Behavioral Problems in CI Children Reported by Parents and Teachers
Frequencies of the Parents’ and Teachers’ Reported Clinical Behavioral Problems Compared to Normative Data
First, we investigated the frequencies of clinical deviant behavioral problems in CI children on the CBCL’s and TRF’s Internalizing, Externalizing, and Total Behavioral Problem Scales.
Frequencies of behavioral problems of the total CI group and the two age groups are presented in Table 3.
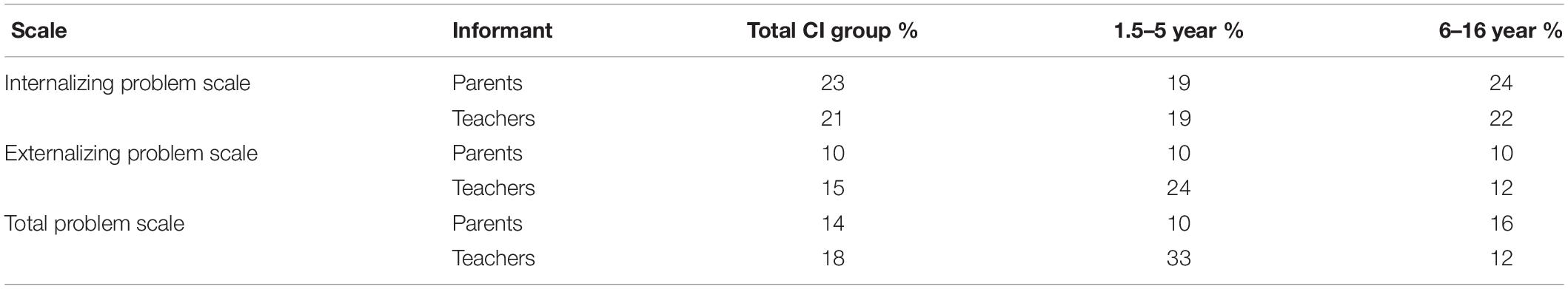
Table 3. Frequencies of deviant internalizing, externalizing and total behavioral problems in the total CI group, and in the two age groups.
The frequencies of reported behavioral problems in CI children aged 6–16, the normative sample aged 6–16 (Tick et al., 2007) and chi-square results are reported in Table 4. The chi-square test for goodness of fit shows that parents of CI children aged 6–16 report comparable rates of internalizing, externalizing and total behavioral problems to parents of the hearing normative sample. Also no differences were found among the internalizing, externalizing, and total behavioral problems reported by teachers of CI children compared with teachers of the hearing normative sample.
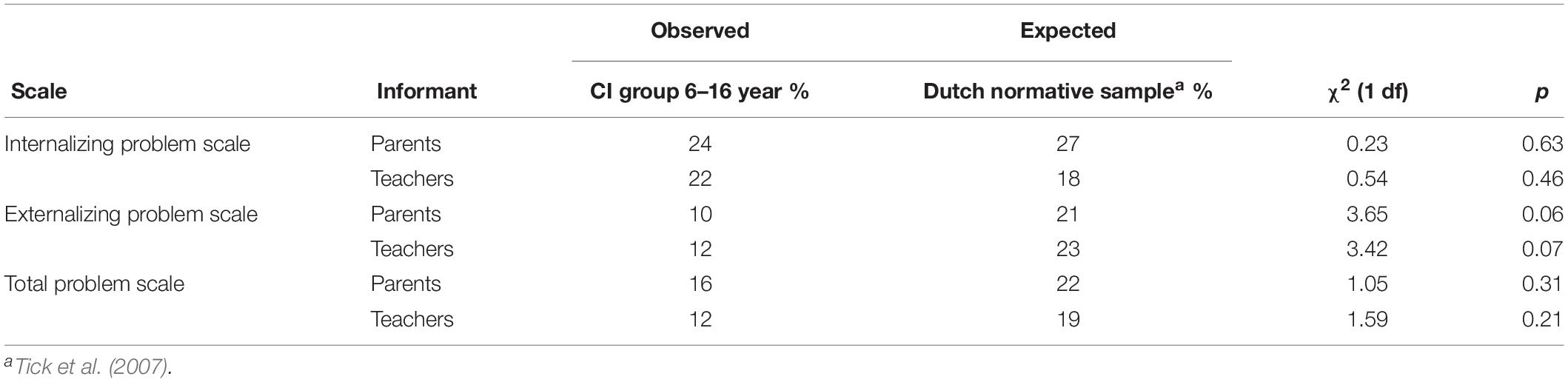
Table 4. Chi-square test for goodness of fit results and frequencies of deviant internalizing, externalizing and total behavioral problems in CI children and the dutch normative sample.
Relationship Between the Parents’ and Teachers’ Reported Context-Related Behavioral Problems in CI Children
The results show overall fair to low agreements between the rates of reported behavioral problems by parents and teachers. The ICCs between the parents’ ratings on the CBCL Internalizing Problem Scale and teachers’ ratings on the TRF Internalizing Problem Scale were 0.40 (p = 0.000), those on the Externalizing Problem Scale were 0.28 (p < 0.01), and those on the Total Problem Scale were 0.32 (p < 0.01). Visual representations of the agreements between teachers’ and parents’ ratings on the three problem scales are shown in Figures 1A–C.
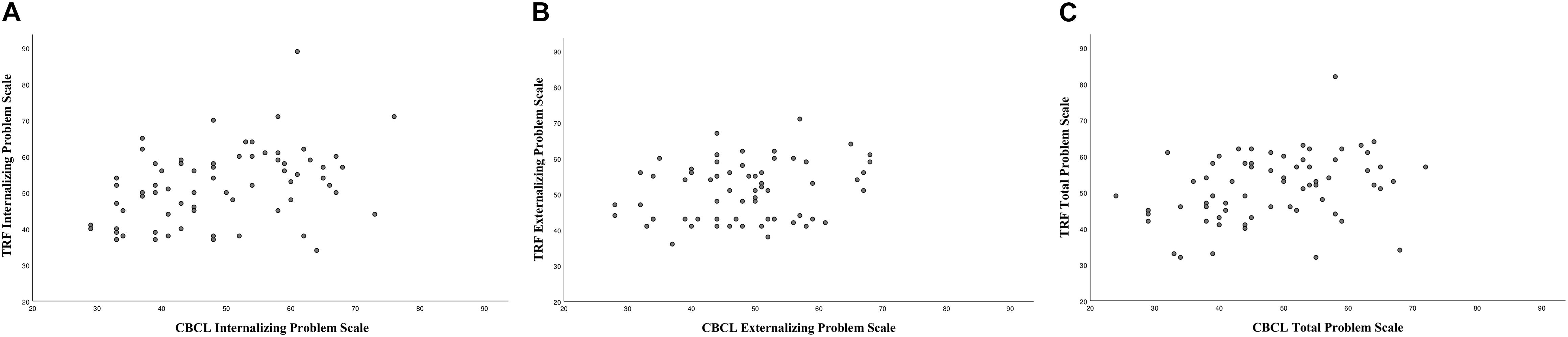
Figure 1. (A–C) Intraclass correlations between teachers’ (TRF) and parents’ (CBCL) ratings on the internalizing, externalizing, and total problem scales.
The Effects of Speech Perception and Receptive Vocabulary on Reported Frequencies of Behavioral Problems
Table 5 shows the results of the total CI group in the four ability level categories on the speech perception and receptive vocabulary test.
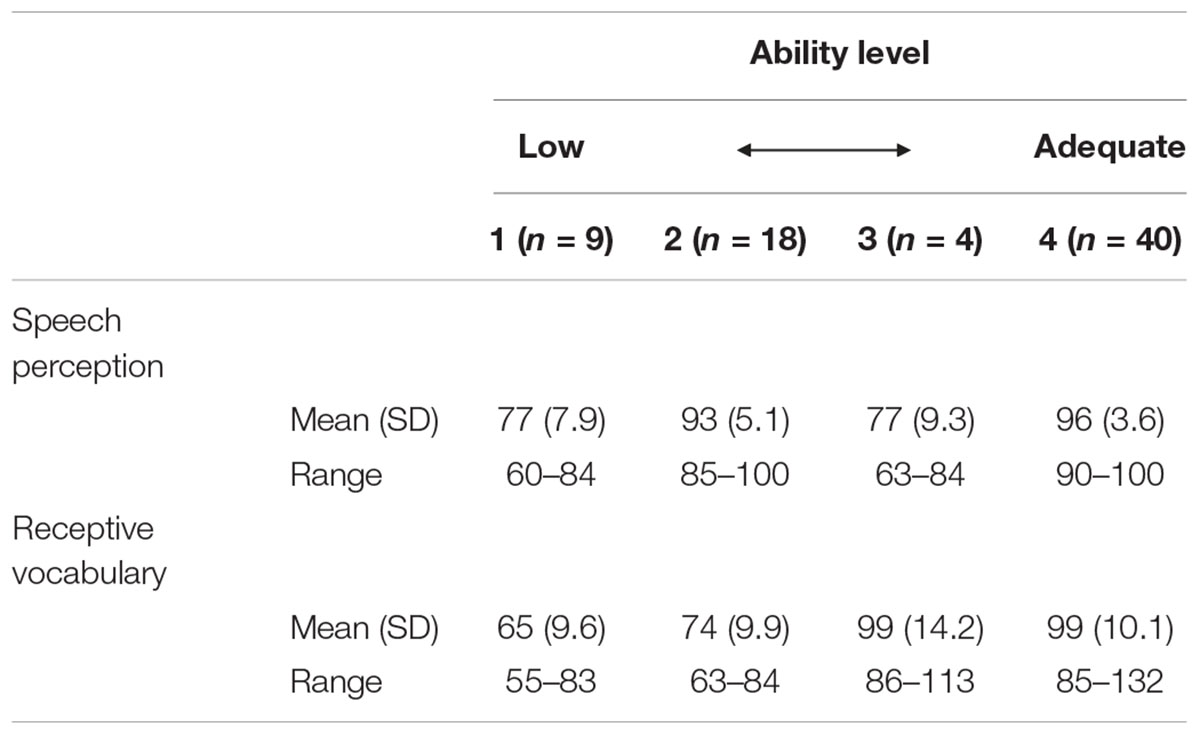
Table 5. Speech perception and receptive vocabulary results of the CI children divided in four ability level categories.
The results of the chi-square test of contingencies and the frequencies of reported internalizing, externalizing and total behavioral problems of CI children divided into the four ability level categories are presented in Table 6. No effect of ability level categories on the frequencies of internalizing and externalizing behavioral problems was found. An effect of ability level categories on the frequencies of behavioral problems reported by teachers was found only on the Total Problem Scale in the TRF. This effect had a Cohen’s w of 0.50, indicating there was a large effect of the ability level on the reported frequencies of total behavioral problems at school. Post hoc analysis showed that there were significant differences between the frequencies of reported behavioral problems at school in the lowest ability level (category 1) and ability level category 2, χ2 (1, n = 27) = 8.862, p < 0.01, and between ability level category 1 and the adequate ability level category 4, χ2 (1, n = 49) = 14.52, p < 0.001. No difference was found between categories 2 and 4.
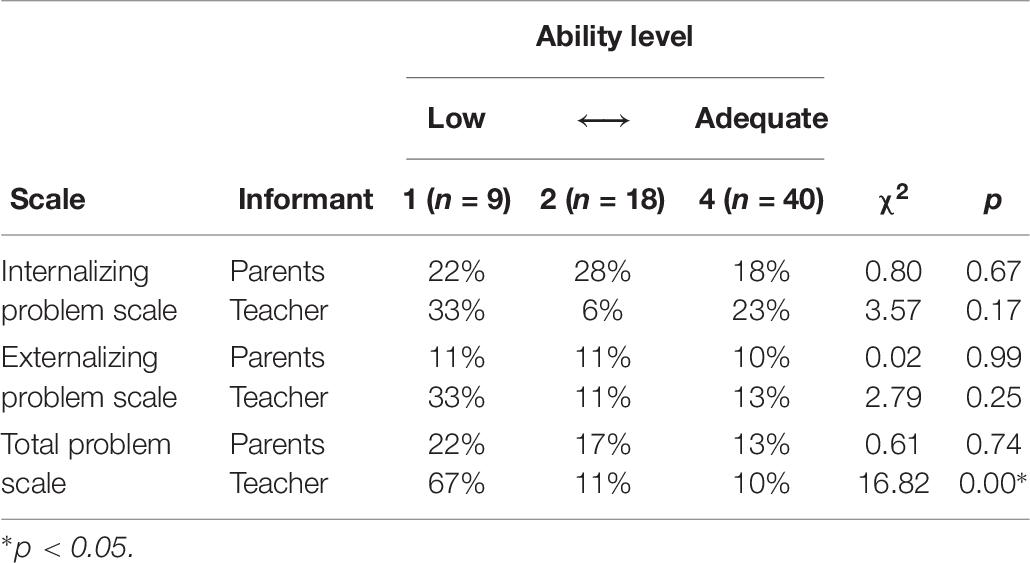
Table 6. Chi-square test of contingencies results and frequencies of reported behavioral problems reported by parents and teachers of CI children divided into speech perception and receptive vocabulary ability levels.
Discussion
Regarding the first aim of this study, the results showed that parents and teachers report a similar proportion of behavioral problems (internalizing, externalizing, and total) in profoundly HI children with CI compared to a hearing normative sample. Considering the previously reported high frequency of behavioral problems in profoundly HI children without CIs in the literature (30 to 50%), the difference is remarkable. The previous frequency of behavioral problems in profoundly HI children without implants was 1.6 to 2.7 times higher than that of the profoundly HI children with CIs in the present study (Mitchell and Quittner, 1996; Vostanis et al., 1997; van Eldik et al., 2004; van Eldik, 2005; van Gent et al., 2007). This difference in reported frequencies of behavioral problems in HI children with and without CI is probably due to the improved speech perception, whereas profoundly HI children with early implantation of CIs nowadays achieve speech perception scores comparable to children with moderate HI wearing hearing aids (Leigh et al., 2016; Nekes, 2016). However, Theunissen et al. (2014b) found that children with CIs show not the same, but less behavioral problems than moderate to severe HI children with hearing aids. They also found no correlations between unaided/aided degree of hearing loss and behavioral problems. These findings indicate that not only the degree of hearing impairment but also other factors are involved in developing behavioral problems in HI children. The other factors could include communicative abilities and language development. This present study confirms that language is also associated with behavioral problems in HI children with CIs in the school environment; children with low speech perception and poor language abilities show higher frequencies of behavioral problems reported by teachers.
Additionally, the results show overall fair to low agreements between the rates of reported behavioral problems by parents and teachers. These low agreement between parents’ and teachers’ rates of behavioral problems is probably due to the interaction between the environment and the communicative abilities of these CI children, as studies show that children’s behavior could be influenced by factors like school environment and family dynamics (Hinshaw and Lee, 2003). This could be an explanation for the differences found, since the children in the home environment communicate mainly with their parents and siblings. Educational contexts require different social, emotional and communication skills, there is more interaction with others like teachers and peers, than the home environment does (Calderon and Greenberg, 2003). Interactions with peers are still difficult for some children with CIs according to Huber et al. (2015). The low agreements between parents’ and teachers’ ratings of behavioral problems in CI children in the present study endorses the statement that information gathering about behavioral problems in children should be based on multi-informant information in different contexts (De Los Reyes et al., 2009; van der End et al., 2012).
Finally, regarding the relationship between speech perception and language skills with the frequency of reported behavioral problems, we observed a difference in the frequencies of total behavioral problems reported by teachers based on the ability level of the CI children. As expected, more children with low speech perception scores and low receptive vocabulary scores show clinically deviant behavioral problems compared to CI children with higher speech perception scores or both higher speech perception scores and higher receptive vocabulary scores. This is in line with other research; whereas adequate language and communication skills are known to prevent behavioral problems and better language development will lead to less behavioral problems (Theunissen et al., 2014a; Netten et al., 2018). In our study teachers reported that 67% (n = 6) of CI children with poor speech perception abilities and poor language development showed behavioral problems against 22% (n = 2) of the parents. This discrepancy between parents and teachers frequency ratings of behavioral problems in CI children with low speech perception and language abilities, and the overall low agreement between parents and teacher ratings could be attributed to the communication and language problems these CI children experience in the school environment as mentioned before. In addition to that, as suggested by Netten et al. (2015), enhancing the communicative abilities of HI children is likely to improve their social- and emotional functioning and diminish behavioral problems in the school environment. These findings may be somewhat limited due to the small sample sizes, especially in the low ability level groups. There are also group differences concerning unilateral and bilateral CI and educational setting. More children in the lowest ability level category have unilateral CI and are attending special schools. This could be related to low speech perception and receptive vocabulary, however, that is something that we have not investigated. Therefore, caution must be applied interpreting the differences in behavioral problems between the ability level categories.
Limitations
The first limitation of the current study is that we only used one receptive vocabulary test as a language measurement. A larger test battery of receptive and expressive language and communication development would be better to investigate the influence of communication problems in CI children on behavioral problems (Netten et al., 2015). Second, our study group and the Dutch normative sample differ in age range, therefore we could only compare the 6–16 group (n = 50) of our study group with the normative sample. A third limitation are the small sample sizes and group differences when measuring the effects of speech perception and receptive vocabulary on reported frequencies of behavioral problems. The small sample sizes could have influenced the statistical power of the analyses. The group differences concerning unilateral and bilateral CI and educational setting of the ability level categories could affect the outcomes in reported behavioral problems, whereas HI children in special educational settings are often more likely to have additional handicaps, lower socioeconomic status (SES) and less-communicative competences (Mitchell and Karchmer, 2011). This can be a factor in the development of behavioral problems. Therefore, caution must be applied interpreting the differences in behavioral problems between the ability level categories. The final limitation is the missing information of SES levels in our study group. Research shows that low SES is a consistent factor associated with behavioral problems (Letourneau et al., 2011). In our study it is unclear what influence SES has on results found.
Conclusion
Parents and teachers report similar frequencies of internalizing, externalizing and total behavioral problems in profoundly HI children with CIs compared to a hearing normative sample. Children with lower speech perception and language levels are more at risk of developing behavioral problems at school. It is therefore important to use a multi-informant approach from different environments. Adequate speech perception and language levels are found to be protective factors for the development of behavior.
Ethics Statement
The study was carried out in accordance with the recommendations of the Committee on Research Involving Human Subjects of the Radboud University Medical Center. All parents of the participants gave written informed consent for the use of the patient’s file data in accordance with the Declaration of Helsinki.
Author Contributions
ML and AV formulated the research question. MB and AV collected the data. All authors provided contributions to the analysis and interpretation of the data. MB wrote the first draft of the manuscript. AV, HM, EM, and ML provided the critical revisions. All authors approved the final version of the manuscript for submission.
Funding
This study was financially supported by the Cochlear Benelux.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Achenbach, T. M., and Rescorla, L. A. (2000). Manual for the ASEBA Preschool Forms & Profiles. Burlington: ASEBA.
Achenbach, T. M., and Rescorla, L. A. (2010). Multicultural Supplement to the Manual for the ASEBA Preschool Forms & Profiles. Burlington: ASEBA.
Barker, D. H., Quittner, A. L., Fink, N. E., Eisenberg, L. S., Tobey, E. A., Niparko, J. K., et al. (2009). Predicting behavior problems in deaf and hearing children: the influences of language, attention, and parent-child communication. Dev. Psychopathol. 21, 373–392. doi: 10.1017/S0954579409000212
Boons, T., De Raeve, L., Langereis, M., Peeraer, L., Wouters, J., and van Wieringen, A. (2013). Expressive vocabulary, morphology, syntax and narrative skills in profoundly deaf children after early cochlear implantation. Res. Dev. Disabil. 34, 2008–2022. doi: 10.1016/j.ridd.2013.03.003
Bosman, A. J., and Smoorenburg, G. F. (1995). Intelligibility of Dutch CVC syllables and sentences for listeners with normal hearing and with three types of hearing impairment. Audiology 34, 260–284. doi: 10.3109/00206099509071918
Brown, J. D., Wissow, L. S., Gadomski, A., Zachary, C., Bartlett, E., and Horn, I. (2006). Parent and teacher mental health ratings of children using primary-care services: interrater agreement and implications for mental health screening. Ambul. Pediatr. 6, 347–351. doi: 10.1016/j.ambp.2006.09.004
Calderon, R., and Greenberg, M. T. (2003). “Chapter: Social and emotional development of deaf children: family, school, and program effects,” in Oxford Handbook of Deaf Studies, Language, and Education, eds M. Marschark and P. E. Spencer (New York, NY: Oxford University Press), 177–189.
Chao, W. C., Lee, L. A., Liu, T. C., Tsou, Y. T., Chan, K. C., and Wu, C. M. (2015). Behavior problems in children with cochlear implants. Int. J. Pediatr. Otorhinolaryngol. 79, 648–653. doi: 10.1016/j.ijporl.2015.02.006
Cicchetti, D. V. (1994). Guidelines, criteria, and rules of thumb for evaluating normed and standerdized assessment intrustments in psychology. Psychol. Assess. 6, 284–290. doi: 10.1037/1040-3590.6.4.284
Colletti, L., Mandala, M., Zoccante, L., Shannon, R. V., and Colletti, V. (2011). Infants versus older children fitted with cochlear implants: performance over 10 years. Int. J. Pediatr. Otorhinolaryngol. 75, 504–509. doi: 10.1016/j.ijporl.2011.01.005
De Los Reyes, A., Henry, D. B., Tolan, P. H., and Wakschlag, L. S. (2009). Linking informant discrepancies to observed variations in young children’s disruptive behavior. J. Abnorm. Child Psychol. 37, 637–652. doi: 10.1007/s10802-009-9307-3
Dettman, S. J., Dowell, R. C., Choo, D., Arnott, W., Abrahams, Y., Davis, A., et al. (2016). Long-term communication outcomes for children receiving cochlear implants younger than 12 months: a multicenter study. Otol. Neurotol. 37, e82–e95. doi: 10.1097/MAO.0000000000000915
Dunn, L. M., and Dunn, D. M. (2005). Peabody Picture Vocabulary Test III-NL (Dutch Version). London: Pearson.
Fulcher, A., Purcell, A. A., Baker, E., and Munro, N. (2012). Listen up: children with early identified hearing loss achieve age-appropriate speech/language outcomes by 3 years-of-age. Int. J. Pediatr. Otorhinolaryngol. 76, 1785–1794. doi: 10.1016/j.ijporl.2012.09.001
Geers, A. E., and Nicholas, J. G. (2013). Enduring advantages of early cochlear implantation for spoken language development. J. Speech Lang. Hear. Res. 56, 643–655. doi: 10.1044/1092-4388(2012/11-0347)
Gentilli, N., and Holwell, A. (2011). Mental health in children with severe hearing impairment. Adv. Psychiatr. Treat. 17, 54–62. doi: 10.1192/apt.bp.109.006718
Hicks, C. B., and Tharpe, A. M. (2002). Listening effort and fatigue in school-age children with and without hearing loss. J. Speech Lang. Hear. Res. 45, 573–584. doi: 10.1044/1092-4388(2002/046)
Hinshaw, S. P., and Lee, S. S. (2003). “Conduct and oppositional defiant disorders,” in Child Psychopathology, 2 Edn, eds E. Mash and R. Barkley (New York, NY: The Guilford Press), 144–198.
Huber, M., Burger, T., Illg, A., Kunze, S., Giourgas, A., Braun, L., et al. (2015). Mental health problems in adolescents with cochlear implants: peer problems persist after controlling for additional handicaps. Front. Psychol. 6:953. doi: 10.3389/fpsyg.2015.00953
Huber, M., and Kipman, U. (2011). The mental health of deaf adolescents with cochlear implants compared to their hearing peers. Int. J. Audiol. 50, 146–154. doi: 10.3109/14992027.2010.533704
Khan, S., Edwards, L., and Langdon, D. (2005). The cognition and behaviour of children with cochlear implants, children with hearing aids and their hearing peers: a comparison. Audiol. Neurootol. 10, 117–126. doi: 10.1159/000083367
Kral, A., and O’Donoghue, G. M. (2010). Profound deafness in childhood. N. Engl. J. Med. 363, 1438–1450. doi: 10.1056/NEJMra0911225
Kuhl, P., and Rivera-Gaxiola, M. (2008). Neural substrates of language acquisition. Annu. Rev. Neurosci. 31, 511–534. doi: 10.1146/annurev.neuro.30.051606.094321
Langberg, J. M., Epstein, J. N., Simon, J. O., Loren, R. E., Arnold, L. E., Hechtman, L., et al. (2010). Parental agreement on ADHD symptom-specific and broadband externalizing ratings of child behavior. J. Emot. Behav. Disord. 18, 41–50. doi: 10.1177/1063426608330792
Leigh, J., Dettman, S., Dowell, R., and Briggs, R. (2013). Communication development in children who receive a cochlear implant by 12 months of age. Otol. Neurotol. 34, 443–450. doi: 10.1097/MAO.0b013e3182814d2c
Leigh, J. R., Dettman, S. J., and Dowell, R. C. (2016). Evidence-based guidelines for recommending cochlear implantation for young children: Audiological criteria and optimizing age at implantation. Int. J. Audiol. 55, 9–18. doi: 10.3109/14992027.2016.1157268
Letourneau, N. L., Duffett-Leger, L., Levac, L., Watson, B., and Young-Morris, C. (2011). Socioeconomic status and child development: a meta-analysis. J. Emot. Behav. Disord. 21, 211–224. doi: 10.1177/1063426611421007
Mitchell, R. E., and Karchmer, M. A. (2011). “Demographic and achievement characteristics of deaf and hard-of-hearing students,” in Oxford Handbook of Deaf Studies, Language, and Education, eds M. Marschark and P. E. Spencer (New York, NY: Oxford University Press), 18–31.
Mitchell, T. V., and Quittner, A. L. (1996). Multimethod study of attention and behavior problems in hearing-impaired children. J. Clin. Child Psychol. 25, 83–96. doi: 10.1207/s15374424jccp2501_10
Moeller, M. P. (2007). Current state of knowledge: psychosocial development in children with hearing impairment. Ear Hear. 28, 729–739. doi: 10.1097/aud.0b013e318157f033
Netten, A. P., Rieffe, C., Ketelaar, L., Soede, W., Gadow, K. D., and Frijns, J. H. M. (2018). Terrible twos or early signs of psychopathology? developmental patterns in early identified preschoolers with cochlear implants compared with hearing controls. Ear Hear. 39, 495–502. doi: 10.1097/AUD.0000000000000500
Netten, A. P., Rieffe, C., Theunissen, S. C., Soede, W., Dirks, E., Korver, A. M., et al. (2015). Early identification: language skills and social functioning in deaf and hard of hearing preschool children. Int. J. Pediatr. Otorhinolaryngol. 79, 2221–2226. doi: 10.1016/j.ijporl.2015.10.008
Niparko, J. K., Tobey, E. A., Thal, D. J., Eisenberg, L. S., Wang, N. Y., Quittner, A. L., et al. (2010). Spoken language development in children following cochlear implantation. JAMA 303, 1498–1506. doi: 10.1001/jama.2010.451
Park, M., Oh, S. H., Chang, S. O., Kim, C. S., and Lee, J. H. (2016). Long-term functional and behavioral-emotional outcomes in children with early cochlear implants: parental testimonies. Int. J. Pediatr. Otorhinolaryngol. 83, 137–142. doi: 10.1016/j.ijporl.2016.01.038
Schroeder, J. F., Hood, M. M., and Hughes, H. M. (2010). Inter-parent agreement on the syndrome scales of the child behavior checklist (CBCL): correspondence and discrepancies. J. Child Fam. Stud. 19, 646–653. doi: 10.1007/s10826-010-9352-0
Stevenson, J., Kreppner, J., Pimperton, H., Worsfold, S., and Kennedy, C. (2015). Emotional and behavioural difficulties in children and adolescents with hearing impairment: a systematic review and meta-analysis. Eur. Child Adolesc. Psychiatry 24, 477–496. doi: 10.1007/s00787-015-0697-1
Stevenson, J., McCann, D., Watkin, P., Worsfold, S., Kennedy, C. AND Hearing Outcomes Study Team. (2010). The relationship between language development and behaviourbehavior problems in children with hearing loss. J. Child Psychol. Psychiatry 51, 77–83. doi: 10.1111/j.1469-7610.2009.02124.x
Svirsky, M. A., Teoh, S. W., and Neuburger, H. (2004). Development of language and speech perception in congenitally, profoundly deaf children as a function of age at cochlear implantation. Audiol. Neurootol. 9, 224–233. doi: 10.1159/000078392
Theunissen, S. C., Rieffe, C., Kouwenberg, M., Soede, W., Briaire, J. J., and Frijns, J. H. (2011). Depression in hearing-impaired children. Int. J. Pediatr. Otorhinolaryngol. 75, 1313–1317. doi: 10.1016/j.ijporl.2011.07.023
Theunissen, S. C., Rieffe, C., Netten, A. P., Briaire, J. J., Soede, W., Schoones, J. W., et al. (2014a). Psychopathology and its risk and protective factors in hearing-impaired children and adolescents: a systematic review. JAMA Pediatr. 168, 170–177. doi: 10.1001/jamapediatrics.2013.3974
Theunissen, S. C., Rieffe, C., Kouwenberg, M., De Raeve, L. J. I., Soede, W., Briaire, J. J., et al. (2014b). Behavioral problems in school-aged hearing-impaired children: the influence of sociodemographic, linguistic, and medical factors. Eur. Child Adolesc. Psychiatry 23, 187–196. doi: 10.1007/s00787-013-0444-4
Theunissen, S. C., Rieffe, C., Soede, W., Briaire, J. J., Ketelaar, L., Kouwenberg, M., et al. (2015). Symptoms of psychopathology in hearing-impaired children. Ear Hear. 36, e190–e198. doi: 10.1097/AUD.0000000000000147
Tick, N. T., van der Ende, J., and Verhulst, F. C. (2007). Twenty-year trends in emotional and behavioral problems in Dutch children in a changing society. Acta Psychiatr. Scand. 116, 473–482. doi: 10.1111/j.1600-0447.2007.01068.x
Vaccari, C., and Marschark, M. (1997). Communication between parents and deaf children: implications for social-emotional development. Child Psychol. Psychiatry Allied Discipl. 38, 793–801. doi: 10.1111/j.1469-7610.1997.tb01597.x
van der Ende, J., Verhulst, F. C., and Tiemeier, H. (2012). Agreement of informants on emotional and behavioral problems from childhood to adulthood. Psychol. Assess. 24, 293–300. doi: 10.1037/a0025500
van Eldik, T. (2005). Mental health problems of Dutch youth with hearing loss as shown on the youth self report. Am. Ann. Deaf 150, 11–16. doi: 10.1353/aad.2005.0024
van Eldik, T., Treffers, P. D., Veerman, J. W., and Verhulst, F. C. (2004). Mental health problems of deaf Dutch children as indicated by parents’ responses to the child behavior checklist. Am. Ann. Deaf 148, 390–395. doi: 10.1353/aad.2004.0002
van Gent, T., Goedhart, A. W., Hindley, P. A., and Treffers, P. D. (2007). Prevalence and correlates of psychopathology in a sample of deaf adolescents. J. Child Psychol. Psychiatry 48, 950–958. doi: 10.1111/j.1469-7610.2007.01775.x
Verhulst, F. C., Van der Ende, J., and Koot, H. M. (1996). Handleiding voor de CBCL/4-18: Nederlandse Versie [Manual for the CBCL/4-18: Dutch Version]. Rotterdam: Sophia Kinderziekenhuis/Erasmus Universiteit.
Vostanis, P., Hayes, M., Du Feu, M., and Warren, J. (1997). Detection of behavioural and emotional problems in deaf children and adolescents: comparison of two rating scales. Child Care Health Dev. 23, 233–246. doi: 10.1111/j.1365-2214.1997.tb00966.x
Wiefferink, C. H., Rieffe, C., Ketelaar, L., and Frijns, J. H. (2012). Predicting social functioning in children with a cochlear implant and in normal-hearing children: the role of emotion regulation. Int. J. Pediatr. Otorhinolaryngol. 76, 883–889. doi: 10.1016/j.ijporl.2012.02.065
Keywords: cochlear implant, hearing loss, behavioral problems, education, speech perception, receptive vocabulary
Citation: Boerrigter M, Vermeulen A, Marres H, Mylanus E and Langereis M (2019) Frequencies of Behavioral Problems Reported by Parents and Teachers of Hearing-Impaired Children With Cochlear Implants. Front. Psychol. 10:1591. doi: 10.3389/fpsyg.2019.01591
Received: 19 September 2018; Accepted: 25 June 2019;
Published: 16 July 2019.
Edited by:
Gian Mauro Manzoni, eCampus University, ItalyReviewed by:
Zahra Jafari, University of Lethbridge, CanadaSeyed Basir Hashemi, Shiraz University of Medical Sciences, Iran
Emanuele Giusti, Catholic University of the Sacred Heart, Italy
Copyright © 2019 Boerrigter, Vermeulen, Marres, Mylanus and Langereis. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Merle Boerrigter, bWVybGUuYm9lcnJpZ3RlckByYWRib3VkdW1jLm5s; Emmanuel Mylanus, ZW1tYW51YWwubXlsYW51c0ByYWRib3VkdW1jLm5s
 Merle Boerrigter
Merle Boerrigter Anneke Vermeulen
Anneke Vermeulen Henri Marres
Henri Marres Emmanuel Mylanus1,2*
Emmanuel Mylanus1,2*