
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
BRIEF RESEARCH REPORT article
Front. Psychol. , 08 May 2019
Sec. Health Psychology
Volume 10 - 2019 | https://doi.org/10.3389/fpsyg.2019.01040
 Lauren B. Shomaker1,2,3*
Lauren B. Shomaker1,2,3* Bernadette Pivarunas1
Bernadette Pivarunas1 Shelly K. Annameier1
Shelly K. Annameier1 Lauren Gulley1,3
Lauren Gulley1,3 Jordan Quaglia4
Jordan Quaglia4 Kirk Warren Brown5
Kirk Warren Brown5 Patricia Broderick6
Patricia Broderick6 Christopher Bell7
Christopher Bell7Introduction: To explore if a brief mindfulness-based intervention (MBI) leads to sustained, improved clinical outcomes in adolescents at-risk for type 2 diabetes (T2D).
Methods: Participants were 12–17y girls with overweight/obesity, elevated depression symptoms, and T2D family history participating in a randomized, controlled pilot trial of a six-session MBI vs. cognitive-behavioral therapy (CBT) group. At baseline and 1-year, mindfulness, depression, insulin resistance (IR), and body composition were assessed with validated instruments.
Results: One-year retention was 71% (n = 12) in MBI; 81% (n = 13) in CBT. At 1-year, depression decreased (Cohen’s d = 0.68) and IR decreased (d = 0.73) in adolescents randomized to MBI compared to those in CBT. There were no significant between-condition differences in mindfulness, adiposity, or BMI.
Discussion: One-year outcomes from this randomized, controlled pilot trial suggest that brief MBI may reduce depression and IR in at-risk adolescents. Replication and exploration of mechanisms within the context of a larger clinical trial are necessary.
Clinical Trial Registration: www.ClinicalTrials.gov, identifier NCT02218138.
Mindfulness has been described in clinical contexts as paying attention in a purposeful way to the present moment, without judgment (Kabat-Zinn, 1994). In adults, mindfulness-based interventions (MBIs) have been utilized for managing common, chronic health conditions like type 2 diabetes (T2D). Randomized controlled trials in adults with diabetes show that MBIs have small-to-moderate effects for decreasing depression and heterogeneous effects for glycemic control (Abbott et al., 2014). MBIs are designed to address depression by increasing frequency of mindful states, thereby providing individuals with more effective ways of coping with stressors that accompany major health conditions.
Learning mindfulness-based coping skills during adolescence has potential to alter progression of metabolic abnormalities. In particular, adolescence is a sensitive period for insulin resistance (IR) that accompanies puberty. Pubertal IR triggers a trajectory toward worsening IR and eventual T2D in vulnerable youth (Kelsey and Zeitler, 2016). Adolescents at-risk for T2D are disproportionately female, from historically marginalized race/ethnicities, and frequently experience depression (Walders-Abramson et al., 2013). Depression symptoms are associated with greater IR in adolescents, predict worsening IR over time, and relate to T2D onset in young adulthood (Shomaker et al., 2011; Suglia et al., 2016). Depression is hypothesized to affect IR, independent of energy balance, through stress-related behavior (e.g., emotional-eating) and physiology (e.g., hypercortisolism). Therefore, intervening to increase mindfulness and decrease depression in adolescents at-risk for T2D is anticipated to ameliorate IR. MBIs may have salutary effects on IR through a number of mechanisms, including decreases in depression and increases in effective self-regulation of attention, stress, emotion, and behaviors important for IR, such as emotional eating (Lyons and Zelazo, 2011).
We conducted a randomized, controlled trial to pilot an MBI in adolescent girls at-risk for T2D with elevated depression symptoms. We had positive findings for the primary outcome of feasibility/acceptability (Shomaker et al., 2017). In secondary analyses, we found that adolescents in MBI had larger post-treatment decreases in depression and IR and larger 6-month decreases in depression, compared to cognitive-behavioral therapy (CBT; Shomaker et al., 2017).
The objective of this brief report was to explore 1-year outcomes. We hypothesized that adolescents randomized to MBI would have lower depression and IR at 1-year than CBT participants, based upon our initial findings and the notion that MBI may be uniquely suited for the high-stress arousal and psychosocial context of adolescents at-risk for T2D (Shomaker et al., 2017). In contrast to CBT depression interventions that focus on restructuring negative thoughts and increasing positive behaviors, MBI centers on cultivating self-regulation through present-focused, non-judgmental attention to one’s body, emotions, and thoughts. The current analysis directly addresses shortcomings of existing literature by relying on a randomized controlled design, using an active comparator, and conducting long-term follow-up (Van Dam et al., 2017).
Adolescents were recruited for a prevention of T2D pilot trial, conducted at an academic setting in the western region of the United States between January 2014–August 2016 (ClinicalTrials.gov: NCT02218138). Participants were girls, mean ± SDage 14.99 ± 1.69y (Range 12–17y) of all racial/ethnic backgrounds (70% non-Hispanic White, 21% Hispanic, 9% American Indian) predisposed to elevated IR by overweight/obesity (BMI ≥ 85th percentile) and T2D family history. The Institutional Review Board of Colorado State University approved all procedures. Youth had elevated depression, based on a total score ≥ 16 on the Center for Epidemiologic Studies-Depression Scale (CES-Dtotalscore 25.27 ± 6.63). Baseline exclusion criteria were pregnancy, major depressive disorder or diagnosis warranting treatment, major medical problem (e.g., T2D), medication affecting mood/insulin, or psychotherapy. Parental guardians provided written informed consent, and adolescents gave written assent, after having the study described to them in detail.
Following an appointment to screen eligibility and collect baseline assessments, adolescents were randomized to a six-session MBI group (Learning to BREATHE; n = 17) or six-session CBT depression prevention group (Blues Program; n = 15) (Shomaker et al., 2017). The randomization sequence was generated by an electronic program using permuted blocks and stratified by age and race/ethnicity. Interventions were matched for time and attention. Sessions were co-facilitated by a clinical psychologist and graduate student in psychology or marriage and family therapy. Phlebotomists were blinded to allocation; trained research associates or graduate research assistants served as assessors of psychosocial characteristics and body measurements, and they were not consistently blinded.
For the current brief report, measures collected at baseline and 1-year were evaluated. The CES-D measured depression symptoms and the Mindful Attention Awareness Scale (MAAS) assessed basic dispositional mindfulness. IR was estimated with homeostasis model assessment of IR (HOMA-IR), a surrogate with good convergent validity with hyperinsulinemic euglycemic clamp-derived measures (George et al., 2011). Adiposity was measured as percentage total fat-mass from dual-energy x-ray absorptiometry. Tanner-breast stage was self-reported. BMI-metrics were determined from fasting weight/height according to Centers for Disease Control and Prevention 2000 standards.
A pilot sample size of n = 15–25 per arm is recommended for informing a main trial in which small-to-moderate standardized effects are anticipated (Whitehead et al., 2016). All variables approximated a normal distribution. Using IBM SPSS Statistics 25, EM (expectation–maximation) was used to impute missing data. Univariate ANCOVA with the intent-to-treat sample was used to evaluate condition (MBI vs. CBT) as a predictor of baseline-to-1-year change in depression and IR. Covariates were race/ethnicity, baseline level of each outcome, age, weight status (overweight BMI 85th–94th percentile vs. obesity BMI ≥ 95th percentile), puberty (Tanner 5 reported breast development vs. Tanner 3–4), adiposity, and 1-year adiposity change. ANCOVA also was used to describe between-condition and within-condition differences in baseline-to-1-year change in dispositional mindfulness, BMI indices, and adiposity. In addition to statistical significance (p < 0.05), we estimated effect size with Cohen’s d (small: 0.2, medium: 0.5, large ≥ 0.8).
Descriptive information on baseline and 1-year sample characteristics is provided in Supplementary Table 1. One-year retention was 71% (n = 12) in MBI; 81% (n = 13) in CBT (p = 0.48). Baseline characteristics were not significantly related to retention.
Table 1 summarizes baseline-to-1-year changes by condition, accounting for covariates. Depression decreased from baseline-to-1-year within MBI and CBT, with a greater decrease in MBI (d = −0.68, p = 0.03; Figure 1). Adolescents in MBI decreased baseline-to-1-year IR compared to stable IR in CBT, with a moderate, between-condition effect size(d = 0.73, p < 0.01).
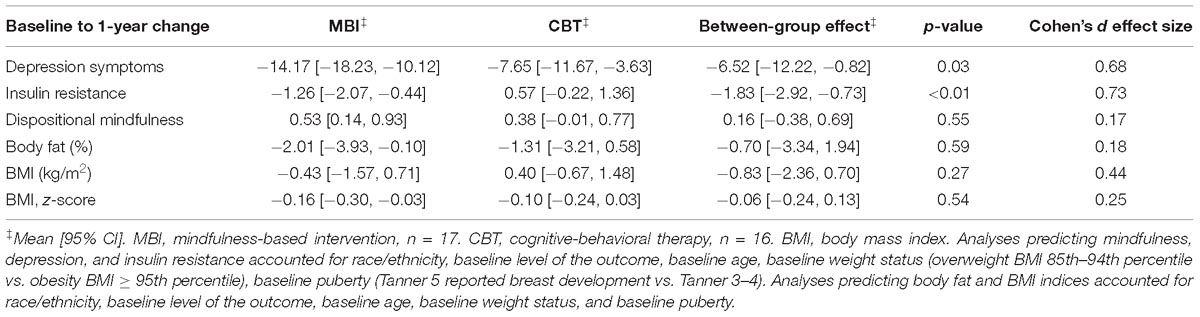
Table 1. Summary of univariate analyses of covariance (ANCOVA) predicting change in outcome from group condition.
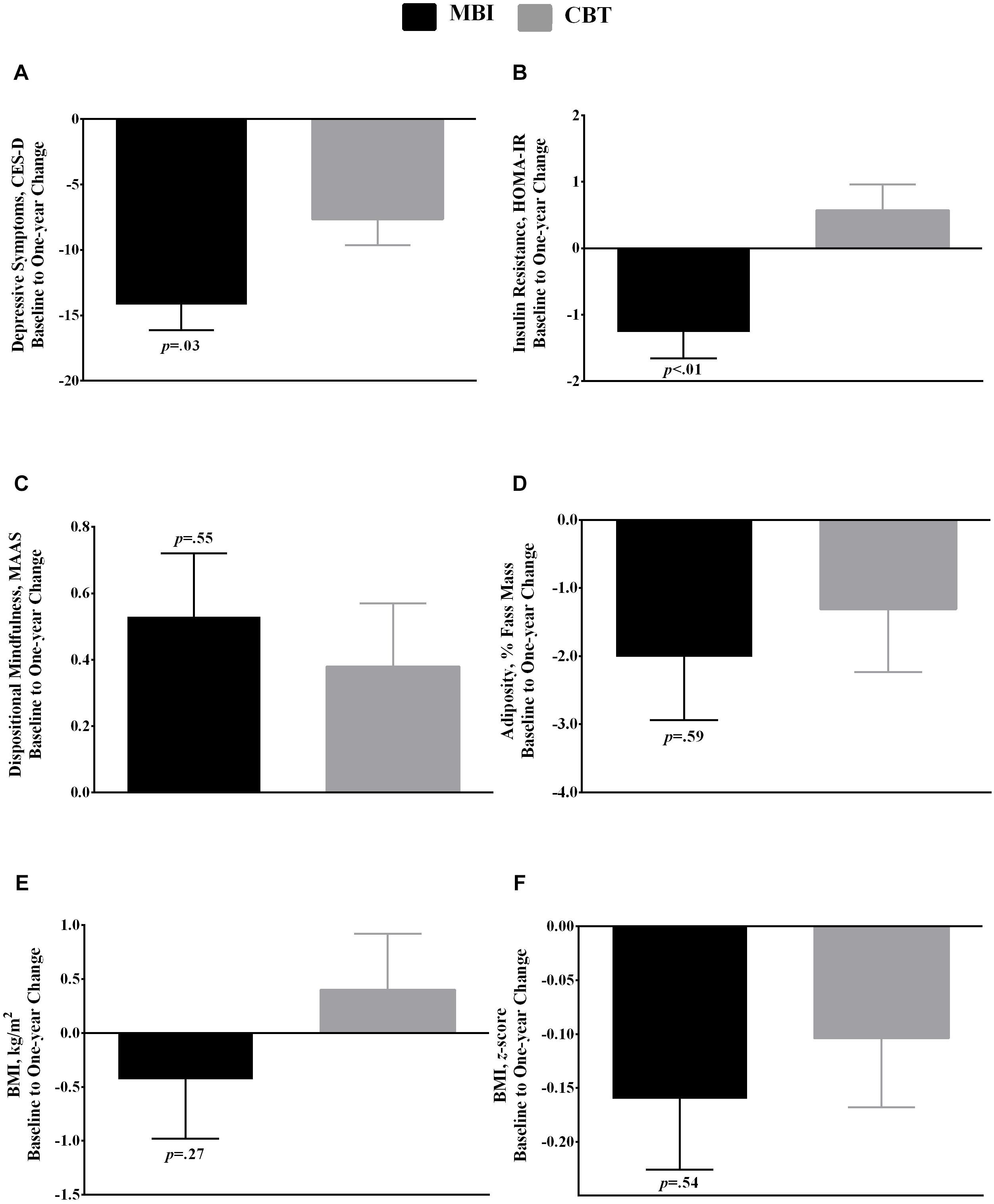
Figure 1. Baseline to 1-year change (Mean, SE) in (A) depression symptoms, (B) homeostasis model assessment of insulin resistance (HOMA-IR), (C) dispositional mindfulness, (D) adiposity (%), (E) body mass index (BMI; k/gm2), and (F) BMI z-score by condition: MBI (mindfulness-based group intervention; n = 17) vs. CBT (cognitive-behavioral therapy; n = 16) group intervention. P-values refer to the between-group difference in baseline to 1-year change, derived from univariate analyses of covariance (ANCOVA) using the intent-to-treat sample with EM (expectation–maximation) to handle missing data. Models a, b, and c accounted for race/ethnicity, baseline level of the outcome, baseline age, baseline weight status (overweight BMI 85th–94th percentile vs. obesity BMI ≥ 95th percentile), baseline puberty (Tanner 5 reported breast development vs. Tanner 3–4), baseline adiposity, and 1-year change in adiposity. Models d and e accounted for race/ethnicity, baseline level of the outcome, baseline age, baseline weight status, and baseline puberty.
There were no other between-condition differences. Mindfulness increased from baseline-to-1-year within MBI, with no within-group change in CBT (dbetween–group = 0.17, p = 0.55). Adiposity decreased within MBI, with no change within CBT (dbetween–group = 0.18, p = 0.59). Likewise, BMI z-score decreased within MBI, with no change within CBT (dbetween–group = 0.25, p = 0.54). BMI raw-score change was stable within both conditions (dbetween–group = 0.44, p = 0.27).
Consistent with previous findings (Shomaker et al., 2017), adolescents at-risk for T2D with elevated depression had greater decreases in depression symptoms 1-year following a six-session MBI, as compared to adolescents who were randomized to CBT. Yet, adolescents in both conditions significantly decreased depression symptoms. Additionally, even after accounting for change in adiposity, we observed a moderate between-condition effect for MBI in reducing 1-year IR, as compared to stable IR in CBT. To our knowledge, this is the first randomized controlled trial to pilot a comparison of MBI and CBT in adolescents. In adults with vascular disease, MBIs have consistently shown greater decreases in depression symptoms as compared to a control condition (Abbott et al., 2014), but equivocal effects for decreasing depression as compared to CBT (Tovote et al., 2015).
In this pilot study, dispositional mindfulness increased at 1-year within MBI only, but the between-condition difference was a non-significant, small effect relative to CBT. One possibility is that by more effectively decreasing depression, MBI improves underlying behavioral and/or physiological factors that affect IR such as sleep, physical activity, eating behavior, and stress arousal. A significant limitation is the pilot nature of the current study; the small sample size warrants caution regarding interpretation of effect sizes (Kraemer et al., 2006). Provided replication with a larger sample, the current findings suggest there may be promise for relatively brief MBI approaches to lessen T2D risk in adolescents with depression. Differentiating mechanisms of MBI vs. CBT in adolescents at-risk for T2D is an important step for future research. Pinpointing mechanisms would help to refine theoretical models and ultimately, aid in developing scalable integrative health interventions for this group of at-risk adolescents.
This study was carried out in accordance with the recommendations of American Psychological Association with written informed consent from all subjects. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Institutional Review Board of Colorado State University.
LS conceived the research design, obtained funding for the study, facilitated the interventions, oversaw data collection, conducted the data analysis, and drafted the manuscript. BP facilitated the interventions, collected the data, and edited the manuscript. SA cleaned the data, contributed to the interpretation of results, and edited the manuscript. LG contributed to the interpretations of results and edited the manuscript. JQ assisted in designing the study, contributed to the data collection, interpreted the results, and edited the manuscript. KB assisted in designing and obtaining funding for the study, interpreted the results, and edited the manuscript. PB designed the intervention, trained and supervised the facilitators, and edited the manuscript. CB assisted in designing and obtaining funding for the study, conducted the statistical analysis, interpreted the results, and edited the manuscript.
This work was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development, National Institutes of Health (R00HD069516).
PB, author of Learning to BREATHE, receives royalty fees from New Harbinger Publications.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyg.2019.01040/full#supplementary-material
Abbott, R. A., Whear, R., Rodgers, L. R., Bethel, A., Thompson Coon, J., Kuyken, W., et al. (2014). Effectiveness of mindfulness-based stress reduction and mindfulness based cognitive therapy in vascular disease: a systematic review and meta-analysis of randomised controlled trials. J. Psychosom. Res. 76, 341–351. doi: 10.1016/j.jpsychores.2014.02.012
George, L., Bacha, F., Lee, S., Tfayli, H., Andreatta, E., and Arslanian, S. (2011). Surrogate estimates of insulin sensitivity in obese youth along the spectrum of glucose tolerance from normal to prediabetes to diabetes. J. Clin. Endocrinol. Metab. 96, 2136–2145. doi: 10.1210/jc.2010-2813
Kelsey, M. M., and Zeitler, P. S. (2016). Insulin resistance of puberty. Curr. Diab. Rep. 16:64. doi: 10.1007/s11892-016-0751-5
Kraemer, H. C., Mintz, J., Noda, A., Tinklenberg, J., and Yesavage, J. A. (2006). Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch. Gen. Psychiatry 63, 484–489. doi: 10.1001/archpsyc.63.5.484
Lyons, K. E., and Zelazo, P. D. (2011). Monitoring, metacognition, and executive function: elucidating the role of self-reflection in the development of self-regulation. Adv. Child Dev. Behav. 40, 379–412. doi: 10.1016/b978-0-12-386491-8.00010-4
Shomaker, L. B., Bruggink, S., Pivarunas, B., Skoranski, A., Foss, J., Chaffin, E., et al. (2017). Pilot randomized controlled trial of a mindfulness-based group intervention in adolescent girls at risk for type 2 diabetes with depressive symptoms. Compl. Ther. Med. 32, 66–74. doi: 10.1016/j.ctim.2017.04.003
Shomaker, L. B., Tanofsky-Kraff, M., Stern, E. A., Miller, R., Zocca, J. M., Field, S. E., et al. (2011). Longitudinal study of depressive symptoms and progression of insulin resistance in youth at risk for adult obesity. Diabetes Care 34, 2458–2463. doi: 10.2337/dc11-1131
Suglia, S. F., Demmer, R. T., Wahi, R., Keyes, K. M., and Koenen, K. C. (2016). Depressive symptoms during adolescence and young adulthood and the development of type 2 diabetes mellitus. Am. J. Epidemiol. 183, 269–276. doi: 10.1093/aje/kwv149
Tovote, K. A., Schroevers, M. J., Snippe, E., Sanderman, R., Links, T. P., Emmelkamp, P. M., et al. (2015). Long-term effects of individual mindfulness-based cognitive therapy and cognitive behavior therapy for depressive symptoms in patients with diabetes: a randomized trial. Psychother. Psychosom. 84, 186–187. doi: 10.1159/000375453
Van Dam, N. T., van Vugt, M. K., Vago, D. R., Schmalzl, L., Saron, C. D., Olendzki, A., et al. (2017). Mind the hype: a critical evaluation and prescriptive agenda for research on mindfulness and meditation. Perspect. Psychol. Sci. 13, 36–61. doi: 10.1177/1745691617709589
Walders-Abramson, N., Nadeau, K. J., Kelsey, M. M., Schmiege, S. J., Ellert, S., Cejka, A., et al. (2013). Psychological functioning in adolescents with obesity co-morbidities. Child. Obes. 9, 319–325. doi: 10.1089/chi.2012.0120
Whitehead, A. L., Julious, S. A., Cooper, C. L., and Campbell, M. J. (2016). Estimating the sample size for a pilot randomised trial to minimise the overall trial sample size for the external pilot and main trial for a continuous outcome variable. Stat. Methods Med. Res. 25, 1057–1073. doi: 10.1177/0962280215588241
Keywords: mindfulness, cognitive-behavioral therapy, depression, insulin resistance, type 2 diabetes, adolescents
Citation: Shomaker LB, Pivarunas B, Annameier SK, Gulley L, Quaglia J, Brown KW, Broderick P and Bell C (2019) One-Year Follow-Up of a Randomized Controlled Trial Piloting a Mindfulness-Based Group Intervention for Adolescent Insulin Resistance. Front. Psychol. 10:1040. doi: 10.3389/fpsyg.2019.01040
Received: 05 October 2018; Accepted: 23 April 2019;
Published: 08 May 2019.
Edited by:
Francesco Pagnini, Catholic University of the Sacred Heart, ItalyReviewed by:
Christianne Joy Lane, University of Southern California, United StatesCopyright © 2019 Shomaker, Pivarunas, Annameier, Gulley, Quaglia, Brown, Broderick and Bell. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lauren B. Shomaker, bGF1cmVuLnNob21ha2VyQGNvbG9zdGF0ZS5lZHU=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.