
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
ORIGINAL RESEARCH article
Front. Psychol. , 08 May 2019
Sec. Psychopathology
Volume 10 - 2019 | https://doi.org/10.3389/fpsyg.2019.01003
The aim of this study was to examine alcohol/drug use and problems across psychiatric diagnoses and to what extent associations between each psychiatric diagnosis and alcohol/drug use and problems were independent from the potential confounding effects of psychiatric comorbidity, socioeconomic status, sex and age. We used a dataset comprising a linkage between a large population-based and cross-sectional study among Norwegian adolescents (the youth@hordaland conducted in 2012) and national registry-based data on specialist mental health care use during the 4 years prior to the survey (2008 to 2011). The study sample included 16 to 19 year olds who participated in the youth@hordaland survey and consented to the linkage with patient registry data (n = 9,408). Among these, 853 (9%) had received specialist mental health care and comprised the clinical group, while the rest (n = 8,555) comprised the comparison group. The main outcome variables were several self-reported indicators for alcohol/drug use, including any alcohol use, frequent alcohol intoxication, high-level alcohol consumption, and lifetime illicit drug use, as well as one indicator for potential alcohol/drug-related problems: a positive CRAFFT-score. Adolescents receiving specialist mental health care (n = 853) reported more frequently alcohol/drug use and problems compared to adolescents not receiving these services (Cohens d’s ranging from 0.09 to 0.29, all p ≤ 0.01). Anxiety, depression, conduct disorders, eating disorders, ADHD, and trauma-related disorders were all associated with single measures of alcohol/drug use and problems, with odds ratios (ORs) ranging from 1.58 to 4.63, all p < 0.05) in unadjusted models. Trauma-related disorders, depression and conduct disorders were also positively associated with higher scores on a combined indicator of alcohol/drug use and problems (ORs ranging from 1.89 to 3.15, all p < 0.01), even after the full adjustment from psychiatric comorbidity and sociodemographic variables (adjusted odds ratios ranging from 1.61 to 2.79, p < 0.05). These results suggest that alcohol/drug use and problems were slightly more common among adolescents who received specialist mental health care during the past 4 years compared with the general adolescent population, and adolescents with trauma-related disorders, depression and conduct disorders were high-risk groups for alcohol/drug use and problems.
Mental health problems are prevalent among children and adolescents, with one in five fulfilling criteria for a psychiatric diagnosis (Canino et al., 2004; Belfer, 2008; Merikangas et al., 2010; Barkmann and Schulte-Markwort, 2012). Approximately, 25% of adolescents with a psychiatric diagnosis have at least one additional psychiatric diagnosis (Costello et al., 2003), indicating that psychiatric comorbidity is common. Psychiatric diagnoses are particularly frequent among adolescents with alcohol/drug-related problems, and it is estimated that 37–80% of adolescents with alcohol/drug-related problems have at least one psychiatric diagnosis (e.g., Regier et al., 1990; Rohde et al., 1996; Armstrong and Costello, 2002). Similarly, among adolescents within a psychiatric inpatient setting, one third of the adolescents fulfilled criteria for a substance use disorder (SUD) (Deas-Nesmith et al., 1998).
Previous studies have demonstrated positive associations between a range of psychiatric diagnoses and adolescent alcohol/drug-related problems. Specifically, these findings include anxiety (Kedzior and Laeber, 2014; Stapinski et al., 2016), attention-deficit/hyperactivity disorder (ADHD) (Groenman et al., 2013; Zulauf et al., 2014), eating disorders (Castro-Fornieles et al., 2009; Bisetto et al., 2011), post-traumatic stress disorder (PTSD) (Wolitzky-Taylor et al., 2012; Haller and Chassin, 2014), conduct disorders (Khoddam et al., 2016), depression (Wolitzky-Taylor et al., 2012; Heron et al., 2013; Edlund et al., 2015), and psychotic disorders (Ferdinand et al., 2005; Addington and Addington, 2007). The majority of previous literature has focused on selected associations between single psychiatric diagnoses and symptoms and alcohol/drug-related problems, and few studies have investigated the full range of common psychiatric diagnoses in a single model.
A notable exception is a recent Norwegian study which reported that illicit drug use was four times higher among adolescents receiving psychiatric services compared to the general population (Mangerud et al., 2014). They also reported that depression was the diagnosis associated with the highest frequencies of alcohol and drug use and autism with the lowest; however, participation in the clinical group was low and psychiatric comorbidity was not investigated. Similarly, a study by Wu et al. (2011) investigated associations between a range of psychiatric diagnoses and SUDs. They reported positive associations with SUDs for mood disorders, ADHD, and conduct disorders, while the role of psychiatric comorbidity was not investigated. A study by Boys et al. (2003) on a broad range of psychiatric diagnoses in relation to alcohol/drug-related problems, reported that there was an increased risk of substance use among those with a psychiatric disorder. However, small numbers did not allow differentiation between separate disorders. In sum, there is still limited knowledge on which psychiatric diagnoses are associated with the highest risk for alcohol/drug use and problems among adolescents.
It is also important to consider psychiatric comorbidity in order to clarify whether specificity of risk is indicative of potentially unique psychological mechanisms, or whether “general mental distress” is primarily driving an increased vulnerability for alcohol/drug-related problems. Although some studies have adjusted for psychiatric comorbidity in associations between single psychiatric diagnoses and selected comorbid psychiatric diagnoses (August et al., 2006; Maslowsky and Schulenberg, 2013), the inclusion of psychiatric comorbidity is overall rare. To our knowledge, no previous studies have analyzed associations between a broad range of psychiatric diagnoses and alcohol/drug use and problems among adolescents, while also attempting to adjust these associations from the potential confounding effects of comorbid psychiatric diagnoses. In addition, socioeconomic status (SES), age and gender have been shown to be associated with both mental health and substance use during adolescence (e.g., Van Oers et al., 1999; Schulte et al., 2009), and are as such important co-variates to be considered.
In the present study, we aimed to examine the frequencies of alcohol/drug use and problems among adolescents receiving specialist mental health care compared with a general population of adolescents. In addition, we investigated associations between a broad range of psychiatric diagnoses and alcohol/drug use and problems, while also accounting for the potential confounding effects of other comorbid psychiatric diagnoses, as well as sex, age, and SES. We hypothesized that all psychiatric diagnostic categories – except autism – would be associated with some measure of alcohol/drug use and problems. The lack of similar studies did not allow for specific hypotheses on which diagnoses would have the strongest associations with substance use after the adjustment for psychiatric comorbidity and demographics.
We employed data from the youth@hordaland-survey, which includes information on child and adolescent mental health, lifestyle, school performance and use of health services. Of all 19,430 adolescents born between 1993 and 1995 living in Hordaland County in Western Norway, 10,253 (53%) agreed to participate. The youth@hordaland-survey is a cross-sectional population-based study carried out during early 2012, when the adolescents ranged from 16 to 19 years of age. Participants received information by email and one school hour was used to complete the questionnaires. In addition, adolescents not going to school received the questionnaires by mail at their home address, and mental health services and other institutions were contacted to allow participation for adolescents in these settings. The questionnaires used in the youth@hordaland-survey were web-based.
We linked data from the youth@hordaland-survey to data from the National Patient Registry (NPR) through the participants’ personal identification number. The NPR is the official national registry in Norway on specialist mental health care services, and includes information on specialist mental health care use and Axis 1 psychiatric diagnoses from January 2008 to December 2011, at a time when the adolescents ranged from 12 to 18 years of age, and before youth@hordaland participation. 845 (8.2%) of the adolescents did not provide consent for merging the data from the youth@hordaland-survey with other registries, and were excluded from the analyses. The final sample therefore included 9,408 participants, of whom 853 (9.1%) had at least one registration in NPR.
The Regional Committee for Medical and Health Research Ethics (REC) in Western Norway approved the study. In accordance with the regulations from the REC and Norwegian health authorities, adolescents aged 16 years and older can make decisions regarding their own health (including participation in research). All participants of the study gave written informed consent themselves to participate in the current study. Parents/guardians have the right to be informed, and in the current study, all parents/guardians received written information about the study in advance.
The adolescents who had received specialist mental health care (n = 853), were assigned to the following diagnostic categories: anxiety (n = 132), depression (n = 172), conduct disorders (n = 32), attention-deficit/hyperactivity disorder (ADHD, n = 154), autism spectrum disorders (n = 46), eating disorders (n = 40), trauma-related disorders (n = 66), psychotic disorders (n = 10), other diagnoses (n = 84), and no Axis 1 psychiatric diagnosis (n = 329). 133 adolescents had psychiatric diagnoses from more than one of the specified diagnostic categories, and were assigned to multiple diagnostic categories. Appendix I details the operationalization of the diagnostic categories. Of note, none of the participants who were registered with mental health care use were given a substance-related disorder diagnosis.
Self-reported mental health problems were measured in order to examine differences between individuals that consented (n = 9,408) to the linkage between the youth@hordaland-survey and the NPR, and those that did not consent to this linkage (n = 845). Specifically, the short version of the Mood and Feelings Questionnaire (SMFQ) (Thapar and McGuffin, 1998) was used to measure symptoms of depression; the SCARED inventory (Birmaher et al., 1999) was used for anxiety symptoms; the Adult ADHD Self-report Scale (ASRS) (Kessler et al., 2007) for symptoms of hyperactivity/inattention; and the Youth Conduct Disorder (YCD) instrument (Lucas et al., 2001) for symptoms of conduct disorders.
We constructed a variable for lifetime alcohol use based on a single item: ‘Have you ever tried alcohol?’ (Yes/No). Similarly, we constructed a variable for lifetime illicit drug use based on a single item: ‘Have you ever tried hash, marijuana or other narcotic substances?’ (Yes/No). We measured frequent alcohol intoxication with the question: ‘Have you ever consumed so much alcohol that you were clearly intoxicated (drunk)?’ The original item had five categories ranging from ‘No, never’ to ‘Yes, more than 10 times.’ Frequent alcohol intoxication was defined as drinking so much that one was clearly intoxicated more than 10 times, and on this basis, a dichotomous variable was created. We added up five items that measured how many glasses of (i) beer, (ii) cider, (iii) wine, (iv) spirits, and (v) illegally distilled spirits the adolescents usually consumed during a time period of 14 days. 5,058 adolescents reported any usual alcohol consumption. The high-level alcohol consumption variable was defined as the above 90th sex-specific percentile alcohol consumption among the adolescents with any usual alcohol consumption, and a dichotomous variable was created for high-level alcohol consumption (Heradstveit et al., 2017). We also used the six-item, validated CRAFFT scale, in order to indicate adolescents that had a positive CRAFFT score. CRAFFT stands for the key words of the six items included in the scale – Car, Relax, Alone, Forget, Friends, Trouble. This scale has been designed to identify potential alcohol-and drug related problems among adolescents and has been demonstrated to have acceptable sensitivity and specificity at a cut-off of ≥2 relative to classifications of problem substance use, substance abuse or substance dependence as identified in structured clinical interviews (Knight et al., 2002; Dhalla et al., 2011). A previous publication based on the youth@hordaland-sample investigated the factor structure and concurrent validity of CRAFFT in relation to self-reported excessive alcohol consumption, frequent binge drinking, and any illicit drug use – and demonstrated a good fit with a single latent construct of alcohol/drug-related problems (Skogen et al., 2013). A dichotomous variable separating those above the cut-off of ≥ 2 on CRAFFT from those below the cut-off were calculated. In our sample the omega internal consistency coefficient (McDonald, 2013) of the CRAFFT scale was 0.88.
Finally, an ordinal variable for level of risky substance use was constructed (ranging from 0 to 4), in which we summed up the number of positive scores on lifetime illicit drug use, frequent alcohol intoxication, high-level alcohol consumption, and CRAFFT-scores ≥ 2.
Age and sex were retrieved from the Norwegian Population Registry, and were available for all participants in the youth@hordaland-sample. In addition, self-reported family financial circumstances was collected as either (1) ‘about the same as others,’ (2) ‘better than others,’ or (3) ‘worse than others.’ Self-reported information on maternal and paternal educational attainment was divided into primary school, high school, or more than 4 years of university or higher education. The variables of self-reported family financial circumstances, paternal educational attainment, and maternal educational attainment were used as a compound measure for SES (Skogen et al., 2014).
All analyses were performed using STATA V.14.0 (StataCorp, 2015), with the exception that the omega internal consistency coefficient for the CRAFFT questionnaire was calculated in R Core Team (2018). First, frequencies of alcohol/drug use and problems, self-reported symptoms of mental health problems, and sociodemographic variables were examined across individuals who gave their consent to the linkage between the youth@hordaland-survey and the NPR, and those who refused to consent to this linkage (Table 1). Second, the sample was described according to age, sex, SES, and alcohol/drug use and problems among adolescents that had received specialist mental health care services compared to the adolescents that had not receiving these services during the past 4 years (Table 2). Third, psychiatric comorbidity rates within each diagnostic category were described, and all investigated psychiatric diagnoses were analyzed in terms of Spearman’s Rank correlations with other psychiatric diagnoses (Table 3). Fourth, logistic regression models were employed to calculate associations between psychiatric diagnoses received within specialist mental health care and single measures of alcohol/drug use and problems. We then adjusted for the potential confounding effects of comorbid psychiatric diagnoses, in order to determine the independence of associations between each psychiatric diagnosis and substance use. For each psychiatric diagnosis that was investigated, all other psychiatric diagnostic categories were separately entered as potential confounding variables. Finally, we adjusted the analyses for the confounding effects of comorbid psychiatric diagnoses, as well as age, sex and SES (Table 4). Finally, ordered logistic regression models were employed to calculate unadjusted and adjusted odds ratios for the associations between psychiatric diagnoses and the total degree of risky substance use (Table 5). Due to the small size of the psychotic disorders group (n = 10), and due to considerable conceptual heterogeneity within the “other diagnoses” group and the “no Axis 1 diagnosis” group, we did not perform analyses of associations between these categories and substance use.
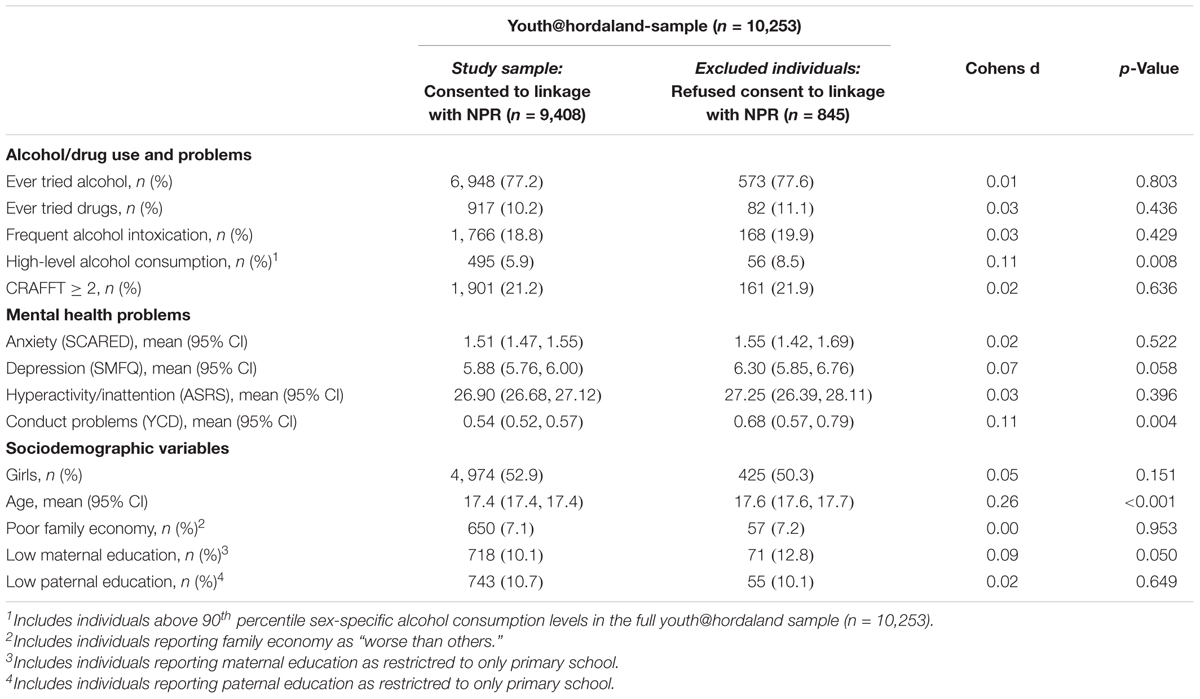
Table 1. Frequencies of alcohol/drug use and problems, mental health problems, and sociodemographic characteristics in adolescents excluded from the study sample (n = 845), compared with adolescents in the study sample (n = 9,408).
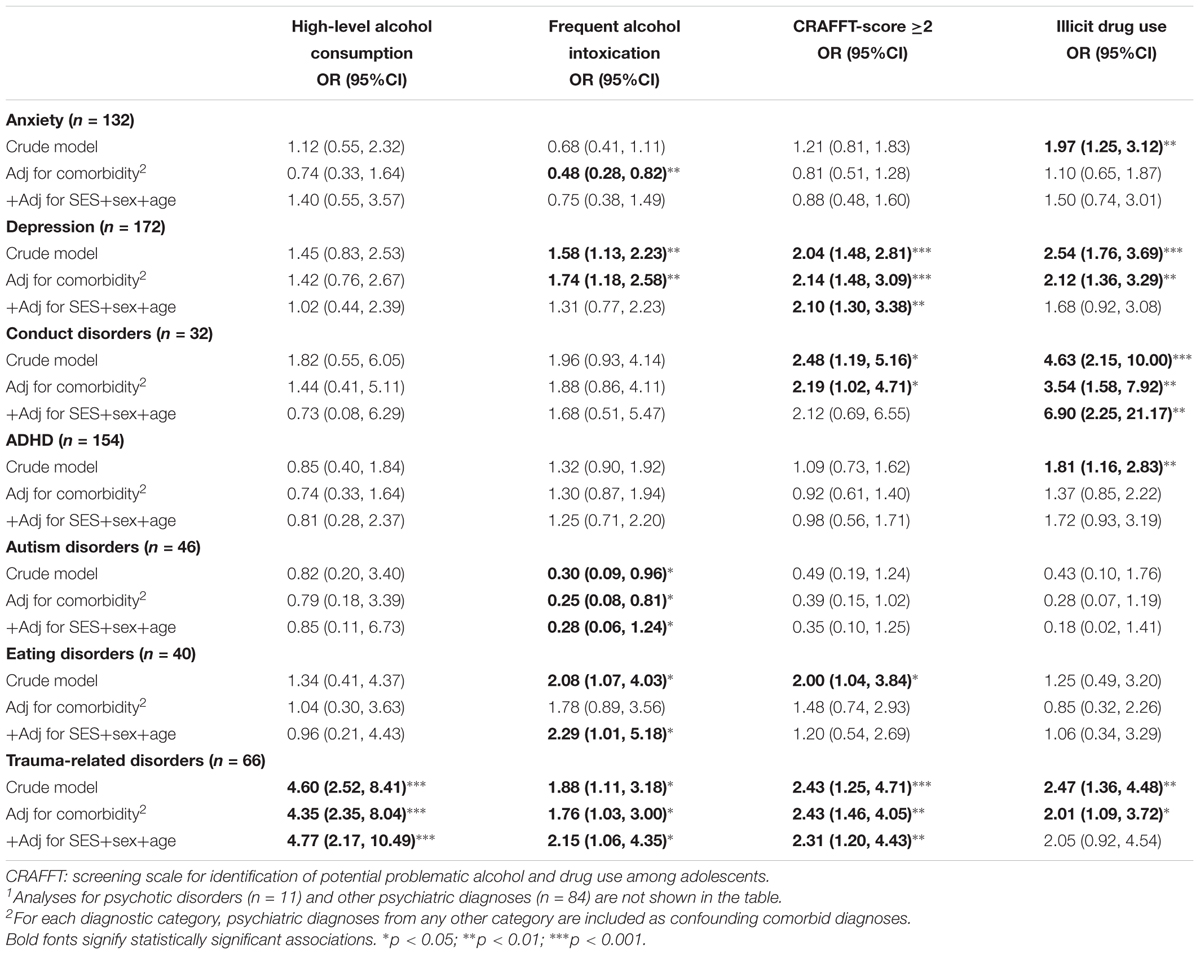
Table 4. Logistic regression analyses of associations between psychiatric diagnoses and alcohol/drug use and problems (n = 9,408)1.
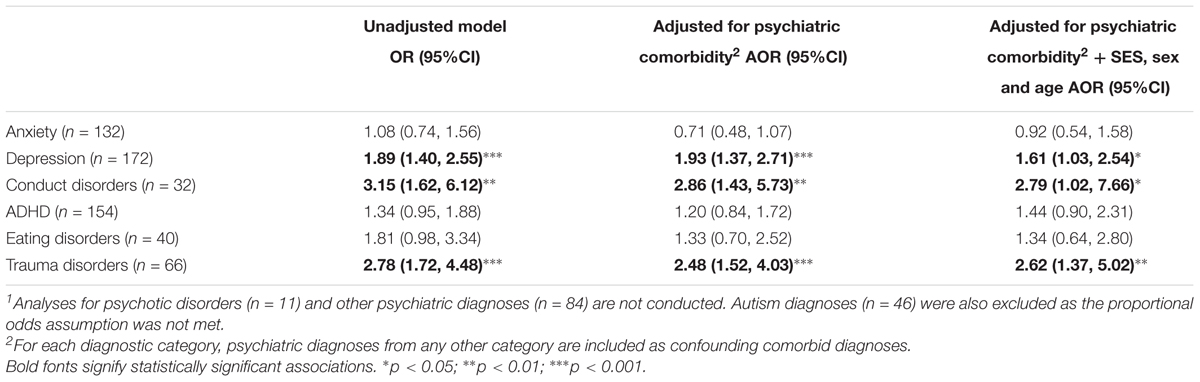
Table 5. Ordered logistic regression analyses of associations between psychiatric diagnoses and the total degree of risky substance use (n = 9,408)1.
For the most part, adolescents who consented to the linkage between the youth@hordaland-survey and the NPR and which therefore constituted the final study sample (n = 9,408), were similar to those that did not consent (n = 845) (Table 1). However, the individuals that refused consent had somewhat higher frequencies of high-level alcohol consumption (8.5 versus 5.9%, d = 0.11, p < 0.01), higher mean symptom levels of self-reported conduct problems (0.68 versus 0.54, d = 0.11, p < 0.01), and were somewhat older (17.6 versus 17.4, p < 0.001).
In the study sample (n = 9,408), 9.1% (n = 853) of the adolescents had received services from Norwegian specialist health care during the past 4 years (2008 to 2011). As outlined in Table 2, adolescents who had received specialist mental health care services were more often female (58.5 versus 52.3%, p = 0.001) and of low SES (d = 0.17, p < 0.001). In addition, adolescents who had received specialist mental health care services had higher frequencies of most alcohol/drug use and problems (d’s ranging from 0.09 to 0.29, all p < 0.05) compared with adolescents that had not received specialist mental health care services. The only exception was on the measure for having ever used alcohol, which was non-significant (p = 0.571).
Frequencies of comorbidity with other psychiatric diagnoses were examined for each of the included psychiatric diagnoses. Among adolescents who had received a psychiatric diagnosis from a specialist mental health care clinic (n = 524), a total of 133 (25.4%) had at least one comorbid psychiatric diagnosis from another diagnostic category (data not shown). Specifically, the prevalence of psychiatric comorbidity were 59.1% (n = 78) for anxiety, 62.2% (n = 107) for depression, 62.5% (n = 20) for conduct disorders, 42.9% (n = 66) for ADHD, 60.1% (n = 28) for autism, 52.5% (n = 21) for eating disorders, 28.8% (n = 19) for trauma-related disorders, 70.0% (n = 7) for psychotic disorders, and 11.8% (n = 39) for “other psychiatric diagnoses.” Table 3 presents the correlation coefficients between the psychiatric diagnoses. Anxiety and depression had the strongest correlation (rs = 0.246, p < 0.001), while all other correlations were either non-significant or had a very small magnitude, spanning from rs = 0.069 to rs = 0.108.
In unadjusted models (Table 4), anxiety was associated with illicit drug use (odds ratio [OR] = 1.97, p < 0.01); depression was associated with frequent alcohol intoxication (OR = 1.58, p < 0.001), a positive CRAFFT score (OR = 2.04, p < 0.001) and illicit drug use (OR = 2.54, p < 0.01); conduct disorders were associated with a positive CRAFFT score (OR = 2.48, p < 0.05) and illicit drug use (OR = 4.63, p < 0.001); ADHD was associated with illicit drug use (OR = 1.81, p < 0.01); eating disorders were associated with frequent alcohol intoxication (OR = 2.08, p < 0.05) and a positive CRAFFT score (OR = 2.00, p < 0.05); trauma-related disorders were associated with all alcohol/drug measures (ORs ranging from 1.88 to 4.60, all p < 0.05). Additionally, autism was negatively associated with frequent alcohol intoxication (OR = 0.30, p < 0.05).
After adjustment for psychiatric comorbidity, anxiety was only negatively associated with frequent alcohol intoxication (adjusted odds ratio [AOR] = 0.48, p < 0.01). Depression was still significantly associated with frequent alcohol intoxication, a positive CRAFFT score and illicit drug use (AORs ranging from 1.74 to 2.14, all p < 0.05). Conduct disorders were positively associated with a positive CRAFFT score (AOR = 2.19, p < 0.05) and illicit drug use (AOR = 3.54, p < 0.01). ADHD and eating disorders were no longer associated with any substance use or problems. Autism was still negatively associated with frequent alcohol intoxication (AOR = 0.25, p < 0.05). Trauma-related disorders were positively associated with all measures of substance use/problems (AORs ranging from 1.76 to 4.35, all p < 0.05).
In fully adjusted models, adjusting for the potential confounding effects of psychiatric comorbidity, SES, sex and age, neither anxiety nor ADHD were significantly associated with any measures of alcohol/drug use and problems. Depression was associated only with a positive CRAFFT score (AOR = 2.10, p < 0.01); conduct disorders were associated only with illicit drug use (AOR = 6.90, p < 0.01); eating disorders were associated only with frequent alcohol intoxication (AOR = 2.29, p < 0.05); and trauma-related disorders were associated with high-level alcohol consumption, frequent alcohol intoxication and a positive CRAFFT-score (AORs ranging from 2.15 to 4.77, all p < 0.05). In addition, autism was negatively associated with frequent alcohol intoxication (AOR = 0.28, p < 0.05).
Using likelihood-ratio tests of proportionality of odds across response categories, we found only non-significant differences between all the psychiatric diagnoses listed in Table 5 and each ordinal level of indicators for risky substance use in the crude models (p-values ranging from 0.27 to 0.93), indicating that the proportional odds assumption underlying the ordered logistic regression models were met (Liao, 1994, p. 41). Autism diagnoses were excluded from this analysis as the proportional odds assumption was not met for this diagnosis.
In unadjusted models employing ordered logistic regression analyses, we found positive associations with the total degree of risky substance use and depression (OR = 1.89, p < 0.001), conduct disorders (OR = 3.15, p < 0.01), and trauma-related disorders (OR = 2.78, p < 0.001). Depression, conduct disorders and trauma-related disorders remained positively associated with the total degree of risky substance use after adjustment for psychiatric comorbidity (AORs ranging from 1.93 to 2.86, p < 0.01). Even in fully adjusted models, accounting for the confounding effects of psychiatric comorbidity, SES, sex and age, we found positive associations with the total degree of risky substance use for trauma-related disorders (AOR = 2.53, p < 0.01), depression (AOR = 1.61, p < 0.05), and conduct disorders (AOR = 2.79, p < 0.05).
The present study is to our knowledge the first to compare a broad range of psychiatric diagnoses and their associations with alcohol/drug use and problems during adolescence, while also addressing the role of psychiatric comorbidity. Frequencies of alcohol/drug use and problems were higher among adolescents who had received specialist mental health care services compared to adolescents who had not received such services during the past 4 years; however, the magnitude of these differences was small overall. Importantly, adolescents receiving treatment for a psychiatric disorder differed from controls on all measures of substance use and problems except any alcohol use. This finding may suggest that experimenting with alcohol is normative in adolescence but that excessive use of alcohol, use of other substances, and substance-related negative consequences are occurring at higher rates in those receiving services for psychiatric disorders. Furthermore, the investigated psychiatric diagnoses varied widely in the extent to which they were associated with alcohol/drug use and problems, particularly when the influence of other comorbid psychiatric diagnoses and demographic variables was accounted for.
In unadjusted models, depression was among the psychiatric diagnoses with the most consistent positive associations with alcohol/drug use and problems. Specifically, we found positive associations between depression and all single measures of alcohol/drug use and problems except high-level alcohol consumption. These associations remained significant after adjustment for psychiatric comorbidity. However, the only independent association between depression and alcohol/drug use and problems, after the additional adjustment for sociodemographic factors, was in relation to a positive CRAFFT-score. These findings lend some support to previous studies that have reported positive associations between depression and self-reported adolescent alcohol-related problems (Harrell et al., 2009) and general alcohol/drug use (Crum et al., 2008; Maslowsky and Schulenberg, 2013). Our study adds to previous findings that report positive associations between depression and alcohol intoxication (Crum et al., 2008; Pedersen, 2013), as our findings suggest that the association between depression and frequent alcohol intoxication was significant in the unadjusted model and after the adjustment of psychiatric comorbidity. However, this association was non-significant after the additional adjustment of sociodemographic factors. Moreover, depression was associated with the total degree of risky substance use, and this association was independent from psychiatric comorbidity and sociodemographic factors. In sum, these findings suggest that depression is a robust indicator for the total degree of risky substance use among adolescents.
We found that anxiety was positively associated with illicit drug use in unadjusted models. However, this association were non-significant after adjustment for psychiatric comorbidity. This finding suggests that no unique association between anxiety and illicit drug use was present in our data. Interestingly, anxiety was negative associated with frequent alcohol intoxication after adjustment for psychiatric comorbidity, but this association was no longer significant after the additional adjustment for sociodemographic variables. In sum, the present study lends little support to an independent association between anxiety and alcohol/drug use or problems among adolescents, and adjustment of psychiatric comorbidity tended to reduce the positive direction of the associations between anxiety and alcohol/drug use and problems, while the additional adjustment of sociodemographic variables did not affect the estimates in a consistent direction. Importantly, the previous literature is characterized by highly inconsistent findings, pointing to both negative (Schmits et al., 2015, 2016; Nelemans et al., 2016; Savage et al., 2016) and positive associations between anxiety and adolescent alcohol/drug use (Pardee et al., 2014; Birrell et al., 2015; Stapinski et al., 2016). Some studies have suggested that different anxiety disorders (Wu et al., 2010; Ohannessian, 2014) and different anxiety typologies within a given disorder (Tomlinson et al., 2013) yield different prediction of alcohol/drug use and problems, and anxiety may also have a role on adolescent alcohol/drug use and problems through interactions with other diagnoses (Lansford et al., 2008). Future studies should expand the scope to also distinguish between subtypes of anxiety disorders (e.g., social anxiety and generalized anxiety) and their independent associations with alcohol/drug use and problems during adolescence. Also of note, future studies could expand with measures of substance use/problems related to drugs with anxiolytic effects (e.g., alcohol and benzodiazepines), as our study did not include measures of alcohol-problems in particular (as CRAFFT is related to potential alcohol and/or drug-related problems) or benzodiazepine use/problems.
In the present study, autism was negatively associated with frequent alcohol intoxication after the adjustment of both psychiatric comorbidity and sociodemographic variables. In addition, all other single measures of alcohol/drug use and problems tended to go in a negative direction; however, these associations were non-significant. A limited number of previous studies have to our knowledge explored associations between autism and alcohol/drug use and problems among adolescents (Ramos et al., 2013; Mangerud et al., 2014), suggesting a low alcohol/drug use in this group. The present study support these findings by indicating that adolescents with autism had significantly lower odds for frequent alcohol intoxication compared with the general adolescent population. A possible explanation for this finding is that the social skills deficits of autistic adolescents may keep them out of the social situations and/or peer relations typically associated with alcohol consumption in adolescence (Santosh and Mijovic, 2006). However, autism may be associated with alcohol/drug use and problems beyond the adolescent years (Butwicka et al., 2017).
Our findings suggest that eating disorders were positively associated with frequent alcohol intoxication and a positive CRAFFT-score in unadjusted analyses. However, eating disorders were no longer significantly associated with any alcohol/drug use and problems measures after the adjustment for psychiatric comorbidity, while eating disorders were positively associated with frequent alcohol intoxication after the additional adjustment for demographic variables. This finding supports previous studies linking eating disorders with specific patterns of alcohol use characterized by a loss of control, such as frequent intoxication (Mustelin et al., 2016) and binge drinking (Khaylis et al., 2009). Previous studies indicate that elevated alcohol/drug use and problems are more likely amongst those with bulimia nervosa and binge eating disorders relative to those with anorexia nervosa (e.g., Gadalla and Piran, 2007). The present study did not, however, distinguish between different subtypes of eating disorders, something that should be considered in future research.
Previous studies have linked both childhood ADHD symptoms (Lee et al., 2011; Heradstveit et al., 2018) and ADHD symptoms during adolescence (August et al., 2006) with adolescent alcohol/drug use and problems. However, several researchers have highlighted that most studies have not controlled for associated psychopathology (August et al., 2006; Lee et al., 2011; Bidwell et al., 2014), therefore leaving doubt on the independence of this association. Our findings were that ADHD was associated with illicit drug use alone; however, this association was non-significant after the adjustment of psychiatric comorbidity as well as after the additional adjustment of sociodemographic variables. These findings suggest that no unique association between ADHD and alcohol/drug use and problems were present in our data, lending support to a study by August et al. (2006). They demonstrated that adolescent ADHD was positively associated with illicit drug use only for individuals with a comorbid externalizing disorder, primarily oppositional defiant disorder. A recent literature review similarly indicated that ADHD does not increase the risk of illicit drug use beyond the effect of conduct-related disorders (Serra-Pinheiro et al., 2013). In sum, our results suggest that ADHD was not independently associated with alcohol/drug use and problems among adolescents, and that comorbid psychiatric disorders may be important confounders in association between ADHD and illicit drug use. However, future studies are encouraged to test whether certain features of ADHD (e.g., impulsivity) might show more unique relations to alcohol/drug use and problems.
A range of previous studies have pointed to positive associations between externalizing problems and alcohol/drug use and problems (e.g., Heron et al., 2013; Hopfer et al., 2013; Cerda et al., 2016; Heradstveit et al., 2018; Pedersen et al., 2018), while studies exploring the independence of these associations with respect to comorbidity are more limited. In the present study, we found that conduct disorders were associated with illicit drug use, a positive CRAFFT score, and the total degree of risky substance use in unadjusted models, while we also found independent associations between conduct problems and illicit drug use and the total degree of risky substance use. Hence, conduct disorders appeared to be an important indicator for alcohol/drug use and problems in this study. Also of note, conduct disorders were the only specific psychiatric diagnosis that had an independent association with illicit drug use, highlighting the importance of this diagnosis in relation to illicit drug use among adolescents. This finding lends support to the deviancy proneness model that highlights deviant behaviors as an important risk factor for illicit drug use among adolescents (Tarter et al., 2006).
In unadjusted models, trauma-related disorders were positively associated with all single measures of alcohol/drug use and problems, while they were positively associated with all single measures except illicit drug use after the combined adjustment for psychiatric comorbidity and sociodemographic variables. This latter finding suggest that psychiatric comorbidity and sociodemographic variables should be taken into account as potential confounders in the associations between trauma-related disorders and illicit drug use. Additionally, trauma-related disorders were independently associated with the total degree of risky substance use. This finding supports previous studies that report positive associations between trauma-related disorders and alcohol/drug use and problems among adolescents (Giaconia et al., 2000; Haller and Chassin, 2014). The mechanisms behind associations between trauma-related problems and alcohol/drug-related problems are complex. A longitudinal, community-based study by Haller and Chassin (2014) found that PTSD symptoms increased the risk for later alcohol/drug-related problems among adolescents, and the authors argued that these results supported a self-medication hypothesis. However, other mechanisms may potentially be at work. For example, early alcohol/drug-related problems often involves chaotic and violent lifestyles, which could possibly increase the risk for trauma exposure (Deykin and Buka, 1997).
The study described here has several strengths. First, the sample consists of a well-defined population-based sample of adolescents aged 16 to 19 years, and was sufficiently large to enable a detailed investigation of the associations of interest. Second, a unique linkage with official registry data on specialist mental health care services was utilized, facilitating an investigation of formal psychiatric diagnoses independently determined according to the ICD-10 by professional mental health practitioners. However, the diagnoses are based on clinical judgment and no inter-rater reliability between the raters exists. Third, we investigated alcohol/drug use and problems across a broad range of diagnostic groups, which is rare in previous research (Mangerud et al., 2014), and enabled us to evaluate the independence of associations with alcohol/drug use and problems across several psychiatric diagnoses. Finally, due to the relatively large sample and comprehensive information about psychiatric diagnoses, we were able to adjust our analyses for psychiatric comorbidity, SES, sex, and age.
Some limitations require consideration when drawing inferences from this study. First, although the measures of psychiatric diagnoses preceded those of alcohol/drug use and problems, the study does not have a stringent longitudinal design, and it is not possible to draw conclusions on the causality between psychiatric diagnoses and alcohol/drug use and problems in this study, since some substance use may have predated the mental health care contacts. Second, the response rate in the population-based sample was 53% and included a relatively low proportion of adolescents with self-reported low SES, who in previous studies are found to have higher levels of mental health problems (e.g., Bøe et al., 2012). Official Norwegian statistics indicate that in 2012, 92% of all adolescents in Norway aged 16 to 18 years of age attended high school, compared with 98% in the youth@hordaland-sample (Hysing et al., 2015). The sample may therefore not have been fully representative of adolescents with psychiatric diagnoses due to selective participation. However, a previous publication from the Bergen Child Study indicated that although non-participation in the survey affected the estimated frequency of mental health problems, it did not affect patterns of associations between sociodemographic characteristics and mental health problems (Heiervang and Goodman, 2011). Nevertheless, our findings on associations between the broad range of psychiatric diagnoses and alcohol/drug use and problems require replication within more comprehensively ascertained clinical samples. Third, we did not differentiate between subtypes of psychiatric diagnoses. Fourth, psychiatric comorbidity was significantly higher within some of the diagnostic categories, particularly anxiety, depression, and conduct disorders. We may therefore have underestimated the independent associations between these psychiatric diagnoses and alcohol/drug use and problems. Fifth, alcohol/drug use and problems were measured by self-report, and does not imply the presence of diagnosable SUDs. In addition, the summed variable of the total degree of risky substance use included both substance use (illicit drug use, high-level alcohol consumption, frequent alcohol intoxication) and substance problems (a positive CRAFFT score). The use of a compound measure can be considered as a limitation, as it is difficult to differentiate between substance use and substance problems. Moreover, this summed variable did not specifically include prescription drug misuse as well as tobacco use. The results may therefore not be generalized to all types of drug use. Sixth, although adolescents that did not consent to the linkage between the youth@hordaland-survey and the NPR were overall similar to those that consented to this linkage, they reported somewhat higher frequency of high-level alcohol consumption, self-reported conduct problems, and higher age. Hence, this limitation may affect the generalizability of our findings. Seventh, the present study included many sets of analyses of associations. Multiple testing might therefore be an issue to consider when interpreting the results. Finally, an important limitation related to the generalizability of the findings from the present study is that individuals with untreated mental health problems in the general youth@hordaland-population were not identified. Psychiatric diagnoses in the present study was restricted to individuals that had received specialist mental health care services during the past 4 years. However, some adolescents in the general population may be suffering from undetected and/or untreated psychiatric disorders, or may have received treatment for psychiatric disorders elsewhere other than through specialist mental health care services (e.g., in private practice or through community-based psychologist services). A range of factors may potentially affect specialist mental health care use, such as functional impairment levels (Hintzpeter et al., 2015) and sociodemographic characteristics (Zwaanswijk et al., 2003). Also, a former wave of the Bergen Child Study concluded that specialist mental health care use differed considerably across psychiatric diagnoses, in which children with emotional disorders were underrepresented in mental health care services (Heiervang et al., 2007). Therefore, our findings on associations between psychiatric diagnoses and alcohol/drug use and problems should be interpreted with caution, particularly in relation to anxiety and depression disorders.
Alcohol/drug use and problems were slightly more common among adolescents who received specialist mental health care during the past 4 years compared with the general adolescent population. All investigated psychiatric diagnoses – except autism – were associated with some measure of hazardous alcohol/drug use and problems, and adolescents with trauma-related disorders, depression, and conduct disorders had particularly high odds for alcohol/drug use and problems.
The Regional Committee for Medical and Health Research Ethics (REC) in Western Norway approved the study. In accordance with the regulations from the REC and Norwegian health authorities, adolescents aged 16 years and older can make decisions regarding their own health (including participation in research), and thus gave consent themselves to participate in the current study. Parents/guardians have the right to be informed, and in the current study, all parents/guardians received written information about the study in advance.
OH has carried out the literature review for the introduction and the discussion section, conducted the statistical analyses, and has written the manuscript. OH, MH, and JS have been involved in the preparation and conduct of the statistical analyses, while all authors (OH, MH, JS, JH, and RS) have reviewed the project and participated in manuscript writing.
This work was supported by the Health Ministry of Western Norway, Fund for Strategic Research on Alcohol and Drug Use (Grant No. 912002). RS was partly funded by the National Institute for Health Research (NIHR) Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Addington, J., and Addington, D. (2007). Patterns, predictors and impact of substance use in early psychosis: a longitudinal study. Acta Psychiatr. Scand. 115, 304–309. doi: 10.1111/j.1600-0447.2006.00900.x
Armstrong, T. D., and Costello, E. J. (2002). Community studies on adolescent substance use, abuse, or dependence and psychiatric comorbidity. J. Consult. Clin. Psychol. 70, 1224–1239. doi: 10.1037//0022-006x.70.6.1224
August, G. J., Winters, K. C., Realmuto, G. M., Fahnhorst, T., Botzet, A., and Lee, S. (2006). Prospective study of adolescent drug use among community samples of ADHD and non-ADHD participants. J. Am. Acad. Child Adolesc. Psychiatry 45, 824–832. doi: 10.1097/01.chi.0000219831.16226.f8
Barkmann, C., and Schulte-Markwort, M. (2012). Prevalence of emotional and behavioural disorders in German children and adolescents: a meta-analysis. J. Epidemiol. Commun. Health 66, 194–203. doi: 10.1136/jech.2009.102467
Belfer, M. L. (2008). Child and adolescent mental disorders: the magnitude of the problem across the globe. J. Child Psychol. Psychiatry 49, 226–236. doi: 10.1111/j.1469-7610.2007.01855.x
Bidwell, L. C., Henry, E. A., Willcutt, E. G., Kinnear, M. K., and Ito, T. A. (2014). Childhood and current ADHD symptom dimensions are associated with more severe cannabis outcomes in college students. Drug Alcohol Depend. 135, 88–94. doi: 10.1016/j.drugalcdep.2013.11.013
Birmaher, B., Brent, D. A., Chiappetta, L., Bridge, J., Monga, S., and Baugher, M. (1999). Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J. Am. Acad. Child Adolesc. Psychiatry 38, 1230–1236. doi: 10.1097/00004583-199910000-00011
Birrell, L., Newton, N. C., Teesson, M., Tonks, Z., and Slade, T. (2015). Anxiety disorders and first alcohol use in the general population. Findings from a nationally representative sample. J. Anxiety Disord. 31, 108–113. doi: 10.1016/j.janxdis.2015.02.008
Bisetto, P. D., Botella, G. Á., and Sancho, M. A. (2011). Eating disorders and drug use in adolescents. Adicciones 24, 9–16.
Bøe, T., Øverland, S., Lundervold, A. J., and Hysing, M. (2012). Socioeconomic status and children’s mental health: results from the bergen child study. Soc. Psychiatry Psychiatr. Epidemiol. 47, 1557–1566. doi: 10.1007/s00127-011-0462-9
Boys, A., Farrell, M., Taylor, C., Marsden, J., Goodman, R., Brugha, T., et al. (2003). Psychiatric morbidity and substance use in young people aged 13–15 years: results from the child and adolescent survey of mental health. Br. J. Psychiatry 182, 509–517. doi: 10.1192/bjp.182.6.509
Butwicka, A., Långström, N., Larsson, H., Lundström, S., Serlachius, E., Almqvist, C., et al. (2017). Increased risk for substance use-related problems in autism spectrum disorders: a population-based cohort study. J. Autism Dev. Disord. 47, 80–89. doi: 10.1007/s10803-016-2914-2
Canino, G., Shrout, P. E., Rubio-Stipec, M., Bird, H. R., Bravo, M., Ramirez, R., et al. (2004). The DSM-IV rates of child and adolescent disordersin puerto rico: prevalence, correlates, service use, and the effects of impairment. Arch. Gen. Psychiatry 61, 85–93.
Castro-Fornieles, J., Díaz, R., Goti, J., Calvo, R., Gonzalez, L., Serrano, L., et al. (2009). Prevalence and factors related to substance use among adolescents with eating disorders. Eur. Addic. Res. 16, 61–68. doi: 10.1159/000268106
Cerda, M., Prins, S. J., Galea, S., Howe, C. J., and Pardini, D. (2016). When psychopathology matters most: identifying sensitive periods when within-person changes in conduct, affective and anxiety problems are associated with male adolescent substance use. Addiction 111, 924–935. doi: 10.1111/add.13304
Costello, E. J., Mustillo, S., Erkanli, A., Keeler, G., and Angold, A. (2003). Prevalence and development of psychiatric disorders in childhood and adolescence. Arch. Gen. Psychiatry 60, 837–844.
Crum, R. M., Green, K. M., Storr, C. L., Chan, Y.-F., Ialongo, N., Stuart, E. A., et al. (2008). Depressed mood in childhood and subsequent alcohol use through adolescence and young adulthood. Arch. Gen. Psychiatry 65, 702–712. doi: 10.1001/archpsyc.65.6.702
Deas-Nesmith, D., Campbell, S., and Brady, K. T. (1998). Substance use disorders in an adolescent inpatient psychiatric population. J. Natl. Med. Assoc. 90, 233–238.
Deykin, E. Y., and Buka, S. L. (1997). Prevalence and risk factors for posttraumatic stress disorder among chemically dependent adolescents. Am. J. Psychiatry 154, 752–757. doi: 10.1176/ajp.154.6.752
Dhalla, S., Zumbo, B., and Poole, G. (2011). A review of the psychometric properties of the CRAFFT instrument: 1999-2010. Curr. Drug Abuse Rev. 4, 57–64. doi: 10.2174/1874473711104010057
Edlund, M. J., Forman-Hoffman, V. L., Winder, C. R., Heller, D. C., Kroutil, L. A., Lipari, R. N., et al. (2015). Opioid abuse and depression in adolescents: results from the national survey on drug use and health. Drug Alcohol Depend. 152, 131–138. doi: 10.1016/j.drugalcdep.2015.04.010
Ferdinand, R. F., Sondeijker, F., Van Der Ende, J., Selten, J. P., Huizink, A., and Verhulst, F. C. (2005). Cannabis use predicts future psychotic symptoms, and vice versa. Addiction 100, 612–618. doi: 10.1111/j.1360-0443.2005.01070.x
Gadalla, T., and Piran, N. (2007). Co-occurrence of eating disorders and alcohol use disorders in women: a meta analysis. Arch. Womens Ment. Health 10, 133–140. doi: 10.1007/s00737-007-0184-x
Giaconia, R. M., Reinherz, H. Z., Hauf, A. C., Paradis, A. D., Wasserman, M. S., and Langhammer, D. M. (2000). Comorbidity of substance use and post-traumatic stress disorders in a community sample of adolescents. Am. J. Orthopsychiatry 70, 253–262. doi: 10.1037/h0087634
Groenman, A. P., Oosterlaan, J., Rommelse, N., Franke, B., Roeyers, H., Oades, R. D., et al. (2013). Substance use disorders in adolescents with attention deficit hyperactivity disorder: a 4-year follow-up study. Addiction 108, 1503–1511. doi: 10.1111/add.12188
Haller, M., and Chassin, L. (2014). Risk pathways among traumatic stress, posttraumatic stress disorder symptoms, and alcohol and drug problems: a test of four hypotheses. Psychol. Addic. Behav. 28, 841–851. doi: 10.1037/a0035878
Harrell, Z. A., Slane, J. D., and Klump, K. L. (2009). Predictors of alcohol problems in college women: the role of depressive symptoms, disordered eating, and family history of alcoholism. Addic. Behav. 34, 252–257. doi: 10.1016/j.addbeh.2008.10.019
Heiervang, E., and Goodman, R. (2011). Advantages and limitations of web-based surveys: evidence from a child mental health survey. Soc. Psychiatry Psychiatr. Epidemiol. 46, 69–76. doi: 10.1007/s00127-009-0171-9
Heiervang, E., Stormark, K. M., Lundervold, A. J., Heimann, M., Goodman, R., Posserud, M.-B., et al. (2007). Psychiatric disorders in Norwegian 8-to 10-year-olds: an epidemiological survey of prevalence, risk factors, and service use. J. Am. Acad. Child Adolesc. Psychiatry 46, 438–447.
Heradstveit, O., Skogen, J. C., Bøe, T., Hetland, J., Pedersen, M. U., and Hysing, M. (2018). Prospective associations between childhood externalising and internalising problems and adolescent alcohol and drug use: the bergen child study. Nord. Stud. Alcohol Drugs 35, 357–371. doi: 10.1177/1455072518789852
Heradstveit, O., Skogen, J. C., Hetland, J., and Hysing, M. (2017). Alcohol and illicit drug use are important factors for school-related problems among adolescents. Front. Psychol. 8:1023. doi: 10.3389/fpsyg.2017.01023
Heron, J., Barker, E. D., Joinson, C., Lewis, G., Hickman, M., Munafò, M., et al. (2013). Childhood conduct disorder trajectories, prior risk factors and cannabis use at age 16: birth cohort study. Addiction 108, 2129–2138. doi: 10.1111/add.12268
Hintzpeter, B., Klasen, F., Schön, G., Voss, C., Hölling, H., Ravens-Sieberer, U., et al. (2015). Mental health care use among children and adolescents in Germany: results of the longitudinal BELLA study. Eur. Child Adolesc. Psychiatry 24, 705–713. doi: 10.1007/s00787-015-0676-6
Hopfer, C., Salomonsen-Sautel, S., Mikulich-Gilbertson, S., Min, S. J., McQueen, M., Crowley, T., et al. (2013). Conduct disorder and initiation of substance use: a prospective longitudinal study. J. Am. Acad. Child Adolesc. Psychiatry 52, 511–518.
Hysing, M., Pallesen, S., Stormark, K. M., Jakobsen, R., Lundervold, A. J., and Sivertsen, B. (2015). Sleep and use of electronic devices in adolescence: results from a large population-based study. BMJ Open 5:e006748. doi: 10.1136/bmjopen-2014-006748
Kedzior, K. K., and Laeber, L. T. (2014). A positive association between anxiety disorders and cannabis use or cannabis use disorders in the general population: a meta-analysis of 31 studies. BMC Psychiatry 14:136. doi: 10.1186/1471-244X-14-136
Kessler, R. C., Adler, L. A., Gruber, M. J., Sarawate, C. A., Spencer, T., and Van Brunt, D. L. (2007). Validity of the world health organization adult ADHD self-report scale (ASRS) screener in a representative sample of health plan members. Int. J. Methods Psychiatr. Res. 16, 52–65. doi: 10.1002/mpr.208
Khaylis, A., Trockel, M., and Taylor, C. B. (2009). Binge drinking in women at risk for developing eating disorders. Int. J. Eat. Disord. 42, 409–414. doi: 10.1002/eat.20644
Khoddam, R., Jackson, N. J., and Leventhal, A. M. (2016). Internalizing symptoms and conduct problems: redundant, incremental, or interactive risk factors for adolescent substance use during the first year of high school? Drug Alcohol Depend. 169, 48–55. doi: 10.1016/j.drugalcdep.2016.10.007
Knight, J. R., Sherritt, L., Shrier, L. A., Harris, S. K., and Chang, G. (2002). Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch. Pediatr. Adolesc. Med. 156, 607–614.
Lansford, J. E., Erath, S., Yu, T., Pettit, G. S., Dodge, K. A., and Bates, J. E. (2008). The developmental course of illicit substance use from age 12 to 22: links with depressive, anxiety, and behavior disorders at age 18. J. Child Psychol. Psychiatry 49, 877–885. doi: 10.1111/j.1469-7610.2008.01915.x
Lee, S. S., Humphreys, K. L., Flory, K., Liu, R., and Glass, K. (2011). Prospective association of childhood attention-deficit/hyperactivity disorder (ADHD) and substance use and abuse/dependence: a meta-analytic review. Clin. Psychol. Rev. 31, 328–341. doi: 10.1016/j.cpr.2011.01.006
Liao, T. F. (1994). Interpreting Probability Models: Logit, Probit, and Other Generalized Linear Models. Thousand Oaks, CA: Sage.
Lucas, C. P., Zhang, H., Fisher, P. W., Shaffer, D., Regier, D. A., Narrow, W. E., et al. (2001). The DISC predictive scales (DPS): efficiently screening for diagnoses. J. Am. Acad. Child Adolesc. Psychiatry 40, 443–449. doi: 10.1097/00004583-200104000-00013
Mangerud, W. L., Bjerkeset, O., Holmen, T. L., Lydersen, S., and Indredavik, M. S. (2014). Smoking, alcohol consumption, and drug use among adolescents with psychiatric disorders compared with a population based sample. J. Adolesc. 37, 1189–1199. doi: 10.1016/j.adolescence.2014.08.007
Maslowsky, J., and Schulenberg, J. E. (2013). Interaction matters: quantifying conduct problem x depressive symptoms interaction and its association with adolescent alcohol, cigarette, and marijuana use in a national sample. Dev. Psychopathol. 25, 1029–1043. doi: 10.1017/S0954579413000357
McDonald, R. P. (2013). Test Theory: A Unified Treatment: Psychology Press. New York, NY: Routledge.
Merikangas, K. R., He, J. P., Burstein, M., Swanson, S. A., Avenevoli, S., Cui, L., et al. (2010). Lifetime prevalence of mental disorders in US adolescents: results from the national comorbidity survey replication–adolescent supplement (NCS-A). J. Am. Acad. Child Adolesc. Psychiatry 49, 980–989. doi: 10.1016/j.jaac.2010.05.017
Mustelin, L., Latvala, A., Raevuori, A., Rose, R. J., Kaprio, J., and Keski-Rahkonen, A. (2016). Risky drinking behaviors among women with eating disorders: a longitudinal community-based study. Int. J. Eat. Disord. 49, 563–571. doi: 10.1002/eat.22526
Nelemans, S. A., Hale, W. W. III, Raaijmakers, Q. A. W., Branje, S. J. T., van Lier, P. A. C., and Meeus, W. H. J. (2016). Longitudinal associations between social anxiety symptoms and cannabis use throughout adolescence: the role of peer involvement. Eur. Child Adolesc. Psychiatry 25, 483–492. doi: 10.1007/s00787-015-0747-8
Ohannessian, C. M. (2014). Anxiety and substance use during adolescence. Subs. Abuse 35, 418–425. doi: 10.1080/08897077.2014.953663
Pardee, C. S., Colder, C. R., and Bowker, J. C. (2014). Dynamic associations among alcohol use and anxiety symptoms in early adolescence. Psychol. Addic. Behav. 28, 1246–1252. doi: 10.1037/a0038372
Pedersen, D. E. (2013). Gender differences in college binge drinking: examining the role of depression and school stress. Soc. Sci. J. 50, 521–529. doi: 10.1016/j.soscij.2013.03.003
Pedersen, M. U., Thomsen, K. R., Heradstveit, O., Skogen, J. C., Hesse, M., and Jones, S. (2018). Externalizing behavior problems are related to substance use in adolescents across six samples from Nordic countries. Eur. Child Adolesc. Psychiatry 27, 1551–1561. doi: 10.1007/s00787-018-1148-6
R Core Team (2018). R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing.
Ramos, M., Boada, L., Moreno, C., Llorente, C., Romo, J., and Parellada, M. (2013). Attitude and risk of substance use in adolescents diagnosed with asperger syndrome. Drug Alcohol Depend. 133, 535–540. doi: 10.1016/j.drugalcdep.2013.07.022
Regier, D. A., Farmer, M. E., Rae, D. S., Locke, B. Z., Keith, S. J., Judd, L. L., et al. (1990). Comorbidity of mental disorders with alcohol and other drug abuse: results from the epidemiologic catchment area (ECA) study. JAMA 264, 2511–2518. doi: 10.1001/jama.264.19.2511
Rohde, P., Lewinsohn, P. M., and Seeley, J. R. (1996). Psychiatric comorbidity with problematic alcohol use in high school students. J. Am. Acad. Child Adolesc. Psychiatry 35, 101–109. doi: 10.1097/00004583-199601000-00018
Santosh, P. J., and Mijovic, A. (2006). Does pervasive developmental disorder protect children and adolescents against drug and alcohol use? Eur. Child Adolesc. Psychiatry 15, 183–188. doi: 10.1007/s00787-005-0517-0
Savage, J. E., Kaprio, J., Korhonen, T., Pulkkinen, L., Rose, R. J., Verhulst, B., et al. (2016). The effects of social anxiety on alcohol and cigarette use across adolescence: results from a longitudinal twin study in Finland. Psychol. Addic. Behav. 30, 462–474. doi: 10.1037/adb0000183
Schmits, E., Mathys, C., and Quertemont, E. (2015). A longitudinal study of cannabis use initiation among high school students: effects of social anxiety, expectancies, peers and alcohol. J. Adolesc. 41, 43–52. doi: 10.1016/j.adolescence.2015.02.009
Schmits, E., Mathys, C., and Quertemont, E. (2016). Is social anxiety associated with cannabis use? The role of cannabis use effect expectancies in middle adolescence. J. Child Adolesc. Subs. Abuse 25, 348–359. doi: 10.1080/1067828x.2015.1039683
Schulte, M. T., Ramo, D., and Brown, S. A. (2009). Gender differences in factors influencing alcohol use and drinking progression among adolescents. Clin. Psychol. Rev. 29, 535–547. doi: 10.1016/j.cpr.2009.06.003
Serra-Pinheiro, M. A., Coutinho, E. S., Souza, I. S., Pinna, C., Fortes, D., Araújo, C., et al. (2013). Is ADHD a risk factor independent of conduct disorder for illicit substance use? A meta-analysis and metaregression investigation. J. Attent. Disord. 17, 459–469. doi: 10.1177/1087054711435362
Skogen, J. C., Bøe, T., Knudsen, A. K., and Hysing, M. (2013). Psychometric properties and concurrent validity of the CRAFFT among Norwegian adolescents. Ung@hordaland, a population-based study. Addict. Behav. 38, 2500–2505. doi: 10.1016/j.addbeh.2013.05.002
Skogen, J. C., Sivertsen, B., Lundervold, A. J., Stormark, K. M., Jakobsen, R., and Hysing, M. (2014). Alcohol and drug use among adolescents: and the co-occurrence of mental health problems. Ung@hordaland, a population-based study. BMJ Open 4:e005357. doi: 10.1136/bmjopen-2014-005357
Stapinski, L. A., Montgomery, A. A., and Araya, R. (2016). Anxiety, depression and risk of cannabis use: examining the internalising pathway to use among chilean adolescents. Drug Alcohol Depend. 166, 109–115. doi: 10.1016/j.drugalcdep.2016.06.032
Tarter, R. E., Vanyukov, M., Kirisci, L., Reynolds, M., and Clark, D. B. (2006). Predictors of marijuana use in adolescents before and after licit drug use: examination of the gateway hypothesis. Am. J. Psychiatry 163, 2134–2140. doi: 10.1176/ajp.2006.163.12.2134
Thapar, A., and McGuffin, P. (1998). Validity of the shortened mood and feelings questionnaire in a community sample of children and adolescents: a preliminary research note. Psychiatry Res. 81, 259–268. doi: 10.1016/s0165-1781(98)00073-0
Tomlinson, K. L., Cummins, K. M., and Brown, S. A. (2013). Social anxiety and onset of drinking in early adolescence. J. Child Adolesc. Subs. Abuse 22, 163–177. doi: 10.1080/1067828x.2012.747994
Van Oers, J., Bongers, I., Van de Goor, L., and Garretsen, H. (1999). Alcohol consumption, alcohol-related problems, problem drinking, and socioeconomic status. Alcohol Alcohol. 34, 78–88. doi: 10.1093/alcalc/34.1.78
Wolitzky-Taylor, K., Bobova, L., Zinbarg, R. E., Mineka, S., and Craske, M. G. (2012). Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict. Behav. 37, 982–985. doi: 10.1016/j.addbeh.2012.03.026
Wu, L.-T., Gersing, K., Burchett, B., Woody, G. E., and Blazer, D. G. (2011). Substance use disorders and comorbid Axis I and II psychiatric disorders among young psychiatric patients: findings from a large electronic health records database. J. Psychiatr. Res. 45, 1453–1462. doi: 10.1016/j.jpsychires.2011.06.012
Wu, P., Goodwin, R. D., Fuller, C., Liu, X., Comer, J. S., Cohen, P., et al. (2010). The relationship between anxiety disorders and substance use among adolescents in the community: specificity and gender differences. J. Youth Adolesc. 39, 177–188. doi: 10.1007/s10964-008-9385-5
Zulauf, C. A., Sprich, S. E., Safren, S. A., and Wilens, T. E. (2014). The complicated relationship between attention deficit/hyperactivity disorder and substance use disorders. Curr. Psychiatry Rep. 16, 1–11.
Zwaanswijk, M., Van Der Ende, J., Verhaak, P. F., Bensing, J. M., and Verhulst, F. C. (2003). Factors associated with adolescent mental health service need and utilization. J. Am. Acad. Child Adolesc. Psychiatry 42, 692–700. doi: 10.1097/01.chi.0000046862.56865.b7
Keywords: alcohol use, illicit drug use, alcohol/drug-related problems, mental health problems, psychiatric diagnoses, adolescence, registry-based data, population-based sample
Citation: Heradstveit O, Skogen JC, Hetland J, Stewart R and Hysing M (2019) Psychiatric Diagnoses Differ Considerably in Their Associations With Alcohol/Drug-Related Problems Among Adolescents. A Norwegian Population-Based Survey Linked With National Patient Registry Data. Front. Psychol. 10:1003. doi: 10.3389/fpsyg.2019.01003
Received: 16 October 2018; Accepted: 15 April 2019;
Published: 08 May 2019.
Edited by:
Danny Horesh, Bar-Ilan University, IsraelReviewed by:
Sherry Stewart, Dalhousie University, CanadaCopyright © 2019 Heradstveit, Skogen, Hetland, Stewart and Hysing. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ove Heradstveit, b3ZoZUBub3JjZXJlc2FyY2gubm8=
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.