- 1Department of Psychology, Catholic University of the Sacred Heart, Milan, Italy
- 2Istituto Auxologico Italiano IRCCS, Psychology Research Laboratory, Ospedale San Giuseppe, Verbania, Italy
- 3Faculty of Psychology, eCampus University, Novedrate, Italy
- 4Department of Psychology, Health and Technology, Centre for eHealth and Wellbeing Research, University of Twente, Enschede, Netherlands
Introduction
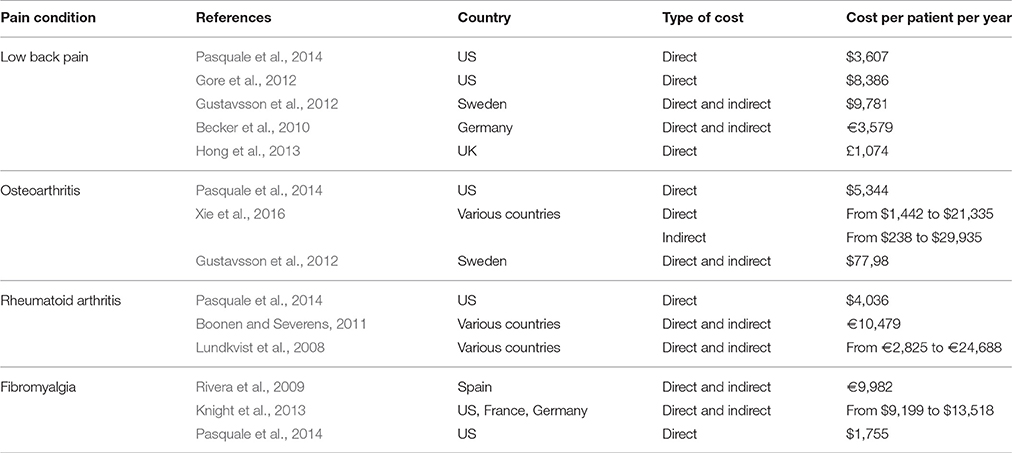
Chronic musculoskeletal pain is the leading sources of disability worldwide, imposing an enormous burden to both societies and healthcare systems (Vos et al., 2012). Direct medical expenses and indirect costs due to losses in work productivity exceed $200 billion in the US (Ma et al., 2014; Park et al., 2016) and are a major source of concern in Europe (Breivik et al., 2013). Mean per capita costs vary from country to country (see Table 1), but are estimated to double the expenses for the care of matched controls (Gore et al., 2012; Hong et al., 2013). Notably, their impact is directly linked both to the severity of the condition and to the presence of mental comorbidities, and can be inflated by concomitant opioid abuse (Baumeister et al., 2012; Manchikanti et al., 2013; Stockbridge et al., 2015; Rayner et al., 2016).
In the last decades, the biopsychosocial model has attempted to answer to the growing imperative need to identify the best practices for the prevention and treatment of chronic pain and related conditions. Scientific research shows that clinical psychology plays a key role within the multidisciplinary approach that is increasingly being suggested for pain management. Its added value is revealed not only by the improvement of the patient experience, but also with regards to economic savings and cost reduction of his care, which is an issue on which modern health services base their strategic decisions. These benefits have been corroborated by studies addressing psychological treatments for chronic musculoskeletal pain, which will be discussed later. However, we argue that the work of clinical psychologists can improve the economic sustainability of chronic pain management in all the stages of the care, from the assessment phase to the rehabilitation period, providing a differentiated contribution depending on the treatment course of the patient (i.e. conservative treatment, surgical intervention). In particular, we suggest that the cost-effectiveness of chronic pain management can be enhanced employing a psychometrically sound, computerized and integrated assessment. After the diagnostic process, psychological techniques and interventions can be useful for pain management or, in case of surgical interventions, to enhance their outcomes.
Economic Benefits of an Integrated Assessment of Pain and Treatment Outcomes and the Role of Modern Psychometric Methods
The multidimensional evaluation of pain and its correlates is crucial during the entire course of the care. Starting from the initial assessment phase, the aim of the pain specialist is to gather detailed information on pain characteristics and to ascertain how these characteristics are intertwined with biomedical, psychosocial and behavioral factors (Dansie and Turk, 2013; Aloisi et al., 2016; Castelnuovo et al., 2016a,b; Tamburin et al., 2016). An integrated assessment of these aspects may have an intrinsic positive clinical effect (Pietilä Holmner et al., 2013). In addition, accurate and objective measures are important for making correct decisions and to lead to a cost-effective management of the following pain management intervention. Standardized measures are fundamental for detecting the presence of contraindication for specific pain management options (Daubs et al., 2010). In this context, psychometrics may provide the tools for a reliable, sensitive and valid assessment of pain and of the outcomes of the treatment. Some authors advocate for the spread integrated and computerized assessment methods which exploit the potential of the most modern statistical models for the construction of valid, specific and user-friendly questionnaires which can be linked to automated dynamic pain assessment systems (Chang, 2013; El Miedany, 2013; Slover et al., 2015). Item Response Theory models can be used to calibrate these tools to assess the person's traits in a reliable and valid manner with the lowest possible amount of item, greatly reducing the administration time. These methods permit to evaluate the relevant aspects ofthe patient's experience and to easily store and access the acquired information throughout the different phases of the treatment and in the follow-up period. Models based on these principles have been specifically developed for musculoskeletal pain conditions with the aim to reduce costs and first proofs of their cost-effectiveness have been found (Wells et al., 2013; El Miedany et al., 2016).
Economic Utility of the Assessment of the Psychological Variables Associated with the Treatment Outcomes in the Surgical Management of Pain
Surgery can be an option to relieve pain in rheumatoid arthritis, osteoarthritis and back conditions (Boonen and Severens, 2011; Gore et al., 2012; Xie et al., 2016). A large number of psychological aspects related to pain, such as anxiety, depression, cognitions, expectations and personality traits can be considered as strong predictors of the outcomes of these interventions (Schade et al., 1999; Trief et al., 2000; DeBerard et al., 2003; Kohlboeck et al., 2004; den Boer et al., 2006; Abbott et al., 2011; Judge et al., 2012; Block et al., 2013; Akins et al., 2015; Anderson et al., 2015; Kunutsor et al., 2016; Alattas et al., 2017; Lindberg et al., 2017; Mancuso et al., 2017). Each of these factors seems to differently affect the various outcomes of the treatment, leading to a boost of the direct and indirect costs of the care. Omitting to consider the psychosocial aspects which can interfere with the surgical intervention may lead to a worst patient experience in terms of pain intensity and quality of life, to a failure to return to work, to an increase in opioid consumption or to repeat other ineffective, potentially harmful and costly treatments. In this contexts, the contribution of a psychologist can be essential. His role is not to decide whether an intervention should be implemented or discarded, but to help physicians to identify the patients at risk of poor outcomes and to suggest how the pain management strategies could be improved. Moreover, his work can be fundamental to prepare the patient for the surgical intervention, e.g., assessing unrealistic expectations or providing education, and to guide him in the post-operative period with the aim to foster his motivation, to facilitate his discharge, and to prevent the conditions which may cause a relapse of the symptoms and a readmission to the hospital (Childs et al., 2014; Louw et al., 2014).
The Economic Utility of Clinical Psychology for Pain Treatment
Several psychological treatment options have been proven to be cost-effective and are available for the clinical management of pain both in traditional and in new technology-based scenarios (Kröner-Herwig, 2009; Trompetter et al., 2014, 2015, 2016; Veehof et al., 2016). In a recent meta-analysis, Pike et al. (2016) found that psychological interventions are successful in reducing the use of healthcare services by the patients. This finding extends the evidence for a positive effect of psychological interventions on pain intensity, pain disability and the quality of life of the treated subjects (Hoffman et al., 2007; Williams et al., 2012; Veehof et al., 2016).
Comprehensive pain programs administered by multidisciplinary teams which include the contribution of a psychologist or which use psychological techniques are associated with a substantial reduction in both the direct and indirect costs of the disease, with a cost saving which is estimated between 8,500$ to 13,000$ per patient per year (Gatchel et al., 2003; Gatchel and Okifuji, 2006). All the components of these programs are fundamental for a cost-effective care of the disease and “carving out” some of them may impair a satisfying recovery to the premorbid productivity levels, leading to an increase in the future use of the healthcare resources (Gatchel and Okifuji, 2006; Gatchel and Mayer, 2008). Moreover, these programs may be enhanced providing intensive psychological therapies for the management of pain. The research is increasingly showing that these interventions are highly effective and lead to considerable cost savings. A group treatment for musculoskeletal pain sufferers based on cognitive behavioral principles resulted in additional 0.0325 Quality Adjusted Life Years (QALY) with respect of the control condition, with an incremental cost per QALY of £5,786 (Taylor et al., 2016). Various RCTs evaluated the cost-effectiveness of group cognitive behavioral approaches for chronic low back pain, with estimates of additional cost per QALY ranging from £1,786 to $7,197 (Linton and Nordin, 2006; Lamb et al., 2010; Norton et al., 2015). An integrated care program for sick-listed back pain patients based on a workplace intervention and graded activity was found to provide work-related economic savings in the amount of £5744 (Lambeek et al., 2010), but graded activity was found to be less cost-effective than exposure in vivo in another trial (Goossens et al., 2015). Non-significant effects were found for a CBT program added to inpatient rehabilitation for chronic low back pain (Schweikert et al., 2006). With regards to the other syndromes, a telephone-delivered CBT for chronic widespread pain sufferers provided a 0.097 additional QALY with respect to a program of tailored exercise, with an incremental cost per QALY of £5917 (Beasley et al., 2015), an internet-delivered Acceptance and Commitment Therapy program for fibromyalgia patients provided cost savings which exceeded the costs of the treatment 2 months after its conclusion (Ljotsson et al., 2014) and a psychoeducational intervention for the same syndrome resulted in 0.12 additional QALY with respect to control (Luciano et al., 2013). Although a systematic evaluation of the cost-effectiveness of all the available programs is beyond the scope of this article, it is established that the costs of various psychological treatments are rapidly overtaken by direct and indirect savings. However, clinical psychologists are not required to indiscriminately implement their therapies. On the contrary, their role is to help the pain management team to identify the characteristics of the patient and to tailor their techniques accordingly. The importance of tailoring the interventions has been long advocated in the literature and some evidence of the benefit of such an approach the have been provided (Turk, 1990; Turk et al., 1996, 1998). In addition, in the clinical practice, the psychologist and the multidisciplinary pain team usually face very complex conditions accompanied by physical or mental comorbidities, which may prevent the use of standardized treatments. The future of the clinical psychology and of the biopsychosocial approach in the field of pain management seems therefore to reside in the possibility to deliver integrated interventions which are personalized in order to be more effective and, at the same time, less expensive (Castelnuovo, 2010a,b; Castelnuovo et al., 2016c).
Author Contributions
All authors listed have made a substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abbott, A. D., Tyni-Lenné, R., and Hedlund, R. (2011). Leg pain and psychological variables predict outcome 2-3 years after lumbar fusion surgery. Eur. Spine J. 20, 1626–1634. doi: 10.1007/s00586-011-1709-6
Akins, P. T., Harris, J., Alvarez, J. L., Chen, Y., Paxton, E. W., Bernbeck, J., et al. (2015). Risk factors associated with 30-day readmissions after instrumented spine surgery in 14,939 patients: 30-day readmissions after instrumented spine surgery. Spine 40, 1022–1032. doi: 10.1097/BRS.0000000000000916
Alattas, S. A., Smith, T., Bhatti, M., Wilson-Nunn, D., and Donell, S. (2017). Greater pre-operative anxiety, pain and poorer function predict a worse outcome of a total knee arthroplasty. Knee Surg. Sports Traumatol. Arthrosc. 25, 3403–3410. doi: 10.1007/s00167-016-4314-8
Aloisi, A. M., Berlincioni, V., Torta, R., Nappi, R. E., Tassorelli, C., Barale, F., et al. (2016). The role of gender, psycho-social factors and anthropological-cultural dimensions on pain in neurorehabilitation. Evidence and recommendations from the Italian consensus conference on pain in Neurorehabilitation. Eur. J. Phys. Rehabil. Med. 52, 730–740.
Anderson, J. T., Haas, A. R., Percy, R., Woods, S. T., Ahn, U. M., and Ahn, N. U. (2015). Clinical depression is a strong predictor of poor lumbar fusion outcomes among workers' compensation subjects. Spine 40, 748–756. doi: 10.1097/BRS.0000000000000863
Baumeister, H., Knecht, A., and Hutter, N. (2012). Direct and indirect costs in persons with chronic back pain and comorbid mental disorders–a systematic review. J. Psychosom. Res. 73, 79–85. doi: 10.1016/j.jpsychores.2012.05.008
Beasley, M., Prescott, G. J., Scotland, G., McBeth, J., Lovell, K., Keeley, P., et al. (2015). Patient-reported improvements in health are maintained 2 years after completing a short course of cognitive behaviour therapy, exercise or both treatments for chronic widespread pain: long-term results from the MUSICIAN randomised controlled trial. RMD Open 1:e000026. doi: 10.1136/rmdopen-2014-000026
Becker, A., Held, H., Redaelli, M., Strauch, K., Chenot, J. F., Leonhardt, C., et al. (2010). Low back pain in primary care: costs of care and prediction of future health care utilization. Spine 35, 1714–1720. doi: 10.1097/BRS.0b013e3181cd656f
Block, A. R., Ben-Porath, Y. S., and Marek, R. J. (2013). Psychological risk factors for poor outcome of spine surgery and spinal cord stimulator implant: a review of the literature and their assessment with the MMPI-2-RF. Clin. Neuropsychol. 27, 81–107. doi: 10.1080/13854046.2012.721007
Boonen, A., and Severens, J. L. (2011). The burden of illness of rheumatoid arthritis. Clin. Rheumatol. 30(Suppl. 1), S3–S8. doi: 10.1007/s10067-010-1634-9
Breivik, H., Eisenberg, E., and O'Brien, T. (2013). The individual and societal burden of chronic pain in Europe: the case for strategic prioritisation and action to improve knowledge and availability of appropriate care. BMC Public Health 13:1229. doi: 10.1186/1471-2458-13-1229
Castelnuovo, G. (2010a). Empirically supported treatments in psychotherapy: towards an evidence-based or evidence-biased psychology in clinical settings? Front. Psychol. 1:27. doi: 10.3389/fpsyg.2010.00027
Castelnuovo, G. (2010b). No medicine without psychology: the key role of psychological contribution in clinical settings. Front. Psychol. 1:4. doi: 10.3389/fpsyg.2010.00004
Castelnuovo, G., Giusti, E. M., Manzoni, G. M., Saviola, D., Gatti, A., Gabrielli, S., et al. (2016a). Psychological considerations in the assessment and treatment of pain in Neurorehabilitation and psychological factors predictive of therapeutic response: evidence and recommendations from the Italian consensus conference on pain in Neurorehabilitation. Front. Psychol. 7:468. doi: 10.3389/fpsyg.2016.00468
Castelnuovo, G., Giusti, E. M., Manzoni, G. M., Saviola, D., Gatti, A., Gabrielli, S., et al. (2016b). Psychological treatments and psychotherapies in the Neurorehabilitation of pain: evidences and recommendations from the Italian consensus conference on pain in Neurorehabilitation. Front. Psychol. 7:115. doi: 10.3389/fpsyg.2016.00115
Castelnuovo, G., Pietrabissa, G., Cattivelli, R., Manzoni, G. M., and Molinari, E. (2016c). Not only clinical efficacy in psychological treatments: clinical psychology must promote cost-benefit, cost-effectiveness, and cost-utility analysis. Front. Psychol. 7:563. doi: 10.3389/fpsyg.2016.00563
Chang, C.-H. (2013). “Dynamic pain assessment: an application of clinical infometrics to personalized pain treatment and management,” in Handbook of Pain and Palliative Care, ed R. Moore (New York, NY: Springer), 121–130.
Childs, S. R., Casely, E. M., Kuehler, B. M., Ward, S., Halmshaw, C. L., Thomas, S. E., et al. (2014). The clinical psychologist and the management of inpatient pain: a small case series. Neuropsychiatr. Dis. Treat. 10, 2291–2297. doi: 10.2147/NDT.S70555
Dansie, E. J., and Turk, D. C. (2013). Assessment of patients with chronic pain. Br. J. Anaesth. 111, 19–25. doi: 10.1093/bja/aet124
Daubs, M. D., Patel, A. A., Willick, S. E., Kendall, R. W., Hansen, P., Petron, D. J., et al. (2010). Clinical impression versus standardized questionnaire: the spinal surgeon's ability to assess psychological distress. J. Bone Joint Surg. Am. 92, 2878–2883. doi: 10.2106/JBJS.I.01036
DeBerard, M. S., Masters, K. S., Colledge, A. L., and Holmes, E. B. (2003). Presurgical biopsychosocial variables predict medical and compensation costs of lumbar fusion in Utah workers' compensation patients. Spine J. 3, 420–429. doi: 10.1016/S1529-9430(03)00116-5
den Boer, J. J., Oostendorp, R. A., Beems, T., Munneke, M., and Evers, A. W. (2006). Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain 123, 45–52. doi: 10.1016/j.pain.2006.02.008
El Miedany, Y. (2013). PROMs in inflammatory arthritis: moving from static to dynamic. Clin. Rheumatol. 32, 735–742. doi: 10.1007/s10067-013-2228-0
El Miedany, Y., El Gaafary, M., Youssef, S., Bahlas, S., Almedany, S., Ahmed, I., et al. (2016). Toward electronic health recording: evaluation of electronic patient-reported outcome measures system for remote monitoring of early Rheumatoid Arthritis. J. Rheumatol. 43, 2106–2112. doi: 10.3899/jrheum.151421
Gatchel, R. J., and Mayer, T. G. (2008). Evidence-informed management of chronic low back pain with functional restoration. Spine J. 8, 65–69. doi: 10.1016/j.spinee.2007.10.012
Gatchel, R. J., and Okifuji, A. (2006). Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J. Pain 7, 779–793. doi: 10.1016/j.jpain.2006.08.005
Gatchel, R. J., Polatin, P. B., Noe, C., Gardea, M., Pulliam, C., and Thompson, J. (2003). Treatment- and cost-effectiveness of early intervention for acute low-back pain patients: a one-year prospective study. J. Occup. Rehabil. 13, 1–9. doi: 10.1023/A:1021823505774
Goossens, M. E. J. B., De Kinderen, R. J. A., Leeuw, M., De Jong, J. R., Ruijgrok, J., Evers, S. M., et al. (2015). Is exposure in vivo cost-effective for chronic low back pain? a trial-based economic evaluation. BMC Health Services Res. 15:549. doi: 10.1186/s12913-015-1212-6
Gore, M., Sadosky, A., Stacey, B. R., Tai, K. S., and Leslie, D. (2012). The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine 37, E668–E677. doi: 10.1097/BRS.0b013e318241e5de
Gustavsson, A., Bjorkman, J., Ljungcrantz, C., Rhodin, A., Rivano-Fischer, M., Sjolund, K. F., et al. (2012). Socio-economic burden of patients with a diagnosis related to chronic pain–register data of 840,000 Swedish patients. Eur. J. Pain 16, 289–299. doi: 10.1016/j.ejpain.2011.07.006
Hoffman, B. M., Papas, R. K., Chatkoff, D. K., and Kerns, R. D. (2007). Meta-analysis of psychological interventions for chronic low back pain. Health Psychol. 26, 1–9. doi: 10.1037/0278-6133.26.1.1
Hong, J., Reed, C., Novick, D., and Happich, M. (2013). Costs associated with treatment of chronic low back pain: an analysis of the UK general practice research database. Spine 38, 75–82. doi: 10.1097/BRS.0b013e318276450f
Judge, A., Arden, N. K., Cooper, C., Kassim Javaid, M., Carr, A. J., Field, R. E., et al. (2012). Predictors of outcomes of total knee replacement surgery. Rheumatology 51, 1804–1813. doi: 10.1093/rheumatology/kes075
Knight, T., Schaefer, C., Chandran, A., Zlateva, G., Winkelmann, A., and Perrot, S. (2013). Health-resource use and costs associated with fibromyalgia in France, Germany, and the United States. Clinicoecon. Outcomes Res. 5, 171–180. doi: 10.2147/CEOR.S41111
Kohlboeck, G., Greimel, K. V., Piotrowski, W. P., Leibetseder, M., Krombholz-Reindl, M., Neuhofer, R., et al. (2004). Prognosis of multifactorial outcome in lumbar discectomy: a prospective longitudinal study investigating patients with disc prolapse. Clin. J. Pain 20, 455–461. doi: 10.1097/00002508-200411000-00011
Kröner-Herwig, B. (2009). Chronic pain syndromes and their treatment by psychological interventions. Curr. Opin. Psychiatry 22, 200–204. doi: 10.1097/YCO.0b013e3283252d5a
Kunutsor, S. K., Whitehouse, M. R., Blom, A. W., and Beswick, A. D. (2016). Patient-related risk factors for periprosthetic joint infection after total joint arthroplasty: a systematic review and meta-analysis. PLoS ONE 11:866. doi: 10.1371/journal.pone.0150866
Lamb, S. E., Hansen, Z., Lall, R., Castelnuovo, E., Withers, E. J., Nichols, V., et al. (2010). Group cognitive behavioural treatment for low-back pain in primary care: a randomised controlled trial and cost-effectiveness analysis. Lancet 375, 916–923. doi: 10.1016/S0140-6736(09)62164-4
Lambeek, L. C., Bosmans, J. E., Van Royen, B. J., Van Tulder, M. W., Van Mechelen, W., and Anema, J. R. (2010). Effect of integrated care for sick listed patients with chronic low back pain: economic evaluation alongside a randomised controlled trial. BMJ 341:c6414. doi: 10.1136/bmj.c6414
Lindberg, M. F., Miaskowski, C., Rustøen, T., Rosseland, L. A., Paul, S. M., Cooper, B. A., et al. (2017). The Impact of demographic, clinical, symptom and psychological characteristics on the trajectories of acute postoperative pain after total knee arthroplasty. Pain Med. 18, 124–139. doi: 10.1093/pm/pnw080
Linton, S. J., and Nordin, E. (2006). A 5-year follow-up evaluation of the health and economic consequences of an early cognitive behavioral intervention for back pain: a randomized, controlled trial. Spine 31, 853–858. doi: 10.1097/01.brs.0000209258.42037.02
Ljótsson, B., Atterlóf, E., Lagerlóf, M., Andersson, E., Jernelóv, S., Hedman, E., et al. (2014). Internet-delivered acceptance and values-based exposure treatment for fibromyalgia: a pilot study. Cogn. Behav. Ther. 43, 93–104. doi: 10.1080/16506073.2013.846401
Louw, A., Diener, I., Landers, M. R., and Puentedura, E. J. (2014). Preoperative pain neuroscience education for lumbar radiculopathy: a multicenter randomized controlled trial with 1-year follow-up. Spine 39, 1449–1457. doi: 10.1097/BRS.0000000000000444
Luciano, J. V., Sabes-Figuera, R., Cardeñosa, E., Peñarrubia-María, M. T., Fernández-Vergel, R., García-Campayo, J., et al. (2013). Cost-utility of a psychoeducational intervention in fibromyalgia patients compared with usual care: an economic evaluation alongside a 12-month randomized controlled trial. Clin. J. Pain 29, 702–711. doi: 10.1097/AJP.0b013e318270f99a
Lundkvist, J., Kastäng, F., and Kobelt, G. (2008). The burden of rheumatoid arthritis and access to treatment: health burden and costs. Eur. J. Health Econ. 8(Suppl. 2), S49–S60. doi: 10.1007/s10198-007-0088-8
Ma, V. Y., Chan, L., and Carruthers, K. J. (2014). The incidence, prevalence, costs and impact on disability of common conditions requiring rehabilitation in the US: stroke, spinal cord injury, traumatic brain injury, multiple sclerosis, osteoarthritis, Rheumatoid Arthritis, limb loss, and back pain. Arch. Phys. Med. Rehabilit. 95, 986–995.e1. doi: 10.1016/j.apmr.2013.10.032
Manchikanti, L., Boswell, M. V., and Hirsch, J. A. (2013). Lessons learned in the abuse of pain-relief medication: a focus on healthcare costs. Expert Rev. Neurother 13, 527–543; quiz 544. doi: 10.1586/ern.13.33
Mancuso, C. A., Reid, M. C., Duculan, R., and Girardi, F. P. (2017). Improvement in pain after lumbar spine surgery: the role of preoperative expectations of pain relief. Clin. J. Pain 33, 93–98. doi: 10.1097/AJP.0000000000000383
Norton, G., McDonough, C. M., Cabral, H., Shwartz, M., and Burgess, J. F. (2015). Cost-utility of cognitive behavioral therapy for low back pain from the commercial payer perspective. Spine 40, 725–733. doi: 10.1097/BRS.0000000000000830
Park, P. W., Dryer, R. D., Hegeman-Dingle, R., Mardekian, J., Zlateva, G., Wolff, G. G., et al. (2016). Cost burden of chronic pain patients in a large integrated delivery system in the United States. Pain Pract. 16, 1001–1011. doi: 10.1111/papr.12357
Pasquale, M. K., Dufour, R., Schaaf, D., Reiners, A. T., Mardekian, J., Joshi, A. V., et al. (2014). Pain conditions ranked by healthcare costs for members of a national health plan. Pain Pract. 14, 117–131. doi: 10.1111/papr.12066
Pietilä Holmner, E., Fahlström, M., and Nordström, A. (2013). The effects of interdisciplinary team assessment and a rehabilitation program for patients with chronic pain. Am. J. Phys. Med. Rehabil. 92, 77–83. doi: 10.1097/PHM.0b013e318278b28e
Pike, A., Hearn, L., and Williams, A. C. (2016). Effectiveness of psychological interventions for chronic pain on health care use and work absence: systematic review and meta-analysis. Pain 157, 777–785. doi: 10.1097/j.pain.0000000000000434
Rayner, L., Hotopf, M., Petkova, H., Matcham, F., Simpson, A., and McCracken, L. M. (2016). Depression in patients with chronic pain attending a specialised pain treatment centre: prevalence and impact on health care costs. Pain 157, 1472–1479. doi: 10.1097/j.pain.0000000000000542
Rivera, J., Rejas, J., Esteve-Vives, J., and Vallejo, M. A. (2009). Resource utilisation and health care costs in patients diagnosed with fibromyalgia in Spain. Clin. Exp. Rheumatol. 27, S39–S45.
Schade, V., Semmer, N., Main, C. J., Hora, J., and Boos, N. (1999). The impact of clinical, morphological, psychosocial and work-related factors on the outcome of lumbar discectomy. Pain 80, 239–249. doi: 10.1016/S0304-3959(98)00210-3
Schweikert, B., Jacobi, E., Seitz, R., Cziske, R., Ehlert, A., Knab, J., et al. (2006). Effectiveness and cost-effectiveness of adding a cognitive behavioral treatment to the rehabilitation of chronic low back pain. J. Rheumatol. 33, 2519–2526.
Slover, J. D., Karia, R. J., Hauer, C., Gelber, Z., Band, P. A., and Graham, J. (2015). Feasibility of integrating standardized patient-reported outcomes in orthopedic care. Am. J. Manag. Care 21, e494–e500.
Stockbridge, E. L., Suzuki, S., and Pagán, J. A. (2015). Chronic pain and health care spending: an analysis of longitudinal data from the Medical Expenditure Panel Survey. Health Serv. Res. 50, 847–870. doi: 10.1111/1475-6773.12263
Tamburin, S., Lacerenza, M. R., Castelnuovo, G., Agostini, M., Paolucci, S., Bartolo, M., et al. (2016). Pharmacological and non-pharmacological strategies in the integrated treatment of pain in neurorehabilitation. evidence and recommendations from the Italian consensus conference on pain in Neurorehabilitation. Eur. J. Phys. Rehabil. Med. 52, 741–752.
Taylor, S. J., Carnes, D., Homer, K., Kahan, B. C., Hounsome, N., Eldridge, S., et al. (2016). Novel three-day, community-based, nonpharmacological group intervention for chronic musculoskeletal pain (copers): a randomised clinical trial. PLoS Med. 13:e1002040. doi: 10.1371/journal.pmed.1002040
Trief, P. M., Grant, W., and Fredrickson, B. (2000). A prospective study of psychological predictors of lumbar surgery outcome. Spine 25, 2616–2621. doi: 10.1097/00007632-200010150-00012
Trompetter, H. R., Bohlmeijer, E. T., Lamers, S. M., and Schreurs, K. M. (2016). Positive psychological wellbeing is required for online self-help acceptance and commitment therapy for chronic pain to be effective. Front. Psychol. 7:353. doi: 10.3389/fpsyg.2016.00353
Trompetter, H. R., Bohlmeijer, E. T., Veehof, M. M., and Schreurs, K. M. (2015). Internet-based guided self-help intervention for chronic pain based on acceptance and commitment therapy: a randomized controlled trial. J. Behav. Med. 38, 66–80. doi: 10.1007/s10865-014-9579-0
Trompetter, H. R., Schreurs, K. M., Heuts, P. H., and Vollenbroek-Hutten, M. M. (2014). The systematic implementation of acceptance & commitment therapy (ACT) in Dutch multidisciplinary chronic pain rehabilitation. Patient Educ. Couns. 96, 249–255. doi: 10.1016/j.pec.2014.05.019
Turk, D. C. (1990). Customizing treatment for chronic pain patients: who, what, and why. Clin. J. Pain 6, 255–270. doi: 10.1097/00002508-199012000-00002
Turk, D. C., Okifuji, A., Sinclair, J. D., and Starz, T. W. (1998). Differential responses by psychosocial subgroups of fibromyalgia syndrome patients to an interdisciplinary treatment. Arthritis Care Res. 11, 397–404. doi: 10.1002/art.1790110511
Turk, D. C., Rudy, T. E., Kubinski, J. A., Zaki, H. S., and Greco, C. M. (1996). Dysfunctional patients with temporomandibular disorders: evaluating the efficacy of a tailored treatment protocol. J. Consult. Clin. Psychol. 64, 139–146. doi: 10.1037/0022-006X.64.1.139
Veehof, M. M., Trompetter, H. R., Bohlmeijer, E. T., and Schreurs, K. M. (2016). Acceptance- and mindfulness-based interventions for the treatment of chronic pain: a meta-analytic review. Cogn. Behav. Ther. 45, 5–31. doi: 10.1080/16506073.2015.1098724
Vos, T., Flaxman, A. D., Naghavi, M., Lozano, R., Michaud, C., Ezzati, M., et al. (2012). Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 380, 2163–2196. doi: 10.1016/S0140-6736(12)61729-2
Wells, A. F., Arnold, L. M., Curtis, C. E., Dunegan, L. J., Lapp, C. W., McCarberg, B. H., et al. (2013). Integrating health information technology and electronic health records into the management of fibromyalgia. Postgrad. Med. 125, 70–77. doi: 10.3810/pgm.2013.07.2678
Williams, A. C., Eccleston, C., and Morley, S. (2012). Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database Syst. Rev. 11:CD007407. doi: 10.1002/14651858.CD007407.pub3
Keywords: pain management, clinical psychology, cost-effectiveness, psychometrics, health psychology, clinical health psychology, clinical health interventions, psychotherapy
Citation: Giusti EM, Pietrabissa G, Manzoni GM, Cattivelli R, Molinari E, Trompetter HR, Schreurs KMG and Castelnuovo G (2017) The Economic Utility of Clinical Psychology in the Multidisciplinary Management of Pain. Front. Psychol. 8:1860. doi: 10.3389/fpsyg.2017.01860
Received: 14 October 2016; Accepted: 06 October 2017;
Published: 31 October 2017.
Edited by:
Alemka Tomicic, Diego Portales University, ChileReviewed by:
Adelaida María A. M. Castro Sánchez, University of Almería, SpainJohannes C. Van Der Wouden, VU University Amsterdam, Netherlands
Copyright © 2017 Giusti, Pietrabissa, Manzoni, Cattivelli, Molinari, Trompetter, Schreurs and Castelnuovo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianluca Castelnuovo, Z2lhbmx1Y2EuY2FzdGVsbnVvdm9AYXV4b2xvZ2ljby5pdA==; Z2lhbmx1Y2EuY2FzdGVsbnVvdm9AdW5pY2F0dC5pdA==
†Present Address: Hester R. Trompetter, Department of Medical and Clinical Psychology, Center for Research on Psychology in Somatic Disorders, Tilburg University, Tilburg, Netherlands
 Emanuele M. Giusti
Emanuele M. Giusti Giada Pietrabissa
Giada Pietrabissa Gian Mauro Manzoni
Gian Mauro Manzoni Roberto Cattivelli
Roberto Cattivelli Enrico Molinari
Enrico Molinari Hester R. Trompetter
Hester R. Trompetter Karlein M. G. Schreurs
Karlein M. G. Schreurs Gianluca Castelnuovo
Gianluca Castelnuovo