- 1Rehabilitation Research Center, Santa Clara Valley Medical Center, San Jose, CA, USA
- 2Department of Neurosurgery, Stanford University, Stanford, CA, USA
- 3Department of Physical Medicine and Rehabilitation, Stanford University, Stanford, CA, USA
- 4Department of Psychology, Stanford University, Stanford, CA, USA
In the general population, females experience depression at significantly higher rates than males. Individuals with traumatic brain injury (TBI) are at substantially greater risk for depression compared to the overall population. Treatment of, and recovery from, TBI can be hindered by depression; comorbid TBI and depression can lead to adverse outcomes and negatively affect multiple aspects of individuals’ lives. Gender differences in depression following TBI are not well understood, and relevant empirical findings have been mixed. Utilizing the Patient Health Questionnaire-9 (PHQ-9) 1 year after TBI, we examined whether women would experience more severe depressive symptoms, and would endorse higher levels of depression within each category of depression severity, than would men. Interestingly, and contrary to our hypothesis, men and women reported mild depression at equal rates; PHQ-9 total scores were slightly lower in women than in men. Men and women did not differ significantly in any PHQ-9 depression severity category. Item analyses, yielded significant gender differences on the following items: greater concentration difficulties (cognitive problems) in men and more sleep disturbances (psychosomatic issues) in women per uncorrected two-sample Z-test for proportions analyses; however, these results were not significant after the family-wise Bonferroni correction. Our results indicate that, in contrast to the general population, mild depression in persons with moderate to severe TBI may not be gender-specific. These findings underscore the need for early identification, active screening, and depression treatment equally for men and women to improve emotional well-being, promote recovery, and enhance quality of life following TBI.
Introduction
Depression is characterized by feelings of sadness, emptiness, hopelessness, and worthlessness. It can also be manifested by concentration problems, fatigue, and a loss of interest in previously enjoyed activities, as well as appetite, weight, and sleep disturbances; recurrent thoughts about death or suicidal ideation may also be present (American Psychiatric Association, 2013). Risk factors for depression include, experiencing adverse events during childhood such as emotional, physical, and sexual abuse (Chapman et al., 2004; American Psychiatric Association, 2013), memory and cognitive biases that influence emotion regulation (Foland-Ross and Gotlib, 2012; Kircanski et al., 2012), and genetic and physiological factors including a family history of depression, specifically among first-degree relatives, in addition to early onset or recurrent forms of depression (Sullivan et al., 2000; American Psychiatric Association, 2013).
Depression can affect multiple facets of life and cause clinically significant impairment or distress to individuals’ physical and emotional well-being, as well as to their social and professional life (American Psychiatric Association, 2013). Functional consequences can range from fairly mild, when depressive symptoms are undetected by others, to full impairment, such as the inability to address one’s own basic self-care needs (American Psychiatric Association, 2013). In the general medical setting, depressed individuals often experience higher levels of physical illness and pain and a diminished capacity for physical, social, and role functioning (American Psychiatric Association, 2013). Suicide is arguably the most serious consequence of depression (American Psychiatric Association, 2013); over half of all suicides transpire within the context of a mood disorder (Mann et al., 2005; Guillamondegui et al., 2011).
The prevalence rate of depression is estimated to be 8–10% in the general population (Guillamondegui et al., 2011). While epidemiologic findings elucidate that females are 70% more likely than males to experience depression (American Psychiatric Association, 2013; National Alliance on Mental Illness, 2016), clear gender differences in symptoms, course, response to treatment, and functional consequences have not been identified (American Psychiatric Association, 2013). Furthermore, some researchers have posited the Diagnostic Statistical Manual (DSM-5) (American Psychiatric Association, 2013), used to diagnose both psychiatric and neurological conditions, includes depressive symptoms that are more readily observed in female-specific depression (Weissman et al., 1984; Breslau et al., 1995; Piccinelli and Wilkinson, 2000; Kenneth et al., 2002).
Risk for depression among individuals with traumatic brain injury (TBI) is markedly higher than that seen in the general population (Scholten et al., 2016). Approximately 25–50% of persons with TBI will experience major depression within the first year after TBI (Scholten et al., 2016), and over 60% of persons are affected within 7 years after injury (Fann et al., 2009), reporting long-term struggles with a mood disorder. Importantly, major depression is associated with adverse outcomes for individuals with TBI (Barker-Collo et al., 2015; Bombardier et al., 2016; Moreno-Lopez et al., 2016), including social isolation, hostility and cognitive deficits (Mauri et al., 2014). Anxiety and addiction, along with other psychiatric conditions, may co-occur with depression in individuals with TBI (Gordon et al., 2006; Guillamondegui et al., 2011). Depression and comorbid psychiatric conditions can complicate depression screening, diagnosis, and treatment in a variety of ways, including depression being masked and ultimately left undiagnosed, and may interfere with an individual’s ability to comply and adhere to treatment (Gordon et al., 2006; Guillamondegui et al., 2011).
Little is known about the development and progression of depression following TBI (Bombardier et al., 2016), particularly among women (Oyesanya and Ward, 2016); this is due, in part, to the high symptom overlap (poor self-regulation, cognitive and inhibitory deficits) between TBI and depression (Schwarzbold et al., 2008). Despite the fact that depression is a frequently reported psychiatric condition following TBI, the extent to which depression influences long-term disability after TBI is not known (Crooks et al., 2007; Guillamondegui et al., 2011). Depression may be masked by cognitive changes, a flat affect, or other deficits commonly seen following TBI; these deficits may be attributed to the absence of post-trauma treatment progress when they are actually due to underlying depression (Guillamondegui et al., 2011). Risk factors for depression following TBI include structural changes in the brain due to injury (Cervos-Navarro and Lafuente, 1991; Xiao et al., 2015). Depression may also be a consequence of injury to the areas of the brain that manage emotions, in particular areas of the limbic system such as the amygdala (Blennow et al., 2012; Harmon et al., 2013). Changes in levels of neurotransmitter chemicals in the brain, which modulate emotions, have also been reported and can increase risk for depression following TBI (Blennow et al., 2012). Psychological response to injury may also elevate risk for depression in TBI (Lukow et al., 2015). Finally, depression can arise as individuals who have experienced TBI face new challenges in adapting to temporary or permanent disability, limitations, or changes in their professional, family, and community life (Lukow et al., 2015). Understanding differences in these factors between men and women is critical to early identification and treatment for depression in order to maximize recovery following TBI.
The Patient Health Questionnaire (PHQ-9) is a powerful clinical tool to study depression; it is able to detect a wide range of depression symptoms (Kroenke et al., 2001). Importantly, the PHQ-9 has been shown to be a sensitive instrument in identifying depression in individuals with TBI, especially in the hospital context (Dyer et al., 2016). The objective of this study was to assess depression, measured by the PHQ-9, in males and females 1 year following TBI. We hypothesized that, compared with males, females will report more symptoms of depression, operationalized as mean PHQ-9 total score, as well as a higher severity of depression within each of the five PHQ-9 depression severity categories, at a 1-year follow-up assessment.
Materials and Methods
Setting
This study was approved by the Santa Clara Valley Medical Center IRB Committee. All participants were admitted to the Rehabilitation Center of Santa Clara Valley Medical Center (SCVMC), a Level I Trauma hospital. The Rehabilitation Center is a specialty unit providing treatment to the most medically complex and acute traumatic brain-injured patients. This work was conducted at the Rehabilitation Research Center, SCVMC.
Participants
Participants were from the Northern California TBI Model Systems of Care (TBIMS) database, a longitudinal study to assess long-term outcomes following TBI (Dahmer et al., 1993). All participants (1) met the TBIMS case definition for TBI (Dahmer et al., 1993); (2) met at least one of the criteria for moderate to severe TBI: post-traumatic amnesia > 24 h, trauma related intracranial neuroimaging abnormalities, loss of consciousness > 30 min, and/or Glasgow Coma Scale (GCS) < 13; (3) were age 16 years or older at the time of injury; and (4) sustained a TBI within California.
Inclusion criteria required that participants had a 1-year follow-up assessment completed between October 2007 and October 2013 (n = 238); these were the corresponding years that the PHQ-9 scores were obtained. Participants with a 1-year follow-up completed between October 2007 and October 2013 who had missing PHQ-9 data were excluded (n = 63); reasons for exclusions and missing data included lost to follow-up, refused follow-up, withdrew from study, incarcerated, expired, unavailable, and physically or cognitively unable to provide PHQ-9 responses. As described below, 175 individuals (n = 131 males; n = 44 females) met the inclusion criteria for analysis.
Participant Characteristics
Demographic variables included sex, age, ethnicity, marital status, and employment status. Of the 238 participants who completed a 1-year follow-up between October 2007 and October 2013, 182 were male (75%) and 56 were female (25%); mean age was 32.38 (SD = 16.76). After excluding participants who were lost to follow-up (n = 7), refused (n = 2), withdrew (n = 1), incarcerated (n = 2), expired (n = 1), unavailable (n = 9), and physically or cognitively unable to provide PHQ-9 responses (n = 41), 131 males and 44 females (n = 175) were available for analysis. The racial and ethnic mix of the study population was White (n = 137), Black (n = 10), Hispanic (n = 65), Asian or Pacific Islander (n = 20), Native American (n = 1), and other (n = 5). Marital status was predominantly single (n = 149), followed by married (n = 61), divorced (n = 15), separated (n = 12), and other (n = 1). Years of education were: ≤8 (n = 7), 9–12 (n = 108), 13–16 (n = 109), and >16 (n = 14).
Procedures
This study was carried out in accordance with the approval of the Institutional Review Board’s Research and Human Subjects Review Committee of SCVMC. All participants understood and provided informed consent to participate or, if unable, family or legal guardian understood and provided informed consent for the patient in accordance with the Declaration of Helsinki. Data regarding injury was collected via medical record abstraction by a research assistant. At 1-year post-injury, a research assistant conducted follow-up assessments for data collection.
Measures
The PHQ-9 (Kroenke et al., 2001) is a self-reported 9-item measure of depression. Scores are totaled and are categorized into level of severity with higher scores indicating greater depressive symptoms (1–4: minimal depression, 5–9: mild depression, 10–14: moderate depression, 15–19: moderately severe depression, 20–27: severe depression). The PHQ-9 has good test-retest reliability (r = 0.84) and internal reliability (α = 0.89) (Kroenke et al., 2001). The PHQ-9 is valid and reliable in persons with TBI (Fann et al., 2005).
Analyses
Demographic variables, as mentioned above, were obtained for all participants who completed a 1-year follow-up assessment between October 2007 and October 2013 (n = 238). The final sample for analyses (n = 175) was then divided into two groups on the basis of sex. For each group, mean PHQ-9 total scores were calculated. A two-tailed t-test was used to compare the average total PHQ-9 scores between the two groups, with alpha set at p < 0.05. The percentages of individuals in each category of depression severity was calculated for each group. Two-sample Z-tests for proportions were then used to compare the categories of male versus female within each category of depression. The percentage of individuals who endorsed each of the 9-items of depressive symptoms was calculated for each group to provide an item analysis assessment. Two-sample Z-tests for proportions were then used to compare the proportion of males versus females for each item.
Initial analysis was conducted using Microsoft Excel; a data analysis cross check was then performed using IBM SPSS Statistics 24. An independent sample t-test was used to cross check for mean PHQ-9 total scores, following an outlier and range check. Chi-squared tests were used to cross check all initial Z-tests run for depression severity categories and item analyses; the Bonferroni correction was applied to correct for any family-wise errors arising from multiple comparisons in the data analyses.
Results
PHQ-9 Total Scores
Both men and women reported experiencing mild levels of depression (PHQ-9 Total Score = 5–9). Total PHQ-9 scores in men (M = 6.04; SD = 6.26) were higher than total PHQ-9 scores in women (M = 5.27; SD = 5.58), but this difference was not statistically significant [t(173) = -0.72; p = 0.47].
PHQ-9 Depression Severity Categories
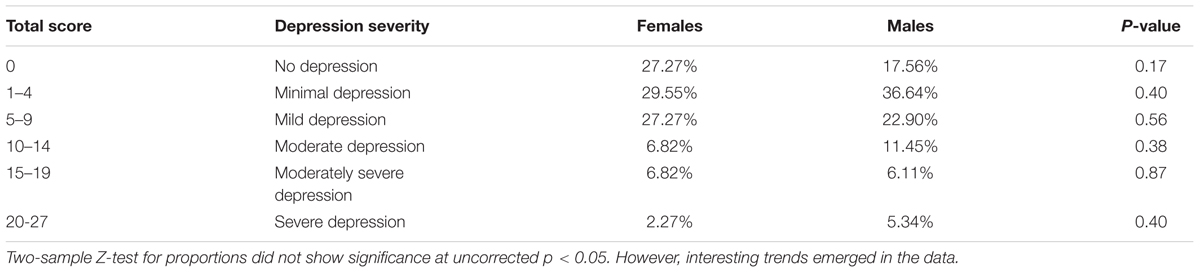
A lower percentage of males (17.56%) than females (27.27%) reported experiencing no symptoms of depression, mild depressive symptoms (22.90% vs. 27.27%), and moderately severe depressive symptoms (6.11% vs. 6.82%); uncorrected two-sample Z-test for proportions analyses comparing males and females, however, revealed no statistically significant differences in any PHQ-9 depression severity category (|z|≥ 0.84; p ≥ 0.16) (see Table 1).
PHQ-9 Item Analysis
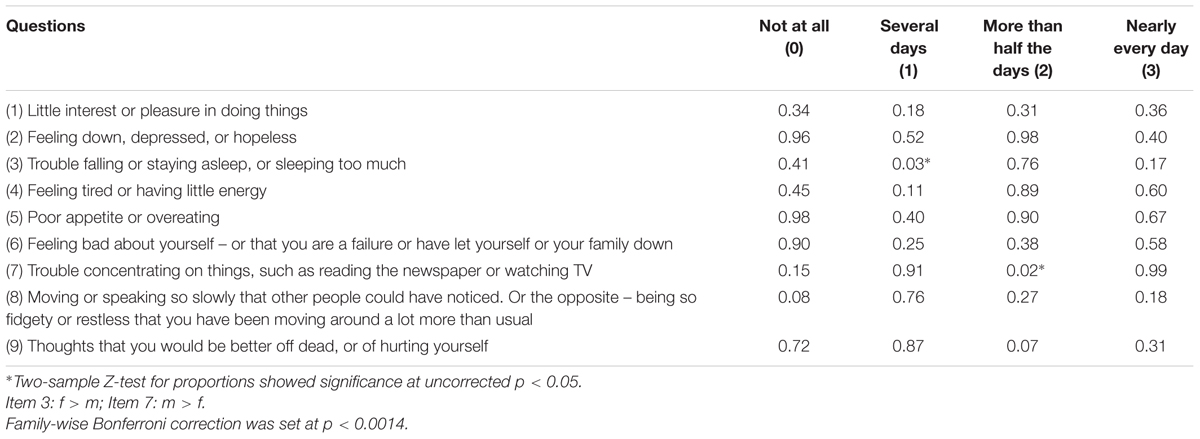
The uncorrected item analysis yielded statistically significant sex differences for the following items: males endorsed “trouble concentrating on things, such as reading the newspaper or watching television” for “more than half the days” to a greater degree than did females (12.21% vs. 0%) (z = 2.43; p = 0.02), and females endorsed “trouble falling or staying asleep or sleeping too much” for “several days” to a greater degree than did males (31.82% vs. 16.79%) (z = -2.13; p = 0.03) (see Table 2). However, these results did not reach significance using Bonferroni corrected alpha of p = 0.0014.
Discussion
Individuals with TBI are at a significantly higher risk compared to the general population for developing both acute and chronic depression (Scholten et al., 2016), and for the emergence of various psychiatric disorders (Iverson et al., 2011; Brandel et al., 2016) such as anxiety and post-traumatic stress disorder (PTSD) (Zaninotto et al., 2016), and suicidal thoughts and behaviors (Fisher et al., 2016). Given the lethality concerns surrounding depression, raising awareness about the prevalence of depression in persons with TBI is especially important.
The present study of sex differences in TBI and depression is critical given recent findings from the Centers for Disease Control and Prevention (2016) indicating that the prevalence of women with mild to severe TBI, as measured by TBI-related Emergency Department visits in the U.S. among the general population, has risen by 49% between 2007 and 2010; rising rates among women have been attributed to more females experiencing falls, motor vehicle accidents, unintentional blunt traumas, and assaults (Centers for Disease Control and Prevention, 2016; Oyesanya and Ward, 2016). Importantly, depression rates are increasing in parallel to the rising rates of TBI (Oyesanya and Ward, 2016). Previous studies reveal that female survivors of TBI are at higher risk for developing depressive disorders than are male survivors (Iverson et al., 2011; Oyesanya and Ward, 2016; Scholten et al., 2016). Other research, however, suggests that there are no gender differences in outcomes post-TBI (Mushkudiani et al., 2007; Slewa-Younan et al., 2008; Renner et al., 2012), and still other findings indicate that males with TBI are at a higher risk for depression than are females (Sigurdardottir et al., 2013; Albrecht et al., 2015), particularly when comparing post-menopausal women with age-matched men (Davis et al., 2006). Investigators have found that younger women have better outcomes than do older women post-TBI; this may be attributable to the neuro-protective effects of hormones found in pre-menopausal women (Kirkness et al., 2004; Wagner et al., 2004; Ley et al., 2013). Despite conflicting results, researchers and clinicians alike are becoming aware of hormonal disturbances that often follow TBI (Ghigo et al., 2005; Schneider et al., 2011; Lauzier et al., 2014). Therefore, it is imperative for depression treatment care plans following TBI to be tailored to each gender specifically to address the physiological and hormonal differences between men and women who are affected by brain injury.
Investigators have suggested that TBI-related depression results from altered functional connectivity of a number of networks in the brain, including white matter abnormalities (Isaac et al., 2015), and neuroadaptions within the thalamus, insula, and subgenual cingulate cortex (Moreno-Lopez et al., 2016). Disruption to the neural circuitry between the limbic system and the prefrontal cortex, that results from diffuse axonal injury (Inglese et al., 2005; Silver et al., 2009), as well as from damage to the hippocampus, amygdala, and prefrontal regions of the brain (Harmon et al., 2013), has also been found to lead to mood disorders that develop as soon as a few weeks or months following the initial injury (Jorge and Starkstein, 2005). A number of other factors, including various adjustment issues and unique barriers that accompany TBI recovery (Moreno-Lopez et al., 2016) such as low levels of social support, being young at time of injury (Ouellet et al., 2009), and lack of hope (Oyesanya and Ward, 2016), may also contribute to depression emergence among the TBI population. Indeed, one of the most disabling symptoms of depression is lack of hope; depression, comorbid with TBI, is therefore a leading contributor to disability following TBI (Oyesanya and Ward, 2016). These contributing factors for depression may help explain why gender differences are not as prevalent among those with TBI compared with the general population. Both males and females with a TBI experience life-altering changes that directly impact their quality of life and productivity. Future research is needed to quantify the extent to which depression emergence post-TBI is a direct result of structural and neurochemical changes that occur in the brain following the injury versus due to the associated barriers in TBI recovery attributable to suffering a TBI.
Interestingly, unlike the general population, the mild depression noted among both males and females with TBI in our study population suggest that depression is not gender-specific. Gender differences may be seen, however, in the manifestation of depression symptoms. We demonstrated that a greater percentage of men reported concentration difficulties, where depression was experienced through cognitive symptoms, while a higher percentage of women indicated sleep disturbance issues, reflecting more psychosomatic symptoms of depression. These exploratory results are consistent with previous research demonstrating that depression symptoms are expressed differently in men and women; whereas men experience cognitive symptoms (Alexandrino-Silva et al., 2013), women are more affected psychosomatically (Alexandrino-Silva et al., 2013; Silverstein et al., 2013); however, our item analyses did not reach statistical significance using a strict Bonferroni correction. These findings warrant further study in order to better understand depression following TBI and its unique impact on each gender. Moreover, our results indicate the need for early identification, active screening, and treatment of mood disorders in both genders equally to improve emotional functioning, reduce disability, promote recovery, and enhance quality of life following TBI.
While this study provides valuable gender comparison information regarding depression following TBI, limitations exist. The present study sample of fewer women (25%) than men (75%) may not be adequate to fully evaluate the gender differences in depression post-TBI; we should note, however, that this gender ratio is representative of individuals who have sustained a moderate to severe TBI across all TBI Model Systems throughout the U.S. (Frost et al., 2013; Model Systems Knowledge Translation Center, 2016) with female TBI representation being even smaller in the Veteran population (Armed Forces Health Surveillance Center, 2013). It is also important to highlight that individuals in this study sample were slightly younger and more racially and ethnically diverse, compared with the Model Systems National Database as a whole (Model Systems Knowledge Translation Center, 2016). Future research is needed to extend this study to assess depression in women and men with TBI across the country. Finally, we used data from only one time point, as opposed to measuring depression over a series of time points, thus limiting our ability to assess spontaneous symptom recovery, relapse, or a change in depression over time. We plan to expand this research by analyzing data from the entire Model Systems National Database, and to assess depression at multiple time points, in order to more fully evaluate depression in women and men following TBI.
Author Contributions
LI is the last author and anchored and directed the project. She also actively wrote sections of the “Introduction” and “Discussion” as well as assisted in directing the data analysis. SL, first author collected the data, conceived of the clinical outcomes, wrote the majority of the manuscripts. All remaining authors contributed to both data interpretation and writing of the paper.
Funding
This work was funded by the National Institute on Disability, Independent Living, and Rehabilitation Research, Administration for Community Living, U.S. Department of Health and Human Services (Grant # H133A11006) to the SCVMC Rehabilitation Research Center Director and Principal Investigator, LI.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
This work was supported by colleagues at Santa Clara Valley Medical Center, Jyodi Mohole and Judith Mills, as well as Drs. Roberta Wang, Henry Huie, and Emily Huang. The subject recruitment and data acquisition team consisted of Laura Jamison and Ketra Toda.
References
Albrecht, J. S., Kiptanui, Z., Tsang, Y., Khokhar, B., Liu, X., Simoni-Wastila, L., et al. (2015). Depression among older adults after traumatic brain injury: a national analysis. Am. J. Geriatr. Psychiatry 23, 607–614. doi: 10.1016/j.jagp.2014.07.006
Alexandrino-Silva, C., Wang, Y. P., Carmen Viana, M., Bulhoes, R. S., Martins, S. S., and Andrade, L. H. (2013). Gender differences in symptomatic profiles of depression: results from the Sao Paulo Megacity Mental Health Survey. J. Affect. Disord. 147, 355–364. doi: 10.1016/j.jad.2012.11.041
American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Arlington, VA: American Psychiatric Publishing. doi: 10.1176/appi.books.9780890425596
Armed Forces Health Surveillance Center (2013). Incident diagnoses of common symptoms (“sequelae”) following traumatic brain injury, active component, U. S. Armed Forces, 2000-2012. Med. Surveil. Mon. Rep. 20, 9–13.
Barker-Collo, S., Jones, A., Jones, K., Theadom, A., Dowell, A., Starkey, N., et al. (2015). Prevalence, natural course and predictors of depression 1 year following traumatic brain injury from a population-based study in New Zealand. Brain Inj. 29, 859–865. doi: 10.3109/02699052.2015.1004759
Blennow, K., Hardy, J., and Zetterberg, H. (2012). The neuropathology and neurobiology of traumatic brain injury. Neuron 76, 886–899. doi: 10.1016/j.neuron.2012.11.021
Bombardier, C. H., Hoekstra, T., Dikmen, S., and Fann, J. R. (2016). Depression trajectories during the first year after traumatic brain injury. J. Neurotrauma 33, 2115–2124. doi: 10.1089/neu.2015.4349
Brandel, M. G., Hirshman, B. R., McCutcheon, B. A., Tringale, K., Carroll, K., Richtand, N. M., et al. (2016). The association between psychiatric comorbidities and outcomes for inpatients with traumatic brain injury. J. Neurotrauma 34, 1005–1016. doi: 10.1089/neu.2016.4504
Breslau, N., Schultz, L., and Peterson, E. (1995). Sex differences in depression: a role for preexisting anxiety. Psychiatry Res. 58, 1–12. doi: 10.1016/0165-1781(95)02765-O
Centers for Disease Control and Prevention (2016). Rates of TBI-Related Emergency Department Visits by Sex – United States, 2001–2010. Available at: https://www.cdc.gov/traumaticbraininjury/data/rates_ed_bysex.html
Cervos-Navarro, J., and Lafuente, J. V. (1991). Traumatic brain injuries: structural changes. J. Neurol. Sci. 103(Suppl.), S3–S14. doi: 10.1016/0022-510x(91)90002-o
Chapman, D. P., Whitfield, C. L., Felitti, V. J., Dube, S. R., Edwards, V. J., and Anda, R. F. (2004). Adverse childhood experiences and the risk of depressive disorders in adulthood. J. Affect. Disord. 82, 217–225. doi: 10.1016/j.jad.2003.12.013
Crooks, C. Y., Zumsteg, J. M., and Bell, K. R. (2007). Traumatic brain injury: a review of practice management and recent advances. Phys. Med. Rehabil. Clin. N. Am. 18, 681–710. doi: 10.1016/j.pmr.2007.06.005
Dahmer, E. R., Shilling, M. A., Hamilton, B. B., Bontke, C. F., Englander, J., Kreutzer, J. S., et al. (1993). A model systems database for traumatic brain injury. J. Head Trauma Rehabil. 8, 12–25. doi: 10.1097/00001199-199308020-00004
Davis, D. P., Douglas, D. J., Smith, W., Sise, M. J., Vilke, G. M., Holbrook, T. L., et al. (2006). Traumatic brain injury outcomes in pre- and post- menopausal females versus age-matched males. J. Neurotrauma 23, 140–148. doi: 10.1089/neu.2006.23.140
Dyer, J. R., Williams, R., Bombardier, C. H., Vannoy, S., and Fann, J. R. (2016). Evaluating the psychometric properties of 3 depression measures in a sample of persons with traumatic brain injury and major depressive disorder. J. Head Trauma Rehabil. 31, 225–232. doi: 10.1097/HTR.0000000000000177
Fann, J. R., Bombardier, C. H., Dikmen, S., Esselman, P., Warms, C. A., Pelzer, E., et al. (2005). Validity of the patient health questionnaire-9 in assessing depression following traumatic brain injury. J. Head Trauma Rehabil. 20, 501–511. doi: 10.1097/00001199-200511000-00003
Fann, J. R., Hart, T., and Schomer, K. G. (2009). Treatment for depression after traumatic brain injury: a systematic review. J. Neurotrauma 26, 2383–2402. doi: 10.1089/neu.2009.1091
Fisher, L. B., Pedrelli, P., Iverson, G. L., Bergquist, T. F., Bombardier, C. H., Hammond, F. M., et al. (2016). Prevalence of suicidal behaviour following traumatic brain injury: longitudinal follow-up data from the NIDRR traumatic brain injury model systems. Brain Inj. 30, 1311–1318. doi: 10.1080/02699052.2016.1195517
Foland-Ross, L. C., and Gotlib, I. H. (2012). Cognitive and neural aspects of information processing in major depressive disorder: an integrative perspective. Front. Psychol. 3:489. doi: 10.3389/fpsyg.2012.00489
Frost, R. B., Farrer, T. J., Primosch, M., and Hedges, D. W. (2013). Prevalence of traumatic brain injury in the general adult population: a meta-analysis. Neuroepidemiology 40, 154–159. doi: 10.1159/000343275
Ghigo, E., Masel, B., Aimaretti, G., Leon-Carrion, J., Casanueva, F. F., Dominguez-Morales, M. R., et al. (2005). Consensus guidelines on screening for hypopituitarism following traumatic brain injury. Brain Inj. 19, 711–724. doi: 10.1080/02699050400025315
Gordon, W. A., Zafonte, R., Cicerone, K., Cantor, J., Brown, M., Lombard, L., et al. (2006). Traumatic brain injury rehabilitation: state of the science. Am. J. Phys. Med. Rehabil. 85, 343–382. doi: 10.1097/01.phm.0000202106.01654.61
Guillamondegui, O. D., Montgomery, S. A., Phibbs, F. T., McPheeters, M. L., Alexander, P. T., Jerome, R. N., et al. (2011). Traumatic Brain Injury and Depression. Rockville, MD: Agency for Healthcare Research and Quality (US).
Harmon, K. G., Drezner, J., Gammons, M., Guskiewicz, K., Halstead, M., Herring, S., et al. (2013). American medical society for Sports Medicine position statement: concussion in sport. Clin. J. Sport. Med. 23, 1–18. doi: 10.1097/JSM.0b013e31827f5f93
Inglese, M., Makani, S., Johnson, G., Cohen, B. A., Silver, J. A., Gonen, O., et al. (2005). Diffuse axonal injury in mild traumatic brain injury: a diffusion tensor imaging study. J. Neurosurg. 103, 298–303. doi: 10.3171/jns.2005.103.2.0298
Isaac, L., Main, K. L., Soman, S., Gotlib, I. H., Furst, A. J., Kinoshita, L. M., et al. (2015). The impact of depression on Veterans with PTSD and traumatic brain injury: a diffusion tensor imaging study. Biol. Psychol. 105, 20–28. doi: 10.1016/j.biopsycho.2014.12.011
Iverson, K. M., Hendricks, A. M., Kimerling, R., Krengel, M., Meterko, M., Stolzmann, K. L., et al. (2011). Psychiatric diagnoses and neurobehavioral symptom severity among OEF/OIF VA patients with deployment-related traumatic brain injury: a gender comparison. Womens Health Issues 21(4 Suppl.), S210–S217. doi: 10.1016/j.whi.2011.04.019
Jorge, R. E., and Starkstein, S. E. (2005). Pathophysiologic aspects of major depression following traumatic brain injury. J. Head Trauma Rehabil. 20, 475–487. doi: 10.1097/00001199-200511000-00001
Kenneth, S., Kendler, Charles, O., Gardner, and Prescott, C. A. (2002). Toward a comprehensive developmental model for major depression in women. Am. J. Psychiatry 159, 1133–1145. doi: 10.1176/appi.ajp.159.7.1133
Kircanski, K., Joormann, J., and Gotlib, I. H. (2012). Cognitive aspects of depression. Wiley Interdiscip. Rev. Cogn. Sci. 3, 301–313. doi: 10.1002/wcs.1177
Kirkness, C. J., Burr, R. L., Mitchell, P. H., and Newell, D. W. (2004). Is there a sex difference in the course following traumatic brain injury? Biol. Res. Nurs. 5, 299–310. doi: 10.1177/1099800404263050
Kroenke, K., Spitzer, R. L., and Williams, J. B. (2001). The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613. doi: 10.1046/j.1525-1497.2001.016009606.x
Lauzier, F., Turgeon, A. F., Boutin, A., Shemilt, M., Cote, I., Lachance, O., et al. (2014). Clinical outcomes, predictors, and prevalence of anterior pituitary disorders following traumatic brain injury: a systematic review. Crit. Care Med. 42, 712–721. doi: 10.1097/CCM.0000000000000046
Ley, E. J., Short, S. S., Liou, D. Z., Singer, M. B., Mirocha, J., Melo, N., et al. (2013). Gender impacts mortality after traumatic brain injury in teenagers. J. Trauma Acute Care Surg. 75, 682–686. doi: 10.1097/TA.0b013e31829d024f
Lukow, H. R. II, Godwin, E. E., Marwitz, J. H., Mills, A., Hsu, N. H., and Kreutzer, J. S. (2015). Relationship between resilience, adjustment, and psychological functioning after traumatic brain injury: a preliminary report. J. Head Trauma Rehabil. 30, 241–248. doi: 10.1097/HTR.0000000000000137
Mann, J. J., Apter, A., Bertolote, J., Beautrais, A., Currier, D., Haas, A., et al. (2005). Suicide prevention strategies: a systematic review. JAMA 294, 2064–2074. doi: 10.1001/jama.294.16.2064
Mauri, M. C., Paletta, S., Colasanti, A., Miserocchi, G., and Altamura, A. C. (2014). Clinical and neuropsychological correlates of major depression following post-traumatic brain injury, a prospective study. Asian J. Psychiatr. 12, 118–124. doi: 10.1016/j.ajp.2014.07.003
Model Systems Knowledge Translation Center (2016). National Data and Statistical Center Traumatic Brain Injury Model Systems National Database: 2015 Profile of People within the Traumatic Brain Injury Model Systems. Available at: http://www.msktc.org/lib/docs/Data_Sheets_/2016_TBIMS_National_Database_Update.pdf
Moreno-Lopez, L., Sahakian, B. J., Manktelow, A., Menon, D. K., and Stamatakis, E. A. (2016). Depression following traumatic brain injury: a functional connectivity perspective. Brain Inj. 30, 1319–1328. doi: 10.1080/02699052.2016.1186839
Mushkudiani, N. A., Engel, D. C., Steyerberg, E. W., Butcher, I., Lu, J., Marmarou, A., et al. (2007). Prognostic value of demographic characteristics in traumatic brain injury: results from the IMPACT study. J. Neurotrauma 24, 259–269. doi: 10.1089/neu.2006.0028
National Alliance on Mental Illness (2016). Depression. Available at: http://www.nami.org/Learn-More/Mental-Health-Conditions/Depression
Ouellet, M. C., Morin, C. M., and Lavoie, A. (2009). Volunteer work and psychological health following traumatic brain injury. J. Head Trauma Rehabil. 24, 262–271. doi: 10.1097/HTR.0b013e3181a68b73
Oyesanya, T. O., and Ward, E. C. (2016). Mental health in women with traumatic brain injury: a systematic review on depression and hope. Health Care Women Int. 37, 45–74. doi: 10.1080/07399332.2015.1005307
Piccinelli, M., and Wilkinson, G. (2000). Gender differences in depression. Critical review. Br. J. Psychiatry 177, 486–492. doi: 10.1192/bjp.177.6.486
Renner, C., Hummelsheim, H., Kopczak, A., Steube, D., Schneider, H. J., Schneider, M., et al. (2012). The influence of gender on the injury severity, course and outcome of traumatic brain injury. Brain Inj. 26, 1360–1371. doi: 10.3109/02699052.2012.667592
Schneider, H. J., Schneider, M., Kreitschmann-Andermahr, I., Tuschy, U., Wallaschofski, H., Fleck, S., et al. (2011). Structured assessment of hypopituitarism after traumatic brain injury and aneurysmal subarachnoid hemorrhage in 1242 patients: the German interdisciplinary database. J. Neurotrauma 28, 1693–1698. doi: 10.1089/neu.2011.1887
Scholten, A. C., Haagsma, J. A., Cnossen, M. C., Olff, M., van Beeck, E. F., and Polinder, S. (2016). Prevalence of and risk factors for anxiety and depressive disorders after traumatic brain injury: a systematic review. J. Neurotrauma 33, 1969–1994. doi: 10.1089/neu.2015.4252
Schwarzbold, M., Diaz, A., Martins, E. T., Rufino, A., Amante, L. N., Thais, M. E., et al. (2008). Psychiatric disorders and traumatic brain injury. Neuropsychiatr. Dis. Treat. 4, 797–816.
Sigurdardottir, S., Andelic, N., Roe, C., and Schanke, A. K. (2013). Depressive symptoms and psychological distress during the first five years after traumatic brain injury: relationship with psychosocial stressors, fatigue and pain. J. Rehabil. Med. 45, 808–814. doi: 10.2340/16501977-1156
Silver, J. M., McAllister, T. W., and Arciniegas, D. B. (2009). Depression and cognitive complaints following mild traumatic brain injury. Am. J. Psychiatry 166, 653–661. doi: 10.1176/appi.ajp.2009.08111676
Silverstein, B., Edwards, T., Gamma, A., Ajdacic-Gross, V., Rossler, W., and Angst, J. (2013). The role played by depression associated with somatic symptomatology in accounting for the gender difference in the prevalence of depression. Soc. Psychiatry Psychiatr. Epidemiol. 48, 257–263. doi: 10.1007/s00127-012-0540-7
Slewa-Younan, S., van den Berg, S., Baguley, I. J., Nott, M., and Cameron, I. D. (2008). Towards an understanding of sex differences in functional outcome following moderate to severe traumatic brain injury: a systematic review. J. Neurol. Neurosurg. Psychiatry 79, 1197–1201. doi: 10.1136/jnnp.2008.147983
Sullivan, P. F., Neale, M. C., and Kendler, K. S. (2000). Genetic epidemiology of major depression: review and meta-analysis. Am. J. Psychiatry 157, 1552–1562. doi: 10.1176/appi.ajp.157.10.1552
Wagner, A. K., Bayir, H., Ren, D., Puccio, A., Zafonte, R. D., and Kochanek, P. M. (2004). Relationships between cerebrospinal fluid markers of excitotoxicity, ischemia, and oxidative damage after severe TBI: the impact of gender, age, and hypothermia. J. Neurotrauma 21, 125–136. doi: 10.1089/089771504322778596
Weissman, M. M., Leaf, P. J., Holzer, C. E. III, Myers, J. K., and Tischler, G. L. (1984). The epidemiology of depression. An update on sex differences in rates. J. Affect. Disord. 7, 179–188. doi: 10.1016/0165-0327(84)90039-9
Xiao, H., Yang, Y., Xi, J. H., and Chen, Z. Q. (2015). Structural and functional connectivity in traumatic brain injury. Neural Regen. Res. 10, 2062–2071. doi: 10.4103/1673-5374.172328
Keywords: depression, mood, traumatic brain injury, concussion, gender
Citation: Lavoie S, Sechrist S, Quach N, Ehsanian R, Duong T, Gotlib IH and Isaac L (2017) Depression in Men and Women One Year Following Traumatic Brain Injury (TBI): A TBI Model Systems Study. Front. Psychol. 8:634. doi: 10.3389/fpsyg.2017.00634
Received: 23 December 2016; Accepted: 09 April 2017;
Published: 05 May 2017.
Edited by:
Michael Noll-Hussong, University of Ulm, GermanyReviewed by:
Susan Elizabeth Esposito, Life University, USAAndrei Irimia, University of Southern California, USA
Copyright © 2017 Lavoie, Sechrist, Quach, Ehsanian, Duong, Gotlib and Isaac. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Linda Isaac, bGluZGEuSXNhYWNAaGhzLnNjY2dvdi5vcmc=
 Sarah Lavoie
Sarah Lavoie Samantha Sechrist
Samantha Sechrist Nhung Quach1
Nhung Quach1 Reza Ehsanian
Reza Ehsanian Linda Isaac
Linda Isaac