- 1Psychology Research Laboratory, Istituto Auxologico Italiano IRCCS, San Giuseppe Hospital, Verbania, Italy
- 2Department of Psychology, Catholic University of Milan, Milan, Italy
- 3Faculty of Psychology, eCampus University, Novedrate, Italy
- 4Cardinal Ferrari Rehabilitation Center, Santo Stefano Rehabilitation Istitute, Fontanellato, Italy
- 5Private Practice, Parma, Italy
- 6Casa di Cura San Pio X S.r.l., HUMANITAS, Milan, Italy
- 7IRCCS Galeazzi Orthopedic Institute, Milan, Italy
- 8Department of Dynamic and Clinical Psychology, Sapienza University of Rome, Rome, Italy
- 9Department of Psychology, Harvard University, Cambridge, MA, USA
- 10Department of Psychology, University of Turin, Turin, Italy
- 11Villa Scassi Hospital, Genova, Italy
- 12Department of Neuroscience “Rita Levi Montalcini”, University of Turin, Turin, Italy
- 13Rehabilitation Unit, Istituto Auxologico Italiano IRCCS, San Giuseppe Hospital, Verbania, Italy
- 14Department of Neurology and Neurorehabilitation, Istituto Auxologico Italiano IRCCS, San Giuseppe Hospital, Verbania, Italy
- 15“Pain Center II Level - Department of Surgery” - ASST Grande Ospedale Metropolitano Niguarda, Milano, Italy
- 16Fondazione Santa Lucia IRCCS, Rome, Italy
- 17Department of Brain and Behavioral Sciences, C. Mondino National Neurological Institute, University of Pavia, Pavia, Italy
- 18School of Psychology, Social Work and Social Policy, University of South Australia, Magill, SA, Australia
- 19Virtual Reality Medical Institute, Brussels, Belgium
- 20Department of Neurological and Movement Sciences, University of Verona, Verona, Italy
- 21For the full list of authors, please see the section at the end of the article
Background: In order to provide effective care to patients suffering from chronic pain secondary to neurological diseases, health professionals must appraise the role of the psychosocial factors in the genesis and maintenance of this condition whilst considering how emotions and cognitions influence the course of treatment. Furthermore, it is important not only to recognize the psychological reactions to pain that are common to the various conditions, but also to evaluate how these syndromes differ with regards to the psychological factors that may be involved. As an extensive evaluation of these factors is still lacking, the Italian Consensus Conference on Pain in Neurorehabilitation (ICCPN) aimed to collate the evidence available across these topics.
Objectives: To determine the psychological factors which are associated with or predictive of pain secondary to neurological conditions and to assess the influence of these aspects on the outcome of neurorehabilitation.
Methods: Two reviews were performed. In the first, a PUBMED search of the studies assessing the association between psychological factors and pain or the predictive value of these aspects with respect to chronic pain was conducted. The included papers were then rated with regards to their methodological quality and recommendations were made accordingly. In the second study, the same methodology was used to collect the available evidence on the predictive role of psychological factors on the therapeutic response to pain treatments in the setting of neurorehabilitation.
Results: The first literature search identified 1170 results and the final database included 189 articles. Factors such as depression, anxiety, pain catastrophizing, coping strategies, and cognitive functions were found to be associated with pain across the various conditions. However, there are differences between chronic musculoskeletal pain, migraine, neuropathy, and conditions associated with complex disability with regards to the psychological aspects that are involved. The second PUBMED search yielded 252 studies, which were all evaluated. Anxiety, depression, pain catastrophizing, coping strategies, and pain beliefs were found to be associated to different degrees with the outcomes of multidisciplinary programs, surgery, physical therapies, and psychological interventions. Finally, sense of presence was found to be related to the effectiveness of virtual reality as a distraction tool.
Conclusions: Several psychological factors are associated with pain secondary to neurological conditions and should be acknowledged and addressed in order to effectively treat this condition. These factors also predict the therapeutic response to the neurorehabilitative interventions.
Introduction
Within neurorehabilitation programs, knowledge of the psychological factors associated with pain is crucial for its treatment. In fact, the differential impact of various pathologies on the patient as well as the way in which subjective features can affect the course of the disease and the treatment effectiveness are recognized as important factors that should be assessed in order to successfully treat pain conditions (Castelnuovo, 2010a,b, 2013; Cipolletta et al., 2014). What the research clearly highlights is that there is a set of psychological variables that are common to different disorders, but also that each pathology is characterized by some specific psychological issues. In this sense, pathologies that result in the experience of neuropathic pain are similar to pathologies associated with nociceptive pain as regard to anxiety, depression, and cognitions, but different if we consider the subjects' responses to and representations of the disease (Daniel et al., 2008). Several psychological variables may contribute to a better or worse outcome to pain treatment. These issues have a direct influence on the treatment itself. In both cases it is necessary to assess and address concerning changes in mood. However, while patients suffering from chronic musculoskeletal pain should be helped not to avoid movements and exercises that are associated with pain, the treatment of patients suffering from neuropathic pain instead should focus on the management of allodynia, for example.
Methods
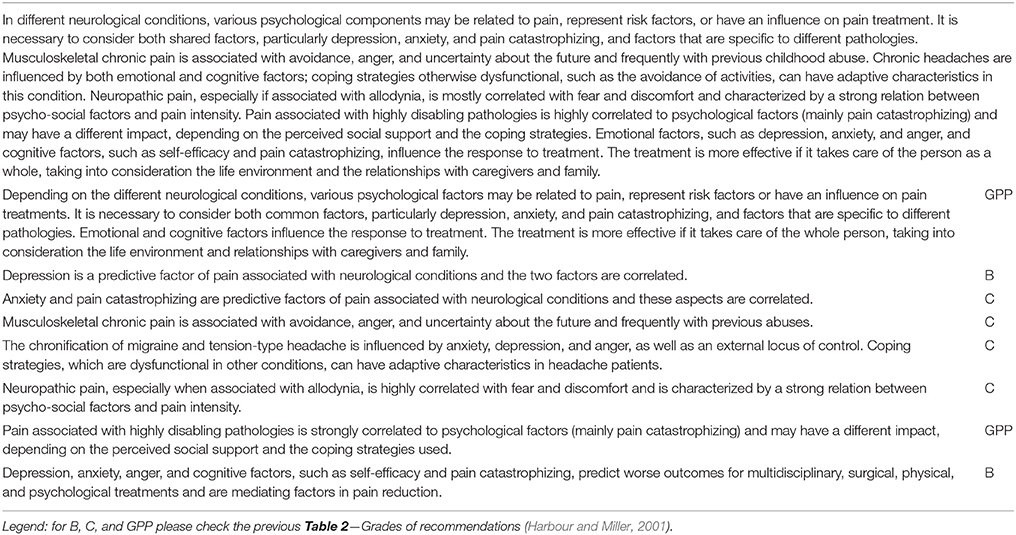
The Italian Consensus Conference on Pain in Neurorehabilitation (ICCPN) is a multidisciplinary board formed in October 2012, aimed at creating the updated guidelines for the treatment of pain in the field of neurorehabilitation (Castelnuovo et al., 2016). A systematic literature review was conducted by the ICCPN, given the importance of psychological factors in the genesis, maintenance, and resolution of pain conditions as well as on the patient's experience of illness. The study was divided in two parts: in the first part we considered the psychological issues associated with pain. We conducted a PubMed search using the keywords: “pain” (restricted to the title), various disorders that are targets of neurorehabilitation (stroke, cerebral palsy, Parkinson's disease, brain injury, multiple sclerosis, post-polio syndrome, Guillain-Barré syndrome, amyotrophic lateral sclerosis, spinal cord injury, concussion, vestibular disorder, neuropathies, neuropathic pain) and a range of psychological variables (depression, anxiety, anger, cognitions, beliefs, catastrophizing, fear avoidance, emotions). The search was conducted in November 2013 and yielded 794 articles. Two upgrades, which were conducted in June 2014 (considering only articles from 2013 to 2014) and in May 2015 (considering articles from 2013 to May 2015), identified, respectively, 169 and 207 more articles. Abstracts or, if necessary, full-text articles were consulted to assess whether studies adhered to the inclusion criteria, namely the presence of at least one psychological factor associated with or predictive of pain in at least one disorder treated in neurorehabilitation services. The final database was composed of 189 articles. The methodological quality of the articles was then evaluated using a checklist specifically created, and assigned a high, medium, or low quality rating. The checklist considered the number of patients included in the study, drop-out rate, risk of bias with regard to the original studies, and the presence of systematic procedures, the comprehensiveness of research and bias risk assessment as regard to the review and meta-analysis. Each article was assigned a level of evidence, on the basis of an adaptation of the SIGN grading system (Table 1) and then recommendations were formulated accordingly (Table 2; Harbour and Miller, 2001).
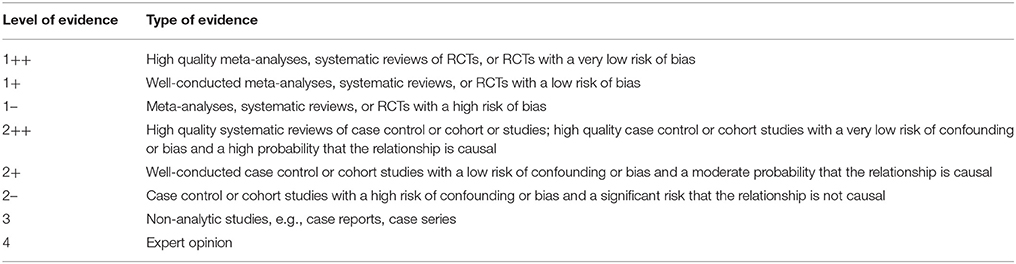
Table 1. Levels of evidence (Harbour and Miller, 2001).
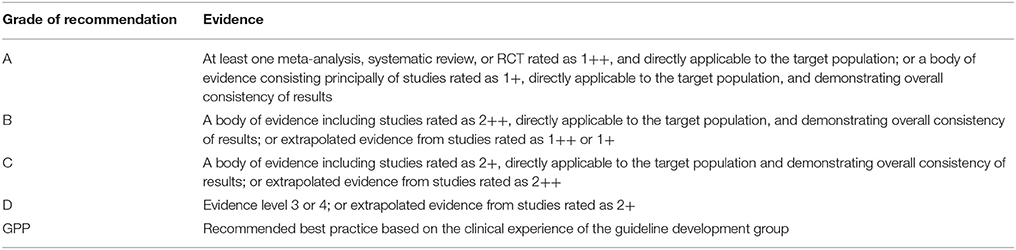
Table 2. Grades of recommendations (Harbour and Miller, 2001).
In the second part we considered the psychological factors predictive of the therapeutic response using the same methodology. We conducted a PubMed search in November 2013, using the terms: “pain” (restricted to the title), the names of various disorders that are treated by neurorehabilitation services, the names of psychological factors and the following terms: moderator, mediator, prognostic factor, impact, predictor, outcome. The search identified 159 articles. An update conducted in May 2015 was restricted to the period from 2013 to 2015 and yielded another 93 articles. All these studies were included and were evaluated with the procedure previously outlined.
Results
As noted before, several psychological factors are commonly associated with pain across different pathologies. Among them, depression has been identified as a crucial factor in a large number of studies. For some disorders, the relationship between depression and pain is correlational, thus it is difficult to identify the direction of the relationship; in other cases, depression can be considered predictive of the occurrence of secondary painful symptoms. Depression is a predictive factor of pain in pathologies such as chronic musculoskeletal pain (Wasserman et al., 2014), multiple sclerosis (Brochet et al., 2009; Harrison et al., 2015), post-stroke pain (O'Donnell et al., 2013), and Parkinson's disease (Wen et al., 2012). A correlation between pain and depression has been highlighted in patients with traumatic brain injuries (Dobscha et al., 2009; Garden and Sullivan, 2010), complex regional pain syndrome (CRPS) type I and II (Lohnberg and Altmaier, 2013; Rewhorn et al., 2014), spinal cord injury (Craig et al., 2013; Avluk et al., 2014; Van Gorp et al., 2015), peripheral diabetic neuropathies (Yoshida et al., 2009; Rekleiti et al., 2013), muscular dystrophies (Alschuler et al., 2012), Parkinson's disease (Zhang et al., 2014; Kass-Iliyya et al., 2015; Mao et al., 2015; Rana et al., 2016), fibromyalgia (Scheidt et al., 2014), and post-herpetic neuralgia (Drolet et al., 2010). Moreover depression is associated with anxiety in patients with headache (Kröner-Herwig et al., 2008; Wieser et al., 2012). The presence of neuropathic components in the pain experienced by the patient correlates with higher values for depressive and anxious symptomatology (Radat et al., 2013; Shaygan et al., 2013; Uher and Bob, 2013); in case of complex conditions the comorbidity with major depressive disorder is high (Proctor et al., 2013). Together with anxiety, alexithymia is also frequently associated with depression (although it can occur without the latter) in influencing the quality of perceived pain, mainly on the affective component and, to a lesser degree, on its sensory component in a relationship mediated by perceived psychological stress (Lumley et al., 2002; Huber et al., 2009; Hosoi et al., 2010). Although it has been studied to a lesser extent compared to depression, anxiety has a high rate of comorbidity with chronic pain conditions and is associated with pain intensity (Ligthart et al., 2013; Radat et al., 2013; Subramaniam et al., 2013). In particular, anxiety is exacerbated by the occurrence of headaches following traumatic brain injuries (Weyer Jamora et al., 2013), predicts chronic musculoskeletal pain following traumas (Castillo et al., 2013), increases in intensity concurrently with post-herpetic neuralgia (Drolet et al., 2010), is associated with diabetic neuropathy (Gore et al., 2005), is correlated with intensity and frequency of headache attacks (Nicholson et al., 2007; Kröner-Herwig et al., 2008) and it is a factor associated with and predicting CRPS (Dilek et al., 2012; Rewhorn et al., 2014) and chronic widespread pain (McBeth et al., 2014). Studies have been conducted on specific aspects of anxiety; in particular, research that has focused on constructs such as anxiety sensitivity (autonomic anxiety linked to the activation of the body) and anxious perception of pain (Wood et al., 2011; Yamaguchi et al., 2013) seems promising. Also, different sets of beliefs are associated with pain in relation to the various disorders that are treated by neurorehabilitation. Among these, pain catastrophizing has been studied in association with different neurological pathologies. In most cases, catastrophic thinking seems predictive of the emergence of painful conditions (Jensen et al., 2011). It is associated with or predicts pain in cerebral palsy (Engel et al., 2013), in lumbar or musculoskeletal pain (Hasenbring et al., 2012; Nakamura et al., 2014), in multiple sclerosis (Osborne et al., 2007; Hirsh et al., 2011; Harrison et al., 2015), in migraine (Radat et al., 2009), in diabetic neuropathy, post-herpetic neuralgia, and post-surgical neuropathic pain (Sullivan et al., 2005), in neuropathic pain due to HIV (Lucey et al., 2011) and in phantom limb pain (Vase et al., 2011). The importance of catastrophizing, in conditions associated with chronic pain, also lies in its mediation effect between the pain intensity and related emotions (Sturgeon et al., 2014). Along with pain catastrophizing, research also identified cognitive variables or maladaptive coping strategies that patients with pain related to neurological diseases tend to use. In particular, self-efficacy is correlated with the presence of pain in the case of stroke (Miller et al., 2013) and mediates the effect of pain on depression in the case of spinal cord injury (Craig et al., 2013). With regard to the coping strategies, both the tendency to avoid moving the painful part in an attempt to prevent increase in pain and the tendency to excessively exercise it are associated with a worse adaptation to the condition (Engel et al., 2000; Jensen et al., 2011; Andrews et al., 2012). A final note on factors associated with pain concerns the bidirectional relationship with the cognitive functions. Different lines of evidence underline the association between the two factors: patients that report chronic pain have lower scores in attentional and learning skills, delayed recall, reaction times, prospective memory, psychomotor skills, recognition of mental and emotional states, and executive functions (Hart et al., 2000; Jongsma et al., 2011; Moriarty et al., 2011; Beaupré et al., 2012; Shin et al., 2013; Miller and Radford, 2014; Zhang et al., 2014). However, it should be noted that a) there are differences between different diseases, b) not all studies have found these associations, c) factors linking pain and cognitive decline are still unclear, d) the direction of the cause-effect relationship is still unclear (Apkarian et al., 2004, 2005, 2013; Berger et al., 2014), e) results can be partly explained by comorbidity with other disorders or the use of drugs, in particular antidepressants (Moriarty et al., 2011; Pickering et al., 2014). Recent evidence indicates that lower scores on cognitive tests may represent a risk factor for the occurrence of post-operative pain and may predict its intensity and the presence of neuropathic components (Attal et al., 2014). As noted earlier, along with the factors that seem to be associated with pain in most diseases, the variables that differentiate between various diseases should be considered. In general, depending on psychological variables involved, the following macro-categories of diseases can be identified: chronic musculoskeletal pain, headache, neuropathic pain, conditions associated with complex and highly disabling pathologies. Musculoskeletal chronic pain conditions are often associated with high levels of depression, and uncertainty regarding the diagnosis and prognosis of the disorder (Daniel et al., 2008), avoidance of activities and exercise (Andrews et al., 2012), and anger (Fernandez and Turk, 1995). Despite being considered a musculoskeletal chronic pain, fibromyalgia has peculiar features, since it is accompanied with even more markedly depressive episodes, and the perceived pain, which is generally more intense compared to other musculoskeletal disorders, has long been considered to overlap with neuropathic pain (Koroschetz et al., 2011; Scheidt et al., 2014). Several studies report a high incidence of physical, emotional and sexual abuses among patients suffering from different forms of musculoskeletal chronic pain (Bailey et al., 2003; Kosseva et al., 2010), which may be associated with post-traumatic symptoms (Ruiz-Párraga and Lopez-Martinez, 2013). Two clarifications are necessary: on the one hand, the presence of previous abuse does not reduce the probability that psychotherapy will be effective (Bailey et al., 2003); on the other hand, the profile of patients suffering from musculoskeletal chronic pain is extremely variable and knowledge of the psychological factors associated with these diseases does not replace the need to assess the individual circumstances of the patient and provide personalized treatment. Research aimed at subgrouping patients according to their psychological characteristics and the risk of pain chronification is still in progress (Hasenbring et al., 2012). Psychological factors associated with migraine and tension-type headache should be considered separately from those of other disorders because the underlying mechanisms are different. Researchers have focused mainly on the association between intensity and frequency of headache attacks and anxiety, depression and anger, as well as on cognitions, attributions and coping styles (Nicholson et al., 2007). In particular, an external locus of control (perception of not having control over the headache) together with high levels of anxiety, depression and pain catastrophizing are associated with a higher probability of chronification of attacks (Radat et al., 2009). Contrary to musculoskeletal pain, dysfunctional coping strategies such as avoidance of social activities, are not always associated with worsening of the patient's condition (Wieser et al., 2012). Neuropathic pain conditions are characterized by discomfort due to pain intensity and allodynia. In this condition, pain avoidance appears as fear of the painful sensation itself and the perception of dangerousness of different activities thereby leading to social withdrawal. This is in contrast to the fear of pain associated with movement which is typical of CRPS and causes increased irritability (Rommel et al., 2005; de Jong et al., 2011). Treatments must address these issues and consider that neuropathic pain is characterized by a significant association between psychosocial factors and pain intensity (Yoshida et al., 2009; Hirsh et al., 2010; Vase et al., 2011). Highly disabling pathologies, such as lateral amyotrophic sclerosis, multiple sclerosis and muscular dystrophies, are also frequently associated with pain. Central and peripheral pain components weave together and strengthen mutually (Seifert et al., 2013). These pathologies are hard to manage and the related pain condition can be associated with higher levels of fatigue and depression, which together significantly affect patients' quality of life (Pagnini et al., 2012; Fernández-de-Las-Peñas et al., 2014; Amtmann et al., 2015). A recent literature review underlined that psychosocial variables, in particular pain catastrophizing, may have medium to great effects on the level of psychological and physical functioning and on the intensity of perceived pain (Jensen et al., 2011). Also, the social support perceived by the patient, and some coping strategies have a core role in the experience of pain: task persistence (the ability to persist in performing hard and effort-requiring actions) can decrease its influence while the tendency to rest and stay alert after painful sensations increases it. The importance of the psychosocial factors listed above is not only based on their direct impact on pain but also on their influence on the therapeutic response to various interventions. The effectiveness of pharmacological treatments, surgery and psychotherapy is mediated by subjective characteristics that may predict worse (or better) outcome. The psychological predictors of the therapeutic response studied so far are both emotional, such as anxiety and depression, and cognitive, in particular pain catastrophizing, coping strategies and beliefs regarding the disease. There is evidence on the role of emotional factors in pain outcomes. Several studies documented the role of depression in influencing outcome of treatments for chronic pain conditions through multidisciplinary programs (Hill et al., 2007; Glombiewski et al., 2010; Miles et al., 2011; Morlion et al., 2011; de Rooij et al., 2013) and in spinal and orthopedic surgeries (Arpino et al., 2004; Celestin et al., 2009; Judge et al., 2012). The role of anxiety in multidisciplinary therapies (McCracken et al., 2002; Flink et al., 2010), physical therapies (Hill et al., 2007) and spinal and orthopedic surgeries (Celestin et al., 2009; D'Angelo et al., 2010; Judge et al., 2012), and that of anger suppression in chronic pain treatment (Burns et al., 1998) have also been demonstrated. Different cognitive factors seem also to have a crucial role, in particular pain catastrophizing in multidisciplinary (Smeets et al., 2006; Vowles et al., 2007; Desrochers et al., 2010; Heutink et al., 2013; Litt and Porto, 2013) and pharmacological treatments (Toth et al., 2014), cognitive flexibility in psychotherapy (Wicksell et al., 2010, 2013), acceptance in multidisciplinary programs and psychotherapy (Vowles et al., 2007; Samwel et al., 2009; Day et al., 2014), self-efficacy in multidisciplinary programs (Kores et al., 1990; Buckelew et al., 1996; Turner et al., 2007; Miles et al., 2011) and in the prognosis of tension-type headache (Holroyd et al., 2009), stress in Internet-based cognitive-behavioral therapies (DasMahapatra et al., 2015), dysfunctional coping strategies in spinal surgeries (Gross, 1986) and multidisciplinary interventions (Nicassio et al., 1997; Rhee et al., 2000; Nielson and Jensen, 2004; Hechler et al., 2010), expectations on the result of the therapies or on the course of the disease in psychotherapies or in multidisciplinary programs (Goossens et al., 2005; Milling et al., 2006, 2007; Galli et al., 2010; Bostick et al., 2015) and in headache treatment (Goldstein et al., 2011), and fear of movement in treatments for musculoskeletal chronic pain (den Boer et al., 2006). It should be underlined that not all the studies agree on the association between these factors and the outcomes and that it is not possible to exclude the presence of publication bias. Moreover, although these studies demonstrate that the conditions pre-existing before treatment may have an influence on the result or that a change of the considered variables is associated with a change in the outcome, a cause-effect relationship between the groups of variables cannot be assumed. Finally, although there is evidence that changes in levels of pain catastrophizing, anxiety and helplessness related to pain can enhance treatment outcomes, it is still unclear whether changes in cognitions correspond to better outcomes (Burns et al., 2003a,b). In relation to the use of virtual reality as a distraction technology a recent systematic review (Triberti et al., 2014) underlined the importance of different psychological factors in the effectiveness of the analgesic distraction. While sense of presence (Riva and Mantovani, 2012; Villani et al., 2012) influence the effectiveness of VR as a distraction tool, anxiety as well as positive emotions directly affect the experience of pain.
Further, issues that need to be considered among the factors that influence the results of treatment results include, on one hand, the core role of professionals, their listening, and communication skills, which are fundamental to maximize both treatment compliance and the therapeutic alliance (Butow and Sharpe, 2013; Farin et al., 2013; Raichle et al., 2014), and, on the other hand, the features of the context in which the patient lives, including the social and work situation and the perceived support received from their own family (Jamison and Virts, 1990; Becker et al., 1998). Further, studies are necessary to reach firm conclusions on the mediating role of these factors and to understand which factors can be seen as contraindications for specific treatments. As previously noted, the treatment for these pain conditions should be aimed at taking care of the individual in the context of their relationships in a wholistic sense, as opposed to simply intervening at a symptom-level. Each of the factors listed above must be seen in the context of their interaction with the person's living environment. Caregivers' responses to the disease can be significantly influenced by the presence of anxiety and depression (Ennis et al., 2013) and, as noted by Syed Hassan et al. (2013), their condition may be particularly distressing because of the need to cope with their own difficulties in the context of providing potentially exhausting care to the named patient. For this purpose, educational interventions have been designed to give patients and caregivers necessary information regarding the characteristics of the pathologies and treatment options, and providing details on potential positive effects on variables related to the family functioning and patient behavior (Daviet et al., 2012).
Conclusions
In conclusion, it is clear that an effective pain treatment in neurorehabilitation must consider both the specific and non-specific psychological factors of various diseases, including the environment in which the person lives and relationships with caregivers and family (see Table 3).
The Italian Consensus Conference on Pain in Neurorehabilitation
The following Authors, who are listed in alphabetical order, contributed to the work of the Italian Consensus Conference on Pain in Neurorehabilitation:
Michela Agostini, Neurorehabilitation Department, Foundation IRCCS San Camillo Hospital, Venice, Italy; Enrico Alfonsi, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy; Anna Maria Aloisi, Department of Medicine, Surgery and Neuroscience, University of Siena, Siena, Italy; Elena Alvisi, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Irene Aprile, Don Gnocchi Foundation, Milan, Italy; Michela Armando, Department of Neuroscience and Neurorehabilitation, Bambin Gesu' Children's Hospital, IRCCS, Rome, Italy; Micol Avenali, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Eva Azicnuda, IRCCS Santa Lucia Foundation, Rome, Italy; Francesco Barale, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Michelangelo Bartolo, Neurorehabilitation Unit, IRCCS INM Neuromed, Pozzilli, Italy; Roberto Bergamaschi, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy; Mariangela Berlangieri, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Vanna Berlincioni, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Laura Berliocchi, Department of Health Sciences, University Magna Graecia of Catanzaro, Catanzaro, Italy; Eliana Berra, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy; Giulia Berto, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Silvia Bonadiman, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Sara Bonazza, Department of Surgery, University of Verona, Verona, Italy; Federica Bressi, Campus Biomedico University, Rome, Italy; Annalisa Brugnera, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Stefano Brunelli, IRCCS Santa Lucia Foundation, Rome, Italy; Maria Gabriella Buzzi, IRCCS Santa Lucia Foundation, Rome, Italy; Carlo Cacciatori, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Andrea Calvo, Rita Levi Montalcini Department of Neuroscience, University of Turin, Turin, Italy; Cristina Cantarella, Physical and Rehabilitation Medicine Unit, Tor Vergata University, Rome, Italy; Augusto Caraceni, Palliative Care, Pain Therapy and Rehabilitation, Fondazione IRCCS Istituto Nazionale dei Tumori di Milano, Milan, Italy; Roberto Carone, Neuro- Urology Department, City Hospital Health and Science of the City of Turin, Turin, Italy; Elena Carraro, Neuropediatric Rehabilitation Unit, E. Medea Scientific Institute, Conegliano, Italy; Roberto Casale, Department of Clinical Neurophysiology and Pain Rehabilitation Unit, Foundation Salvatore Maugeri IRCCS, Montescano, Italy; Paola Castellazzi, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Gianluca Castelnuovo, Psychology Research Laboratory, Istituto Auxologico Italiano IRCCS, Ospedale San Giuseppe, Verbania, Italy, Department of Psychology, Catholic University of Milan, Italy; Adele Castino, ASL of the Province of Lodi, Lodi, Italy; Rosanna Cerbo, Hub Terapia del Dolore Regione Lazio, Policlinico Umberto I, Sapienza University, Rome Italy; Adriano Chiò, Rita Levi Montalcini Department of Neuroscience, University of Turin, Turin, Italy; Cristina Ciotti, Physical and Rehabilitation Medicine Unit, Tor Vergata University, Rome, Italy; Carlo Cisari, Department of Health Sciences, Università del Piemonte Orientale, Novara, Italy; Daniele Coraci, Department of Orthopaedic Science, Sapienza University, Rome, Italy; Elena Dalla Toffola, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, IRCCS Policlinico San Matteo Foundation, Pavia; Giovanni Defazio, Department of Basic Medical Sciences, Neuroscience and Sensory Organs, Aldo Moro University of Bari, Bari, Italy; Roberto De Icco, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Ubaldo Del Carro, Section of Clinical Neurophysiology and Neurorehabilitation, San Raffaele Hospital, Milan, Italy; Andrea Dell'Isola, Department of Health Sciences, Università del Piemonte Orientale, Novara, Italy; Antonio De Tanti, Cardinal Ferrari Rehabilitation Center, Santo Stefano Rehabilitation Institute, Fontanellato, Italy; Mariagrazia D'Ippolito, IRCCS Santa Lucia Foundation, Rome, Italy; Elisa Fazzi, Childhood and Adolescence Neurology and Psychiatry Unit, City Hospital, Brescia, Italy, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy; Adriano Ferrari, Children Rehabilitation Unit, IRCCS Arcispedale S.Maria Nuova, Reggio Emilia, Italy; Sergio Ferrari, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Francesco Ferraro, Section of Neuromotor Rehabilitation, Department of Neuroscience, Azienda Ospedaliera Carlo Poma, Mantova, Italy; Fabio Formaglio, Palliative Care, Pain Therapy and Rehabilitation, Fondazione IRCCS Istituto Nazionale dei Tumori di Milano, Milan, Italy; Rita Formisano, IRCCS Santa Lucia Foundation, Rome, Italy; Simone Franzoni, Poliambulanza Foundation Istituto Ospedaliero, Geriatric Research Group, Brescia, Italy; Francesca Gajofatto, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Marialuisa Gandolfi, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Barbara Gardella, IRCCS Policlinico San Matteo Foundation, Pavia; Pierangelo Geppetti, Department of Health Sciences, Section of Clinical Pharmacology and Oncology, University of Florence, Florence, Italy; Alessandro Giammò, Neuro-Urology Department, City Hospital Health and Science of the City of Turin, Turin, Italy; Raffaele Gimigliano, Department of Physical and Mental Health, Second University of Naples, Naples, Italy; Emanuele Maria Giusti, Department of Psychology, Catholic University of Milan, Italy; Elena Greco, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Valentina Ieraci, Department of Oncology and Neuroscience, University of Turin, City Hospital Health and Science of the City of Turin, Turin, Turin, Italy; Marco Invernizzi, Department of Health Sciences, Università del Piemonte Orientale, Novara, Italy; Marco Jacopetti, University of Parma, Parma, Italy; Marco Lacerenza, Casa di Cura San Pio X S.r.l., HUMANITAS, Milan, Italy; Silvia La Cesa, Department of Neurology and Psychiatry, University Sapienza, Rome, Italy; Davide Lobba, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Gian Mauro Manzoni, Psychology Research Laboratory, Istituto Auxologico Italiano IRCCS, Ospedale San Giuseppe, Verbania, Italy, Department of Psychology, Catholic University of Milan, Italy; Francesca Magrinelli, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Silvia Mandrini, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy; Umberto Manera, Rita Levi Montalcini Department of Neuroscience, University of Turin, Turin, Italy; Paolo Marchettini, Pain Medicine Center, Hospital San Raffaele, Milan, Italy; Enrico Marchioni, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy; Sara Mariotto, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Andrea Martinuzzi, Neuropediatric Rehabilitation Unit, E. Medea Scientific Institute, Conegliano, Italy; Marella Masciullo, IRCCS Santa Lucia Foundation, Rome, Italy; Susanna Mezzarobba, Department of Medicine, Surgery and Health Sciences, University of Trieste, Trieste, Italy; Danilo Miotti, Palliative Care and Pain Therapy Unit, Fondazione Salvatore Maugeri IRCCS, Scientific Institute of Pavia, Pavia, Italy; Angela Modenese, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Marco Molinari, IRCCS Santa Lucia Foundation, Rome, Italy; Salvatore Monaco, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Giovanni Morone, IRCCS Santa Lucia Foundation, Rome, Italy; Rossella Nappi, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy, IRCCS Policlinico San Matteo Foundation, Pavia; Stefano Negrini, Don Gnocchi Foundation, Milan, Italy, Department of Clinical and Experimental Sciences, University of Brescia, Brescia, Italy; Andrea Pace, Neuro-Oncology Unit, Regina Elena National Cancer Institute of Rome, Rome, Italy; Luca Padua, Don Gnocchi Foundation, Milan, Italy, Institute of Neurology, Catholic University, Rome, Italy; Emanuela Pagliano, Developmental Neurology Unit, C. Besta Neurological Institute Foundation, Milan, Italy; Valerio Palmerini, Hub Terapia del Dolore Regione Lazio, Policlinico Umberto I, Sapienza University, Rome Italy; Stefano Paolucci, IRCCS Santa Lucia Foundation, Rome, Italy; Costanza Pazzaglia, Don Gnocchi Foundation, Milan, Italy; Cristiano Pecchioli, Don Gnocchi Foundation, Milan, Italy; Alessandro Picelli, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Carlo Adolfo Porro, Department of Biomedical, Metabolic and Neural Sciences, University of Modena and Reggio Emilia, Modena, Italy; Daniele Porru, IRCCS Policlinico San Matteo Foundation, Pavia; Marcello Romano, Neurology Unit, Azienda Ospedaliera Ospedali Riuniti Villa Sofia Cervello, Palermo, Italy; Laura Roncari, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Riccardo Rosa, Hub Terapia del Dolore Regione Lazio, Policlinico Umberto I, Sapienza University, Rome Italy; Marsilio Saccavini, ASL 2 Bassa Friulana-Isontina, Italy; Paola Sacerdote, Department of Pharmacological and Biomolecular Sciences, University of Milano, Milano, Italy; Giorgio Sandrini, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Donatella Saviola, Cardinal Ferrari Rehabilitation Center, Santo Stefano Rehabilitation Institute, Fontanellato, Italy; Angelo Schenone, Department of Neuroscience, Rehabilitation, Ophthalmology, Genetics, Maternal and Child Health (DiNOGMI), University of Genoa, Genoa, Italy; Vittorio Schweiger, Department of Surgery, University of Verona, Verona, Italy; Giorgio Scivoletto, IRCCS Santa Lucia Foundation, Rome, Italy; Nicola Smania, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Claudio Solaro, Neurology Unit, ASL3, Genoa, Italy; Vincenza Spallone, Department of Systems Medicine, University Tor Vergata, Rome, Italy; Isabella Springhetti, Functional Recovery and Rehabilitation Unit, IRCCS Fondazione S. Maugeri, Pavia, Italy; Stefano Tamburin, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Cristina Tassorelli, C. Mondino National Institute of Neurology Foundation, IRCCS, Pavia, Italy, Department of Brain and Behavioural Sciences, University of Pavia, Pavia, Italy; Michele Tinazzi, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Rossella Togni, Department of Clinical, Surgical, Diagnostic and Pediatric Sciences, University of Pavia, Pavia, Italy; Monica Torre, IRCCS Santa Lucia Foundation, Rome, Italy; Riccardo Torta, Department of Oncology and Neuroscience, University of Turin, City Hospital Health and Science of the City of Turin, Turin, Turin, Italy; Marco Traballesi, IRCCS Santa Lucia Foundation, Rome, Italy; Marco Tramontano, IRCCS Santa Lucia Foundation, Rome, Italy; Andrea Truini, Department of Neurology and Psychiatry, University Sapienza, Rome, Italy; Valeria Tugnoli, Neurological Unit, University Hospital of Ferrara, Ferrara, Italy; Andrea Turolla, Neurorehabilitation Department, Foundation IRCCS San Camillo Hospital, Venice, Italy; Gabriella Vallies, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Elisabetta Verzini, Department of Neurological and Movement Sciences, University of Verona, Verona, Italy; Mario Vottero, Neuro-Urology Department, City Hospital Health and Science of the City of Turin, Turin, Italy; Paolo Zerbinati, Neuro- orthopaedic Program, Hand Surgery Department, Santa Maria Hospital MultiMedica, Castellanza, Italy.
Author Contributions
All authors listed, have made substantial, direct and intellectual contribution to the work, and approved it for publication.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Alschuler, K. N., Jensen, M. P., Goetz, M. C., Smith, A. E., Verrall, A. M., and Molton, I. R. (2012). Effects of pain and fatigue on physical functioning and depression in persons with muscular dystrophy. Disabil. Health J. 5, 277–283. doi: 10.1016/j.dhjo.2012.07.002
Amtmann, D., Askew, R. L., Kim, J., Chung, H., Ehde, D. M., Bombardier, C. H., et al. (2015). Pain affects depression through anxiety, fatigue, and sleep in multiple sclerosis. Rehabil. Psychol. 60, 81–90. doi: 10.1037/rep0000027
Andrews, N. E., Strong, J., and Meredith, P. J. (2012). Activity pacing, avoidance, endurance, and associations with patient functioning in chronic pain: a systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 93, 2109–2121 e2107. doi: 10.1016/j.apmr.2012.05.029
Apkarian, A. V., Baliki, M. N., and Farmer, M. A. (2013). Predicting transition to chronic pain. Curr. Opin. Neurol. 26, 360–367. doi: 10.1097/WCO.0b013e32836336ad
Apkarian, A. V., Bushnell, M. C., Treede, R. D., and Zubieta, J. K. (2005). Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain 9, 463–484. doi: 10.1016/j.ejpain.2004.11.001
Apkarian, A. V., Sosa, Y., Krauss, B. R., Thomas, P. S., Fredrickson, B. E., Levy, R. E., et al. (2004). Chronic pain patients are impaired on an emotional decision-making task. Pain 108, 129–136. doi: 10.1016/j.pain.2003.12.015
Arpino, L., Iavarone, A., Parlato, C., and Moraci, A. (2004). Prognostic role of depression after lumbar disc surgery. Neurol. Sci. 25, 145–147. doi: 10.1007/s10072-004-0248-x
Attal, N., Masselin-Dubois, A., Martinez, V., Jayr, C., Albi, A., Fermanian, J., et al. (2014). Does cognitive functioning predict chronic pain? Results from a prospective surgical cohort. Brain 137(Pt 3), 904–917. doi: 10.1093/brain/awt354
Avluk, O. C., Gurcay, E., Gurcay, A. G., Karaahmet, O. Z., Tamkan, U., and Cakci, A. (2014). Effects of chronic pain on function, depression, and sleep among patients with traumatic spinal cord injury. Ann. Saudi. Med. 34, 211–216. doi: 10.5144/0256-4947.2014.211
Bailey, B. E., Freedenfeld, R. N., Kiser, R. S., and Gatchel, R. J. (2003). Lifetime physical and sexual abuse in chronic pain patients: psychosocial correlates and treatment outcomes. Disabil. Rehabil. 25, 331–342. doi: 10.1080/0963828021000056866
Beaupré, M., De Guise, E., and McKerral, M. (2012). The association between pain-related variables, emotional factors, and attentional functioning following mild traumatic brain injury. Rehabil. Res. Pract. 2012:924692. doi: 10.1155/2012/924692
Becker, N., Højsted, J., Sjogren, P., and Eriksen, J. (1998). Sociodemographic predictors of treatment outcome in chronic non-malignant pain patients. Do patients receiving or applying for disability pension benefit from multidisciplinary pain treatment? Pain 77, 279–287. doi: 10.1016/S0304-3959(98)00105-5
Berger, S. E., Baria, A. T., Baliki, M. N., Mansour, A., Herrmann, K. M., Torbey, S., et al. (2014). Risky monetary behavior in chronic back pain is associated with altered modular connectivity of the nucleus accumbens. BMC Res. Notes 7:739. doi: 10.1186/1756-0500-7-739
Bostick, G. P., Toth, C., Dick, B. D., Carr, E. C., Stitt, L. W., and Moulin, D. E. (2015). An adaptive role for negative expected pain in patients with neuropathic pain. Clin. J. Pain 31, 438–443. doi: 10.1097/AJP.0000000000000135
Brochet, B., Deloire, M. S., Ouallet, J. C., Salort, E., Bonnet, M., Jové, J., et al. (2009). Pain and quality of life in the early stages after multiple sclerosis diagnosis: a 2-year longitudinal study. Clin. J. Pain 25, 211–217. doi: 10.1097/AJP.0b013e3181891347
Buckelew, S. P., Huyser, B., Hewett, J. E., Parker, J. C., Johnson, J. C., Conway, R., et al. (1996). Self-efficacy predicting outcome among fibromyalgia subjects. Arthritis Care Res. 9, 97–104.
Burns, J. W., Glenn, B., Bruehl, S., Harden, R. N., and Lofland, K. (2003a). Cognitive factors influence outcome following multidisciplinary chronic pain treatment: a replication and extension of a cross-lagged panel analysis. Behav. Res. Ther. 41, 1163–1182. doi: 10.1016/S0005-7967(03)00029-9
Burns, J. W., Johnson, B. J., Devine, J., Mahoney, N., and Pawl, R. (1998). Anger management style and the prediction of treatment outcome among male and female chronic pain patients. Behav. Res. Ther. 36, 1051–1062. doi: 10.1016/S0005-7967(98)00080-1
Burns, J. W., Kubilus, A., Bruehl, S., Harden, R. N., and Lofland, K. (2003b). Do changes in cognitive factors influence outcome following multidisciplinary treatment for chronic pain? A cross-lagged panel analysis. J. Consult. Clin. Psychol. 71, 81–91. doi: 10.1037/0022-006X.71.1.81
Butow, P., and Sharpe, L. (2013). The impact of communication on adherence in pain management. Pain 154(Suppl. 1), S101–107. doi: 10.1016/j.pain.2013.07.048
Castelnuovo, G. (2010a). Empirically supported treatments in psychotherapy: towards an evidence-based or evidence-biased psychology in clinical settings? Front. Psychol. 1:27. doi: 10.3389/fpsyg.2010.00027
Castelnuovo, G. (2010b). No medicine without psychology: the key role of psychological contribution in clinical settings. Front. Psychol. 1:4. doi: 10.3389/fpsyg.2010.00004
Castelnuovo, G. (2013). Good communication and outcome after anaesthesia. Anaesthesia 68, 1203–1204. doi: 10.1111/anae.12469
Castelnuovo, G., Giusti, E., Manzoni, G. M., Saviola, D., Gatti, A., Gabrielli, S., et al. (2016). Psychological treatments and psychotherapies in the neurorehabilitation of pain: evidences and recommendations from the Italian Consensus Conference on Pain in Neurorehabilitation. Front. Psychol. 7:115. doi: 10.3389/fpsyg.2016.00115
Castillo, R. C., Wegener, S. T., Heins, S. E., Haythornthwaite, J. A., Mackenzie, E. J., Bosse, M. J., et al. (2013). Longitudinal relationships between anxiety, depression, and pain: results from a two-year cohort study of lower extremity trauma patients. Pain 154, 2860–2866. doi: 10.1016/j.pain.2013.08.025
Celestin, J., Edwards, R. R., and Jamison, R. N. (2009). Pretreatment psychosocial variables as predictors of outcomes following lumbar surgery and spinal cord stimulation: a systematic review and literature synthesis. Pain Med. 10, 639–653. doi: 10.1111/j.1526-4637.2009.00632.x
Cipolletta, S., Consolaro, F., and Horvath, P. (2014). When health is an attitudinal matter. A qualitative research. J. Humanist. Psychol. 54, 391–413. doi: 10.1177/0022167813507630
Craig, A., Tran, Y., Siddall, P., Wijesuriya, N., Lovas, J., Bartrop, R., et al. (2013). Developing a model of associations between chronic pain, depressive mood, chronic fatigue, and self-efficacy in people with spinal cord injury. J. Pain 14, 911–920. doi: 10.1016/j.jpain.2013.03.002
D'Angelo, C., Mirijello, A., Ferrulli, A., Leggio, L., Berardi, A., Icolaro, N., et al. (2010). Role of trait anxiety in persistent radicular pain after surgery for lumbar disc herniation: a 1-year longitudinal study. Neurosurgery 67, 265–271. doi: 10.1227/01.NEU.0000371971.51755.1C
Daniel, H. C., Narewska, J., Serpell, M., Hoggart, B., Johnson, R., and Rice, A. S. (2008). Comparison of psychological and physical function in neuropathic pain and nociceptive pain: implications for cognitive behavioral pain management programs. Eur. J. Pain 12, 731–741. doi: 10.1016/j.ejpain.2007.11.006
DasMahapatra, P., Chiauzzi, E., Pujol, L. M., Los, C., and Trudeau, K. J. (2015). Mediators and moderators of chronic pain outcomes in an online self-management program. Clin. J. Pain 31, 404–413. doi: 10.1097/AJP.0000000000000125
Daviet, J. C., Bonan, I., Caire, J. M., Colle, F., Damamme, L., Froger, J., et al. (2012). Therapeutic patient education for stroke survivors: non-pharmacological management. A literature review. Ann. Phys. Rehabil. Med. 55, 641–656. doi: 10.1016/j.rehab.2012.08.011
Day, M. A., Thorn, B. E., and Rubin, N. J. (2014). Mindfulness-based cognitive therapy for the treatment of headache pain: a mixed-methods analysis comparing treatment responders and treatment non-responders. Complement. Ther. Med. 22, 278–285. doi: 10.1016/j.ctim.2013.12.018
de Jong, J. R., Vlaeyen, J. W., de Gelder, J. M., and Patijn, J. (2011). Pain-related fear, perceived harmfulness of activities, and functional limitations in complex regional pain syndrome type I. J. Pain 12, 1209–1218. doi: 10.1016/j.jpain.2011.06.010
den Boer, J. J., Oostendorp, R. A., Beems, T., Munneke, M., and Evers, A. W. (2006). Continued disability and pain after lumbar disc surgery: the role of cognitive-behavioral factors. Pain 123, 45–52. doi: 10.1016/j.pain.2006.02.008
de Rooij, A., Roorda, L. D., Otten, R. H., van der Leeden, M., Dekker, J., and Steultjens, M. P. (2013). Predictors of multidisciplinary treatment outcome in fibromyalgia:a systematic review. Disabil. Rehabil. 35, 437–449. doi: 10.3109/09638288.2012.699582
Desrochers, G., Bergeron, S., Khalifé, S., Dupuis, M. J., and Jodoin, M. (2010). Provoked vestibulodynia: psychological predictors of topical and cognitive-behavioral treatment outcome. Behav. Res. Ther. 48, 106–115. doi: 10.1016/j.brat.2009.09.014
Dilek, B., Yemez, B., Kizil, R., Kartal, E., Gulbahar, S., Sari, O., et al. (2012). Anxious personality is a risk factor for developing complex regional pain syndrome type I. Rheumatol. Int. 32, 915–920. doi: 10.1007/s00296-010-1714-9
Dobscha, S. K., Clark, M. E., Morasco, B. J., Freeman, M., Campbell, R., and Helfand, M. (2009). Systematic review of the literature on pain in patients with polytrauma including traumatic brain injury. Pain Med. 10, 1200–1217. doi: 10.1111/j.1526-4637.2009.00721.x
Drolet, M., Brisson, M., Schmader, K. E., Levin, M. J., Johnson, R., Oxman, M. N., et al. (2010). The impact of herpes zoster and postherpetic neuralgia on health-related quality of life: a prospective study. CMAJ 182, 1731–1736. doi: 10.1503/cmaj.091711
Engel, J. M., Schwartz, L., Jensen, M. P., and Johnson, D. R. (2000). Pain in cerebral palsy: the relation of coping strategies to adjustment. Pain 88, 225–230. doi: 10.1016/S0304-3959(00)00330-4
Engel, J. M., Wilson, S., Tran, S. T., Jensen, M. P., and Ciol, M. A. (2013). Pain catastrophizing in youths with physical disabilities and chronic pain. J. Pediatr. Psychol. 38, 192–201. doi: 10.1093/jpepsy/jss103
Ennis, N., Rosenbloom, B. N., Canzian, S., and Topolovec-Vranic, J. (2013). Depression and anxiety in parent versus spouse caregivers of adult patients with traumatic brain injury: a systematic review. Neuropsychol. Rehabil. 23, 1–18. doi: 10.1080/09602011.2012.712871
Farin, E., Gramm, L., and Schmidt, E. (2013). The patient-physician relationship in patients with chronic low back pain as a predictor of outcomes after rehabilitation. J. Behav. Med. 36, 246–258. doi: 10.1007/s10865-012-9419-z
Fernandez, E., and Turk, D. C. (1995). The scope and significance of anger in the experience of chronic pain. Pain 61, 165–175. doi: 10.1016/0304-3959(95)00192-U
Fernández-de-Las-Peñas, C., Ortega-Santiago, R., Ortíz-Gutiérrez, R., Caminero, A. B., Salom-Moreno, J., and Arendt-Nielsen, L. (2014). Widespread pressure pain hypersensitivity in patients with multiple sclerosis with and without pain as sign of central sensitization. Clin. J. Pain 31, 66–72. doi: 10.1097/AJP.0000000000000084
Flink, I. K., Boersma, K., and Linton, S. J. (2010). Catastrophizing moderates the effect of exposure in vivo for back pain patients with pain-related fear. Eur. J. Pain 14, 887–892. doi: 10.1016/j.ejpain.2010.02.003
Galli, U., Ettlin, D. A., Palla, S., Ehlert, U., and Gaab, J. (2010). Do illness perceptions predict pain-related disability and mood in chronic orofacial pain patients? A 6-month follow-up study. Eur. J. Pain 14, 550–558. doi: 10.1016/j.ejpain.2009.08.011
Garden, N., and Sullivan, K. A. (2010). An examination of the base rates of post-concussion symptoms: the influence of demographics and depression. Appl. Neuropsychol. 17, 1–7. doi: 10.1080/09084280903297495
Glombiewski, J. A., Hartwich-Tersek, J., and Rief, W. (2010). Depression in chronic back pain patients: prediction of pain intensity and pain disability in cognitive-behavioral treatment. Psychosomatics 51, 130–136. doi: 10.1176/appi.psy.51.2.130
Goldstein, L. H., Seed, P. T., Clark, L. V., Dowson, A. J., Jenkins, L. M., and Ridsdale, L. (2011). Predictors of outcome in patients consulting their general practitioners for headache: a prospective study. Psychol. Health 26, 751–764. doi: 10.1080/08870446.2010.493217
Goossens, M. E., Vlaeyen, J. W., Hidding, A., Kole-Snijders, A., and Evers, S. M. (2005). Treatment expectancy affects the outcome of cognitive-behavioral interventions in chronic pain. Clin. J. Pain 21, 18–26. doi: 10.1097/00002508-200501000-00003
Gore, M., Brandenburg, N. A., Dukes, E., Hoffman, D. L., Tai, K. S., and Stacey, B. (2005). Pain severity in diabetic peripheral neuropathy is associated with patient functioning, symptom levels of anxiety and depression, and sleep. J. Pain Symptom Manage. 30, 374–385. doi: 10.1016/j.jpainsymman.2005.04.009
Gross, A. R. (1986). The effect of coping strategies on the relief of pain following surgical intervention for lower back pain. Psychosom. Med. 48, 229–241. doi: 10.1097/00006842-198603000-00008
Harbour, R., and Miller, J. (2001). A new system for grading recommendations in evidence based guidelines. BMJ 323, 334–336. doi: 10.1136/bmj.323.7308.334
Harrison, A. M., Silber, E., Mccracken, L. M., and Moss-Morris, R. (2015). Beyond a physical symptom: the importance of psychosocial factors in multiple sclerosis pain. Eur. J. Neurol. 22, 1443–1452. doi: 10.1111/ene.12763
Hart, R. P., Martelli, M. F., and Zasler, N. D. (2000). Chronic pain and neuropsychological functioning. Neuropsychol. Rev. 10, 131–149. doi: 10.1023/A:1009020914358
Hasenbring, M. I., Hallner, D., Klasen, B., Streitlein-Böhme, I., Willburger, R., and Rusche, H. (2012). Pain-related avoidance versus endurance in primary care patients with subacute back pain: psychological characteristics and outcome at a 6-month follow-up. Pain 153, 211–217. doi: 10.1016/j.pain.2011.10.019
Hechler, T., Kosfelder, J., Vocks, S., Mönninger, T., Blankenburg, M., Dobe, M., et al. (2010). Changes in pain-related coping strategies and their importance for treatment outcome following multimodal inpatient treatment: does sex matter? J. Pain 11, 472–483. doi: 10.1016/j.jpain.2009.09.002
Heutink, M., Post, M. W., Overdulve, C. W., Pfennings, L. E., van de Vis, W., Vrijens, N. L., et al. (2013). Which pain coping strategies and cognitions are associated with outcomes of a cognitive behavioral intervention for neuropathic pain after spinal cord injury? Top. Spinal Cord Inj. Rehabil. 19, 330–340. doi: 10.1310/sci1904-330
Hill, J. C., Lewis, M., Sim, J., Hay, E. M., and Dziedzic, K. (2007). Predictors of poor outcome in patients with neck pain treated by physical therapy. Clin. J. Pain 23, 683–690. doi: 10.1097/AJP.0b013e3181468e67
Hirsh, A. T., Bockow, T. B., and Jensen, M. P. (2011). Catastrophizing, pain, and pain interference in individuals with disabilities. Am. J. Phys. Med. Rehabil. 90, 713–722. doi: 10.1097/PHM.0b013e31822409b2
Hirsh, A. T., Kupper, A. E., Carter, G. T., and Jensen, M. P. (2010). Psychosocial factors and adjustment to pain in individuals with postpolio syndrome. Am. J. Phys. Med. Rehabil. 89, 213–224. doi: 10.1097/PHM.0b013e3181c9f9a1
Holroyd, K. A., Labus, J. S., and Carlson, B. (2009). Moderation and mediation in the psychological and drug treatment of chronic tension-type headache: the role of disorder severity and psychiatric comorbidity. Pain 143, 213–222. doi: 10.1016/j.pain.2009.02.019
Hosoi, M., Molton, I. R., Jensen, M. P., Ehde, D. M., Amtmann, S., O'Brien, S., et al. (2010). Relationships among alexithymia and pain intensity, pain interference, and vitality in persons with neuromuscular disease: considering the effect of negative affectivity. Pain 149, 273–277. doi: 10.1016/j.pain.2010.02.012
Huber, A., Suman, A. L., Biasi, G., and Carli, G. (2009). Alexithymia in fibromyalgia syndrome: associations with ongoing pain, experimental pain sensitivity and illness behavior. J. Psychosom. Res. 66, 425–433. doi: 10.1016/j.jpsychores.2008.11.009
Jamison, R. N., and Virts, K. L. (1990). The influence of family support on chronic pain. Behav. Res. Ther. 28, 283–287. doi: 10.1016/0005-7967(90)90079-X
Jensen, M. P., Moore, M. R., Bockow, T. B., Ehde, D. M., and Engel, J. M. (2011). Psychosocial factors and adjustment to chronic pain in persons with physical disabilities: a systematic review. Arch. Phys. Med. Rehabil. 92, 146–160. doi: 10.1016/j.apmr.2010.09.021
Jongsma, M. L., Postma, S. A., Souren, P., Arns, M., Gordon, E., Vissers, K., et al. (2011). Neurodegenerative properties of chronic pain: cognitive decline in patients with chronic pancreatitis. PLoS ONE 6:e23363. doi: 10.1371/journal.pone.0023363
Judge, A., Arden, N. K., Cooper, C., Kassim Javaid, M., Carr, A. J., Field, R. E., et al. (2012). Predictors of outcomes of total knee replacement surgery. Rheumatology (Oxford). 51, 1804–1813. doi: 10.1093/rheumatology/kes075
Kass-Iliyya, L., Kobylecki, C., Mcdonald, K. R., Gerhard, A., and Silverdale, M. A. (2015). Pain in multiple system atrophy and progressive supranuclear palsy compared to Parkinson's disease. Brain Behav. 5:e00320. doi: 10.1002/brb3.320
Kores, R. C., Murphy, W. D., Rosenthal, T. L., Elias, D. B., and North, W. C. (1990). Predicting outcome of chronic pain treatment via a modified self-efficacy scale. Behav. Res. Ther. 28, 165–169. doi: 10.1016/0005-7967(90)90029-I
Koroschetz, J., Rehm, S. E., Gockel, U., Brosz, M., Freynhagen, R., Tollë, T. R., et al. (2011). Fibromyalgia and neuropathic pain–differences and similarities. A comparison of 3057 patients with diabetic painful neuropathy and fibromyalgia. BMC Neurol. 11:55. doi: 10.1186/1471-2377-11-55
Kosseva, M., Schild, S., Wilhelm-Schwenk, R., Biewer, W., and Häuser, W. (2010). [Comorbid depression mediates the association of childhood/adolescent maltreatment and fibromyalgia syndrome. A study with patients from different clinical settings]. Schmerz 24, 474–484. doi: 10.1007/s00482-010-0969-0
Kröner-Herwig, B., Morris, L., and Heinrich, M. (2008). Biopsychosocial correlates of headache: what predicts pediatric headache occurrence? Headache 48, 529–544. doi: 10.1111/j.1526-4610.2007.00945.x
Ligthart, L., Gerrits, M. M., Boomsma, D. I., and Penninx, B. W. (2013). Anxiety and depression are associated with migraine and pain in general: an investigation of the interrelationships. J. Pain 14, 363–370. doi: 10.1016/j.jpain.2012.12.006
Litt, M. D., and Porto, F. B. (2013). Determinants of pain treatment response and nonresponse: identification of TMD patient subgroups. J. Pain 14, 1502–1513. doi: 10.1016/j.jpain.2013.07.017
Lohnberg, J. A., and Altmaier, E. M. (2013). A review of psychosocial factors in complex regional pain syndrome. J. Clin. Psychol. Med. Settings 20, 247–254. doi: 10.1007/s10880-012-9322-3
Lucey, B. P., Clifford, D. B., Creighton, J., Edwards, R. R., McArthur, J. C., and Haythornthwaite, J. (2011). Relationship of depression and catastrophizing to pain, disability, and medication adherence in patients with HIV-associated sensory neuropathy. AIDS Care 23, 921–928. doi: 10.1080/09540121.2010.543883
Lumley, M. A., Smith, J. A., and Longo, D. J. (2002). The relationship of alexithymia to pain severity and impairment among patients with chronic myofascial pain: comparisons with self-efficacy, catastrophizing, and depression. J. Psychosom. Res. 53, 823–830. doi: 10.1016/S0022-3999(02)00337-9
Mao, C. J., Chen, J. P., Zhang, X. Y., Chen, Y., Li, S. J., Li, J., et al. (2015). Parkinson's disease patients with pain suffer from more severe non-motor symptoms. Neurol. Sci. 36, 263–268. doi: 10.1007/s10072-014-1942-y
McBeth, J., Lacey, R. J., and Wilkie, R. (2014). Predictors of new-onset widespread pain in older adults: results from a population-based prospective cohort study in the UK. Arthritis Rheumatol. 66, 757–767. doi: 10.1002/art.38284
McCracken, L. M., Gross, R. T., and Eccleston, C. (2002). Multimethod assessment of treatment process in chronic low back pain: comparison of reported pain-related anxiety with directly measured physical capacity. Behav. Res. Ther. 40, 585–594. doi: 10.1016/S0005-7967(01)00074-2
Miles, C. L., Pincus, T., Carnes, D., Homer, K. E., Taylor, S. J., Bremner, S. A., et al. (2011). Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. Eur. J. Pain 15, 775 e771–e711. doi: 10.1016/j.ejpain.2011.01.016
Miller, L. A., and Radford, K. (2014). Testing the effectiveness of group-based memory rehabilitation in chronic stroke patients. Neuropsychol. Rehabil. 24, 721–737. doi: 10.1080/09602011.2014.894479
Miller, K. K., Combs, S. A., Van Puymbroeck, M., Altenburger, P. A., Kean, J., Dierks, T. A., et al. (2013). Fatigue and pain: relationships with physical performance and patient beliefs after stroke. Top. Stroke Rehabil. 20, 347–355. doi: 10.1310/tsr2004-347
Milling, L. S., Reardon, J. M., and Carosella, G. M. (2006). Mediation and moderation of psychological pain treatments: response expectancies and hypnotic suggestibility. J. Consult. Clin. Psychol. 74, 253–262. doi: 10.1037/0022-006X.74.2.253
Milling, L. S., Shores, J. S., Coursen, E. L., Menario, D. J., and Farris, C. D. (2007). Response expectancies, treatment credibility, and hypnotic suggestibility: mediator and moderator effects in hypnotic and cognitive-behavioral pain interventions. Ann. Behav. Med. 33, 167–178. doi: 10.1007/BF02879898
Moriarty, O., McGuire, B. E., and Finn, D. P. (2011). The effect of pain on cognitive function: a review of clinical and preclinical research. Prog. Neurobiol. 93, 385–404. doi: 10.1016/j.pneurobio.2011.01.002
Morlion, B., Kempke, S., Luyten, P., Coppens, E., and Van Wambeke, P. (2011). Multidisciplinary pain education program (MPEP) for chronic pain patients: preliminary evidence for effectiveness and mechanisms of change. Curr. Med. Res. Opin. 27, 1595–1601. doi: 10.1185/03007995.2011.595779
Nakamura, M., Nishiwaki, Y., Sumitani, M., Ushida, T., Yamashita, T., Konno, S., et al. (2014). Investigation of chronic musculoskeletal pain (third report): with special reference to the importance of neuropathic pain and psychogenic pain. J. Orthop. Sci. 19, 667–675. doi: 10.1007/s00776-014-0670-8
Nicassio, P. M., Radojevic, V., Weisman, M. H., Schuman, C., Kim, J., Schoenfeld-Smith, K., et al. (1997). A comparison of behavioral and educational interventions for fibromyalgia. J. Rheumatol. 24, 2000–2007.
Nicholson, R. A., Houle, T. T., Rhudy, J. L., and Norton, P. J. (2007). Psychological risk factors in headache. Headache 47, 413–426. doi: 10.1111/j.1526-4610.2006.00716.x
Nielson, W. R., and Jensen, M. P. (2004). Relationship between changes in coping and treatment outcome in patients with Fibromyalgia Syndrome. Pain 109, 233–241. doi: 10.1016/j.pain.2004.01.002
O'Donnell, M. J., Diener, H. C., Sacco, R. L., Panju, A. A., Vinisko, R., Yusuf, S., et al. (2013). Chronic pain syndromes after ischemic stroke: PRoFESS trial. Stroke 44, 1238–1243. doi: 10.1161/STROKEAHA.111.671008
Osborne, T. L., Jensen, M. P., Ehde, D. M., Hanley, M. A., and Kraft, G. (2007). Psychosocial factors associated with pain intensity, pain-related interference, and psychological functioning in persons with multiple sclerosis and pain. Pain 127, 52–62. doi: 10.1016/j.pain.2006.07.017
Pagnini, F., Lunetta, C., Banfi, P., Rossi, G., Fossati, F., Marconi, A., et al. (2012). Pain in Amyotrophic lateral Sclerosis: a psychological perspective. Neurol. Sci. 33, 1193–1196. doi: 10.1007/s10072-011-0888-6
Pickering, G., Pereira, B., Clère, F., Sorel, M., de Montgazon, G., Navez, M., et al. (2014). Cognitive function in older patients with postherpetic neuralgia. Pain Pract. 14, E1–E7. doi: 10.1111/papr.12079
Proctor, S. L., Estroff, T. W., Empting, L. D., Shearer-Williams, S., and Hoffmann, N. G. (2013). Prevalence of substance use and psychiatric disorders in a highly select chronic pain population. J. Addict. Med. 7, 17–24. doi: 10.1097/ADM.0b013e3182738655
Radat, F., Lantéri-Minet, M., Nachit-Ouinekh, F., Massiou, H., Lucas, C., Pradalier, A., et al. (2009). The GRIM2005 study of migraine consultation in France. III: psychological features of subjects with migraine. Cephalalgia 29, 338–350. doi: 10.1111/j.1468-2982.2008.01718.x
Radat, F., Margot-Duclot, A., and Attal, N. (2013). Psychiatric co-morbidities in patients with chronic peripheral neuropathic pain: a multicentre cohort study. Eur. J. Pain 17, 1547–1557. doi: 10.1002/j.1532-2149.2013.00334.x
Raichle, K., Ehde, D., Dillworth, T., Sullivan-Singh, S., Osborne, T., Jensen, M., et al. (2014). Therapeutic alliance is associated with outcomes of psychosocial interventions for persons with chronic pain and disability. J. Pain 15, S105. doi: 10.1016/j.jpain.2014.01.430
Rana, A. Q., Qureshi, A. R., Rahman, L., Jesudasan, A., Hafez, K. K., and Rana, M. A. (2016). Association of restless legs syndrome, pain, and mood disorders in parkinson's disease. Int. J. Neurosci. 126, 116–120. doi: 10.3109/00207454.2014.994208
Rekleiti, M., Sarafis, P., Saridi, M., Toska, A., Melos, C., Souliotis, K., et al. (2013). Investigation of depression in Greek patients with diabetic peripheral neuropathy. Glob. J. Health Sci. 5, 107–114. doi: 10.5539/gjhs.v5n5p107
Rewhorn, M. J., Leung, A. H., Gillespie, A., Moir, J. S., and Miller, R. (2014). Incidence of complex regional pain syndrome after foot and ankle surgery. J. Foot Ankle Surg. 53, 256–258. doi: 10.1053/j.jfas.2014.01.006
Rhee, S. H., Parker, J. C., Smarr, K. L., Petroski, G. F., Johnson, J. C., Hewett, J. E., et al. (2000). Stress management in rheumatoid arthritis: what is the underlying mechanism? Arthritis Care Res. 13, 435–442. doi: 10.1002/1529-0131(200012)13:63.3.CO;2-A
Riva, G., and Mantovani, F. (2012). From the body to the tools and back: a general framework for presence in mediated interactions. Interact. Comput. 24, 203–210. doi: 10.1016/j.intcom.2012.04.007
Rommel, O., Willweber-Strumpf, A., Wagner, P., Surall, D., Malin, J. P., and Zenz, M. (2005). [Psychological abnormalities in patients with complex regional pain syndrome (CRPS)]. Schmerz 19, 272–284. doi: 10.1007/s00482-004-0337-z
Ruiz-Párraga, G. T., and López-Martínez, A. E. (2013). The contribution of posttraumatic stress symptoms to chronic pain adjustment. Health Psychol. 33, 958–967. doi: 10.1037/hea0000040
Samwel, H. J., Kraaimaat, F. W., Crul, B. J., van Dongen, R. D., and Evers, A. W. (2009). Multidisciplinary allocation of chronic pain treatment: effects and cognitive-behavioural predictors of outcome. Br. J. Health Psychol. 14, 405–421. doi: 10.1348/135910708X337760
Scheidt, C. E., Mueller-Becsangèle, J., Hiller, K., Hartmann, A., Goldacker, S., Vaith, P., et al. (2014). Self-reported symptoms of pain and depression in primary fibromyalgia syndrome and rheumatoid arthritis. Nord. J. Psychiatry 68, 88–92. doi: 10.3109/08039488.2013.782566
Seifert, C. L., Mallar Chakravarty, M., and Sprenger, T. (2013). The complexities of pain after stroke-a review with a focus on central post-stroke pain. Panminerva Med. 55, 1–10.
Shaygan, M., Böger, A., and Kröner-Herwig, B. (2013). Clinical features of chronic pain with neuropathic characteristics: a symptom-based assessment using the pain DETECT questionnaire. Eur. J. Pain 17, 1529–1538. doi: 10.1002/j.1532-2149.2013.00322.x
Shin, N. Y., Kang, D. H., Jang, J. H., Park, S. Y., Hwang, J. Y., Kim, S. N., et al. (2013). Impaired recognition of social emotion in patients with complex regional pain syndrome. J. Pain 14, 1304–1309. doi: 10.1016/j.jpain.2013.05.008
Smeets, R. J., Vlaeyen, J. W., Kester, A. D., and Knottnerus, J. A. (2006). Reduction of pain catastrophizing mediates the outcome of both physical and cognitive-behavioral treatment in chronic low back pain. J. Pain 7, 261–271. doi: 10.1016/j.jpain.2005.10.011
Sturgeon, J. A., Zautra, A. J., and Arewasikporn, A. (2014). A multilevel structural equation modeling analysis of vulnerabilities and resilience resources influencing affective adaptation to chronic pain. Pain 155, 292–298. doi: 10.1016/j.pain.2013.10.007
Subramaniam, M., Vaingankar, J. A., Abdin, E., and Chong, S. A. (2013). Psychiatric morbidity in pain conditions: results from the Singapore Mental Health Study. Pain Res. Manag. 18, 185–190. doi: 10.1155/2013/798205
Sullivan, M. J., Lynch, M. E., and Clark, A. J. (2005). Dimensions of catastrophic thinking associated with pain experience and disability in patients with neuropathic pain conditions. Pain 113, 310–315. doi: 10.1016/j.pain.2004.11.003
Syed Hassan, S. T., Jamaludin, H., Abd Raman, R., Mohd Riji, H., and Wan Fei, K. (2013). Mental trauma experienced by caregivers of patients with diffuse axonal injury or severe traumatic brain injury. Trauma Mon. 18, 56–61. doi: 10.1016/j.jamda.2016.02.032
Toth, C., Brady, S., and Hatfield, M. (2014). The importance of catastrophizing for successful pharmacological treatment of peripheral neuropathic pain. J. Pain Res. 7, 327–338. doi: 10.2147/JPR.S56883
Triberti, S., Repetto, C., and Riva, G. (2014). Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol. Behav. Soc. Netw. 17, 335–345. doi: 10.1089/cyber.2014.0054
Turner, J. A., Holtzman, S., and Mancl, L. (2007). Mediators, moderators, and predictors of therapeutic change in cognitive-behavioral therapy for chronic pain. Pain 127, 276–286. doi: 10.1016/j.pain.2006.09.005
Uher, T., and Bob, P. (2013). Neuropathic pain, depressive symptoms, and C-reactive protein in sciatica patients. Int. J. Neurosci. 123, 204–208. doi: 10.3109/00207454.2012.746335
Van Gorp, S., Kessels, A. G., Joosten, E. A., Van Kleef, M., and Patijn, J. (2015). Pain prevalence and its determinants after spinal cord injury: a systematic review. Eur. J. Pain 19, 5–14. doi: 10.1002/ejp.522
Vase, L., Nikolajsen, L., Christensen, B., Egsgaard, L. L., Arendt-Nielsen, L., Svensson, P., et al. (2011). Cognitive-emotional sensitization contributes to wind-up-like pain in phantom limb pain patients. Pain 152, 157–162. doi: 10.1016/j.pain.2010.10.013
Villani, D., Repetto, C., Cipresso, P., and Riva, G. (2012). May I experience more presence in doing the same thing in virtual reality than in reality? An answer from a simulated job interview. Interact. Comput. 24, 265–272. doi: 10.1016/j.intcom.2012. 04.008
Vowles, K. E., McCracken, L. M., and Eccleston, C. (2007). Processes of change in treatment for chronic pain: the contributions of pain, acceptance, and catastrophizing. Eur. J. Pain 11, 779–787. doi: 10.1016/j.ejpain.2006.12.007
Wasserman, R. A., Brummett, C. M., Goesling, J., Tsodikov, A., and Hassett, A. L. (2014). Characteristics of chronic pain patients who take opioids and persistently report high pain intensity. Reg. Anesth. Pain Med. 39, 13–17. doi: 10.1097/AAP.0000000000000024
Wen, H. B., Zhang, Z. X., Wang, H., Li, L., Chen, H., Liu, Y., et al. (2012). Epidemiology and clinical phenomenology for Parkinson's disease with pain and fatigue. Parkinsonism Relat. Disord. 18(Suppl. 1), S222–S225. doi: 10.1016/S1353-8020(11)70068-2
Weyer Jamora, C., Schroeder, S. C., and Ruff, R. M. (2013). Pain and mild traumatic brain injury: the implications of pain severity on emotional and cognitive functioning. Brain Inj. 27, 1134–1140. doi: 10.3109/02699052.2013.804196
Wicksell, R. K., Kemani, M., Jensen, K., Kosek, E., Kadetoff, D., Sorjonen, K., et al. (2013). Acceptance and commitment therapy for fibromyalgia: a randomized controlled trial. Eur. J. Pain 17, 599–611. doi: 10.1002/j.1532-2149.2012.00224.x
Wicksell, R. K., Olsson, G. L., and Hayes, S. C. (2010). Psychological flexibility as a mediator of improvement in Acceptance and Commitment Therapy for patients with chronic pain following whiplash. Eur. J. Pain 14, 1059e1051–1059 e1011. doi: 10.1016/j.ejpain.2010.05.001
Wieser, T., Walliser, U., Womastek, I., and Kress, H. G. (2012). Dysfunctional coping in headache: avoidance and endurance is not associated with chronic forms of headache. Eur. J. Pain 16, 268–277. doi: 10.1016/j.ejpain.2011.06.011
Wood, R. L., McCabe, M., and Dawkins, J. (2011). The role of anxiety sensitivity in symptom perception after minor head injury: an exploratory study. Brain Inj. 25, 1296–1299. doi: 10.3109/02699052.2011.624569
Yamaguchi, R., Nicholson Perry, K., and Hines, M. (2013). Pain, pain anxiety and emotional and behavioural problems in children with cerebral palsy. Disabil. Rehabil. 36, 125–130. doi: 10.3109/09638288.2013.782356
Yoshida, S., Hirai, M., Suzuki, S., Awata, S., and Oka, Y. (2009). Neuropathy is associated with depression independently of health-related quality of life in Japanese patients with diabetes. Psychiatry Clin. Neurosci. 63, 65–72. doi: 10.1111/j.1440-1819.2008.01889.x
Keywords: pain management, clinical psychology, health psychology, chronic pain, neurorehabilitation
Citation: Castelnuovo G, Giusti EM, Manzoni GM, Saviola D, Gatti A, Gabrielli S, Lacerenza M, Pietrabissa G, Cattivelli R, Spatola CAM, Corti S, Novelli M, Villa V, Cottini A, Lai C, Pagnini F, Castelli L, Tavola M, Torta R, Arreghini M, Zanini L, Brunani A, Capodaglio P, D'Aniello GE, Scarpina F, Brioschi A, Priano L, Mauro A, Riva G, Repetto C, Regalia C, Molinari E, Notaro P, Paolucci S, Sandrini G, Simpson SG, Wiederhold B and Tamburin S on behalf of the Italian Consensus Conference on Pain in Neurorehabilitation (2016) Psychological Considerations in the Assessment and Treatment of Pain in Neurorehabilitation and Psychological Factors Predictive of Therapeutic Response: Evidence and Recommendations from the Italian Consensus Conference on Pain in Neurorehabilitation. Front. Psychol. 7:468. doi: 10.3389/fpsyg.2016.00468
Received: 19 January 2016; Accepted: 16 March 2016;
Published: 19 April 2016.
Edited by:
Omar Carlo Gioacchino Gelo, Universita del Salento/Sigmund Freud University, ItalyReviewed by:
Sabrina Cipolletta, University of Padua, ItalyClaudia Cormio, National Cancer Research Institute “Giovanni Paolo II”, Italy
Copyright © 2016 Castelnuovo, Giusti, Manzoni, Saviola, Gatti, Gabrielli, Lacerenza, Pietrabissa, Cattivelli, Spatola, Corti, Novelli, Villa, Cottini, Lai, Pagnini, Castelli, Tavola, Torta, Arreghini, Zanini, Brunani, Capodaglio, D'Aniello, Scarpina, Brioschi, Priano, Mauro, Riva, Repetto, Regalia, Molinari, Notaro, Paolucci, Sandrini, Simpson, Wiederhold and Tamburin on behalf of the Italian Consensus Conference on Pain in Neurorehabilitation. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Gianluca Castelnuovo, Z2lhbmx1Y2EuY2FzdGVsbnVvdm9AdW5pY2F0dC5pdA==
 Gianluca Castelnuovo
Gianluca Castelnuovo Emanuele M. Giusti
Emanuele M. Giusti Gian Mauro Manzoni
Gian Mauro Manzoni Donatella Saviola
Donatella Saviola Arianna Gatti
Arianna Gatti Samantha Gabrielli
Samantha Gabrielli Marco Lacerenza
Marco Lacerenza Giada Pietrabissa
Giada Pietrabissa Roberto Cattivelli
Roberto Cattivelli Chiara A. M. Spatola
Chiara A. M. Spatola Stefania Corti
Stefania Corti Margherita Novelli
Margherita Novelli Valentina Villa
Valentina Villa Andrea Cottini
Andrea Cottini Carlo Lai
Carlo Lai Francesco Pagnini
Francesco Pagnini Lorys Castelli
Lorys Castelli Mario Tavola11
Mario Tavola11 Riccardo Torta
Riccardo Torta Marco Arreghini
Marco Arreghini Loredana Zanini
Loredana Zanini Amelia Brunani
Amelia Brunani Paolo Capodaglio
Paolo Capodaglio Guido E. D'Aniello
Guido E. D'Aniello Lorenzo Priano
Lorenzo Priano Alessandro Mauro
Alessandro Mauro Giuseppe Riva
Giuseppe Riva Claudia Repetto
Claudia Repetto Enrico Molinari
Enrico Molinari Paolo Notaro
Paolo Notaro Stefano Paolucci
Stefano Paolucci Susan G. Simpson
Susan G. Simpson Brenda Wiederhold
Brenda Wiederhold