- 1Department of Perinatal Imaging and Health, Centre for the Developing Brain, St. Thomas' Hospital, King's College London, London, UK
- 2Department of Psychosis Studies, Institute of Psychiatry, Psychology and Neuroscience, King's College London, London, UK
Very preterm birth (VPT; < 32 weeks of gestation) has been associated with an increased risk to develop cognitive and socio-emotional problems, as well as with increased vulnerability to psychiatric disorder, both with childhood and adult onset. Socio-emotional impairments that have been described in VPT individuals include diminished social competence and self-esteem, emotional dysregulation, shyness and timidity. However, the etiology of socio-emotional problems in VPT samples and their underlying mechanisms are far from understood. To date, research has focused on the investigation of both biological and environmental risk factors associated with socio-emotional problems, including structural and functional alterations in brain areas involved in processing emotions and social stimuli, perinatal stress and pain and parenting strategies. Considering the complex interplay of the aforementioned variables, the review attempts to elucidate the mechanisms underlying the association between very preterm birth, socio-emotional vulnerability and psychopathology. After a comprehensive overview of the socio-emotional impairments associated with VPT birth, three main models of socio-emotional development are presented and discussed. These focus on biological vulnerability, early life adversities and parenting, respectively. To conclude, a developmental framework is used to consider different pathways linking VPT birth to psychopathology, taking into account the interaction between medical, biological, and psychosocial factors.
Introduction
Very preterm birth (VPT; < 32 weeks of gestation) is common and represents up to 13% of all births (Goldenberg et al., 2008). In the last decades, significant improvements in the management of high risk pregnancies has led to higher survival of babies born very preterm (Fanaroff et al., 2003). However, such improved survival has been associated with an increase in prevalence of neonatal problems and long-term morbidity, as very preterm infants are at greater risk of brain damage and consequent neurological disorders, neuropsychological, and behavioral impairments in childhood and later in life (Delobel-Ayoub et al., 2009; Nosarti et al., 2012; Arpi and Ferrari, 2013; Ball et al., 2013; Anderson, 2014).
Approximately 5–15% of VPT children experience motor and sensory deficits, such as cerebral palsy, vision, and hearing problems (Wood et al., 2005; Woodward et al., 2006) and more than 50% of children born extremely preterm (≤ 26 gestational weeks) experience academic difficulties (Johnson et al., 2009), with lower scores in reading, spelling, and arithmetic (Aarnoudse-Moens et al., 2009; Hutchinson et al., 2013). Together with these impairments, behavioral problems are reported in about 25% of VPT children, which can be summarized into a fairly consistent behavioral phenotype, characterized by inattention, anxiety, socio-emotional, and internalizing problems (Johnson and Marlow, 2011; Arpi and Ferrari, 2013). Such behavioral phenotype manifests in increased rates of subclinical symptomatology that, at the furthest end of the distribution, meet clinical criteria (Elgen et al., 2002; Johnson and Marlow, 2011). VPT children are thus at higher risk than controls of developing psychiatric disorders, including attention deficit and hyperactivity disorder (ADHD), autism spectrum disorder (ASD), anxiety and depression (Johnson and Marlow, 2011; Treyvaud et al., 2013) while VPT adults show a significant increase in the prevalence of ADHD (Halmøy et al., 2012), ASD (Moster et al., 2009), non-affective psychosis (Nosarti et al., 2012), depression, anxiety (Walshe et al., 2008), eating disorder (Micali et al., 2015), and bipolar affective disorder (Abel et al., 2010; Nosarti et al., 2012).
Early life deficits in socio-emotional processing have been studied as antecedents of later subclinical behavioral and psychiatric problems (e.g., Briggs-Gowan and Carter, 2008). Furthermore, research has suggested that social functioning plays a clinically relevant role in predicting the course and outcomes of several psychiatric disorders (Cannon et al., 1997; Van Os et al., 2010). Animal and human studies have put forward the hypothesis that social defeat and social exclusion, defined here collectively as the “negative experience of being excluded from the majority group” (Selten et al., 2013), as well as chronic psychosocial stress, may act as risk factors for psychiatric disorders. This hypothesis is based on the observation that individuals described as having atypical social development, poor social competence and high social anxiety are at greater risk of developing psychopathology than typically developing individuals, both in childhood and in adult life (Cannon et al., 1997; Selten and Cantor-Graae, 2005; Van Os et al., 2010; Van Os, 2013).
Atypical socio-emotional development has been described in VPT individuals (Hille et al., 2001; Bhutta et al., 2002) as early as the first year of life (Landry et al., 1990). Since socio-emotional functioning involves the ability to learn to successfully interact and communicate within a social context and to efficiently deal with emotions, it requires a skilful coordination of multiple processes (Iarocci et al., 2007; Happé and Frith, 2014), comprising social information processing, together with several other cognitive, perceptual and motor skills. It has been suggested that possible underlying causes of atypical socio-emotional development in VPT samples include deficits in basic cognitive skills: for instance, impairments in attention orienting may affect later development of gaze-following, leading to impairments in socio-communicative abilities (Karmiloff-Smith et al., 2012). Likewise, deficits in multisensory processing may affect speech perception, subsequently resulting in difficulties in communication and social interactions (Wickremasinghe et al., 2013; Stevenson et al., 2014).
In this paper, based on findings linking socio-emotional behavioral problems and psychopathology and showing high prevalence of such problems in VPT samples, we will explore possible underlying mechanisms linking VPT birth, socio-emotional vulnerability and mental health outcomes. We will focus on selective biological and environmental factors associated with VPT birth that during the course of development may interact with and affect socio-emotional processing, including structural and functional alterations in brain areas involved in processing emotions and social stimuli, perinatal stress and pain and parenting strategies.
Very preterm birth has been described as a complex amalgam of destructive and developmental disturbances, which may result in altered maturation of the highly-vulnerable developing brain (Volpe, 2009). Therefore, at least some of the behavioral and psychiatric problems described in VPT samples may be associated with differences in neurodevelopment, the life-long process by which the brain grows and adapts to change. Specific volumetric alterations have been described in brain areas involved in socio-emotional processing in VPT individuals (Peterson et al., 2000; Gimenez et al., 2006; Nosarti et al., 2008, 2014; Gousias et al., 2012; Rogers et al., 2012), although only a few studies to date have directly explored such brain alterations in conjunction with socio-emotional behavioral outcomes (e.g., Healy et al., 2013). Recent studies focusing on patterns of connectivity throughout the brain have identified alterations in thalamocortical and corticostriatal connections in VPT samples (Ball et al., 2015; Karolis et al., 2016), which are known to be crucial for social and emotional processing (Pauly et al., 2008), behavioral flexibility (Makinson and Huguenard, 2014), as well as high-order executive functions (Eisenberg and Berman, 2010). Functional alterations in these specific brain regions and connections have been described in neuropsychiatric disorders characterized by deficits in self-regulation and attention (Clerkin et al., 2013), suggesting that high order cognitive and emotional processes are subserved by dynamic interactions between brain networks, none of which is specifically “cognitive” or “affective” (Pessoa, 2008). In fact, impaired general cognition has been related to and associated with behavioral problems in VPT populations (Bayless et al., 2008; Mansson et al., 2014).
Another factor thought to affect socio-emotional development of infants born preterm is their exposure to early life stress and pain during their life-saving stay in the neonatal intensive care unit (NICU). VPT infants are exposed to repeated procedural pain-related stress during a period of rapid brain maturation and physiological vulnerability, and several studies have shown an impact of these procedures on altered neurodevelopment and hypothalamic-pituitary-adrenal (HPA) programming (Grunau, 2013; Brummelte et al., 2015), including greater internalizing behaviors in childhood (Vinall et al., 2013; Ranger et al., 2014).
A further important potential explanatory factor for impaired socio-emotional development in VPT individuals may involve the effects of early parental behavior. Life threating events in the perinatal period and the immature behavioral organization of preterm born infants may increase overall parental psychological distress and alter the interaction between child and primary carer, potentially interfering with the establishment of long-term positive parent-child relational patterns. Parental mental health has in fact been associated with children's early socio-emotional development, as it plays a pivotal role in protecting against the effects of early stress (Vinall and Grunau, 2014) and scaffolding the development of affective self-regulation (Feldman, 2007).
In this paper we will begin with a summary of socio-emotional behavioral problems in VPT infants, children and adults and describe psychiatric disorders which have been associated with VPT birth. We will consider the possible antecedents of such problems, especially impairments in social information processing, and in related cognitive and motor domains. We will then review the findings of neuroimaging studies which have investigated socio-emotional behavioral problems and psychiatric outcomes in VTP samples. We will also review some literature focusing on potential environmental influences on socio-emotional behavioral problems, such as exposure to neonatal pain and early parental behavior.
To conclude, we will consider the interplay between biological vulnerabilities, early life stress and early parental behavior in order to elucidate possible developmental mechanisms linking VPT birth, socio-emotional development and psychopathology.
Socio-Emotional Behavioral Problems in Very Preterm Born Individuals
The term “behavior problems” defines a wide spectrum of difficulties in behavioral self-regulation, comprising attention, and hyperactive/aggressive behaviors; sleep, eating, and sensory sensitivity problems; as well as problems with peers, anxiety, depression, and somatic symptoms. Well-validated behavioral screening questionnaires are usually administered to investigate behavioral morbidity and these tools, such as the Child Behavioral Check List (CBCL; Achenbach, 1991, 1992) and the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997), provide time- and cost-efficient measures for large-scale use (Johnson and Marlow, 2011).
Despite a relative paucity of studies in preterm-born individuals in infancy and adulthood, with most investigations focusing on school-age samples, behavioral problems have been reported as early as during the first 2 years of life (see Arpi and Ferrari, 2013 for review). However, VPT birth seems not to confer a risk for generalized behavioral morbidity, but appears to be associated with a specific triad of behavioral outcomes, characterized by inattention, emotional, and socialization difficulties, and with a greater risk of internalizing problems. The consistency of this behavioral profile in VPT samples has led to definition of a “preterm behavioral phenotype” (Johnson and Marlow, 2011).
Whilst a greater emphasis has been placed in the literature on attention problems, several studies have described socialization and emotion problems in VPT samples from infancy to adult life. The importance of a successful socio-emotional development for adult psychosocial adjustment has only recently been recognized, with studies showing a foundational contribution of socio-emotional development to later adaptive functioning, academic achievement and mental health (Emde et al., 1993; Shonkoff and Phillips, 2000). For instance, researchers have shown that more than half of typically developing children, identified as having socio-emotional problems during school-age, were already experiencing similar difficulties earlier in life, at 12–36 months (Briggs-Gowan and Carter, 2008). In the following section we will summarize the results of studies linking early socio-emotional difficulties to later well-being in VPT samples.
Socio-Emotional Behavioral Problems in Infancy (0–2 Years)
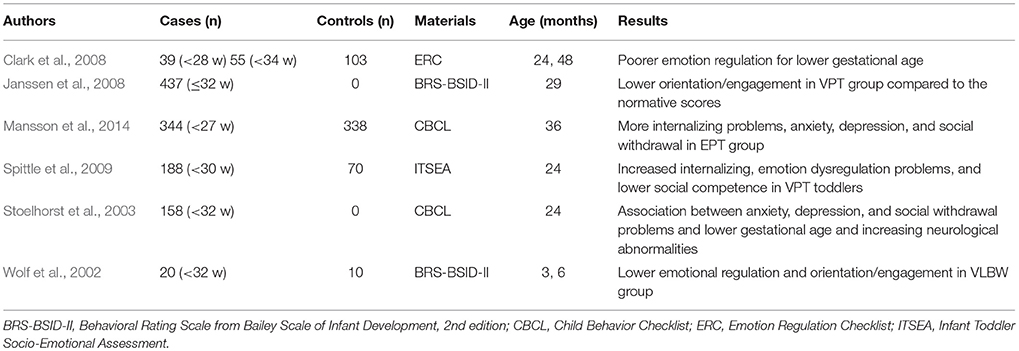
Although it is difficult to recognize behavioral problems during children's early developmental stages, due to their heterogeneous and highly changeable nature, the few studies conducted to date have shown a consistent pattern of impaired socio-emotional development following VPT birth (Arpi and Ferrari, 2013). Poorer emotional regulation and orientation/engagement was described in infants and toddlers born VPT and/or with a very low birth weight (VLBW; ≤ 1500 grams) compared to controls (Wolf et al., 2002; Janssens et al., 2009). VPT toddlers were further found to experience increased internalizing, emotion dysregulation problems and lower social competence compared to their age-matched peers (Clark et al., 2008; Spittle et al., 2009; Table 1).
Socio-Emotional Behavioral Problems in Childhood
A large number of studies in preterm-born children have described a behavioral profile that seems consistent with the preterm behavioral phenotype described earlier, and we invite the reader to refer to three meta-analyses for further details (Bhutta et al., 2002; Aarnoudse-Moens et al., 2009; Arpi and Ferrari, 2013). According to published findings, very preterm-born children show significant emotional difficulties relative to peers and these difficulties are identified by elevated scores on CBCL anxiety/depression and SDQ emotional difficulties scales.
Socialization and peer relationships represent another area of concern in VPT children, which are characterized by impaired social skills and social withdrawal. During preschool- and school-age, VPT children consistently show higher scores on peer problems (SDQ) and social withdrawal (CBCL) subscales and are described as being “not liked by peers,” “rather solitary, tend to play alone,” “too dependent.” Similar findings were reported in geographically diverse samples: social problems scores, as measured by the CBCL, were higher in four population-based cohorts of extremely low birth weight children (ELBW; ≤ 1000 grams) born in 1977–1987 compared to controls (Hille et al., 2001). More recently, screening questionnaires for ASD found that VPT children compared to controls displayed significantly more symptoms reflecting social difficulties, i.e., higher rates of social and communication problems (Williamson and Jakobson, 2014a,b in children; Wong et al., 2014 in toddlers). It is also worth noticing that the majority of studies describe VPT children as having higher group mean scores on socio-emotional scales than term-born peers, even when such scores do not reach clinical cut-offs. Such findings highlight the importance of using dimensional measures of symptomatology to describe the pattern of impairments observed in VPT populations.
While published studies agree about the presence of socio-emotional difficulties in VPT samples, there seems to be less consensus on the prevalence of internalizing versus externalizing behaviors. Whereas the former is a term used to describe problems such as social withdrawal, somatic complains, anxiety, and depression, the latter refers to delinquent and aggressive behaviors (Achenbach, 1991). For further discussion on internalizing versus externalizing behaviors in VPT samples we would like to refer the reader to Johnson and Marlow (2011), Bhutta et al. (2002), Aarnoudse-Moens et al. (2009) and Arpi and Ferrari (2013).
Socio-Emotional Behavioral Problems in Adolescence
Adolescence refers to the period of life that marks the transition from childhood to adulthood, and is a critical stage of development associated with dramatic cognitive, physical, and emotional changes, during which several brain regions underlying psychosocial and executive functions reach maturity. The biological and physical transitions associated with puberty happen in concomitance with major socio-emotional changes, such as the shift from dependency on parents to autonomy, increased educational and societal demands, changes in social affiliations and expectations. During adolescence, socialization abilities become increasingly sophisticated and assume a crucial role in facilitating social interactions including social acceptance and the attainment of social dominance.
Pre-existing socio-emotional vulnerability is then expected to become more evident during this time, and this may be why adolescence is regarded as a key developmental stage in terms of emergence and early expression of behavioral issues. It is during this period that social rejection and peer victimization become critical risk factors for psychopathology, and the increased complexity of the social network in which the adolescent finds him/herself is thought to further exacerbate pre-existing socialization problems.
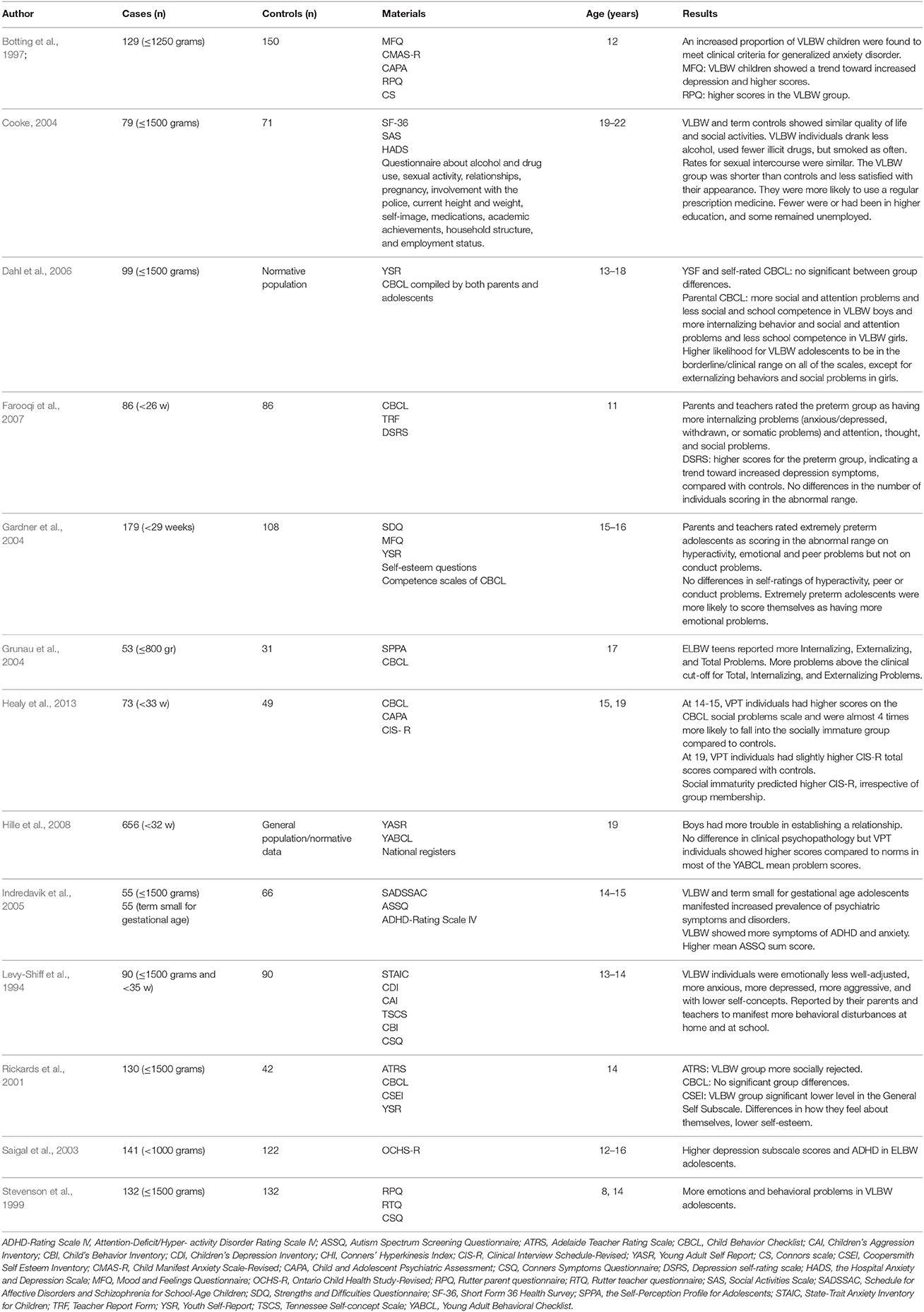
Studies of behavioral problems in VPT adolescents are limited, but seem to suggest a persistence of significant behavioral difficulties, showing a 3- to 8-fold increased risk compared to term controls (using a cut-off of >90th percentile for defining clinically significant behavioral problems; Johnson and Wolke, 2013 please refer to Table 2 for a list of studies describing socio-emotional behavioral problems in adolescents). Patterns of impairment observed in preterm adolescents seem consistent with the “preterm behavioral phenotype,” despite variability in prevalence estimates for different behavioral problems. VPT adolescents have been described as being more socially isolated, as having lower self-esteem (Rickards et al., 2001) and higher social problems scores than controls (Levy-Shiff et al., 1994; Grunau et al., 2004; Indredavik et al., 2005; Hille et al., 2008; Healy et al., 2013). Furthermore, they have been found to show higher incidence of “autistic-like” traits (Indredavik et al., 2004).
No consensus has yet been reached concerning the severity of emotional problems in preterm born adolescents (Nosarti et al., 2010) and the evidence for increased anxiety and depression is inconsistent (Johnson and Wolke, 2013). However, most case-control and birth cohort studies have described preterm adolescents as being emotionally vulnerable compared to controls. Significantly higher scores in preterm samples were reported using both the CBCL/SDQ emotional problems scales (Saigal et al., 2003; Gardner et al., 2004; Indredavik et al., 2005; Dahl et al., 2006; Farooqi et al., 2007) and specific tools assessing depression and anxiety (Botting et al., 1997; Saigal et al., 2003).
However, several other studies failed to detect significant emotional problems in VPT individuals (Rickards et al., 2001; Cooke, 2004; Grunau et al., 2004). A recent investigation by Hall and Wolke highlighted the need for longitudinal studies showing high stability of emotional problems and long lasting effects of child behavioral disturbances in a large cohort of VPT children from 6 to 13 years old (Hall and Wolke, 2012).
Methodological issues complicate the interpretation of results, as the type of “informer” used to collect information regarding emotional difficulties seems to affect findings. For instance, parents of VLBW adolescents reported more emotional difficulties in their offspring compared to parents of typically developing peers, whereas the VLBW adolescents in question declared less emotional problems than controls (Dahl et al., 2006).
Other possible confounding factors need to be taken into account when studying emotional difficulties in preterm adolescents: (1) symptoms of anxiety and depression show different life courses, with anxiety having a typical onset in childhood, compared to depression that mostly emerges in adolescence; (2) there are significant gender differences in prevalence of specific disorders, i.e., women are twice more likely to suffer from depression compared to men; (3) symptoms of anxiety and depression are highly comorbid, with anxiety often being a precursor to depression. Furthermore, in the preterm literature, anxiety and depression are often simultaneously investigated, which makes it difficult to disentangle the relative prevalence of dimension-specific symptoms (Johnson and Marlow, 2011).
Socio-Emotional Behavioral Problems in Adulthood
There is emerging evidence of increased socio-emotional behavioral problems also among young adults who were born prematurely (Hack et al., 2004; Hille et al., 2008; Boyle et al., 2011; Lund et al., 2012; Saigal, 2014). Together with behavioral difficulties, personality traits of preterm born young adults have also been examined. Despite the use of different assessment methods and the investigation of geographically disparate cohorts, very preterm born individuals have quite consistently been described as being less extroverted, more cautious, shyer, and more risk aversive than controls (Allin et al., 2006; Hack, 2006; Pesonen et al., 2008; Schmidt et al., 2008; Hertz et al., 2013; Eryigit-Madzwamuse et al., 2015). Furthermore, all studies except the one by Pesonen et al. (2008) reported higher levels of neuroticism in preterm-born adults. These personality traits have been associated with an increased vulnerability to develop psychopathology (Kendler et al., 2006; Widiger, 2011; Hertz et al., 2013).
Recent investigations from the Nordic countries using population-based records have permitted large-scale studies of different aspects of preterm born adults' socio-emotional life. Even when free from major disabilities, preterm born adults are more likely to be living in the parental home. Norwegian, Swedish and Finnish cohort studies reported that preterm born adults were less likely to be married or cohabiting (Lindström et al., 2007; Kajantie et al., 2008; Moster et al., 2009), were less likely to have ever had sexual intercourse (Darlow et al., 2013) and reported fewer sexual partners compared to controls (Hack et al., 2002; Hille et al., 2008; Kajantie et al., 2008; Männistö et al., 2015). Although results are not conclusive, current evidence suggests that VPT individuals have a poorer social life, spend less time with friends, have fewer friends, have less confidence in romantic situations and tend to perceive themselves as less attractive (Lund et al., 2012; Saigal, 2014). These data support the idea that possible socio-emotional issues persist in preterm populations even during adulthood.
Psychiatric Disorders in Very Preterm Born Individuals
In addition to higher rates of behavioral problems, accumulating evidence supports an association between prematurity and increased risk of developing mental health problems. A recent meta-analysis revealed that preterm born children, adolescents and adults are about 3.5 times more likely to be diagnosed with a psychiatric disorder compared to term born peers (Burnett et al., 2011).
Psychiatric Disorders in Childhood
Diagnostic studies describe a 3- to 4-fold risk of developing psychiatric disorders in preterm-born children compered to controls (Johnson and Marlow, 2011). Furthermore, preterm birth is associated with a specific pattern of disorders that mirrors the behavioral findings previously described: with preterm born children showing higher prevalence of ADHD (mainly the inattentive type), ASD and emotional disorders compared to their term born peers (Johnson and Marlow, 2011; Treyvaud et al., 2013). Published studies report a 2- to 3-fold risk for ADHD in VPT/VLBW children (Botting et al., 1997; Indredavik et al., 2004) and a 4-fold increased risk in extremely preterm (EPT; < 26 weeks of gestation) and ELBW children (Hack et al., 2009; Johnson et al., 2010b). The inattentive ADHD subtype seems to be prevalent and the clinical presentation of the disorder is quite different from that observed in children with ADHD who were not born VPT/VLBW, as it is associated with neurocognitive impairments and social difficulties, such as shyness, withdrawal and internalizing problems (Diamond, 2005).
Autism spectrum disorder has been reported as being 4–12 times more prevalent among ex-preterm children compared to controls (Williams et al., 2006; Fombonne, 2009) with symptoms believed to be qualitatively different from classical autistic traits, in this case being mediated by cognitive impairments, including distractibility and inattention (Hille et al., 2001; Elgen et al., 2002). Moreover, in contrast to the characteristic larger head circumference found in ASD children, in preterm children ASD symptoms have been found to be significantly associated with smaller head circumference (Johnson et al., 2010a).
Together with ADHD and ASD, diagnostic studies describe an increased prevalence of emotional disorders following VPT/VLBW, indicating a specific risk for anxiety in childhood. In contrast to the general population, emotional disorders do not show a female prevalence and seem associated with cognitive impairments (Johnson and Marlow, 2011).
Psychiatric Disorders in Adolescence and Adulthood
While diagnostic studies in preterm children mirror the profile of impairments described by a “preterm behavioral phenotype,” in adolescence and young adulthood prematurity has been defined as a single independent risk factor for a wide range of psychiatric disorders (Nosarti et al., 2012).
Different study designs have complementarily been used to investigate the prevalence of psychiatric disorders in preterm individuals. On the one hand, register studies in Scandinavian countries have provided a fruitful source of information using population-wide records. These studies have shown a stepwise increase in hospital admissions with decreasing gestational age (Lindström et al., 2007), and an increased risk of receiving a psychiatric diagnosis (Abel et al., 2010) and pharmacological treatments (Crump et al., 2010) in preterm born individuals compared to term-born peers. A higher risk of anorexia nervosa has been further reported in VPT girls (Cnattingius et al., 1999), as well as an increased prevalence of ADHD and ASD in VPT adults (Moster et al., 2009; Halmøy et al., 2012). These results suggest that several psychiatric outcomes may be associated with the same risk factor and a recent population-based study of 1,300,000 individuals demonstrated that VPT birth conferred an increased risk of hospitalization for non-affective psychosis, depressive and bipolar disorder, independently of other neonatal risk factors (Nosarti et al., 2012). Such findings suggest the existence of similar developmental mechanisms linking various psychiatric disorders, an idea which is supported by the results of family studies showing an increased risk of a variety of psychiatric disorders, including those not considered as being clinically associated, in individuals with a psychiatric family history (Dean et al., 2010).
Although these data from population-wide studies are informative, conditions that do not require pharmacological intervention or hospitalization, such as anxiety or mood disorders, are not recorded into register studies and alternative sources of information should be also pursued in order to gain diagnostic details. Clinical case-control studies employing psychopathology questionnaires reported an increased risk of mood and anxiety disorders associated with premature birth (Botting et al., 1997; Elgen et al., 2002; Indredavik et al., 2004; Walshe et al., 2008; Johnson et al., 2010a; see Burnett et al., 2011 for review), with several birth cohort studies suggesting almost a 2-fold risk of anxiety problems in VPT/VLBW populations (9.9% vs. 5.5% prevalence; Sømhovd et al., 2012), as well as a significant association between prematurity, intrauterine growth and depression (Thompson et al., 2001; Gale and Martyn, 2004; Alati et al., 2007; Raikkonen et al., 2008).
Brain Correlates of Socio-Emotional and Mental Health Problems
Converging evidence shows that survivors of very preterm birth are at substantial risk of brain injury in the perinatal period (Volpe, 2009). Primary focal lesions of the immature brain occur during a period of rapid development (for instance, the brain roughly triples in weight during the third trimester of gestation), and such lesions may disrupt programmed corticogenesis (Volpe, 2009) and subsequent typical maturational processes by altering cortical and subcortical developmental patterns (Hack and Taylor, 2000).
Given the association between prematurity and altered neurodevelopment (Ball et al., 2013), specific structural and functional brain alterations may underlie the socio-emotional difficulties associated with VPT birth. A huge amount and variety of mental operations are devoted to social information and emotion processing (Happé and Frith, 2014), and anatomically distributed networks have been shown to be part of a so-called social brain (Blakemore, 2008). These networks involve regions in the temporal lobe for processing faces, amygdala and insula for detecting and responding empathetically to others' emotions, orbitofrontal areas for emotional evaluation, threat detection and emotion regulation, medial prefrontal areas and superior temporal regions for the automatic attribution of mental states, while parietal and prefrontal areas have been implicated in processing other people's actions (Kennedy and Adolphs, 2012).
Volumetric alterations in some of these areas have been shown in VPT samples in childhood and adolescence: decreased gray matter concentration in orbitofrontal cortex (Gimenez et al., 2006; please see Ganella et al., 2015 for differences in orbitofrontal cortex sulcogyral pattern in EPT/ELBW adolescents), reduced volume of fusiform gyrus (Nosarti et al., 2008; Gousias et al., 2012), amygdala (Peterson et al., 2000), insula (Nosarti et al., 2008, 2014), and hippocampus (Nosarti et al., 2002; Abernethy et al., 2004; Rogers et al., 2012; Omizzolo et al., 2014; Aanes et al., 2015; Figure 1).
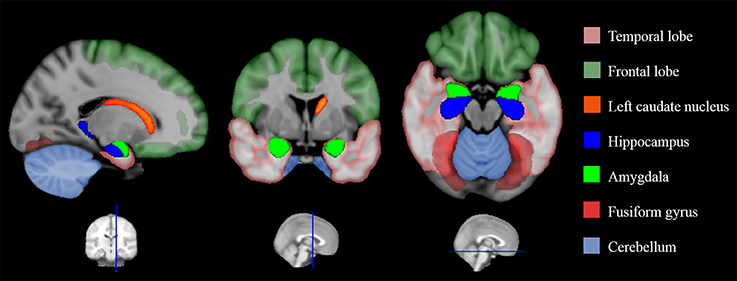
Figure 1. Structural alterations in the social brain found in preterm individuals. This is a graphic representation of a summary of the studies reviewed in Table 3. Colored areas highlight brain regions involved in processing socio-emotional stimuli that have been shown to display structural alterations in very preterm samples.
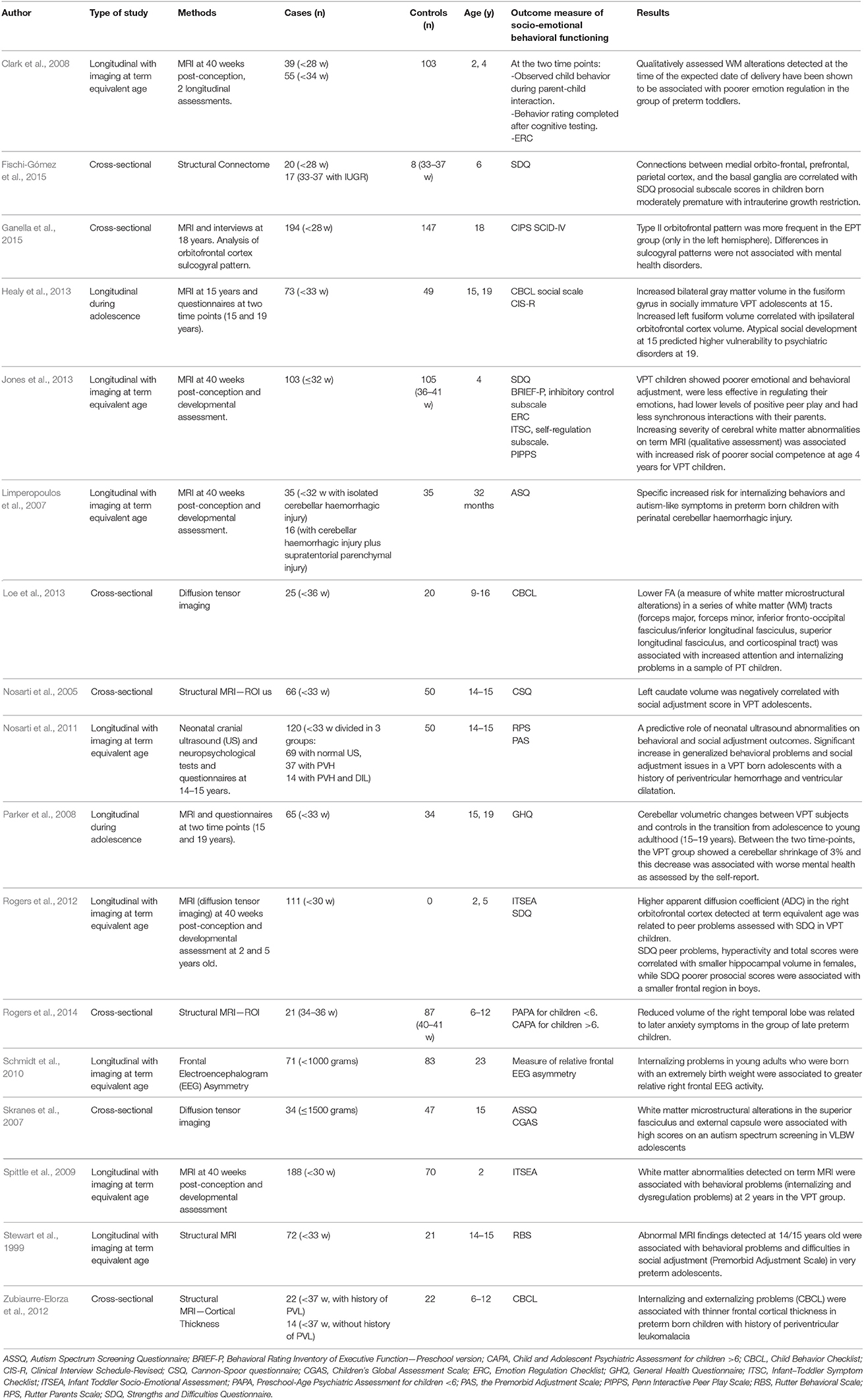
Only a few studies to date have investigated socio-emotional outcomes following preterm birth in association with structural and functional brain alterations (Nosarti et al., 2014; please refer to Table 3 for a list of studies associating MRI findings with socio-emotional outcomes).
Results of neuroimaging studies looking at defined cross-sectional time points showed significant associations between smaller volume of left caudate nucleus (Nosarti et al., 2005) and right superior temporal lobe (Rogers et al., 2014) and social adjustment and anxiety problems, respectively. Caudate abnormalities were also described in ASD (Qiu et al., 2010), suggesting a role of the caudate nucleus in reciprocal social and communicative behavior, possibly due to its complex connections within cortical-basal ganglia circuits underlying emotional and cognitive habits (Arnsten and Rubia, 2012). Structural brain alterations in temporal cortex have been described as core long-term consequences of VPT (Nosarti et al., 2008, 2014). Furthermore, alterations of the superior temporal lobe have been specifically associated with anxiety disorders (Corbetta et al., 2008).
Internalizing and externalizing problems were also associated with thinner prefrontal cortices in VPT children (Zubiaurre-Elorza et al., 2012) providing further support for the importance of frontal cortex maturation for appropriate behavioral control and inhibition (Shaw et al., 2012). Another aspect of brain function that has been related to internalizing problems in ELBW young adults was greater relative right frontal electroencephalography (EEG) activity. This measure is thought to be linked to the processing of negative emotions and has been suggested as a possible mechanism predisposing individuals to experience problems in stress regulation (Schmidt et al., 2010).
The association between socio-emotional problems and gray matter in the “social brain” were studied by Healy et al. (2013), who found that socially immature VPT adolescents (i.e., those with worse scores on the CBCL social problems scale) had increased bilateral gray matter volume in the fusiform gyrus compared to their VPT peers with age-appropriate CBCL scores, suggesting neurodevelopmental delays. Socio-emotional problems have been also associated with alterations in white matter (WM) areas that connect different brain regions involved in the processing of social stimuli and in WM tracts known to play a role in attention and working memory. Microstructural alterations in the superior fasciculus and external capsule were associated with high scores on an autism spectrum screening in VLBW adolescents (Skranes et al., 2007), while microstructural alterations in several WM tracts (forceps major, forceps minor, inferior fronto-occipital fasciculus/inferior longitudinal fascisculus, superior longitudinal fasciculus, and corticospinal tract) were associated with increased attention and internalizing problems in preterm children (Loe et al., 2013). Another recent study further described significant associations between WM connectivity in medial orbito-frontal, prefrontal, parietal cortex, and the basal ganglia and SDQ prosocial subscale scores in 6 years old children born moderately preterm (32 to < 37 weeks of gestation) with intrauterine growth restriction (Fischi-Gómez et al., 2015).
These studies highlight the complex interplay among different brain structures and the role of their connectivity in maintaining unimpaired social cognition and social behaviors. Fronto-striato-cerebellar circuits in addition to fronto-limbic and fronto-parietal networks seem to contribute to optimal socio-emotional behaviors. The “social brain,” far from being a modular and anatomically defined set of brain areas, appears to rely on distributed circuits, with the processing of social stimuli requiring the coordinated action of systems regulating attention, cognitive control, motivation, emotion and social cognition.
Structural and functional brain alterations associated with VPT birth in the early stages of development may affect later development of these networks. Results of the few longitudinal studies conducted to date have reported a significant association between perinatal white matter alterations and socio-emotional outcomes in childhood, pointing to the possibility of identifying possible biomarkers of outcome long before the actual manifestation of any potential problem (Clark et al., 2008; Spittle et al., 2009; Jones et al., 2013).
Higher apparent diffusion coefficient (ADC), reflecting possible WM pathology, in right orbitofrontal cortex detected at term equivalent age in VPT infants was related to peer problems at 5 years, supporting the idea of the involvement of the orbitofrontal cortex in theory of mind, social cognition, and social regulation (Rogers et al., 2012). The same study also described gender differences in the association between socio-emotional development at age 5 and regional brain maturation at term: SDQ peer problems, hyperactivity and total scores were correlated with smaller hippocampal volume in females, while poorer SDQ prosocial scores were associated with a smaller frontal region in boys. Another study described a specific increased risk for internalizing behaviors and autism-like symptoms in preterm born children with perinatal cerebellar haemorrhagic injury, highlighting the role of cerebellum in behavioral and social dysfunctions (Limperopoulos et al., 2007). Together with these finding, Nosarti et al. (2011) showed a predictive role of neonatal ultrasound abnormalities on behavioral and social adjustment outcomes in adolescence. They described a significant increase in generalized behavioral problems and social adjustment issues in a VPT born adolescents with a history of periventricular hemorrhage and ventricular dilatation, highlighting the importance of the integrity of subcortical periventricular areas for the optimal development of networks underlying socio-emotional functioning.
Only one study to date has investigated mental health and socio-emotional development in VPT samples in association with volumetric changes beyond the first weeks of life. Parker et al. (2008) compared cerebellar volumetric changes between VPT individuals and controls during the transition from adolescence to young adulthood (14–19 years). Between the two time-points, the VPT group showed 3% cerebellar shrinkage, and this decrease was associated with worse mental health, as assessed by a self-report (the General Health Questionnaire). This study highlights the need and importance of longitudinal investigations to shed light on the dynamic patterns of cortical and subcortical maturation associated with socio-emotional development and psychiatric outcomes (Shaw et al., 2010).
Pathways to Psychopathology
Despite a great prevalence of socio-emotional and psychiatric problems in individuals born very preterm, the underlying mechanisms that lead from preterm birth to socio-emotional vulnerability and psychopathology are far from understood. The hypothesis that socio-emotional difficulties lay on the causal pathway to developing psychiatric disorder has been supported by a great wealth of studies and socio-emotional problems have been considered as an important risk factor for psychopathology (Carter et al., 2004).
According to the social defeat hypothesis of mental illness, successful social functioning, including adequate social and emotional support, represents a protective factor against the development of psychiatric disorder (Selten and Cantor-Graae, 2005). Chronic experience of psychosocial stress and social adversity often results in social marginalization and feelings of inferiority, and these in turn increase an individual's risk for psychopathology. This conceptualization finds support in animal studies (see the “intruder-resident paradigm”) and in epidemiological human research, which shows a higher incidence of psychiatric outcomes in populations experiencing high social stress, such as migrants and individuals raised in urban environments (Van Os et al., 2010).
Dopamine dysregulation has been put forward as representing the possible biological mechanism linking social defeat with an increased risk of psychopathology: long-term exposure to social defeat may lead to sensitization of the mesolimbic dopamine system, to increases in its baseline activity, and thereby to a greater risk for psychosis (Selten and Cantor-Graae, 2005). Moreover, socio-emotional difficulties, such as affective dysregulation (as well as alterations in dopaminergic function), have been described as features characterizing the “extended phenotype,” and as a behavioral expression of vulnerability for psychiatric disorders (Van Os and Linscott, 2012).
Despite current evidence linking socio-emotional vulnerability with an increased risk of developing psychopathology, to date only a few studies have investigated the etiology of socio-emotional risk in VPT samples. The following section will offer an overview of several possible mechanisms which have been put forward in order to understand socio-emotional vulnerability and its antecedents.
Socio-Emotional Problems as a Result of Impaired Social Competence and their Neural Substrates
The term “social competence” refers to a variety of mental mechanisms aimed at supporting successful social functioning, including emotional self-regulation, social cognitive processing, positive communication and prosocial social relationships (Bornstein et al., 2010; Jones et al., 2013). Specific brain networks have been found to subserve these processes and to form the so-called “social brain” (Kennedy and Adolphs, 2012). Cross-sectional and longitudinal investigations of the associations between social competence and socio-emotional behavioral adjustment abound in the literature (Masten et al., 2006; Parker et al., 2006; Rubin et al., 2006). Overall, results of such studies suggest that deficits in social competence detected early in life contribute to the formation of internalizing problems, which may develop later on.
In light of these studies, several authors support a sociobiological vulnerability approach, which postulates that the increased social vulnerability seen in VPT samples occurs as a result of specific alterations in the “social brain,” as part of the neurodevelopmental sequelae of VPT birth (Healy et al., 2013). However, although social competence, achieved in the context of its typically developing neural substrates, has been recognized as the cornerstone of successful social adjustment, to date only a few studies have systematically investigated the early development of social competence in children born preterm. Furthermore, there is a paucity of investigations that have comprehensively assessed core aspects of development known to represent the milestones of successful social functioning.
Early-Life Joint Attention
Joint attention skills have been described as important precursors of social development (Baron-Cohen, 1991; Carpenter et al., 1998; Mundy and Gomes, 1998) and have been extensively investigated in the context of ASD research. Studies by Landry (1986) reported difficulties in joint attention in 6 months old infants born very preterm: these infants showed more problems engaging in joint play and initiating joint-attention interactions with their mothers, and exhibited more gaze aversion compared to their term-born peers (Garner et al., 1991; Smith and Ulvund, 2003).
Emotion Recognition
Four studies to date have investigated the ability to recognize facial emotional expressions in preterm born individuals. Recognizing facial emotional expressions is fundamental for developing effective social interactions and social adjustment (Saarni, 1999), and deficits in emotional understanding are associated with socio-emotional problems and psychiatric disorders (Denham et al., 2003; Dunn, 2010). Difficulties in emotion recognition were described in preterm children: Witt et al. (2014) reported less accurate naming of facial expressions of emotions in a sample of 42 months old VPT children compared to controls, while Potharst et al. (2013) reported similar finding in VPT children aged 5. Wocadlo and Rieger (2006) provided comparable results in a sample of 8 year olds and confirmed the role of emotion recognition for successful social functioning, showing an association between impaired emotion recognition, less popularity and more negative nominations from peers (Wocadlo and Rieger, 2006). Using a more complex test of social perceptual skills, Williamson and Jakobson (2014a) also described problems in interpreting others' emotions in 8–11 years old VPT children.
Emotion Regulation
Emotion regulation refers to a child's ability to modulate his/her emotions in response to people and situations, using a range of cognitive, physiological and behavioral processes/strategies allowing for empathic and socially appropriate behavior. Emotion regulation has increasingly been recognized as a potentially crucial marker of later psychosocial risk (Cole et al., 1994; Lawson and Ruff, 2004). Emotion regulation was longitudinally tested in a group of VPT children at 2 and 4 years using three different measures, consisting of two questionnaires (the emotion-regulation subscale from the Emotion Regulation Checklist and the Infant–Toddler Symptom Checklist) and in observational ratings of the child's emotion regulation during a session of developmental testing. Higher mean levels of emotional dysregulation emerged at both time points in the VPT group compared to controls (Clark et al., 2008; Jones et al., 2013).
Social Cognition
The term “social cognition” refers to the fundamental abilities to perceive, store, analyze, process, categorize, reason with, and behave toward other conspecifics (Pelphrey and Carter, 2008). Biological motion perception and theory of mind reasoning are two essential aspects of social cognition. Biological motion perception is defined as the ability to perceive and interpret body movements and is considered as a hallmark of social cognition (Pavlova, 2012). Theory of mind is defined as the ability to understand that other people may have different motivations and emotions from one's own and that people's behavior is guided by their inner states (Carlson and Moses, 2001). Impaired theory of mind has been described as a core deficit in autism spectrum disorder and has been linked to social anxiety and low popularity with peers (Happé and Frith, 2014).
Only a few studies to date have investigated these aspects of social cognition in preterm populations, and overall results suggest suboptimal functioning in both. VPT born children were less able to process biological motion and to attribute mental states than their term-born peers (Pavlova et al., 2008; Taylor et al., 2009; Williamson and Jakobson, 2014a,b; in VPT children with periventricular leukomalacia). However, no significant impairments in theory of mind tests were found by Jones et al. (2013) in a sample of VPT children aged 4, although the authors suggested the need for further investigations, as the psychometric utility of traditional false belief tests used in this study has been questioned.
Social Competence Investigated Using Questionnaires
Two studies to date have investigated social competence using the social competence scale of the Infant Toddler Socio-Emotional Assessment (ITSEA) and the Vineland scales (Sparrow et al., 1989), respectively. In both studies, VPT born children aged 2–5 scored significantly lower than their term born peers (Spittle et al., 2009; Alduncin et al., 2014).
Further research is needed to examine the presence of specific impairments in social cognition, emotion regulation, communicative skills and interactive behaviors in preterm children. More research is also required to shed light on possible alterations in patterns of neurodevelopment associated with impaired social competence, as no study thus far has targeted the possible neural underpinning of impaired social competence in preterm populations. A growing area of interest is focusing on the identification of early markers of social impairments, as studies have shown a predictive role of early abnormal patterns of attention orienting and eye gazing in discriminating individuals at risk for impaired social competence (Wass et al., 2015).
Socio-Emotional Problems Resulting from Cognitive and Motor Impairments
The previously described socio-biological vulnerability model explains socio-emotional difficulties resulting from possible structural and functional brain alterations in the “social brain” and postulates that, in preterm born individuals, socio-emotional brain networks and associated mental processes show atypical neurodevelopmental trajectories. These specific socio-biological alterations are thought to be due to preterm birth itself and to the range of possible clinically adverse events associated with it. In contrast to this model, several authors advocate for a non-specific etiology of socio-emotional difficulties in preterm populations, suggesting that cognitive impairments may mediate the association between preterm birth and socio-emotional difficulties. It is in fact well known that preterm birth represents a risk factor for a variety of neurodevelopmental sequelae and that impaired general cognitive functions (IQ) is a common finding. Convincing evidence exists to suggest that overall cognitive ability is reduced in preterm populations, and a recent meta-analysis describes a gradient effect of VPT birth on IQ, with an average estimated decline of 1.5 IQ points for each weekly decrease in gestational age for those born < 33 weeks of gestation (Kerr-Wilson et al., 2012; Anderson, 2014).
The hypothesis of a non-specific cognitive origin of socio-emotional behavioral problems explains the pattern of behavioral problems observed in VPT samples by hypothesizing a role of perinatal diffuse white matter injury in both cognitive and socio-emotional outcomes. In this model, the biological vulnerabilities associated with prematurity are thought not to be limited to areas involved in social information processing, but to affect several networks causing widespread functional impairments. This hypothesis brings attention to the role of thalamocortical connections, which are among the most severely damaged structures after preterm birth (Volpe, 2009; Kostović and Judaš, 2010; Ball et al., 2013) and play a crucial role in brain development (Kostović and Jovanov-Milošević, 2006), adversely affecting the maturation of several cortical and subcortical brain regions throughout the brain (Hack and Taylor, 2000; Ball et al., 2013). Moreover, altered thalamocortical connectivity in preterm infants has been found to predict general cognitive functions at 2 years of age (Ball et al., 2015).
The hypothesis of a cognitive root of socio-emotional difficulties comes from research investigating multiple predictors of behavior in the general population, as well as in preterm individuals (Goodman et al., 1995). Several studies have shown a co-occurrence of cognitive and socio-emotional difficulties, highlighting the important contribution of cognitive abilities to interpersonal skills and social maturity (Hughes et al., 2000; Stuss and Alexander, 2000; Heiervang et al., 2001; Kuntsi et al., 2001; Clark et al., 2002). Moreover, low IQ is one of the characteristic features of the extended phenotype and a core marker of vulnerability to psychopathology (Van Os and Linscott, 2012).
A possible pathway through which cognition influences behavioral problems may be through its effect on academic achievement: cognitive and learning difficulties may affect school performance, and academic underperformance may in turn contribute to children's psychosocial problems, posing risks for victimization and social exclusion (Gadeyne et al., 2004; Nadeau et al., 2004).
The model of socio-emotional difficulties following preterm birth is supported by a series of studies which found that cognitive abilities explained the observed increase in socio-emotional difficulties in preterm born samples. Mansson et al. (2014) showed a mediating effect of the mental developmental index (MDI) on internalizing problems in a sample of EPT toddlers. In line with these findings, in a sample of VPT born 8 year olds, the association between birth status, emotional symptoms and poorer social skills was mediated by IQ (Bayless et al., 2008).
Similar findings emerged from diagnostic studies: Johnson et al. (2010a), found that cognitive impairment accounted for more than half of the excess of socio-communication problems in 10 year olds born EPT with a diagnosis of autism, while in another cohort of 11 years old EPT children cognitively impaired children accounted for a significant portion of the diagnosed emotional disorders (Johnson et al., 2010b).
Another factor thought to mediate socio-emotional difficulties in preterm populations is neuromotor impairment. Up to 40% of children born very preterm suffer minor motor problems (Kieviet Piek et al., 2009) and motor difficulties have been shown to have far-reaching implications for socio-emotional function, as they have been linked with low self-esteem, difficulties in peer relations, isolation and emotional disorders (Skinner and Piek, 2001). In a study by Nadeau et al. (2001), neuromotor problems were found to explain sensitive and isolated behaviors in EPT born 5-years-olds.
However, despite the findings of studies summarized above, showing a consistent association between cognitive impairment and socio-emotional vulnerability in VPT samples, in the majority of cases, cognitive and motor impairments alone do not account for the excess of socio-emotional problems seen in VPT individuals, and further investigation of the etiology of such problems is required (Johnson and Marlow, 2014).
Socio-Emotional Problems Result from Environmental Factors—Early Life Stress and Parenting
Other possible mechanisms that could be studied in order to achieve a greater understanding of the etiology of socio-emotional problems in VPT individuals are environmental factors thought to interact throughout child development. Two principal factors have been described in the preterm literature, namely painful experiences in the perinatal period and parental stress in the early stages of life.
Perinatal Pain Exposure and Socio-Emotional Vulnerability
Together with an increased risk of medical complications, very preterm birth exposes infants to prolonged and repeated pain-related procedures as part of their care in the neonatal intensive care unit. Neonatal pain is quantified as the number of skin-breaking procedures from birth to term equivalent age and has been found to be associated with altered stress hormone (cortisol) regulation and lower motor and cognitive functions at 8 and 18 months corrected age (Grunau et al., 2009). Greater pain-related stress has been recently associated with greater internalizing (anxiety and depression) behaviors at 18 months corrected age (Vinall et al., 2013) and 7 years (Ranger et al., 2014).
Although the role of neonatal pain in the etiology of internalizing behavioral difficulties is unknown, these new findings are in line with results of animal studies which showed that rat pups exposed to neonatal pain exhibited more anxiety-mediated behaviors in adulthood than control animals (Anand et al., 1999). Moreover, recent studies have demonstrated substantial effects of neonatal pain on the vulnerable developing brain, triggering both oxidative stress and inflammatory reactions, affecting the development of preoligodendrocytes and subplate neurons due to the excessive release of glutamate and influxes of calcium (Vinall and Grunau, 2014).
Neonatal pain has been associated with altered white matter microstructure and subcortical delayed gray matter maturation (Smith et al., 2011; Brummelte et al., 2012). These findings are particularly relevant in light of recent studies reporting a predicting role of brain alterations detected in the neonatal period for later socio-emotional behavioral problems (see the Section Brain Correlates of Socio-Emotional and Mental Health Problems).
Parental Stress in the Early Stages of Life
Parental behavior plays a crucial role in the early stages of their child's life, as developmental vulnerability is associated with parents' ability to buffer against high-risk events.
An example of the protective role of parenting is found in the studies described above: among preterm children exposed to greater pain procedures, parental sensitivity and non-hostility were shown to predict reduced internalizing behaviors at both 18 months and 7 years (Vinall et al., 2013; Ranger et al., 2014). Several other studies provided strong evidence for the role of parenting in protecting against early life stress, and in population-based surveys, parenting style and parental mental health (especially depression and anxiety) were shown to modulate socio-emotional development. Maternal distress, in particular, was associated with children's behavioral difficulties and this association held true for VPT children (Treyvaud, 2014).
Preterm birth and hospitalization are highly stressful experiences for parents. Preterm delivery interrupts the normal process of becoming a parent and parenting distress seems to persist long beyond hospital discharge, with parents showing ongoing concerns about their child's health and development. Parents of children born very preterm have been described as having more psychological distress (Huhtala et al., 2011, 2012, 2014; Schappin et al., 2013), depression (Silverstein et al., 2010; Vigod et al., 2010), and post-traumatic stress symptoms (Pierrehumbert et al., 2003; Kersting et al., 2004; Ahlund et al., 2009) than parents of term-born children. Although limited evidence is available regarding the stability of these symptoms, parental functioning seems to improve with time, with the first period of the child's life appearing as the “at-risk” time window for parental mental health (Treyvaud, 2014).
Maternal depression and parental stress may modify a mother's adjustment to her child, her perceptions, attitudes and parenting styles, thereby impacting on the child's socio-emotional outcomes. In support of this hypothesis, parental stress was shown to act as an independent predictor of internalizing behaviors in VLBW 2 year olds (Zelkowitz et al., 2011). Other evidence comes from the investigations of Huhtala et al. (2011, 2012, 2014) who described a significant association between poorer parental mental health and emotional behavioral problems in VLBW 2, 3, and 5 year olds. Similar results were described by Treyvaud et al. (2010, 2012): parental mental health and a more optimal home environment were associated with better socio-emotional regulation in VPT toddlers aged 2 years. Similarly, lower levels of maternal anxiety and intrusivity predicted better social skills also in VPT 4 year olds (Jones et al., 2013). Finally, McCormick et al. (1996) described a negative association between emotional well-being and behavioral problems and maternal mental health in VLBW school aged children.
Maternal depression was found to impact children's social abilities: Silverstein et al. (2010) described an association between maternal depression, negative perceptions of their child's social skills and reduced age appropriate behaviors in a sample of VPT toddlers. Maternal distress was also found to predict internalizing problems and social skills in samples of 36 and 48 months old children, respectively (Miceli et al., 2000; Assel et al., 2002).
These studies highlight the role of parental mental health on a child's socio-emotional development, although not much is known regarding the mechanisms through which parental status may affect different trajectories of socio-emotional development. According to the studies illustrated at the beginning of the section, a possible mechanism could involve a mediating role of parenting on the effect of early stressful adverse life events (Vinall et al., 2013; Ranger et al., 2014), possibly in scaffolding the child's development of self-regulation (Rueda et al., 2004).
Despite this, it is worth noticing that parenting itself is influenced by both children's and parents' characteristics. Therefore, the causal direction of the association between socio-emotional behavioral problems in childhood and parenting is difficult to establish (Treyvaud, 2014).
Developmental Mechanisms Underlying the Association Between Preterm Birth, Socio-Emotional Difficulties and Psychopathology
According to the studies reviewed here, several factors can contribute to the understanding of the association between preterm birth, socio-emotional difficulties and psychopathology. However, further investigation is required to shed light on the mechanisms through which these factors dynamically interplay during development in preterm born samples. In this paper we focused on the description of socio-biological vulnerabilities, neurocognitive/motor deficits and environmental influences as possible factors linking preterm birth and an increased vulnerability to socio-emotional behavioral problems.
Although such factors have been independently associated with the type of socio-emotional problems seen in preterm populations, only a few studies to date have analytically investigated their interactions during the course of development. According to a bio-ecological, transactional, developmental framework (Sameroff and Chandler, 1975; Bronfenbrenner, 1986; Lerner, 1991; Sameroff, 1995), various aspects of development including neural maturation, psycho-social functioning, familiar and cultural environment, dynamically interact in the first years of life. Within this framework, preterm birth concomitantly affects all these aspects of development, precipitating a cascade of neurodevelopmental outcomes which affect the individual, together with the entire family and extended social systems. According to this model, biological vulnerabilities and environmental factors are believed to interdependently interact and contribute to socio-emotional and psychiatric outcomes.
Here we propose an integrative model that takes into account the reciprocal effect of interacting aspects of development (Figure 2). In this model, early brain alterations associated with preterm birth challenge the typical trajectory of brain development and (directly or indirectly) affect socio-emotional development. The effect of neonatal pain and stress may lead to disrupted development of subplate neurons and preoligodendrocytes, which lead to subsequent alterations in brain microstructure. These processes may occur in addition to perinatal brain injury associated with VPT birth and are thought to contribute to later socio-emotional disturbances.
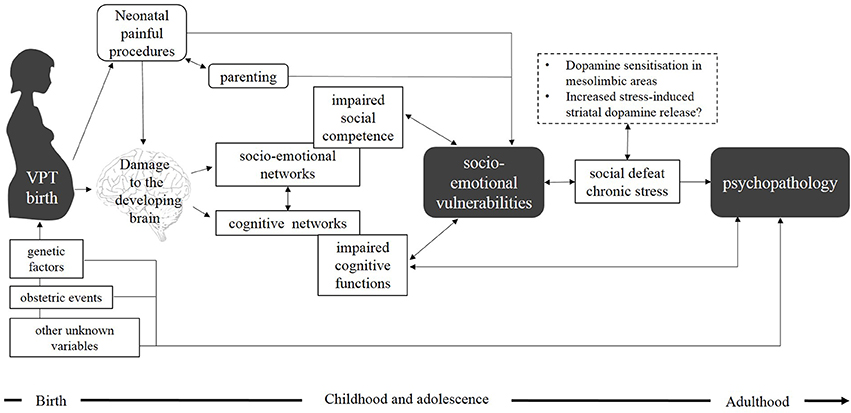
Figure 2. Adapted from Healy et al. (2013) an integrative model showing biological and environmental factors underlying the association between very preterm birth, socio-emotional vulnerabilities, and psychopathology. According to the model, VPT birth (caused by a combination of genetic factors, obstetric events, and other variables) leads to brain alterations in both socio-emotional and cognitive networks. These alterations might underlie socio-emotional vulnerabilities in childhood (possibly due to both deficits in social competence or to more general impaired cognitive functions). Painful procedures and stress experienced during the neonatal period may also impact the development of subplate neurons and preoligodendrocytes, resulting in alterations in brain microstructure. Parenting and parental mental health may mediate the effect of these early adverse events and act either as protective or exacerbating risk factors. Children and adolescents at socio-emotional risk may then be exposed to experiences of social exclusion and social victimization (social defeat and chronic social stress), which have been associated with dopamine sensitization in mesolimbic areas and increased stress-induced striatal dopamine release. We propose that dopamine dysfunction may mediate the association between socio-emotional vulnerabilities and psychopathology and contribute to increased risk of developing psychiatric morbidity in adulthood. In this model we have included a direct reciprocal link between impaired cognitive functions and psychopathology bypassing an intermediate emotional vulnerability stage.
During the first stages of development, parenting and parental mental health mediate offspring's neurodevelopmental outcomes, by acting either as protective or exacerbating risk factors. Parental stress and psychological well-being have in fact been described as being fundamental for a healthy development of self-regulatory abilities and socio-emotional development. Compromised parent-child interactions may confer a further developmental risk for socio-emotional problems.
The complex interplay between these factors place preterm individuals at increased risk for socio-emotional behavioral problems, and these in turn contribute to the risk of developing psychiatric disorder later in life. The association between behavioral problems and psychopathology is supported by the social defeat hypothesis of mental disorders, which suggests that psychiatric vulnerability is increased due to the effect of socio-emotional difficulties on children's experiences of social exclusion and social victimization. Social stress and isolation may affect the dopamine system through a process of dopamine sensitization or increased stress-induced dopamine release. This dopaminergic dysfunction has been associated with an increased risk for psychopathology. Whilst this is the framework we are using in our review, we also acknowledge research which has suggested a direct reciprocal link between impaired cognitive functions and psychopathology bypassing an intermediate emotional vulnerability stage (McGrath et al., 2015).
When considering the possible causal relationship between these factors, a large number of other variables need to be taken into account, as a series of morbidities commonly associated with preterm birth can contribute to the association between socio-emotional difficulties and psychopathology. For instance, parental psychiatric history has been described as a risk factor for both preterm birth and child's psychopathology, making it more difficult to disentangle the relative contribution of prematurity to psychiatric outcomes. Moreover, genetic factors may be included in this model, as specific genetic variants have been associated with an increased risk for psychopathology in conditions of biological risk (Cannon et al., 2002; Dean et al., 2010; Nosarti, 2013).
Biological risk may include early brain insults associated with VPT birth, such as hypoxia/ischemia and periventricular leukomalacia (Volpe, 2009). Animal models suggest early brain injury leads to altered prefrontal-hippocampal development leading in turn to increased striatal dopamine release (Mittal et al., 2008). In this context, neurodevelopmental alterations may produce lasting effects on dopamine function, increasing mesolimbic dopamine response to stressful stimuli (Boksa and El-Khodor, 2003; Lipska, 2004; Boksa, 2010). As previously described, dopaminergic dysfunction is associated with an increased susceptibility to environmental stressors and an increased risk of psychopathology. According to these studies, dopamine dysregulation (following perinatal brain lesions) provides a rational mechanism linking premature brain injuries to psychopathology, but further work is clearly needed to elucidate exactly how perinatal lesions can affect the dopamine system and in turn increase the risk for socio-emotional and psychiatric problems.
Conclusions
The studies summarized in this article indicate that socio-emotional disturbances are highly prevalent among samples of individuals who were born very preterm and that preterm birth represents an independent risk factor for psychiatric disorder.
In order to increase our understanding of the association between VPT birth and vulnerability to developing socio-emotional and psychiatric problems we explored the complex interplay between biological vulnerabilities and environmental influences, including functional and structural brain alterations, neonatal pain and stress and non-optimal parenting strategies. We hypothesized that the association between socio-emotional difficulties and psychopathology may be mediated by a repeated experience of psychosocial stress and social defeat, resulting in lasting effects on dopaminergic function, leading to behavioral impairments.
A broader understanding of the complex interactions amongst biological and environmental factors remains the goal of further investigations. The elucidation of the mechanisms linking preterm birth, socio-emotional and psychiatric problems could provide an evidence-based rationale for developing and delivering new effective interventions meant to specifically reinforce protective factors (e.g., intervention on parental stress) or to target specific factors found to be precursors of socio-emotional and psychiatric difficulties in preterm born individuals.
New findings on early markers of outcome will help us explain the cascade of socio-emotional behavioral difficulties often described in preterm born individuals, will provide a better understanding of their brain substrates and will open the way to new effective contributions to support child development.
Author Contributions
AM: Study conception and design, data interpretation and write up. CN: Study conception and design, data interpretation and write up.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The study was supported by the Medical Research Council, UK (ref. MR/K004867/1 and MR/K0006355/1). We thank the National Institute for Health Research (NIHR) Biomedical Research Centre at South London, Maudsley NHS Foundation Trust, Centre for the Developing Brain, Division of Imaging Sciences and Biomedical Engineering, King's College London, King's Health Partners, and St. Thomas' Hospital for their continuing support.
References
Aanes, S., Bjuland, K. J., Skranes, J., and Løhaugen, G. C. C. (2015). Memory function and hippocampal volumes in preterm born very-low-birth-weight (VLBW) young adults. Neuroimage 105, 76–83. doi: 10.1016/j.neuroimage.2014.10.023
Aarnoudse-Moens, C. S. H., Weisglas-Kuperus, N., van Goudoever, J. B., and Oosterlaan, J. (2009). Meta-analysis of neurobehavioral outcomes in very preterm and/or very low birth weight children. Pediatrics 124, 717–728. doi: 10.1542/peds.2008-2816
Abel, K. M., Wicks, S., Susser, E. S., Dalman, C., Pedersen, M. G., Mortensen, P. B., et al. (2010). Birth weight, schizophrenia, and adult mental disorder: is risk confined to the smallest babies? Arch. Gen. Psychiatry 67, 923–930. doi: 10.1001/archgenpsychiatry.2010.100
Abernethy, L. J., Cooke, R. W. I., and Foulder-Hughes, L. (2004). Caudate and hippocampal volumes, intelligence, and motor impairment in 7-year-old children who were born preterm. Pediatr. Res. 55, 884–893. doi: 10.1203/01.PDR.0000117843.21534.49
Achenbach, T. (1992). Manual for the Child Behavior Checklist/2-3 and 1992 Profile. Burlington, VT: University of Vermont Department of Psychiatry.
Achenbach, T. (1991). Manual for the Child Behavior Checklist/4—18 and 1991 Profile. Burlington, VT: University of Vermont Department of Psychiatry.
Ahlund, S., Clarke, P., Hill, J., and Thalange, N. K. S. (2009). Post-traumatic stress symptoms in mothers of very low birth weight infants 2-3 years post-partum. Arch. Women's Ment. Health 12, 261–264. doi: 10.1007/s00737-009-0067-4
Alati, R., Lawlor, D. A., Mamun, A. A. L., Williams, G. M., Najman, J. M., Bor, W., et al. (2007). Is there a fetal origin of depression? Evidence from the Mater University Study of Pregnancy and its outcomes. Am. J. Epidemiol. 165, 575–582. doi: 10.1093/aje/kwk036
Alduncin, N., Huffman, L. C., Feldman, H. M., and Loe, I. M. (2014). Executive function is associated with social competence in preschool-aged children born preterm or full term. Early Hum. Dev. 90, 299–306. doi: 10.1016/j.earlhumdev.2014.02.011
Allin, M., Rooney, M., Cuddy, M., Wyatt, J., Walshe, M., Rifkin, L., et al. (2006). Personality in young adults who are born preterm. Pediatrics 117, 309–316. doi: 10.1542/peds.2005-0539
Anand, K. J., Coskun, V., Thrivikraman, K. V., Nemeroff, C. B., and Plotsky, P. M. (1999). Long-term behavioral effects of repetitive pain in neonatal rat pups. Physiol. Behav. 66, 627–637. doi: 10.1016/S0031-9384(98)00338-2
Anderson, P. J. (2014). Neuropsychological outcomes of children born very preterm. Semin. Fetal Neonatal Med. 19, 90–96. doi: 10.1016/j.siny.2013.11.012
Arnsten, A. F. T., and Rubia, K. (2012). Neurobiological circuits regulating attention, cognitive control, motivation, and emotion: Disruptions in neurodevelopmental psychiatric disorders. J. Am. Acad. Child Adolesc. Psychiatry 51, 356–367. doi: 10.1016/j.jaac.2012.01.008
Arpi, E., and Ferrari, F. (2013). Preterm birth and behaviour problems in infants and preschool-age children: a review of the recent literature. Dev. Med. Child Neurol. 55, 788–796. doi: 10.1111/dmcn.12142
Assel, M. A., Landry, S. H., Swank, P. R., Steelman, L., Miller-Loncar, C., and Smith, K. E. (2002). How do mothers' childrearing histories, stress and parenting affect children's behavioural outcomes? Child Care Health Dev. 28, 359–368. doi: 10.1046/j.1365-2214.2002.00285.x
Ball, G., Boardman, J. P., Aljabar, P., Pandit, A., Arichi, T., Merchant, N., et al. (2013). The influence of preterm birth on the developing thalamocortical connectome. Cortex 49, 1711–1721. doi: 10.1016/j.cortex.2012.07.006
Ball, G., Pazderova, L., Chew, A., Tusor, N., Merchant, N., Arichi, T., et al. (2015). Thalamocortical connectivity predicts cognition in children born preterm. Cereb. Cortex 25, 4310–4318. doi: 10.1093/cercor/bhu331
Baron-Cohen, S. (1991). “Precursors to a theory of mind: understanding attention in others,” in Natural Theories of Mind: Evolution, Development and Simulation of Everyday Mindreading, ed A. Whiten (Cambridge, MA: Basil Blackwell), 233–251.
Bayless, S. J., Pit-ten Cate, I. M., and Stevenson, J. (2008). Behaviour difficulties and cognitive function in children born very prematurely. Int. J. Behav. Dev. 32, 199–206. doi: 10.1177/0165025408089269
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M., and Anand, K. J. (2002). Cognitive and behavioral outcomes of school-aged children who were born preterm: a meta-analysis. J. Am. Med. Assoc. 288, 728–737. doi: 10.1001/jama.288.6.728
Blakemore, S.-J. (2008). The social brain in adolescence. Nat. Rev. Neurosci. 9, 267–277. doi: 10.1038/nrn2353
Boksa, P., and El-Khodor, B. F. (2003). Birth insult interacts with stress at adulthood to alter dopaminergic function in animal models: Possible implications for schizophrenia and other disorders. Neurosci. Biobehav. Rev. 27, 91–101. doi: 10.1016/S0149-7634(03)00012-5
Boksa, P. (2010). Effects of prenatal infection on brain development and behavior: a review of findings from animal models. Brain Behav. Immun. 24, 881–897. doi: 10.1016/j.bbi.2010.03.005
Bornstein, M. H., Hahn, C.-S., and Haynes, O. M. (2010). Social competence, externalizing, and internalizing behavioral adjustment from early childhood through early adolescence: developmental cascades. Dev. Psychopathol. 22, 717–735. doi: 10.1017/S0954579410000416
Botting, N., Powls, A., Cooke, R. W., and Marlow, N. (1997). Attention deficit hyperactivity disorders and other psychiatric outcomes in very low birthweight children at 12 years. J. Child Psychol. Psychiatry 38, 931–941. doi: 10.1111/j.1469-7610.1997.tb01612.x
Boyle, M. H., Miskovic, V., Van Lieshout, R., Duncan, L., Schmidt, L. A., Hoult, L., et al. (2011). Psychopathology in young adults born at extremely low birth weight. Psychol. Med. 41, 1763–1774. doi: 10.1017/S0033291710002357
Briggs-Gowan, M. J., and Carter, A. S. (2008). Social-emotional screening status in early childhood predicts elementary school outcomes. Paediatrics 121, 957–962. doi: 10.1542/peds.2007-1948
Bronfenbrenner, U. (1986). Ecology of the family as a context for human development: research perspectives. Dev. Psychol. 22, 723–742. doi: 10.1037/0012-1649.22.6.723
Brummelte, S., Grunau, R. E., Chau, V., Poskitt, K. J., Brant, R., Vinall, J., et al. (2012). Procedural pain and brain development in premature newborns. Ann. Neurol. 71, 385–396. doi: 10.1002/ana.22267
Brummelte, S., Chau, C. M. Y., Cepeda, I. L., Degenhardt, A., Weinberg, J., Synnes, A. R., et al. (2015). Cortisol levels in former preterm children at school age are predicted by neonatal procedural pain-related stress. Psychoneuroendocrinology 51, 151–163. doi: 10.1016/j.psyneuen.2014.09.018
Burnett, A. C., Anderson, P. J., Cheong, J., Doyle, L. W., Davey, C. G., and Wood, S. J. (2011). Prevalence of psychiatric diagnoses in preterm and full-term children, adolescents and young adults: a meta-analysis. Psychol. Med. 41, 2463–2474. doi: 10.1017/S003329171100081X
Carlson, S. M., and Moses, L. J. (2001). Individual differences in inhibitory control and children's theory of mind. Child Dev. 72, 1032–1053. doi: 10.1111/1467-8624.00333
Cannon, M., Jones, P. B., and Murray, R. M. (2002). Obstetric complications and schizophrenia: historical and meta-analytic review. Am. J. Psychiatry 159, 1080–1092. doi: 10.1176/appi.ajp.159.7.1080
Cannon, M., Jones, P., Gilvarry, C., Rifkin, L., McKenzie, K., Foerster, A., and Murray, R. M. (1997). Premorbid social functioning in schizophrenia and bipolar disorder: similarities and differences. Am. J. Psychiatry 154, 1544–1550.
Carpenter, M., Nagell, K., and Tomasello, M. (1998). Social cognition, joint attention, and communicative competence from 9 to 15 months of age. Monogr. Soc. Res. Child Dev. 63, 1–143. doi: 10.2307/1166214
Carter, A. S., Briggs-Gowan, M. J., and Davis, N. O. (2004). Assessment of young children's social-emotional development and psychopathology: recent advances and recommendations for practice. J. Child Psychol. Psychiatry 45, 109–134. doi: 10.1046/j.0021-9630.2003.00316.x
Clark, C. A. C., Woodward, L. J., Horwood, J. L., and Moor, S. (2008). Development of emotional and behavioral regulation in children born extremely preterm and very preterm: biological and social influences. Child Dev. 79, 1444–1462. doi: 10.1111/j.1467-8624.2008.01198.x
Clark, C., Prior, M., and Kinsella, G. (2002). The relationship between executive function abilities, adaptive, behaviour, and academic achievement in children with externalising behaviour problems. J. Child Psychol. Psychiatry Allied Discipl. 43, 785–796. doi: 10.1111/1469-7610.00084
Clerkin, S. M., Schulz, K. P., Berwid, O. G., Fan, J., Newcorn, J. H., Tang, C. Y., et al. (2013). Thalamo-cortical activation and connectivity during response preparation in adults with persistent and remitted ADHD. Am. J. Psychiatry 170, 1011–1019. doi: 10.1176/appi.ajp.2013.12070880
Cnattingius, S., Hultman, C. M., Dahl, M., and Sparén, P. (1999). Very preterm birth, birth trauma, and the risk of anorexia nervosa among girls. Arch. Gen. Psychiatry 56, 634–638. doi: 10.1001/archpsyc.56.7.634
Cole, P. M., Michel, M. K., and Teti, L. O. (1994). The development of emotion regulation and dysregulation: a clinical perspective. Monogr. Soc. Res. Child Dev. 59, 73–100.
Cooke, R. W. I. (2004). Health, lifestyle, and quality of life for young adults born very preterm. Arch. Dis. Child. 89, 201–206. doi: 10.1136/adc.2003.030197
Corbetta, M., Patel, G., and Shulman, G. L. (2008). The reorienting system of the human brain: from environment to theory of mind. Neuron 58, 306–324. doi: 10.1016/j.neuron.2008.04.017
Crump, C., Winkleby, M. A., Sundquist, K., and Sundquist, J. (2010). Preterm birth and psychiatric medication prescription in young adulthood: a Swedish national cohort study. Int. J. Epidemiol. 39, 1522–1530. doi: 10.1093/ije/dyq103
Dahl, L. B., Kaaresen, P. I., Tunby, J., Handegård, B. H., Kvernmo, S., and Rønning, J. A. (2006). Emotional, behavioral, social, and academic outcomes in adolescents born with very low birth weight. Pediatrics 118, 449–459. doi: 10.1542/peds.2005-3024
Darlow, B. A., Horwood, L. J., Pere-Bracken, H. M., and Woodward, L. J. (2013). Psychosocial outcomes of young adults born very low birth weight. Pediatrics 132, e1521–e1528. doi: 10.1542/peds.2013-2024
Delobel-Ayoub, M., Arnaud, C., White-Koning, M., Casper, C., Pierrat, V., Garel, M., et al. (2009). Behavioral problems and cognitive performance at 5 years of age after very preterm birth: the EPIPAGE Study. Pediatrics 123, 1485–1492. doi: 10.1542/peds.2008-1216
Dean, K., Stevens, H., Mortensen, P. B., Murray, R. M., Walsh, E., and Pedersen, C. B. (2010). Full spectrum of psychiatric outcomes among offspring with parental history of mental disorder. Arch. Gen. Psychiatry 67, 822–829. doi: 10.1001/archgenpsychiatry.2010.86
Denham, S. A., Blair, K. A., DeMulder, E., Levitas, J., Sawyer, K., Auerbach-Major, S., et al. (2003). Preschool emotional competence: pathway to social competence? Child Dev. 74, 238–256. doi: 10.1111/1467-8624.00533
Diamond, A. (2005). Attention-deficit disorder (attention-deficit/ hyperactivity disorder without hyperactivity): a neurobiologically and behaviorally distinct disorder from attention-deficit/hyperactivity disorder (with hyperactivity). Dev. Psychopathol. 17, 807–825. doi: 10.1017/S0954579405050388
Dunn, J. R. (2010). Health behavior vs the stress of low socioeconomic status and health outcomes. JAMA 303, 1199–1200. doi: 10.1001/jama.2010.332
Eisenberg, D. P., and Berman, K. F. (2010). Executive function, neural circuitry, and genetic mechanisms in schizophrenia. Neuropsychopharmacology? 35, 258–277. doi: 10.1038/npp.2009.111
Elgen, I., Sommerfelt, K., and Markestad, T. (2002). Population based, controlled study of behavioural problems and psychiatric disorders in low birthweight children at 11 years of age. Arch. Disease Childhood Fetal Neonatal Edit. 87, F128–F132. doi: 10.1136/fn.87.2.F128
Emde, R. N., Bingham, R. D., and Harmon, R. J. (1993). “Classification and the diagnostic process in infancy,” in Handbook of Infant Mental Health, ed C. H. Jr. Zeanah (New York, NY: Guilford Publications), 225–235.
Eryigit-Madzwamuse, S., Strauss, V., Baumann, N., Bartmann, P., and Wolke, D. (2015). Personality of adults who were born very preterm. Arch. Dis. Child. Fetal Neonatal Ed. 100, F524–F529. doi: 10.1136/archdischild-2014-308007
Fanaroff, A. A., Hack, M., and Walsh, M. C. (2003). The NICHD Neonatal Research Network: changes in practice and outcomes during the first 15 years. Semin. Perinatol. 27, 281–287. doi: 10.1016/S0146-0005(03)00055-7
Farooqi, A., Hägglöf, B., Sedin, G., Gothefors, L., and Serenius, F. (2007). Mental health and social competencies of 10- to 12-year-old children born at 23 to 25 weeks of gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics 120, 118–133. doi: 10.1542/peds.2006-2988
Feldman, R. (2007). Parent-infant synchrony and the construction of shared timing; physiological precursors, developmental outcomes, and risk conditions. J. Child Psychol. Psychiatry Allied Discipl. 48, 329–354. doi: 10.1111/j.1469-7610.2006.01701.x
Fischi-Gómez, E., Vasung, L., Meskaldji, D.-E., Lazeyras, F., Borradori-Tolsa, C., Hagmann, P., et al. (2015). Structural brain connectivity in school-age preterm infants provides evidence for impaired networks relevant for higher order cognitive skills and social cognition. Cereb. Cortex 25, 2793–2805. doi: 10.1093/cercor/bhu073
Fombonne, E. (2009). Epidemiology of pervasive developmental disorders. Pediatr. Res. 65, 591–598. doi: 10.1203/PDR.0b013e31819e7203
Gadeyne, E., Ghesquiere, P., and Onghena, P. (2004). Psychosocial functioning of young children with learning problems. Journal of Child Psychology & Psychiatry 45, 510–521. doi: 10.1111/j.1469-7610.2004.00241.x
Gale, C. R., and Martyn, C. N. (2004). Birth weight and later risk of depression in a national birth cohort. Br. J. Psychiatry 184, 28–33. doi: 10.1192/bjp.184.1.28
Ganella, E. P., Burnett, A., Cheong, J., Thompson, D., Roberts, G., Wood, S., et al. (2015). Abnormalities in orbitofrontal cortex gyrification and mental health outcomes in adolescents born extremely preterm and/or at an extremely low birth weight. Hum. Brain Mapp. 36, 1138–1150. doi: 10.1002/hbm.22692
Gardner, F., Johnson, A., Yudkin, P., Bowler, U., Hockley, C., Mutch, L., et al. (2004). Behavioral and emotional adjustment of teenagers in mainstream school who were born before 29 weeks' gestation. Pediatrics 114, 676–682. doi: 10.1542/peds.2003-0763-L
Garner, P. W., Landry, S. H., and Richardson, M. A. (1991). The development of joint attention skills in very-low-birth-weight infants across the first 2 years. Infant Behav. Dev. 14, 489–495. doi: 10.1016/0163-6383(91)90035-Q
Gimenez, M., Junque, C., Vendrell, P., Narberhaus, A., Bargallo, N., Botet, F., et al. (2006). Abnormal orbitofrontal development due to prematurity. Neurology 67, 1818–1822. doi: 10.1212/01.wnl.0000244485.51898.93
Goldenberg, R. L., Culhane, J. F., Iams, J. D., and Romero, R. (2008). Epidemiology and causes of preterm birth. Lancet 371, 75–84. doi: 10.1016/S0140-6736(08)60074-4
Goodman, R., Simonoff, E., and Stevenson, J. (1995). The impact of child IQ, parent IQ and sibling IQ on child behavioural deviance scores. J. Child Psychol. Psychiatry 36, 409–425. doi: 10.1111/j.1469-7610.1995.tb01299.x
Goodman, R. (1997). The strengths and difficulties questionnaire: a research note. J. Child Psychol. Psychiatry 38, 581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x
Gousias, I. S., Edwards, A. D., Rutherford, M. A., Counsell, S. J., Hajnal, J. V., Rueckert, D., et al. (2012). Magnetic resonance imaging of the newborn brain: manual segmentation of labelled atlases in term-born and preterm infants. Neuroimage 62, 1499–1509. doi: 10.1016/j.neuroimage.2012.05.083
Grunau, R. E., Whitfield, M. F., Petrie-Thomas, J., Synnes, A. R., Cepeda, I. L., Keidar, A., et al. (2009). Neonatal pain, parenting stress and interaction, in relation to cognitive and motor development at 8 and 18 months in preterm infants. Pain 143, 138–146. doi: 10.1016/j.pain.2009.02.014
Grunau, R. E. (2013). Neonatal pain in very preterm infants: long-term effects on brain, neurodevelopment and pain reactivity. Rambam Maimonides. Med. J. 4:e0025. doi: 10.5041/RMMJ.10132
Grunau, R. E., Whitfield, M. F., and Fay, T. B. (2004). Psychosocial and academic characteristics of extremely low birth weight (< or =800 g) adolescents who are free of major impairment compared with term-born control subjects. Pediatrics 114, e725–e732. doi: 10.1542/peds.2004-0932
Hack, M., Youngstrom, E. A., Cartar, L., Schluchter, M., Taylor, H. G., Flannery, D., et al. (2004). Behavioral outcomes and evidence of psychopathology among very low birth weight infants at age 20 years. Pediatrics 114, 932–940. doi: 10.1542/peds.2003-1017-L
Hack, M. (2006). Young adult outcomes of very-low-birth-weight children. Sem. Fetal Neonatal Med. 11, 127–137. doi: 10.1016/j.siny.2005.11.007
Hack, M., Taylor, H. G., Schluchter, M., Andreias, L., Drotar, D., and Klein, N. (2009). Behavioral outcomes of extremely low birth weight children at age 8 years. J. Dev. Behav. Pediatrics 30, 122–130. doi: 10.1097/DBP.0b013e31819e6a16
Hack, M., and Taylor, H. G. (2000). Perinatal brain injury in preterm infants and later neurobehavioral function. JAMA 284, 11–12. doi: 10.1001/jama.284.15.1973
Hack, M., Flannery, D. J., Schluchter, M., Cartar, L., Borawski, E., and Klein, N. (2002). Outcomes in young adulthood for very-low-birth-weight infants. New England J. Med. 346, 149–157. doi: 10.1056/NEJMoa010856
Hall, J., and Wolke, D. (2012). A comparison of prematurity and small for gestational age as risk factors for age 6-13 year emotional problems. Early Hum. Dev. 88, 797–804. doi: 10.1016/j.earlhumdev.2012.05.005
Halmøy, A., Klungsøyr, K., Skjærven, R., and Haavik, J. (2012). Pre- and perinatal risk factors in adults with attention-deficit/hyperactivity disorder. Biol. Psychiatry 71, 474–481. doi: 10.1016/j.biopsych.2011.11.013
Happé, F., and Frith, U. (2014). Annual research review: towards a developmental neuroscience of atypical social cognition. J. Child Psychol. Psychiatry Allied Discipl. 55, 553–577. doi: 10.1111/jcpp.12162
Healy, E., Reichenberg, A., Nam, K. W., Allin, M. P. G., Walshe, M., Rifkin, L., et al. (2013). Preterm birth and adolescent social functioning-alterations in emotion-processing brain areas. J. Pediatrics 163, 1596–1604. doi: 10.1016/j.jpeds.2013.08.011
Heiervang, E., Stevenson, J., Lund, A., and Hugdahl, K. (2001). Behaviour problems in children with dyslexia. Nord. J. Psychiatry 55, 251–256. doi: 10.1080/080394801681019101
Hertz, C. L., Mathiasen, R., Hansen, B. M., Mortensen, E. L., and Greisen, G. (2013). Personality in adults who were born very preterm. PLoS ONE 8:e66881. doi: 10.1371/journal.pone.0066881
Hille, E. T. M., Den Ouden, A. L., Saigal, S., Wolke, D., Lambert, M., Paneth, N., et al. (2001). Behavioural problems in children who weigh 1000 g or less at birth in four countries. Lancet 357, 1641–1643. doi: 10.1016/S0140-6736(00)04818-2
Hille, E. T. M., Dorrepaal, C., Perenboom, R., Gravenhorst, J. B., Brand, R., and Verloove-Vanhorick, S. P. (2008). Social lifestyle, risk-taking behavior, and psychopathology in young adults born very preterm or with a very low birthweight. J. Pediatrics 152, 793–800. e1–e4. doi: 10.1016/j.jpeds.2007.11.041
Hughes, C., White, A., Sharpen, J., and Dunn, J. (2000). Antisocial, angry, and unsympathetic: “hard-to-manage” preschoolers' peer problems and possible cognitive influences. J. Child Psychol. Psychiatry 41, 169–179. doi: 10.1017/S0021963099005193
Huhtala, M., Korja, R., Lehtonen, L., Haataja, L., Lapinleimu, H., Munck, P., et al. (2011). Parental psychological well-being and cognitive development of very low birth weight infants at 2 years. Acta Paediatrica (Oslo, Norway?: 1992), 100, 1555–1560. doi: 10.1111/j.1651-2227.2011.02428.x
Huhtala, M., Korja, R., Lehtonen, L., Haataja, L., Lapinleimu, H., and Rautava, P. (2012). Parental psychological well-being and behavioral outcome of very low birth weight infants at 3 years. Pediatrics 129, e937–e944. doi: 10.1542/peds.2011-2411
Huhtala, M., Korja, R., Lehtonen, L., Haataja, L., Lapinleimu, H., Rautava, P., et al. (2014). Associations between parental psychological well-being and socio-emotional development in 5-year-old preterm children. Early Hum. Dev. 90, 119–124. doi: 10.1016/j.earlhumdev.2013.12.009
Hutchinson, E. A., De Luca, C. R., Doyle, L. W., Roberts, G., and Anderson, P. J. (2013). School-age outcomes of extremely preterm or extremely low birth weight children. Pediatrics 131, e1053–e1061. doi: 10.1542/peds.2012-2311
Iarocci, G., Yager, J., and Elfers, T. (2007). What gene-environment interactions can tell us about social competence in typical and atypical populations. Brain Cogn. 65, 112–127. doi: 10.1016/j.bandc.2007.01.008
Indredavik, M. S., Vik, T., Heyerdahl, S., Kulseng, S., Fayers, P., and Brubakk, A.-M. (2004). Psychiatric symptoms and disorders in adolescents with low birth weight. Arch. Disease Childhood Fetal Neonatal Edn. 89, F445–F450. doi: 10.1136/adc.2003.038943
Indredavik, M. S., Skranes, J. S., Vik, T., Heyerdahl, S., Romundstad, P., Myhr, G. E., et al. (2005). Low-birth-weight adolescents: psychiatric symptoms and cerebral MRI abnormalities. Pediatr. Neurol. 33, 259–266. doi: 10.1016/j.pediatrneurol.2005.05.002
Janssen, A. J. W. M., Nijhuis-van Der Sanden, M. W. G., Akkermans, R. P., Oostendorp, R. A. B., and Kollée, L. A. A. (2008). Influence of behaviour and risk factors on motor performance in preterm infants at age 2 to 3 years. Dev. Med. Child Neurol. 50, 926–931. doi: 10.1111/j.1469-8749.2008.03108.x
Janssens, A., Uvin, K., Van Impe, H., Laroche, S. M. F., Van Reempts, P., and Deboutte, D. (2009). Psychopathology among preterm infants using the Diagnostic Classification Zero to Three. Acta Paediatr. 98, 1988–1993. doi: 10.1111/j.1651-2227.2009.01488.x
Johnson, S., Hollis, C., Kochhar, P., Hennessy, E., Wolke, D., and Marlow, N. (2010a). Autism spectrum disorders in extremely preterm children. J. Pediatrics 156, 525–531.e2. doi: 10.1016/j.jpeds.2009.10.041
Johnson, S., Hollis, C., Kochhar, P., Hennessy, E., Wolke, D., and Marlow, N. (2010b). Psychiatric disorders in extremely preterm children: longitudinal finding at age 11 years in the EPICure study. J. Am. Acad. Child Adolesc. Psychiatry 49, 453–463.e1. doi: 10.1097/00004583-201005000-00006
Johnson, S., Hennessy, E., Smith, R., Trikic, R., Wolke, D., and Marlow, N. (2009). Academic attainment and special educational needs in extremely preterm children at 11 years of age: the EPICure study. Arch. Disease Childhood. Fetal Neonatal Edn. 94, F283–F289. doi: 10.1136/adc.2008.152793
Johnson, S., and Marlow, N. (2011). Preterm birth and childhood psychiatric disorders. Pediatr. Res. 69, 22–28. doi: 10.1203/PDR.0b013e318212faa0
Johnson, S., and Marlow, N. (2014). Growing up after extremely preterm birth: lifespan mental health outcomes. Semin. Fetal Neonatal Med. 19, 97–104. doi: 10.1016/j.siny.2013.11.004
Johnson, S., and Wolke, D. (2013). Behavioural outcomes and psychopathology during adolescence. Early Hum. Dev. 89, 199–207. doi: 10.1016/j.earlhumdev.2013.01.014
Jones, K. M., Champion, P. R., and Woodward, L. J. (2013). Social competence of preschool children born very preterm. Early Hum. Dev. 89, 795–802. doi: 10.1016/j.earlhumdev.2013.06.008
Kajantie, E., Hovi, P., Räikkönen, K., Pesonen, A.-K., Heinonen, K., Järvenpä, A.-L., et al. (2008). Young adults with very low birth weight: leaving the parental home and sexual relationships—Helsinki study of very low birth weight adults. Pediatrics 122, e62–e72. doi: 10.1542/peds.2007-3858
Karmiloff-Smith, A., D'Souza, D., Dekker, T. M., Van Herwegen, J., Xu, F., Rodic, M., et al. (2012). Genetic and environmental vulnerabilities in children with neurodevelopmental disorders. Proc. Natl. Acad. Sci. U.S.A. 109, 17261–17265. doi: 10.1073/pnas.1121087109
Karolis, V. R., Froudist-Walsh, S., Brittain, P. J., Kroll, J., Ball, G., Edwards, A. D., et al. (2016). Reinforcement of the brain's rich-club architecture following early neurodevelopmental disruption caused by very preterm birth. Cereb. Cortex 26, 1322–1335. doi: 10.1093/cercor/bhv305
Kendler, K. S., Gatz, M., Gardner, C. O., and Pedersen, N. L. (2006). Personality and major depression. Arch. Gen. Psychiatry 63, 1113–1120. doi: 10.1001/archpsyc.63.10.1113
Kennedy, D. P., and Adolphs, R. (2012). The social brain in psychiatric and neurological disorders. Trends Cogn. Sci. 16, 559–572. doi: 10.1016/j.tics.2012.09.006
Kerr-Wilson, C. O., MacKay, D. F., Smith, G. C. S., and Pell, J. P. (2012). Meta-analysis of the association between preterm delivery and intelligence. J. Public Health 34, 209–216. doi: 10.1093/pubmed/fdr024
Kersting, A., Dorsch, M., Wesselmann, U., Lüdorff, K., Witthaut, J., Ohrmann, P., et al. (2004). Maternal posttraumatic stress response after the birth of a very low-birth-weight infant. J. Psychosom. Res. 57, 473–476. doi: 10.1016/j.jpsychores.2004.03.011
Kieviet, J. F., Piek, J. P., Aarnoudse-Moens, C. S., and Oosterlaan, J. (2009). Motor development in very preterm and very low-birth-weight children. Am. Med. Associat. 302, 2235–2242. doi: 10.1001/jama.2009.1708
Kostović, I., and Judaš, M. (2010). The development of the subplate and thalamocortical connections in the human foetal brain. Acta Paediatr. 99, 1119–1127. doi: 10.1111/j.1651-2227.2010.01811.x
Kostović, I., and Jovanov-Milošević, N. (2006). The development of cerebral connections during the first 20-45 weeks' gestation. Sem. Fetal Neonatal Med. 11, 415–422. doi: 10.1016/j.siny.2006.07.001
Kuntsi, J., Oosterlaan, J., and Stevenson, J. (2001). Psychological mechanisms in hyperactivity: I. Response inhibition deficit, working memory impairment, delay aversion, or something else? J. Child Psychol. Psychiatry Allied Discipl. 42, 199–210. doi: 10.1111/1469-7610.00711
Landry, S. H. (1986). Preterm infants' responses in early joint attention interactions. Infant Behav. Dev. 9, 1–14. doi: 10.1016/0163-6383(86)90034-2
Landry, S. H., Chapieski, M. L., Richardson, M. A., Palmer, J., and Hall, S. (1990). The social competence of children born prematurely: effects of medical complications and parent behaviors. Child Dev. 61, 1605–1616. doi: 10.2307/1130768
Lawson, K. R., and Ruff, H. A. (2004). Early attention and negative emotionality predict later cognitive and behavioural function. Int. J. Behav. Dev. 28, 157–165. doi: 10.1080/01650250344000361
Lerner, R. M. (1991). Changing organism-context relations as the basic process of development: a developmental context perspective. Dev. Psychol. 27, 27–32. doi: 10.1037/0012-1649.27.1.27
Levy-Shiff, R., Einat, G., Har-Even, D., Mogilner, S., Lerman, M., and Krikler, R. (1994). Emotional and behavioral adjustment in children born prematurely. J. Clin. Child Psychol. 23, 323–333. doi: 10.1207/s15374424jccp2303_10
Limperopoulos, C., Bassan, H., Gauvreau, K., Robertson, R. L., Sullivan, N. R., Benson, C. B., et al. (2007). Does cerebellar injury in premature infants contribute to the high prevalence of long-term cognitive, learning, and behavioral disability in survivors? Pediatrics 120, 584–593. doi: 10.1542/peds.2007-1041
Lindström, K., Winbladh, B., Haglund, B., and Hjern, A. (2007). Preterm infants as young adults: a Swedish national cohort study. Pediatrics 120, 70–77. doi: 10.1542/peds.2006-3260
Lipska, B. K. (2004). Using animal models to test a neurodevelopmental hypothesis of schizophrenia. CRSN Symposium 29, 282–286.
Loe, I. M., Lee, E. S., and Feldman, H. M. (2013). Attention and internalizing behaviors in relation to white matter in children born preterm. J. Dev. Behav. Pediatr. 34, 156–164. doi: 10.1097/DBP.0b013e3182842122
Lund, L. K., Vik, T., Lydersen, S., Løhaugen, G. C. C., Skranes, J., Brubakk, A.-M., et al. (2012). Mental health, quality of life and social relations in young adults born with low birth weight. Health Q. Life Outcomes 10:146. doi: 10.1186/1477-7525-10-146
Makinson, C. D., and Huguenard, J. R. (2014). Attentional flexibility in the thalamus: now we're getting SOMwhere. Nat. Neurosci. 18, 2–4. doi: 10.1038/nn.3902
Männistö, T., Vääräsmäki, M., Sipola-leppänen, M., and Tikanmäki, M. (2015). Independent living and romantic relations among young adults born preterm. Pediatrics 135, 290–297. doi: 10.1542/peds.2014-1345
Mansson, J., Stjernqvist, K., and Backstrom, M. (2014). Behavioral outcomes at corrected age 2.5 years in children born extremely preterm. J. Dev. Behav. Pediatr. 35, 435–442. doi: 10.1097/DBP.0000000000000082
Masten, A. S., Burt, K. B., and Coatsworth, J. D. (2006). “Competence and psychopathology in development,” in Developmental Psychopathology, 2nd Edn.Vol. 3, eds D. Cicchetti and D. J. Cohen (NewYork, NY: Wiley), 696–738.
McCormick, M. C., Workman-Daniels, K., and Brooks-Gunn, J. (1996). The behavioral and emotional well-being of school-age children with different birth weights. Pediatrics 97, 18–25.
McGrath, L. M., Braaten, E. B., Doty, N. D., Willoughby, B. L., Wilson, H. K., O'Donnell, E. H., et al. (2015). Extending the ‘cross-disorder’ relevance of executive functions to dimensional neuropsychiatric traits in youth. J. Child Psychol. Psychiatry. doi: 10.1111/jcpp.12463. [Epub ahead of print].
Micali, N., Kothari, R., Nam, K. W., Gioroukou, E., Walshe, M., Allin, M., et al. (2015). Eating disorder psychopathology, brain structure, neuropsychological correlates and risk mechanisms in very preterm young adults. European Eating Disorders Review 23, 147–155. doi: 10.1002/erv.2346
Miceli, P. J., Goeke-Morey, M. C., Whitman, T. L., Kolberg, K. S., Miller-Loncar, C., and White, R. D. (2000). Brief report: birth status, medical complications, and social environment: individual differences in development of preterm, very low birth weight infants. J. Pediatric Psychol. 25, 353–8. doi: 10.1093/jpepsy/25.5.353
Mittal, V. A., Ellman, L. M., and Cannon, T. D. (2008). Gene-environment interaction and covariation in schizophrenia: the role of obstetric complications. Schizophr. Bull. 34, 1083–1094. doi: 10.1093/schbul/sbn080
Moster, D., Lie, R. T., and Markestad, T. (2009). Long-term medical and social consequences of preterm birth. Obstetr. Anesthes.Digest 29, 68–69. doi: 10.1097/01.aoa.0000350603.68744.9e
Mundy, P., and Gomes, A. (1998). Individual differences in joint attention skill development in the second year. Infant Behav. Dev. 21, 469–482. doi: 10.1016/S0163-6383(98)90020-0
Nadeau, L., Boivin, M., Tessier, R., Lefebvre, F., and Robaey, P. (2001). Mediators of behavioral problems in 7-year-old children born after 24 to 28 weeks of gestation. J. Dev. Behav. Pediatrics 22, 1–10. doi: 10.1097/00004703-200102000-00001
Nadeau, L., Tessier, R., Lefebvre, F., and Robaey, P. (2004). Victimization: a newly recognized outcome of prematurity. Dev. Med. Child Neurol. 46, 508–513. doi: 10.1111/j.1469-8749.2004.tb01007.x
Nosarti, C., Al-Asady, M. H. S., Frangou, S., Stewart, A. L., Rifkin, L., and Murray, R. M. (2002). Adolescents who were born very preterm have decreased brain volumes. Brain 125(Pt 7), 1616–1623. doi: 10.1093/brain/awf157
Nosarti, C., Murray, R. M., and Hack, M. E. (2010). Neurodevelopmental Outcomes of Preterm Birth. Cambridge: Cambridge University Press.
Nosarti, C. (2013). Structural and functional brain correlates of behavioral outcomes during adolescence. Early Hum. Dev. 89, 221–227. doi: 10.1016/j.earlhumdev.2013.02.002
Nosarti, C., Giouroukou, E., Healy, E., Rifkin, L., Walshe, M., Reichenberg, A., et al. (2008). Grey and white matter distribution in very preterm adolescents mediates neurodevelopmental outcome. Brain 131, 205–217. doi: 10.1093/brain/awm282
Nosarti, C., Allin, M. P., Frangou, S., Rifkin, L., and Murray, R. M. (2005). Hyperactivity in adolescents born very preterm is associated with decreased caudate volume. Biol. Psychiatry 57, 661–666. doi: 10.1016/j.biopsych.2004.12.003
Nosarti, C., Nam, K. W., Walshe, M., Murray, R. M., Cuddy, M., Rifkin, L., et al. (2014). Preterm birth and structural brain alterations in early adulthood. Neuroimage 6, 180–191. doi: 10.1016/j.nicl.2014.08.005
Nosarti, C., Reichenberg, A., Murray, R. M., Cnattingius, S., Lambe, M. P., Yin, L., et al. (2012). Preterm birth and psychiatric disorders in young adult life. Arch. Gen. Psychiatry 69, 610–617. doi: 10.1001/archgenpsychiatry.2011.1374
Nosarti, C., Walshe, M., Rushe, T. M., Rifkin, L., Wyatt, J., Murray, R. M., et al. (2011). Neonatal ultrasound results following very preterm birth predict adolescent behavioral and cognitive outcome. Dev. Neuropsychol. 36, 118–135. doi: 10.1080/87565641.2011.540546
Omizzolo, C., Scratch, S. E., Stargatt, R., Kidokoro, H., Thompson, D. K., Lee, K. J., et al. (2014). Neonatal brain abnormalities and memory and learning outcomes at 7 years in children born very preterm. Memory, 22, 605–615. doi: 10.1080/09658211.2013.809765
Parker, J. G., Rubin, K. H., Erath, S. A., Wojslawowicz, J. C., and Buskirk, A. A. (2006). “Peer relationships, child development, and adjustment: a developmental psychopathology perspective,” in Developmental Psychopathology, 2nd Edn. Vol. 1, eds D. Cicchetti and D. J. Cohen (New York, NY: Wiley), 419–493.
Parker, J., Mitchell, A., Kalpakidou, A., Walshe, M., Jung, H. Y., Nosarti, C., et al. (2008). Cerebellar growth and behavioural & neuropsychological outcome in preterm adolescents. Brain 131, 1344–1351. doi: 10.1093/brain/awn062
Pauly, K., Seiferth, N. Y., Kellermann, T., Backes, V., Vloet, T. D., Shah, N. J., et al. (2008). Cerebral dysfunctions of emotion-cognition interactions in adolescent-onset schizophrenia. J. Am. Acad. Child Adolesc. Psychiatry 47, 1299–1310. doi: 10.1097/CHI.0b013e318184ff16
Pavlova, M., Sokolov, A. N., Birbaumer, N., and Krageloh-Mann, I. (2008). Perception and understanding of others' actions and brain connectivity. J. Cogn. Neurosci. 20, 494–504 doi: 10.1162/jocn.2008.20034
Pavlova, M. A. (2012). Biological motion processing as a hallmark of social cognition. Cereb. Cortex 22, 981–995. doi: 10.1093/cercor/bhr156
Pelphrey, K. A., and Carter, E. J. (2008). Brain mechanisms for social perception: lessons from autism and typical development. Ann. N.Y. Acad. Sci. 1145, 283–299. doi: 10.1196/annals.1416.007
Pesonen, A. K., Räikkönen, K., Heinonen, K., Andersson, S., Hovi, P., Järvenpä, A. L., et al. (2008). Personality of young adults born prematurely: the Helsinki study of very low birth weight adults. J. Child Psychol. Psychiatry Allied Discipl. 49, 609–617. doi: 10.1111/j.1469-7610.2007.01874.x
Pessoa, L. (2008). On the relationship between emotion and cognition. Nat. Rev. Neurosci. 9, 148–158. doi: 10.1038/nrn2317
Peterson, B. S., Vohr, B., Staib, L. H., Cannistraci, C. J., Dolberg, A., Schneider, K. C., et al. (2000). Regional brain volume abnormalities and long-term cognitive outcome in preterm infants. JAMA 284, 1939–1947. doi: 10.1001/jama.284.15.1939
Pierrehumbert, B., Nicole, A., Muller-Nix, C., Forcada-Guex, M., and Ansermet, F. (2003). Parental post-traumatic reactions after premature birth: implications for sleeping and eating problems in the infant. Arch. Disease Childhood Fetal Neonatal Edn. 88, F400–F404. doi: 10.1136/fn.88.5.F400
Potharst, E. S., van Wassenaer-Leemhuis, A. G., Houtzager, B. A., Livesey, D., Kok, J. H., Last, B. F., et al. (2013). Perinatal risk factors for neurocognitive impairments in preschool children born very preterm. Dev. Med. Child Neurol. 55, 178–184. doi: 10.1111/dmcn.12018
Qiu, A., Adler, M., Crocetti, D., Miller, M. I., and Mostofsky, S. H. (2010). Basal ganglia shapes predict social, communication, and motor dysfunctions in boys with autism spectrum disorder. J. Am. Acad. Child Adolesc. Psychiatry 49, 539–551.e1–e4. doi: 10.1016/j.jaac.2010.02.012
Raikkonen, K., Pesonen, A. K., Heinonen, K., Kajantie, E., Hovi, P., Jarvenpaa, A.-L., et al. (2008). Depression in young adults with very low birth weight. Arch. Gen. Psychiatry 65, 290–296. doi: 10.1001/archgenpsychiatry.2007.40
Ranger, M., Synnes, A. R., Vinall, J., and Grunau, R. E. (2014). Internalizing behaviours in school-age children born very preterm are predicted by neonatal pain and morphine exposure. Eur. J. Pain 18, 844–852. doi: 10.1002/j.1532-2149.2013.00431.x
Rickards, A. L., Kelly, E. A., Doyle, L. W., and Callanan, C. (2001). Cognition, academic progress, behavior and self-concept at 14 years of very low birth weight children. J. Dev. Behav. Pediatrics 22, 11–18. doi: 10.1097/00004703-200102000-00002
Rogers, C. E., Anderson, P. J., Thompson, D. K., Kidokoro, H., Wallendor, M., Treyvaud, K., et al. (2012). Regional cerebral development at term relates to school-age social-emotional development in very preterm children. J. Am. Acad. Child Adolesc. Psychiatry 51, 181–191. doi: 10.1016/j.jaac.2011.11.009
Rogers, C. E., Barch, D. M., Sylvester, C. M., Pagliaccio, D., Harms, M. P., Botteron, K. N., et al. (2014). Altered gray matter volume and school age anxiety in children born late preterm. J. Pediatrics 165, 928–935. doi: 10.1016/j.jpeds.2014.06.063
Rubin, K. H., Bukowski, W. M., and Parker, J. G. (2006). “Peer interactions, relationships, and groups,” in Handbook of Child Psychology, 6th Edn. Vol. 3, eds W. Damon, R. M. Lerner, and N. Eisenberg (New York, NY: Wiley), 571–645.
Rueda, M. R., Posner, M. I., and Rothbart, M. K. (2004). “Attentional control and self-regulation,” in Handbook of Self-Regulation: Research, Theory, and Applications, Vol. 2, eds R. F. Baumeister and K. D. Vohs (New York, NY: Guilford Press), 284–299.
Saigal, S. (2014). Functional outcomes of very premature infants into adulthood. Sem. Fetal Neonatal Med. 19, 125–130. doi: 10.1016/j.siny.2013.11.001
Saigal, S., Pinelli, J., Hoult, L., Kim, M. M., and Boyle, M. (2003). Psychopathology and social competencies of adolescents who were extremely low birth weight. Pediatrics 111(5 Pt 1), 969–975. doi: 10.1542/peds.111.5.969
Sameroff, A. J. (1995). “General systems theories and developmental psychopathology,” in Developmental Psychopathology, Vol. 1: Theory and Methods, eds D. Cicchetti and D. J.Cohen (New York, NY: John Wiley & Sons, Inc), 659–695.
Sameroff, A., and Chandler (1975). Transactional models in early social relations. Hum. Dev. 18, 65–79 doi: 10.1159/000271476
Schappin, R., Wijnroks, L., Uniken Venema, M. M. A. T., and Jongmans, M. J. (2013). rethinking stress in parents of preterm infants: a meta-analysis. PLoS ONE 8:54992. doi: 10.1371/journal.pone.0054992
Schmidt, L. A., Miskovic, V., Boyle, M. H., and Saigal, S. (2008). Shyness and timidity in young adults who were born at extremely low birth weight. Pediatrics 122, e181–e187. doi: 10.1542/peds.2007-3747
Schmidt, L. A., Miskovic, V., Boyle, M., and Saigal, S. (2010). Frontal electroencephalogram asymmetry, salivary cortisol, and internalizing behavior problems in young adults who were born at extremely low birth weight. Child Dev. 81, 183–199. doi: 10.1111/j.1467-8624.2009.01388.x
Selten, J. P., and Cantor-Graae, E. (2005). Social defeat: risk factor for schizophrenia? Br. J. Psychiatry 187, 101–102. doi: 10.1192/bjp.187.2.101
Selten, J. P., Van Der Ven, E., Rutten, B. P. F., and Cantor-Graae, E. (2013). The social defeat hypothesis of schizophrenia: an update. Schizophr. Bull. 39, 1180–1186. doi: 10.1093/schbul/sbt134
Shaw, P., Gogtay, N., and Rapoport, J. (2010). Childhood psychiatric disorders as anomalies in neurodevelopmental trajectories. Hum. Brain Mapp. 31, 917–925. doi: 10.1002/hbm.21028
Shaw, P., Malek, M., Watson, B., Sharp, W., Evans, A., and Greenstein, D. (2012). Development of cortical surface area and gyrification in attention-deficit/hyperactivity disorder. Biol. Psychiatry 72, 191–197. doi: 10.1016/j.biopsych.2012.01.031
Shonkoff, J. P., and Phillips, D. A. (eds.). (2000). From Neurons to Neighborhoods: The Science of Early Childhood Development. Washington, DC: National Academies Press.
Silverstein, M., Feinberg, E., Young, R., and Sauder, S. (2010). Maternal depression, perceptions of children's social aptitude and reported activity restriction among former very low birthweight infants. Arch. Dis. Child. 95, 521–525. doi: 10.1136/adc.2009.181735
Skinner, R. A., and Piek, J. P. (2001). Psychosocial implications of poor motor coordination in children and adolescents. Hum. Mov. Sci. 20, 73–94. doi: 10.1016/S0167-9457(01)00029-X
Skranes, J., Vangberg, T. R., Kulseng, S., Indredavik, M. S., Evensen, K. A. I., Brubakk, A. M., et al. (2007). Clinical findings and white matter abnormalities seen on diffusion tensor imaging in adolescents with very low birth weight. Brain 130, 654–666. doi: 10.1093/brain/awm001
Smith, L., and Ulvund, S. E. (2003). The role of joint attention in later development among preterm children: linkages between early and middle childhood. Soc. Dev. 12, 222–234. doi: 10.1111/1467-9507.00230
Smith, G. C., Gutovich, J., Smyser, C., Pineda, R., Newnham, C., Tjoeng, T. H., et al. (2011). Neonatal intensive care unit stress is associated with brain development in preterm infants. Ann. Neurol. 70, 541–549. doi: 10.1002/ana.22545
Sømhovd, M. J., Hansen, B. M., Brok, J., Esbjørn, B. H., and Greisen, G. (2012). Anxiety in adolescents born preterm or with very low birthweight: a meta-analysis of case-control studies. Dev. Med. Child Neurol. 54, 988–994. doi: 10.1111/j.1469-8749.2012.04407.x
Sparrow, S. S., Cicchetti, D. V., and Balla, D. A. (1989). The vineland adaptive behavior scales. Major Psychol. Assessm. Instrum. 2, 199–231.
Spittle, A. J., Treyvaud, K., Doyle, L. W., Roberts, G., Lee, K. J., Inder, T. E., et al. (2009). Early emergence of behavior and social-emotional problems in very preterm infants. J. Am. Acad. Child Adolesc. Psychiatry 48, 909–918. doi: 10.1097/CHI.0b013e3181af8235
Stevenson, C. J., Blackburn, P., and Pharoah, P. O. (1999). Longitudinal study of behaviour disorders in low birthweight infants. Arch. Disease Childhood Fetal Neonatal Edn. 81, F5–F9. doi: 10.1136/fn.81.1.F5
Stevenson, R. A., Segers, M., Ferber, S., Barense, M. D., and Wallace, M. T. (2014). The impact of multisensory integration deficits on speech perception in children with autism spectrum disorders. Front. Psychol. 5:379. doi: 10.3389/fpsyg.2014.00379
Stewart, A. L., Rifkin, L., Amess, P. N., Kirkbride, V., Townsend, J. P., Miller, D. H., et al. (1999). Brain structure and neurocognitive and behavioural function in adolescents who were born very preterm. Lancet 353, 1653–1657. doi: 10.1016/S0140-6736(98)07130-X
Stoelhorst, G. M. S. J., Martens, S. E., Rijken, M., van Zwieten, P. H. T., Zwinderman, A. H., Wit, J. M., et al. (2003). Behaviour at 2 years of age in very preterm infants (gestational age < 32 weeks). Acta Paediatr. 92, 595–601. doi: 10.1111/j.1651-2227.2003.tb02513.x
Stuss, D. T., and Alexander, M. P. (2000). Executive functions and the frontal lobes: a conceptual view. Psychol. Res. 63, 289–298. doi: 10.1007/s004269900007
Taylor, N. M., Jakobson, L. S., Lewis, D., and Maurer, T. L. (2009). Differential vulnerability of global motion, global form, and biological motion processing in full-term and preterm children. Neuropsychologia 47, 2766–2778. doi: 10.1016/j.neuropsychologia.2009.06.001
Thompson, C., Syddall, H., Rodin, I. A. N., Osmond, C., David, J. P., and Barker, D. J. P. (2001). Birth weight and the risk of depressive disorder in late life. Br. J. Psychiatry 179, 450–455. doi: 10.1192/bjp.179.5.450
Treyvaud, K. (2014). Parent and family outcomes following very preterm or very low birth weight birth: a review. Sem. Fetal Neonatal Med. 19, 131–135. doi: 10.1016/j.siny.2013.10.008
Treyvaud, K., Anderson, V. A., Lee, K. J., Woodward, L. J., Newnham, C., Inder, T. E., et al. (2010). Parental mental health and early social-emotional development of children born very preterm. J. Pediatr. Psychol. 35, 768–777. doi: 10.1093/jpepsy/jsp109
Treyvaud, K., Doyle, L. W., Lee, K. J., Roberts, G., Lim, J., Inder, T. E., et al. (2012). Social-emotional difficulties in very preterm and term 2 year olds predict specific social-emotional problems at the age of 5 years. J. Pediatr. Psychol. 37, 779–785. doi: 10.1093/jpepsy/jss042
Treyvaud, K., Ure, A., Doyle, L. W., Lee, K. J., Rogers, C. E., Kidokoro, H., et al. (2013). Psychiatric outcomes at age seven for very preterm children: rates and predictors. J. Child Psychol. Psychiatry Allied Discipl. 54, 772–779. doi: 10.1111/jcpp.12040
Van Os, J. (2013). The dynamics of subthreshold psychopathology: implications for diagnosis and treatment. Am. J. Psychiatry 170, 695–698. doi: 10.1176/appi.ajp.2013.13040474
Van Os, J., Kenis, G., and Rutten, B. P. F. (2010). The environment and schizophrenia. Nature 468, 203–212. doi: 10.1038/nature09563
Van Os, J., and Linscott, R. J. (2012). Introduction: the extended psychosis phenotype—Relationship with schizophrenia and with ultrahigh risk status for psychosis. Schizophr. Bull. 38, 227–230. doi: 10.1093/schbul/sbr188
Vigod, S. N., Villegas, L., Dennis, C.-L., and Ross, L. E. (2010). Prevalence and risk factors for postpartum depression among women with preterm and low-birth-weight infants: a systematic review. BJOG 117, 540–550. doi: 10.1111/j.1471-0528.2009.02493.x
Vinall, J., and Grunau, R. E. (2014). Impact of repeated procedural pain-related stress in infants born very preterm. Pediatr. Res. 75, 584–587. doi: 10.1038/pr.2014.16
Vinall, J., Miller, S. P., Synnes, A. R., and Grunau, R. E. (2013). Parent behaviors moderate the relationship between neonatal pain and internalizing behaviors at 18 months corrected age in children born very prematurely. Pain 154, 1831–1839. doi: 10.1016/j.pain.2013.05.050
Volpe, J. J. (2009). Brain injury in premature infants: a complex amalgam of destructive and developmental disturbances. Lancet Neurol. 8, 110–124. doi: 10.1016/S1474-4422(08)70294-1
Walshe, M., Rifkin, L., Rooney, M., Healy, E., Nosarti, C., Wyatt, J., et al. (2008). Psychiatric disorder in young adults born very preterm: role of family history. Eur. Psychiatry 23, 527–531. doi: 10.1016/j.eurpsy.2008.06.004
Wass, S. V., Jones, E. J. H., Gliga, T., Smith, T. J., Charman, T., Johnson, M. H., et al. (2015). Shorter spontaneous fixation durations in infants with later emerging autism. Sci. Rep. 5:8284. doi: 10.1038/srep08284
Wickremasinghe, A. C., Rogers, E. E., Johnson, B. C., Shen, A., Barkovich, A. J., and Marco, E. J. (2013). Children born prematurely have atypical sensory profiles. J. Perinatol. 33, 631–635. doi: 10.1038/jp.2013.12
Widiger, T. A. (2011). Personality and psychopathology. World Psychiatry 10, 103–106. doi: 10.1002/j.2051-5545.2011.tb00024.x
Williams, J. G., Higgins, J. P. T., and Brayne, C. E. G. (2006). Systematic review of prevalence studies of autism spectrum disorders. Arch. Dis. Child. 91, 8–15. doi: 10.1136/adc.2004.062083
Williamson, K. E., and Jakobson, L. S. (2014a). Social attribution skills of children born preterm at very low birth weight. Dev. Psychopathol. 26, 889–900. doi: 10.1017/S0954579414000522
Williamson, K. E., and Jakobson, L. S. (2014b). Social perception in children born at very low birthweight and its relationship with social/behavioral outcomes. J. Child Psychol. Psychiatry 55, 990–998. doi: 10.1111/jcpp.12210
Witt, A., Theurel, A., Tolsa, C. B., Lejeune, F., Fernandes, L., de Jonge, L. V. H., et al. (2014). Emotional and effortful control abilities in 42-month-old very preterm and full-term children. Early Hum. Dev. 90, 565–569. doi: 10.1016/j.earlhumdev.2014.07.008
Wocadlo, C., and Rieger, I. (2006). Social skills and nonverbal decoding of emotions in very preterm children at early school age. Eur. J. Dev. Psychol. 3, 48–70. doi: 10.1080/17405620500361894
Wolf, M. J., Koldewijn, K., Beelen, A., Smit, B., Hedlund, R., and de Groot, I. J. M. (2002). Neurobehavioral and developmental profile of very low birthweight preterm infants in early infancy. Acta Paediatr. 91, 930–938. doi: 10.1111/j.1651-2227.2002.tb02858.x
Wong, H. S., Huertas-Ceballos, A., Cowan, F. M., and Modi, N. (2014). Evaluation of early childhood social-communication difficulties in children born preterm using the quantitative checklist for autism in toddlers. J. Pediatrics 164, 26–33.e1. doi: 10.1016/j.jpeds.2013.07.013
Wood, N. S., Costeloe, K., Gibson, A. T., Hennessy, E. M., Marlow, N., and Wilkinson, A. R. (2005). The EPICure study: associations and antecedents of neurological and developmental disability at 30 months of age following extremely preterm birth. Arch. Disease Childhood Fetal Neonatal Edn. 90, F134–F140. doi: 10.1136/adc.2004.052407
Woodward, L. J., Anderson, P. J., Austin, N. C., Howard, K., and Inder, T. E. (2006). Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N. Engl. J. Med. 355, 685–694. doi: 10.1056/NEJMoa053792
Zelkowitz, P., Na, S., Wang, T., Bardin, C., and Papageorgiou, A. (2011). Early maternal anxiety predicts cognitive and behavioural outcomes of VLBW children at 24 months corrected age. Acta Paediatrica Inter. J. Paediatrics 100, 700–704. doi: 10.1111/j.1651-2227.2010.02128.x
Keywords: preterm, socio-emotional, brain, pain, stress, parenting
Citation: Montagna A and Nosarti C (2016) Socio-Emotional Development Following Very Preterm Birth: Pathways to Psychopathology. Front. Psychol. 7:80. doi: 10.3389/fpsyg.2016.00080
Received: 17 September 2015; Accepted: 14 January 2016;
Published: 12 February 2016.
Edited by:
Alessandra Simonelli, University of Padova, ItalyReviewed by:
Debora Marques Miranda, Universidade Federal de Minas Gerais, BrazilIsabela Sallum, Universidade Federal de Minas Gerais, Brazil
Copyright © 2016 Montagna and Nosarti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chiara Nosarti, Y2hpYXJhLm5vc2FydGlAa2NsLmFjLnVr
 Anita Montagna
Anita Montagna Chiara Nosarti
Chiara Nosarti