- 1School of Management, Beijing University of Chinese Medicine, Beijing, China
- 2Department of Pediatrics, China-Japan Friendship Hospital, Beijing, China
- 3National Institute of Chinese Medicine Development and Strategy, Beijing University of Chinese Medicine, Beijing, China
Background: In previous observational studies and meta-analyses, childhood attention deficit hyperactivity disorder (ADHD) is found to have a significant association with screen time. However, the causal associations between them remain unclear.
Method: This study performed a bidirectional two-sample Mendelian randomization (MR) analysis to confirm the causality between screen time and childhood ADHD. Large-scale genome-wide association studies (GWAS) datasets derived from the Psychiatric Genomics Consortium (PGC) and the UK Biobank were used to identify single nucleotide polymorphisms (SNPs) associated with exposure and outcome. Four categories of datasets were selected to represent screen time. The SNPs that are significantly associated with exposure data (P < 5e-08) and have a strong correlation with the exposure in the F-statistic (F > 10) were selected as instrumental variables. This study also used the PhenoScanner V2 database and the LDlink webtool to exclude confounding factors, and the MR-PRESSO method (p < 0.05) was employed to eliminate outliers with bias. Five commonly used methods were employed to assess the interaction and the Inverse Variance Weighted (IVW) method was utilized as the primary basis for determining the MR estimates in this study.
Results: The MR analysis revealed that the length of mobile phone use (OR, 1.848; 95% CI, 1.3360-2.5558; p=2.07e-4) and the time spent watching television (OR, 2.104; 95% CI, 1.3958-3.1703; p=3.8e-4) increased the risk of childhood ADHD. Although the causal relationships were exclusively identified through the IVW and weighted median methods, the results retained their statistical significance following correction. In the reverse analysis, no evidence was found to support an effect of childhood ADHD on screen time. The sensitivity analysis conducted on the significant findings revealed no evidence of horizontal pleiotropy or heterogeneity.
Conclusion: This study provides some evidence for the causality of screen time and childhood ADHD. Given the limitations of our study, further research is required to comprehensively investigate this relationship.
1 Introduction
Attention Deficit Hyperactivity Disorder (ADHD) is a long-term neurodevelopmental condition, with predisposing factors occurring in early childhood (1), whose manifestations and affective effects can last into adulthood (1). Approximately 8–12% of children worldwide are diagnosed with ADHD (2), and over 60% of them experience psychological disorders and symptoms well into adulthood (3, 4). According to the results of a recent meta-analysis, in the world, the prevalence of childhood ADHD is approximated to be 7.2% (5), while the disease affects about 2.5% of adults (6). The Global Burden of Disease (GBD) study indicates that between 1990 and 2019, the global age-standardized incidence and prevalence of ADHD declined by -4.77% and -8.75%, respectively (7). However, the prevalence and disease impact of ADHD may be underreported according to the GBD figures (7). An increasing number of children with ADHD causes heavy burdens on society, families, and individual development. It is well known that the etiology of ADHD involves a complex interplay between environmental and genetic risk factors. Several studies have demonstrated that psychosocial disorders, environmental pollutants, and prenatal and postnatal variables are prevalent risk factors for ADHD. However, the origin and pathophysiology of ADHD are still unclear due to the disorder’s complexity and variety.
There is growing concern that youngsters who spend too much time on screens may develop psychological and cognitive issues as a result of their excessive screen usage. The suggested daily limit of two hours can be readily exceeded by children due to their lack of self-control. This average daily screen time for 8- to 18-year-olds increased by 1.17 hours in the ten years between 1999 and 2009 (8). The proportion of children aged 0 to 8 who had access to a mobile device increased, rising from 52% in 2011 to 75% in 2013 (9).
However, there is still a debate over the intrinsic link between screen usage and childhood ADHD. Reviews have indicated a strong association between screen exposure and ADHD or characteristics linked with ADHD, such as impulsivity and inattention (10, 11). A cross-sectional study from the Karachi National Institute of Child Health demonstrated a positive correlation between screen usage and ADHD in children (12). Nevertheless, research from the tertiary care facility in Sri Lanka found no correlation between screen time and clinically diagnosed ADHD (13).
Mendelian randomization (MR) is an analytical approach for ascertaining the causality between exposure variables and outcomes. As instrumental variables (IVs), the method makes use of single nucleotide polymorphisms (SNPs) derived from pooled data in genome-wide association studies (GWAS). If the SNP associated with the genetic variant is specifically linked to the exposure factor and impacts the disease solely through the exposure factor, then exposure factors are deemed causally related to disease. Since MR is based on the theory that genetic variants are randomly assigned during transmission from parent to child, it can mitigate the effects of reverse causality and other confounding variables by satisfying specific conditions. This means that when it comes to establishing the causal association between environmental factors and disease, MR is able to offer greater evidence than traditional observational research. Therefore, this study sought to investigate the possible causality between screen time and childhood ADHD using bidirectional two-sample MR analysis and to offer fresh data supporting the need for early intervention and treatment of ADHD.
2 Methods
2.1 Study design
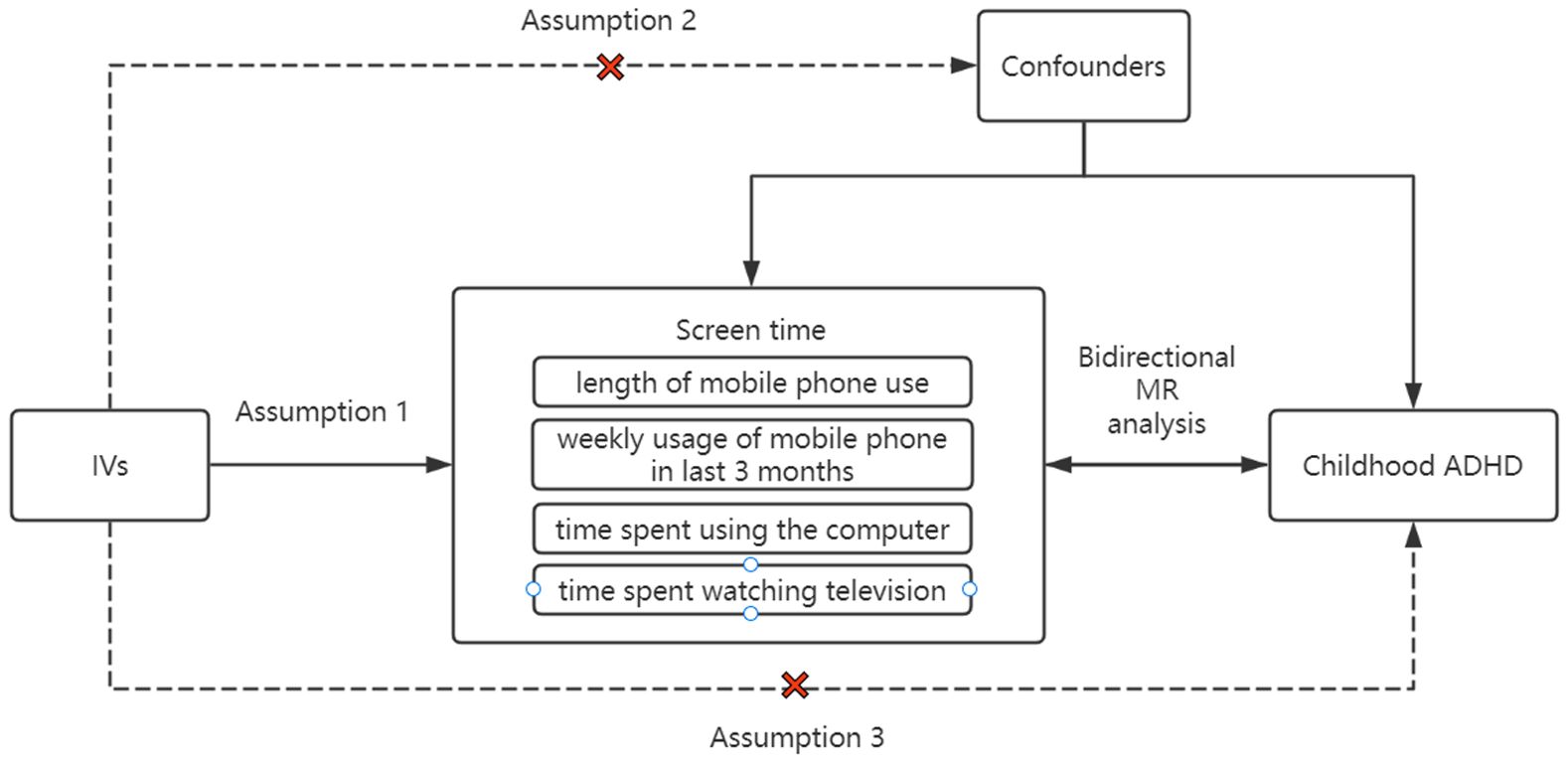
This study employed bidirectional two-sample MR analysis to confirm the causality between screen time and childhood ADHD. Four categories of datasets representing screen time were chosen, including time spent watching television, length of mobile phone use, time spent using the computer (Qu et al.)1, and weekly usage of mobile phone in last 3 months (14, 15). Based on the GWAS database, the data collected from European populations, as with the ADHD dataset. Initially, we used the data on screen time in four categories as exposure and the ADHD data as outcome. Afterwards, we switched the screen time data and ADHD data for MR analysis. Throughout the Mendelian randomization analysis, the following three assumptions had to be strictly met (Figure 1): (1) the close association between exposure and instrumental variables; (2) the independence of instrumental variables from any potential confounders that may affect the results; and (3) the exclusive impact of instrumental variables on outcomes through exposure, without any influence from other factors.
2.2 Data source for screen time and ADHD
The GWAS summary data for ADHD was obtained from the Psychiatric Genomics Consortium (PGC) (https://pgc.unc.edu/for-researchers/download-results), consisting of 225,534 individuals (186,843 healthy controls and 38,691 ADHD patients). The diagnosis of ADHD in all cases was conducted by psychiatrists following ICD10 (F90.0, F90.1, F98.8), which resulted in the identification of 27 genome-wide loci and 76 potential risk genes independently associated with ADHD (16).
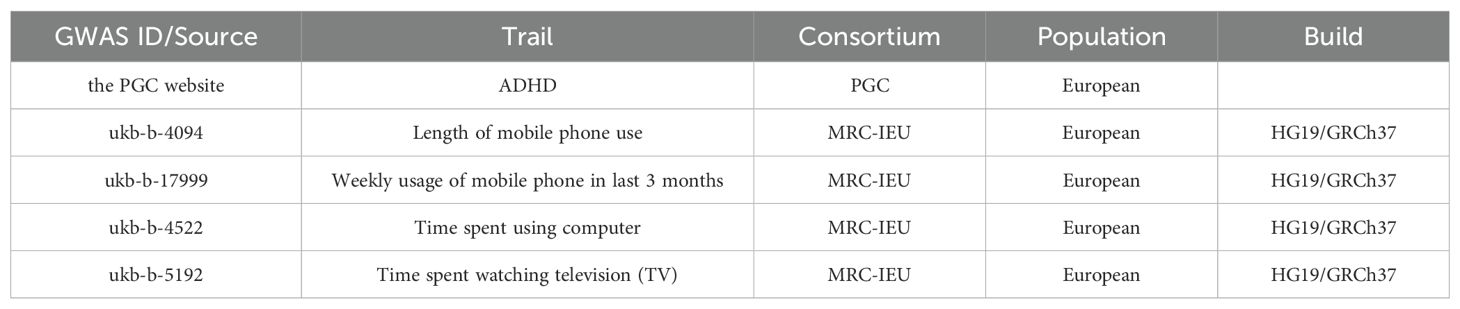
The screen time data came from self-reported questionnaires collected by the UK Biobank Assessment Center (ACE). The questionnaires included data from eight sub-surveys on physical activity, electronic device use, insomnia, and smoking. The electronic device usage survey contained the use of cell phones (time of use, side of the head) and computer games. Two datasets derived from this survey were selected for the study: length of mobile phone use and weekly usage of mobile phone over past 3 months. In addition, data on time spent using the computer and time spent watching television were added to the exposure data to increase the breadth of the study. All exposure data were from European populations and consisted of four datasets (ukb-b: 5192, 4094, 4522, 17999). The dataset ukb-b-5192 included 437887 participants; dataset ukb-b-4094 included 456972 participants; dataset ukb-b-4522 included 360895 participants; dataset ukb-b-17999 included 386626 participants. All the data sources used for MR analysis are detailed in Table 1.
2.3 Instrumental variables selection
This study extracted genome-wide SNPs that are significantly associated with exposure data (P < 5e-08) as initial instrumental variables. Using a reference panel of 1,000 genomic European populations, SNPs with linkage disequilibrium (LD) in the initial instrumental variables were removed under the threshold condition (R2 < 0.001) and a window size of 10 Mb to ensure the independent validity of the SNPs. Subsequently, the formula F = β2/se2 was used to calculate the F-statistic for each SNP and screen for SNPs with a strong correlation with the exposure data (F > 10). To exclude the influence of confounding factors on causal effects, we retrieved the relevant traits of strongly correlated SNPs from the PhenoScanner V2 database and the LDlink webtool, including negative mood, educational status, body mass index, ADHD behavior, mental disorders and other diseases. Outliers with bias in the SNPs were screened and eliminated using the MR-PRESSO method (p<0.05). The retained SNPs were used as final instrumental variables for conducting Mendelian randomization analysis.
2.4 Bidirectional analyses of Mendelian randomization
To assess the potential causal association between screen time and childhood ADHD, a two-sample MR analysis was conducted using four distinct categories of screen time as exposure factors and ADHD as the outcome variable. Five common methods were used to assess the interaction: inverse variance weighting (IVW), weighted median, MR-Egger, weighted, and simple median. Compared to other methods, the IVW method provides more accurate and stable assessment results (17, 18). Therefore, the IVW method was utilized as the main basis for determining the MR estimates in this study. Reverse Mendelian randomization analyses were conducted to test the possibility of reverse causality, using ADHD as the exposure factor and the four categories of screen time as the outcome variable.
2.5 Sensitivity analysis
In this study, the MR-Egger regression intercept method was applied to evaluate for horizontal pleiotropy in the MR estimates, with a p-value < 0.05 considered to be horizontal pleiotropy. Horizontal pleiotropy indicates that genetic variants influence multiple biological pathways, which contradicts the fundamental assumption of IVs in MR analysis. Specifically, IVs are presumed to affect the outcome exclusively through the exposure of interest. A p-value of less than 0.05 in the horizontal pleiotropy test suggests that the IVs employed in the MR analysis violate this premise. Consequently, the conclusions derived from the analysis lack statistical significance. The Cochran’s Q statistic was utilized to test for heterogeneity using the IVW method and the MR-Egger regression method, with a p-value < 0.05 considered to be heterogeneous. Leave-one-out sensitivity analyses were applied to assess the presence of directional pleiotropy and determine the effect of each SNP on the causal effect. MR-PRESSO tests were used to identify outliers in the SNPs, and MR analyses were performed again after removing the outliers. The entire analysis was carried out using RStudio (version 4.2.1) with the packages “MendelianRandomization”, “TwoSampleMR”, and “VariantAnnotation”.
3 Results
3.1 Selection of IVs
This study initially identified 32, 6, 82, and 112 valid SNPs as instrumental variables for the length of mobile phone use, weekly usage of mobile phones in the last 3 months, time spent using the computer, and time spent watching television. All of these SNPs were independent in LD and had F-statistics greater than 10. The number of excluded SNPs that contained traits such as negative mood, educational status, body mass index, ADHD behavior, psychiatric disorders, and other disorders were 15, 4, 46, and 76 for four types of screen time, respectively.MR-PRESSO outlier detection removed 2, 0, 0, and 2 outliers. 13, 1, 34, and 33 were the final numbers of instrumental variables employed in the MR analysis. The GWAS data of weekly usage of mobile phone over the past 3 months was screened with only one SNP for MR analysis, preventing the use of analysis methods such as IVW. Therefore, only the results of the other three types were considered.
3.2 Causal effect of screen time on childhood ADHD
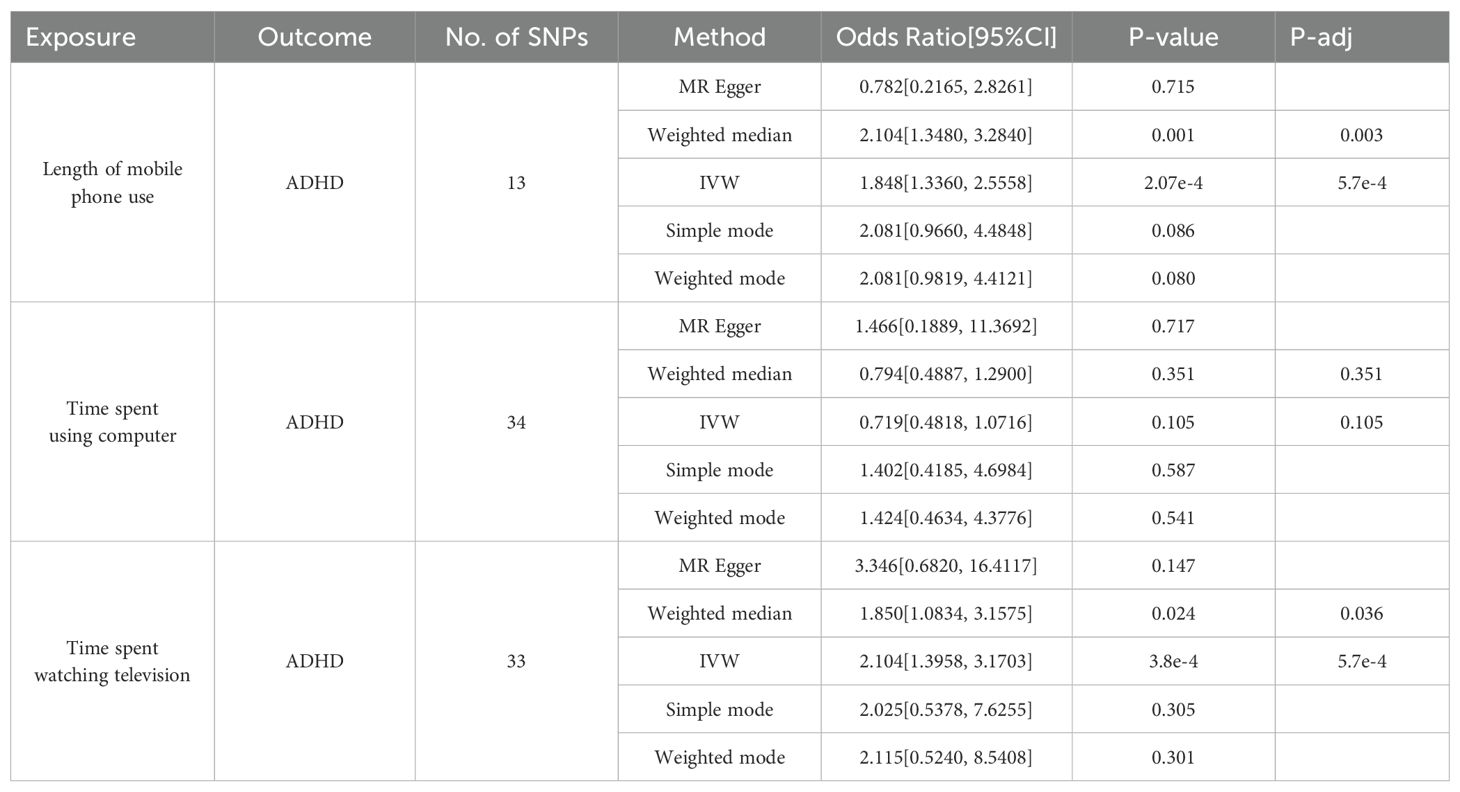
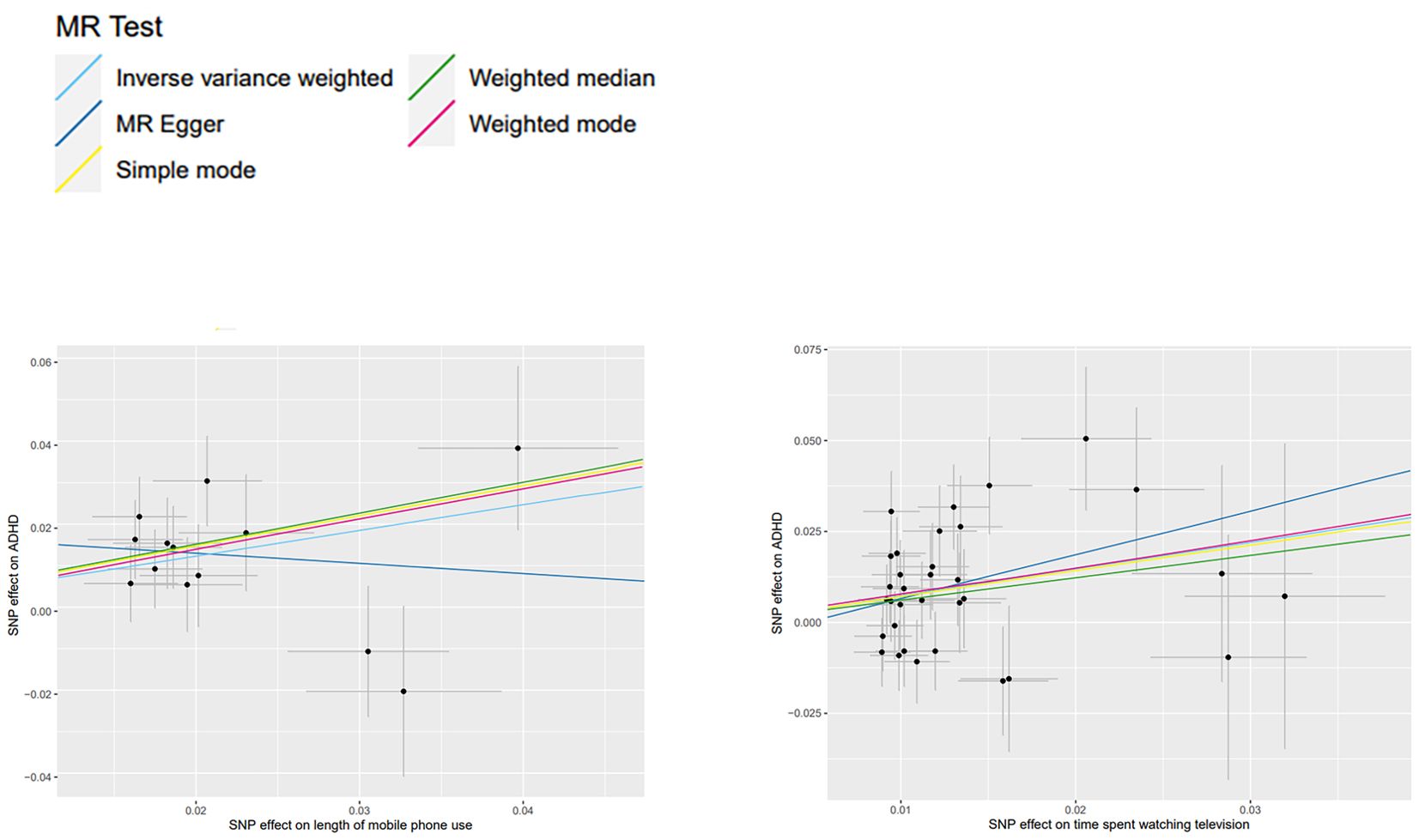
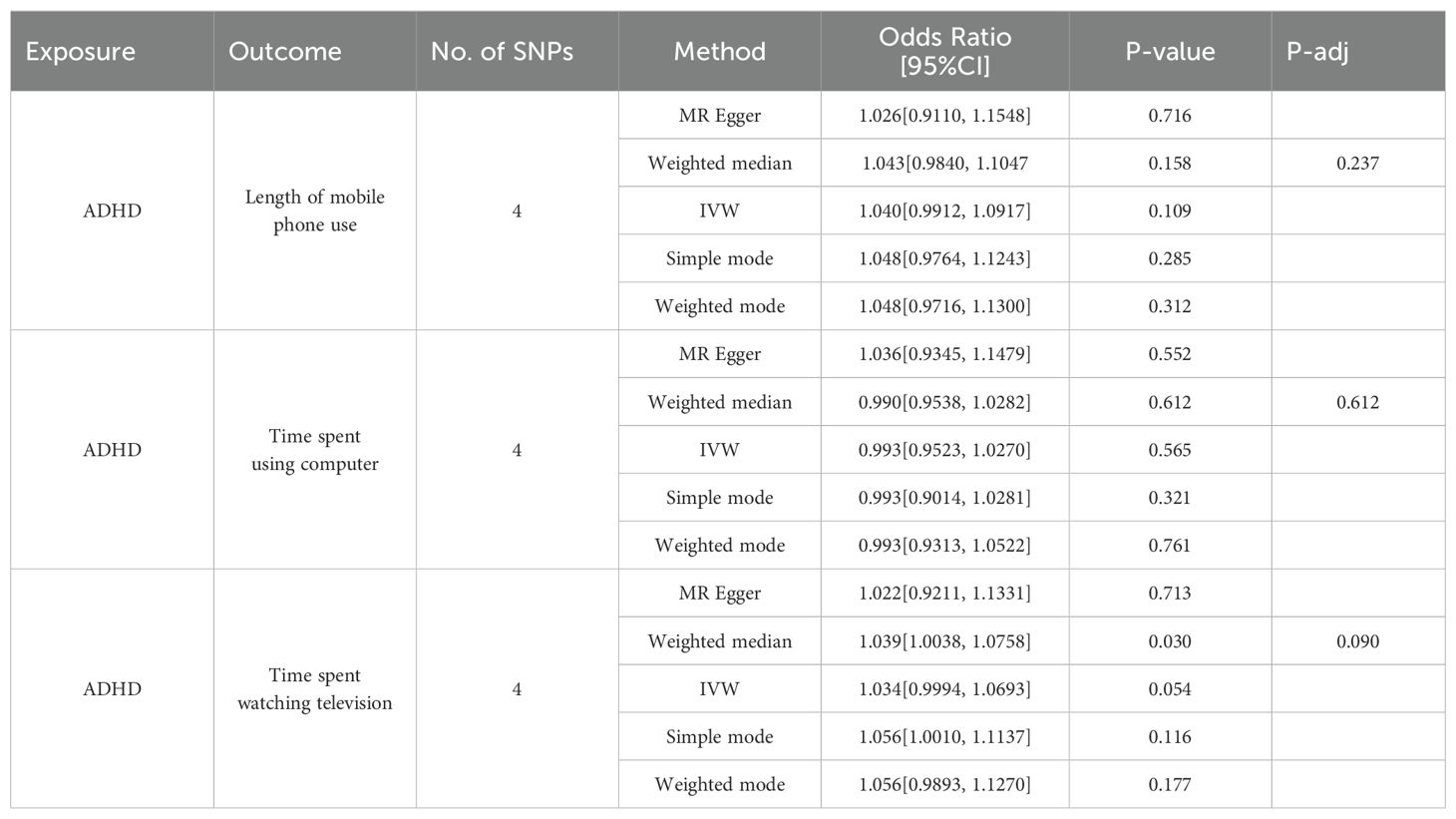
The IVW method revealed that the length of mobile phone use (OR, 1.848; 95% CI, 1.3360-2.5558; p=2.07e-4), the time spent watching television (OR, 2.104; 95% CI, 1.3958-3.1703; p=3.8e-4) had a causal relationship with childhood ADHD. To enhance the reliability of the results, we conducted a False Discovery Rate (FDR) correction employing the Benjamini-Hochberg method to mitigate the impacts of multiple exposures on our findings. The adjusted p-value remained below 0.05 (Table 2), indicating that prolonged exposure to both categories of screen time is associated with an elevated risk of childhood ADHD. Before and after adjustment, the Weighted median method consistently produced results consistent with the IVW method, while the other methods exhibited statistically insignificant p-values. Additionally, no significant association was found between the time spent with computers (IVW: OR, 0.719; 95% CI, 0.4818-1.0716; p=0.105) and childhood ADHD in any of the MR methods. Detailed statistical results of five models are provided (Table 2). After rigorous exclusion of SNPs, our study provides evidence that screen time and childhood ADHD may be causally related (Figure 2).
3.3 Causal effect of childhood ADHD on screen time
This study performed MR analyses utilizing ADHD data as the exposure and screen time as the outcome to elucidate the inverse associations. The results (Table 3) indicated that there is minimal evidence to suggest a reverse causality between screen time and childhood ADHD. All of the IVW results were not statistically significant. A weak causal relationship was identified exclusively in the findings derived from the Weighted Median method between childhood ADHD and both the weekly mobile phone usage over the past 3 months (OR, 1.037; 95% CI, 1.0013-1.1169; p=0.045) and the time spent watching television (OR, 1.039; 95% CI, 1.0038-1.0758; p=0.030). However, their corrected p-value was greater than 0.05.
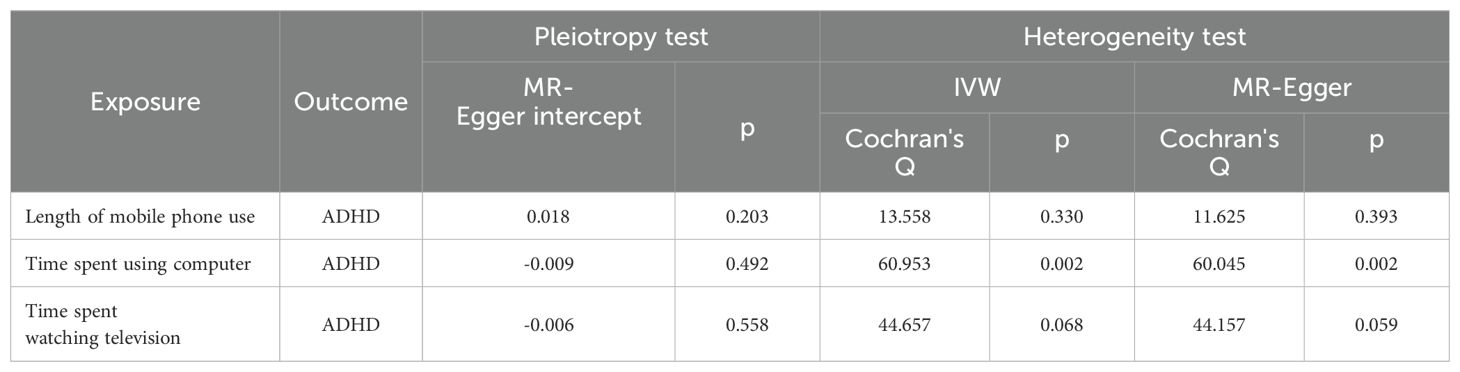
3.4 Sensitivity analysis
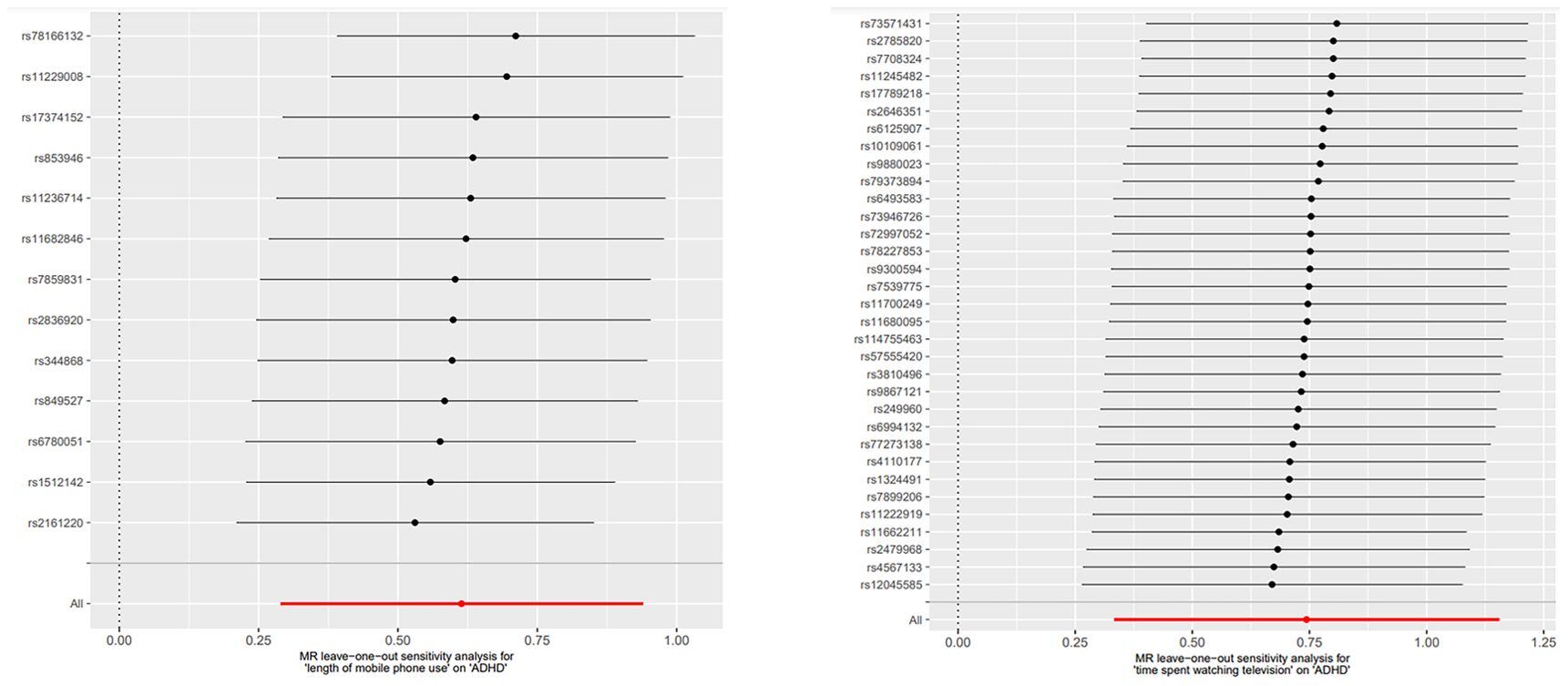
The MR-Egger regression intercept results indicated the absence of horizontal pleiotropy in all MR analyses (Table 4). In the MR analyses, heterogeneity was observed solely for the time spent using computer, suggesting the presence of confounders in the SNPs used for MR analyses (Table 4). However, as the MR analysis results for this category of screen time and childhood ADHD were not statistically significant, they did not impact the conclusions drawn. The funnel plot’s symmetry also led to the same conclusion (Figure 3). Leave-one-out sensitivity analyses demonstrated that no one SNP was responsible for the causal relationships between two types of screen time (the length of mobile phone use and the time spent watching television) and childhood ADHD (Figure 4).
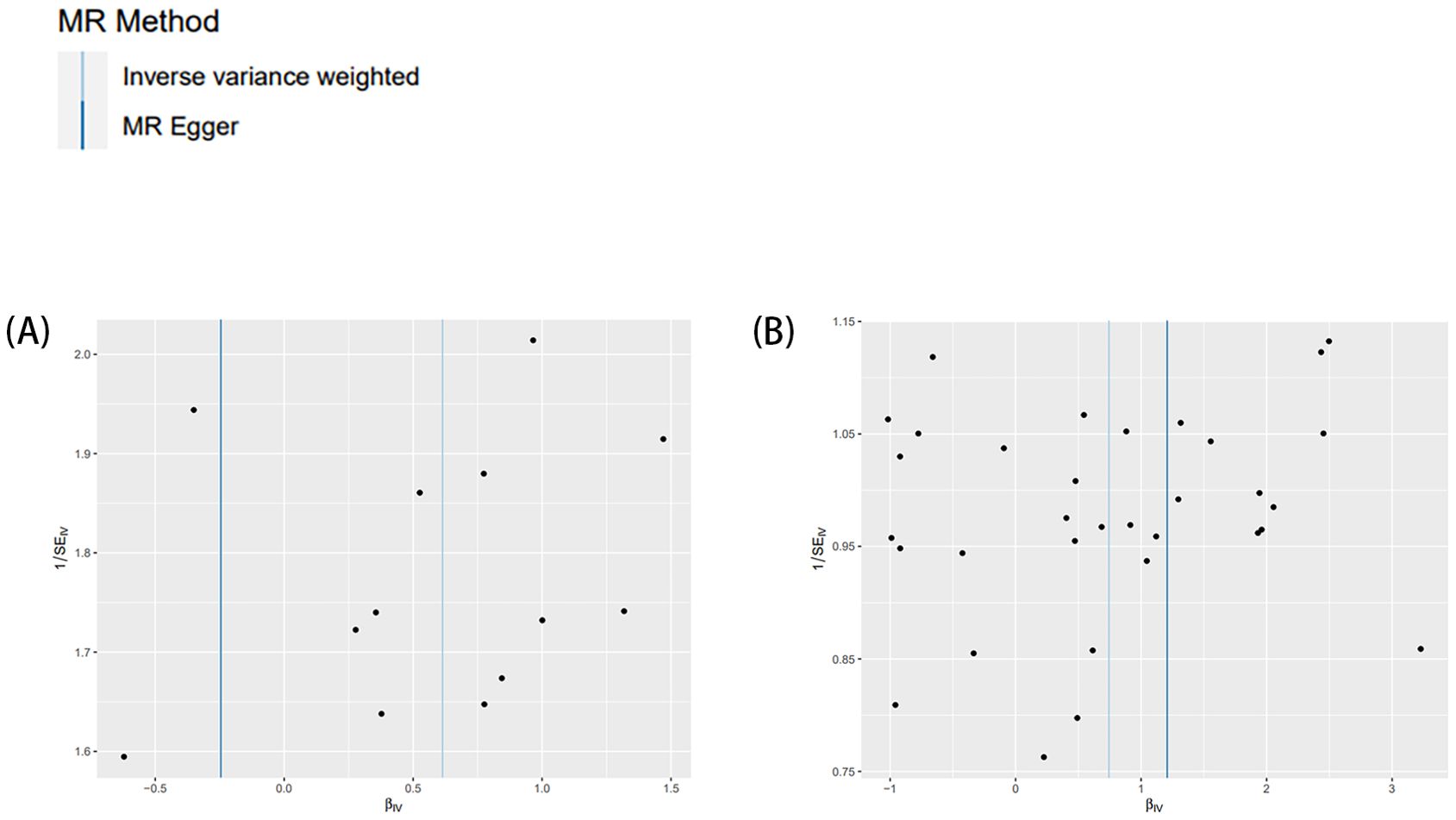
Figure 3. Funnel plots employed to assess heterogeneity. Exposure two screen times and outcome ADHD. (A) length of mobile phone use; (B) time spent watching television.
4 Discussion
This study utilized bidirectional two-sample MR analysis to evaluate the genetic underpinnings of the causal relationship between screen time and childhood ADHD. From the available large-scale GWAS pooled data, four categories of data characterizing screen time were extracted. The findings of this study indicated that the time spent watching television and the length of mobile phone use was significant causally associated with the disorder only in IVW and Weighted median method. This indicates that the causality we have identified may not be as robust as observed and warrants further investigation through more comprehensive and detailed studies.
The rising prevalence of ADHD among children has significant financial implications for societal development, family relationships, and personal advancement. As the prevalence of electronic device usage among children and adolescents continues to increase, it is imperative to assess the impact of screen time on their physical health, cognitive development, and overall growth. Previous research has demonstrated a growing interest in exploring the correlation between excessive screen exposure and adverse effects on various aspects of health, including psychological, social, and neurological effects (10). Meanwhile, Observational studies have indicated that prolonged screen time may have detrimental consequences on mental and physical health outcomes, such as obesity and myopia, in the pediatric population. A cohort study involving 3826 adolescents suggests that the use of social media and television may exacerbate depressive symptoms (19). A meta-analysis further indicates a correlation between screen time based on sedentary behavior and an elevated risk of depression (20). A review covers studies from 1999 to 2014 revealed that the majority of previous studies had found negative associations between screen usage and both shorter sleep duration and increased sleep difficulties (21). A cross-sectional Canadian study suggests that screen use may serve as a risk factor for anxiety and sadness among teenagers (22). Excessive screen time is related to a greater incidence of depression among adolescents and heightened levels of anxiety in both males and females. Furthermore, increased exposure to screen media has been linked to a greater risk of adolescent obesity (23). Prolonged periods of sedentary behavior in front of a screen are strongly correlated with negative health outcomes, such as suboptimal cognitive-behavioral functioning and diminished psychosocial wellbeing.
Excessive screen usage can affect the prevalence of ADHD at the behavioral level through visual or auditory stimuli. When presenting with stimuli unrelated to behavioral reactions, those with ADHD exhibit increased brain activity (24). Research indicates that a fast-paced program of screen media may exacerbate ADHD-related behaviors, including attentional difficulties in children (25). An experimental study utilizing a mouse model of excessive sensory stimulation corroborated that prolonged exposure to audiovisual media during childhood results in cognitive and behavioral deficits (26). Similarly, longitudinal naturalistic studies have demonstrated that early screen exposure is associated with diminished executive functioning in children (27). Research has demonstrated that children with ADHD engage in screen-based activities to meet their reward sensitivity needs (28), which results in them using screens more frequently than normal kids. Screen-based activities may decrease children’s use of motor functions and increase their likelihood of exhibiting symptoms of ADHD. According to another research, eye movement-focused interventions have also been found to improve cognitive and motor functions in children with ADHD (29). Additionally, children who engage in screen-based activities may be less likely to use their kinesthetic senses, which could predispose them to exhibit symptoms of ADHD. Furthermore, numerous studies have demonstrated that physical activity can enhance executive functioning in children diagnosed with ADHD (30).
Screen time may have an indirect impact on childhood ADHD by altering various lifestyle factors. Specifically, the severity of ADHD symptoms in children may be influenced by increased screen time, which can lead to decreased sleep quality or exacerbate existing sleep disturbances. A study involving 374 French children found that nighttime screen usage significantly affected sleep disruptions, which in turn were directly associated with symptoms of ADHD in this population (31). A study conducted in Shanghai, China found that screen usage before bedtime exacerbated symptoms of ADHD in children (32). Additionally, teenagers with ADHD who use screens at night experience shorter sleep durations and increased sleep disturbances (33). Studies conducted in English-speaking countries have indicated that lifestyle factors such as screen time may play a mediating role in the association between childhood ADHD and sleep quality (34). Furthermore, a mediation analysis involving nearly 4,000 high school students in Canada identified impulsivity as a significant mediator of ADHD symptoms among underlying behaviors brought on by screen usage (35). Therefore, we can employ mediated Mendelian randomization for further causal interpretation in subsequent studies to provide additional insight into the causal mechanisms underpinning the effect of screen time on childhood ADHD.
This study examined the genetic basis of the causal association between screen time and childhood ADHD through four perspectives and utilized five different models to assess causality for the first time. The potential cause-and-effect relationship between childhood ADHD and screen time highlights the importance of implementing effective screen time control measures for children and adolescents. Nevertheless, this study has some limitations. Firstly, it should be noted that not all employed methods substantiated the causal relationship we identified. Secondly, through examining scatter plots, we observed that the statistically significant causality might be dominated by certain SNPs, which could be pivotal in the association between screen time and childhood ADHD. Therefore, it is crucial to have access to larger data samples and employ more advanced MR analysis methods to obtain more accurate and precise relationships.
5 Conclusion
This study investigated the underlying causality between screen time and childhood ADHD through a genetic lens. The findings suggested that screen time may be a significant factor in the formation and development of ADHD in children, providing novel insights for further investigation into preventive measures for ADHD in this population.
Data availability statement
Publicly available datasets were analyzed in this study. This data can be found here: https://gwas.mrcieu.ac.uk/datasets/ukb-b-4094/; https://gwas.mrcieu.ac.uk/datasets/ukb-b-17999/; https://gwas.mrcieu.ac.uk/datasets/ukb-b-4522/; https://gwas.mrcieu.ac.uk/datasets/ukb-b-5192/; https://figshare.com/articles/dataset/adhd2022/22564390.
Author contributions
ZM: Writing – original draft, Software, Formal analysis. BA: Writing – review & editing, Conceptualization. WW: Writing – review & editing, Software, Data curation. TN: Writing – review & editing, Software, Data curation. YC: Writing – review & editing, Visualization. XM: Writing – review & editing, Visualization. YH: Writing – review & editing, Writing – original draft, Methodology, Conceptualization.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by the “Study on Commercial Insurance Related to Chinese Medicine Health Services” (Grant No. GHC-2022-ZFGM-014).
Acknowledgments
We extend our appreciation to the website administrators and researchers who are responsible for maintaining the databases utilized in this research.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
- ^ Qu Y, Huang X, Mi J, Chen X, Wu B, Xu J. Education, socioeconomic status, leisure sedentary behaviours and female infertility: Mendelian randomization study. Research Square. Under Review Jan 08, 2024. doi: 10.21203/rs.3.rs-3770062/v1
References
1. Campbell SB, Halperin JM, Sonuga-Barke EJS. A developmental perspective on attention-deficit/hyperactivity disorder (ADHD). Handbook of Developmental Psychopathology In: New York: Springer US (2014).
2. Faraone SV, Sergeant J, Gillberg C, Biederman J. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry. (2003) 2:104–13.
3. Polanczyk GV, Salum GA, Sugaya LS, Caye A, Rohde LA. Annual research review: A meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J Child Psychol Psychiatry. (2015) 56:345–65. doi: 10.1111/jcpp.12381
4. Cherkasova MV, Roy A, Molina BSG, Scott G, Weiss G, Barkley RA, et al. Review: Adult outcome as seen through controlled prospective follow-up studies of children with attention-deficit/hyperactivity disorder followed into adulthood. J Am Acad Child Adolesc Psychiatry. (2022) 61:378–91. doi: 10.1016/j.jaac.2021.05.019
5. Thomas R, Sanders S, Doust J, Beller E, Glasziou P. Prevalence of attention-deficit/hyperactivity disorder: a systematic review and meta-analysis. Pediatrics. (2015) 135:e994–1001. doi: 10.1542/peds.2014-3482
6. Faraone SV, Asherson P, Banaschewski T, Biederman J, Buitelaar JK, Ramos-Quiroga JA, et al. Attention-deficit/hyperactivity disorder. Nat Rev Dis Primers. (2015) 1:15020. doi: 10.1038/nrdp.2015.20
7. Cortese S, Song M, Farhat LC, Yon DK, Lee SW, Kim MS, et al. Incidence, prevalence, and global burden of ADHD from 1990 to 2019 across 204 countries: data, with critical re-analysis, from the Global Burden of Disease study. Mol Psychiatry. (2023) 28:4823–30. doi: 10.1038/s41380-023-02228-3
8. Magee CA, Lee JK, Vella SA. Bidirectional relationships between sleep duration and screen time in early childhood. JAMA Pediatr. (2014) 168:465–70. doi: 10.1001/jamapediatrics.2013.4183
9. Reid Chassiakos Y, Radesky J, Christakis D, Moreno MA, Cross C, Communications CO, et al. Children and adolescents and digital media. Pediatrics. (2016) 138. doi: 10.1542/peds.2016-2593
10. Lissak G. Adverse physiological and psychological effects of screen time on children and adolescents: Literature review and case study. Environ Res. (2018) 164:149–57. doi: 10.1016/j.envres.2018.01.015
11. Stiglic N, Viner RM. Effects of screentime on the health and well-being of children and adolescents: a systematic review of reviews. BMJ Open. (2019) 9:e023191. doi: 10.1136/bmjopen-2018-023191
12. Ahmer Z, Dar MS, Arif M, Shah M, Ain NU, Habiba UE, et al. Screen time and its relationship with attention deficit hyperactivity disorder among children attending A tertiary care hospital. J Pak Med Assoc. (2023) 73:1847–51. doi: 10.47391/jpma.8031
13. Attygalle UR, Hewawitharana G, Wijesinghe CJ. Migraine, attention deficit hyperactivity disorder and screen time in children attending a Sri Lankan tertiary care facility: are they associated? BMC Neurol. (2020) 20:275. doi: 10.1186/s12883-020-01855-5
14. Socrates A. Establishing behavioural networks in psychiatric genetics: polygenic scoring, cross-trait prediction, mediation, and Mendelian randomisation. London: King's College London (2021).
15. Luo J, Chen Y, Tao Y, Xu Y, Yu K, Anwar O, et al. Causal associations between digital device use and suicide risk: A bidirectional Mendelian randomization study. J Affect Disord. (2024) 350:513–20. doi: 10.1016/j.jad.2024.01.126
16. Demontis D, Walters GB, Athanasiadis G, Walters R, Therrien K, Nielsen TT, et al. Genome-wide analyses of ADHD identify 27 risk loci, refine the genetic architecture and implicate several cognitive domains. Nat Genet. (2023) 55:198–208. doi: 10.1038/s41588-022-01285-8
17. Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG. Sensitivity analyses for robust causal inference from mendelian randomization analyses with multiple genetic variants. Epidemiology. (2017) 28:30–42. doi: 10.1097/ede.0000000000000559
18. Bowden J, Del Greco MF, Minelli C, Davey Smith G, Sheehan N, Thompson J. A framework for the investigation of pleiotropy in two-sample summary data Mendelian randomization. Stat Med. (2017) 36:1783–802. doi: 10.1002/sim.7221
19. Boers E, Afzali MH, Newton N, Conrod P. Association of screen time and depression in adolescence. JAMA Pediatr. (2019) 173:853–9. doi: 10.1001/jamapediatrics.2019.1759
20. Wang X, Li Y, Fan H. The associations between screen time-based sedentary behavior and depression: a systematic review and meta-analysis. BMC Public Health. (2019) 19:1524. doi: 10.1186/s12889-019-7904-9
21. Hale L, Guan S. Screen time and sleep among school-aged children and adolescents: a systematic literature review. Sleep Med Rev. (2015) 21:50–8. doi: 10.1016/j.smrv.2014.07.007
22. Maras D, Flament MF, Murray M, Buchholz A, Henderson KA, Obeid N, et al. Screen time is associated with depression and anxiety in Canadian youth. Prev Med. (2015) 73:133–8. doi: 10.1016/j.ypmed.2015.01.029
23. Robinson TN, Banda JA, Hale L, Lu AS, Fleming-Milici F, Calvert SL, et al. Screen media exposure and obesity in children and adolescents. Pediatrics. (2017) 140:S97–s101. doi: 10.1542/peds.2016-1758K
24. Tegelbeckers J, Bunzeck N, Duzel E, Bonath B, Flechtner HH, Krauel K. Altered salience processing in attention deficit hyperactivity disorder. Hum Brain Mapp. (2015) 36:2049–60. doi: 10.1002/hbm.22755
25. Beyens I, Valkenburg PM, Piotrowski JT. Screen media use and ADHD-related behaviors: Four decades of research. Proc Natl Acad Sci U.S.A. (2018) 115:9875–81. doi: 10.1073/pnas.1611611114
26. Christakis DA, Ramirez JSB, Ferguson SM, Ravinder S, Ramirez JM. How early media exposure may affect cognitive function: A review of results from observations in humans and experiments in mice. Proc Natl Acad Sci U.S.A. (2018) 115:9851–8. doi: 10.1073/pnas.1711548115
27. McHarg G, Ribner AD, Devine RT, Hughes C. Infant screen exposure links to toddlers' inhibition, but not other EF constructs: A propensity score study. Infancy. (2020) 25:205–22. doi: 10.1111/infa.12325
28. Yang A, Rolls ET, Dong G, Du J, Li Y, Feng J, et al. Longer screen time utilization is associated with the polygenic risk for Attention-deficit/hyperactivity disorder with mediation by brain white matter microstructure. EBioMedicine. (2022) 80:104039. doi: 10.1016/j.ebiom.2022.104039
29. Janmohammadi S, Haghgoo HA, Farahbod M, Overton PG, Pishyareh E. Effect of a visual tracking intervention on attention and behavior of children with Attention Deficit Hyperactivity Disorder. J Eye Mov Res. (2020) 12. doi: 10.16910/jemr.12.8.6
30. Ziereis S, Jansen P. Effects of physical activity on executive function and motor performance in children with ADHD. Res Dev Disabil. (2015) 38:181–91. doi: 10.1016/j.ridd.2014.12.005
31. Cavalli E, Anders R, Chaussoy L, Herbillon V, Franco P, Putois B. Screen exposure exacerbates ADHD symptoms indirectly through increased sleep disturbance. Sleep Med. (2021) 83:241–7. doi: 10.1016/j.sleep.2021.03.010
32. Tong L, Ye Y, Yan Q. The moderating roles of bedtime activities and anxiety/depression in the relationship between attention-deficit/hyperactivity disorder symptoms and sleep problems in children. BMC Psychiatry. (2018) 18:298. doi: 10.1186/s12888-018-1879-4
33. Becker SP, Lienesch JA. Nighttime media use in adolescents with ADHD: links to sleep problems and internalizing symptoms. Sleep Med. (2018) 51:171–8. doi: 10.1016/j.sleep.2018.06.021
34. Hong GCC, Conduit R, Wong J, Di Benedetto M, Lee E. Diet, physical activity, and screen time to sleep better: multiple mediation analysis of lifestyle factors in school-aged children with and without attention deficit hyperactivity disorder. J Atten Disord. (2021) 25:1847–58. doi: 10.1177/1087054720940417
Keywords: childhood attention deficit hyperactivity disorder, Mendelian randomization study, screen time, causal relationships, genetic
Citation: Meng Z, Ao B, Wang W, Niu T, Chen Y, Ma X and Huang Y (2024) Relationships between screen time and childhood attention deficit hyperactivity disorder: a Mendelian randomization study. Front. Psychiatry 15:1441191. doi: 10.3389/fpsyt.2024.1441191
Received: 30 May 2024; Accepted: 28 August 2024;
Published: 23 September 2024.
Edited by:
Lambert Zixin Li, Stanford University, United StatesReviewed by:
Hanyang Shen, Stanford University, United StatesXian Li, Johns Hopkins University, United States
Copyright © 2024 Meng, Ao, Wang, Niu, Chen, Ma and Huang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Youliang Huang, aHVhbmd5bEBidWNtLmVkdS5jbg==
 Zhuo Meng1
Zhuo Meng1 Youliang Huang
Youliang Huang