- Department of Neuropsychology and Psychopharmacology, Faculty of Psychology and Neuroscience, Maastricht University, Maastricht, Netherlands
Anxiety disorders are the most common type of psychiatric disorders among Western countries. Evidence-based treatment modalities including pharmacological and cognitive-behavioral therapy result in deficient treatment responses. Historical and recent research suggests psychedelic drugs may be efficacious in alleviating anxiety-related symptoms among healthy and clinical populations. The main aim of the present study was investigation of the effects of psilocybin-containing truffles, when taken in a supportive group setting, on ratings of state and trait anxiety across self-reported healthy volunteers. Attendees of psilocybin ceremonies were asked to complete a test battery at three separate occasions: before the ceremony (baseline), the morning after, and 1 week after the ceremony. The test battery included questionnaires assessing state and trait anxiety (State-Trait Anxiety Inventory), mindfulness capacities (Five Facet Mindfulness Questionnaire), and personality (Big Five Inventory). Additionally, the psychedelic experience was quantified with the Persisting Effects Questionnaire and the Ego Dissolution Inventory. The total amount of psilocybin-containing truffles consumed by each participant was recorded, and a sample of the truffles was analyzed to determine psilocin concentrations. Fifty-two attendees (males = 25; females = 25; others = 2) completed parts of the baseline assessment, 46 (males = 21; females = 24; others = 1) completed assessments the morning after the ceremony, and 23 (males = 10; females = 13) completed assessments at the 1-week follow-up. Average psilocin consumption across individuals was 27.1 mg. The morning after the ceremony, we observed medium reductions in anxiety measures (both state and trait) compared to baseline ( = 6.4; p < 0.001 and = 6; p = 0.014, respectively), which persisted over a 1-week period post-ceremony ( = 6.7; p = 0.001 and = 8.6; p = 0.004, respectively). At 1 week post-ceremony, the non-judging facet of the mindfulness scale was increased ( = 1.5; p = 0.03), while the personality trait neuroticism decreased ( = 5.2; p = 0.005), when compared to baseline. Additionally, we found ratings of ego dissolution (mean: 59.7, SD: 28.3) and changes in neuroticism to be the strongest predictors of reductions in state and trait anxiety, respectively. In sum, results suggest rapid and persisting (up to 1 week) anxiolytic effects in individuals with sub-clinical anxiety symptoms, which are related to the acute experience of ego dissolution, as well as lasting changes in trait neuroticism. Results also add support to the feasibility and potential efficacy of group sessions with psychedelics. To understand whether these effects extend to wider populations suffering from heightened anxiety, and the mechanisms involved, further experimental research is needed.
Introduction
Anxiety disorders (e.g., generalized anxiety disorder, panic disorder, social phobia) are the most common psychiatric disorders, with a current worldwide prevalence of 7.3% (1, 2). They were also found to be burdensome and costly to individuals and wider society (3). Despite such a widespread presence, current treatments only provide partial success rates, with pharmacological therapies (benzodiazepine and antidepressant medications) resulting in response rates (typically defined as >50% decrease in symptoms relative to baseline) of 50.8–58.3% (4, 5), and cognitive behavioral therapies (CBT) resulting in response rates of 51.7–53.6% (5, 6) in adults with anxiety disorders. Additionally, the combination of the two approaches has not been found to result in more promising outcomes, with a response rate of 54.2% (5). Further studies have concluded that the exact rate of treatment response also varies per anxiety disorder. For instance, in patients with a lifetime panic disorder, the response rates drop drastically to about 13% for each of the aforementioned therapeutic modalities (7), whereas patients with comorbid anxiety and depression tend to prematurely terminate treatment more frequently than patients with a single diagnosis (8). The above findings illustrate a rising urgency within the field of mental health for efficient fast-acting treatment options that prove efficacious for the large heterogeneous cluster that makes up anxiety disorders, and that persist after treatment.
Before criminalization of psychedelic drugs in the 1970s, studies combining administration of a psychedelic drug and psychological therapy found significant improvements in anxiety-related symptomatology (9). Recently, there has been a resurgence of interest regarding the therapeutic potential of these substances, including psilocybin, ayahuasca, and LSD, in treating an array of different mental health disorders (10–14). More modern trials have assessed the efficacy of psychedelics to reduce anxiety symptoms among patients with a life-threatening illness, and have demonstrated large significant reductions in ratings of anxiety, with a response rate of 60–80% (defined as >50% decrease in measure relative to baseline), sustained over the course of 6–12 months post treatment (15–17), and in a smaller cohort up to 4.5 years post treatment (18). Similar reductions in ratings of anxiety symptoms have been demonstrated in trials assessing the efficacy of a psychedelic to alleviate symptoms of treatment-resistant depression (12, 19, 20), and in naturalistic samples with heterogeneous mental health status (21–23). In healthy volunteers, the persisting effect of psychedelics on feelings of anxiety have been mixed, with one study reporting persisting reductions in acute (state) anxiety 1 week, and reductions in personality-related (trait) anxiety 1 month after psilocybin ingestion (24), and another study reporting no changes in trait anxiety 1 and 12 months after LSD (25). The questionable rigidity in the research design of the earlier studies, including lack of statistical analysis and validated outcome measures (9), and the promising findings of modern trials, warrant further investigation of the persisting effects of ingestion of a psychedelic drug on acute and personality-related anxiety, independent of life-threatening illness or comorbid depression. Furthermore, if psychedelic substances do reduce anxiety, it is of interest to understand what psychological processes may be at play.
The personality trait neuroticism, reflecting an individual’s tendency to experience negative emotions, sensitivity to aversive cues, and insufficient ability to cope with stress, has been found to be the personality trait that is the most strongly associated with many forms of psychopathology (26–31), and a core vulnerability factor common to anxiety and mood disorders (32). Although it has been argued that personality traits are relatively stable throughout adulthood, an array of clinical work has shown that personality is amenable to changes across the lifespan (33), with neuroticism being found to fluctuate to one standard deviation across the lifespan (34). As such, it has been suggested that reducing neuroticism should be the primary focus of therapeutic interventions when treating psychopathologies such as anxiety (33). It has been repeatedly found that ingestion of a psychedelic drug can induce rapid and persisting changes in personality traits, and particularly reductions in neuroticism, in both healthy and clinical populations (24, 35–41). Thus, given the reduction in self-rated neuroticism found after ingestion of a psychedelic, it could be suggested that one mechanism by which psychedelic substances induce persisting changes in anxiety levels could be by altering maladaptive personality structures which exacerbate anxiety. However, the relationship between psychedelic-induced changes in anxiety and psychedelic-induced changes in neuroticism has yet to be assessed.
A further psychological process which may be of particular salience when discussing therapeutic efficacy for anxiety, and which psychedelics have been repeatedly found to enhance, are mindfulness capacities (10, 22, 23, 42–46). Mindfulness has been described as “paying attention in a particular way: on purpose, in the present moment, and non-judgmentally” (47). It is generally considered multifaceted, including capacities such as being able to: notice or attend to internal feelings, thoughts, and external simulation (“observing”), label feelings, thoughts and experience with words (“describing”), attending to what is happening in the present moment (“acting with awareness”), take a non-evaluative stance toward internal thoughts and feelings (“non-judgment of inner experience”), and being able to allow emotions and thoughts to come and go, without being interfered by them (“non-reactivity to inner experience”). Given that one of the core components of anxiety disorders is the practice of excessive rumination on non-present fears, leading to a vicious circle of higher levels of physical arousal and more worrying (48), individuals suffering from anxiety disorders typically lack or have lower levels of mindfulness capacities (49). Accordingly, it has been shown that interventions which enhance mindfulness capacities, such as mindfulness-based stress reduction training (MBSR), can be an effective form of treatment for people with anxiety disorders (50), resulting in higher efficiency and improvement rates than cognitive-behavioral group therapy (51). That said, the relationship between psychedelic-induced changes in mindfulness capacities, and psychedelic-induced changes in anxiety, has yet to be assessed.
Finally, another important factor when thinking about therapeutic applications is the longevity of effects. Usually when taking conventional anxiolytics the treatment duration will vary but might extend over months (5, 6). For psychedelics, persisting effects on personality or wellbeing can be found up to 12 months after a single dose administration (25), whereas increased mindfulness capacities have been found to persist up to 3 months (43). It has been suggested by some studies that the intensity or quality of the psychedelic experience determines the treatment outcome (52–54). Specifically, it has been repeatedly found that psychedelic-induced mystical-type experiences and ego dissolution, the latter a phenomenon characterized by the reduction in self-referential awareness, disruption self-world boundaries, and increased feelings of unity with one’s surroundings (55), correlates with long-term (positive) outcomes (23, 52–54, 56–58). Thus, in the present study we also assessed whether we could predict sub-acutechanges in anxiety based on acute ratings of ego dissolution.
In sum, anxiety symptoms and disorders evoke a notable impact on people’s lives, yet the existing treatment options are of limited success. Based on this and previous findings of psychedelic-induced alleviation of anxiety in clinical populations, the present study was designed to assess the sub-acute effects of psilocybin in self-reported healthy retreat attendees on state and trait anxiety, when taken in a supportive group setting. The population is informative to investigate as sub-clinical, “healthy” samples often report meaningful anxiety symptoms that impact one’s well-being and quality of life (59–63), however, due to the lack of clinically established severity of symptoms, it is unlikely that this population is recruited into randomized clinical trials. Thus, this sample of retreat attendees presents an opportunity to explore psychedelic-induced effects in a clinically under-represented, but highlighly salient sample. Additionally, the retreat setting presents an opportunity to assess the feasibility and efficacy of group sessions with psychedelic substances, a likely increasingly popular context upon regulatory rescheduling of psychedelic compounds, as well as a potentially more cost- and time-efficient clinical therapeutic approach. In this context, we also aimed to replicate the previously reported findings on the substance’s ability to increase mindfulness capacities and decrease neuroticism (10, 22, 23, 37–39, 43, 44, 46). As previously rationalized, that such changes may be related to reductions in anxiety, we further aimed to assess whether changes in mindfulness capacities and neuroticism correlated with changes in anxiety. Lastly, we wanted to assess the relationship between psychedelic-induced changes in state and trait anxiety and ego dissolution.
We hypothesized that, compared to baseline, reductions in state and trait anxiety and neuroticism would be observed 24 h and 7 days after ingestion of psilocybin, whereas mindfulness capacities would be enhanced. Furthermore, we hypothesized that reductions in ratings on both aspects of anxiety would be negatively correlated with enhancements in mindfulness capacities and positively correlated with reductions in the personality trait, neuroticism. Finally, we hypothesized that positive changes in ratings of anxiety would be correlated with higher subjective ratings of ego dissolution, the latter measured with the Ego Dissolution Inventory (55).
Materials and Methods
Participants and Study Procedure
Participants were volunteers attending legal psilocybin retreats in the Netherlands, organized by the Psychedelic Society UK. Attendees of those ceremonies were either invited to participate in the study on site, or contacted the researchers by email after hearing about the study through the retreat organizers. To participate in the study, volunteers had to be a minimum of 18 years old and proficient in English. Participants were assessed 3 times: at baseline (the evening before psilocybin ingestion), within 24 h after psilocybin ingestion (hereafter referred to as: sub-acute) and 7 days after psilocybin ingestion (hereafter referred to as: follow-up). Seven-days later, participants received the final follow-up measurement online (through Qualtrics). The total amount of truffles (g) taken by each participant was recorded, and a sample of the truffles was taken to determine the concentrations of alkaloids afterwards.
The study was conducted in accordance with the Declaration of Helsinki and subsequent amendments concerning research in humans and was approved by the Ethics Review Committee of Psychology and Neuroscience and Maastricht University (ERCPN-175_03_2017_A5). Participation was voluntary and no incentives to participate were provided. All volunteers gave their written informed consent prior to participation. The research team was not involved in the screening, preparation, organization, administration, and supervision of the psilocybin ceremonies that were visited.
Psilocybin Retreats
Prior to participation in the retreat, personal intakes were done by the facilitators, which included screening for (and excluding) individuals with psychiatric disorders or taking psychiatric medications, and medical factors like high blood pressure.
The setting in which psilocybin was taken was the same throughout all of the retreats. Participants stayed in a large house set in nature, hosted by at least two or more experienced psilocybin facilitators. They arrived the evening before psilocybin administration, and were able to get acquainted with each other, the facilitators, and the schedule of the retreat. Participants were able to discuss their intentions in the group, and participated in group activities to get to know each other. The next day, after a group breakfast, participants received the psilocybin-containing truffles around noon, in a tea form. Facilitators provided music, tools to draw and/or write, food, and overall support. Support was not a guiding of the experience, but more so making sure participants were safe, comfortable, and holding space when necessary. In the evening, all participants and facilitators came back together as a group. The next morning, all participants had breakfast together, had time for integration experiences (including drawing, journaling, walking) and had a closing group meeting. To note: the retreat attendees were individuals who wanted to have a safe psychedelic experience. No therapy was given during the retreat, but rather the role of the facilitators was to provide a safe space for this experience, and to encourage reflection on the experience in the following days.
Psilocybin
Participants ingested the truffles in a tea form, guided by the facilitators. To do this, the truffles were crushed, and boiling hot ginger tea was added. After infusing for a few minutes, the participants drank the tea, and were subsequently free to add more water and repeat the process 2–3 times. Afterwards participants could eat the remaining truffle contents in the cup. Previous experimental studies have demonstrated that subjective alterations after psilocybin intake begin 20–40 min following administration, peak around 60–90 min, and subside by 6 h post-intake (64). However, anecdotal reports suggest that when ingested in tea form, subjective alterations are felt more quickly, and for a shorter amount of time (65).
The total amount of psilocybin truffles taken by each participant was recorded, and a sample of the truffles was taken to determine concentrations of psilocybin and its metabolite, psilocin. The German Central Customs Authority determined the contents of psilocin and psilocybin after freeze-drying the truffles using a previously described HPLC method (66).
Assessments
The assessments included a basic demographic section and six questionnaires: the State-Trait Anxiety Inventory (STAI), the Five Facet Mindfulness Questionnaire (FFMQ), the Big Five Inventory (BFI), the Persisting Effects Questionnaire (PEQ), and the Ego Dissolution Inventory (EDI). All materials were provided in English. The STAI and FFMQ were filled out three times, i.e., at baseline, sub-acute session, and follow-up. The BFI was administered twice, during the baseline and the follow-up session. Whereas the remaining 2 questionnaires were only completed once; the EDI during the sub-acute session, to assess the magnitude of the psychedelic experience in retrospect, and the PEQ at the 7 day follow-up, to assess persisting effects and the significance of the experience.
State-Trait Anxiety Inventory
The State-Trait Anxiety Inventory [STAI; (67)] is a 40-item rating scale with a 4-point response format, ranging from 1 (almost never) to 4 (almost always) that is scored into two sub-scales (state anxiety and trait anxiety). For “state” anxiety questions, participants were asked to select the response for each item that best describes how they feel “right now, that is, at this moment.” For “trait” anxiety questions, participants were asked to select the response that best describes how they “generally feel, that is, most of the time.” The reverse-scored and (e.g., “I feel pleasant”) and direct-scored (e.g., “I feel nervous and restless”) items are summed per each subscale to create a total score which ranges between 20 and 80, with higher scores indicating greater anxiety. Internal consistency coefficients for the scale have been shown to range from 0.86 to 0.95 and test-retest reliability coefficients from 0.65 to 0.75 over a 2-month interval (68). Considerable evidence attests to the construct and concurrent validity of the scale (68). When evaluating clinical anxiety according to the STAI, a cutoff score of 40 for state anxiety is commonly used to define probable clinical levels of anxiety, whereas a cut-off score of 44 for trait anxiety is used (69).
Five Facet Mindfulness Questionnaire
The Five Facet Mindfulness Questionnaire, 39 items, [FFMQ; (70)] measures five different factors: (1) Observe: noticing external and internal experiences, e.g., body sensations, thoughts, or emotions; (2) Describe: putting words to, or labeling the internal experience; (3) Acting with awareness: focusing on the present activity instead of behaving mechanically; (4) Non-judging the inner experience: taking a non-evaluative stance toward the present experience, thoughts, or emotions; and (5) Non-reacting to the inner experience: allowing thoughts and feelings to come, without getting caught up in, or carried away, by them. Sample item of the Observe dimension is: “When I take a shower or bath, I stay alert to the sensations of water on my body.” Participants were asked to rate the degree of concordance with each statement on a 5-point Likert scale that ranges from 1 (never or very true) to 5 (very often or always true), for 39 statements. The FFMQ has shown adequate psychometric properties in both non-clinical and clinical samples. Cronbach’s α for each individual sub-scale range from 0.75 to 0.91 (70), and the internal consistency of the scale in our sample was of 0.83 and 0.86 (pre- and post-intake, respectively).
Big Five Inventory
The Big Five Inventory [BFI-44; (71)] was used to measure the Big Five personality dimensions, specifically: (1) Extraversion (8 items); (2) Agreeableness (9 items); (3) Conscientiousness (9 items); (4) Neuroticism (8 items) and Openness (10 items), total of 44 items. Those prototypical traits defining each of the Big Five dimensions are assessed by short and easy-to-understand phrases, for example: “I see myself as someone who is talkative.” The items are rated on a 5-point Likert scale ranging from 1 (disagree strongly) to 5 (agree strongly). The direct and reverse-scored items for each dimension are summed together to create a total score, which, given the variability in terms of number of items, ranges between 8 and 40, 9 and 45, or 10 and 50. The BFI scales have shown substantial internal consistency, retest reliability, and clear factor structure, as well as considerable convergent and discriminant validity with longer Big Five measures (72, 73).
Persisting Effects Questionnaire
The Persisting Effects Questionnaire (PEQ) is a 143-item long scale aiming to assess changes in attitudes, moods, behavior, and spiritual experience (74). Prior research found that PEQ is sensitive to the prolonged effects of psychedelics, occurring even a 1 year after the ingestion (25). Due to time constraints, the current study used a shortened version of the scale (90 items), including five out of six main categories: attitudes about life (Number of items (N) = 26); attitudes about self (N = 22); mood changes (N = 18); relationships (N = 18); and behavioral changes (N = 2). The 86 items of these five categories were rated on a 6-point scale (ranging from 0 = none to 5 = extreme). The scores of the resulting 10 scales (positive and negative scales for each of 5 categories) were assessed by calculating mean (SE) separately for each category.
The questionnaire also included four questions rated on an eight-point scale (1 = no more than routine, and 8 = the single most meaningful experience of my life): (1) “How personally meaningful was the experience?”; (2) “Indicate the degree to which the experience was spiritually significant to you?”; (3) “How psychologically challenging were the most psychologically challenging portions of the experiences?”; (4) “How personally psychologically insightful to you were the experiences?” (57, 75).
Ego Dissolution Inventory
The Ego Dissolution Inventory (EDI) is an eight-item self-report scale that assesses the participant’s experience of ego dissolution (76). In the present study, the original, English version was used to acquire a better understanding of the experiences the participants had about ego dissolution during the psilocybin ceremony. For example “I experienced a dissolution of my “self” or ego” and “I felt at one with the universe.” The participants answered the scale with endpoints of either 0% (No, not more than usual) or 100% (Yes, I experienced this completely/entirely). The EDI was scored by calculating the mean of all items, with a higher total score indicating a stronger experience of ego dissolution. The scale has been shown to have excellent internal consistency (76). The investigation of convergent validity of the scale has shown strong positive correlations between EDI and the mystical-type (or “peak”) of experience (76).
Statistical Analyses
Data analyses and visualizations were performed using the Seaborn (version 0.11.2), Statsmodels (version 0.12.2), Scipy (version 1.7.1), and Patsy (version 0.5.1) packages for Python 3.8. A separate multi-linear regression model using the ordinary least square method (OLS) was fit for each outcome variable. The model included Session encoded as a dummy independent variable of three levels: baseline, the sub-acute and follow-up sessions. Subsequently, separate contrasts were performed between baseline and sub-acute as well as baseline and follow-up sessions.
Quantification of the acute experience was done by analyzing the results of EDI. Descriptive statistics (mean, standard deviation, range of scores) were calculated for the ratings of ego dissolution, together with a visual representation of kernel density estimation. To quantify the persisting functional outcomes of the experience, main outcome measures and additional questions of the PEQ were aggregated and reported in a tabular form.
Additionally, we sought to examine previously reported associations between anxiety and personality (77, 78) as well as between anxiety and mindfulness capacities (49, 50). Given that ratings of ego dissolution have been shown to correlate with persisting effects after a psychedelic experience in both clinical and naturalistic studies (23, 52–54, 56, 57), we tested for the possible associations between EDI scores and changes in anxiety. Canonical correlations (79) were conducted to evaluate the association between psilocybin-induced changes in (i) self-rated mindfulness capacities and neuroticism, (ii) ratings of ego dissolution, and (iii) state and trait anxiety. Variables were separated into two sets; set 1 included the psychological processes (i) and acute ratings of ego dissolution (ii) as predictors, and set 2 included the anxiety variables as criterion (iii). Canonical correlations were chosen as this approach assesses the relationship between two multivariate data sets, allowing investigation of variables that may have multiple causes and effects, while also reducing the potential of type 1 error (79).
Finally, we ran an exploratory analysis (independent sample t-tests and chi-square tests) with a twofold purpose: (1) to examine if there are differences between psilocybin-naïve and experienced participants on the anxiety measures (both state and trait anxiety); (2) to assess attrition factors for variables that have previously found to be significant in similar studies [i.e., demographic variables and personality traits; (80)], as well as study-specific factors of interest [i.e., baseline anxiety levels (state and trait) and acute drug effects (EDI scores)].
For all statistical analyses, the alpha criterion level of statistical significance was set at p ≤ 0.05 and Cohen‘s effect (d) size was reported in case of significant results to demonstrate the effect’s magnitude with 0.2–0.5 considered as small, 0.5–0.8 as a medium, and >0.8 as large effect size (81).
Results
Participants and Dose
Demographic information and concentrations of the psilocybin sample are all previously published elsewhere, and briefly summarized here (82).
Participants
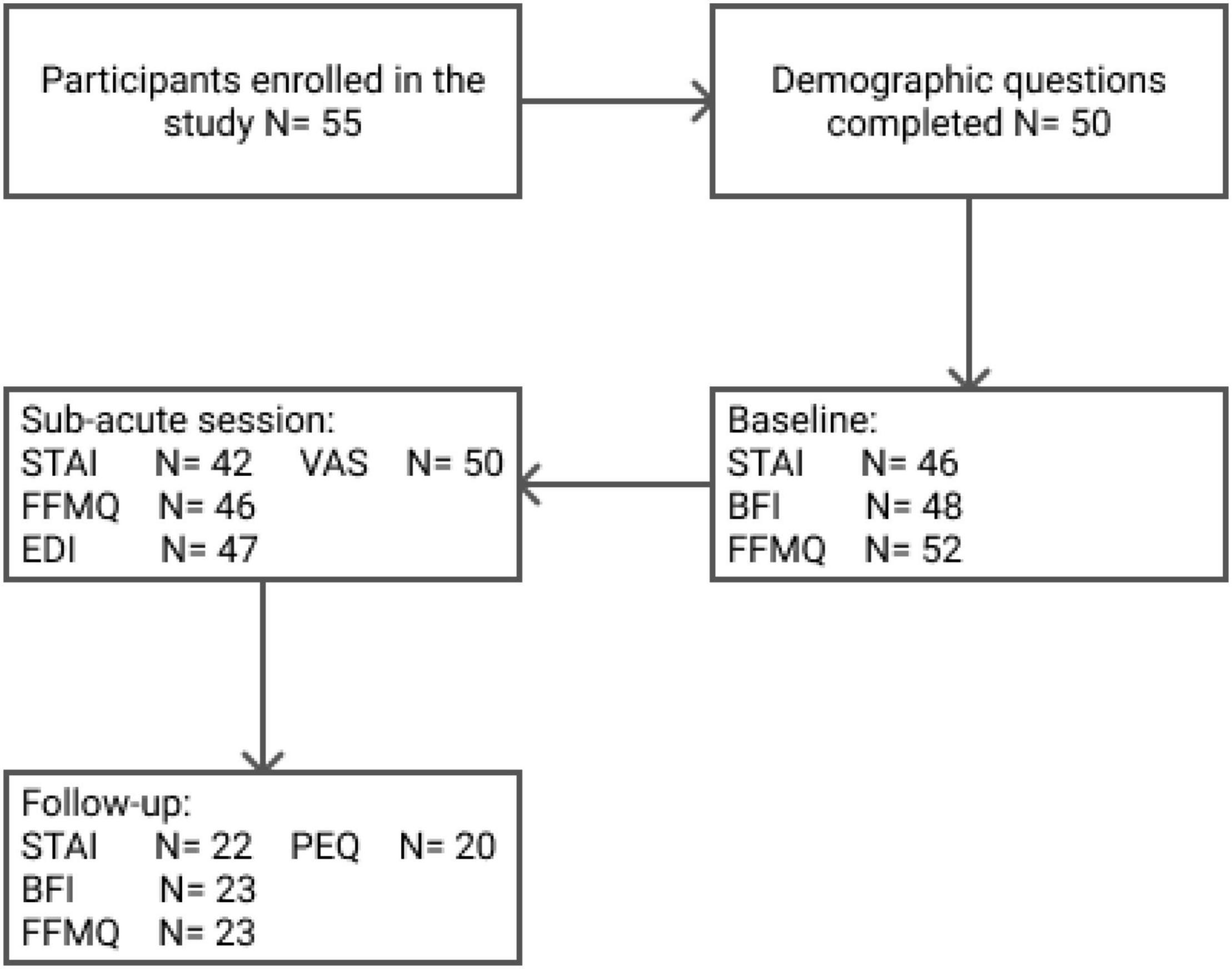
Fifty-five volunteers agreed to participate in the present study and signed the informed consent. Of those 55 participants, 47% (N = 26) identified themselves as males, 47% (N = 26) as females, and 5% (N = 3) reported identification with other gender categories. The exact numbers of participants’ enrollment and questionnaire completion are shown in Figure 1. Incomplete or missing test batteries were due to time constraints, as attendees must carry on with the semi-fixed retreat schedule, or participant drop-out.
The mean age of the entire group was 34.8 (SD = 8.9), ranging from 20 to 58 years. The highest completed levels of education were graduate school (41.8%), undergraduate school (41.8%), secondary school (7.3%), or undisclosed (9.1%). Most participants were from Europe (80%), while the rest were from North America (7.3%), Africa (3.6%), Central America (1.8%), Asia (1.8%), or undisclosed (5.4%). About half of the sample had previous experience with classical psychedelics (psilocybin = 52.7%; LSD = 40%; ayahuasca = 52.7%; DMT = 58%), MDMA (56%), and the majority had experience with cannabis (78%). For 69.1% of the participants, this was the first time taking a psychedelic in a retreat setting.
Psilocybin Sample
The truffle sample (15 grams; Psilocybe Hollandia) contained 1.9 mg of psilocybin and 10.5 mg of psilocin. Participants ingested an average (SD) 34.2 (8.9) grams of truffles. Once ingested, psilocybin is quickly metabolized to psilocin at a calculation factor of 0.719, resulting in a final (average) psilocin consumption of 27.1 mg.
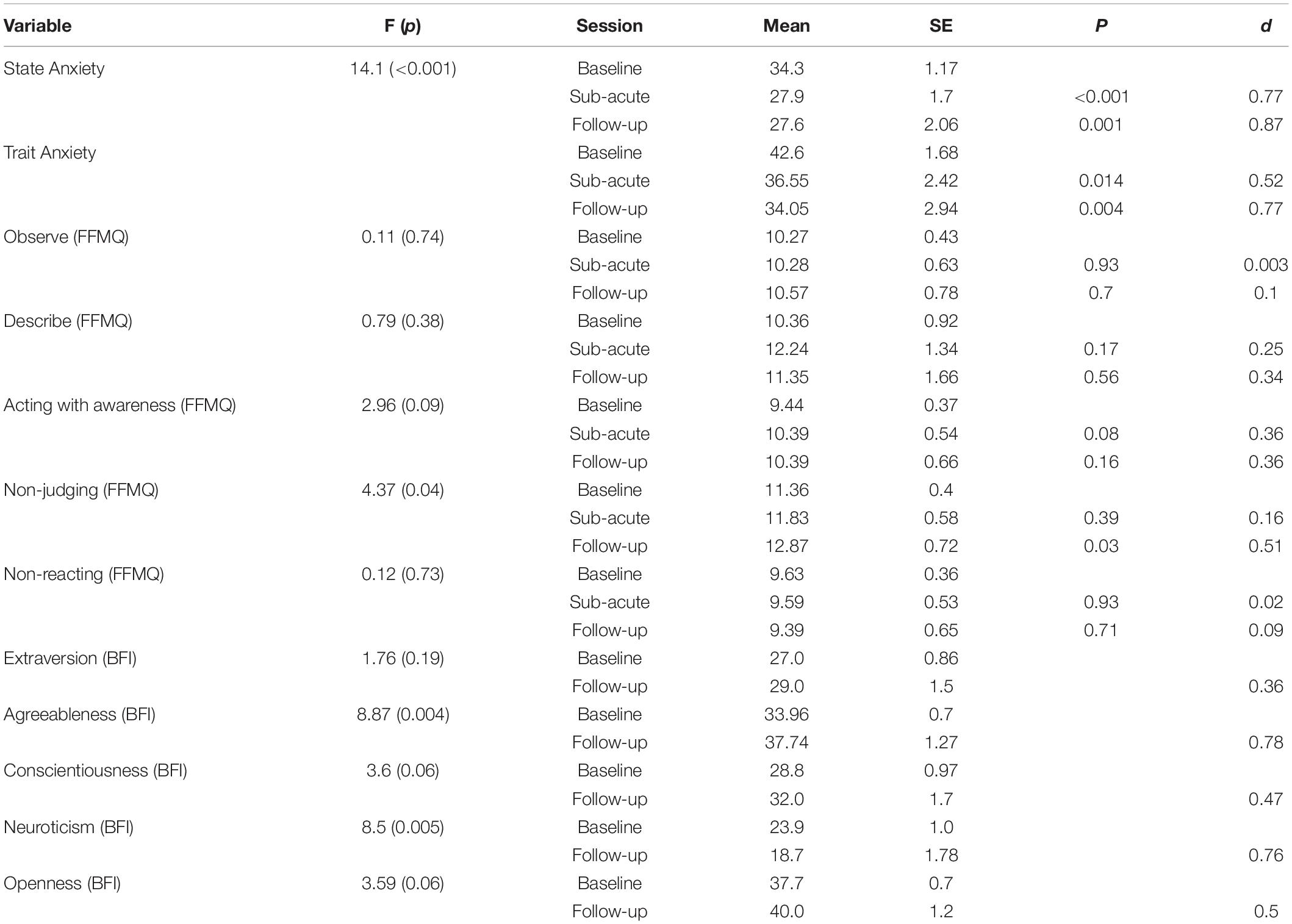
State-Trait Anxiety Inventory
Overall 46 (at baseline), 42 (at the morning after the ceremony), and 22 (at 1 week after the ceremony) participants completed all the parts of STAI and were included into analyses. The OLS multi-linear regression revealed a significant main effect of Session [F(2, 107) = 14.10; p < 0.001] on scores capturing state anxiety. Compared to baseline, participants’ state anxiety reports were 6.4 points lower the morning after the psilocybin ceremony (p < 0.001; d = 0.77), and 6.7 points lower 1 week after the ceremony (p = 0.001; d = 0.87; Figure 2). Session was also found to have significant effects on estimates of trait anxiety [F(2, 107) = 10.13; p = 0.002]. Specifically, compared to baseline, self-rated trait anxiety was about 6 points lower the morning after the ceremony (p = 0.014; d = 0.52) and 8.6 points lower 1 week after the ceremony (p = 0.004; d = 0.77; Figure 3) on a 60- point range.
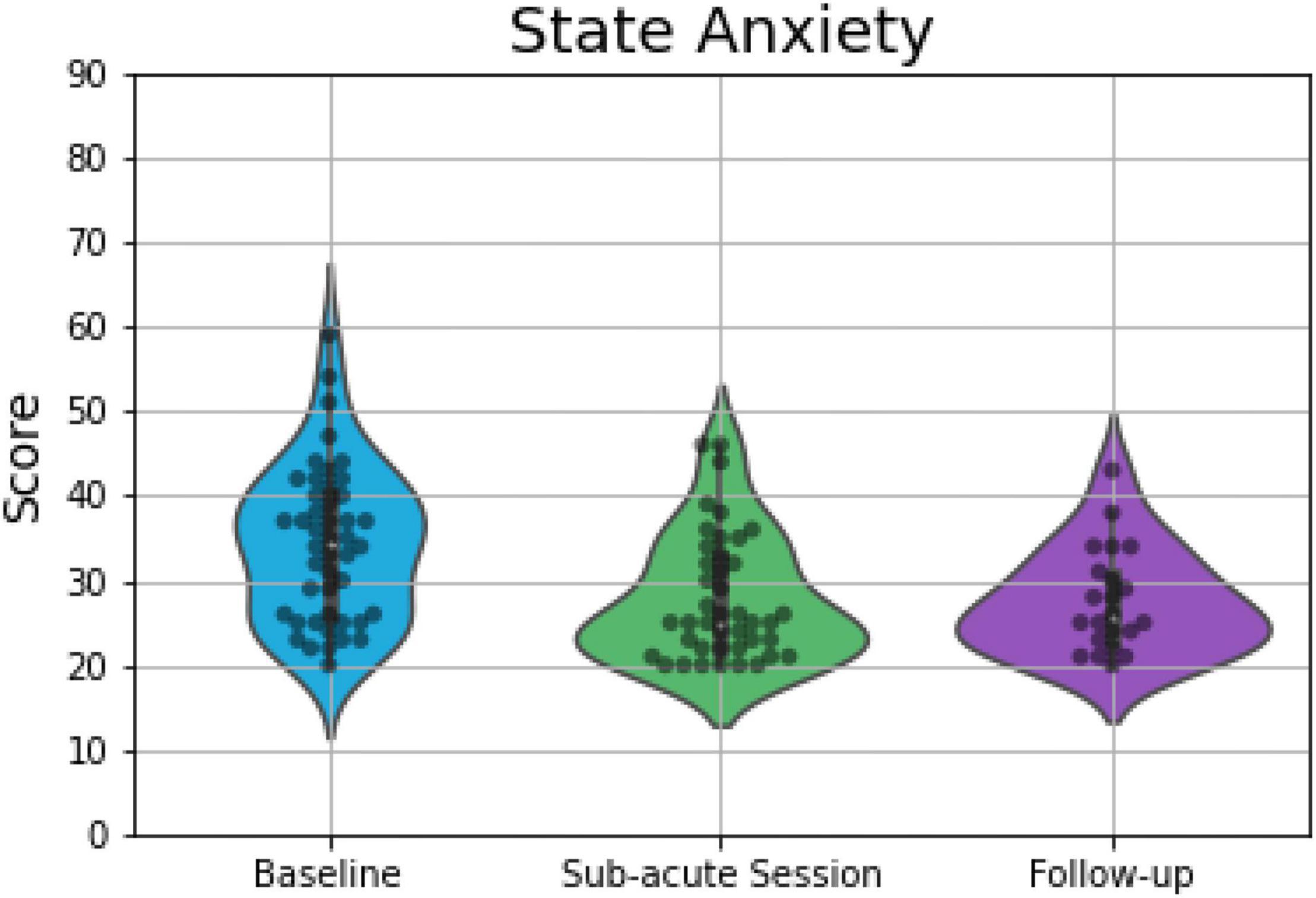
Figure 2. Violin plots displaying scores on measures of state anxiety, which demonstrated significant differences between baseline and the other two time points. The plot consists of median (SE) ratings of state anxiety before, 1-day after and 7-days after psilocybin truffles. The thick line indicates the interquartile range, whereas the white dot indicates the median. Each gray dot indicates a data point, whereas the density is scaled to the relative count across all bins. Wider sections of the violin plot represent a higher probability of observations of a given value.
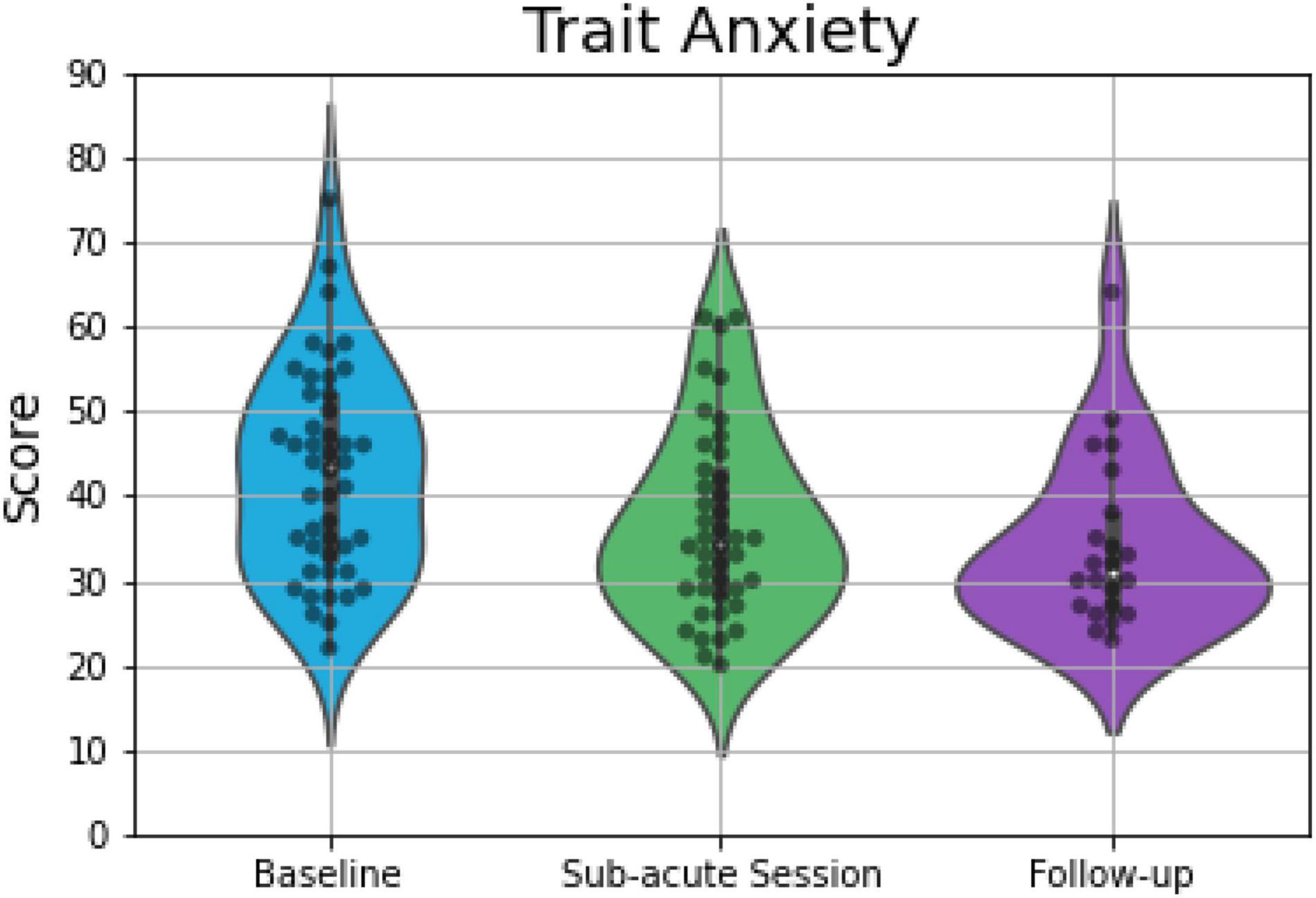
Figure 3. Violin plots displaying scores on measures of trait anxiety, which demonstrated significant differences between baseline and the other two time points. The plot consists of median (SE) ratings of trait anxiety before, 1-day after and 7-days after psilocybin truffles. The thick line indicates the interquartile range, whereas the white dot indicates the median. Each gray dot indicates a data point, whereas the density is scaled to the relative count across all bins. Wider sections of the violin plot represent a higher probability of observations of a given value.
Five Facet Mindfulness Questionnaire
In total, 52 (at baseline), 46 (at the sub-acute session), and 23 (at the follow-up session) participants completed the FFMQ. The OLS multi-linear regression revealed a significant main effect of Session on the Non-judge dimension [F(2, 118) = 4.37; p = 0.04] of the FFMQ. The contrasts analysis showed, in comparison to the baseline, a 0.5 increase in non-judgmental mindfulness capacities the morning after the ceremony (p < 0.39; d = 0.17) and 1.5 increase at the follow-up (p = 0.03; d = 0.51). There was no main effect of Session on the remaining, four facets (Table 1).
Big Five Inventory
The BFI was completed by 48 and 23 participants at baseline and follow-up, respectively. The OLS multi-linear regression model revealed a significant main effect of Session on Neuroticism [F(1, 69) = 8.46; p = 0.005] and Agreeableness [F(1, 69) = 8.87; p = 0.004] of the BFI. The two traits showed an opposite pattern of changes over time. While, in comparison with baseline, participants scored 5.2 points lower on Neuroticism (d = 0.76) at the follow-up, they scored 3.8 points higher on Agreeableness (d = 0.78). There were no main effects of Session on the remaining three personality traits (Table 1).
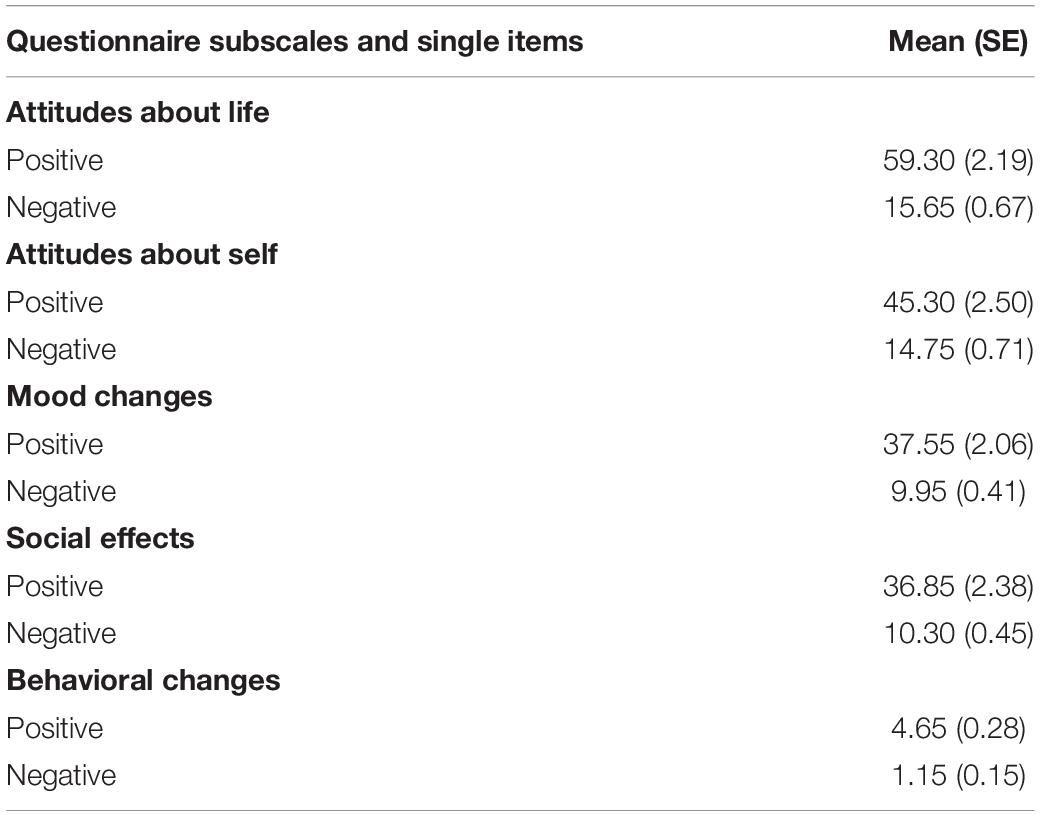
Persisting Effects Questionnaire
In total, 20 participants filled in the PEQ 7 days after the ceremony. Mean (SE) of the positive and negative ratings assessing attitudes, mood, social effects, and behavior are presented in Table 2.
On the question, “how personally meaningful was the experience,” 2 (10%) rated it as the single most meaningful experience of their lives, whereas 10 (50%) and 2 (10%), rated it as among the 5 and 10 most meaningful experiences of their lives, respectively. Two participants (10%) rated it as similar to the meaningful experiences that occur on average once every 5 years, three (15%) stated it to be similar to meaningful experiences that occur once a year, and one (5.0%) stated it was similar to experiences that occur on average once a month.
On the question, “how spiritually significant was the experience,” 3 (15%) rated it as the most spiritually significant experience of their lives, whereas 8 (40%) and 3 (15%) rated it as among the 5 and 10 most spiritual experiences of their lives, respectively. Three participants (15%) rated it as similar to the spiritually meaningful experiences that occur on average once every year, 2 (10%) stated it was similar to spiritually meaningful experiences that occur once a month, and one (5.0%) stated it was no more spiritual than a routine, everyday experience.
In regards to how psychologically challenging the experience was, 1 (5%) rated it as the single most difficult or challenging experience of their lives, 6 (30%) rated it as among the 5 most challenging experiences of their life, and 1 (5%) rated it as among the top 10 most challenging experiences of their lives, followed by 3 (15%) stating it was similar to the challenging experiences that occur every 5 years, 3 (15%) who said occur every once a year, 4 (20%) who said occur once a month, 1 (10%) who said occur once a week, and 1 (10%) who stated it was no more psychologically challenging than a routine, everyday experience.
Finally, regarding the psychological insightfulness of the experience, 7 (35%) stated the experience to be the single most psychologically insightful experience of their life, 6 (30%) and 2 (10%) stated among the 5 and 10 most insightful experiences, respectively. Three (15%) stated that the experience was similar to psychologically insightful experiences that occur on average once every 5 years, one (5%) stated similar to experiences that occur on average once a month, and one (5%) stated the experience was no different from every psychologically insightful experience.
Ego Dissolution Inventory
The EDI was completed by 47 participants the morning after the ceremony. The mean (SD) of participants who filled in the Ego Dissolution Inventory was 59.7 (28.3), with ratings varying between 3 (minimal reported score) and 100 (maximal reported score). The kernel density estimate of the probability density function of the individual EDI scores is presented in Figure 4.
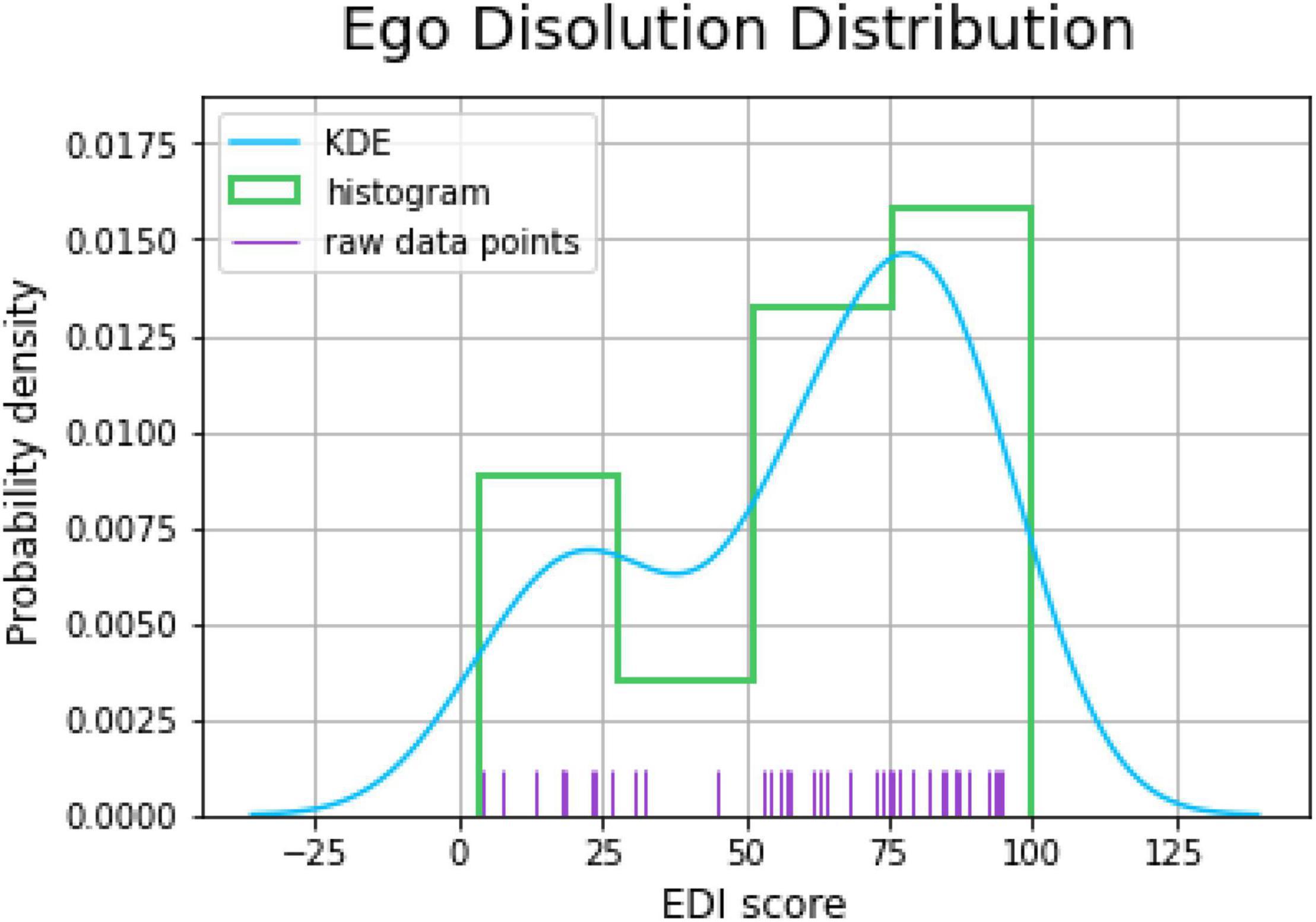
Figure 4. Probability distribution plot of the experience of ego dissolution as assessed by the EDI morning after the psilocybin ceremony. The plot depicted kernel density estimation (KDE), histogram, and raw data points.
Hypothesis-Driven Correlations
A canonical correlation analysis was conducted using the three psychological variables which demonstrated significant effects as predictors (follow-up (change) scores on non-judge dimension of FFMQ, follow-up (change) neuroticism scores, and EDI scores) of the four anxiety outcome measures: sub-acute and follow-up (change) scores on state and trait anxiety measures. The analysis yielded three functions with squared canonical correlations (Rc2) of 0.891, 0.324, and 0.096 for each successive function. The full model across all functions was statistically significant [F(12, 18.81) = 2.81, p = 0.022], explaining 93.4% of the variance. From this model, the first two functions were considered noteworthy in the context of this study, explaining 89.1% and 32.4% of the variance, respectively.
Table 3 presents the standardized canonical function coefficients, the structure coefficients (rs), and the squared structure coefficients (rs2) for each function, as well as the communalities (h2) across the functions for each variable [for an in-depth explanation and interpretation of canonical correlations and associated terminology, the reader is referred to (79)]. Function 1 indicated that the dominant contributors were sub-acute and long-term changes in trait anxiety, whereas the dominant predictor was the change in neuroticism, and the secondary predictor was changes in non-judgment. Overall, this function suggests that the strongest predictor of changes in trait anxiety were changes in neuroticism.

Table 3. Canonical solution for psychological variables predicting state and trait anxiety for Functions 1 and 2.
Function 2 indicated that the dominant contributors were sub-acute and long-term changes in state anxiety, with the dominant predictor of ratings of EDI. Overall, this function suggests that the strongest predictor of changes in state anxiety was higher ratings in ego dissolution.
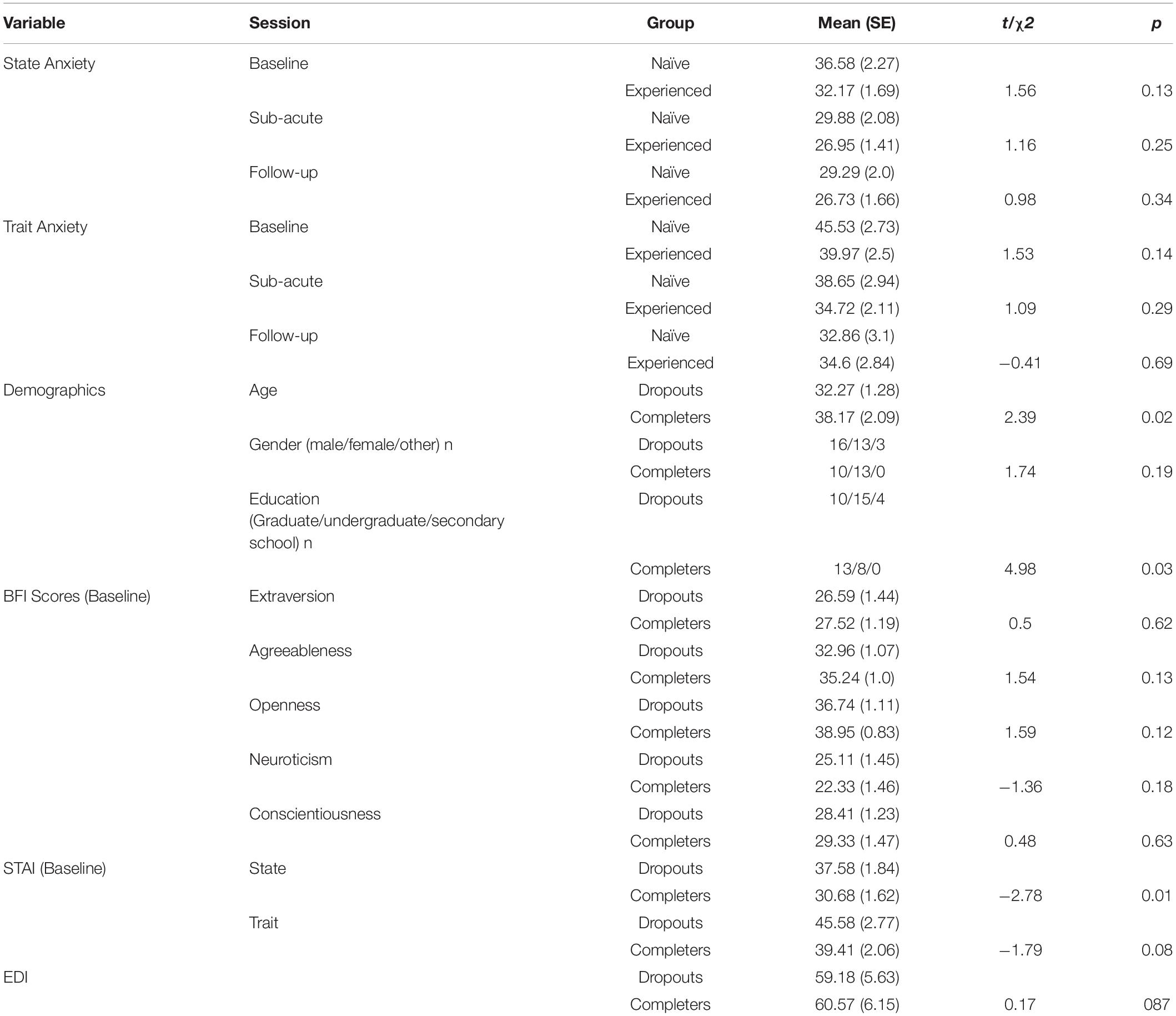
Exploratory Analysis
The first goal of the exploratory analysis was to evaluate whether participants with a previous experience with psilocybin (N = 29) differed from the naïve participants (N = 21) on measures of anxiety. None of the six independent sample t-tests (2 STAI measurements × 3 assessment points) found significant differences between the groups (see Table 4 for details), suggesting that the previous experience with psilocybin had no effect on the anxiety changes observed in the present study. The second goal of the exploratory analysis was to investigate the determinants of attrition. Tests (9 independent sample t-tests: Age, 5 personality traits, 2 STAI measurements, and EDI score; 2 chi-square tests: Gender, Education) revealed significant differences for the age (t = 2.39; p = 0.02), education (χ2 = 4.98; p = 0.03), and baseline state anxiety (t = −2.78; p = 0.01) between those who completed the 1-week follow-up assessment (N = 23) and those who did not (N = 32). Analysis indicated that those who dropped out were younger, reached a lower level of education, and had higher baseline state anxiety levels than those who completed the study. There were no significant differences between the groups in terms of gender, personality traits, baseline trait anxiety, or ego dissolution (see Table 4 for details).
Of note, anecdotal statements from the participants who dropped out also claimed demographic-unrelated reasons for not completing the study, or for turning in the follow-up measurement past the 1 week deadline (meaning the follow-up measurement was not included in our final analysis). Reasons included travel, as many people attended the retreat from abroad, and stayed in the Netherlands for some time afterward to travel around, or work, as some people took time off to attend the retreat, and thus used the following week to catch up on work.
Discussion
The impact of anxiety symptoms and disorders on people’s lives and the treatment challenges are well-known within the field of mental health (2, 5, 7, 83, 84). The current study investigated the effects of a single administration of psilocybin on ratings of state and trait anxiety across retreat attendees, when taken in a supportive retreat setting. We further explored hypothesized psychological processes which may predict reductions in anxiety. Compared to baseline measures, we observed medium to large reductions in state anxiety ratings, and medium decreases in trait anxiety ratings, which persisted over a 1 week period post the ingestion of psilocybin. Additionally, we found enhancements in self-rated mindfulness capacities and alterations in personality traits at 1 week post ceremony. Regarding the post-retreat changes in anxiety, analyses showed that ratings of neuroticism and ego dissolution were the most strongly correlated with reductions in trait and state anxiety, respectively.
The present study’s findings are in line with results from historical (clinical) studies, which suggest reductions of anxiety symptoms after a combination of psychedelic drug administration and psychological therapy (85). Similarly, recent clinical studies have found reductions of anxiety in patients with life-threatening illness and/or comorbid treatment-resistant depression after administration of psilocybin (16, 17, 19, 20), LSD (15), and ayahuasca (12). Our findings complement clinical work by demonstrating sub-acute reductions in both anxiety estimates in a self-reported healthy population, whom demonstrate STAI ratings under the clinical threshold (69). This population is informative because sub-clinical, psychologically “healthy” samples often report meaningful anxiety symptoms that impact daily life, including feelings of distress and impairments in cognitive functioning, work performance, and sleep quality (59–63). Importantly, as these symptoms do not meet diagnostic criteria for a clinical disorder, such symptoms often go untreated, and such populations are often under-represented in clinical trials. Thus, the current findings provide preliminary evidence that psilocybin-assisted psychotherapy may also be a treatment option for individuals with sub-clinical anxiety symptoms, if they choose to seek an intervention for their symptoms.
That said, two previous experimental studies assessing the effect of a psychedelic on anxiety symptoms in healthy volunteers have demonstrated mixed results. Whereas one study showed reductions in state anxiety 1 week post administration, and reductions in trait anxiety 1 month post-administration, of a high dose of psilocybin (25 mg/70 kg), another study found no changes in trait anxiety one and 12 months after a high dose of LSD (200 μg) (24, 25). Additionally, previous naturalistic work with individuals reporting heterogenous mental health status also found reductions in anxiety after participation in a 5-MeO-DMT ceremony (22), however a more recent placebo-controlled observational study found that state anxiety ratings decreased 24 h after volunteers ingested either a placebo, or the psychedelic substance ayahuasca, during the context of a group retreat (86). Taking these findings together, one could hypothesize that the significant reduction in anxiety-related symptoms in our self-reported healthy sample is due to both pharmacological and extra-pharmacological factors. A noteworthy extra-pharmacological factor in our study, and some of the previously mentioned studies (22, 86), is the consumption of a psychedelic drug in a group context. Psychedelic drugs have been found to modulate social cognition and interpersonal experiences (87), and individuals whom have undergone psychedelic therapy with psychological support have indicated that increased feelings of social connectedness were an important aspect of the therapeutic process (88). Thus taking together the aforementioned reports, as well as reports from historical research with psychedelic-assisted group therapy [see (89), for a review], it could be hypothesized that the incorporation of groups into psychedelic-assisted psychotherapy may enhance therapeutic outcomes (89). Whereas contemporary psychedelic-assisted group therapy trials are currently limited to one (90), outside of the clinical setting psychedelic drugs have been used for centuries in traditional communal settings. Thus, the retreat setting captured in this study adds further evidence to the feasibility and efficacy of group sessions with psychedelic substances. The latter should also be highlighted, as it will likely be an increasingly popular context upon regulatory rescheduling of psychedelic compounds, as well as a potentially more cost- and time-efficient clinical therapeutic approach.
In line with previous studies (37–39), we detected 1-week decreases in trait neuroticism, which has been shown to be strongly associated with the acuity and comorbidity levels of a range of mental disorders (77, 78). Interestingly, levels of neuroticism have been found to correlate positively with frontolimbic serotonin 5-HT2A receptor binding, the latter being the main target of psychedelic drugs (28, 91), suggesting direct 5-HT2A agonism may be the biological basis by which these substances alter neuroticism. Findings from the current and previous studies suggest that a psychedelic-assisted intervention can reduce levels of neuroticism, which are related to reductions in anxiety ratings in our study, and could be related to reductions of symptoms of comorbid conditions such as depression or post-traumatic stress disorder as seen in other studies. We also found post-retreat increases in trait agreeableness, which is in line with a previous naturalistic work done by Weiss et al. (41). Other studies have shown either no changes in agreeableness post-psilocybin experience in depressed patients (37) or higher agreeableness scores among psychedelics users when compared to the general population (38). In contrast with other studies (20, 43), we did not observe meaningful changes in openness. The changes observed in the present study were marginally significant and of moderate effect size (p = 0.06: d = 0.5), which may have been due to dropout rate and decreased power during the 1-week assessment. In sum, the effects of psychedelic substances on neuroticism seem to be more robust and more frequently reported, compared to changes in other personality traits such as agreeableness or openness.
Lastly, the present study aimed to further explore hypothesis-driven correlational relationships between changes in mindfulness and neuroticism and changes in anxiety. Although there was an increase in mindfulness capacities following intake of psilocybin, there were no strong associations between changes in mindfulness capacities and anxiety ratings. In regards to neuroticism, in line with theoretical conceptualizations of neuroticism and trait anxiety as stable, personality-dependent dispositions, we found that sub-acute and 1-week reductions in trait anxiety were most strongly correlated with reductions in neuroticism. Namely, change scores in neuroticism and trait anxiety shared about 89% of the variance variability, pointing out a strong interdependency between the two variables. Although trait anxiety and neuroticism inherently share overlapping constructs, it is important to state that they are not identical (92, 93). Neuroticism via the BFI consists of facets much broader than the construct of trait anxiety via the STAI, including anxiety, angry hostility, depression, self-consciousness, impulsivity, and vulnerability. Future studies should assess what facets of neuroticism correlate with trait anxiety, and what facets overlap with trait anxiety.
Additionally, we also found that the strongest correlator of sub-acute and 1-week changes in state anxiety were ratings of ego dissolution, sharing about 32% of the variance. Specifically, the higher the rating of ego dissolution during the acute experience, the larger the decrease in state anxiety scores both 24 h and 1 week after the experience. A recent review of twenty studies assessing the clinical response to psychedelics in patients with a range of psychological disorders concluded that the main predictive factor of a response to a psychedelic is the intensity of the acute psychedelic experience (94). That said, it has yet to be systematically assessed whether such a “peak” experience is necessary for long-term outcomes (95), or whether the subjective experiences elicited by psychedelic substances are merely epiphenomena of the underlying neurobiological mechanisms, the latter which are conveying any beneficial effects. Additionally, it is possible that other psychological components play important roles in mediating long-term outcomes of psychedelic experience, for instance insight/breakthrough or catharsis, suggestibility, and reliving of trauma have been suggested as important factors determining the psychedelic experience (15, 88, 96–100). Therefore, we should remain cautious when developing and interpreting specific theoretical frameworks of psychedelics’ (psychological) mechanisms of action and focus future efforts on testing these frameworks in the context of experimental studies.
The objectives were tested using a naturalistic, observational design, with attendees of psilocybin ceremonies. Although, this sort of setting has high rates of ecological validity, as it closely resembles a typical environment associated with psychedelic usage (101–104), it also comes with a range of confounding variables, including lack of control over participant inclusion or substance administration The present study was conducted with a self-selected sample of self-determined healthy individuals. To have an indication of the amount of truffles individuals took, we asked for a sample that was analyzed afterward and we asked how much truffles participants consumed. This allows comparisons between findings of our study and that of controlled studies. Another point is that longitudinal studies traditionally come with high dropout rates (105, 106); our study was not different in that sense. The concern of such dropouts is that they could create problematic biases in the data, with for example only those individuals experiencing benefits from the experience being motivated to continue responding to the questions. A recent study investigating potential determinants of study attrition in web-based prospective studies on psychedelic use identified that baseline predictors of attrition (i.e., age, educational levels, and personality traits) were consistent with those reported in longitudinal studies in other scientific disciplines, suggesting their transdisciplinary relevance (80). Moreover, they did not find an association between attrition and psychedelic advocacy or negative drug experiences, advocating against the concerns about problematic biases in these and related data. Finally, the absence of a control group or placebo hampers the ability to draw hard conclusions as to pharmacological vs. extra-pharmacological effects, as it has been found that the retreat setting alone also produces changes in psychological outcomes (86). Future studies should be designed to further assess the contribution of pharmacological versus extra-pharmacological factors [see e.g., (107) for a thorough discussion and recommendations].
Conclusion
Taken together, the present study suggests persisting reductions in anxiety symptoms and trait neuroticism, and increases in mindfulness capacities, after ingestion of psilocybin in a supportive group setting. Given the important role of set and setting on the outcome of psychedelic experience (102, 104), future studies should systematically evaluate the contribution of these extra-pharmacological factors to the treatment outcome, in order to optimize therapeutic strategies. Additionally, naturalistic retreat studies such as this, as well as modern clinical trials (90), are beginning to demonstrate feasibility, safety, and efficacy of group sessions with psychedelics, across different disorders. As it is likely that psychedelic-assisted psychotherapy will be costly and time-consuming for both the patient and the practitioners, future studies exploring the feasibility of group therapy could potentially substantially lower treatment costs, resulting in a more financially accessible treatment option.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Review Committee of Psychology and Neuroscience, Maastricht University, Faculty of Psychology and Neuroscience, Maastricht, Netherlands. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NM, KK, and JR conceived of the presented idea. NM and MU collected the data. MK and NM conducted the statistical analysis. MK, NM, and KK prepared the first draft of the manuscript. All authors discussed the results and contributed to the final manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to acknowledge and thank Stefana Bosse and the Psychedelic Society United Kingdom for their collaboration and permission to collect data at their experience weekends. We would like to thank Hannes Kettner and Beatrice Da Rios for helping with data collection. We would like to thank all participants for their time and effort. We would also like to thank the reviewers, whose comments and questions improved the quality of the manuscript.
References
1. Sansone RA, Sansone LA. Psychiatric disorders: a global look at facts and figures. Psychiatry. (2010) 7:16–9.
2. Stein DJ, Scott KM, de Jonge P, Kessler RC. Epidemiology of anxiety disorders: from surveys to nosology and back. Dialogues Clin Neurosci. (2017) 19:127–36. doi: 10.31887/DCNS.2017.19.2/dstein
3. Kandola A, Vancampfort D, Herring M, Rebar A, Hallgren M, Firth J, et al. Moving to beat anxiety: epidemiology and therapeutic issues with physical activity for anxiety. Curr Psychiatry Rep. (2018) 20:63. doi: 10.1007/s11920-018-0923-x
4. Baldwin DS. Room for improvement in the pharmacological treatment of anxiety disorders. Curr Pharm Des. (2008) 14:3482–91. doi: 10.2174/138161208786848810
5. Otto MW, McHugh RK, Kantak KM. Combined pharmacotherapy and cognitive-behavioral therapy for anxiety disorders: medication effects, glucocorticoids, and attenuated treatment outcomes. Clin Psychol. (2010) 17:91–103. doi: 10.1111/j.1468-2850.2010.01198.x
6. Loerinc AG, Meuret AE, Twohig MP, Rosenfield D, Bluett EJ, Craske MG. Response rates for CBT for anxiety disorders: need for standardized criteria. Clin Psychol Rev. (2015) 42:72–82. doi: 10.1016/j.cpr.2015.08.004
7. Brown C, Schulberg HC, Madonia MJ, Shear MK, Houck PR. Treatment outcomes for primary care patients with major depression and lifetime anxiety disorders. Am J Psychiatry. (1996) 153:1293–300. doi: 10.1176/ajp.153.10.1293
8. Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. J Abnorm Psychol. (2001) 110:585–99. doi: 10.1037//0021-843x.110.4.585
9. Weston NM, Gibbs D, Bird CIV, Daniel A, Jelen LA, Knight G, et al. Historic psychedelic drug trials and the treatment of anxiety disorders. Depress Anxiety. (2020) 37:1261–79. doi: 10.1002/da.23065
10. Carhart-Harris RL, Kaelen M, Bolstridge M, Williams TM, Williams LT, Underwood R, et al. The paradoxical psychological effects of lysergic acid diethylamide (LSD). Psychol Med. (2016) 46:1379–90. doi: 10.1017/S0033291715002901
11. Grob CS, Danforth AL, Chopra GS, Hagerty M, McKay CR, Halberstadt AL, et al. Pilot study of psilocybin treatment for anxiety in patients with advanced-stage cancer. Arch Gen Psychiatry. (2011) 68:71–8. doi: 10.1001/archgenpsychiatry.2010.116
12. Osório F, de L, de L, Osório F, Sanches RF, Macedo LR, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression: a preliminary report. Braz J Psychiatry. (2015) 37:13–20. doi: 10.1590/1516-4446-2014-1496
13. Palhano-Fontes F, Barreto D, Onias H, Andrade KC, Novaes MM, Pessoa JA, et al. Rapid antidepressant effects of the psychedelic ayahuasca in treatment-resistant depression: a randomized placebo-controlled trial. Psychol Med. (2019) 49:655–63. doi: 10.1017/S0033291718001356
14. Sanches RF, de Lima Osório F, dos Santos RG, Macedo LRH, Maia-de-Oliveira JP, Wichert-Ana L, et al. Antidepressant effects of a single dose of ayahuasca in patients with recurrent depression. J Clin Psychopharmacol. (2016) 36:77–81. doi: 10.1097/jcp.0000000000000436
15. Gasser P, Holstein D, Michel Y, Doblin R, Yazar-Klosinski B, Passie T, et al. Safety and efficacy of lysergic acid diethylamide-assisted psychotherapy for anxiety associated with life-threatening diseases. J Nerv Ment Dis. (2014) 202:513–20. doi: 10.1097/NMD.0000000000000113
16. Griffiths RR, Johnson MW, Carducci MA, Umbricht A, Richards WA, Richards BD, et al. Psilocybin produces substantial and sustained decreases in depression and anxiety in patients with life-threatening cancer: a randomized double-blind trial. J Psychopharmacol. (2016) 30:1181–97. doi: 10.1177/0269881116675513
17. Ross S, Bossis A, Guss J, Agin-Liebes G, Malone T, Cohen B, et al. Rapid and sustained symptom reduction following psilocybin treatment for anxiety and depression in patients with life-threatening cancer: a randomized controlled trial. J Psychopharmacol. (2016) 30:1165–80. doi: 10.1177/0269881116675512
18. Agin-Liebes GI, Malone T, Yalch MM, Mennenga SE, Ponté KL, Guss J, et al. Long-term follow-up of psilocybin-assisted psychotherapy for psychiatric and existential distress in patients with life-threatening cancer. J Psychopharmacol. (2020) 34:155–66. doi: 10.1177/0269881119897615
19. Carhart-Harris RL, Bolstridge M, Day CMJ, Rucker J, Watts R, Erritzoe DE, et al. Psilocybin with psychological support for treatment-resistant depression: six-month follow-up. Psychopharmacology. (2018) 235:399–408. doi: 10.1007/s00213-017-4771-x
20. Carhart-Harris RL, Bolstridge M, Rucker J, Day CMJ, Erritzoe D, Kaelen M, et al. Psilocybin with psychological support for treatment-resistant depression: an open-label feasibility study. Lancet Psychiatry. (2016) 3:619–27. doi: 10.1016/s2215-0366(16)30065-7
21. Jiménez-Garrido DF, Gómez-Sousa M, Ona G, Dos Santos RG, Hallak JEC, Alcázar-Córcoles MÁ, et al. Effects of ayahuasca on mental health and quality of life in naïve users: a longitudinal and cross-sectional study combination. Sci Rep. (2020) 10:4075. doi: 10.1038/s41598-020-61169-x
22. Uthaug MV, Lancelotta R, van Oorsouw K, Kuypers KPC, Mason N, Rak J, et al. A single inhalation of vapor from dried toad secretion containing 5-methoxy-N,N-dimethyltryptamine (5-MeO-DMT) in a naturalistic setting is related to sustained enhancement of satisfaction with life, mindfulness-related capacities, and a decrement of psychopathological symptoms. Psychopharmacology. (2019) 236:2653–66. doi: 10.1007/s00213-019-05236-w
23. Uthaug MV, van Oorsouw K, Kuypers KPC, van Boxtel M, Broers NJ, Mason NL, et al. Sub-acute and long-term effects of ayahuasca on affect and cognitive thinking style and their association with ego dissolution. Psychopharmacology. (2018) 235:2979–89. doi: 10.1007/s00213-018-4988-3
24. Barrett FS, Doss MK, Sepeda ND, Pekar JJ, Griffiths RR. Emotions and brain function are altered up to one month after a single high dose of psilocybin. Sci Rep. (2020) 10:2214. doi: 10.1038/s41598-020-59282-y
25. Schmid Y, Liechti ME. Long-lasting subjective effects of LSD in normal subjects. Psychopharmacology. (2018) 235:535–45. doi: 10.1007/s00213-017-4733-3
26. Caspi A, Roberts BW, Shiner RL. Personality development: stability and change. Ann Rev Psychol. (2005) 56:453–84. doi: 10.1146/annurev.psych.55.090902.141913
27. Clark LA. Temperament as a unifying basis for personality and psychopathology. J Abnorm Psychol. (2005) 114:505–21. doi: 10.1037/0021-843X.114.4.505
28. Frokjaer VG, Vinberg M, Erritzoe D, Baaré W, Holst KK, Mortensen EL, et al. Familial risk for mood disorder and the personality risk factor, neuroticism, interact in their association with frontolimbic serotonin 2A receptor binding. Neuropsychopharmacology. (2010) 35:1129–37. doi: 10.1038/npp.2009.218
29. Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Ann Rev Clin Psychol. (2011) 7:269–95. doi: 10.1146/annurev-clinpsy-032210-104540
30. Krueger RF, Tackett JL. Personality and psychopathology: working toward the bigger picture. J Pers Disord. (2003) 17:109–28. doi: 10.1521/pedi.17.2.109.23986
31. Ormel J, Jeronimus BF, Kotov R, Riese H, Bos EH, Hankin B, et al. Neuroticism and common mental disorders: meaning and utility of a complex relationship. Clin Psychol Rev. (2013) 33:686–97. doi: 10.1016/j.cpr.2013.04.003
32. Zinbarg RE, Mineka S, Bobova L, Craske MG, Vrshek-Schallhorn S, Griffith JW, et al. Testing a hierarchical model of neuroticism and its cognitive facets: latent structure and prospective prediction of first onsets of anxiety and unipolar mood disorders during 3 years in late adolescence. Clin Psychol Sci. (2016) 4:805–24.
33. Roberts BW, Luo J, Briley DA, Chow PI, Su R, Hill PL. A systematic review of personality trait change through intervention. Psychol Bull. (2017) 143:117–41. doi: 10.1037/bul0000088
34. Roberts BW. Commentary: from kindling to conflagration: self-regulation and personality change. In: Schaie KW, Carstensen LL editors, Social Structures, Aging and Self Regulation in the Elderly. New York, NY: Springer Publishing Company (2006). p. 85–94.
35. Bouso JC, González D, Fondevila S, Cutchet M, Fernández X, Ribeiro Barbosa PC, et al. Personality, psychopathology, life attitudes and neuropsychological performance among ritual users of ayahuasca: a longitudinal study. PLoS One. (2012) 7:e42421. doi: 10.1371/journal.pone.0042421
36. Bouso JC, Palhano-Fontes F, Rodríguez-Fornells A, Ribeiro S, Sanches R, Crippa JAS, et al. Long-term use of psychedelic drugs is associated with differences in brain structure and personality in humans. Eur Neuropsychopharmacol. (2015) 25:483–92. doi: 10.1016/j.euroneuro.2015.01.008
37. Erritzoe D, Roseman L, Nour MM, MacLean K, Kaelen M, Nutt DJ, et al. Effects of psilocybin therapy on personality structure. Acta Psychiatr Scand. (2018) 138:368–78. doi: 10.1111/acps.12904
38. Johnstad PG. The psychedelic personality: personality structure and associations in a sample of psychedelics users. J Psychoactive Drugs. (2021) 53:97–103. doi: 10.1080/02791072.2020.1842569
39. Kiraga MK, Mason NL, Uthaug MV, van Oorsouw KIM, Toennes SW, Ramaekers JG, et al. Persisting effects of ayahuasca on empathy, creative thinking, decentering, personality, and well-being. Front Pharmacol. (2021) 12:2714. doi: 10.3389/fphar.2021.721537
40. Nour MM, Evans L, Carhart-Harris RL. Psychedelics, personality and political perspectives. J Psychoactive Drugs. (2017) 49:182–91. doi: 10.1080/02791072.2017.1312643
41. Weiss B, Nygart V, Pommerencke LM, Carhart-Harris R, Erritzoe D. Examining psychedelic-induced changes in social functioning and connectedness in a naturalistic online sample using the five-factor model of personality. Front Psychol. (2021) 12:749788. doi: 10.3389/fpsyg.2021.749788
42. Eleftheriou ME, Thomas E. Examining the potential synergistic effects between mindfulness training and psychedelic-assisted therapy. Front Psychiatry. (2021) 12:707057. doi: 10.3389/fpsyt.2021.707057
43. Madsen MK, Fisher PM, Stenbæk DS, Kristiansen S, Burmester D, Lehel S, et al. A single psilocybin dose is associated with long-term increased mindfulness, preceded by a proportional change in neocortical 5-HT2A receptor binding. Eur Neuropsychopharmacol. (2020) 33:71–80. doi: 10.1016/j.euroneuro.2020.02.001
44. Murphy-Beiner A, Soar K. Ayahuasca’s “afterglow”: improved mindfulness and cognitive flexibility in ayahuasca drinkers. Psychopharmacology. (2020) 237:1161–9. doi: 10.1007/s00213-019-05445-3
45. Payne JE, Chambers R, Liknaitzky P. Combining psychedelic and mindfulness interventions: synergies to inform clinical practice. ACS Pharmacol Transl Sci. (2021) 4:416–23. doi: 10.1021/acsptsci.1c00034
46. Uthaug MV, Lancelotta R, Szabo A, Davis AK, Riba J, Ramaekers JG. Prospective examination of synthetic 5-methoxy-N,N-dimethyltryptamine inhalation: effects on salivary IL-6, cortisol levels, affect, and non-judgment. Psychopharmacology. (2020) 237:773–85. doi: 10.1007/s00213-019-05414-w
47. Kabat-Zinn J. Wherever you Go, There you are: Mindfulness Meditation in Everyday Life. (2009). Available online at: https://play.google.com/store/books/details?id=cVCZAAAAQBAJ (accessed December 12, 2021).
48. Dar KA, Iqbal N. Worry and rumination in generalized anxiety disorder and obsessive compulsive disorder. J Psychol. (2015) 149:866–80. doi: 10.1080/00223980.2014.986430
49. Goldin PR, Gross JJ. Effects of mindfulness-based stress reduction (MBSR) on emotion regulation in social anxiety disorder. Emotion. (2010) 10:83–91. doi: 10.1037/a0018441
50. Ramel W, Ramel W, Goldin PR, Carmona PE, McQuaid JR. The effects of mindfulness meditation on cognitive processes and affect in patients with past depression. Cogn Ther Res. (2004) 28:433–55. doi: 10.1023/b:cotr.0000045557.15923.96
51. Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behav Res Ther. (2007) 45:2518–26. doi: 10.1016/j.brat.2007.04.011
52. Griffiths RR, Johnson MW, Richards WA, Richards BD, Jesse R, MacLean KA, et al. Psilocybin-occasioned mystical-type experience in combination with meditation and other spiritual practices produces enduring positive changes in psychological functioning and in trait measures of prosocial attitudes and behaviors. J Psychopharmacol. (2018) 32:49–69. doi: 10.1177/0269881117731279
53. MacLean KA, Johnson MW, Griffiths RR. Mystical experiences occasioned by the hallucinogen psilocybin lead to increases in the personality domain of openness. J Psychopharmacol. (2011) 25:1453–61. doi: 10.1177/0269881111420188
54. Roseman L, Nutt DJ, Carhart-Harris RL. Quality of acute psychedelic experience predicts therapeutic efficacy of psilocybin for treatment-resistant depression. Front Pharmacol. (2018) 8:974. doi: 10.3389/fphar.2017.00974
55. Nour MM, Carhart-Harris RL. Psychedelics and the science of self-experience. Br J Psychiatry. (2017) 210:177–9. doi: 10.1192/bjp.bp.116.194738
56. Bogenschutz MP, Forcehimes AA, Pommy JA, Wilcox CE, Barbosa PCR, Strassman RJ. Psilocybin-assisted treatment for alcohol dependence: a proof-of-concept study. J Psychopharmacol. (2015) 29:289–99. doi: 10.1177/0269881114565144
57. Griffiths RR, Johnson MW, Richards WA, Richards BD, McCann U, Jesse R. Psilocybin occasioned mystical-type experiences: immediate and persisting dose-related effects. Psychopharmacology. (2011) 218:649–65. doi: 10.1007/s00213-011-2358-5
58. Garcia-Romeu AR, Griffiths R, Johnson WM. Psilocybin-Occasioned mystical experiences in the treatment of tobacco addiction. Curr Drug Abuse Rev. (2014) 7:157–64. doi: 10.2174/1874473708666150107121331
59. Andrea H, Bültmann U, Beurskens AJHM, Swaen GMH, van Schayck CP, Kant IJ. Anxiety and depression in the working population using the HAD scale–psychometrics, prevalence and relationships with psychosocial work characteristics. Soc Psychiatry Psychiatr Epidemiol. (2004) 39:637–46. doi: 10.1007/s00127-004-0797-6
60. Fox E, Russo R, Bowles R, Dutton K. Do threatening stimuli draw or hold visual attention in subclinical anxiety? J Exp Psychol Gen. (2001) 130:681–700.
61. Ng J, Chan HY, Schlaghecken F. Dissociating effects of subclinical anxiety and depression on cognitive control. Adv Cogn Psychol. (2012) 8:38–49. doi: 10.2478/v10053-008-0100-6
62. Spira AP, Friedman L, Aulakh JS, Lee T, Sheikh JI, Yesavage JA. Subclinical anxiety symptoms, sleep, and daytime dysfunction in older adults with primary insomnia. J Geriatr Psychiatry Neurol. (2008) 21:149–53. doi: 10.1177/0891988707317120
63. Wetherell JL, Le Roux H, Gatz M. DSM-IV criteria for generalized anxiety disorder in older adults: distinguishing the worried from the well. Psychol Aging. (2003) 18:622–7. doi: 10.1037/0882-7974.18.3.622
64. Hasler F, Grimberg U, Benz MA, Huber T, Vollenweider FX. Acute psychological and physiological effects of psilocybin in healthy humans: a double-blind, placebo-controlled dose-effect study. Psychopharmacology. (2004) 172:145–56. doi: 10.1007/s00213-003-1640-6
65. Erowid. Mushroom Tea Preparation. (2015). Available online at: https://erowid.org/plants/mushrooms/mushrooms_prep2.shtml (accessed November 15, 2021).
66. Laussmann T, Meier-Giebing S. Forensic analysis of hallucinogenic mushrooms and khat (Catha edulisForsk) using cation-exchange liquid chromatography. Forensic Sci Int. (2010) 195:160–4. doi: 10.1016/j.forsciint.2009.12.013
67. Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (Form Y)(“Self-Evaluation Questionnaire”. Palo Alto, CA: Consulting Psychologists Press (1983).
68. Spielberger CD. State-Trait Anxiety Inventory: Bibliography. 2nd ed. Palo Alto, CA: Consulting Psychologists Press (1989).
69. Ercan I, Hafizoglu S, Ozkaya G, Kirli S, Yalcintas E. Examining cut-off values for the state-trait anxiety inventory/examinando los puntajes de corte para el inventario de ansiedad estado-rasgo. Rev Argentina Clín Psicol. (2015) 24:143–8.
70. Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. (2006) 13:27–45. doi: 10.1177/1073191105283504
71. John OP, Donahue EM, Kentle RL. The Big Five Inventory – Versions 4a and 54. Berkeley, CA: University of California (1991).
72. Benet-Martínez V, John OP. Los cinco grandes across cultures and ethnic groups: multitrait multimethod analyses of the big five in Spanish and English. J Pers Soc Psychol. (1998) 75:729–50. doi: 10.1037//0022-3514.75.3.729
73. John OP, Srivastava S. The big-five trait taxonomy: history, measurement, and theoretical perspectives. In: Pervin LA, John OP editors. Handbook of Personality: Theory and Research. (Vol. 2). Berkeley, CA: University of California Berkeley (1999).
74. Griffiths RR, Richards WA, McCann U, Jesse R. Psilocybin can occasion mystical-type experiences having substantial and sustained personal meaning and spiritual significance. Psychopharmacology. (2006) 187:268–83; discussion 284–92. doi: 10.1007/s00213-006-0457-5
75. Johnson MW, Garcia-Romeu A, Cosimano MP, Griffiths RR. Pilot study of the 5-HT2AR agonist psilocybin in the treatment of tobacco addiction. J Psychopharmacol. (2014) 28:983–92. doi: 10.1177/0269881114548296
76. Nour MM, Evans L, Nutt D, Carhart-Harris RL. Ego-dissolution and psychedelics: validation of the ego-dissolution inventory (EDI). Front Hum Neurosci. (2016) 10:269. doi: 10.3389/fnhum.2016.00269
77. Bienvenu OJ, Samuels JF, Costa PT, Reti IM, Eaton WW, Nestadt G. Anxiety and depressive disorders and the five-factor model of personality: a higher- and lower-order personality trait investigation in a community sample. Depress Anxiety. (2004) 20:92–7. doi: 10.1002/da.20026
78. Cuijpers P, van Straten A, Donker M. Personality traits of patients with mood and anxiety disorders. Psychiatry Res. (2005) 133:229–37. doi: 10.1016/j.psychres.2004.10.006
79. Sherry A, Henson RK. Conducting and interpreting canonical correlation analysis in personality research: a user-friendly primer. J Pers Assess. (2005) 84:37–48. doi: 10.1207/s15327752jpa8401_09
80. Hübner S, Haijen E, Kaelen M, Carhart-Harris RL, Kettner H. Turn on, tune in, and drop out: predictors of attrition in a prospective observational cohort study on psychedelic use. J Med Int Res. (2021) 23:e25973. doi: 10.2196/25973
81. Leary MR. Introduction to Behavioral Research Methods. (Vol. 6). London: Pearson Education Limited (2014).
82. Mason NL, Mischler E, Uthaug MV, Kuypers KPC. Sub-Acute effects of psilocybin on empathy, creative thinking, and subjective well-being. J Psychoactive Drugs. (2019) 51:123–34. doi: 10.1080/02791072.2019.1580804
83. Brown TA, Barlow DH. Comorbidity among anxiety and mood disorders: implications for treatment and DSM-IV. J Consult Clin Psychol. (1995) 63:408–41.
84. World Health Organization. Depression and Other Common Mental Disorders: Global Health Estimates. Rep. CC BY-NC-SA 3.0 IGO. Geneva: World Health Organization (2017).
85. Mascher E. Psycholytic therapy: statistics and indications. In: Brill H editor, Official Publication of the American College of Neuropsychopharmacology. New York, NY: Excerpta Medica (1967) p. 441–4.
86. Uthaug MV, Mason NL, Toennes SW, Reckweg JT, de Sousa Fernandes Perna EB, Kuypers KPC, et al. A placebo-controlled study of the effects of ayahuasca, set and setting on mental health of participants in ayahuasca group retreats. Psychopharmacology. (2021) 238:1899–910. doi: 10.1007/s00213-021-05817-8
87. Preller KH, Vollenweider FX. Modulation of social cognition via hallucinogens and “entactogens”. Front Psychiatry. (2019) 10:881. doi: 10.3389/fpsyt.2019.00881
88. Watts R, Day C, Krzanowski J, Nutt D, Carhart-Harris R. Patients’ accounts of increased “connectedness” and “acceptance” after psilocybin for treatment-resistant depression. J Humanist Psychol. (2017) 57:520–64. doi: 10.1177/0022167817709585
89. Trope A, Anderson BT, Hooker AR, Glick G, Stauffer C, Woolley JD. Psychedelic-Assisted Group Therapy: A Systematic Review. J Psychoact Drugs. (2019) 51:174–188. doi: 10.1080/02791072.2019.1593559
90. Anderson BT, Danforth A, Daroff PR, Stauffer C, Ekman E, Agin-Liebes G, et al. Psilocybin-assisted group therapy for demoralized older long-term AIDS survivor men: an open-label safety and feasibility pilot study. EClinicalMedicine. (2020) 27:100538. doi: 10.1016/j.eclinm.2020.100538
91. Frokjaer VG, Mortensen EL, Nielsen FA, Haugbol S, Pinborg LH, Adams KH, et al. Frontolimbic serotonin 2A receptor binding in healthy subjects is associated with personality risk factors for affective disorder. Biol Psychiatry. (2008) 63:569–76. doi: 10.1016/j.biopsych.2007.07.009
92. Hoppe JM, Frick A, Åhs F, Linnman C, Appel L, Jonasson M, et al. Association between amygdala neurokinin-1 receptor availability and anxiety-related personality traits. Transl Psychiatry. (2018) 8:168. doi: 10.1038/s41398-018-0163-1
93. Kotov R, Gamez W, Schmidt F, Watson D. Linking “big” personality traits to anxiety, depressive, and substance use disorders: a meta-analysis. Psychol Bull. (2010) 136:768–821. doi: 10.1037/a0020327
94. Romeo B, Hermand M, Pétillion A, Karila L, Benyamina A. Clinical and biological predictors of psychedelic response in the treatment of psychiatric and addictive disorders: a systematic review. J Psychiatr Res. (2021) 137:273–82. doi: 10.1016/j.jpsychires.2021.03.002
95. Olson DE. The subjective effects of psychedelics may not be necessary for their enduring therapeutic effects. ACS Pharmacol Transl Sci. (2021) 4:563–7. doi: 10.1021/acsptsci.0c00192
96. Belser AB, Agin-Liebes G, Swift TC, Terrana S, Devenot N, Friedman HL, et al. Patient experiences of psilocybin-assisted psychotherapy: an interpretative phenomenological analysis. J Humanist Psychol. (2017) 57:354–88. doi: 10.1177/0022167817706884
97. Eisner BG, Cohen S. Psychotherapy with lysergic acid diethylamide. J Nerv Ment Dis. (1958) 127:528–39. doi: 10.1097/00005053-195812000-00006
98. Frederking W. Intoxicant drugs (mescaline and lysergic acid diethylamide) in psychotherapy. J Nerv Ment Dis. (1955) 121:262–6. doi: 10.1097/00005053-195503000-00010
99. Richards WA. Mystical and archetypal experiences of terminal patients in DPT-assisted psychotherapy. J Relig Health. (1978) 17:117–26. doi: 10.1007/BF01532413
100. Russ SL, Elliott MS. Antecedents of mystical experience and dread in intensive meditation. Psychol Conscious Theor Res Pract. (2017) 4:38–53.
101. Frecska E, Bokor P, Winkelman M. The therapeutic potentials of ayahuasca: possible effects against various diseases of civilization. Front Pharmacol. (2016) 7:35. doi: 10.3389/fphar.2016.00035
102. Hartogsohn I. Set and setting, psychedelics and the placebo response: an extra-pharmacological perspective on psychopharmacology. J Psychopharmacol. (2016) 30:1259–67. doi: 10.1177/0269881116677852
103. Lawn W, Hallak JE, Crippa JA, Dos Santos R, Porffy L, Barratt MJ, et al. Well-being, problematic alcohol consumption and acute subjective drug effects in past-year ayahuasca users: a large, international, self-selecting online survey. Sci Rep. (2017) 7:15201. doi: 10.1038/s41598-017-14700-6
104. Sapoznikow A, Walsh Z, Tupper KW, Erowid E, Erowid F. The influence of context on ayahuasca experiences: an analysis of experience reports. J Psychedelic Stud. (2019) 3:288–94.
105. Chatfield MD, Brayne CE, Matthews FE. A systematic literature review of attrition between waves in longitudinal studies in the elderly shows a consistent pattern of dropout between differing studies. J Clin Epidemiol. (2005) 58:13–9. doi: 10.1016/j.jclinepi.2004.05.006
106. Young AF, Powers JR, Bell SL. Attrition in longitudinal studies: who do you lose? Aust N Z J Public Health. (2006) 30:353–61. doi: 10.1111/j.1467-842x.2006.tb00849.x
Keywords: psilocybin, anxiety, mindfulness, personality, neuroticism
Citation: Kiraga MK, Kuypers KPC, Uthaug MV, Ramaekers JG and Mason NL (2022) Decreases in State and Trait Anxiety Post-psilocybin: A Naturalistic, Observational Study Among Retreat Attendees. Front. Psychiatry 13:883869. doi: 10.3389/fpsyt.2022.883869
Received: 25 February 2022; Accepted: 01 June 2022;
Published: 07 July 2022.
Edited by:
Felix Mayer, Florida Atlantic University, United StatesReviewed by:
Nicky Mehtani, University of California, San Francisco, United StatesChristopher Nicholas, University of Wisconsin-Madison, United States
Copyright © 2022 Kiraga, Kuypers, Uthaug, Ramaekers and Mason. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Natasha Leigh Mason, bmF0YXNoYS5tYXNvbkBtYWFzdHJpY2h0dW5pdmVyc2l0eS5ubA==
 Maggie Kamila Kiraga
Maggie Kamila Kiraga Kim P. C. Kuypers
Kim P. C. Kuypers Malin Vedoy Uthaug
Malin Vedoy Uthaug Johannes G. Ramaekers
Johannes G. Ramaekers Natasha Leigh Mason
Natasha Leigh Mason