- 1Division of Biology and Public Health, Mokwon University, Daejeon, South Korea
- 2Seoul Health Foundation, Seoul, South Korea
- 3College of Korean Medicine, Sangji University, Wonju, South Korea
- 4College of Nursing, Kyung Hee University, Seoul, South Korea
Background: Amid the COVID-19 pandemic, quarantine measures are key to containing the spread of the virus. Millions of people have been required to quarantine throughout the pandemic; the quarantine itself is considered detrimental to mental health conditions.
Objective: This study aims to investigate the factors associated with depression and anxiety among quarantined people in Seoul, South Korea.
Methods: An online cross-sectional survey was administered from October to November 2020 involving people who were living in Seoul, aged 19 years or above, under a 2-week mandatory quarantine. Their mental health status was measured using the Patient Health Questionnares-9 (PHQ-9) and the General Anxiety Disorder-7 (GAD-7).
Results: Overall, 1,135 respondents were finally included, resulting in a 22.0% response rate. After controlling for potential confounders, variables, such as the “second half of quarantine period” (OR = 1.78 95% CI: 1.10–2.88), “female” (OR = 1.91 95% CI: 1.16–3.16), and “having pre-existing depression” (OR = 8.03 95% CI: 2.96–21.78) were significantly associated with depression while being quarantined. Those with correct knowledge about the rationale behind for the quarantine (OR = 0.39 95% CI: 0.21–0.72), an understanding of quarantine rules (OR = 0.68 95%CI: 0.52–0.91), and those who felt supported by others (OR = 0.74 95% CI: 0.55–0.99) were less likely to develop depression while quarantining. Similarly, anxiety was significantly associated with the second week (OR = 4.18 95% CI: 1.44–12.09), those with an unstable job status (OR = 3.95 95% CI: 1.60–9.79), perceived support (OR = 0.66, 95% CI: 0.45–0.96), and the fear of being infected (OR = 7.22 95% CI: 1.04–49.95).
Conclusions: This study highlights the need to develop precautionary measures to prevent depression and anxiety among people undergoing COVID-19 quarantine. In particular, individuals with depression prior to quarantine should be carefully monitored during the quarantine. Further studies with larger populations are needed.
Introduction
Owing to the global efforts to overcome the SARS-CoV-2 (COVID-19), widespread vaccinations have finally become a reality (1, 2). Nevertheless, the world has been battling this novel virus since the first case was reported from Wuhan, China in late 2019.
As the pandemic progressed, strategies to have targeted means of identifying cases, minimizing the spread of the virus, and mitigating its clinical manifestations among those already infected (3, 4). Given that COVID-19 is droplet borne, restricting the spread of the virus is key to controlling the pandemic's longevity. Hence, a quarantine strategy-identifying cases through timely but accurate testing so as to determining who to quarantine, and in which way—is vital to containing this virus. Accordingly, more than a billion people across more than 50 countries and territories were asked to remain confined to their homes (5). A growing number of studies demonstrated that health outcomes, notably, quality of life and psychological burden among quarantined people have significantly worsened (6–15). Thus, it is necessary to explore the factors contributing to poor health outcomes during quarantine so as to identify vulnerable groups that may require preemptive interventions. Previous research documented findings stating that sociodemographic features, such as age, gender, education, marital status, prolonged one's quarantine period, and pre-existing morbidities were associated with poor mental health conditions during the quarantine period (7–15).
Known for its successful control over this new virus (16–18), South Korea, armed with knowledge gained from the Middle East Respiratory Syndrome (MERS) epidemic in 2015 (19), has enforced a 14-day mandatory quarantine for inbound travelers and anyone who comes into contact with confirmed cases. This has been achieved via meticulous contact tracing and a widespread and aggressive testing policy in place since the early stages of the outbreak. According to the most recent data (20), South Korea's case fatality rate of COVID-19 was 1.78%, with 1,316 deaths and 73,918 cases (as of January 20, 2021), and the total number of tested people was 5,043,988, approximately 9.8% of the total population. Additionally, the total number of quarantined individuals reached 820,223 (as of November 17, 2020) (21).
However, factors associated with mental disorders among people under mandatory quarantine have not been sufficiently explored in the Korean context. Therefore, this study investigates factors associated with mental health disorders (depression and anxiety) among individuals undergoing COVID-19 quarantine; to the best of our knowledge, this is the first study on this topic pertaining to the context of South Korea.
Methods
Subjects
The Seoul COVID-19 Study (SCS) is a joint project initiated by the Seoul Metropolitan Government and the Seoul Health Foundation. It aims to investigate the performances of the Seoul government's countermeasures against COVID-19. The SCS focuses on people who used the screening posts for COVID-19 testing, the asymptomatic cases admitted in the residential centers for surveillance, and quarantined people who tested negative. The SCS for quarantine (SCS-Q) has been conducted from October to November 2020 involving those who live in Seoul, covering those above the age of 19 who were under the 2-week mandatory quarantine at the time of the study.
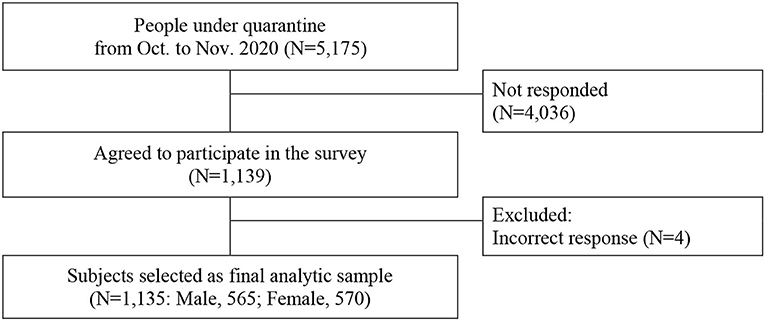
Considering the legal imposition of the no-contact rule with currently quarantined people, an online cross-sectional survey was designed. The targeted respondents were provided with the information regarding this study via text messages containing the URL of the survey questionnaires, and they voluntarily participated in the current study's cross-sectional online survey. A total of 5,175 people under quarantine were asked to participate. Responding to the survey was based on the participants' consent. Of those asked to participate, 1,139 (22.0% response rate) out of them agreed and filled in the questionnaires. Four individuals' answers were excluded due to incorrect response about quarantined days. Finally, 1,135 respondents were included in this study (Figure 1). Participation was consensual.
Outcomes
Depressive Symptoms
Depressive symptoms among quarantined people were evaluated using the Patient Health Questionnaires-9 (PHQ-9). The PHQ-9 is a validated measure of depressive symptoms and widely used in primary care and research settings. It contains nine items evaluating symptomatology of depression during the previous 2 weeks, including lack of interest, feeling depressed, sleep-related troubles, feeling tired, appetite change, feeling guilty or indulging in self-blame, concentration issues, feeling restless/slowed down, and suicidal ideations (22). The response options for each question were “never,” “several days,” “more than half of the days,” and “almost every day,” scored from 0 to 3 in order, indicating the perceived frequency of depressive symptoms (over the 2 weeks leading up to the questionnaire). The total score ranges from 0 to 27. The higher the score, the more severe the depressive symptoms (22). Prior literature has suggested using a cut-off of 10 to detect major depressive disorder (with a sensitivity 0.85 and a specificity 0.89) (23). Previous research documented the reliability and validity of the Korean translated version of PHQ-9 (24). In this study, we set “during the quarantine” as the timeframe of the PHQ-9 instead of “during the previous 2 weeks.” In this study, the Cronbach's alpha was found to be 0.89.
Anxiety Symptoms
The Generalized Anxiety Disorder-7(GAD-7), a widely used instrument, was employed to assess anxiety disorders. It is a seven-item questionnaire regarding the symptomatology of anxiety over the past 2 weeks (leading up to the questionnaire). It includes questions regarding feeling anxious/nervous, uncontrollable worrying, trouble relaxing, feeling annoyed/irritable, and feeling afraid (25). Response options per item indicate the perceived frequency of the anxiety symptom specified for each concern in the 2 weeks leading up to the questionnaire; these are labeled as “never (0),” “several days (1),” “more than half of the days (2),” and “almost every day (3),” with a total score ranging from 0 to 21 (25). Previous studies have reported that GAD-7 as an appropriate assessment tool for detecting generalized anxiety disorder (at 89% sensitivity and 82% specificity when using a cut-off value of 10 or above) when compared to a structured psychiatric interview (26). The reliability and validity of the Korean translated version of the GAD-7 has been previously reported (27). We set “during the quarantine” as the timeframe for the GAD-7 instead of “over the past 2 weeks.” In this study, the Cronbach's alpha was found to be 0.93.
Health-Related Quality of Life
A widely used generic instrument of health-related quality of life (HRQoL), the EuroQol-5Dimensions (EQ-5D) (28), was employed to assess HRQoL among the quarantined. The EQ-5D comprises five questions concerning mobility, self-care, usual activities, pain or discomfort, and psychological status. The EQ-5D scores ranging from 0 to 1, indicating death to perfect health, were calculated based on the Korean Tariff (29, 30).
Covariates
Sociodemographic characteristics of the respondents were collected. Additionally, we drew information regarding their health status before the quarantine by enquiring about any pre-existing chronic diseases including hypertension, diabetes and depression, and asking them to self-rate their health status.
Furthermore, we included variables related to health administration for quarantine. First, it was hypothesized that it is vital for the presence of trust in health authorities—who have taken countermeasures against COVID-19 to adopt sound quarantine, and to correctly understand why people should be confined at home for 2 weeks and under what conditions. Thus, “trust in health authorities,” “reason for being quarantined (e.g., inbound travelers and contacts with a confirmed case),” and “knowledge about the rationale for quarantine (e.g., to protect myself or to protect others)” were assessed on a five-point Likert scale.
For an effective 14-day mandatory quarantine, an understanding of the quarantine rules, the perceived support received during quarantine, and the satisfaction with the essential supplies provided free of charge by local offices were asked on a five-point Likert scale.
Additionally, questions about “quarantine days elapsed at the time of survey” and “concerns, such as fear of infection, financial crisis, and the risk of unemployment” were asked. In particular, number of days of quarantine elapsed at the time of survey was divided into two groups; first week (Day1–Day7) and second week (Day8–Day14).
Statistical Analysis
Categorical variables were expressed as frequencies and percentages, and continuous variables via their means and standard deviations (SDs). Chi-square test for categorical variables and the Student's t-test for means were performed. Mann-Whitney median test was used for the skewed distribution. Fisher's exact test for categorical variables was used when appropriate.
To identify factors contributing to health outcomes during quarantine, multivariable regression models were applied by considering the distribution and attributes of the outcome variables. For example, a standard logistic regression was employed for the dichotomous outcome variables such as depression and anxiety. However, as the EQ-5D scores range from 0 to 1 with a left-skewed distribution, a beta logit regression was used after rescaling the EQ-5D scores to avoid bounded values (31). All statistical analyses were performed using the SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
Basic Characteristics of Study Population
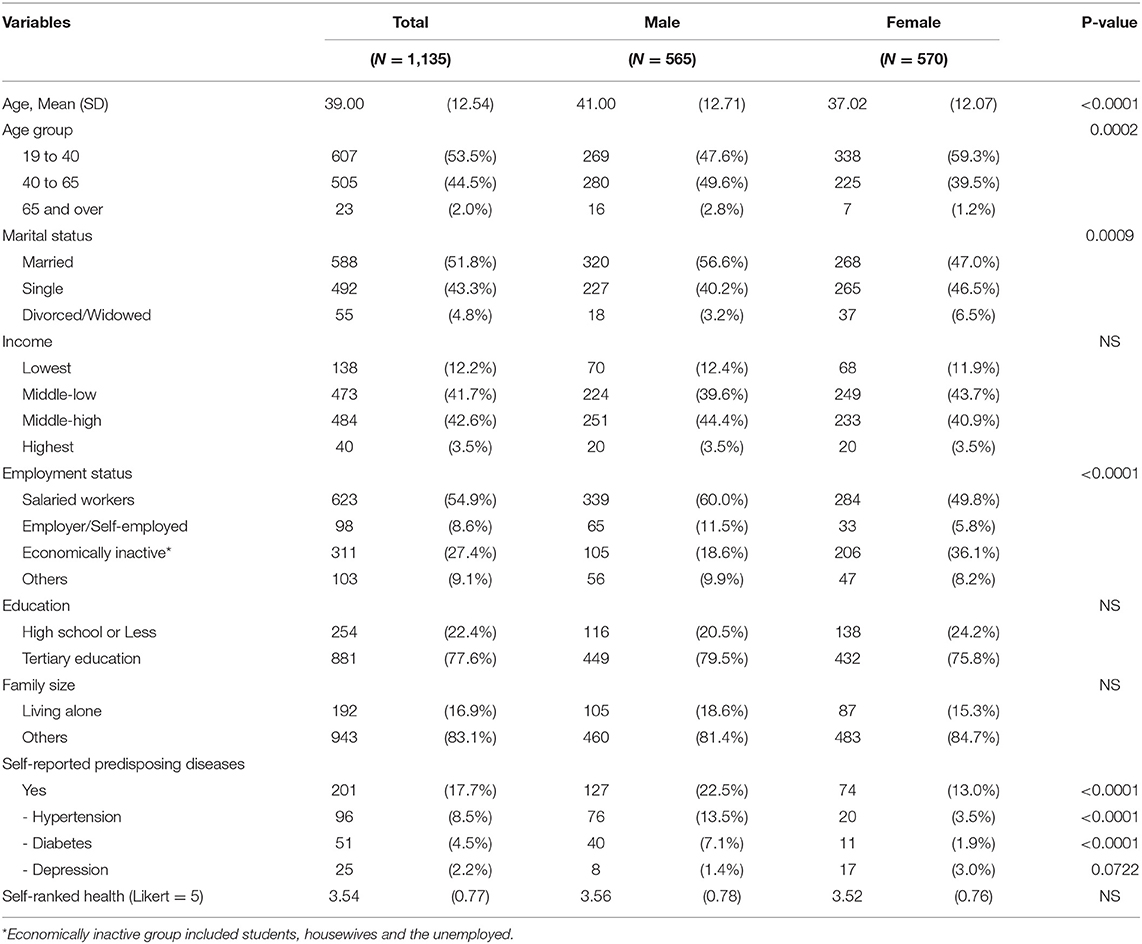
Table 1 shows the basic characteristics of the respondents. The average age of respondents was 39.00 (SD 12.54), which is relatively younger than the general population, with a significant difference between male and female (p < 0.0001). Most respondents were salaried workers (males 60.0% vs. females 49.8%). However, women constituted a relatively bigger proportion of the economically inactive group, which includes housewives, students, and the unemployed (women 36.1% vs. men 18.6%). Men were more likely to have pre-existing diseases, such as hypertension and diabetes than women (p < 0.0001). Self-reported pre-existing depression was more prevalent in women than in men (3.0% vs. 1.4%) at the 10% of significance level (p = 0.0722).
Quarantining
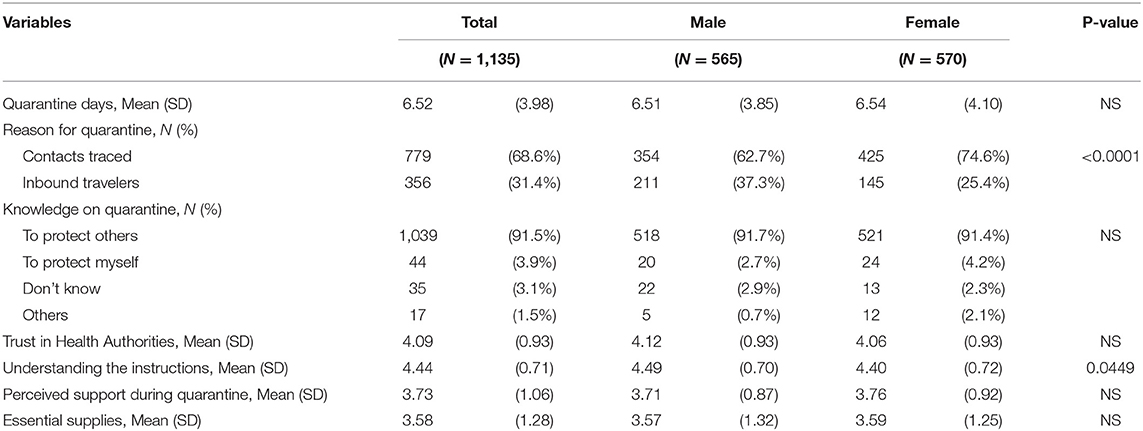
Table 2 presents the general information regarding quarantining as determined via a five-point Likert scale; these items include quarantine days at the time of survey, quarantine-related knowledge and understanding, social support, essential supplies provided by district offices, and trust in health authorities among the respondents under quarantine. The mean quarantine period at the time of survey response was 6.52 (SD 3.98) days; 68.6% of the respondents were quarantined owing to the contact with confirmed cases (men 62.7% vs. women 74.6%, p < 0.0001); the remaining participants were inbound travelers. Most quarantined people correctly understood that quarantine is necessary to protect others (men 91.7% vs. women 91.4%) and showed a high degree of confidence in the health authorities (4.09 SD 0.93 out of 5.0) who have been planning and implementing countermeasures (including quarantine) against the pandemic (men 4.12 SD 0.93 vs. women 4.06 SD 0.93). The difference in understanding of the quarantine instructions was marginally significant between men and women (4.49 [SD 0.70] vs. 4.40 [SD 0.72], respectively, p = 0.045); the overall score was high at 4.44 (SD 0.71). Perceived support during quarantine scored 3.73(SD 1.06) with no significant difference in men (3.71 SD 0.87) and women (3.76 SD 0.92). The respondents were mostly satisfied with the quarantine supplies being provided by the district public health centers (3.58 SD 1.28).
Outcomes
The differences in depression and anxiety as per the quarantine period was divided into the first week (Day1–Day7) and the second week (Day8–Day14), as depicted in Figure 2. Depression and anxiety increased significantly in the second period. Particularly, depression increased from 6.54 to 10.75% (p = 0.014), whereas anxiety increased from 3.69 to 6.49% (p = 0.040).
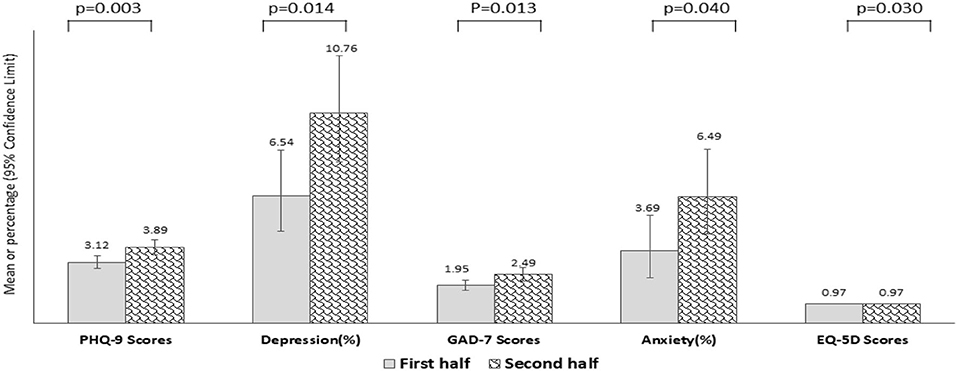
Figure 2. Depression, Anxiety, and Health-related Quality of life by quarantine period (First vs. Second week during the quarantine).
Factors Associated With Health Outcomes
Table 3 shows the results of multivariable regression analyses used to examine the factors associated with each outcome of this study.
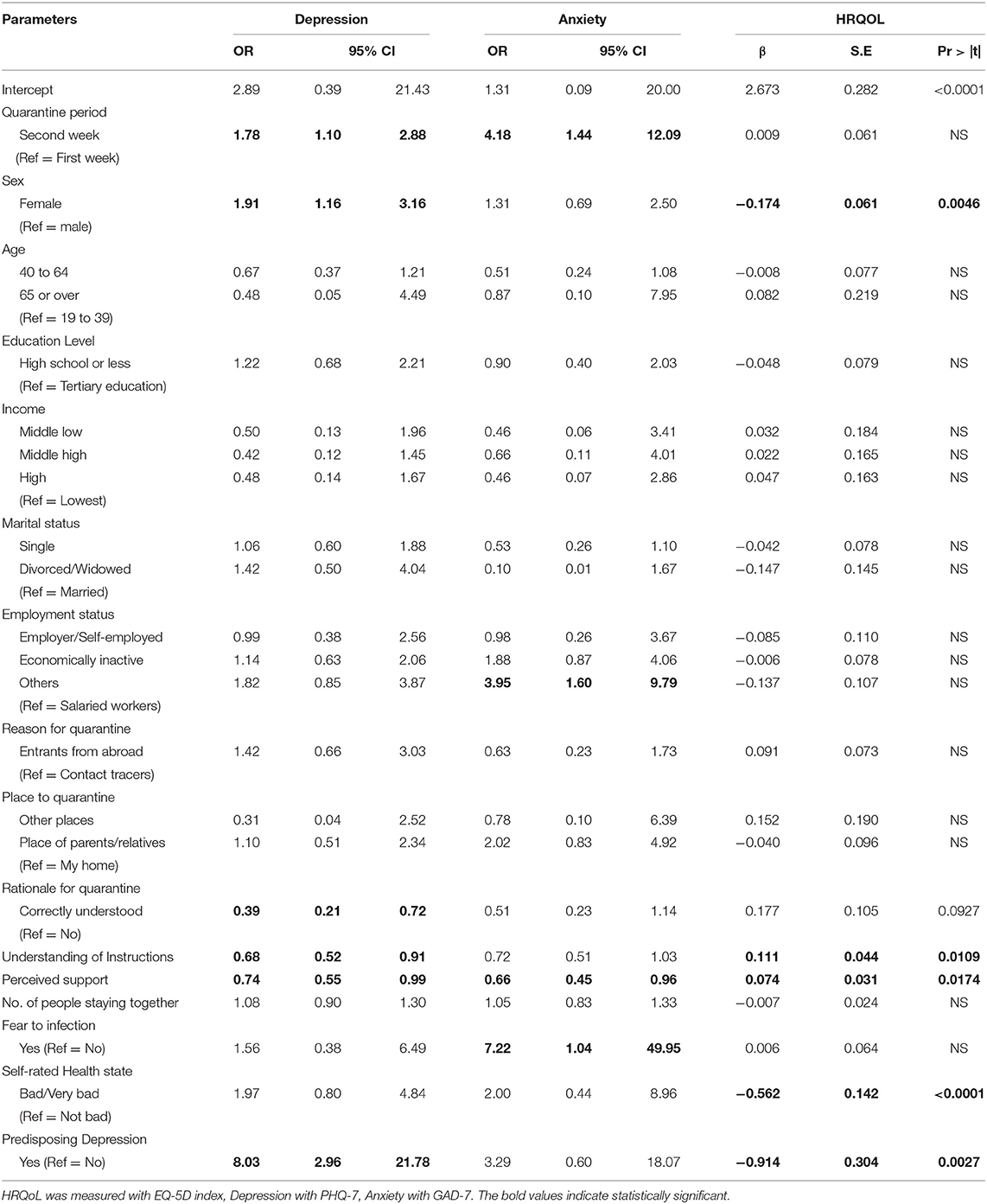
Table 3. Results of the multivariable regression analyses investigating factors associated with depression, anxiety, and HRQoL.
Depression
The logistic analysis showed that variables, such as quarantine period, sex, rationale for quarantine, the understanding of quarantine rules, perceived social support, and predisposing depression were all significantly associated with depression during the quarantine. Notably, the likelihood of suffering from depression in the second half of the quarantine period was 1.78 times (95% CI: 1.10–2.88) higher than that in the first half. As expected, women were more likely to suffer depression during quarantine than men (OR = 1.91 95% CI: 1.16–3.16), and those who already suffered depression as a predisposing health condition also displayed a higher likelihood to report depression during quarantine (OR = 8.03 95% CI: 2.96–21.78). However, people who were correctly aware of the rationale for quarantine (OR = 0.39 95% CI: 0.21–0.72) such as the need to protect others, those who understood the quarantine instructions well (OR = 0.68 95% CI: 0.52–0.91), and those who felt supported by others during self-quarantine (OR = 0.74 95% CI: 0.55–0.99) were all less likely to suffer from depression during quarantine.
Anxiety
Anxiety was also significantly associated with the quarantine period, employment status, perceived support, and fear to infection. The second half of the 14-day quarantine period increased the likelihood of experiencing anxiety by a factor of 4.18 (95% CI: 1.44–12.09) when compared to the first half of the quarantine period. Those who reported their employment status as “others” were 3.95 times (95% CI: 1.60–9.79) more likely to develop anxiety than wage workers. Presumably, “others” implied they were, job-wise, in transition due to the pandemic. For instance, temporary workers who were expected to quit their jobs or were uncertain about their employment status. On the other hand, perceived support from others significantly reduced the likelihood of anxiety during quarantine (OR = 0.66, 95% CI: 0.45–0.96). Unlike depression, fear of further infection was the most critical factor in the manifestation of anxiety among quarantined individuals. People with a fear of being infected with COVID-19 tended to develop anxiety 7.22 times more than those who did not (95% CI: 1.04–49.95).
HRQoL
A beta regression revealed no significant difference in HRQoL in the two halves of the quarantine period. Women had, on an average, 16.0% lower EQ-5D scores than men [exp (−0.174) = 0.84, p = 0.005]. A one-unit increase in the level of understanding of the quarantine rules significantly increased HRQoL by 11.7% (p = 0.0109). Moreover, consistent with the results of depression and anxiety, a one-unit increase level in perceived support from others during quarantine was associated with 7.7% higher EQ-5D scores (p = 0.0174). For those who considered themselves to have “bad” or “very bad” health conditions, the HRQoL scores reduced by 43.0% during quarantine when compared to others (moderate/good/very good) (p < 0.0001). Similar to depression, people with predisposing depression tended to experience a 59.9% decrease in EQ-5D scores than those without predisposing depression (p = 0.0027).
Discussion
This online study is, to the best of our knowledge, the first attempt to investigate the significant factors contributing to depression, anxiety, and HRQoL among quarantined individuals living in Seoul, South Korea (N = 1,135) during the COVID-19 pandemic. According to our findings, factors including quarantine period, perceived social support, and knowledge about quarantine (such as the rationale for the quarantine and the quarantine rules) critically mattered for depression, anxiety, and quality of life of individuals under quarantine during the COVID-19 pandemic.
First, our study reconfirmed that the longer the quarantine period, the higher the likelihood of experiencing depression and anxiety. During the second half of the quarantine period, the likelihoods of depression and anxiety were 1.78 and 4.18 times higher than in the first half, respectively. This is consistent to findings outlined in previous studies (6, 8, 9, 32). Brooks et al. (6) identified the duration of quarantine as one of the stressors for poor mental health, and Hawryluck et al. (32) showed that more than 10 days of quarantine was highly associated with post-traumatic stress symptoms compared with those who underwent <10 days of quarantine. As a longer exposure to stressful situations can adversely affect one's mental health, long-term isolation can negatively affect mental health such as increased levels of depression and anxiety.
We also found that perceived support during quarantine was significantly associated with reduced incidence of depression and anxiety, as well as improved HRQoL. It is a well-known fact that social support is beneficial for mental and physical health (33–35). Although social support in this study was measured by a single-item questionnaire regarding the perceived levels of support by others during the quarantine, the findings comply to results from previous studies. However, our study is the first to reveal the significant association of social support with mental disorders and one's quality of life as experienced throughout quarantine amidst the COVID-19 pandemic.
Furthermore, it is noteworthy that a correct understanding behind the rationale for the need to quarantine, along with the related rules thereof, was one of the significant factors for successfully enduring self-quarantine without experiencing depression or with better quality of life overall. Brooks et al. (6) suggested that ensuring that the quarantined individuals have both a good understanding of the disease and the reason for quarantine by providing sufficient information should be prioritized because inadequate information acted as a stressor for those who had been quarantined. Reynolds et al. (36) have also suggested that the provision of a clear rationale to quarantined individuals, an improved preparation for the quarantine, or education thereof should be implemented to limit the psychological impact of the event, based on the experiences of the Severe Acute Respiratory Syndrome (SARS) outbreak.
Beyond these findings, there have been previous studies indicating that pre-existing mental health conditions are associated with increased risks of worsening mental health (9, 37, 38); this finding has been corroborated in our study. Even during the quarantine, those who have already suffered from depression were 8.03 times more likely to have depression and tended to have 59.9% reduced quality of life throughout quarantine. Thus, such cases must be specially cared for.
Furthermore, health authorities should pay attention to high-risk groups (e.g., people with pre-existing depression, limited social support, or women) and develop precautionary measures to prevent mental health disorders during quarantine. Education/communication with quarantined individuals to provide appropriate knowledge on quarantine and epidemiological information on the disease can help them become less stressed.
Studies on HRQoL during the COVID-19 quarantine have been inadequately addressed (15). Further studies are required regarding the health utility or disutility among those who are quarantined. We first investigated the factors influencing the EQ-5D scores of quarantined people in South Korea. However, research based on a nationwide sample is needed.
Additionally, our findings demonstrated that anxiety, but not depression or quality of life, was strongly associated with the fear of further infection and occupational stability. Self-rated health status only showed a significant association with HRQoL.
Limitations
This study has some limitations that are important to note. First is the inherent age-based selection bias because the survey was online. Thus, older adults who are not comfortable with the use of the internet could easily be omitted. Additionally, people living in Seoul were the primary participants of this study. Hence, our findings are hardly generalizable to the entire population of South Korea. Second, the response rate was only 22.0% in our study. Although it is known that the typical downside of online survey is lower response rate (39), we conducted the online survey in consideration of the quarantining conditions of the study subjects. A variety of strategies including enticements in the form of incentives to complete surveys is recommended to improve the response rate of the online survey (39). However, we didn't provide any form of incentives to increase the response rate in this study. Third, one of our major findings was that predisposing depression was 8.03 times more likely to develop depression during COVID 19 quarantine. However, only 25 out of 1,135 (2.2%) reported having suffered from depression prior to quarantine, which may incorporate sampling error. Further studies with larger populations are needed. Lastly, we had to slightly modify the timeframes of the validated measures of depression (PHQ-9) and anxiety (GAD-7) to suit the limited setting of the quarantine.
Recommendations
With the prolonged combat against COVID-19, healthy quarantine is required. Particularly, high-risk groups (e.g., people with pre-existing depression, limited social support, or women) should be provided with special attention and undertake precautionary prevention measures. Various measures should be taken to actively support the quarantined people at the community level, as led by the district office. Furthermore, a clear explanation of the quarantine guidelines seems to be critical for those who are quarantined. Since the degree of understanding of the guidelines and the purpose of quarantine proved significant in improving the quality of life and preventing depressive symptoms, it is important to educate and communicate with people in quarantine. As it was found that longer periods of quarantine were associated with increased incidence of depression and anxiety, precautionary measures should be developed in accordance with the quarantine period and appropriately implemented to prevent depression and anxiety.
Conclusions
This study highlights the need to develop precautionary measures to prevent depression and anxiety among people undergoing COVID-19 quarantine. In particular, individuals with depression prior to quarantine should be carefully monitored during the quarantine. Further studies with larger populations are needed.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The Institutional Review board of Seoul Metropolitan City (IRB No. 2020-10-0001) approved this study. All participants provided online informed consent before beginning the survey. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
H-YK conceived the study. H-YK, YK, and S-YL established the consortium between Seoul Health Foundation and the affiliated districts of the Seoul Metropolitan Government. H-YK and S-YL performed the analyses. H-YK and YK drafted the manuscript. All authors contributed to finalizing the manuscript.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's Note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Acknowledgments
We would like to express our gratitude to workers and volunteers on the frontline during the COVID-19 pandemic for their sacrifice and professionalism. We also appreciate the individuals who were quarantined for taking part in this study. We thank the persons in charge of quarantine management in each district center for providing information to those in quarantine, thereby enabling us to administer the survey.
Abbreviations
COVID-19, SARS-CoV-2 virus diseases 2019; PHQ-9, Patient Health Questionnaires-9; GAD-7, Generalized Anxiety Disorders-7; HRQoL, Health-related Quality of Life; EQ-5D, Euroqol-5 Dimensions.
References
1. Bingham K. The UK Government's Vaccine Taskforce: strategy for protecting the UK and the world. Lancet. (2021) 397:68–70. doi: 10.1016/S0140-6736(20)32175-9
2. Hughes MT, Kahn J, Kachalia A. Who goes first? Government leaders and prioritization of SARS-CoV-2 vaccines. N Engl J Med. (2021) 384:e15. doi: 10.1056/NEJMpv2036128
3. World Health Organization (WHO). Considerations for Quarantine of Individuals in the Context of Containment for Coronavirus Disease (COVID-19): Interim Guidance, 19 March 2020. World Health Organization (2020). Available online at: https://apps.who.int/iris/handle/10665/331497 (accessed December 10, 2020).
4. World Health Organization (WHO) Regional Office for Europe. Strengthening the Health System Response to COVID-19: Technical Guidance #1: Maintaining the Delivery of Essential Health Care Services While Mobilizing the Health Workforce for the COVID-19 Response, 18 April 2020. World Health Organization. Regional Office for Europe (2020). Available online at: https://apps.who.int/iris/handle/10665/332559 (accessed December 10, 2020).
5. Agence France Press (AFP). A World Shut in: More Than a Billion People Stay Home for Coronavirus Business Standard. (2020). Available online at: https://www.business-standard.com/article/pti-stories/more-than-1-bn-people-worldwide-told-to-stay-home-over-virus-120032300839_1.html (accessed March 23, 2020).
6. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
7. Fernandez RS, Crivelli L, Guimet NM, Allegric RF, Pedreiraa ME. Psychological distress associated with COVID-19 quarantine: latent profile analysis, outcome prediction and mediation analysis. J Affect Disord. (2020) 277:75–84. doi: 10.1016/j.jad.2020.07.133
8. Pandey D, Bansal S, Goyal S, Garg A, Sethi N, Pothiyill DI, et al. Psychological impact of mass quarantine on population during pandemics-The COVID-19 Lock-Down (COLD) study. PLoS ONE. (2020) 15:e0240501. doi: 10.1371/journal.pone.0240501
9. Daly Z, Slemon A, Richardson CG, Salway T, McAuliffe C, Gadermann AM, et al. Associations between periods of COVID-19 quarantine and mental health in Canada. Psychiatry Res. (2021) 295:113631. doi: 10.1016/j.psychres.2020.113631
10. Benke C, Autenrieth LK, Asselmann E, Pane-Farre CA. Lockdown, quarantine measures, and social distancing: associations with depression, anxiety and distress at the beginning of the COVID-19 pandemic among adults from Germany. Psychiatry Res. (2020) 293:113462. doi: 10.1016/j.psychres.2020.113462
11. Bartoszek A, Walkowiak D, Bartoszek A, Kardas G. Mental Well-Being (depression, loneliness, insomnia, daily life fatigue) during covid-19 related home-confinement-a study from Poland. Int J Environ Res Public Health. (2020) 17:7417. doi: 10.3390/ijerph17207417
12. Burke T, Berry A, Taylor LK, Stafford O, Murphy E, Shevlin M, et al. Increased psychological distress during COVID-19 and quarantine in ireland: a national survey. J Clin Med. (2020) 9:3481. doi: 10.3390/jcm9113481
13. de Lima CVC, Candido EL, da Silva JA, Albuquerque EV, Soares LM, do Nascimento MM, et al. Effects of quarantine on mental health of populations affected by Covid-19. J Affect Disord. (2020) 275:253–4. doi: 10.1016/j.jad.2020.06.063
14. Peng M, Mo B, Liu Y, Xu M, Song X, Liu L, et al. Prevalence, risk factors and clinical correlates of depression in quarantined population during the COVID-19 outbreak. J Affect Disord. (2020) 275:119–24. doi: 10.1016/j.jad.2020.06.035
15. Ferreira LN, Pereira LN, da Fe Bras M, Ilchuk K. Quality of life under the COVID-19 quarantine. Qual Life Res. (2021) 30:1389–405. doi: 10.1007/s11136-020-02724-x
16. Tharoor I. South Korea's Coronavirus Success Story Underscores How the US Initially Failed. (2020). Available online at: https://www.washingtonpost.com/world/2020/03/17/south-koreas-coronavirus-success-story-underscores-how-us-initially-failed/ (accessed March 17, 2020).
17. Jeong GH, Lee HJ, Lee J, Lee JY, Lee KH, Han YJ, et al. Effective control of COVID-19 in South Korea: cross-sectional study of epidemiological data. J Med Internet Res. (2020) 22:e22103. doi: 10.2196/22103
18. Lee HS, Dean D, Baxter T, Griffith T, Park S. Deterioration of mental health despite successful control of the COVID-19 pandemic in South Korea. Psychiatry Res. (2021) 295:113570. doi: 10.1016/j.psychres.2020.113570
19. OurWorldinData. Emerging COVID-19 Success Story: South Korea Learned the Lessons of MERS. Exemplars in Global Health (EGH). (2020). Available online at: https://ourworldindata.org/covid-exemplar-south-korea (accessed June 30, 2020).
20. OurworldinData. Coronavirus Pandemic (COVID-19) – Statistics and Research. (2021). Available online at: https://ourworldindata.org/coronavirus (accessed January 20, 2021).
21. Ministry of Interior Safety (MOIS). A Preemptive Response System in Preparation for the Recurrence of COVID-19. (2020). Available online at: ://www.mois.go.kr/frt/bbs/type010/commonSelectBoardArticle.do?bbsId=BBSMSTR_000000000008&nttId=81155 (accessed November 17, 2020).
22. Kroenke K, Spitzer RL. The PHQ-9: a new depression diagnostic and severity measure. Psychiatr Ann. (2002) 32:509–15. doi: 10.3928/0048-5713-20020901-06
23. Manea L, Gilbody S, McMillan D. Optimal cut-off score for diagnosing depression with the Patient Health Questionnaire (PHQ-9): a meta-analysis. CMAJ. (2012) 184:281–2. doi: 10.1503/cmaj.110829
24. Han C, Jo SA, Kwak JH, Pae CU., Steffens D, Jo I, et al. Validation of the Patient Health Questionnaire-9 Korean version in the elderly population: the Ansan Geriatric study. Compr Psychiatry. (2008) 49:218–23. doi: 10.1016/j.comppsych.2007.08.006
25. Kroenke K, Spitzer RL, Williams J, Monahan PO, Lowe B. Anxiety disorders in primary care: prevalence, impairment, comorbidity, and detection. Ann Intern Med. (2007) 146:317–25. doi: 10.7326/0003-4819-146-5-200703060-00004
26. Spitzer RL, Kroenke K, Williams J, Lowe B. A brief measure for assessing generalized anxiety disorder the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1037/t02591-000
27. Seo J, Park S. Validation of the Generalized Anxiety Disorder-7 (GAD-7) and GAD-2 in patients with migraine. J Headache Pain. (2015) 16:97. doi: 10.1186/s10194-015-0583-8
28. The EuroQol Group. EuroQol - a new facility for the measurement of health-related quality of life. Health Policy. (1990) 16:199–206. doi: 10.1016/0168-8510(90)90421-9
29. Lee YK, Nam HS, Chuang LH, Kim KY, Yang HK, Kwon IS, et al. South Korean time trade-off values for EQ-5D health states: modeling with observed values for 101 health states. Value Health. (2009) 12:1187–93. doi: 10.1111/j.1524-4733.2009.00579.x
30. Jo MW, Yun SC, Lee SI. Estimating quality weights for EQ-5D health states with the time trade-off method in South Korea. Value Health. (2008) 11:1186–9. doi: 10.1111/j.1524-4733.2008.00348.x
31. Verkuilen J, Smithson M. Mixed and mixture regression models for continuous bounded responses using the beta distribution. J Educ Behav Stat. (2016) 37:82–113. doi: 10.3102/1076998610396895
32. Hawryluck L, Gold WL, Robinson S, Pogorski S, Galea S, Styra R. SARS control and psychological effects of quarantine, Toronto, canada. Emerg Infect Dis. (2004) 10:1206–12. doi: 10.3201/eid1007.030703
33. Umberson D, Montez JK. Social relationships and health: a flashpoint for health policy. J Health Soc Behav. (2010) 51:S54–66. doi: 10.1177/0022146510383501
34. Peirce RS, Frone MR, Russell M, Cooper ML, Mudar P. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychol. (2000) 19:28–38. doi: 10.1037/0278-6133.19.1.28
35. Shi B. Perceived social support as a moderator of depression and stress in college students. Soc Behav Pers. (2021) 49:1–9. doi: 10.2224/sbp.9893
36. Reynolds DL, Garay JR, Deamond SL, Moran MK, Gold W, Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. (2008) 136:997–1007. doi: 10.1017/S0950268807009156
37. Cullen W, Gulati G, Kelly BD. Mental health in the COVID-19 pandemic. QJM Int J Med. (2020) 113:311–2. doi: 10.1093/qjmed/hcaa110
38. Neelam K, Duddu V, Anyim N, Neelam J, Lewis S. Pandemics and pre-existing mental illness: a systematic review and meta-analysis. Brain Behav Immun Health. (2021) 10:100177. doi: 10.1016/j.bbih.2020.100177
Keywords: quarantine, depression, anxiety, quality of life, EQ-5D, COVID-19
Citation: Kwon H-Y, Kim Y and Lee S-Y (2022) What Matters for Depression and Anxiety During the COVID-19 Quarantine?: Results of an Online Cross-Sectional Survey in Seoul, South Korea. Front. Psychiatry 13:706436. doi: 10.3389/fpsyt.2022.706436
Received: 07 May 2021; Accepted: 26 January 2022;
Published: 07 March 2022.
Edited by:
Elham Ahmadian, Tabriz University of Medical Sciences, IranCopyright © 2022 Kwon, Kim and Lee. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Hye-Young Kwon, aGFleW91bmdrd29uMDExMUBnbWFpbC5jb20=
 Hye-Young Kwon
Hye-Young Kwon Yongjoo Kim
Yongjoo Kim Seung-Young Lee2,4
Seung-Young Lee2,4