- 1Department of Applied Cell Sciences, School of Advanced Technologies in Medicine, Tehran University of Medical Sciences, Tehran, Iran
- 2Department of Epidemiology, School of Public Health and Safety, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 3Research Center for Social Determinants of Health, Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 4Department of Cell and Molecular Biology and Microbiology, Faculty of Biological Science and Technology, University of Isfahan, Isfahan, Iran
- 5Department of Biology, Science and Research Branch, Islamic Azad University, Tehran, Iran
- 6Student Research Committee, School of Medicine, Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 7Shahid Beheshti University of Medical Sciences, Tehran, Iran
- 8Hematology, Oncology and Stem Cell Transplantation Research Center, Research Institute for Oncology, Hematology and Cell Therapy, Tehran University of Medical Sciences, Tehran, Iran
- 9Cancer Research Centre, Shahid Beheshti University of Medical Sciences, TehranIran
- 10Cell Therapy and Hematopoietic Stem Cell Transplantation Research Center, Research Institute for Oncology, Hematology, and Cell Therapy, Tehran University of Medical Sciences, Tehran, Iran
Background: Ubiquitin-specific peptidases (USPs), also known as deubiquitinating enzymes (DUBs), play a crucial role in maintaining cellular homeostasis by selectively removing ubiquitin molecules from targeted proteins. This process affects protein stability, subcellular localization, and activity, thereby influencing processes such as DNA repair, cell cycle regulation, and apoptosis. Abnormal USP activities have been linked to various diseases, including cancer. Emerging evidence in lymphoma studies highlights the significance of USPs in controlling signaling pathways related to cancer initiation and progression and presents them as potential therapeutic targets.
Aim: This study aimed to elucidate the multifaceted roles of USPs in lymphoma.
Methods: This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. Articles published in English up to May 2023 were retrieved from PubMed, Web of Science, and Scopus. The inclusion criteria focused on studies investigating the role of USPs in lymphoma cancer, involving human subjects or relevant lymphoma cell lines, exploring molecular mechanisms and signaling pathways, and assessing diagnostic or prognostic value.
Results: After the selection process, 23 studies were selected for analysis. USPs were found to affect various aspects of lymphoma development and progression. Specific USPs were identified with roles in cell-cycle regulation, apoptosis modulation, drug resistance, DNA repair, and influence of key oncogenic pathways, such as B cell receptor (BCR) signaling.
Conclusion: This systematic review underscores the emerging role of USPs in lymphoma and their potential as therapeutic targets. Inhibitors of USPs, such as USP14 inhibitors, show promise in overcoming drug resistance. The dynamic interplay between USPs and lymphoma biology presents an exciting opportunity for future research and the development of more effective treatments for patients with lymphoma. Understanding the intricate functions of USPs in lymphoma offers new insights into potential therapeutic strategies, emphasizing the significance of these enzymes in the context of cancer biology.
1 Introduction
Ubiquitin-specific peptidases (USPs), also known as deubiquitins (DUBs), play an important role in maintaining cellular homeostasis by selectively cleaving ubiquitin molecules from targeted proteins. This deubiquitination process affects protein stability, subcellular localization, and activity, allowing complex cellular processes, such as deoxyribonucleic acid (DNA) repair, cell-cycle regulation, resistance to infection, and apoptosis. Given the diverse nature of these enzymes, it is not surprising that their abnormal activities have been linked to many human diseases, including cancer (Bhattacharya et al., 2020; Gatti et al., 2020; Qin et al., 2022; Ramakrishna et al., 2015; Yuan et al., 2018).
In the field of lymphoma, emerging evidence indicates the significant influence of USPs, which play important roles in the cancer process. These enzymes control important signaling pathways involved in the initiation and progression of lymphoma, including the regulation of survival, growth, and immunity. As researchers have uncovered the subtleties of these interactions, USPs have emerged as promising therapeutic targets in lymphoma (Hariri and St-Arnaud, 2021; Rojo-Arreola et al., 2020; Shen et al., 2023).
The ubiquitin–protease system (UPS) is likely involved in human brain development since a defect in the gene encoding the E3 ligase E6-AP has been directly implicated in the cause of Angelman syndrome. The UPS operates through several enzymatic steps, including ubiquitin ligases that bind ubiquitin molecules to target proteins and USPs that degrade the molecules and determine the fate of the tagged proteins (Bachiller et al., 2020; Crawford and Irvine, 2013; Lescouzeres and Bomont, 2020; Morrow et al., 2015; Thapa et al., 2020; Yang et al., 2016).
USPs are part of the UPS and contribute to the balance between protein synthesis and degradation. Disruption of this balance can lead to abnormal or damaged cells, resulting in cancer and other diseases. In lymphoma, disruption of the protein degradation pathway can lead to uncontrolled cell proliferation, apoptosis evasion, and a boost of the immune system (Crawford and Irvine, 2013; Kukharsky et al., 2022; Liu et al., 2023; McKinnon and Tabrizi, 2014).
The repertoire of deubiquitination enzymes is broad and diverse, with more than 100 members having different substrate specificities and cellular localizations. Various enzymes have been implicated in the development of lymphoma. For example, USP9X, a DUB known for its role in DNA repair and cell cycle, is overexpressed in certain lymphoma subtypes and contributes to cell survival and disease resistance. Conversely, USP7, a key regulator of p53 stability, plays a role in promoting lymphomagenesis through its ability to inhibit p53-mediated apoptosis (Li et al., 2021; Li et al., 2022; Park et al., 2022; Pawlak et al., 2021; Qi et al., 2020; Qian et al., 2015; Toloczko et al., 2017; Wang et al., 2019; Zhan et al., 2017; Zhou et al., 2018).
Another member of the USP family, USP15, is indirectly involved in nuclear factor kappa B (NF-κB) signaling. NF-κB is a regulator of inflammation and the immune system and is often dysregulated in lymphoma. USP15 potentiates key components of the NF-κB pathway, leading to activation and subsequent oncogenicity. These examples illustrate the subtle and complex roles of deubiquitination enzymes in the development of lymphoma biology (Zhang et al., 2015; Zhong et al., 2021; Zhou et al., 2020).
Lymphomagenesis is a multifactorial process that is usually driven by the activation of specific signals that promote the growth and survival of cancer cells. USPs have emerged as important regulators because of their ability to regulate the stability and function of proteins involved in these pathways (DeKroon et al., 2018; Jakos et al., 2020; Jiang and Cong, 2016).
One of the most studied pathways in lymphoma is the B-cell receptor (BCR) signaling pathway. Dysfunction of this pathway can lead to uncontrolled B-cell proliferation and lymphoma development. Here, USPs such as OTU deubiquitinase (OTUB1) and CYLD were identified as key regulators that exert their potential by controlling the degradation of key signals in the BCR pathway. For example, OTUB1 supports B-cell survival by stabilizing B-cell lymphoma 6 (BCL6), a transcriptional repressor associated with lymphomagenesis (De Santis et al., 2022; Jiao et al., 2020; Schneider et al., 2016).
The interaction between ubiquitin-specific peptidases and lymphoma provides an interesting explanation for the development of the cancer microenvironment. This review assessed the complex functions of UPS in signaling, protein stability, and immune system regulation during lymphomagenesis.
2 Materials and methods
2.1 Data sources and search strategies
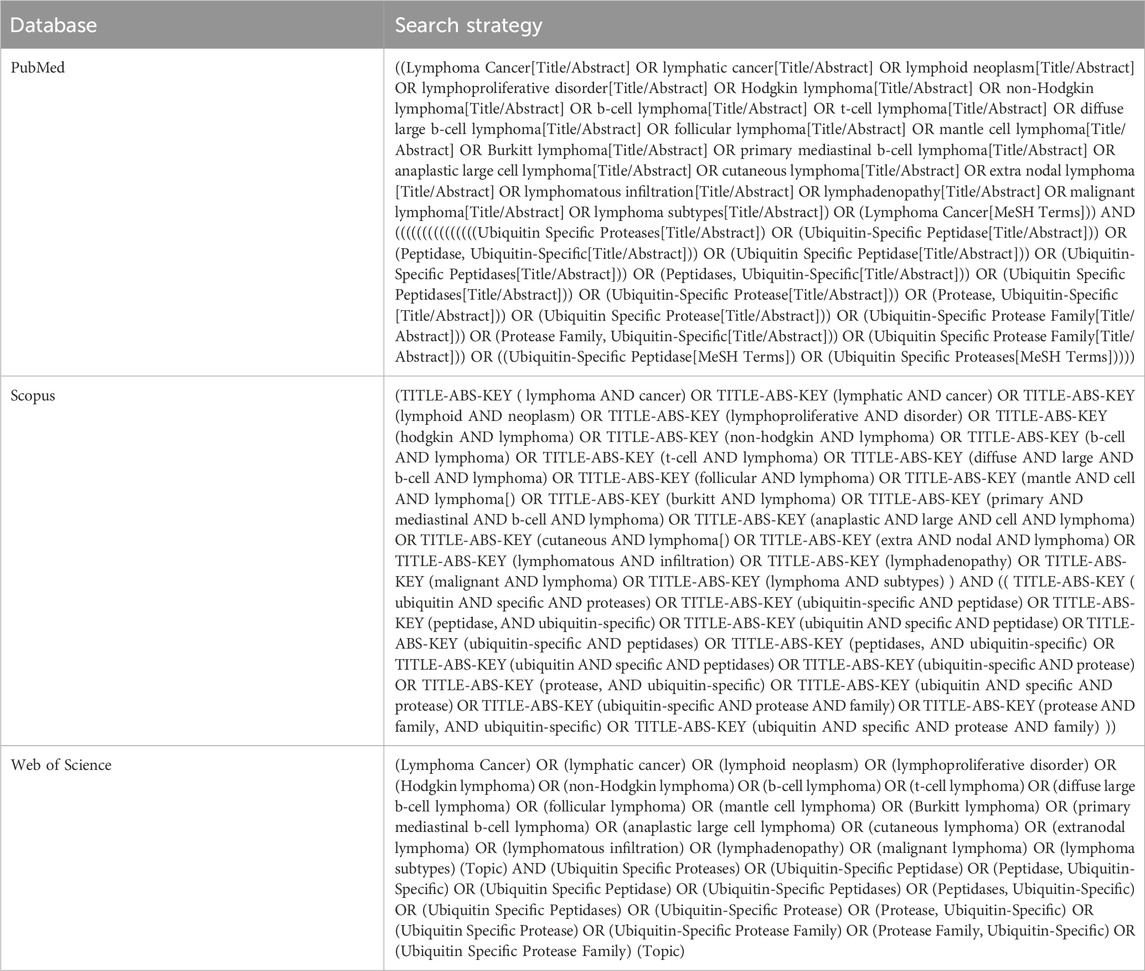
This study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (Moher et al., 2015). We have included articles published in English until May 2023. Three databases, namely, PubMed, Web of Science, and Scopus, were searched for relevant studies. The exact search strategies used in this study are presented in Table 1. EndNote version 21 was used to manage and deduplicate the retrieved articles and the screening process.
2.2 Inclusion and exclusion criteria
The following inclusion and exclusion criteria were used to select appropriate articles:
Inclusion criteria: 1) studies that investigated the role of USPs in lymphoma cancer; 2) studies published in English; 3) original articles; 4) studies focusing on human subjects or relevant lymphoma cell lines; 5) articles that provide insights into the involvement of USPs in the pathogenesis, progression, diagnosis, prognosis, or treatment of lymphoma; 6) studies that explore the molecular mechanisms or signaling pathways associated with USPs in lymphoma; 7) articles that investigate the potential of USPs as therapeutic targets in lymphoma; 8) studies examining the diagnostic or prognostic value of USPs in lymphoma.
Exclusion criteria: 1) studies not directly related to the role of USPs in lymphoma cancer; 2) non-English publications; 3) non-original articles such as review studies, conference abstracts, editorials, or letters; 4) animal or in vitro studies not directly applicable to lymphoma; 5) duplicate articles or studies with insufficient data; 6) studies that primarily focus on other types of cancer without substantial inclusion of lymphoma.
3 Results
3.1 Study selection
In total, 354 records were extracted from all databases (Figure 1 represents the study selection approach). After excluding duplicates, non-original (including review articles, letters, and editorials), and irrelevant articles, 23 studies were selected for an accurate evaluation of the role of USPs in lymphoma cancer (Table 2).

Figure 1. Flowchart of the study selection procedure. The flow diagram was made based on the PRISMA guidelines.
3.1.1 USPs regulate cell cycle progression by regulating cycle-related factors
USP2 stabilizes cyclin D1, which participates in homologous recombination (HR)-mediated DNA repair. In numerous cell types, it promotes cell-cycle progression from G1 to S. USP2 becomes active or overexpressed in several cancers, such as mantle cell lymphoma, a subtype of non-Hodgkin’s lymphoma. It has been demonstrated that ML364 (small-molecule USP2 and USP8 inhibitor) induces cell-cycle arrest through cyclin D1 degradation by inhibiting USP2.
In CD4+ T cells, USP12 stabilizes B-cell lymphoma/leukemia 10 (BCL10), leading to the activation of the NF-κB signaling pathway. USP12 plays an important role in the differentiation, activation, and proliferation of the CD4+ T cell phenotype, but it is not observed in CD8+ T cells. According to a recent study, USP12 plays a critical role in prostate cancer through deubiquitination of androgen receptors to increase Ak strain transforming (AKT) signaling. Knockdown of USP12 in HeLa cells leads to cell-cycle arrest and reduced transcription of BMI-1, c-Myc, and cyclin D2; therefore, USP12 may adjust cell-cycle progression (Fu et al., 2021).
USP44 is a significant regulator of the cell cycle, DNA repair, and gene expression. USP44 deficiency in the Emu-Myc mouse B-cell lymphoma model causes early lethality (Lin et al., 2019).
3.1.2 The role of USPs in apoptosis
Several key factors have been recognized to play important roles in apoptosis, one of the most important being the tumor suppressor gene p53, and its activity inhibits the generation of tumors. USP2 is described as an oncogene due to its capability to inhibit apoptosis. USP2a has been investigated in numerous cancers, and it has been revealed that higher expression of USP2a is related to advanced stages. In advanced cutaneous T-cell lymphoma (CTCL), the expression of USP2a was lower than that of normal T-lymphocytes, suggesting that it is a tumor suppressor in CTCL, unlike in solid cancers. Wei et al. demonstrated that the knockdown of USP2 causes increased apoptosis after PUVA treatment in MyLa 2000, suggesting that USP2 can display therapeutic resistance. They showed that p53 activation can promote USP2 induction. They also illustrated that USP2 stabilized mouse double minute 2 homolog (Mdm2), but more evidence is needed to link USP2 deubiquitinase activity with Mdm2-p53 signaling. They also explained that USP2 may play an anti-apoptotic role in CTCL and exert a reverse effect in PUVA (Wei et al., 2016).
Kaposi’s sarcoma-associated herpesvirus (KSHV) expresses a series of open reading frames (ORFs) to prevent premature apoptosis and support its viability. Considering that USP7 is a p53 deubiquitinase, KSHV ORF45 inhibits the interactions between USP7 and p53 by binding to p53. As a result, the accumulation and localization of p53 decrease in the cytoplasm, and its transcriptional function decreases.
Under normal circumstances, USP7 binds to human double minute 2 (HDM2) via the death domain-associated protein death-associated protein 6 (DAXX), which prevents the self-ubiquitination of HDM2 and causes the degradation of p53 by HDM2 accumulation. However, in the context of DNA damage, HDM2 dissociates from the USP7–DAXX complex, resulting in self-ubiquitination and subsequent degradation of HDM2, and then USP7 binds to p53 (Alzhanova et al., 2021). USP15 stabilizes MDM2 and regulates p53 function, thus boosting tumor cell survival (Qu et al., 2018).
Based on a recent experiment, USP9X overexpression was found associated with diffuse large B-cell lymphoma (DLBCL) development and progression. USP9X expression was four times greater in malignant cells, including Farage and Pfeiffer cells, than in normal B cells. Inhibition of this USP using siRNA downregulates the expression of Mcl-1 and upregulates the expression of caspase-3, Bak, and cytochrome C; therefore, knockdown of USP9X induces cell apoptosis and decreases cell proliferation in DLBCL (Peng et al., 2020).
Furthermore, USP9X upregulation plays a key role in the formation of mantle cell lymphoma (MCL) via different pathways, including enhanced cell proliferation and cell cycle, inhibition of cell death, and induction of angiogenesis. USP9X is present at high levels in both peripheral blood mononuclear cells (PBMCs) and MCL cells of patients with MCL. Because USP9X affects cell migration and angiogenesis by elevating CCND1-mediated SOX11 expression, USP9X suppression leads to the downregulation of USP9X protein levels in Z-138 and Jeko-1 cell lines and inhibits tumor development in mice in vivo. In addition, USP9X knockdown shortens the duration of the S stage; reduces the expression of cyclin-dependent kinase 4 (CDK4), cyclin-dependent kinase 6 (CDK6), and proliferating cell nuclear antigen (PCNA); and increases P21 protein expression (Huang et al., 2022a).
USP21 was shown to be overexpressed in the DLBCL lymphoid tissue compared with matching healthy tissues and cell lines such as A20 and SU-DHL-4. It increases the growth of DLBCL cells through cysteine 221 (the catalytic site of USP21), but it does not affect cell death. In addition, USP21 participates in the development of lymphoma through the stabilization of enhancer of zeste homolog 2 (EZH2), which is required for generating germinal centers and lymphoma tumors. There is a positive correlation between the elevated expression of USP21 and high mortality in patients; therefore, small interfering RNA (siRNA) knockdown of USP21 and consequent reduction of tumor cell proliferation may be a promising treatment for DLBCL (Ma et al., 2021).
LIM homeobox 2 (LHX2) is an oncogene that promotes malignancy in breast cancer and pancreatic ductal adenocarcinoma. LHX2 adjusts USP18 expression in cancers with poor prognosis. In addition, the reduction of the expression of the immune gene USP18 can decrease the number of activated dendritic cells (aDC), resulting in poor prognosis (Zhao et al., 2021). In addition, a disorder in USP18 expression in Burkitt lymphoma can lead to interferon (IFN)-stimulated gene expression. Therefore, it is likely that USP18 regulates IFN-I-associated immune responses to develop extranodal diffuse large B-cell lymphoma (EN DLBCL) with poor prognosis. The mitogen-activated protein kinase (MAPK) pathway is a possible downstream pathway of USP18 that plays a role in cellular processes such as proliferation, differentiation, and apoptosis. Overall, USP18 plays a potential role via the MAPK pathway and aDCs in EN DLBCL. In addition to USP12, it regulates the MAPK signaling pathway because its knockout leads to impaired MAPK activity in cells (Zhao et al., 2021).
USP7 regulates various activities, including DNA repair, cell cycle progression, protein localization, and apoptosis. USP7 is overexpressed in lymphomas in dogs, and P5091 is an inhibitor that has cytotoxic effects in canine lymphoma and cancer cells. USP7i likely stabilizes the p53 protein and, therefore, may cause apoptosis (Pawlak et al., 2021).
3.1.3 USP function in the DNA repair pathway
USP44 plays an important role in DNA repair through its DUB catalytic function on the histones H2B and H2A and promotes gene silencing. USP44 deficiency and overexpression are prone to errors in chromosome separation, aneuploidy, and cancer; for example, its overexpression was noted in T-cell acute lymphoblastic leukemia (Lin et al., 2019). USP34 expression increases in the germinal center B-cell-like (GCB) subtype of DLBCL cases, and USP34 is correlated with Wnt signaling activation by destabilization of β-catenin. In addition, USP34 responds to DNA damage and is a downstream target of mutant ataxia telangiectasia in DNA damage (Li et al., 2018).
UBP43, also known as USP18, is encoded by an interferon-stimulated gene (ISG) and functions as a remover of the ISG15 polypeptide from ISGylated proteins. This protease negatively regulates IFN-I signaling by blocking STAT phosphorylation, leading to a reduction in the induction of ISGs. This inhibition occurs via the direct displacement of Janus kinase 1 (JAK1) from the IFN-α/β receptor. A reduction in the IFN-inducible expression of UBP43 leads to a notable delay in the negative feedback regulation of type-I interferon signaling in Burkitt lymphoma (BL) cell lines (including Akata A.2 and A.15), regardless of their Epstein–Barr virus (EBV) status (Ruf et al., 2009).
3.1.4 USPs and drug resistance
The use of drugs that inhibit proteasome (mainly bortezomib) activity in multiple myeloma is currently a standard therapy. One way of targeting the proteasome is through USPs such as USP14 for different cancer types, including lymphoma, and even cancer cells resistant to bortezomib (Delforoush et al., 2017).
USP24 has anti-apoptotic tumoral activity in myeloma cells and is overexpressed in drug-resistant cells. It was also found that enhanced USP24 expression was regularly observed in the interfollicular zones of splenic marginal zone lymphoma (SMZL) patients. Given its role in regulating tumor microenvironment signaling, USP24 has been identified as a potential therapeutic target (Robinson et al., 2020).
USP1 can act as an oncogene and is highly expressed in DLBCL patients. High expression of USP1 is associated with poor prognosis in DLBCL. USP1 plays an important role in the rituximab/chemotherapy resistance of DLBCL via deubiquitination of MAX (highly expressed in DLBCL cells). Knockdown of USP1 leads to inhibition of cell proliferation, cell-cycle arrest, reduced MAX/MYC, and autophagy in DLBCL cells (Li et al., 2023).
Some members of the USP family are considered possible targets of anticancer agents, such as USP7, which targets c-Myc. USP7 inhibition destabilizes the CHK1 protein, resulting in AML cells being sensitized to the chemotherapeutic factor cytarabine. Targeting USP1 may also be another therapeutic strategy for MYC-related tumors. Eµ-Myc/cRel−/− lymphomas have downregulated the expression of USP1 and checkpoint kinase 1 (CHK1) protein that results in resistance to treatment by specific CHK1i. The loss of the CHK1 pathway is related to the downregulation of CHK1, and USP1 inhibition with ML323 can contribute to CHK1 inhibitor resistance (Hunter et al., 2022b).
USP39 elimination in the B-cell lineage prevented the transition from pre-pro-B cells to pro-B cells in the bone marrow, resulting in substantial reduction in mature B cells in peripheral tissues. USP39 ablation in Em-Myc mice successfully controls the expansion of malignant pre-B cells, lowered B-cell lymphomagenesis, and boosted survival. Because the spliceosome component of USP39 has a role in B-cell development and in controlling the rearrangement of immunoglobulin genes, targeting USP39 could represent a promising therapeutic strategy for treating B-cell lymphoma (Ruan et al., 2022).
USP37 expression is positively associated with c-MYC expression in activated B-cell-like-DLBCL (ABC-DLBCL) but not with its GCB subtype. USP37 stabilizes c-MYC and causes unusual cell growth. USP22 and USP36 regulate the cellular turnover of c-MYC in breast cancer, and c-MYC expression is stabilized by USP28 and USP37 in colon carcinoma and lung cancer, respectively. Other USPs, including USP13, USP16, USP17, and USP22, can maintain c-MYC expression in the GCB subtype of DLBCL (Kamran et al., 2023).
Viruses such as Kaposi’s sarcoma-associated herpesvirus (KSHV) control deubiquitination. KSHV is the causative agent of Kaposi’s sarcoma, primal effusion lymphoma, and the plasmablastic shape of multicentric Castleman disease. Here, USP9X plays a pro-viral role, and its depletion prevents virus reactivation and the production of infectious virions (Chappell et al., 2023).
3.1.5 USPs as targets for drug development in cancer prevention
USP29 stabilizes MYC and hypoxia-inducible factor 1-alpha (HIF1α); therefore, it enables tumor cells to respond to both normoxia and hypoxia. Knockout of Usp29 significantly prolongs the survival of tumor-bearing mice by reducing the expressions of MYC and HIF1α in neuroblastoma and B-cell lymphoma. Therefore, USP29 can be used as a new therapeutic target for treating cancer (Tu et al., 2021).
USP7 expression was significantly increased in three cancer types, including DLBCL. ABC-DLBCL is a subtype of non-Hodgkin’s lymphoma with a poor prognosis; its survival is related to the activation of BCR signaling. USP7 stabilizes WD repeat-containing protein 5 (WDR5) and mixed-lineage leukemia 2 (MLL2) (parts of lysine-specific methyltransferase complex) in ABC-DLBCL cells. The expression of USP7 is upregulated in ABC-DLBCL cells and downregulated in GCB-DLBCL cells; therefore, USP7 inhibition has a serious effect on ABC-DLBCL cells, contrary to that observed in GCB-DLBCL cells. ABC-DLBCL cells upregulate the expression of some components of BCR signaling, and USP7 inhibition decreases the expression of upregulated parts of BCR signaling and plays an important role in therapeutic targets (Wu et al., 2022a).
Latent membrane protein 1 (LMP1) is expressed in EBV-associated lymphomas. USP2a is detected in LMP1-positive Burkitt’s lymphoma (BL) cells and mediates the stabilization of fatty acid synthase (FASN). FASN expression is notably correlated with distant lymph node metastasis. USP2a inhibition through ML364 decreased FASN levels and inhibited the proliferation of LMP1-positive BL cell lines. Targeting USP2a is an effective strategy for future investigation of ML364 treatment in malignancies with LMP1-positive expression (Hulse et al., 2021).
The fact that we only considered three databases (PubMed, Web of Science, and Scopus) may prove to be a limitation to our study. In addition, the exclusion of studies published in other languages may constitute another limitation of our study.
4 Conclusion
In conclusion, this systematic review delved into the emerging and intricate role of USPs in lymphoma, shedding light on their potential as therapeutic targets. The landscape of research on USPs in lymphoma has revealed a novel and promising avenue for understanding and potentially treating this complex group of hematologic malignancies. Through an extensive literature review, this article highlights the diverse functions of USPs, which span critical cellular processes such as cell-cycle regulation, apoptosis, DNA repair, and drug resistance. A comprehensive understanding of how USPs influence these processes in the context of lymphoma is essential for researchers and clinicians seeking to unravel the intricacies of this disease.
As our understanding of the intricate roles of USPs in lymphoma deepens, the prospect of developing more effective and targeted treatment options for patients with lymphoma becomes increasingly feasible. The dynamic interplay between USPs and lymphoma biology presents an exciting opportunity for further research and clinical exploration to improve the outcomes and quality of life for patients affected by this heterogeneous group of malignancies. Future investigations in this field may unveil novel and innovative strategies for combating lymphoma, reaffirming the significance of USPs as a focal point of interest in cancer research and therapy.
5 Key points
1. USPs and cellular homeostasis: USPs, also known as deubiquitinase (DUBs), are essential for maintaining cellular balance by selectively removing ubiquitin molecules from target proteins. The deubiquitination process influences protein stability, subcellular localization, and activity, contributing to critical cellular processes such as DNA repair, cell-cycle regulation, immunity, and apoptosis.
2. USPs and human diseases: dysregulation of USP activities is associated with various human diseases, including cancer. Abnormalities in these enzymes can lead to disruption of cellular processes, resulting in conditions such as cancer. The versatile nature of USPs makes them a potential therapeutic target.
3. USPs in lymphoma: in lymphoma, USPs play a significant role in controlling the signaling pathways that affect cancer initiation and progression. They regulate critical factors involved in cell survival, growth, and immunity. The abnormal activities of USPs are linked to the development of lymphoma, highlighting their potential as therapeutic targets.
4. Ubiquitin–proteasome system (UPS): understanding the effects of USPs on lymphoma requires a better understanding of the ubiquitin–proteasome system (UPS). The UPS regulates protein degradation and function through a series of enzymatic steps, including ubiquitin ligases and USPs. Aberrations in this system can lead to cancer and other diseases by disrupting the balance between protein synthesis and degradation.
5. Diverse roles of USPs: with more than 100 members, USPs exhibit diverse substrate specificity and cellular localizations. Specific USPs are implicated in the development of lymphoma, influencing processes such as DNA repair, cell-cycle progression, apoptosis, and immune response regulation.
6. Targeting USPs for therapy: given the intricate roles of USPs in lymphomagenesis, they are potential targets for therapeutic intervention. Inhibiting specific USPs could disrupt cancer-promoting pathways, thereby leading to new treatment strategies for lymphoma and related malignancies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material; further inquiries can be directed to the corresponding authors.
Author contributions
MS-S: Data curation, Investigation, Writing–original draft, Writing–review and editing. ST: Data curation, Investigation, Writing–original draft, Writing–review and editing. AH: Investigation, Methodology, Project administration, Validation, Visualization, Writing–original draft, Writing–review and editing. ShT: Data curation, Investigation, Writing–review and editing. A-HB: Data curation, Investigation, Writing–review and editing. AT-T: Data curation, Investigation, Writing–original draft, Writing–review and editing. MN: Data curation, Investigation, Writing–original draft, Writing–review and editing. ZS: Supervision, Writing–review and editing. JV: Supervision, Validation, Writing–review and editing. SR: Methodology, Supervision, Validation, Writing–review and editing. AM-J: Investigation, Methodology, Resources, Supervision, Validation, Writing–original draft, Writing–review and editing. MA: Investigation, Supervision, Writing–review and editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This study was funded partially by the Shahid Beheshti University of Medical Sciences, Tehran, Iran (grant number: 43005899).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors, and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alzhanova, D., Meyo, J. O., Juarez, A., and Dittmer, D. P. (2021). The ORF45 protein of Kaposi sarcoma-associated herpesvirus is an inhibitor of p53 signaling during viral reactivation. J. Virol. 95 (23), e0145921. doi:10.1128/JVI.01459-21
Bachiller, S., Alonso-Bellido, I. M., Real, L. M., Perez-Villegas, E. M., Venero, J. L., Deierborg, T., et al. (2020). The ubiquitin proteasome system in neuromuscular disorders: moving beyond movement. Int. J. Mol. Sci. 21 (17), 6429. doi:10.3390/ijms21176429
Bhattacharya, U., Neizer-Ashun, F., Mukherjee, P., and Bhattacharya, R. (2020). When the chains do not break: the role of USP10 in physiology and pathology. Cell Death Dis. 11 (12), 1033. doi:10.1038/s41419-020-03246-7
Chappell, D. L., Sandhu, P. K., Wong, J. P., Bhatt, A. P., Liu, X., Buhrlage, S. J., et al. (2023). KSHV viral protein kinase interacts with USP9X to modulate the viral lifecycle. J. Virol. 97 (3), e0176322. doi:10.1128/jvi.01763-22
Crawford, L. J., and Irvine, A. E. (2013). Targeting the ubiquitin proteasome system in haematological malignancies. Blood Rev. 27 (6), 297–304. doi:10.1016/j.blre.2013.10.002
Davis, M. I., Pragani, R., Fox, J. T., Shen, M., Parmar, K., Gaudiano, E. F., et al. (2016). Small molecule inhibition of the ubiquitin-specific protease USP2 accelerates cyclin D1 degradation and leads to cell cycle arrest in colorectal cancer and mantle cell lymphoma models. J. Biol. Chem. 291 (47), 24628–24640. doi:10.1074/jbc.M116.738567
DeKroon, R. M., Gunawardena, H. P., Edwards, R., and Raab-Traub, N. (2018). Global proteomic changes induced by the epstein-barr virus oncoproteins latent membrane protein 1 and 2A. mBio 9 (3), e00959. doi:10.1128/mBio.00959-18
Delforoush, M., Berglund, M., Edqvist, P. H., Sundström, C., Gullbo, J., and Enblad, G. (2017). Expression of possible targets for new proteasome inhibitors in diffuse large B-cell lymphoma. Eur. J. Haematol. 98 (1), 52–56. doi:10.1111/ejh.12784
De Santis, F., Romero-Cordoba, S. L., Castagnoli, L., Volpari, T., Faraci, S., Fuca, G., et al. (2022). BCL6 and the Notch pathway: a signaling axis leading to a novel druggable biotarget in triple negative breast cancer. Cell Oncol. (Dordr) 45 (2), 257–274. doi:10.1007/s13402-022-00663-y
Fu, Y., Wang, P., Zhao, J., Tan, Y., Sheng, J., He, S., et al. (2021). USP12 promotes CD4(+) T cell responses through deubiquitinating and stabilizing BCL10. Cell Death Differ. 28 (10), 2857–2870. doi:10.1038/s41418-021-00787-y
Gatti, V., Bernassola, F., Talora, C., Melino, G., and Peschiaroli, A. (2020). The impact of the ubiquitin system in the pathogenesis of squamous cell carcinomas. Cancers (Basel) 12 (6), 1595. doi:10.3390/cancers12061595
Hariri, H., and St-Arnaud, R. (2021). Expression and role of ubiquitin-specific peptidases in osteoblasts. Int. J. Mol. Sci. 22 (14), 7746. doi:10.3390/ijms22147746
Huang, G., Liao, J., Wang, M., Huang, Y., Tang, M., and Hao, Y. (2022a). USP9X increased tumor angiogenesis in mantle cell lymphoma by upregulation of CCND1-mediated SOX11. Mediterr. J. Hematol. Infect. Dis. 14 (1), e2022048. doi:10.4084/MJHID.2022.048
Huang, G., Liao, J. J., Wang, M. L., Huang, Y. L., Tang, M. J., and Hao, Y. Y. (2022b). USP9X increased tumor angiogenesis in mantle cell lymphoma by upregulation of CCND1- mediated SOX11. Mediterr. J. Hematol. Infect. Dis. 14, e2022048. doi:10.4084/MJHID.2022.048
Hulse, M., Johnson, S. M., Boyle, S., Caruso, L. B., and Tempera, I. (2021). Epstein-barr virus-encoded latent membrane protein 1 and B-cell growth transformation induce lipogenesis through fatty acid synthase. J. Virol. 95 (4), e01857. doi:10.1128/JVI.01857-20
Hunter, J. E., Campbell, A. E., Hannaway, N. L., Kerridge, S., Luli, S., Butterworth, J. A., et al. (2022a). Regulation of CHK1 inhibitor resistance by a c-Rel and USP1 dependent pathway. Biochem. J. 479 (19), 2063–2086. doi:10.1042/bcj20220102
Hunter, J. E., Campbell, A. E., Hannaway, N. L., Kerridge, S., Luli, S., Butterworth, J. A., et al. (2022b). Regulation of CHK1 inhibitor resistance by a c-Rel and USP1 dependent pathway. Biochem. J. 479 (19), 2063–2086. doi:10.1042/BCJ20220102
Jakos, T., Pislar, A., Pecar Fonovic, U., and Kos, J. (2020). Lysosomal peptidases in innate immune cells: implications for cancer immunity. Cancer Immunol. Immunother. 69 (2), 275–283. doi:10.1007/s00262-019-02447-0
Jiang, X., and Cong, F. (2016). Novel regulation of Wnt signaling at the proximal membrane level. Trends Biochem. Sci. 41 (9), 773–783. doi:10.1016/j.tibs.2016.06.003
Jiao, J., Lv, Z., Zhang, P., Wang, Y., Yuan, M., Yu, X., et al. (2020). AID assists DNMT1 to attenuate BCL6 expression through DNA methylation in diffuse large B-cell lymphoma cell lines. Neoplasia 22 (3), 142–153. doi:10.1016/j.neo.2020.01.002
Kamran, D. E. S., Hussain, M., and Mirza, T. (2023). Investigating in situ expression of c-MYC and candidate ubiquitin-specific proteases in DLBCL and assessment for peptidyl disruptor molecule against c-MYC-USP37 complex. Molecules 28 (6), 2441. doi:10.3390/molecules28062441
Kukharsky, M. S., Everett, M. W., Lytkina, O. A., Raspopova, M. A., Kovrazhkina, E. A., Ovchinnikov, R. K., et al. (2022). Protein homeostasis dysregulation in pathogenesis of neurodegenerative diseases. Mol. Biol. Mosk. 56 (6), 967–978. doi:10.1134/s0026893322060115
Lescouzeres, L., and Bomont, P. (2020). E3 ubiquitin ligases in neurological diseases: focus on gigaxonin and autophagy. Front. Physiol. 11, 1022. doi:10.3389/fphys.2020.01022
Li, C., Huang, L., Lu, H., Wang, W., Chen, G., Gu, Y., et al. (2018). Expression and clinical significance of ubiquitin-specific-processing protease 34 in diffuse large B-cell lymphoma. Mol. Med. Rep. 18 (5), 4543–4554. doi:10.3892/mmr.2018.9447
Li, C., Xia, J., Franqui-Machin, R., Chen, F., He, Y., Ashby, T. C., et al. (2021). TRIP13 modulates protein deubiquitination and accelerates tumor development and progression of B cell malignancies. J. Clin. Invest 131 (14), e146893. doi:10.1172/JCI146893
Li, J., Dai, Y., Ge, H., Guo, S., Zhang, W., Wang, Y., et al. (2022). The deubiquitinase USP7 promotes HNSCC progression via deubiquitinating and stabilizing TAZ. Cell Death Dis. 13 (8), 677. doi:10.1038/s41419-022-05113-z
Li, X. Y., Wu, J. C., Liu, P., Li, Z. J., Wang, Y., Chen, B. Y., et al. (2023). Inhibition of USP1 reverses the chemotherapy resistance through destabilization of MAX in the relapsed/refractory B-cell lymphoma. Leukemia 37 (1), 164–177. doi:10.1038/s41375-022-01747-2
Lin, Y. H., Forster, M., Liang, Y., Yu, M., Wang, H., Robert, F., et al. (2019). USP44 is dispensable for normal hematopoietic stem cell function, lymphocyte development, and B-cell-mediated immune response in a mouse model. Exp. Hematol. 72, 1–8. doi:10.1016/j.exphem.2019.01.001
Liu, Z., Wang, P., Zhao, Y., Po Lai, K., and Li, R. (2023). Biomedical importance of the ubiquitin-proteasome system in diabetes and metabolic transdifferentiation of pancreatic duct epithelial cells into β-cells. Gene 858, 147191. doi:10.1016/j.gene.2023.147191
Ma, H., Luo, X., Zhou, P., He, N., Zhou, J., Liu, M., et al. (2021). USP21 promotes cell proliferation by maintaining the EZH2 level in diffuse large B-cell lymphoma. J. Clin. Lab. Anal. 35 (3), e23693. doi:10.1002/jcla.23693
McKinnon, C., and Tabrizi, S. J. (2014). The ubiquitin-proteasome system in neurodegeneration. Antioxid. Redox Signal 21 (17), 2302–2321. doi:10.1089/ars.2013.5802
Moher, D., Shamseer, L., Clarke, M., Ghersi, D., Liberati, A., Petticrew, M., et al. (2015). Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 4 (1), 1. doi:10.1186/2046-4053-4-1
Morrow, J. K., Lin, H. K., Sun, S. C., and Zhang, S. (2015). Targeting ubiquitination for cancer therapies. Future Med. Chem. 7 (17), 2333–2350. doi:10.4155/fmc.15.148
Park, H. B., Hwang, S., and Baek, K. H. (2022). USP7 regulates the ERK1/2 signaling pathway through deubiquitinating Raf-1 in lung adenocarcinoma. Cell Death Dis. 13 (8), 698. doi:10.1038/s41419-022-05136-6
Pawlak, A., Bajzert, J., Bugiel, K., Hernández Suárez, B., Kutkowska, J., Rapak, A., et al. (2021). Ubiquitin-specific protease 7 as a potential therapeutic target in dogs with hematopoietic malignancies. J. Vet. Intern Med. 35 (2), 1041–1051. doi:10.1111/jvim.16082
Peng, W., Zhong, M. Z., and Tang, Y. H. (2020). Effect of siRNA interference of ubiquitin-specific protease 9X on apoptosis and growth of diffuse large B cell lymphoma cell line. Mater Express 10 (3), 446–453. doi:10.1166/mex.2020.1653
Qi, S. M., Cheng, G., Cheng, X. D., Xu, Z., Xu, B., Zhang, W. D., et al. (2020). Targeting USP7-mediated deubiquitination of MDM2/MDMX-p53 pathway for cancer therapy: are we there yet? Front. Cell Dev. Biol. 8, 233. doi:10.3389/fcell.2020.00233
Qian, J., Pentz, K., Zhu, Q., Wang, Q., He, J., Srivastava, A. K., et al. (2015). USP7 modulates UV-induced PCNA monoubiquitination by regulating DNA polymerase eta stability. Oncogene 34 (36), 4791–4796. doi:10.1038/onc.2014.394
Qin, B., Zhou, L., Wang, F., and Wang, Y. (2022). Ubiquitin-specific protease 20 in human disease: emerging role and therapeutic implications. Biochem. Pharmacol. 206, 115352. doi:10.1016/j.bcp.2022.115352
Qu, C. J., Kunkalla, K., Vaghefi, A., Frederiksen, J. K., Liu, Y. D., Chapman, J. R., et al. (2018). Smoothened stabilizes and protects TRAF6 from degradation: a novel non-canonical role of smoothened with implications in lymphoma biology. Cancer Lett. 436, 149–158. doi:10.1016/j.canlet.2018.08.020
Ramakrishna, S., Suresh, B., and Baek, K. H. (2015). Biological functions of hyaluronan and cytokine-inducible deubiquitinating enzymes. Biochim. Biophys. Acta 1855 (1), 83–91. doi:10.1016/j.bbcan.2014.11.006
Robinson, J. E., Greiner, T. C., Bouska, A. C., Iqbal, J., and Cutucache, C. E. (2020). Identification of a splenic marginal zone lymphoma signature: preliminary findings with diagnostic potential. Front. Oncol. 10, 640. doi:10.3389/fonc.2020.00640
Rojo-Arreola, L., Garcia-Carreno, F., Romero, R., and Diaz Dominguez, L. (2020). Proteolytic profile of larval developmental stages of Penaeus vannamei: an activity and mRNA expression approach. PLoS One 15 (9), e0239413. doi:10.1371/journal.pone.0239413
Ruan, G. X., Li, Y., Chen, W., Huang, H., Zhang, R., Chen, C., et al. (2022a). The spliceosome component Usp39 controls B cell development by regulating immunoglobulin gene rearrangement. Cell Rep. 38 (6), 110338. doi:10.1016/j.celrep.2022.110338
Ruan, G.-X., Li, Y., Chen, W., Huang, H., Zhang, R., Chen, C., et al. (2022b). The spliceosome component Usp39 controls B cell development by regulating immunoglobulin gene rearrangement. Cell Rep. 38 (6), 110338. doi:10.1016/j.celrep.2022.110338
Ruf, I. K., Houmani, J. L., and Sample, J. T. (2009). Epstein-Barr virus independent dysregulation of UBP43 expression alters interferon-stimulated gene expression in Burkitt lymphoma. PLoS One 4 (6), e6023. doi:10.1371/journal.pone.0006023
Schneider, C., Kon, N., Amadori, L., Shen, Q., Schwartz, F. H., Tischler, B., et al. (2016). FBXO11 inactivation leads to abnormal germinal-center formation and lymphoproliferative disease. Blood 128 (5), 660–666. doi:10.1182/blood-2015-11-684357
Shen, J., Lin, X., Dai, F., Chen, G., Lin, H., Fang, B., et al. (2023). Ubiquitin-specific peptidases: players in bone metabolism. Cell Prolif. 56 (8), e13444. doi:10.1111/cpr.13444
Thapa, P., Shanmugam, N., and Pokrzywa, W. (2020). Ubiquitin signaling regulates RNA biogenesis, processing, and metabolism. Bioessays 42 (1), e1900171. doi:10.1002/bies.201900171
Toloczko, A., Guo, F., Yuen, H. F., Wen, Q., Wood, S. A., Ong, Y. S., et al. (2017). Deubiquitinating enzyme USP9X suppresses tumor growth via LATS kinase and core components of the hippo pathway. Cancer Res. 77 (18), 4921–4933. doi:10.1158/0008-5472.CAN-16-3413
Tu, R., Kang, W., Yang, M., Wang, L., Bao, Q., Chen, Z., et al. (2021). USP29 coordinates MYC and HIF1α stabilization to promote tumor metabolism and progression. Oncogene 40 (46), 6417–6429. doi:10.1038/s41388-021-02031-w
Wang, Z., Kang, W., You, Y., Pang, J., Ren, H., Suo, Z., et al. (2019). USP7: novel drug target in cancer therapy. Front. Pharmacol. 10, 427. doi:10.3389/fphar.2019.00427
Wei, T., Biskup, E., Rahbek Gjerdrum, L. M., Niazi, O., Ødum, N., and Gniadecki, R. (2016). Ubiquitin-specific protease 2 decreases p53-dependent apoptosis in cutaneous T-cell lymphoma. Oncotarget 7 (30), 48391–48400. doi:10.18632/oncotarget.10268
Wu, Y., Gu, H., Bao, Y., Lin, T., Wang, Z., Gu, D., et al. (2022a). USP7 sustains an active epigenetic program via stabilizing MLL2 and WDR5 in diffuse large B-cell lymphoma. Cell Biochem. Funct. 40 (4), 379–390. doi:10.1002/cbf.3702
Wu, Y. Y., Gu, H. Y., Bao, Y. H., Lin, T., Wang, Z. Y., Gu, D. H., et al. (2022b). USP7 sustains an active epigenetic program via stabilizing MLL2 and WDR5 in diffuse large B-cell lymphoma. Cell Biochem. Funct. 40 (4), 379–390. doi:10.1002/cbf.3702
Yang, X. D., Xiang, D. X., and Yang, Y. Y. (2016). Role of E3 ubiquitin ligases in insulin resistance. Diabetes Obes. Metab. 18 (8), 747–754. doi:10.1111/dom.12677
Yuan, T., Yan, F., Ying, M., Cao, J., He, Q., Zhu, H., et al. (2018). Inhibition of ubiquitin-specific proteases as a novel anticancer therapeutic strategy. Front. Pharmacol. 9, 1080. doi:10.3389/fphar.2018.01080
Zhan, M., Sun, X., Liu, J., Li, Y., Li, Y., He, X., et al. (2017). Usp7 promotes medulloblastoma cell survival and metastasis by activating Shh pathway. Biochem. Biophys. Res. Commun. 484 (2), 429–434. doi:10.1016/j.bbrc.2017.01.144
Zhang, H., Wang, D., Zhong, H., Luo, R., Shang, M., Liu, D., et al. (2015). Ubiquitin-specific protease 15 negatively regulates virus-induced type I interferon signaling via catalytically-dependent and -independent mechanisms. Sci. Rep. 5, 11220. doi:10.1038/srep11220
Zhao, C., Huang, R., Zeng, Z., Yang, S., Lu, W., Liu, J., et al. (2021). Downregulation of USP18 reduces tumor-infiltrating activated dendritic cells in extranodal diffuse large B cell lymphoma patients. Aging (Albany NY) 13 (10), 14131–14158. doi:10.18632/aging.203030
Zhong, M., Zhou, L., Fang, Z., Yao, Y. Y., Zou, J. P., Xiong, J. P., et al. (2021). Ubiquitin-specific protease 15 contributes to gastric cancer progression by regulating the Wnt/β-catenin signaling pathway. World J. Gastroenterol. 27 (26), 4221–4235. doi:10.3748/wjg.v27.i26.4221
Zhou, J., Wang, J., Chen, C., Yuan, H., Wen, X., and Sun, H. (2018). USP7: target validation and drug discovery for cancer therapy. Med. Chem. 14 (1), 3–18. doi:10.2174/1573406413666171020115539
Zhou, Q., Cheng, C., Wei, Y., Yang, J., Zhou, W., Song, Q., et al. (2020). USP15 potentiates NF-κB activation by differentially stabilizing TAB2 and TAB3. Febs J. 287 (15), 3165–3183. doi:10.1111/febs.15202
Nomenclature
USPs ubiquitin-specific peptidases.
DUBs deubiquitinases.
UPS ubiquitin–proteasome system.
DNA deoxyribonucleic acid.
DLBCL diffuse large B-cell lymphoma.
NF-κB nuclear factor Kappa B.
BCR B-cell receptor.
CTCL cutaneous T-cell lymphoma.
IFN interferon.
EBV Epstein–Barr virus.
LMP1 latent membrane protein 1.
GCB germinal center B-cell-like.
ABC activated B-cell-like.
HDM2 human double minute 2.
DAXX death-associated protein 6.
CDK4 cyclin-dependent kinase 4.
CDK6 cyclin-dependent kinase 6.
PCNA proliferating cell nuclear antigen.
EZH2 enhancer of zeste homolog 2.
siRNA small interfering RNA.
MAPK mitogen-activated protein kinase.
IFN interferon.
JAK1 Janus kinase 1.
CHK1 checkpoint kinase 1.
HIF1α hypoxia-inducible factor 1-alpha.
MLL2 mixed-lineage leukemia 2.
WDR5 WD repeat-containing protein 5.
OTUB1 OTU deubiquitinase.
HR homologous recombination.
AKT Ak strain transforming.
Mdm2 mouse double minute 2 homolog.
HDM2 human double minute 2.
Keywords: ubiquitin-specific peptidases, USPs, cancer, lymphoma, non-Hodgkin, Hodgkin
Citation: Samareh Salavatipour M, Tavakoli S, Halimi A, Tavoosi S, Baghsheikhi A-H, Talebi-Taheri A, Niloufari M, Salehi Z, Verdi J, Rahgozar S, Mosavi-Jarrahi A and Ahmadvand M (2024) Ubiquitin-specific peptidases in lymphoma: a path to novel therapeutics. Front. Pharmacol. 15:1356634. doi: 10.3389/fphar.2024.1356634
Received: 15 December 2023; Accepted: 14 October 2024;
Published: 27 November 2024.
Edited by:
Wen Huiwu, Shanghai Ocean University, ChinaReviewed by:
Ramcharan Singh Angom, Mayo Clinic Florida, United StatesDana-Lynn Koomoa-Lange, Western New England University, United States
Copyright © 2024 Samareh Salavatipour, Tavakoli, Halimi, Tavoosi, Baghsheikhi, Talebi-Taheri, Niloufari, Salehi, Verdi, Rahgozar, Mosavi-Jarrahi and Ahmadvand. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Alireza Mosavi-Jarrahi, cm1vc2F2aUB5YWhvby5jb20=; Mohammad Ahmadvand, bWFobWFkdmFuZEBzaW5hLnR1bXMuYWMuaXI=
†These authors have contributed equally to this work and share first authorship
 Maryam Samareh Salavatipour
Maryam Samareh Salavatipour Shirin Tavakoli
Shirin Tavakoli Aram Halimi
Aram Halimi Shima Tavoosi4
Shima Tavoosi4 Amir-Hossein Baghsheikhi
Amir-Hossein Baghsheikhi Javad Verdi
Javad Verdi Soheila Rahgozar
Soheila Rahgozar Alireza Mosavi-Jarrahi
Alireza Mosavi-Jarrahi Mohammad Ahmadvand
Mohammad Ahmadvand