
95% of researchers rate our articles as excellent or good
Learn more about the work of our research integrity team to safeguard the quality of each article we publish.
Find out more
REVIEW article
Front. Pediatr. , 20 March 2023
Sec. Neonatology
Volume 11 - 2023 | https://doi.org/10.3389/fped.2023.1114587
This article is part of the Research Topic Bronchopulmonary Dysplasia: Latest Advances View all 13 articles
Background: Bronchopulmonary Dysplasia (BPD) is a chronic condition that affects preterm infants and is associated with long-term complications. Haemodynamic effects of BPD can lead to right ventricular (RV) dysfunction.
Objective: To synthesise and map the evidence of echo parameters used in identifying RV dysfunction in the first two weeks-after-birth (WAB) of preterm infants with early BPD.
Information Sources: This scoping review included the databases: Medline, CINAHL, PubMed, EMBASE, Scopus, ProQuest, Web of Science, Cochrane Library, JBI Evidence-Based Practise and Gray Literature.
Search Strategy: The search utilised Boolean operators and descriptors registered in Medical Subject Headings.
Inclusion and exclusion criteria: Included were studies utilising echo parameters to examine RV function in preterm infants with early BPD in the first two WAB.
Synthesis of results: The results are presented as a map of the extracted findings in a tabular format with a narrative summary.
Results: Eight studies were included. Differences were observed in the number and timing of echo scans performed in the first two WAB and the variations in the echo parameters used to compare preterm infants with and without early BPD. Only echo scans performed at the end of the first WAB, demonstrated significant differences in the echo parameters measurements between preterm infants with and without BPD. Studies using RV Myocardial Performance Index (MPI) to identify RV-dysfunction associated with early BPD demonstrated similar findings. The Pulsed-Wave Doppler technique identified differences in RV-MPI between preterm infants with and without BPD, while Tissue-Doppler-Imaging did not demonstrate similar results. Speckle tracking can measure strain (S) and strain rate (SR) and diagnose RV-dysfunction. However, the findings of studies that utilised speckle tracking varied. Finally, two of the included studies added blood tests to their diagnostic model of early BPD, which was able to demonstrate significant differences in blood test results between BPD-affected and control preterm infants.
Conclusion: BPD could adversely affect the myocardium function of the RV; these negative influences can be captured in the first two WAB. However, there are still knowledge gaps regarding the appropriate number, timing and the most suitable echo parameters to assess RV function.
Bronchopulmonary Dysplasia (BPD) was first described in 1967 (1). It affects the immature lungs of preterm infants. Preterm infants born before 32 weeks of gestation are at a greater risk of developing BPD, especially those requiring respiratory support with higher oxygen requirements (2). The incidence rate of this disease remains high; a moderate and severe form of BPD affects almost a third of the preterm infants born before 32 weeks of gestation (3). The incidence rate of BPD is expected to continue to be elevated, especially when the viability threshold is reduced to 22 weeks of gestation, while more at-risk extreme preterm infants are expected to survive (4).
Bronchopulmonary Dysplasia negatively affects the normal growth and development of the immature lungs’ alveoli and vascular bed through complex processes, which can reduce gas exchange surfaces and subsequently result in a decline in pulmonary function (5). The vascular pathogenesis theory hypothesises that as the premature heart and the premature lungs' vascular bed are closely interlinked, a negative effect on one of them will also be reflected on the other. Abnormally affected lungs by early BPD will also impair angiogenesis of the vascular bed of the lungs and the formation of pulmonary vascular disease (PVD), which can adversely affect the function of the right ventricle (RV) of the heart.
The pulmonary vascular remodelling results in a rise in the vascular tone, altered reactivity, vasoconstriction, and increased pulmonary vascular resistance (6). These histologic changes can increase the RV afterload pressure. Subsequently, the chronic increase in RV afterload pressure and hypoxic episodes can result in RV dysfunction, hypertrophy and, in severe cases, failure (7). Furthermore, severe forms of BPD are associated with a higher incidence of pulmonary arterial hypertension (8), which results from an increase in pulmonary arterial pressure and is associated with significant co-morbidities and high mortality rates (9).
The literature showed that the pathological effects of early BPD and respiratory insufficiency could manifest as early as day 7 of postnatal life (10). Data from 1,735 infants born between 23 and 30 weeks of gestational age showed that the proportion of these preterm infants needing oxygen decreases from birth to day 7 of postnatal life, followed by a steep rise in the number of infants requiring oxygen in the same cohort at the start of the second week postnatal (10). Additionally, studies, albeit limited, such as by Czernik et al., 2012 (11), demonstrated that the negative effect of PVD associated with early BPD on the function of the RV is present as early as the first two weeks after birth.
To address the gap in knowledge and provide state-of-the-art current knowledge, the aim of this scoping review is to identify, synthesise and map the evidence of echo parameters used in identifying dysfunction of the RV in the first two weeks of postnatal life of preterm infants with early BPD. This review will examine the echo parameters in preterm infants born before 32 weeks of gestation since these infants are at higher risk of developing BPD. In addition, the review will include studies which performed echo scans in the first two weeks of postnatal life as it is the period when early BPD starts to manifest clinically. Specifically, the scoping review questions were: (i) What techniques are used to capture echo images in preterm infants? (ii) When are the echo scans performed in the first two weeks after birth? (iii) What echo parameters are used to assess the haemodynamic effects of early BPD on the function of the right ventricle? and (iv) How are the echo parameters measured and analysed?
The preliminary literature search on 01 April 2022 in Medline (OVID), Cochrane Library, PROSPERO and the JBI Evidence Synthesis Database revealed no scoping or systematic review available or currently being developed about this subject.
The proposed scoping review is conducted according to Joanna Briggs Institute (JBI) methodology (Peters M. D. J., 2020). Also, this scoping review used the reporting guideline “Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews (PRISMA-ScR): checklist and explanation” (12).
Participants: The scoping review included studies that examined the first two weeks of postnatal life of preterm infants born before 32 weeks of gestation.
Concept: The review included studies that examined the haemodynamic effects of PVD associated with early BPD on the RV function through the analyses of the echo parameters. The included studies should have at least one echo scan performed in the first two weeks after the birth of the participating preterm infants. In addition, eligible studies should have compared the data collected from echo parameters analyses in preterm infants with and without BPD.
Context: The review included studies that recruited preterm infants admitted to a neonatal intensive care unit.
This scoping review considered all study designs, including experimental and quasi-experimental studies. Randomised controlled trials, non-randomised controlled trials, before and after studies and interrupted time-series studies were assessed for eligibility. Any systematic reviews that meet the inclusion criteria were considered, but none were retrieved. The review also considered analytical observational studies, such as prospective and retrospective cohort studies, case-control studies and analytical cross-sectional studies. There were no limitations regarding the date of the publication.
Papers were excluded if they did not fit in the conceptual framework of this review. In addition, studies were excluded if they used different imaging modalities, such as Magnetic Resonance Imaging or Computed Tomography or were not available in full text. Studies that did not assess the RV function or echo scans performed after the first two weeks after birth were also excluded. Studies were excluded if they were unavailable in English or were animal studies.
The selected text words and index terms, such as preterm infants, right ventricular function, bronchopulmonary dysplasia, and echocardiography, were utilised to formulate a full search strategy (Table 1).
A comprehensive search strategy was followed and consisted of three steps.
First step: An initial limited search of two online databases, Medline (OVID) and CINHAL Plus Full text (EBSCOhost), was conducted to allocate related articles. The examination of the relevant articles resulted in the identification of the text words included in the titles and the abstracts and the index terms related to these articles to guide the subsequent detailed search as per the advice of a research librarian.
Second step: The full search strategy was applied to the included databases with the identified keywords and index terms. The descriptors registered in the Medical Subject Headings (MeSH) were used wherever possible. The synonyms were combined with the Boolean operator “OR” while the groups of words were combined with the operator “AND” (Table 1). The following databases were searched: Medline (OVID), CINAHL Plus with Full Text (EBSCOhost), PubMed, EMBASE, Scopus, ProQuest, Web of Science, Cochrane Library, JBI Evidence Based Practise (EBP) and Gray Literature (British Library, google scholar & EThOS).
Third step: A reference list containing all the identified studies was formed. There were no scoping nor systematic reviews identified.
A full search was performed by two reviewers (WM and JML). Any unresolved dispute was discussed with a third reviewer (EN).
The studies were selected from the included databases. All the identified citations were uploaded into EndNote 20 (Clarivate Analytics, PA, USA), followed by removing duplicates. Then, studies were selected by two reviewers (WM and JML) in two stages; titles and abstracts review; and full-text review, against the inclusion criteria. A detailed assessment of the full text of the selected articles against the inclusion criteria was performed by two independent reviewers (WM and JML). Any disagreements were discussed and resolved by both reviewers.
Two independent reviewers (WM and JL) performed the data extraction process using the tool developed by the reviewers for this purpose. The data extraction tool contained details of the population, concept, context, methodology and relevant findings. No modifications to the data extraction tool were performed.
The final scoping review full report of the search results is presented in the PRISMA flow diagram (Figure 1). There were 501 records identified from 12 databases. Sixty-two duplicates were removed, leaving 439 records eligible for the first screening stage, i.e., titles and abstracts were screened. After the exclusion of 415 records, only 24 papers were eligible for the second stage of full-text screening. Sixteen articles were excluded (Figure 1), and eight studies were included in the final critical appraisal and analysis.
Data were extracted from the full texts of the eight included studies and detailed into two tables (Tables 2, 3). Table one described the studies' methodologies, while table two included details about the echo scans' timing, echo parameters analyses and the key findings. The results are presented in narrative descriptions and mapping of the data.
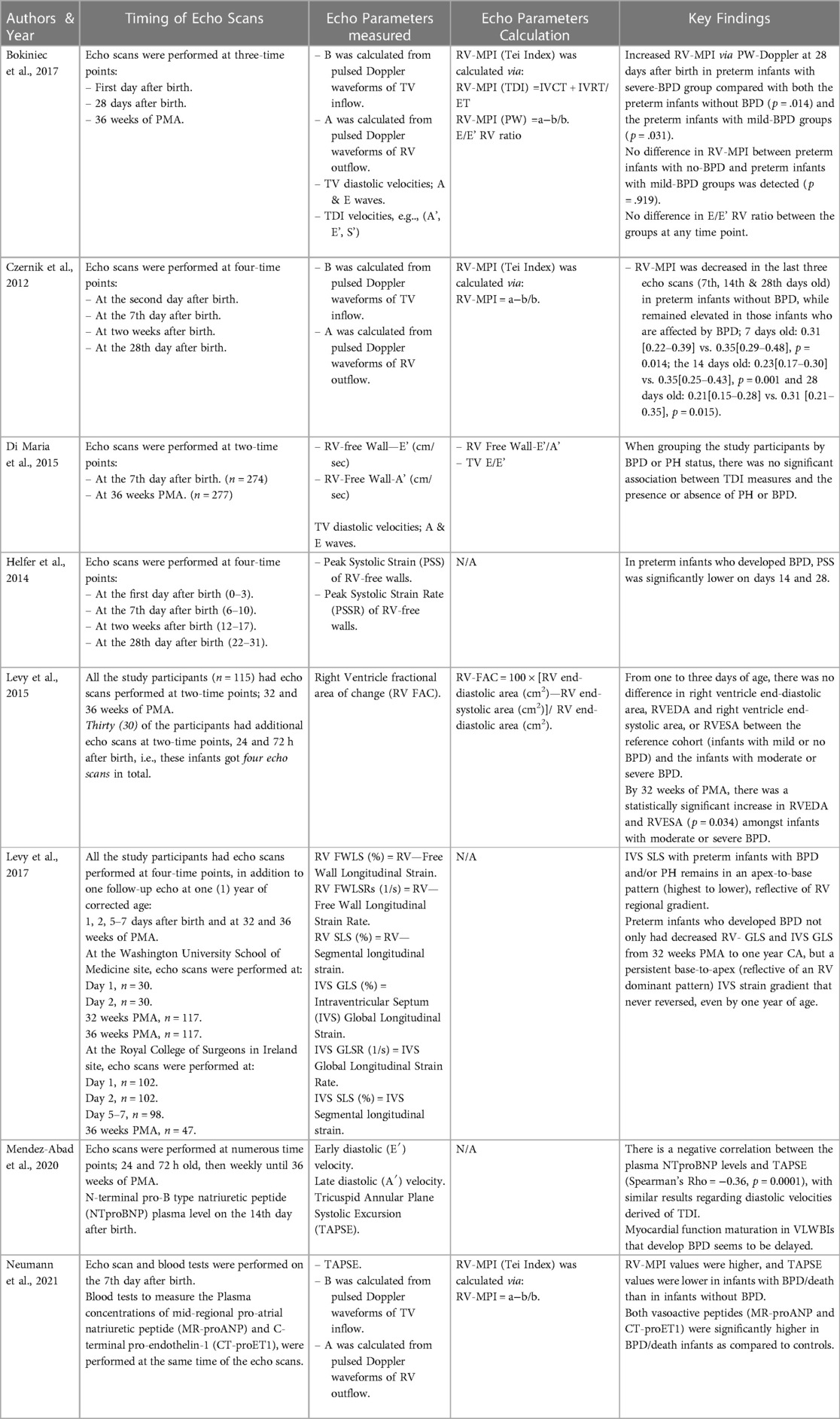
Table 3. Selected studies details related to authorship, the timing, analysis and the key findings of the echo scans. .
The eight included studies were conducted in the USA and European countries. All studies were conducted in tertiary perinatal centres. Only four studies examined exclusively preterm infants born before 32 weeks of gestation (11, 13–15) (Table 1). The study by Helfer et al., 2014, included preterm infants born at 32 weeks gestation as the recruitment was per birth weight rather than gestational age (16). Another study included preterm infants with a higher gestation age, and the birth weight needed to be within a specific range (≤34 weeks gestation and birth weight between 500 and 1,250 grams) (17). The other two studies by Levy and colleagues focused on recruiting preterm infants with lower gestational age (23–28 weeks of gestation) (18, 19).
Different definitions to diagnose BPD were used in the selected eight studies. Czernik et al., 2012, diagnosed preterm infants with BPD based on their oxygen requirement to maintain pre-ductal arterial saturations of 92% at 36 weeks PMA (20, 21). Levy et al., 2017, utilized a modified Shennan definition (22). While the remaining six studies used the definition set in the NIH workshop (23). There is a lack of the definition of an early BPD, i.e., during the first two weeks after birth, in the selected studies.
Several techniques were used to capture the echo images in the selected studies, such as 2D echo images, Pulsed wave (PW) Doppler, Tissue Doppler Imaging (TDI), 2D speckle tracking and M-mode.
The studies' timing and frequency of echo scans varied (Table 2). Three studies performed one echo scan within the first two weeks after birth (13, 15, 17); one study had the echo scans performed on the first day after birth (DAB) (17), and the other two studies performed the echo scans at the 7th DAB, respectively (13, 15). The remaining five studies had several echo scans performed within the first two weeks after birth (11, 14, 16, 18, 19). There were variations between the studies regarding the timing when the echo scans were performed in the first 14 days after birth; Czernik et al., 2012 trial, the echo scans were performed on day 2, 7, 14 after birth (11); Helfer et al., 2014 study team performed the echo scans on day 1, 7, 14 after birth (16); Levy et al., 2015 study team performed the echo scans on day 1 and day 7 after birth (18); Levy et al., 2017 study teams performed the echo scans on day 1, 2, 5 and 7 after Birth (19); finally, Mendez-Abad et al., 2020 team per, the echo scans were performed on day 1, 3, 7, 14 after birth (14).
The critically appraised studies utilised different echo parameters to assess the function of the RV in healthy preterm infants (controls) and the ones affected by BPD (cases); RV-myocardial performance index (MPI), RV strain (S) and strain rate (SR), RV fractional area of change (RV-FAC), TDI systolic- and diastolic-velocities and tricuspid annular plane systolic excursion (TAPSE).
Studies utilising RV-MPI to assess RV function, the calculation of RV-MPI was performed by using one of the following two equations:
– RV-MPI calculation in TDI echo images: RV-MPI (TDI) = IVCT + IVRT/ET.(IVCT = Isovolumic Contraction Time; IVRT = Isovolumic Relaxation Time; ET = Ejection Time)
– RV-MPI calculation in PW echo images: RV-MPI (PW) = a−b/b.(a = the measurement between cessation and onset of the tricuspid valve inflow; b = the ejection time of the RV outflow)
Four studies showed a delay in the normal maturation of the RV-MPI, i.e., persistently raised RV-MPI in BPD-affected preterm infants in comparison to the controls. The differences in the RV-MPI between the two groups (preterm infants with and without early BPD) were detected in the echo scans performed after the first three days after birth (11, 13–15). In addition, Neumann et al., 2021, demonstrated that TAPSE is lower in BPD-affected preterm infants (15).
Other findings were identified when examining all the included studies. Neumann et al., 2021, demonstrated that TAPSE is lower in BPD-affected preterm infants (15). Levy et al., 2015, showed differences in the RV-FAC measurements between controls and BPD-affected preterm infants when assessed at 32 weeks of PMA echo scans (18). Two studies utilising S and SR also demonstrated statistically significant differences in these measurements between their controls and the cases of preterm infants (16, 19). However, the study by Helfer et al., 2014, demonstrated that the differences in the S & SR measurements between controls and BPD-affected preterm infants would start to manifest in the echo scans at day 14 after birth while the study of Levy et al., 2017, the S & SR differences between the controls and the cases of preterm infants with BPD, did not manifest till the echo scan at 32 weeks of PMA (16, 19).
In addition to using echo parameters, two of the eight studies performed blood tests. Mendez-Abad et al., 2020, analysed N-terminal pro-B type natriuretic peptide (NTproBNP) plasma level on day 14 after birth (14). Neumann et al., 2021, analysed the plasma concentrations of mid-regional pro-atrial natriuretic peptide (MR-proANP) and C-terminal pro-endothelin-1 (CT-proET1) on day 7 after birth (15). Both studies demonstrated a statistically significant difference in the plasma levels of the selected tests between the controls and BPD-affected preterm infants.
There were methodological variations between the selected studies. There are differences in the number and the timing of echo scans performed in the first two weeks of postnatal life, together with the variations in the echo parameters used to compare the preterm infants as controls and the preterm infants affected by BPD.
Echo scans performed in the first three days after birth did not demonstrate a difference in the echo parameters measurements between the control group and preterm infants with early BPD. In comparison, significant differences in the echo parameters measurements between the controls and preterm infants with BPD were seen in the echo scans performed at the end of the first week after birth and the subsequent weeks (11, 13, 15, 16). Similarly, the study by Levy et al., 2015, showed that RV-FAC measurements in the first three days after birth did not differ between preterm infants without BPD and the ones who have BPD (18).
Studies using RV-MPI to identify RV dysfunction associated with early BPD have similar findings. Bokiniec et al., 2017, showed that PW-Doppler could identify the differences in RV-MPI between controls and preterm infants affected by early BPD, while TDI could not demonstrate differences in RV-MPI between preterm infants with and without BPD (13). The trials conducted by Czernik et al., 2012, and Neumann et al., 2021 showed similar results when RV-MPI via PW-Doppler could identify RV dysfunction in preterm infants with early BPD (11, 15). While Mendez et al. 2020 findings demonstrated that RV-MPI and diastolic velocities via TDI can be still a useful tool since it could detect the cardiac maturational changes in preterm infants. The same study showed that diastolic velocities via TDI are capable of recognising RV dysfunction in infants with early BPD (14).
Despite the limitations of PW-Doppler in calculating RV-MPI, e.g., it utilises the measurements from different cardiac cycles, three of the eight selected studies used PW-Doppler and were able to diagnose RV dysfunction in preterm infants with early BPD. On the other hand, despite TDI being a valuable and practical tool in assessing RV's systolic and diastolic function, TDI was unable to identify the RV dysfunction (13, 17). This could be explained by the inherent limitations of TDI, which is angle-dependent and influenced by the global cardiac motion and the inability to differentiate between passive and active motion (24). In addition, velocities and displacements depend on the cardiac sizes; hence, larger hearts have higher velocities and displacements. Therefore, it is crucial to normalise the TDI measurements according to the cardiac size (25). None of the studies that utilised TDI technique normalised the cardiac TDI measurements, which might negatively affect the ability of these studies to demonstrate a significant difference in the TDI measurements between controls and cases.
Speckle tracking can be used to measure S and SR and diagnose RV dysfunction. However, the findings of the studies that utilised speckle tracking in this review varied. A study by Levy et al., 2017, could not diagnose the RV dysfunction in the echo scans performed at day 1, 2, and 5 to 7 after birth (19). In contrast, a study by Helfer et al., 2014, demonstrated a significant difference in the S and SR between preterm infants with and without BPD when echo scans were performed at day 14 after birth (16). The findings of these two studies demonstrate that results can vary even when a reliable technique such as speckle tracking was used. This might be well related to the timing of the echo scans, i.e., if the echo scan were performed too soon, it might not capture the hemodynamic changes related to RV dysfunction that is associated with early BPD.
Furthermore, two of the selected eight studies added blood tests to their diagnostic model of early BPD (14, 15). Both studies demonstrated that adding specific blood tests would enhance the diagnostic ability of RV dysfunction associated with early BPD (14, 15).
Although, adding a specific blood test to a diagnostic model might enhance its diagnostic ability, it might also have a negative impact on its applicability in many perinatal centres worldwide, especially in developing countries, due to, for example, the cost and unavailability of these blood tests. Likewise, it will negate the idea of having a diagnostic model based on a practical, applicable and non-invasive test such as an echo scan.
The primary strength of this review was its broad literature search. The process of synthesising the scientific evidence was transparent and systematic in identifying and mapping the evidence related the use of echocardiography to diagnose RV dysfunction associated with early BPD. Nevertheless, as this review designed as a systematic scoping review, it did not assess the quality of the evidence, so it does not provide the scientific basis to inform clinical decision making. Finally, language restrictions may have led to the exclusion of a few studies.
This scoping review showed the need to develop a diagnostic model based on a non-invasive echo scan. The review demonstrated the emergence of unanswered questions regarding the practicalities of when and how many echo scans are needed and which cardiac parameter is required to diagnose early BPD in preterm infants.
BPD will adversely affect the myocardium function of the RV; these negative influences can be captured in the first two weeks of postnatal life (15, 17). However, there are still knowledge gaps regarding the appropriate number, timing of the echo scans and the most suitable cardiac parameters to assess RV function.
WM: contributed to the main design and detailed concept and discussion of this review article; he drafted the first manuscript. JML: as a senior author revised the manuscript and added details to it. EN and JH revised the manuscript and added details. All authors contributed to the article and approved the submitted version.
Janice Parker-Elliott, research librarian at the Medical Library, University Hospital Plymouth NHS Trust and Samantha Brown, Information Specialist, Library & Digital Support, Charles Seale-Hayne Library, University of Plymouth are thanked by the authors for their guidance and support in the development of the search strategy.
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
1. Northway WH Jr., Rosan RC, Porter DY. Pulmonary disease following respirator therapy of hyaline-membrane disease. Bronchopulmonary dysplasia. N Engl J Med. (1967) 276(7):357–68. doi: 10.1056/NEJM196702162760701
2. Higgins RD, Jobe AH, Koso-Thomas M, Bancalari E, Viscardi RM, Hartert TV, et al. Bronchopulmonary dysplasia: executive summary of a workshop. J Pediatr. (2018) 197:300–8. doi: 10.1016/j.jpeds.2018.01.043
3. NNAP, National Neonatal Audit Programme, Annual report on 2019 data. 2020, Royal College of Paediatrics and Child Health
4. Siffel C, et al. Global incidence of bronchopulmonary dysplasia among extremely preterm infants: a systematic literature review. J Matern Fetal Neonatal Med. (2021) 34(11):1721–31. doi: 10.1080/14767058.2019.1646240
5. Alvira CM. Aberrant pulmonary vascular growth and remodeling in bronchopulmonary dysplasia. Front Med. (2016) 3:21. doi: 10.3389/fmed.2016.00021
6. Ambalavanan N, Mourani P. Pulmonary hypertension in bronchopulmonary dysplasia. Birth Defects Res Part A Clin Mol Teratol. (2014) 100(3):240–6. doi: 10.1002/bdra.23241
7. Mourani PM, Mullen M, Abman SH. Pulmonary hypertension in bronchopulmonary dysplasia. Prog Pediatr Cardiol. (2009) 27(1-2):43–8. doi: 10.1016/j.ppedcard.2009.09.007
8. Mirza H, Ziegler J, Ford S, Padbury J, Tucker R, Laptook A. Pulmonary hypertension in preterm infants: prevalence and association with bronchopulmonary dysplasia. J Pediatr. (2014) 165(5):909. doi: 10.1016/j.jpeds.2014.07.040
9. Seth SA, Soraisham AS, Harabor A. Risk factors and outcomes of early pulmonary hypertension in preterm infants. J Matern Fetal Neonatal Med. (2018) 31(23):3147–52. doi: 10.1080/14767058.2017.1365129
10. Bancalari , Claure N, Jobe AH, Laughon MM. Chapter 6—Definitions and Diagnostic Criteria of Bronchopulmonary Dysplasia: Clinical and Research Implications,. Third Edition ed. The Newborn Lung 2019: Elsevier.
11. Czernik C, Rhode S, Metze B, Schmalisch G, Bührer C. Persistently elevated right ventricular index of myocardial performance in preterm infants with incipient bronchopulmonary dysplasia. PloS One. (2012) 7(6):e38352. doi: 10.1371/journal.pone.0038352
12. Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA Extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. (2018) 169(7):467–73. doi: 10.7326/M18-0850
13. Bokiniec R, Wlasienko P, Borszewska-Kornacka M, Szymkiewicz-Dangel J. Echocardiographic evaluation of right ventricular function in preterm infants with bronchopulmonary dysplasia. Echocardiography. (2017) 34(4):577–86. doi: 10.1111/echo.13489
14. Mendez-Abad P, Zafra-Rodriguez P, Lubian-Lopez S, Benavente-Fernandez I. Myocardial function maturation in very-low-birth-weight infants and development of bronchopulmonary dysplasia. Front Pediatr. (2020) 7:556. doi: 10.3389/fped.2019.00556.32010652
15. Neumann RP, Schulzke SM, Pohl C, Wellmann S, Metze B, Minke AK, et al.. Right ventricular function and vasoactive peptides for early prediction of bronchopulmonary dysplasia. PLoS One. (2021) 16(9):1–12. doi: 10.1371/journal.pone.0257571
16. Helfer S, Schmitz L, Bührer C, Czernik C. Tissue Doppler-derived strain and strain rate during the first 28 days of life in very low birth weight infants. Echocardiography. (2014) 31(6):765–72. doi: 10.1111/echo.12463
17. Di Maria MV, Younoszai AK, Sontag MK, Miller JI, Poindexter BB, Ingram DA, et al. Maturational changes in diastolic longitudinal myocardial velocity in preterm infants. J Am Soc Echocardiogr. (2015) 28(9):1045–52. doi: 10.1016/j.echo.2015.04.016
18. Levy PT, Dioneda B, Holland MR, Sekarski TJ, Lee CK, Mathur A, et al. Right ventricular function in preterm and term neonates: reference values for right ventricle areas and fractional area of change. J Am Soc Echocardiogr. (2015) 28(5):559–69. doi: 10.1016/j.echo.2015.01.024
19. Levy PT, El-Khuffash A, Patel MD, Breatnach CR, James AT, Sanchez AA, et al. Maturational patterns of systolic ventricular deformation mechanics by two-dimensional speckle-tracking echocardiography in preterm infants over the first year of age. J Am Soc Echocardiogr. (2017) 30(7):685. doi: 10.1016/j.echo.2017.03.003
20. Sahni R, Ammari A, Suri MS, Milisavljevic V, Ohira-Kist K, Wung JT, et al. Is the new definition of bronchopulmonary dysplasia more useful? J Perinatol. (2005) 25(1):41–6. doi: 10.1038/sj.jp.7211210
21. Shennan AT, Dunn MS, Ohlsson A, Lennox AK, Hoskins EM. Abnormal pulmonary outcomes in premature infants: prediction from oxygen requirement in the neonatal period. Pediatrics. (1988) 82(4):527–32. doi: 10.1542/peds.82.4.527
22. Poindexter BB, Feng R, Schmidt B, Aschner JL, Ballard RA, Hamvas A, et al. Comparisons and limitations of current definitions of bronchopulmonary dysplasia for the prematurity and respiratory outcomes program. Ann Am Thorac Soc. (2015) 12(12):1822–30. doi: 10.1513/AnnalsATS.201504-218OC
23. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. (2001) 163(7):1723–9. doi: 10.1164/ajrccm.163.7.2011060
24. Mittal S. Basics of tissue Doppler revisited. J Indian Acad Echocardiography Cardiovascular Imaging. (2017) 1(2):126–32. doi: 10.4103/jiae.jiae_34_17
Keywords: preterm infants, right ventricular function, bronchopulmonar dysplasia, echocardiogaphy, haemodynamic effects, scoping review
Citation: Muhsen W, Nestaas E, Hosking J and Latour JM (2023) Echocardiography parameters used in identifying right ventricle dysfunction in preterm infants with early bronchopulmonary dysplasia: A scoping review. Front. Pediatr. 11:1114587. doi: 10.3389/fped.2023.1114587
Received: 2 December 2022; Accepted: 27 February 2023;
Published: 20 March 2023.
Edited by:
Xiaoguang Zhou, Nanjing Children's Hospital, ChinaReviewed by:
Benjamim Ficial, Integrated University Hospital Verona, Italy© 2023 Muhsen, Nestaas, Hosking and Latour. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wisam Muhsen d2lzYW0ubXVoc2VuQHBseW1vdXRoLmFjLnVr
Specialty Section: This article was submitted to Neonatology, a section of the journal Frontiers in Pediatrics
Disclaimer: All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.
Research integrity at Frontiers

Learn more about the work of our research integrity team to safeguard the quality of each article we publish.