- 1Division of Obstetrics & Gynecology, KK Women’s and Children’s Hospital, Singapore, Singapore
- 2Duke-NUS Medical School, Singapore, Singapore
- 3Endocrinology Service, KK Women’s and Children’s Hospital, Singapore, Singapore
- 4Lee Kong Chian School of Medicine, Nanyang Technological University, Singapore, Singapore
- 5Department of Reproductive Medicine, KK Women’s and Children’s Hospital, Singapore, Singapore
- 6Department of Nutrition and Dietetics, KK Women’s and Children’s Hospital, Singapore, Singapore
- 7Department of Pediatrics, KK Women’s and Children’s Hospital, Singapore, Singapore
- 8Physical Education & Sports Science, National Institute of Education, Nanyang Technological University, Singapore, Singapore
- 9Department of Neonatology, KK Human Milk Bank, KK Women’s and Children’s Hospital, Singapore, Singapore
Introduction: Research on early childhood caregiver feeding practices and eating behaviors is limited, especially within Asian populations. This study examined these practices across key feeding domains of variety, autonomy, and mealtime setting and timing, stratified by three age groups: 0 to <7 months, 7 to <13 months, and 13 to <36 months.
Methods: A cross-sectional survey of 1,307 caregivers from a multi-ethnic population in Singapore captured demographic data, feeding practices, child eating behaviors, and caregivers’ knowledge, attitudes, and practices. One-way analysis of variance (ANOVA), independent T-tests and the chi-square test were used to assess feeding practices and eating behaviors across age groups.
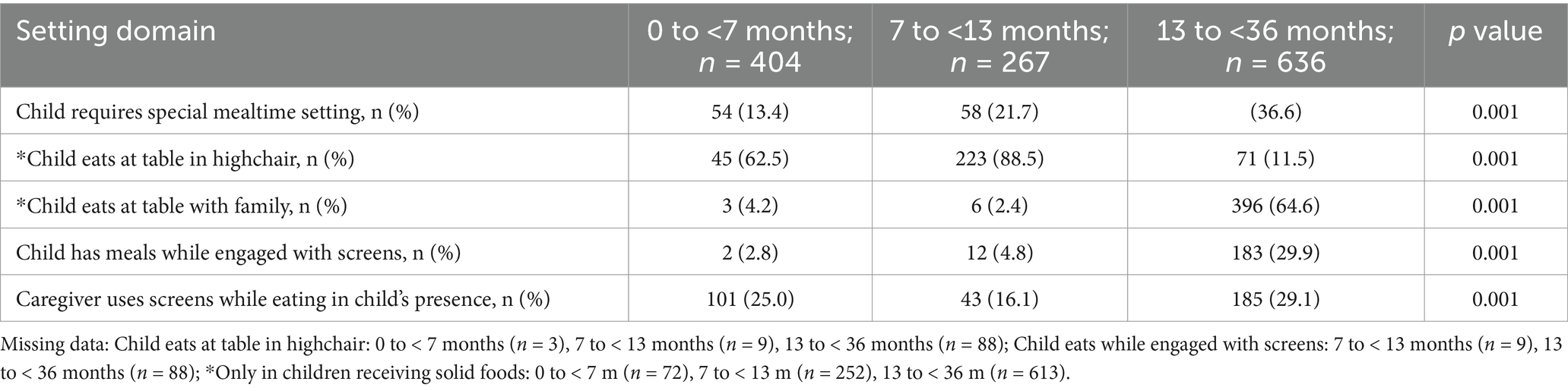
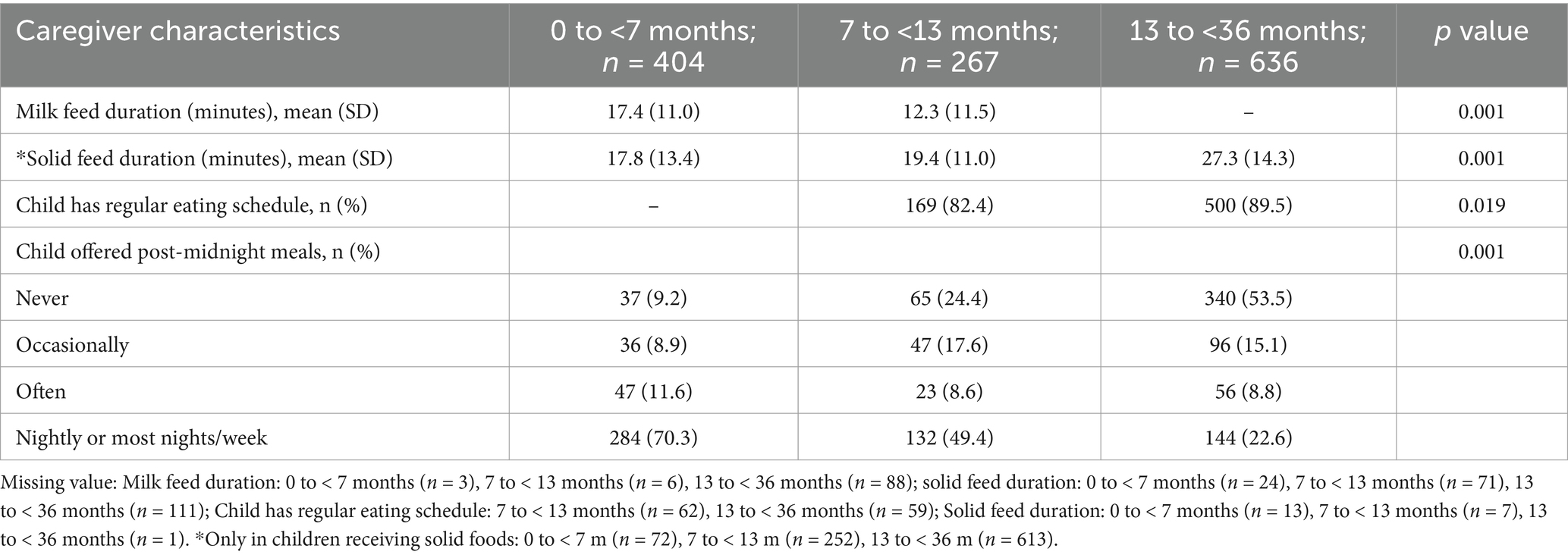
Results: Regarding dietary variety, 14.8 and 6.1% of infants aged 7 to <13 months were offered three or fewer food groups frequently and daily, respectively. Additionally, 11.9% of infants were receiving processed foods often. At this age, only 1.0% of infants were consuming sugar-sweetened beverages (SSBs) often, while 2.0% consumed them daily. Among older children (aged 13 to <36 months), 8.1% were offered a limited variety of three food groups, while 4.5% were offered fewer than three. In contrast, a significantly higher proportion frequently consumed processed foods (24.0%) and sugar-sweetened beverages (25.2%; p < 0.05). In terms of autonomy, only 75.4% of infants (7– < 13 months) and 89.5% of older children (13– < 36 months) were able to self-feed. Caregivers of older children (13– < 36 months) were less likely to recognize hunger and satiety cues compared to those of infants (0–< 13 months; p < 0.05). Older children (13– < 36 months) also more frequently required special mealtime settings (36.6%), viewed screens during meals (29.9%), and were less likely to be offered post-midnight meals nightly (22.6% compared to infants; 70.3%; 0–< 13 months; p < 0.05).
Conclusion: These findings underscore the need for culturally tailored educational interventions to improve suboptimal feeding practices in children under three in Singapore’s multiethnic population.
Introduction
Caregiver feeding practices and early childhood eating behaviors are fundamental for a child’s healthy growth, development, and shaping of life-long (1, 2) healthy eating behaviors and dietary patterns (3). Infants and toddlers are key targets (4) with early childhood feeding practices implicated in programming lifelong risks for non-communicable diseases like obesity, diabetes, heart disease, and certain cancers (5, 6). Caregivers play a central role in shaping eating behaviors through optimal feeding practices early in life, determining what, when, and how much children eat (7). The literature identifies four key domains that significantly impact early childhood nutrition: variety (8, 9), autonomy (10–12), setting (13–15), and timing (16–21), all of which help shape children’s dietary habits and overall health.
Early exposure to diverse flavors and textures during the appropriate timing of solid food introduction (16) fosters the acceptance of healthy foods (22) and builds habits that often persist into later life (23), highlighting the importance of varied food access in early childhood (8, 9). Dietary variety is associated with a better nutritional profile (24, 25) essential to achieve adequate coverage of macro- and micronutrient needs (8), and reduced food fussiness at later ages (26). In addition, an authoritative feeding style which promotes child autonomy within structured boundaries, supports optimal self-regulation in eating (12). Evidence suggests that this approach where caregivers decide when, where, and what food is offered, while children decide if and how much to eat, best fosters children’s ability to recognize hunger and fullness cues, consumption of a variety of food and achieve a nutritionally adequate diet (27). In contrast, relying solely on parental cues may undermine children’s self-regulation of food intake, increasing the risk of overeating and weight gain (10).
Children’s eating behaviors are also shaped within the family context, with the mealtime setting playing a critical role. Parental monitoring and consistent family mealtime routines during early childhood foster a supportive food environment that can significantly improve children’s overall diet quality (28). Studies show that frequent family meals are linked to healthier eating behaviors in children, including higher fruit and vegetable intake (29), and reduced risk of disordered eating (30). It also matters whether parents eat the same food as their children, as role-modeling of this behavior has been linked to lower levels of food fussiness, greater food enjoyment in children (13) and heathier dietary intake in children (31, 32). In contrast, factors like eating away from the dining table and mealtime distractions (e.g., screen time viewing) are associated with feeding problems (14), higher intake of ultra processed foods (15), sweets and desserts, sugar sweetened beverage consumption in young children (33), higher total energy intake and an increased risk for obesity (34).
The timing of child feeding practices includes critical components such as, the pace at which a child eats (18–20, 35), and the schedule of meal timings (36). The World Health Organization recommends exclusive breastfeeding for the first 6 months of life, with continued breastfeeding for up to 2 years or beyond (16). Complementary foods should be introduced in a timely manner, starting at 6 months of age. Some evidence suggests that introducing complementary foods too early (at or before 4 months) may increase the risk of childhood overweight (37) compared to introduction at 4–6 months or after 6 months. Eating rate has also been identified as a marker for future weight and fat gain (20) where in preschoolers, eating rate at age 4 correlated positively with weight and adiposity at age 6, independent of maternal weight, linking rapid eating with excessive weight gain (19). Furthermore, recent evidence indicates that the timing of food intake may influence body weight regulation (36). Observational studies in children indicate that meal timing, particularly consuming a large proportion of energy later in the day and into the evening, may negatively affect weight status. For example, studies have shown that decreasing nighttime feedings for infants aged 6–12 months aids in managing calorie intake, supporting healthy growth (38, 39). Furthermore, infants consuming more calories at night (after 7 pm) than during the day at 12 months have been associated with greater body fat gain and an increased risk of overweight and obesity by 24 months (40).
Despite substantial evidence, implementing healthy feeding practices in multi-ethnic Asian settings continues to face persistent challenges and gaps, often influenced by factors such as ethnicity, cultural misconceptions (41, 42) and the role of primary caregivers contributing to suboptimal practices (43, 44) that may differ from those seen in Western contexts. Building on these identified gaps, there is a need to further investigate and understand caregiver feeding practices and children’s eating behaviors in these populations. Thus, this study aims to describe caregiver feeding practices, and eating behavior in children in Singapore, focusing on three distinct age groups: infants aged 0 to <7 months, infants aged 7 to <13 months, and toddlers aged 12 to <36 months. The study emphasizes key feeding dimensions, including variety, autonomy, setting, and timing, within a multi-ethnic Asian population.
Methods
Study sample
This study employed a cross-sectional design, enlisting caregivers as part of the Integrated Variety Autonomy Setting Timing feeding practices study in infants’ and toddlers’ (I-VAST) study. A convenience sampling method was employed to select caregivers from various study sites in Singapore. Eligible caregivers were individuals who were either Singaporean or permanent residents, caring for children aged 0 to below 36 months of age, and were able to understand English. Caregivers were excluded from the study if their children did not fall within the specified age range or if they were unable to understand English. Age-appropriate surveys were developed, tailored to accommodate each specific age group (Supplementary Figure S1). Responses were collected from children in three age groups: (1) 0–<7 months, (2) 7–<13 months, and (3) 13–<36 months. The survey was distributed via a QR code, targeting eligible caregivers with children aged 0 to <36 months. Participation in the survey was considered as implied consent upon accessing the QR code and completing the survey. All participants will access the survey electronically through the FormSG platform.1 The research procedures for this study received formal approval for an exempt review from the SingHealth Centralized Institutional Review Board (CIRB Ref No.: 2023–2,539). All the authors and caregivers of the children surveyed have provided consent for the publication of this manuscript.
Data collection
Between October 2023 and April 2024, a total of 1,307 responses were collected in total. The online questionnaire was designed with adaptive functionality, ensuring that only age-appropriate questions appeared based on the caregiver-selected child’s age group. This streamlined the questionnaire, presenting caregivers with relevant items tailored to their child’s age group. The survey gathered data on the child’s baseline characteristics, feeding and eating practices pertaining to the domains of variety, autonomy, setting, and timing, as well as the knowledge, attitudes, and practices of caregivers. Caregivers provided their demographic characteristics and reported on their child’s feeding and eating behaviors. They were asked to recall their child’s most recent typical week when responding to the survey. The survey questionnaire was developed and reviewed by members of the College of Pediatrics and Child Health Singapore-Integrated Platform for Research in Advancing Maternal & Child Health Outcomes (CPCHS-IPRAMHO) Feeding and Eating in Infants and Young Children Study Group. The workgroup reached a consensus on four key domain areas, comprising ‘Variety’, ‘Autonomy’, ‘Setting’, and ‘Timing’ domains that parents and caregivers should prioritize to foster healthy eating behaviors and habits in infants and young children (45). These areas include promoting food variety, encouraging eating autonomy, creating distraction-free family mealtimes, and establishing regular daytime eating schedules. The development of the survey questionnaire went through an expert review and thorough literature review, establishing its content validity. The survey took 10–15 min in total duration to complete.
Caregiver feeding practices
Caregivers were asked to report whether they had introduced solids or liquids other than milk to their child, and if so, at what age. In the context of the questionnaire, “milk” refers to either breast milk or formula. Based on a national breastfeeding survey conducted in 2011, we assume that approximately 80% of infants aged 0 to <7 months are still receiving breast milk. However, by 7 months and older, the majority of children are likely to be receiving formula milk (46). Additionally, caregivers were asked to indicate what percentage of their child’s total food intake was made up of milk feeds. To assess food preparation, caregivers were asked if their child ate the same food as the rest of the family, and if the meals were prepared with added sugar or salt. Parental perceptions and practices regarding child feeding and eating were assessed through four key questions. Caregivers were asked if they found it difficult to get their child to eat, had concerns about their child’s weight, and whether mealtimes were generally challenging. They also ranked their priorities when selecting and providing food during meals.
Assessment of variety
The survey assessed the child’s exposure to different food groups (e.g., starches and grains, proteins, fruits, and vegetables), including a variety of textures and flavors. To capture the intake of discretionary foods, caregivers were also asked to report the frequency (never, occasionally, a few times a month, once a week, a few times a week, or daily) with which their child was offered packaged, canned, or processed foods and sugar-sweetened beverages (SSBs; e.g., sugary drinks, malt drinks, yogurt drinks).
Assessment of autonomy
To assess feeding autonomy and the child’s mealtime experience, caregivers were asked if the child had begun feeding themselves: using finger foods for children aged 7 to under 13 months, and using their hands or utensils for children aged 13 to under 36 months. They were also asked if their child enjoyed mealtimes, and if they believed their child was consuming sufficient amounts of milk and solids. To evaluate caregiver attentiveness and responsiveness to the child’s hunger and satiety cues from birth, caregivers were asked whether they could recognize when their child was hungry or full, and whether they encouraged their child to finish all the food or milk provided.
Assessment of setting
To assess if children were being provided an appropriate environment for a nurturing and secure feeding and eating environment, caregivers were asked if they had to do anything special to help their child feed (such as using distractions with toys), if the child was seated on a highchair during meals (only for children 0 to below 7 months old, and 7 months to below 13 months) and if they were having their meals seated together with the family at the table (only for children 13 months to less than 36 months old). The use of screen time during meals was assessed by asking parents if they engaged in screen time while eating in the presence of the child, and if the child had meals in front of a screen or an electronic device.
Assessment of timing
To evaluate whether caregivers were gradually transitioning from round-the-clock feeding to a more structured daytime feeding as their child neared 1 year old, caregivers were asked if their child had regular milk or solid feeding times (only for children aged 7 to 12 months and 13 to 35 months). They were also asked whether their child was still being given milk between midnight and 6 a.m. To assess the child’s eating behavior, particularly the speed of eating, caregivers reported how long their child typically took to complete a milk feed or a main meal.
Statistical analyses
Continuous datasets that were normally distributed are presented as the mean and standard deviation (SD). A one-way analysis of variance (ANOVA) or independent t-test was used to compare continuous variables across age groups, while the chi-square test was employed to analyze differences in categorical variables. Sex- and age-specific body mass index (BMI) z-scores were derived using the WHO references for children 0–5 years of age (47). Statistically significant results were determined at 2-sided p < 0.05. All analyses were performed using STATA software version 13 (StataCorp, College Station, United States).
Results
Characteristics of study population
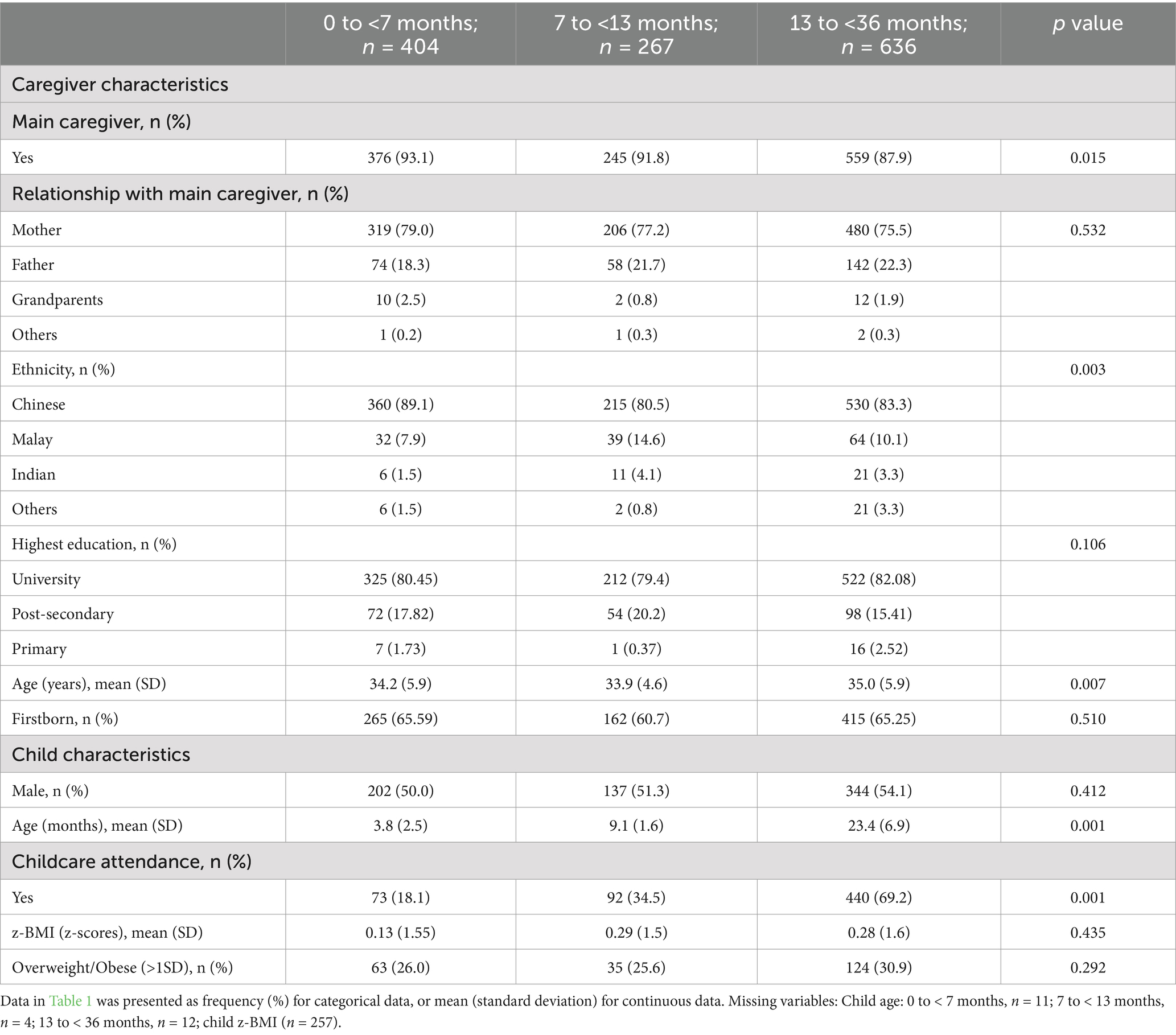
The proportion of respondents who were the main caregivers was 93.1% in the youngest age group (0 to <7 months), 91.8% in the 7 to <13 months group, and 87.9% in the 13 to <36 months group, with a majority being mothers. With regards to ethnic distribution, Chinese respondents were the largest proportion across the age groups: 89.1% in the 0 to <7 months group, 80.5% in the 7 to <13 months group, and 83.3% in the 13 to <36 months group. The average age of caregivers ranged from 33.9 (SD: 4.6) years in the 7 to <13 months group to 35.0 (5.9) years in the 13 to <36 months group. The average age of children was 3.8 (SD: 2.5) months in the 0 to <7 months group, 9.1 (SD: 1.6) months in the 7 to <13 months group, and 23.4 (SD: 6.9) months in the 13 to <36 months group. Childcare attendance was highest among children in the 13 to <36 months group (69.2%) compared to the youngest group (18.1%; Table 1). There were no statistically significant differences found with the other characteristics presented.
Caregiver feeding practices across the different age groups
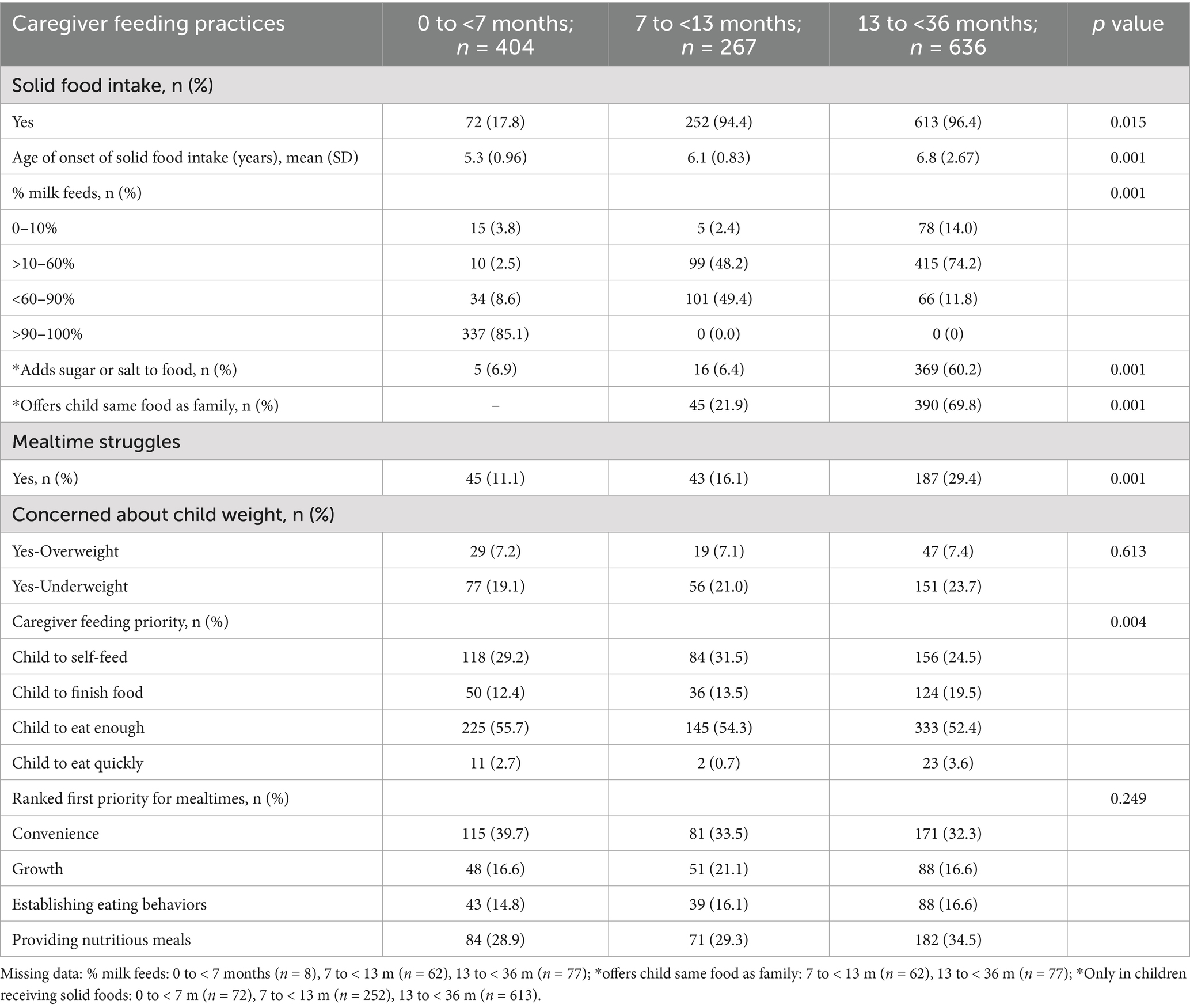
Caregiver feeding practices differed significantly by age groups (all p < 0.05), with the exception of parents’ mealtime first priority ranking (convenience, growth, establishing eating behaviors, or providing nutritious meals; Table 2). The highest proportions of children on solids were in the 7 to <13 months (94.4%) and 13 to <36 months (96.4%) groups, with average starting ages of 6.1 (SD: 0.83) and 6.8 (SD: 2.67) months, respectively. Most 0 to <7 month olds (85.1%) were still receiving over 90 to 100% of their feeds from milk. Among 7 to <13 month olds, 49.4% received less than 60 to 90% of their feeds from milk, while 74.2% of 13 to <36 month olds received between more than 10 to 60% of their feeds from milk.
Caregivers were more likely to add salt or sugar to a child’s food in the older age group of 13 to <36 months (60.2%), compared to 7 to <13 months (6.4%) and 0 to <7 months (6.9%). Caregivers of 13 to <36 month olds were also more likely to offer the same foods as the family (69.8%), compared those of 7 to <13 month olds (21.9%). Mealtime struggles increased with age: 11.1% in the 0 to <7 months group, 16.1% in the 7 to <13 months group, and 29.4% in the 13 to <36 months group. Across all age groups, more than half of caregivers prioritized ensuring their child ate enough. Caregivers of 7 to <13 month olds were most likely to prioritize self-feeding (31.5%), while those of 13 to <36 month olds prioritized getting their child to finish all their food (19.5%) and eat quickly (3.6%). Convenience ranked highest as the mealtime priority (32.3–39.7%), followed by nutritious meals (28.9–34.5%), child growth (16.1–21.1%), and establishing eating behaviors (14.8–16.6%) across all age groups (p > 0.05; Table 2).
Feeding practices in the variety domain
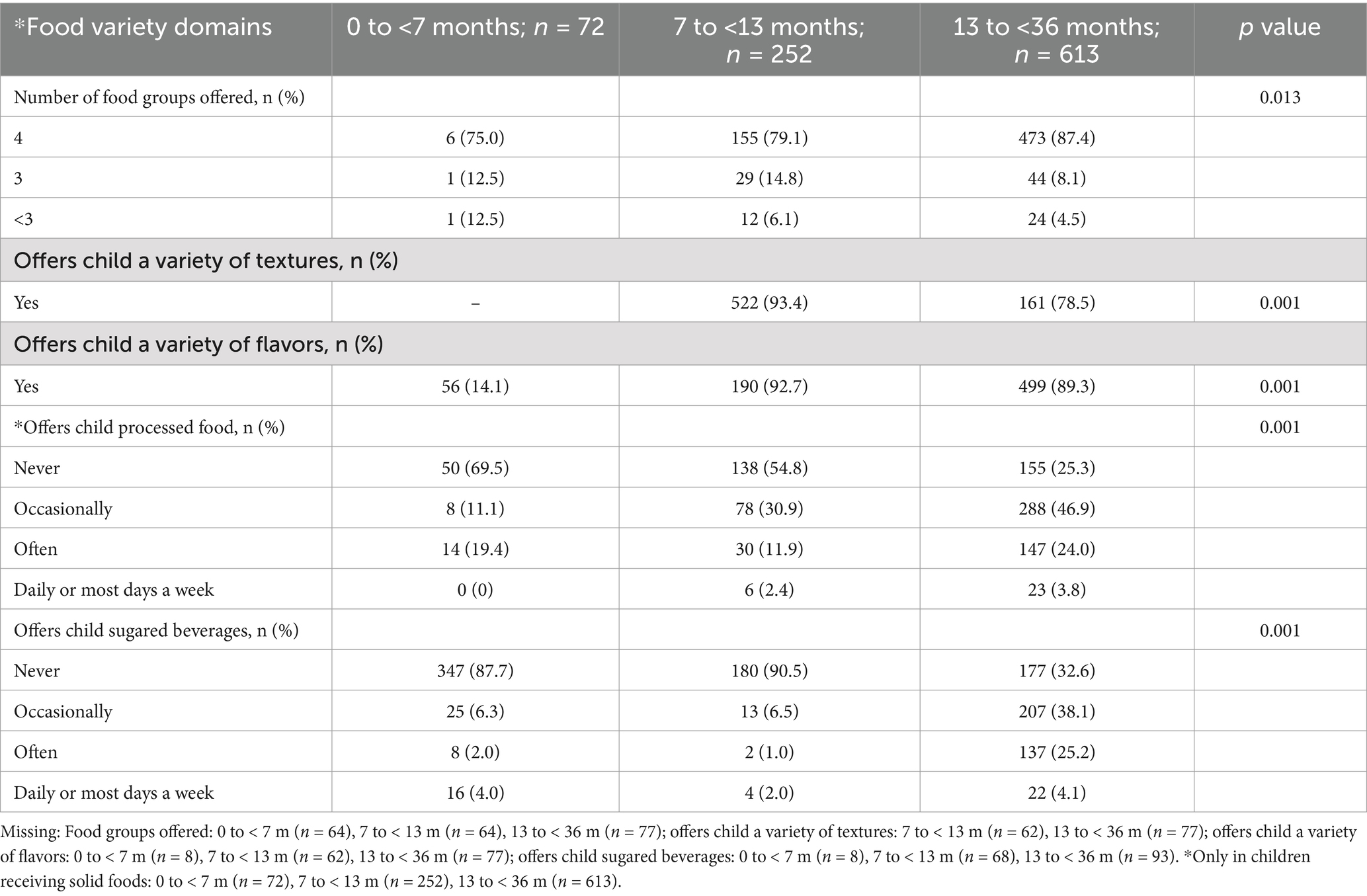
All feeding practices in the variety domain in Table 3 were significantly different across the age groups (all p < 0.05). Children aged 13 to <36 months were most likely to receive foods containing all four major food groups (87.4%), compared to the younger age groups (7 to <13 months: 79.1% and 0 to <7 months: 75.0%). A higher proportion of 7 to <13 month olds were offered varied textures (93.4%) and flavors (92.7%), compared to the older group of 13- < 36 months olds (textures: 78.5% and flavors: 89.3%). In infancy (0 to <7 months), 25.0% were offered fewer than four major food groups, while 30.5% were offered processed foods and 12.3% consumed SSBs. The highest proportion of children frequently consuming processed foods (24.0%) and SSBs (25.2%) were in the oldest age group (13 to <36 months), compared to younger age groups (Table 3).
Feeding practices in the autonomy and satiety domain
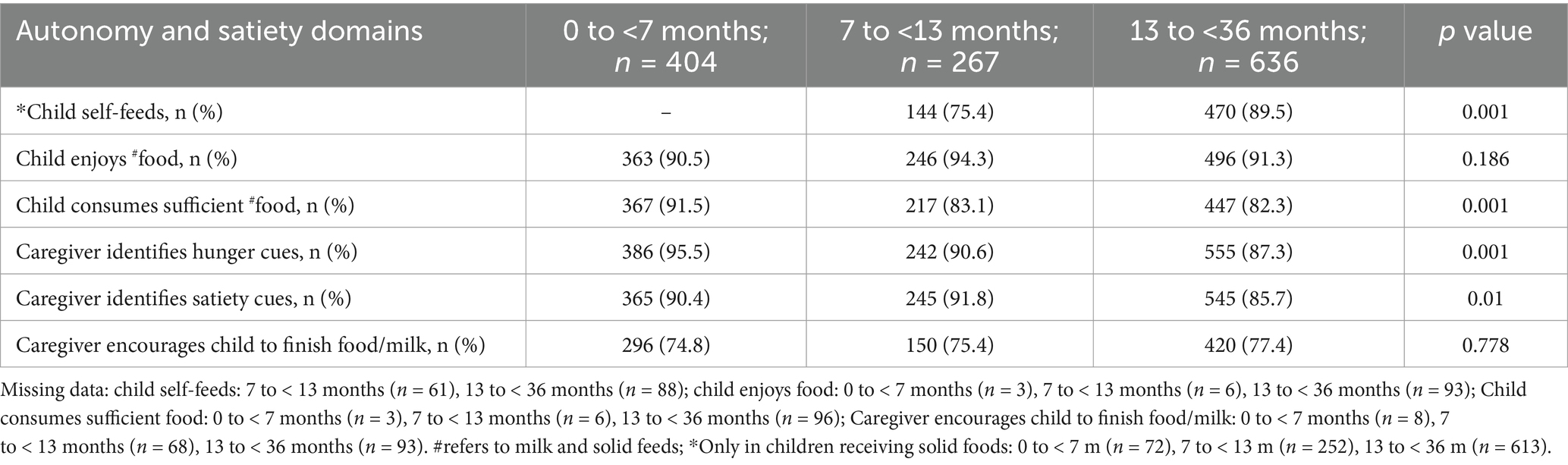
All practices differed significantly by age group, except for the enjoyment of food and the caregiver’s encouragement for the child to finish all food or milk. A higher proportion of 13 to <36 month olds were self-feeding (89.5%) compared to 7 to <13 month olds (75.4%). Overall, the likelihood of identifying hunger and satiety cues was lowest in caregivers of n children in the oldest age group (13 to <36 months). Caregivers of children aged 0 to <7 months were more likely to perceive their child as eating enough (91.5%) and to recognize hunger cues (95.5%), compared to caregivers of children in older age groups. In contrast, caregivers of children aged 7 to <13 months were most likely to identify satiety cues (91.8%; Table 4).
Feeding practices in the setting and timing domain
All feeding practices in these domains significantly differed among the age groups (p < 0.05; Tables 5, 6). Children aged 13 to <36 months were most likely to need a special mealtime setting (36.6%), use screens during meals (29.9%), and have caregivers using screens during meals (29.1%), compared to the younger age groups (all p < 0.05). A higher proportion of children aged 7 to <13 months ate in a highchair at the table (88.5%) compared to those aged 0 to <7 months (62.5%), while the highest proportion of children who sat at the table with the family during meals times were aged 13 to <36 months olds (64.6%; Table 5). Infants aged 0 to <7 months had a longer average milk feeding duration [17.4 (SD: 11.0)] minutes compared to 7 to <13 month olds [12.3 (SD: 11.5)] minutes. However, 13 to <36 month olds had the longest solid feeding duration [27.3 (SD: 14.3 min)], and were more likely to follow a regular eating schedule (89.5%), and least likely to have post-midnight feeds (46.5%), compared to the younger age groups (Table 6).
Discussion
This study is the first to comprehensively describe feeding habits of infants and toddlers in Asia across key feeding domains. Mealtime challenges increased with age, affecting a significant proportion of caregivers and children. One-third of caregivers reported difficulties in feeding toddlers. Dietary variety was limited for 20% of infants (0–12 months) and 12.6% of toddlers (13–35 months). Processed food consumption began early, with over one-third of infants being offered such foods and one in eight consuming sugar-sweetened beverages (SSBs). By toddler age, over half consumed both processed foods and SSBs. Feeding autonomy issues were also prominent: 24.6% of infants (7–12 months) and 10.5% of toddlers struggled with self-feeding. Additionally, many caregivers of toddlers were less attuned to their children’s hunger and satiety cues. Toddlers were also more likely to require specific mealtime settings, use screens during meals, and continue post-midnight feedings. Our data further indicate that caregivers’ main priority during meals is ensuring that their child eats enough. While this priority decreases as the child grows older, a greater emphasis is placed on children finishing their meals and eating quickly. Across all age groups, caregivers consistently ranked convenience as their main priority during mealtimes, followed by the provision of nutritious meals. In contrast, promoting child growth and fostering healthy eating behaviors were given lower priority. These findings underscore the need for targeted efforts to promote healthier eating habits among young children in Singapore.
Currently, the only other local cohort examining feeding practices within Singapore is the Growing Up in Singapore Towards healthy Outcomes (GUSTO) study, which reported variations in feeding practices, but focused solely on infants at 9 and 12 months of age and limited feeding practices (41). Compared to our findings, nearly 70% of infants in the GUSTO cohort at 9 and 12 months of age were reported to consume juices and sweetened drinks (41), representing a significantly higher proportion than observed in this study. However, it is important to note that the GUSTO study captured the intake of fruit juices, which could have included 100% fruit juice or sugar-sweetened juices, whereas our study specifically focused only on sugar-sweetened beverages. This difference in categorization may explain the inflated proportions observed between the two studies. The high consumption of SSBs among toddlers in this study is consistent with findings from another local study from the Singapore population, which found that nearly 60% of 18-month-old children consumed SSBs. These beverages predominantly included sweetened drinks such as both carbonated and non-carbonated options, prepackaged fruit juices with added sugars, and sweetened soy milk (48). In terms of diet variety, children aged 12 to <36 months in our study demonstrated better food group variety compared to their Western counterparts aged 12 to <24 months in the 2016 US Feeding Infants and Toddlers Study (FITS) (49), where 20% did not consume any fruits or vegetables. However, in the United Arab Emirates (UAE)—an economically advanced nation similar to Singapore—a study of children aged 6 months to 2.5 years found that most did not meet the recommended daily or weekly intake of essential food groups (50). Notably, toddlers had a higher weekly median intake of chips and sweets compared to fruits and vegetables (50). Likewise, in our Singapore cohort of children aged 12 to <36 months, while 87.4% received food from essential groups, over 70% consumed processed foods. Feeding practices in the Asia-Pacific region, as shown in both rural and urban areas of China, India, and Indonesia in children under 5 years old, consistently reflect low dietary variety (51). Nutrient-dense, protein-rich foods, fruits, and vegetables are less commonly provided, with a reliance on staples such as rice, cereals, and noodles. A significant proportion of children, particularly in India and Indonesia, consumed energy-dense, nutrient-poor snacks and sugary drinks (51). Similarly, reports from Pakistan indicate low dietary diversity in complementary foods for infants aged 6 to 9 months (52). Collectively, these findings highlight a concerning trend: many parents offer less nutritious food and beverage options as their children enter toddlerhood. This practice can negatively impact overall diet quality early on, setting patterns that may adversely affect children’s long-term health and weight status.
The development of emerging child feeding autonomy necessitates caregiver support to offer the foundation and structure needed to establish healthy habits and routines (53). This support includes engaging in reciprocal nurturing feeding practices, such as attentively responding to a child’s hunger and satiety cues, creating a conducive mealtime environment, and minimizing distractions during meals (54). These practices further encourage children to develop preferences for healthy foods and beverages and promote autonomous eating (53). In this study, caregivers of toddlers were observed to be less responsive to recognizing hunger and satiety cues. Concordant with our study observations, Leahy et al. reported that as children grow older, typically between the ages of 3 to 5 years, there is a noticeable decline in responsive feeding practices (55). In the context of the culture in Singapore, caregivers may be less attuned to a child’s hunger and satiety cues at older ages, as approximately 70% of children at 2 years old are already enrolled in childcare centers (56) where feeding practices might not be as individualized as those in a home setting. With respect to child autonomy during mealtimes, our study found that approximately 75% of infants aged 7 to <13 months were able to self-feed. This rate is notably higher than that reported in an Asian cohort from China, where only 10% of infants aged 6–11 months could self-feed (57). It also surpasses findings from a Western population study in the United Kingdom, where 55% of infants aged 8–12 months were reported to self-feed (58). Western cultures generally promote higher rates of infant self-feeding due to norms emphasizing early independence and self-reliance. Conversely, many Asian cultures adopt more authoritarian feeding approaches, with lower responsiveness but greater control (59). Feeding practices are influenced by cultural norms and societal influences, which vary across regions. Singapore’s diverse cultural environment likely contributes to a combination of traditional and modern feeding practices, reflected in these findings.
Our data also revealed that mealtime struggles increased as children transitioned from infancy to toddlerhood. In this age group, there was also a greater need for specific mealtime settings, and an increase in screen use during meals. This underscores the importance of establishing healthy eating practices early, as failing to do so may contribute to suboptimal eating behaviors later in life (22, 60, 61). Meta-analyses confirmed that a greater quantity of screen time is associated with an increased risk of obesity (62, 63). Furthermore, the increase in screen time in children has been linked to poor eating behaviors, such as a preference for energy-dense (64), nutrient-poor foods (65), reduced consumption of fruits and vegetables (66), and a higher intake of SSBs (67). Interestingly, screen use by caregivers during meals was more prevalent across all age groups, with the highest incidence observed among those with toddlers. While physically present, caregivers’ phone use often results in distraction and reduced responsiveness to their children’s needs (68). Myruski et al. found that parental phone use during mealtimes is linked to less healthy feeding practices, including reduced positive modeling, and increased negative behaviors such as emotional regulation issues or pressuring children to eat (68). Our findings emphasize the need for targeted interventions and educational programs to promote responsive feeding practices among caregivers early in childhood, aiming to prevent escalating mealtime struggles at later ages.
When examining the timing domain in this study, we found that as children grow, they tend to spend more time eating and adopt increasingly regular eating schedules, a trend reflected in our findings. The need for nighttime feed declines for newborns as they age (69), and by 12 months of age, the need for nighttime feeding should no longer be necessary (39). However, our findings indicated that nearly half of children aged 12 to <36 months were still being offered post-midnight meals, which is most likely to be in the form of milk feeds. Research on meal timing in children is limited, but chrono nutrition, an emerging field of study within childhood nutrition, sheds light on key aspects of feeding behavior, including the timing of food intake (i.e., when meals are consumed) (21). There is increasing evidence that a later eating rhythm may contribute to a higher risk of overweight and obesity in children. Although few studies have examined this aspect of chrono nutrition, it has been suggested that late-evening eating may negatively impact cardiometabolic health, increasing the risk of weight gain and adverse lipid profiles later on in life (70).
The key strengths of our study include its large sample size of 1,307 caregivers, providing a robust representation of feeding practices within Singapore’s diverse population. Moreover, our study is unique in its comprehensive assessment of multiple dimensions of feeding, including variety, autonomy, mealtime setting, and timing. By analyzing these practices across different age groups, we have generated valuable insights into age-specific behaviors and developmental stages, thereby highlighting opportunities for targeted interventions to support healthy feeding practices.
Several limitations of our study should be acknowledged. First, the majority of caregivers surveyed were from the Chinese ethnic group with university-level education, which may introduce sampling bias and limit the generalizability of our findings to other ethnic and socioeconomic groups. Second, our study relied on retrospective self-reports from caregivers, making it susceptible to recall bias, especially when recalling specific foods and feeding practices over a typical week. Additionally, social desirability bias may have influenced caregivers to provide responses they deemed more socially acceptable; however, the anonymity of the survey helps mitigate this potential bias. Lastly, while our survey addressed established guidelines and key feeding domains, it did not capture certain extrinsic factors, such as caregiver stress, cultural beliefs, and family dynamics, which could also influence feeding practices. Furthermore, future studies should include ethnic minorities to ensure that the results are valid and applicable to a wider population, and longitudinal research will be essential to track feeding practices and eating behaviors over time.
Conclusion
In conclusion, dietary variety was limited for some infants and toddlers, with the early introduction of processed foods and sugar-sweetened beverages being common. Feeding autonomy challenges, reduced caregiver responsiveness to hunger and satiety cues, and behaviors such as reliance on specific mealtime settings, screen use during meals, and continued post-midnight feedings in toddlers were also observed. These findings underscore the critical role of caregivers in shaping early childhood feeding practices across key domains. Our study reinforces the importance of the Singapore Guidelines for Eating and Feeding in Infants and Young Children (71) and highlights the need for culturally tailored interventions to enhance complementary feeding practices and expand caregiver knowledge across diverse, multi-ethnic populations. Future research should focus on developing and evaluating such interventions to improve feeding practices and nutritional outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors upon reasonable request.
Author contributions
PQ: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft, Writing – review & editing. DC: Conceptualization, Data curation, Writing – original draft, Writing – review & editing. SLL: Writing – review & editing. CO: Conceptualization, Writing – review & editing. CNT: Writing – review & editing. MYHC: Writing – review & editing. TBKC: Writing – review & editing. FY: Writing – review & editing. MCC: Writing – review & editing. KHT: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was supported by the Integrated Platform for Research in Advancing Metabolic Health Outcomes in Women and Children (IPRAMHO)—Singapore Ministry of Health’s National Medical Research Council Center grant NMRC/CG/C008A/2017_KKH.
Acknowledgments
Integrated Platform for Research in Advancing Maternal & Child Health Outcomes (CPCHS-IPRAMHO) Feeding and Eating in Infant and Young Children Study Group committee: Mei Chien Chua, Daniel Wei Keong Chan, Chengsi Ong, Phaik Ling Quah, See Ling Loy, Chee Wai Ku, Victor Samuel Rajadurai, Wee Meng Han, Marion AW, Pei Ling Ooi, Kah Tzay Low, Yu Shan Lim, Mary Foong-Fong Chong, Benny Kai Guo Loo, Alvin Chang, Fang Kuan Chiou, Mythili Pandi, Wei Zhi Leo, Kok Hian Tan, Fabian Yap.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
References
1. Epstein, LH, Paluch, RA, Roemmich, JN, and Beecher, MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol. (2007) 26:381–91. doi: 10.1037/0278-6133.26.4.381
2. da Costa, MP, Severo, M, Araujo, J, and Vilela, S. Longitudinal tracking of diet quality from childhood to adolescence: the interplay of individual and sociodemographic factors. Appetite. (2024) 196:107279. doi: 10.1016/j.appet.2024.107279
3. Berti, C, and Socha, P. Infant and young child feeding practices and health. Nutrients. (2023) 15. doi: 10.3390/nu15051184
4. Centers for Disease C, Prevention. School health guidelines to promote healthy eating and physical activity. MMWR Recomm Rep. (2011) 60:1–76.
5. Herman, KM, Craig, CL, Gauvin, L, and Katzmarzyk, PT. Tracking of obesity and physical activity from childhood to adulthood: the physical activity longitudinal study. Int J Pediatr Obes. (2009) 4:281–8. doi: 10.3109/17477160802596171
6. Park, MH, Falconer, C, Viner, RM, and Kinra, S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. (2012) 13:985–1000. doi: 10.1111/j.1467-789X.2012.01015.x
7. Wood, AC, Blissett, JM, Brunstrom, JM, Carnell, S, Faith, MS, Fisher, JO, et al. Caregiver influences on eating behaviors in young children: a scientific statement from the American Heart Association. J Am Heart Assoc. (2020) 9:e014520. doi: 10.1161/JAHA.119.014520
8. Nicklaus, S. Development of food variety in children. Appetite. (2009) 52:253–5. doi: 10.1016/j.appet.2008.09.018
9. Maier-Noth, A. The development of healthy eating and food pleasure in infancy. Nestle Nutr Inst Workshop Ser. (2023) 97:62–71. doi: 10.1159/000529008
10. Grammer, AC, Balantekin, KN, Barch, DM, Markson, L, and Wilfley, DE. Parent-child influences on child eating self-regulation and weight in early childhood: a systematic review. Appetite. (2022) 168:105733. doi: 10.1016/j.appet.2021.105733
11. Schratz, LM, Larkin, O, Dos Santos, N, and Martin, C. Caregiver influences on eating behaviors in children: an opportunity for preventing obesity. Curr Atheroscler Rep. (2023) 25:1035–45. doi: 10.1007/s11883-023-01171-6
12. Patrick, H, Nicklas, TA, Hughes, SO, and Morales, M. The benefits of authoritative feeding style: caregiver feeding styles and children’s food consumption patterns. Appetite. (2005) 44:243–9. doi: 10.1016/j.appet.2002.07.001
13. Palfreyman, Z, Haycraft, E, and Meyer, C. Parental modelling of eating behaviours: observational validation of the parental modelling of eating Behaviours scale (PARM). Appetite. (2015) 86:31–7. doi: 10.1016/j.appet.2014.08.008
14. Powell, F, Farrow, C, Meyer, C, and Haycraft, E. The importance of mealtime structure for reducing child food fussiness. Matern Child Nutr. (2017) 13. doi: 10.1111/mcn.12296
15. Martin-Calvo, N, Usechi, A, Fabios, E, Gomez, SF, and Lopez-Gil, JF. Television watching during meals is associated with higher ultra-processed food consumption and higher free sugar intake in childhood. Pediatr Obes. (2024) 19:e13130. doi: 10.1111/ijpo.13130
16. Pearce, J, Taylor, MA, and Langley-Evans, SC. Timing of the introduction of complementary feeding and risk of childhood obesity: a systematic review. Int J Obes. (2013) 37:1295–306. doi: 10.1038/ijo.2013.99
17. Fogel, A, Fries, LR, McCrickerd, K, Goh, AT, Quah, PL, Chan, MJ, et al. Oral processing behaviours that promote children’s energy intake are associated with parent-reported appetitive traits: results from the GUSTO cohort. Appetite. (2018) 126:8–15. doi: 10.1016/j.appet.2018.03.011
18. Ohkuma, T, Hirakawa, Y, Nakamura, U, Kiyohara, Y, Kitazono, T, and Ninomiya, T. Association between eating rate and obesity: a systematic review and meta-analysis. Int J Obes. (2015) 39:1589–96. doi: 10.1038/ijo.2015.96
19. Berkowitz, RI, Moore, RH, Faith, MS, Stallings, VA, Kral, TV, and Stunkard, AJ. Identification of an obese eating style in 4-year-old children born at high and low risk for obesity. Obesity (Silver Spring). (2010) 18:505–12. doi: 10.1038/oby.2009.299
20. Stunkard, AJ, Berkowitz, RI, Schoeller, D, Maislin, G, and Stallings, VA. Predictors of body size in the first 2 y of life: a high-risk study of human obesity. Int J Obes Relat Metab Disord. (2004) 28:503–13. doi: 10.1038/sj.ijo.0802517
21. Al Abdi, T, Andreou, E, Papageorgiou, A, Heraclides, A, and Philippou, E. Personality, Chrono-nutrition and Cardiometabolic health: a narrative review of the evidence. Adv Nutr. (2020) 11:1201–10. doi: 10.1093/advances/nmaa051
22. Mura Paroche, M, Caton, SJ, Vereijken, C, Weenen, H, and Houston-Price, C. How infants and young children learn about food: a systematic review. Front Psychol. (2017) 8:1046. doi: 10.3389/fpsyg.2017.01046
23. Nicklaus, S, Boggio, V, Chabanet, C, and Issanchou, S. A prospective study of food variety seeking in childhood, adolescence and early adult life. Appetite. (2005) 44:289–97. doi: 10.1016/j.appet.2005.01.006
24. Royo-Bordonada, MA, Gorgojo, L, Ortega, H, Martin-Moreno, JM, Lasuncion, MA, Garces, C, et al. Greater dietary variety is associated with better biochemical nutritional status in Spanish children: the four provinces study. Nutr Metab Cardiovasc Dis. (2003) 13:357–64. doi: 10.1016/S0939-4753(03)80004-2
25. Vispute, S, Mandlik, R, Sanwalka, N, Gondhalekar, K, and Khadilkar, A. Dietary diversity and food variety scores and their association with nutrition and health status of Indian children and adolescents: a multicenter study. Nutrition. (2023) 111:112039. doi: 10.1016/j.nut.2023.112039
26. Vilela, S, Hetherington, MM, Oliveira, A, and Lopes, C. Tracking diet variety in childhood and its association with eating behaviours related to appetite: the generation XXI birth cohort. Appetite. (2018) 123:241–8. doi: 10.1016/j.appet.2017.12.030
27. Arlinghaus, KR, Vollrath, K, Hernandez, DC, Momin, SR, O’Connor, TM, Power, TG, et al. Authoritative parent feeding style is associated with better child dietary quality at dinner among low-income minority families. Am J Clin Nutr. (2018) 108:730–6. doi: 10.1093/ajcn/nqy142
28. Mou, Y, Jansen, PW, Raat, H, Nguyen, AN, and Voortman, T. Associations of family feeding and mealtime practices with children’s overall diet quality: results from a prospective population-based cohort. Appetite. (2021) 160:105083. doi: 10.1016/j.appet.2020.105083
29. Glanz, K, Metcalfe, JJ, Folta, SC, Brown, A, and Fiese, B. Diet and health benefits associated with in-home eating and sharing meals at home: a systematic review. Int J Environ Res Public Health. (2021) 18. doi: 10.3390/ijerph18041577
30. Harrison, ME, Norris, ML, Obeid, N, Fu, M, Weinstangel, H, and Sampson, M. Systematic review of the effects of family meal frequency on psychosocial outcomes in youth. Can Fam Physician. (2015) 61:e96–e106.
31. Quah, PL, Syuhada, G, Fries, LR, Chan, MJ, Lim, HX, Toh, JY, et al. Maternal feeding practices in relation to dietary intakes and BMI in 5 year-olds in a multi-ethnic Asian population. PLoS One. (2018) 13:e0203045. doi: 10.1371/journal.pone.0203045
32. Gregory, JE, Paxton, SJ, and Brozovic, AM. Maternal feeding practices, child eating behaviour and body mass index in preschool-aged children: a prospective analysis. Int J Behav Nutr Phys Act. (2010) 7:55. doi: 10.1186/1479-5868-7-55
33. Lutz, MR, Orr, CJ, Shonna Yin, H, Heerman, WJ, Flower, KB, Sanders, LM, et al. Television time, especially during meals, is associated with less healthy dietary practices in toddlers. Acad Pediatr. (2024) 24:741–7. doi: 10.1016/j.acap.2023.09.019
34. Teekavanich, S, Rukprayoon, H, Sutchritpongsa, S, and Rojmahamongkol, P. Electronic media use and food intake in Thai toddlers. Appetite. (2022) 176:106121. doi: 10.1016/j.appet.2022.106121
35. Fogel, A, Goh, AT, Fries, LR, Sadananthan, SA, Velan, SS, Michael, N, et al. Faster eating rates are associated with higher energy intakes during an ad libitum meal, higher BMI and greater adiposity among 4.5-year-old children: results from the growing up in Singapore towards healthy outcomes (GUSTO) cohort. Br J Nutr. (2017) 117:1042–51. doi: 10.1017/S0007114517000848
36. Peters, B, Vahlhaus, J, and Pivovarova-Ramich, O. Meal timing and its role in obesity and associated diseases. Front Endocrinol (Lausanne). (2024) 15:1359772. doi: 10.3389/fendo.2024.1359772
37. Daniels, L, Mallan, KM, Fildes, A, and Wilson, J. The timing of solid introduction in an ‘obesogenic’ environment: a narrative review of the evidence and methodological issues. Aust N Z J Public Health. (2015) 39:366–73. doi: 10.1111/1753-6405.12376
38. O’Shea, KJ, Ferguson, MC, Esposito, L, Hammer, LD, Avelis, C, Hertenstein, D, et al. The impact of reducing the frequency of night feeding on infant BMI. Pediatr Res. (2022) 91:254–60. doi: 10.1038/s41390-021-01397-7
39. Wee, PH, Loy, SL, Toh, JY, Tham, EKH, Cheung, YB, Godfrey, KM, et al. Circadian feeding patterns of 12-month-old infants. Br J Nutr. (2017) 117:1702–10. doi: 10.1017/S0007114517001684
40. Cheng, TS, Loy, SL, Toh, JY, Cheung, YB, Chan, JK, Godfrey, KM, et al. Predominantly nighttime feeding and weight outcomes in infants. Am J Clin Nutr. (2016) 104:380–8. doi: 10.3945/ajcn.116.130765
41. Toh, JY, Yip, G, Han, WM, Fok, D, Low, YL, Lee, YS, et al. Infant feeding practices in a multi-ethnic Asian cohort: the GUSTO study. Nutrients. (2016) 8. doi: 10.3390/nu8050293
42. Manikam, L, Lingam, R, Lever, I, Alexander, EC, Amadi, C, Milner, Y, et al. Complementary feeding practices for south Asian young children living in high-income countries: a systematic review. Nutrients. (2018) 10. doi: 10.3390/nu10111676
43. Quah, PL, Cheng, TS, Cheung, YB, Yap, F, Saw, SM, Godfrey, KM, et al. Maternal and infant correlates of maternal feeding beliefs and practices in a multi-ethnic Asian population: the GUSTO (growing up in Singapore towards healthy outcomes) study. Public Health Nutr. (2016) 19:2789–98. doi: 10.1017/S1368980016000744
44. Tan, BQM, Hee, JM, Yow, KS, Sim, X, Asano, M, and Chong, MF. Feeding-related knowledge, attitudes, and practices among grandparents in Singapore. Nutrients. (2019) 11. doi: 10.3390/nu11071696
45. Chua, MC, Chan, DWK, Ong, C, Quah, PL, and Loy, SL, Singapore Guidelines For Feeding And Eating In Infants And Young Children. College of Paediatrics and Child Health Singapore (CPCHS). (2024) Available at: https://www.ams.edu.sg (Accessed October 03, 2024).
46. Chua, L, and Aye, MW. Prevalence of breastfeeding in Singapore. Res & Strat Plann Div Health Promot Board. (2013) 2013:10–14.
47. World Health Organization G-. Global action plan for the prevention and control of noncommunicable diseases. (2013–2020). Available from: https://cpeg-gcep.shinyapps.io/igrowup_cpeg/ (Accessed January 21, 2025).
48. Quah, PL, Kleijweg, J, Chang, YY, Toh, JY, Lim, HX, Sugianto, R, et al. Association of sugar-sweetened beverage intake at 18 months and 5 years of age with adiposity outcomes at 6 years of age: the Singapore GUSTO mother-offspring cohort. Br J Nutr. (2019) 122:1303–12. doi: 10.1017/S0007114519002253
49. Roess, AA, Jacquier, EF, Catellier, DJ, Carvalho, R, Lutes, AC, Anater, AS, et al. Food consumption patterns of infants and toddlers: findings from the feeding infants and toddlers study (FITS) 2016. J Nutr. (2018) 148:1525S–35S. doi: 10.1093/jn/nxy171
50. Ali, HI, Magriplis, E, Attlee, A, Al Dhaheri, AS, Cheikh Ismail, L, and Stojanovska, L. Feeding practices of infants and toddlers by their mothers in selected northern emirates of the United Arab Emirates. Nutrients. (2022) 14. doi: 10.3390/nu14183719
51. Sirkka, O, Abrahamse-Berkeveld, M, and van der Beek, EM. Complementary feeding practices among young children in China, India, and Indonesia: a narrative review. Curr Dev Nutr. (2022) 6:nzac092. doi: 10.1093/cdn/nzac092
52. Manikam, L, Sharmila, A, Dharmaratnam, A, Alexander, EC, Kuah, JY, Prasad, A, et al. Systematic review of infant and young child complementary feeding practices in south Asian families: the Pakistan perspective. Public Health Nutr. (2018) 21:655–68. doi: 10.1017/S1368980017002956
53. Perez-Escamilla, R, Jimenez, EY, and Dewey, KG. Responsive feeding recommendations: harmonizing integration into dietary guidelines for infants and young children. Curr Dev Nutr. (2021) 5:nzab076
54. Pérez-Escamilla, R, Jimenez, EY, and Dewey, KG. Responsive feeding recommendations: harmonizing integration into dietary guidelines for infants and young children. Current Develop Nutrit. (2021) 5:nzab076. doi: 10.1093/cdn/nzab076
55. Leahy, KE, Birch, LL, and Rolls, BJ. Reducing the energy density of an entree decreases children’s energy intake at lunch. J Am Diet Assoc. (2008) 108:41–8. doi: 10.1016/j.jada.2007.10.015
56. Tham, EH, Tan, PT, Loo, EXL, Goh, AEN, Teoh, OH, Yap, F, et al. Early childcare enrollment and childhood wheezing phenotypes. Pediatr Allergy Immunol. (2019) 30:122–7. doi: 10.1111/pai.12983
57. Song, G, Chang, J, Guan, H, Zhang, Y, Zhang, T, and Zhang, Z. Professional feeding guidance improved Infants’ self-feeding proportion during complementary foods introduction in Beijing, China: an exploratory study. Children (Basel). (2023) 10. doi: 10.3390/children10111740
58. Government. S. Scottish Maternal and Infant Nutrition Survey. (2017). [data collection] UK Data Service. SN: 8477, 2019; doi: 10.5255/UKDA-SN-8477-1
59. Le, Q, Greaney, ML, and Lindsay, AC. Nonresponsive parenting feeding styles and practices and risk of overweight and obesity among Chinese children living outside mainland China: an integrative review of the literature. Int J Environ Res Public Health. (2023) 20. doi: 10.3390/ijerph20054090
60. Birch, LL, and Doub, AE. Learning to eat: birth to age 2 y. Am J Clin Nutr. (2014) 99:723S–8S. doi: 10.3945/ajcn.113.069047
61. Mallan, K, and Miller, N. Effect of parental feeding practices (i.e., responsive feeding) on Children’s eating behavior. Nestle Nutr Inst Workshop Ser. (2019) 91:21–30. doi: 10.1159/000493675
62. Li, C, Cheng, G, Sha, T, Cheng, W, and Yan, Y. The relationships between screen use and health indicators among infants, toddlers, and preschoolers: a Meta-analysis and systematic review. Int J Environ Res Public Health. (2020) 17. doi: 10.3390/ijerph17197324
63. Fang, K, Mu, M, Liu, K, and He, Y. Screen time and childhood overweight/obesity: a systematic review and meta-analysis. Child Care Health Dev. (2019) 45:744–53. doi: 10.1111/cch.12701
64. La Marra, M, Caviglia, G, and Perrella, R. Using smartphones when eating increases caloric intake in young people: an overview of the literature. Front Psychol. (2020) 11:587886. doi: 10.3389/fpsyg.2020.587886
65. Jusiene, R, Urbonas, V, Laurinaityte, I, Rakickiene, L, Breidokiene, R, Kuzminskaite, M, et al. Screen use during meals among young children: exploration of associated variables. Medicina (Kaunas). (2019) 55. doi: 10.3390/medicina55100688
66. Perez-Farinos, N, Villar-Villalba, C, Lopez Sobaler, AM, Dal Re Saavedra, MA, Aparicio, A, Santos Sanz, S, et al. The relationship between hours of sleep, screen time and frequency of food and drink consumption in Spain in the 2011 and 2013 ALADINO: a cross-sectional study. BMC Public Health. (2017) 17:33. doi: 10.1186/s12889-016-3962-4
67. Bornhorst, C, Wijnhoven, TM, Kunesova, M, Yngve, A, Rito, AI, Lissner, L, et al. WHO European childhood obesity surveillance initiative: associations between sleep duration, screen time and food consumption frequencies. BMC Public Health. (2015) 15:442. doi: 10.1186/s12889-015-1793-3
68. Myruski, S, Gulyayeva, O, Birk, S, Perez-Edgar, K, Buss, KA, and Dennis-Tiwary, TA. Digital disruption? Maternal mobile device use is related to infant social-emotional functioning. Dev Sci. (2018) 21:e12610. doi: 10.1111/desc.12610
69. Brown, A, and Harries, V. Infant sleep and night feeding patterns during later infancy: association with breastfeeding frequency, daytime complementary food intake, and infant weight. Breastfeed Med. (2015) 10:246–52. doi: 10.1089/bfm.2014.0153
70. St-Onge, MP, Ard, J, Baskin, ML, Chiuve, SE, Johnson, HM, Kris-Etherton, P, et al. Meal timing and frequency: implications for cardiovascular disease prevention: a scientific statement from the American Heart Association. Circulation. (2017) 135:e96–e121. doi: 10.1161/CIR.0000000000000476
Keywords: infant, early childhood, feeding practices, eating behaviors, early life nutrition
Citation: Quah PL, Chan DWK, Loy SL, Ong C, Tan C-HN, Chia MYH, Chua TBK, Yap F, Chua MC and Tan KH (2025) Caregiver feeding practices for infants and toddlers and their eating behaviors in Singapore. Front. Nutr. 12:1540031. doi: 10.3389/fnut.2025.1540031
Edited by:
Elma Izze da Silva Magalhães, Federal University of Rio Grande do Sul, BrazilReviewed by:
Melesse Belayneh, Bahir Dar University, EthiopiaCátia Ficagna, Federal University of Rio Grande do Sul, Brazil
Copyright © 2025 Quah, Chan, Loy, Ong, Tan, Chia, Chua, Yap, Chua and Tan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Phaik Ling Quah, cXVhaC5waGFpay5saW5nQGtraC5jb20uc2c=
†These authors have contributed equally to this work and share first authorship
 Phaik Ling Quah
Phaik Ling Quah Daniel Wei Keong Chan2,3,4†
Daniel Wei Keong Chan2,3,4† See Ling Loy
See Ling Loy Chengsi Ong
Chengsi Ong Michael Yong Hwa Chia
Michael Yong Hwa Chia Fabian Yap
Fabian Yap Kok Hian Tan
Kok Hian Tan