- 1Department of Nutrition and Dietetics, School of Public Health, College of Medicine and Health Sciences, Bahir Dar University, Bahir Dar, Ethiopia
- 2Department of Nutrition and Dietetics, Faculty of Public Health, Institute of Health, Jimma University, Jimma, Ethiopia
Background: Mid-Upper Arm Circumference (MUAC) or Weight-for-Length Z-Score (WHZ) are used to screen for acute malnutrition in children. The relative merits of MUAC and WHZ, as well as whether they ought to be used separately, are still up for debate. Considering the significant impact of acute malnutrition on a large number of children in Africa, along with the constraints on resources, it is crucial to critically assess the validity of simple and widely used tools utilized in both African communities and clinical settings. Therefore, this study aimed to assess the diagnostic test accuracy of MUAC in screening acute malnutrition among children aged 6–59 months in Africa.
Methods: A systematic review and meta-analysis study was conducted to pool evidence on the diagnostic performance of MUAC compared to WHZ among children aged 6 to 59 months across various studies in Africa. The StataMP 17.0 software was utilized for analysis, employing a Bivariate Random-effects Meta-Analysis model. Sensitivity, specificity, the Diagnostic Odds Ratio, and the Area Under the Curve were calculated. Heterogeneity was assessed using Cochrane’s Q statistic and the I2 test. Additionally, meta-regression, subgroup analysis, sensitivity analysis, and assessments for publication bias were employed. The overall level of diagnostic test accuracy was estimated using a random-effects meta-analysis model.
Results: Seventeen studies were included in the meta-analysis. The pooled sensitivity and specificity were 38.1% (95% CI: 30.7, 46.1%) and 94.9% (95% CI: 93.2, 96.2%), respectively. The summary receiver operating characteristic curve plot showed that MUAC had good accuracy in detecting acute malnutrition (AUC = 0.85, 95% CI: 0.82, 0.88). The pooled level of diagnostic odds ratio was 13.22 (95% CI: 9.68, 16.77). The rate of misclassification in screening for acute malnutrition using MUAC was observed to be 11.7%.
Conclusion: The MUAC demonstrated low sensitivity but high specificity in diagnosing acute malnutrition in children aged 6 to 59 months across various regions of Africa. Furthermore, it was found that MUAC provides good diagnostic test accuracy when compared to WHZ. To enhance its accuracy, it is suggested to increase the MUAC cutoff thresholds.
Background
Malnutrition in children is a global issue, particularly in Africa, but often goes underdiagnosed due to diagnostic concerns (1, 2). A low Weight-for-Length/Height z-score (WHZ) or bilateral pitting edema or low Mid-Upper Arm Circumstance (MUAC) are indicators of acute malnutrition (wasting), a type of undernutrition. This falls into two categories: moderate acute malnutrition (MAM) and severe acute malnutrition (SAM), collectively known as Global Acute Malnutrition (GAM). MAM is defined as a MUAC measurement ≥11.5 cm and < 12.5 cm, or a WHZ ≥ −3 SD and < −2 SD, based on World Health Organization (WHO) criteria, for children aged 6–59 months. SAM is diagnosed by bilateral pitting edema or severe wasting (MUAC <11.5 cm or WHZ < −3 SD) (3, 4).
MUAC examinations are a simpler and more affordable alternative for both community and clinical settings than WHZ. WHZ involves weight and height measurements and has barriers in terms of resource availability, portability, and technical abilities, particularly in community setting evaluations. MUAC is less prone to measurement errors and can be completed by a single person. For many years, MUAC assessments have been used to identify acute malnutrition. The WHO recommends utilizing WHZ or MUAC, or a combination of the two, as well as looking for signs of edema, to identify children suffering from acute malnutrition for treatment (3, 5).
The relative merits of MUAC and WHZ, as well as whether they ought to be used separately, are still up for debate. Both WHZ and MUAC identify child groups that overlap but are not identical (2, 6, 7). The poor sensitivity of MUAC at standard cutoffs has serious consequences for program efficacy. Suggesting that the metric is only able to identify just a small proportion of the overall number of wasted children. In the process of treating acute malnutrition, this will also have an impact on case identification, limit the number of children who are eligible for treatment, and ultimately have an impact on the overall rates of admission and discharge. Studies proposed varied ideal MUAC cutoff values for different age groups and sexes rather than having a standard set of cutoff values for all children in the age range of 6–59 months (3, 8).
In nutrition services, proving the agreement between wasting assessment indicators and putting solutions into practice is essential. This might lessen the likelihood that children will be treated inappropriately. Children from diverse ethnic groups with varying body frames require more research, as evidenced by these discrepancies in studies when compared to WHO recommendations (8).
Given that a large number of children in Africa are affected by acute malnutrition, and there are limited resources available, special attention should be paid to the validity of simple and widely used tools in African communities and clinical settings (9). The available evidence of MUAC’s performance versus the WHZ in children varies across different research conducted in Africa (10–13). Summarizing the current evidence in Africa is critical for evidence-based practice in nutrition and health. Therefore, this systematic review and meta-analysis aimed to summarize the currently available evidence on the diagnostic accuracy of MUAC in screening acute malnutrition among children aged 6–59 months in Africa.
Methods
Protocol registration and reporting
This review protocol was prepared following Preferred Reporting Items for Systematic Review and Meta-analysis of Diagnostic Test Accuracy Studies (PRISMA-DTA) guidelines.
Eligibility criteria
The diagnostic accuracy of MUAC (index test) was validated against WHZ (reference standard) for detecting acute malnutrition (the condition of interest) in children aged 6 to 59 months in Africa (target population). This review included diagnostic test accuracy studies published in English that either reported or allowed for the calculation of true positive (TP), false positive (FP), false negative (FN), and true negative (TN) values based on the provided metrics. All cross-sectional studies conducted at the community level, including survey-based research, were considered. Moreover, studies performed at the hospital level that screened all patients, not just those already screened and admitted for malnutrition treatment, were also included. Only studies that utilized the WHO 2006 child growth standards to calculate WHZ were considered.
Search and study selection
A systematic search was conducted across PubMed/MEDLINE, EMBASE, Scopus, Cochrane Library, and Web of Science databases. In addition, a comprehensive search was undertaken using various sources such as Google Scholar, university repositories, and reference lists of established articles. The search was carried out from its commencement till October 20, 2024.
The search terms used were (“validation” OR “accuracy” OR “performance” OR “predictive ability” OR “diagnostic ability” OR “diagnostic accuracy” OR “precision” OR “reliability” OR “correlation” OR “agreement” OR “sensitivity” OR “specificity”) AND (“MUAC” OR “mid upper arm circumference” OR “mid-upper arm circumference”) AND (“wasting” OR “acute malnutrition” OR “undernutrition” OR “malnutrition”) AND (“infant” OR “child” OR “preschool”) AND (“Algeria” OR “Angola” OR “Benin” OR “Botswana” OR “Burkina Faso” OR “Burundi” OR “Cabo Verde” OR “Cameroon” OR “Central African Republic” OR “Chad” OR “Comoros” OR “Congo” OR “Cote d Ivoire” OR “Democratic Republic Of The Congo” OR “Djibouti” OR “Egypt” OR “Equatorial Guinea” OR “Eritrea” OR “Eswatini” OR “Ethiopia” OR “Gabon” OR “Gambia” OR “Ghana” OR “Guinea” OR “Guinea-Bissau” OR “Kenya” OR “Lesotho” OR “Liberia” OR “Libya” OR “Madagascar” OR “Malawi” OR “Mali” OR “Mauritania” OR “Mauritius” OR “Morocco” OR “Mozambique” OR “Namibia” OR “Niger” OR “Nigeria” OR “Rwanda” OR “Sao Tome and Principe” OR “Senegal” OR “Seychelles” OR “Sierra Leone” OR “Somalia” OR “South Africa” OR “South Sudan” OR “Sudan” OR “Tanzania” OR “Togo” OR “Tunisia” OR “Uganda” OR “Zambia” OR “Zimbabwe”).
Data collection process
Two independent reviewers evaluated the articles for overall study quality and inclusion in the review. Any ambiguous information or disagreements among the reviewers were handled through consensus. The data extraction tool includes author names, publication year, study area, participant ages, study design, sample size, index test, and reference standard. In addition, the tool contains information on TP, FP, FN, and TN results of MUAC as compared to WHZ.
Definitions for data extraction
Acute malnutrition was operationally defined with MUAC <12.5 cm as the index test and WHZ < −2 SD as the reference standard. TP was classified as a diagnosis of acute malnutrition based on MUAC, which was confirmed by WHZ. FP was labeled as a diagnosis of acute malnutrition based on MUAC, but it was confirmed by WHZ to be not acutely malnourished. FN was categorized as a diagnosis of not acutely malnourished based on MUAC, which was later confirmed by WHZ to be acutely malnourished. TN was classified as a diagnosis of not acutely malnourished based on MUAC and confirmed by WHZ.
Risk of bias and applicability
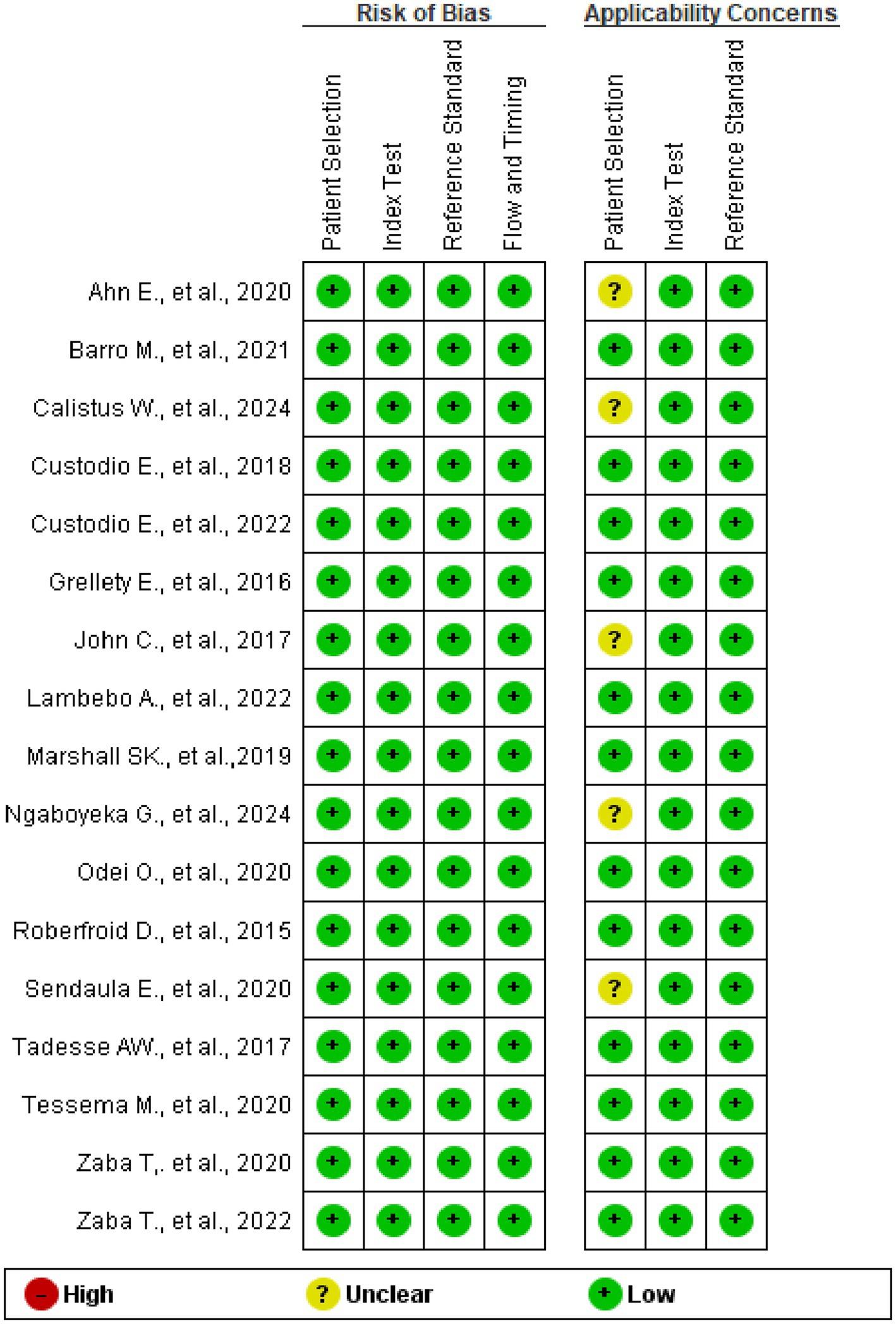
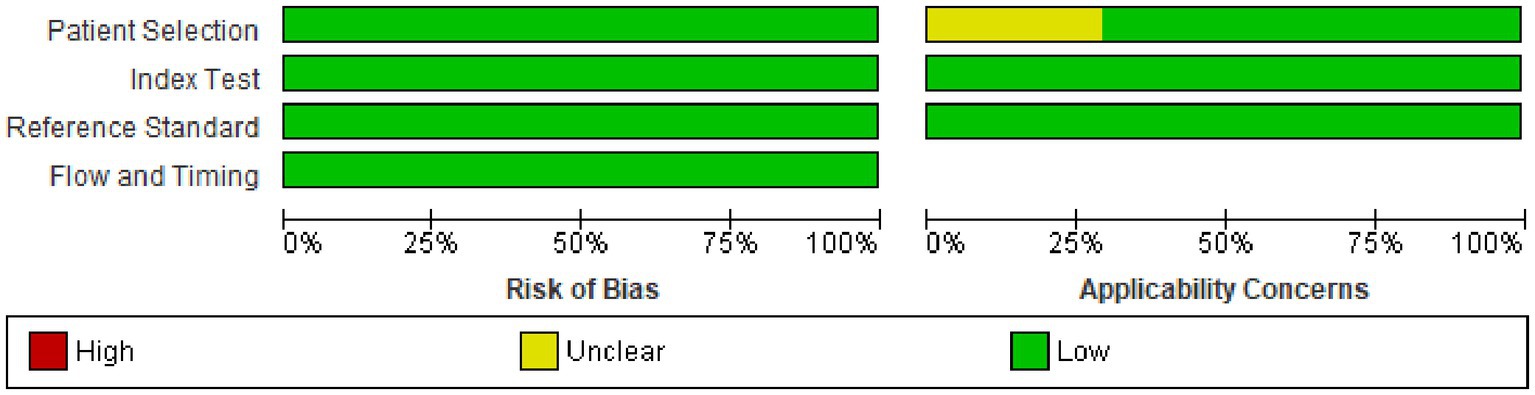
The Quality Assessment of Diagnostic Accuracy Studies-2 (QUADAS-2) tool was used to evaluate study bias and applicability across four domains: patient selection, index test, reference standard, and participant flow and timing using Review Manager 5.3 Software (14). The results were then presented in graphs. The publication bias was checked by Egger’s test and funnel plot of asymmetry using the Diagnostic Odds Ratio (DOR) as effect size.
Diagnostic accuracy measures and meta-analysis
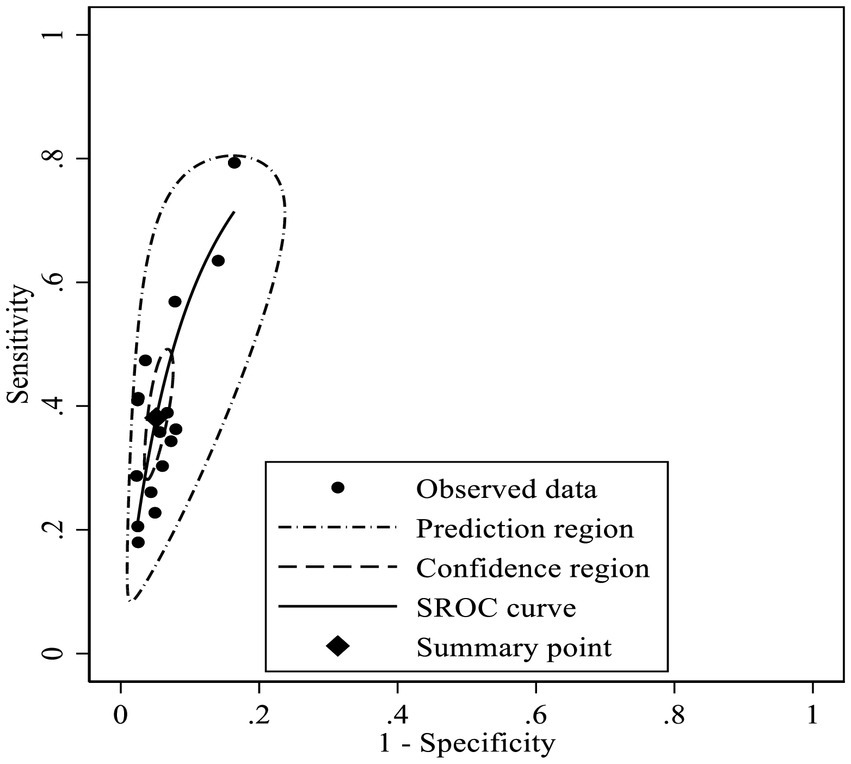
The extracted data were imported to StataMP 17.0 for further processing and analysis. The metadta statistical package was used for meta-analysis (15, 16). Another statistical procedure, midas, was employed to calculate the Area Under the Curve (AUC) (16, 17). Sensitivity, specificity, and the Diagnostic Odds Ratio (DOR) were calculated for each study using data from two-by-two tables. The meta-analysis provided pooled estimates of sensitivity, specificity, and DOR, along with 95% confidence intervals, which were visualized through forest plots. A Summary Receiver Operating Characteristic (SROC) plot was constructed using the Bivariate Random-Effects Meta-Analysis (BRMA) model, incorporating 95% confidence and prediction regions. The Area Under the Curve (AUC) was interpreted according to predefined criteria: fail (0.5–0.6), poor (0.6–0.7), fair (0.7–0.8), good (0.8–0.9), and excellent accuracy (0.9–1.0) (18).
The heterogeneity across studies was checked using the Cochrane Q test and Inconsistency index (I2) statistic. Additionally, the heterogeneity was also assessed by visual inspection of the paired forest plots and SROC plots. The heterogeneity was declared low, moderate, or high when I2 statistic results became 25, 50%, or 75%, respectively. Since all the included studies used the same thresholds for MUAC and WHZ to diagnose acute malnutrition, the use of different thresholds was not a concern for this study, which addresses one of the major sources of heterogeneity in diagnostic accuracy within systematic reviews and meta-analyses. To further investigate heterogeneity, meta-regression and a subgroup analysis were performed considering the available covariates. A sensitivity analysis was conducted to demonstrate the influence of individual studies on the overall estimates of the meta-analysis.
Results
Study selection
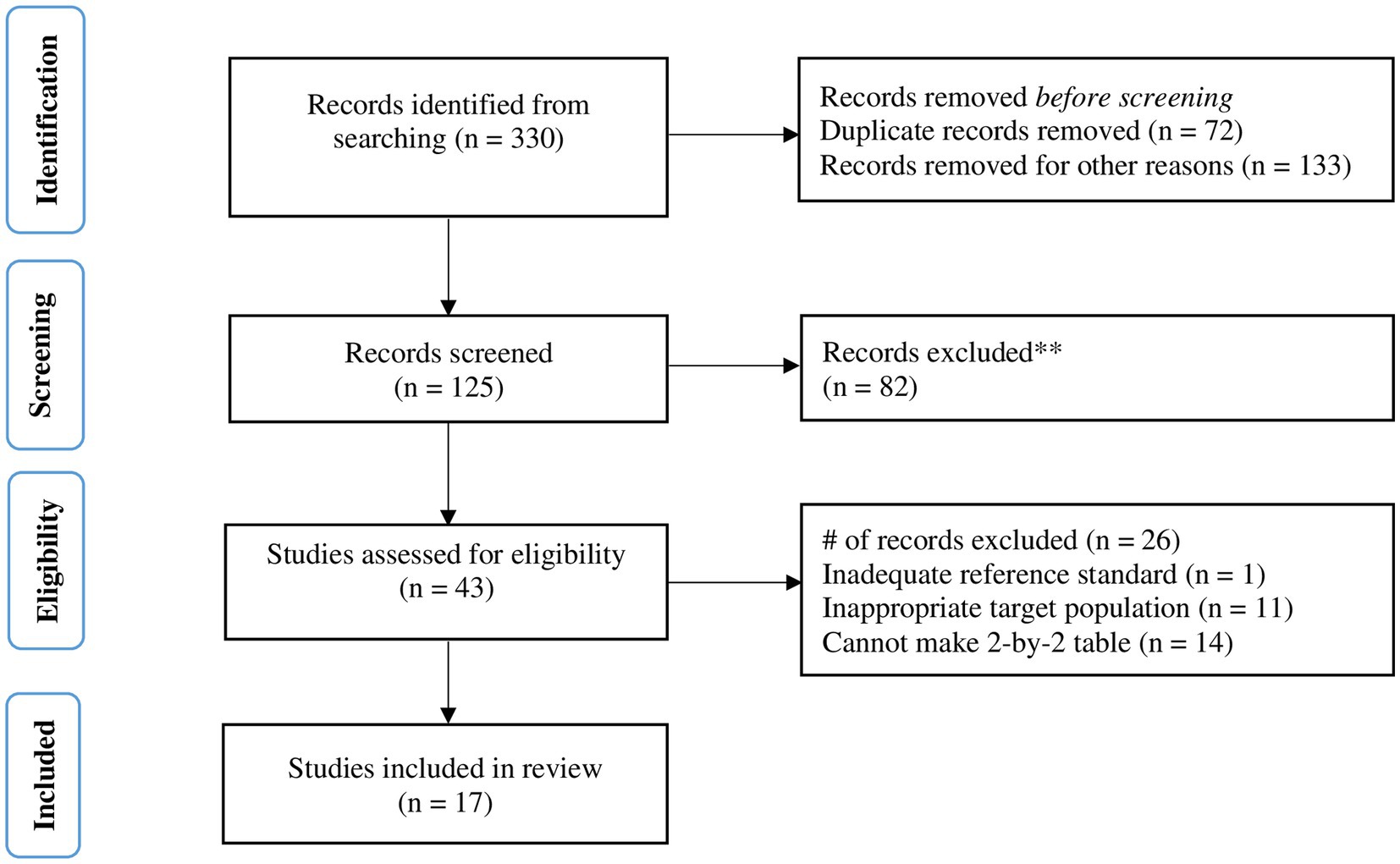
The search strategy yielded a total of 330 results from published studies. After excluding studies for various reasons, such as duplication, publication dates prior to the development of the WHO 2006 growth standards, and other criteria, 125 studies were retrieved for screening. Of the 43 studies assessed for eligibility, 26 were excluded for various reasons, including issues related to the appropriateness of the reference standard and index test thresholds, the suitability of the target population, and the ability to create a 2-by-2 table. True positive (TP), false positive (FP), false negative (FN), and true negative (TN) results were obtained either directly from the studies or calculated from other provided parameters, such as prevalence, sensitivity, or specificity. Ultimately, 17 studies were included in the meta-analysis (Figure 1).
Study characteristics
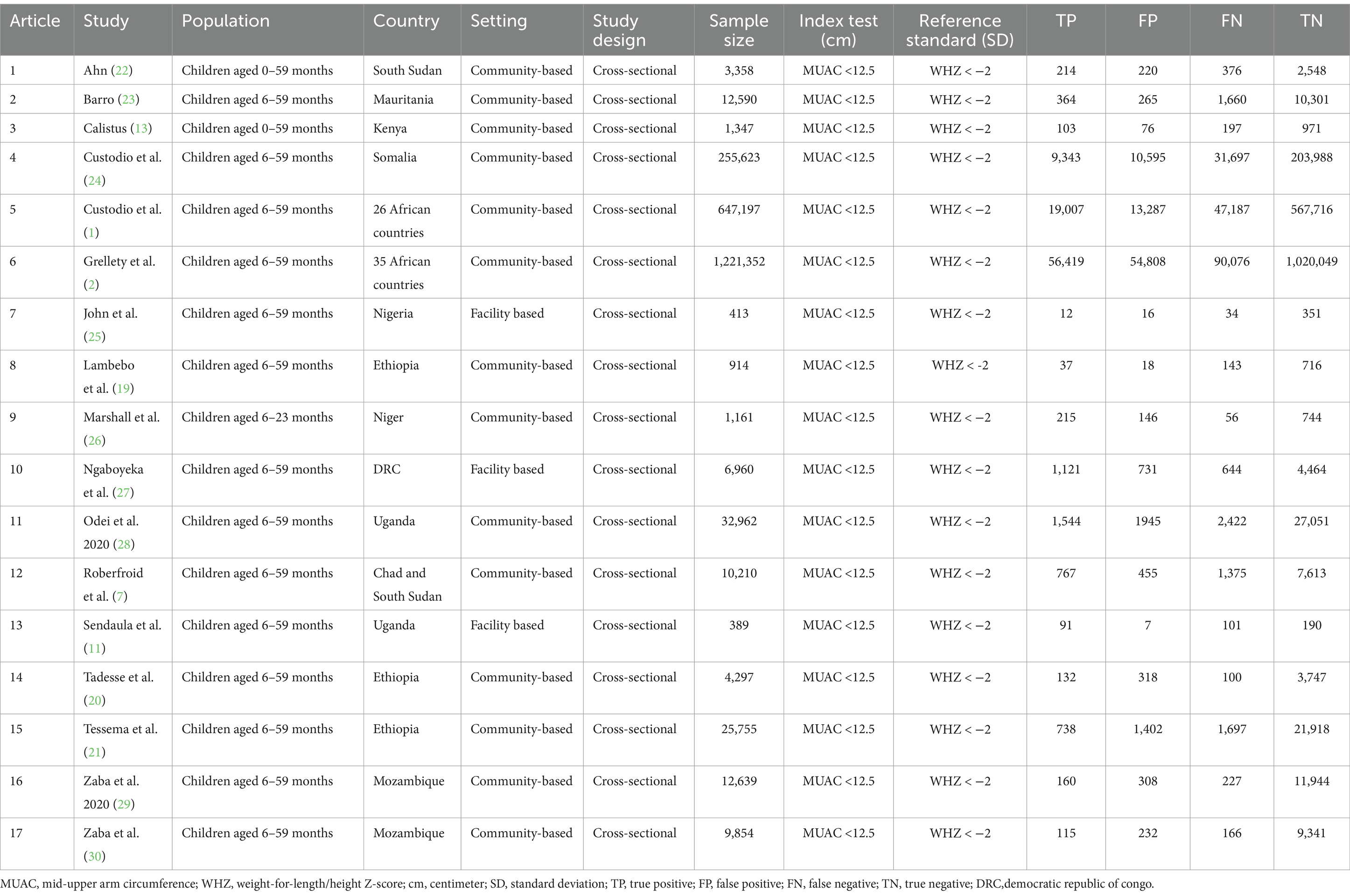
A total of 2,247,021 children were included in this meta-analysis. The minimum sample size was 389 participants in a study conducted in Uganda (11) and the largest sample size was 1,221,352 in a survey conducted in 35 African countries (2). From the total of the reviewed studies, three studies were conducted in Ethiopia (19–21) and the other are conducted in various countries (1, 2, 7, 11, 13, 19–30) (Table 1).
Risk of bias and applicability
According to the QUADAS-2 tool assessment, no risk of bias was detected in any of the studies across the four domains. Regarding applicability concerns, five studies have unclear issues related to participant selection. The concern arises from facility-based studies and the lack of clear information about the inclusion of children under six months of age alongside those aged 6–59 months, for whom inclusion is confirmed (Figures 2, 3).
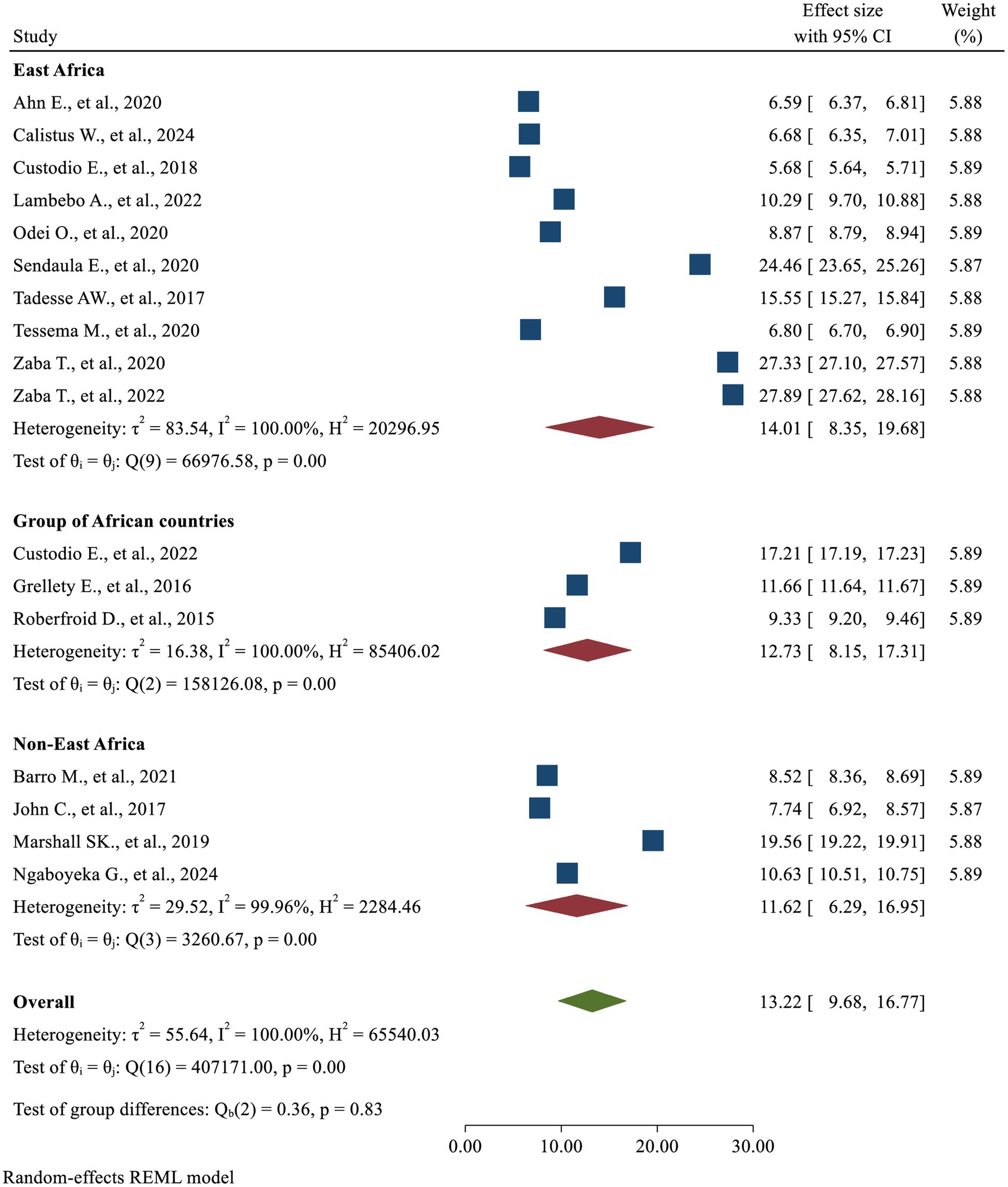
Diagnostic accuracy of MUAC
This review findings revealed that high heterogeneity was detected in the fixed model and the random-effects model provided a better fit to the data (p-value <0.0001). The correlation (rho) between sensitivity and specificity on the logit scale was −0.73. There was a nearly equivalent level of heterogeneity in sensitivity (τ2 = 0.46, I2 = 96.8%) and specificity (τ2 = 0.39, I2 = 95.6%). The generalized between-study heterogeneity without chance as indicated by bivariate I2 statistic was also high (τ2 = 0.08, I2 = 94.58%). There were non-overlapping confidence intervals in the forest plot showing heterogeneity in the magnitude of effects (Figure 4).
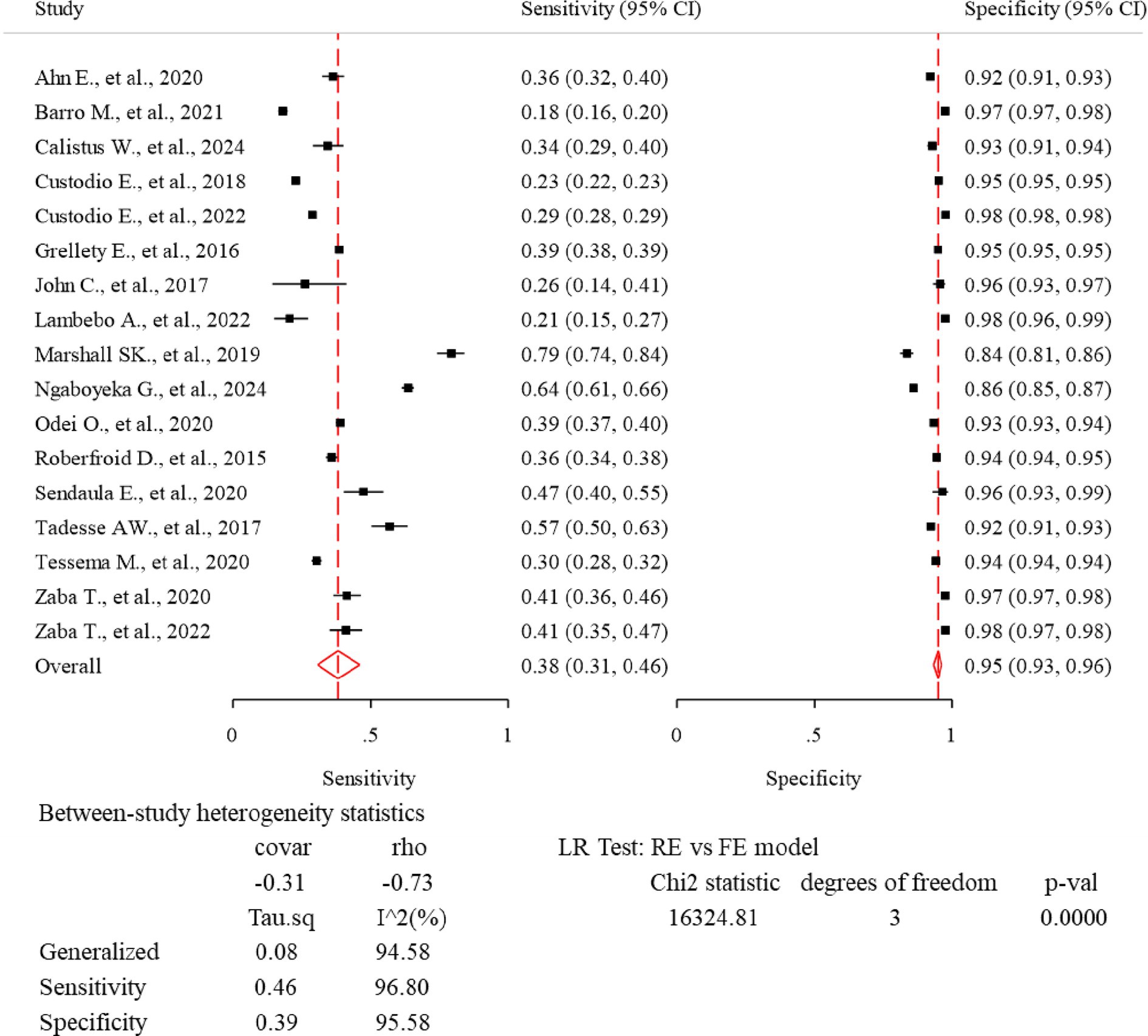
Figure 4. Forest plot—meta-analysis of diagnostic accuracy of MUAC to diagnose acute malnutrition among children aged 6–59 months in Africa.
The lowest sensitivity of MUAC for detecting acute malnutrition was 18.0% in Mauritania (23), while the highest sensitivity was 79.3% in Niger (26). The lowest specificity of MUAC to detect acute malnutrition was 83.6% in Niger (26), and the highest specificity was 97.7% in a study conducted in 26 African countries (1). The pooled sensitivity and specificity were 38.1% (95% CI: 30.7, 46.1%) and 94.9% (95% CI: 93.2, 96.2%), respectively (Figure 4). The rate of misclassification in screening for acute malnutrition using MUAC was observed to be 11.7%. The SROC plot showed that MUAC had good accuracy in detecting acute malnutrition (AUC = 0.85, 95% CI 0.82, 0.88) (Figures 5, 6).
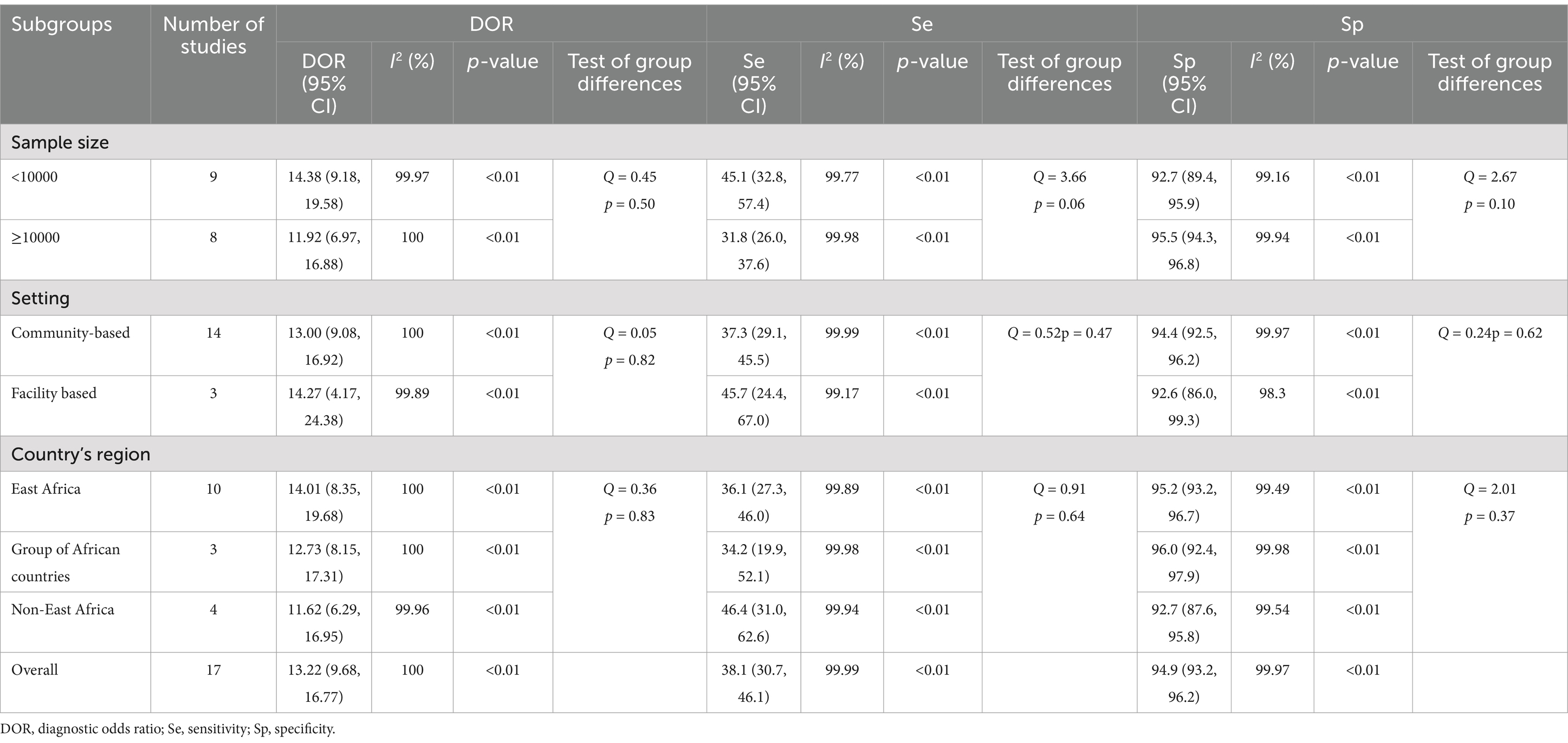
Results based on DOR
While analyzing the pooled diagnostic accuracy of MUAC using Diagnostic Odds Ratio (DOR), significantly high heterogeneity was revealed across studies (I2 = 100%, p < 0.01), which means that using a fixed-effects model would have led to an unreliable estimate. Therefore, a random-effect model was a better fit to the data (I2 = 100%, p < 0.01) and the pooled level of DOR was 13.22 (95% CI: 9.68, 16.77) (Figure 7).
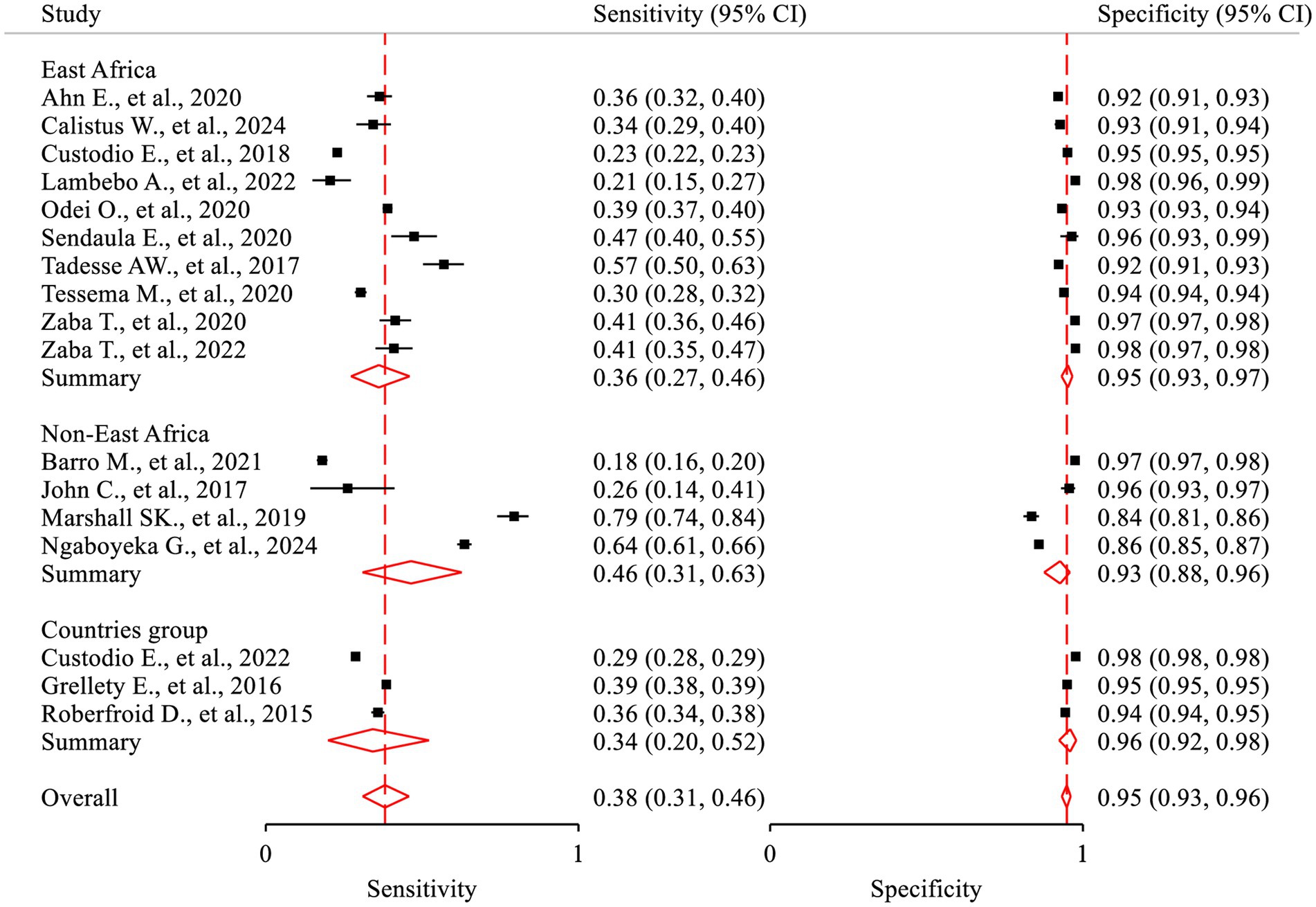
Meta-regression and subgroup analysis
A meta-regression analysis was performed to investigate the potential sources of heterogeneity using a univariate regression model, which considered the sample size as a factor. However, no statistically significant findings were observed (p-value = 0.890). Subgroup analysis was also conducted using the metan package based on selected variables, such as the country’s region, study setting, and sample size. The results of the subgroup analysis indicated a relatively comparable level of DOR across the groups (Table 2; Figure 8). The pooled sensitivity (Sp = 46.4, 95%CI: 31.0, 62.6) in the Non-East Africa Region was relatively higher than in the East Africa Region (Se = 36.1, 95%CI: 27.3, 46.0). On the contrary, the pooled specificity showed a slight decrement while going from the East Africa Region (Sp = 95.2, 95%CI: 93.2, 96.7) to the Non-East Africa Region (Sp = 92.7; 95%CI: 87.6, 95.8) (Table 2; Figure 9).
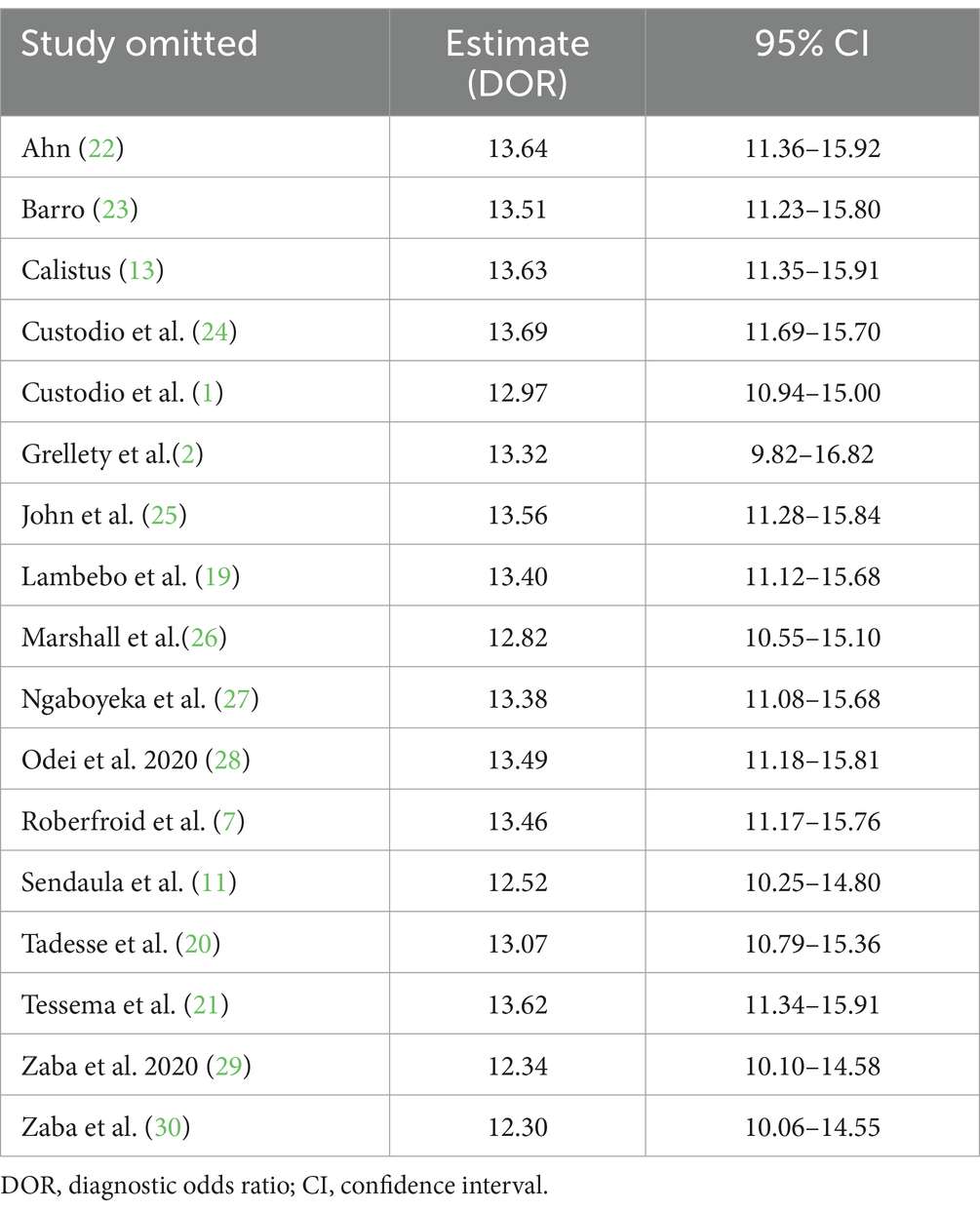
Sensitivity analysis
A sensitivity analysis was conducted to demonstrate the influence of individual studies on the overall estimates of the meta-analysis. The point estimate of an individual study “omitted” analysis lies inside the confidence interval of the “combined” analysis. This analysis indicated that the meta-analysis summary estimate was robust and not dependent on any one study (Table 3; Figure 10).
Publication bias
The publication bias was checked by Egger’s test and funnel plot of asymmetry using the DOR as effect size. Funnel plots designed separately for sensitivity and specificity (following a logit transformation) are probably not very effective in identifying sample size effects. Interpreting the two associated funnel plots along with the two tests for assessing asymmetry can be quite challenging. Therefore, the analysis was limited to funnel plots derived from the DOR. The result of Egger’s test (p = 0.391) suggested that there was no publication bias. There was a symmetric pattern around the overall effect, which indicated no publication bias, even though most of the studies fell outside the 95% CI (Figure 11).
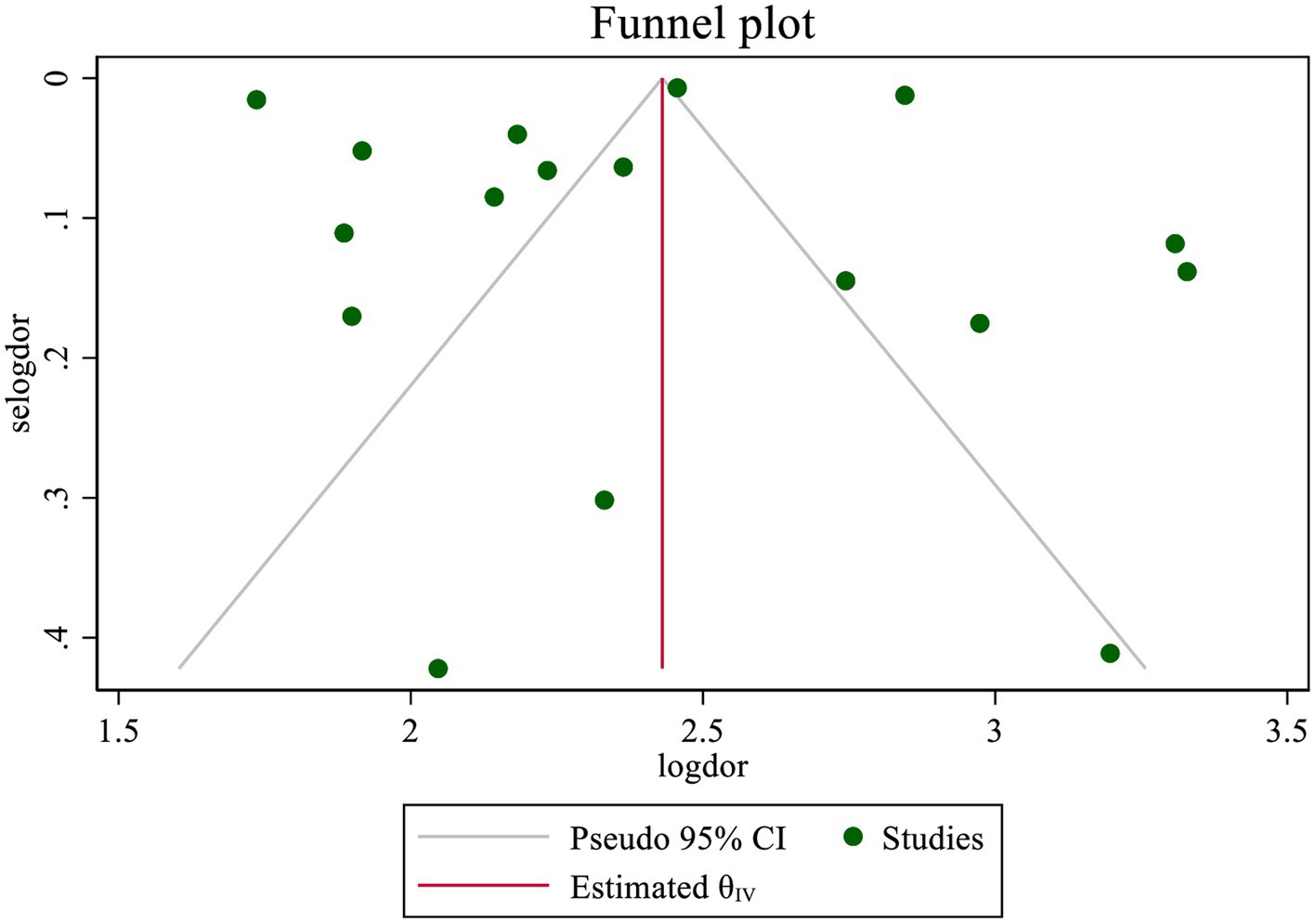
Figure 11. Funnel plot—meta-analysis of diagnostic accuracy of MUAC to diagnose acute malnutrition using DOR among children aged 6–59 months in Africa.
Discussion
This systematic review and meta-analysis were conducted to assess the diagnostic test accuracy of MUAC against WHZ in screening acute malnutrition among children aged 6–59 months in Africa. This review indicated that the pooled sensitivity and specificity of MUAC in detecting acute malnutrition were found to be 38.1 and 94.9%, respectively. The limited sensitivity and high specificity of MUAC have been reported in another systematic review and meta-analysis (8) and original research in India (31), Nepal (32) and Cambodia (33). However, another study in India revealed that MUAC showed greater sensitivity (63.7%) while maintaining comparable specificity (95.8%) (34). Similarly, a study conducted in Bangladesh reported a higher sensitivity of 63.2%, although the specificity was comparatively lower at 85.3% (35). The observed disparity may stem from a complex interplay of biological, cultural, and environmental factors that differ across racial and ethnic groups, which can result in variations in anthropometric dimensions associated with the body frame.
This low sensitivity has significant implications for screening initiatives and nutritional management. Inadequate identification and missing of undernourished children can result in delayed diagnoses, exacerbating severe health complications and even leading to fatalities. Failure to recognize malnourished individuals may have enduring consequences on their health and overall quality of life. Additionally, inaccurate diagnoses in children could result in inefficient allocation of resources and ineffective interventions. One possible explanation for this low sensitivity may lie in the MUAC cutoff threshold; increasing this cutoff may potentially enhance sensitivity. The standard MUAC cutoffs may not adequately capture the full spectrum of malnutrition across different populations. Increasing the MUAC cutoff threshold could potentially enhance sensitivity by identifying a broader range of at-risk children who might otherwise be overlooked. However, raising the cutoff also poses the risk of reducing specificity, which could lead to an increase in false positives and place additional strain on already limited resources. Therefore, adjusting cutoffs should be carefully evaluated and validated within specific contexts to balance sensitivity and specificity, ensuring the accurate identification of malnourished children and enhancing the effectiveness of interventions (6).
The MUAC showed an 11.7% misclassification rate when screening for acute malnutrition. This designates that a considerable number of children were improperly classified, leading to many being overlooked in the screening process and incorrectly deemed free of acute malnutrition, while some others were erroneously diagnosed as malnourished. Such a misclassification of nearly one in ten children poses a significant public health concern.
This study revealed that MUAC was a more precise measurement compared to its sensitivity. Children diagnosed with acute malnutrition based on MUAC have a significant likelihood of also being affected by acute malnutrition, as validated by WHZ. This indicates that employing MUAC as a screening tool was efficient for treatment, ultimately saving time and resources by lowering the incidence of false positives in acute malnutrition assessments.
The diagnostic test accuracy of MUAC for acute malnutrition was good (AUC = 0.85). This discriminatory performance was comparable to findings from other original research conducted in Asia (31, 32, 34, 36) and higher than study in Cambodia (33). The strong accuracy of this simple and user-friendly measurement was encouraging and suggested that MUAC could potentially represent WHZ assessments in both community and clinical settings. Furthermore, this level of performance could be further improved to achieve excellent diagnostic test accuracy with appropriate adjustments to the cutoff values.
The pooled DOR of 13.22 indicates that MUAC demonstrates high discriminatory performance. A higher DOR signifies that MUAC is more effective at distinguishing between individuals with and without acute malnutrition, the condition of interest. As a measure of test performance, the DOR combines sensitivity and specificity, providing prevalence-independent indicators while also reflecting overall accuracy in a single metric. This means that MUAC measurements are well-suited for identifying children with acute malnutrition or those in need of intervention.
Although not statistically significant, the visible pooled sensitivity in the Non-East Africa Region (46.4%) was marginally higher than in the East Africa Region (36.1%), while the pooled specificity slightly decreased from 95.2% in the East Africa Region to 92.7% in the Non-East Africa Region. These differences may be explained by variations in body composition and anthropometric characteristics between regions, which can influence the accuracy of MUAC as a screening tool. Differences in body frame, such as muscle mass, fat distribution, and overall arm circumference, could lead to variations in how malnutrition is detected and classified across diverse populations.
This meta-analysis faced a limitation due to notable heterogeneity between the studies. To address this, a meta-regression and subgroup analysis were performed, taking potential variables into account. A key strength of this study lies in its use of consistent cutoff values for both the index test and the reference standard, effectively eliminating any bias related to diagnostic thresholds. Furthermore, potential performance indicators were executed to pool the diagnostic accuracy of MUAC assessments across various studies conducted in multiple African countries.
Conclusion
The MUAC demonstrated low sensitivity but high specificity in diagnosing acute malnutrition in children aged 6 to 59 months across various regions of Africa. Furthermore, it was found that MUAC provides good diagnostic test accuracy when compared to WHZ. To enhance its accuracy, it is suggested to increase the MUAC cutoff thresholds.
Author contributions
YM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft. TB: Conceptualization, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing. NF: Conceptualization, Investigation, Methodology, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research, authorship, and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Custodio, E, Mwirigi, L, Tefera, N, Perez-Hoyos, A, Baille, B, Nyawo, M, et al. Assessing the use of acute malnutrition indicators for nutrition surveillance: Results from 682 283 child observations in 27 low-and middle-income countries (2022). Available online at: https://repisalud.isciii.es/rest/api/core/bitstreams/245db118-7fec-4acf-bba0-5280d50a7ec4/content (Accessed 15 October 2024).
2. Grellety, E, and Golden, MH. Weight-for-height and mid-upper-arm circumference should be used independently to diagnose acute malnutrition: policy implications. BMC Nutr. (2016) 2:10. doi: 10.1186/s40795-016-0049-7
3. World Health Organization. Guideline: Updates on the management of severe acute malnutrition in infants and children: World Health Organization; (2013). Available online at: https://iris.who.int/bitstream/handle/10665/95584/9789241506328_eng.pdf?sequence=1. (Accessed 20 February 2024)
4. World Health Organization. WHO child growth standards and the identification of severe acute malnutrition in infants and children: Joint statement by the World Health Organization and the United Nations Children’s fund. (2009). Available online at: https://iris.who.int/bitstream/handle/10665/44129/9789241598163_eng.pdf?sequence=1 (Accessed 23 February 2024).
6. Cashin, K, and Oot, L. Guide to anthropometry: A practical tool for program planners, managers, and implementers. Washington, DC: Food and Nutrition Technical Assistance III Project (FANTA)/FHI 360 (2018).
7. Roberfroid, D, Huybregts, L, Lachat, C, Vrijens, F, Kolsteren, P, and Guesdon, B. Inconsistent diagnosis of acute malnutrition by weight-for-height and mid-upper arm circumference: contributors in 16 cross-sectional surveys from South Sudan, the Philippines, Chad, and Bangladesh. Nutr J. (2015) 14:86. doi: 10.1186/s12937-015-0074-4
8. Lambebo, A, Mezemir, Y, Tamiru, D, and Belachew, T. Sensitivity and specificity of mid-upper arm circumference for assessment of severe acute malnutrition among children ages 6 to 59 months: systematic review and meta-analysis. Nutrition. (2023) 107:111918. doi: 10.1016/j.nut.2022.111918
9. World Health Organization. Levels and trends in child malnutrition: UNICEF/WHO/World Bank Group joint child malnutrition estimates: Key findings of the 2023 edition 2023. Available online at: https://iris.who.int/bitstream/handle/10665/368038/9789240073791-eng.pdf?sequence=1. (Accessed 14 December 2023).
10. Abitew, DB, Yalew, AW, Bezabih, AM, and Bazzano, AN. Comparison of mid-upper-arm circumference and weight-for-height Z-score in identifying severe acute malnutrition among children aged 6–59 months in South Gondar zone, Ethiopia. J. Nutr. Metabol. (2021) 2021:1–10. doi: 10.1155/2021/8830494
11. Sendaula, E, Joan, K, Gloria, AOO, Nicolette, N-B, Denis, O, Elizabeth, KB, et al. Performance of MUAC and associated factors in the prediction of acute malnutrition among children 6-59 at Mulago hospital. Kampala J Nutr Hum Health. (2020) 3:1–7.
12. Ngaboyeka, G, Mulume, A, Lurhagire, E, Neven, A, Zigabe, L, Balolebwami, S, et al. The performance of upper arm circumference for age in diagnosing severe acute malnutrition in children aged 6 to 59 months in south Kivu. Lwiro Cohort: Eastern Democratic Republic of Congo (2024).
13. Wilunda, Calistus, Thuita, Faith, Mwangi, Bonventure, Flax, Valerie L., Lutter, Chessa K., Adair, Linda, et al. Comparison of indicators for assessing wasting among children younger than 5 years: A longitudinal study in northern Kenya. (2024). Available online at: https://www.medrxiv.org/content/10.1101/2024.08.14.24311972v1.full.pdf. (Accessed 14 October 2024).
14. Whiting, PF, Rutjes, AWS, Westwood, ME, Mallett, S, Deeks, JJ, Reitsma, JB, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med. (2011) 155:529–36. doi: 10.7326/0003-4819-155-8-201110180-00009
15. Nyaga, VN, and Arbyn, M. Metadta: a Stata command for meta-analysis and meta-regression of diagnostic test accuracy data – a tutorial. Arch Public Health. (2022) 80:95. doi: 10.1186/s13690-021-00747-5
16. Nyaga, VN, and Arbyn, M. Comparison and validation of metadta for meta-analysis of diagnostic test accuracy studies. Res Synth Methods. (2023) 14:544–62. doi: 10.1002/jrsm.1634
17. Dwamena, BA, Sylvester, R, and Carlos, RC. Midas: meta-analysis of diagnostic accuracy studies. (2009) Available online at: http://fmwwwbcedu/repec/bocode/m/midaspdf (Accessed February 8, 2017)
18. Saeed, S, Baratloo, A, Elfil, M, and Negida, A. Evidence based emergency medicine; part 5: receiver operating curve and area under the curve. Emergency. (2016):4.
19. Lambebo, A, Mezemir, Y, Tamiru, D, and Belachew, T. Validating the diagnostic performance of MUAC in screening moderate acute malnutrition and developing an optimal cut-off for under five children of different regions in Ethiopia. PLoS One. (2022) 17:e0273634. doi: 10.1371/journal.pone.0273634
20. Tadesse, AW, Tadesse, E, Berhane, Y, and Ekström, E-C. Comparison of mid-upper arm circumference and weight-for-height to diagnose severe acute malnutrition: a study in southern Ethiopia. Nutrients. (2017) 9:267. doi: 10.3390/nu9030267
21. Tessema, M, Laillou, A, Tefera, A, Teklu, Y, Berger, J, and Wieringa, FT. Routinely MUAC screening for severe acute malnutrition should consider the gender and age group bias in the Ethiopian non-emergency context. PLoS One. (2020) 15:e0230502. doi: 10.1371/journal.pone.0230502
22. Ahn, E, Ouma, C, Loha, M, Dibaba, A, Dyment, W, Kim, J, et al. Do we need to reconsider the CMAM admission and discharge criteria?; an analysis of CMAM data in South Sudan. BMC Public Health. (2020) 20:511. doi: 10.1186/s12889-020-08657-x
23. Barro, M, Baro, MD, Cisse, D, Zagre, N, Ba, T, Baro, SN, et al. Upper arm length along with mid-upper arm circumference to enhance wasting prevalence estimation and diagnosis: sensitivity and specificity in 6–59-months-old children. Family Medicine Community Health. (2021) 9:e000748. doi: 10.1136/fmch-2020-000748
24. Custodio, E, Martin-Cañavate, R, Di Marcantonio, F, Molla, D, Abukar, Y, and Kayitakire, F. MUAC-for-age more useful than absolute MUAC for nutritional surveillance in Somalia: results from nineteen cross-sectional surveys (2007–2016). BMC Nutr. (2018) 4:8. doi: 10.1186/s40795-018-0213-3
25. John, C, Ocheke, IE, Diala, U, Adah, RO, and Envuladu, EA. Does mid upper arm circumference identify all acute malnourished 6–59 month old children, in field and clinical settings in Nigeria? South African J Clin Nutr. (2017) 30:55–9. doi: 10.1080/16070658.2016.1255486
26. Marshall, SK, Monárrez-Espino, J, and Eriksson, A. Performance of mid-upper arm circumference to diagnose acute malnutrition in a cross-sectional community-based sample of children aged 6–24 months in Niger. Nutr Res Pract. (2019) 13:247–55. doi: 10.4162/nrp.2019.13.3.247
27. Ngaboyeka, G, Bisimwa, G, Neven, A, Mwene-Batu, P, Kambale, R, Ongezi, E, et al. Arm circumference for age, arm circumference and weight-for-height z-score for the evaluation of severe acute malnutrition: a retrospective cohort study in eastern Democratic Republic of Congo. BMC Public Health. (2024) 24:587. doi: 10.1186/s12889-024-18083-y
28. Odei Obeng-Amoako, GA, Myatt, M, Conkle, J, Muwaga, BK, Aryeetey, R, Okwi, AL, et al. Concurrently wasted and stunted children 6-59 months in Karamoja, Uganda: prevalence and case detection. Matern Child Nutr. (2020) 16:e13000. doi: 10.1111/mcn.13000
29. Zaba, T, Nyawo, M, and Álvarez Morán, JL. Does weight-for-height and mid upper-arm circumference diagnose the same children as wasted? An analysis using survey data from 2017 to 2019 in Mozambique. Arch Public Health. (2020) 78:1–14. doi: 10.1186/s13690-020-00462-7
30. Zaba, T, Conkle, J, Nyawo, M, Foote, D, and Myatt, M. Concurrent wasting and stunting among children 6-59 months: an analysis using district-level survey data in Mozambique. BMC Nutr. (2022) 8:15. doi: 10.1186/s40795-022-00508-9
31. Gosalia, VV. Diagnostic accuracy of mid-upper arm circumference for the detection of acute malnutrition among children aged 6–60 months: a diagnostic accuracy study. JRHS. (2024) 24:e00612. doi: 10.34172/jrhs.2024.147
32. Lamsal, KP, Parajuli, KR, Pun, BK, Adhikari, RP, Bashyal, M, Dangol, B, et al. Accuracy of using mid-upper arm circumference to detect wasting among children aged 6-59 months in Nepal. Global Health Sci Practice. (2021) 9:881–9. doi: 10.9745/GHSP-D-20-00450
33. Laillou, A, Prak, S, de Groot, R, Whitney, S, Conkle, J, Horton, L, et al. Optimal screening of children with acute malnutrition requires a change in current WHO guidelines as MUAC and WHZ identify different patient groups. PloS one. (2014) 9:e101159. doi: 10.1371/journal.pone.0101159
34. Sougaijam, R, Gupta, S, Raut, A, Bharambe, M, and Garg, B. Validating the MUAC (mid-upper arm circumference) cut-off for detection of severe acute malnutrition in children aged 6–59 months in rural Maharashtra. Indian Pediatr. (2019) 56:209–12. doi: 10.1007/s13312-019-1502-x
35. Hossain, MI, Ahmed, T, Arifeen, SE, Billah, SM, Faruque, A, Islam, MM, et al. Comparison of midupper arm circumference and weight-for-height z score for assessing acute malnutrition in Bangladeshi children aged 6-60 mo: an analytical study. Am J Clin Nutr. (2017) 106:1232–7. doi: 10.3945/ajcn.116.139881
Keywords: acute malnutrition, MUAC, WHZ, validation, diagnostic accuracy, children, Africa
Citation: Menber Y, Belachew T and Fentahun N (2025) Diagnostic accuracy of MUAC for assessment of acute malnutrition among children aged 6–59 months in Africa: systematic review and meta-analysis. Front. Nutr. 12:1536386. doi: 10.3389/fnut.2025.1536386
Edited by:
Monica Tarcea, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, RomaniaReviewed by:
Orkun Tolunay, University of Health Sciences, TürkiyePraveen Kumar, Lady Hardinge Medical College and Associated Hospitals, India
Copyright © 2025 Menber, Belachew and Fentahun. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yonatan Menber, bmF0YW5pZW0yMUBnbWFpbC5jb20=
 Yonatan Menber
Yonatan Menber Tefera Belachew
Tefera Belachew Netsanet Fentahun
Netsanet Fentahun