- 1Shengli Clinical Medical College of Fujian Medical University, Fuzhou, China
- 2Department of Neurology, Shengli Clinical Medical College of Fujian Medical University, Fuzhou University Affiliated Provincial Hospital, Fujian Provincial Hospital, Fuzhou, China
- 3Department of Neurology, Fujian Institute of Geriatrics, Fujian Medical University Union Hospital, Fuzhou, China
- 4Fujian Key Laboratory of Molecular Neurology, Institute of Clinical Neurology, Institute of Neuroscience, Fujian Medical University, Fuzhou, China
- 5Department of Neurology, Shengli Clinical Medical College of Fujian Medical University, Fuzhou University Affiliated Provincial Hospital, Fujian Provincial Hospital, Fuzhou, China
Background: Cholesterol is a critical component of the human body, particularly within the brain, where it plays an essential role in maintaining cellular structure and function. In addition, the blood lipid profile has been recognized as a significant factor influencing cognitive performance. However, the association between the ratio of total cholesterol (TC) to high-density lipoprotein cholesterol (HDL-C) and cognitive function remains unclear.
Methods: This community-based, cross-sectional study was conducted using data from middle-aged and older adults (aged ≥45 years) participating in the China Health and Retirement Longitudinal Study (CHARLS). The primary exposure of interest was the ratio of TC to HDL-C, while the main outcome was cognitive function, assessed using cognition scores. The association between the TC-HDL-C ratio and cognitive performance was examined using multiple linear regression analyses and restricted cubic spline modeling to assess potential nonlinear relationships.
Results: A total of 8,914 participants were included in the analysis. Within a certain range, a higher TC-HDL-C ratio was significantly associated with improved cognitive scores (p < 0.05) among middle-aged and older adults. This relationship remained significant even after adjusting for sociodemographic and health-related factors. Moreover, restricted cubic spline analyses revealed a significant nonlinear association (p for nonlinearity <0.05) between the TC-HDL-C ratio and cognition scores. Subgroup analyses further highlighted differential effects of the TC-HDL-C ratio across specific population subgroups. Sensitivity analyses consistently supported the robustness of the observed relationship between the TC-HDL-C ratio and cognitive function.
Conclusion: Our findings confirm a significant nonlinear relationship between the TC-HDL-C ratio and cognitive performance in middle-aged and elderly individuals, even after adjusting for sociodemographic factors. These results underscore the potential importance of maintaining an appropriate TC-HDL-C ratio to support cognitive health in aging populations.
1 Introduction
With the aging population, the prevalence of dementia has risen significantly, presenting major challenges to families and society in China. Dementia is a leading cause of disability and dependency among older adults, with cognitive decline often serving as a precursor to its onset. Therefore, identifying and addressing factors associated with cognitive decline is critical for early prevention and intervention.
Lipid metabolism has been widely studied in relationship to cognitive performance, with conventional lipid parameters such as high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), triglycerides (TG), and total cholesterol (TC) commonly investigated (1–3). In recent years, unconventional lipid parameters, including non-high-density lipoprotein cholesterol (NHDL-C), the NHDL-C/HDL-C ratio, TG/HDL-C ratio, and TC-HDL-C ratio, have been proposed as more sensitive predictors of metabolic and vascular conditions such as diabetes and hypertension (4–7). For example, a retrospective longitudinal study demonstrated that an elevated TG/HDL-C ratio was associated with poorer cognitive performance in individuals with mild cognitive impairment and Alzheimer’s disease (8). However, to date, no studies have examined the relationship between the TC-HDL-C ratio and cognition in Chinese populations.
The TC-HDL-C ratio, which reflects the balance of cholesterol ester-rich lipoproteins, is influenced by both triglyceride and LDL-C levels (9). This parameter has been established as a sensitive predictor of diabetes, as well as cardiovascular and cerebrovascular events, in multiple studies (4, 10, 11). Notably, a long-term prospective study conducted in Sweden identified the TC-HDL-C ratio as a stronger predictor of ischemic heart disease compared to non-HDL-C (12). Furthermore, extreme values of the TC-HDL-C ratio—whether too high or too low—have been associated with increased all-cause mortality in the general population (13). Given the known links between lipid metabolism and diseases such as diabetes, cardiovascular disease, and cognitive dysfunction, exploring the association between the TC-HDL-C ratio and cognition is of significant clinical value.
Despite the growing body of research on lipid parameters, the relationship between the TC-HDL-C ratio and cognitive performance remains unexplored. To address this gap, we conducted a cross-sectional study based on a Chinese community-based cohort. Our study aims to investigate the association between the TC-HDL-C ratio and cognition, providing novel insights into the potential role of lipid metabolism in preventing cognitive decline and supporting public health strategies aimed at reducing the burden of dementia.
2 Materials and methods
2.1 Study population and ethical statement
The China Health and Retirement Longitudinal Study (CHARLS) is a large-scale interdisciplinary survey implemented jointly by Wuhan University and Peking University. Funded by the National Natural Science Foundation of China (NSFC), CHARLS aims to collect high-quality microdata representing households and individuals aged 45 years and older across China. The study received ethical approval from the Peking University Ethics Committee (Ethics number: IRB00001052–11015), and all participants provided written informed consent (14).
In the 2015 survey, 20,197 participants were enrolled. For the current study, participants were excluded if they were under 45 years old (N = 1,010) or had missing data on body mass index (BMI) (N = 1,824), gender (N = 4), marital status (N = 33), hypertension (N = 2,074), diabetes (N = 170), stroke (N = 140), totalcognition scores (N = 1,425), the Center for Epidemiological Studies Depression Scale-10 (CESD-10) (N = 1,450), drinking status (N = 10), education (N = 21), sleep duration (N = 284), total cholesterol (N = 2,238), lipid medications (N = 587) or coronary heart disease (N = 64). After these exclusions, 8,263 participants were included in the cross-sectional analysis.
2.2 Data collection and measurement
Data were collected through face-to-face questionnaire interviews and physical examinations. The questionnaires captured demographic information, self-reported health status, and health-related behaviors. Anthropometric data were measured by trained researchers using standardized protocols (15).
2.3 Cognition scores measurement
According to the Health and Retirement Study and CHARLS, two dimensions of cognitive functioning were captured: situational memory and executive functioning. Situational memory is measured by immediate recall and delayed recall (score range, 0–20, with higher scores indicating better functioning). Mental status scores are assessed by orientation, computational, and visuospatial abilities (score range, 0–11, with higher scores indicating better functioning). Global cognition was defined as the total cognition scores of these 2 components with a scale ranging from 0 to 31 points, with higher scores indicating better function (16).
2.4 Blood sample collection
Venous blood were collected from primary respondents and their spouses for routine blood tests, including measurements of total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), ultrasensitive C-reactive protein (hs-CRP), glycated hemoglobin, and genetic markers. Routine blood tests were conducted locally in surveyed counties and cities, while specialized indicators were analyzed in a centralized laboratory designated by the National Center for Disease Control and Prevention (17).
2.5 Definition of TC-HDL-C ratio
The formula was used to calculate TC-HDL-C ratio:
2.6 Definitions of covariates
Covariates were selected based on clinical relevance and prior research. Demographic factors included age, gender, residential location, marital status, education level, alcohol consumption, and smoking status. Hypertension and diabetes were identified through self-reports, physical examinations, or routine blood tests. Stroke and coronary heart disease was defined as a participant’s self-report of a physician-diagnosed stroke or coronary heart disease. BMI was calculated as weight (kg) divided by height squared (m2). Depression was diagnosed using CESD-10, with scores >9 indicating depression. Sleep duration was calculated as the sum of napping time (hours) and nighttime sleep duration (hours). The usage of lipid medications were defined as a participants self-report.
2.7 Statistical analysis
Continuous variables were expressed as mean ± standard deviation (SD) for normally distributed data or median and interquartile range (IQR) for non-normally distributed data. Categorical variables were reported as frequencies and percentages. Between-group comparisons were conducted using the Student’s t-test, Chi-square test, or Kruskal-Wallis test.
The association between the TC-HDL-C ratio and cognition scores was analyzed using multiple linear regression. Results were presented as partial regression coefficients (β) with 95% confidence intervals (CI). Three models were used for the analysis:
Model I: Unadjusted.
Model II: Adjusted for BMI, age, gender, location, and education.
Model III: Fully adjusted for BMI, age, marital status, gender, location, hypertension, diabetes, stroke, depression, drinking, smoking, education, sleep duration, lipid medications, and coronary heart disease.
Restricted cubic splines (RCS) were employed based on the covariates in Model III to explore potential nonlinear relationships between the TC-HDL-C ratio and cognition scores. Subgroup analyses were also conducted to investigate whether the effect of the TC-HDL-C ratio differed across various populations or conditions. RCS models were applied to the subgroup analyses to identify potential nonlinearities.
2.8 Sensitivity analyses
To test the robustness of the results, three sensitivity analyses were performed:
1. Excluding participants with cognition scores greater or less than twice the standard deviation to assess the influence of outliers.
2. Employing robust linear regression to account for the effects of extreme values.
3. Using a generalized additive model (GAM) to confirm the nonlinear association between the TC-HDL-C ratio and cognition scores.
All statistical analyses were performed using R software (version 4.1.3) and EmpowerStats (version 4.2). A p-value <0.05 was considered statistically significant.
3 Results
3.1 Baseline characteristics of participants based on TC-HDL-C ratio quartiles
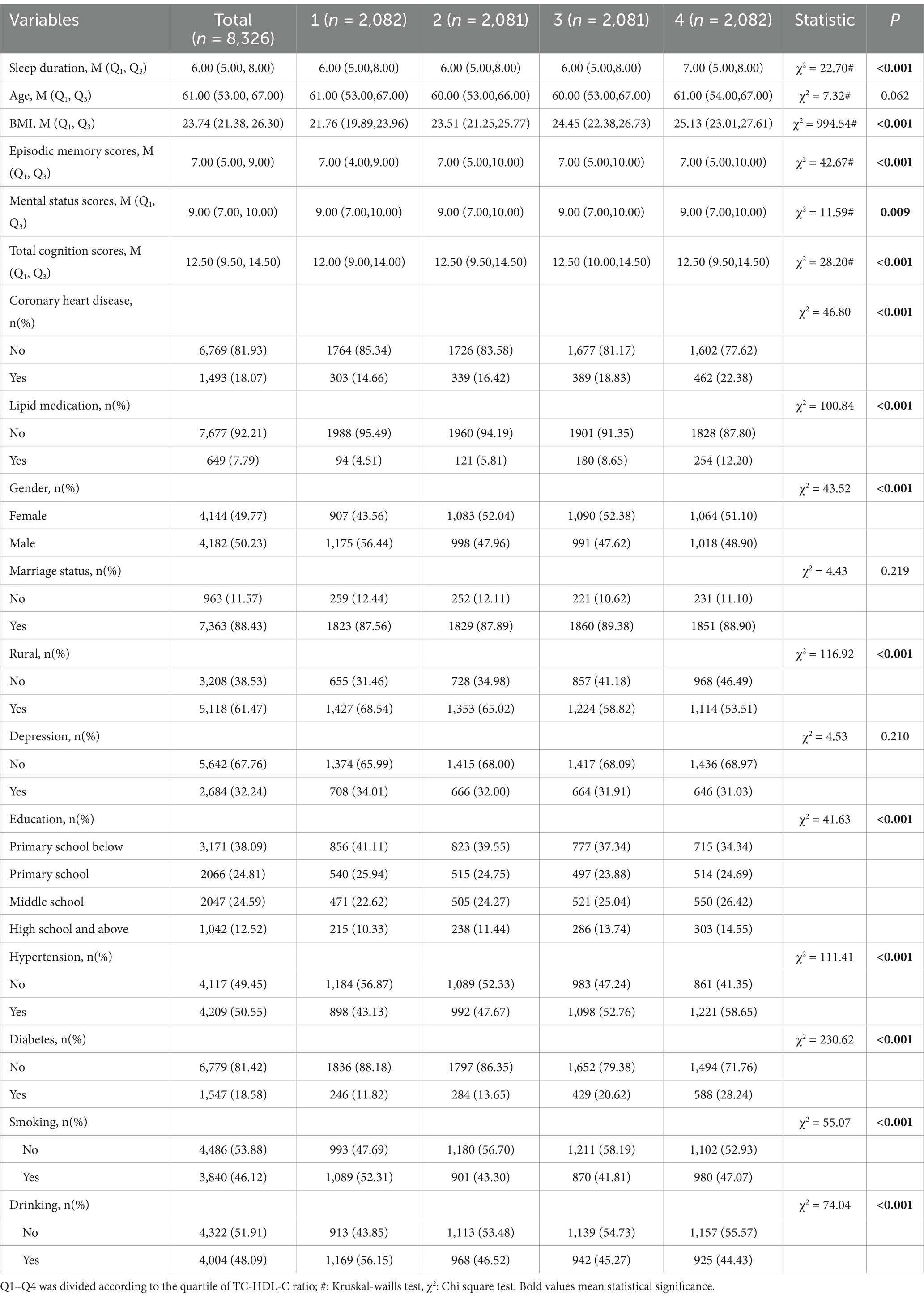
A total of 8,914 participants met the inclusion criteria and were enrolled in the analysis. Participants were divided into four groups based on the quartiles of the TC-HDL-C ratio: Q1 (≤ 3.089), Q2 (3.089 to ≤3.63), Q3 (3.63 to ≤4.24), and Q4 (≥ 4.24).
No significant differences were observed in BMI and age across the four groups. Similarly, gender, marital status, diabetes status, and sleep duration were not significantly different among the groups. However, higher TC-HDL-C ratios were associated with increased prevalence of stroke, hypertension, alcohol consumption, and smoking. Participants in the higher TC-HDL-C ratio quartiles were more likely to live in rural areas and have lower levels of education (Table 1).
3.2 Association between TC-HDL-C ratio and cognitive ability among middle-aged and elder population
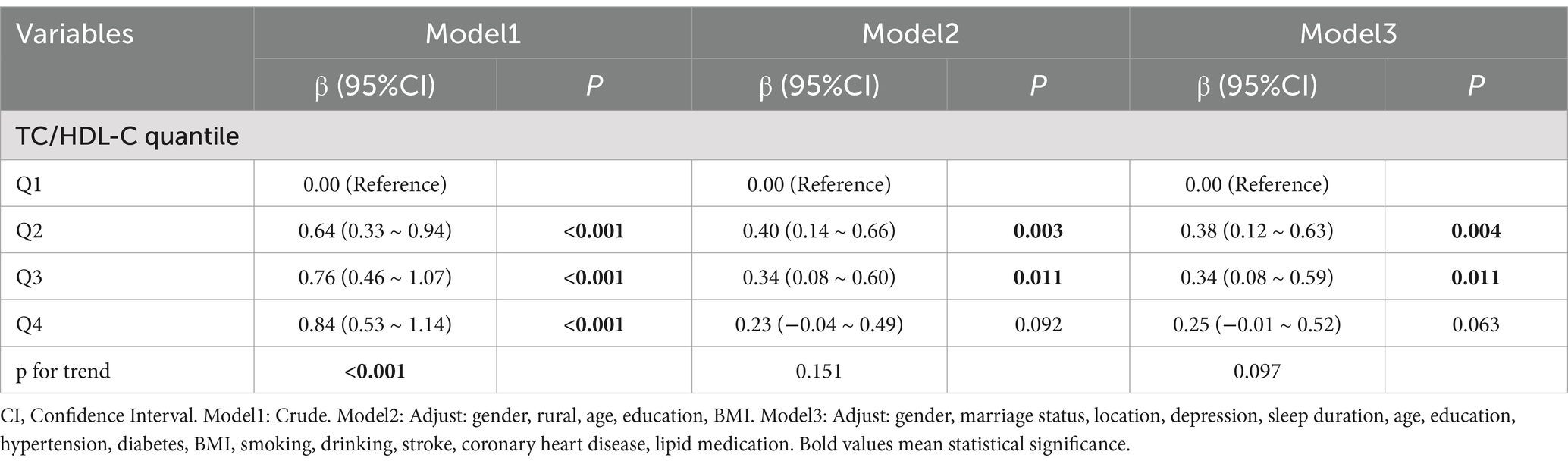
In the unadjusted model, multiple linear regression analysis revealed a positive association between TC-HDL-C ratio and cognitive scores (p for trend <0.001) (Table 2). To confirmed the analysis, partially adjusted and fully adjusted models were employed. In Model II, participants with TC-HDL-C ratio between 3.089 and 4.24 (Q2 and Q3) demonstrated better cognitive scores compared to those in Q1 (≤ 3.089) (Q2 compared to Q1: β: 0.40, p = 0.003; Q3 compared to Q1: β: 0.34, p = 0.011) (Table 2).
Interestingly, no protective effect of TC/HDL-C was observed for participants in Q4 (≥ 4.26) (β: 0.25, p = 0.063) (Table 2). The results of the fully adjusted Model III were consistent with those of Model II (Q2 compared to Q1: β: 0.38, p = 0.004; Q3 compared to Q1: β: 0.34, p = 0.011) (Table 2).
Given that cognition scores in the CHARLS survey comprise episodic memory scores and mental status scores, the association between TC-HDL-C ratio and these components was further investigated. Interestingly, in fully adjusted model III, TC-HDL-C ratio was positively correlated with episodic memory scores (Q2 compared to Q1: β: 0.32, p < 0.001; Q3 compared to Q1: β: 0.29, p = 0.003; Q4 compared to Q1: β: 0.32, p = 0.001) (Supplementary Table S1). However, no linear relationship was identified between TC-HDL-C ratio and mental status scores (Q2 compared to Q1: β: 0.06, p = 0.38; Q3 compared to Q1: β: 0.04, p = 0.574; Q4 compared to Q1: β: −0.07, p = 0.334) (Supplementary Table S2).
3.3 Nonlinear association between TC-HDL-C ratio and cognitive ability
To further explore the relationship between TC-HDL-C ratio and cognitive ability, restricted cubic spline (RCS) analysis was performed. The results indicated that a nonlinear model provided a better fit than a linear model after adjusting for all covariates (p for overall <0.001, p for nonlinear = 0.001, turning point = 3.60) (Figure 1A). Specifically, cognition scores increased with TC-HDL-C ratio up to a turning point (TC-HDL-C ratio = 3.60). Beyond this threshold, total cognition scores declined slightly and then plateaued.
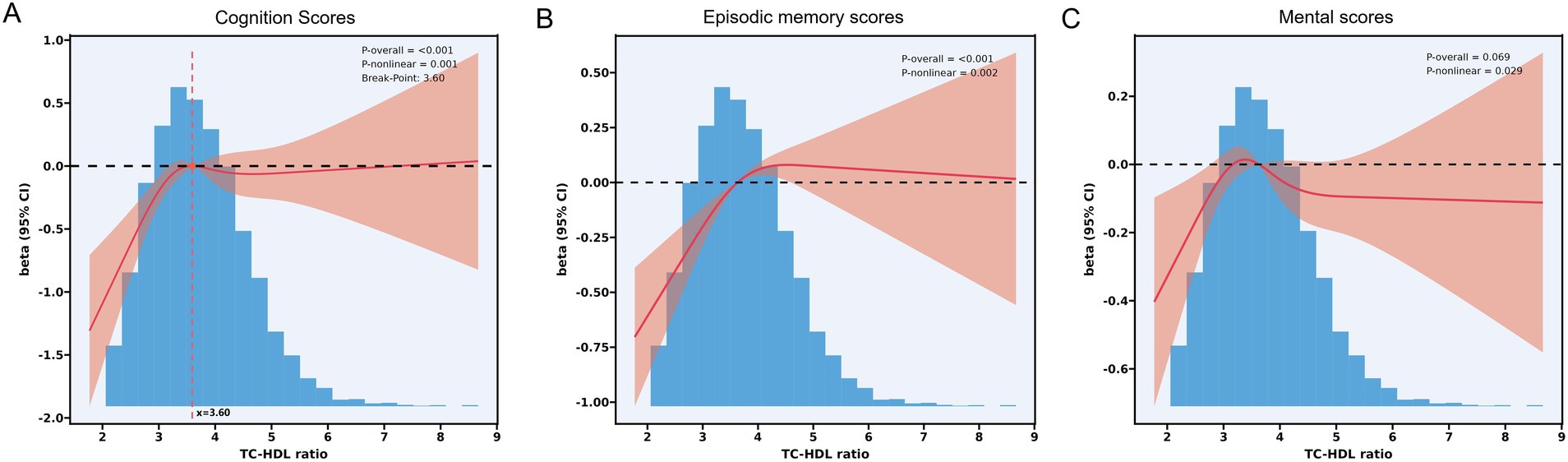
Figure 1. (A) RCS analysis between TC-HDL-C ratio and total cognition scores. p for overall <0.001; p for nonlinear = 0.001. Breaking point = 3.60. (B) RCS analysis between TC-HDL-C ratio and mental status scores. p for overall = 0.069; p for nonlinear = 0.029. (C) RCS analysis between TC-HDL-C ratio and episodic memory scores. p for overall <0.001; p for nonlinear = 0.002.
Piecewise linear regression analysis revealed a positive association between TC-HDL-C ratio and cognition scores when TC/HDL-C was below the turning point (Model I: β = 0.86, p < 0.001; Model II: β = 0.58, p < 0.001; Model III: β = 0.55, p < 0.001) (TC-HDL-C ratio = 3.60) (Table 3). However, no significant linear relationship was observed beyond this threshold. (Model I: β = 0.07, p < 0.416; Model II: β = −0.08, p = 0.295; Model III: β = −0.05, p < 535) (Table 3).
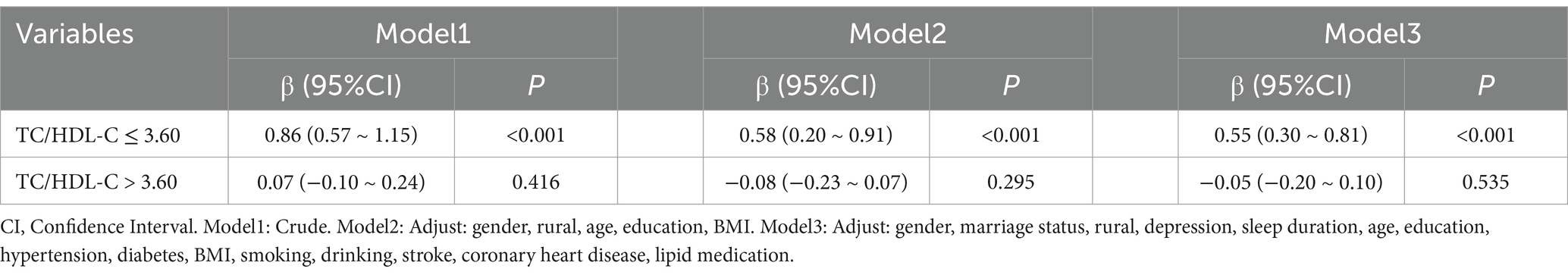
Table 3. Piecewise multiple linear regression between TC-HDL-C ratio and total cognition scores according to turning point.
RCS analysis also detected nonlinear relationships between TC-HDL-C ratio and both episodic memory scores and mental status scores (Figures 1B,C). A strong nonlinear association was observed between TC-HDL-C ratio and episodic memory scores (p for overall = 0.069; p for nonlinear = 0.029) (Figure 1B). Similarly, a nonlinear relationship was detected between TC-HDL-C ratio and mental status score (p for overall = 0.069, p for nonlinearity = 0.029) (Figure 1C).
3.4 Subgroup analysis
Subgroup analyses revealed that the association between TC-HDL-C ratio and cognitive scores varied by gender. Among females, participants in Q2 and Q3 had significantly higher cognitive scores compared to those in Q1 (Q2 compared to Q1: β = 0.48, p = 0.014; Q3 compared to Q1: β = 0.51, p = 0.010). Meanwhile, participants in Q2 had significantly higher total cognition scores compared to those in Q1 (β = 0.34, p = 0.048) (Figure 2A). In age subgroup, participants of Q2 and Q3 groups that aged between 50 years to 79 years had a significant relationship between TC-HDL-C ratio and total cognition scores (Q2 compared to Q1: β = 0.38, p = 0.007; Q3 compared to Q1: β = 0.35, p = 0.012) (Figure 2B). For BMI subgroup analysis, multiple linear regression shows that, in BMI between 18.5 and 24 subgroup, participants in Q3 and Q2 had a strong linear relationship between TC-HDL-C ratio and cognition scores (Q2 compared to Q1: β = 0.35, p = 0.048; Q3 compared to Q1: β = 0.38, p = 0.047) (Figure 2C).
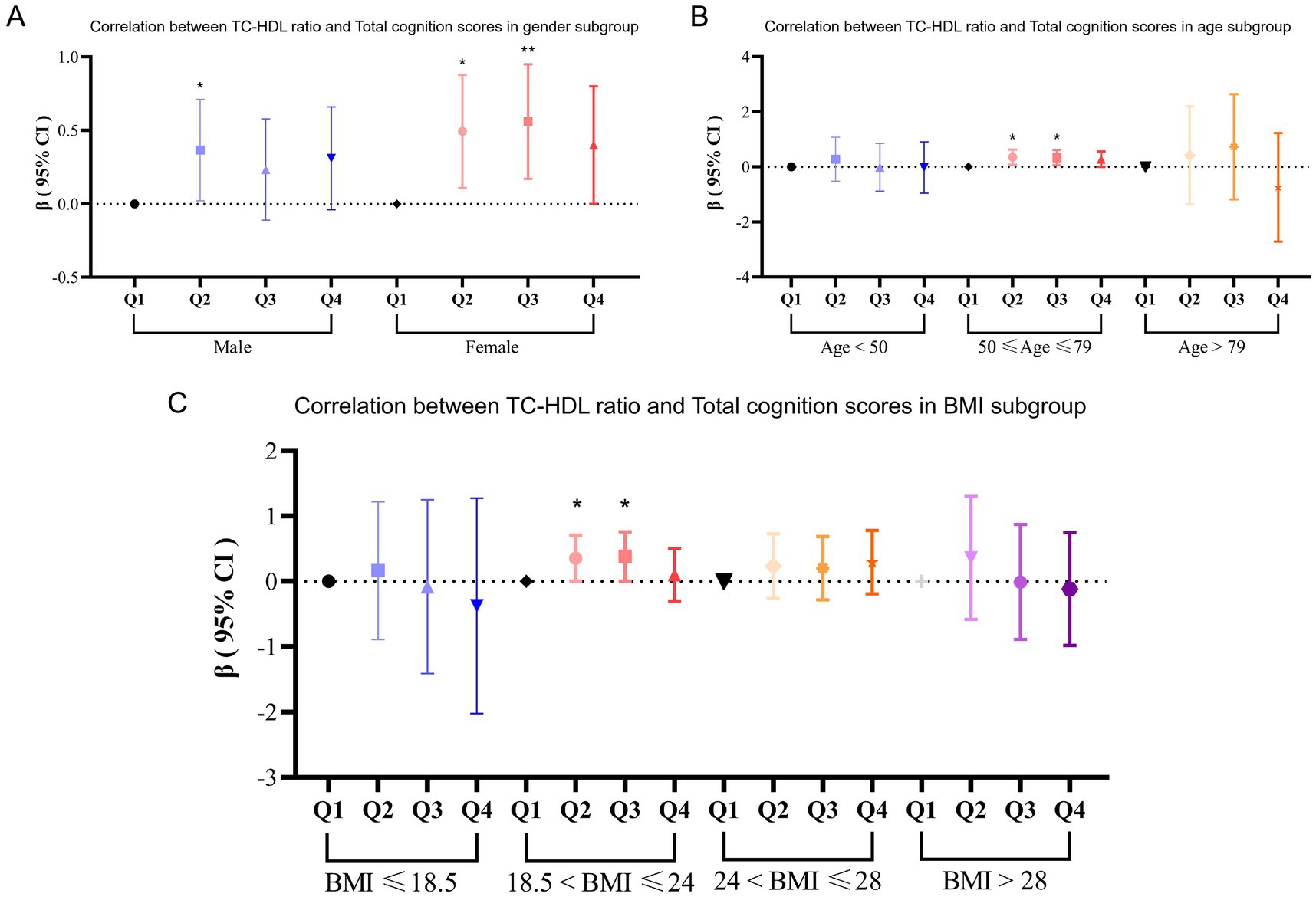
Figure 2. (A) Subgroup analysis between TC-HDL-C ratio and total cognition scores according to age. (B) Subgroup analysis between TC-HDL-C ratio and total cognition scores according to gender. (C) Subgroup analysis between TC-HDL-C ratio and total cognition scores according to BMI.
Meanwhile, RCS analysis demonstrated significant nonlinear relationships within each subgroup. For participants aged between 50 years and 79 years, the relationship between TC-HDL-C ratio and total cognition scores followed an inverse L-shaped curve (p for nonlinear = 0.003, turning points = 3.60). In contrast, for participants aged ≥80 years, an inverse U-shaped curve was found (p for nonlinear = 0.011, turning points = 3.66) (Figures 3A–C). In male subgroup, TC-HDL-C ratio had an nearly inverse L-shaped curve with total cognition scores. In addition, in female, TC-HDL-C ratio had an inverse U-shaped curve with total cognition ability, which suggests that too-high and too-low TC-HDL-C ratio might increase the risk of cognition decline (Figures 3D,E). However, in BMI subgroup, only participants whose BMI between 18.5 and 24 had a nonlinear association between TC-HDL-C ratio and total cognition scores (p for nonlinear = 0.038) (Figures 3F–I).
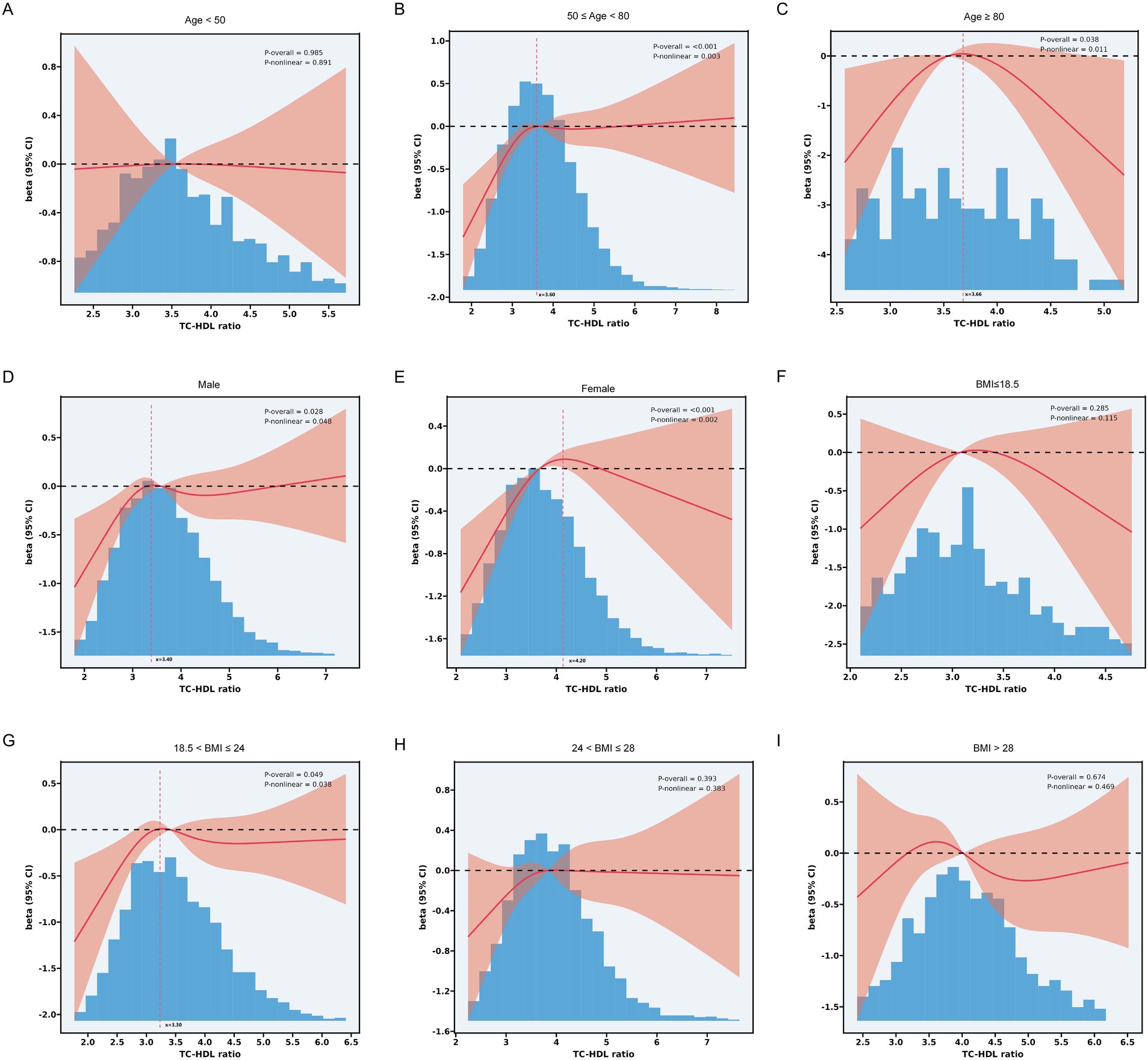
Figure 3. (A) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants aged < 50 years. (B) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants aged between 50-79 years. (C) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants aged ≥ 80. (D) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in male. (E) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in female. (F) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants whose BMI ≤ 18.5. (G) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants whose BMI between 18.5 and 24. (H) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants whose BMI between 24 and 28. (I) Subgroup RCS analysis between TC-HDL-C ratio and total cognition scores in participants whose BMI > 28.
3.5 Sensitivity analyses
To ensure the robustness of the findings, a series of sensitivity analyses was conducted:
1. Participants with cognition scores greater or less than twice the standard deviation were excluded. The results showed that the Q2 group remained linearly associated with cognition scores (Supplementary Table S3).
2. Robust regression confirmed the main findings (Q2 compared to Q1: β = 0.037, p = 0.013) (Supplementary Table S4).
3. Generalized additive models (GAM) supported the nonlinear relationships identified in the RCS analysis, showing similar trends (p for smooth term = 0.0303) (Supplementary Figure 1).
4 Discussion
The relationship between blood lipid levels and cognition is complex and has yielded conflicting findings across studies. While some research suggests that higher total cholesterol (TC) increases the risk of mild cognitive impairment (1, 18, 19), a double-blind, randomized, placebo-controlled trial reported that lowering lipid levels does not confer protective effects on cognition in older adults (20). Conversely, other studies have found that elevated serum total cholesterol is associated with better cognitive performance (21, 22). Recent evidence indicates that the relationship between plasma lipid levels and cognition may be nonlinear (3, 23, 24). Although high-density lipoprotein cholesterol (HDL-C) has traditionally been viewed as protective for cognitive health, emerging research suggests that excessive HDL-C levels might impair cognition (25–27). These discrepancies can largely be attributed to heterogeneity in study populations, variations in methods of assessing cognitive function, and differences in study designs. Together, these findings suggests the complexity of the relationship between lipid metabolism and cognition, highlighting it as a challenging topic for research.
Unconventional lipid parameters have gained attention for their potential to elucidate the relationship between lipid metabolism and cognition. High remnant cholesterol (RC) has been associated with poor cognitive outcomes, and lower RC/TC ratios may reduce the risk of cognitive impairment. In China, a cross-sectional study reported a U-shaped relationship between non-HDL-C levels and cognitive scores (28). However, longitudinal research has suggested no significant association between the TC-HDL-C ratio and dementia development (29). To our knowledge, the present study is the first to specifically investigate the association between the TC-HDL-C ratio and cognitive function in a Chinese population. Given the widespread use of the TC-HDL-C ratio as a predictor of metabolic disorders such as atherosclerosis, cardiovascular disease, and diabetes (12, 30), Its potential link to cognitive function is of interest. Notably, individuals with both Alzheimer’s disease and metabolic disorders exhibit worse cognitive performance than those without metabolic disorders (31). Additionally, diabetes has been shown to be associated with mild cognitive dysfunction, further supporting the connection between metabolic health and cognition (32). However, studies on the TC-HDL-C ratio as a lipid metabolic parameter in relation to cognitive function remain scarce.
Mechanistically, cholesterol plays a vital role in neuronal function. As an essential component of cell membranes, cholesterol is particularly critical in the central nervous system, where it is synthesized by astrocytes and transported to neurons. It is indispensable for processes such as myelination, synaptic plasticity, and neuronal signaling, all of which underpin cognitive function. Cholesterol deficiency in animal models has been shown to impair learning and memory, effects that can be reversed by cholesterol supplementation (33, 34). In aging and disease models, such as Huntington’s disease, increasing brain cholesterol levels has been linked to improved synaptic function and cognitive performance (35, 36). These findings suggest that higher TC levels may have protective effects on cognition, though this relationship is likely context-dependent and influenced by other metabolic factors.
Traditional views have categorized LDL as detrimental and HDL-C as beneficial, but emerging evidence challenges this binary perspective (37). High HDL-C levels, for instance, have been associated with increased fracture risk in older adults (38), and non-HDL-C levels have been positively correlated with global cognitive function (24). These findings prompt a reassessment of the relationships between different lipid fractions and cognition.
Our study, based on a large Chinese cohort, is the first to uncover a nonlinear relationship between the TC-HDL-C ratio and cognitive scores, identifying a turning point at a ratio of 3.50. Interestingly, the effects of the TC-HDL-C ratio differed by age group. Among middle-aged participants, cognitive performance plateaued at the turning point. In contrast, among older adults, cognitive performance worsened with increasing TC-HDL-C ratios beyond the turning point. This dose–response relationship was consistent across gender subgroup analyses, further supporting the robustness of our findings.
This study has several strengths. First, it is based on a large, community-based cohort of middle-aged and older adults, enhancing the generalizability of the findings to similar populations. Second, the use of advanced statistical methods, such as restricted cubic splines and sensitivity analyses, allowed us to robustly examine the nonlinear relationships between TC-HDL-C ratio and cognition.
However, several limitations should be acknowledged. As a cross-sectional study, we were unable to infer causality between the TC-HDL-C ratio and cognitive performance. Although we adjusted for numerous potential confounders, residual confounding remains a possibility. Many studies have revealed that changes in hormone levels will lead to changes in lipid metabolism profiles. Thyroid hormones affect lipid metabolism by regulating lipid synthesis and catabolism in the liver. Hypothyroidism usually leads to higher cholesterol levels, while hyperthyroidism may lead to lower cholesterol levels. In addition to this, thyroid hormones have the ability to affect cognition directly by influencing brain function. Thus, the lack of data on thyroid-related disorders would lead to a possible bias in our findings. Numerous studies has demonstrated that the menopause is associated with significant hormonal changes that can affect both lipid levels and cognitive performance (39). In this study, due to the lack of data on menopause, this leads us to conclude that there may be a potential bias among women with perimenopausal syndrome. Additionally, the study population was ethnically homogenous, limiting the generalizability of our findings to diverse populations. For people of different age groups, their cognitive ability thresholds are age-specific. Due to the lack of recognized thresholds for the cognitive scores used by CHARLS in the Chinese population, this may lead to either an overestimation or underestimation of the relationship between the TC-HDL-C ratio and cognition. Future longitudinal studies are needed to validate these findings and clarify the causal relationship between the TC-HDL-C ratio and cognitive outcomes. Research on more diverse populations is also necessary to enhance the applicability of these results to global populations.
5 Conclusion
Our study provides novel insights into the relationship between the TC-HDL-C ratio and cognitive function. We identified a significant nonlinear association, with a turning point at a TC-HDL-C ratio of 3.60. These findings emphasize the need to consider lipid metabolism in cognitive health assessments and suggest that maintaining an optimal TC-HDL-C ratio may help preserve cognitive function, particularly in aging populations. Further longitudinal and multicenter studies are warranted to confirm these findings and explore their broader implications for public health and clinical practice.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Peking University (Ethics number: IRB00001052–11015). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YZ: Formal analysis, Investigation, Methodology, Validation, Visualization, Writing – original draft. H-LX: Formal analysis, Investigation, Methodology, Validation, Writing – review & editing. X-LL: Formal analysis, Investigation, Methodology, Writing – review & editing. Z-TC: Validation, Writing – review & editing. Q-YY: Conceptualization, Project administration, Supervision, Writing – review & editing. Z-HZ: Conceptualization, Funding acquisition, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research, authorship, and/or publication of this article. This research was funded by the Fujian Provincial Key Clinical Specialties Construction Project (grant no. 2024015).
Acknowledgments
We are grateful to all those who have made suggestions for this work. We thank all the members of Movement Disorder lab.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnut.2025.1525348/full#supplementary-material
References
1. An, Y, Zhang, X, Wang, Y, Wang, Y, Liu, W, Wang, T, et al. Longitudinal and nonlinear relations of dietary and serum cholesterol in midlife with cognitive decline: results from EMCOA study. Mol Neurodegener. (2019) 14:51. doi: 10.1186/s13024-019-0353-1
2. Solomon, A, Kåreholt, I, Ngandu, T, Wolozin, B, Macdonald, SW, Winblad, B, et al. Serum total cholesterol, statins and cognition in non-demented elderly. Neurobiol Aging. (2009) 30:1006–9. doi: 10.1016/j.neurobiolaging.2007.09.012
3. Huan, S, Liu, M, Liu, Z, Gao, J, and Yin, G. Association between dietary and serum cholesterol and cognitive function among the U.S. elderly from NHANES 2011-2014. J Alzheimers Dis. (2023) 95:625–40. doi: 10.3233/JAD-230422
4. Yang, T, Liu, Y, Li, L, Zheng, Y, Wang, Y, Su, J, et al. Correlation between the triglyceride-to-high-density lipoprotein cholesterol ratio and other unconventional lipid parameters with the risk of prediabetes and type 2 diabetes in patients with coronary heart disease: a RCSCD-TCM study in China. Cardiovasc Diabetol. (2022) 21:93. doi: 10.1186/s12933-022-01531-7
5. Sheng, G, Kuang, M, Yang, R, Zhong, Y, Zhang, S, and Zou, Y. Evaluation of the value of conventional and unconventional lipid parameters for predicting the risk of diabetes in a non-diabetic population. J Transl Med. (2022) 20:266. doi: 10.1186/s12967-022-03470-z
6. Li, B, Zhou, X, Liu, Y, Zhang, Y, and Mu, Y. Remnant cholesterol is more strongly associated with arterial stiffness than traditional lipids and lipid ratios in the general Chinese population. J Atheroscler Thromb. (2024) 31:587–602. doi: 10.5551/jat.64146
7. Li, B, Liu, Y, Zhou, X, Chen, L, Yan, L, Tang, X, et al. Remnant cholesterol is more positively related to diabetes, prediabetes, and insulin resistance than conventional lipid parameters and lipid ratios: a multicenter, large sample survey. J Diabetes. (2024) 16:e13592. doi: 10.1111/1753-0407.13592
8. Pillai, JA, Bena, J, Bekris, L, Kodur, N, Kasumov, T, Leverenz, JB, et al. Alzheimer’s disease neuroimaging initiative. Metabolic syndrome biomarkers relate to rate of cognitive decline in MCI and dementia stages of Alzheimer's disease. Alzheimers Res Ther. (2023) 15:54. doi: 10.1186/s13195-023-01203-y
9. Criqui, MH, and Golomb, BA. Epidemiologic aspects of lipid abnormalities. Am J Med. (1998) 105:48S–57S. doi: 10.1016/s0002-9343(98)00212-5
10. Quispe, R, Elshazly, MB, Zhao, D, Toth, PP, Puri, R, Virani, SS, et al. Total cholesterol/HDL-cholesterol ratio discordance with LDL-cholesterol and non-HDL-cholesterol and incidence of atherosclerotic cardiovascular disease in primary prevention: the ARIC study. Eur J Prev Cardiol. (2020) 27:1597–605. doi: 10.1177/2047487319862401
11. Xiao, B, Cao, C, Han, Y, Yang, F, Hu, H, and Luo, J. A non-linear connection between the total cholesterol to high-density lipoprotein cholesterol ratio and stroke risk: a retrospective cohort study from the China health and retirement longitudinal study. Eur J Med Res. (2024) 29:175. doi: 10.1186/s40001-024-01769-9
12. Calling, S, Johansson, SE, Wolff, M, Sundquist, J, and Sundquist, K. Total cholesterol/HDL-C ratio versus non-HDL-C as predictors for ischemic heart disease: a 17-year follow-up study of women in southern Sweden. BMC Cardiovasc Disord. (2021) 21:163. doi: 10.1186/s12872-021-01971-1
13. Zhou, D, Liu, X, Lo, K, Huang, Y, and Feng, Y. The effect of total cholesterol/high-density lipoprotein cholesterol ratio on mortality risk in the general population. Front Endocrinol. (2022) 13:1012383. doi: 10.3389/fendo.2022.1012383
14. Zhao, Y, Yisong, H, Smith, JP, Strauss, J, and Yang, G. Cohort profile: the China health and retirement longitudinal study (CHARLS). Int J Epidemiol. (2014) 43:61–8. doi: 10.1093/ije/dys203
15. Zhao, Y, Strauss, J, Yang, G, Giles, J, Hu, P, Hu, Y, et al. China health and retirement longitudinal study: 2011–2012 national baseline user’s guide National School of Development, Peking University (2013). Available at: https://charls.pku.edu.cn/en/data/User2011.pdf
16. Lin, L, Cao, B, Chen, W, Li, J, Zhang, Y, and Guo, VY. Association of adverse childhood experiences and social isolation with later-life cognitive function among adults in China. JAMA Netw Open. (2022) 5:e2241714. doi: 10.1001/jamanetworkopen.2022.41714
17. Chen, X, Crimmins, E, Hu, PP, Kim, JK, Meng, Q, Strauss, J, et al. Venous blood-based biomarkers in the China health and retirement longitudinal study: rationale, design, and results from the 2015 wave. Am J Epidemiol. (2019) 188:1871–7. doi: 10.1093/aje/kwz170
18. Guo, Y, Li, P, Ma, X, Huang, X, Liu, Z, Ren, X, et al. Association of circulating cholesterol level with cognitive function and mild cognitive impairment in the elderly: a community-based population study. Curr Alzheimer Res. (2020) 17:556–65. doi: 10.2174/1567205017666200810165758
19. He, Q, Li, Q, Zhao, J, Wu, T, Ji, L, Huang, G, et al. Relationship between plasma lipids and mild cognitive impairment in the elderly Chinese: a case-control study. Lipids Health Dis. (2016) 15:146. doi: 10.1186/s12944-016-0320-6
20. Bosch, J, O'Donnell, M, Swaminathan, B, Lonn, EM, Sharma, M, Dagenais, G, et al. Effects of blood pressure and lipid lowering on cognition: results from the HOPE-3 study. Neurology. (2019) 15:e1435–46. doi: 10.1212/WNL.0000000000007174
21. Leritz, EC, McGlinchey, RE, Salat, DH, and Milberg, WP. Elevated levels of serum cholesterol are associated with better performance on tasks of episodic memory. Metab Brain Dis. (2016) 31:465–73. doi: 10.1007/s11011-016-9797-y
22. Ma, C, Yin, Z, Zhu, P, Luo, J, Shi, X, and Gao, X. Blood cholesterol in late-life and cognitive decline: a longitudinal study of the Chinese elderly. Mol Neurodegener. (2017) 12:24. doi: 10.1186/s13024-017-0167-y
23. Xie, YY, Zhao, L, Gao, LJ, Xu, RX, Gao, Y, Dou, KF, et al. Association between remnant cholesterol and verbal learning and memory function in the elderly in the US. Lipids Health Dis. (2022) 21:120. doi: 10.1186/s12944-022-01729-4
24. Zhang, Q, Zhang, M, Chen, Y, Cao, Y, and Dong, G. Nonlinear relationship of non-high-density lipoprotein cholesterol and cognitive function in American elders: a cross-sectional NHANES study (2011-2014). J Alzheimers Dis. (2022) 86:125–34. doi: 10.3233/JAD-215250
25. Zhou, F, Deng, W, Ding, D, Zhao, Q, Liang, X, Wang, F, et al. High low-density lipoprotein cholesterol inversely relates to dementia in community-dwelling older adults: the Shanghai aging study. Front Neurol. (2018) 9:952. doi: 10.3389/fneur.2018.00952
26. Hussain, SM, Robb, C, Tonkin, AM, Lacaze, P, Chong, TT, Beilin, LJ, et al. Association of plasma high-density lipoprotein cholesterol level with risk of incident dementia: a cohort study of healthy older adults. Lancet Reg Health West Pac. (2023) 43:100963. doi: 10.1016/j.lanwpc.2023.100963
27. Huang, H, Yang, B, Yu, R, Ouyang, W, Tong, J, and Le, Y. Very high high-density lipoprotein cholesterol may be associated with higher risk of cognitive impairment in older adults. Nutr J. (2024) 23:79. doi: 10.1186/s12937-024-00983-9
28. Li, L, Zhuang, L, Xu, Z, Jiang, L, Zhai, Y, Liu, D, et al. U-shaped relationship between non-high-density lipoprotein cholesterol and cognitive impairment in Chinese middle-aged and elderly: a cross-sectional study. BMC Public Health. (2024) 24:1624. doi: 10.1186/s12889-024-19164-8
29. Beydoun, MA, Beason-Held, LL, Kitner-Triolo, MH, Beydoun, HA, Ferrucci, L, Resnick, SM, et al. Statins and serum cholesterol's associations with incident dementia and mild cognitive impairment. J Epidemiol Community Health. (2011) 65:949–57. doi: 10.1136/jech.2009.100826
30. Jung, HW, Hong, SP, and Kim, KS. Comparison of apolipoprotein B/A1 ratio, TC/HDL-C, and lipoprotein (a) for predicting outcomes after PCI. PLoS One. (2021) 16:e0254677. doi: 10.1371/journal.pone.0254677
31. Hishikawa, N, Fukui, Y, Sato, K, Kono, S, Yamashita, T, Ohta, Y, et al. Cognitive and affective functions in Alzheimer's disease patients with metabolic syndrome. Eur J Neurol. (2016) 23:339–45. doi: 10.1111/ene.12845
32. Casagrande, SS, Lee, C, Stoeckel, LE, Menke, A, and Cowie, CC. Cognitive function among older adults with diabetes and prediabetes, NHANES 2011-2014. Diabetes Res Clin Pract. (2021) 178:108939. doi: 10.1016/j.diabres.2021.108939
33. Micale, V, Scapagnini, G, Colombrita, C, Mazzola, C, Alkon, DL, and Drago, F. Behavioral effects of dietary cholesterol in rats tested in experimental models of mild stress and cognition tasks. Eur Neuropsychopharmacol. (2008) 18:462–71. doi: 10.1016/j.euroneuro.2007.11.006
34. Dufour, F, Liu, QY, Gusev, P, Alkon, D, and Atzori, M. Cholesterol-enriched diet affects spatial learning and synaptic function in hippocampal synapses. Brain Res. (2006) 1103:88–98. doi: 10.1016/j.brainres.2006.05.086
35. Valenza, M, Chen, JY, Di Paolo, E, Ruozi, B, Belletti, D, Ferrari Bardile, C, et al. Cholesterol-loaded nanoparticles ameliorate synaptic and cognitive function in Huntington's disease mice. EMBO Mol Med. (2015) 7:1547–64. doi: 10.15252/emmm.201505413
36. Birolini, G, Valenza, M, Ottonelli, I, Talpo, F, Minoli, L, Cappelleri, A, et al. Chronic cholesterol administration to the brain supports complete and long-lasting cognitive and motor amelioration in Huntington's disease. Pharmacol Res. (2023) 194:106823. doi: 10.1016/j.phrs.2023.106823
37. Olsson, AG, Angelin, B, Assmann, G, Binder, CJ, Björkhem, I, Cedazo-Minguez, A, et al. Can LDL cholesterol be too low? Possible risks of extremely low levels. J Intern Med. (2017) 281:534–53. doi: 10.1111/joim.12614
38. Hussain, SM, Ebeling, PR, Barker, AL, Beilin, LJ, Tonkin, AM, and McNeil, JJ. Association of plasma high-density lipoprotein cholesterol level with risk of fractures in healthy older adults. JAMA Cardiol. (2023) 8:268–72. doi: 10.1001/jamacardio.2022.5124
Keywords: cholesterol, cognition ability, CHARLS, TC-HDL-C ratio, middle-aged, elderly
Citation: Zhou Y, Xu H-L, Lin X-L, Chen Z-T, Ye Q-Y and Zhao Z-H (2025) The nonlinear association of ratio of total cholesterol to high density lipoprotein with cognition ability: evidence from a community cohort in China. Front. Nutr. 12:1525348. doi: 10.3389/fnut.2025.1525348
Edited by:
Luciana Mosca, Sapienza University of Rome, ItalyReviewed by:
Eleonora Poggiogalle, Sapienza University of Rome, ItalyMario Fontana, Sapienza University of Rome, Italy
Copyright © 2025 Zhou, Xu, Lin, Chen, Ye and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qin-Yong Ye, dW5pb25xeXllOEBmam11LmVkdS5jbg==; Zhen-Hua Zhao, OTIwMTU1MTA4N0Bmam11LmVkdS5jbg==
†These authors have contributed equally to this work
 Yi Zhou
Yi Zhou Hao-Ling Xu3,4†
Hao-Ling Xu3,4† Zhi-Ting Chen
Zhi-Ting Chen Qin-Yong Ye
Qin-Yong Ye Zhen-Hua Zhao
Zhen-Hua Zhao